NURSING NUR2633 Maternal Child Health Final Exam 1,2&3,100% CORRECT
Document Content and Description Below
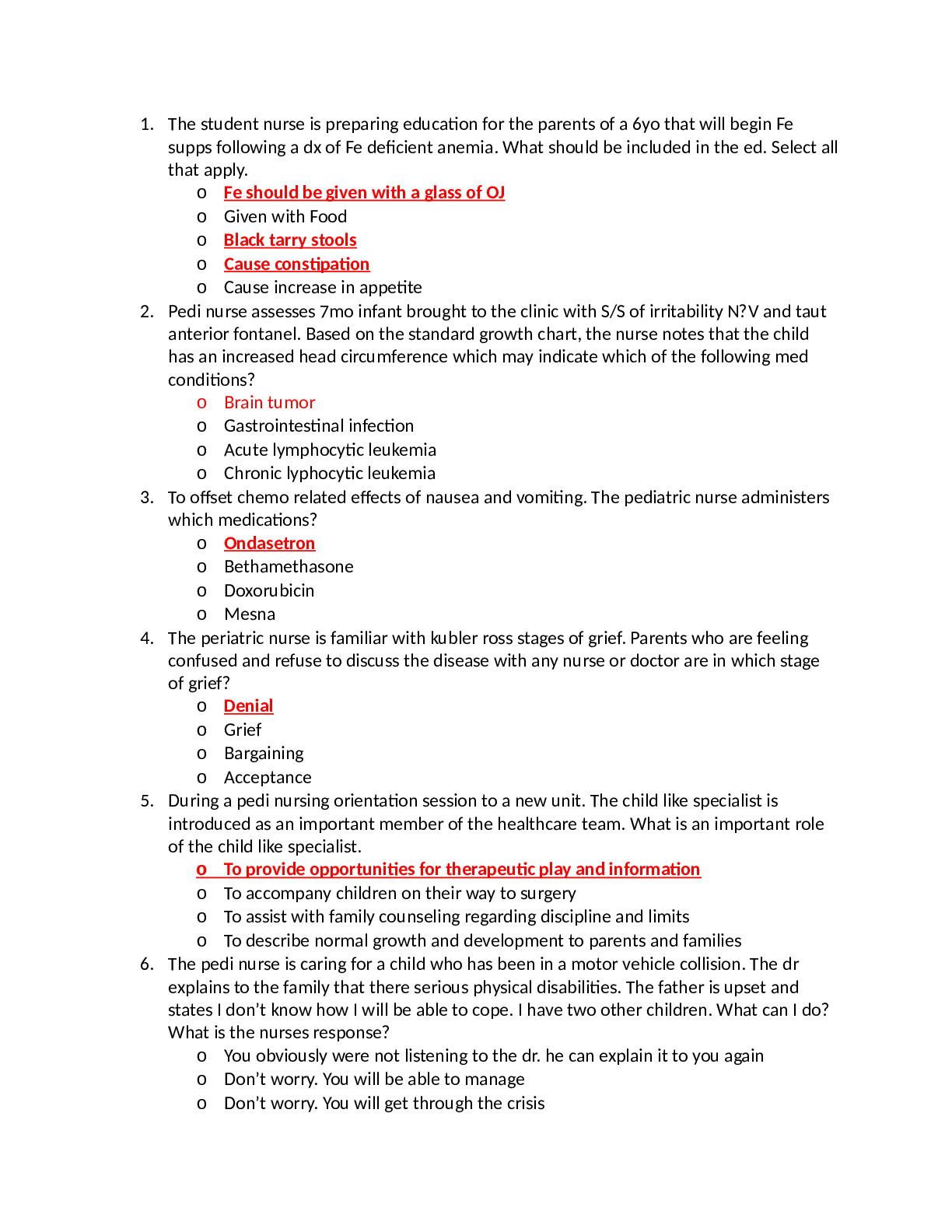
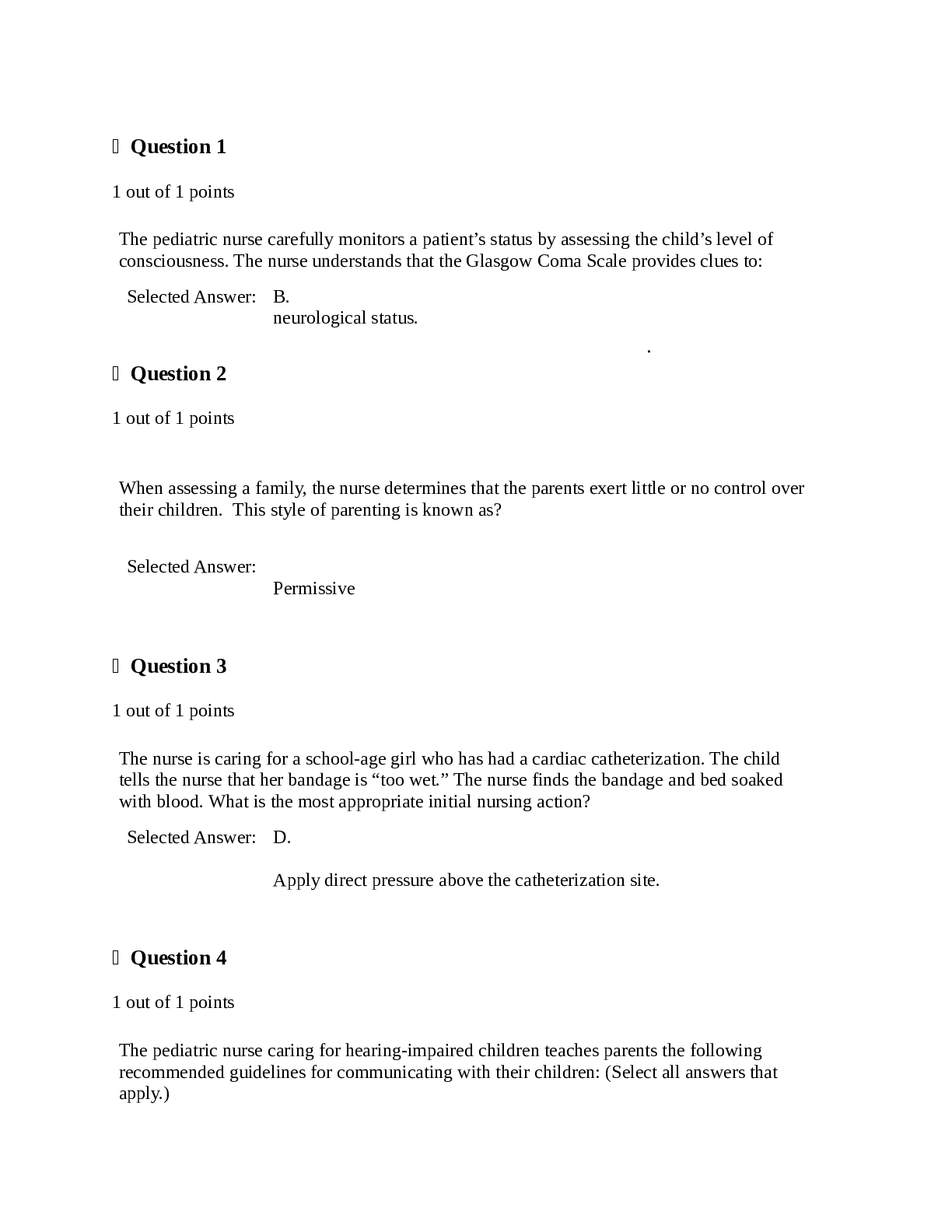
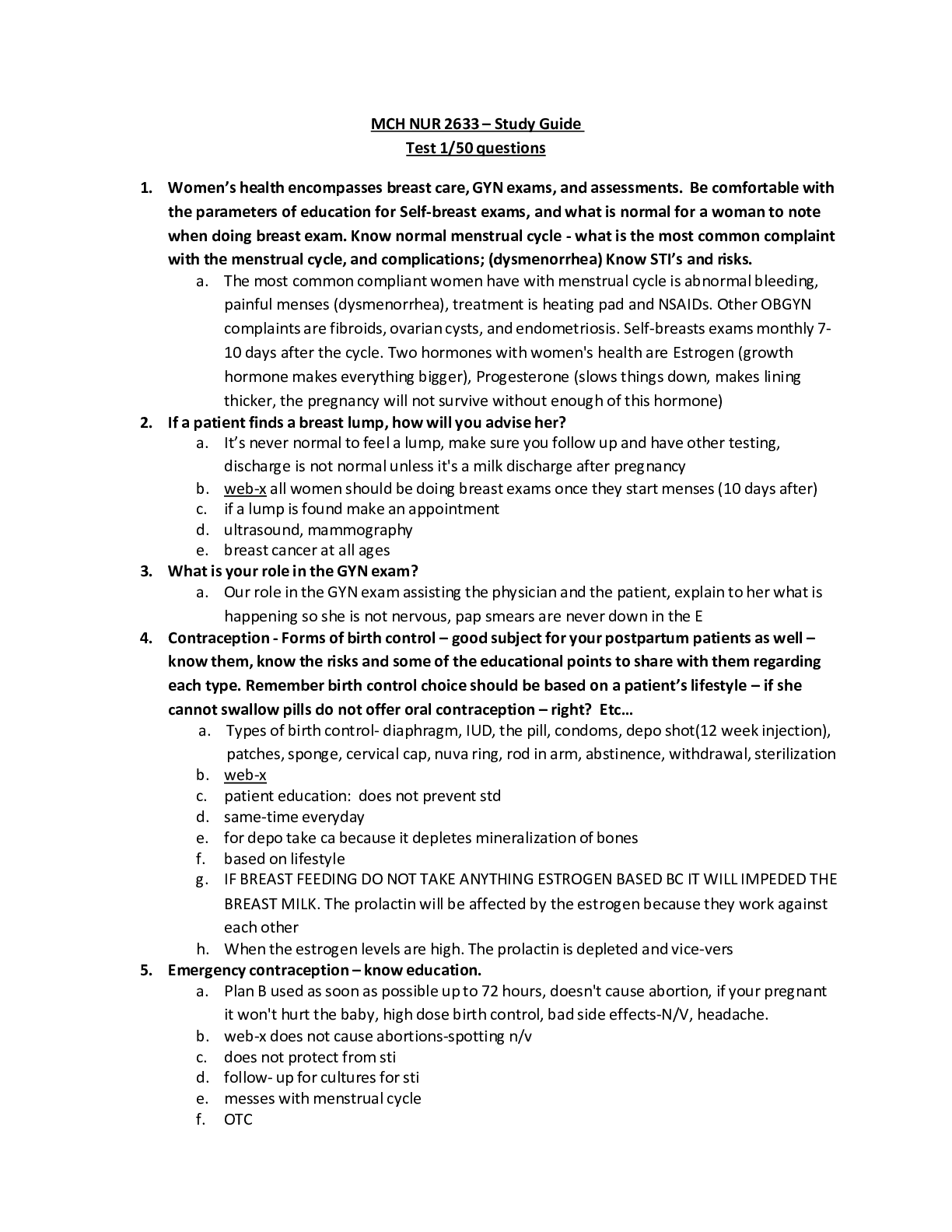
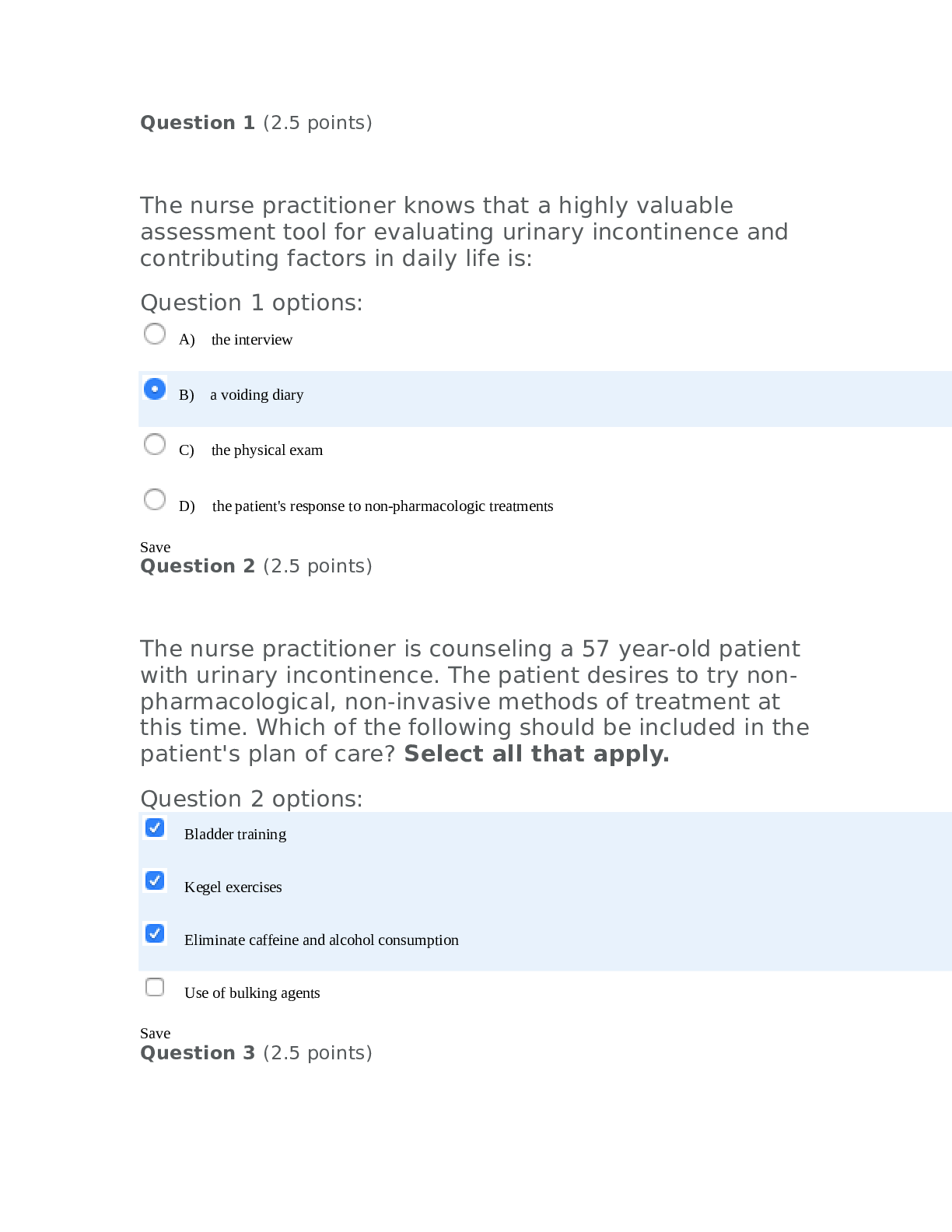
NURSING NUR2633 Maternal Child Health Final Exam 1,2&3 • Quickening: o Maternal awareness of fetal movement ▪ 17-20 weeks • Toxoplasmosis: o Associated with the consumption of infested... undercooked meat and poor hand washing after handling cat litter ▪ Educate on having someone else change the cat’s litter pan and to avoid consuming uncooked meat • Blood Volume: o Because of the increase in plasma the hematocrit will appear low, especially at 32-34 weeks gestation. A hemoglobin of 11.2 and hematocrit of 38% would be considered normal • Natural Family Planning: o Identifying the fertile time during the cycle and using abstinence or other contraceptive methods during the fertile period requires motivation and considerable counseling • IPV (Intimate Partner Violence) o Nurse should routinely screen all of their patients. Using words such as, “do you feel safe in your current environment and relationships?” • Recreational Drugs o The use of these drugs can harm the fetus, causing miscarriage/spontaneous abortion and low birth weight • First Prenatal Visit (3) o The patient has appropriate questions for her potential provider that include: ▪ The opportunity to use complementary and alternative methods during labor and birth ▪ And opportunity to meet other providers in the practice ▪ The health care provider’s beliefs and practices concerning epidural anesthesia the routine use of episiotomy • Quadruple Screen: o Screening test to determine birth defects ▪ Screens for 4 pregnancy hormones ▪ Normal Results o Usually done between the 15th and 22nd week ▪ Most accurate between the 16th and 18th week o Abnormal result does NOT mean baby has a birth defect ▪ Most testing should be done ▪ If the test is abnormal, you may want to talk or have a referral fo a genetic counselor • Vegetarian Diet: o Recommend vitamin B12 and iron supplements • Emergency Contraceptive: o Nausea and vomiting is a common side effect, an over the counter antiemetic can be taken 1 hour before each contraceptive dose to prevent nausea • Primary Dysmenorrhea (cramps): • The use of non-steroidal anti-inflammatory drugs (NSAIDS) as an optimal pharmacological therapydms sSSvestational Diabetes Mellitus: o Recommend that all pregnant women be screened during the 24th and 28th weeks of gestation vdcd • Mother’s Blood Sugar: o Infants who are producing more insulin because of the high maternal glucose develop MACROSOMIA (meaning big body) • Side-Lying Position: o Side-lying in the lateral position decreases pressure on the vena cava and is common instruction given to increase venous return and increases fetal circulation, circulatory volume and placental and renal perfusion • Fundal Height: o 14 weeks is slightly above the symphysis pubis • Urgent Reportable Signs in Pregnancy: o Vaginal bleeding o Rupture of membranes o Headaches that do not respond to usual therapy • GTPAL o GRAVIDA- pregnant woman o Term- carried to term o P- number of preterm deliveries o A- number of abortions/spontaneous or induced o L- number of living children • Cardiac Output: o Increases and peaks around 20-24th week (second trimester) o Frequently it is 10-15 beats higher to facilitate the extra volume • EDD or EDB o Naegele’s Rule: ▪ Subtract 3 FULL months + 7 days • Nutritional Counseling: o Essential nutritional elements are protein, iron, folic acid, calcium and water • Breast Self-Exam: o Step 1: exam with arms down o Step 2: exam with arms up o Step 3: signs of fluid discharge o Step 4: feel while lying down o Step 5: feel while sitting or standing • Nausea and Pregnancy: o Avoid trigger foods o Small frequent meals, plain dry crackers, remaining upright after eating Exam 2 • Newborns Addicted to Drugs: o INCESSANT CRYING • Fractures Can Occur from Birth: o Large babies can become lodged in the birth canal, and the CLAVICLE can fracture during the process of birth • Spinal Anesthesia- Epidural (4): o Intake and Output o Blood Pressure o Respiratory Rate o Fetal Heart Rate • Preeclampsia: o Nursing care would include administering magnesium sulfate according to the agency policy • Assessment of Postpartum Woman (3): o Assessment of pain and provide pain medication o Ongoing physical assessment o Notification to the provider if the RR is still elevated an hour after med admin • Mental Health Questions: o Ask to hear about how things are going in their own words. o Use words like, “tell me about…” • Erythromycin Ointment and Vitamin K: o Start at the inner cannulas and move to the outer cannulas o Dab excess on the skin, but DO NOT wash it away • Symptoms of Early Labor: o Excited or irritable related to answering multiple questions about contractions o Her pulse rate will be 100 beats per minute o Her pulse rate will be 100 beats per minute • Headache and the Postpartum Patient: o INQUIRE about the location and the severity of the headache • Fetal Monitor Indicates Late Decelerations: o Change positions ▪ NOT on back o Turn Pitocin off if it was running o Decelerations always need to be documented but should have an ACTION by the nurse o Oxygen may be administered by face mask (8-10 L/min) • Afterpains: o When baby breastfeeds, the uterus contracts and feels just like a labor pain • Interventions: baby has blue tinge to lips, gums and tongue 4 hours after birth (3): o Monitor vital signs o Oxygen therapy o Request an echocardiogram • Blood Pressure Drops When Prepping for Spinal Anesthesia: o Do NOT place patient in supine position o Place a wedge under the patient’s left hip • Jaundice: o Discoloration may be noted on the skin surface, sclera and mucus membranes • Precipitous Delivery: o Happening very quickly o the single thing that will save the mother’s life: ▪ massage the uterine fundus with continual lower segment support • Preterm Labor: o Corticosteroid therapy is presently the only treatment shown to improve fetal survival when given to a woman in preterm labor between 24-33 weeks • Betamethasone: o Corticosteroid o Given to mom to help baby’s lungs mature • Mother does not want to really touch her infant: o Do not correct her or tell her how to act or feel o We would SUPPORT the mother in her reaction to the newborn • Discharge instructions for a C-Section: o Only lift the weight of the baby for 2 weeks o Abdominal exercises are not recommended until 6 weeks post-op • Preterm Rupture of Membranes: o The nurse will: ▪ Monitor fetal heart rate ▪ Administer antibiotics ▪ Monitor vital signs ▪ And do a SPECULUM EXAM • Not a vaginal exam • Jaundice (HYPERBILIRUBEMIA): o Inadequate intake may lead to jaundice ▪ Encourage the frequent feeding of breastmilk to avoid this • Blood pressure and Pregnancy: o High blood pressure: ▪ Hypertension o Chronic Hypertension: ▪ Hypertension that was present before becoming pregnant o Gestational Hypertension: ▪ High blood pressure that first occurs in the second half (after 20 weeks) of pregnancy o Problems that occur due to hypertension: ▪ Fetal growth restriction ▪ Preeclampsia ▪ Preterm delivery ▪ Placental abruption ▪ Cesarean delivery o How is chronic hypertension during pregnancy managed? ▪ Ultrasound exams may be done throughout pregnancy ▪ Usually begins during the 3rd trimester ▪ NON Stress Tests (NST) • Preeclampsia: o Due to high blood pressure o Signs: ▪ Proteinuria ▪ Low platelet count o Usually occurs after 20 weeks pregnancy ▪ During the 3rd trimester ▪ If before 32 weeks it is called early-onset preeclampsia o Causes: ▪ First pregnancy ▪ Hx of preeclampsia ▪ Hx of chronic HTN ▪ Over 40 ▪ Carrying more than one baby ▪ Certain medical conditions such as: • Diabetes, thrombophilia, lupus ▪ Obesity ▪ In vitro fertilization o Risks for baby: ▪ May need immediate delivery ▪ Preterm = complications o Risks for mother: ▪ Increased risk of cardiovascular disease and kidney disease ▪ Can lead to seizures, also known as eclampsia ▪ Can also lead to HELLP Syndrome o Management: ▪ Corticosteroids ▪ Meds may also be given to lower blood pressure and to help prevent seizures • HELLP Syndrome: o Hemolysis, Elevated Liver enzymes, and Low Platelet count • Reason to not give an epidural: o Decreased platelet count ▪ Platelets less than 90,000 (100,000 is considered low normal) • What to administer before an epidural: o Rapid IV infusion of 500 mL of normal saline ▪ Avoid bradycardia in baby and sudden drop of blood pressure from mother • A woman gave birth to twins via c section who was on bedrest prior to delivery, has a known venous clot in the leg. She states that she feels” very anxious and has pain in her chest” (Classic symptoms of a pulmonary emboli) Her respiratory rate is 28. o The first thing you should do: SUMMON HELP • Emergencies During Labor (3): o Cord prolapse: ▪ Cord presents before the baby o Placenta may abrupt o Uterus may rupture • When the patient has a deceleration: Noted in the question as a non-reassuring fetal heart rate: o The best answer would be to have the mother change position, left lateral if not already there EXAM 3 • How to assist a child to cope? o When a parent does everything for a child, this does not allow the child to learn • Play: o Parallel Play: ▪ Toddlers play with the same materials but do not play together- two children playing with trucks next to each other o Associated play: ▪ Preschoolers- loosely organized with our organization, division of labor, or mutual goal- helps children learn to share, simple rules and concepts • Airway: o Stridor or frog-like noises can occur when the airway is compromised o It is important to maintain the airway • Cystic Fibrosis: o Describing to a parent would include: ▪ Thick mucus that affects exocrine glands and several body systems ▪ Increased mucous production causes obstruction and stasis of fluid, providing a rich habitat for growth ▪ In later childhood, the reproductive system is affected as ovarian ducts and vas deferens may be occluded, leading to infertility • Infantile Colic: o Irritability and fussiness about the same time every day, usually during the late afternoon of evening. o Infant pulls both legs and arms into a flexed position. • Food Fads: o Are normal and this tendency will pass • Contraindications to vaccinations: o A previous severe allergic reaction to the vaccine • Health teaching for immunosuppressed children: o Teaching the parents the benefit of hand washing is an important measure • Teaching for children with diabetes (3): o Diet o Insulin o Exercise • Glascow Coma Scale: o A pediatric scale to assess neurological status ▪ Eye opening, verbal response, motor response • Communication with hearing impaired children: o Talk slowly and loudly o Obtain the child’s attention before speaking o Be at eye level • Sprained ankle: o Apply ACE wrap to apply pressure and reduce swelling at the joint • Communication with a very young child: o Use a doll or toy as a transition object • Minimizing separation anxiety in a hospitalized toddler? o Encourage the parents to room in • Best drug to use immediately post-op: o Morphine • Debridement of burn wounds: o Fentanyl and Midazolam can be given for pain relief • Burn Injury: o Primary complication is infection • Anemia: o Nursing diagnosis: ▪ Activity intolerance related to generalized weakness • Children with Renal Failure: o At risk for water and sodium retention • Sickle Cell Disease: o Chronic lifelong illness o Nursing interventions (2): ▪ Hydration ▪ Pain management • Nursing care in cardiac catheterization: o Direct pressure above the catheterization site • Urinary tract infection: o Predisposition: ▪ Short urethra in young girls • Hydrocephalus: o Recognition: ▪ Bulging fontanel and dilated scalp veins • Discipline (3): o Younger child: ▪ Distraction o Older Children: ▪ Removal of privileges ▪ Consequences for actions • Genetic Testing: NEW MATERIAL o All women should be asked about their family and genetic history ▪ Further tests depending on information provided o Pregnancy Associated Plasma Protein-A (PAPP-A) and free b-Human Chorionic Gonadotropin (free b-hCG) during the 1st trimester o Triple screening and quadruple screening during the 2nd trimester o Screened for potential neural tube defects, trisomy 13, trisomy 18, trisomy 21 o If positive, REFER TO A GENETIC SPECIALIST for further testing and counseling • Vegetarian Diet: o Diet includes vegetables, fruits, legumes, nuts, seeds and grains o Some include fish, poultry, eggs and dairy ▪ No beef or pork o Ovolactovegetarians: ▪ Consume plants and dairy products o Pregnant: ▪ Lack adequate amounts of IRON and ZINC ▪ B-12 Deficient ▪ Counseled to consume vitamin B-12 fortified supplements • Soy milk • B-12 Supplements ▪ Nutritional counseling and ongoing assessment of maternal weight gain and lab testing for anemia to ensure maternal-fetal well-being • Factors that Contribute to Fatigue: o 1st Trimester: ▪ Increased production of progesterone • Causes fatigue- particularly during the day ▪ Increased blood volume • Can result in anemia ▪ Women with decreased iron stores • “true” iron-deficient anemia ▪ Fetal development: • Increased need for oxygen • Increased workload demands ▪ Emotional stress o 2nd Trimester: ▪ Normally increased energy and endurance • Able to focus on planning ▪ Causes of fatigue: • Depression, anemia, external stressors o 3rd Trimester: ▪ Maternal weight-bearing load increases ▪ Decreased lung expansion ▪ Increased pressure on the bladder • Voiding at night during sleep • Signs of Danger: o Severe and persistent vomiting may be a sign of hyperemesis gravidarum ▪ Risk for weight loss and dehydration ▪ Managed with fluids, small frequent meals, emotional support ▪ Dehydration may require IV fluids and hospitalization o Abdominal cramping and vaginal spotting or bleeding may indicate a spontaneous abortion (before 20 weeks gestation) o Preeclampsia: ▪ Increased blood pressure after 20 weeks gestation ▪ Early signs and symptoms: • Headache • Vision changes • Elevated BP • Edema ▪ May include seizure precautions: • NURSE WOULD ADMINISTER MAGNESIUM SULFATE ACCORDING TO AGENCY POLICY o Premature rupture of membranes before the onset of labor: ▪ Monitor for signs of infection ▪ DO NOT PERFORM A DIGITAL EXAM (only speculum) o Gestational diabetes: ▪ Get screened between 24 and 28 weeks • Glucose challenge test ▪ Increased risk of macrosomia • Newborn at Risk: o Respiratory system: ▪ Fetal lung maturity ▪ 35-36 weeks gestation newborns are at risk of respiratory distress syndrome (RDS) o Circulatory system: ▪ In utero fetal blood is shunted from the lungs and liver and supplied to the rest of the body, such as the brain and the heart to accomidate rapid growth ▪ At birth, 3 shunts close (ductus arteriosus, foramen ovale, and ductus venosus) circulation converts to adult circulation o Neurological system: ▪ Newborns are immature because of limited synaptic and dendritic interconnections in the brain and immature myelination of the nerve cells ▪ Preterm newborn has increased risk for neurological immaturity • results in inability to cope with stimuli at birth ▪ Deficits can be short or long term • Neonatal Abstinence Syndrome: o Drugs can cross the placenta: ▪ Long half-life in fetal circulation ▪ Bind to CNS receptors ▪ Cause cell damage o S/S: ▪ INCESSANT CRYING, irritable, tremors, loose stools, sneezing and stuffy nose o Provide quiet and dark environment, gently rock and hold infant, provide comfort and security o Assess every 3 hours ▪ NAS scoring system • Score of 7 or higher for 3 consecutive scorings = o Uncomfortable and need medication o Mothers addicted to methadone are encouraged to breastfeed to offset withdrawal symptoms in newborn o DON’T USE NARCAN ▪ Can increase the severity of withdrawal ▪ If infant is in distress at the time of delivery, use positive pressure O2 • Pediatric IV line: o Peripheral IV is short-term o PICC lines are long-term • Tonsillitis: o Prevention: ▪ Good handwashing ▪ Avoid second hand smoke and crowded places during flu season ▪ Avoid touching eyes and nose o Nursing care: ▪ Cool mist humidifiers ▪ Warm saline gargles ▪ Throat lozenges ▪ Antipyretics o Surgery: ▪ Removal of tonsils • Have to lay on side to facilitate drainage • Avoid coughing, blowing nose and clearing throat • Check secretions and vomitus for fresh blood • Can put ice pack on neck ▪ First given cool water, crushed ice, flavored ice pops ▪ Then given gelatin, cooked fruit, sherbet, mashed potatoes ▪ Avoid red/brown fluids/foods ▪ Avoid milk, ice cream, pudding • They coat the throat causing the child to clear throat and may bleed ▪ Sign of bleeding: • Continuous swallowing • Croup: o Larynx, trachea and bronchi ▪ Marked by swelling and erythema o Most often in children aged 2 ▪ More common in boys in winter months o Can lead to obstruction ▪ Decrease in airway diameter and narrow larynx • Influenza: o Both A and B can cause epidemics ▪ They mutate and create new strains o Spread by droplet ▪ Cough, sneeze, talking o Preventions: ▪ frequent hand washing ▪ covering the mouth and nose when sneezing or coughing ▪ properly disposing of used tissues ▪ avoiding close contact with persons who may have become infected ▪ Influenza vaccines are now widely used for prevention. • Two routes: o IM and nasal spray o Nursing Care: ▪ Emphasize adequate sleep and rest ▪ increased fluids and electrolyte solution ▪ teach importance of annual vaccination • Appendicitis: o S/S: ▪ Pain around the umbilicus, pain awakes child, followed by pain in RLQ, rebound tenderness with pain over McBurney’s point, guarding o Perforation is suspected when pain is relieved without intervention ▪ If perforated: will need post-op antibiotics o Nursing care: ▪ Monitor intake and output ▪ Wound care ▪ Pain control ▪ NPO for 24 hours or until peristalsis returns ▪ Keep the wound clean and dry • Sports injury: o Prevention: ▪ Pre and post stretching ▪ Wear helmet • Blood Transfusion Therapy: o Conditions that delay therapy: ▪ Fever ▪ Lack of IV access ▪ Child is unable to be closely monitored by staff ▪ Complex medication regimen o Transfusion must be started within 30 minutes after leaving the blood bank. ▪ The max time for infusion is 4 hours because of the risk for bacterial contamination and cell lysis o Check to see if any premedications were ordered before administration o Use PPE: ▪ Goggles and gloves o All blood products must be checked at the patient’s bedside by two HCP and using two patient identifiers o Start the infusion slow for the first 15 minutes ▪ Stay with patient for 15 minutes o Do not infused any other solutions at the same time with blood through the same IV line ▪ only exception is NS o Don’t add medications to blood o Jehovah witness: ▪ opposed to receiving blood and blood products. ▪ They cannot have it re-infused if removed from the body so self-donation is also prohibited [Show More]
Last updated: 1 year ago
Preview 1 out of 30 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$15.00
Document information
Connected school, study & course
About the document
Uploaded On
Oct 31, 2021
Number of pages
30
Written in
Additional information
This document has been written for:
Uploaded
Oct 31, 2021
Downloads
0
Views
88