*NURSING > STUDY GUIDE > STUDY GUIDE for C475 Care of Older Adult Objective Assessment / Exam questions are taken from the Le (All)
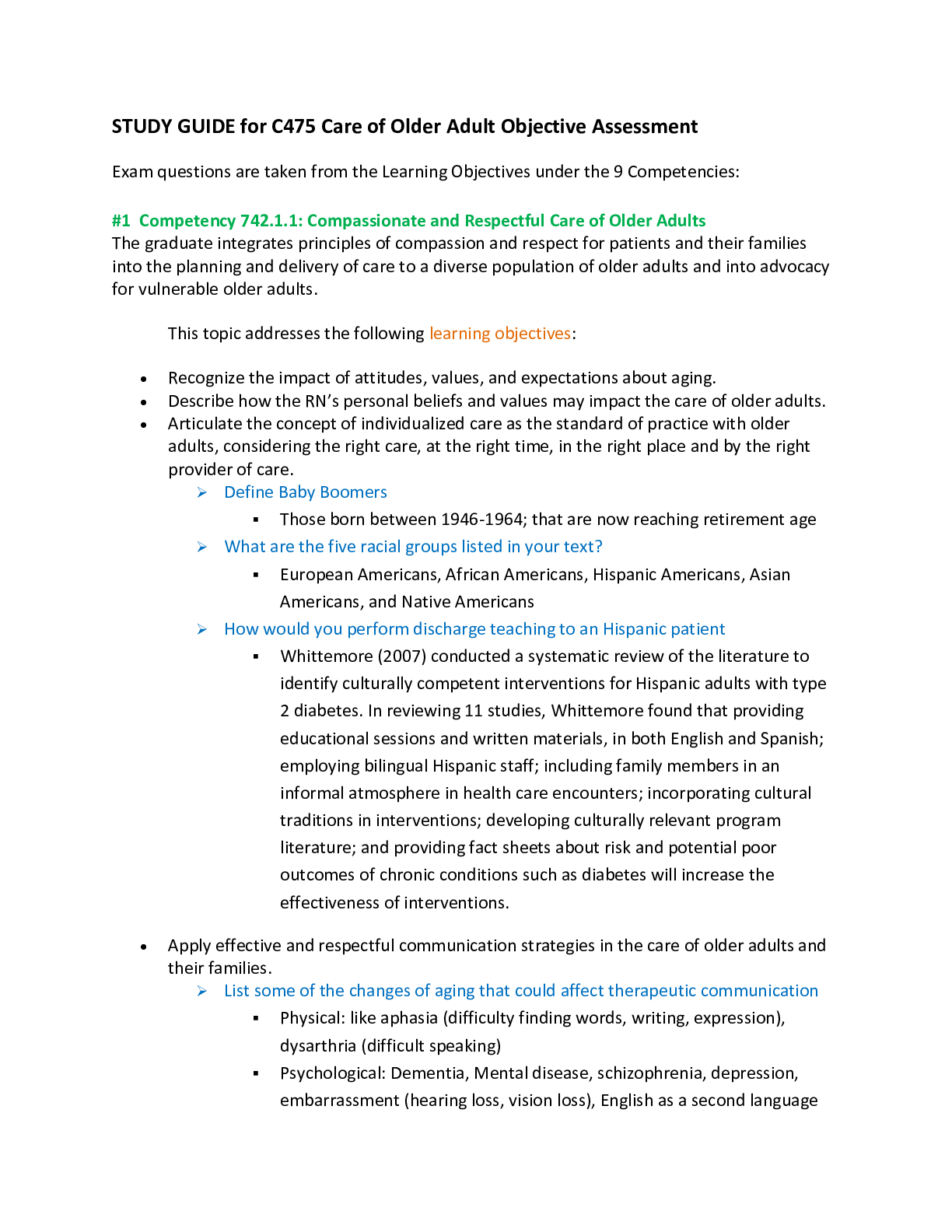
STUDY GUIDE for C475 Care of Older Adult Objective Assessment / Exam questions are taken from the Learning Objectives under the 9 Competencies.
Document Content and Description Below
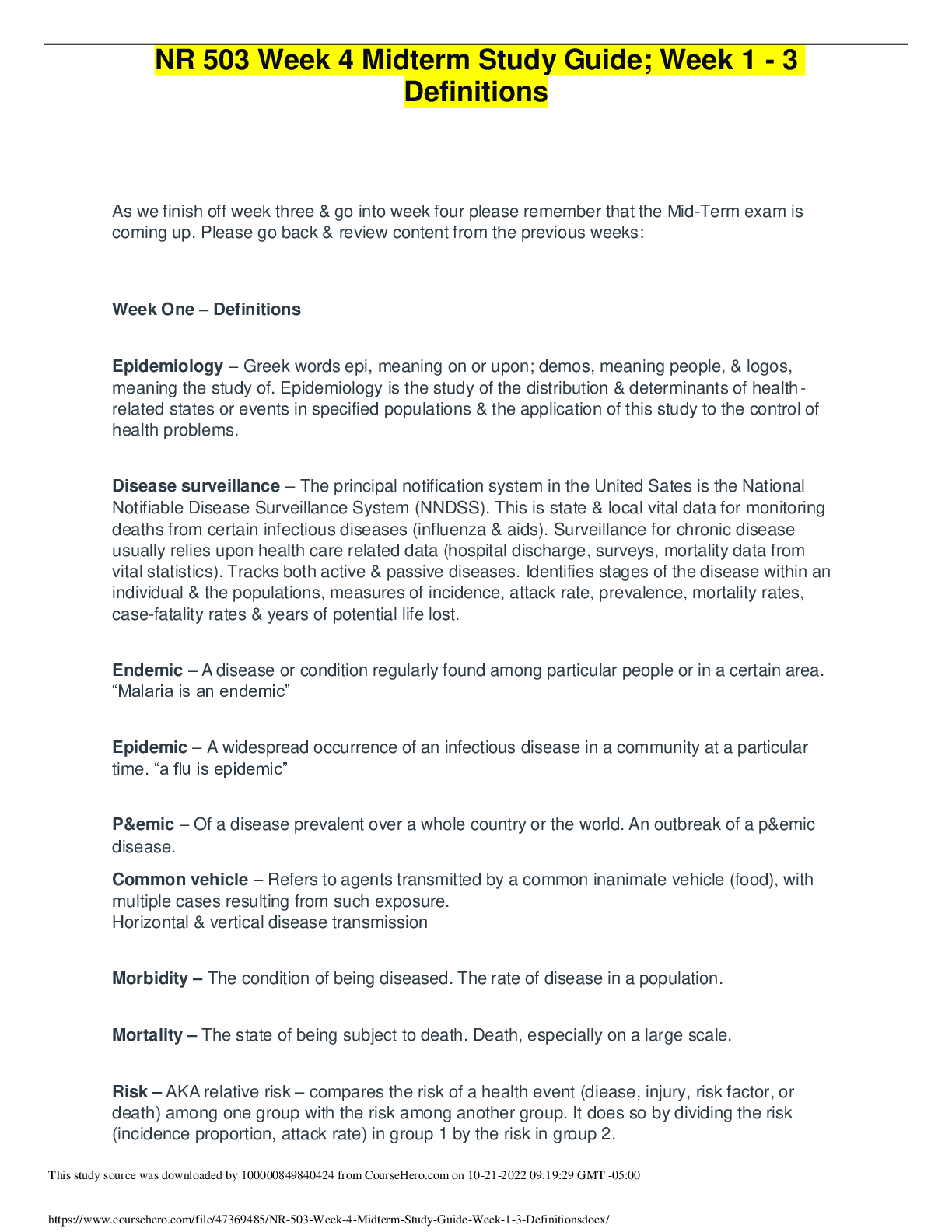
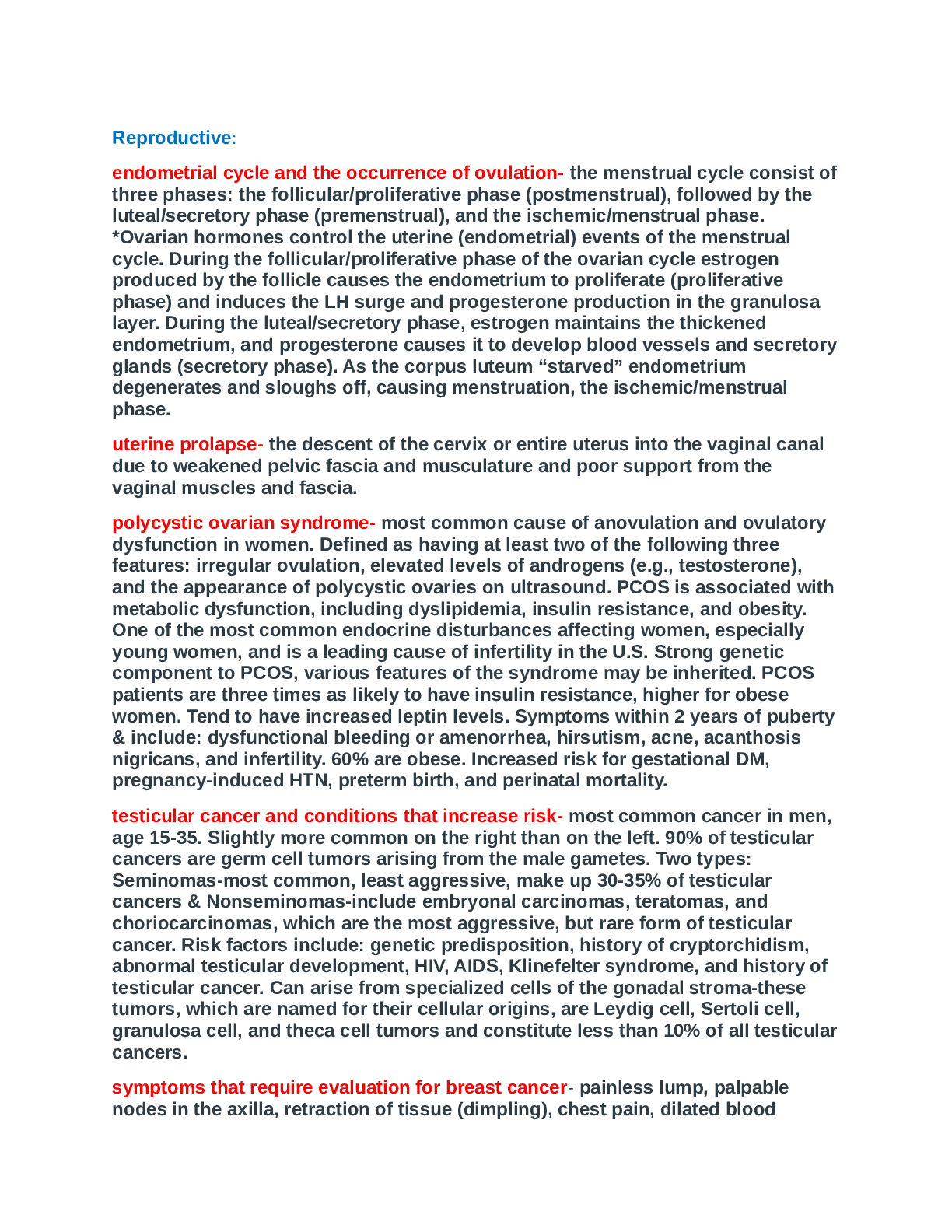
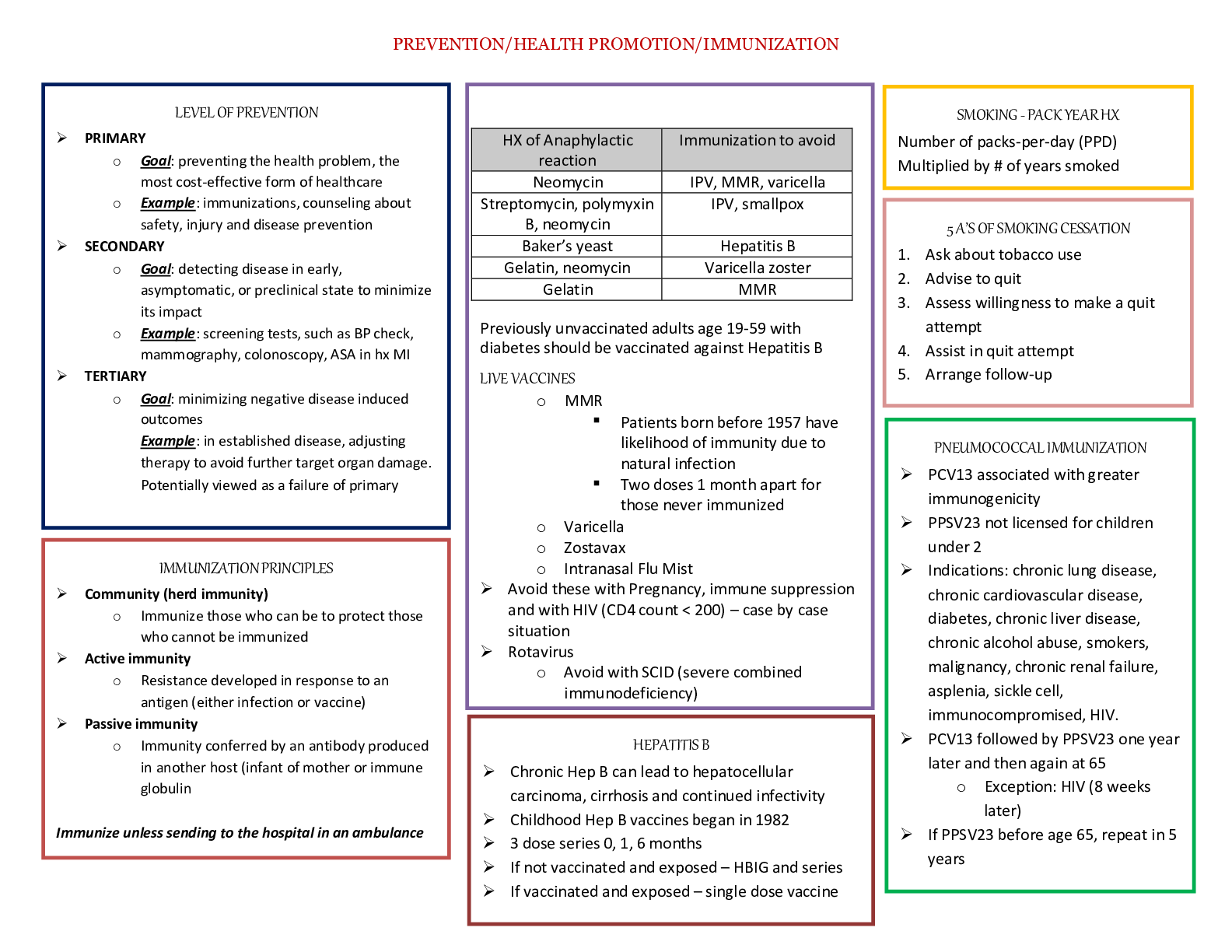
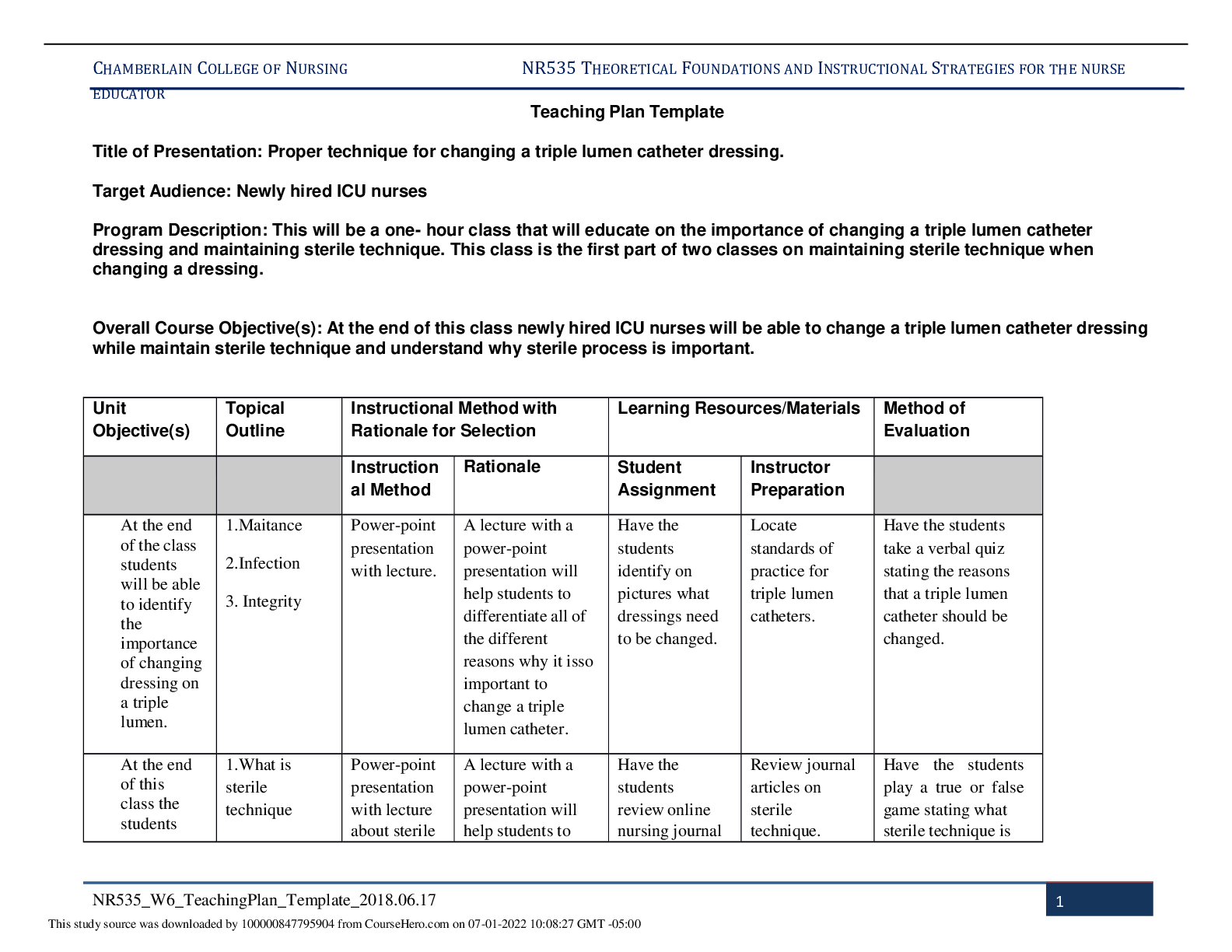
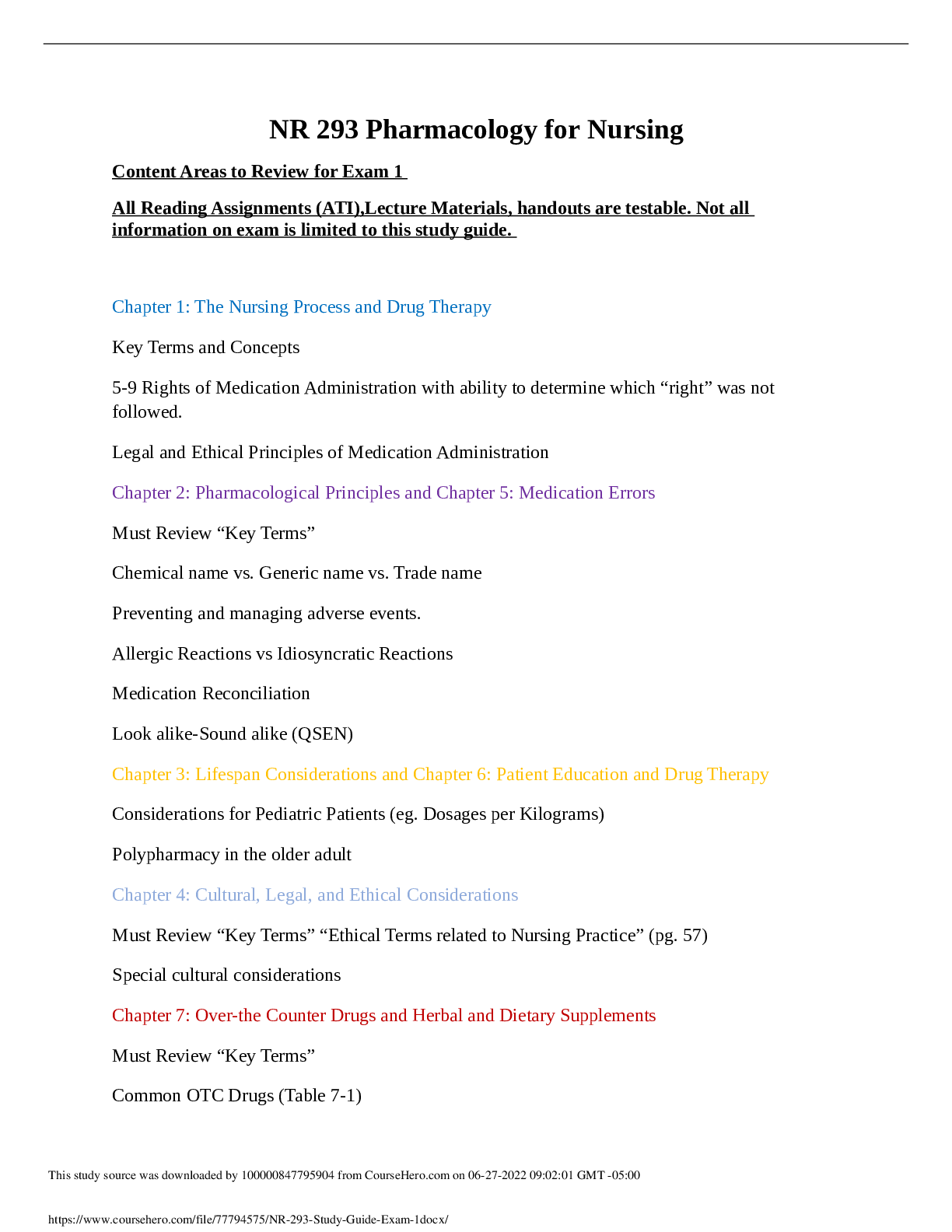
STUDY GUIDE for C475 Care of Older Adult Objective Assessment Exam questions are taken from the Learning Objectives under the 9 Competencies: #1 Competency 742.1.1: Compassionate and Respectful ... Care of Older Adults The graduate integrates principles of compassion and respect for patients and their families into the planning and delivery of care to a diverse population of older adults and into advocacy for vulnerable older adults. This topic addresses the following learning objectives: • Recognize the impact of attitudes, values, and expectations about aging. THE WAY YOU VIEW AGEING IF OFTEN A PRODUCT OF YOUR ENVIRONMENT. MANY OF OUR IDEAS ABOUT AGEING MAY NOT BE GROUNDED IN FACT AND BE NEGATIVE. • Describe how the RN’s personal beliefs and values may impact the care of older adults. MAY WORRY ABOUT YOUR OWN AGEING AND WHAT IT MEANS. MAY NOT LIKE OLDER PEOPLE. MAY BE FEARFUL OF THE ELDERLY • Articulate the concept of individualized care as the standard of practice with older adults, considering the right care, at the right time, in the right place and by the right provider of care. ACUTE CARE HOSPITAL, REHAB FACILITY, HOME, LONG TERM CARE (NURSING HOME) , HOME HEALTH, HOSPICE, RESPITE CARE, CONTINUING CARE RETIREMENT COMMUNITY (CCRC) ➢ Define Baby Boomers Those born between 1946 and 1964 ➢ What are the five racial groups listed in your text? Blacks, non Hispanic whites, Hispanics, American Indian, Asian, Pacific Islander ➢ How would you perform discharge teaching to an Hispanic patient I would include the family. If Spanish speaking only give materials in Spanish and use an interpreter if necessary • Apply effective and respectful communication strategies in the care of older adults and their families. ➢ List some of the changes of aging that could affect therapeutic communication VISION; THE LENDS CHANGES IN COLOR, MAKING IT DIFFICULT FOR THE AGING EYE TO DISTINGUISH COLORS ON THE BLUE-GREEN HUE. LENS BECOMES FLATTER, DENSER DECREASING THE ABILITY TO ACCOMMODATE. PUPILLARY RELEX SLOWS MAKING IT MORE DIFFICULT TO SEE IN LOWER LIGHT, CATARACTS. TREATMENT: POSITION OBJECTS WITHIN THEIR VISUAL FIELD, INCLUDING YOURSELF WHEN SPEAKING TO THEM. GIVE THEM VERBAL INDICATIONS OF YOUR ACTIONS SO AS NOT TO STARTLE THEM. REDUCE UNNEECESSARY CLUTTER. HEARING: LOSS OF SENSITIVITY TO PITCH, POOR WORK RECOGNITION, HEARING LOSS,. TREATMENT: DO NOT SHOUT, PROJECT YOUR VOICE FROM THE DIAPHRAGM MAKING IT DEEPER, MAKE USE OF THE PERSONS OTHER UNIMPAIRED SENSES. STAND IN FRONT OF THE PERSON SO THEY CAN LIP READ, USE GESTURES, SPEAK TO GOOD EAR, LIMIT BACKGROUND NOICE, USE SHORT SENTENCES AND SPEAK CLEARLY, WRITE IT SPEECH: DECREASED SALIVA PRODUCTION, LOSS OF TEETH DYSARTHRIA(DISTURBED ARTICULATION CAUSED BY DISTURBANCE IN THE CONTROL OF SPEECH MUSCLES) APHASIA, TREATMENT: RELAXING ENVIRONMENT, MAKE EYE CONTACT, POSITION YOURSELF IN CLOSE JPROXIMITY, FACIAL EXPRESSIONS AND BODY LANGUAGE, USE SHORT UNCOMPLICATAED SENTENCES, CONSTANTLY REPHRASING, DO NOT CORRECT THE ELDER AND BE RESPECTFUL TOUCH: RECUCTION IN NUMBER OF RECEPTOR,, DECREASE BLOOD FLOOW, REDUCED TACTILE AND VIBRATION SENSATIONS TREATMENT: HAVE THEM REVERT TO ENJOYABLE ACTIVITIES THAT CAPITALIZE ON STRENGTHS AND ABILITIES THEY HAVE MAINTAINED. MOVEMENT: DECREASED BODY STRENGTH TREATMENT: USE ASSISTIVE DEVICES, PILL ORGANIZER, CLOTHES WITH LARGE BUTTONS, HANDRAILS COGNITIVE: DECLINE IN INFO PROCESSING SPEED, DIVIDED ATTENTION, SHORT TERM MEMORY TREATMENT: BE CALM AND REASSURING, DO NOT SHOUT, FACE THE PERSON AND SPEAK SLOWLEY, GENTLE TOUCH, EYE LEVEL WITH THE PERSON, ORIENTING THE PERSON, REFER TO PERSON BY NAME, ELIMINATE BACKGROUND NOICE, BREAK TASKS INTO SMALL MANAGEABLE STEPS, SIMPLE DIRECTIONS, TELL PERSON WHAT YOU ARE PLANNING TO DO AND REPEAT IT, ENCOURAGE PERSON TO DO AS MUCH AS THEY CAN, PRAISE EFFORTS, PHYSCHOLOGICAL: SAME SATISFACTION AS YOUNGER ADULTS: MAY BE DEPRESSED. ➢ Note the ways to communicate or assist a patient with disabilities such as hearing deficits, vision impairments, or aphasia and dysarthria. Be familiar with the types of hearing devices. How should you address the older adult during therapeutic communication? HEARING DEVICES; (ALD) ASSISTIVE LISTENING DEVICE IS ANY TYPE OF DEVICE THAT CAN HELP A PERSON FUNCTION BETTER IN DAY TO DAY LIING. MAY BE USED WITH OR WITHOUT A HEARING AID. HEARING AIDS: (BTE) BEHIND THE EAR. 1 INCH LONG. DELIVERS AMPLIFIED SOUND INTO THE EAR CANAL. ADJUSTABLE VOLUME AND BATTERY POWERED. SUITABLE FOR INTIRE RANGE OF HEARING LOSS. (OTE) OVER THE EAR: VERY SMALL AND SITS ON TOP OF THE OUTER EAR (ITE) IN THE EAR: CUSOM FITTED, MOLDED TO CONTOUR OF OUTER EAR. ADJUSTABLE VOLUME, BATTERY, GOOD FOR MILD HEARING LOSS. SOME USERS HAVE DIFFICULTY SEEING OR MANIPULATING THE CONTROL AND BATTERY (ITC) IN THE CANAL: TINY DEVICES FIT INTO EAR CANAL. CUSOMIZED, THEIR SMALL SIZE CAN BE A DRAWBACK FOR SOME PEOPLE (CIC) COMPLETELY IN THE CANAL: THE SMALLEST TYPE OF DEVICE IN THE EAR CLASS. FITS WITHING THE CANAL. MOST EXPENSIVE, SMALL SIZE IS A DISADVANTAGE BECAUSE OF DIFFICULTY IN HANDLING. ➢ Know the abbreviations or acronyms, such as AAC. Know which hearing aids cover the widest range of hearing loss. See the box on Types of Hearing Aids in chapter 5. Both hearing aids and AAC will be mentioned again in Chapter 16. (AAC) AUGMENTATIVE AND ALTERNATIVE COMMUNICATION: A GROUP OF COMPONENTS INCLUDING SYMBOLS, AIDS, STRATEGIES AND TECHNIQUES USED BY PEOPLE TO ENHANCE COMMUNICATION. RANGE FROM SIMPLE, LOW TECH DEVICES SUCH AS ALPHABET OR HIGH TECH SUCH AS COMPUTER DEVICES THAT RECORD AND STRANSLATE THE SPOKEN WORK INTO PRINT. ➢ Make sure you understand what patients could benefit from the use of the AAC. PATIENTS WITH DYSARTHRIA ➢ Understand what things can occur to make it difficult to communicate ➢ Which type of hearing aid covers the entire range of hearing loss? ➢ What factors in a diverse aging population affect communication? PHYSICAL CHANGES FROM NORMAL AGING AS WELL AS THOSE ASSOC. WITH DISEASE PROCESS. • Support individual health goals that range from healthy activities to simply achieving comfort. • Illustrate compassionate and individualized care for older adults with chronic illness that reduces symptom burden and seeks to preserve quality of life. #2 Competency 742.1.2: Health Promotion/Maintenance and Living Environments of Older Adults The graduate evaluates the older adults' life world with special awareness of the diversity among the health status of older adults, individualizing care according to the physical, mental/cognitive, functional, and psycho-social well-being of an elder patient, along with support systems in place. *You will notice that Competencies two through five overlap one another. Some of the information for one topic may be found in another topic or another competency. Don’t become frustrated. It will all come together. This topic addresses the following learning objectives: • Identify functional and physical changes in the aging adult that would necessitate changes to the living environment. POOR BALANCE AND GAIT, HEARING, VISION, ETC • Identify cognitive, psychological, and social changes common to the aging adult that would necessitate changes to the living environment. DEPRESSION, DEMENTIA, ABUSE, • Recognize steps to mitigate common physical safety issues. • Analyze the living environment of a given older adult with special awareness of the functional, physical, cognitive, psychological, and social changes of aging. ➢ What are the five A’s to tobacco cessation? FOR PEOPLE WHO ARE READY TO QUITE SMOKING. *ASK ABOUT SMOKING STATUS AT EACH VIST ▪ ADVISE CLIENT TO QUIT SMOKING ▪ ASSESS CLIENT’S WILLINGNESS TO QUIT SMOKING ▪ ASSIST CLIENT TO QUIT SUSING COUNSELING AND PHARMACOTHERAPY ▪ ARRANGE FOR FOLLOW UP WITHIN ONE WEEK OF SCHEDULED TIME TO QUIT ➢ What are the Five R’s to tobacco cessation? FOR THOSE WHO NEED ADDITIONAL MOTIVATION BEFORE THEY ARE READY TO QUIT.. • RELEVANCE: ASK THE CLIENT TO THINK ABOUT WHY QUITTING MAY BE RELEVANT FOR HIM • RISKS OF SMOKING ARE IDENTIFIED BY THE CLIENT • REWARDS OF QUITTING ARE IDENTIFIED BY THE CLIENT • ROADBLOCKS OR BARRIERS TO QUITTING ARE IDENTIFIED BY THE CLIENT • REPETITION OF THIS PROCESS AT EVERY CLINIC VISIT ➢ What is the criterion for the pneumococcal vaccine? GIVEN ONCE FOR CLIENTS WHO ARE 65 YRS OR OLDER. ONE TIME REVACCINATION FOR CLIENTS 75 AND OLDER WHO HAVE NOT BEEN VACCINATED IN 5 YRS OR MORE ➢ In most cases of elder abuse who is the perpetrator? A FAMILY MEMBER ➢ What 5 areas do Healthy People 2010 and the USPSTF suggest that nurses focus on to promote health & prevent disability in the older adult? (see page 356 in text) PHYSICAL ACTIVITY, NUTRITION, TOBACCO USE, SAFETY AND IMMUNIZATIONS ➢ Describe the difference between ADLs and IADLs (instrumental activities of daily living) (ADL) ACTIVITIES OF DAILY LIVING: ACTIVITIES PERFORMED IN THE COURSE OF DAILY LIFE; THEY INLUE BATHING, DRESSING, TRANSFERRING, WALKING, EATING, AND CONTINENCE (IADLs) INSTRUMENTAL ACTIVITIES OF DAILY LIVING.: ACTIVITIES RELATED TO INDEPENDENT LIVING; THEY INCLUDE MEAL PREP, MONEY MANAGEMENT, SHOPPING, HOUSEWORK, AND USING A PHONE ➢ List the nutritional assessment tests to determine risk for diet-related chronic illness (see text page 359) ✓ SERUM ALBUMIN(LESS THAN 3.5 OSSOC WITH MALNUTRITION ✓ BMI 22-27 IS NORMAL ✓ ADULT TREATMENT PANEL (ATPIII) CHOLESTEROL LESS THAN 150 POSES NUTRITIONAL RISK ✓ ADL AND IADL MEASURES: ASSESS CLIENTS ABILITY TO EAT AND PREPARE FOOD AND SHOP ✓ DIETARY REFERENCE INTAKES AND RECOMMENDED DAILY ALLOWANCE: FOOD DIARIES FOR 24 TO 48 HRS ✓ DEPRESSION AND DEMENTIA; BOTH RISK FACTORS FOR NUTRITIONAL COMPROMISE ➢ Review the USPSTF Screening Recommendations for Older Adults, Table 12-1 on page 376 in text. (USPSTF) U.S. PREVENTIVE SERVIES TASK FORCE= EVALUATES THE BENEFITS OF INDIVIDUAL SERVICES AND TO CREATE AGE, GENDER, AND RISK BASED RECOMMENDATIONS ABOUT SERVICES THAT SHOULD BE INCORPORATED INTO PROMARY MEDICAL CARE. USPSTF SCREENING RECOMMENDATIONS: PHYSICAL ACTIVITY, NUTRITION, TOBACCO USE, SAFETY, IMMUNIZATIONS, DEPRESSION, DEMENTIA, ETOH, ELDER ABUSE, LIPIDS, HTN, ASA THERAPY, CVA, THYROID DZ, OSTEOOROSIS, VISION AND HEARING, PROSTATE CA, BREAST CA, COLORECTAL CA. HEALTHY PEOPLE 2010 IS AND INITIATIVE OF US DEPT HEALTH AND HUMAN SERVICES THAT UTILIZED THE SKILLS AND KNOWLEDGE OF AN ALLIANCE OF ORGANIZTIONS TO DEVELOP A SET OF HEALTH CARE OBJECTIVES DISIGNED TO INCERASE THE QUALITY AND QUANTITY OF YEARS OF HEALTHY LIFE. ➢ Review the I HATE FALLING risk assessment tool, Box 12-4 on page 361. What can the nurse recommend to reduce risk of falling? ✓ INLFAMATION OF JOINTS, HYPOTENSION, AUDITORY OR VISUAL IMPAIRMENT, TREMOR, EQUILIBRIUM JPROBLEMS, FOOT PROBLEMS, ARRHYTHMIAS, LEG LENGTH DISCREPANCY, GENERAL WEAKNESS, ILLNESS, POOR NUTRITION, GAIT DISTURBANCE. TX: BALANCE AND STRENGTHENING EXERCISE PROGRAMS, HOME SAFETY ASSESSMENT AND TRAINING, MEDICATION MONITORING AND ADJUSTMENT #3 Competency 742.1.3: Health Needs of Older Adults The graduate effectively collaborates with patients, families and inter-professional team members in planning primary, secondary, tertiary and end-of-life care that addresses older adults' physical, mental, psychosocial and spiritual needs and preferences and responses to changes in health status and related treatments. This topic addresses the following learning objectives: • Identify how the physiological changes of aging affect the organs involved in absorption and excretion of medications sorption is defined as the movement of a drug from the site of administration, across biological barriers, into the plasma. Although the rate of drug movement through the body may decrease with age, the extent of drug absorption is least affected by age. Certain disease states, however, and the simultaneous use of several medications have been shown to decrease absorption of some medications OLDER PEOPLE HAVE LESS WATER AND MORE FAT IN THEIR BODIES SO DRUGS THAT ARE FAT SOLUBLE TAKE LONGER TO METABOLIZE. (DIAZEPAM) HEPATIC MASS AND BLOOD FLOW DECREASE WITH AGE.THEREFORE HEPATIC METABOLISM IS DECREASED. RENAL AND RENAL BLOOD FLOW ARE ALSO DECREASED. NORMAL DOSES IN A YOUNG PERSON CAN BE TOXIC IN AN ELDERLY PERSON. THE EFFECTS OF DRUGS IN ELDERLY CAN BE EITHER GREATER OR LESS. INCREASED RESPONSE AND EFFECT TO BENZODIAZEPINES, OPIATES AND WARFARIN IN THE ELDERLY. The presence or absence of food may reduce or increase the bioavailability of a medication, leading to unanticipated effects. The first “lethal” food–drug interaction recognized was that of cheese and monoamine oxidase inhibitors (MAOIs). The interaction of food and drug in this instance could lead to extremely high blood pressure and stroke. Grapefruit juice is known to interact with antihistamines, and greens with warfarin. Herbal and dietary supplements may interact with medications, affecting metabolism of the drug. Natural licorice may induce hypertension and interfere with certain drugs. Antibiotics may be susceptible to chelation and absorption by fortified cereals, calcium-fortified orange juice, or protein beverages. These interactions reduce the efficacy of the antibiotic and may lead to antibiotic-resistant bacteria (McCabe, 2004). Malnutrition can also affect the metabolism of medications • Recognize functional changes and mobility issues that may threaten independence in the older adult. • Identify factors that may contribute to alterations in nutrition, metabolism, and elimination in older adults. • Recognize the signs and symptoms of geriatric syndromes and the subsequent frailty that may result. • Apply knowledge of the aging process and associated risk factors; skills in history-taking and assessment; and respect for the dignity of older adults in a comprehensive, individualized assessment. • Identify and use valid and reliable standardized tools of functional assessment in older adults. • Identify and use valid and reliable standardized tools of cognitive assessment in older adults. • Observe for risks or the presence of the five most common geriatric syndromes (pressure ulcers, incontinence, falls, functional decline, and delirium, including hypokinetic delirium). • Compare specified theories of aging, including the genetic theory. • Describe how to use evidence-based assessment tools and methods to conduct a comprehensive assessment of an older adult. • Promote quality outcomes through the application of evidence-based practices specific to the care needs of older adults. • Promote evidence-based practice by utilizing the Beer list of potentially unsafe medications for the elderly. • Contribute to interdisciplinary plans of care to promote health, reduce risk, and prevent disease in older adults. • Contribute to interdisciplinary care plans that address common acute and chronic health conditions, such as arthritis, diabetes, cardiovascular diseases that may lead to congestive heart failure, and dementia. • Consider potential drug side effects in assessing adverse symptoms in older adults. ➢ There are three types of assessments: Physical, Cognitive and Functional. ✓ Physical assessment is assessing the patient’s physical health. It included vital signs, assessing for pain, blood pressure problems, irregular heartbeat, abnormal breath sounds, etc. you know these because as a nurse you are always assessing the patient. In addition, for older adults you want to assess cognitive function. ✓ Functional assessment is assessing what the older adult can still for themselves. Bathing, eating, getting dress, brushing their teeth and more are functional abilities. Functional abilities can be altered due to physical impairment and illness. Dr. Katz and Dr. Barthel developed ADL/IADL indexes to measure the patients functional abilities. You should have noticed that ADL is used throughout the book. This is because the ADL's can determine the patient's care plan. It determines whether they are safe in the current environment. It impacts their ability to participate in health promotion and disease prevention. Cognitive- thought processing, thinking and reasoning skills. Know the normal cognitive changes as a result of aging. Dementia is not normal. You will need to understand the difference between delirium and demential Delirium is a serious disturbance in a person's mental abilities that results in a decreased awareness of one's environment and confused thinking. The onset of delirium is usually sudden, often within hours or a few days. Delirium can often be traced to one or more contributing factors, such as a severe or chronic medical illness, medication, infection, surgery, or drug or alcohol abuse. Dementia and delirium may be particularly difficult to distinguish, and a person may have both. In fact, frequently delirium occurs in people with dementia. Dementia is the progressive decline of memory and other thinking skills due to the gradual dysfunction and loss of brain cells. The most common cause of dementia is Alzheimer's disease Some differences between the symptoms of delirium and dementia include: • Onset. The onset of delirium occurs within a short time, while dementia usually begins with relatively minor symptoms that gradually worsen over time. • Attention. The inability to stay focused or maintain attention is significantly impaired with delirium. A person in the early stages of dementia remains generally alert. • Fluctuation. The appearance of delirium symptoms can fluctuate significantly and often throughout the day. While people with dementia have better and worse times of day, their memory and thinking skills stay at a fairly constant level during the course of a day. There are special tools to assess the older adult that have been proven to produce accurate results. You must be familiar with those tools specific for the older adult. The exam will use the acronyms for the tools. For example, CAM, MMSE, CDT, SPICES. Make sure you know what these stand for and can answer when they are to be used or what the results of these assessment tools will tell you. (MMSE) MINI MENTAL STATE EXAM: COGNITIVE ASSESSMENT TOOL. COGNITIVE (FNCTN OF ATTN, MEMORY, LANGUAGE, VISUOSPATIAL SKILLS AND EXECUTIVE CAPACITY. MMSE MEASURES ORIENTATION, REGISTRATION, ATTENTION AND CALCULATION, SHORT TERM RECALL, LANGUAGE AND VISUOSPATIAL FNCTN. DOES NOT MEASURE EXECUTIVE FNCTN.THE RESULTS CAN VARY BY AGE AND EDUCATIONAL BACKGROUND. Takes 10 min. normal 24 to 30, mild cognitive impairment 20 to 30, moderate impairment 10 to 19, sever impairment 1 to 9, 0 is profound MINI COG: ADMINISTERED IN 5 MIN OR LESS. CONISISTS OF 3 ITEMS OF RECALL AND A CLOCK DRAWING TEST. (CDT) CLOCK DRAWING TEST: (CAM) CONFUSION ASSESSMENT METHOD: ID AND RECOGNIZE DELIRIUM. LONG CAM CAN PROVIDE ADDTL INFO ABOUT A PTS BEHAVIOR A SHORT CAM IS PROVEN TO BE EFFECTIVE IN IDENTIFYING DELIRIUM. CAN COMPLETE IN 5 MIN. (SPICES) FALLL RISK ASSESSMENT: Sleep disorders, Problems with eating and feeding, Incontinence, Cjonfusion, Evidence of falls, Skin breakdown ➢ Be familiar with the pain assessment tools, and how unrelieved pain can lead to prolonged hospitalization. ➢ Know Katz Index of ADL and Barthel Index both are in chapter 7. You will see ADL and IADL throughout the rest of the entire book. KATZ: DISTINGUISH BETWEEN INDEPENDENCE AND DEPENDENCE IN ACTIVITIES. ADDRESSES THE NEED FOR ASSISTANCE IN BATHING, EATING, DRESSING, TRANSFER, TOILETING AND CONTINENCE. BARTHEL INDEX: MEASURES FUNCTNL LEVELS OF SELF CARE AND MOBILITY, RATES THE ABILITY TO FEED AND GROOM, BATHE, TOILET, WALK, CLIMB STAIRS, CONTIL BOWEL AND BLADDER. ➢ The Mini Mental State Examination (MMSE) is the most extensively used cognitive assessment tool (page 246). The Mini-Cog can be done in 5 minutes see also www.consultgerirn.org. ➢ They may also mention CDT (Clock Drawing Test) which is commonly done with the Mini- Cog evaluation. ➢ Be familiar with ConsultGeriRn.org web videos: Katz Index of Independence in Activities of Daily Living and Administering and Interpreting the Mini-Cog, The Geriatric Depression Scale (GDS) Short Form Assessment, Delirium: The under-recognized Medical Emergency, The Modified Caregiver Strain Index (CSI) ➢ You have to know the physiological changes that occur which make the older adult more susceptible to adverse drug reactions. ✓ Five Rights of Medication Administration ✓ RIGHT MED, RIGHT DOSE, RIGHT TIME, RIGHT ROUTE, RIGHT PATIENT ✓ The most common drugs that alter lab results ISONIAZID, LEVODOPA, MORPHINE VIT. C AND PCN GMAY LEAD TO FALSE + GLUCOSE I URINE ✓ Polypharmacy- why is the older adult more apt to polypharmacy. PRESCRIBED ADDTNL DRUGS TO REAT SIDE EFFECTS OF MEDS THAT THEY ALREADY TAKE. DEFINES AS USE OF MORE MEDS THAN ARE CLINICALLY INDICATED. CAN INCLUDE OTC’s. ✓ Beers’ List of Inappropriate drugs for Older Adults- this is in the e-text and www.consultgerirn.org. Make sure you are familiar with this. Benzodiazepines are mentioned quite a bit ✓ ANTICHOLINERGICS, 1ST GENERATION ANTIHISTAMINES, ANTIPARKINSON AGENTS, ANTISPASMODICS, ANTITHROMBOTICS (PERSANTINE AND TICLID), NITROFURANTOIN, ARBs (DOXAZOSIN, PRAZOSIN, TERAZOSIN, ALPHA BLOCKERS CENTRAL (CLONIDINE, GUANABENZ, GUANFACINE, METHYLDOPA, RESERPINE) ANTIARRHYTHMIC (AMIODARONE, DOFETILIDE, DRONEDARONE, FLECAINIDE, IBUTILIDE, PROCAN, PROPAFENONE, QUINDINE, SOTALOL), DISOPYRAMIDE, DRONEDARONE, DIGOXIN, IMMEDIATE RELEASE NIFIDEPINE, ANTIPSYCHOTICS, BARBITURATES, BENZODIAZEPINES, NON BENZO HYPNOTICS, ESTROGENS, SLIDING SCALE INSULIN, MEGESTROL, GLYBURIDE, METOCLOPRAMIDE, MEPERIDINE, NSAIDS, PENTAZOCINE, MUSCLE RELAXANTS. ✓ ➢ MAP- this means medication assistance program and it will be mentioned in a later chapter. Make sure you understand what it is. This is a choice you can offer your patient who cannot pay for their medication. PHARMACEUTICAL CO PROVIDE FREE MEDS TO PEOPLE WHO CANT AFFORT TO BUY THEIRS. RX ASSIST OFFERS A DATABASE OF THESE PT ASSISTANCE PROGRAMS. ➢ You want to advise your patients to become very familiar with their pharmacist. Only use one pharmacy for all their medications, including over the counter (OTC) and herbal remedies. The pharmacist can alert the patient to potential drug reactions. ➢ Know the common classes cause ADR: antipsychotics, antihistamines, benzodiazepine (Atarax, restoril, florazepam, diazepam, Librium, Xanax, Restyl, Paxil), Muscle relaxants, anti-anxiety drugs, anti-convulsants, antiemetics, analgesics (ADR) ADVERSE DRUG REACTION. THE ABOVE DRUGS CAN CAUSE CONFUSION AND/OR SEDATION #4 Competency 742.1.4: Promoting Independence and Autonomy While Reducing Risk Factors in Older Adults The graduate recommends techniques to co-create health and illness management practices with older adults and their families (caregivers) that ensure safety and optimal maintenance of functional ability, taking into account patient characteristics and needs and patient and caregiver vulnerabilities as well as strengths. This topic addresses the following learning objectives: • Identify ethical principles for preserving autonomy while reducing risk in the care of older adults. • Describe strategies for preventing morbidity and mortality associated with the use of physical and chemical restraints in older adults. • Determine appropriate best practices to co-create a plan of care with the patient, family and other caregivers. • Explain how you would assist older adults, families, and caregivers to balance the need for autonomy and safety when making everyday decisions. • Apply ethical and legal principles to the complex issues that arise in the care of older adults. • Identify appropriate principles of care commensurate with older adults' vulnerabilities and the frequency and intensity of care needs. • Assess the effectiveness of various steps taken to assist health professionals in recognizing and reporting suspected mistreatment of older adults or abuse of resources. • Recommend appropriate individualized care practices to eliminate the use of physical and chemical restraints in older adults. • Recommend techniques to create health practices of a given older adult and family to address identified patient vulnerabilities. ➢ Define autonomy and self-determination. AUTONOMY: INDEPENDENCE. ➢ SELF DETERMINATION: MOTIVATION ➢ What is frailty? What are the characteristics? PHYSICAL WEAKNESS, FRAILITY IS A MEDICAL CONDITION NOT A INEVITABLE RESULT OF AGEING. THIN, WEAK, TIRE EASILY. FRAIL PEOPLE SUFFER FROM 3 OR MORE OF 5 SXMPTMS. THESE INCLUDE UNINTENTIONAL WEIGHT LOSS, MUSCLE LOSS, WEAKNESS, FATIGUE, SLOW WALKING AND LOW LEVELS OF PHYSICAL ACTIVITY. ➢ What is the Kohlman Evaluation of Living Skills (KELS)? ASSESS 17 DAILY LIVING SKILLS UNDER 5 CATEGORIES –SELFCARE, SAFETY AND HEALTH, MONEY MANAGEMENT, TRANSPORTATION AND TELEPHONE USE,WORK AND LEISURE. IT EVALUATES APPROPRIATENESS FOR INDEPENDENT/COMMUNITY LIVING. ➢ What are the factors that influence the quality of life of an older adult? PERCEPTION OF PERSON BEING EVALUATED. CONSIDER THE WHOLE PERSON. NUTRITION, WELL BEING, RELIGION, LIVING ARRANGEMENTS, PHYSICAL ACTIVITY, SOCIAL INTERACTIONS, PHYSICAL MENTAL EMOTIONAL FNCTNING, DISEASE MANAGEMENT, INDEPENDENCE, HEALTH, CONSIDER PERSON, FAMILY/CAREGIVER, COMMUNITY ➢ What is the one of the most common role changes faced by the aging person? List all. RETIREMENT, HEALTH TRANSITION, LOSS OF SPOUSE, ROLE REVERSAL WITH SPOUSE OR CHILDREN, DRIVING, IADLS, BADLS, ➢ What is role reversal for the older adult? THE ELDER MOVES FROM CARE PROVIDER TO CARE RECIPIENT. SOME OLDER PERSONS MAY ENJOY THE DEPENDENCY OF THEIR FAILING HEALTH, TAXING THE FAMILIES. ➢ List and describe the care options for the older adult? INDEPENDENT LIVING WITH HELP, FAMILY HOME, ADULT DAYCARE, SENIOR LIVING COMPLEXES, ASSISTED LIVING, PAID HOME CAREGIVERS, EXTENDED CARE FACILITIES, ➢ What is the Borg Category Rating Scale? RATE THEIR OWN LEVEL OF EXERCISE AND TARGET THEIR DESIRED LEVEL OF ACTIVITY. SCALE OF LEAST EFFORT-6 TO MAX EFFORDT-20. ENDURANCE TRAINING AND STRENGTH TRAINING ZONES. GOAL IS 30 MIN A DAY. MAY INCREASE IN 10 MIN INCREMENTS UNTIL YOU REACH THAT. STRENGTH TRAINING IS REC. TWICE/WEEK, BUT NOT FOR CONSECUTIVE DAYS WITH SAME MUSCLE GRP. ➢ What are the common signs of abuse in an older adult and who is mostly to be the abuser? PRESENCE OF SEVERAL INRIES IN DIDFFERENT STAGES OF REPAIR, DELAYS IN SEEKING TX, INJURIES THAT CANT BE EXPLAINED, CONTRADICTORY EXPLANATIONS, BRUISES, BURNS, WELTS, RESTRAINT MARKS, DEHYDRATION, MALNUTRITION, DECUBS, POOR HYGIENE, DEPRESSION, WITHDRAWAL, AGITATION, MED MISUSE, PATTERN OF MISSED OR CANCELLED APPTS, FREQUUENT CHANGES IN HEALTH CARE PROVIDERS, DISCHARGE, BLEEDING OR PAIN IN RECTUM, VAGINA OR STD, MISSING PROSTHETIC DEVICES (DENTURES, GLASSES HEARING AIDES) ➢ List common tools used to assess abuse in the older adult? EVALUATE THROUGH HISTORY WITH PT, CAREGIVERS, AND OTHERS TAKEN SEPARATELY. HOME VISITS, PHYSICAL EXAM, MENTAL STATUS, LABS FOR DEHYDRATION, MALNUTRITION, MED ABUSE AND FRACTURES OR OTHER INURIES. (H-S/EAST) HWALEK SENGSTOCK ELDER ABUSE SCREENING TEST ➢ Describe the Framingham Heart Study. What did it look at and what were the findings? RISK FACTORS ASSOC WITH CAD. STUDY BEGAN WITH 5000 MALES AND FEMALES. RISK FACTORS IDENTIFIED: AGE GREATER THAN OR = TO 50, HTN, SMOKING, OBESITY, FAMILY HX, DIABETES, SEDENTARY LIFESTYLE, ABN LIPID LEVELS ➢ What are the risk factors for stroke? Describe the statistical data in regards to strokes and the older adult. STROKE IS THE 3RD LEADING CAUSE OF DEATH IN US WITH MORE THAN 2/3RDS OF STROKE OCCURRING IN PERSONS AGE 65 AND OVER. 36% STROKES SUFFERED BY PTS 80 TO 89 WERE RELATED TO NONVALVULAR AFIB. COUMADIN REDUCES RISK BY 68% AND ASPRIN REDUCES IT BY 21%. RISK FACTORS INCLUDE: INCREASED AGE, HTN, SMOKING AND DIABETES. PEOPLE WITH CAD ARE AT A GREATER RISK CUZ SAME ETIOLOGY. OTHER RISK FACTORS: ETOH, SMOKING, SEDENTARY LIFESTYLE, HIGH FAT DIET, A FIB, CAROTID STENOSIS. ➢ What are other disease processes the older adult is at risk for? Explain the prevalence and how to prevent or control the illness HEART DZ, HTN (90%), INCREASE CHOL, THYROID(17% FEMALE, 6% MALE), OSTEOPOROSIS(14% HIGHER RISK), VISION AND HEARING LOSS, PROSTATE CA (LEADING CAUSE OF CA DEATH IN MEN), BREAST CA (3- 4%), ➢ Instruct the patient to obtain all medications (prescription and nonprescription) at one pharmacy so that pharmacists can check for potentially dangerous interactions. The pharmacist can serve as the central figure who maintains a list of medications and screens for drug-drug interactions to avoid harmful situations. #5 Competency 742.1.5: Promoting Health and Independence in Older Adults. The graduate selects appropriate evidence-based standards of health promotion, risk reduction, and disease prevention in older adult populations. This topic addresses the following learning objectives: • Explain how to facilitate older adults' active engagement and participation in their own healthcare. • After discussing evidence-based health promotion activities, facilitate the development of health promotion goals with a given older adult. • Analyze evidence-based research regarding risk reduction and disease prevention in older adults. • Describe strategies to enhance the physical and mental function of older adults. • Identify common risk factors that contribute to functional decline in older adults. • Identify the principles for improving functional ability and quality of life for the older adult. • Articulate psychosocial interventions for maximizing a given older adult’s quality of life. ➢ What is the definition of a fall? And what can happen to an older adult after a fall? RAPIDLY AND FREELY WITHOUT CONTROL FROM A HIGHER TO A LOWER LEVEL. LOSE ONES BALANCE AND COLLAPSE. FALLS CAN RESULT IN INJURY, LOSS OF INDEPENDENCE, REDUCED QUALITY OF LIFE, AND DEATH. FRACTURES, LACERATIONS AND BRUISES. IF THEY CANT GET UP DEHYDRATION, SORES RHABDOMYOLYSIS, HYPOTHERMIA, PNEUOMONA. ➢ What are the risks for falls? (Past history of falls is a major risk factor!) INTRINSIC (COGNITIVE IMPAIRMENT, MEDS, ETOH, IMPAIRED MOBILITY, FALL HX, ILLNESS, ELIMINATION PROBLEMS, SENSORY DEFECTS, FRAILTY, POSTURAL HYPOTENSION) EXTRINSIC (PPOR LIGHTING, POOR COLOR DISTINCTION, CLUTTER, UNFAMILIAR ENVIRONMENT, STAIRS, THROW RUGS, UNSUITABLE FOOTWEAR, RESTRAINTS, SIDE RAILS) ➢ What are intrinsic risk factors? What are extrinsic risk factors? INTRINSIC: RELATED TO CHANGES ASSOC WITH AGING. BALANCE PROBLEMS, COGNITION AND JUSCULOSKELETAL FNCTN. EXTRINSIC: ENVIRONMENTAL HAZARDS SUCH AS POOR LIGHTING, STAIRS, CLUTTER, THROW RUGS. ➢ Among older adults living in the community, when and where do most falls occur? MORE THAN HALF HAPPEN AT HOME ➢ What can you do to prevent falls? REMOVE THROW RUGS, SECURE CARPET EDGES, REMOVE LOW FURNITURE AND OBJECTS ON FLOOR, REDUCE CLUTTER, REMOVE CORDS, CHECK LIGHTING, INSTALL HANDRAILS ON STAIRCASES, ELIMINATE CHAIRS THAT ARE TOO LOW TO SIT AND GET OUT OF, AVOID FLOOR WAX, INSTALL GRAB BARS IN TUB, USE RUBBER MATS IN TUB, RAISED TOILET SEAT, REPAIR CRACKED SIDEWALKS, TRIM SHRUBS, LIGHTING. IN HOSPITAL: NON SKID SLIPPERS, COMMODE CLOSE TO BED, CALL LIGHT IN REACH, BED IN LOW, ➢ What are the types of restraints used? BELTS, VESTS, PELVIC TIES, MITTS, SPECIALIZED CHAIRS, BED SIDE RAILS. ➢ What are the effects of restraint use on the elderly? CAN DECREAE THEIR QUALITY OF LIFE. INCREASE FALL AND INJURY RISK. ➢ What are alternatives techniques (instead of restraints) to deal with wandering, combative or confused patients? PLACE PT NEAR NURSES STTION, USE OF CALL BUTTON OR ALERTING DEVICE, KEEP NECESSARY ITEMS HANDY, SITTER, RELAXED CALM SURROUNDINGS, EYEGLASSES/HEARING AIDS, POSITIONING DEVICES (BODY PILLOWS/WEDGES), ADEQUATE PAIN MANAGEMENT. ➢ Identify ways to promote healthy living among the elderly ➢ What are the two most widely publicized components of health promotion? EXERCISE AND NUTRITION ➢ What are some of the preventive care services covered under Medicare? PX, CARDIOVASCULAR SCREEN Q 5 YRS, CERVICAL CA Q 2 YRS, PAPS, COLORECTAL SCHREEN (COLONSCOPY Q 10 YS, SIGMOIDOSCOPY Q 4 RS), DENSITOMETRY Q 2 YRS, DIABETES SCREEN, MAMMOGRAM, PROSTATE CA SCREEN, SMOKING CESSATION, IMMUNIZATION ➢ Describe a health contract. IT GIVES INSTRUCTIONS, SET GOALS, IDENTIFY MOTIVATION, IMPLEMENTS A PLAN OF ACTION, IDENTIFY POTENTIAL PROBLEMS, ENCOURAGES. THE CONTRACT IS SIGNED AND DATED. PROGRESS IS ASSESSED AFTER 1 WEEK, AND REVIEWED AT END OF MONTH. ALLEGED TO HAVE ADVANTAGES OVER VERAL COMMUNICATION. IT IDENTIFIES AND ENHANCES MOTIVATION, CLARIFIES MEASURABLE AND MODEST GOALS, SUGGEST TIPS TO REMEMBER NEW BEHAVIORS, PROVIDES A PLANNED WAY TO INVOLVE SUPPORT PERSONS ➢ Explain Bailey's Bull's eyes GOAL IS FOR PEOPLE TO CONSUME NUTRITIOUS FOODS THAT ARE LISTED IN THE CENTER OF IT. THESE FOOD ARE LOW IN SATURATED FAT, SUGAR AND SODIU, AND HIGH IN FIBER. THEY INCLUDE SKIM MILK, NONFAT YOGURT, FRUITS AND VEGES, WHOLE GRAINS, BEANS AND LEGUMES, WATER PACKED TUNA. AS YOU MOVE TO FOODS LISTED IN THE RINGS FARTER AWAY FROM THE BULLS EYE YOU EAT MORE BAD FOODS AND IN THE OUTER RING IS MOSTLY CHEESES, ICE CREAM, BUTTER, WHOLE MILK, CAKE, BEEF CHIPS. BULLS EYE IS MADE TO FIT CLIENT. BEGIN WITH A BLANK ONE AND FILL IN WHAT THE PATIENT USUALLY CONSUMES TO EACH OF THE RINGS. FIRST RING IS NUTRITIOUS, SECOND RING NOT QUITE AS NUTRIENT DENSE, THE THIRD RING IS NEUTRAL (PRODUCTS NOT HAMRFUL OR HELPFUL) ➢ Discuss Healthy People 2010 and 2000.HEALTHY PEOPLE 2000 INITIATED BY US PUBLIC HEALTH SVC IN EFFORT TO REDUCE PREVENTABLE DEATH AND DISABILITY. HEALTHY PEOPLE 2010 NEW INITIATIVE UNDER WAY. THEY GIVE RECOGNITION TO HEALTH PROMOTION, RATHER THAN WARS ON DISEASE. THEY ARE HEALTH ORIENTED AND THEY RECOGNIZED SOCIOECONOMIC, LIFESTYLE AND OTHER INFLUENCES THAT IMPACT OUR ABILITY TO ATTAIN AND MAINTAIN HEALTH. FOCUSED ON DOCUMENTING BASELINES, SETTING OBJECTIVES AND MONITORING PROGRESS. ➢ Define health promotion vs. health screening. HEALTH PROMOTION: EXERCISE AND NUTRITION, MEDICARE AND HEALTHY PEOPLE INITIATIVES. HEALTH PROMOTION INCLUDES SELF MANAGEMENT THROUGH HEALTH CONTRACTS, PROTOTING MENTAL HEALTH THROUGH LIFE REVIEWS, PROMOTING REENGAGEMENT RATHER THAN RETIREMENT AND PROMOTING HEALTH OF FRAIL ELDERS. HEALTH ASSESSMENT: INVOLVES PERFORMANCE TOOLS (CAN CLIENT RISE FROM A CHAIR, WALK 10 FEET, ASSESS FNCTNL STATUS ➢ What are the three types of prevention and provide an explanation and example of each. PRIMARY (TO PREVENT A DISEASE FROM OCCURRING IE IMMUNIZATIONS), SECONDARY (EARLY DETECTION AND MANAGEMENT IE COLONSCOPY), TERTIARY (MANAGE CLINICAL DISEASED IN ORDER TO PREVENT THEM FROM PROGRESSING IE BETA BLOCKERS TO HELP REMODEL THE HEART IN CHF) ➢ What is the chronic disease self-management program (CDSMP)? A 17 HOUR COURSE FOR PTS WITH CHRONIC DZ TAUGHT BY LAY PEOPLE. GOAL IS TO IMPROVE SX MNGMNT, MAINTAIN FNCTNL ABILITY, ADHERE TO MED REGIMENS. ➢ What are the barriers to physical activity for the older adult? LACK OF ACCESS TO SAFE AREAS TO EXERCISE, PAIN, FATIGUE, IMPAIRMENT IN SENSORY FNCTN AND MOBILITY. ➢ What is the risk for a sedentary life style? FRAILITY , ISCHEMIC STROKE, ➢ What are the four leading causes of death in the US? CANCER, DIABETES, CAD AND CVA ➢ Are older adults at risk for poor nutrition? If so, why? Explain the barriers for older adults in regards to good nutrition? DUE TO FACT THEY HAVE MULTIPLE CHRONIC ILLNESSES, TOOTH OR MOUTH PROBLEMS, SOCIALLY ISOLATED, ECONOMIC HARDSHIP, MULTIPLE MEDS. ➢ What is a healthy weight or BMI and when should we be concerned? 22 TO 27. OVER OR UNDER ➢ What are the lab values that could show malnutrition in the older adult? SERUM ALBUMIN LESS THAN 3.5, CHOLESTEROL LESS THAN 150 ➢ Explain the general guidelines to dietary counseling. LIMIT ALCOHOL TO ONE DRINK/DAY FOR WOMEN 2 FOR MEN, LIMIT FAT AND CHOLESTEROL, BALANCED CALORIC INTAKE, DAILY CALCIUM, B12 IN CRYSTALLINE FORM, VIT D 400 TO 600 IU, WHOLE GRAINS, FRUITS AND VEGES, ADEQUATE WATER. ➢ What are the environmental risk factors that be dangerous for an older adult? Can you explain ways to modify the environment to address these safety issues? AS PER FALLS ➢ Some of the risk factors are client related. What changes of aging can make the patient at risk? ➢ Are older adults at risk for alcohol abuse? If they are, what can be done to re- educate them and prevent harm? 6 TO 11% CAGE IS A SELF REPORTING QUESTIONAIRE. CUT DOWN, ANNOYANCE, GUILT, EYE OPENER #6 Competency 742.1.6: Technology-Assisted Care of Older Adults The graduate collaborates with patients, families and the inter-professional team to select the appropriate application of technology to enhance older adults' safety and independence. This topic addresses the following learning objectives: • Recognize the value of electronic health records to care coordination among older adults across various health care settings and providers. • Identify the major types of assistive technology commonly used to enhance older adults’ function, independence, and safety. • Explain the teaching methods for introducing an older adult patient to a new technology. • Select appropriate communication technology to promote optimal transitions of care for older adults. • Select cost-effective assistive technology to promote quality of life for older adults. • Select strategies for collaborating with older adults, families, and caregivers on applying technology to enhance function, independence, and safety. • Recommend steps to successfully introduce a new technology to an older adult in a given situation. • Evaluate an older adult’s response to a newly introduced assistive technology. Assistive technology is designed to fill the patient’s gap in functional ability. This goes back to the ADLs and IADLs. What can they do and what can they not do. Can we put something in place to help them? 1 Chapter 16 is the technology chapter. There is a loss of strength, balance, visual and auditory, cognitive, and/or memory changes that occur as we age. Assistive technology is designed to help us with these losses & bridge the gap between capabilities and care needs. 1 It is anything that can enhance the function of some physical or mental ability that is impaired. It can be a cane, walker, glassed, hearing aids, wheelchair, bath bench, elevated toilet seat. All of this is assistive technology. It is filling the functional gap. 1 How do you teach an older adult about the assistive technology? Chapter 9- How older adults learn. Focus on the practical application and benefits of using them. Which type of patients are more likely to use assistive devices? CONSIDER IF THEY ARE VISUAL OR AUDITORY LEARNERS. CONSIDER BARRIERS (EDUCATION, EYESIGHT, HEARING) KEEP FORMAT SIMPLE, USE SHORTER WORDS, USE PICTURES, USE SHORTER SENTENCES, USE ACTIVE VOICE. USE EARPHONES, DECREASE BACKGROUND NOICE, CHANGE SCREEN RESOLUTIONS,. WHITE ELDERS WHO LIVE ALONE IN THE SOUTH, ARE PHYSICALLY DISABLED, TAKE MORE MEDS AND ARE LESS DEPRESSED TEND TO USE MORE EQUIPMENT AND DEVICES THAN NON WHITE ELDERS WHO LIVE IN THE NORTH AND HAVE LESS DISABILITY, TAKE FEWER MEDS AND ARE MORE DEPRESSED. 2 Review Box 16-1 on page 564: Guidelines for Introducing Technology & Teaching the Elderly about its Use DEVICE MUST BE PERCEIVED AS NEEDED, DISBELIEF IN ONES CAPABILITY MAY BE AN OBSTACLE IN ACCEPTING NEW TECHNOLOGY, GENEROUS TIME AS WELL AS REPEATED SHORT TRAINING SESSIONS, MORE STRESS SHOULD BE PUT ON PRACTICAL APPLICATION OF THE DEVICE THAN TECHNICAL FEATURES, ONLY SELECTIVE, CENTRAL FACTS SHOULD BE PRESENTED, MNEMONICS AND CUES WILL AFFECT SELF EFFICACY, TRAINING SESSIONS SHOULD BE HELD IN THE HOME OR NATURAL MEETING PLACE, INSTRUCTOR SHOULD BE WELL KNOWN BY THE ELDERLY, GOOD ATTITUDE OF INSTRUCTOR 3 Briefly discuss assistive robots and sensor-based monitoring systems that we may see used in the future and why they may be useful DEVELOP ROBOTS THAT ASSIST OLDER ADULTS SUFFERING FROM CHRONIC DISORDERS IN THEIR EVERYDAY LIFE. A ROBOT REMINDER FOR THOSE THAT HAVE SHORT TERM MEMORY, TELE-PRESENCE, MOBILE MANIPULATION; SEMI INTELLIGENT MOBILE MANIPULATOR INTEGRATES ROBOTIC STRENGTH WITH A PERSONS SENSES AND INELLECT. CAN DO LAUNDRY. SOCIAL INTERACTION = CAN ROBOTS TAKE OVER CERTAIN SOCIAL FNCTNS SENSOR BASED MONITERING: GOAL TO ALLOW PT TO REMAIN IN HOME. LOW COST SENSORS THAT DETECT MOVEMENT AND PRESSURE. DATA ANALYSIS TOOL, CAREGIVER MAY RECEIVE ALERTS OF A PROBLEM IN THE HOE. #7 Competency 742.1.7: Care Transitions The graduate evaluates the effectiveness of the healthcare environment and the influence of health policy in providing care that maximizes the function and independence of older adults in accordance with individual patient characteristics and patient and family needs. This topic addresses the following learning objectives: ➢ Explain the implications of an aging population for health policy. MAY CAUSE A PUBLIC HEALTH CRISIS WITH SO MANY BABY BOOMERS. PROVIDERS ARE AGEING RAPIDLY AND WILL BE LESS AS WELL. ➢ Compare the foundational principles, goals, and methods of identified government programs and other community health initiatives available to older adults. ➢ Identify community resources for older adults that facilitate autonomy and quality of life for a given scenario. ➢ Compare the opportunities and constraints of supportive living arrangements on the function and independence of older adults. ➢ Analyze healthcare trends related to the independence and autonomy of older adults. ➢ Analyze a given policy or legislative act that promotes or hinders the independence and autonomy of older adults. ➢ Compare the benefits and limitations of the major forms of reimbursement on the delivery of healthcare services to older adults, differentiating the roles of Medicare and Medicaid. ➢ Explain the elements of the triple aim of healthcare reform as reflected in the care of older adults. ➢ Evaluate the influence of payer systems on access, quality, and affordability of healthcare for older adults. ➢ The Patient Protection and Affordable Care Act was signed into law in 2010. The intention: 1 Eliminate lifetime limits for health insurance coverage for essential services 1 Eliminate the ability of insurance companies to rescind coverage 1 Free Preventative care 1 Development of a prevention and public health fund. 1 Increase access to affordable care, including a provision for preexisting 1 Quality improvement and risk reduction ➢ The Independence at Home Demonstration: NP’s worked with patients to help them experience a higher level of independence through better management of their chronic illnesses ➢ Provisions that have already taken effect: 1 Improved drug discounts for Medicare recipients 1 Coverage for young adults through parental health insurance until age 26. 1 Expanding coverage for early retirees 1 National preexisting-condition insurance plan to assist those individuals without coverage for at least 6 months due to a prior condition. 1 2012 mandate The US Supreme Court upheld provisions to expand Medicaid and Medicare coverage a The Medicare expansion program requires participating states to expand coverage to most individuals under the age of 65 with income below poverty levels outlined in the Act. 1 The intent of PPACA in terms of Medicare is to reduce overall cost while maintaining coverage to those entitled to Medicare. 1 A national Medicare pilot program will be developed to provide Medicare recipients with more options for long-term care, including primary care services in their homes rather than institutional care. 1 Increase services that will impact the older population include providing wellness and prevention programs at no cost to the individual and prescription drug discounts. ➢ Need to know what Part A and Part B of Medicare covers PART A HELPS TO COVER INPATIENT HOSPITAL CARE, INPT CARE IN A SKILLED NURSING FACILITY, HOSPICE CARE AND HOME HEALTH CARE. AVAILABLE WITHOUT CHARGE FOR THOSE THAT ARE ELIGIBLE. IF NOT ELIGIBLE YOU CAN STILL GET BUT PAY A PREMIUM. ESTABLISHES BENEFIT PERIODS. 90 DAYS INPT (MAY BE ADDTL COST) PART B COVERS SOME COST OF LABS, HOME HEALTH CARE, DOCTOR SVCS, OUTPT THERAPIES, MENTAL HEALTH SVCE AND OUTPT HOSPITAL. IT IS NOT MANDATORY AND IS NOT FUNDED BY MEDICARE TRUST FUND. YOU MAY PAY FOR IT OUT OF SS CHECK. PREMIUMS BASED ON INCOME. THERE IS ALSO A YEARLY DEDUCTIBLE AND 20%. ➢ What is Medicaid---what does it cover and who is eligible? TITLE XIX OF SOCIAL SECURITY ACT. FINANCED BY STATE AND FEDERAL GOV BUT ADMINISTERED BY THE STATE. COVERAGE/ELIGIBILITY DIFFER FROM STATE TO STATE. 3 TYPES (FOR LOW INCOME FAMILIES AND PEOPLE WITH DISABILITIES, LONG ERM CARE, SUPPLEMENTAL FOR LOW INCOME MEDICARE PTS) IT WILL PAY FOR WHAT MEDICARE DOESN’T PLUS COPAYS AND DEDUCTIBLES. ➢ What is Triple Aim of healthcare reform? 3 AIMS: IMPROVING THE EXPERIENCE OF CARE, IMPROVING THE HEALTH OF POPULATIONS AND REDUCING PER CAPITA COST OF HEALTH CARE. WHY? BECAUSE US HEALTH CARE IS THE MOST COSTLY IN THE WORLD. #8 Competency: Care of the Adult with Alterations in Functional Ability The graduate determines the needs of older adults and their families & caregivers in coordinating patient-centered, safe transitions of care that aim to assure the least restrictive environment relative to strengths and vulnerabilities, and reduce unnecessary hospitalizations. This topic addresses the following learning objectives: ➢ Review each of the transitions models provided in the COS. What do they attempt to accomplish? ➢ What are the problems associated with patient transfers ➢ What is the importance of discharge med reconciliation? ➢ What can be done to eliminate the problems? ➢ Cover the interdisciplinary team. Who is usually on the team? Who is most likely not going to be at a meeting? What is the team’s purpose and what is the role of the Nurse? Physician, social worker, RN or nurse practitioner, pharmacist, dietician, physical therapist occupational therapist. RN ASSESSES, PLANS, PROVIDES, COORDINATES AND EVALUATES CARE WHICH FOCUSES ON HEALTH, OPTIMAL WELLNESS, DISEASE PREVENTION AND ADVOCACY #9 Competency 742.1.9: Palliative and End-of-life Care The graduate collaborates with patients and families to support palliative care needs in order to reduce symptom burden and treatment fatigue and enhance quality of life, as well as end-of-life care that is compassionate, respectful, patient centered, and family supported. This topic addresses the following learning objectives: • Identify fundamentals of pain and symptom management in the palliative care of patients with chronic illness. • Determine the needs and wishes of patients and families related to palliative care. • Recognize aspects of care, including pain and symptom management, as priorities that contribute to a dignified end-of-life experience. • Identify legal and ethical standards related to end-of-life care. • Describe effects of grief and mourning on older adults and their families. • Determine the needs and wishes of patients nearing the end of life. • Assess the availability of services and resources to provide comprehensive end-of-life care. • Recommend appropriate interventions to facilitate the wishes of the dying and their families. ➢ You must be able to explain the differences between curative, palliative, and end of life or hospice care. CURATIVE; LIFE PROLONGING AND ACUTE CARE OPTIONS THAT FOCUS ON CURE. PALLIATIVE CARE: RELIEVES PAIN, SYMPTMS AND STRESS CAUSED BY SERIOUS ILLNESS IMPROVING PATIENTS QUALITY OF LIFE. PALLIATIVE CARE CAN BE GIVEN IN THE HOME, BUT MOST COMMONLY TAKES PLACE IN THE HOSPITAL, LTC, ETC. HOSPICE DOES THE SAME AS PALLIATIVE CARE BUT OFTEN RELIES ON FAMILY CAREGIVER AS WELL AS VISITING HOSPICE NURSE. HOSPICE YOU MUST BE CONSIDERED TO BE TERMINAL WITHIN 6 MONTHS TO BE ELIGIBLE FOR BENEFITS. PALLIATIVE CAER CAN BE RECEIVED AT ANY TIME ➢ Make sure you understand what advance directives and living wills are as well as DNR and AND request. What is the nurse’s role in this? What are the steps to initiating and caring out the patients request especially when family disagrees/ ADVANCE DIRECTIVES LEGALLY BINDING DOCUMENTATION OF ONES MEDICAL CARE DESIRES KNOWN IN CASE THEY BECOME INCAPABLE OF DOING SO LIVING WILL = LEGAL DIRECTIONS FOR MEDICAL CARE IN CASE THE PERSON IS UNABLE TO MAKE THEIR WISHES KNOWN SUCH AS DNR. DNR = DO NOT RESUSITATE, DURABLE POWER OF ATTORNEY = ALLOWS A PROXY TO MAKE MEDICAL DECISIONS FOR ANOTHER ➢ What are the signs of impending death? FISH OUT OF WATER BREATHING, CANNOT AWAKENED ARE THE SIGNS MINUTES BEFORE DEATH. ➢ What are they 2 main categories of pain? Nociceptive pain and Neuropathic pain. What types of medications works best with these types? NOCICEPTIVE PAIN IS DIVIDED INTO TWO TYPES (SOMATIC AND VISCERAL) SOMATIC PAIN INVOLVES THESE SXMS: TISSUE INJURY RESULTING IN STIMULATION OF AFFERENT NERVE ENDINGS, SKELETAL SYSTEM, SOFT TISSUE, JOINTS, SKIN OR CONNECTIVE TISSUE, TYPICALLY CAN LOCALIZEE THE PAIN, MAY DESCRIBE AS DULL ACHE, THROB, OR GNAWING, BEST TREATED WITH NSAIDS OR STEROIDS AND PARTIALLY RESPONSPIVE TO OPOID THERAPY. EXAMPLES ARE BONE FX, BONE METS, MUSCLE STRAIN. VISCERAL NOCICEPTIVE PAIN INVOLVES: ACTIVATION OF NOCICEPTORS, INTERNAL ORGANS, PT UNABLE TO LOCALLIZE, MAY USE HAND TO SHOW AREA AFFECTED BECAUSE PJAIN MAY BE DIFFUSE, DESCRIBE AS DEEP, ACHING, CRAMPING OR SENSATION OF PRESSURE, VERY RESPONSIVE TO OPOID THERAPY, EXAMPLES: SHOULDER PAIN, SECONDARRY TO LUND OR LIVER METS. NEUROPATHIC PAIN INVOLVES INJURY TO PERIPHERAL NERVES OR CNS, MAY DESCRIBE AS SHOOTING, STABBING, BURNING OR SHOCK LIKE, MAY BE CONSTANT OR INTERMITTENT, LESS RESPONSIVE TO OPOIDS, RESPONDS BEST TO ANTICONVULSANTS OR TRICYCLIC ANTIDEPRESSANTS, EXAMPES: HERPES ZOSTER OR DIABETIC NEUROPATHY. ➢ Should an older adult in pain and receiving palliative care be concerned with addiction? NO ➢ Recognize aspects of care, including pain and symptom management as priorities that contribute to a dignified end-of-life experience. MILD PAIN 91 TO 3) NSAIDS OR TYLENOL (4000MG/DAY OR LESS FOR TYLENOL) MODERATE PAIN: (4 TO 6) LOW DOSE SHORTACTING OPIOIDS IN COMBO WITH TYLENOL AND NSAIDS, CEILING DOSE FOR OPOIDS CUZ OF TYLENOL AND NSAID USE. SEVERE PAIN (7 TO 10) NO TYLENOL OR NSAIDS JUST OPOIDS NO CEILING DOSE SO CAN USE HIGHER DOSES. NONOPOIDS AND ADJUVANTS MAY ALSO BE USED AT THIS STEP SHORT HALF LIFE DRUGS: MORPHINE, HYDROMORPHONE, OXYCODONE ARE EASIER TO TITRATE THAN LONGER HALF LIFE AGONIST SUCH AS FENTANY PATCH AND METHODONE. MORPHINE IS GOLD STANDARD ONLY TRY LONG ACTING MORPHINE AFTER TRYING SEVERAL DAYS OF THE SHORT ACTIING. OPOIDS ARE CONSTIPATING USE A STOOL SOFTENER. How is quality of life influenced by burden of symptoms? ➢ Identify legal and ethical standards related to end-of-life care. ➢ Describe effects of grief and mourning on older adults and their families.PHASES: PERIOD OF NUMBNESS WHICH PROVIDES SOME EMOTIONAL PROTECTION FOR SHORT TIME, PERIOD OF YEARNING (DENY THE LOSS), MAY INCLUDE FEELINGS OF ANGER, PHASE OF DISORGANIZATION AND DESPAIR INCLUDES DIFFICULTY FNCTING IN ENVIRONMENT, MOURNER BEGINS TO FIGURE OUT HOW TO FNCTN IN EACH AREA OF DISARRAY. PHASE OF REORGANIZED BEHAVIOR IS WHEN ONE PULLS LIFE BACK TOGETHER AND A NEW NORMAL CAN BE IDENTIFIED. ANTICIPATORY GRIEF, HOPELESSNESS, HOPE, ➢ Determine the needs and wishes of patients nearing the end of life. MOST PEOPLE WISH TO DIE AT HOME. ➢ Assess the availability of services and resources to provide comprehensive end-of-life care. HOSPICE, RN, HHA, PASTOR, SOCIAL WORKER, MD, PT OT , END OF LIFE INPT HOSPICE CARE, ➢ Recommend appropriate interventions to facilitate the wishes of the dying and their families. ➢ What are “5 Wishes”? A MOVEMENT THAT ENCOURAGES PEOPLE TO PROVIDE MORE SPECIFIC INSTRUCTIONS THAN THOSE OFFERED B A LIVING WILL INCLUDING ONES WISHES IN 5 CATEGORIES: THE PERSON CHOSEN TO MAKE DECISIONS (DURABLE POWER OF ATTORNEY), THE KIND OF TX THE PERSON WANTS OR DOESN’T WANT (LIVING WILL), HOW COMFORTABLE THE PERSON WANTS TO BE, HOW THE PERSON WANTS TO BE TXD BY OTHERS, WHAT THE PERSON WANTS HIS OR HER LOVED ONES TO KNOW. AN AND ORDER IS MORE POSITIVE THAN THE NEGATIVE DNR ORDER. AND IS GIVING SOMETHING (PALLIATIVE CARE) DNR IS TAKING SOMETHING AWAY BOTH THE SAME JUST VIEWED DIFFERENTLY COMPONENTS OF PEACEFUL DYING: INSTILLING GOOD MEMORIES, UNITING WITH FAMILY, AVOID SUFFERING, MAINTAIN ALERTNESS, CONTROL, PROVACY, DIGNITY AND SUPPORT, BECOME SPIRITUALLY READY, SAY GOODBYE, DIE QUIETLY AFFORDABLE CARE ACT ALSO HAS MONEY TO TRAIN WORKERS IE CNA’s,. it eliminates preexisting illness, get rid of lifetime and annual cap on benefits. Improve data collection to change future policies. CLASS ACT: US PUBLIC LONGTERM CARE INSURANCE. PAYROLL DEDUCTION, CAN OPT OUT. NEED IMPAIRMENT FOR 90 DAYS. COVER ADL ASSIST DEVICES. COVERS MEDICATION IN THE DONUT HOLE. LARGE DR OFFICES USE 1 % OF PAY. SMALL WOULD GET 2 %, EXTRA, MEDIUM GRPS ELIGIBLE FOR BONUSES. DR BONUSES CALCULATED ON QUALITY MEASURES. LOW INCOME PEOPLE WITHOUT KIDS WILL BE ELIGIBLE FOR MEDICAID. BRADEN SCORE LOOKS AT SENSORY PERCEPTION, MOISTURE, ACTIVITY, MOBILITY, NUTRITION, AND FRICTION AND SHEAR. Very High Risk: Total Score 9 or less • High Risk: Total Score 1012 • Moderate Risk: Total Score 1314 • Mild Risk: Total Score 1518 • No Risk: Total Score 1923 DECUB ULCER. STAGE 1= BLANCHABLE SKIN STAGE 2, PARTIAL THICKNESS, SHALLOW OPEN ULCER STAGE 3 FULL THICKNESS TISSUE LOSS, SUBQ FAT MAY BE VISIBLE STAGE 4 FULL THICKNESS WITH EXPOSED BONE, TENDON OR MUSCLE MMSE MINI MENTAL STATUS EXAM. EASY TO USE GERIATRIC DEPRESSION SCALE (GDS) HAVE PT ANSWER THE QUESTIONS THEMSELVES RATHER THAN ASKING THEM THE QUESTIONS (THEY CAN BE MORE HONEST) IS THE GOLD STANDARD TEST FOR DEPRESSION CORNELL SCALE FOR DEPRESSION IN DEMENTIA (CSDD) GIVEN BY DR OR SOMEONE QUALIFIED TO GIVE A DIAGNOSIS. PATIENT FAMILY AND CAREGIVERS ARE INTERVIEWED ANXIETY SCALES: HAMILTON, BECK AND ZUNG ASSESSMENT TOOLS FOR BURDEN IN CAREGIVERS CAREGIVERE STRAIN INDEX GOOD ASSESSMENT [Show More]
Last updated: 1 year ago
Preview 1 out of 25 pages
.png)
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 01, 2021
Number of pages
25
Written in
Additional information
This document has been written for:
Uploaded
Nov 01, 2021
Downloads
0
Views
110








.png)