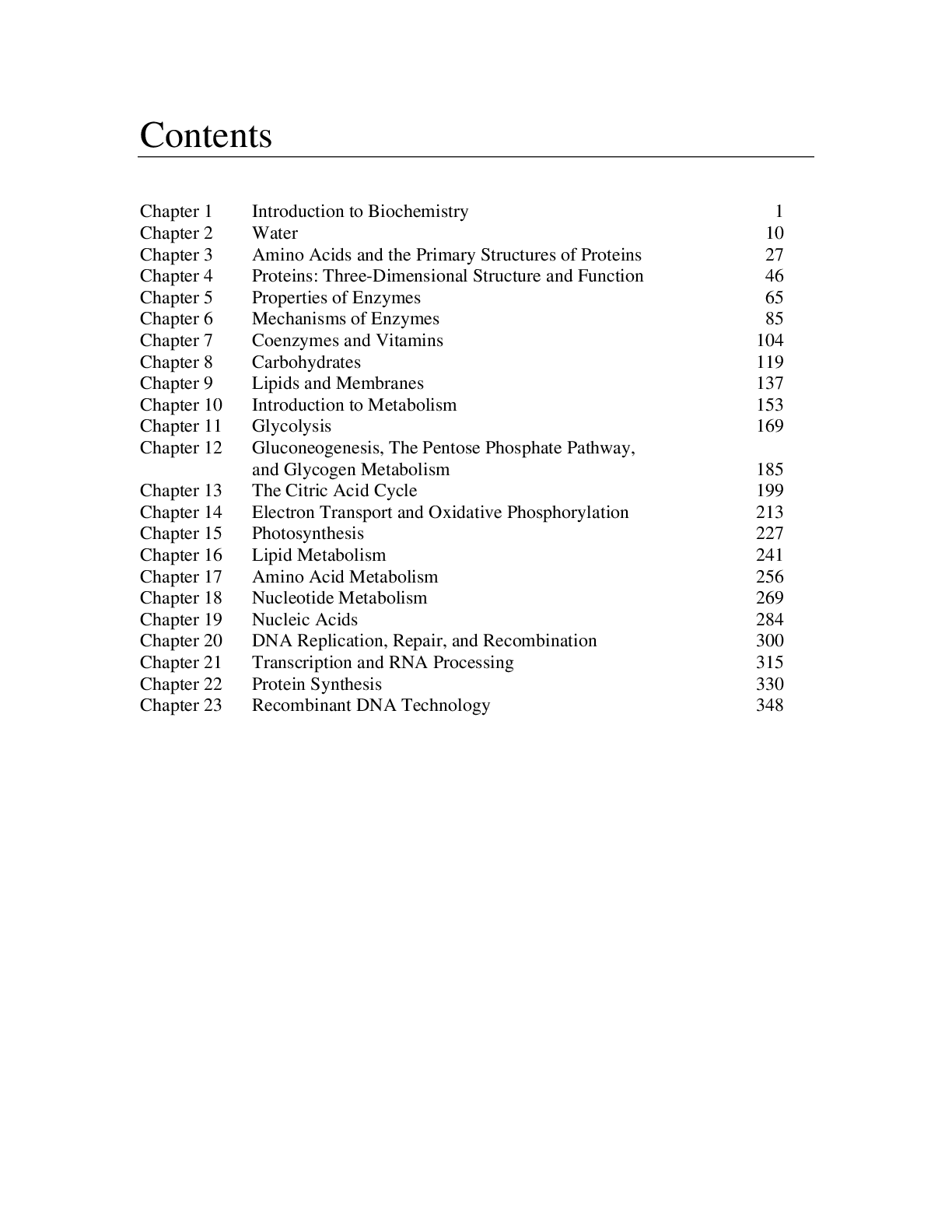
*NURSING > EXAM > Final Exam Blueprint ALL ANSWERS 100% CORRECT SPRING FALL-2022 SOLUTION GUARANTEED GRADE A+ (All)
Final Exam Blueprint ALL ANSWERS 100% CORRECT SPRING FALL-2022 SOLUTION GUARANTEED GRADE A+
Document Content and Description Below
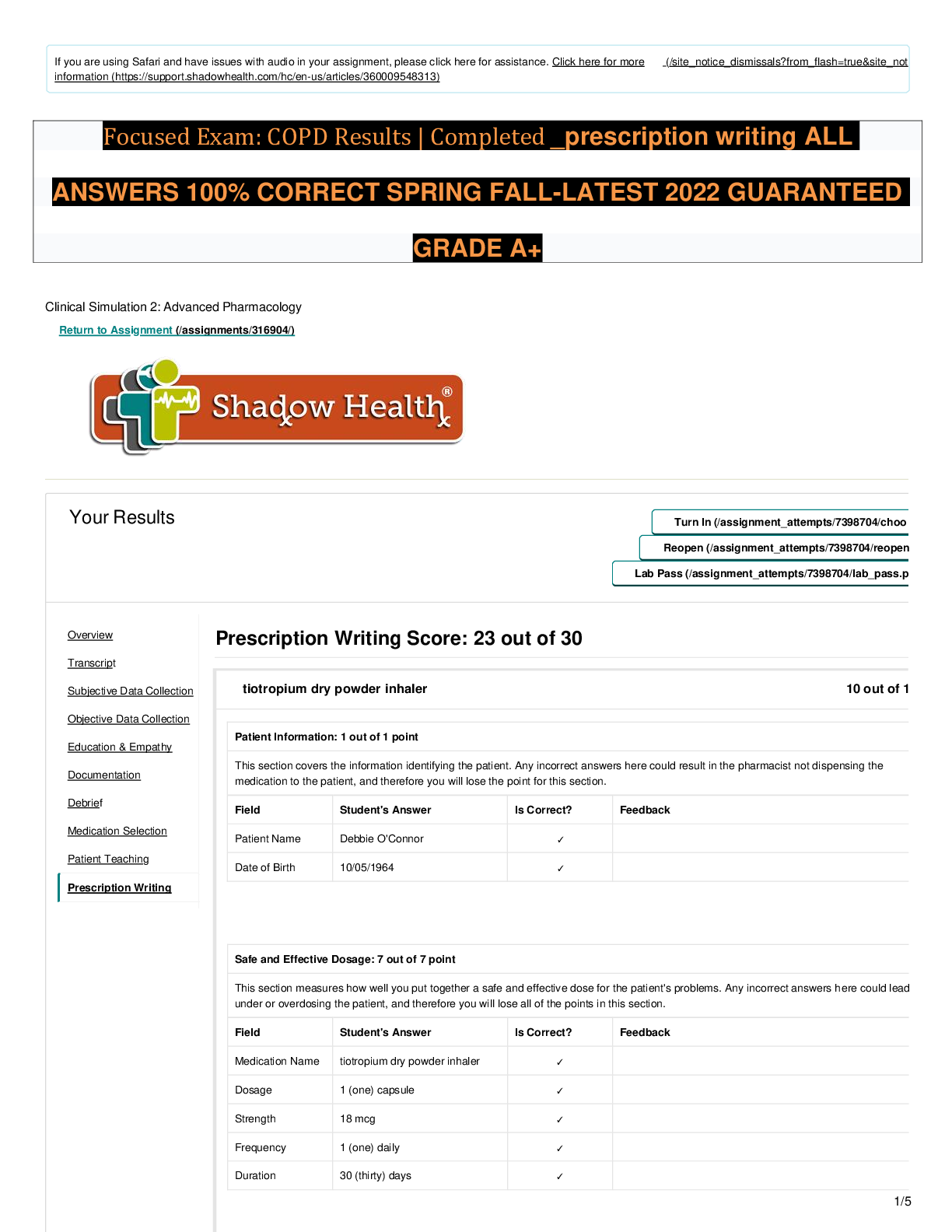
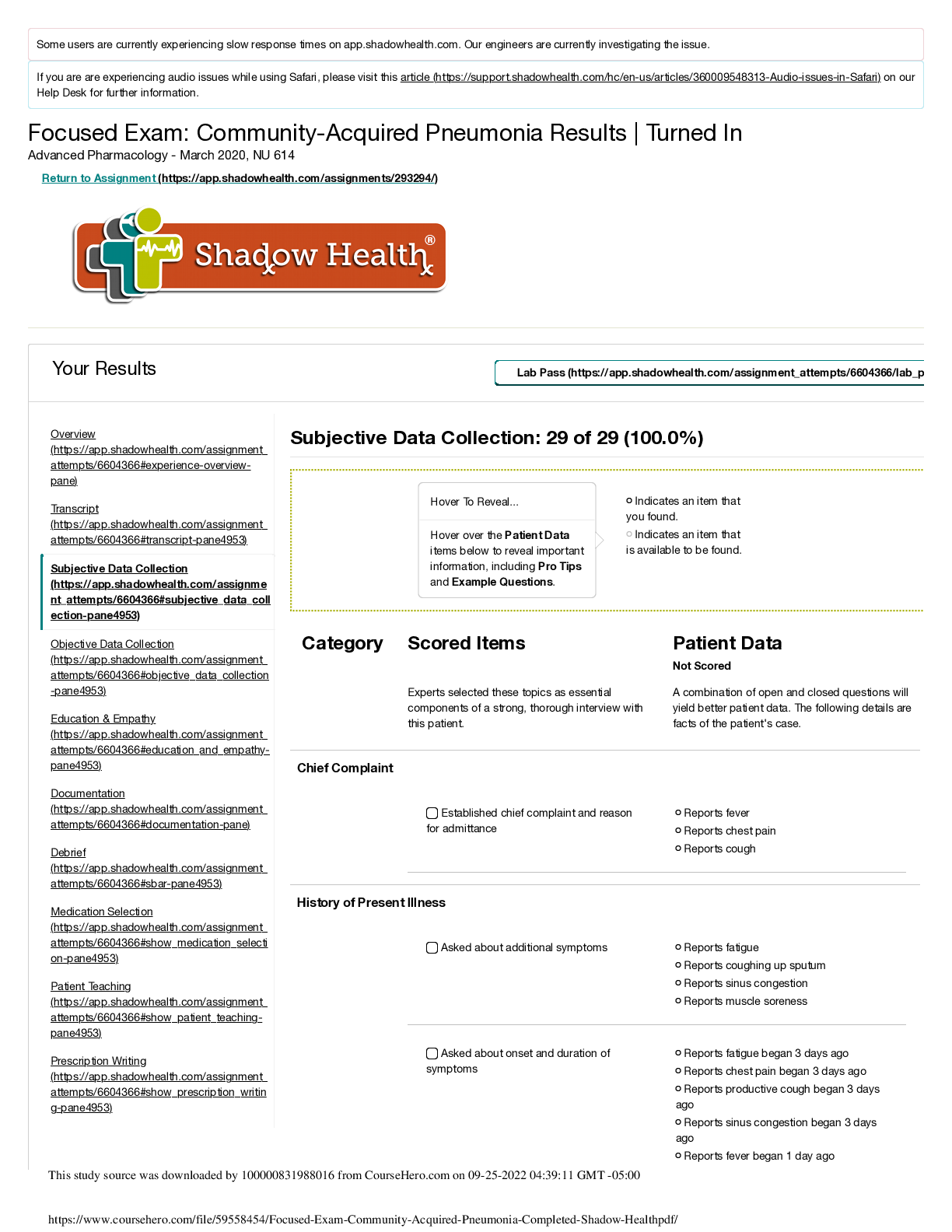
Prescribing Basics: 2 questions Prescriptive authority regulated by the state BON in each state. Tall man lettering to highlight dissimilaries with look-alike names *Prescription contains… Physici... ans Name, Address, and telephone number are required to be included in the prescription. DEA number (two letters, five numbers) if the prescription is for controlled substance, Patient name and DOB (also may include address and weight), Date Rx is written (expires 1 year after date issued), Name of drug and strength- avoid trailing zeroes, use leading zeroes, Directions with indications/route of administration and frequency, write out number of refills, quantity of drug, signature, NPI number (9 or 11 numbers), sign as A-PNP or role recognized by the BON Drug schedules – one is most addictive, up to schedule 5. 1) heroin, LSD, marijuana. 2) oxycodone, hydrocodone, methamphetamines. 3) codeine, ketamine, testosterone. 4) Xanax, valium, ambien, tramadol. 5) antidiarrheal, antitussives, Lomotil, lyrica. *calculation question Pharmacology Principles: 3 questions Pharmacodynamics – effect of drugs on body. Works by receptors. Usually proteins that interact with drugs. Agonist – produce receptor stimulation, conformational change every time they bind. Partial agonist – properties between agonists and antagonists. Submaximal effect. Stimulate only some of the receptors. Antagonist – affinity for receptor but NO intrinsic activity. Affinity allows antagonist to bind to receptors, but lack of intrinsic activity prevents receptor activation. Blocks action of drugs (example Narcan). Therapeutic range – between minimum effective concentration and toxic concentration. Working effectivity with no toxicity or adverse effects. Wider therapeutic range is better! Easiest to control. Bioavailability – percentage of dose of drug that survives first pass through liver and reaches blood stream. Half life – time required for amount of drug to decline by 50%. Shorter half life admin more frequently. 4.5-5 half lives to get to steady state and to eliminate from body. Pharmacokinetics – what body does to drug. Absorption, distribution, metabolism, elimination. (ADME) Parenteral (bypass first pass), then oral, then lungs, then skin, eye and ears for best absorption. Distribution affected by lipid/water solubility, PH, protein binding, size of molecule. Protein binding – unbound drug is free drug which is active. When 2 highly bound drugs are given it increases the level of one of the drugs, leading to toxicity. IE warfarin and phenytoin are both highly protein bound. Low plasma protein result in more free drug. May be in elderly, so decrease dose of medication. T3 and T4 both highly protein bound. 1% of drug is powerful. Distribution – BBB (only lipid soluble will pass) – these such as narcotics, only work because they do cross BBB. Some meds we do not want to pass. Placental barrier (many drugs can pass) so be careful with drugs in pregnancy. Metabolism – liver. Chemical change of a drug structure to enhance excretion, inactivate drug, increase therapeutic action, activate prodrug, increase or decrease toxicity. Substrate – agent that is metabolized by an enzyme into a metabolite and product and eventually excreted. *Inhibitors – compete with other drugs for a particular enzyme affecting the metabolism (decreases) of the substrate and decreases the excretion of the substrate and increasing the circulating drug. Need to decrease dose of substrate if start on an inhibitor. INH increases substrate. *Inducer – competes with other drugs for a particular enzyme affecting metabolism of the substrate (increases) decreasing the efficacy of the drug. Need to increase dose of substrate if start on an inducer. IND decreases substrate. Renal excretion – passive glomerular filtration, active tubular secretion, tubular reabsorption. Pharmacogenomics: 1 question Pharmacogenomics- the study of the influence of hereditary factors on the response of individual organism to drugs, and the study of variations of DNA and RNA characteristics as related to drug response. Pharmacogenetic tests mentioned on drug labels can be classified as “test required”, “test recommended”, and “information only”. Currently there are 4 drugs requiring to have pharmacogenetic testing performed before they are prescribed: Cetuximab, Trastuzumab, Maraviroc, and Dasatinib. No genetic testing is required by the FDA for the initiation of medications such as warfarin, carbamazepine, valproic avid and abacavir are currently in place, such tests are recommended prior to initial dosing. BBW initiated in December 2007- on carbamazepine label – testing recommended for HLA-B 1502 in patient with Asian ancestry due to high risk of developing SJS or toxic epidermal necrolysis (TEN). Drugs across the lifespan: 3 questions Lack of evidence-based literature on safe and effective use of meds in children. Neonates at greater risk for toxicity with highly protein-bound drugs because protein binding decreased, increasing amount of free drug available. Adult level of renal function achieved at 12 months. Most accurate device for measuring liquid dose for child – oral syringe. *lifespan changes in elderly- watch for Cholenergic SE, Neuro SE, sedative SE Prevent medication errors – write out the term daily, no zeros after decimal point. Drug sensitivity in the very young results from immature organs, in elderly from organ system degeneration. Pediatric organ immaturity – at risk for elevated drug levels, delayed elimination. Gastric acidity does not reach adult values for 2 years. Elderly drug complications due to altered pharmacokinetics, multiple and severe illnesses, multiple-drug therapy, poor adherence. Altered absorption of drugs in elderly result in delayed drug response. Four factors that alter drug distribution in elderly – increased body fat, decreased lean body mass, decreased body water, reduced serum albumin Nalidixic acid may cause cartilage erosion in children. Fluoroquinolones in pediatric – tendon rupture. Reduced albumin causes free drug to rise. Elderly, proper index of renal function is creatinine clearance. Then GFR. Increase in adverse reactions in geriatric population – polypharmacy, greater use of drugs with low therapeutic index, poor adherence, inadequate supervision, severe illness. Adverse effects in the elderly – Beers list. Drugs that inhibit cell wall synthesis: 2 questions Gram + = strep, staph, enterococcus Penicillin- bacteriocidal with Beta Lactam ring- MOA- weaken cell wall causing bacteria to take up excess water and rupture Resistance factors- inability for PCNs to reach target, inactivation of PCNs by bacterial enzyme, production of PCN binding protein that have a low affinity for PCNs Narrow Spectrum (Penicillinase sensitive)- Naficillin, Oxacillin, Dicloxacillin Broad Spectrum – Ampicillin, Amoxicillin Extended- Spectrum- Ticarcillin, Piperacillin Beta Lactamase Inhibitors- Clavulanic Acid, Tazobactam, Sulbactam Cephalasporins- binds to penicillin binding proteins (PBPs), disrupts cell wall synthesis, causing cell to lyse. First generation cephalosporins – gram positive cocci. Second and third generation more broad spectrum – gram positive and gram negative. !st generation- prophylactic for surgery- never for active infection • Cephazolin (do not give with alcohol) • Cephalexin • Cefadroxil 2nd generation- works against URI- pneumonia from h. flu, klebsiella, pneumoniacocci, staphylococci • Cefotetan (do not give with alcohol or drugs that promote bleeding) • Cefprozil • Cefoxitin • Cefuroxime • Cefactor 3rd generation- preferred gram -, treats meningitis • Ceftriaxone (do not give with drugs that promote bleeding, or calcium) • Cefixime • Cefditoren • Cefotaxime 4th generation- Used to treat HAP, pseudomonas aeruginosa • Cefepime • Ceftolozone 5th generation- used to treat MRSA • Ceftaroline *which can cause bleeding, which contraindicated with alcohol? If have an anaphylactic reaction, do not give PCNs or Cephalosporins. If not anaphylactic, can give cephalosporins. Vancomycin – active against MRSA, bacteriocidal, red man syndrome. Bacteriostatic inhibitors of protein synthesis: 1 question Tetracyclines- non-lethal inhibitors of protein synthesis- Broad Spectrum Used to treat: Infectious Disease, Acne, Peptic Ulcer disease, Periodontal disease, RA, Mycoplasma Pneumoniae, helicobacter Pylori, lyme disease, anthrax, RMSF Do not give with calcium, iron, mag, aluminum, zinc, laxatives, antacids- decreases absorption- wait a couple of hours between Adverse reactions- GI irritation, staining of bones and teeth in children less than 8 years (only exception is with the infection of RMSF and doxycycline), superinfection, renal toxicity, photo sensitivity, caution of women in childbearing age. -Diarrhea may indicate potential life-threatening superinfection - High dose may be associated with liver damage (tetracycline- Short acting, Doxycycline- long acting, Minocycline- long acting) Macrolides (Mycins)- Bacteriostatic or Bacteriocidal- inhibit protein synthesis, broad spectrum Used if: a patient is allergic to PCNs, whooping cough, active diptheria, coryne bacterium, diptheriae, chlamydia infections, m. pneumoniae, group A strep pyogens, may also be used as an alternative for PCN G if allergic. Drug interactions- CYP3A4, Cisapride, ergotamine or dihydroergotamine, terfenadine, astemizole, lovastatin, simvastatin Adverse Effects- GI, QT prolongation and sudden cardiac death, superinfection, thrombophlebitis, transient hearing loss Clindamycin- BBW- can cause C-diff. Example: Erythromycin, (Others: Clarithromycin, Azithromycin- prolong QT) Rifampin, Metronidazole, and Floroquinolones- inhibit synthesis of DNA or RNA by binding directly to nucleic acids or interacting with enzymes required for nucleic acid synthesis Aminoglycosides MOA – inhibit protein synthesis, can cause ototoxicity and nephrotoxicity. Gentamicin – continues to exert antibacterial effects even after plasma levels decrease below detectable levels – reaction will stay for a while. Erythromycin – can prolong QT interval, so pause simvastatin while taking erythromycin! Traveler’s diarrhea – ciprofloxacin for E.Coli (gram negative bacillus) Sulfonamides – most common SE is skin reactions. Allergy to sulfa – usually skin rx. Ciprofloxacin – tendonitis and tendon rupture may occur. Drugs used for UTIs: 2 question *Tx UTIs. 80% E.Coli, then Proteus and Klebsiella. Most UTI gram- d/t cause from intestinal bacteria. Prophylaxis -SMZ/TMP- 3x/wk for 6 months [Show More]
Last updated: 1 year ago
Preview 1 out of 36 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 26, 2022
Number of pages
36
Written in
Additional information
This document has been written for:
Uploaded
Jul 26, 2022
Downloads
0
Views
47