*NURSING > EXAM > NR 508 ADVANCED PHARMACOLOGY QUIZZES 07 Sets- (Questions and Answers ) Newest 2020/2021: (100% Corre (All)
NR 508 ADVANCED PHARMACOLOGY QUIZZES 07 Sets- (Questions and Answers ) Newest 2020/2021: (100% Correct Answers)
Document Content and Description Below
ADVANCED PHARMACOLOGY QUIZZES Question 1 0 / 0 pts Which of the following statements is true about the prescribing practices of physicians? Even though most physicians claim to place little weig... ht on drug advertisements, pharmaceutical representatives, and patient preference and state that they rely on academic sources for drug information, a study showed that commercial rather than scientific sources of drug information dominated their drug information materials. Younger physicians tend to prescribe fewer and more appropriate drugs. Antibiotics have dropped out of the top five classifications of drugs prescribed. Most physicians have a therapeutic armamentarium of about 144 drugs. Question 2 0 / 0 pts A primary care NP recommends an over-the-counter medication for a patient who has acid reflux. When teaching the patient about this drug, the NP should tell the patient: Because patients often increase over-the-counter drug doses themselves, it is important to reinforce the need to follow the manufacturer’s recommendations for dosing. As with any drug, interactions may occur with other medications. Antacids do not cause sedation, so patients need not be cautioned to avoid other sedating medications. Question 3 0 / 0 pts A woman who has been taking a COCP for 2 months tells the primary care NP that she has had several headaches, breakthrough bleeding, and nausea. The NP should counsel the woman: Correct! Breakthrough bleeding, nausea, and headaches are common during the first 3 months of therapy and should improve without intervention. Progestin-only pills are used for lactating women only. Prolonged bleeding and severe headache would warrant discontinuation of the COCP. Backup contraception is not indicated. Question 4 0 / 0 pts A patient asks a primary care nurse practitioner (NP) about using over-the-counter medications to treat an upper respiratory infection with symptoms of cough, fever, and nasal congestion. The NP should: Correct! A basic principle guiding over-the-counter use is to look at specific symptoms and treat each separately because some products contain therapeutic doses of one ingredient and subtherapeutic doses of others. Cough preparations containing acetaminophen often do not contain therapeutic doses, and patients often overdose when they supplement with acetaminophen. Over-the-counter medications are effective at recommended doses. Patients should follow dosing recommendations on the package. Question 5 0 / 0 pts A patient has recurrent symptoms and tells the primary care NP that she can’t remember to take her medication all the time. The NP should: Correct! If the attitude is that the patient has a problem for the health care provider to solve, then the provider owns the problem and often hastens to solve it. When patients own their problems, they are more likely to engage in their care and treatment. Giving shortened regimens, providing written information, and administrating medication in the clinic are examples of the provider solving the problem for the patient. Question 6 0 / 0 pts A postpartum woman will begin taking the minipill while she is nursing her infant. The primary care NP should instruct the patient: Minipills are used primarily in breastfeeding women. There is no increased risk for thromboembolic events for women taking these pills. It is not necessary to use a backup method of contraception. Women should be advised to contact the provider when they stop nursing so that a COCP can be prescribed. The more disrupted the bleeding pattern, the more likely it is that ovulation is inhibited. Question 7 0 / 0 pts A patient who weighs 170 lb wishes to lose weight, with a target weight goal of 125 lb. To initiate a program that will result in a loss of 1 lb per week, the primary care NP should recommend a dietary intake of _____ kcal. To lose weight, a patient must decrease intake to below the level needed to maintain weight. The patient must decrease daily calorie consumption by 500 kcal for each pound he or she wishes to lose weekly. Because it takes approximately 10 kcal per pound to maintain weight, the NP can assume that the patient currently takes in 1700 kcal/day and should recommend a diet of 1200 kcal/day for weight loss. Question 8 0 / 0 pts A patient who has hypothyroidism and is obese begins therapy with orlistat. The primary care NP teaches the patient about this drug and then asks the patient to describe its use. Which statement by the patient indicates understanding of the teaching? In long-term studies on the use of orlistat, most of the weight loss occurred during the first months. Patients should not be counseled to eat a high-fat diet; the maximum amount of fat excretion is around 25% to 30%. Patients should take fat-soluble vitamins, but the vitamins should be taken at different times and not with orlistat. Orlistat interferes with levothyroxine absorption, so the two drugs should be taken at different times, and thyroid levels should be monitored with an increase in levothyroxine dose only when indicated by thyroid levels. Question 9 0 / 0 pts A patient with chronic back pain that is unrelieved by prescription analgesic medications asks a primary care nurse practitioner (NP) about acupuncture treatments. The NP should tell this patient: Current literature does not allow definitive conclusions to be drawn regarding the use of complementary and alternative medicine (CAM) because much of what appears in the literature continues to be based on observational reports and small studies. Biofield therapy has not been shown to be more effective than acupuncture. Creatine is used to increase muscle mass. Question 10 0 / 0 pts The primary care nurse practitioner (NP) is using critical thinking skills when: Correct! Practitioners use critical thinking skills by reviewing and analyzing current knowledge and synthesizing approaches to apply to unique patient situations. Using standardized protocols, adhering to scientific principles, and following practices of seasoned mentors may be useful, but these do not encompass the concept of critical thinking, which requires the practitioner to use what is known in new situations. Question 11 0 / 0 pts The primary care NP prescribes an inhaled corticosteroid for a patient who has asthma. The third-party payer for this patient denies coverage for the brand that comes in the specific strength the NP prescribes. The NP should: The second step of medical decision making takes into account benefits versus costs along with an understanding that it is impossible to do everything because of limited resources. The NP should prescribe what is covered and evaluate its effectiveness; if it does not work, the third-party payer may be approached about the need for the other medication. Providing samples is not always possible, and this practice is being discouraged, so it is not a viable solution. Asking patients to pay out of pocket ultimately may be necessary but carries risks that the patient will not obtain the medication. Writing a letter of medical necessity may be indicated if the available drugs are not effective but is not the initial step. Question 12 0 / 0 pts A primary care NP prepares to teach a patient about the management of a chronic condition. The patient says, “I don’t want to know all of that. Just tell me what to take and when.” The NP should initially: The patient has stated expectations about care and treatment for the condition. The NP should begin by respecting that and providing the amount of information the patient wants. As the therapeutic relationship grows, the NP may elicit more active participation and understanding. Question 13 0 / 0 pts In every state, prescriptive authority for NPs includes the ability to write prescriptions: All states now have some degree of prescriptive authority granted to NPs, but not all states allow authority to prescribe controlled substances. Many states still require some degree of physician involvement with certain types of drugs. Question 14 0 / 0 pts A primary care NP has prescribed phentermine for a patient who is obese. The patient loses 10 lb in the first month but reports that the drug does not seem to be suppressing appetite as much as before. The NP should: continue the phentermine at the same dose. Tolerance to the effects of phentermine usually develops within a few weeks of starting therapy. When this occurs, the drug should be discontinued, not increased. Phentermine use is not recommended longer than a few weeks. Question 15 0 / 0 pts A patient asks the primary care NP which medication to use for mild to moderate pain. The NP should recommend: Providers should use generic drug names when prescribing drugs or recommending them to patients, unless a particular brand is essential for some reason. Because acetaminophen can have many trade names, it is important for patients to understand that the drug is the same for all to avoid overdosing on acetaminophen. APAP is a commonly used abbreviation but should not be used when recommending the drug to patients. Question 16 0 / 0 pts The primary care NP prescribes an extended-cycle monophasic pill regimen for a young woman who reports having multiple partners. Which statement by the patient indicates she understands the regimen? The extended-cycle pills have fewer pill-free intervals, so women have only four periods a year. Patients take pills every day. Because this patient has multiple partners, she should continue to use condoms. This type of pill has the same side effects as other types. Question 17 0 / 0 pts A patient who has diabetes mellitus and congestive heart failure takes insulin and warfarin. The patient will begin taking exogenous testosterone to treat secondary hypogonadism. The primary care NP should recommend: Correct! Patients with diabetes may require a decrease in insulin dose because of the metabolic effects of androgens. More frequent blood glucose monitoring should be performed. Warfarin doses may need to be decreased because androgens increase sensitivity to anticoagulants. Question 18 0 / 0 pts A woman who has been taking a COCP tells the primary care NP that, because of frequent changes in her work schedule, she has difficulty remembering to take her pills. The woman and the NP decide to change to a vaginal ring. The NP will instruct her to insert the ring: ou Answered Patients should be switched from a COCP to a vaginal ring by insertion within 7 days after the last active pill. No backup method is needed. Patients do not need to continue one more cycle of COCPs. Women taking progestin-only pills insert the ring on the last day of the pill pack. Question 19 0 / 0 pts A primary care NP is developing a clinical practice guideline for management of a patient population in a midsized suburban hospital. The NP should: Clinical guidelines should be written using all available evidence as well as expert opinion. Existing guidelines from a different type of hospital may not be based on data generalizable to this population. Third-party payer guidelines are usually weighted toward decreased costs. Long-standing protocols often do not take into account current knowledge and research. Question 20 0 / 0 pts To increase the likelihood of successful pharmacotherapy, when teaching a patient about using a medication, the primary care nurse practitioner (NP) should: You Answered It is important that the patient “owns the problem” and has a part in the solution. Providing education about the medication, stressing the importance of following medication instructions, and distributing package inserts may be useful, but it is essential that patients take an active role in their care. Question 21 0 / 0 pts A 50-year-old woman reports severe, frequent hot flashes and vaginal dryness. She is having irregular periods. She has no family history of CHD or breast cancer and has no personal risk factors. The primary care NP should recommend: Oral contraceptive pills are not approved by the U.S. Food and Drug Administration for management of perimenopausal symptoms except to treat irregular menstrual bleeding. This patient has a low risk for CHD and breast cancer, so oral contraceptive pills are relatively safe. She is also at risk for pregnancy, so oral contraceptive pills can help to prevent that. Question 22 0 / 0 pts A man who has secondary hypogonadism associated with pituitary dysfunction will begin exogenous testosterone therapy. The patient asks the primary care NP about future chances of fathering children. The NP should tell him that: Men with secondary hypogonadism may become fertile with exogenous testosterone. Question 23 0 / 0 pts A 50-year-old woman who is postmenopausal is taking an aromatase inhibitor as part of a breast cancer treatment regimen. She calls her primary care NP to report that she has had hot flashes and increased vaginal discharge but no bleeding. The NP should: Any abnormal vaginal discharge should be reported immediately and should be evaluated with a gynecologic examination to rule out carcinoma. She is not showing signs of ovulation, so contraception is not necessary. She should not stop taking the medication unless the gynecologic examination is positive. These are common side effects but are not always normal. UnansweredQuestion 24 0 / 0 pts A patient receives an inhaled corticosteroid to treat asthma. The patient asks the primary care NP why the drug is given by this route instead of orally. The NP should explain that the inhaled form: An inhaled corticosteroid goes directly to the site of action and does not have to pass through gastrointestinal tract absorption or the liver to get to the lungs. It is generally well absorbed at this site, although dosing is not necessarily easier to regulate because it is not always clear how much of an inhaled drug gets into the lungs. Question 25 0 / 0 pts A patient who takes warfarin (Coumadin) experiences excessive bleeding, even though serum drug levels are normal. The primary care NP should question this patient about the use of: Correct! Ginkgo biloba decreases blood viscosity and can enhance the effects of warfarin. Feverfew, echinacea, and green tea do not have this effect. Question 1 0 / 0 pts The primary care NP is prescribing a medication for an off-label use. To help prevent a medication error, the NP should: When prescribing a drug for an off-label use, the provider should specify this on the written prescription and should provide a rationale so that the pharmacist understands why the prescription is different from the normal use. Calling the pharmacist would not provide written documentation. Merely writing the different instructions can lead to errors if the pharmacist changes the label to conform to usual standards. The patient may forget verbal instructions and follow the usual regimen instead. Question 2 0 / 0 pts To increase the likelihood of successful pharmacotherapy, when teaching a patient about using a medication, the primary care nurse practitioner (NP) should: It is important that the patient “owns the problem” and has a part in the solution. Providing education about the medication, stressing the importance of following medication instructions, and distributing package inserts may be useful, but it is essential that patients take an active role in their care. Question 3 0 / 0 pts A patient comes to the clinic and asks the primary care NP about using a newly developed formulation of the drug the patient has been taking for a year. When deciding whether or not to prescribe this formulation, the NP should: About 6 to 12 months of postmarketing experience can yield information about drug efficacy and side effects, so patients should be cautioned to wait for these data. Drug company promotional materials have biased information. Most new drugs are more expensive, and costs alone should not determine drug choice. Extended-release forms are often more expensive. Question 4 0 / 0 pts A sexually active patient tells the primary care NP that she has been unable to get her new COCP pill pack until today and has missed 3 days of pills. The NP should tell her to: Patients who miss 2 or more pills at the beginning or end of a pack should use emergency contraceptive pills, such as the Plan B pill, restart a new pill pack, and use backup contraception for 7 days. Question 5 0 / 0 pts Osteopenia is diagnosed in a 55-year-old woman who has not had a period in 15 months. She has a positive family history of breast cancer. The primary care NP should recommend: Although estrogen slows the progression of osteoporosis, it also increases the risk of breast cancer when initiated early in menopause. This woman should receive a nonhormonal treatment for osteoporosis and may receive HT in 5 years if menopausal symptoms persist. Testosterone therapy, estrogen-only therapy, and estrogen-progesterone therapy are not indicated. Question 6 0 / 0 pts A patient asks a primary care NP whether over-the-counter drugs are safer than prescription drugs. The NP should explain that over-the-counter drugs are: Correct! Over-the-counter products have a wider margin of safety because most of these drugs have undergone rigorous testing before marketing and further refinement through years of over-the-counter use by consumers. When labels are understood and followed, over-the-counter medications are safe. Over-the-counter medications are regulated by the FDA. Question 7 0 / 0 pts A primary care NP is developing a clinical practice guideline for management of a patient population in a midsized suburban hospital. The NP should: Clinical guidelines should be written using all available evidence as well as expert opinion. Existing guidelines from a different type of hospital may not be based on data generalizable to this population. Third-party payer guidelines are usually weighted toward decreased costs. Long-standing protocols often do not take into account current knowledge and research. Question 8 0 / 0 pts A patient bursts into tears when the primary care NP diagnoses diabetes. The NP should: To help patients participate in their disease management, the NP must have an understanding of the patient’s concerns and fears. The first step when the patient is obviously upset is to determine what the patient knows and fears about the disease. Question 9 0 / 0 pts A patient is diagnosed with lupus and reports occasional use of herbal supplements. The primary care NP should caution this patient to avoid: Patients with lupus who take echinacea may experience an increase in symptoms, even if the patient is taking immunosuppressants. Question 10 0 / 0 pts A patient takes an oral medication that causes gastrointestinal upset. The patient asks the primary care NP why the drug information insert cautions against using antacids while taking the drug. The NP should explain that the antacid may: Changing the pH of the gastric mucosa can alter the absorption of the drug. Drug distribution is not affected. It may indirectly cause drug toxicity if a significant amount more of the drug is absorbed. It would decrease stomach upset. Question 11 0 / 0 pts A patient receives an inhaled corticosteroid to treat asthma. The patient asks the primary care NP why the drug is given by this route instead of orally. The NP should explain that the inhaled form: An inhaled corticosteroid goes directly to the site of action and does not have to pass through gastrointestinal tract absorption or the liver to get to the lungs. It is generally well absorbed at this site, although dosing is not necessarily easier to regulate because it is not always clear how much of an inhaled drug gets into the lungs. Question 12 0 / 0 pts The primary care NP is reviewing evidence-based recommendations about the off-label use of a particular drug. Which recommendation should influence the NP’s decision about prescribing the medication? Randomized, experimental studies yield the best data about use of medications. Patient reports carry the least weight because bias can occur and other factors can influence outcomes. Pharmaceutical company reports are biased. Question 13 0 / 0 pts A primary care NP prescribes a COCP for a woman who is taking them for the first time. After teaching, the woman should correctly state the need for using a backup form of contraception if she: Vomiting and diarrhea may cause oral contraceptive failure, so women should be advised to use backup contraception if they experience these. The other conditions do not lead to oral contraceptive failure. Question 14 0 / 0 pts A patient who has diabetes mellitus and congestive heart failure takes insulin and warfarin. The patient will begin taking exogenous testosterone to treat secondary hypogonadism. The primary care NP should recommend: Patients with diabetes may require a decrease in insulin dose because of the metabolic effects of androgens. More frequent blood glucose monitoring should be performed. Warfarin doses may need to be decreased because androgens increase sensitivity to anticoagulants. Question 15 0 / 0 pts A patient asks the primary care NP which medication to use for mild to moderate pain. The NP should recommend: Providers should use generic drug names when prescribing drugs or recommending them to patients, unless a particular brand is essential for some reason. Because acetaminophen can have many trade names, it is important for patients to understand that the drug is the same for all to avoid overdosing on acetaminophen. APAP is a commonly used abbreviation but should not be used when recommending the drug to patients. Question 16 0 / 0 pts The primary care nurse practitioner (NP) writes a prescription for an antibiotic using an electronic drug prescription system. The pharmacist will fill this prescription when: Correct! E-sign effectively voids requirements that prescriptions be written on paper or printed as a hard copy. Some scheduled drugs still require written copies. Faxed copies of this drug would be allowed but are not necessary for the pharmacist to fill the prescription. The patient’s electronic medical record stands as evidence of the need for a prescription of a drug but is not needed for the pharmacist to fill the prescription. Question 17 0 / 0 pts A primary care NP wishes to order a drug that will be effective immediately after administration of the drug. Which route should the NP choose? The sublingual route is preferred for quick action because the drug is directly absorbed into the bloodstream and avoids the pass through of the liver, where much of an oral drug is metabolized. Rectal routes have unpredictable absorption rates. Topical routes are the slowest. Intramuscular routes are slow. Question 18 0 / 0 pts A patient develops hepatotoxicity from chronic acetaminophen use. The primary care NP may recommend: Milk thistle has been shown to protect the liver after exposure to hepatotoxins such as acetaminophen, ethanol, and halothane. The other supplements listed do not have this effect. Question 19 0 / 0 pts A 55-year-old woman has not had menstrual periods for 5 years and tells the primary care nurse practitioner (NP) that she is having increasingly frequent vasomotor symptoms. She has no family history or risk factors for coronary heart disease (CHD) or breast cancer but is concerned about these side effects of hormone therapy (HT). The NP should: The current gap hypothesis regarding breast cancer supports initiating HT 5 years or more after menopause. To decrease risk for CHD, HT should begin at the time of menopause. HT will relieve vasomotor symptoms at all stages of menopause. Herbal supplements have estrogenizing effects and carry the same risks as estrogen therapy. Question 20 0 / 0 pts Which of the following has influenced an emphasis on primary care education in medical schools? The Physician Payment Review Commission in 1992 directly increased financial reimbursement to clinicians who provide primary care. Coupled with a shortage of primary care providers, this incentive led medical schools to place greater emphasis on preparing primary care physicians. Competition from nonphysicians increased coincidentally as professionals from other disciplines stepped up to meet the needs. Nonphysicians have had increasing success at providing primary care and have been shown to be safe and effective. Question 21 0 / 0 pts A thin 52-year-old woman who has recently had a hysterectomy tells the primary care NP she is having frequent hot flashes and vaginal dryness. A recent bone density study shows early osteopenia. The woman’s mother had CHD. She has no family history of breast cancer. The NP should prescribe: HT relieves symptoms of menopause and prevents osteoporosis. When started soon after menopause, HT can reduce CHD risk. Breast cancer risk may be decreased if HT is begun 5 years after onset of menopause. This woman has a higher risk of CHD and osteoporosis, so initiating therapy now is a good option. Because she has had a hysterectomy, estrogen-only therapy is indicated. Question 22 0 / 0 pts A patient reports taking antioxidant supplements to help prevent cancer. The primary care NP should: Epidemiologic evidence indicates that people who eat fruits and vegetables regularly have a decreased risk of cancer. Although retrospective studies have suggested major benefits from antioxidants, no intervention studies have determined conclusively that antioxidants prevent cancer. Large doses of vitamin A can produce a yellow hue to the skin. Antioxidants can be beneficial, but in certain populations, such as smokers, they may be harmful. Question 23 0 / 0 pts When prescribing a medication for a chronic condition, the primary care NP should tell the patient: Nonscheduled drugs may be ordered with refills so that the patient does not have to be seen each time a refill is needed. It is important to determine how closely a patient should be monitored while taking a drug for a chronic condition and to let the patient know how frequently he or she needs to be seen. Patients may contact a pharmacy when they still have authorized refills to pick up, but this is determined by the clinician. Pharmacists usually cannot dispense more than 30 days’ worth of a medication. Question 24 0 / 0 pts A patient who has an upper respiratory infection reports using over-the-counter cold preparations. The primary care NP should counsel this patient to use caution when taking additional over-the-counter medications such as: Correct! Cold preparations often contain antipyretics such as acetaminophen or aspirin. Patients should be cautioned about taking additional antipyretics to avoid overdose. Question 25 0 / 0 pts A patient will begin taking two drugs that are both protein-bound. The primary care NP should: Protein-bound drugs bind to albumin, and serum albumin levels may affect how drugs are distributed. The provider should monitor drug levels, actions, and side effects and change dosing accordingly. Increasing the dose of both drugs is not recommended unless monitoring indicates. Increasing dietary protein does not affect this. Staggering the drugs will not affect this. Question 1 0 / 0 pts A patient is newly diagnosed with type 2 diabetes mellitus. The primary care NP reviews this patient’s laboratory tests and notes normal renal function, increased triglycerides, and deceased HDL levels. The NP should prescribe: Metformin is recommended as initial pharmacologic treatment for type 2 diabetes. It has been shown to decrease triglycerides and LDLs. Question 2 0 / 0 pts A patient who has type 2 diabetes mellitus will begin taking a bile acid sequestrant. Which bile acid sequestrant should the primary care NP order? All bile acid sequestrants are equally effective. Colesevelam has an additional indication to improve glycemic control in adults with type 2 diabetes and so should be selected when prescribing a bile acid sequestrant for this patient. Question 3 0 / 0 pts A 55-year-old woman has a history of myocardial infarction (MI). A lipid profile reveals LDL of 130 mg/dL, HDL of 35 mg/dL, and triglycerides 150 mg/dL. The woman is sedentary with a body mass index of 26. The woman asks the primary care NP about using a statin medication. The NP should: This woman would be using a statin medication for secondary prevention because she already has a history of MI, so a statin should be prescribed. Dietary and lifestyle changes should be a part of therapy, but not the only therapy. She is relatively young, and quality-of-life issues are not a concern. There is no clinical evidence to support use of statins as primary prevention in women. Question 4 0 / 0 pts A 40-year-old patient is in the clinic for a routine physical examination. The patient has a body mass index (BMI) of 26. The patient is active and walks a dog daily. A lipid profile reveals low-density lipoprotein (LDL) of 100 mg/dL, high-density lipoprotein (HDL) of 30 mg/dL, and triglycerides of 250 mg/dL. The primary care nurse practitioner (NP) should: Testing for type 2 diabetes should be considered in all adults with a BMI greater than 25 who have risk factors such as HDL less than 35 mg/dL or triglycerides greater than 250 mg/dL. A fasting plasma glucose level greater than 126 mg/dL indicates diabetes. Metformin is not indicated unless testing is positive. Lifestyle changes may be part of the treatment plan. Serum insulin level is not indicated. Question 5 0 / 0 pts An African-American patient who is obese has persistent blood pressure readings greater than 150/95 mm Hg despite treatment with a thiazide diuretic. The primary care NP should consider prescribing a(n): You Answered African-American patients are considered good candidates for calcium channel blockers to treat hypertension. Treatment with calcium channel blockers as monotherapy in African-American patients has proved to be more effective than some other classes of antihypertensive agents. Question 6 0 / 0 pts The primary care nurse practitioner (NP) sees a patient in the clinic who has a blood pressure of 130/85 mm Hg. The patient’s laboratory tests reveal high-density lipoprotein, 35 mg/dL; triglycerides, 120 mg/dL; and fasting plasma glucose, 100 mg/dL. The NP calculates a body mass index of 29. The patient has a positive family history for cardiovascular disease. The NP should: The patient’s blood pressure indicates prehypertension, but the patient does not have cardiovascular risk factors such as hyperlipidemia or hyperinsulinemia. The body mass index indicates that the patient is overweight but not obese. Pharmacologic treatment is not recommended for prehypertension unless compelling reasons are present. The findings are not normal, so it is appropriate to counsel the patient about diet and exercise. Question 7 0 / 0 pts A patient who has had a previous myocardial infarction has a blood pressure of 135/82 mm Hg. The patient’s body mass index is 28, and the patient has a fasting plasma glucose of 105 mg/dL. The primary care NP should prescribe: This patient has prehypertension but has a compelling reason for treatment. Patients who have had a myocardial infarction should be treated with a β-blocker and angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker (ARB). Question 8 0 / 0 pts A patient who has stable angina and uses sublingual nitroglycerin tablets is in the clinic and begins having chest pain. The primary care NP administers a nitroglycerin tablet and instructs the patient to lie down. The NP’s next action should be to: When a patient experiences an acute attack of angina in the clinic, the primary care NP should be prepared to treat the condition. After giving nitroglycerin, oxygen should be administered. An electrocardiogram is not immediately indicated. Chewable aspirin is given if the angina is unrelieved and when the patient is being transported to the hospital. EMS should be activated if there is no pain relief 5 minutes after the first dose of nitroglycerin. Question 9 0 / 0 pts A patient has been taking levothyroxine 100 mcg daily for several months. The patient comes to the clinic with complaints of insomnia and irritability. The primary care NP notes a heart rate of 92 beats per minute. The NP should: When signs of thyrotoxicosis occur, the drug should be decreased or temporarily discontinued for 5 to 7 days. Liothyronine is not indicated. Propylthiouracil is not indicated. Question 10 0 / 0 pts A patient who takes a calcium channel blocker is in the clinic for an annual physical examination. The cardiovascular examination is normal. As part of routine monitoring for this patient, the primary care NP should evaluate: Patients who take calcium channel blockers should have periodic renal and LFTs. Question 11 0 / 0 pts A patient who is newly diagnosed with type 2 diabetes mellitus has not responded to changes in diet or exercise. The patient is mildly obese and has a fasting blood glucose of 130 mg/dL. The patient has normal renal function tests. The primary care NP plans to prescribe a combination product. Which of the following is indicated for this patient? Obese patients with normal renal function and elevated fasting plasma glucose may be started on a combination of metformin and a second-generation sulfonylurea. Question 12 0 / 0 pts A 75-year-old patient who has cardiovascular disease reports insomnia and vomiting for several weeks. The primary care NP orders thyroid function tests. The tests show TSH is decreased and T4 is increased. The NP should consult with an endocrinologist and order: Patients with hyperthyroidism, or Graves’ disease, will require radioactive iodine. Elderly patients and patients with cardiovascular disease should be pretreated with an antithyroid medication such as methimazole. Thyrotropin is used to diagnose thyroid cancer. Levothyroxine is used to treat hypothyroidism. Propylthiouracil is also a thyroid suppressant, but methimazole is preferred. Question 13 0 / 0 pts A child who has congenital hypothyroidism takes levothyroxine 75 mcg/day. The child weighs 15 kg. The primary care NP sees the child for a 3-year-old check-up. The NP should consult with a pediatric endocrinologist to discuss: In congenital hypothyroidism, therapy may be stopped for 2 to 8 weeks after the patient reaches 3 years of age. If TSH levels remain normal, thyroid supplementation may be discontinued permanently. Question 14 0 / 0 pts A primary care NP sees a 46-year-old male patient and orders a fasting lipoprotein profile that reveals LDL of 190 mg/dL, HDL of 40 mg/dL, and triglycerides of 200 mg/dL. The patient has no previous history of coronary heart disease, but the patient’s father developed coronary heart disease at age 55 years. The NP should prescribe: Correct! HMG-CoA reductase inhibitors are used to treat hyperlipidemia when the LDL is the primary lipid elevation. This patient has risk factors of being a man older than 45 years, with a positive family history of coronary heart disease before age 55 in a male first-degree relative. Gemfibrozil is used for patients with elevated triglycerides and low HDL. Bile acid sequestrants are used as adjunctive and not first-line therapy for reducing LDL. A combination product is not indicated for first-line therapy. Question 15 0 / 0 pts A patient who has stable angina pectoris and a history of previous myocardial infarction takes nitroglycerin and verapamil. The patient asks the primary care nurse practitioner (NP) why it is necessary to take verapamil. The NP should tell the patient that verapamil: Verapamil decreases the force of smooth muscle contraction in the smooth muscle of the coronary and peripheral vessels; this results in coronary artery dilation, which lowers coronary resistance and improves blood flow through collateral vessels as well as oxygen delivery to ischemic areas of the heart. Calcium channel blockers do not increase the rate or force of contraction of the heart. Question 16 0 / 0 pts A patient has three consecutive blood pressure readings of 140/95 mm Hg. The patient’s body mass index is 24. A fasting plasma glucose is 100 mg/dL. Creatinine clearance and cholesterol tests are normal. The primary care NP should order: The patient has stage I hypertension. Because there are no compelling indications for other treatment, a thiazide diuretic should be used initially to treat the hypertension. Dietary and lifestyle changes should also be recommended but are not sufficient for patients with stage I hypertension. Other drugs may be added later if thiazide diuretic therapy fails. Question 17 0 / 0 pts A patient who takes nitroglycerin for stable angina pectoris develops hypertension. The primary care NP should contact the patient’s cardiologist to discuss adding: You Answered Nifedipine and related drugs are potent vasodilators, which makes them more effective for hypertension than verapamil and diltiazem. Amlodipine is not a first-line drug. Question 18 0 / 0 pts A patient who has a history of angina has sublingual nitroglycerin tablets to use as needed. The primary care nurse practitioner (NP) reviews this medication with the patient at the patient’s annual physical examination. Which statement by the patient indicates understanding of the medication? Although the traditional recommendation is for patients to take up to 3 nitroglycerin doses over 15 minutes before accessing emergency medical services (EMS), more recent guidelines suggest an alternative strategy to reduce delays in emergency care. These include instructions to call 9-1-1 immediately if pain persists for 5 minutes after the first dose. Aspirin is recommended when the patient is being transported to emergency care and is not recommended as an adjunct to nitroglycerin with each episode of chest pain. The three doses of nitroglycerin are given 5 minutes apart over 15 minutes. Question 19 0 / 0 pts A patient who has type 2 diabetes mellitus takes metformin (Glucophage). The patient tells the primary care NP that he will have surgery in a few weeks. The NP should recommend: Insulin should be considered for patients with diabetes during times of physical stress, such as illness or surgery. Question 20 0 / 0 pts A patient who is taking nifedipine develops mild edema of both feet. The primary care NP should contact the patient’s cardiologist to discuss: You Answered Mild to moderate peripheral edema occurs in the lower extremities in about 10% of patients; this is caused by arterial dilation, not by left ventricular dysfunction. Amlodipine is less likely to have this effect. Renal function tests are not indicated. Increasing the nifedipine dose would worsen the symptoms. Question 21 0 / 0 pts A patient who has primary hyperlipidemia and who takes atorvastatin (Lipitor) continues to have LDL cholesterol of 140 mg/dL after 3 months of therapy. The primary care NP increases the dose from 10 mg daily to 20 mg daily. The patient reports headache and dizziness a few weeks after the dose increase. The NP should: When used in combination with a low-dose statin, ezetimibe has been noted to produce an additional 18% reduction in LDL. Because this patient continues to have elevated LDL along with side effects of the statin, the NP should resume the lower dose of the statin and add ezetimibe. Atorvastatin is given once daily. Cholestyramine and omega-3 supplements are not indicated. Question 22 0 / 0 pts A primary care NP orders thyroid function tests. The patient’s TSH is 1.2 microunits/mL, and T4 is 1.7 ng/mL. The NP should: Primary hypothyroidism is the most common form of hypothyroidism. Use of certain drugs, such as lithium, and diseases such as Hashimoto’s thyroiditis can cause hypothyroidism but are less likely. The patient does not have signs of hyperthyroidism. Question 23 0 / 0 pts The primary care NP sees a new patient who has diabetes and hypertension and has been taking a thiazide diuretic for 6 months. The patient’s blood pressure at the beginning of treatment was 150/95 mm Hg. The blood pressure today is 138/85 mm Hg. The NP should: Evidence-based guidelines suggest that optimal control of hypertension to less than 130/80 mm Hg could prevent 37% of cardiovascular disease in men and 56% in women, so this patient, although showing improvement, could benefit from the addition of another medication. An angiotensin-converting enzyme inhibitor is an appropriate drug for patients who also have diabetes. β-Blockers and aldosterone antagonist medications are not recommended for patients with diabetes. Question 24 0 / 0 pts A primary care NP prescribes levothyroxine for a patient to treat thyroid deficiency. When teaching this patient about the medication, the NP should: Patients should be told not to change brands of the medication; there is potential variability in the bioequivalence between manufacturers. The medication should be taken at approximately the same time each day before breakfast or on an empty stomach. Patients should be instructed to contact the provider if signs of thyrotoxicosis are present. Thyroid replacement medications are usually given for life. Question 25 0 / 0 pts An 80-year-old male patient will begin taking an α-antiadrenergic medication. The primary care NP should teach this patient to: All antihypertensives can cause orthostatic hypotension, so patients should be cautioned to avoid sudden changes in position and to use caution when bathing because a hot bath or shower may aggravate dizziness. Older patients are at increased risk for falls and should be cautioned to ask for assistance. Patients taking α-antiadrenergics should consume extra fluids because dehydration can increase the risk of orthostatic hypotension. Patients should take the medication at bedtime because drowsiness is a common side effect. Priapism is not a side effect of these drugs. Question 1 0 / 0 pts A patient who will begin using nitroglycerin for angina asks the primary care NP how the medication works to relieve pain. The NP should tell the patient that nitroglycerin acts to: Nitrates relax vascular smooth muscle via stimulation of intracellular cyclic guanosine monophosphate production with the major effect being to reduce myocardial oxygen demand. Nitrates do not dissolve atheromatous lesions, prevent catecholamine release, or reduce C-reactive protein levels. UnansweredQuestion 2 0 / 0 pts A primary care NP sees a 46-year-old male patient and orders a fasting lipoprotein profile that reveals LDL of 190 mg/dL, HDL of 40 mg/dL, and triglycerides of 200 mg/dL. The patient has no previous history of coronary heart disease, but the patient’s father developed coronary heart disease at age 55 years. The NP should prescribe: HMG-CoA reductase inhibitors are used to treat hyperlipidemia when the LDL is the primary lipid elevation. This patient has risk factors of being a man older than 45 years, with a positive family history of coronary heart disease before age 55 in a male first-degree relative. Gemfibrozil is used for patients with elevated triglycerides and low HDL. Bile acid sequestrants are used as adjunctive and not first-line therapy for reducing LDL. A combination product is not indicated for first-line therapy. UnansweredQuestion 3 0 / 0 pts A patient who has a history of angina has sublingual nitroglycerin tablets to use as needed. The primary care nurse practitioner (NP) reviews this medication with the patient at the patient’s annual physical examination. Which statement by the patient indicates understanding of the medication? Although the traditional recommendation is for patients to take up to 3 nitroglycerin doses over 15 minutes before accessing emergency medical services (EMS), more recent guidelines suggest an alternative strategy to reduce delays in emergency care. These include instructions to call 9-1-1 immediately if pain persists for 5 minutes after the first dose. Aspirin is recommended when the patient is being transported to emergency care and is not recommended as an adjunct to nitroglycerin with each episode of chest pain. The three doses of nitroglycerin are given 5 minutes apart over 15 minutes. UnansweredQuestion 4 0 / 0 pts The primary care NP sees a new patient who has diabetes and hypertension and has been taking a thiazide diuretic for 6 months. The patient’s blood pressure at the beginning of treatment was 150/95 mm Hg. The blood pressure today is 138/85 mm Hg. The NP should: Evidence-based guidelines suggest that optimal control of hypertension to less than 130/80 mm Hg could prevent 37% of cardiovascular disease in men and 56% in women, so this patient, although showing improvement, could benefit from the addition of another medication. An angiotensin-converting enzyme inhibitor is an appropriate drug for patients who also have diabetes. β-Blockers and aldosterone antagonist medications are not recommended for patients with diabetes. UnansweredQuestion 5 0 / 0 pts An 80-year-old female patient with a history of angina has increased TSH and decreased T4. The primary care NP should prescribe _____ mcg of _____. Elderly individuals may experience exacerbation of cardiovascular disease and angina with thyroid hormone replacement. It is advisable to start low at 25 mcg and work up as tolerated. Liothyronine is a synthetic T3. UnansweredQuestion 6 0 / 0 pts A 45-year-old patient who has a positive family history but no personal history of coronary artery disease is seen by the primary care NP for a physical examination. The patient has a body mass index of 27 and a blood pressure of 130/78 mm Hg. Laboratory tests reveal low-density lipoprotein, 110 mg/dL; high-density lipoprotein, 70 mg/dL; and triglycerides, 120 mg/dL. The patient does not smoke but has a sedentary lifestyle. The NP should recommend: This patient is overweight but not obese, and blood lipids are within normal limits. Blood pressure is not elevated. Exercise is recommended as an initial risk reduction strategy because of its positive effects on blood pressure and blood lipids. Aspirin is generally given to patients older than 55 to 65 who are at risk. Statin medications and thiazide diuretics are not indicated. UnansweredQuestion 7 0 / 0 pts A 55-year-old patient with no prior history of hypertension has a blood pressure greater than 140/90 on three separate occasions. The patient does not smoke, has a body mass index of 24, and exercises regularly. The patient has no known risk factors for cardiovascular disease. The primary care NP should: If the patient is younger than 20 or older than 50 years old at the onset of elevated blood pressure, the NP should look for causes of secondary hypertension. The physical examination should include a careful cardiovascular assessment. This patient will need pharmacologic treatment, but not until the underlying cause of hypertension is determined. UnansweredQuestion 8 0 / 0 pts A patient who has hyperlipidemia has been taking atorvastatin (Lipitor) 60 mg daily for 6 months. The patient’s initial lipid profile showed LDL of 180 mg/dL, HDL of 45 mg/dL, and triglycerides of 160 mg/dL. The primary care NP orders a lipid profile today that shows LDL of 105 mg/dL, HDL of 50 mg/dL, and triglycerides of 120 mg/dL. The patient reports muscle pain and weakness. The NP should: Hepatotoxicity and muscle toxicity are the two primary adverse effects of greatest concern with statin use. Patients who report muscle discomfort or weakness should have a CK-MM level drawn. LFTs are indicated with signs of hepatotoxicity. It is not correct to change the dosing schedule. Gemfibrozil is not indicated. UnansweredQuestion 9 0 / 0 pts A patient with Graves’ disease is taking methimazole. After 6 months of therapy, the primary care NP notes normal T3 and T4 and elevated TSH. The NP should: Once clinical levels of thyrotoxicosis have been resolved, elevated TSH indicates a need to reduce the dosage. A CBC with differential is performed at the beginning of treatment and when signs of infection are present. Liver function tests may be monitored periodically but are not indicated by the current laboratory results. Levothyroxine is not indicated. UnansweredQuestion 10 0 / 0 pts A patient who is taking nifedipine develops mild edema of both feet. The primary care NP should contact the patient’s cardiologist to discuss: Mild to moderate peripheral edema occurs in the lower extremities in about 10% of patients; this is caused by arterial dilation, not by left ventricular dysfunction. Amlodipine is less likely to have this effect. Renal function tests are not indicated. Increasing the nifedipine dose would worsen the symptoms. UnansweredQuestion 11 0 / 0 pts A patient who has type 2 diabetes mellitus takes metformin (Glucophage). The patient tells the primary care NP that he will have surgery in a few weeks. The NP should recommend: Insulin should be considered for patients with diabetes during times of physical stress, such as illness or surgery. UnansweredQuestion 12 0 / 0 pts A primary care NP prescribes a nitroglycerin transdermal patch, 0.4 mg/hour release, for a patient with chronic stable angina. The NP should teach the patient to: To avoid tolerance, the patient should remove the patch after 12 hours. The transdermal patch is not changed four times daily or used on a prn basis. The patch is applied once daily. UnansweredQuestion 13 0 / 0 pts An African-American patient who is obese has persistent blood pressure readings greater than 150/95 mm Hg despite treatment with a thiazide diuretic. The primary care NP should consider prescribing a(n): African-American patients are considered good candidates for calcium channel blockers to treat hypertension. Treatment with calcium channel blockers as monotherapy in African-American patients has proved to be more effective than some other classes of antihypertensive agents. UnansweredQuestion 14 0 / 0 pts A child who has congenital hypothyroidism takes levothyroxine 75 mcg/day. The child weighs 15 kg. The primary care NP sees the child for a 3-year-old check-up. The NP should consult with a pediatric endocrinologist to discuss: In congenital hypothyroidism, therapy may be stopped for 2 to 8 weeks after the patient reaches 3 years of age. If TSH levels remain normal, thyroid supplementation may be discontinued permanently. UnansweredQuestion 15 0 / 0 pts An 80-year-old male patient will begin taking an α-antiadrenergic medication. The primary care NP should teach this patient to: All antihypertensives can cause orthostatic hypotension, so patients should be cautioned to avoid sudden changes in position and to use caution when bathing because a hot bath or shower may aggravate dizziness. Older patients are at increased risk for falls and should be cautioned to ask for assistance. Patients taking α-antiadrenergics should consume extra fluids because dehydration can increase the risk of orthostatic hypotension. Patients should take the medication at bedtime because drowsiness is a common side effect. Priapism is not a side effect of these drugs. UnansweredQuestion 16 0 / 0 pts A 40-year-old patient is in the clinic for a routine physical examination. The patient has a body mass index (BMI) of 26. The patient is active and walks a dog daily. A lipid profile reveals low-density lipoprotein (LDL) of 100 mg/dL, high-density lipoprotein (HDL) of 30 mg/dL, and triglycerides of 250 mg/dL. The primary care nurse practitioner (NP) should: Testing for type 2 diabetes should be considered in all adults with a BMI greater than 25 who have risk factors such as HDL less than 35 mg/dL or triglycerides greater than 250 mg/dL. A fasting plasma glucose level greater than 126 mg/dL indicates diabetes. Metformin is not indicated unless testing is positive. Lifestyle changes may be part of the treatment plan. Serum insulin level is not indicated. UnansweredQuestion 17 0 / 0 pts A patient who is newly diagnosed with type 2 diabetes mellitus has not responded to changes in diet or exercise. The patient is mildly obese and has a fasting blood glucose of 130 mg/dL. The patient has normal renal function tests. The primary care NP plans to prescribe a combination product. Which of the following is indicated for this patient? Obese patients with normal renal function and elevated fasting plasma glucose may be started on a combination of metformin and a second-generation sulfonylurea. UnansweredQuestion 18 0 / 0 pts A patient reports fatigue, weight loss, and dry skin. The primary care nurse practitioner (NP) orders thyroid function tests. The patient’s thyroid stimulating hormone (TSH) is 40 microunits/mL, and T4 is 0.1 ng/mL. The NP should refer the patient to an endocrinologist and prescribe: This patient has hypothyroidism and should be treated with levothyroxine. Methimazole is a thyroid suppressant. Liothyronine is synthetic T3. Propylthiouracil is a thyroid suppressant. UnansweredQuestion 19 0 / 0 pts A patient who has insulin-dependent type 2 diabetes reports having difficulty keeping blood glucose within normal limits and has had multiple episodes of both hypoglycemia and hyperglycemia. As adjunct therapy to manage this problem, the primary care NP should prescribe: Pramlintide is indicated in patients with type 1 diabetes and insulin-dependent type 2 diabetes and is helpful for patients with wide glycemic swings. Repaglinide requires a functioning pancreas to be effective. Glyburide and metformin are first-line oral agents and are not indicated. UnansweredQuestion 20 0 / 0 pts A patient who has primary hyperlipidemia and who takes atorvastatin (Lipitor) continues to have LDL cholesterol of 140 mg/dL after 3 months of therapy. The primary care NP increases the dose from 10 mg daily to 20 mg daily. The patient reports headache and dizziness a few weeks after the dose increase. The NP should: When used in combination with a low-dose statin, ezetimibe has been noted to produce an additional 18% reduction in LDL. Because this patient continues to have elevated LDL along with side effects of the statin, the NP should resume the lower dose of the statin and add ezetimibe. Atorvastatin is given once daily. Cholestyramine and omega-3 supplements are not indicated. UnansweredQuestion 21 0 / 0 pts A patient with primary hypercholesterolemia is taking an HMG-CoA reductase inhibitor. All of the patient’s baseline LFTs were normal. At a 6-month follow-up visit, the patient reports occasional headache. A lipid profile reveals a decrease of 20% in the patient’s LDL cholesterol. The NP should: LFTs should be performed at baseline, 12 weeks after initiation of therapy, and only periodically thereafter. Headaches are common side effects, but do not raise concern about hepatotoxicity. CK-MM tests are indicated if patients report muscle pain or weakness. It is not necessary to decrease the medication. UnansweredQuestion 22 0 / 0 pts A patient who has stable angina and uses sublingual nitroglycerin tablets is in the clinic and begins having chest pain. The primary care NP administers a nitroglycerin tablet and instructs the patient to lie down. The NP’s next action should be to: When a patient experiences an acute attack of angina in the clinic, the primary care NP should be prepared to treat the condition. After giving nitroglycerin, oxygen should be administered. An electrocardiogram is not immediately indicated. Chewable aspirin is given if the angina is unrelieved and when the patient is being transported to the hospital. EMS should be activated if there is no pain relief 5 minutes after the first dose of nitroglycerin. UnansweredQuestion 23 0 / 0 pts A patient who has stable angina is taking nitroglycerin and a β-blocker. The patient tells the primary care NP that the cardiologist is considering adding a calcium channel blocker. The NP should anticipate that the cardiologist will prescribe: Nitrates and β-blockers are first-line therapy for stable angina. Calcium channel blockers should be reserved for patients who cannot take these agents or patients whose symptoms are not controlled with these agents. Verapamil is one of the calcium channel blockers that should be used. The other calcium channel blockers are not recommended for this purpose. UnansweredQuestion 24 0 / 0 pts A 75-year-old patient who has cardiovascular disease reports insomnia and vomiting for several weeks. The primary care NP orders thyroid function tests. The tests show TSH is decreased and T4 is increased. The NP should consult with an endocrinologist and order: Patients with hyperthyroidism, or Graves’ disease, will require radioactive iodine. Elderly patients and patients with cardiovascular disease should be pretreated with an antithyroid medication such as methimazole. Thyrotropin is used to diagnose thyroid cancer. Levothyroxine is used to treat hypothyroidism. Propylthiouracil is also a thyroid suppressant, but methimazole is preferred. UnansweredQuestion 25 0 / 0 pts A primary care NP prescribes levothyroxine for a patient to treat thyroid deficiency. When teaching this patient about the medication, the NP should: Patients should be told not to change brands of the medication; there is potential variability in the bioequivalence between manufacturers. The medication should be taken at approximately the same time each day before breakfast or on an empty stomach. Patients should be instructed to contact the provider if signs of thyrotoxicosis are present. Thyroid replacement medications are usually given for life. Question 1 0 / 0 pts A patient who has disabling intermittent claudication is not a candidate for surgery. Which of the following medications should the primary care NP prescribe to treat this patient? Correct! Patients with disabling intermittent claudication who are not candidates for surgery or catheter-based intervention should be treated with cilostazol rather than pentoxifylline. Warfarin is not indicated. Patients with chronic limb ischemia are treated with lifelong aspirin therapy. Question 2 0 / 0 pts A patient who has severe arthritis and who takes nonsteroidal antiinflammatory drugs (NSAIDs) daily develops a duodenal ulcer. The patient has tried a cyclooxygenase-2 selective NSAID in the past and states that it is not as effective as the current NSAID. The primary care nurse practitioner (NP) should: You Answered Patients with NSAID-induced ulcer should discontinue the NSAID if possible and use an acid suppressant. This patient has severe arthritis and so cannot discontinue the NSAID. In a situation such as this, a PPI is indicated. Cimetidine is a histamine-2 blocker, which would be a second-line choice, but cimetidine has many serious side effects. Bland diets are not effective in treating ulcers. Corticosteroids are not indicated. Question 3 0 / 0 pts A patient in the clinic reports heartburn 30 minutes after meals, a feeling of fullness, frequent belching, and a constant sour taste. The patient has a normal weight and reports having a high-stress job. The primary care NP should recommend: This patient has symptoms of GERD. PPIs are first-line medications for treating GERD and may be started empirically. Antacids are not first-line medications. Changes in diet are not recommended as treatment but may help with symptoms. Patients with symptoms unrelieved by PPIs should be referred for possible endoscopy. Question 4 0 / 0 pts A patient who has gastroesophageal reflux disease (GERD) undergoes an endoscopy, which shows a hiatal hernia. The patient is mildly obese. The patient asks the primary care nurse practitioner (NP) about treatment options. The NP should tell this patient that: Correct! People with GERD often have hiatal hernia, but this is not the cause of GERD. The approach to treatment of GERD may include lifestyle changes, medications, and surgery. OTC antacids are sometimes used but are rarely used as first-line treatment. Question 5 0 / 0 pts A patient who takes a thiazide diuretic will begin taking an ACE inhibitor. The primary care NP should counsel the patient to: ACE inhibitors have a first-dose effect that may cause a precipitous symptomatic fall in blood pressure, particularly in patients receiving diuretics. The patient should be counseled about rising quickly from sitting or lying down. Wheezing and shortness of breath are unlikely. An increased dose of diuretic and a reduction in fluid intake are not indicated and may add to hypotension. Question 6 0 / 0 pts A patient comes to the clinic with a 4-day history of 10 to 12 liquid stools each day. The patient reports seeing blood and mucus in the stools. The patient has had nausea but no vomiting. The primary care NP notes a temperature of 37.9° C, a heart rate of 96 beats per minute, and a blood pressure of 90/60 mm Hg. A physical examination reveals dry oral mucous membranes and capillary refill of 4 seconds. The NP’s priority should be to: Acute diarrhea is usually mild and self-limited. Nonpharmacologic measures, especially bowel rest and adequate hydration, are helpful and should be a priority. Stool cultures may be ordered after hydration therapy is begun. Metronidazole is indicated if C. difficile is present. Opioid antidiarrheals may prolong symptoms. Question 7 0 / 0 pts A patient is in the clinic for an annual physical examination. The primary care NP obtains a medication history and learns that the patient is taking a β-blocker and nitroglycerin. The NP orders laboratory tests, performs a physical examination, and performs a review of systems. Which finding may warrant discontinuation of the β-blocker in this patient? β-Blockers may cause bronchospasm in susceptible patients, and discontinuation of the β-blocker may be required. β-Blockers may cause an insignificant increase in serum triglycerides. Exercise intolerance, fatigue, and gastrointestinal side effects are common. Question 8 0 / 0 pts The primary care NP sees a patient who has a history of hypertension and alcoholism. The patient is not taking any medications. The NP auscultates crackles in both lungs and palpates the liver 2 cm below the costal margin. Laboratory tests show an elevated creatinine level. The NP will refer this patient to a cardiologist and should prescribe: In the treatment of heart failure, loop diuretics relieve the congestive symptoms of pulmonary and congestive edema. Loop diuretics are also useful to treat states of volume excess in cirrhosis and renal insufficiency. Because this patient has a history of alcoholism and has an enlarged liver on examination, furosemide is a good first choice to relieve this patient’s congestive symptoms. Spironolactone and chlorthalidone are not loop diuretics. Albuterol might be used for symptomatic treatment only. Question 9 0 / 0 pts The primary care NP is considering prescribing captopril (Capoten) for a patient. The NP learns that the patient has decreased renal function and has renal artery stenosis in the right kidney. The NP should: Correct! Question 10 0 / 0 pts A patient who has had four to five liquid stools per day for 4 days is seen by the primary care NP. The patient asks about medications to stop the diarrhea. The NP tells the patient that antidiarrheal medications are: Treatment of patients with acute diarrhea with antidiarrheals can prolong infection and should be avoided if possible. Antidiarrheals are best used in patients with mild to moderate diarrhea and are used for comfort and not cure. They should not be used for patients with bloody diarrhea or high fever because they can worsen the disease. Prolonged diarrhea can indicate a more serious cause, and antidiarrheals should not be used in those cases. Question 11 0 / 0 pts A patient has been taking antibiotics to treat recurrent pneumonia. The patient is in the clinic after having diarrhea for 5 days with six to seven liquid stools each day. The primary care NP should: Correct! The guidelines for treatment of diarrhea emphasize comprehensive evaluation before treatment begins. Antibiotic use points to C. difficile as a possible cause, and metronidazole is often used to treat mild to moderate infection. Vancomycin is used when C. difficile is severe. Diphenoxylate can worsen the infection because it slows transit time of the bacteria in the gut. Prolonged diarrhea during antibiotic therapy should be investigated. Question 12 0 / 0 pts A primary care NP sees a patient who is about to take a cruise and reports having had motion sickness with nausea on a previous cruise. The NP prescribes the scopolamine transdermal patch and should instruct the patient to apply the patch: The transdermal system allows steady-state plasma levels of scopolamine to be reached rapidly and maintained for 3 days. The onset of action is approximately 4 hours. The patch should be changed every 3 days and left on at all times, not as needed. Question 13 0 / 0 pts A patient who has been taking propranolol for 6 months reports having nocturnal cough and shortness of breath. The primary care NP should: Nocturnal cough and shortness of breath may be a side effect of propranolol, which can cause bronchospasm because it is a nonselective â-blocker. The NP should discuss a selective β-blocker with the patient’s cardiologist. â-Blockers should never be stopped abruptly. Bradycardia and hypotension are signs of toxicity. Increasing activity would not counter these side effects if bronchospasm is the cause. Question 14 0 / 0 pts A patient who has GERD with erosive esophagitis has been taking a PPI for 4 weeks and reports a decrease in symptoms. The patient asks the primary care NP if the medication may be discontinued. The NP should tell the patient that: Once PPIs have proven clinically effective for treatment of patients with esophagitis, therapy should be continued long-term and titrated down to the lowest effective dose based on symptom control. PPI therapy is considered safer than surgery and should be tried first before surgery is performed. GERD is a lifelong syndrome and is not curable. Question 15 0 / 0 pts A patient reports having episodes of dizziness, nausea, and lightheadedness and describes a sensation of the room spinning when these occur. The primary care NP will refer the patient to a specialist who, after diagnostic testing, is likely to prescribe: Correct! Patients with vertigo may experience whirling or a feeling of the room spinning around. In true vertigo, the patient can identify the direction in which the room is spinning. Anticholinergics are the most effective agents in cases of motion sickness or vertigo. Meclizine has a specific indication to treat vertigo. Question 16 0 / 0 pts A patient comes to the clinic with a complaint of gradual onset of left-sided weakness. The primary care NP notes slurring of the patient’s speech. A family member accompanying the patient tells the NP that these symptoms began 4 or 5 hours ago. The NP will activate the emergency medical system and expect to administer: Alteplase is used to treat ischemic stroke but is contraindicated if onset of symptoms occurred 3 hours previously. The administration of anticoagulation or antiplatelet agents during the first 24 hours is not recommended. The oral administration of aspirin within 24 to 48 hours after stroke onset is recommended. Question 17 0 / 0 pts A patient who is taking an oral anticoagulant is in the clinic in the late afternoon and reports having missed the morning dose of the medication because the prescription was not refilled. The primary care NP should counsel this patient to: Consistency is the key to successful warfarin treatment, and the patient should take the medication at the same time every day. For missed doses, the patient should take the medication as soon as possible after the missed dose or not at all that day. Because it is late afternoon, the patient should skip the dose and resume normal scheduling the next day. It is not necessary to avoid foods high in vitamin K. Patients should not double up the next day. Question 18 0 / 0 pts A patient who has congestive heart failure and arthritis has been taking chlorthalidone (Zaroxolyn) 25 mg daily for 6 months. The primary care NP notes a persistent blood pressure of 145/90 mm Hg. The NP should: For diuretic resistance, the NP should evaluate factors such as patient nonadherence, physiologic causes, and drugs that may increase resistance, including nonsteroidal antiinflammatory drugs (NSAIDs). This patient has arthritis, and it is likely that NSAID use may be causing diuretic resistance. A second drug, such as furosemide, should be added after the cause of diuretic resistance is determined. The maximum daily dose of chlorthalidone is 100 mg per day, but increasing the dose is not recommended to treat diuretic resistance. Recommending salt substitutes is not indicated. Question 19 0 / 0 pts An 80-year-old patient who has persistent AF takes warfarin (Coumadin) for anticoagulation therapy. The patient has an INR of 3.5. The primary care NP should consider: This patient’s INR is only minimally prolonged, so no dose reduction is required. The NP should recheck the INR periodically. If the INR becomes more prolonged, lowering the dose of warfarin is recommended. If the INR approaches 5, omitting a dose and resuming at a lower dose is recommended. Vitamin K is used for an INR of 9 or greater. Question 20 0 / 0 pts A 2-year-old child has chronic “toddler’s” diarrhea, which has an unknown but benign etiology. The child’s parent asks the primary care NP if a medication can be used to treat the child’s symptoms. The NP should recommend giving: Correct! Antidiarrheals are not recommended in children. Opioids are contraindicated in children younger than 2 years. Bismuth and attapulgite are not recommended in children younger than 3 years of age. Oral rehydration with electrolyte solution is safe for young children. Question 21 0 / 0 pts The primary care NP refers a patient to a cardiologist who diagnoses long QT syndrome. The cardiologist has prescribed propranolol (Inderal). The patient exercises regularly and is not obese. The patient asks the NP what else can be done to minimize risk of sudden cardiac arrest. The NP should counsel the patient to: Patients with long QT syndrome should avoid situations in which they might overheat or get dehydrated. This patient should be encouraged to drink plenty of fluids while exercising and should avoid activities such as yoga and hot baths. Implantable cardioverter-defibrillators are used for high-risk patients. Procainamide can cause long QT syndrome. Question 22 0 / 0 pts A patient takes an antispasmodic and an occasional antidiarrheal medication to treat IBS. The patient comes to the clinic and reports having dry mouth, difficulty urinating, and more frequent constipation. The primary care NP notes a heart rate of 92 beats per minute. The NP should: Patients taking antispasmodic medications should be monitored for anticholinergic side effects, such as increased heart rate, dry mouth, difficulty urinating, and constipation. The NP should lower the dose if needed. TCAs are used to treat pain long-term. Because the antidiarrheal medication is used as needed, there is no reason to discontinue it. Increasing water intake may improve symptoms associated with side effects but would not treat the underlying cause of these symptoms. Question 23 0 / 0 pts A patient who has been taking quinidine for several years reports lightheadedness, fatigue, and weakness. The primary care NP notes a heart rate of 110 beats per minute. The serum quinidine level is 6 μg/mL. The NP should: The therapeutic level for quinidine is 2 to 5 ìg/mL. Some patients have therapeutic responses at up to 6 μg/mL. The NP should order ECG, CBC, LFT, and renal function tests. Question 24 0 / 0 pts An 80-year-old patient with chronic stable angina has begun taking nadolol (Corgard) 20 mg once daily in addition to taking nitroglycerin as needed. After 1 week, the patient reports no change in frequency of nitroglycerin use. The primary care nurse practitioner (NP) should change the dose of nadolol to _____ mg _____ daily. β-Blockers are the treatment of choice for chronic stable and unstable angina. Their therapeutic effect is dose dependent, and drug titration should be based on frequency of angina symptoms and nitroglycerin use. Nadolol should be started at 20 mg daily for elderly patients when treating angina and should be increased by 20 mg every 3 to 7 days if symptoms do not improve. Nadolol is given once daily. Question 25 0 / 0 pts A woman has severe IBS and takes hyoscyamine sulfate (Levsin), simethicone (Phazyme), and a TCA. She reports having continued severe diarrhea. The primary care NP should: Alosetron is given only to women with severe chronic diarrhea-predominant IBS and only after anatomic or biochemical abnormalities of the GI tract have been excluded. Because this woman’s symptoms are persistent and severe, diphenoxylate and increased dietary fiber are not indicated. Question 1 0 / 0 pts A patient reports having episodes of dizziness, nausea, and lightheadedness and describes a sensation of the room spinning when these occur. The primary care NP will refer the patient to a specialist who, after diagnostic testing, is likely to prescribe: Patients with vertigo may experience whirling or a feeling of the room spinning around. In true vertigo, the patient can identify the direction in which the room is spinning. Anticholinergics are the most effective agents in cases of motion sickness or vertigo. Meclizine has a specific indication to treat vertigo. UnansweredQuestion 2 0 / 0 pts A patient who has been taking digoxin 0.25 mg daily for 6 months reports that it is not working as well as it did initially. The primary care NP should: Clinicians should be aware that generic digoxin marketed by different companies may not be bioequivalent to the branded digoxin (Lanoxin). Patients with hyperkalemia would show intensified effects, not diminished effects of digoxin. Patients with diminished effects may have received a generic brand. It is not correct to increase the dose of digoxin without first obtaining a digoxin level. Because this patient is reporting decreased effects, it is unnecessary to suspect toxicity. UnansweredQuestion 3 0 / 0 pts A patient who takes digoxin reports taking psyllium (Metamucil) three or four times each month for constipation. The primary care NP should counsel this patient to: Laxatives can affect the absorption of drugs in the intestine by decreasing transit time. Digoxin is a drug that is affected by decreased transit time. Patients should be counseled to take the drugs 2 hours apart. UnansweredQuestion 4 0 / 0 pts A patient comes to the clinic with a 4-day history of 10 to 12 liquid stools each day. The patient reports seeing blood and mucus in the stools. The patient has had nausea but no vomiting. The primary care NP notes a temperature of 37.9° C, a heart rate of 96 beats per minute, and a blood pressure of 90/60 mm Hg. A physical examination reveals dry oral mucous membranes and capillary refill of 4 seconds. The NP’s priority should be to: Acute diarrhea is usually mild and self-limited. Nonpharmacologic measures, especially bowel rest and adequate hydration, are helpful and should be a priority. Stool cultures may be ordered after hydration therapy is begun. Metronidazole is indicated if C. difficile is present. Opioid antidiarrheals may prolong symptoms. UnansweredQuestion 5 0 / 0 pts A 2-year-old child has chronic “toddler’s” diarrhea, which has an unknown but benign etiology. The child’s parent asks the primary care NP if a medication can be used to treat the child’s symptoms. The NP should recommend giving: Antidiarrheals are not recommended in children. Opioids are contraindicated in children younger than 2 years. Bismuth and attapulgite are not recommended in children younger than 3 years of age. Oral rehydration with electrolyte solution is safe for young children. UnansweredQuestion 6 0 / 0 pts A primary care NP sees a patient 2 days after an outpatient surgical procedure. The patient reports using ondansetron for nausea. The NP notes a blood pressure of 88/56 mm Hg, and the patient reports feeling faint. The NP should suspect: Hypotension and faintness are signs of overdose of ondansetron, and drug toxicity is the more likely cause of this patient’s decrease in blood pressure. UnansweredQuestion 7 0 / 0 pts A patient with a previous history of myocardial infarction (MI) who takes nitroglycerin for angina develops hypertension. The primary care NP is considering ordering an ACE inhibitor. Preliminary laboratory tests reveal decreased renal function. The NP should: ACE inhibitors are contraindicated in patients with bilateral renal stenosis. Because this patient has decreased renal function, perfusion studies are indicated. If the patient does not have bilateral renal stenosis, a low-dose ACE inhibitor may be used. An ARB is indicated if perfusion studies show bilateral renal stenosis. A thiazide diuretic is not indicated. UnansweredQuestion 8 0 / 0 pts A patient who has migraine headaches has begun taking timolol and 2 months after beginning this therapy reports no change in frequency of migraines. The patient’s current dose is 30 mg once daily. The primary care NP should: When giving timolol for migraine prophylaxis, the provider should inform the patient that it may take several weeks for therapy to be effective. The dose should be titrated and maintained for a minimum of 3 months before the treatment is deemed a failure. It may be necessary to change to propranolol if the therapy is not effective in 1 month. The maximum dose of timolol for migraine prophylaxis is 30 mg. Drug effectiveness is determined by patient response, not serum drug levels. UnansweredQuestion 9 0 / 0 pts The primary care NP sees a patient who has heart failure following an MI 6 months before this visit. The patient has been taking an ACE inhibitor, nitroglycerin, furosemide, and hydrochlorothiazide. The NP auscultates crackles in both lungs and notes pitting edema of both feet. The NP should prescribe: Spironolactone has been shown to be of particular benefit in the treatment of severe congestive heart failure when added to an ACE inhibitor and a loop diuretic. UnansweredQuestion 10 0 / 0 pts A patient has been taking antibiotics to treat recurrent pneumonia. The patient is in the clinic after having diarrhea for 5 days with six to seven liquid stools each day. The primary care NP should: The guidelines for treatment of diarrhea emphasize comprehensive evaluation before treatment begins. Antibiotic use points to C. difficile as a possible cause, and metronidazole is often used to treat mild to moderate infection. Vancomycin is used when C. difficile is severe. Diphenoxylate can worsen the infection because it slows transit time of the bacteria in the gut. Prolonged diarrhea during antibiotic therapy should be investigated. UnansweredQuestion 11 0 / 0 pts A patient who has cerebral palsy is wheelchair dependent and receives enteral nutrition via a gastrostomy tube. The patient has infrequent, hard bowel movements despite using a high-fiber formula and receiving 1500 mL of fluid per day. The NP should order: Fluids, fiber, and exercise, which help most people, are not applicable to people who are wheelchair bound. Other individuals with congestive heart failure are unable to tolerate these mechanisms. Osmotic laxatives, such as polyethylene glycol are used to manage long-term constipation. It is essential for clinicians to know their patients and assess what is reasonable for them to do. UnansweredQuestion 12 0 / 0 pts A patient reports having occasional acute constipation with large, hard stools and pain and asks the primary care NP about medication to treat this condition. The NP learns that the patient drinks 1500 mL of water daily; eats fruits, vegetables, and bran; and exercises regularly. The NP should recommend: Mild short-term constipation may be treated with a saline laxative or a bulk laxative as needed. Daily laxatives are not recommended. Glycerin suppositories can cause irritation of the rectum with long-term use. UnansweredQuestion 13 0 / 0 pts A primary care NP sees a patient who is about to take a cruise and reports having had motion sickness with nausea on a previous cruise. The NP prescribes the scopolamine transdermal patch and should instruct the patient to apply the patch: The transdermal system allows steady-state plasma levels of scopolamine to be reached rapidly and maintained for 3 days. The onset of action is approximately 4 hours. The patch should be changed every 3 days and left on at all times, not as needed. UnansweredQuestion 14 0 / 0 pts A patient who is taking an oral anticoagulant is in the clinic in the late afternoon and reports having missed the morning dose of the medication because the prescription was not refilled. The primary care NP should counsel this patient to: Consistency is the key to successful warfarin treatment, and the patient should take the medication at the same time every day. For missed doses, the patient should take the medication as soon as possible after the missed dose or not at all that day. Because it is late afternoon, the patient should skip the dose and resume normal scheduling the next day. It is not necessary to avoid foods high in vitamin K. Patients should not double up the next day. UnansweredQuestion 15 0 / 0 pts A primary care NP is preparing to order digoxin for an 80-year-old patient who has systolic heart failure. The NP obtains renal function tests, which are normal. The NP should: In primary care settings, slow digitalization rather than a loading dose is generally recommended because of the risk of toxicity. Digitalization may be achieved within 1 week with the use of small daily maintenance doses. UnansweredQuestion 16 0 / 0 pts A primary care NP sees a 3-year-old patient who has been vomiting for several days. The child has had fewer episodes of vomiting the past day and is now able to take sips of fluids without vomiting. The child has dry oral mucous membranes, 2-second capillary refill, and pale but warm skin. The child’s blood pressure is 88/46 mm Hg, the heart rate is 110 beats per minute, and the temperature is 37.2° C. The NP should: The use of antiemetics in children is discouraged for cases of uncomplicated vomiting. The child has compensated, mild dehydration and is now able to tolerate fluids, so oral rehydration is indicated. UnansweredQuestion 17 0 / 0 pts A patient who has type 2 diabetes is seen by a primary care NP for a physical examination. The NP notes a blood pressure of 140/95 mm Hg on three occasions. A urinalysis reveals macroalbuminuria. The patient’s serum creatinine is 1.9 mg/dL. Adhering to evidence-based practice, the NP should prescribe: In patients with type 2 diabetes, hypertension, macroalbuminuria, and renal insufficiency (serum creatinine 1.5 mg/dL), ARBs have been shown to delay the progression of nephropathy. Losartan is an ARB. The other medications are ACE inhibitors. UnansweredQuestion 18 0 / 0 pts A patient who has severe arthritis and who takes nonsteroidal antiinflammatory drugs (NSAIDs) daily develops a duodenal ulcer. The patient has tried a cyclooxygenase-2 selective NSAID in the past and states that it is not as effective as the current NSAID. The primary care nurse practitioner (NP) should: Patients with NSAID-induced ulcer should discontinue the NSAID if possible and use an acid suppressant. This patient has severe arthritis and so cannot discontinue the NSAID. In a situation such as this, a PPI is indicated. Cimetidine is a histamine-2 blocker, which would be a second-line choice, but cimetidine has many serious side effects. Bland diets are not effective in treating ulcers. Corticosteroids are not indicated. UnansweredQuestion 19 0 / 0 pts A patient who has been taking propranolol for 6 months reports having nocturnal cough and shortness of breath. The primary care NP should: Nocturnal cough and shortness of breath may be a side effect of propranolol, which can cause bronchospasm because it is a nonselective â-blocker. The NP should discuss a selective β-blocker with the patient’s cardiologist. â-Blockers should never be stopped abruptly. Bradycardia and hypotension are signs of toxicity. Increasing activity would not counter these side effects if bronchospasm is the cause. UnansweredQuestion 20 0 / 0 pts A patient who is at risk for DVT tells the primary care NP she has just learned she is pregnant. The NP should expect that this patient will use which of the following anticoagulant medications? Heparin does not cross the placental barrier and is the drug of choice for anticoagulation therapy during pregnancy, despite its category C classification. Aspirin is not recommended during the last 3 months of pregnancy. Dabigatran is not recommended. Warfarin crosses the placental barrier. UnansweredQuestion 21 0 / 0 pts An 80-year-old patient has begun taking propranolol (Inderal) and reports feeling tired all of the time. The primary care NP should: Elderly patients have described sedation and sleep disturbances with β-blockers. Elderly patients often need lower doses of these drugs. Patients should not be advised to discontinue the medication abruptly. UnansweredQuestion 22 0 / 0 pts A postmenopausal woman develops NSAID-induced ulcer. The primary care NP should prescribe: PPIs carry a possible increased risk of fractures in postmenopausal women. The NP should begin therapy with a histamine-2 blocker, such as ranitidine. UnansweredQuestion 23 0 / 0 pts A patient takes hydrochlorothiazide to treat hypertension and asks the primary care NP why it is necessary to reduce sodium intake while taking this medication. The NP should explain that decreasing sodium is necessary to: If dietary salt intake is high, the amount of sodium lost in response to the diuretic may be partially or completely offset by postdiuretic sodium retention. Sodium restriction does not prevent renal insufficiency or minimize the incidence of hypokalemia. Sodium restriction is necessary to maintain the drug’s effectiveness but does not increase the chance of discontinuing the medication. UnansweredQuestion 24 0 / 0 pts A patient comes to the clinic with a complaint of gradual onset of left-sided weakness. The primary care NP notes slurring of the patient’s speech. A family member accompanying the patient tells the NP that these symptoms began 4 or 5 hours ago. The NP will activate the emergency medical system and expect to administer: Alteplase is used to treat ischemic stroke but is contraindicated if onset of symptoms occurred 3 hours previously. The administration of anticoagulation or antiplatelet agents during the first 24 hours is not recommended. The oral administration of aspirin within 24 to 48 hours after stroke onset is recommended. UnansweredQuestion 25 0 / 0 pts A patient who has diabetic gastroparesis sees a gastroenterology specialist who orders metoclopramide (Reglan). Within 24 hours, the patient describes having extrapyramidal symptoms (EPS) to the primary care NP. The NP will contact the gastroenterologist and should expect to prescribe: Cogentin is indicated to treat EPS side effects of medications such as metoclopramide. The patient should be monitored during the first 24 to 48 hours for any adverse reactions. Should EPS occur, treat with intramuscular diphenhydramine (Benadryl) 50 mg or benztropine (Cogentin) 1 to 2 mg Question 1 2 / 2 pts A primary care NP is developing a clinical practice guideline for management of a patient population in a midsized suburban hospital. The NP should: Clinical guidelines should be written using all available evidence as well as expert opinion. Existing guidelines from a different type of hospital may not be based on data generalizable to this population. Third-party payer guidelines are usually weighted toward decreased costs. Long-standing protocols often do not take into account current knowledge and research. Question 2 2 / 2 pts A primary care NP prescribes a nitroglycerin transdermal patch, 0.4 mg/hour release, for a patient with chronic stable angina. The NP should teach the patient to: To avoid tolerance, the patient should remove the patch after 12 hours. The transdermal patch is not changed four times daily or used on a prn basis. The patch is applied once daily. Question 3 2 / 2 pts A patient is diagnosed with asthma. The primary care nurse practitioner (NP) prescribes an inhaled corticosteroid and an inhaled bronchodilator medication and provides education about how to use inhalers. At a follow-up visit 2 weeks later, the patient’s pulmonary function tests are worse. The NP should: Follow-up visits present an opportunity for the NP to evaluate learning. A first step when symptoms have not improved is to ask the patient to describe what he or she does. A detailed written plan and a review of asthma symptoms are a part of education but should have been given at the initial visit along with hands-on instruction and demonstrations. Until it is determined whether or not the patient understands and follows the prescribed regimen, it is not correct to change the plan of care. Question 4 2 / 2 pts A patient who will undergo surgery in implant a biosynthetic heart valve asks the primary care NP whether any medications will be necessary postoperatively. The NP should tell the patient that it will be necessary to take: Patients with biosynthetic valves should receive anticoagulation for 3 months with long-term aspirin prophylaxis. Patients with biosynthetic valves should receive anticoagulation for 3 months (INR goal, 2 to 3). Long-term prophylaxis for these patients should include aminosalicylic acid (75 to 100 mg daily), unless AF is present. Question 5 2 / 2 pts A patient has a BMI of 35, a fasting plasma glucose of 120 mg/dL, elevated triglycerides, and a history of myocardial infarction. The primary care NP plans to initiate dietary and lifestyle counseling and should consider prescribing: Patients who take Onexa have shown improvement in blood glucose levels and triglyceride levels, so this combination is a good choice for this patient. Question 6 2 / 2 pts A patient who has severe arthritis and who takes nonsteroidal antiinflammatory drugs (NSAIDs) daily develops a duodenal ulcer. The patient has tried a cyclooxygenase-2 selective NSAID in the past and states that it is not as effective as the current NSAID. The primary care nurse practitioner (NP) should: Patients with NSAID-induced ulcer should discontinue the NSAID if possible and use an acid suppressant. This patient has severe arthritis and so cannot discontinue the NSAID. In a situation such as this, a PPI is indicated. Cimetidine is a histamine-2 blocker, which would be a second-line choice, but cimetidine has many serious side effects. Bland diets are not effective in treating ulcers. Corticosteroids are not indicated. Question 7 2 / 2 pts A patient comes to the clinic reporting dizziness and fatigue associated with nausea and vomiting. The primary care NP suspects anemia and orders a complete blood count. The patient’s hemoglobin is elevated. The NP correctly concludes that the patient is not anemic. The NP has made an error in: Faulty hypothesis triggering occurs when the clinician fails to consider appropriate initial hypotheses. The patient had nausea and vomiting, which can cause dehydration, leading to orthostatic hypotension and dizziness. The NP made an assumption that the dizziness was caused by anemia and ordered a complete blood count. Faulty information gathering occurs when clinicians fail to order appropriate tests. An error in context formulation occurs when clinicians and patients have different goals. Errors in knowledge base would occur if the practitioner did not perform a complete history and physical, missing important information. An error in cost-versus-benefit analysis could occur if the clinician ordered expensive tests that were not necessary for diagnosis and treatment. Question 8 2 / 2 pts A patient who has diabetes is taking metformin 1000 mg daily. At a clinic visit, the patient reports having abdominal pain and nausea. The primary care NP notes a heart rate of 92 beats per minute. The NP should: Symptoms of lactic acidosis include nausea, abdominal pain, and tachycardia. Tests should include electrolytes, ketones, and serum glucose. Question 9 2 / 2 pts An 80-year-old patient asks a primary care NP about OTC antacids for occasional heartburn. The NP notes that the patient has a normal complete blood count and normal electrolytes and a slight elevation in creatinine levels. The NP should recommend: Elderly patients with renal failure should not take antacids containing magnesium because of the risk of hypermagnesemia. Sodium-containing antacids may cause fluid retention in elderly patients. Aluminum hydroxide is not as effective as calcium carbonate. Question 10 2 / 2 pts A patient who has angina is taking nitroglycerin and long-acting nifedipine. The primary care NP notes a persistent blood pressure of 90/60 mm Hg at several follow-up visits. The patient reports lightheadedness associated with standing up. The NP should consult with the patient’s cardiologist about changing the medication to: Verapamil and diltiazem are less likely to cause hypotension than nifedipine and related drugs, such as isradipine and amlodipine. Question 11 2 / 2 pts A patient comes to the clinic to discuss weight loss. The primary care NP notes a BMI of 32 and performs a health risk assessment that reveals no obesity-related risk factors. The NP should recommend: This patient is grade 2 overweight (obese), so a short-term course of phentermine is useful, especially as there are no cardiovascular risk factors. Orlistat is a second-line drug. Surgical intervention is indicated when other therapies fail. Changes in diet and physical activity alone do not bring immediate results, and patients often get discouraged. Question 12 2 / 2 pts A patient brings written information about a medication to a primary care NP about a new drug called Prism and wants to know if the NP will prescribe it. The NP notes that the information is from an internet site called “Prism.com.” The NP should tell this patient that: Commercial internet sites are identifiable by “com” at the end of their web address. Many provide reliable information, but others may be more interested in selling something. Nonprofit groups use “org” at the end of their web addresses. Internet information is reliable as long as the internet user is aware of how things are posted and by whom. Question 13 2 / 2 pts A primary care NP is preparing to order digoxin for an 80-year-old patient who has systolic heart failure. The NP obtains renal function tests, which are normal. The NP should: In primary care settings, slow digitalization rather than a loading dose is generally recommended because of the risk of toxicity. Digitalization may be achieved within 1 week with the use of small daily maintenance doses. Question 14 2 / 2 pts A patient who weighs 170 lb wishes to lose weight, with a target weight goal of 125 lb. To initiate a program that will result in a loss of 1 lb per week, the primary care NP should recommend a dietary intake of _____ kcal. To lose weight, a patient must decrease intake to below the level needed to maintain weight. The patient must decrease daily calorie consumption by 500 kcal for each pound he or she wishes to lose weekly. Because it takes approximately 10 kcal per pound to maintain weight, the NP can assume that the patient currently takes in 1700 kcal/day and should recommend a diet of 1200 kcal/day for weight loss. Question 15 2 / 2 pts A primary care nurse practitioner (NP) prescribes a drug to an 80-year-old African-American woman. When selecting a drug and determining the correct dose, the NP should understand that the knowledge of how age, race, and gender may affect drug excretion is based on an understanding of: Pharmacokinetics is the study of the action of drugs in the body and may be thought of as what the body does to the drug. Factors such as age, race, and gender may change the way the body acts to metabolize and excrete a drug. Bioavailability refers to the amount of drug available at the site of action. Pharmacodynamics is the study of the effects of drugs on the body. Anatomy and physiology is a basic understanding of how the body functions. Question 16 2 / 2 pts A patient who takes a calcium channel blocker is in the clinic for an annual physical examination. The cardiovascular examination is normal. As part of routine monitoring for this patient, the primary care NP should evaluate: Patients who take calcium channel blockers should have periodic renal and LFTs. Question 17 2 / 2 pts A patient has been diagnosed with IBS and tells the primary care NP that symptoms of diarrhea and cramping are worsening. The patient asks about possible drug therapy to treat the symptoms. The NP should prescribe: Dicyclomine has indirect and direct effects on the smooth muscle of the gastrointestinal (GI) tract. Both actions help to relieve smooth muscle spasm. Mesalamine is used to treat ulcerative colitis. Simethicone acts locally to treat symptoms of trapped air and gas. Metoclopramide is used to increase motility. Question 18 2 / 2 pts A patient who is taking an oral anticoagulant is in the clinic in the late afternoon and reports having missed the morning dose of the medication because the prescription was not refilled. The primary care NP should counsel this patient to: Consistency is the key to successful warfarin treatment, and the patient should take the medication at the same time every day. For missed doses, the patient should take the medication as soon as possible after the missed dose or not at all that day. Because it is late afternoon, the patient should skip the dose and resume normal scheduling the next day. It is not necessary to avoid foods high in vitamin K. Patients should not double up the next day. Question 19 2 / 2 pts A patient who takes spironolactone for heart failure has begun taking digoxin (Lanoxin) for atrial fibrillation. The primary care NP provides teaching for this patient and asks the patient to repeat back what has been learned. Which statement by the patient indicates understanding of the teaching? Correct! Patients should be taught to reduce their overall sodium intake by avoiding salty foods and not adding salt while cooking. Spironolactone is a potassium-sparing diuretic and carries a risk of hyperkalemia, which can make the myocardium more sensitive to the effects of digoxin. Hypercalcemia can predispose the patient to digoxin toxicity. Salt substitutes are high in potassium. Question 20 2 / 2 pts The primary care NP sees a new African-American patient who has blood pressure readings of 140/90 mm Hg, 130/85 mm Hg, and 142/80 mm Hg on three separate occasions. The NP learns that the patient has a family history of hypertension. The NP should: African Americans tend to respond better than whites to diuretic monotherapy, so this is an appropriate starting therapy. Calcium-channel blockers and ARBs are preferred as adjunct medications in African Americans. Question 21 2 / 2 pts An African-American patient is taking captopril (Capoten) 25 mg twice daily. When performing a physical examination, the primary care nurse practitioner (NP) learns that the patient continues to have blood pressure readings of 135/90 mm Hg. The NP should: Some African-American patients do not appear to respond as well as whites in terms of blood pressure reduction. The addition of a low-dose thiazide diuretic often allows for efficacy in blood pressure lowering that is comparable with that seen in white patients. Increasing the captopril dose is not indicated. Losartan is an angiotensin receptor blocker (ARB) and is not indicated in this case. Question 22 2 / 2 pts A patient who has a history of chronic constipation uses a bulk laxative to prevent episodes of acute constipation. The patient reports having an increased frequency of episodes. The primary care NP should recommend: Patients treated for long-term constipation should begin with a bulk laxative. If that is not effective, the addition of a second laxative may be necessary. Using two laxatives from the same category is not recommended. A stool softener, such as docusate sodium, is appropriate. Bisacodyl is not a second-line treatment. Lactulose and polyethylene glycol are from the same category. Question 23 2 / 2 pts A woman with IBS has been taking antispasmodic medications and reports some relief, but she tells the primary care NP that the disease is interfering with her ability to work because of increased pain. The NP should consider prescribing: TCAs and selective serotonin reuptake inhibitors (SSRIs) have been shown to reduce symptoms and are useful for long-term treatment. Alosetron is ordered by a GI specialist if symptoms are resistant to all other interventions and has been shown to be effective in women with diarrhea-predominant IBS. Misoprostol is used to treat NSAID-induced ulcers. Simethicone acts locally to treat symptoms of trapped air and gas. Question 24 2 / 2 pts A 55-year-old woman has not had menstrual periods for 5 years and tells the primary care nurse practitioner (NP) that she is having increasingly frequent vasomotor symptoms. She has no family history or risk factors for coronary heart disease (CHD) or breast cancer but is concerned about these side effects of hormone therapy (HT). The NP should: The current gap hypothesis regarding breast cancer supports initiating HT 5 years or more after menopause. To decrease risk for CHD, HT should begin at the time of menopause. HT will relieve vasomotor symptoms at all stages of menopause. Herbal supplements have estrogenizing effects and carry the same risks as estrogen therapy. Question 25 2 / 2 pts A patient who has atrial fibrillation (AF) has been taking warfarin (Coumadin). The primary care nurse practitioner (NP) plans to change the patient’s medication to dabigatran (Pradaxa). To do this safely, the NP should: There are no requirements for monitoring the INR or other measures for patients taking dabigatran. When changing from warfarin, it is recommended that dabigatran be initiated when the INR is less than 2. Question 26 2 / 2 pts A 45-year-old patient who has a positive family history but no personal history of coronary artery disease is seen by the primary care NP for a physical examination. The patient has a body mass index of 27 and a blood pressure of 130/78 mm Hg. Laboratory tests reveal low-density lipoprotein, 110 mg/dL; high-density lipoprotein, 70 mg/dL; and triglycerides, 120 mg/dL. The patient does not smoke but has a sedentary lifestyle. The NP should recommend: This patient is overweight but not obese, and blood lipids are within normal limits. Blood pressure is not elevated. Exercise is recommended as an initial risk reduction strategy because of its positive effects on blood pressure and blood lipids. Aspirin is generally given to patients older than 55 to 65 who are at risk. Statin medications and thiazide diuretics are not indicated. Question 27 2 / 2 pts A sexually active patient tells the primary care NP that she has been unable to get her new COCP pill pack until today and has missed 3 days of pills. The NP should tell her to: Patients who miss 2 or more pills at the beginning or end of a pack should use emergency contraceptive pills, such as the Plan B pill, restart a new pill pack, and use backup contraception for 7 days. Question 28 2 / 2 pts A patient who has insulin-dependent type 2 diabetes reports having difficulty keeping blood glucose within normal limits and has had multiple episodes of both hypoglycemia and hyperglycemia. As adjunct therapy to manage this problem, the primary care NP should prescribe: Correct! Pramlintide is indicated in patients with type 1 diabetes and insulin-dependent type 2 diabetes and is helpful for patients with wide glycemic swings. Repaglinide requires a functioning pancreas to be effective. Glyburide and metformin are first-line oral agents and are not indicated. Question 29 2 / 2 pts The primary care NP sees a new patient for a routine physical examination. When auscultating the heart, the NP notes a heart rate of 78 beats per minute with occasional extra beats followed by a pause. History reveals no past cardiovascular disease, but the patient reports occasional syncope and shortness of breath. The NP should: Premature ventricular contractions are premature ventricular beats with a compensatory pause. This patient has no prior history, but does have syncope and shortness of breath. The NP should order an ECG and refer the patient to a cardiologist for further evaluation. If there were no other symptoms, the NP could order stress testing. Medications are not indicated without further testing and without consultation with a cardiologist. Question 30 2 / 2 pts A patient who has migraine headaches has begun taking timolol and 2 months after beginning this therapy reports no change in frequency of migraines. The patient’s current dose is 30 mg once daily. The primary care NP should: When giving timolol for migraine prophylaxis, the provider should inform the patient that it may take several weeks for therapy to be effective. The dose should be titrated and maintained for a minimum of 3 months before the treatment is deemed a failure. It may be necessary to change to propranolol if the therapy is not effective in 1 month. The maximum dose of timolol for migraine prophylaxis is 30 mg. Drug effectiveness is determined by patient response, not serum drug levels. Question 31 2 / 2 pts A patient who has breast cancer has been taking toremifene for 2 weeks. She tells her primary care NP that she thinks her tumor has grown larger. The NP should: Toremifene can cause tumor flare in the first few weeks of therapy, but the tumor later regresses. An ultrasound is unnecessary at this stage. The NP does not need to notify the oncologist unless this continues to worsen. Question 32 2 / 2 pts A CNM: CNMs have prescriptive authority in all 50 states. They may treat partners of women for sexually transmitted diseases. They have full prescriptive authority and are not limited to drugs used during childbirth. They practice in many other types of settings. Question 33 2 / 2 pts The primary care NP is preparing to prescribe a diuretic for a patient who has heart failure. The patient reports having had an allergic reaction to sulfamethoxazole-trimethoprim (Bactrim) previously. The NP should prescribe: Patients who are allergic to sulfa drugs should avoid diuretics that are sulfonamide derivatives. Ethacrynic acid is the only choice that is not a sulfonamide derivative. Question 34 2 / 2 pts In every state, prescriptive authority for NPs includes the ability to write prescriptions: All states now have some degree of prescriptive authority granted to NPs, but not all states allow authority to prescribe controlled substances. Many states still require some degree of physician involvement with certain types of drugs. Question 35 2 / 2 pts The primary care NP is seeing a patient for a hospital follow-up after the patient has had a first myocardial infarction. The patient has a list of the prescribed medications and tells the NP that “no one explained anything about them.” The NP’s initial response should be to: When a patient is first diagnosed with a medical problem, education must start with explaining the pathophysiology in terms the patient will understand. When patients understand what has happened to them, they can move on to consider what to do about it. The other responses are part of an education plan but are not the initial response. Question 36 2 / 2 pts A patient with primary hypercholesterolemia is taking an HMG-CoA reductase inhibitor. All of the patient’s baseline LFTs were normal. At a 6-month follow-up visit, the patient reports occasional headache. A lipid profile reveals a decrease of 20% in the patient’s LDL cholesterol. The NP should: LFTs should be performed at baseline, 12 weeks after initiation of therapy, and only periodically thereafter. Headaches are common side effects, but do not raise concern about hepatotoxicity. CK-MM tests are indicated if patients report muscle pain or weakness. It is not necessary to decrease the medication. Question 37 2 / 2 pts A patient receives an inhaled corticosteroid to treat asthma. The patient asks the primary care NP why the drug is given by this route instead of orally. The NP should explain that the inhaled form: An inhaled corticosteroid goes directly to the site of action and does not have to pass through gastrointestinal tract absorption or the liver to get to the lungs. It is generally well absorbed at this site, although dosing is not necessarily easier to regulate because it is not always clear how much of an inhaled drug gets into the lungs. Question 38 2 / 2 pts The primary care nurse practitioner (NP) sees a patient for a physical examination and orders laboratory tests that reveal low-density lipoprotein (LDL) of 100 mg/dL, high-density lipoprotein (HDL) of 30 mg/dL, and triglycerides of 350 mg/dL. The patient has no previous history of coronary heart disease. The NP should consider prescribing: Fibric acid derivatives, such as gemfibrozil, are indicated for reducing the risk that coronary heart disease may develop in patients without a history of coronary heart disease who have low HDL cholesterol levels and elevated triglyceride levels. This patient’s LDL is within normal limits, so a 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitor, such as simvastatin, is not indicated. Ezetimibe is a selective cholesterol absorption inhibitor, used to reduce total and LDL cholesterol. Nicotinic acid is used to treat hyperlipidemia in patients who have failed dietary therapy. Question 39 2 / 2 pts A woman who is taking a progestin-only pill has just stopped nursing her 9-month-old infant and tells the primary care NP that she would like to space her children about 2 years apart. The NP should: Serum folate levels may be decreased by oral contraceptives. Women who become pregnant shortly after stopping oral contraceptive use may have a greater chance of birth defects. This woman should become pregnant in about 6 months if she wants to space her children 2 years apart, so she needs an oral contraceptive. Progestin-only pills are used only during lactation. Question 40 2 / 2 pts A primary care NP sees a 3-year-old patient who has been vomiting for several days. The child has had fewer episodes of vomiting the past day and is now able to take sips of fluids without vomiting. The child has dry oral mucous membranes, 2-second capillary refill, and pale but warm skin. The child’s blood pressure is 88/46 mm Hg, the heart rate is 110 beats per minute, and the temperature is 37.2° C. The NP should: The use of antiemetics in children is discouraged for cases of uncomplicated vomiting. The child has compensated, mild dehydration and is now able to tolerate fluids, so oral rehydration is indicated. Question 41 2 / 2 pts A patient has been using an herbal supplement for 2 years that the primary care NP knows may have toxic side effects. The NP should: It is important for primary care NPs to inform patients of any known risks associated with herbal supplements. Asking the patient to stop an herbal remedy immediately when the patient has been using it for 2 years would probably be met with resistance. The NP should realize that referral to a CAM provider can incur legal liabilities if the CAM provider does not have proper competencies and licensure. Likewise, unless there is evidence-based documentation about the safety and efficacy of a product, the NP should not prescribe these therapies. Question 42 2 / 2 pts An 80-year-old patient who has persistent AF takes warfarin (Coumadin) for anticoagulation therapy. The patient has an INR of 3.5. The primary care NP should consider: This patient’s INR is only minimally prolonged, so no dose reduction is required. The NP should recheck the INR periodically. If the INR becomes more prolonged, lowering the dose of warfarin is recommended. If the INR approaches 5, omitting a dose and resuming at a lower dose is recommended. Vitamin K is used for an INR of 9 or greater. Question 43 2 / 2 pts A patient is in the clinic complaining of nausea and vomiting that has lasted 2 to 3 days. The patient has dry oral mucous membranes, a blood pressure of 90/56 mm Hg, a pulse of 96 beats per minute, and a temperature of 38.8° C. The primary care NP notes a capillary refill of greater than 3 seconds. The NP should: If vomiting is not controlled, dehydration may occur. Patients who are dehydrated, as this patient is, must be treated with IV fluids in a hospital or emergency department setting. Question 44 2 / 2 pts A patient asks a primary care NP whether over-the-counter drugs are safer than prescription drugs. The NP should explain that over-the-counter drugs are: Over-the-counter products have a wider margin of safety because most of these drugs have undergone rigorous testing before marketing and further refinement through years of over-the-counter use by consumers. When labels are understood and followed, over-the-counter medications are safe. Over-the-counter medications are regulated by the FDA. Question 45 2 / 2 pts A patient has been taking levothyroxine 100 mcg daily for several months. The patient comes to the clinic with complaints of insomnia and irritability. The primary care NP notes a heart rate of 92 beats per minute. The NP should: Question 46 2 / 2 pts A patient who has asthma and who is known to the primary care NP calls the NP after hours and asks for a refill of an albuterol metered-dose inhaler. The patient has not been seen in the clinic for more than a year. The NP should: The patient needs the medication and is known to the NP so a refill is not inconsistent with practice guidelines. However, further refills should not be provided until the patient is seen and has an updated asthma action plan. The patient should be informed of this; simply refilling the prescription sends a message that it is acceptable to get refills without being seen. Question 47 2 / 2 pts A patient wants to know why a cheaper version of a drug cannot be used when the primary care NP writes a prescription for a specific brand name of the drug and writes, “Dispense as Written.” The NP should explain that a different brand of this drug: Different formulations of the same drug may have varying degrees of bioavailability, and it may be important to stick to a particular brand for drugs with narrow therapeutic ranges. All drugs with similar active ingredients should have the same therapeutic actions and side effects and should be equally safe. Question 48 2 / 2 pts A patient who has congestive heart failure and arthritis has been taking chlorthalidone (Zaroxolyn) 25 mg daily for 6 months. The primary care NP notes a persistent blood pressure of 145/90 mm Hg. The NP should: For diuretic resistance, the NP should evaluate factors such as patient nonadherence, physiologic causes, and drugs that may increase resistance, including nonsteroidal antiinflammatory drugs (NSAIDs). This patient has arthritis, and it is likely that NSAID use may be causing diuretic resistance. A second drug, such as furosemide, should be added after the cause of diuretic resistance is determined. The maximum daily dose of chlorthalidone is 100 mg per day, but increasing the dose is not recommended to treat diuretic resistance. Recommending salt substitutes is not indicated. Question 49 2 / 2 pts The primary care NP sees a patient who has a history of hypertension and alcoholism. The patient is not taking any medications. The NP auscultates crackles in both lungs and palpates the liver 2 cm below the costal margin. Laboratory tests show an elevated creatinine level. The NP will refer this patient to a cardiologist and should prescribe: In the treatment of heart failure, loop diuretics relieve the congestive symptoms of pulmonary and congestive edema. Loop diuretics are also useful to treat states of volume excess in cirrhosis and renal insufficiency. Because this patient has a history of alcoholism and has an enlarged liver on examination, furosemide is a good first choice to relieve this patient’s congestive symptoms. Spironolactone and chlorthalidone are not loop diuretics. Albuterol might be used for symptomatic treatment only. Question 50 2 / 2 pts A patient with chronic back pain that is unrelieved by prescription analgesic medications asks a primary care nurse practitioner (NP) about acupuncture treatments. The NP should tell this patient: Current literature does not allow definitive conclusions to be drawn regarding the use of complementary and alternative medicine (CAM) because much of what appears in the literature continues to be based on observational reports and small studies. Biofield therapy has not been shown to be more effective than acupuncture. Creatine is used to increase muscle mass. Question 51 2 / 2 pts A patient with congestive heart failure will begin therapy with a diuretic medication. The primary care NP orders laboratory tests, which reveal a glomerular filtration rate (GFR) of 25 mL/minute. The initial drug the NP should prescribe is: Correct! Thiazides are the most frequently used and the least expensive drugs administered to treat hypertension and are considered first-line treatments. In patients with a GFR less than 30 mL/minute, thiazides are relatively ineffective, with the exception of metolazone. Furosemide may be added as a second-line drug. Potassium-sparing diuretics, such as spironolactone, should be used with great caution or avoided altogether in patients with renal insufficiency. Question 52 2 / 2 pts The primary care NP sees a patient several months after a myocardial infarction (MI). The patient has been taking furosemide to treat heart failure. The NP notes that the patient has edema of the hands, feet, and ankles. The NP should add which drug to this patient’s regimen? The addition of a thiazide to a loop diuretic along with sodium restriction may be useful in the treatment of refractory edema in patients with congestive heart failure. Ethacrynic acid is a loop diuretic. The other two options are potassium-sparing diuretics. Question 53 2 / 2 pts An important difference between physician assistants (PAs) and NPs is PAs: PAs commonly have co-signature requirements and work under physician supervision. Question 54 2 / 2 pts A primary care NP is developing a handout to give to patients who will begin self-administering insulin. When developing this handout, the NP should: When developing patient education materials, it is important to limit content to one or two educational objectives and list what the patient will learn and do after reading the material. Written materials should not be too detailed but rather presented using bulleted points. When possible, material should use common words and phrases and avoid medical terms. Question 55 2 / 2 pts An 80-year-old patient has begun taking propranolol (Inderal) and reports feeling tired all of the time. The primary care NP should: Elderly patients have described sedation and sleep disturbances with β-blockers. Elderly patients often need lower doses of these drugs. Patients should not be advised to discontinue the medication abruptly. Question 56 2 / 2 pts An 80-year-old male patient will begin taking an α-antiadrenergic medication. The primary care NP should teach this patient to: All antihypertensives can cause orthostatic hypotension, so patients should be cautioned to avoid sudden changes in position and to use caution when bathing because a hot bath or shower may aggravate dizziness. Older patients are at increased risk for falls and should be cautioned to ask for assistance. Patients taking α-antiadrenergics should consume extra fluids because dehydration can increase the risk of orthostatic hypotension. Patients should take the medication at bedtime because drowsiness is a common side effect. Priapism is not a side effect of these drugs. Question 57 2 / 2 pts A woman who uses a transdermal contraceptive calls the primary care NP to report that while dressing that morning she discovered that the patch had come off and she was unable to find the patch. The NP should tell her to apply a new patch and: If a transdermal patch has been discovered to be loose or has come off, patients should use a backup method of contraception. It is not necessary to use oral contraceptives. A home pregnancy test is not indicated. Question 58 2 / 2 pts A woman who has been taking a COCP tells the primary care NP that, because of frequent changes in her work schedule, she has difficulty remembering to take her pills. The woman and the NP decide to change to a vaginal ring. The NP will instruct her to insert the ring: Correct! Patients should be switched from a COCP to a vaginal ring by insertion within 7 days after the last active pill. No backup method is needed. Patients do not need to continue one more cycle of COCPs. Women taking progestin-only pills insert the ring on the last day of the pill pack. Question 59 2 / 2 pts A 12-year-old patient has acute diarrhea and an upper respiratory infection. Other family members have had similar symptoms, which have resolved. The primary care NP should recommend: Antidiarrheals are not generally recommended in children. Bismuth is not recommended in children younger than 16 years of age with viral illnesses because it can mask symptoms of Reye’s syndrome. Oral rehydration with electrolyte solution is safe. Question 60 2 / 2 pts A patient is taking drug A and drug B. The primary care NP notes increased effects of drug B. The NP should suspect that in this case drug A is a cytochrome P450 (CYP450) enzyme: If drug A is a CYP450 enzyme inhibitor, it decreases the capacity of the enzyme to metabolize drug B, causing more of drug B to be available. A substrate is a drug acted on by the enzyme. If drug B is an enzyme inducer, it would cause increased metabolism of drug A. [Show More]
Last updated: 1 year ago
Preview 1 out of 131 pages
Instant download
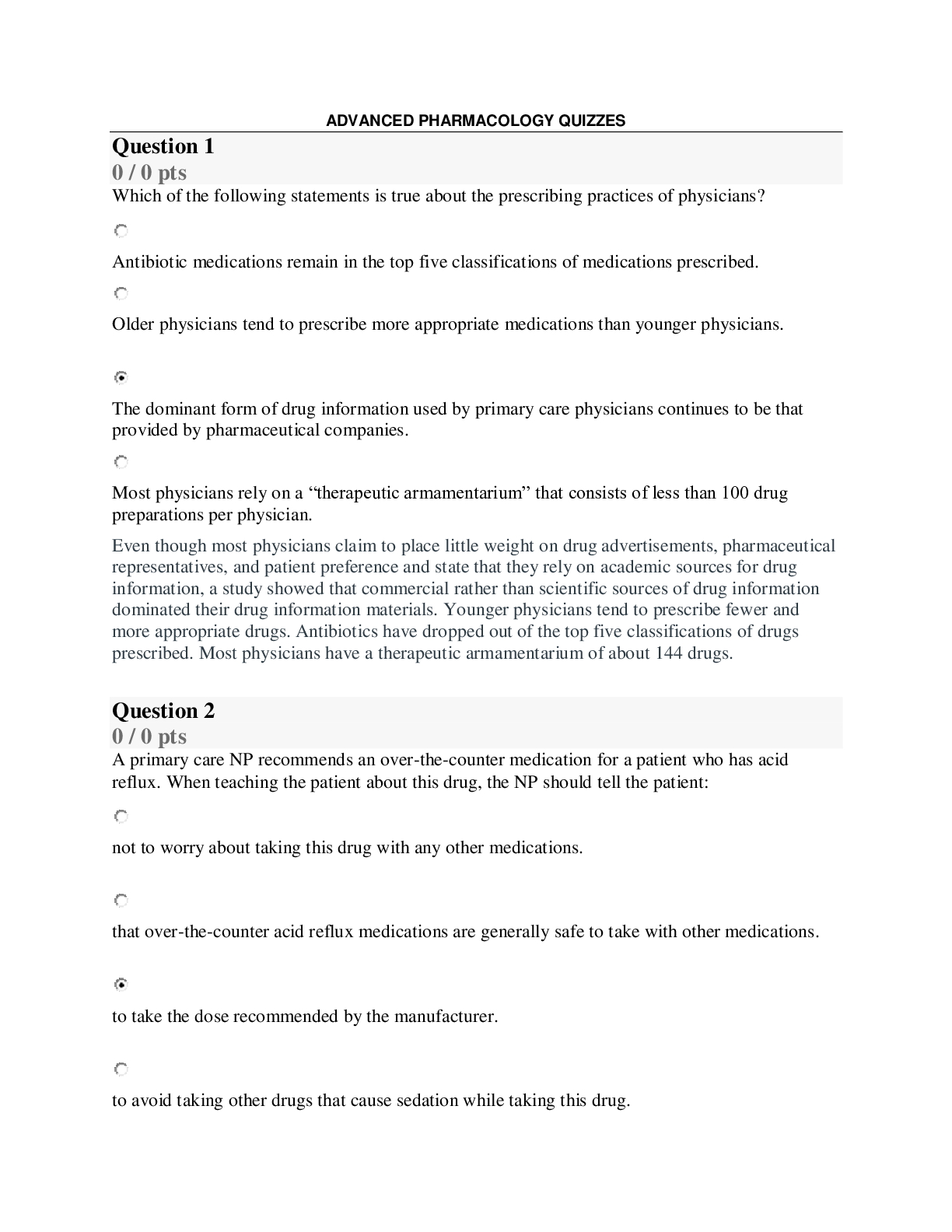
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Dec 19, 2020
Number of pages
131
Written in
Additional information
This document has been written for:
Uploaded
Dec 19, 2020
Downloads
0
Views
37

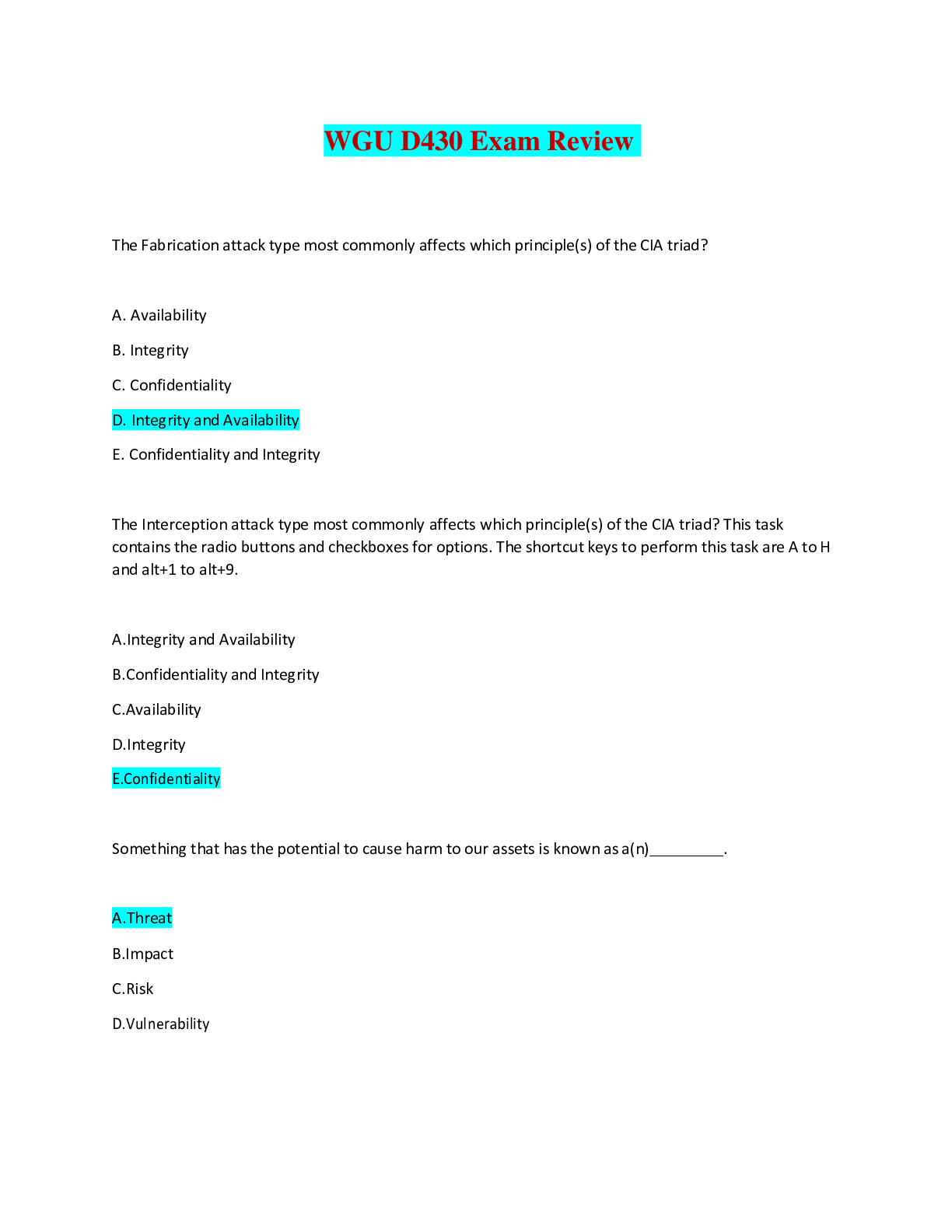
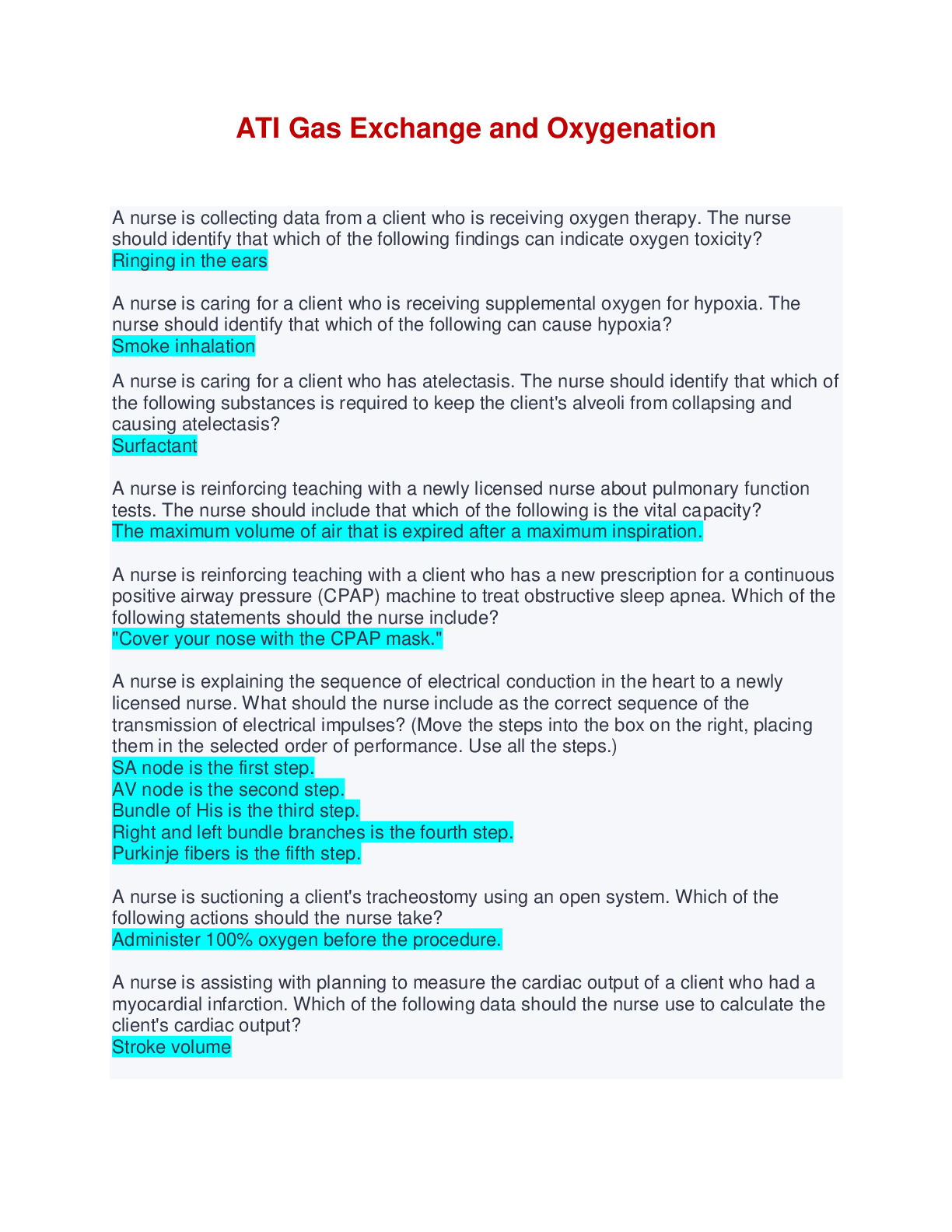
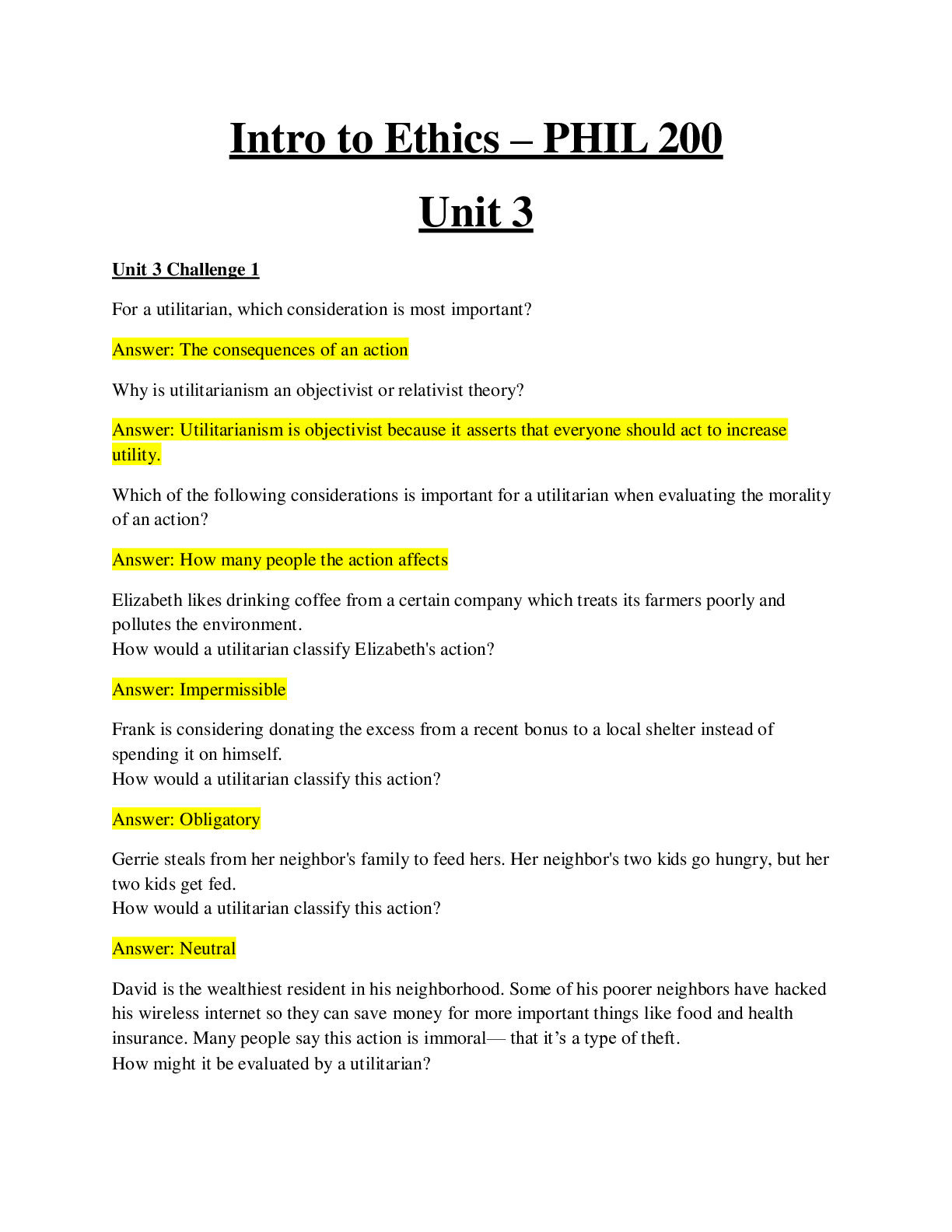





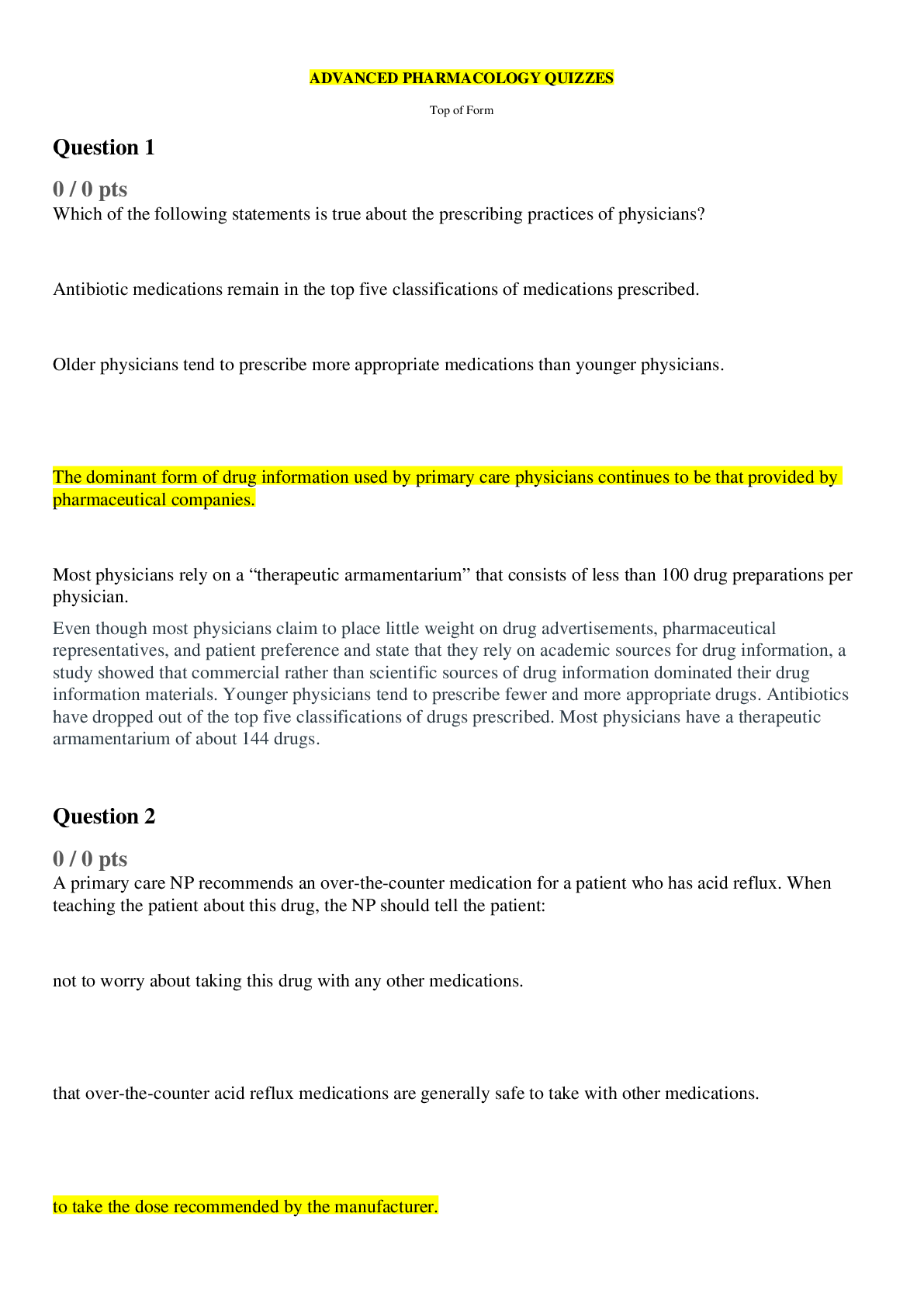
.png)