Topics to Review for fundamentals final ATI during Adult Health 1.
Document Content and Description Below
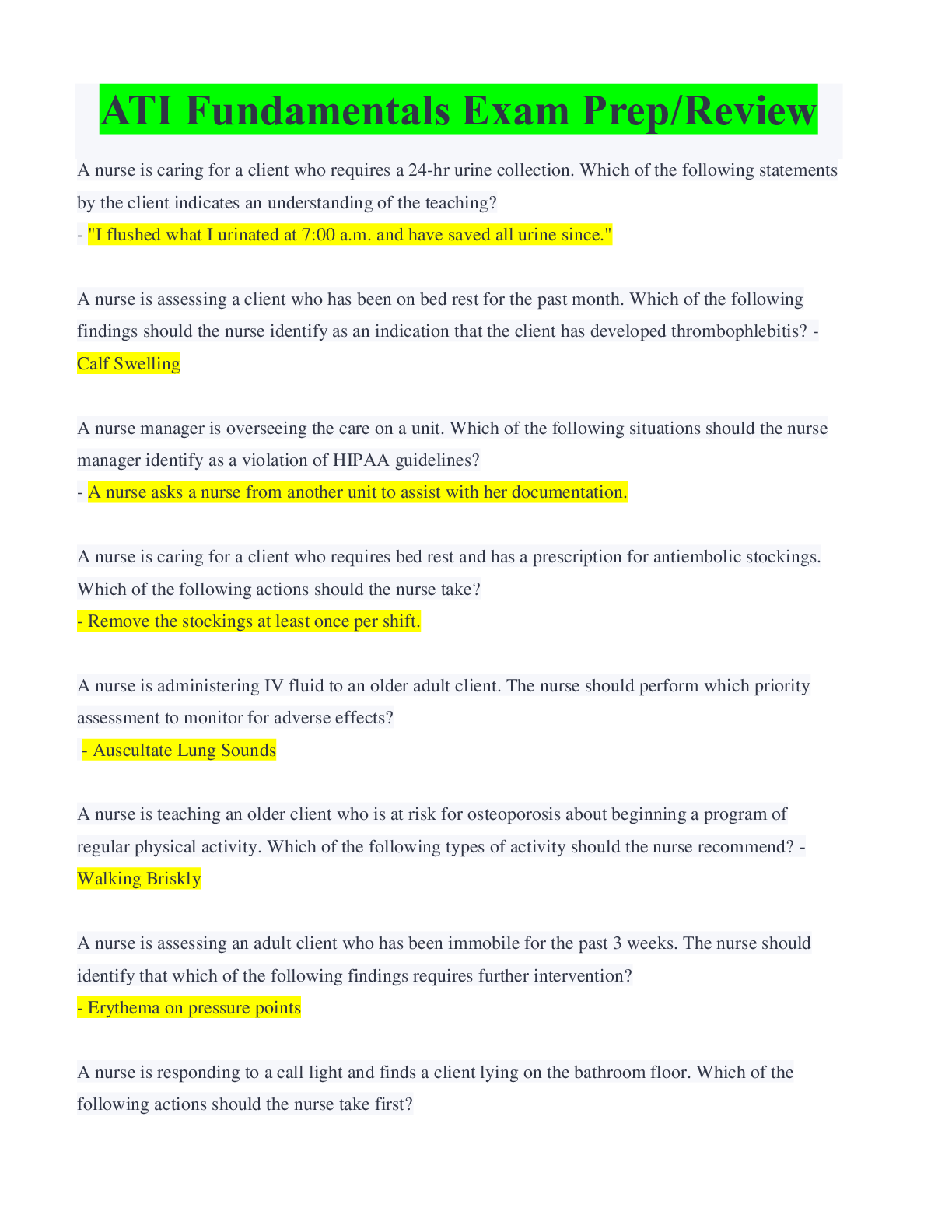
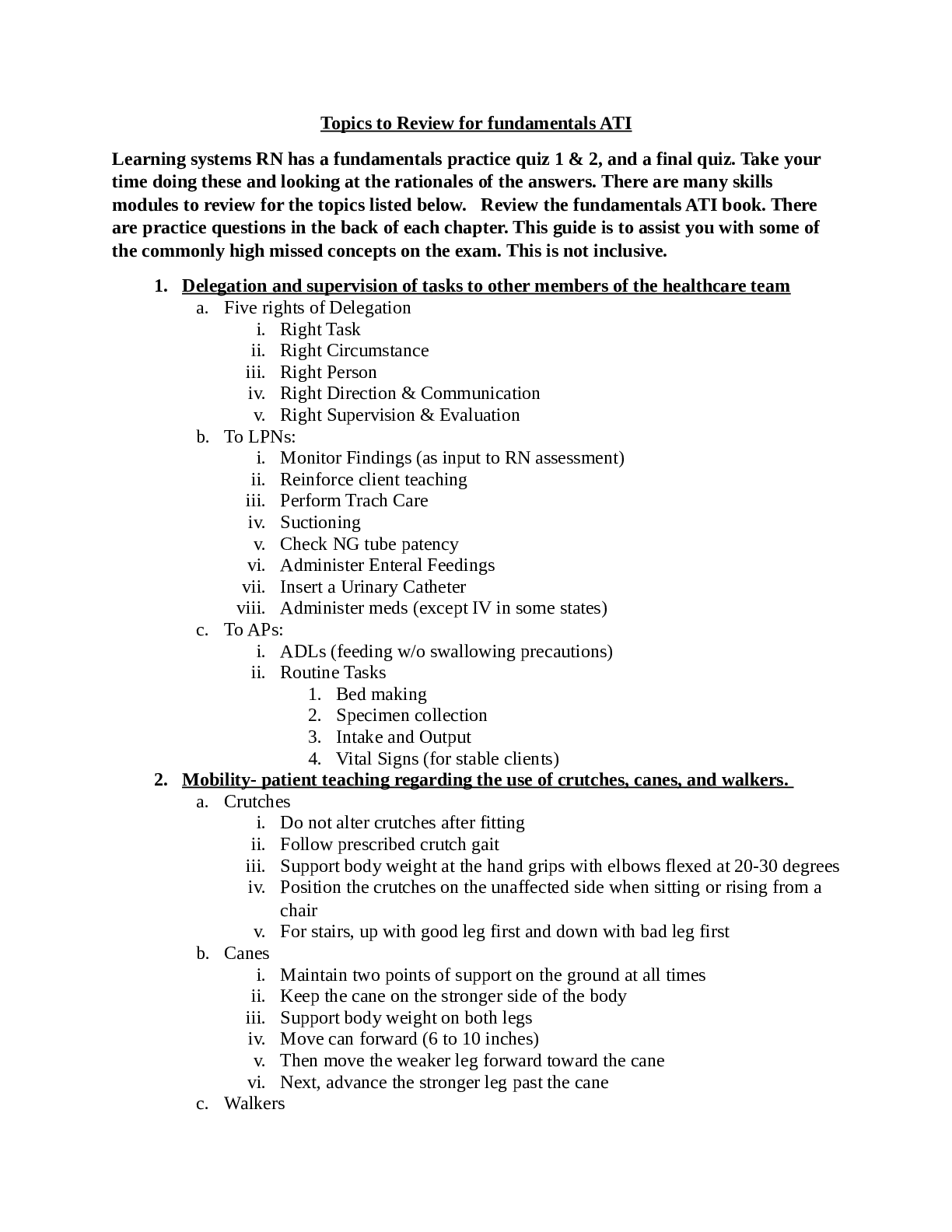
Learning systems RN has a fundamentals practice quiz 1 & 2, and a final quiz. Take your time doing these and looking at the rationales of the answers. There are many skills modules to review for the... topics listed below. Review the fundamentals ATI book. There are practice questions in the back of each chapter. This guide is to assist you with some of the commonly high missed concepts on the exam. This is not inclusive. 1. Delegation and supervision of tasks to other members of the healthcare team a. Five rights of Delegation i. Right Task ii. Right Circumstance iii. Right Person iv. Right Direction & Communication v. Right Supervision & Evaluation b. To LPNs: i. Monitor Findings (as input to RN assessment) ii. Reinforce client teaching iii. Perform Trach Care iv. Suctioning v. Check NG tube patency vi. Administer Enteral Feedings vii. Insert a Urinary Catheter viii. Administer meds (except IV in some states) c. To APs: i. ADLs (feeding w/o swallowing precautions) ii. Routine Tasks 1. Bed making 2. Specimen collection 3. Intake and Output 4. Vital Signs (for stable clients) 2. Mobility- patient teaching regarding the use of crutches, canes, and walkers. a. Crutches i. Do not alter crutches after fitting ii. Follow prescribed crutch gait iii. Support body weight at the hand grips with elbows flexed at 20-30 degrees iv. Position the crutches on the unaffected side when sitting or rising from a chair v. For stairs, up with good leg first and down with bad leg first b. Canes i. Maintain two points of support on the ground at all times ii. Keep the cane on the stronger side of the body iii. Support body weight on both legs iv. Move can forward (6 to 10 inches) v. Then move the weaker leg forward toward the cane vi. Next, advance the stronger leg past the cane c. Walkers i. A walker is a lightweight, movable device that stands about waist high and consists of a metal frame with handgrips, four widely placed sturdy legs, and one open side (Figure 39-12). Because it has a wide base of support, the walker provides great stability and security during walking. A walker can be used by a patient who is weak or has problems with balance. Walkers with wheels are useful for patients who have difficulty lifting and advancing the walker as they walk because of limited balance or endurance. However, the disadvantage is that the walker can roll forward when weight is applied. You measure walkers by having patients relax their arms at the side of their body and stand up straight. The top of the walker should line up with the crease on the inside of the wrist. Elbows should be flexed about 15 to 30 degrees when standing inside the walker, with hands on the handgrips. A patient holds the handgrips on the upper bars, takes a step, moves the walker forward, and takes another step. A walker requires a patient to lift the device up and forward. Teach patients how to use walkers safely and avoid risk of falling. 3. Preventative interventions for complications of immobility a. Complications of Immobility i. Integumentary 1. Increased pressure on skin 2. Decreased Circulation ii. Respiratory 1. Decreased respiratory movement 2. Stasis of secretions, resulting in atelectasis & hypostatic pneumonia 3. Decreased cough response iii. Cardiovascular 1. Orthostatic hypotension 2. Less fluid volume 3. Decreased CO 4. Increased oxygenation requirement/risk of thrombus iv. Metabolic 1. Decreased protein, basal met rate, appetite 2. Loss of weight 3. Alterations in calcium, fluid, and electrolytes 4. Decreased urine elimination resulting in renal calculi v. Elimination 1. Urinary stasis 2. Decreased fluid intake 3. Decrease peristalsis 4. Constipation, fecal impaction, then diarrhea vi. Musculoskeletal 1. Decrease strength, mass, endurance 2. Impaired balance 3. Osteoporosis 4. Contractures, foot drop, altered joint mobility vii. Neurological 1. Altered sensory perception 2. Ineffective coping 3. Changes in emotional status: depression, anxiety 4. Behavior changes: withdrawal, passivity b. Prevention of the Complications i. Turn patient every 1 to 2 hours, teach clients to turn themselves every 15 minutes, sit in chair up to 1 hour (changing weight every 15 minutes) ii. Monitor nutritional intake iii. Provide skin and perineal care iv. Auscultate lungs every 2 hours v. Use incentive spirometer vi. Drink 2 k mL everyday vii. Auscultate heart sounds, do vitals, check apical/peripheral pulses viii. Palpate for edema, measure circumference of both calves and thighs ix. Do ROM, use SCDs/TED hose, use stool softener x. Provide a high calorie, high protein diet xi. Monitor I and Os xii. Teach bladder and bowel training xiii. Cluster care to promote a proper sleep-wake cycle, xiv. Maintain orientation of time xv. Involve clients in daily care xvi. Provide stimuli (books, magazines, etc.) xvii. Help clients maintain body image 4. Diets- foods on each type including measures to prevent aspiration. a. Patients with dysphagia are at risk for aspiration and need more help with feeding and swallowing. A speech-language pathologist (SLP) identifies patients at risk and provides recommendations for therapy. Provide a 30-minute rest period before eating and position the patient in an upright, seated position in a chair or raise the head of the bed to 90 degrees. Have the patient flex the head slightly to a chin-down position to help prevent aspiration. If the patient has unilateral weakness, teach him or her and the caregiver to place food in the stronger side of the mouth. With the help of an SLP, determine the viscosity of foods that the patient tolerates best using trials of different consistencies of foods and fluids. Thicker fluids are generally easier to swallow. The American Dietetic Association published the National Dysphagia Diet Task Force National Dysphagia Diet in 2010 to provide uniformity of diets provided to patients with dysphagia. There are four levels of diet: dysphagia puree, dysphagia mechanically altered, dysphagia advanced, and regular. The four levels of liquid include thin liquids (low viscosity), nectar like liquids (medium viscosity), honey like liquids (viscosity of honey), and spoon-thick liquids (viscosity of pudding) (NDDTF, 2010). [Show More]
Last updated: 1 year ago
Preview 1 out of 27 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 07, 2021
Number of pages
27
Written in
Additional information
This document has been written for:
Uploaded
Sep 07, 2021
Downloads
0
Views
36


.png)
.png)
 (1).png)