Emergeny Medicine > QUESTIONS & ANSWERS > Emergency Medicine SAEM Quizzes, Comprehensive Exam test bank (answered correctly/deeply elaborated) (All)
Emergency Medicine SAEM Quizzes, Comprehensive Exam test bank (answered correctly/deeply elaborated) .
Document Content and Description Below
SAEM Quizzes + SEAM comprehensive exam Test Bank_ Answered /Rationales. (first 30 pages free) Regarding the diagnosis of acute appendicitis, all the following are true EXCEPT: A. Vital signs are u... sually abnormal, even early in the course of acute appendicitis. B. Rebound is usually elicited only after the appendix has ruptured or infarcted. C. Rovsing's sign is pain in the right lower quadrant upon palpation of the left lower quadrant. D. The obturator sign is pain upon flexion and internal rotation of the hip. E. The psoas sign is pain upon extension of the hip. - A. Vital signs are usually abnormal, even early in the course of acute appendicitis. The answer is A. The presentation of acute appendicitis varies tremendously. Early in its course, vital signs including temperature may be normal. Once perforation has occurred, the rate of low-grade fever (<38 C) increases to about 40%. Other variations in presentation include pain in the right upper quadrant, typically from a retrocecal or retroiliac appendix. Rosving's sign is described as: A. Tenderness in the right upper quadrant that is worse with inspiration. B. Pelvic pain upon flexion of the thigh while the patient is supine. C. Pelvic pain upon internal and external rotation of the thigh with the knee flexed. D. Pain that increases with the release of pressure of palpation. E. Pain in the right lower quadrant when left lower quadrant is palpated. - E. Pain in the right lower quadrant when left lower quadrant is palpated. The answer is E. Rosving's sign is pain in the right lower quadrant when the left lower quadrant is palpated. Rebound tenderness occurs with the release of pressure. The iliopsoas sign is pain associated with thigh flexion. The obturator sign is pain that occurs with thigh rotation. All of these signs are associated with appendicitis. Murphy's sign is cessation of inspiration during palpation of the right upper quadrant and is associated with acute cholecystitis. In establishing a differential diagnosis of abdominal pain, which of the following is true? A. Radiation of pain to the scapula is suggestive of acute hepatitis. B. Cervical motion tenderness is a useful physical finding for differentiating women with or without acute appendicitis. C. In patients with sickle cell anemia who present with abdominal pain and diarrhea, shigellosis should be a top consideration. D. The onset of pain prior to the occurrence of nausea and vomiting is more often suggestive of a surgical etiology. E. Diverticulitis tends to cause pain in the right upper quadrant. - D. The onset of pain prior to the occurrence of nausea and vomiting is more often suggestive of a surgical etiology. The answer is D. Pain prior to nausea and vomiting is often suggestive of a surgical etiology of the pain, such as small bowel obstruction. Cervical motion tenderness has been noted in up to 25% of women with acute appendicitis. Patients with sickle cell anemia are prone to Salmonella infections. Radiation of pain to the scapula is classically present in acute choleycystitis. Diverticulitis pain is generally located in the left lower quadrant. Of the following pain patterns, which is the least likely associated with diagnosis of peptic ulcer disease? A. non-radiating, burning epigastric pain B. pain that awakens a patient in the middle of the night C. unrelenting pain over a period of weeks D. relief of abdominal pain with antacids E. pain that is worse preceding a meal - C. unrelenting pain over a period of weeks The answer is C. Pain from peptic ulcer disease typically occurs in periods of exacerbation and remission. Unrelenting pain over weeks or months should suggest an alternative diagnosis. Pain is classically described as non-radiating, burning epigastric pain. Some patients may also complain of chest or back pain. Pain is frequently severe enough to awaken patients from sleep in early morning hours but is often not present upon waking in the morning, as gastric acid secretion peaks around 2 a.m. and nadirs upon awakening. A mother brings her 6 week old boy to the emergency room. She states the baby has been vomiting everything she's tried to feed him for the past 12 hours. She states that he usually eats readily and completes an entire feeding, but he is unable to keep anything down. The emesis is non-bloody and non-bilious, however it is projectile in nature. What is the most likely condition in this patient? A. viral gastroenteritis B. constipation C. appendicitis D. intussusception E. pyloric stenosis - E. pyloric stenosis The answer is E. Hypertrophic pyloric stenosis typically presents in the second to sixth week of life and is four times more common in males than females. Infants with hypertrophic pyloric stenosis typically are vigorous eaters but shortly afterward regurgitate the entire feeding contents in a projectile fashion. The emesis is non-bilious. The classic finding on exam is an "olive" palpable in the abdomen, and diagnosis is typically via ultrasound. Intussusception typically presents between the ages of 5 and 12 months. Gastroenteritis is characterized by diarrhea as well as vomiting. Neither constipation nor appendicitis typically present with protracted vomiting, though the latter condition tends to present atypically in young children (and elderly adults). A 46 year old woman presents to the emergency department complaining of abrupt onset of intermittent severe pain in the left flank and abdomen that woke her from sleep. She is pacing around the stretcher and appears extremely uncomfortable. She has never experienced this type of pain previously and denies fevers or other symptoms. Renal calculus is suspected. Which of the following is true regarding the diagnosis of renal calculi in this patient? A. Urinalysis demonstrating hematuria confirms the diagnosis. B. KUB detects less than 10% of calculi. C. Helical CT scan greater than 95% sensitive and specific for renal calculi. D. Ultrasound is the study of choice for detecting small ureteral calculi. E. Intravenous pyelogram (IVP) may be used in patients with renal insufficiency. - C. Helical CT scan greater than 95% sensitive and specific for renal calculi. The answer is C. Helical CT scan has been shown to be both highly sensitive and specific in the diagnosis of renal calculi. It is the preferred modality for evaluation in many centers. Although urinalysis typically demonstrates hematuria in patients with renal calculi, hematuria is not specific enough to confirm the diagnosis, and imaging is warranted in all first-time presenters. KUB detects approximately 60-70% of calculi (though studies addressing this issue are somewhat methodologically flawed). Ultrasound is not reliable for detecting small calculi, but is 85-94% sensitive and 100% specific at demonstrating hydronephrosis. IVP is contraindicated in patients with renal insufficiency due to the dye load necessary to perform the study. A 50 year old man presents with 1 day of gradually worsening, intermittent, left lower quadrant pain associated with loose stools. He has had no fevers or bloody bowel movements. Similar symptoms in the past were self-limited. All vital signs lie within normal limits. Physical examination shows mild tenderness in the left lower quadrant, normal active bowel sounds and neither masses nor peritoneal signs. His primary-care physician can see him tomorrow in his clinic. What should be done next in the E.D.? A. Discharge home after a single dose of IV antibiotics B. Discharge home on high-fiber diet, laxatives and stool softeners C. Gastroenterology consult for endoscopy D. Admit for observation and serial examinations - B. Discharge home on high-fiber diet, laxatives and stool softeners The answer is B. This patient has classic diverticulosis (saclike protrusions of colonic mucosa through the muscularis) without signs of acute diverticulitis (inflammation of diverticula). Usually these patients can be managed as outpatients with a high-fiber diet and treatments to decrease intestinal spasm. If the patient develops fever or pain increases he may need further evaluation to rule out abscess formation. Diverticulitis is treated with antibiotics, bowel rest and analgesics. You are treating a 25 year old male with the recent diagnosis of Crohn's disease in the ED. Regarding Crohn's disease, you know that: A. Lesions are typically contiguous B. Small bowel involvement is rare C. Bleeding is common due to superficial bowel wall inflammation D. There is a small increased risk of colon cancer - D. There is a small increased risk of colon cancer The answer is D. Although Crohn's disease may involve the entire bowel tract, the rectum is rarely involved. Involved areas are typically non-contiguous (known as "skip lesions") and the inflammation involves all of the layers of the bowel wall--resulting in many of the complications of Crohn's such as abscess and fistula formation, intestinal obstruction, and perforation. The risk of colon cancer is only slightly elevated above baseline. In contrast, Ulcerative colitis begins in the rectum and may spread to the upper parts of the colon but never involves the small intestine. The ulcerations are contiguous and involve only the colonic mucosa. The incidence of colon cancer may be increased up to 30 times over baseline. A 53 year old obese woman presents to the emergency department, accompanied by three of her children, complaining of severe abdominal pain that began this afternoon after lunch. Physical exam reveals marked RUQ tenderness. Likely findings on this patient would include all of the following EXCEPT: A. positive sonographic Murphy's sign B. pain in the right scapula C. leukocytosis with left shift D. marked inguinal lymphadenopathy E. aminotransferases and bilirubin within normal limits - D. marked inguinal lymphadenopathy The answer is D. This woman is likely suffering from acute cholecystitis. Predisposing factors include female gender, obesity, increased age and increased parity. Inflammation of the gallbladder causes RUQ pain and sonographic Murphy's sign (inspiratory arrest, due to pain, while the ultrasound probe is positioned over the gallbladder). Pain may radiate to the right scapula. Lab studies usually show leukocytosis with or without a left shift, and aminotransferases and bilirubin are usually within normal limits. A 45 year old woman presents with right upper quadrant pain and fever. The pain is worse after eating. On physical exam she has a Murphy's sign. The most likely diagnosis is: A. Appendicitis B. Diverticulitis C. Cholelithiasis D. Cholecystitis E. Mesenteric Ischemia - D. Cholecystitis The answer is D. Right upper quadrant pain, fever and a Murphy's sign suggests cholecystitis. Cholelithiasis presents with similar pain, but is not associated with fever or a Murphy's sign All of the following factors predispose to cecal volvulus EXCEPT: A. pregnancy B. age 25-35 C. prior abdominal surgery D. marathon running E. severe chronic constipation -E. severe chronic constipation The answer is E. Cecal volvulus occurs as a result of abnormal fixation of the right colon and increased mobility of the cecum. Depending on the degree of rotation around the mesenteric axis, cecal volvulus can lead to twisting of the mesentery and its blood vessels. Cecal volvulus occurs most commonly in people 25-35 years old and should be suspected in cases of bowel obstruction without known risk factors. Prior abdominal surgery and pregnancy predispose to obstruction or cecal volvulus; however, chronic constipation is not known to predispose to cecal volvulus. Interestingly, marathon runners have been found to have a higher incidence of cecal volvulus, perhaps from having a thin, flexible mesentery that more easily permits rotation of the cecum around the mesenteric pedicle. Which of the following pairings of referred pain and causal disease is least likely to be encountered? A. sacral pain—ovarian torsion B. inguinal pain—ureteral colic C. epigastric pain—myocardial infarction D. shoulder pain—ruptured spleen E. thoracic back pain—pancreatitis - A. sacral pain—ovarian torsion Ovarian torsion may cause lower abdominal pain, pelvic pain, adnexal tenderness, and cervical motion tenderness, but it is not known to cause sacral pain. A 72 year old man with a history of diverticulosis presents with vague abdominal pain for the past day. His physical exam is notable for normal vital signs, left lower quadrant abdominal tenderness without rebound or guarding, and guaiac positive brown stool. Work-up including KUB and abdominal/pelvic CT scan reveals diverticulitis without perforation. Of the following choices, which is the most appropriate management of this patient? A. type and cross two units of packed red blood cells B. immediate surgical intervention C. discharge on oral pain medications D. barium enema to evaluate for carcinoma of the colon E. admission for intravenous antibiotics and fluids - E. admission for intravenous antibiotics and fluids The answer is E. For mild episodes of diverticulitis in which there is no evidence of perforation or peritonitis, there is no indication for immediate surgical intervention. Conservative management with intravenous fluids and antibiotics as well as bowel rest is typically first attempted. Although colon carcinoma may be a precipitating factor in the development of diverticulitis, barium enema should be avoided in the acute period due to high risk of bowel perforation. Although some patients with mild cases of diverticulitis may be discharged home with conservative treatment, the elderly are at higher risk of perforation and should be admitted. *Guaiac positive stool* in seen in up to *50%* of patients with diverticulitis. There is no reason to suspect acute blood loss requiring transfusion in diverticulitis. Regarding esophageal perforation, which of the following is INCORRECT: A. Esophageal perforation has been reported as a complication of nasogastric tube placement, endotracheal intubation, and esophagotracheal Combitube intubation. B. Esophageal perforation may result from forceful vomiting, coughing, childbirth or heavy lifting. C. Over 80% of esophageal perforations are iatrogenic, usually as complications of upper endoscopy, dilation, or sclerotherapy. D. Over 90% of spontaneous esophageal perforations occur in the proximal esophagus. E. Iatrogenic perforations of the esophagus usually occur in the proximal esophagus or esophagogastric junction. - D. Over 90% of spontaneous esophageal perforations occur in the proximal esophagus. Over 90% of spontaneous esophageal perforations occur in the *distal* esophagus, whereas iatrogenic perforations are frequently at the pharyngoesophageal junction or the esophagogastric junction. Foreign body or caustic substance ingestion, severe blunt injury or penetrating trauma, and carcinoma are other causes of esophageal perforation. Working in the ED, you have identified a bony object wedged in the mid-esophagus of a 45 year old patient. Failure to promptly remove a foreign body impacted in the esophagus could result in: A. Esophageal perforation and mediastinitis B. Epiglottal edema and airway obstruction C. The rapid development of xerostomia D. Barrett's esophagitis - A. Esophageal perforation and mediastinitis The answer is A. The complications of esophageal foreign bodies are rare but serious. They include esophageal erosion and perforation, mediastinitis, esophagus-to-trachea or esophagus-to-vasculature fistula formation, stricture formation, diverticuli formation, and tracheal compression (from both the esophageal foreign body and resultant edema or infection). Air trapping is a sign of a foreign body of the airway. Rarely, airway foreign bodies act as one-way valves that could cause hyperinflation of a lung segment, with resultant bleb rupture and pneumothorax formation. A mother brings her 35 year old son to the emergency department because of tremor and mutism for the past three days. His mother found him in his room this morning lying stiffly in his bed, soiled with urine and feces. He appears confused and will not respond to questions. He was diagnosed with schizophrenia last year and has been on several medications. Last month after his most recent hospital admission for schizophrenia, he was discharged with a prescription for haloperidol. On physical exam, he is visibly diaphoretic and has vital signs as follows: T 102.7, BP 140/98, P 112, R 12. His neuromuscular exam shows extremely rigid extremities, and his laboratory values are notable for a white blood cell count of 15000/mm3 and abnormally elevated creatine phosphokinase levels. What is the most likely explanation for these findings? A. neuroleptic-induced acute dystonia B. neuroleptic malignant syndrome C. schizophrenia, catatonic type D. tardive dyskinesia - B. neuroleptic malignant syndrome The answer is B. Neuroleptic malignant syndrome (NMS) is an idiosyncratic, life-threatening reaction to antipsychotic medications, with haloperidol being the most common cause. It is characterized by elevated temperatures, "lead pipe" muscle rigidity, altered mental status, choreoathetosis, tremors, and autonomic dysfunction (e.g., diaphoresis, labile blood pressure, incontinence, dysrhythmias). While this patient's temperature is only 102.7, students should note that any patients with temperatures greater than 105 most likely have non-infectious etiologies for temperature elevation. NMS is thought to be due to too much D2 blockade in the substantia nigra and hypothalamus. Treatment consists of stopping the causative agent and providing supportive care. Medications such as *dantrolene, bromocriptine, amantadine, and lorazepam* are also often used. Tardive dyskinesia (choice A) is a chronic movement disorder that results from prolonged use of antipsychotics and can include involuntary and periodic movements of the tongue or lips, mouth puckering, or flailing movements either of the extremities or of the spine. Neuroleptic-induced acute dystonia (choice C) is an acute spasm of a muscle or muscle group associated with the use of antipsychotic agents. It presents with patients complaining of neck twisting (torticollis), fixed upper gaze, facial muscle spasms, or dysarthria from tongue protrusions. In a similar family with dystonia, neuroleptic-induced akathisia (choice D) is an extrapyramidal syndrome that is manifest by agitation and restlessness. Schizophrenia, catatonic type (choice B), a diagnosis of exclusion, usually does not present with this degree of impairment. A 25 year old man returns to the ED, 24 hours after being released from the hospital with a new diagnosis of schizophrenia. He has recently started to take haloperidal for his psychotic symptoms. In the ED he is noted to have involuntary contractions of the muscles of the face, a protruding tongue, deviation of the head to one side, and sustained upward deviation of the eyes. Vital signs are stable, and initial labs show no electrolyte or hematological abnormalities. Of the following choices, the preferred medication for this condition is: A. diphenhydramine B. lorazepam C. phenobarbital D. metoprolol - A. diphenhydramine The answer is A. Acute dystonia, the most common adverse effect seen with neuroleptic agents, occurs in up to 5% of patients. Dystonic reactions, which can occur at any point during long-term therapy and up to 48 hours after administration of neuroleptics in the emergency department, involve the sudden onset of involuntary contraction of the muscles in the face, neck, or back. The patient may have protrusion of the tongue (buccolingual crisis), deviation of the head to one side (acute torticollis), sustained upward deviation of the eyes (oculogyric crisis), extreme arching of the back (opisthotonos), or rarely laryngospasm. These symptoms tend to fluctuate, decreasing with voluntary activity and increasing under emotional stress, which occasionally misleads emergency physicians to believe they may be hysterical in nature. Dystonic reactions should be treated with *IM or IV benztropine (Cogentin®), 1 to 2 mg*, or *diphenhydramine (Benadryl®), 25 to 50 mg*. Intravenous administration usually results in near-immediate reversal of symptoms. Patients should receive oral therapy with the same medication for 48 to 72 hours to prevent recurrent symptoms. A 70 year old male with acute delirium requires administration of haloperidol for agitation. Which of the following is a recognized side effect of haloperidol? A. first degree heart block B. nephrogenic diabetes insipidus C. prolonged QT interval D. transient hepatitis - C. prolonged QT interval The answer is C. Nephrogenic diabetes insipidus may be associated with lithium. Potential side effects of haloperidol include acute dystonia, prolonged QT interval, Parkinsonism, and akathisia A 19 year old woman is brought to the emergency department by her friends because she has been saying that she is a superhero and trying to run into traffic to prove that she is indestructible. The friends report that she has been using drugs but they do not know which ones. Which of the following pairs of ocular finding and recreational drug is commonly observed? A. dilated pupils - heroin B. internuclear ophthalmoplegia - marijuana C. pinpoint pupils - amphetamines D. vertical nystagmus – phencyclidine - D. vertical nystagmus - phencyclidine The answer is D. Sympathomimetics (cocaine, amphetamines) cause dilated pupils. Opiates (heroin) cause pinpoint pupils. Internuclear ophthalmoplegia is associated with multiple sclerosis. CN VI palsy is not associated with any specific drugs. A 42 year old former custodial worker presents stating, "I think that people can hear what I am thinking." In the emergency department, he becomes extremely agitated and threatening, and his psychoses become more severe. In choosing an antipsychotic medication, which of the following would be the most appropriate choice? A. haloperidol B. chlorpromazine C. thioridazine D. ketamine - A. haloperidol The answer is A. Haloperidol is the most studied high potency antipsychotic agent used in agitated patients. Typical dosing is *5-10 mg IM every 10-30 minutes*. Unlike thioridazine, haloperidol *does not cause respiratory depression*, has *negligible anticholinergic side effects*, and rarely causes hypotension. Although benzodiazepines can be used in the agitated patient, respiratory depression can occur, and close monitoring is essential. A 20 year old college student is brought to the emergency department by campus police after he was found by his roommate saying people in the TV were trying to kill him. Which of the following criteria is not an indication for admission? A. first-time psychiatric episode B. demonstrates risk for suicide C. inadequate psychosocial support D. lacks capacity to cooperate with treatment - A. first-time psychiatric episode The answer is A. For an acute psychiatric episode, the first goal is medically stabilizing the patient. Subsequently, a patient who presents without previous history of a psychiatric episode does not necessarily need to be admitted. This, of course, depends on the identity and severity of the condition, and whether it can be treated in the emergency department. A 55 year-old male presents with new onset agitation and confusion. Which of the following medical histories would suggest a psychiatric (non-organic) cause? A. History of diabetes mellitus only B. History of alcohol abuse only C. History of hypothyroidism only D. History of chronic obstructive pulmonary disease only - C. History of hypothyroidism only The answer is C. Although hyperthyroidism may result in an agitated state, hypothyroidism is not generally associated with violent behavior. All other answers are potentially treatable medical problems that could account for the presentation of an agitated or violent patient. After assuring the safety of all parties involved, the emergency department physician should rule out organic causes of agitation. In dealing with the potential violent patient, the emergency physician should: A. Approach the patient in a calm, controlled and professional manner B. Assume that the strength of the doctor-patient relationship will ensure safety C. Deal with the patient in a isolated room to protect the patient's privacy D. Use a loud voice and threaten to call security if the patient becomes agitated - A. Approach the patient in a calm, controlled and professional manner The answer is A. Excessive eye contact may be interpreted as a sign of aggression (answer A). Emergency physicians are encouraged to maintain intermittent eye contact with the patient and to keep a professional and calm demeanor. Also a physician should never deal with an agitated or violent patient alone in an isolated room (answer D). Doors should always remain open and exits should never be blocked. Ample security should be close at hand before interviewing the patient (answer E). Finally, involved parties are encouraged to remove any personal effects (e.g. neckties, necklaces, earrings, etc.) that could be used as a weapon by the violent patient. A 35 year-old male is placed on his back on the gurney in physical restraints for violent behavior. Which life-threatening complication can arise? A. circulatory obstruction B. Metabolic acidosis C. Asphyxia D. Rhabdomyolysis - B. Metabolic acidosis The answer is B. Bruises and abrasions are the most common complication of physical restraints. After restraint application, patients need to be monitored frequently and positions changed to prevent neurovascular complications such as circulatory obstruction, pressure sores, and rhabdomyolysis. Positional asphyxia can arise when patients are placed into the prone or hobbled position. Protracted struggle against restraints can promote a significant metabolic acidosis that has been associated with cardiovascular collapse. Patients who continue to struggle with physical restraints should be chemically restrained as well Which medication is ideal for the agitated or combative patient? A. Nitrous oxide B. Hydromorphone C. Haloperidol D. Propofol - The answer is C. Drugs with a relatively short half-life allow for more careful monitoring of chemically restrained patients. Patients may be given multiple administrations of the restraining agent as needed. Antipsychotics (such as haloperidol) and benzodiazepines (such as lorazepam) exhibit most of these characteristics and are commonly used in combination in the emergency department. The use of 5 mg of haloperidol IV/IM with 2 mg of lorazepam IV/IM, repeated every 30 minutes as needed, is recommended for the combative patient who does not have contraindications to these medications. Half doses should be used in the elderly. 19 year old man is brought in to the emergency department by EMS after being found obtunded in his apartment. No additional history is available. On arrival, the patient is minimally responsive with sonorous respirations and a palpable rapid pulse. The most appropriate initial diagnostic test would be A. Arterial blood gas B. Electrocardiogram C. Fingerstick glucose D. Urine drug screen - C. Fingerstick glucose The answer is C. Hypoglycemia is a common and readily treatable cause for altered mental status. An ABG is unlikely to be diagnostic and more likely to reflect secondary abnormalities caused by respiratory depression. While a urine drug screen may show positives, it cannot quantitate the amount of a substance or the time period in which the exposure occurred so a positive screen may not reflect cause and effect. An EKG, while a part of a toxicology evaluation, is not an appropriate initiate screening test for an unstable patient until airway and readily reversible causes have been addressed. A 27 year old is found unresponsive in his car in the hospital parking lot and brought in by security. During your initial evaluation you find him to be cyanotic with pulse oximetry reading 82% on room air with a respiratory rate of 4 breaths per minute. Radial pulses are present at 120 bpm. Pupils are 1mm bilaterally. Your team is having difficulty finding a vein for an intravenous line due to extensive scarring of his arms. You are suspicious of an overdose, which medication would you want to rapidly administer as a potential antidote in this situation? A. Glucose B. Naloxone C. Thiamine D. Flumazenil - B. Naloxone The answer is B. The patient has stigmata of an opiate overdose with hypopnea, cyanosis, and miotic pupils. In addition, intravenous drug users often use up their veins. While hypoglycemia can definitely cause a depressed mental status and needs to be assessed, it should not result in respiratory depression or miotic pupils. Thiamine is utilized to prevent Wernicke's encephalopathy particularly in malnourished patients who present with hypoglycemia but is not an antidote per se. Flumazenil can be used to temporarily reverse the respiratory depression caused by benzodiazepines but also carries with it the risk of precipitating withdrawal and uncontrollable seizures in chronic benzodiazepine users. As a result, it is not recommended for routine use in patients with altered mental status. A 53 year-old known alcoholic presents with agitation, vomiting and altered mental status. His fingerstick glucose is 148. His serum ethanol level is undetectable and his head CT is normal. An ABG shows a pH of 7.21, pCO2 of 34, pO2 of 98 on room air. His basic chemistry panel includes a sodium of 136, potassium 4.1, chloride 108, bicarbonate 14, BUN 12, creatinine 1.1. What substance are you concerned that he may have ingested: A. Ethylene glycol B. Salicylates C. Isopropyl alcohol D. Methanoleeette - C. Isopropyl alcohol The patient is presenting with a non anion gap metabolic acidosis. Isopropyl alcohol is metabolized via alcohol dehydrogenase to acetone which accumulates and causes significant ketosis but not an anion gap. Other toxic alcohols such as methanol and ethylene glycol are ultimately metabolized to formic and glycolic acids which cause toxic effects and an anion gap metabolic acidosis. Salicylates result in an anion gap metabolic acidosis with a superimposed respiratory alkalosis. The following mnemonic can be used to recall the common causes of an increased anion gap metabolic acidosis: CAT MUDPILES; C - cyanide A - alcoholic ketoacidosis T - toluene M - methanol U - uremia D - diabetic ketoacidosis P - paraldehyde I - isoniazid/iron L - lactate E - ethylene glycol S - salicylates Isopropyl alcohol causes a ketosis without an acidosis. In treating hepatitis secondary to alcoholic liver disease, all of the following are true EXCEPT: A. Treatment is primarily supportive including fluids and electrolyte correction. B. Glucose should be administered prior to thiamine to avoid precipitating acute Wernicke's encephalopathy C. Magnesium replacement should be initiated empirically except in the setting of contraindications such as renal failure or hypermagnesemia. D. Coexisting gastritis should be sought out and treated appropriately. E. Nutritional status should be assessed with attention to possible protein restriction. - B. Glucose should be administered prior to thiamine to avoid precipitating acute Wernicke's encephalopathy The answer is B. Alcoholics often have low thiamine levels due to poor nutrition, and low glucose levels due to the suppression of gluconeogenesis by alcohol. However, thiamine should always be replaced prior to glucose to avoid the potential complication of precipitating Wernicke's encephalopathy. Magnesium levels may appear normal on laboratory testing, but alcoholics typically have low magnesium stores and should be given magnesium empirically unless contraindications for magnesium exist. Alcoholics should also be evaluated for gastritis and overall nutritional status and should be referred appropriately. A 45 year old man is brought to the E.D., with markedly altered mental status as reported by someone who stays with him at a homeless shelter. The patient is very confused and obtunded, and unable to provide a cogent history; the person who brought him to the E.D. notes the patient has a "drinking problem." The patient's vital signs are normal, except for a respiratory rate of 22. As he lays in the stretcher, his appearance is as depicted in the Figure. Of the following choices, which physical finding is most likely to be present on physical examination? [image] A. Homan's sign B. anterior chest pain upon leaning forward, which is relieved by lying flat C. dendritic rash on the posterior thorax, with a sentinel lesion noted on the left shoulder D. upon elevation of the arms to 90-degrees (in 0-degrees abduction), and pronation of the hands with fingers spread, wrists and interphalangeal joints are characterized by jerky alternations of extension and flexion E. increase in systolic blood pressure by more than 10 mmHg with inspiration - D. upon elevation of the arms to 90-degrees (in 0-degrees abduction), and pronation of the hands with fingers spread, wrists and interphalangeal joints are characterized by jerky alternations of extension and flexion The answer is D. This patient has marked ascites (which may incidentally account for his mild tachypnea due to impairment of respiratory excursion). The most likely explanation given the limited information available is liver disease, and asterixis ("liver flap") as described in choice D is a likely marker of advanced hepatic failure. A 60 year old male presents with new onset confusion. Which of the following suggests a functional, as opposed to an organic etiology? A. abnormal vital signs B. acute onset C. auditory hallucinations D. disorientation - C. auditory hallucinations The answer is C. The other findings are all characteristic of organic confusional states. Hallucinations can occur with both organic and functional causes of confusion. Hallucinations associated with organic confusion may be visual, tactile, or auditory. Hallucinations in patients with functional disease tend to be auditory. Delirium is defined as: A. a stressed psychological state resulting from extreme emotional stimulus B. abnormal behavior associated with decreased alertness and decreased psychomotor activity C. abnormal behavior accompanied by hallucinations, occurring in an oriented patient D. a global inability to relate to the environment and process sensory input - D. a global inability to relate to the environment and process sensory input The answer is D. Alterations in mental status resulting from extreme emotional stimulus would usually be functional abnormalities. Patients with delirium manifest increases in alertness and psychomotor activity. Delirium is more than simple alteration of mental status. Delirium is an organic confusional state. Patients with delirium may have hallucinations, but patients who are oriented are more likely to have functional causes for altered mental status. Which of the following statements regarding psychotic behavior is true? A. Brief psychotic episodes, often precipitated by events such as death of a loved one, can be characterized by extremely bizarre behavior and speech B. Delusions are defined as false beliefs that are not amenable to arguments or facts to the contrary C. Delusional disorder usually results in impairment in daily functioning D. Schizophreniform disorder is present when a patient meets the diagnostic criteria for schizophrenia but the process has been present for less than one year - B. Delusions are defined as false beliefs that are not amenable to arguments or facts to the contrary B. Psychosis can be limited to nonbizarre delusions; patients with this disorder (delusional disorder) rarely have impairment in daily functioning. Fixed, false beliefs that are not held by others with a patient's cultural background are characteristic of delusional thinking. A 75 year old female is brought the to emergency department by a family member with a history of progressive forgetfulness and confusion. She has a history of dementia. The most common cause of dementia in the elderly patient is: A. Alzheimer's disease B. Parkinson's disease C. Pick's disease D. Vascular dementia - A. Most dementia is Alzheimer's type. The second most common cause of dementia is vascular dementia, which accounts for 10 to 20% of all dementias. Primary degenerative dementias include Alzheimer's disease, vascular dementia, subcortical dementias involving the basal ganglia and thalamus (e.g., progressive supranuclear palsy, Huntington's chorea, Parkinson's disease), and Pick's disease, also known as dementia of the frontal lobe type. Smaller percentages are attributable to causes such as anoxic encephalopathy, hepatolenticular degeneration, tumors, and slow virus infections. A 65 year old male is brought to the emergency department after he was found wandering on the street. He is unkempt and confused. A diagnosis of delirium, rather than dementia, is more likely if which of the following is true? A. there has been a slow progressive loss of memory B. the sleep-wake cycle is unaffected C. there is a change in the level of consciousness D. the confusion is worse during the day - C. there is a change in the level of consciousness The answer is C. Patients with delirium have disturbances in consciousness, cognition, and perception. These disturbances tend to occur over a short period of time (hours to days). The delirious patient may be somnolent or agitated. Thought process may be mildly disturbed or grossly disorganized. The clinical presentation may be subdued or explosive, and the course can fluctuate over minutes to hours. The patient's sleep-wake cycle may be altered or reversed; agitation is often present during the night. An acute confusional state can also be one of the protean manifestations of a metabolic or nutritional abnormality, including hepatic encephalopathy, acute renal failure, and diabetic ketoacidosis or hyperosmolarity. An 80 year old nursing home patient is brought to the emergency department with an acute onset of confusion. Which of the following metabolic abnormalities is the most likely explanation? A. hypocalcemia B. hypokalemia C. hypernatremia D. hyperphosphatemia - C. hypernatremia The answer is C. The differential diagnosis of acute confusional states is lengthy. It includes many metabolic/nutritional abnormalities including hypoglycemia, hypo-/hypernatremia, and hypercalcemia. Hypokalemia alone, however, is not a common cause of altered mental status. Which factor is least reliable in differentiating between organic and inorganic causes of confusion? A. acute versus chronic onset B. Vital sign abnormalities C. Presence of attention deficit D. Signs of trauma - C. Presence of attention deficit The answer is C. Presence of an attention deficit is common to all confusional states. All the other options may be used to differentiate organic versus non-organic causes of confusion. Characteristics of organic causes include acute onset, abnormal vital signs, fluctuating level of consciousness, possibly signs of trauma, and/or focal neurologic signs. Inorganic (functional) causes commonly illustrate chronic onset, stable vital signs, absence of trauma or focal neurologic symptoms, and/or delusions and illusions. With regard to specific causes of hypertension, which of the following is true? A. Hypertensive encephalopathy is more likely than hypertensive stroke in patients whose mental status changes are reversible B. Hypertensive encephalopathy causes adverse outcomes over days or weeks, rather than hours C. Patients with stroke syndromes must have blood pressure normalized as quickly as possible to reduce the risks of worsening neurological deficit D. Laboratory analysis is rarely useful in cases of confirmed pediatric hypertension E. Laboratory analysis is rarely useful in cases of confirmed hypertension in pregnant patients - A. Hypertensive encephalopathy is more likely than hypertensive stroke in patients whose mental status changes are reversible The answer is A. Hypertensive encephalopathy is a true medical emergency, and can cause coma and death over hours; however, encephalopathy due to hypertension is more likely reversible than encephalopathy from other causes. Avoidance of overzealous blood pressure lowering is particularly critical for patients with strokes. Laboratory analysis can be important in cases of hypertension in pediatric patients (for whom renal/renovascular or pheochromocytoma may be identified) and in pregnant patients (for whom laboratory testing can help establish diagnoses such as the HELLP syndrome). A 29 year old woman is found seizing by her husband and is rushed to the emergency department. On presentation, she is noted to have a BP of 162/112, is still seizing, and looks puffy all over. Her husband tells you that they are expecting their first child in a few months. Which of the following is the next best step in this patient's care? A. Control the seizures with magnesium sulfate. B. Draw blood to check CBC, LFT's, BUN, and creatinine. C. Notify the labor floor that the patient is in the emergency department. D. Perform a CT scan of head if seizures persist. E. Start hydralazine to decrease the patient's blood pressure. - A. Control the seizures with magnesium sulfate. The answer is A. Antihypertensive therapy is only indicated in eclampsia if the diastolic blood pressure remains > 110 mm Hg after seizures are controlled because rapid lowering of blood pressure can result in uterine hypoperfusion. All the other choices (A-D) are appropriate in the management of the patient with eclampsia. Which of the following is *not* a feature of febrile seizures? A. generalized tonic-clonic seizure B. duration less than 15 minutes C. associated with a rapid rise in body temperature D. occurs in children ages 3 months to 5 years E. associated with postictal state of 30 minutes - E. associated with postictal state of 30 minutes The answer is E. Febrile seizure is not associated with a postictal period. The child usually rapidly regains alertness. Intracranial mass or infection should be a concern if the duration of seizure is greater than 15 minutes or if altered mental status persists after the cessation of seizure activity. A 47 year old man with a history of alcohol abuse presents to the ED after having a seizure. His past includes both seizures and blackouts. His last alcoholic drink was the previous evening. This morning he experienced palpitations, diaphoresis, and dizziness before losing consciousness and having a seizure lasting under a minute. Which of the following is *true* statement with to alcohol and its association with seizures? A. In people with an underlying seizure disorder, excessive alcohol intake is a risk-factor for seizure due to increased likelihood of head injury, predisposition to metabolic disorders, and lowered seizure threshold. B. Alcohol intake itself can precipitate seizures due to the neurotoxic effects of alcohol and its metabolites. C. Cessation of alcohol can precipitate seizures as part of the alcohol withdrawal syndrome. D. All of the above statements are true. E. All of the above statements are false. - D. All of the above statements are true. A 68 year old diabetic male, previously living independently, is brought in by his family. He has been acting abnormally for two days. The family reports he is awake all night and sleepy during the day. He is confused about where he is and the time of day, and sometimes doesn't recognize his daughter and son-in-law. At other times he appears and acts almost normally. Which of the following is *true* regarding his condition? A. Infection is an unlikely cause of his condition unless his temperature is > 102°. B. Dementia is the most likely cause of his condition and the family must be counseled. C. Medications are an unlikely cause of this condition in the elderly. D. Patients can be agitated and combative, or calm and quiet in this condition. E. Treatment includes maximizing sensory input. - D. Patients can be agitated and combative, or calm and quiet in this condition. The answer is D. The scenario describes a patient with delirium, a condition in which patients may be agitated and combative, or calm and quiet. The most common cause of delirium in the elderly is medications, accounting for 22-39% of cases. Infection and metabolic abnormalities are other common causes, and delirium may be the first indication that an infection is present. An elderly patient with delirium resulting from an infection may have a normal temperature, a low temperature, or a high temperature. Delirium is characterized by an *acute onset of a disturbance in level of consciousness, cognition and attentiveness*. It has a fluctuating course, and alterations in sleep-wake cycles are common. Dementia, in contrast, has a slower course, that is gradually progressive over months to years, and consciousness is preserved. In addition to correcting the underlying cause, it is important to minimize stimulation, because the patient with delirium has difficulty processing stimuli. An 18 year old hockey player is hit in the mouth with a puck, fracturing a maxillary canine tooth. He brings the severed piece of tooth with him. On physical exam, the tooth is fractured halfway between the tip and the gumline. The root of the tooth is still firmly intact. The exposed fracture site has a yellowish tinge without blood. Of the following choices, which is the most appropriate management for this patient? A. No specific treatment required B. Application of calcium hydroxide, placement of aluminum foil, and dental follow-up C. Placement of tooth fragment in saline gauze, outpatient dental follow-up D. Immediate dental consult to avoid abscess formation E. Replace fractured piece and place acrylic splint - D. Immediate dental consult to avoid abscess formation The answer is D. Ellis II dental fracture involves enamel and dentin. The fracture site typically has a yellowish tinge. Ellis III dental fractures are characterized by exposure of pinkish pulp and often blood. These fractures require immediate dental consultation to prevent abscess formation. A 22 year old man is punched in the nose during a fight. He presents to the emergency department with obvious nasal bone deformity. Pressure controls the bleeding. Physical exam reveals no maxillary bone or orbital rim tenderness, intact vision and extraocular movement. The oropharynx and mandible are unremarkable. Nasal inspection reveals a swollen, ecchymotic, tender nasal septum. Which of the following is the most appropriate initial step? A. Outpatient follow-up with an ENT specialist to surgically correct a deviated septum B. Plastic surgery consult for immediate reduction of nasal fracture C. Facial CT scan to rule out more serious facial fractures D. Incision and drainage of the septal hematoma followed by nasal packing E. Needle aspiration of the septal hematoma - D. Incision and drainage of the septal hematoma followed by nasal packing A 24 year old woman is playing racquetball and sustains a direct blow from the ball to the right eye. She presents to the emergency department complaining of eye pain and double vision. On exam, her right eye does not track properly with upward gaze. This finding suggests which of the following injuries? A. Inferior orbital wall fracture B. Superior orbital rim fracture C. Ethmoid fracture D. Zygomatic arch fracture E. Inferior orbital rim fracture - A. Inferior orbital wall fracture The answer is A. The patient most likely has an orbital floor fracture with entrapment. A 32 year old man is struck several times in the head with a baseball bat. Upon emergency medical service arrival, he is mildly confused, vomits once, and complains of a severe headache. The emergency medical technicians establish two large-bore IVs. Prior to arrival at the emergency department, he loses consciousness and begins to seize. He is actively seizing when he is brought into the trauma bay. What should be the first step in the management of this patient? A. Administration of phenytoin 1000mg IV B. Administration of mannitol 50 g IV C. Rapid sequence intubation using paralytic agent D. Emergency craniotomy E. Administration of 2 liters NS bolus - C. Rapid sequence intubation using paralytic agent The answer is C. The airway should be managed as the first priority in this patient. The other maneuvers may be helpful but are secondary to securing an airway and providing oxygenation/ventilation. Airway comes first! A 46 year old man is brought in by EMS after a motor vehicle collision in which he was an unrestrained driver. Although he has no obvious injury to his head or neck, he complains of chest pain and appears very short of breath. His vital signs are: T 99.2 F, BP 85/57, HR 123, RR 36, SpO2 95% on non-rebreather. The CXR demonstrates a tension pneumothorax. Of the following, which is the most appropriate next step in this man's care? A. Placement of a chest tube followed by a chest xray to determine proper placement B. Transfusion of 2 units of O-negative packed red blood cells C. Performance of a chest CT scan to further delineate the pathology D. Placement of a needle decompression device, followed by repeat CXR - D. Placement of a needle decompression device, followed by repeat CXR This patient needs emergent chest decompression and this is rapidly done by needle thoracostomy. A chest CT may be performed, but only once he is stabilized. A formal chest tube will be placed, but placement may not be rapid enough and he may decompensate in the meantime. Transfusion of blood does nothing to correct the physiology of a tension pneumothorax The most sensitive bedside test for nerve injury in a finger after trauma is: A. light touch B. O'Riain wrinkle test C. pain D. temperature sensation E. two-point discrimination - E. two-point discrimination The correct answer is E. Light touch is a good screening test, but two-point discrimination is more sensitive and should be used routinely in evaluating injuries to digits. The O'Riain wrinkle test involves placing the digit in warm water and looking for wrinkling of the digital pulps. Presence of wrinkling indicates the nerve is intact. Which is *not* part of the Ottawa ankle rules? A. inability to walk 4 steps at the time of the injury B. inability to walk 4 steps in the emergency department C. tenderness over the lateral malleolus D. tenderness over the medial malleolus E. tenderness over the talus - E. tenderness over the talus The correct answer is E. The Ottawa ankle rules are a validated (for adults) set of physical exam findings to determine if an ankle X-ray is needed after an injury. If any of the first 4 answers is present or if there is *tenderness over the navicular or base of the 5th metatarsal*, an X-ray should be obtained. If the correct answer to all questions is no, then an X-ray is not needed. Choose the INCORRECT statement regarding thoracentesis from the anterior approach (needle decompression): A. An upright chest X-ray should always be performed following a thoracentesis to confirm the successful relief of a tension pneumothorax and the absence of hemothorax or other complications. B. A 14- to 20-gauge needle is inserted perpendicularly over the superior edge of the rib. C. The recommended insertion site is the second intercostal space, midaxillary line. D. After the needle is inserted into the pleural space, a rush of air confirms the presence of a tension pneumothorax. E. If a tension pneumothorax is confirmed via needle decompression, then a thoracostomy tube should be placed as soon as possible. - C. The recommended insertion site is the second intercostal space, midaxillary line. The answer is C. The recommended insertion site for needle decompression of tension pneumothoraces is the second intercostal space along the midclavicular line. If a lateral approach is needed, the recommended insertion site is the fourth or fifth intercostal space in the midaxillary line. The lateral approach poses a greater risk of parenchymal injury. The needle should always be inserted over the superior edge of the rib as the neurovascular bundle runs along the inferior margin (answer B). The remaining answers are all correct statements regarding thoracentesis (answers C, D, E). In a patient with a suspected ruptured globe from penetrating trauma to the eye, all of the following should be performed EXCEPT: A. ascertainment of intraocular pressure via tonometry B. administration of broad spectrum antibiotic therapy C. visual acuity assessment D. ascertainment of tetanus status E. ophthalmology consultation - A. ascertainment of intraocular pressure via tonometry The answer is A. Tonometry should not be performed in patients with suspected ruptured globe, as application of the Tono-Pen pressure to the eye may cause the vitreous humor to exude from the eye, thereby complicating the injury. Tetanus status is important to check, as ocular injuries, like skin injuries, may be a portal for tetanus exposure. Broad-spectrum antibiotic therapy is indicated. Anti-emetic therapy may be helpful in preventing the elevations in intraocular pressure associated with vomiting. Visual acuity assessment is important and ophthalmology consultation is critical. Following a motor vehicle crash, a 25 year old man presents complaining of a painful right eye. Visual acuity is 20/200 in the right eye and 20/25 in the left eye. The right eye protrudes from the orbit and the patient has right eye pain with extraocular movement. What is the most likely cause of his symptoms? A. retrobulbar hematoma B. chemosis C. hyphema D. orbital blow-out fracture E. ruptured globe - A. retrobulbar hematoma The answer is A. Traumatic proptosis with impaired extraocular movements is classic for retrobulbar hematoma. Sequelae include optic nerve ischemia and secondary visual impairment. A ruptured globe presents with enophthalmos, not proptosis, as vitreous humor leaks out of the eye. Neither hyphema nor chemosis causes proptosis. Orbital blowout fractures can cause inferior rectus muscle entrapment and secondary pain with impairment of extraocular movement. Yet, they do not present with proptosis - unless complicated by retrobulbar pathology. Following a brawl at a local bar, a gentleman presents with an impressive right-sided periorbital ecchymosis. All of the following physical examination findings would suggest an orbital blowout fracture EXCEPT: A. diplopia with upward gaze B. right-sided infraorbital subcutaneous emphysema C. right-sided epistaxis D. proptosis E. anesthesia of the right infraorbital region - D. proptosis D. Orbital blowout fractures classically involve the *maxillary or ethmoid sinus* and consequently often cause either epistaxis (through the connection of the maxillary sinus with the nose) or subcutaneous emphysema (through the entry of air from the sinuses into the subcutaneous tissue). A fracture through the maxillary sinus may extend through the portal by which the second branch of the trigeminal nerve exits, thus causing anesthesia of the ipsilateral infraorbital region. *If the inferior rectus muscle gets trapped within the fracture of the inferior orbital wall, patients will be unable to look upward causing diplopia with upward gaze*. Orbital blowout fractures are not typified by proptosis. In fact, proptosis in the setting of trauma should prompt physicians to suspect the possibility of a retrobulbar hematoma. The patient depicted in the figure presents to the ED just after sustaining a pellet-gun wound to the right eye. What do the arrows most likely indicate? [image] A. hyphema B. iritis C. keratitis D. pterygium E. hypopion - A. hyphema The answer is A. The patient has a *fluid level/meniscus in the anterior chamber*, that is most likely indicative of hyphema (collection of blood). Hypopion (collection of purulent material) is less likely in this setting, and keratitis (corneal inflammation) and iritis (inflammation of the iris) are not indicated by the arrows. A pterygium is a growth which is visible on the sclera, and which crosses the limbus onto the cornea. The patient in the figure sustained minor blunt trauma to the eye, and has a normal head/orbital computed tomography (CT) scan. Ophthalmological examination is normal, other than the blood as shown in the figure (the blood does not cross the limbus). Of the choices below, which diagnosis is the most likely based upon the figure? [image] A. foreign body B. ruptured anterior chamber C. subconjunctival hemorrhage D. hyphema E. globe rupture - C. subconjunctival hemorrhage The answer is C. The subconjunctival blood as depicted in this patient, can be expected to resorb without intervention over days to weeks. The figure does not suggest rupture of anterior chamber or hyphema; globe rupture and foreign body are less likely given the normal examination and CT scan. A patient presents with a self-inflicted wound, with resultant loss of vision in the right eye. With regard to the figure, which of the following statements is most likely true? [image] A. Medial canthotomy should be performed immediately. B. If ambulance providers contact medical control about a patient with this injury, they should be directed to replace the globe back into the orbit. C. Search for other self-inflicted injuries (or ingestions) is paramount. D. Life-threatening hemorrhage is a major risk with this injury. E. The patient will probably recover visual function. - C. Search for other self-inflicted injuries (or ingestions) is paramount. The answer is C. The patient is unlikely to recover any visual function, which renders more important parallel efforts to identify (treatable) injuries or ingestions that are less obvious than the ocular avulsion. Lateral (not medial) canthotomy is an emergency procedure that may be indicated in some patients with ocular injury and retrobulbar hematoma (with resultant traction on the optic nerve), but the procedure is unlikely to help this patient. Since manipulation of an injured globe risks further trauma and extrusion of vitreous humor, prehospital recommendations for eye trauma are limited to protection of the injured eye and expedited transport to definitive care. Life-threatening hemorrhage is not a major risk with this type of injury. What is the most common cause of death in Americans aged 20 to 40 years? A. Drug overdose B. Trauma C. Cancer D. AIDS-related illness E. Pneumonia - B. Trauma Following a motor vehicle collision, in which of the following patients is an emergency department Caesarian section most likely indicated, assuming a fetus at 29-weeks gestation? A. Mother with gunshot wound to abdomen, blood pressure 96/42; fetal heart tones undetectable B. Mother with severe head trauma, blood pressure 170/90; fetal heart tones 120 beats per minute C. Mother with abdominal pain, blood pressure of 80/40; fetal heart tones 100 beats per minute D. Mother with vaginal bleeding, blood pressure 118/78; fetal heart tones 80 beats per minute E. Mother pulseless and apneic for 2 minutes' duration and still in arrest; fetal heart tones of 100 beats per minute - E. Mother pulseless and apneic for 2 minutes' duration and still in arrest; fetal heart tones of 100 beats per minute The answer is E. Though emergency C-section after maternal death is a rarely indicated procedure, rapid intervention (within minutes) of maternal demise has resulted in viable births. A 76 year old restrained driver is involved in a head-on collision at about 35 mph. He arrives at the emergency department in a cervical collar and on a backboard. His only complaint is neck pain, and he has mild posterior neck tenderness. A CT scan of the neck shows no fracture and only degenerative arthritis. Upon re-evaluation you note the patient has difficulty raising his arms against gravity and there is decreased grip strength bilaterally. The remainder of his neurological exam is normal. What is the most appropriate management for this patient? A. Administration of IV steroids and ordering of cervical MRI B. Immediate neurosurgical decompression C. Flexion and extention radiographs to rule out ligamentous injury D. Discharge home with a hard cervical collar with neurosurgical follow-up E. Reassurance and discharge with NSAIDs given the non-anatomical distribution of weakness - A. Administration of IV steroids and ordering of cervical MRI The answer is A. Central cord syndrome results from a hyperextension injury, typically in elderly patients with significant degenerative joint disease. The ligamentum flavum buckles into the cord, resulting in a contusion of the cord's central portion. A 46 year old construction worker falls 6 feet off a ladder onto a concrete surface and has sudden and severe low back pain. The pain radiates down his right leg and he develops numbness over the anterior shin and dorsum of the foot. On physical exam he has decreased sensation to pinprick over the dorsum of the right foot (medially) and some weakness in right foot dorsiflexion. At which level is a protruding intervertebral disc most likely? A. L1-L2 B. L2-L3 C. L3-L4 D. L4-L5 E. L5-S1 - D. L4-L5 The answer is D. Sensation of the dorsal aspect of the foot and dorsiflexion of the foot are functions of the L5 nerve root. Herniation of the L4-5 disc would result in compression of L5. Which of the following cervical spine fractures is considered stable? A. Transverse process fracture B. Flexion teardrop fracture C. Bilateral facet dislocation D. Hangman's fracture of C2 E. Jefferson fracture of C1 - A. Transverse process fracture The answer is A. A transverse process fracture involves only one of the supporting spinal columns (the posterior column) and is therefore stable. A 23 year old man is stabbed in the anterior neck with a 3-inch knife during a street fight. At the scene, there is some bleeding, which is controlled with direct pressure. He presents to the emergency department breathing comfortably and in no distress. His pulse is 88, blood pressure 126/76, and oxygen saturation 99% on room air. There is a 1cm laceration 2cm above the right sternoclavicular junction, lateral to the trachea. There is mild oozing and no obvious underlying hematoma. There is no obvious subcutaneous air, and he has clear lung sounds. What is the most appropriate management for this patient? A. Local wound exploration and discharge home if no significant injury identified B. Angiography, esophogram, and admission for observation C. Local wound exploration and discharge home after 6-hour observation period D. CT scan of the neck and discharge home after 6 hours of observation E. Immediate operative exploration - B. Angiography, esophogram, and admission for observation The answer is B. Zone I penetrating neck injuries are located between the sternal notch and the cricoid cartilage. A major concern is injury to non-compressible vascular structures such as common carotid, vertebral, subclavian, aortic arch. Other structures in this area include trachea, esophagus, and lung apices. Physical exam is often unreliable and angiography, esophogram, and observation are warranted. Which of the following patients should undergo abdominal trauma evaluation? A. 22 year old with stab wound to fourth intercostal space on right B. 30 year old with pelvic pain and tenderness after fall C. 25 year old restrained passenger in high-speed MVA; no abdominal complaints D. None of the above E. All of the above - E. All of the above The answer is E. The diaphragm can rise to as high a level as the fourth intercostal space and can be injured by stab wounds at this level. Unsuspected injuries are common in high speed motor vehicle crashes. Pelvic injuries are associated with intra-abdominal injuries and can distract a patient from such an injury. Therefore, all of these patients need an evaluation of their abdomens. Which of the following trauma patients can be managed conservatively without immediate laparotomy in the OR? A. 27 year old man with hemoperitoneum by bedside ultrasound; hypotensive B. 19 year old man with splenic laceration; peritoneal signs on exam C. 24 year old man with liver laceration; hemodynamically stable D. 30 year old man with a gunshot wound to the epigastrium E. All of the above should go to the OR for exploratory laparotomy. - C. 24 year old man with liver laceration; hemodynamically stable Which of the following is an accurate statement? A. Bedside ultrasound is the test of choice for diagnosing solid organ injury. B. Diagnostic peritoneal lavage usually cannot identify the presence of hemoperitoneum. C. Bedside ultrasound can image the retroperitoneum. D. Bedside ultrasound can reliably determine the etiology of hemoperitoneum. E. Diagnostic peritoneal lavage cannot determine the etiology of hemoperitoneum. - E. Diagnostic peritoneal lavage cannot determine the etiology of hemoperitoneum. The answer is E. Diagnostic peritoneal lavage is extremely sensitive for the detection of hemoperitoneum and can lead to many negative laparotomies. Neither bedside ultrasound nor diagnostic peritoneal lavage can identify the source of the hemorrhage though. A trauma ultrasound at the bedside can only identify fluid in the peritoneal cavity, and CT scan is the test of choice for diagnosing solid organ injury. A 36 year old man is a restrained driver involved in a high speed MVA where his car is struck on the driver's side door with significant intrusion. His physical exam is significant for a large contusion on his left flank. His abdominal exam is benign and rectal exam reveals a normal prostate. A Foley catheter is placed with return of gross hematuria. Which test is indicated to evaluate for the presence of urologic injury? A. CT abdomen / pelvis with IV and transurethral contrast B. Ultrasound of the bladder C. CT abdomen / pelvis without contrast D. Ultrasound of the kidneys E. CT abdomen / pelvis with IV contrast alone - A. CT abdomen / pelvis with IV and transurethral contrast In which of these patients is emergency department thoracotomy indicated? A. All of the above should undergo emergency department thoracotomy. B. Unbelted driver in a high-speed motor vehicle crash who loses his pulse while being extricated, and arrives at the E.D. after a 45-minute transport C. Patient with stab wound to the anterior chest who is dyspneic with an oxygen saturation of 80% and a blood pressure of 168/102 D. Pedestrian struck with massive pelvic fractures who loses pulses and blood pressure at the scene E. Patient with a gunshot wound to the chest who upon arrival is unconscious and pulseless, with a systolic blood pressure of 60 - E. Patient with a gunshot wound to the chest who upon arrival is unconscious and pulseless, with a systolic blood pressure of 60 The answer is E. Emergency Department thoracotomy is a controversial procedure. When chosen carefully, successful resuscitation can occur. Cardiac arrest due to blunt trauma has a dismal success rate and is generally not considered an indication for ED thoracotomy. Thoracotomy for penetrating chest wounds has the best success rate. An awake patient with a relatively normal blood pressure does not need one performed in the Emergency Department. An unconscious and pulseless patient with a detectable blood pressure has the best chance for survival. A 32 year old female is shot with a 38-caliber pistol at close range in the right anterior chest. She presents to the emergency department intoxicated and yelling. Her vitals include a pulse of 92, blood pressure of 134/84, and oxygen saturation of 97%. She has clear breath sounds bilaterally. The entrance wound is just above the right breast and an exit wound is noted in the right axilla. What is the most appropriate management of this patient? A. IV access, endotracheal intubation and simultaneous placement of a right chest tube, bedside ultrasound, portable chest X-ray, and admission to the ICU if stable B. IV access, portable chest X-ray, tube thoracostomy, and exploratory thoracotomy in the OR to search for cardiac or pulmonary vascular injury C. IV access, endotracheal intubation, emergency department thoracotomy to search for cardiac or pulmonary vascular injury D. IV access, portable chest X-ray, right chest tube placement if X-ray shows a pneumo- or hemothorax, admission to the ICU for observation E. IV access, endotracheal intubation, CT scan of chest to look for pneumo- or hemothorax, or injuries to the heart or great vessels - A. IV access, endotracheal intubation and simultaneous placement of a right chest tube, bedside ultrasound, portable chest X-ray, and admission to the ICU if stable During a bar fight, a 42 year old man is stabbed in the left side with an unknown weapon. He presents to the emergency department with dyspnea, pulse of 108, blood pressure of 138/92, and oxygen saturation of 94% on room air. He has absent breath sounds on the left side; you note a small puncture wound in the midaxillary line at the level of the 10th rib. His abdominal exam is normal. Two large-bore IVs are established. What is the appropriate management of this patient? A. Left-sided chest tube, portable chest x-ray, and admission B. Left-sided chest tube, portable chest x-ray, diagnostic peritoneal lavage, and admission C. Endotracheal intubation, left-sided chest tube, portable chest x-ray, and admission D. Endotracheal intubation, portable chest x-ray, exploratory laparotomy in the OR, and admission E. Left-sided chest tube, portable chest x-ray, and abdominal CT scan - E. Left-sided chest tube, portable chest x-ray, and abdominal CT scan Which is the most common associated neurological finding with a distal radius fracture? A. Weakness with flexion at the finger MCP joints B. Wrist drop C. Decreased sensation over the hypothenar eminance D. Weakness of finger adduction E. Decreased sensation over the thenar eminance - E. Decreased sensation over the thenar eminance The answer is E. This finding is due to median nerve injury. An 82 year old woman with osteoporosis slips and falls onto her right hip. She cannot get up and is brought to the emergency department by ambulance. As you enter the room you notice her right leg is abducted and externally rotated. What type of injury does she most likely have? A. Subtrochanteric femur fracture B. Intertrochanteric femur fracture C. Femoral neck fracture D. Acetabular fracture E. Posterior hip dislocation - C. Femoral neck fracture The answer is C. Patients with dislocation tend to have internal (not external) rotation. A 22 year old running back is struck from behind by a 300-pound lineman. The blow occurs below the knee as his foot is firmly planted and two other linemen are holding his upper body. He presents to the emergency department with gross anterior dislocation of the tibia on the femur. His foot is cool and pale, and dorsalis pedis and posterior tibial pulses are not detected by Doppler ultrasound. What is the most appropriate management for this patient? A. Open reduction in OR with exploration of popliteal artery B. Immediate reduction in emergency department under conscious sedation without X-rays C. Immediate orthopedic consultation without attempts to manipulate the knee D. Immediate arteriography to assess for popliteal artery disruption - B. Immediate reduction in emergency department under conscious sedation without X-rays The answer is B. A knee dislocation frequently injures the popliteal artery, threatening the survival of the limb. Immediate reduction for the dislocation is warranted to attempt to restore flow through the artery, and should be attempted by the ED physician without waiting for orthopedics. Transport to the OR is an unnecessary delay, and while arteriography will be indicated, the most urgent priority is restoring blood flow. A patient falls onto his face, and has a CT scan of the face as shown in the Figure. Which indirect finding suggestive of possible facial fracture is present on the CT? [image] A. Fluid (blood) in the sinuses B. Nasal fracture C. Exopthalmos D. Extra-sinus air - A. Fluid (blood) in the sinuses The answer is A. Blood in the sinuses can be a useful indirect indicator of facial fracture. A 41 year old man is seen in the emergency department after a street fight where he punched another man in the mouth. He has a small, jagged laceration over the dorsum of the metacarpophalangeal joint of his right hand. The wound is irrigated copiously, tetanus is given, and the wound is left open to heal by secondary intention because of the infection risk. In addition to treating Streptococcus and Staphylococcus species, antibiotics must also treat which other bacterial species? A. Escherichia. coli B. Actinomyces israelii C. Eikenella corrodens D. Pasteurella multocida - C. Eikenella corrodens The answer is C. There are many species of bacteria in the human mouth, and Eikenella corrodens is an aggressive one, frequently causing infection in the first 24 hours after injury. A young male patient presented to the emergency department with a history of single gunshot wound from unknown source and caliber. He was hemodynamically stable and had little pain in the right lower quadrant of the abdomen, which was the site of two wounds about 6 inches apart (see Figure). No other wounds were identified during physical examination. Which of the following statements regarding this case is true? [image] A. The superior-medial wound (at the top right of the Figure) is likely the entrance wound, and the inferior-lateral wound is likely the exit wound, of a single missile B. If it is suspected that the two wounds are from the same missile, the emergency department physician's documentation should note which wound is the entrance, and which is the exit C. Wound description is essential for the emergency medicine specialist. However, description of a wound as to entrance or exit is best left to forensic examination. D. The two wounds are more likely than not the result of two separate missiles - C. Wound description is essential for the emergency medicine specialist. However, description of a wound as to entrance or exit is best left to forensic examination. The answer is C. The overall evidence points to a superior-medial to inferior-lateral wound trajectory, with subcutaneous ecchymosis indicating the missile track and the more ragged wound at the inferior-lateral (groin) region most likely an exit wound. However, though wound description is very important for the emergency physician (both as a guide to injury evaluation and also as an early characterization of wounds, before interventions such as wound exploration obscure physical findings), speculation as to whether wounds are entrance or exit wounds are best left off of the E.D. record. Clinicians tend to oversimplify and/or misinterpret physical wound characteristics. Thus, the best course is a meticulous description (or photograph) of the wound, noting items such as tattooing (i.e. of gunpowder) or stellate tissue destruction (which can be due to expansion of gun barrel gases in a contact wound) but leaving interpretation of the physical evidence to forensics experts. The wound characteristics are not consistent with self-inflicted injury, though the ED physician should have a low index of suspicion for psychiatric consultation when there is doubt on this subject. A patient presents to the ED after a fall with chest pain. A chest xray shows a rib fracture but no pneumothorax, and a chest CT is ordered. What is the most appropriate treatment for a small pneumothorax, detected only on chest CT, in a hemodynamically stable trauma patient? A. 100% oxygen B. Heliox by face mask C. Immediate needle decompression D. Chest tube placement - A. 100% oxygen The answer is A. An occult pneumothorax may resorb with only oxygen administration, not requiring invasive management. Needle decompression is used for tension pneumothorax, and heliox may be used for reactive airway disease to reduce resistance to flow. You are practicing in a trauma center a receive a call from an outlying facility that they would like to transfer a male patient to you with a spinal cord injury after significant flexion and compression of the vertebral body. What does this injury pattern tell you about the patient's symptoms? [image] Figure used with permission from Hamilton et al, Emergency Medicine: An approach to clinical problem-solving A. The patient likely has symptoms on only one side of the his body B. Patients with anterior cord syndromes have only sensory symptoms C. The patient likely disproportionately greater weakness in the lower extremities (as compared to the upper extremities) D. The patient likely has paralysis and loss of sensation to pain and temperature bilaterally below the lesion - D. The patient likely has paralysis and loss of sensation to pain and temperature bilaterally below the lesion The answer is D. Answer A describes central cord syndrome, typically caused by hyperextension. Answer C describes Brown-Sequard Syndrome, caused by hemisection of the cord. Answer B is anterior cord, often caused by flexion and injury to the anterior spinal artery; patient with this cord syndrome often have more than just sensory symptoms. A trauma patient resuscitated in the ED, has a post-tube thoracostomy computed tomography (CT) scan as depicted in the figure. What finding is present? [image] A. Pericardial tamponade B. Aortic rupture leading to a right hemothorax C. Chest tube not within the thoracic cavity D. Persistent pneumothorax - D. Persistent pneumothorax The answer is D. The chest CT shows a chest tube in place on the right, with incomplete reinflation of the lung. The left hemithorax is grossly normal, but there is a large right pulmonary contusion, as well as pneumothorax and small hemothorax on the right. The aorta appears intact (aortic injuries usually leak into the left hemithorax, not the right). In differentiating high voltage electrical injury from lightning injury, which of the following is your best discriminator? A. Deep burns B. Fractures or dislocations C. Loss of consciousness D. Cardiac arrest - A. Deep burns The answer is A. Patients with high voltage injury commonly present with devastating burns. The burns are most severe at the source and ground contact points. The most common sites of contact with the source include the hands and the skull. The most common areas of ground contact are the heels. Deep burns occur in less than 5% of lightning injuries. Electrical injuries may cause four types of superficial burns or skin changes: linear burns, punctate burns, feathering, or thermal burns. Loss of consciousness, cardiac arrest and orthopedic injuries can be seen in both high voltage electrical injury and lightning injury. Electrolyte abnormalities are not common in either injury. Using the rule of 9s, what is the approximate burn surface area of a victim who has sustained second-degree burns to the anterior chest and anterior area of both arms? A. 20% B. 25% C. 30% D. 35% - B. 25% A right-handed patient sustains a circumferential burn (see figure) to the distal right forearm and hand, which is cool despite warm ambient temperature. Regarding the initial assessment and management of the patient, which of the following is correct? [image] A. As shown in the Figure, the burn represents about 10% of total body surface area B. Pain medication should be withheld pending obtaining operative consent for emergency burn debridement C. Prophylactic penicillin should be given to any patient with a significant burn D. The involved areas of this 3rd-degree burn would be expected to be mostly insensate - D. The involved areas of this 3rd-degree burn would be expected to be mostly insensate [Show More]
Last updated: 1 year ago
Preview 1 out of 178 pages
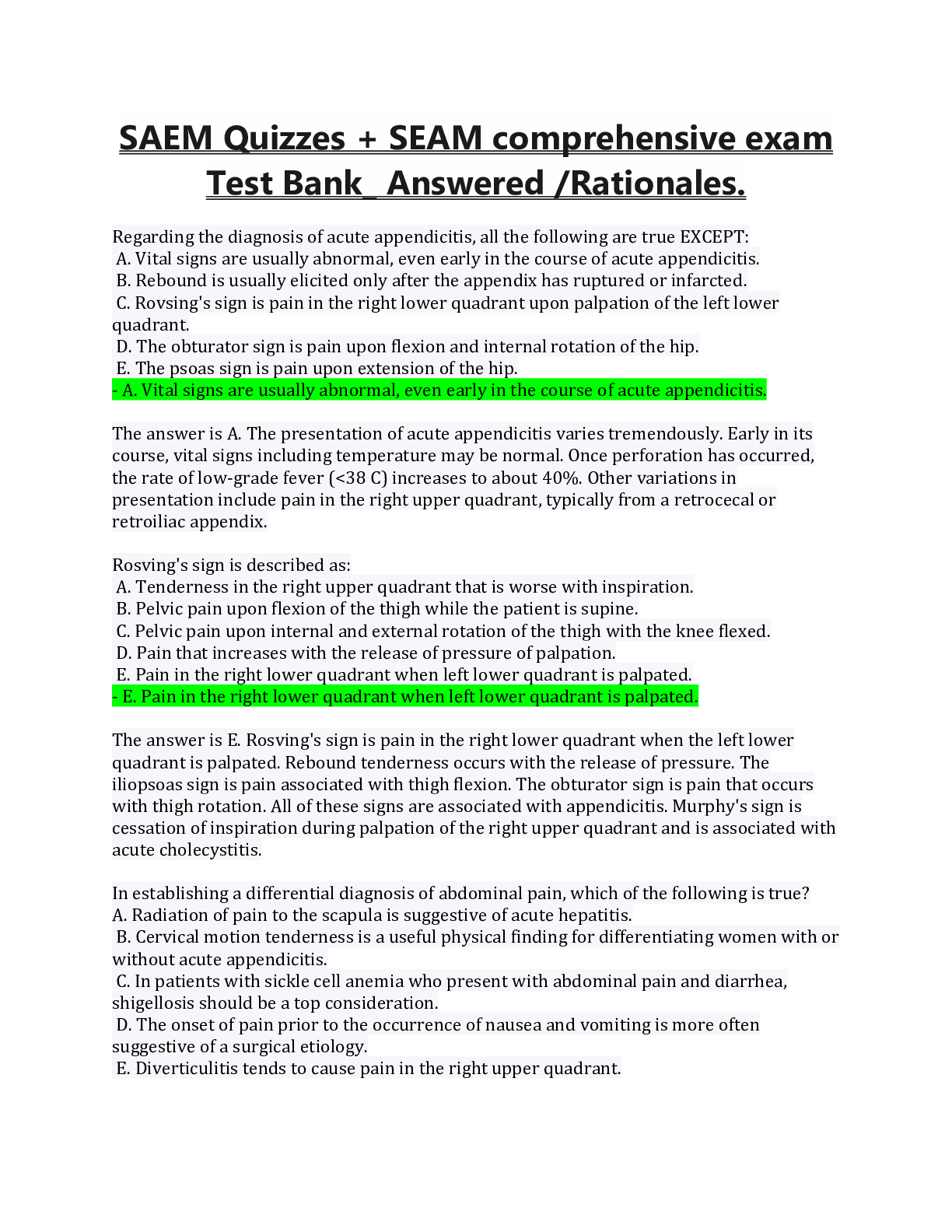
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 18, 2022
Number of pages
178
Written in
Additional information
This document has been written for:
Uploaded
Apr 18, 2022
Downloads
1
Views
172

.png)
.png)