*NURSING > STUDY GUIDE > NR566 Week 3 and 4 Study Outline Completed docx. (All)
NR566 Week 3 and 4 Study Outline Completed docx.
Document Content and Description Below
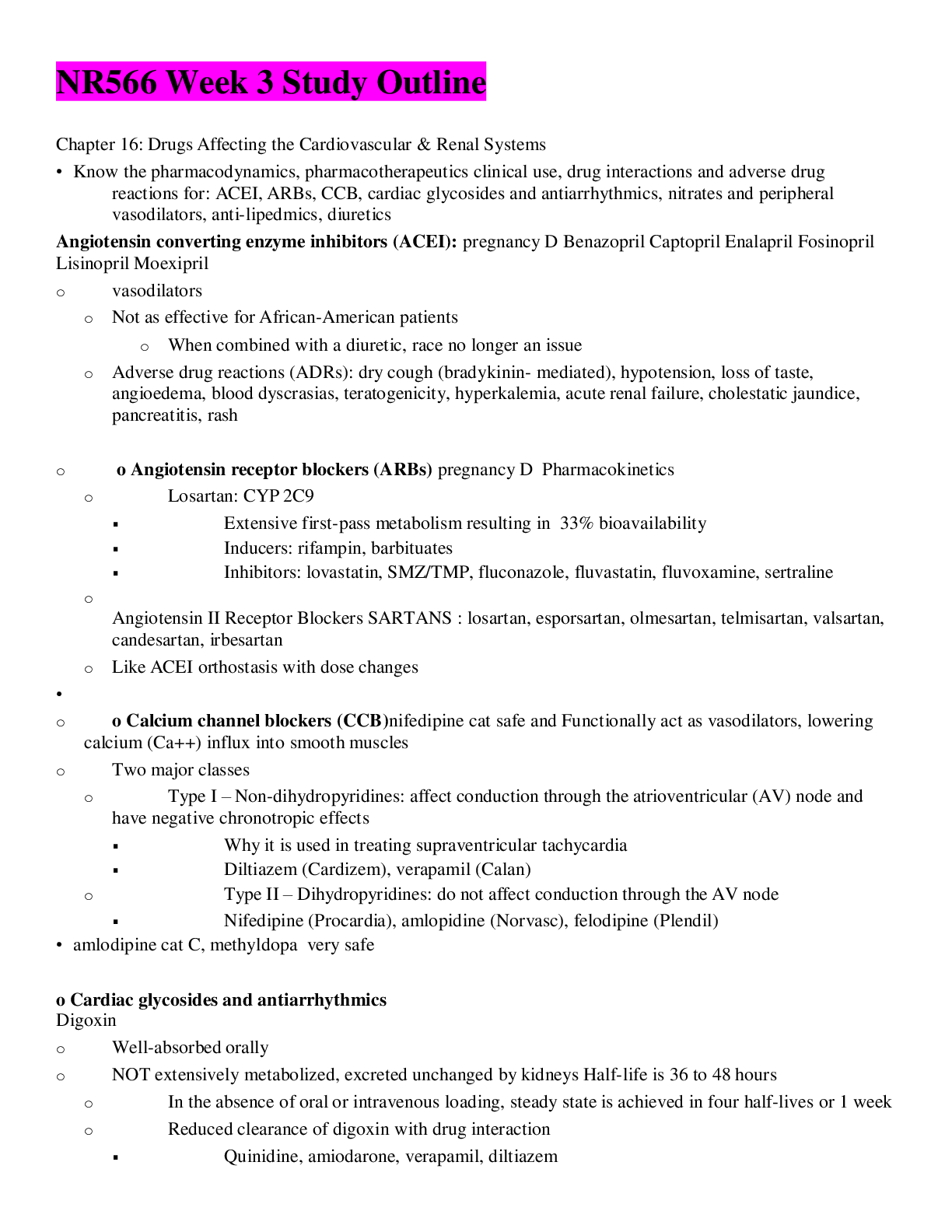
NR566 Week 3 Study Outline Chapter 16: Drugs Affecting the Cardiovascular & Renal Systems • Know the pharmacodynamics, pharmacotherapeutics clinical use, drug interactions and adverse drug react... ions for: ACEI, ARBs, CCB, cardiac glycosides and antiarrhythmics, nitrates and peripheral vasodilators, anti-lipedmics, diuretics Angiotensin converting enzyme inhibitors (ACEI): pregnancy D Benazopril Captopril Enalapril Fosinopril Lisinopril Moexipril o vasodilators o Not as effective for African-American patients o When combined with a diuretic, race no longer an issue o Adverse drug reactions (ADRs): dry cough (bradykinin- mediated), hypotension, loss of taste, angioedema, blood dyscrasias, teratogenicity, hyperkalemia, acute renal failure, cholestatic jaundice, pancreatitis, rash o o Angiotensin receptor blockers (ARBs) pregnancy D Pharmacokinetics o Losartan: CYP 2C9 ▪ Extensive first-pass metabolism resulting in 33% bioavailability ▪ Inducers: rifampin, barbituates ▪ Inhibitors: lovastatin, SMZ/TMP, fluconazole, fluvastatin, fluvoxamine, sertraline o Angiotensin II Receptor Blockers SARTANS : losartan, esporsartan, olmesartan, telmisartan, valsartan, candesartan, irbesartan o Like ACEI orthostasis with dose changes • o o Calcium channel blockers (CCB)nifedipine cat safe and Functionally act as vasodilators, lowering calcium (Ca++) influx into smooth muscles o Two major classes o Type I – Non-dihydropyridines: affect conduction through the atrioventricular (AV) node and have negative chronotropic effects ▪ Why it is used in treating supraventricular tachycardia ▪ Diltiazem (Cardizem), verapamil (Calan) o Type II – Dihydropyridines: do not affect conduction through the AV node ▪ Nifedipine (Procardia), amlopidine (Norvasc), felodipine (Plendil) • amlodipine cat C, methyldopa very safe o Cardiac glycosides and antiarrhythmics Digoxin o Well-absorbed orally o NOT extensively metabolized, excreted unchanged by kidneys Half-life is 36 to 48 hours o In the absence of oral or intravenous loading, steady state is achieved in four half-lives or 1 week o Reduced clearance of digoxin with drug interaction ▪ Quinidine, amiodarone, verapamil, diltiazem o ADRs o Gastrointestinal (GI) most common: anorexia, nausea/vomiting, diarrhea o Central nervous system: fatigue, disorientation, depression, hallucinations, visual disturbances – yellow vision and green halos around lights o Toxicity: atrial arrhythmias/tachycardia in children o Cardiac: bradycardia, premature ventricular contractions, junctional and AV block arrhythmias, and bigeminy o Avoid using in patients with normal left ventricular systolic function o Monitoring o Diagnosis of toxicity is based on both clinical and laboratory data o Toxicity commonly occurs with serum levels greater than 2 ng/mL o Monitor potassium levels • • o Nitrates and peripheral vasodilators nitrates work on veins and reduce preload, hydralazine is a vasodilator • o Anti-lipidemics • o Diuretics treat symptoms of congestions, help the body get rid of excess fluid, reduce symptoms that result in excess fluids like shortness of breath doing this it reduces heart failure (aldosterone inhibitors) • Also know: • o ACEIs & ARBs benefits in other conditionsHTN, HEART FAILURE, SLOWING RENAL DISEASE , CARDIOVASCULAR DISEASE AS WELL • o Dosing schedules • o Management of ACEI side effects • o Therapeutic monitoring for cardiac glycosides and antiarrhythmics • Chapter 28: Chronic Stable Angina & Low Risk Unstable Angina Differentiate between myocardial oxygen supply & demand Angina: Ischemia caused by the imbalance between myocardial oxygen supply (MOS) and myocardial oxygen demand (MOD) produces pain referred to as angina. • Ischemia occurs when demand exceeds supply • Chronic stable angina (exertional angina) is caused by narrowing of the arterial lumen and hardening of the arterial walls so that the affected vessels cannot dilate in response to the increased MOD associated with physical exertion or emotional stres Etiology, diagnosis and risk factors The major risk factors for CAD are age, family history, smoking, hypertension, hypercholesterolemia, low HDL cholesterol, and diabetes mellitus. These risk factors are used in the Framingham equations for calculating the 10-year risk for the development of coronary heart disease (Anderson et al, 2007) and in the new risk equations that aim at uncovering a 7 year risk In addition, conditions that decrease oxygen supply and increase oxygen demand are also major risk factors for ischemic heart disease. These include heart failure anemia), hypertension (hyperthyroidism), valvular heart disease, and morbid obesity. • There are also noncardiac disorders that mimic angina because their primary symptom is chest pain. These include pulmonary embolism, pneumonia, pneumothorax, gastroesophageal spasm or reflux, cholecystitis, peptic ulcer, pancreatitis, rib fractures, herpes zoster, and panic disorder. Some of these disorders also decrease oxygen supply and can cause angina • Women often have symptoms of angina that are atypical and may include fatigue, shortness of breath without chest pain, nausea and vomiting, back pain, jaw pain, dizziness, and weakness ( Grading criteria for levels of angina The lower the class, the more likely the patient's angina can be controlled by lifestyle modification and intermittent nitroglycerin (Table 28-2). The higher the class, the more likely the patient will require multiple drug therapy. The ACC/AHA guidelines have a classification system that incorporates the NYHA/CCS system and additional data. • Class I Proven coronary artery disease without symptoms :::::::: Ordinary physical activity, such as walking or climbing stairs, does not cause angina. Angina occurs with strenuous, rapid, or prolonged exertion at work or recreation. • Class II Angina only with unusually strenuous physical exertion ::::::::::Slight limitation of ordinary activity. Angina occurs on walking or climbing stairs rapidly; walking uphill; walking or stair climbing after meals; in cold wind; under emotional stress; or only during the few hours after awakening. Walking more than two blocks on the level and climbing more than one flight of ordinary stairs at a normal pace and in normal conditions does not cause angina. • Class III Angina during routine physical activity:::::::: Marked limitations of ordinary activity. Angina occurs on walking one to two blocks on the level and climbing one flight of stairs in normal conditions and at a normal pace. • Class IV Angina during minimal activity or rest :::::::::Inability to carry on any physical activity without discomfort. Angina may occur at rest. • • Differentiate between short & long acting nitrates Treatment and rational drug selection low doses of nitroglycerin preferentially dilate the veins more than the arterioles. The resulting decrease in venous return to the heart decreases left ventricular end-diastolic pressure (preload), resulting in decreased wall tension and an increased transmyocardial gradient. This increased gradient improves perfusion between the coronary arteries on the outside of the heart and the subendocardium on the inside of the heart, resulting in increased oxygen supply to the myocardium. • Higher doses of nitrates dilate arterial vessels, which decreases systemic vascular resistance (afterload). Additionally, the higher doses cause further dilation of venous vessels, which results in venous pooling and decreased venous return to the heart. MOD is reduced by the reduced cardiac workload. Nitrates also dilate coronary arteries to some extent, but doing so is difficult in severe atherosclerotic arteries, and this effect is now thought to be only a small part of their action in relieving ischemia. • Drug Choice Favorable Effects Unfavorable Effects Nitrates Heart failure Hypertension Beta-Adrenergic Blockers Heart failure Arrhythmias, atrial tachycardia Hypertension “Stage fright” Migraine headaches Hyperthyroidism Migraine headaches MI Advanced AV block Uncontrolled or severe reactive airway disease Claudication/Raynaud's disease (can use betaj- selective drug) Diabetes mellitus (may try betaj-selective drug) Post-MI Depression ACE Inhibitors Diabetes mellitus Heart failure Hyperlipidemia Hypertension Contraindicated in pregnancy Bilateral renal artery stenosis Angioedema history • Drug Choice Favorable Effects Unfavorable Effects Direct Renin Inhibitors Hypertension Contraindicated in pregnancy Bilateral renal artery stenosis Angioedema history HMG-CoA Reductase Inhibitors (Statins) Hyperlipidemia Hypertension Contraindicated in pregnancy Myopathy history Calcium Channel Blockers Dihydropyridines Hypertension, isolated systolic hypertension Systolic heart failure Peripheral edema Raynaud's disease, peripheral vascular disease Verapamil Atrial tachycardias Advanced AV block Hypertension Constipation Migraine headache Heart failure MI Concurrent use with beta blockers may cause additive bradycardia Diltiazem Atrial tachycardia Advanced AV block Diabetes mellitus Heart failure MI Amlodipine Atherosclerosis Heart failure • Understand which drugs increase myocardial oxygen supply ACE inhibitors also affect both the MOS and the MOD sides of the equation • CCBs primarily affect the supply–demand equation on the demand side of the equation • Beta blockers affect the supply–demand equation on the demand side. Direct renin inhibitors (DRIs) decrease plasma renin activity, thus blocking the conversion of angiotensinogen to angiotensin I. As with ACE inhibitors, this also decreases the thickening of coronary artery walls, resulting in increased MOS • • Statins should be included in the treatment regimen for angina. Their role is on the MOS side of the equation; reduction in LDL cholesterol levels plays a significant role in decreasing the formation of atherosclerotic plaque. • Long-acting nitrate effects For patients who respond well to sublingual or translingual nitroglycerin and who experience angina episodes more than “rarely,” and who are intolerant of beta blockers, long-acting oral or transdermal nitrates are generally indicated. Among the available drugs, the most cost-effective are isosorbide mononitrate (Imdur) given daily or nitroglycerin transdermal patches applied daily with a 10 to 12 hour nitrate-free interval to prevent nitrate tolerance. The timing of the nitrate-free interval should coincide with the time of fewest episodes of angina, which is typically at night. The administration schedule that seems most effective is 7 a.m. and 2 p.m. daily. Headache is the most common adverse reaction but resolves over time. Starting with low doses and slowly increasing the dose reduces the incidence of headache. • Combinations of a long-acting nitrate and a beta blocker are also safe, effective, and low in cost. Their effects are additive, permitting lower doses of both drugs, and their adverse reactions often cancel out. The beta blocker slows any reflex tachycardia caused by the nitrate, which helps to reduce MOD. Combinations of long-acting nitrates and CCBs are rarely used because of the high risk for hypotension and because their adverse reaction profiles are additive. This combination is usually reserved for refractory cases of vasospastic angina. • • Nitroglycerine rationale for route of administration chosen Patient education regarding nitroglycerine use Nitrates are the oldest and best studied of the antianginals, are cost-effective, and have a variety of routes of administration that allow flexibility for the patient. They are more effective than beta blockers in relieving and preventing anginal episodes in patients with vasospastic angina. Nitroglycerin 0.3 to 0.4 mg sublingual tablets or translingual spray is used for immediate symptom relief. All patients with angina should carry some form of rapid-acting nitrate with them at all times. They should be instructed to use this medication at the first sign of angina, even if they are uncertain if the symptoms are angina. If symptoms have not improved after 5 minutes of taking one dose of this drug, the patient should call 9-1- 1 for medical attention. This recommendation has been updated from the previous recommendation of taking up to three doses before calling EMS. This change encourages earlier contacting of EMS by patients with symptoms suggestive of ACS. • Reducing tolerance to nitrate therapy When the drug combination greatly improves angina, it is worthwhile to attempt gradual reduction of prior drug doses over time. For example, if the addition of a beta blocker to high-dose nitrate therapy greatly improves angina, gradual reduction in the nitrate doses can be tried. • • Initial drug therapy recommendations for patients with angina and alternative agents to use when contraindicated • ACE inhibitors and beta-adrenergic blockers are the mainstays of initial drug therapy for patients with angina ( • The second-generation dihydropyridine CCBs (amlodipine and felodipine) and long-acting nitrates can be used for treatment of angina in patients when beta blockers and ACE inhibitors are ineffective or contraindicated • Short-acting, sublingual nitrates can be used in patients with mild, stable CAD for immediate relief on an as needed basis • • Drugs contraindicated in patients with angina Myocardial Infarction Angina is usually associated with CAD, the major underlying mechanism behind MI. Both aspirin and beta blockers have been associated with MI prophylaxis and have the strongest evidence for their use. Aspirin is prescribed as for all patients with CAD. Diltiazem (Cardizem) in its long-acting form has been shown to decrease mortality for patients with non–Q wave MIs. Non-dihydropyridine CCBs should be avoided after MI for patients with poor ejection fractions (less than 40%) because of their negative inotropic effects. Nitrates tend to cause reflex tachycardia. They should be used with caution. • Ch. 36 Heart Failure Heart failure is commonly associated with higher grades of angina. Several drugs used to treat angina also reduce blood pressure and improve myocardial function to reduce the risk for development of heart failure. ACE inhibitors are associated with decreased morbidity and mortality from heart failure and are first-line therapy for that disorder. Their “cousins,” the angiotensin II receptor blockers (ARBs), are being used for treatment of heart failure in patients who cannot tolerate an ACE inhibitor. The negative inotropic effects of beta-adrenergic blockers were thought to make heart failure worse and were avoided in the past. More recent data about their role in reducing sympathetic nervous system discharge have moved them into first-line therapy in heart failure for patients with left ventricular systolic dysfunction • Non-dihydropyridine CCBs should be avoided in heart failure based on their negative inotropism. • • Hypertension All patients with angina should have their blood pressure assessed and managed consistent with the JNC 8 guidelines to a goal of less than 150/90 mm Hg, or 140/90 mm Hg if diabetic (James et al, 2014). Lifestyle modifications are the first approach to treatment of both hypertension and angina. Emphasis is placed on control of weight; reduced intake of sodium, saturated fat, cholesterol, and alcohol; and increased physical activity for both disease processes. All drug classes used to treat angina are helpful in the treatment of hypertension. ACE inhibitors and direct renin inhibitors are useful in blood pressure control based on their vasodilating effects and their ability to reduce extracellular fluid volume. Both of these actions also assist in the treatment and prevention of angina. Beta blockers are no longer first-line therapy in hypertension. • The only class of antianginal drugs that negatively affects hypercholesterolemia is the beta blockers. Nonselective beta blockers can increase triglycerides and LDL cholesterol and reduce the level of HDL. New evidence has shown that cardioselective beta blockers do not have as significant an effect on serum lipids (Singh, Singh, Singh, Jain, & Singh, 2012; Wai et al, 2012). Because of the availability of cardioselective beta blockers, these should be considered for use when there are other compelling reasons for the use of a beta blocker, such as MI prophylaxis • Peripheral-Vascular Diseases The vasoconstrictive effects of nonselective beta blockers have an adverse effect on peripheral blood flow that may limit their use for patients with concomitant peripheral-vascular disease (PVD). Although these drugs are not contraindicated, caution is advised when prescribing this drug class to patients with severe PVD. The peripheral vasodilating effects of the dihydropyridine group of CCBs have resulted in their having an off-label use in the treatment of Raynaud's disease. They are the drugs of choice for patients with concomitant PVD. • ACE inhibitors are the drugs of choice for patients with diabetes. • Asthma and Chronic Airway Diseases Beta blockers in both oral and topical ophthalmic forms may exacerbate asthma and other chronic airway diseases. Although they may exacerbate disease, they should not be avoided unless the patient has severe or uncontrolled airway disease. • Appropriate calcium channel blockers are a good alternative for those patients with severe or uncontrolled airway disease. • The latest evidence, although very limited, states that beta blockers and thiazide diuretics are the drug classes most associated with erectile dysfunction • Nitrates are the cheapest of the antianginals • Betablockers are in the middle • CCBs and ACE inhibitors are the most expensive antianginals. • Initial laboratory studies should include an ECG and fasting lipid profile. Further tests in patients with chronic angina are based on history and physical findings and may include chest x-ray, CT angiography of the coronary arteries, or transthoracic echocardiography (Woodard et al, 2012); complete blood count (CBC); and tests for diabetes, thyroid function, and renal function (ICSI, 2011). Any further laboratory tests are largely based on the need to monitor concomitant disease states. Angina not under control after lifestyle, add nitrate, still not working, add BB for pt with or with out previous MI, add statin for LDL >100 and Add ACE I for pt with LV dysfunction , still not working, add drugs for concomitant disease, still not refer cardiologist • Chapter 36: Heart Failure • Pathophysiology and classification of heart failure • Etiology, diagnosis, risk factors and clinical findings • Differentiate between systolic and diastolic dysfunction and know common causes of each • Drugs to avoid • Diagnostic testing • Treatment and rational drug selection • Limited role of digoxin in treatment • Symptoms of digoxin toxicity • Drugs contraindicate in patients with heart failure • Heart failure treatments according to stage of failure • • Chapter 39: Hyperlipidemia Etiology:. the care focus is expanding beyond just CAD or coronary heart disease (CHD) to include CVD issues of peripheral vascular disease and strokes as equally important endpoints for evaluating therapeutic effect. One-third of the American population is considered to be at high risk for CVD. The perfect storm of an obesity epidemic, uncontrolled hypertension, metabolic syndromes, and rampant consumption of nutritionally risky diets combined with high stress and lack of regular exercise are all components of the problem. • , diagnosis: Atherosclerosis is characterized by deposits of cholesterol and lipoproteins in artery walls. Three major classes of lipoproteins are found in the serum of fasting individuals: low-density lipoproteins (LDL), high-density lipoproteins (HDL), and very-low-density lipoproteins (VLDL). Guidelines for identifying risk for CAD and CVD have traditionally focused on serum cholesterol levels above 200 mg/dL, fasting trigylceride TG levels above 150 mg/dL, and LDL levels above 100 mg/dL. The newest guidelines place a stronger emphasis upon individual risk factors with lifestyle and pharmacological therapies individualized to reduce that risk. , risk factors and clinical findings contribute to Low HDL Cigarette smoking Drugs: beta blockers, anabolic steroids, progestational agents Elevated serum triglycerides Genetic factors (approximately 50% of cases) Overweight and obesity (probably most important) Physical inactivity Type 2 diabetes mellitus Very high carbohydrate intake (>60% of total energy intake) • The therapeutic goal for the management of hyperlipidemia is to reduce morbidity and mortality from CVD by reducing atherogenesis. Research suggests that at least a 30% to 40% decrease in LDL levels needs to be achieved to reach this goal • These risks fall into modifiable and nonmodifiable categories. The modifiable risk factors such as diet, smoking behavior, and exercise are targets of therapy through lifestyle modifications. Nonmodifiable risk factors include age, gender, race, and family history. • In addition to encouraging patients not to smoke, advanced practice nurses need to place emphasis on helping patients achieve optimal weight, BP, and glucose metabolism and to exercise. • Diagnostic testing & monitoring Some experts still recommend also including inflammatory marker control, non-HDL targets, HDL-C levels, TG, and peripheral vascular prevention and stroke prevention targets (Ridker & Cook, 2013). For the first time in the 2013 guidelines, a strong emphasis upon patient involvement in therapeutic decision making and lifestyle interventions to include weight control, exercise, smoking cessation, and taking a long-term look at risk rather than just reacting to disease states. Of critical importance to nurse prescribers is that a laboratory value is not the goal; the reduction of risk and the prevention of CV events is the true target. • Monitoring for effectiveness of dietary therapy involves weight loss, BMI reduction, and lipid lowering. Drug therapy is not usually initiated until a 3-month trial of dietary therapy has been completed; the exception is concurrent drug therapy for those patients with DM or metabolic syndrome. Selection of an agent to treat a lipid disorder is based on a minimum of two lipoprotein levels done 1 to 4 weeks apart during maximum dietary therapy and on individualized risk. This provides a baseline for future evaluation of whether a drug needs to be added to improve treatment efficacy. Baseline lab data (liver function, ALT or AST, and CK) should be gathered before drug treatment begins. Serial monitoring of liver labs are no longer indicated for most patients. • . Levels of serum LDL cholesterol should be evaluated 6 to 8 weeks after initiating therapy. Nicotinic acid is the exception to this rule, with repeat measurements done when the patient's prescribed dose has been stable for 4 to 6 weeks. For all of these drugs, a second measurement of LDL cholesterol levels is done 6 weeks after the first measurement. A minimum of two measurements is used for establishing the efficacy of the treatment plan. For all treatment regimens, if the dose of a drug is increased, or another drug is added to the treatment regimen, the patient's laboratory data should be evaluated in another 6 to 8 weeks. • After the desired LDL cholesterol range is reached, patients should be followed at 8 to 12 week intervals for 1 year. After 1 year of therapy, during which the patient's response to the treatment regimen has been established and there is no evidence of toxicity, patients should be followed at 4 to 6 month intervals. • • Differentiate statins according to strength Treatment and rationale drug selection The following sections blend the new guidelines with the decades of evidence of all risk factors for the prescriber to consider when selecting medications. The higher the CV risk, the more aggressive the statin treatment recommendations in the new guidelines. Any risk prediction over 7.5% is now earmarked as needing a discussion about whether to start statin therapy • Of note in the 2013 guidelines is a recommendation not to use statins in advanced heart failure patients. • Zero to one risk factor LDL lower than 160: TLC initiated and for 3 months ( after 6 weeks LDL panel is redrawn , if LDL is better then continue course if not and LD increase 160-189 then add drug therapu . • Alternative therapies (Omega 3 fatty acids) • Hyperlipidemia medications associated with improved cardiac outcomes • Benefits and mechanism of action for non-statin hyperlipidemia medications • Chapter 39: Hypertension Etiology Hypertension (HTN) is the most common cardiovascular disease in the United States, and it is also a problem worldwide. T Systemic arterial pressure is a function of stroke volume, heart rate, and total peripheral resistance. Alterations in any of these factors result in changes in blood pressure. The major organs involved in regulation of blood pressure are the heart (heart rate [HR] and stroke volume [SV]), the sympathetic nervous system (SNS), total peripheral resistance (TPR), and the kidney (extracellular fluid volume and secretion of renin) Disease processes that affect total peripheral resistance include any that narrow the arteriolar radius or increase blood viscosity This system works well in the maintenance of BP during normal activities; however, in the presence of long- standing HTN, the baroreceptors adapt to the elevated BP levels and “reset” what the body accepts as “normal” BP. Diminished responsiveness to these baroreceptors is one of the most significant cardiovascular effects of aging and a major factor in the lifetime risk of HTN. The level of BP is strongly familial, and studies of rare genetic disorders affecting BP have led to the identification of genetic abnormalities associated with several rare forms of HTN. Evidence suggests that angiotensin II also stimulates growth of vascular smooth muscle and may contribute to atherosclerosis and HTN. , diagnosis Confirmation of a diagnosis of HTN is based on BP elevation documented at three different times. Standard measurement techniques, including out-of-office or home blood pressure measurements, can be used when confirming an initially elevated blood pressure and for all subsequent measures during follow-up and treatment Children over 3 years of age who are seen in a medical setting should have their BP measured at The recommended tests are used for therapeutic decision making and baseline values for determination of progression or stabilization of the systemic impact of HTN: 1. A 12-lead ECG. 2. Urinalysis, including urinary albumin or albumin/creatinine ratio. For those patients with diabetes or renal disease, the latter test of albumin should also be done annually. The presence of albuminuria, including microalbuminuria, even in the setting of a normal glomerular filtration rate (GFR), is associated with increased cardiovascular risk. 3. Blood glucose and hematocrit. 4. Serum potassium. 5. Creatinine and the corresponding estimated GFR. There is a strong relationship between decreased GFR and increases in CV morbidity and mortality . 6. Serum calcium. 7. Lipid profile. Elevated levels of high-sensitivity C-reactive protein (HS-CRP), homocysteine, and heart rate may also be considered in patients with cardiovascular disease (CVD) but without other risk factors. , risk factors the positive relationship between hypertension and CV risk has been long established. The presence of each additional risk factor is assumed to compound the risk from HTN year risk of classic considerations for coronary heart disease (CHD) related to the major risk factors of total serum cholesterol, serum high-density lipid (HDL) level, smoking, diabetes, and left ventricular hypertrophy (LVH). 30% to 65% are obese, a problem frequently compounded by high sodium intake, sedentary lifestyle, and excessive use of alcohol and clinical findings • The first goal of HTN management is reduction in CV risk • The second goal is prevention of this endorgan damage. • Lifestyle modifications directed at correcting these contributing factors may benefit the patient regardless of the primary course of the HTN and are an important part of first-line therapy. Multiple well-controlled trials have shown that a weight loss of as little as 5 to 10 kg can have a significant beneficial effect on HTN • • Treatment and rationale drug selection Normal: <120. <80 encourage lifestyle modification no drugs, Prehypertension: 120-139 80-89 lifesytle modification, no antihypernstive but for compelling indication Hypertension stage 1 140-159 . 90-99 lifestylem thiazide type diuretic for most, May : ACEI, ARB, CCB, or combo Hypertension stage 2. >_ 160. >_100 lifestyle, two drug combo for most, usually thiazide tyoe and ACEI or ARB, or BB, or CCB. The new guidelines emphasize the ACE/ARB family of medications plus diuretics before any other drug group in most cases Diuretics lower BP by depleting the body of sodium and reducing extracellular fluid volume Agents that act in the renin-angiotensin-aldosterone system (RAAS) reduce pressure by decreasing sodium and water retention (aldosterone action), by decreasing vasoconstriction (angiotensin direct action), and by increasing vasodilation (bradykinin action). Adrenergic blockers and other drugs acting on the SNS lower blood pressure by reducing peripheral vascular resistance, inhibiting cardiac contractility, and increasing venous pooling in capacitance vessels. Calcium channel blockers act as vasodilators to reduce pressure by relaxing vascular smooth muscle, thereby dilating resistance vessels and increasing the area over which blood must flow, and through their negative inotropic activity to reduce cardiac output. Direct vasodilators produce the same effect as the calcium channel blockers on vascular smooth muscle Centrally acting agents produce vasodilation mainly through reduction in norepinephrine Angiotensin-converting enzyme (ACE) inhibitors, for example, are drugs of choice in diabetes mellitus, heart failure, and myocardial infarction (MI) Antihypertensives contraindicated in pregnancy ACE inhibitors and ARBs should not be prescribed for pregnant or sexually active girls because of their teratogenic effects. ACE inhibitors, ARBs, and DRI should never be used in pregnancy. • Methyldopa has been studied the most and is typically recommended for women whose chronic hypertension is first diagnosed in pregnancy. Beta-adrenergic blockers are equally effective and are safe during the second and third trimesters, but their use in the first trimester has been associated with growth retardation in the fetus. Labetalol is equally effective as methyldopa and has fewer side effects. If the hypertension is diagnosed before the pregnancy, diuretics and some antihypertensives may be continued Preferred antihypertensives for blacks In African Americans, calcium channel blockers are suggested as first line BP therapy in lieu of the ACE family due to a common lower renin response in this ethnic group If these modifications do not result in achievement of the BP goal, diuretics have been proved in RCTs to reduce morbidity and mortality and are the first agents of choice unless there are compelling reasons to choose another drug class (Gerber et al, 2013). Calcium channel blockers are recommended as first-line therapy for African Americans Contraindications for beta blockers here is increased risk of cardiogenic shock and HF with beta blockers; • Precautions and education for beta blockers not first line therapy b/c they r week when it comes to stroke prevention Antihypertensive step therapy recommendations and monitoring initial monotherapy drug choice is inadequate, several options are considered: (1) maxing out the dose of the first drug, (2) adding another drug, or (3) substitution of a different drug. • “Pseudo resistance” can trick the provider into upping a dose or adding medications when the actual cause is poor adherence, lifestyle factors, and an irregular/improper dosing schedule • JNC 8 hypertension guidelines • Preferred class for initial drug therapy in hypertension treatment : Thiazides diuretics • Added benefits of beta blocker therapy for hypertension • Although HTN is generally accepted to be a lifelong disease, after it has been controlled effectively for at least 1 year, a decrease in the dosage and number of antihypertensive drugs may be considered. The reduction should be deliberate, slow, and progressive and accompanied by vigilant BP monitoring. Step- down therapy is often successful for patients who also are making lifestyle modifications. NR566 Week 4 Study Outline Many questions are written to assess your clinical application of the material from the textbook, in real-world scenarios. Chapter 25: Drugs Used in Treating Inflammatory Processes (p. 801-834 only) • Know the pharmacodynamics, pharmacotherapeutics clinical use, drug interactions and adverse drug reactions for: NSAIDS, ASA, gout medications o Non-steroidal anti-inflammatory drugs (NSAIDs) aspirin, ketoprofen [Actron, Orudis], flurbiprofen (Ansaid), indomethacin [Indocin], piroxicam [Feldene], sulindac [Clinoril]) are mainly selective for COX-1. Some (e.g., ibuprofen [Advil, Motrin], naproxen [Aleve, Naprosyn], diclofenac [Cambia, Cataflam, Voltaren]) are slightly selective for COX-1, and others (e.g., etodolac [Lodine], nabumetone [Relafen], meloxicam [Mobic]) are slightly selec Three COX-2 selective drugs (e.g., celecoxib [Celebrex], rofecoxib [Vioxx], valdecoxib [Bextra]) have been developed that appear not to inhibit COX-1. At that time, a Black-Box Warning was placed on all NSAIDs and on celecoxib related to this risk. All OTC NSAIDs also had their labeling revised to include more specific information about potential GI and cardiovascular risks the well-described, serious, potentially life-threatening GI bleeding associated with their use NSAIDS inhibit cyclo-oxygenase (COX-1 and COX-2) activity, thus inhibiting prostaglandin synthesis. COX-1 is present in all tissues and cells, especially platelets; endothelial cells; the GI tract; and renal microvasculature, glomeruli, and collecting ducts. COX-2 is an "inducible" enzyme that is synthesized mainly in response to pain and inflammation. NSAIDs are primarily used for their anti-inflammatory activity but are also effective analgesics for the relief of mild to moderate pain. Perhaps the most common NSAID is acetaminophen which can be used as an analgesic or an antipyretic. The mechanism of action for acetaminophen is not well-known. However, it is thought to act by inhibiting central and peripheral prostaglandin synthesis. Acetaminophen reduces fever by direct actions on the hypothalamic heat-regulating centers. o Absorption o Rapidly absorbed after oral administration o Food delays absorption. o Acetaminophen is also rapidly and almost completely absorbed after oral administration. o o Metabolism o NSAIDs are metabolized by liver and excreted in urine. o Acetaminophen is metabolized by liver. o When acetaminophen is taken regularly or in large doses, the stores of glutathione become depleted and hepatic necrosis may occur. • Most common ADR: GI disturbances Take with food to reduce GI upset. Monitor for ulcers and GI bleed. • Acute renal insufficiency §Inhibit platelet aggregation and may increase bleeding time • Fluid retention and peripheral edema §Indomethacin may aggravate depression or other psychiatric disturbances. • COX-2 inhibitors and all NSAIDs have Black Box warning for patients related to cardiovascular risk. They may all increase the chance of heart attack or stroke. • Acute hepatic necrosis occurs with doses of 10 to 15 gm. Doses above 25 gm are usually fatal. • Acetaminophen poisoning treatment Refer to poison center. Get acetaminophen level. Oral N-acetylcysteine is a specific antidote for acetaminophen toxicity o Clinical use : Rheumatoid arthritis o Use NSAID or celecoxib to reduce joint pain and swelling. o Follow American College of Rheumatology suggestions for treatment. o Increased risk for complications, so monitor closely o Osteoarthritis o Acetaminophen or NSAIDs can be used for pain. o Gout o Indomethacin, naproxen, and sulindac o Mild to moderate pain o Nonopioid analgesia includes NSAIDs and acetaminophen. o Ibuprofen and naproxen most commonly used o Primary dysmenorrhea o NSAIDs (ibuprofen or naproxen) are drugs of choice. o Tendonitis and bursitis o Indomethacin SR, naproxen, and sulindac o Fever o Ibuprofen is drug of choice. • Drug of choice for mild to moderate pain in Pregnancy Patients with history of GI bleed Aspirin allergy, blood coagulation disorders, upper GI disease • Drug of choice for fever Above adults Children Especially children with fever during flu-like illness • The NSAIDs are Pregnancy Category C (etodolac [Lodine], flurbiprofen, ibuprofen, indomethacin, ketoprofen ketorolac, mefenamic acid, nabumetone, naproxen, oxaprozin [Daypro]), piroxicam [Feldene], sulindac). Diclofenac is Pregnancy Category C before 30 weeks’ gestation and Pregnancy Category D after 30 weeks’ gestation. T • Acetaminophen is Pregnancy Category B. • o Aspirin (ASA) All salicylates have analgesic, anti-inflammatory, antipyretic, and antiplatelet actions. The pharmacological effects are qualitatively similar. Salicylates lower body temperature through their effect on the hypothalamic thermostat and vasodilation of peripheral vessels, thus enhancing dissipation of heat. The anti- inflammatory and analgesic activities are mediated through inhibition of prostaglandin synthesis in the same manner as NSAIDs. However, aspirin more potently inhibits prostaglandin synthesis and has greater anti- inflammatory activity than the NSAIDs. The acetyl group of the aspirin molecule is thought to be responsible for these differences. Aspirin acetylates the cyclo-oxygenase enzyme in the prostaglandin biosynthesis pathway; therefore, it may be theoretically classified as a COX inhibitor. Aspirin also irreversibly inhibits platelet aggregation • Salicylates are rapidly and completely absorbed after oral administration • Salicylic acid is eliminated by renal excretion of salicylic acid and by oxidation and conjugation of metabolites by the liver. • Aspirin has a half-life of 15 to 20 minutes. • Precautions and contraindications • Taking salicylates, especially aspirin, by children or adolescents with influenza or chickenpox has been associated with the development of Reye syndrome, a rare but life-threatening condition characterized by vomiting, lethargy, and eventually delirium and coma • Aspirin should be avoided for 1 week before any surgery because of the increased risk for post-operative bleeding due to its antiplatelet effects. • contraindicated for patients with active peptic ulcer disease or other GI bleeding–related disorders or a history of such disorders. Salsalate and choline salicylate may cause less GI irritation and bleeding than aspirin. Aspirin is Pregnancy Category D Ingestion during pregnancy may produce anemia in the mother and increase the risk for postpartum hemorrhage. Inhibition of prostaglandin synthesis may cause constriction of the ductus arteriosus and other possible untoward effects in the fetus. Avoid use in pregnancy, especially during the third trimester. • After aspirin ingestion salicylate is excreted in breast milk in low concentrations/: avoid high dose • Aspirin should not be used in children with acute febrile illness. Children with dehydration appear more at risk for salicylate toxicity. • • Adverse Drug Reactions The most common adverse reaction to salicylates is GI irritation and bleeding • The amount of blood lost from GI bleeding secondary to salicylate use is usually clinically insignificant, but with prolonged use it can result in iron deficiency anemia. • Aspirin sensitivity is more prevalent in patients with asthma, nasal polyps, or chronic urticaria. • Salicylates are ototoxic at increased blood levels. They should be discontinued if dizziness, tinnitus, or impaired hearing develops. Temporary hearing loss disappears gradually when the drug is stopped. • Aspirin is the salicylate of choice for reduction of fever in adults, mild to moderate pain, RA, TIA, MIs rheumatic fver, juvenile rheumatoid fever, OA • Aspirin is the gold standard against which others are judged. It is inexpensive, available OTC, the most potent analgesic in the class, and short-acting, so acute pain can be managed without long-term effects and adverse reactions. It has limitations, however. It is Pregnancy Category D, especially in the third trimester and contraindicated in children with influenza or chickenpox. ADRs • The most common adverse reactions are ototoxicity and GI irritation and bleeding. Advise patients to report tinnitus; unusual bleeding from the gums; bruising; black, tarry stools; or fever lasting longer than 3 days. Patients who are taking salicylates should not use alcohol or other substances that increase GI irritation. Reye syndrome practically disappeared after the Centers for Disease Control and Prevention (CDC) started warning against giving aspirin to children or adolescents with influenza, influenza-like syndromes, or chickenpox (varicella) because of a possible association with Reye syndrome, a “public health triumph” (Monto, 1999). Parents should be informed of the risk of Reye syndrome and educated regarding not giving aspirin to a child with a viral illness. • o Gout medications Medication Rationale Drug Selection NSAIDs such as naproxen • (500mg twice daily) or indomethacin (50mg three • times daily) • NSAIDs are great for younger patients (less than 60 years old) who do not have a history of renal, cardiovascular or active GI disease. NSAIDs have shown to be effective when used at full doses. NSAIDS are readily available and do not require a prescription so may be favorable for some patients. Oral glucocorticoids or intrarticular glucocorticoid • injection • Corticosteroids if there is a contraindication for NSAIDs Either corticosteroid or NSAID could be used for treatment of a gout flare Colchicine • Colchicine is a reasonable alternative to NSAIDs and is comparable to other agents when taken within 24 hours of the acute flare onset. • Colchicine is associated with gastrointestinal toxicity and can cause nausea, vomiting, and diarrhea. • Colchicine should be administered in a total dose on day 1 not to exceed 1.8 mg, either taken as 0.6 mg three times on the first day or by taking 1.2 mg for the first dose followed by 0.6 mg an hour later; on subsequent days, colchicine is taken once or twice daily until flare resolution. • Colchicine can also be taken daily in reduced doses for prophylaxis. associated with hepatotoxicity. They are not recommended for patients with severe hepatic dysfunction. If patients taking these drugs develop anorexia, weight loss, or pruritus, evaluation of liver function should be part of the diagnostic work-up. GI tract. Symptoms include nausea, vomiting, diarrhea, and abdominal pain. These symptoms are particularly troublesome for patients with a history of peptic ulcer disease or active peptic ulcer disease. • Very few drug interactions Medication Rationale Drug Selection • Pregnancy Category C • Allopurinol is the drug of choice for patients who o Have renal dysfunction o Overproduce uric acid • Although allopurinol is commonly used to decrease levels of uric acid and prevent future episodes of gout, this initial therapy may precipitate an attack. Therefore, concomitant use of colchicine is recommended. allopurinol is widely distributed to tissues. Colchicine concentrates mainly in white blood cells. • Allopurinol acts directly on purine metabolism, reducing the production of uric acid, without disrupting the biosynthesis of vital purines. Allopurinol allopurinol generally leads to a fall in both serum and urinary uric acid in 2 to 3 days. The magnitude of this decrease is dose-dependent. A week or more of treatment may be necessary before the full effects of the drug can be seen. associated with hepatotoxicity. They are not recommended for patients with severe hepatic dysfunction. If patients taking these drugs develop anorexia, weight loss, or pruritus, evaluation of liver function should be part of the diagnostic work-up. Allopurinol is associated with a maculopapular skin rash that sometimes is scaly or exfoliative. The incidence of this adverse reaction is increased in the presence of renal disorders. Because skin reactions may be severe and sometimes fatal, the drug should be discontinued at the first sign of rash. The most severe reactions include fever, chills, arthralgia, cholestatic jaundice, eosinophilia, mild leukocytosis, or leukopenia. Pregnancy Category C Febuxostat • Febuxostat is another option for patients who overproduce uric acid. • Febuxostat is used to treat hyperuricemia in patients with gout. The goal is to have a serum uric acid level of less than 6 mg/ dL. It may take 2 weeks or more to see the effect of febuxostat. Febuxostat absorption is decreased with a high-fat meal, but there is not a clinically significant change in serum uric acid concentration, so it may be taken without regard to food Febuxostat, a xanthine oxidase inhibitor, is contraindicated in patients being treated with drugs requiring xanthine oxidase for metabolism (azathioprine, mercaptopurine, or theophylline) because of increased risk Medication Rationale Drug Selection for toxicity. Pregnancy Category C Uricosuric drugs: Probenecid (PREg B) and sulfinpyrazone (PREG D….do not give unless no other drugs can help) Uricosuric drugs, unlike antigout drugs, increase the rate of uric acid secretion. Both probenecid and sulfinpyrazone inhibit renal tubular reabsorption of urate and thus increase the renal excretion of uric acid and decrease serum uric acid levels. Effective uricosuria reduces the miscible urate pool, retards urate deposition, and promotes reabsorption of urate deposits. Sulfinpyrazone also competitively inhibits platelet prostaglandin synthesis, which prevents platelet aggregation and gives the drug an antithrombotic effect. Both drugs lack anti- inflammatory activity. They are most useful for patients with reduced urinary excretion of uric acid. • robenecid crosses the placenta without producing adverse effects in the fetus or infant. Sulfinpyrazone also crosses the placenta but may be hazardous to the fetus. • GI tract. Symptoms include nausea, vomiting, diarrhea, and abdominal pain. These symptoms are particularly troublesome for patients with a history of peptic ulcer disease or active peptic ulcer disease. • Probenecid and sulfinpyrazone are sulfa-based drugs. They have been associated with hypersensitivity reactions • Probenecid inhibits the tubular secretion of most penicillins and cephalosporins and increases plasma levels by any route these antibiotics are given. Sulfinpyrazone reduces renal tubular secretion of organic anions (e.g., antimicrobials and sulfonamides) and displaces other anions bound extensively to plasma proteins (e.g., tolbutamide, warfarin). • • Also know: o Drug of choice for treatment of gout and most common adverse effects The main adverse reaction for all these drugs is GI distress. Taking these drugs with food or milk may minimize gastric irritation. • Probenecid and sulfinpyrazone are sulfa-based drugs that have been associated with hypersensitivity reactions related to this base. Patients should be asked about sulfa allergies and taught the indications of a hypersensitivity reaction and the importance of reporting it. A hypersensitivity reaction requires immediate discontinuance of the drug. Other symptoms to report with these drugs include sore throat, fatigue, yellowing of the skin or eyes, and unusual bleeding or bruising. These drugs have been associated with blood dyscrasias and hepatotoxicity. • Allopurinol is the drug of choice because it is the only drug in this group that blocks urate production. • Drowsiness and dizziness have occasionally affected patients who are taking allopurinol • • Allopurinol or febuxostat is best for patients who overproduce uric acid • Probenecid is best for pt who undersecrete uric acid ( good renal function) • Sulfinpyrazone is best for pt who undersecrete and need antiplatelet • o Role of NSAID use in treatment of gout: indomethacin, naproxen, sulindac and ibuprofen and ketoprofen • o Gout medications that require renal or hepatic dose adjustments • Colchicine: renal and hepatic • Allopurinol: renal and hepatic • Febuxostat: liver function test at 2 and 4 months • o Allopurinol drug interactions and medications to avoid • avoid concurrent use, ACEI:, aluminum salts, ampicillin Separate administration anticoags (use warfarin), cyclophosphamide ( if used monitor bleeding) , theophylline, select different respiratory drug thiazide diuretics (avoid concurrent use), thiopurines, ( avoid concurrent use ) uricosuric agents (dosage adjustments ) o Signs of aspirin toxicity Respiratory alkalosis is seen initially. Hyperpnea and tachypnea occur as a result of increased CO2 production and a direct stimulatory effect of the salicylate on the respiratory center in the brain. Other symptoms include nausea, vomiting, hypokalemia, tinnitus, disorientation, irritability, seizures, dehydration, hyperthermia, thrombocytopenia, and other hematological disorders. Treatment for salicylate toxicity includes induction of emesis or gastric lavage to remove any unabsorbed drug from the stomach. Activated charcoal diminishes salicylate absorption if it is given within 2 hours of ingestion. Salicylate levels and acid–base, fluid, and electrolyte balances are carefully monitored. The rest of therapy is supportive. Forced alkaline diuresis by administering sodium bicarbonate increases salicylate excretion. Hemodialysis is reserved for those patients with severe poisoning Aspirin may potentiate the anticoagulant action of heparin, warfarin, or thrombolytic agents • • Acetaminophen is a common cause of poisoning, either intentional or accidental, due to the lay public's underestimating the toxicity of the drug. A single dose of 150 mg/kg of acetaminophen in children or 7.5 g to 10 g in adults may be toxic • • Week 4 contains the midterm exam which covers content from weeks 1, 2, 3 & 4. Be sure to use the study outlines from weeks 1-3 along with this outline to prepare for the exam. [Show More]
Last updated: 1 year ago
Preview 1 out of 17 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 22, 2021
Number of pages
17
Written in
Additional information
This document has been written for:
Uploaded
Oct 22, 2021
Downloads
0
Views
27




.png)