*NURSING > Summary > NR 508 Week 5 TD, Quiz and Summary | 100% Verified | Chamberlain College of Nursing. (All)
NR 508 Week 5 TD, Quiz and Summary | 100% Verified | Chamberlain College of Nursing.
Document Content and Description Below
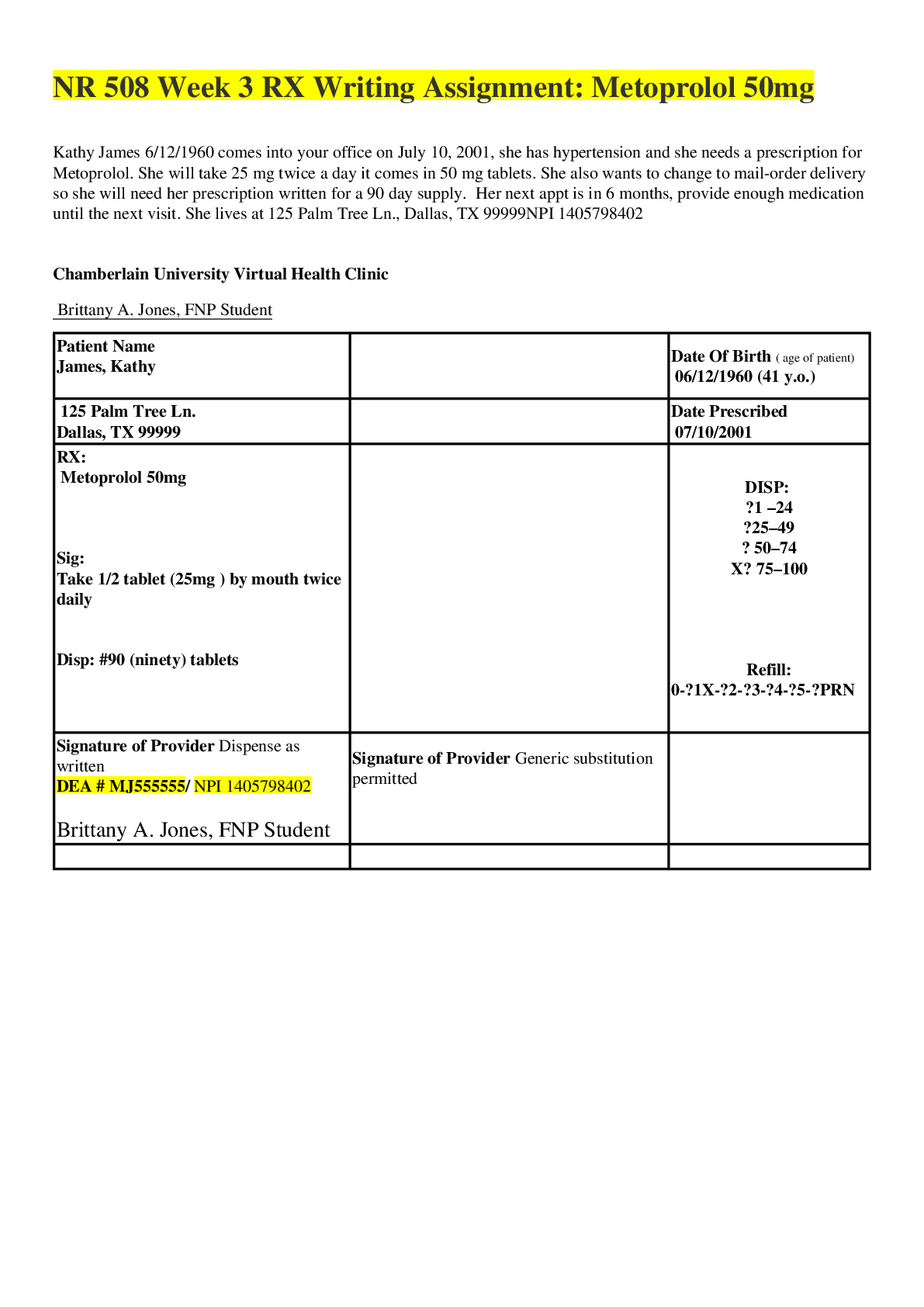
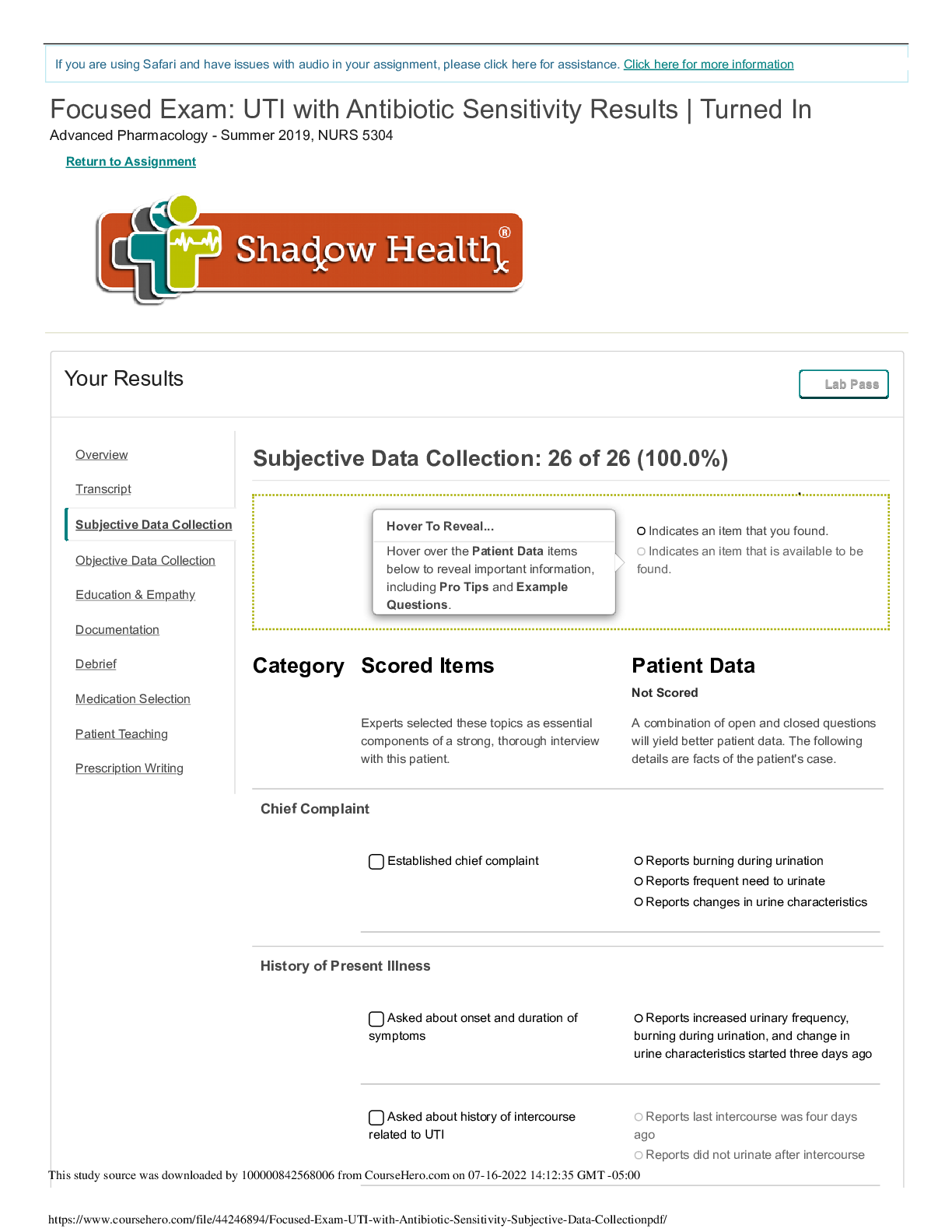
NR 508 Week 5 TD, Quiz and Summary PART 1: Leroy is a 70 year-old-man, whose wife passed away 5 years ago, and whose 2 children live out-of–state. His neighbor caretaker (Ms. Webb, a middle-ag... ed retired CNA, whom his children hired to provide home care to him 3x/week) brings him to your clinic. He presents with quite severe confusion, incidentally to very minor changes in his environment, which provokes some violence (a symptom which startles Ms. Webb), increasingly impaired judgment, and increasing repetitiousness and inconsistencies in his usual beh\avior. Upon initial work-up and physical exam, you notice an increased respiratory rate, a slight fever (100°F), and costovertebral angle tenderness on his right side. Please provide a list of differential diagnoses, as well as an indication of your primary diagnosis. Pyelonephritis, renal stones, renal abcess, bacterial prostatitis, • What additional tests would you order to confirm a diagnosis? Once this has been completed, please indicate and describe your chosen pharmacological treatment with inclusion of dose and mechanism of action of your chosen prescription. Trimethoprim- sulfamethoxazole (Bactrim), Levofloxacin (Levaquin), Take into consideration pt’s CrCl Pyelonephritis. Urinary tract infections encompass both the upper and lower portions of the urinary tract. Cysitits, also known as a bladder infection, is considered a lower urinary tract issue while pyelonephritis, also known as a kidney infection, is considered an upper urinary tract issue (Hooton, 2016). Acute pyelonephritis (APN) is responsible for approximately 14 percent of all UTIs (Enikeev, Glybochko, Alyaev, Enikeev, & Rapoport, 2017). If APN is left untreated it can cause patients to become septic as well as cause destruction of the parenchyma and kidney abscess (Piccoli et al., 2011). APN can be classified as complicated or non-complicated. Complicated involves underlying, predisposing factors such as diabetes, HIV, obstruction, stones, neoplasms, reflux nephropathy, or a collagen disease (Piccoli et al., 2011). Uncomplicated is when the patient does not have any underlying factors as previously mentioned (Piccoli et al., 2011). However, according to Hooton (2016), APN is typically considered complicated in most men who are over 50 years of age because most usually have some urologic abnormality. The clinical definition of pyelonephritis is based on presentation and includes costovertebral angle tenderness, fever, and a positive urine culture (Piccoli et al., 2011). Some patients, although rare, may present with signs of sepsis, shocks, acute renal failure, or multiple organ dysfunction, also known as MODs (Hooton, 2016). The patients urine culture will typically reveal Escherichia coli however, Staphylococcus saprophyticus may be present as well as some forms of Enterobacteriaceae, which include Klebsiella pneumonia and Proteus mirabilis (Hooton, 2016). Diagnosing APN is based on the clinical assessment and lab work. A urinalysis (UA) is a valuable diagnostic tool because it will reveal pyuria (Hooton, 2016). Almost all male patients who have pyelonephritis will have a UA that is positive for pyuria; if the UA is negative for pyuria, other diagnoses should also be considered, especially some sort of obstruction (Hooton, 2016). Patients who are very ill and/or have symptoms of urosepsis should be evaluated using radiographic imaging (Hooton, 2016). Cat Scan (CT) or ultrasound are typically used however, CT (without contrast) has become the standard study because of it’s ability to also show obstructions, gas-forming infections, calculi, abscesses, and hemorrhage (Hooton, 2016). Antibiotics should be initiated immediately, preferably with results of the urine culture. If the urine culture is not available, start the patient on a broad- spectrum antibiotic until culture results and susceptibility are known. Leroy is suffering from pyelonephritis, most likely complicated based on his age however, his medical history was not given so I cannot say definitively. Leroy also seems to be septic, After assessing Leroy, I would order a UA, urine culture, CBC, and CMP. The CBC is to evaluate WBCs and the CMP is to evaluate for renal and hepatic function. Considering Leroy is experiencing altered mental status (AMS) with some combativeness and lives alone, I would send him to the hospital for further evaluation and workup. In the hospital they will most likely order a CT of his abdomen and pelvis and begin IV antibiotic therapy with ceftriaxone (Rocephin) or levofloxacin (Levaquin). If Leroy had not presented to the office with AMS and combativeness (most likely related to urosepsis), I could have prescribed him an oral antibiotic to be taken at home. The oral antibiotic options that are appropriate for pyelonephritis are cipro, levofloxacin, or trimethoprim-sulfamethoxazole (Hooton, 2016). If oral antibiotics were appropriate for this situation, I would have prescribed cipro 250mg 1 tab PO BID for 7 days. I would choose 250mg over 500mg because of Leroy’s age, his presumed altered CrCl, and the possibility of tendinitis/tendon rupture, peripheral neuropathy, and central nervous system effects that can occur with fluoroquinolones (Epocrates, 2017). Cipro is a broad-spectrum antibiotic that covers gram positive and gram negative bacteria. Cipro is a bactericidal agent by way of inhibiting topoisomerase II and topoisomerase IV (Epocrates, 2017). Topoisomerase II is the enzyme that opposes excess supercoiling of DNA with transcription or replication (Epocrates, 2017). Topoisomerase IV is an enzyme that assists in separating daughter DNA molecules (Epocrates, 2017). The target for gram-negative bacteria is topoisomerase II (or DNA gyrase A subunit) and in gram-positive bacteria, the target is typically topoisomerase IV (Epocrates, 2017). Fluoroquinolones, including cipro, have a long post-antibiotic effect on gram-negative organisms, such as E. coli (Epocrates, 2017). Renal Abscess. Renal abscesses are typically caused by Escherichia coli, S. aureus, and Klebsiella pneumonia (Meyrier, 2016). Renal abscesses are more common that perinephric abscesses. Focal renal abscesses are common with pyelonephritis, especially with patients who have anatomical abnormalities (Meyrier, 2016). Additionally, two-thirds of patients with a renal abscess happen in patients that have renal stones (Meyrier, 2016). The predisposing risk factors associated with the development of renal abscesses are diabetes, urinary tract abnormalities, renal stones, pregnancy, cysts, neurogenic bladder, obstructions, polycystic kidneys, and papillary necrosis (Meyrier, 2016). Clinical manifestations associated with a renal abscess include vague lumbo-abdominal pain, fever, fatigue, weight loss, pallor, and sweats (Meyrier, 2016). A UA, if the abscess is communicating with the collecting system, will typically show pyuria, with moderate proteinuria and bacteriuria (Meyrier, 2016). Erythrocyte sedimentation rate (ESR), c-reactive protein (CRP), and WBCs are typically always elevated (Meyrier, 2016). Diagnostic imaging used to diagnose a renal abscess include x-ray, ultrasound, and CT with contrast, which is the preferred method (Meyrier, 2016). Based on Leroy’s clinical presentation, I do not believe he has a renal abscess. Acute bacterial prostatitis. ABP is an acute infection within the prostate, typically associated with a gram-negative bacteria (Meyrier & Fekete, 2015). The pathogens most often associated with ABP include E. coli, Klebsiella, enterobacter, serratia, pseudomonas aeruginosa, and proteus organisms (Meyrier & Fekete, 2015). The origin of the infection usually begins in the urethra or bladder and travels through the prostatic ducts (Meyrier & Fekete, 2015). Occasionally, gram-positive cocci bacteria can cause ABP, these include S. aureus, enterococci, and streptococci (Meyrier & Fekete, 2015). Clinical manifestations of ABP include fever, pelvic or perineal pain, myalgia, malaise, dysuria, chills, cloudy urine and other urinary issues (Meyrier & Fekete, 2015). Lab work will reveal pyuria, peripheral leukocytosis, elevated ESR and CRP levels, bacteriuria, elevated serum prostate specific antigen (PSA) levels, and sometimes blood cultures may be positive (Meyrier & Fekete, 2015). When assessed, the prostate exam will reveal a firm yet edematous, warm, and very tender prostate (Meyrier & Fekete, 2015). These findings are typically enough to confirm the diagnosis of ABP (Meyrier & Fekete, 2015). A urine gram-stain and culture should be ordered to determine causative organism and subsequent antibiotic treatment (Meyrier & Fekete, 2015). Based Leroy’s clinical presentation, I do not believe he has ABP. Bhat, R.A., Khan, I., & Mir, T. (2013). Emphysematous pyelonephritis: Outcome with conservative management. Indian Journal of Nephrology, 23(6), 444-447. http://proxy.chamberlain.edu:8080/login? url=http://search.ebscohost.com/login.aspx? direct=true&db=a9h&AN=91993339&site=eds-live&scope=site Enikeev, D.V., Glybochko, P., Alyaev, Y., Enikeev, M., & Rapoport, L. (2017). Imaging technologies in the diagnosis and treatment of acute pyelonephritis. Urologia, 84(3), 179-184. http://proxy.chamberlain.edu:8080/login? url=http://search.ebscohost.com/login.aspx? direct=true&db=a9h&AN=124338900&site=eds-live&scope=site Epocrates (2017). Epocrates, Inc. (Version 17.5.2) [Mobile application software]. Hooton, T. (2016). Acute complicated cystitis and pyelonephritis. UpToDate. Retrieved from https://www.uptodate.com/contents/acute- complicated-cystitis-and-pyelonephritis? source=search_result&search=pyelonephritis&selectedTitle=1~83 Meyrier, A. (2016). Renal and perinephric abscess. UpToDate. Retrieved from https://www.uptodate.com/contents/renal-and-perinephric-abscess? source=search_result&search=renal abcess&selectedTitle=1~58 Meyrier, A. & Fekete, T. (2015). Acute bacterial prostatitis. UpToDate. Retrieved from https://www.uptodate.com/contents/acute-bacterial- prostatitis?source=search_result&search=bacterial prostatitis&selectedTitle=1~150 Piccoli, G., Consiglio, V., Deagostini, M., Serra, M., Biolcati, M., Ragni, F., & … Porpiglia, F. (2011). The clinical and imaging presentation of acute “non complicated” pyelonephritis, A new profile for an ancient disease. BMC Nephrology, 12(68). http://proxy.chamberlain.edu:8080/login? url=http://search.ebscohost.com/login.aspx? direct=true&db=edswsc&AN=000304371600001&site=eds-live&scope=site PART 2: The patient is diagnosed with a severe urinary tract infection (pyelonephritis), and you decide to prescribe him sulfamethoxazole/trimethoprim (SMX/TMP) 800/160mg one tab PO Q12h x14 days Over the next couple of weeks, the symptoms associated with his UTI diminish, and his mental status improves. However, Ms. Webb brings him back to your clinic with symptoms, which scare her yet again, and she explains that she thinks he may have a relapse of his UTI. These symptoms include a high fever (103.6°F) and tachypnea, and upon pulmonary examination at your clinic, you hear crackles, and find classic findings of lung consolidation. • What laboratory tests should you order, and what is your primary diagnosis at this point and subsequent steps in his treatment and management? CXR, Lactic acid to evaluate for sepsis, primary dx is pneumonia secondary to complicated pyelonephritis and/or urosepsis. The most common cause of pneumonia is Streptococcus pneumoniae (aka pneumococcus) • Once explained, please indicate and describe your chosen pharmacological treatment with inclusion of dose and mechanism of action of your chosen prescription. Rocephin or Avelox, tx’s both levofloxacin 750 Q24 x5 days (Monitor CrCl) Patients who are positive for acute pyelonephritis (APN) that have a recurrent infection a few weeks after the initial treatment should be evaluated for complicated pyelonephritis (Hooton, 2016). A urine culture needs to be repeated and the provider should begin treatment with another antibiotic if indicated by culture and sensitivity results (Hooton, 2016) or use a longer course of the initial medication treatment (Epocrates, 2017). If the bacterial strain and susceptibilities remain the same on the repeat culture, a renal CT or ultrasound should be ordered (Epocrates, 2017). A complicated infection is typically linked to another underlying issue, which increases the risk of failure with initial treatment methods (Hooton, 2016). Complicated pyelonephritis is associated with multiple microbial organisms; it encompasses all microbes associated with uncomplicated pyelonephritis (Escherichia coli, Staphylococcus saprophyticus, Klebsiella pneumonia, and Proteus mirabilis) plus Serratia, Pseudomonas, staphylococci, fungi, and enterococci (Hooton, 2016). According to Papadakis and McPhee (2017), the drug of choice for pyelonephritis in the outpatient setting is a fluoroquinolone for 7 days. An alternative choice is Bactrim DS, however it is not the first choice (Papadakis & McPhee, 2017). Patients with pyelonephritis who are acutely ill, such as Leroy, should be hospitalized and started on ceftriaxone (Rocephin) or levofloxacin (Levaquin) IV (Papadakis & McPhee, 2017). In all the literature I have read, it is recommended that patients with complicated forms of UTIs should receive intravenous antibiotics because they have a higher risk for failing the initial oral antibiotic treatment. The patient is 74 years old, is experiencing AMS with increasing impaired judgment and combativeness, is tachypenic, and febrile. The patient lives alone and only receives care 3 times a week from a caregiver who is currently frightened by his behavior. It would be inappropriate to send this patient home on oral antibiotics because of his mental state and because he was on the verge of becoming septic. Now the patient has become septic and will need a more aggressive form of treatment. Leroy’s current diagnosis should be partially treated pyelonephritis with superimposed community acquired pneumonia. The patient should most definitely be admitted now. The best course of action would be to obtain a chest x-ray, obtain a lactic acid and procalcitonin level to gauge severity of sepsis, repeat urine cultures with sensitivity, and repeat CBC and CMP. Since we still do not know what bacteria(s) are responsible for his infection, gram-positive and gram-negative coverage should be initiated. Medications can be adjusted for sensitivity plus CrCl and GFR once labs results are available. To begin with, the patient should receive IV Rocephin for it’s mostly gram-negative properties and Vancomycin for it’s gram-positive properties plus its effectiveness with community acquired pneumonia (PDR, 2017). Rocephin provides coverage for sepsis, community acquired pneumonia, and complicated UTIs by providing (PDR, 2017). Rocephin should be started at 2G IV Q24 hours for 14 days. Rocephin is a third generation cephalosporin that is mostly bactericidal and inhibits bacterial cell wall synthesis because it adheres to penicillin-binding proteins inside the bacteria wall (PDR, 2017). The ability of Rocephin to inhibit synthesis leads to bacteria cell wall lysis (PDR, 2017). Vancomycin should be given in one dose at 250mg IV x 1 and then pharmacy should adjust the dose based on the patients CrCl and GFR. Vanco is also bactericidal and it binds to precursor units, specifically the D-alanyl- D-alanine of the peptide precursor unit, which prevents peptidoglycan polymerase and transpeptidation reactions (PDR, 2017). The end result is a change in the bacteria cell wall permeability, which leads to cell death (PDR, 2017). Epocrates (2017). Epocrates, Inc. (Version 17.5.2) [Mobile application software]. Hooton, T. (2016). Acute complicated cystitis and pyelonephritis. UpToDate. Retrieved from https://www.uptodate.com/contents/acute- complicated-cystitis-and-pyelonephritis?source=see_link Papadakis, M. & McPhee, S. (Eds.). (2017). Current medical diagnosis and treatment. New York, NY: McGraw Hill. PDR (2017). PDR, LLC. (Version 2000136, A: 2.0.4.0) [Mobile application software] PART 3: Upon receipt of laboratory results, you notice that his eGFR is ~40mL/min, his serum creatinine is 3.0 mg/dl (Stage 3 probably acute renal failure), and his BUN is 50 mg/dl. (CrCl = 21.9 ml/min/1.73m2) Need fluids, vanco adjustment, • How will the medication regimen(s) have to be adjusted given these new laboratory findings, and how should you be monitoring for efficacy and toxicity of this patient’s pharmacological profile with a summary of where this patient currently stands in his medical treatment? Leroy has Stage 3 kidney disease. At his age, I would assume it is chronic. However, since we do not have baseline lab work to go off of I cannot say definitively if it is chronic, medication related, or both. Regardless, Leroy is still suffering from unresolved pyelonephritis and pneumonia, therefore medications must be adjusted based on these results. Urea is mainly produced in the liver and then excreted via the renal tubules (Lerma, 2014). For this reason, BUN levels can be indicative of renal or liver functioning. In regards to Leroy, it would be nice to know what his liver enzymes are as well. Filtered urea goes through passive reabsorption within the proximal renal tubule (Lerma, 2014). When a patient is experiencing intravascular volume depletion, water and sodium reabsorption is heightened while urea reabsorption increases as well, resulting in an unequal increase of BUN in relation to creatinine levels (Lerma, 2014). An increased BUN-to-creatinine ratio can be indicative of a patient experiencing decreased renal perfusion (Lerma, 2014). This ratio can also be influenced by other factors, which include aminoglycoside antibiotics and cephalosporins (Lerma, 2014). The glomerular filtration rate (GFR) indicates how many functioning nephrons still remain and therefore allows providers the ability to stage kidney disease (Vadde, 2013). A declining creatinine clearance (CrCl) will denote a declining GFR and subsequent decreased renal function (Vadde, 2013). A decreased CrCl and GFR can be attributed to progressing kidney disease or from renal hypoperfusion related to medications, dehydration, heart failure, hypotension, and shock (Vadde, 2013). Leroy was prescribed Rocephin 2G IV Q24 hours for 14 days and Vancomycin 250mg IV x 1 dose and then pharmacy to adjust dosing based on CrCl and GFR. According to Epocrates and PDR (2017), dosing adjustments are not indicated with Rocephin in patients with renal impairment unless there is hepatic impairment as well; then the dose should not be more than 2G per day. For patients with hepatic and renal dysfunction, prothrombin time should be monitored because of increased risk for bleeding (Epocrates, 2017). The vancomycin will require a dosing adjustment based on Leroy’s calculated CrCl of 21.9 ml/min/1.73m2. According to Epocrates (2017), a patient with a CrCl of 10 to 50 should be administered 15mg/kg x 1 then usual dosing Q24-96 hours. Per Epocrates (2017), for community acquired pneumonia, vanco should be 15-20 mg/kg IV Q8-12 hours for a minimum of 5 days. To make sure vanco drug levels are therapeutic and not toxic, a vanco peak and trough should be monitored; toxicity is greater than 20 mcg/mL (Epocrates, 2017). With vanco, you need a baseline BUN and creatinine and then continue monitoring regularly (Epocrates, 2017). Epocrates (2017). Epocrates, Inc. (Version 17.5.2) [Mobile application software]. Lerma, E. (2014). Blood urea nitrogen (BUN). Medscape. Retrieved from http://emedicine.medscape.com/article/2073979-overview Vadde, R. (2013). Creatinine clearance. Medscape. Retrieved from http://emedicine.medscape.com/article/2117892-overview - a2 PDR (2017). PDR, LLC. (Version 2000136, A: 2.0.4.0) [Mobile application software] SUMMARY: This week, we discussed Leroy who presented with a pyelonephritis. Sulfamethoxazole/trimethoprim (SMX/TMP) was prescribed beginning with 2 g initially as a loading dose, followed by 1 g as a maintenance dose BID as described in Part 2. Mechanistically, Sulfonamides have bacteriostatic activity and exert their effect by being a competitive antagonist, inhibiting the synthesis of folic acid, thereby preventing the reproduction of bacteria that synthesize folic acid. Additionally, trimethoprim bonds to dihydrofolate reductase, another enzyme essential for folate synthesis. Our patient eventually was also diagnosed with community-acquired pneumonia (CAP) with many of you correctly prescribing Fluoroquinolone. Quinolones inhibits DNA gyrase, an enzyme essential in the transcription, replication and repair of bacterial DNA. In part 3, we discussed his compromised renal function, which increases the half-life of fluoroquinolone. As such, a dosage adjustment (decreased) was needed. Some of you prescribed a systemic quinolone such as ciprofloxacin. These may also be utilized however should be prescribed with caution in patients with CNS disorders (ie seizures) or cerebrovascular disease (ie cerebral arteriosclerosis). PEER: Hi Kelly, I agree with your choice of medication. According to Papadakis and McPhee (2017), the likely causative pathogens for pyelonephritis are E. coli, K. pneumoniae, Proteus species, and S. saprophyticus. Per Papadakis and McPhee (2017), the drug of choice for the outpatient treatment of pyelonephritis is fluoroquinolones for 7 days. According to Epocrates (2017), the fluoroquinolones of choice for mild-to-moderate symptoms associated with uncomplicated disease are cefixime, ciprofloxacin, and ofloxacin, with the secondary choice being levofloxacin or Bactrim. An alternative medication, if there is contraindication or resistance to the preferred choice, is Bactrim DS taken twice daily for 7 to 14 days (Papadakis & McPhee, 2017). For the acutely ill patient with pyelonephritis requiring hospitalization, the likely causative organisms include E. coli, Klebsiella, Enterobacter, and Pseudomonas (Papadakis & McPhee, 2017). Rocephin 1G Q24H, Cipro 400mg Q12H, or Levaquin 500mg daily are the medications of choice in this scenario (Papadakis & McPhee, 2017). Of course, a UA and culture with sensitivity should be ordered and empiric antibiotic treatment should be initiated while waiting on the results of the culture. Papadakis, M. & McPhee, S. (Eds.). (2017). Current medical diagnosis and treatment. New York, NY: McGraw Hill. QUIZ: A patient has a sore throat with fever. The primary care NP observes erythematous 4+ tonsils with white exudate. A rapid antigen strep test is negative, and a culture is pending. The NP orders amoxicillin as empiric treatment. The patient calls the next day to report a rash. The NP should suspect: a serum sickness reaction to the penicillin. penicillin drug allergy. scarlatiniform rash from the streptococcal infection. a viral cause for the patient’s symptoms. Flag this Question Question 20 pts A patient is taking amantadine to treat a viral infection. The patient calls the primary care NP to report having blurred vision. The NP should: tell the patient to stop the medication immediately. question the patient about suicidal ideation. counsel the patient to avoid driving until this subsides. tell the patient to come to the clinic for an electroencephalogram. Flag this Question Question 30 pts A primary care NP sees a patient who has fever, flank pain, and dysuria. The patient has a history of recurrent urinary tract infections (UTIs) and completed a course of trimethoprim-sulfamethoxazole (TMP/SMX) the week before. A urine test is positive for leukocyte esterase. The NP sends the urine for culture and should treat this patient empirically with: TMP/SMX. gemifloxacin. ciprofloxacin. azithromycin. Flag this Question Question 40 pts An 80-year-old patient who has COPD takes TMP/SMX for acute exacerbations, which occur three or four times each year. To monitor this patient for adverse drug reactions, the primary care NP should order: blood urea nitrogen and creatinine. liver function tests. a complete blood count (CBC) with differential. serum bilirubin levels. Flag this Question Question 50 pts A sexually active woman is being treated for streptococcal pharyngitis. The patient takes oral contraceptive pills (OCPs). Which penicillin should the primary care NP prescribe for this patient? Penicillin G Dicloxacillin Ampicillin Penicillin V Flag this Question Question 60 pts A patient was diagnosed with tinea corporis and given topical ketoconazole. The patient tells the primary care nurse practitioner (NP) that the infection is not getting better. The NP should: obtain a culture of the infection site. recommend 3 more weeks of treatment with the topical medication. prescribe oral ketoconazole. prescribe griseofulvin. Flag this Question Question 70 pts A patient who has BPH is taking doxazosin and finasteride. The patient asks the primary care NP whether he has an increased risk of prostate cancer. The NP should tell him: his cancer risk is the same as any other man his age. he has an increased risk of a certain type of cancer. doxazosin will increase his cancer risk, but only slightly. his overall cancer risk is increased. Flag this Question Question 80 pts A patient who is taking isoniazid and rifampin for latent TB is seen by the primary care NP for a routine follow-up visit. The patient reports having nausea, vomiting, and a decreased appetite. The NP should: ask about alcohol intake. order liver and renal function tests and serum glucose. reassure the patient that these side effects are common. suggest taking the medications with food. Flag this Question Question 90 pts A 70-year-old patient will begin taking cefdinir (Omnicef) for an acute exacerbation of COPD. Before initiating therapy, the primary care NP should order: coagulation studies. an electrocardiogram (ECG). a creatinine clearance test. liver function tests (LFTs). Flag this Question Question 100 pts A patient is taking tetracycline for a rickettsial infection and reports having heartburn. The primary care NP should: ask the patient how the medication is taken. recommend drinking milk when taking the medication. tell the patient to use antacids when heartburn occurs. tell the patient to take the medication with food. Flag this Question Question 110 pts A patient comes to the clinic with a history of fever of 102° F for several days, poor appetite, and cough. A sputum culture is pending, but Gram stain indicates a bacterial infection. The primary care nurse practitioner (NP) should: prescribe an antibiotic when culture and sensitivity results are known. begin empirical antibiotic therapy. use a broad-spectrum antibiotic for initial treatment. offer symptomatic treatment only unless the patient’s condition worsens. Flag this Question Question 120 pts A young woman will begin taking minocycline. The primary care NP should tell this patient to: use a backup form of contraception if currently taking oral contraceptive pills. avoid taking antacids while taking this drug. always take the medication on an empty stomach. expect headaches while taking this medication. Flag this Question Question 130 pts A primary care NP sees a 6-month-old patient who has a persistent staccato cough. The NP is aware that there is a pertussis outbreak in the community. The NP should obtain appropriate cultures and treat empirically with: azithromycin. erythromycin. telithromycin. clarithromycin. Flag this Question Question 140 pts A patient has urethritis. The primary care NP should prescribe: tetracycline. demeclocycline. minocycline. doxycycline. Flag this Question Question 150 pts A patient with group A β-hemolytic streptococcal pharyngitis is treated with penicillin V. At a follow-up visit 2 weeks later, the patient presents with edema of the hands and feet, blood pressure of 140/85 mm Hg, and cola- colored urine. A urine dipstick shows proteinuria. The primary care NP should: obtain an ASO titer and creatinine clearance. perform a repeat throat culture. order oral amoxicillin-clavulanate for 14 days. prescribe 10 more days of penicillin V. Flag this Question Question 160 pts A 60-year-old patient comes to the clinic reporting a sudden onset of a painful rash that began the day before. The primary care NP notes a vesicular rash along a dermatome on one side of the patient’s back. The patient has a low-grade fever. The NP will prescribe: varicella vaccine. amantadine (Symmetrel). metronidazole (Flagyl). acyclovir (Zovirax). Flag this Question Question 170 pts A man who has cardiovascular disease and takes nitroglycerin for angina pain develops erectile dysfunction. The primary care NP who cares for this patient should recommend: use of a vacuum constriction device. testosterone injections. sildenafil (Viagra). vascular reconstruction surgery. Flag this Question Question 180 pts Which antibiotic requires administration of a loading dose? Zithromax E-Mycin Erythrocin Ilosone Flag this Question Question 190 pts A patient who has had two recent urinary tract infections is in the clinic with dysuria and fever. The primary care NP reviews the patient’s chart and notes that in both previous cases the causative organism and sensitivity were the same. The NP should: order a urine culture and sensitivity and wait for results before treating. order a urine culture and treat empirically pending culture results. treat the patient empirically without a culture. order a microscopic evaluation of the urine and an antibiotic. Flag this Question Question 200 pts A primary care nurse practitioner (NP) is prescribing once-daily azithromycin to a 25-year-old woman. When teaching her about the drug, the NP should tell her to: take the medication on an empty stomach. use a backup contraception method other than oral contraceptive pills. expect severe gastrointestinal side effects while taking this drug. cut the pill in half and take twice daily if side effects are severe. Flag this Question Question 210 pts A primary care NP sees a patient who was recently hospitalized for infection and treated with gentamicin for 10 days. The patient tells the NP that the drug was discontinued early because “my blood level was too high.” The NP should order: a serum blood urea nitrogen (BUN) and creatinine. a urinalysis and complete blood count. a serial audiometric test. serum calcium, magnesium, and sodium. Flag this Question Question 220 pts A patient has begun treatment for HIV. The primary care NP should monitor the patient’s complete blood count (CBC) at least every months. 3 to 6 1 to 3 9 to 12 6 to 9 Flag this Question Question 230 pts A female patient presents with grayish, odorous vaginal discharge. The primary care NP performs a gynecologic examination and notes vulvar and vaginal erythema. Testing of the discharge reveals a pH of 5.2 and a fishy odor when mixed with a solution of 10% potassium hydroxide. The NP should: order metronidazole 500 mg twice daily for 7 days. order topical fluconazole. withhold treatment until culture results are available. prescribe a clotrimazole vaginal suppository for 7 days. Flag this Question Question 240 pts A patient tells the primary care NP that he has difficulty getting and maintaining an erection. The NP’s initial response should be to: evaluate his cardiovascular status. order a papaverine injection test to screen for erectile dysfunction. perform a medication history. prescribe sildenafil (Viagra). Flag this Question Question 250 pts A female patient has vaginal candidiasis and has taken a single dose of fluconazole without resolution of the infection. The primary care NP obtains a culture and should order: griseofulvin for 4 weeks. another dose of fluconazole. oral ketoconazole. topical miconazole (Monistat) SUMMARY: This week, we discussed Leroy who presented with a pyelonephritis. Sulfamethoxazole/trimethoprim (SMX/TMP) was prescribed beginning with 2 g initially as a loading dose, followed by 1 g as a maintenance dose BID as described in Part 2. Mechanistically, Sulfonamides have bacteriostatic activity and exert their effect by being a competitive antagonist, inhibiting the synthesis of folic acid, thereby preventing the reproduction of bacteria that synthesize folic acid. Additionally, trimethoprim bonds to dihydrofolate reductase, another enzyme essential for folate synthesis. Our patient eventually was also diagnosed with community-acquired pneumonia (CAP) with many of you correctly prescribing Fluoroquinolone. Quinolones inhibits DNA gyrase, an enzyme essential in the transcription, replication and repair of bacterial DNA. In part 3, we discussed his compromised renal function, which increases the half-life of fluoroquinolone. As such, a dosage adjustment (decreased) was needed. Some of you prescribed a systemic quinolone such as ciprofloxacin. These may also be utilized however should be prescribed with caution in patients with CNS disorders (ie seizures) or cerebrovascular disease (ie cerebral arteriosclerosis). [Show More]
Last updated: 1 year ago
Preview 1 out of 20 pages
 (1).png)
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 11, 2021
Number of pages
20
Written in
Additional information
This document has been written for:
Uploaded
Nov 11, 2021
Downloads
0
Views
63

 (1).png)



.png)