*NURSING > SHADOW HEALTH > Comprehensive Assessment _ Completed _ Shadow Health Latest Updated, Graded A (All)
Comprehensive Assessment _ Completed _ Shadow Health Latest Updated, Graded A
Document Content and Description Below
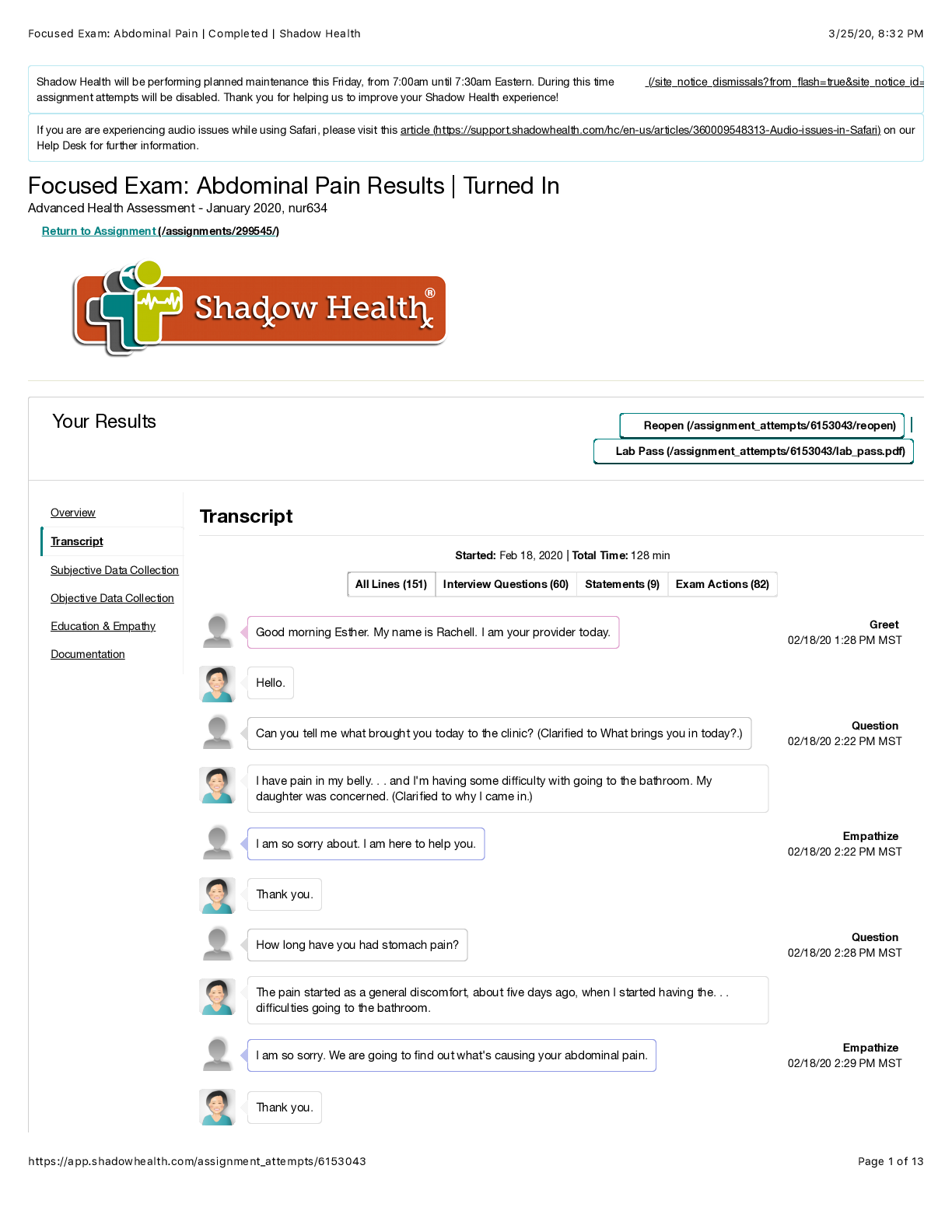
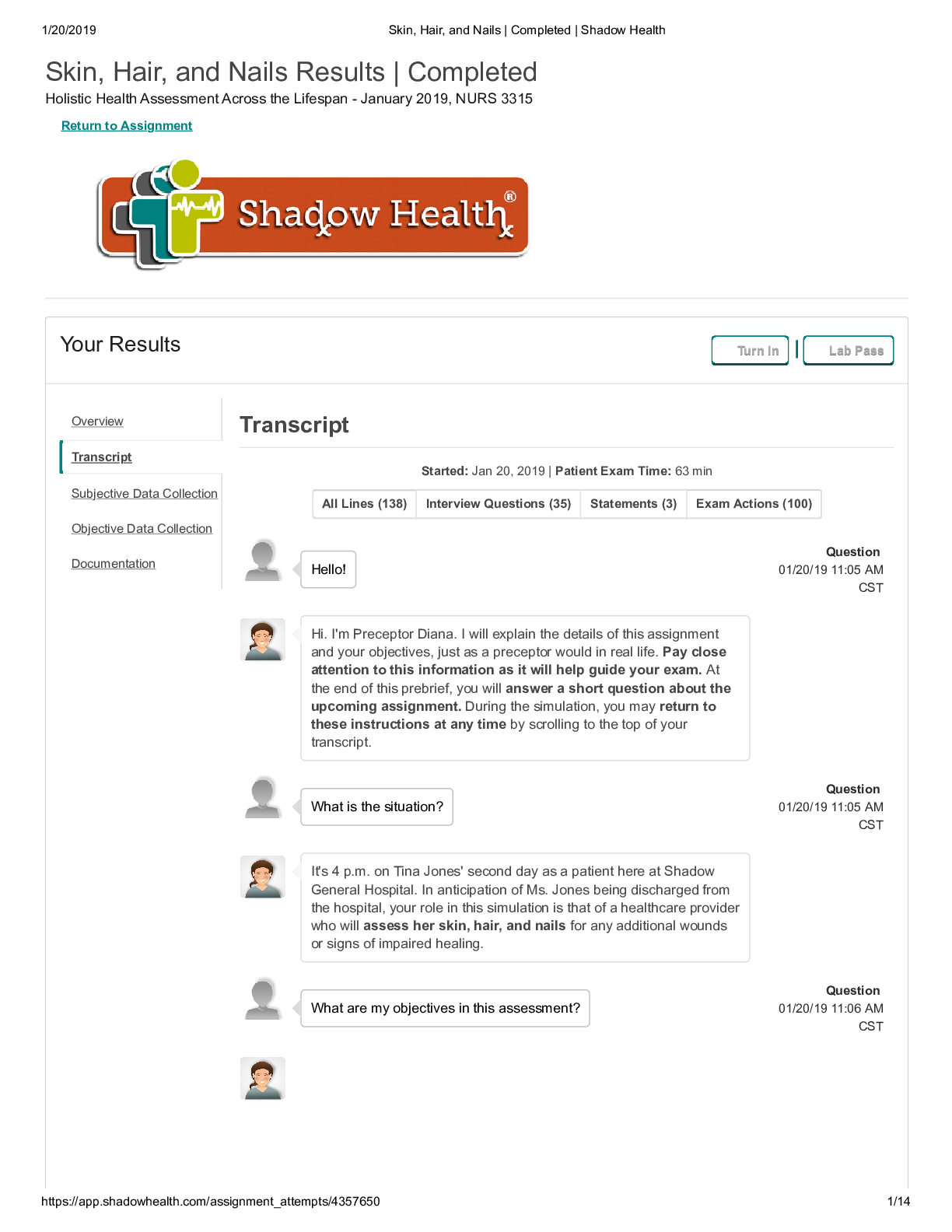
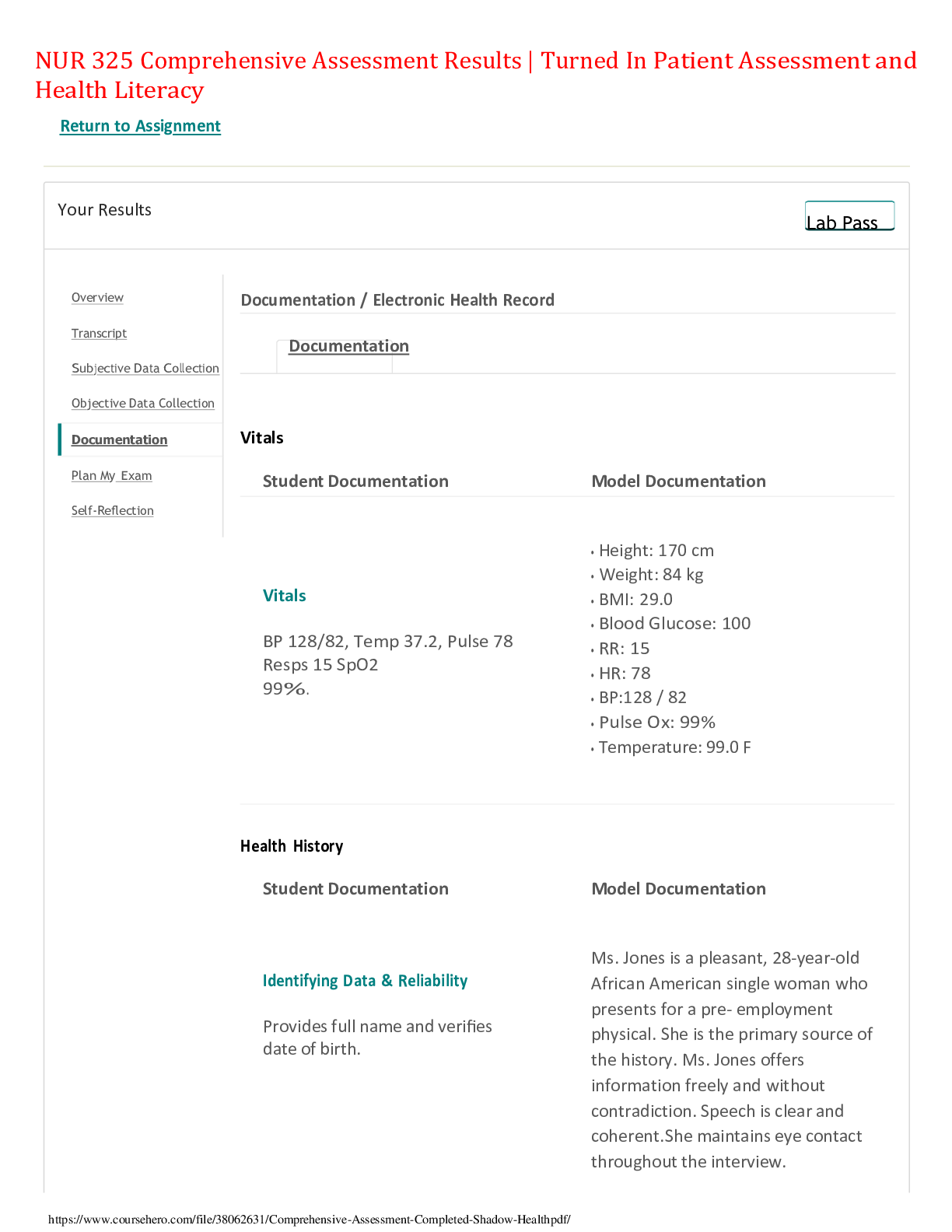
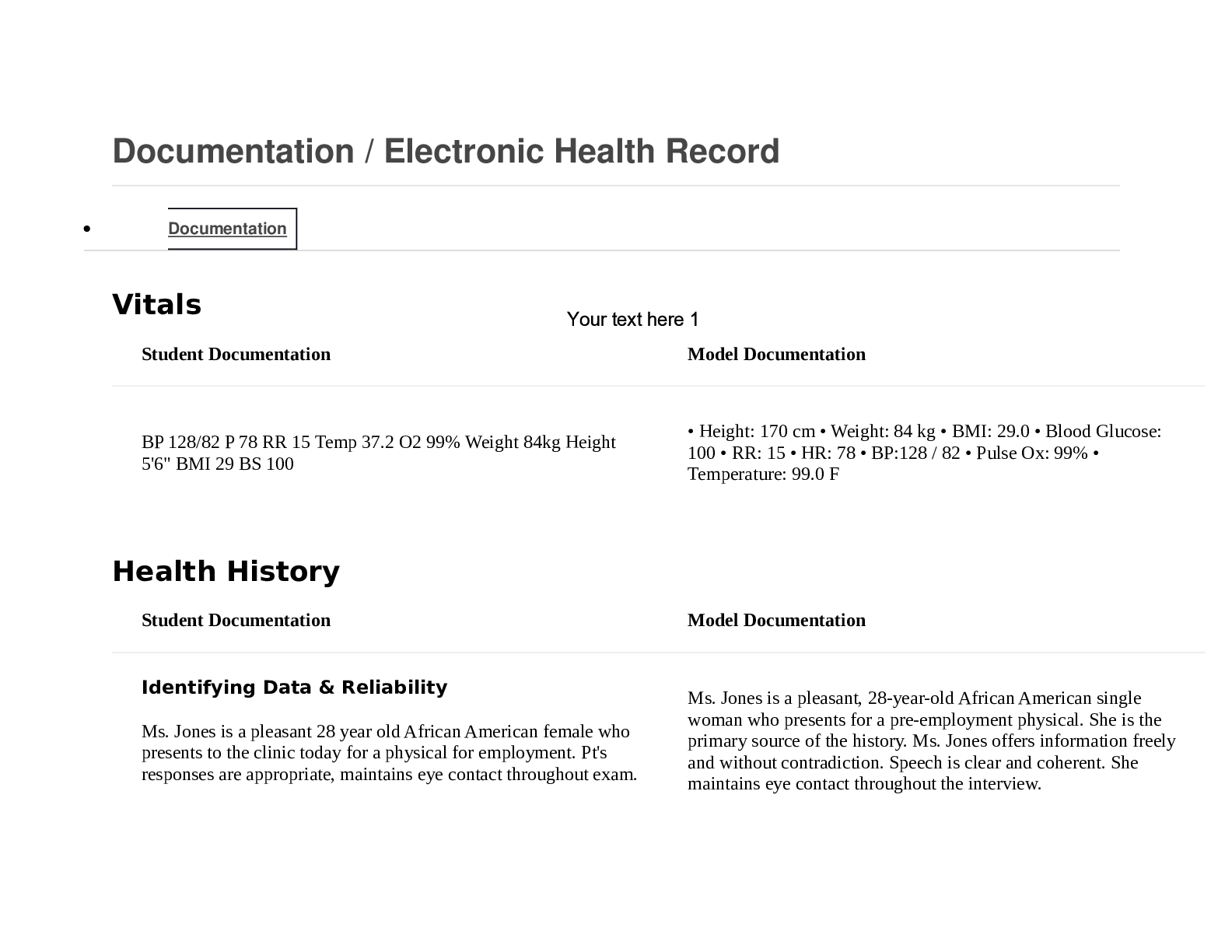
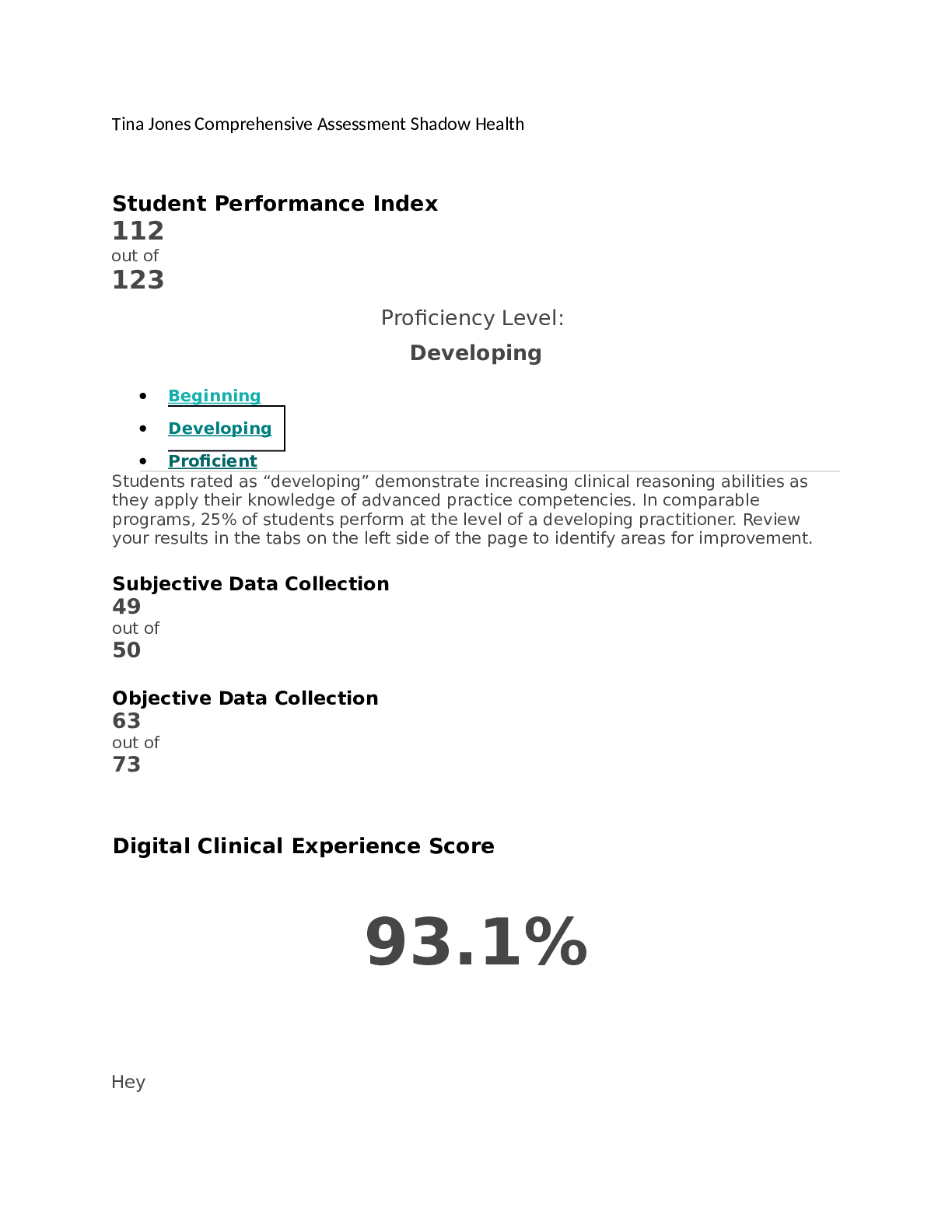
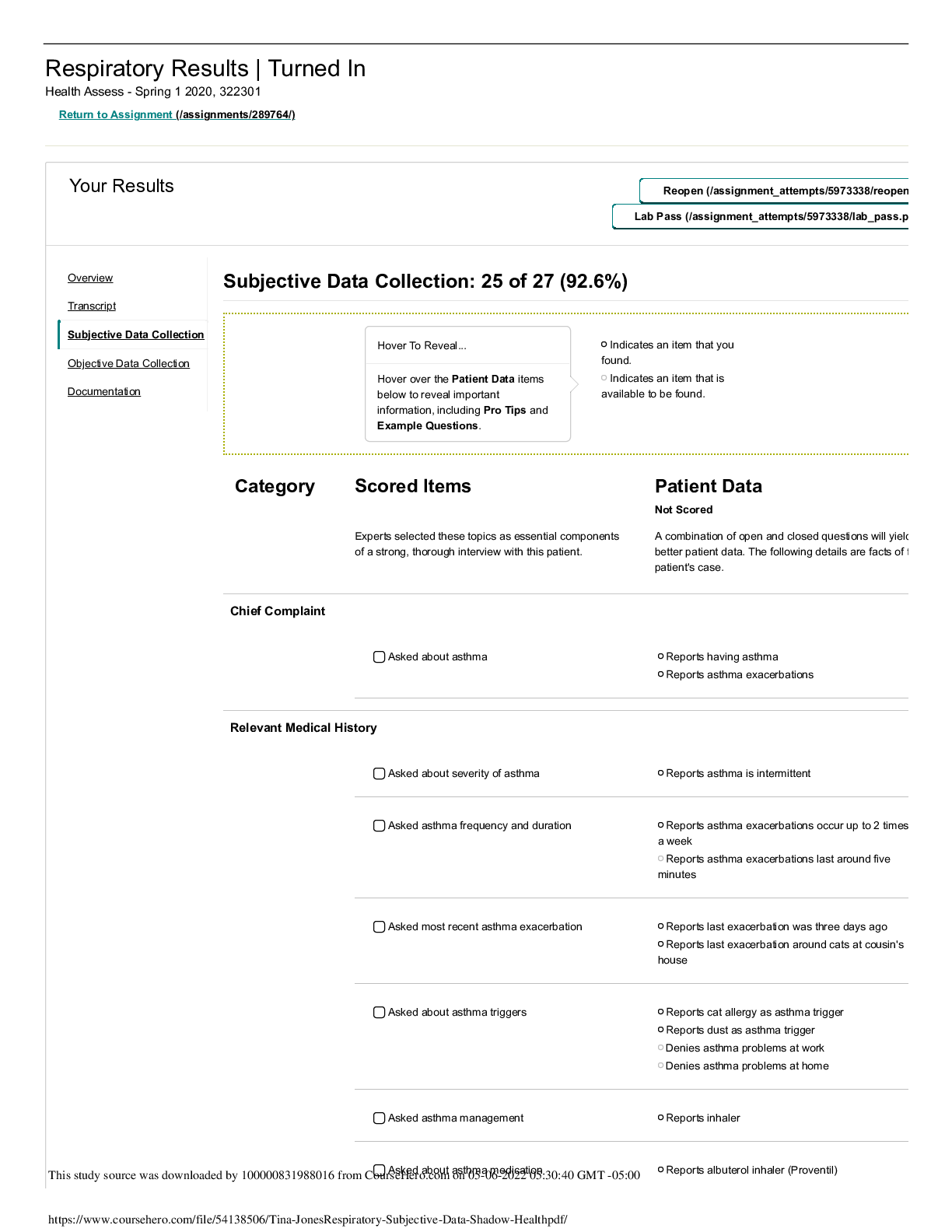
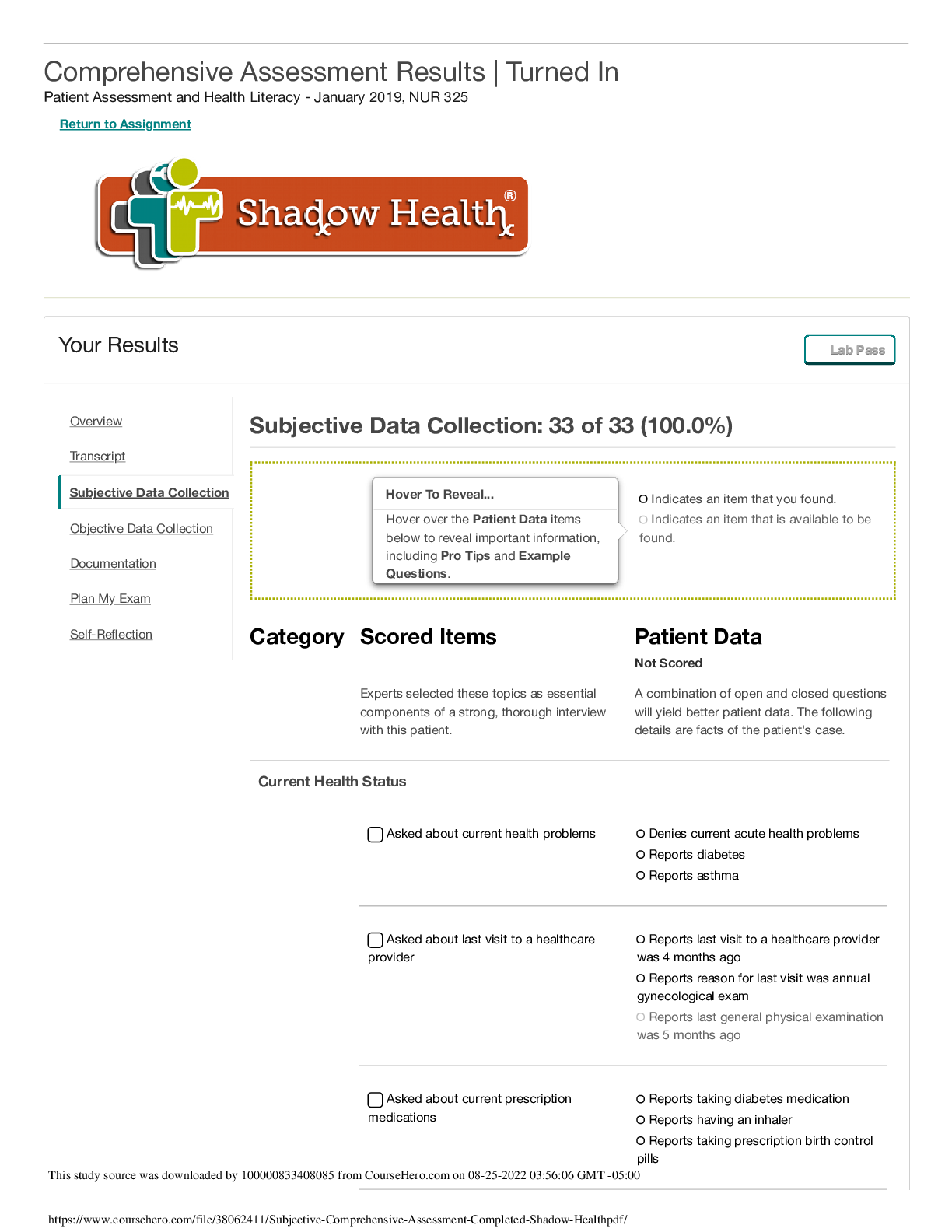
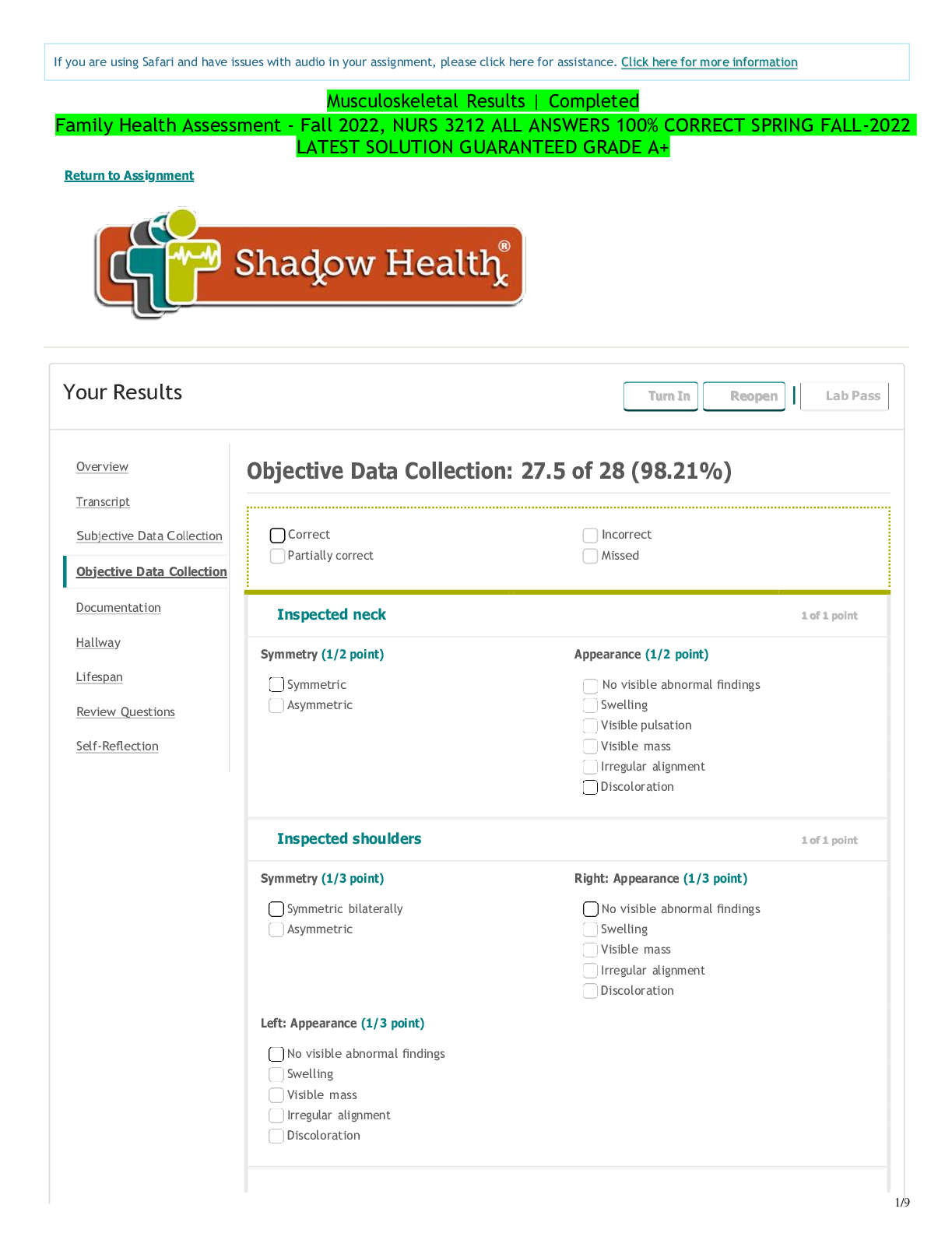
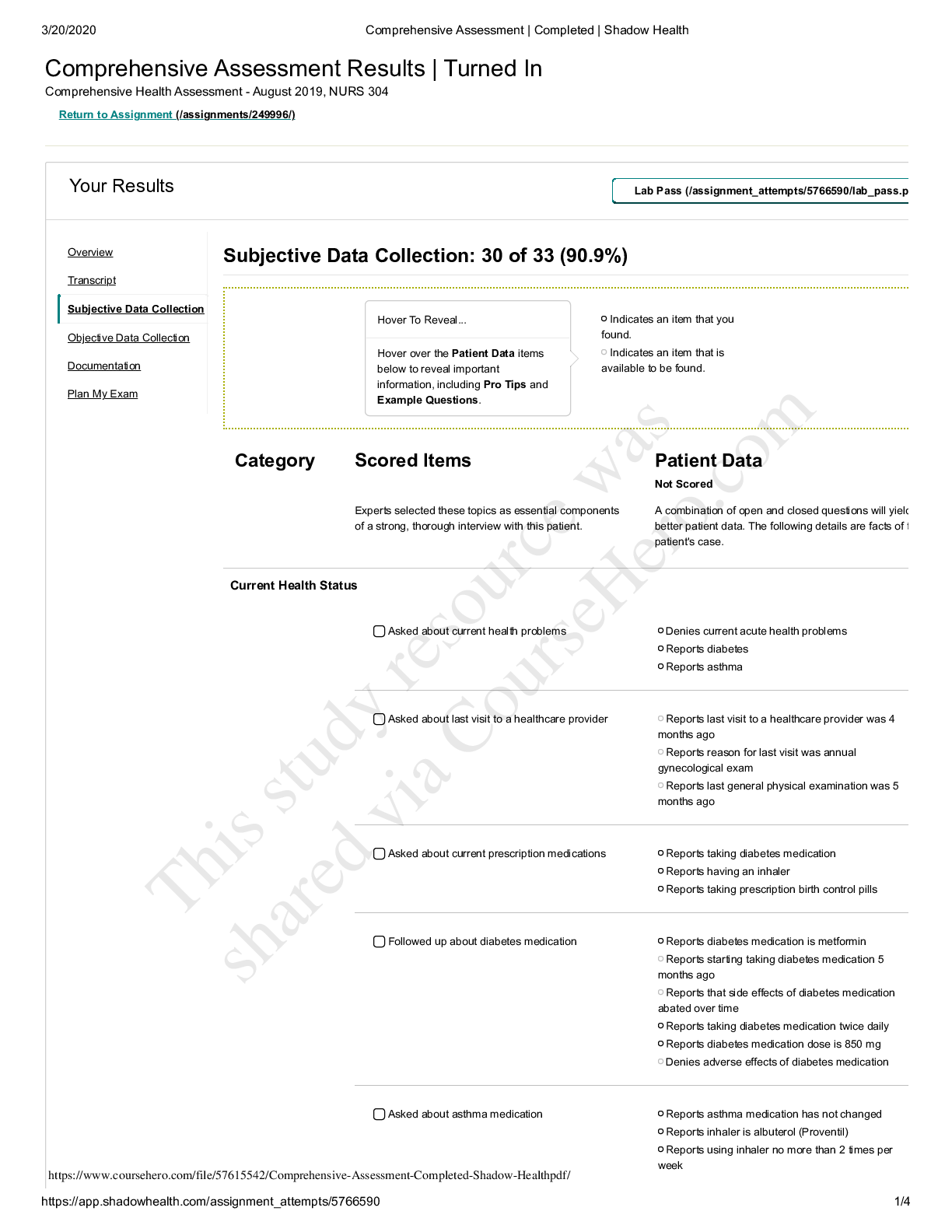
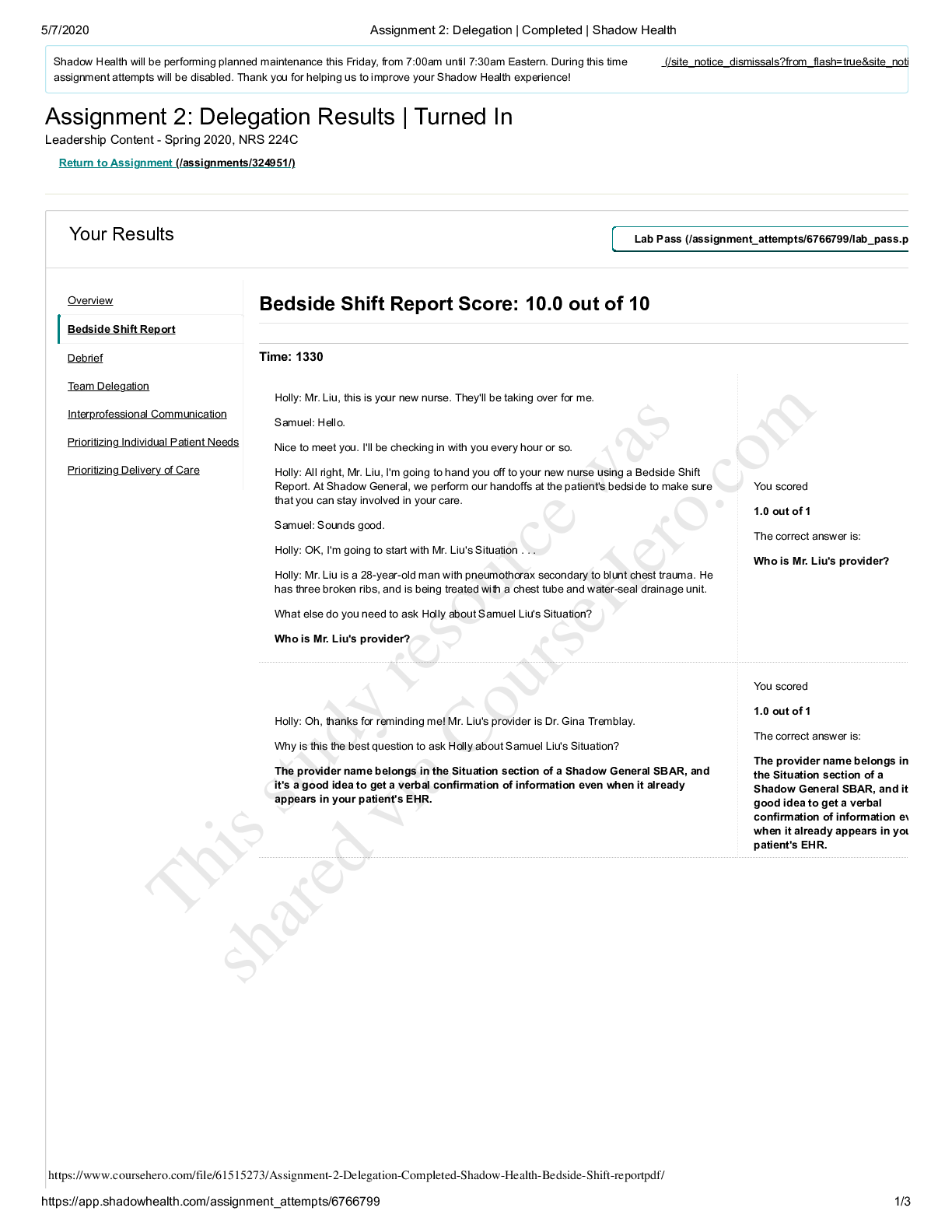
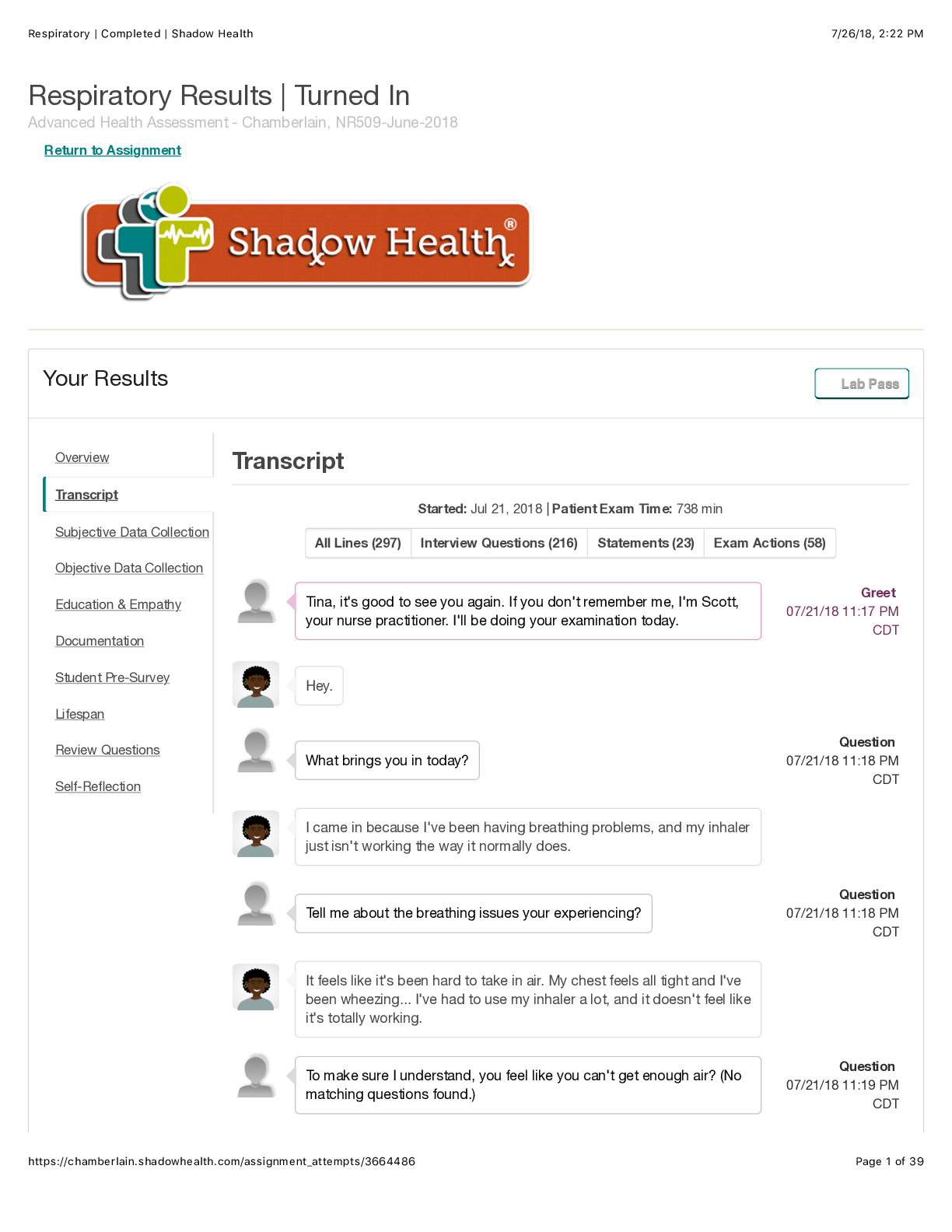
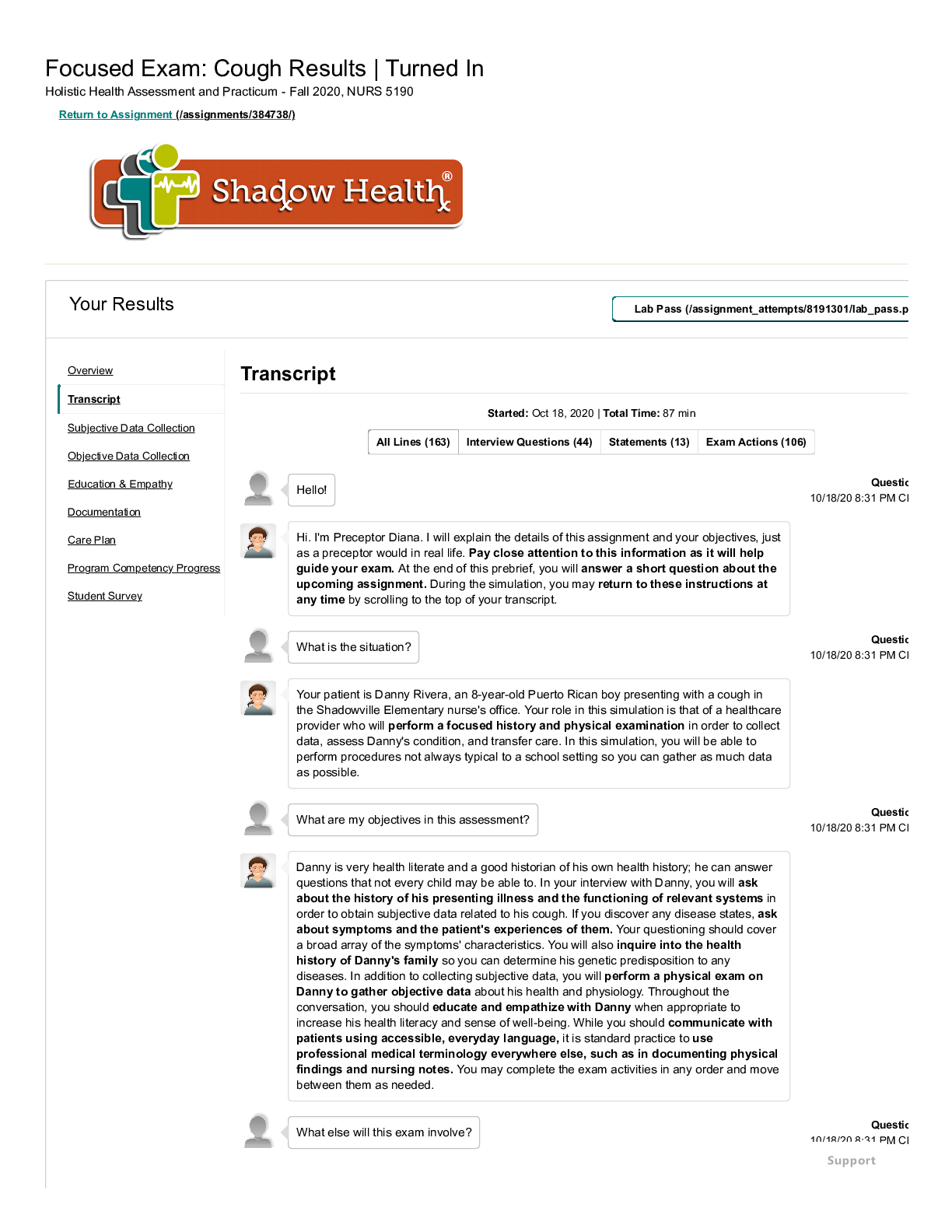
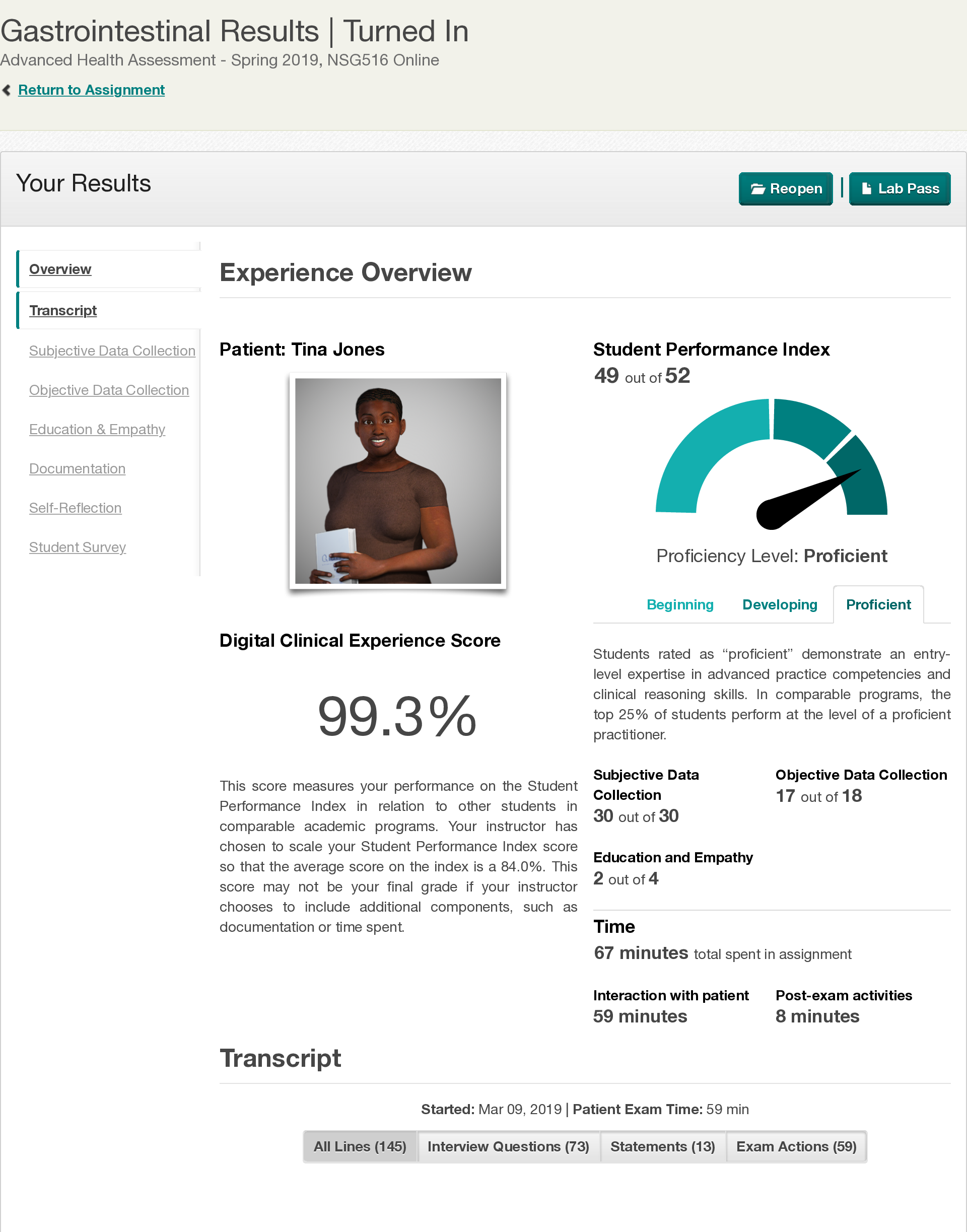
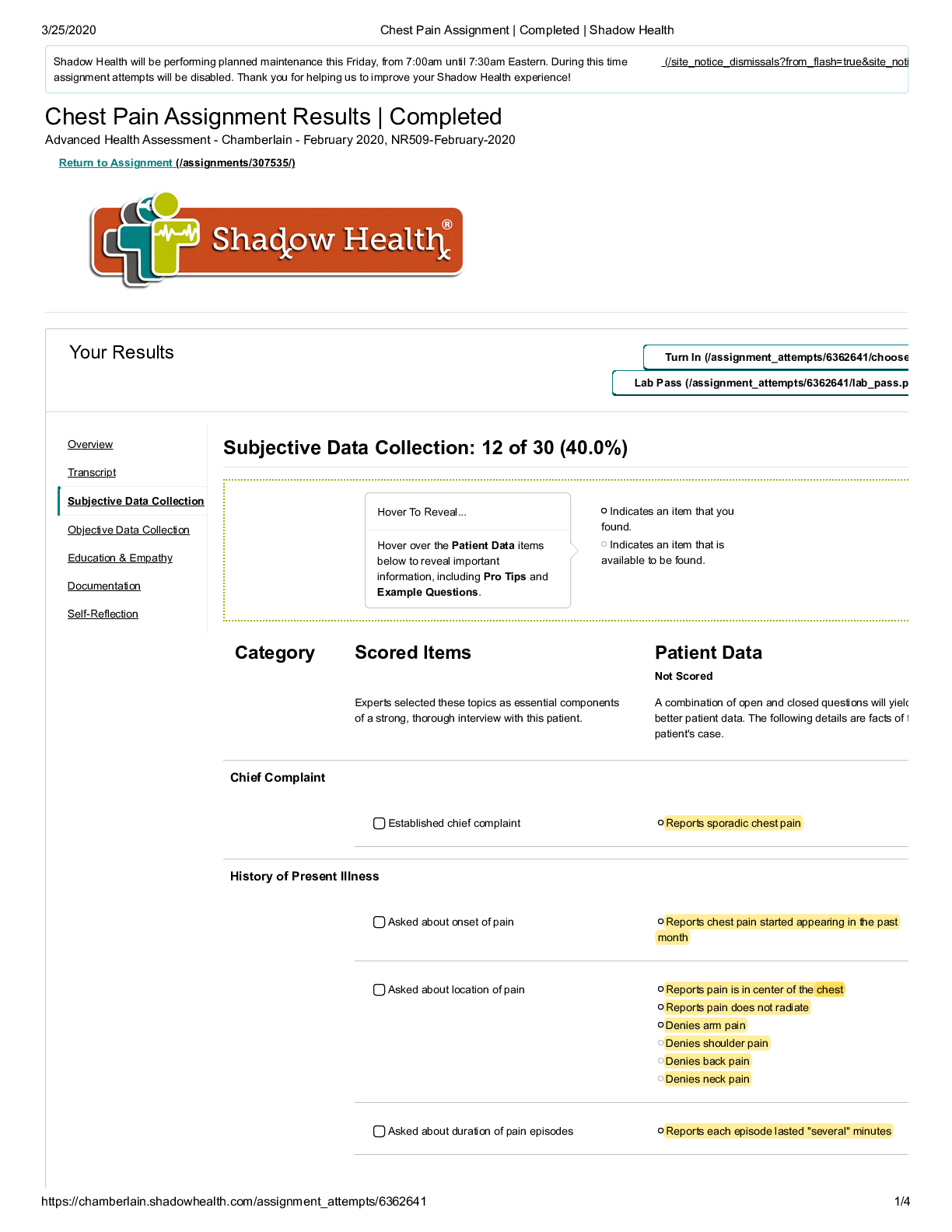
Comprehensive Assessment Results | Turned In Patient Assessment and Health Literacy - January 2019, NUR 325 Return to Assignment Your Results LLaabb PPaassss Documentation Vitals Student Documen... tation Model Documentation Vitals BP 128/82, Temp 37.2, Pulse 78 Resps 15 SpO2 99%. • Height: 170 cm • Weight: 84 kg • BMI: 29.0 • Blood Glucose: 100 • RR: 15 • HR: 78 • BP:128 / 82 • Pulse Ox: 99% • Temperature: 99.0 F Health History Student Documentation Model Documentation Identifying Data & Reliability Provides full name and verifies date of birth. Ms. Jones is a pleasant, 28-year-old African American single woman who presents for a preemployment physical. She is the primary source of the history. Ms. Jones offers information freely and without contradiction. Speech is clear and coherent. She maintains eye contact throughout the interview. General Survey Ms. Jones is a pleasant, well-groomed 28 year old AFrican American female wearing glasses to correct nearsightedness, Ms. Jones is alert and oriented, seated upright on the examination table, and is in no apparent distress. She is well-nourished, well-developed, and dressed appropriately with good hygiene. Reason for Visit Ms. Jones presents to clinic today for a preemployment physical. "I came in because I'm required to have a recent physical exam for the health insurance at my new job." Overview Transcript Subjective Data Collection Objective Data Collection Documentation Plan My Exam Self-Reflection Documentation / Electronic Health Record This study source was downloaded by 100000831988016 from CourseHero.com on 04-27-2022 04:58:01 GMT -05:00 https://www.coursehero.com/file/38062631/Comprehensive-Assessment-Completed-Shadow-Healthpdf/ Student Documentation Model Documentation History of Present Illness REports no current health issues. Hx of Asthma (Albuterol); Diabetes (Metformin) and Polycystic Ovaria Syndrome (Yaz). Patient rates current health at an 8/10. Ms. Jones reports that she recently obtained employment at Smith, Stevens, Stewart, Silver & Company. She needs to obtain a pre-employment physical prior to initiating employment. Today she denies any acute concerns. Her last healthcare visit was 4 months ago, when she received her annual gynecological exam at Shadow Health General Clinic. Ms. Jones states that the gynecologist diagnosed her with polycystic ovarian syndrome and prescribed oral contraceptives at that visit, which she is tolerating well. She has type 2 diabetes, which she is controlling with diet, exercise, and metformin, which she just started 5 months ago. She has no medication side effects at this time. She states that she feels healthy, is taking better care of herself than in the past, and is looking forward to beginning the new job. Medications Metformin 850 mg PO BID; Albuterol number of mcg not available on visit; 2-3 puffs INH PRN / asthma; Yaz 1 tab PO daily. Advil OTC 200 mg PO PRN • Metformin, 850 mg PO BID (last use: this morning) • Drospirenone and ethinyl estradiol PO QD (last use: this morning) • Albuterol 90 mcg/spray MDI 1-3 puffs Q4H prn (last use: yesterday) • Acetaminophen 500-1000 mg PO prn (headaches) • Ibuprofen 600 mg PO TID prn (menstrual cramps: last taken 6 weeks ago) Allergies PCN, pediatric onset, rash / urticaria. CAts; asthma exacerbator, runny nose. • Penicillin: rash • Denies food and latex allergies • Allergic to cats and dust. When she is exposed to allergens she states that she has runny nose, itchy and swollen eyes, and increased asthma symptoms. This study source was downloaded by 100000831988016 from CourseHero.com on 04-27-2022 04:58:01 GMT -05:00 https://www.coursehero.com/file/38062631/Comprehensive-Assessment-Completed-Shadow-Healthpdf/ Student Documentation Model Documentation Medical History Dx asthma as a child; triggers exertion and cats. NIDDM treated with Metformin 850 mg PO BID, FBS consistently around 90. Diagnosed with PCOS 4 months ago, Tx with Yaz; regular menses since beginning Yaz, patient reports decrease in hirsutism. Inpatient stay for infected right foot wound 6 months ago, patient denies concerns presently. DEnies surgical history. Reports No pregnancies. Asthma diagnosed at age 2 1/2. She uses her albuterol inhaler when she experiences exacerbations, such as around dust or cats. Her last asthma exacerbation was yesterday, which she resolved with her inhaler. She was last hospitalized for asthma in high school. Never intubated. Type 2 diabetes, diagnosed at age 24. She began metformin 5 months ago and initially had some gastrointestinal side effects which have since dissipated. She monitors her blood sugar once daily in the morning with average readings being around 90. She has a history of hypertension which normalized when she initiated diet and exercise. No surgeries. OB/GYN: Menarche, age 11. First sexual encounter at age 18, sex with men, identifies as heterosexual. Never pregnant. Last menstrual period 2 weeks ago. Diagnosed with PCOS four months ago. For the past four months (after initiating Yaz) cycles regular (every 4 weeks) with moderate bleeding lasting 5 days. Has new male relationship, sexual contact not initiated. She plans to use condoms with sexual activity. Tested negative for HIV/AIDS and STIs four months ago. Health Maintenance Compliant with medication regime, reporting consistent use and consistent time of day. REcent intentional loss of 10 pounds, patient credits lifestyle changes of diet and exercise. Patient exercises 30-40 minutes / day, 4-5 x / week, eats balanced diet and snacks. Monitors blood glucose q AM, reports results typically around 90. Last Pap smear 4 months ago. Last eye exam three months ago. Last dental exam five months ago. PPD (negative) ~2 years ago. Immunizations: Tetanus booster was received within the past year, influenza is not current, and human papillomavirus has been received. She reports that she believes she is up to date on childhood vaccines and received the meningococcal vaccine for college. Safety: Has smoke detectors in the home, wears seatbelt in car, and does not ride a bike. Uses sunscreen. Guns, having belonged to her dad, are in the home, locked in parent’s room. Family History Father- deceased, MVA. Hx Diabetes Mother, alive, HTN. Paternal Grandfather, deceased Colon cancer, age 60s; Hx HTN, Diabetes. Maternal grandfather: Deceased MI (80 years) HTN, hyperlipidemia. Grandmother Deceased, CVA, HTN. Sister-Asthma • Mother: age 50, hypertension, elevated cholesterol • Father: deceased in car accident one year ago at age 58, hypertension, high cholesterol, and type 2 diabetes • Brother (Michael, 25): overweight • Sister (Britney, 14): asthma • Maternal grandmother: died at age 73 of a stroke, history of hypertension, high cholesterol • Maternal grandfather: died at age 78 of a stroke, history of hypertension, high cholesterol • Paternal grandmother: still living, age 82, hypertension • Paternal grandfather: died at age 65 of colon cancer, history of type 2 diabetes • Paternal uncle: alcoholism • Negative for mental illness, other cancers, sudden death, kidney disease, sickle cell anemia, thyroid problems This study source was downloaded by 100000831988016 from CourseHero.com on 04-27-2022 04:58:01 GMT -05:00 https://www.coursehero.com/file/38062631/Comprehensive-Assessment-Completed-Shadow-Healthpdf/ Student Documentation Model Documentation Social History Denies tobacco, nicotine or recreational substance ues. Reports ETOH intake of 2-3 drinks "a couple of times per month." Currently resides with mother and sister, but is moving into her own apartment in one month. Reports new relationship, not yet sexual but patient reports that she anticipates it will become [Show More]
Last updated: 1 year ago
Preview 1 out of 8 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 27, 2022
Number of pages
8
Written in
Additional information
This document has been written for:
Uploaded
Apr 27, 2022
Downloads
0
Views
101

.png)
.png)

 LATEST QUESTIONS AND COMPLETE SOLUTIONS.png)