*NURSING > CASE STUDY > NR 603 Week 2 Case Discussion: Pulmonary – Part 1 (GRADED) (All)
NR 603 Week 2 Case Discussion: Pulmonary – Part 1 (GRADED)
Document Content and Description Below
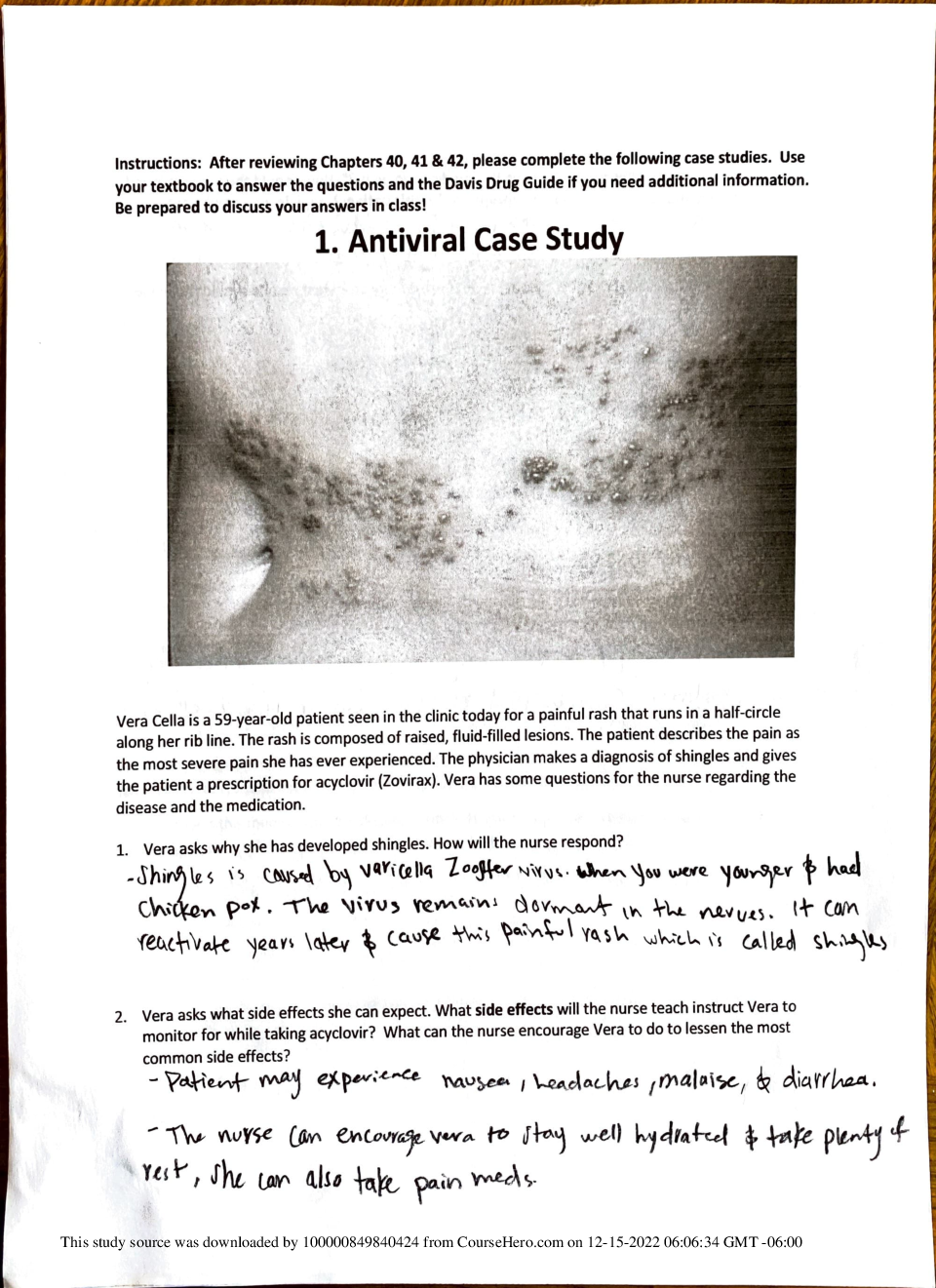
NR 603 Week 2 Case Discussion: Pulmonary – Part 1 (GRADED) 1. What is your primary diagnosis for Michelle given the pattern of occurrence of symptoms, exam results, and recent history? Include ... the rationale and a reference for your diagnoses. 2. What is your first-line treatment plan for Michelle including medications, labs, education, referrals, and follow-up? Identify the drug class of each medication you prescribe and exactly what symptom it is targeted to address. 3. Address Michelle's request for an antibiotic Dr. Deering and class, Primary Diagnosis: Based on the presenting symptoms and assessment findings within this case study, the primary diagnosis for Michelle is occupational asthma. Occupational asthma (OA), or work-related asthma (WRA), is the most common occupational lung disease in the United States (Global Initiative for Asthma [GINA], 2019). OA results from exposure to a stimulus, such as dust, grain, flour, latex, insects, and mold, found in the workplace environment (Jolly et al., 2015). Exposure to these types of allergens causes symptoms of asthma, including coughing, wheezing, chest tightness, and shortness of breath (Dao & Bernstein, 2018). Nasal congestion and eye irritation can also occur as a result of OA. In this case study, Michelle presents with shortness of breath while she is at work. When she is not at work, she has relief and no longer experiences difficulty breathing. Even on weekends when she is at home, she denies respiratory symptoms. Individuals diagnosed with OA tend to have more symptomatic days and exacerbations of asthma symptoms while they are exposed daily to a particular allergen in the workplace. Since Michelle has a history of seasonal allergies, she is at an increased risk of developing occupational asthma. One of the main risk factors for occupational asthma is atopy, which is characterized by a sensitivity to allergens (Dao & Bernstein, 2018). Therefore, individuals with atopy often have seasonal allergies, allergic skin rashes, and food allergies. In this case study, Michelle has a history of seasonal allergies and has seen an allergy specialist. Upon physical examination, Michelle was noted to have inspiratory and expiratory wheezing, thin exudates to bilateral nares, and a pale, boggy mucosa. These findings are indicative of inflammation within the respiratory mucosa from the irritant. The thin exudates within the nares are related to allergic rhinitis, which is an inflammation caused by the immune system’s response to an allergen (Pralong & Cartier, 2017). The wheezing is a result of airway narrowing from bronchoconstriction or mucosal edema (Pralong & Cartier, 2017). Michelle’s respiratory symptoms occur within a few hours of working in the bakery. She starts every morning baking bread and pastries for the day as a Baker’s assistant. Therefore, it can be safe to assume that Michelle is experiencing OA due to the type of flour used at the bakery. Even though staying away from the irritant is the best way to improve outcomes, we must initiate some tests to properly diagnose her before taking individuals away from work. In the office, Michelle had a pulmonary function test (PFT) performed. Airflow obstructions occurs when FEV1/FVC is less than 70%. Therefore, the result of FEV1/FVC 60% before the bronchodilator is indicative of airflow obstruction. After the bronchodilator was given, there was an increase of 15% in FEV1/FVC. This is considered an appropriate bronchodilator response. The existence of airflow obstruction coupled with a positive bronchodilator response is suggestive of asthma diagnosis (Pralong & Cartier, 2017). Currently, Michelle experiences symptoms of shortness of breath and wheezing five days a week within a few hours of working in the bakery. She denies exacerbations at night, and is able to sleep through the night with no issues. Based on Michelle’s frequency of symptoms and PFT results, she is considered a mild persistent asthmatic. First-line Treatment Plan: The treatment for occupational asthma is the same treatment for asthma. For mild persistent asthma, inhaled corticosteroids (ICSs) are the preferred first line medication treatment (GINA, 2019). I would prescribe fluticasone propionate 88 mcg inhaled BID. Low dose ICS target the small airways and reduce inflammation by decreasing activity of inflammatory cells and mediators (Hollier, 2018). The reduction of inflammation will help decrease mucosal edema and mucus production that cause rhinorrhea, cough, wheeze, and shortness of breath (Hollier, 2018). At the same time, a short-acting bronchodilator, such as albuterol, should be prescribed to treat exacerbations. I would prescribe albuterol 2 puffs every 4-6 hours as needed for shortness of breath. Short-acting bronchodilators are considered rescue inhalers, which help dilate the bronchi in the lungs and increase airflow (GINA, 2019). Widening the airways will help relieve breathing difficulties. Lastly, I would prescribe a leukotriene blocker, such as Singulair 10 mg daily, to prevent asthma symptoms and manage seasonal allergies. I would educate Michelle to discontinue her current use of Zyrtec. Leukotriene antagonists block the release of mast cells responsible for airway edema and inflammation (Hollier, 2018). This class of medication will help reduce wheezing and runny nose from the inflammation. While staying away from the irritant will drastically improve asthmatic symptoms, it may be difficult for Michelle to quit this current job since she is temporarily working at the bakery for financial reasons. Therefore, I would refer her to an allergist to have a skin prick testing done. According to the American College of Occupational and Environmental Medicine (Jolly et al., 2015), a skin prick testing is strongly recommended for diagnostic testing for occupational asthma. Cereal flour, particularly wheat flour, is considered one of the most common types of occupational asthma (Jolly et al., 2015). While there is a high probability that the flour used in the bakery is the allergen, a skin prick test can help identify other allergens that may play a role in Michelle’s occupational asthma. This includes rye, barley, rice, and oats. House dust mites, storage mites, and fungus should also be checked (Jolly et al., 2015). It is important to educate Michelle on ways to manage occupational asthma. Avoiding triggers is the best way to treat OA. In this case, staying away from the type of flour used in baking breads and pastries will help alleviate asthmatic symptoms. If this is not possible due to financial reasons, taking medications to prevent symptoms and treating acute asthma episodes are important educational topics. The goal of asthma self-management is to control and prevent asthma attacks (Pralong & Cartier, 2017). Therefore, I would educate Michelle on a personalized asthma action plan. I would include education on how to take each medication to prevent asthma episodes, as well as to treat acute asthma attacks. I would educate Michelle on when to use rescue inhalers and the symptoms associated with an acute asthma attack. A return demonstration of inhaler use is imperative for Michelle since this is her first time using inhalers. Side effects of ICS, leukotriene blockers, and short-acting bronchodilators should be educated as well. Side effects include: heart palpitations, dry mouth, headaches, nausea, vomiting, cough, and stomach pain (Hollier, 2018). I would like to follow-up with Michelle in 4 weeks to evaluate her response to treatment. If she is able to control symptoms during the 4 week follow-up, I would then follow-up with her in three months. It is important for Michelle to record asthma control. This entails whether she experiences less asthmatic symptoms, quick relief from rescue inhalers, little to no side effects of asthma medication, and no interruption in daily activities. However, if she experiences shortness of breath unrelieved by short-acting bronchodilators or chest pain, she will need to be instructed to go to the emergency room. If the frequency and severity of asthma increases within the next two weeks, I would instruct her to return to the office and I will reassess her and evaluate for additional treatment. For example, if Michelle reports using rescue inhalers more than 2 times a week, I would need to add a long-acting inhaled bronchodilator to better manage her asthma symptoms. If Michelle’s symptoms are very severe to the point where she cannot perform her daily activities or complete her job duties, the discussion of completely removing herself from the workplace must be encouraged. Addressing Michelle’s Request for Antibiotics: While antibiotics are one of the greatest advances in medicine, overprescribing has certainly been an issue due to increased bacterial resistance. Like many people, Michelle feels that antibiotics have helped treat her symptoms before. Therefore, it is no surprise that she would request to have another antibiotic prescription. In this case, I would tell her: “Michelle, antibiotics would not be an appropriate treatment in your case. Even though it may have made you feel better when you went to the urgent care a few weeks ago, this is an allergic response to something in your current workplace. Antibiotics are prescribed to treat bacterial infections. Even for common colds, which are usually viral, we do not prescribe antibiotics because they have no effect on viruses. Overuse of antibiotics can actually make bacteria stronger and resistant to medications. This makes it harder for us to treat any future bacterial infections if they are resistant. In your particular case, your asthma symptoms are triggered by an allergen, not from bacteria. Therefore, our focus should be improving your asthma symptoms through medication and preventing future asthma attacks.” In Michelle’s case, it is important to explain to her that this is an allergic response. Therefore, an antibiotic is not indicated. The treatment for asthma should be focused on alleviating symptoms, avoiding triggers, and preventing the progression of asthma. References Dao, A., & Bernstein, D.I. (2018). Occupational exposure and asthma. Annals of Allergy, Asthma, & Immunology, 120(5), 468-475. doi:10.1016/j.anai.2018.03.026 Global Initiative for Asthma. (2019). Pocket guide for asthma management and prevention. Retrieved from https://ginasthma.org/wp-content/uploads/2019/04/GINA-2019-main-Pocket- Guide-wms.pdf Hollier, A. (2018). Clinical guidelines in primary care. Lafayette, LA: Advanced Practice Education Associates, Inc. Jolly, A.T., Klees, J.E., Pacheco, K.A., Guidotti, T.L., Kipen, H.M., Biggs, J.J., . . . Harber, P. (2015). Occupational/work-related asthma medical treatment guideline. American College of Occupational and Environmental Medicine, 57(10), 121-128. Pralong, J.A., & Cartier, A. (2017). Review of diagnostic challenges in occupational asthma. Current Allergy and Asthma Reports, 17(1), 1-7. doi:10.1007/s11882-017-0676-3 1. Determine appropriate treatment plan for Michelle. Discuss medications, doses, Durable Medical Equipment, and any testing, and apply these directly to her case. Provide your rationale with evidence. 2. Decide whether she is safe to return home, include any prescriptions, or if a referral to a higher level of care is required. Discuss the criteria used to make your decision, how a referral is made and defend your position. 3. Discuss relevant education and follow up plan. Dr. Deering and class, Having influenza is problematic for someone like Michelle who has asthma. This is because people with asthma have sensitive airways and a viral infection can cause more inflammation of the airways. A viral infection in the lungs can trigger asthma attacks and worsen asthma symptoms (Centers for Disease Control and Prevention [CDC], 2018). Even though asthma is not considered a risk factor for getting influenza, people with asthma are more likely to develop respiratory complications after getting sick with the flu than people who do not have asthma. Treatment Plan: With Influenza A, there are both non-pharmacological and pharmacological treatment plans for Michelle. Since the onset of symptoms began within two days, I would prescribe oseltamivir (Tamiflu) 75 mg twice a day for five days. Oseltamivir is an antiviral medication used to treat flu symptoms (Uyeki et al., 2018). Antiviral drugs can lessen fever and other symptoms and shorten the time that Michelle is sick. They can also prevent serious flu complications, such as pneumonia. With her history of asthma, her respiratory symptoms (cough, wheezing, and shortness of breath) may worsen when there is a viral infection (Uyeki et al., 2018). I would also prescribe Prednisone 40 mg daily for five days. The Infectious Disease Society of America guidelines recommend oral corticosteroids for individuals with asthma exacerbations. Prednisone is a corticosteroid used to treat inflammation and help minimize the severity of flu- like symptoms (Uyeki et al., 2018). It is also important that she continues to take her albuterol 2 puffs every 4-6 hours as needed, fluticasone propionate 88 mcg inhaled BID, and Singulair 10 mg daily (Global Initiative for Asthma [GINA], 2019). These asthma medications will help improve her symptoms that are triggered by the viral infection. It is important that Michelle has adequate medical equipment to treat her flu-like symptoms and exacerbated asthma symptoms, such as inhalers. If she has close contact with other people in the household, Michelle is encouraged to have a standard face mask to avoid spreading the viral infection. At this time, Michelle does not require further testing. A chest x-ray is not indicated at this time because she does not exhibit symptoms consistent with pneumonia (Uyeki et al., 2018). This would include greenish or yellow sputum, chills, night sweats, nausea, vomiting, or shallow breathing. Since Michelle currently has a fever, it is clear that she has some type of infectious process. She is also hemodynamically stable. Therefore, a CBC is not required unless we need to rule out sepsis. The plan to treat her with antivirals would not change based on a CBC. Influenza is primarily diagnosed through clinical presentation (symptoms of sudden onset of fever, dry cough, and rhinorrhea) and history taking (the presence of Influenza A in the workplace) (CDC, 2018). In this particular case study, Michelle also has a positive swab test for Influenza A. When to return home and referral for high level of care: Influenza is more severe than a common cold and can worsen other health problems, such as asthma in Michelle’s case. Before I decide whether Michelle is safe to return home, I would perform a pulmonary function test (PFT) test and assess the improvement of her breathing after a bronchodilator. If she has a positive bronchodilator response, I would have her wait in the office and re-assess her in thirty minutes to see if her breathing improves. Since she is able to speak and only has shortness of breath with exertion, it is safe to say that she does not require emergent treatment at this time (Uyeki et al., 2018). Therefore, Michelle is safe to return home and I would advise Michelle to minimize contact with other people, which means staying at home and away from work. Michelle is still considered contagious up to 24 hours even after the fever resolves (CDC, 2018). I would advise Michelle to stay home for about 3-5 days. At this point, a referral for a higher level of care is not required. Influenza is often a self-limiting illness for healthy individuals (CDC, 2018). Symptom management is important in recovering from the flu. However, it is important to tell Michelle that her history of asthma may increase the risk of developing flu complications. Therefore, she must go to the emergency room if she develops extreme shortness of breath unrelieved by albuterol, persistent chest pain, severe muscle pain, severe vomiting, or fever/cough that improves but then worsens (Uyeki et al., 2018). Education and Follow-up Plan: Providing education for Michelle is important to alleviate discomforting symptoms associated with influenza A. Michelle should be educated on how to take oseltamivir, as well as side effects. Common side effects of oseltamivir include diarrhea, nausea, vomiting, dizziness, and headaches (Sexton, 2018). While taking oseltamivir, she is encouraged to try nonpharmacologic management for symptom management. This includes saline nose drops for nasal congestion, increase fluid intake, rest, hand washing, and humidified air to prevent drying of respiratory secretions (CDC, 2018). Side effects of systemic corticosteroids, which include sleep disturbance, GERD, and mood changes, should also be educated (GINA, 2019). Michelle can also take over-the-counter Ibuprofen (400 mg PO every 4-6 hours) or Tylenol (650 mg PO every 6 hours) to help reduce fever and relieve body aches. She can also take over-the-counter Dextromethorphan (Robitussin DM) 10 mL PO every 4 hours PRN cough. As previously mentioned, Michelle’s history of asthma may increase the risk of developing flu complications. She must be educated on signs and symptoms that require immediate attention. This includes difficulty breathing, persistent chest pain, severe vomiting, and fever/cough that improves but returns (GINA, 2019). Michelle should also be encouraged to return to the office if symptoms worsen or do not improve within five days. If Michelle experiences a productive cough with green-colored sputum, chills, sweating, or sharp chest pains when breathing in, I would be concerned about Michelle developing pneumonia. Antibiotics would need to be prescribed in the event of bacterial pneumonia. Education for future prevention of the flu is also essential for Michelle. Now that Michelle will understand that asthma can worsen with viral infections, Michelle should be educated on getting annual flu shots when available. For individuals with asthma, the injectable flu shot is preferred over the nasal spray vaccine because the nasal spray can potentially trigger asthma symptoms (Sexton, 2018). References Centers for Disease Control and Prevention. (2018). What you should know about influenza. Retrieved from https://www.cdc.gov/flu/pdf/freeresources/updated/antiviral-factsheet- updated.pdf Global Initiative for Asthma. (2019). Difficult-to-treat and severe asthma in adolescent and adult patients: Diagnosis and management https://ginasthma.org/wp-content/uploads/2019/04/GINA- Severe-asthma-Pocket-Guide-v2.0-wms-1.pdf Sexton, S. (2018). Influenza vaccination recommendations for 2018-2019: Updates from ACIP. American Family Physician, 98(8), 541-542. Uyeki, T. M., Bernstein, H. H., Bradley, J. S., Englund, J. A., File Jr, T. M., Fry, A. M., . . . Ison, M. G. (2018). Clinical practice guidelines by the Infectious Diseases Society of America: 2018 update on diagnosis, treatment, chemoprophylaxis, and institutional outbreak management of seasonal influenza. Clinical Infectious Diseases, 68(6), e1-e47. doi:10.1093/cid/ciy866 Hi Brittany, Thanks for starting us off with this week’s discussion! You provided details to support your primary diagnosis of mild persistent asthma. It is evident that Michelle has many risk factors associated with asthma, including history of seasonal allergies, former smoker, and irritant exposure. She also presents clinically with intermittent shortness of breath, wheezing, and chest tightness. Lastly, her symptoms do not occur daily since she experiences them five days out of the week while she is at work. With the information provided in this case study, I can see why you did not establish work-related asthma, or occupational asthma, as your primary diagnosis. To confirm a diagnosis of occupational asthma, diagnostic tests are indicated, such as spirometry, immunologic testing, and peak expiratory flow comparison between work and off work (Pralong & Cartier, 2017). While a series of pulmonary function testing (PFT) can confirm a diagnosis of asthma, it cannot diagnose occupational asthma. Your educational topics for Michelle were appropriate. Thoroughly explaining how to use an inhaler is beneficial for Michelle to receive the adequate dosage. An inhaled spacer can help control the intake of the medication. The spacer also helps reduce the amount of medication that stays in the throat or tongue after breathing in a dose (Plaza, Giner, Rodrigo, Dolovich, & Sanchis, 2018). However, Michelle would need to be reminded to thoroughly clean the device to avoid an infection or irritation of your mouth from residual medication or moisture (Plaza et al., 2018). A return demonstration on how to use an inhaler in the office will ensure that Michelle understands how to use an inhaler for the first time. Lastly, reminding Michelle to receive annual flu shots is also important. Individuals with asthma are at an increased risk for influenza because lung function can be extremely compromised. Viral infections can trigger and worsen asthma symptoms. Unfortunately, people with asthma are more prone to developing respiratory complications after viral infections than people who do not have asthma (Greenhawt, 2014). Therefore, annual influenza vaccination remains the most effective way to prevent contracting influenza. When considering the influenza vaccine for asthmatics, the injectable flu shot is preferred over the nasal spray vaccine because the nasal spray can potentially trigger asthma symptoms (Greenhawt, 2014). References Greenhawt, M. (2014). Influenza vaccination in asthmatic patients. The Journal of Allergy and Clinical Immunology, 133(4), 1233-1234. doi:10.1016/j.jaci.2014.02.009 Plaza, V., Giner, J., Rodrigo, G.J., Dolovich, M.B., & Sanchis, J. (2018). Errors in the use of inhalers by healthcare professionals: A systematic review. The Journal of Allergy and Clinical Immunology: In practice,6(3), 987-995. doi:10.1016/j.jaip.2017.12.032 Pralong, J.A., & Cartier, A. (2017). Review of diagnostic challenges in occupational asthma. Current Allergy and Asthma Reports, 17(1), 1-7. doi:10.1007/s11882-017-0676-3 A CXR is not needed to diagnose this case as it is written. I am wondering what evidence would prompt you to do a CXR ? Dr. Deering, Thanks for your question! You are absolutely right in that a chest x-ray is not warranted in this particular case study. Michelle presented clinically with signs and symptoms associated with mild persistent asthma. Based on the information presented in the case study, her asthma symptoms were related to an allergen from work. Even though a chest x-ray is not considered an initial imaging option for asthma, the value of a chest x-ray is significant in detecting complications of asthma, such as pneumonia, or other problems that mimic asthma symptoms (Terraneo et al., 2014). The majority of asthmatic patients suffer mild to moderate disease that can be well controlled with standard therapy of bronchodilators and inhaled corticosteroids. Unfortunately, the principal causes of asthma exacerbations are considered viral infections, such as influenza or respiratory syncytial virus, or bacterial infections, such as pneumonia (Watkins & Lemonovich, 2015). A chest x-ray would be considered if Michelle came in the office with complaints of greenish or yellow sputum production, fever, night sweats, chills, sharp chest pain when breathing in, shortness of breath, nausea, or vomiting (Terraneo et al., 2014). Symptoms of asthma and pneumonia can be very similar in the initial stage. As the infection progresses, productive sputum may accompany coughing and wheezing. Therefore, asthma symptoms may worsen when there is an infection. Other assessment findings that would warrant a chest x-ray include tachypnea, increased respirations, diminished breath sounds, crackles, tactile fremitus, or consolidation on percussion (Watkins & Lemonovich, 2015). References Terraneo, S., Polverino, E., Cilloniz, C., Amaro, R., Vennera, M., Gabarrus, A., . . . Torres, A. (2014). Severity and outcomes of community acquired pneumonia in asthmatic patients. Respiratory Medicine, 108(11), 1713-1722, doi:10.1016/j.rmed.2014.09.001 Watkins, R.R. & Lemonovich, T.L. (2015). Diagnosis and management of community-acquired pneumonia in adults. American Family Physician, 83(11), 1299-1306 [Show More]
Last updated: 1 year ago
Preview 1 out of 9 pages
.png)
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 07, 2021
Number of pages
9
Written in
Additional information
This document has been written for:
Uploaded
Sep 07, 2021
Downloads
0
Views
54



.png)


.png)