*NURSING > SHADOW HEALTH > Shadow Health Comprehensive Assessment Tina Jones -Documentation /Electronic Health Record. (All)
Shadow Health Comprehensive Assessment Tina Jones -Documentation /Electronic Health Record.
Document Content and Description Below
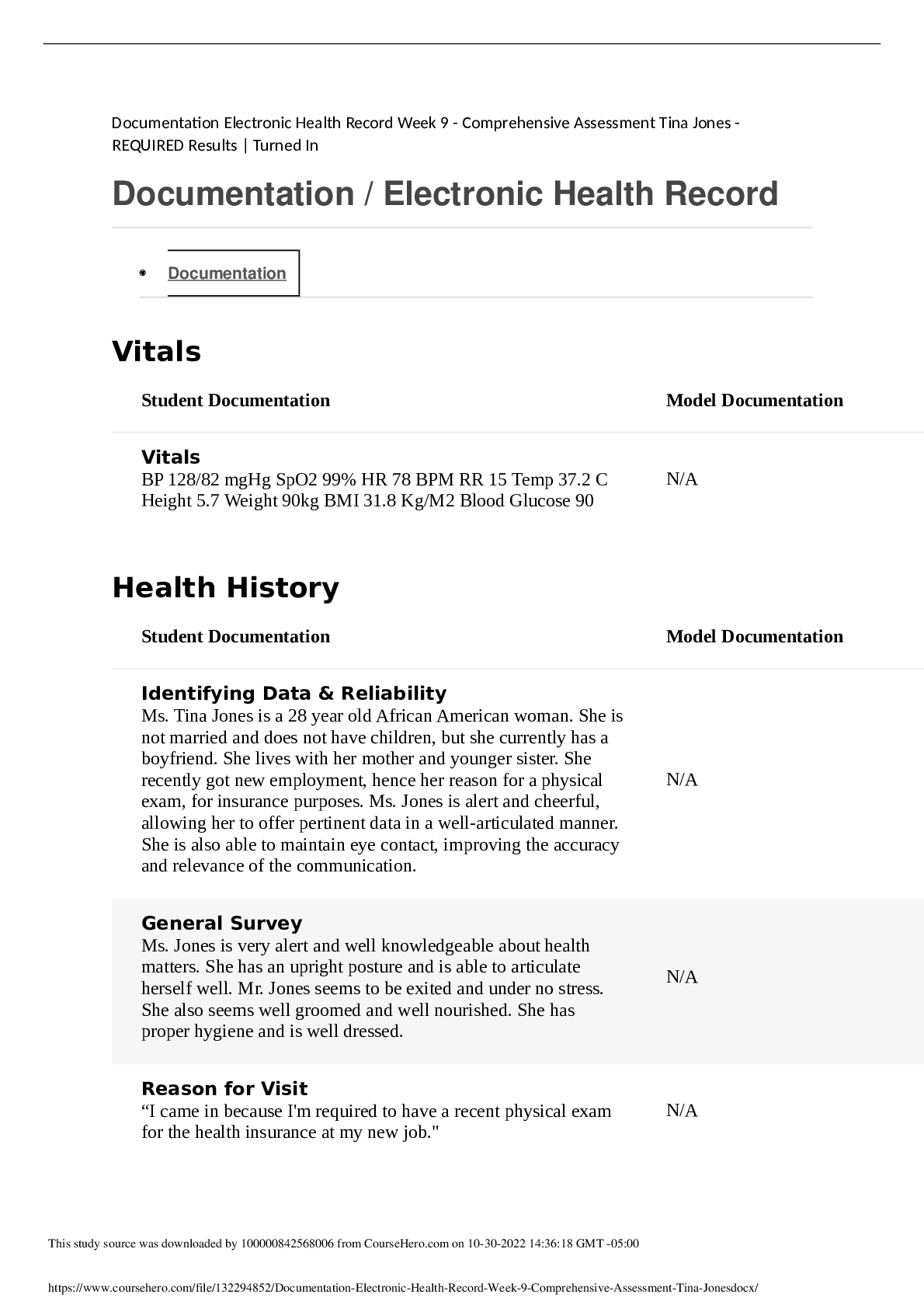
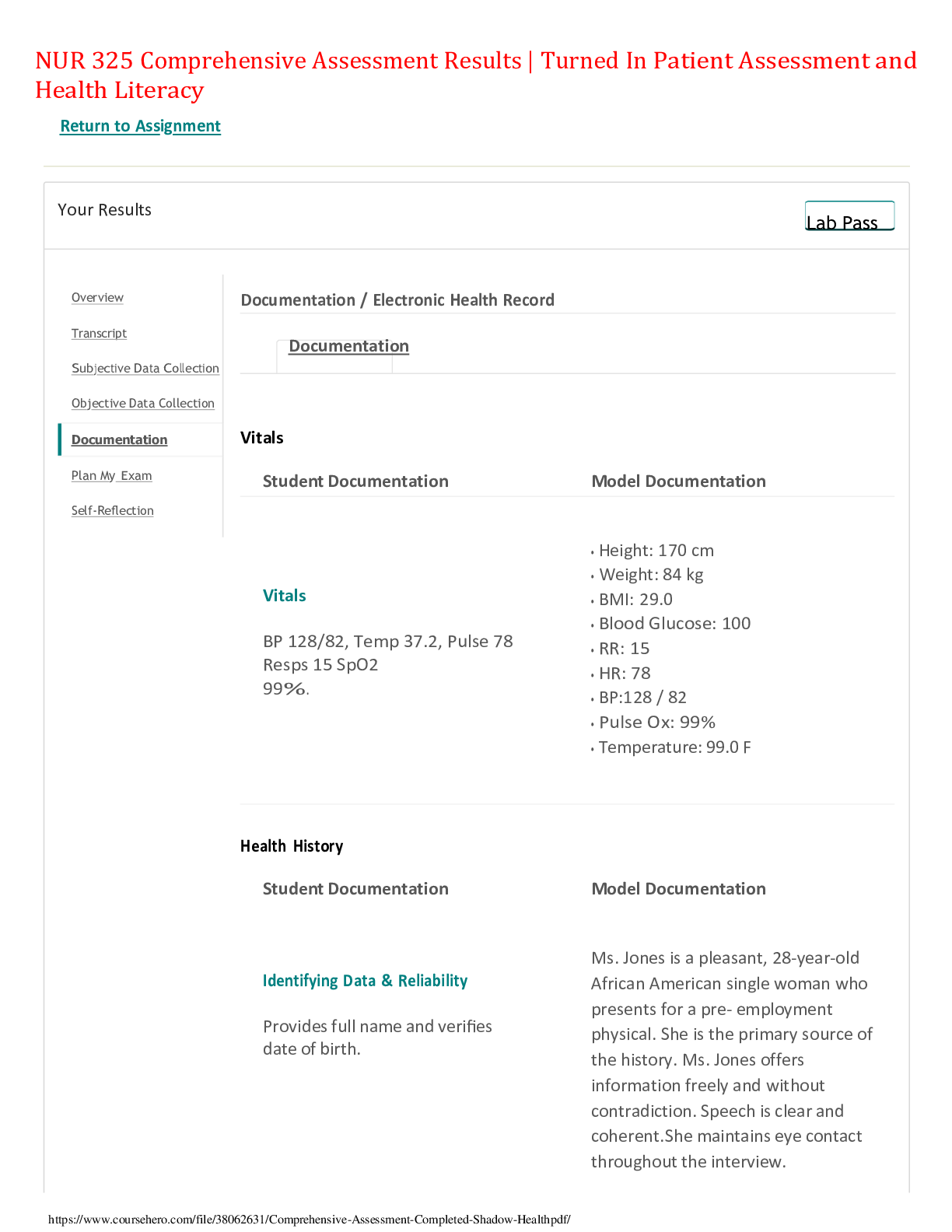
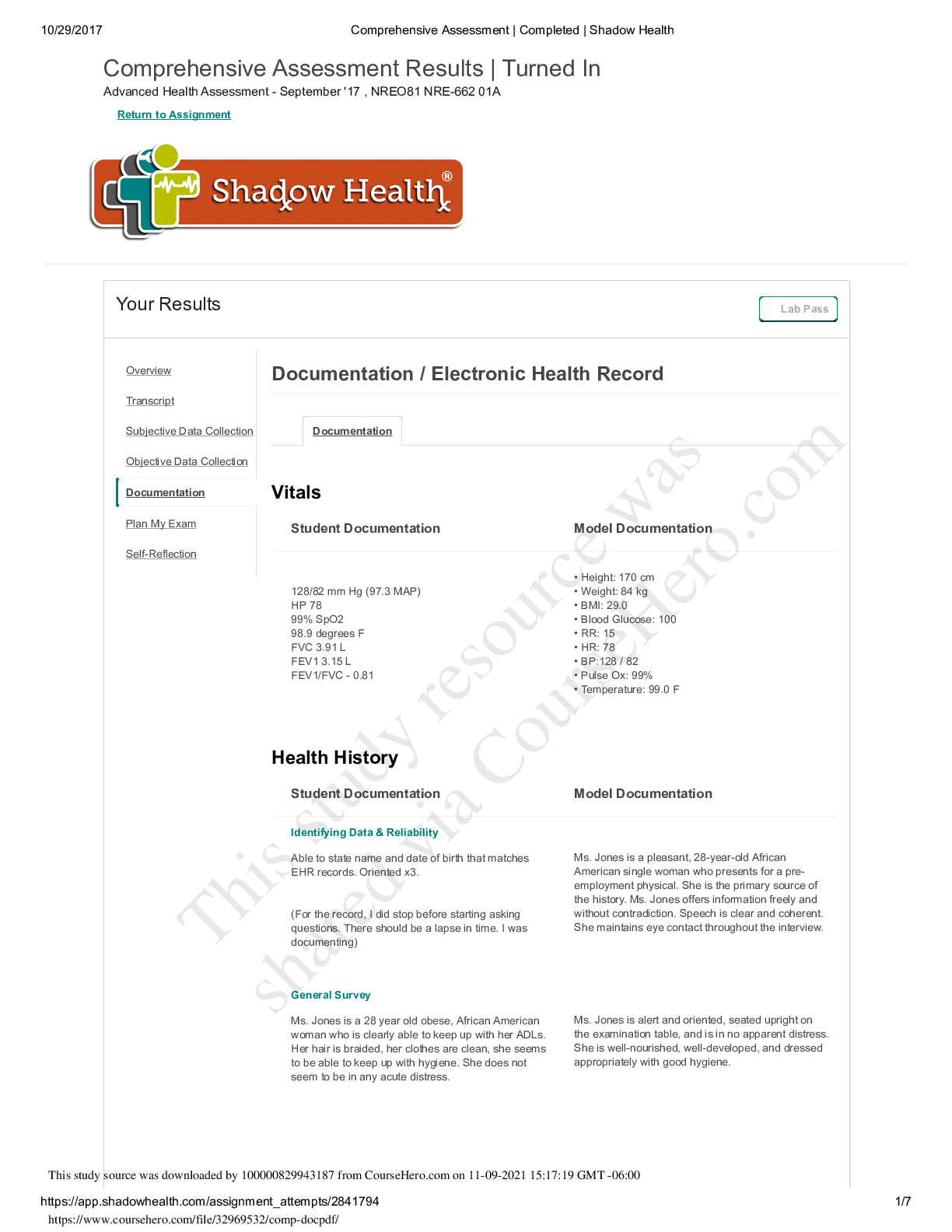
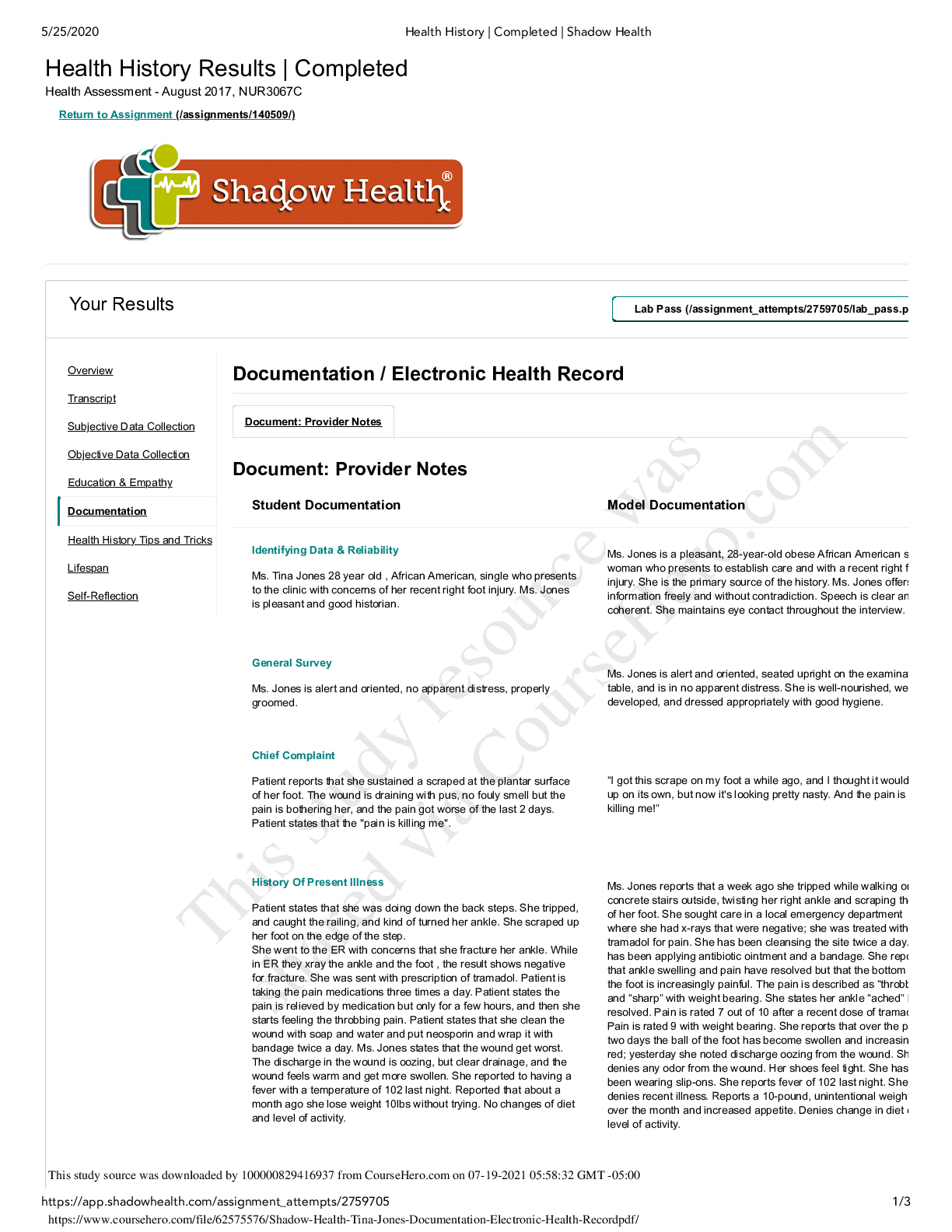
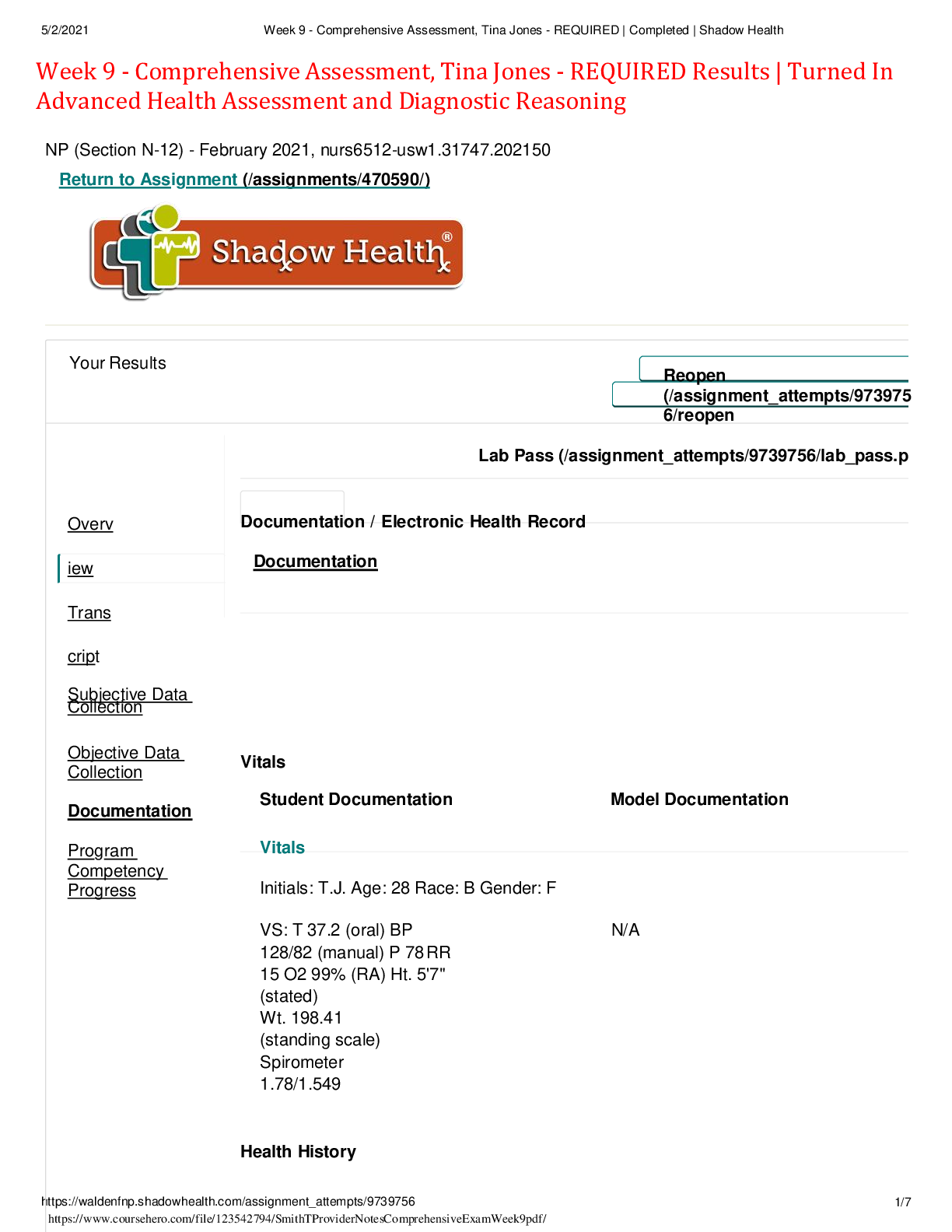
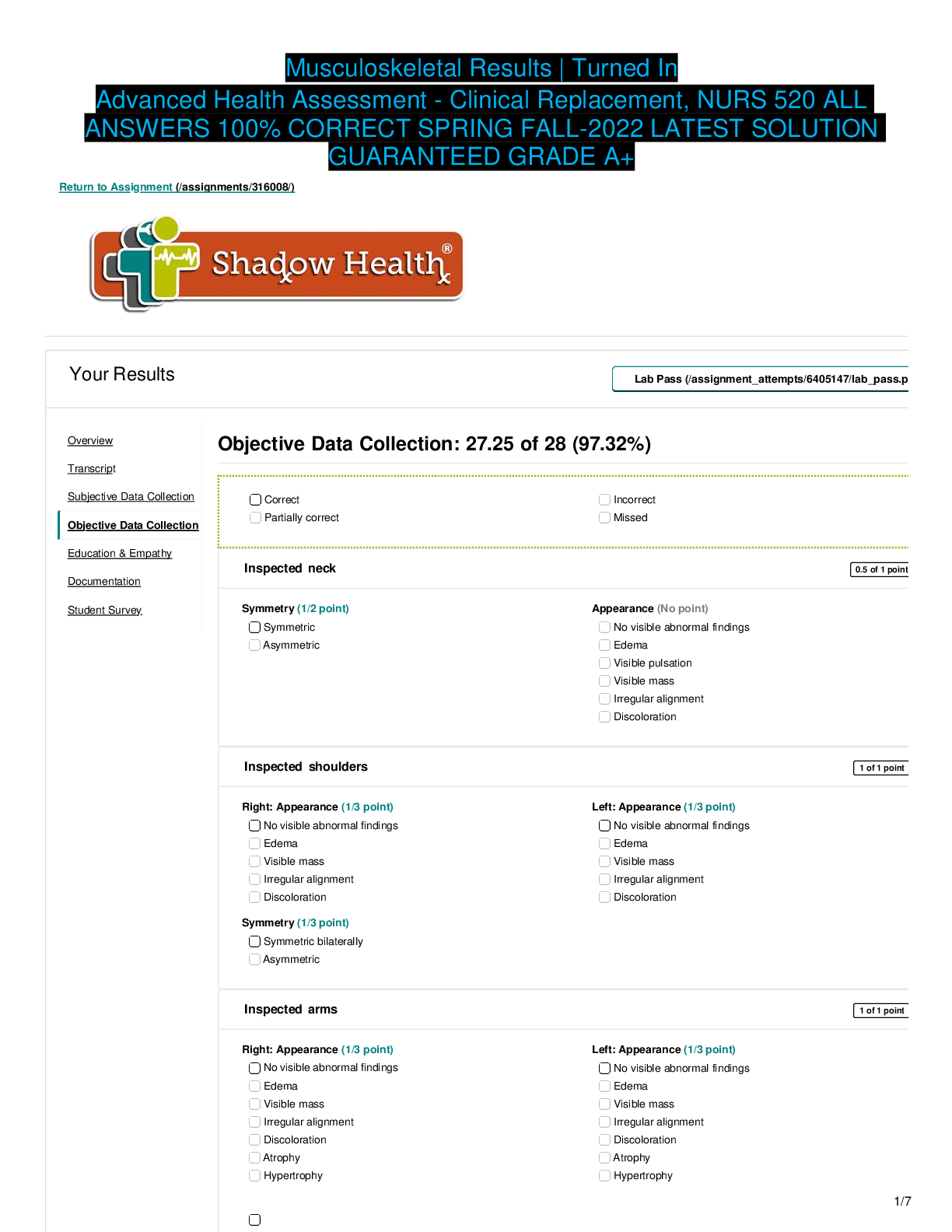
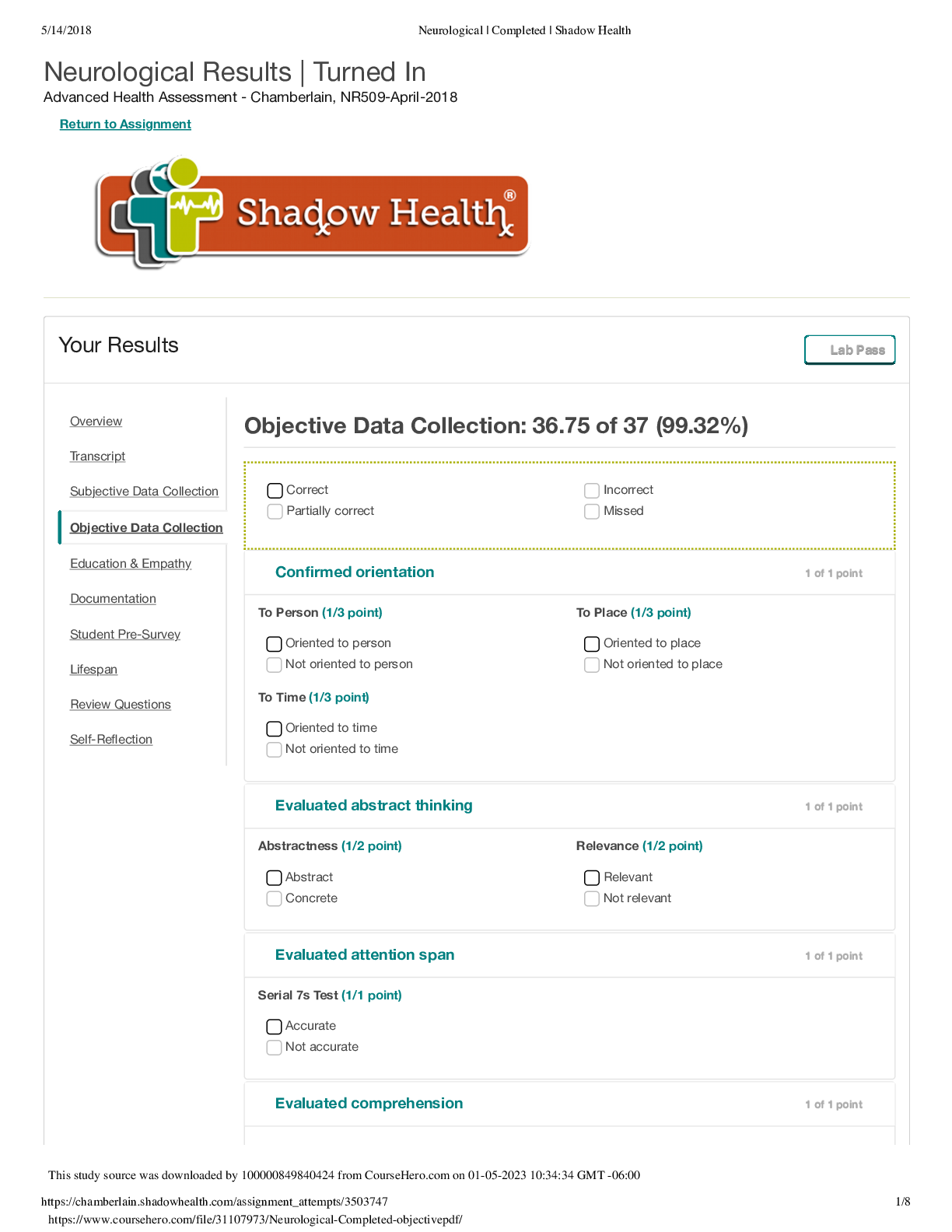
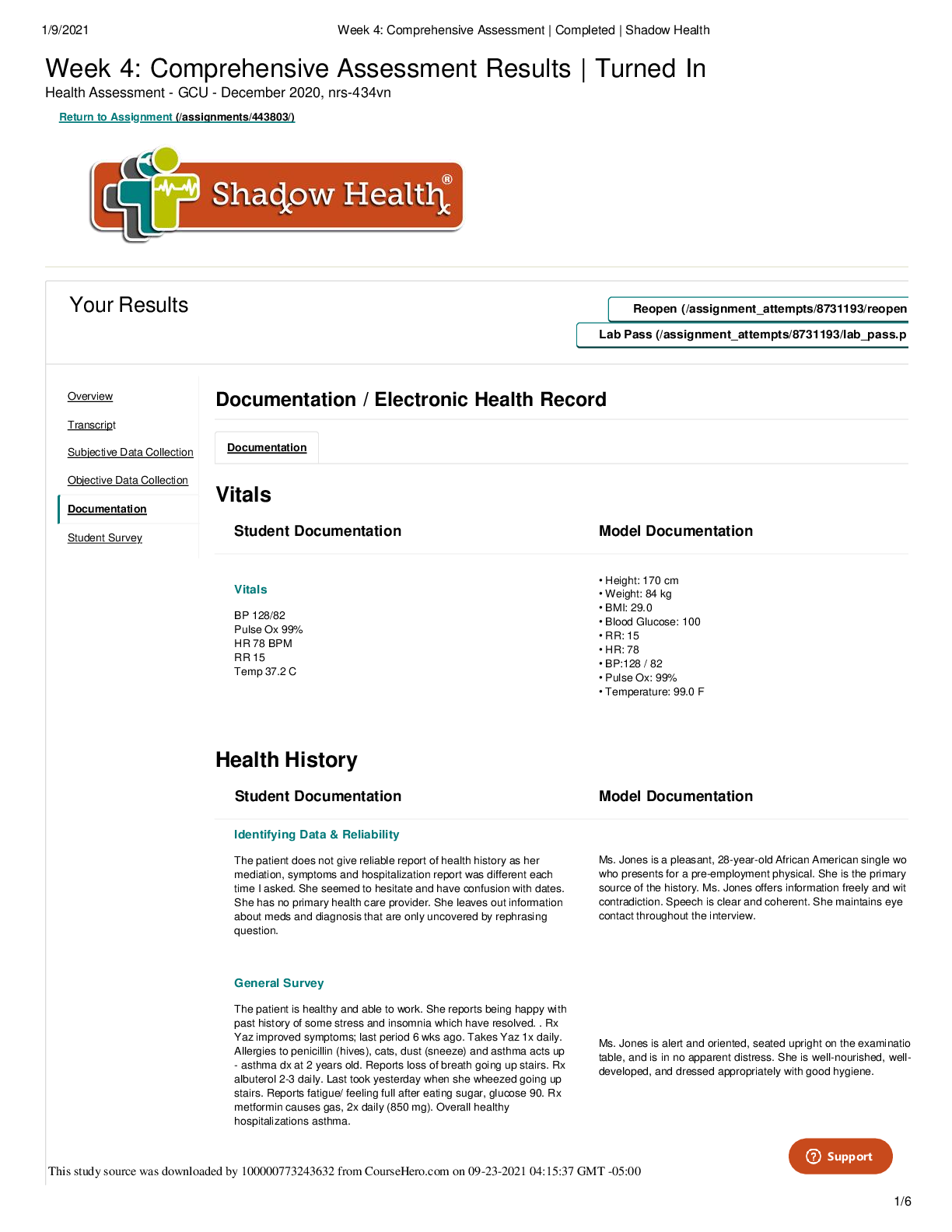
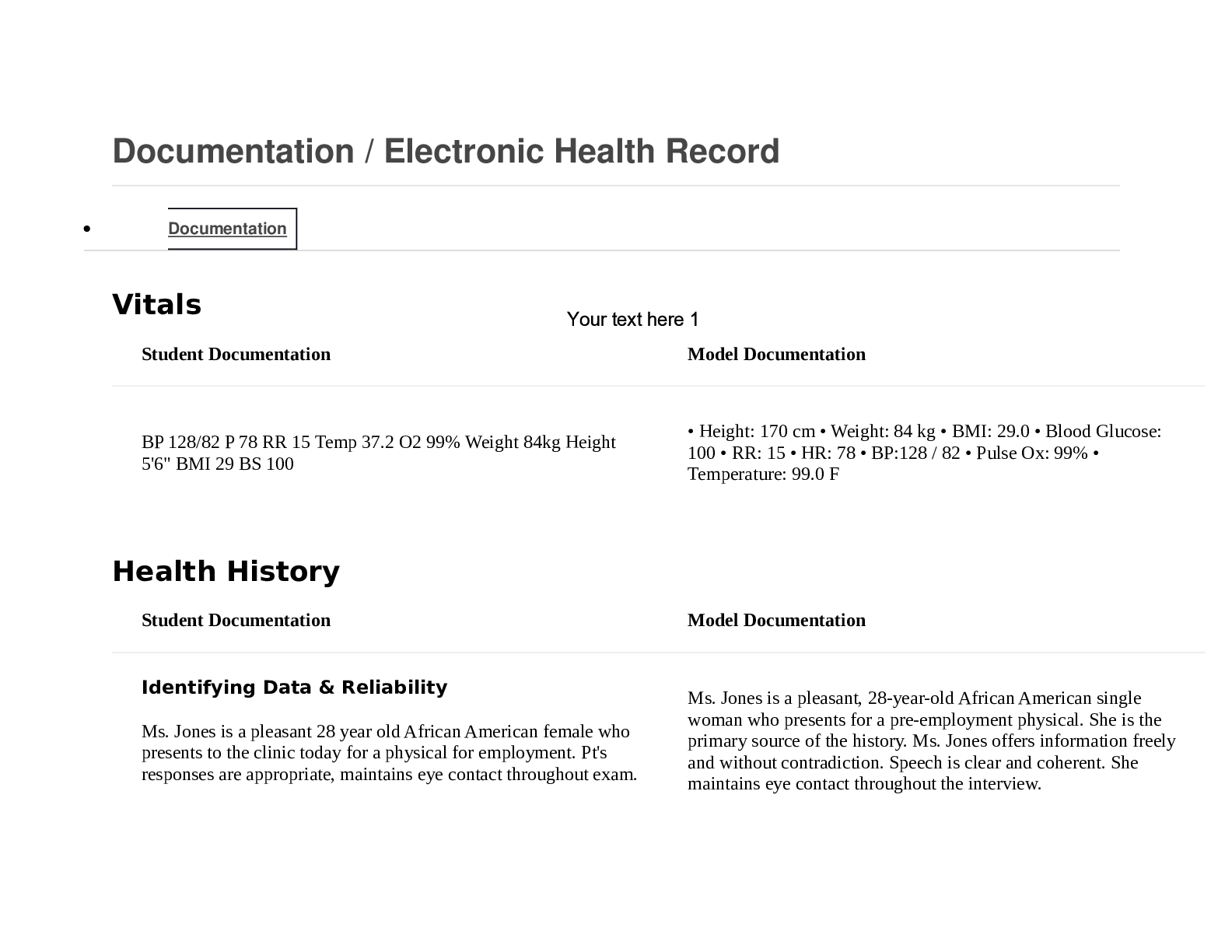
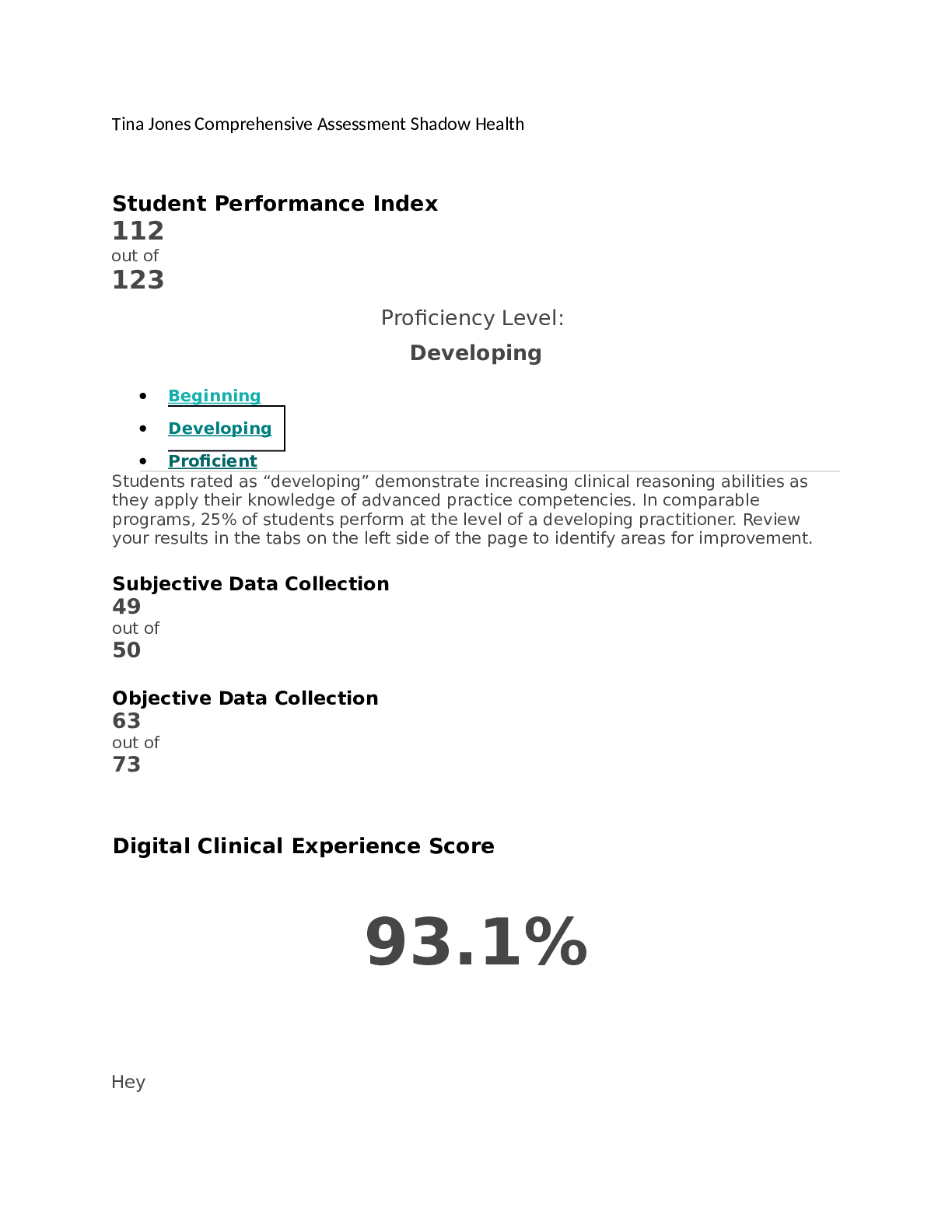
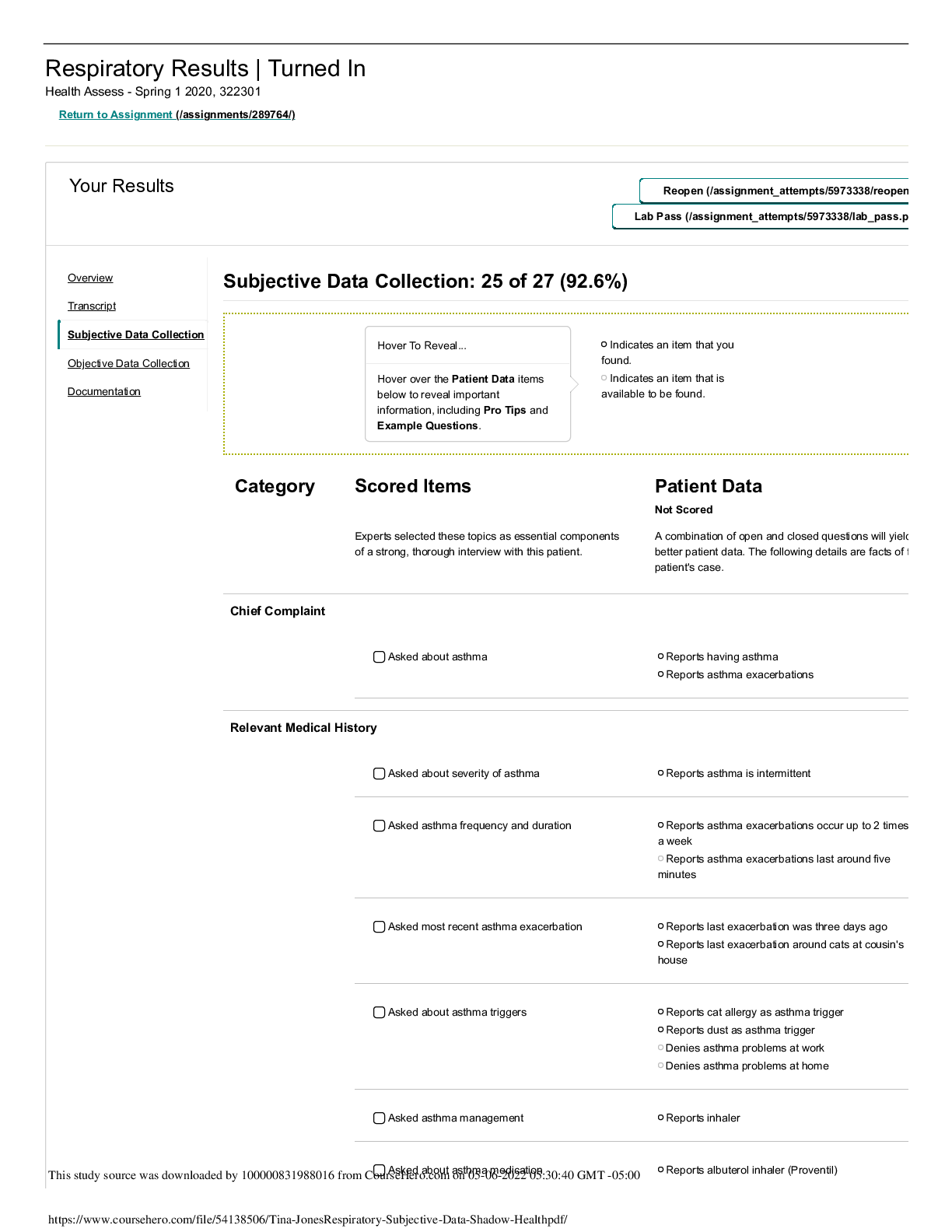
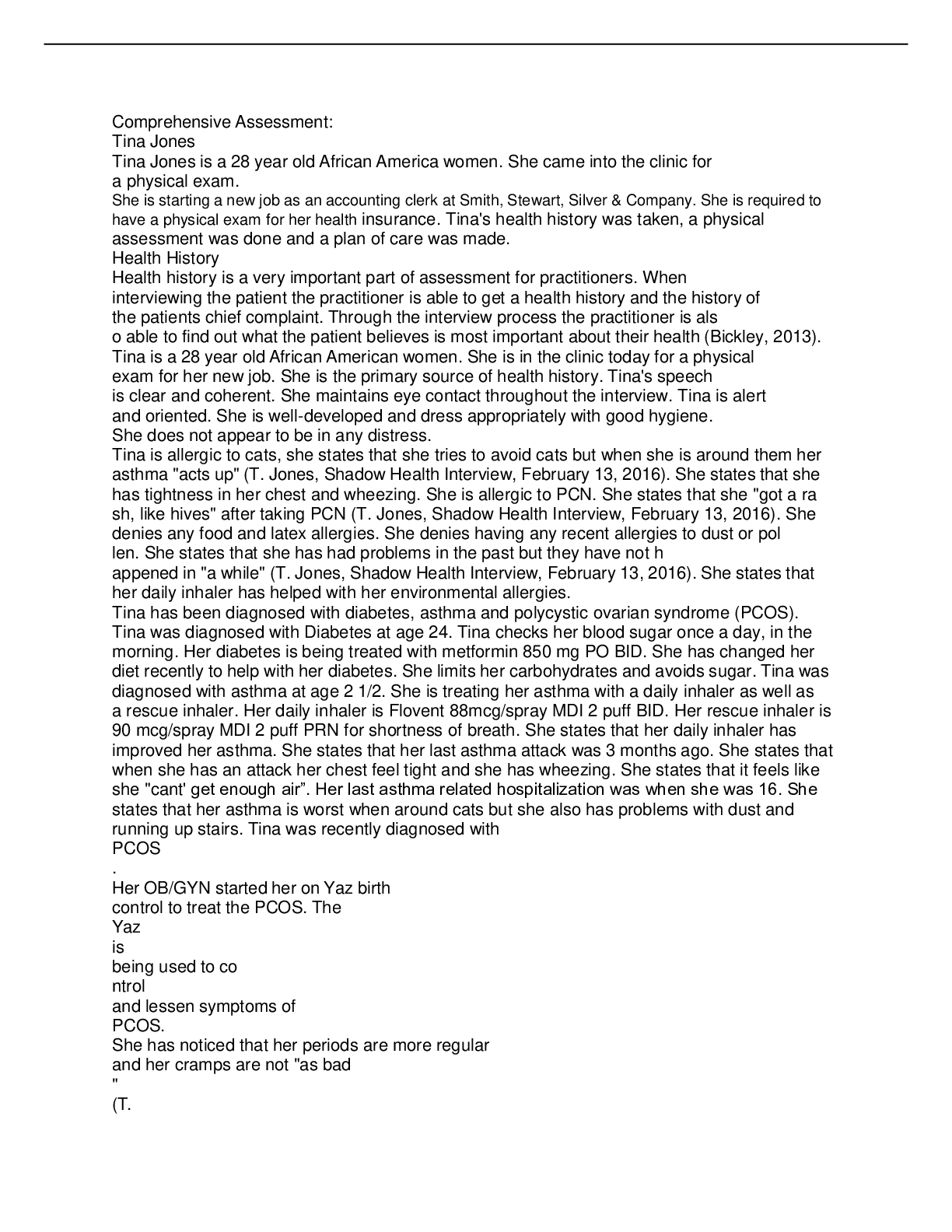
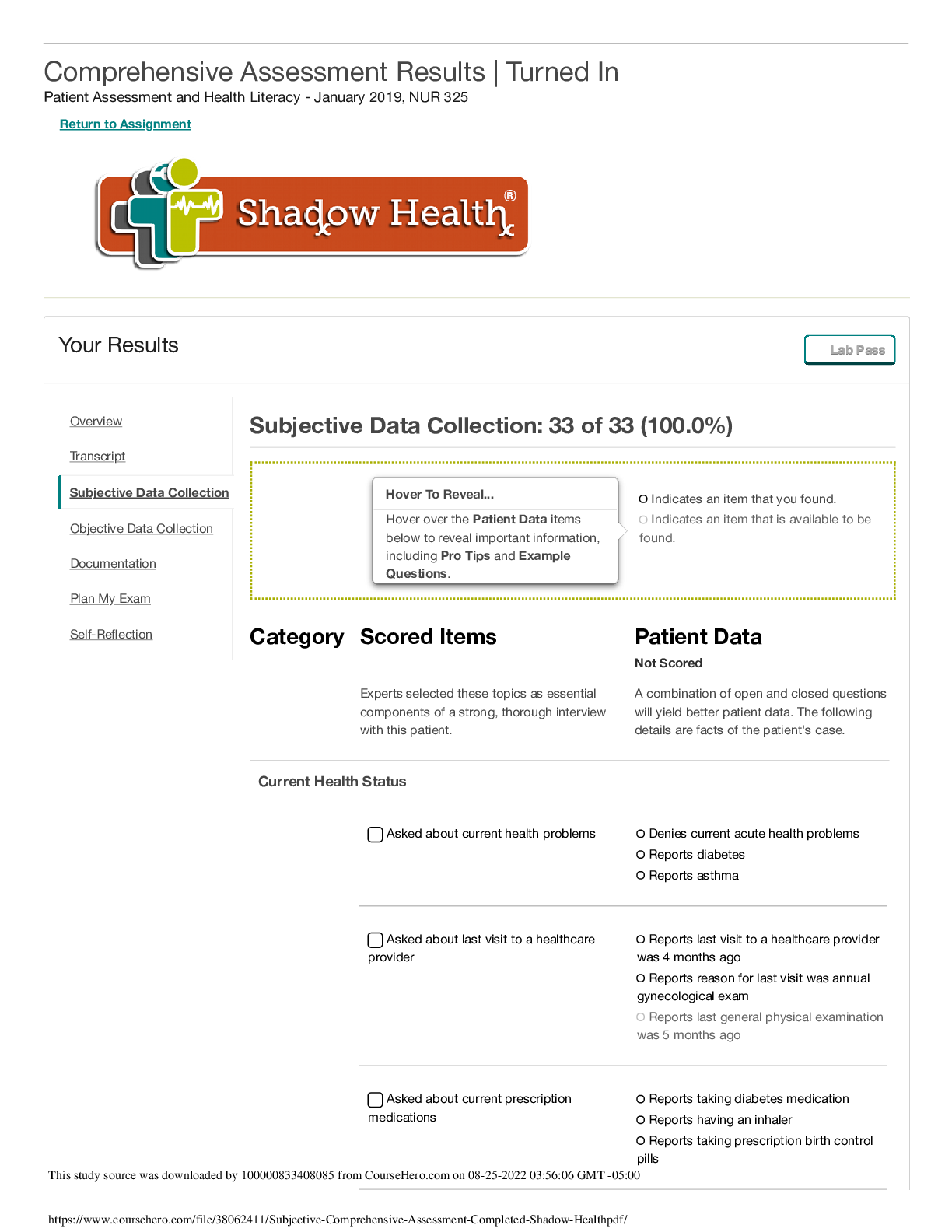
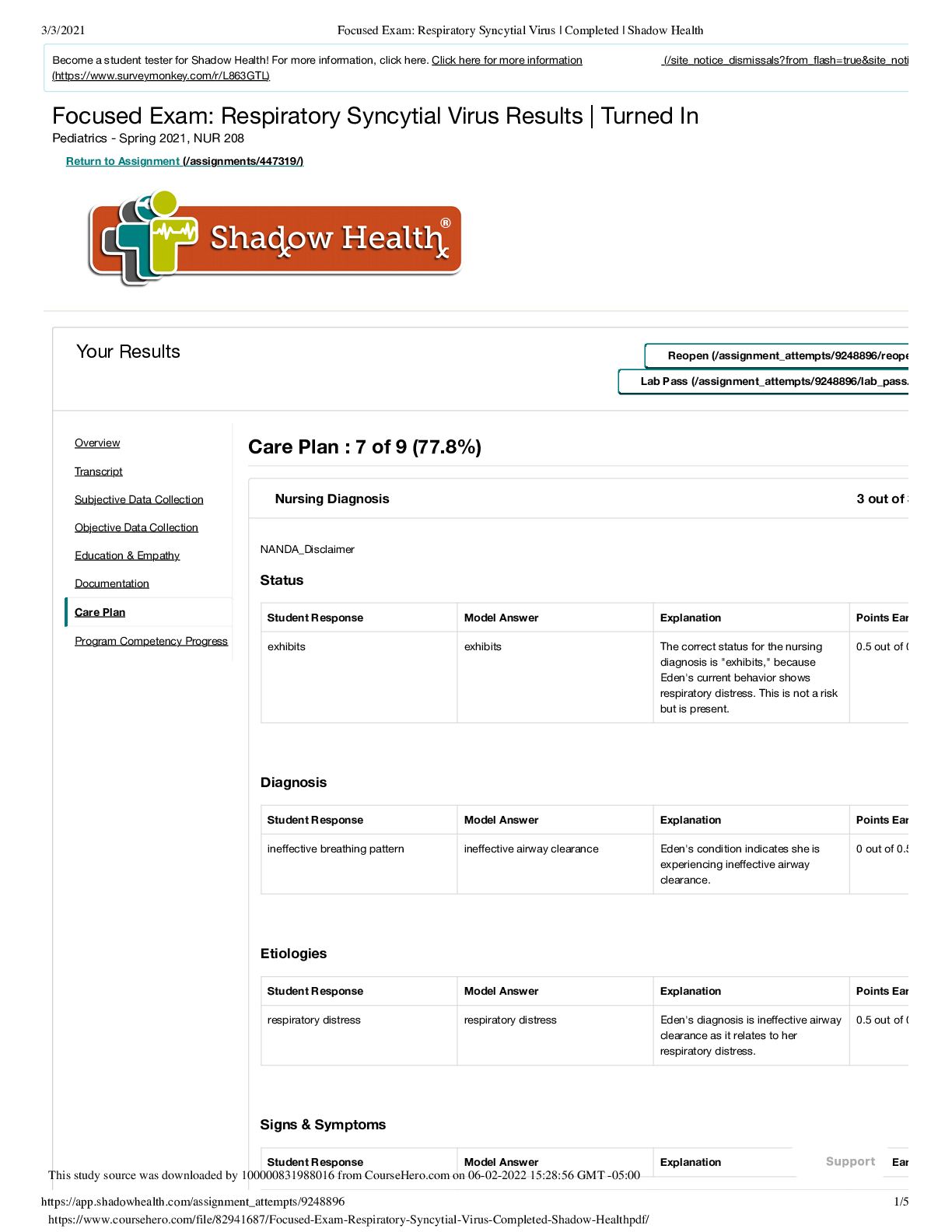
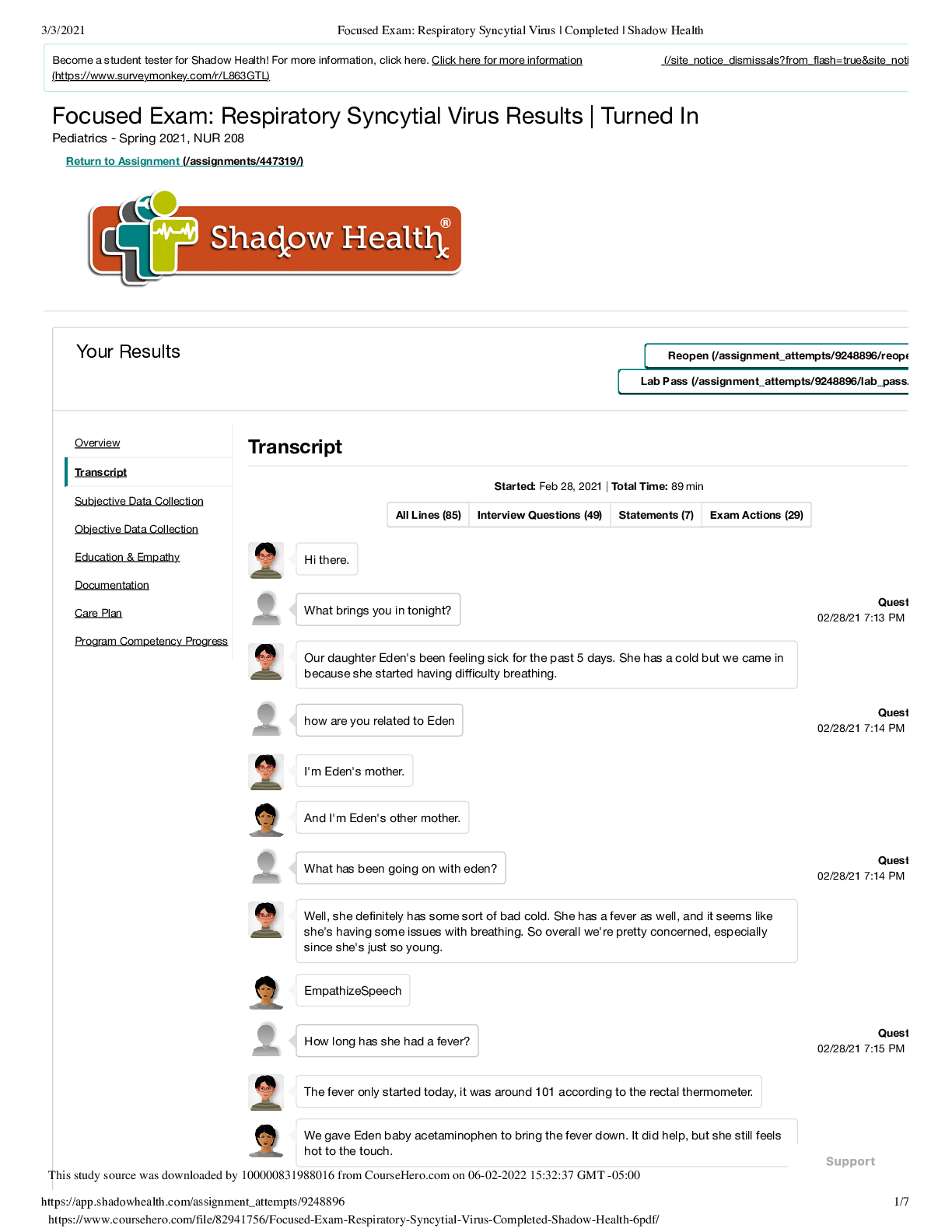
Week 4: Comprehensive Assessment Results | Turned In Health Assessment - GCU - December 2020, nrs-434vn Return to Assignment (/assignments/443803/) Your Results Reopen (/assignment_attempts/8731193... /reopen Lab Pass (/assignment_attempts/8731193/lab_pass.p Overview Transcript Subjective Data Collection Documentation / Electronic Health Record Documentation Objective Data Collection Documentation Student Survey Vitals Student Documentation Model Documentation Vitals BP 128/82 Pulse Ox 99% HR 78 BPM RR 15 Temp 37.2 C • Height: 170 cm • Weight: 84 kg • BMI: 29.0 • Blood Glucose: 100 • RR: 15 • HR: 78 • BP:128 / 82 • Pulse Ox: 99% • Temperature: 99.0 F Health History Student Documentation Model Documentation Identifying Data & Reliability The patient does not give reliable report of health history as her mediation, symptoms and hospitalization report was different each time I asked. She seemed to hesitate and have confusion with dates. She has no primary health care provider. She leaves out information about meds and diagnosis that are only uncovered by rephrasing question. Ms. Jones is a pleasant, 28-year-old African American single wo who presents for a pre-employment physical. She is the primary source of the history. Ms. Jones offers information freely and wit contradiction. Speech is clear and coherent. She maintains eye contact throughout the interview. General Survey The patient is healthy and able to work. She reports being happy with past history of some stress and insomnia which have resolved. . Rx Yaz improved symptoms; last period 6 wks ago. Takes Yaz 1x daily. Allergies to penicillin (hives), cats, dust (sneeze) and asthma acts up - asthma dx at 2 years old. Reports loss of breath going up stairs. Rx albuterol 2-3 daily. Last took yesterday when she wheezed going up stairs. Reports fatigue/ feeling full after eating sugar, glucose 90. Rx metformin causes gas, 2x daily (850 mg). Overall healthy hospitalizations asthma. Ms. Jones is alert and oriented, seated upright on the examinatio table, and is in no apparent distress. She is well-nourished, welldeveloped, and dressed appropriately with good hygiene. This study source was downloaded by 100000773243632 from CourseHero.com on 09-23-2021 04:15:37 GMT -05:00 Support 1/9/2021 Week 4: Comprehensive Assessment | Completed | Shadow Health Student Documentation Model Documentation 2/6 Reason for Visit Recent Physical needed for health insurance at new job "I came in because I'm required to have a recent physical exam the health insurance at my new job." History of Present Illness No current illness, just asthma and diabetes. Also dx of PCOS unreported in chart. Ms. Jones reports that she recently obtained employment at Smi Stevens, Stewart, Silver & Company. She needs to obtain a preemployment physical prior to initiating employment. Today she d any acute concerns. Her last healthcare visit was 4 months ago, when she received her annual gynecological exam at Shadow H General Clinic. Ms. Jones states that the gynecologist diagnosed with polycystic ovarian syndrome and prescribed oral contracept at that visit, which she is tolerating well. She has type 2 diabetes which she is controlling with diet, exercise, and metformin, which just started 5 months ago. She has no medication side effects at time. She states that she feels healthy, is taking better care of he than in the past, and is looking forward to beginning the new job. Medications Albuterol inhaler for wheezing - can take up to 3x daily but last use was yesterday when she rain upstairs. Yaz for birth control and to control PCOS. metformin 2x daily (850 mg) for type 2 diabetes. She takes Advil for cramps, the OTC dose but has not taken it since her last period over 6 weeks ago. She has taken tetracycline for acne but didnt remember the dose. No supplements. • Metformin, 850 mg PO BID (last use: this morning) • Drospirenone and ethinyl estradiol PO QD (last use: this morni • Albuterol 90 mcg/spray MDI 1-3 puffs Q4H prn (last use: yester • Acetaminophen 500-1000 mg PO prn (headaches) • Ibuprofen 600 mg PO TID prn (menstrual cramps: last taken 6 weeks ago) Allergies PCN, hives, has been avoiding med since she reacted. Did not remember date. She was little. Doctor told her not to take it again. Environmental allergies to dust and cats. No others reported. Dx asthma exacerbated by allergies and wheezing. • Penicillin: rash • Denies food and latex allergies • Allergic to cats and dust. When she is exposed to allergens she states that she has runny nose, itchy and swollen eyes, and increased asthma symptoms. Medical History She had a rt ankle injury 6 mo ago falling down stairs; hospitalized for inury but took no pain medication. Dx PCOS 4 months prior and reports cramps during period. hospitalized as a kid 5x for asthma and stayed overnight. Did not remember dates. Uses an inhaler about every day. She has some pain in back but could not identify when it started. Her diabtes was diagnosed at age 24 and she has a history of insomnia and acne (took tetracycline) but is no longer taking it. Took no med for sleep. Problems sort of went away. Asthma diagnosed at age 2 1/2. She uses her albuterol inhaler w she experiences exacerbations, such as around dust or cats. He asthma exacerbation was yesterday, which she resolved with he inhaler. She was last hospitalized for asthma in high school. Nev intubated. Type 2 diabetes, diagnosed at age 24. She began metformin 5 months ago and initially had some gastrointestinal s effects which have since dissipated. She monitors her blood sug once daily in the morning with average readings being around 90 She has a history of hypertension which normalized when she initiated diet and exercise. No surgeries. OB/GYN: Menarche, ag First sexual encounter at age 18, sex with men, identifies as heterosexual. Never pregnant. Last menstrual period 2 weeks ag Diagnosed with PCOS four months ago. For the past four month (after initiating Yaz) cycles regular (every 4 weeks) with moderat bleeding lasting 5 days. Has new male relationship, sexual conta not initiated. She plans to use condoms with sexual activity. Test negative for HIV/AIDS and STIs four months ago. [Show More]
Last updated: 1 year ago
Preview 1 out of 6 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 30, 2022
Number of pages
6
Written in
Additional information
This document has been written for:
Uploaded
Mar 30, 2022
Downloads
0
Views
225

.png)
.png)