*NURSING > SHADOW HEALTH > NUR550 Focused Note -Chest Pain – Brian Foster (All)
NUR550 Focused Note -Chest Pain – Brian Foster
Document Content and Description Below
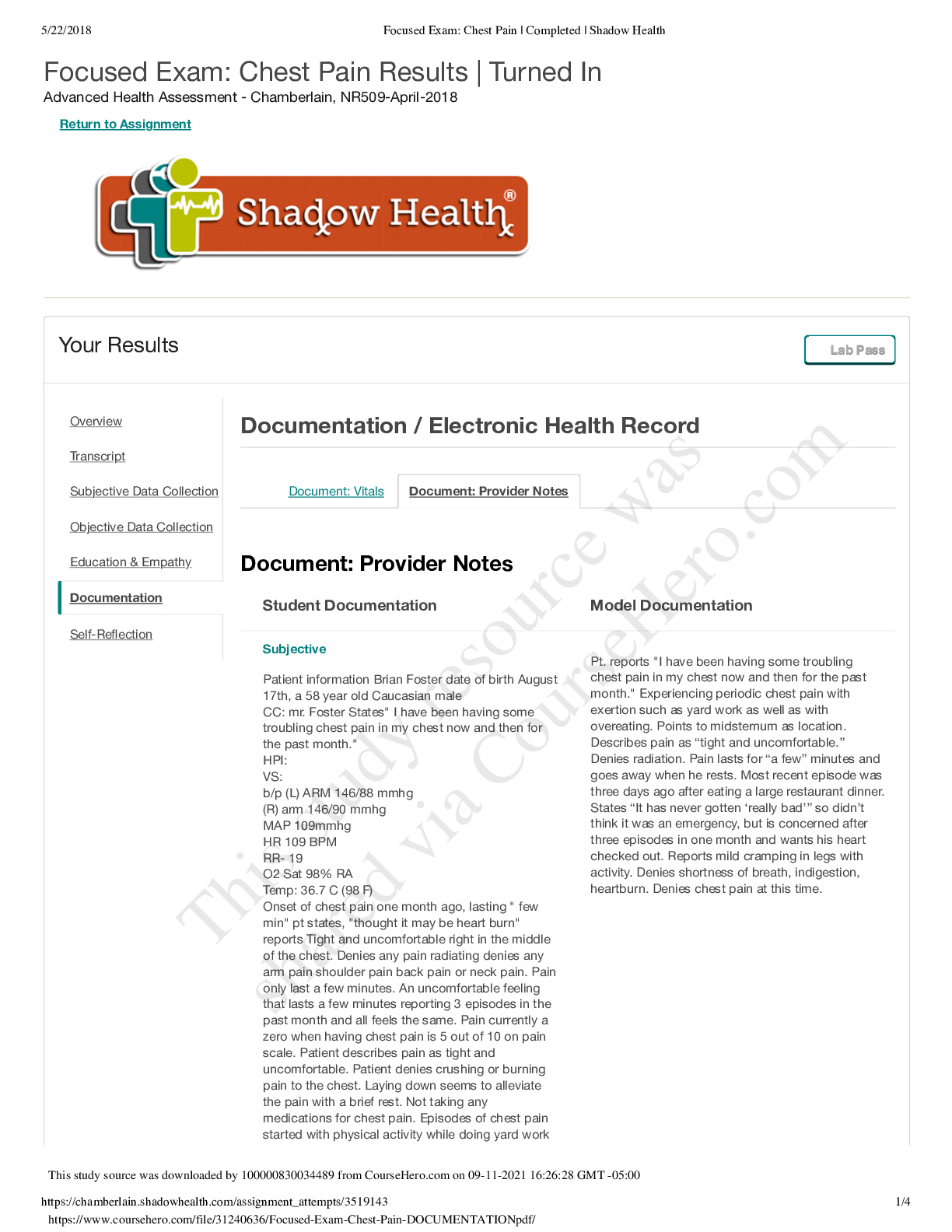
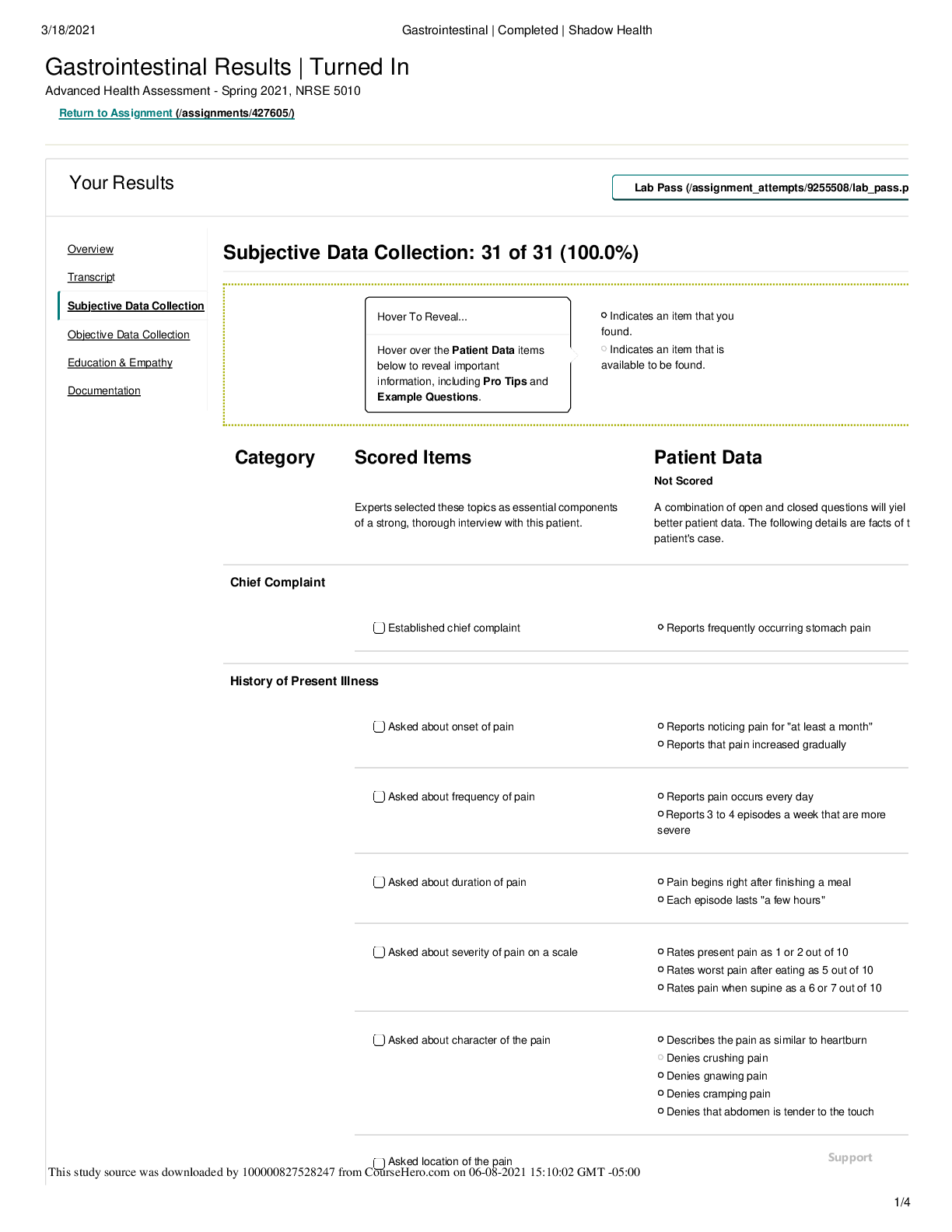
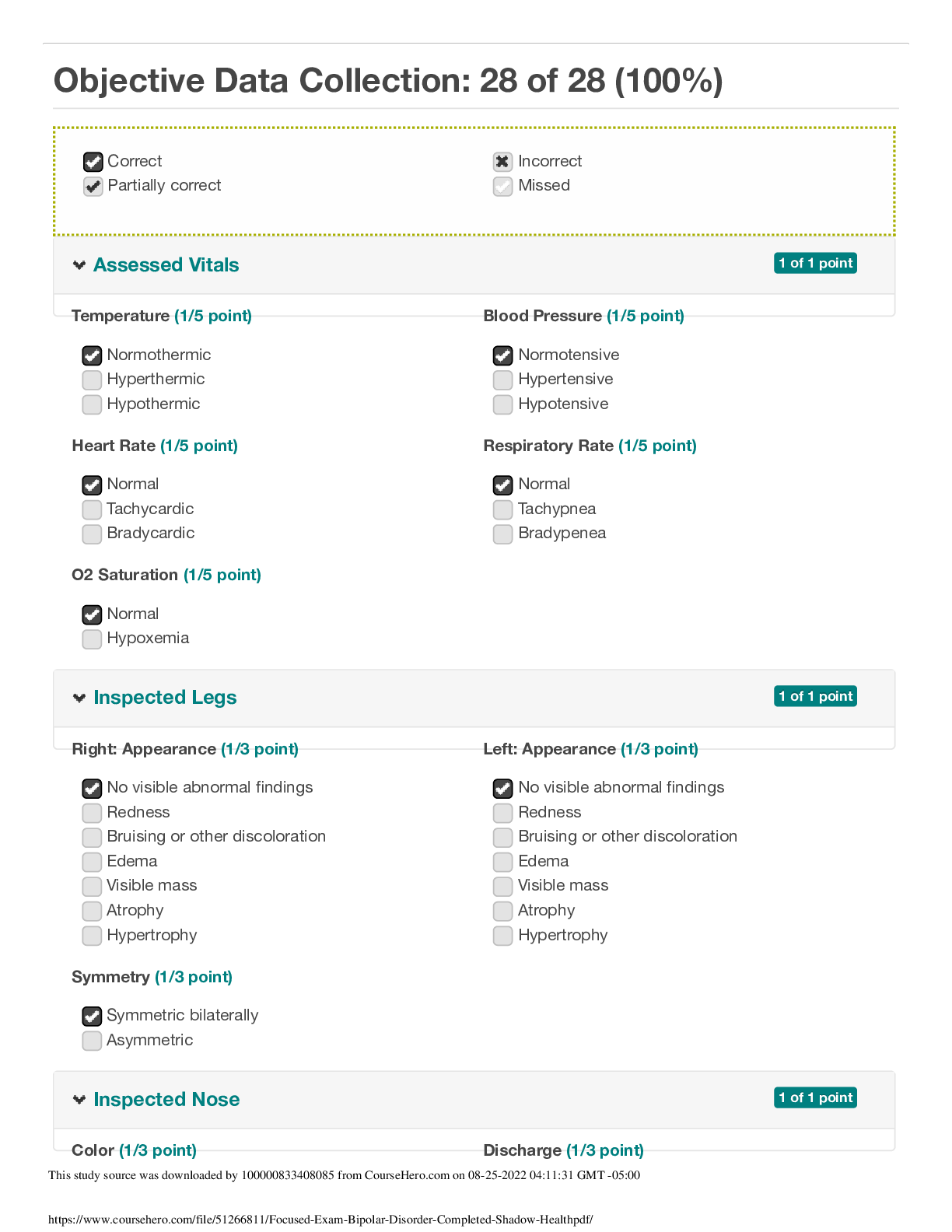
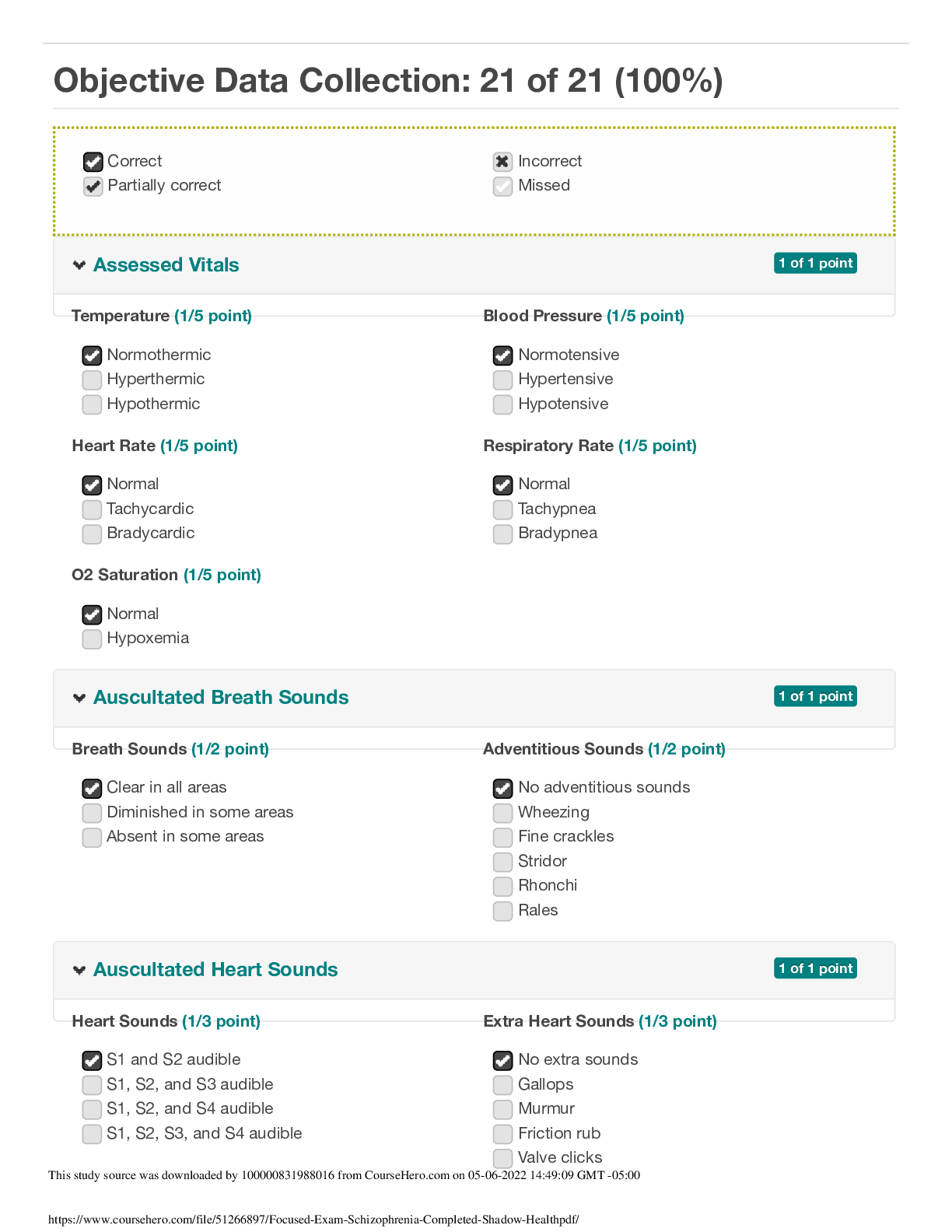
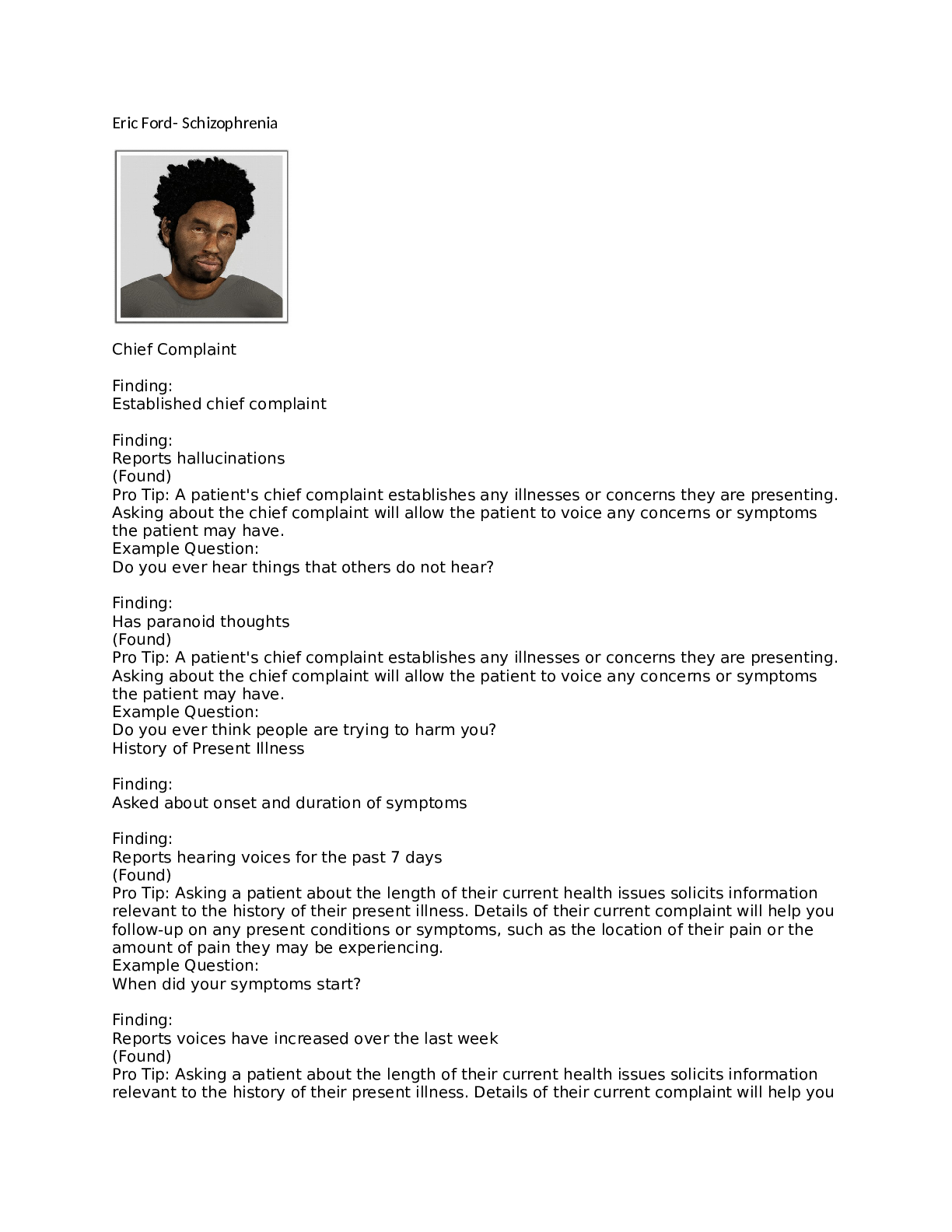
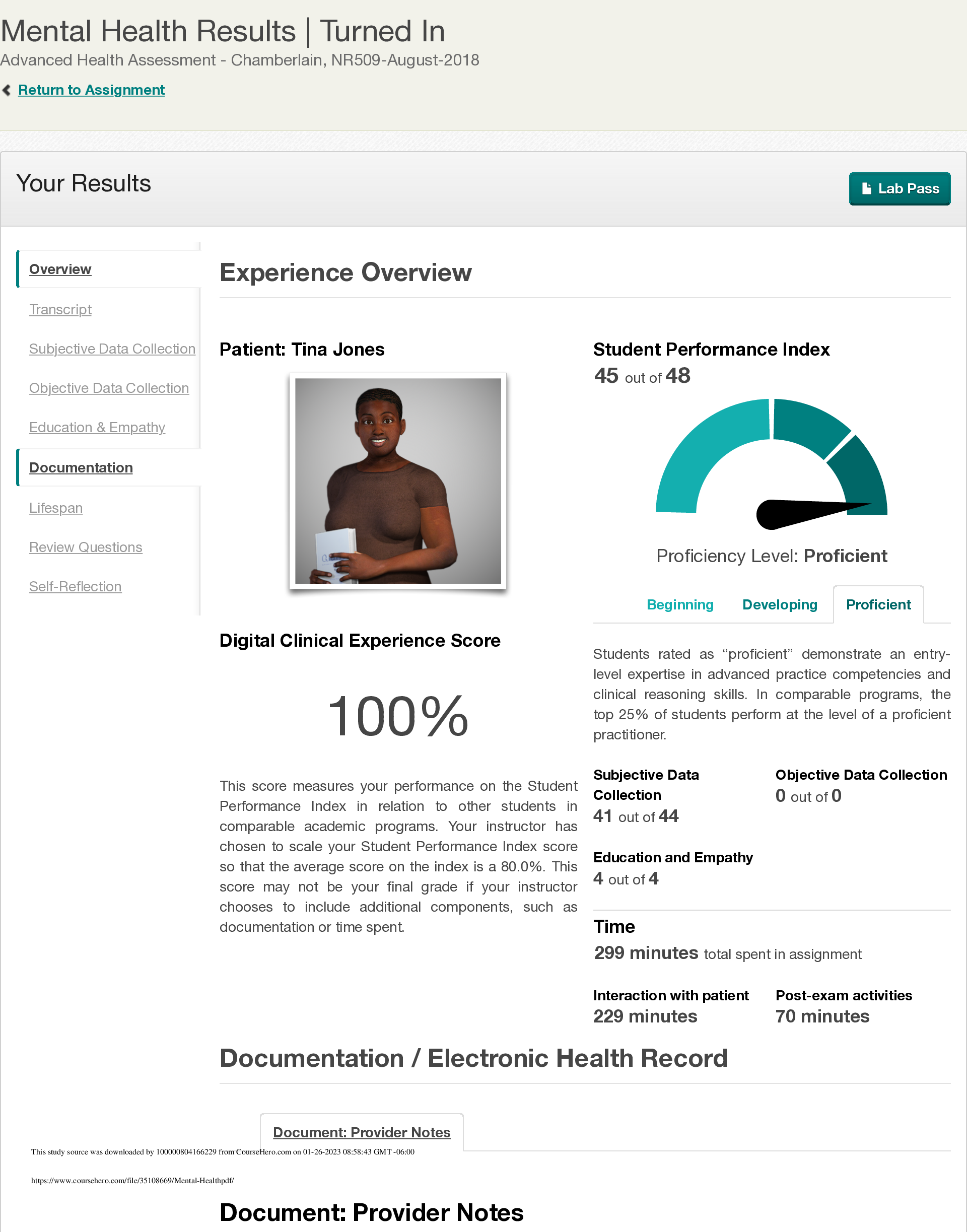
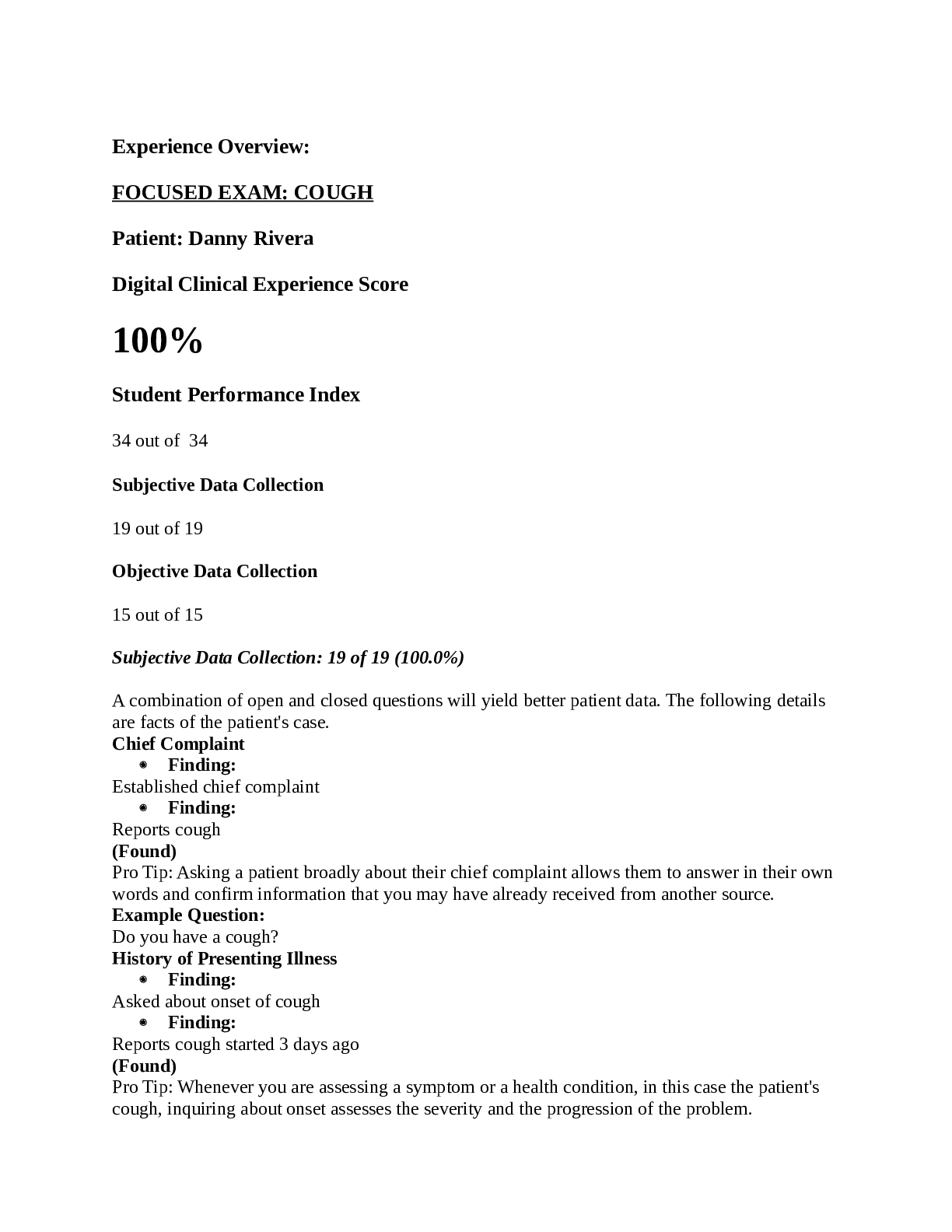
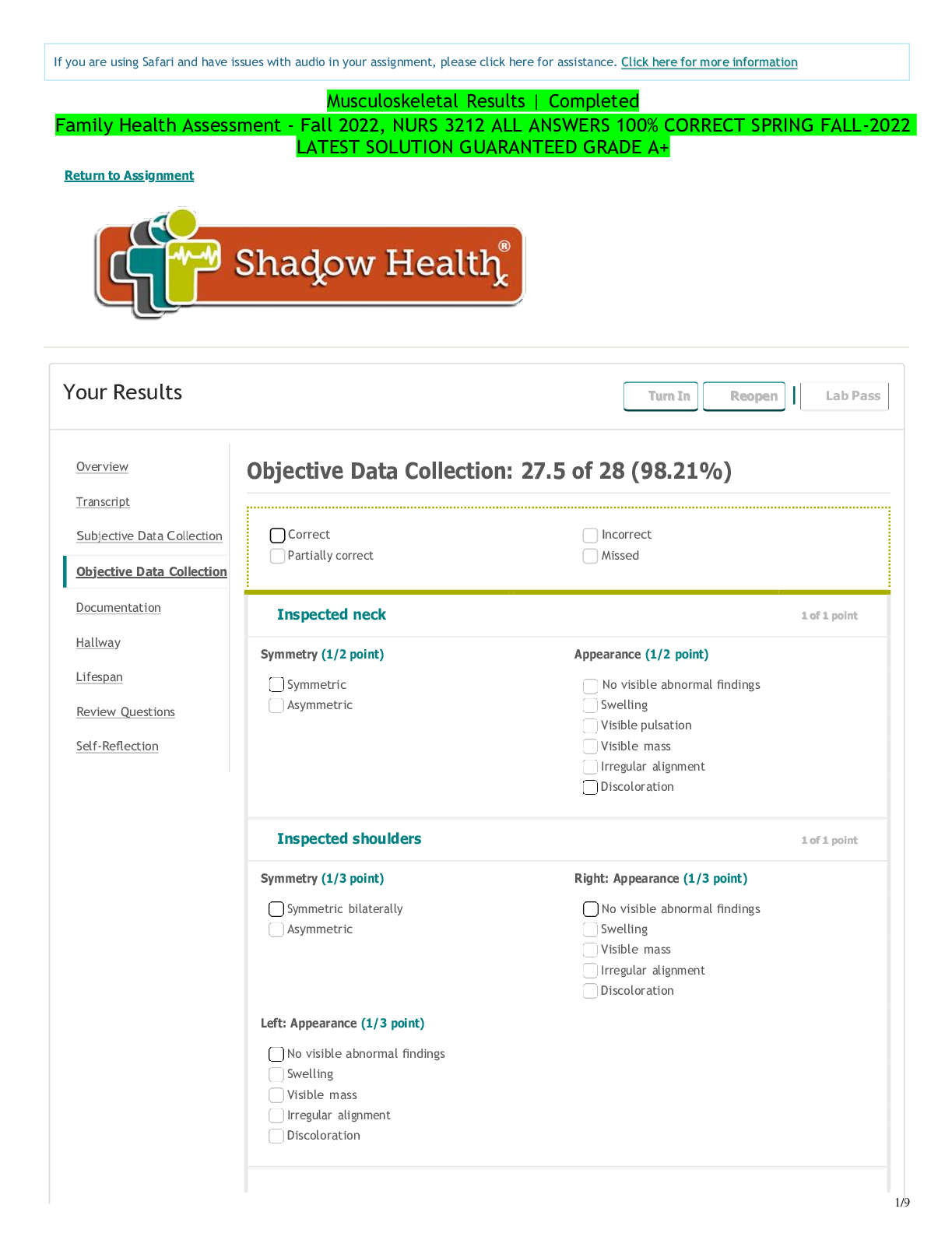
NUR550 Focused Note -Chest Pain – Brian Foster After you complete the focused assessment (virtual simulation), please write a paper using the following as headings/subheadings in APA format. Int... roduction (with purpose statement – one paragraph) Focus of the Assessment (in one paragraph describe how and what aspects of the health assessment you will focus on based on the chief complaint ) Focused Health History (This is a summary of the subjective section of the assessment – what did you find? What questions did you ask? What additional questions would you have asked?) Physical examination (This is a summary of the objective section of the assessment – what were your health assessment findings? What instruments/tools did you use to assess the patient?) Documented Evidence (This is a summary of your ‘differential diagnoses’ – what may be causing the symptoms on this patient? Use EBP and research to support your differential diagnoses) Plan of Care (This is a summary of potential recommendations which may include follow-up visits, patient/family teaching, labs, diagnostic testing, etc.) Conclusion (one brief paragraph summarizing your experience working with this patient) References (Please use EBP and research studies to support the documented evidence and plan of care sections) Focused Note Subjective: Patient Name or initials: Brian Foster Informant: The informant is the patient who is a reliable historian. Chief Complaint (CC): Chest pain History of present illness (HPI): Mr. Foster notes intermittent pain for a month, felt like heartburn, and lasted only a couple of minutes. He notes when the pain occurs it is mostly midsternum. The sensation is tightness of the chest. Mr. Foster notes the pain presents during physical activity. He states, “The first time it happened He notes lying still, or rest helps to alleviate the pain. Allergies: Codeine. Codeine causes nausea and vomiting. Medications: Metoprolol 100mg PO daily which he takes for his high blood pressure. Atorvastatin 20mg PO daily at bedtime, last dose 10pm at bedtime yesterday, and Omega-3 fish oil 1200 mg PO BID, last dose 8am, which he is on for his high cholesterol. Past History: Mr. Foster denies any surgical history. Past medical history include stage II high blood pressure diagnosed one year ago, and high cholesterol also diagnosed one year ago. Family History: Mr. Foster’s father passed away at the age of 75 from colon cancer. His PMH included hypertension, hyperlipidemia, colon CA, and obesity. Mr. Foster’s mother is still living. She is 80 years of age, and her PMH include type-2 diabetes, and hypertension. Mr. Foster’s brother passed away at the age of 24 from a motor vehicle accident. His sister is still living, and is 52 years of age. Her PMH include type-2 diabetes, and hypertension. Mr. Fosters’ son is living, is 26 years old, and relatively healthy. His daughter is 19 years of age, still living, and has asthma. Personal and Social History: Mr. Foster does not have a past or present history of tobacco use, however he does acknowledge drinking 2-3 alcoholic beverages a week. Mr. Foster also denies a history of illicit drug use. Health Promotion/Maintenance Activities: Mr. Foster was told to cut out red meat from his diet. He was also instructed to continue to take his medications as prescribed, and was told to weigh himself at the same time wearing the same clothing daily. Mr. Foster was also instructed to do some light exercises at least 3 to 4 days per week. He was told to eat fresh fruits and vegetables. Mr. Foster was instructed to follow up with his PCP and cardiologist. Tobacco Use: Mr. Foster does not currently smoke and does not require health promotion teaching regarding tobacco use. Alcohol and Drug use: Mr. Foster has no history of recreational drug use, however he was urged to reduce his alcohol intake to 1-2 drinks per week. Pertinent Review of systems (ROS): General: Mr. Foster notes gaining 15 to 20lbs over the last couple of years. The weight gain does not appear to be out of the ordinary. No complaint of fatigue noted. No muscle weakness or weight loss. Neck: No neck pain, nor limited range of motion noted. Respiratory: No shortness of breath, cough, or wheezing noted. CV: Mr. Foster does note chest pain on exertion, however, denies syncope, tachycardia, palpitations, or orthopnea. Peripheral Vascular: No intermittent claudication, thrombophlebitis, swelling, or leg cramps noted by Mr. Foster. Psych/behavior: Patient notes no change in mood, and low stress levels. Mr. Foster is developmentally appropriate. Include three additional questions you would ask the patient or informant and state how that information would assist you in formulating a diagnosis. 1. Have you experienced this type of chest pain before? · This would allow me to determine whether or not the pain is new or has occurred before. · This would also discern the level of frequency, i.e., how often the pain comes on; has the pain stopped for weeks to months, and eventually returned. 2. When was the last time you had your lipid levels checked? · Lipid and triglyceride levels would provide diagnostic information regarding possible vessel occlusion. · It would also help steer the patient plan of care, and medication treatment/possible surgical intervention. 3. Have you had a recent echocardiogram done? · A recent echocardiogram would provide diagnostic information, and allow visualization of pertinent structures of the heart. · It would also provide confirmation of possible vessel occlusion. Objective: Document all findings, avoid the word negative or normal. It is important that you learn to deduce that the patient has no remarkable findings. Vital Signs: Current blood pressure is 146/90, O2 saturation is 98% on room air, and heart rate is 109, respiratory rate is 19, and temperature is 36.7 orally. Height/Weight/BMI: Mr. Foster weighs 197lbs. He is 5’11, and current BMI is 27.5. Physical Exam Constitutional/General survey: Mr. Foster is generally well appearing, has no cognitive deficit, is a good historian, and is in a pleasant mood. Skin is warm and dry, and no tenting is found on examination. Neck: No neck pain or limited range of motion found. No jugular vein distention found. JVD is 3cm above the sternal angle. A bruit is auscultated in the right carotid artery, with a positive thrill, and amplitude of 3+. No bruit found in the left carotid artery, with no thrill and amplitude of 2+. Thorax: Point of maximal impulse found to be displaced laterally; with brisk tapping, and a diameter of less than 3cm. Respiratory: Lung sounds are clear in bilateral anterior lung fields. Lung sounds are clear in posterior upper lung fields, with fine crackles in bilateral posterior lower lung fields. Abdomen: No bruits noted of the abdominal aorta. No tenderness or masses noted on palpation. The liver is palpable, however the spleen is not. Right and left kidneys are not palpable. CV: ECG performed found Mr. Foster to be in normal sinus rhythm with no ST changes. Chest pain is noted only with physical activity. Peripheral vascular: 1+ Tibial and DP pulses found bilaterally. 1+ popliteal pulses noted bilaterally with no thrill. 2+ femoral and radial pulses noted bilaterally, and 2+ brachial pulses found bilaterally. Varicosities noted in bilateral lower extremities with cyanosis and minimal swelling. Identify what information is missing from the physical exam or state what additional exam elements you would have included. Assessment: Mr. Foster has chest pain, potentially related to vessel occlusion and coronary artery disease (Bickley, Szilagyi, and In Hoffman, 2017). Mr. Foster’s chest pain may also be related to his obesity, and lack of exercise. He also eats an excessive amount of red meat, and imbibes in an excessive amount of alcohol given his health history. The type of pain described is what is referred to as typical chest pain. That is, “Chest pain that usually occurs with or is made worse by physical exertion or stress” (Hildreth, Burke, and Glass, 2009, p. 1498). Differential diagnosis: Stable angina pectoris. Mr. Foster has a relatively poor diet, does not exercise, and has not had a recent 2D echo, or stress test to confirm cardiovascular function. He notes some weight gain over the past couple of years, and that the pain is affecting his level of physical activity. Plan: This will depend on your findings and the assessment. The expectation is to include: Diagnosis: Exertional chest pain relieved by rest Diagnostics: Echocardiogram, and stress test. Pharmacology: Continue current course of medications, which include Lopressor for blood pressure management, Lipitor for high cholesterol, and omega-3 fish oil in managing heart disease. Start patient on new course of nitroglycerin for chest pain episodes. Education/Counseling: Proper and routine monitoring of lipid levels, cardiac markers, and weight. Changes in diet, and exercise, and routine doctors for required adjustments to medications. Health Promotion/Anticipatory Guidance: Mr. Foster will start to engage in light exercise three to four days per week. He will also cut back on his red meat intake, and will eat healthier foods. Referrals: Mr. Foster is being referred to a cardiologist for further testing, and possible admission to a hospital cardiac unit for continuous ECG monitoring and routine lab work up. Mr. Foster will likely, also require a cardiac heart catheterization. According to Rivera, Nadel, and Brown (2005), cardiac catheterization will allow diagnostic visualization of vessels and degree of stenotic occlusion (p. 71). Follow-up: He is to follow up with a cardiologist in two days time, and will schedule a follow up with our office within three days. Self-Assessment: Given Mr. Fosters symptoms, I believe an adequate health history and physical examination was performed. The assessment was focused on cardiovascular presentation, as well as an abdominal examination to rule out GI involvement. His plan of care reflects current complaint, as well as thorough subjective and objective findings. [Show More]
Last updated: 1 year ago
Preview 1 out of 4 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 29, 2020
Number of pages
4
Written in
Additional information
This document has been written for:
Uploaded
Oct 29, 2020
Downloads
0
Views
195





 Transcript.png)