*NURSING > EXAM REVIEW > NR 601(SOLVED) Comprehensive Final exam study guide and practice questions (All)
NR 601(SOLVED) Comprehensive Final exam study guide and practice questions
Document Content and Description Below
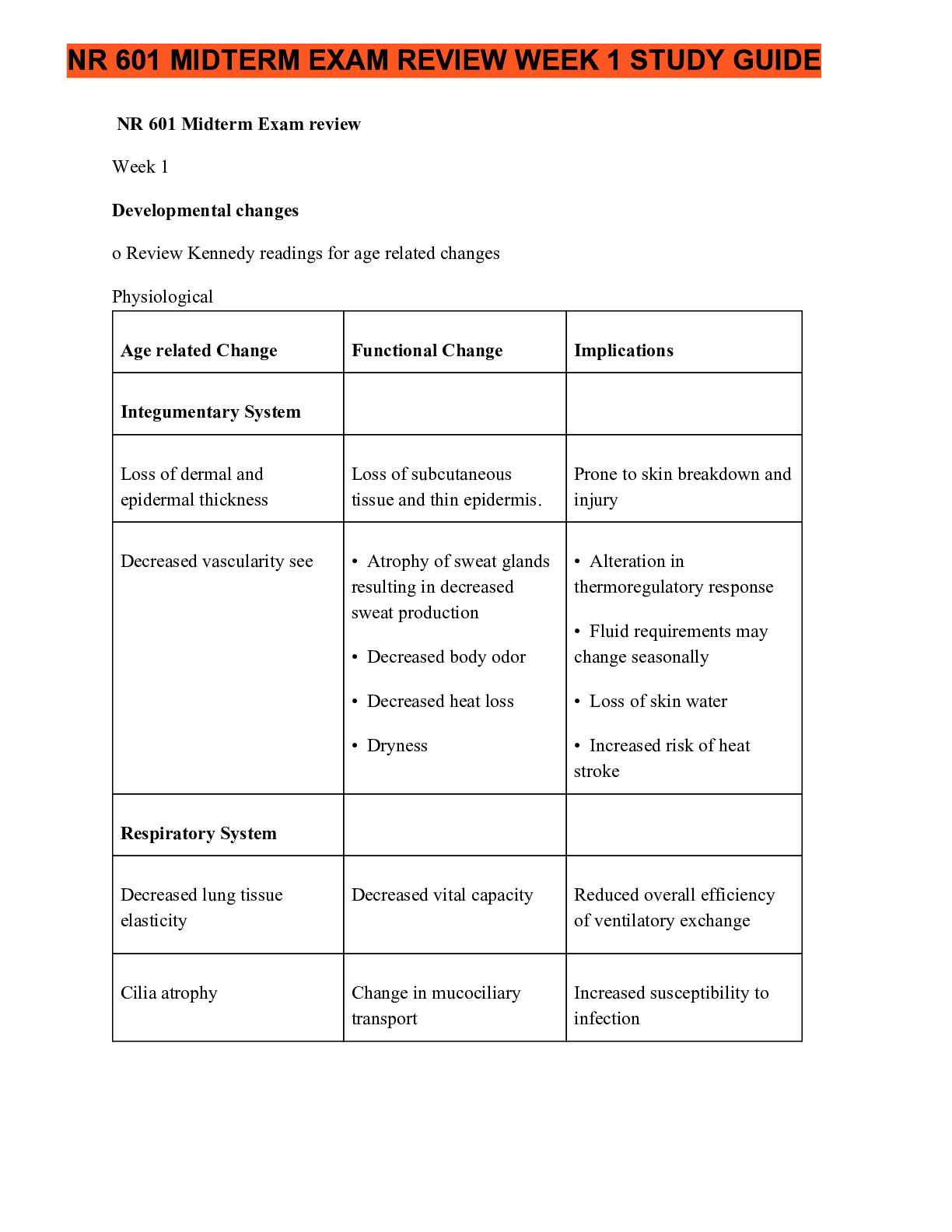
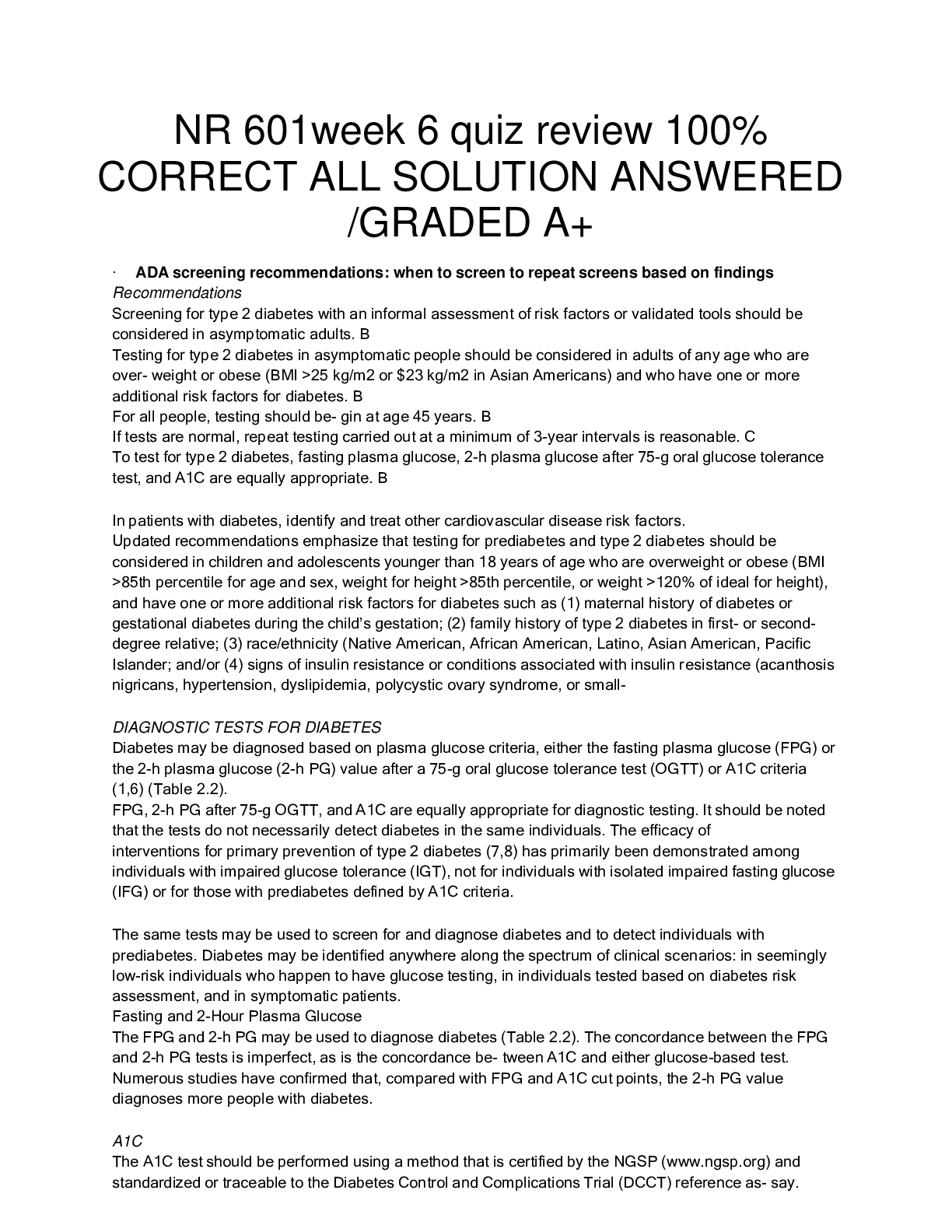
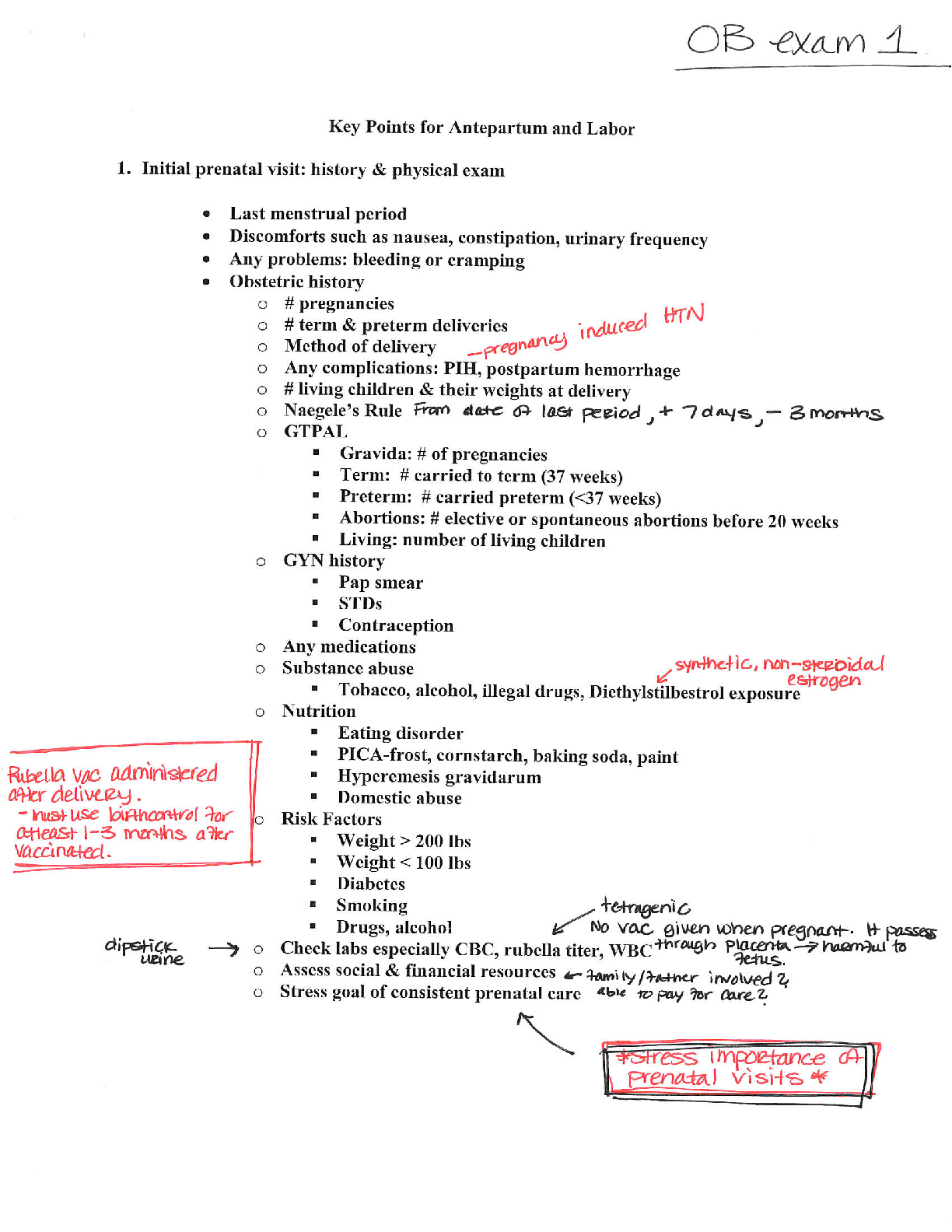
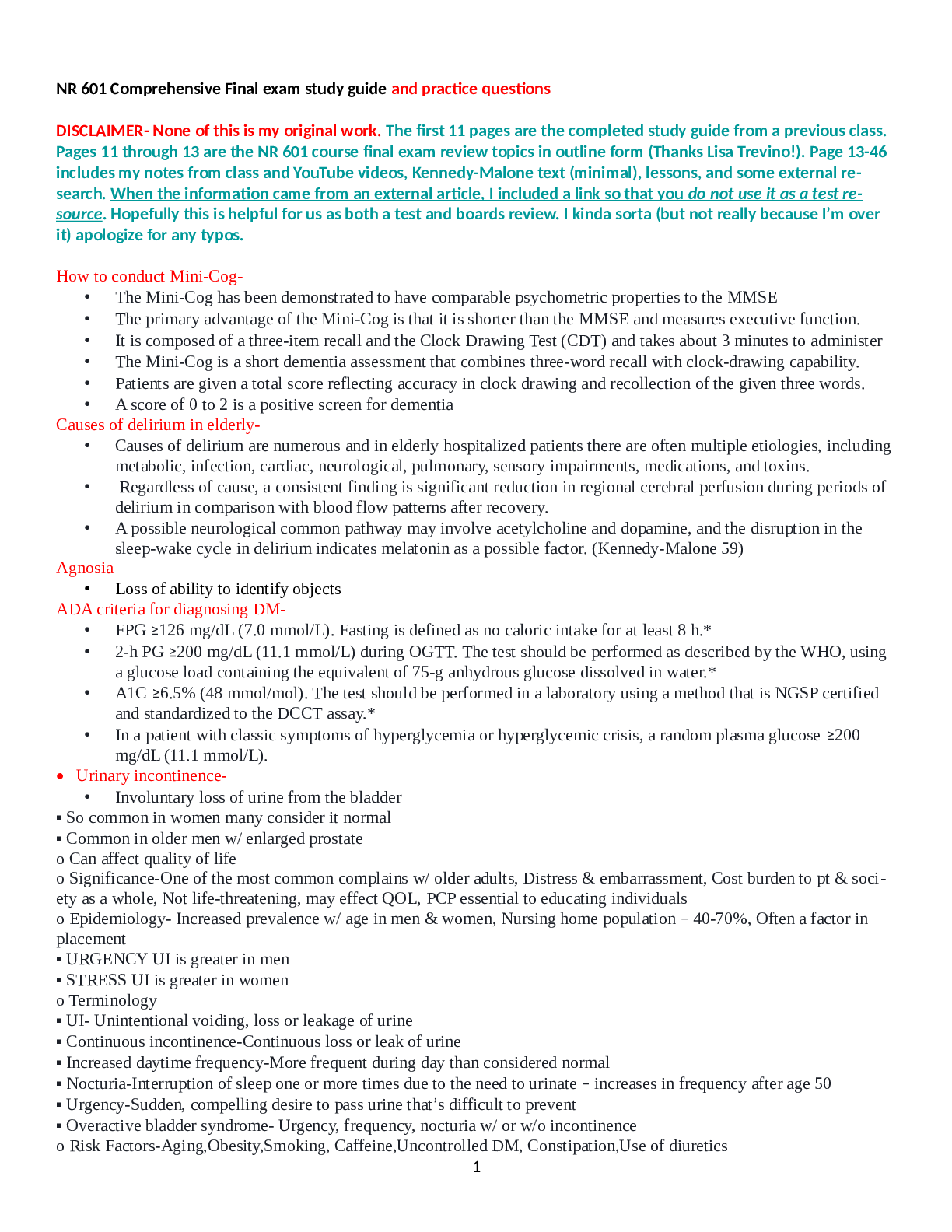
NR 601 final review.docx NR 601 Comprehensive Final exam study guide and practice questions DISCLAIMER- None of this is my original work. The first 11 pages are the completed study guide from a prev... ious class. Pages 11 through 13 are the NR 601 course final exam review topics in outline form (Thanks Lisa Trevino!). Page 13-46 includes my notes from class and YouTube videos, Kennedy-Malone text (minimal), lessons, and some external research. When the information came from an external article, I included a link so that you do not use it as a test resource. Hopefully this is helpful for us as both a test and boards review. I kinda sorta (but not really because I’m over it) apologize for any typos. How to conduct Mini-Cog The Mini-Cog has been demonstrated to have comparable psychometric properties to the MMSE The primary advantage of the Mini-Cog is that it is shorter than the MMSE and measures executive function. It is composed of a three-item recall and the Clock Drawing Test (CDT) and takes about 3 minutes to administer The Mini-Cog is a short dementia assessment that combines three-word recall with clock-drawing capability. Patients are given a total score reflecting accuracy in clock drawing and recollection of the given three words. A score of 0 to 2 is a positive screen for dementia Causes of delirium in elderly Causes of delirium are numerous and in elderly hospitalized patients there are often multiple etiologies, including metabolic, infection, cardiac, neurological, pulmonary, sensory impairments, medications, and toxins. Regardless of cause, a consistent finding is significant reduction in regional cerebral perfusion during periods of delirium in comparison with blood flow patterns after recovery. A possible neurological common pathway may involve acetylcholine and dopamine, and the disruption in the sleep-wake cycle in delirium indicates melatonin as a possible factor. (Kennedy-Malone 59) Agnosia Loss of ability to identify objects ADA criteria for diagnosing DM FPG ≥126 mg/dL (7.0 mmol/L). Fasting is defined as no caloric intake for at least 8 h.* 2-h PG ≥200 mg/dL (11.1 mmol/L) during OGTT. The test should be performed as described by the WHO, using a glucose load containing the equivalent of 75-g anhydrous glucose dissolved in water.* A1C ≥6.5% (48 mmol/mol). The test should be performed in a laboratory using a method that is NGSP certified and standardized to the DCCT assay.* In a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, a random plasma glucose ≥200 mg/dL (11.1 mmol/L). • Urinary incontinence Involuntary loss of urine from the bladder ▪ So common in women many consider it normal ▪ Common in older men w/ enlarged prostate o Can affect quality of life o Significance-One of the most common complains w/ older adults, Distress & embarrassment, Cost burden to pt & society as a whole, Not life-threatening, may effect QOL, PCP essential to educating individuals o Epidemiology- Increased prevalence w/ age in men & women, Nursing home population – 40-70%, Often a factor in placement ▪ URGENCY UI is greater in men ▪ STRESS UI is greater in women o Terminology ▪ UI- Unintentional voiding, loss or leakage of urine ▪ Continuous incontinence-Continuous loss or leak of urine ▪ Increased daytime frequency-More frequent during day than considered normal ▪ Nocturia-Interruption of sleep one or more times due to the need to urinate – increases in frequency after age 50 ▪ Urgency-Sudden, compelling desire to pass urine that’s difficult to prevent ▪ Overactive bladder syndrome- Urgency, frequency, nocturia w/ or w/o incontinence o Risk Factors-Aging,Obesity,Smoking, Caffeine,Uncontrolled DM, Constipation,Use of diuretics o Risk Factors by gender-Women:Aging, obesity, smoking, caffeine intake, DM, pregnancy, multiparity, estrogen deficiency, hx of pelvic surgery, diuretics 1Men:Aging, obesity, smoking, caffeine, DM, prostate dx, hx of prostate surgery, hx of UTIs, diuretics o Physical changes w/ aging that contribute to UI ▪ Lower urinary tract-Detrusor muscle over activity,Decrease in detrusor contractility, Increase in post void residual,Decrease in urethral blood flow ▪ Women – decrease in urethral closure pressure,Low estrogen following menopause - leads to atrophy of ureteral mucosal epithelium & increase in urethral sensation ▪ Men can experience constriction of urethra due to BPH which may result in bladder outlet obstructing symptoms - Initial clinical workup for UI in Men o PMH, PE, UA, DRE: Eval of prostate,PSA w/ new onset in men - UI workup in women:Exclude underlying causes,PMH, PE, UA, Pelvic exam, vaginal exam, perineal, Identify estrogen status of pt, Pelvic prolapse, fistula, -Cough test, Integrity of pelvic musculature, leaking of urine ▪ Full bladder ▪ Standing position ▪ Asked to cough ▪ If urine leak is observed, stress incontinence is confirmed - Red flags in males o Higher level of suspicion for serious diseases, Refer to urology if Previous pelvic surgery, Pelvic radiation, Pelvic pain, Severe incontinence, Severe UTI symptoms, Recurrent urologic infection,Abnl Prostate exam,Elevated PSA o Be alert to these with NEW ONSET UI- Hematuria,Pelvic pain,Abdominal mass, Dysuria, Proteinuria, Glucosuria, CVA tenderness,Nodular prostate,Any new neuro symptoms - Goals of treatment: Reduce symptoms, Improve QOL, Increase social activity, Reduce leakage volumes, increase dryness, use less protection; Increase independence in incontinence management; Decrease caregiver burden - 1st line management guidelines o AHRQ guidelines for management of UI in women ▪ Behavioral therapy ▪ Lifestyle modification ▪ Try for 3 months before pharm management o Weight loss, Smoking cessation(Tobacco is a bladder irritant),Less coughing o Dietary changes-Alcohol, soda, coffee with or without caffeine, acidic foods and spicy foods o Maintain adequate fluid balance to reduce constipation, provide adequate flow to kidneys - Behavioral strategies:Bladder training, Bladder control strategies,Timed voiding,Kegels, Pelvic floor training - 2nd line management - Medication o Antimuscarinic medication: 1st line for women ▪ Block the parasympathetic muscarinic receptors ▪ Inhibit involuntary detrusor contractions ▪ Side effects due to the effects on other muscarinic receptors o Outcomes unpredictable and side effects common o Common s/e: Dry mouth**, Blurred vision, Constipation,Nausea,Dizziness, Headache o AntimuscarinicsMechanism of action ● Blocks acetylcholine at muscarinic receptors, relaxes bladder smooth muscle, inhibits involuntary detrusor contractions (anticholinergic) ● CYP3A4 substrates ▪ Indications: UI and OAB ▪ Contraindications: Untreated/uncontrolled narrow angle glaucoma,Gastric retention, Urinary retention ▪ Precautions:CNS depression,Caution in elderly ● Renal dosing o CrCl <30 o Beta 3 Adrenergic Agonist – Mirabegron (Myrbetriq) ▪ Also approved for UI and OAB ▪ Clinical trials – significant reduction in incontinence and micturations ● No anticholinergic s/e ▪ Mech of action ● Selectively stimulates beta-3 adrenergic receptors 2● Relaxes smooth muscle – bladder ▪ Contraindications/caution: HTN- Do not use if SBP >180, DBP >100 ▪ Avoid severe renal/liver disease ▪ Dose – 25-50mg PO QD ▪ CrCl <30 – max 25mg - 2nd line of UI in Males – Alpha 1 blockers o Men, not women! o Alpha 1 blockers antagonize peripheral alpha 1 adrenergic receptors o Used in men d/t high incidence of BPH in aging men o Alpha antagonists ▪ Alpha 1A – prostatic smooth muscle relaxation ▪ 1B – vascular smooth muscle contraction ▪ 1D – bladder muscle contraction and sacral spinal cord innervation o Meds ▪ Doxazosin SE: Dizziness, dyspnea, edema, fatigue, somnolence ▪ Terazosin SE: Asthenia, dizziness, postural hypotension ▪ Tamsulosin SE:Abnormal ejaculation, asthenia, back pain, dizziness, increased cough ▪ Alfuzosin- CrCl <30 use with caution, SE: Dizziness, URI ▪ Silodosin SE- Retrograde ejaculation Differentials as cause for erectile dysfunction- Differential diagnosis: o Vascular, Endocrine, Neurological, Neurovascular, Substance abuse, End-organ disease, Psychogenic, Social causes (Kennedy-Malone 376) Elder abuse Types- o Physical, Emotional, Sexual, Neglect, Exploitation, Abandonment, Self-Neglect Risk Factors- o Age, Gender, Cognitive Impairment, Living Arrangement, Social Isolation Signs of abuse- o bruises, slap marks, unexplained burns, increased accidents, lack of hygiene, failure to meet medical needs, weight loss, decubiti, changes in personality, decreased interaction, unexplained STD Provider responsibility in reporting abuse o If you suspect elder abuse perform a physical exam and order any necessary tests. o Include a cognitive screen. o Document your findings. This includes what the patient says and your objective findings. o You may need to interview your patient and the caregiver separately to see if the stories are the same. o Be aware of your state laws regarding mandatory reporting of suspected abuse. Differentials as cause for hematuria- Differentials per class notes Dietary substances o Caffeine, spices, Tomatoes, chocolate, alcohol, Citrus, soy sauce, & some herbal meds Medication o Beta-lactam antibiotics, sulfonamide, NSAIDs, Cipro, allopurinol, Tagamet, & dilantin Anticoagulation and papillary necrosis o Coumadin, Heparin, aspirin, & NSAIDs Glomerular nephritis Hydrocarbons (glue, paint) NSAIDs Urolithiasis menses Terazosin use(s)- Alpha blocker for BPH. 1-10 mg P.O. nightly. Caution in those with cataracts and in elderly. Side effects o hypotension, priapism, dizziness, dyspnea, tachycardia. 3 2nd Line Management of UI in males ***Alpha 1 Blockers Pharmacologic agents for men with urinary incontinence differ from women; Alpha 1 blocker antagonize peripheral alpha-1 adrenergic receptors and commonly referred to as alpha 1 blockers *Lifestyle changes and Behavioral Management are first-line but when not effective alpha 1 blocker is initiated; *This difference in choice of medication for men is due to the high incidence of BPH associated with aging men Alpha 1 Adrenergic Receptor antagonists Alpha 1A- Prosthetic smooth muscle relaxation Alpha 1B- Vascular smooth muscle contraction Alpha 1D -Bladder muscle contraction and sacral spinal cord innervation UTIs in men and women UTI treatment guidelines BPH- Progressive, benign hyperplasia of prostate gland tissue Etiology/incidence- o Cause is uncertain, About 50% of men have it by 60, By age 85, 90% have it o Most common cause of bladder outlet obstruction in men over 50 Symptoms are attributed to mechanical obstruction of the urethra by the enlarged prostate gland Signs/Symptoms- o Gradual worsening of the following, Frequency, urgency, urge incontinence, Nocturia, dysuria, Weak urinary stream, dribbling, hesitancy, Sensation of full bladder even after voiding, Retention Diff Dx- o Urethral stricture, Prostate or bladder cancer, Neurogenic bladder, Bladder calculus, Acute or chronic prostatitis, Bladder neck contractor, Medications that affect micturition Physical findings- o Abdomen,May have distended bladder secondary to retention; Prostate,Nontender w/ asymmetric or symmetrical enlargement, gross enlargement atypical, Consistency is smooth, rubbery (eraser), Nodules may be present Differentiation from BPH and CA needs biopsy Tests/Findings o UA-No hematuria or UTI, Urinary flow rate, Voided volume and peak urinary flow rate (uroflowmetry) may detect obstruction flow, Abdominal US – rules out upper tract patho, PSA, Consider PVR urine volume, Cr to assess renal function, elevated levels suggest urinary retention or underlying renal disease – refer this patient Treatment/Management- o Refer men who have the following, Refractory urinary retention who have failed one attempt at cath removal, Recurrent infection, recurrent retention, refractory hematuria, bladder stone, large bladder, diverticula, or renal insufficiency related to BPH, Consider referral if complications exist or if patients have severe symptoms Management- o Men who have no indications for surgery, Discuss risks/benefits of all options, Watchful waiting (observation), Behavioral techniques to reduce symptoms, Limit fluid after dinner, Avoid medications such as Antidepressants, Antiparkinson drugs, Antipsychotics, Antispasmodics, Cold meds, Diuretics Medication Treatments o Alpha adrenergic blocker – for smaller prostates o 5-alpha adrenergic blocker – larger prostates o Combo therapy is an alpha-adrenergic blocker and finasteride is used now for men w/ large prostates Surgery has the best chance for relief of symptoms, but greater risks Follow up: o Teach signs/symptoms of retention and obstruction, 4o If observing for now, recheck every 6-12 months, o In use of meds, recheck in 4-6 weeks, o If post surgery follow up is at the discretion of the urologist Acanthosis nigricans A sign of insulin resistance that can be seen in African Americans associated with colon cancer, obesity and DM Delirium treatment- (Kennedy p. 560). Identify causes, prevent delirium though complications of identified disorders. \ Focus on safety. Frequent reassurance and re-orientation. First generation --haloperidol. Second generation (olanazapine, risperidone, ziprasidone and quitiapine) antipsychotics to control behavioral symptoms. Essential tremor vs. Parkinson’s Disease Essential tremor is an action tremor 6 to 8 Hz, Parkinson’s tremor is a resting tremor which is 3 to 6 Hz. (Kennedy p. 425) Seizure causes In older adults stroke is the most common underlying cause of seizures. Other causes include neurodegenerative disorders, brain tumors and head injuries. (Kennedy p 438) Hospice & palliative care- Hospice: o Last 6 mos of life. Uses palliative care principles to support pt and family. Includes bereavement services. Covered by Medicare/Medicaid, most private insurance. Interdisciplinary care, medical service, supplies, drugs Palliative Care: o To relieve pain and improve QOL. Used early in dz process. Interdisciplinary Care. Provides care for the entire dz process, from diagnosis to death, including bereavement services. Pain- Pain assessment tools: o Visual Analogue Scale o Numerical Analogue Scale o Wong Baker FACES o Pain Assessment in Advanced Dementia scale Types of pain: o Somatic, o Visceral, o Neuropathic Framework for pharmacological interventions for pain: The WHO Step Ladder o 1st step: NSAIDs and Tylenol for mild pain o 2nd step: Opioids added, usually with APAP for moderate to severe pain with functional impairment and or decreased QOL o 3rd step: Opioid pain meds, sometimes around the clock for severe pain Adjuvant meds: o Tricyclic antidepressants, Nortriptyline, Desipramine, Duloxetine, Gabapentin, Pregabalin, Lidocaine 5% patch, Capsaicin cream, Corticosteroids, Calcitonin, Baclofen Pain management in elderly Delirium vs. dementia- Delirium- o rapid onset (hours to days). o Poor memory, disorientation, speech disturbance, perceptual disturbance. o Typically fluctuates over course of day. 5o History may reveal cause-medical condition, intoxication or withdrawal, use of med, toxin exposure or combination. (Kennedy 558). Dementia- o Alz Disease most common. o An acquired persistent intellectual impairment with compromise in multiple spheres of mental activity. o Signal symptoms: confusion, impaired short-term memory, cog dysfunction. o Progression is typically slow. o Could be reversible (secondary to treatable systemic disorder), or irreversible (primarily caused by progressive systemic or neuro disorder). o ***hallmark*** anosognosia- the patient is unaware of impairment and denies illness(kennedy, p.562) o Alz. ChEIs - cornerstone of pharm therapy as acetylcholine is important for brain cell function. Steps of the grieving process Grief is the emotional response to loss, Mourning is the outward social expression of loss Types of grief: o Anticipatory-experienced before death, can be experienced by everyone including the patient o Normal- encompasses the typical emotional, physical, cognitive, and spiritual reactions to a loss o Complicated-chronic, delayed, exaggerated, masked or disenfranchised Stages of Grief: o Notification and shock o Experiencing the loss emotionally and cognitively o Reintegration Tasks of grieving: o Acknowledging the reality of death o Sharing in the process of working through the pain of grief o Reorganizing the family system, restructuring the relationship with the deceased, and reinvesting in other relationships and life pursuits Kennedy p. 631 Alzheimer’s treatment Signs and symptoms- o Preclinical can last 2-4+ years, impaired memory (excused or covered), poor judgement, decreased spontaneity, increased social anxiety, insidious instrumental ADL losses (bill paying, money handling), preserved basic ADLs o Mild/Moderate- lasts 2-10 years, obvious memory impairment, overt instrumental ADL impairment, basic ADL failing, behavioral difficulties, shortened attention span, language difficulty, variable social skills, supervision required o Severe- last 1-2+ years, memory fragments only, no recognition of familiar people, requires assistance with basic ADLs, reduced mobility, weight loss, fewer troublesome behaviors, infections, seizures, dysphagia, incontinence, groaning, moaning, grunting First line pharmacological treatment- o Cholinesterase inhibitors donepezil (Aricept) o Memantine (Namenda) added at the moderate to severe stage Kennedy p 567-568 Sexuality sundowning metformin side effects- GI side effects take with supper. Most patients adjust to these SE. ADVERSE effect- Lactic acidosis. B12 deficiency Biguanides (Metformin) has become a cornerstone of drug treatment for type 2 disease, based on its proven efficacy not only in controlling glucose intolerance but also in significantly reducing risk of important macro- and microvascular outcomes, especially in overweight and obese patients (as found in the UKPDS study referred to 6earlier and below). In glycemic treatment algorithms for type 2 disease, initiation of metformin is recommended at the time of diagnosis along with diet and exercise. Mechanism of Action. Metformin differs from the traditional oral hypoglycemics (i.e., the sulfonylureas) in that it does not stimulate endogenous insulin secretion; rather, drugs of this class enhance tissue responsiveness to insulin. Consequently, biguanides are less likely to induce hypoglycemia and are particularly effective in the treatment of overweight patients with tissue resistance to insulin. Biguanides facilitate insulin uptake by peripheral tissue, especially muscle and liver, and decrease hepatic gluconeogenesis and basal glucose output, thereby helping to lower fasting glucose levels. Glucose utilization also improves in adipose and intestinal tissues. The net result is an improvement in fasting and postprandial hyperglycemia. Insulin demand declines as glucose utilization improves. Serum lipid abnormalities also improve. Preparations. Metformin is the only biguanide approved in the United States for the treatment of type 2 diabetes. The drug is rapidly and well-absorbed in the small intestine, with peak plasma concentrations in 2 hours. It is rapidly excreted unchanged by the kidneys. Impaired renal function (creatinine >1.5 mg/dL in men and >1.4 mg/dL in women) is a contraindication for use, especially at full doses. The drug is not metabolized by the liver. The original biguanide, phenformin, is no longer marketed because of its associated risk for lactic acidosis and an excess cardiovascular mortality (see later discussion). Dosing. The starting dose of metformin is 500 mg once daily with dinner. After 1 week, the dose is increased to twice daily, given with the two largest meals of the day (usually breakfast and dinner) to minimize gastrointestinal upset. The dose can be increased by 500 mg every 1 to 2 weeks until treatment goals are met or the maximum dose of 2,000 to 2,500 mg/d is reached. An extended-release formulation is also available, which can help to improve compliance. Efficacy. When used as monotherapy in an obese person with moderate glucose intolerance, metformin’s efficacy in terms of glycemic control (i.e., lowering fasting glucose and glycosylated hemoglobin levels) is about the same as that of a second-generation sulfonylurea. Incidence of monotherapy treatment failure is less for metformin than for glyburide (21% vs. 34% at 5 years). A synergistic effect is achieved when combined with sulfonylurea therapy in patients who do not respond well to metformin alone. Unlike the sulfonylureas, metformin is effective even in severe fasting hyperglycemia (>300 mg/dL), indicative of poor beta-cell responsiveness. Plasma triglycerides and LDL cholesterol levels are decreased. In the UKPDS trial noted earlier, obese patients (>120% of ideal weight) with type 2 diabetes treated with metformin and attaining target glycemic control achieved clinically important, statistically significant, sustained long-term reductions in risks of microvascular disease and macrovascular complications (i.e., myocardial infarction, stroke, and cardiovascular death); all-cause mortality was also significantly reduced. These findings make metformin one of the few antihyperglycemic drugs with demonstrated ability to reduce macrovascular risk, the holy grail of diabetes management. Adverse Effects. The most common side effect of biguanide therapy is dose-related gastrointestinal upset (nausea, diarrhea, bloating, abdominal discomfort). The risk for serious prolonged hypoglycemia is minimal. Lactic acidosis represents the most potentially serious adverse effect. One of the original biguanides—phenformin —was taken off the market by the U.S. Food and Drug Administration (FDA) in 1977 because of its association with fatal episodes of lactic acidosis. The risk for lactic acidosis associated with metformin is greatest in the setting of hypoxemia, hypovolemia, and states with decreased tissue perfusion and in renal insufficiency (creatinine >1.5 mg/dL). Accumulation of the drug secondary to reduced excretion results in impaired hepatic metabolism of lactate. Other risk factors include binge drinking, use of intravenous radiologic contrast agents, hepatic failure (lactate is metabolized by the liver), and serious underlying illness, particularly heart failure.Long- term data on safety have yet to be accumulated. Because insulin secretion is not increased with metformin use, weight gain does not occur; some patients may even lose weight. Patients who are to undergo a radiologic procedure that requires intravenous iodinated contrast should have their metformin therapy held for a few days prior to the procedure and remain well hydrated. Patient Selection. Based on the landmark results of the UKPDS, obese patients should be considered especially good candidates for metformin therapy. The drug helps to reverse their insulin resistance, peripheral responsiveness to insulin improves, and insulin needs decrease, so hyperinsulinism and its adverse effects, including weight gain, are minimized. The typical candidate is a moderately obese person with type 2 diabetes who has persistent moderate hyperglycemia (fasting glucose between 140 and 240 mg/dL, glycosylated hemoglobin >7.0%) despite a full program of diet and exercise. Early addition of metformin is suggested. Other candidates for metformin include obese patients who do not achieve tight control while taking a sulfonylurea at maximal doses. In this setting, metformin is added to the oral hypoglycemic program to improve control through 7its complementary mode of action. The sulfonylurea dose is reduced to lessen the risk for hypoglycemia. Combination therapy is most effective when initiated before the onset of symptomatic hyperglycemia (fasting glucose >250 mg/dL). Nonobese patients are also reasonable candidates for metformin. Typically, metformin lowers fasting blood glucose by approximately 20%.Patients who started drug therapy with a sulfonylurea and become unresponsive to maximal doses have likely exhausted their beta-cell reserve and can be switched to metformin or considered for exogenous insulin therapy (sometimes in conjunction with metformin). The same pertains to the severely hyperglycemic obese patient (fasting glucose >300 mg/dL). Some diabetologists use metformin to supplement an insulin program in obese type 2 diabetics who require large insulin doses and have difficulty losing weight. The combined program helps to reduce insulin requirements and the appetite stimulation and weight gain that accompany hyperinsulinism. Caution and careful patient monitoring are required when a patient taking exogenous insulin is started on metformin; the insulin requirement may drop considerably, putting the patient at risk for hypoglycemia. Use in pregnancy is not associated with major congenital malformations. ACC 2017 Guideline for High Blood Pressure in Adults- 2017 HTN guidelines Normal BP is defined as <120/<80 mm Hg Elevated BP 120-129/<80 mm Hg Hypertension stage 1 is 130-139 or 80-89 mm Hg Hypertension stage 2 is ≥140 or ≥90 mm Hg. Acute prostatitis kennedy 380. lower urinary tract symptoms- o frequency, pain on urination or pain increasing with urination. Acute bacterial prostatitis- o presence of more than 10 WBC per high power field on mid-stream urine collection. If acutely ill, hospitalization. o Treat with Cipro 500mg BID x 10 days or Levaquin 500mg daily x 10 days. o Choose a fluroquinolone - it penetrates prostate tissue well. Education o May need a stool softener. Repeat UA is recommended. Avoid anal intercourse. Use condom to prevent reintroduction of bacteria into urethra. Beta blocker side effects in diabetics- Can mask the symptoms of hypoglycemia How to diagnosis HF and COPD via CXR findings- Chest x-ray: for COPD o This exam can help support the diagnosis of COPD by producing images of the lungs to evaluate symptoms of shortness of breath or chronic cough. o While chest x-rays may not show COPD until it is severe, the images may show enlarged lungs, irregular air pockets (bullae) or a flattened diaphragm. o A chest x-ray may also be used to determine if another condition may be causing symptoms similar to COPD. (Malone 207) – o chest X-ray in advanced COPD with emphysema May reveal hyperinflation bullae or blebs and a flat hemidiaphragm. OA HF stages- ACCF/AHA STAGES: o A: At high risk for HF w/o structural heart Dz or Sx o B: Structural heart dz w/o s/sx of HF o C: Structural heart dz w/ prior or current sx of HF o D: Refractory HF requiring specialized interventions New York Heart Association classes- o I No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, dyspnea (shortness of breath). o II Slight limitation of physical activity. Comfortable at rest. Ordinary physical activity results in fatigue, palpitation, dyspnea (shortness of breath). 8o III Marked limitation of physical activity. Comfortable at rest. Less than ordinary activity causes fatigue, palpitation, or dyspnea. o IV Unable to carry on any physical activity without discomfort. Symptoms of heart failure at rest. If any physical activity is undertaken, discomfort increases. Causes for insomnia – Anxiety, stress, and depression are some of the most common causes of chronic insomnia. Having difficulty sleeping can also make anxiety, stress, and depression symptoms worse. Other common emotional and psychological causes include anger, worry, grief, bipolar disorder, and trauma. Prescription for insomnia – Avoid caffeine for 12 hours before bedtime, d/c alcohol and unnecessary sleep interrupting drugs, OTC melatonin RX ramelteon can be tried, if ineffective initiate a short acting sedative-hypnotic such as zolpidem (Ambien) or zaleplon (Sonata) for 1 week or less If a benzodiazepine is used, temazepam (Restoril) is relatively short acting Approved pharmacological therapy includes temazepam for sleep onset insomnia, eszopiclone (Lunesta) for sleep onset and sleep maintenance, zolpidem CR and zolpidem for sleep maintenance, and saleplon and ramelteon for sleep onset insomnia Kennedy p 597-588 TABLE 232–4 Effective Drugs for Insomnia Agent (Brand Name) Onset Duration Dose (mg) Benzodiazepine receptor agonists Zaleplon (Sonata)a Rapid Zolpidem (Ambien)a Rapid Zolpidem (Ambien CR)a Zolpidem (Intermezzo) (sublingual) Zolpidem (Zolpimist) (oral spray) Rapid Rapid Rapid Eszopiclone (Lunesta) Rapid Benzodiazepines Triazolam (Halcion)a Rapid Diazepam (Valium)a Rapid Estazolam Rapid– Intermediate Short Long 0.124– 0.25 2–5 Intermediate 1–2 Quazepam (Doral)a Intermediate Long 15 9 $ ($$) $ ($$) $ $$ ($$$$) Short Short– intermediate 5–10 5–10 Intermediate 6.125– 12.5 Very short Short Short– intermediate 1.75– 3.5 10 1–3 Relative Cost (Brand) May impair AM performance; ? anterograde amnesia; modest potential for abuse, withdrawal, dependence; drug–drug effects $ ($$$$) May be used for awakenings at night; possible interaction with inducers of CYP 3A4 $ ($$$$) Potential interaction with inducers of CYP 3A4 $$$ ($$$$) Intermediate-release preparation; greater risk of morning sedation $$$$ $$$$ $$$$$ Sublingual, for middle-of-night awakening ? Faster onset of action; ease of use might lead to excess dosing Bad taste, potential interactions with ketoconazole, nefazodone, and inducers of CYP 3A4 Potential for dependence, tolerance, abuse, rebound insomnia, psychomotor retardation Anterograde amnesia Generic only CommentsFlurazepam (Dalmane)a Intermediate Long Lorazepam (Ativan)a Intermediate Clonazepam (Klonopin)a 15–30 $ ($$$) Intermediate 1 $ ($$$) Intermediate Long Oxazepam (Serax)a Intermediate– slow Temazepam (Restoril)a Melatonin Receptor Agonists Ramelteon (Rozerem) Rapid Antidepressants Doxepin (Silenor) Short 8 $$ Intermediate– slow Short– intermediate 0.5–1.0 $ ($$) 10–15 $$ ($$$) Intermediate 15 $ ($$$) No potential for abuse Rapid Long 3–6 $$$ GOLD criteria- Malone 207) Gold standard = Spirometry for measuring airflow limitation. o GOLD Classification (post bronchodilator FEV1) o GOLD1 (mild): FEV1 > 80% predicted o GOLD2 (Moderate): 50-79% predicted o GOLD 3 (Severe): 30-49% predicted o GOLD 4 (Very Severe): FEV1 < 30% predicted Treatment = individualize according to stages, cormorbidities, and patient goals. Treatment is targeted towards improvement of health status, And functional status, prevention of disease progression avoidance of exacerbations or complications prevention of treatment side effects and management of exacerbation. COPD management program Risk factor reduction. Assessment and monitoring. Stable chronic management. Management of exacerbation. Smoking cessation is the most effective cost effective intervention and should be promoted every visit. No current drug therapy has proven to influence the progressive decline of COPD. Malone 208 - inhaled bronchodilators maybe useful and stable COPD patients. Arrhythmia evaluation SIG-E-CAPS- S: sleep (insomnia or hypersomnia) I: interests (diminished interest or pleasure); G: guilt: (excessive or inappropriate guilt; feeling worthless); E: energy (loss of or fatigue); C: concentration (diminished concentration or indecisiveness); A: appetite (decrease or increase; weight gain or weight loss); P: psychomotor retardation/agitation (move slow, agitated, restless); S: suicide (recurrent thoughts of death, ideation, or attempt) DEXA scan results findings- (Pg 499) 10 Very-low-dose preparation may be helpful in elderly with chronic insomnia.• BMD measurement is expressed as the number of standard deviations from the mean for normal young adults of the same sex (T-score) and as the number of standard deviations from the mean for persons of the same sex and age (Z score). • The World Health Organization diagnostic criterion for osteoporosis is a T-score of less than -2.5. Osteopenia is defined as a T-score between -1.0 and -2.5. A Z score of less than -1.5 suggests a secondary cause of osteoporosis • Osteoporosis: -2.5 or lower • Osteopenia: -1 to -2.5 (lower than normal bone density w/o full osteoporosis) Anxiety treatment- • Treatment for anxiety should reduce symptoms and improve functioning. • Simply listening, being compassionate, and showing respect are important to improving outcomes. Treat comorbid depression and medical conditions that cause anxiety. • There are no large-scale studies of pharmacotherapy for late-life anxiety disorders to guide treatment decisions. • Start low and go slow with medication dosing to avoid risks from drug interactions, because older adults are more likely to take many medications and may have side effects from aging changes in absorption, metabolism, distribution, and excretion of medication. • Evaluate and manage side effects, because as many as 25% of patients stop taking medication in the first 6 months due to side effects. • First-line treatment is the selective serotonin reuptake inhibitors (SSRIs) o citalopram (Celexa), escitalopram (Lexapro), and sertraline (Zoloft). In older adults, they have the least risk of drug interactions, side effects, or worsening existing medical conditions. o Benzodiazepines, including lorazepam (Ativan), alprazolam (Xanax), and clonazepam (Klonopin), are effective according to research but are not the first choice due to the risk of falls and confusion. Research supports referral to psychotherapy for older adults, but this recommendation is limited to GAD and no other anxiety disorders (American Psychiatric Association, n.d.; Cassidy & Rector, 2008; Hollander & Simeon, 2008; Lenze et al., 2005; Lenze & Wetherell, 2009; Mohlman, 2005; National Institute of Mental Health, n.d.; Stanley et al., 2003; Wetherell, Lenze, & Stanley, 2005; Wetherell, Sorrell, Thorp, & Patterson, 2005). (Kennedy-Malone 553-554) ************************************************************************************************** FINAL EXAM NR 601 (Thanks Lisa Trevino!) The test covers weeks 1-8 content. 25% is weeks 1-4. 75% is weeks 5-8 Week 1 topics include: Aging (Chapter 1) Exercise (Chapter 3) Chest disorders: COPD, bronchitis Week 1 presentations In week 1 the required readings included: The physiologic changes of aging, Exercise, Polypharmacy Chest disorders were discussed in Kennedy-Malone et al Chapter 8 as well Gorroll Week 1 presentations WEEK 2 • Cardiac • Polypharmacy • Guidelines: – 2017 ACC/AHA guidelines for management of heart failure – 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults – 2017 blood pressure guidelines – Beers Criteria Week 2 topics included cardiac concerns Polypharmacy 112017 ACC/AHA guidelines for management of heart failure 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults 2017 ACC/AHA HTN guidelines Beers criteria- its purpose New York Heart Association functional classifications for heart failure (Gorroll) WEEK 3 Health Promotion prevention education Mental health Insomnia Health promotion is discussed in Kennedy-Malone Chapter 2. Review vaccine recommendations, organisms responsible for outbreaks and patient education. Know the types of prevention: primary, secondary and tertiary. Mental health: review required readings and presentation Anxiety & Depression Somatic complaints, screening tools, mnemonics, contributing factors, appropriate labs: purpose and rationale and goals of treatment. Note symptoms and factors that are distinct to the elderly. Know first line treatments Insomnia: know the types of insomnia and recommended first line treatments. WEEK 4 Osteoporosis Polymyalgia rheumatica Rheumatoid arthritis Osteoarthritis Pain Review Chapter 12 of Kennedy –Malone et al Osteoporosis- review assigned readings and the recorded lecture. Know signs and symptoms, diagnostic tests and treatment Polymyalgia rheumatica and Rheumatoid arthritis, osteoarthritis - signs and symptoms, diagnostic tests and treatment Review the types of pain, common treatments WEEK 5 In week 5 the focus was diabetes. Review the presentation Know the risk factors – modifiable and nonmodifiable Physical exam findings Know the appropriate screening tests- this is based on the ADA guidelines which you reviewed when you completed the case study. Interpret screening test results and the appropriate next step. Appropriate diagnoses: prediabetes, diabetes type 2 Common medications, medication side effects. Education for side effects Review the complications and which are most common. Know recommended referrals for diabetic patients. Review the ACC 2017 Guidelines for assessment and treatment of BP in diabetic patients. This includes BP ranges and appropriate first line recommendations for diabetic patients. WEEK 6 12Week 6 GU and GYN Disorders • Sexuality – Kennedy Chapter 11- Disorders: Erectile dysfunction, atrophic vaginitis, GSM, BPH Urinary UA dip interpretation Sexuality lecture Kennedy Chapter 11 covered urological and gynecological disorders Diagnose and initial treatment for a UTI, treatment for multiple UTIs These included atrophic vaginitis, BPH, ED, prostate cancer and prostatitis. Know the pathophysiology, presenting signs and symptoms, physical exam findings, appropriate next step, appropriate treatments and follow up recommendations Side effects of medications Eg: BPH has treatment recommendations based on severity. Incontinence” types of incontinence WEEK 7 • Delirium & Dementia • Stroke, TIA, seizures • Tremor Elder Abuse Kennedy Malone readings and lecture Delirium and dementia: causes, signs and symptoms. What differentiates between the two. Appropriate screening tools. Treatment options Common comorbid condition Kennedy Malone and other required reading CVA and TIA, tremor Seizures Parkinson's including the information within differential diagnoses. Medication classes used for treatment. Alzheimer’s disease signs and symptoms, first line treatment. Delirium and dementia: causes, presenting signs and symptoms. Risk factors. What differentiates between the two. Appropriate screening tools. Treatment options Common comorbid conditions. Screenings: best screening test for delirium, MiniCog- know how the test is performed and how to interpret the results Tremor: differentiate types of tremors Elder abuse: signs of abuse, provider responsibility in reporting abuse Week 8 • Palliative Care, Hospice, Pain, Grief Review the presentation & Chapter 21 Pain: types of pain, pain management, the WHO step ladder ___________________________________________________________________________________________ Week 1 video & lesson notes (taken directly from videos- refer to lesson videos for sources): Leading causes of death in Older Adults > 65 y/o: Heart disease, cancer, and chronic lower respiratory disease Ask older adults specifically about chronic pain; they may not volunteer the info. Chronic pain is not a normal effect of aging. Functional assessment, pain assessment, and med review on all patients- especially elderly COPD is the #1 cause of chronic morbidity & mortality worldwide & the 3rd leading cause of US death COPD risk factors- smoking; occupational & environmental exposures; severe childhood lung infections; GERD, TB, low socioeconomic status Alpha-1 antitrypsin deficiency- extremely rare COPD cause; mostly of northern European heritage. 13 GOLD criteria- consider COPD in anyone with dyspnea, chronic cough or sputum production or above risks COPD- expiratory labor COPD PE: WNL early on then lung hyperinflation, decreased BS, basilar wheezing, distant S1S2 r/t hyperinflation; cyanosis, clubbing, pursed lip breathing, accessory muscles, posturing (lean forward), JVD CAT- 8 items; measure COPD health status impairment CPQ- clinical COPD questionnaire; self-administered; measure clinical control of patients with COPD MMRC questionnaire (Modified British Medical Research Council) breathlessness measurement- relates to other health measures & predicts mortality risk for COPDer CAT, CPQ, MMRC are all adapted from GOLD guidelines Spirometry is the gold standard for diagnosing COPD – do on anyone with s/s > 40 years old- showing persistent airflow limitation Diagnostic aids: CXR, ABG, Alpha-1 angiotrypsin level, high-resolution chest CT, lung volumes and diffusing capacity, pulse ox, exercise testing, and composite scores Stage & severity of COPD based on spirometry pre-& post bronchodilator COPD mgt goals: 1. Id. disease severity (airflow limitation) 2. Id. Health impact of COPD 3. Future event risk GOLD COPD stage Spirometry classification (2014) Stage FEV1:FV C Mild Moderate Severe <0.70 <0.70 <0.70 Very severe <0.70 FEV1 > or = 80% of predicted value 50-79% of predicted value 30-49% of predicted value < 30% of predicted value OR < 50% of predicted value with chronic respiratory failure Pulmonary Differential Diagnoses for COPD/ other: Asthma, Bronchogenic carcinoma, Bronchiectasis, TB, CF, Interstitial lung disease, Bronchiolitis obliterans, Alpha-1 antitrypsin deficiency, Pleural effusion, Pulmonary edema, Recurrent aspiration, Tracheobronchomalacia, Recurrent pulmonary emboli, foreign body Non-Pulmonary Differential Diagnoses for COPD/ other: HF, hyperventilation syndrome/ panic attacks, vocal cord dysfunction, undx OSA, Aspergillosis, chronic fatigue syndrome Med management of COPD: 1. Bronchodilators – don’t slow COPD progression; do increase airflow, decreased WOB, Imp. exercise tol. 2. Bronchodilators a. Beta 2 agonists (LABA, SABA) i. MOA- Stimulate Beta2 adrenergic receptors, increasing cyclic AMP & relaxing airway smooth muscle ii. Adverse effects- tachycardia, palpitations, tremors, cramping, insomnia, hypokalemia, prolonged QT, interval hyperglycemia iii. levalbuterol no advantage over albuterol (per her; in real life levalbuterol has less cardiac effects) b. Anticholinergic aka antimuscarinic (long-acting <LAMA>, short-acting <SAMA>) i. MOA- blocks effect of acetylcholine on muscarinic-type 3 receptors; thus, bronchodilation ii. dry mouth and constipation c. Combinations – slightly increased bronchodilation than either agent alone d. Oral bronchodilator- Theophylline- use if symptoms with inhalers or can’t afford inhalers 14i. Concerns re: toxicity (elderly – hallucination, tachycardia, liver disease, HF) & drug interactions (CYP 1A2, CYP 3A4) ii. Therapeutic range (5-12 mcg/mL) iii. Use slow-release (generic available) 3. Oral corticosteroids a. Poor predictor of long-term response to inhaled steroids in COPD b. Long-term po steroids not recommended for stable COPD. Add inhaled steroids to inh bronchodilators with severe COPD or frequent exacerbation. c. Improve exacerbation frequency, QOL, hospitalization rates- doesn’t slow COPD progression d. Need to use with a LABA for COPD patients 4. Inhaled corticosteroids (ICS) a. ICS monotherapy is only FDA approved for treatment of asthma, not COPD b. Adverse reaction- candidiasis and dysphonia – RINSE after use c. Systemic absorption with high doses (1,000 mcg/d)- bruising, cataracts, reduced bone mineral density. d. Increased pneumonia risk & LABA+ICS no real improvement in exacerbation frequency e. Save ICS for severe COPD - FEV1 of less than 50% predicted 5. Improve spirometry use, Vaccinations (pneumaVAX <55 if smoker/ 65+ if non-smoker), Pulmonary rehabilitation, COPD registry, quit smoking, diet/exercise Agent (Trade name) Albuterol (ProAir, Ventolin, Proventil) Levalbuterol (Xopenex) Salmeterol (Serevent) Formoterol (Perforomist) Arformoterol (Brovana) Ipratropium (Atrovent) Titotropium (Spiriva) Agent class SABA SABA LABA LABA LABA SAMA LAMA Albuterol + Ipratropium (DuoNeb) SABA+SAM A Fluticasone/ salmeterol (Advair) Budesonide/ formoterol (Symbicort) Mometasone/ formoterol (Dulera) Inhaler type (mcg/puff) Dose/frequency MDI (Metered dose) (90) 1-2 inh Q4-6 hrs PRN MDI (45) 1-2 inh Q4-6 hrs PRN DPI (Dry powder) (50) 1 inh BID DPI (12) 1 inh BID N/A MDI (17) 2 puffs q6h DPI (18) 1 inh (DPI)/2 inhalations (SMI-soft mist) QD MDI (90+18) 1 inh QID ICS + LABA DPI (100/250/500+50) 1 inh BID ICS + LABA MDI (80/160 + 4.5) 2 inh BID ICS + LABA MDI (100/200 + 5) NOT FDA ap for COPD (just asthma) Lesson Link to GOLD guidelines https://goldcopd.org/ and https://lms.courselearn.net/lms/CourseExport/files/bb47abfc-cc87-411a-8365- 8471f7735d90/Asthma_and_COPD.pdf differentiating asthma and COPD Great COPD link: https://www.healthquality.va.gov/guidelines/CD/copd/VADoDCOPDPocketCard.pdf 15 Nebulizer Solution 0.63, 1.25 mg/3 mL; 2.5 mg/0.5 mL; 2.5 mg/3mL 0.31, 0.63, 1.25 mg/3mL N/A 20 mcg/ 2 mL 15 mcg/2 mL 0.5 mg/2.5 mL N/A 2.5+0.5 mg/3mLSpirometry measures: Flow loops indicate validity of results, but flow loops WILL NOT be on boards or tests – just included them because they help make sense of the changes in values Spirometry- tech enters age, weight, race, sex & height - when looking at results you don’t need this- it’s pre- calculated in the results Spirometry Results and GOLD classifications: Normal values 16 GOLD classifications post bronchodilatorFEV1 (step 2 grade severity) FEV1 80% to 120% GOLD 1 mild FEV1 > = 80% predicted GOLD 2 moderate FEV1 50% to 79% predicted GOLD 3 severe FEV1 30% to 49% predicted GOLD 4 Very severe FEV1 < 30% predicted FVC FEV1/FVC ratio (step 1 = determine if obstruction) 80% to 120% > 70% (no obstruction) Step 3- Reversibility? A. Test spirometry pre and post bronchodilator (SABA or SAMA) B. Post testing is 10-15 minutes after SABA/SAMA C. ATS criteria: “significant response” is > = 12% FEV1 or FVC improvement and an absolute improvement of > = 0.2 L D. : “significant response” indicates asthma (due to reversibility) Interpreting PFT results Step 1: Check the ratio to see if obstruction exists. Is FEV1/FVC low? <70 = Obstructive defect or COPD Step 2: grade severity with FEV1 post bronchodilation to classify by GOLD criteria GOLD 1 mild FEV1 > = 80% predicted GOLD 2 moderate FEV1 50% to 79% predicted GOLD 3 severe FEV1 30% to 49% predicted GOLD 4 Very severe FEV1 < 30% predicted Step 3- Reversibility Is there a 12% FEV1 or FVC increase post bronchodilation? Yes = reversible TYPICAL PNEUMONIA SYNDROME- (see lesson;Hutt & Kramer, 2002; Furman, Rayner, & Tobin, 2004): Fast fever, cough = new/worse; purulent sputum (rusty, green), pleuritic CP; Lobar infiltrate on chest X-ray (day 2+ - may become infiltrates) indicating pulm consolidation; Consider Streptococcus pneumoniae & other bacterial pathogens ATYPICAL PNEUMONIA- (see lesson; Hutt & Kramer, 2002; Furman, Rayner, & Tobin, 2004): Gradual fever, dry cough, min secretions, HA, malaise, myalgias, pharyngitis, GI distress. crackles (rales); Abnormal or patchy chest X-ray pattern. Consider mycoplasma or chlamydia, pneumoniae, or oral anerobes. Viral pneumonia may be atypical in presentation. Helpful images below from this video (Thanks to Nicole Popovich-Johnson): youtube spirometry video link 17FVC essentially same as VC FVC essentially same as VC. In obstructive lung disease, the graph (image above left) shifts to the left due to increased RV (because of air trapping); VC stays same but TLC increases due to increased FRC and increased RV. line R upper image below – Dotted line is the normal lung, solid lines (shifted left) are obstructive lung spirometry. Restrictive lung disease = lungs don’t fully expand; reduced lung volume & TLC (sarcoidosis, pneumoconiosis, Interstitial lung disease i.e. pulmonary fibrosis; Neuromuscular disease, i.e. MD or ALS); graph shifts to right to due to decreased TLC; In restrictive FEV1/FVC is not as affected as in obstructive disorders ******************************************************************************************* 18Week 2 notes: BPH and BP: Alpha blockers include doxazosin mesylate (Cardura), prazosin hydrochloride (Minipress), and terazosin hydrochloride (Hytrin); If we start on alpha blocker, they should follow up in 4-6 weeks. PROSCAR (finasteride): inhibitor of steroid Type II 5α-reductase, an intracellular enzyme that converts the androgen testosterone into 5α- dihydrotestosterone (DHT). For BPH & male pattern baldness. 19 [Show More]
Last updated: 1 year ago
Preview 1 out of 75 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 08, 2021
Number of pages
75
Written in
Additional information
This document has been written for:
Uploaded
Sep 08, 2021
Downloads
0
Views
57