*NURSING > iHuman > NURSING 211Abruption Placentae with Preterm Labor and Delivery Unfolding Reasoning,100% CORRECT (All)
NURSING 211Abruption Placentae with Preterm Labor and Delivery Unfolding Reasoning,100% CORRECT
Document Content and Description Below
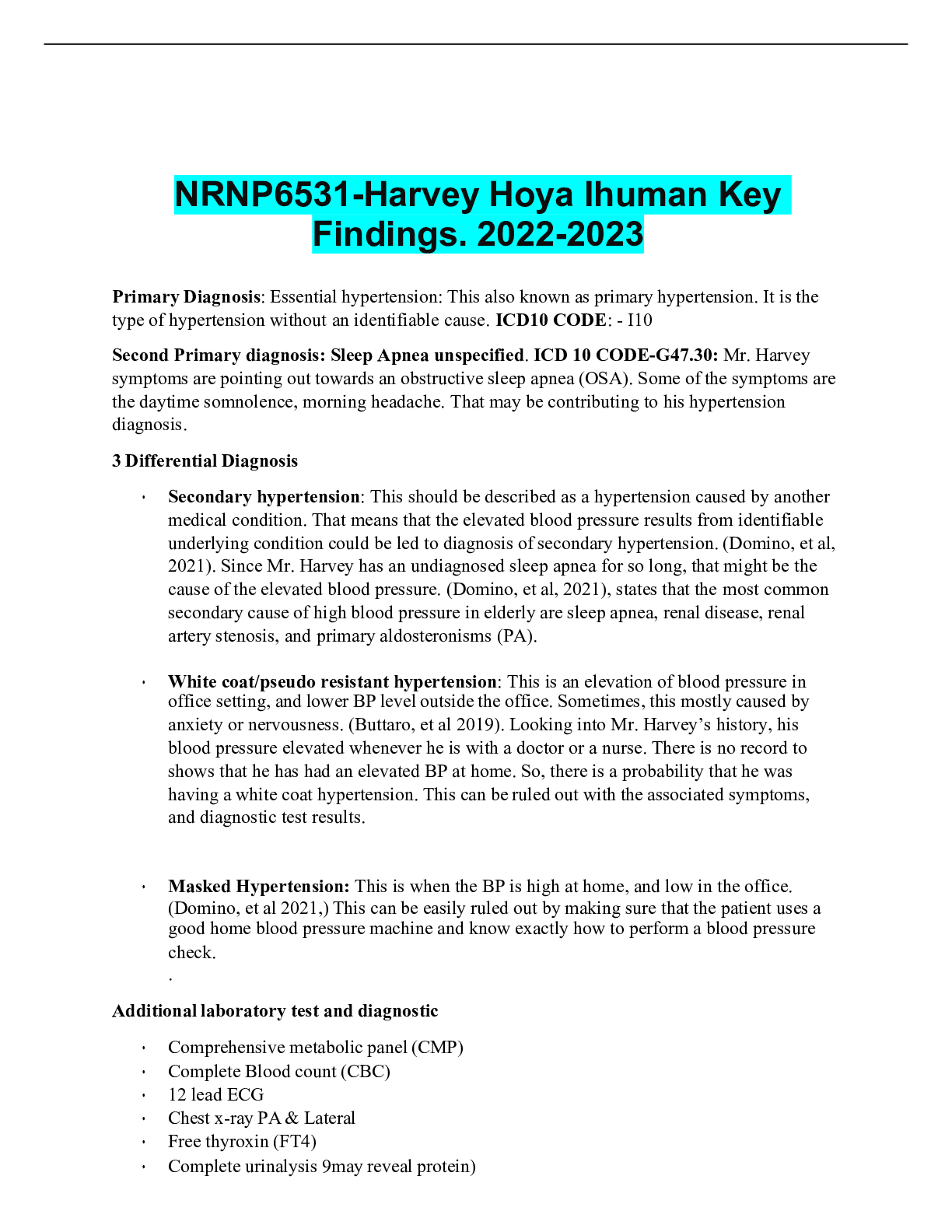
NURSING 211Abruption Placentae with Preterm Labor and Delivery Unfolding Reasoning Michelle Moore, 38 years old Primary Concept Perfusion Interrelated Concepts (In order of emphasis) 1.... Reproduction 2. Oxygenation 3. Pain 4. Clinical Judgment 5. Patient Education 6. Communication 7. Collaboration © 2019 Keith Rischer/www.KeithRN.com UNFOLDING Reasoning Case Study: ANSWER KEY Abruptio Placentae with Preterm Labor and Delivery History of Present Problem: Michelle Moore is a 38-year-old who is 29 weeks pregnant. She began prenatal care at 18 weeks gestation because she was waiting to become insured. She is currently in the Labor and Delivery Unit of the hospital following a call to her primary care provider. She reported that she had a sudden onset of constant severe uterine pain and began to notice that she had vaginal bleeding that bright red, soaked a maxi pad and then began soaking through her underwear. Her baby has not been moving as actively as normal since the pain and bleeding started. Personal/Social History: Michelle works at a fast-food restaurant, standing on her feet for long hours. She usually works in the evenings and weekends. She is estranged from the father of the baby. Michelle’s father is able to help her with childcare once or twice a week. Michelle denies substance use including alcohol during her pregnancy. Michelle smokes 10 cigarettes daily, and says that she has decreased usage, but the stress of the pregnancy and having little support makes it difficult for her to quit. Michelle reports that she usually eats at work to save money, and most meals consist of fried foods and diet sodas. Michelle has a small apartment, but says she often has difficulty paying the rent on time, since child care is so expensive. She has a six-year old son who was born prematurely at 35 weeks. Michelle was diagnosed with a partial abruption during that delivery. Past Medical History (PMH): Home Meds: Pharm. Classification: Expected Outcome: • Gravida 4, Para 1 with a partial abruption at 35 weeks • Two spontaneous abortions in the first trimester • Menses began at age 12, are usually 29 days apart, lasting for 4-5 days, with moderate-to-light flow. • Successfully breast fed her first child for 11 months. • Vaccinations are up to date. • Michelle is biracial: African American and Asian, and she was tested for sickle cell trait. Lab results reveal Michelle is a carrier of the trait. It is unknown if the father of the baby is also a carrier. 1. Prenatal vitamin 1 tab PO daily 2. Acetaminophen 650 mg PO PRN every 6 hours for infrequent, mild headaches 1. Multivitamin 2. Analgesic 1. Pt will maintain adequate iron and vitamin levels during pregnancy 2. Pt will be free of mild headaches What data from the histories are RELEVANT and must be interpreted as clinically significant by the nurse? RELEVANT Data from Present Problem: Clinical Significance: • 38 yrs old • 29 weeks pregnant • Present at PCP direction • Severe uterine pain • Bright red vaginal bleeding • Reduced fetal movement since onset of bleeding and pain • Maturity of handling situation • If situation escalates to delivery, will need to take required steps and mobilize appropriate personnel • Adds immediate validity to situation – facilitates communication • Uterine pain with bright red blood is an indication of possible placental abruption • Reduction of fetal movement is indication of possible fetal distress RELEVANT Data from Social History: Clinical Significance: • Works long and night/weekend hours • Baby’s father not involved; her father has limited time to help • Smokes • Stress of work combined with poor nutrition, and smoking can negatively impact fetal development • Support network is insufficient • Inability to meet financial needs can add psychosocial stress • Eats at work • Difficulty paying rent/expensive childcare • Hx of premature birth • Hx of placental abruption • Increased stress hormones can negatively impact pregnancy • Hx increases odds of both premature and placental abruption occurring in subsequent pregnancies Patient Care Begins: Current VS: P-Q-R-S-T Pain Assessment (5th VS): T: 98.5 F/ 36.9 C (oral) Provoking/Palliative: Constant, nothing makes it worse or better P: 122 (regular) Quality: “knife-like” R: 24 (regular) Region/Radiation: abdominal BP: 132/64 MAP: 87 Severity: 9/10 O2 sat: 96% room air Timing: constant What VS data are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT VS Data: Clinical Significance: • Slightly pyretic • Tachycardic • Tachypnic • Increased BP • O2Sat • Pain 9/10, severe and constant/no relief • Main vital signs all support patient report of pain • Elevated HR could be due to hemorrhage • Constant pain and severity levels need to be immediately addressed • O2 level indicates good oxygenation which is the first step to make sure baby is as well Current Assessment: GENERAL APPEARANCE: 5’ 4” (162.5 cm) tall and weighs 165 pounds (75 kg), including 25 pounds (11.4 kg) she gained during this pregnancy. Appears uncomfortable, groaning and holding abdomen RESP: Breath sounds clear with equal aeration bilaterally, labored respiratory effort CARDIAC: Pale, cool/dry, no edema, heart sounds regular with no abnormal beats, equal with palpation at radial/pedal/post-tibial landmarks NEURO: Alert and oriented to person, place, time, and situation (x4) FETAL Monitoring: Electronic Fetal Monitoring: Fetal heart rate 150, minimum variability trending towards absent variability around the baseline, late decelerations, no accelerations noted. Contractions are frequent: every 1-2 minutes; uterus is board-like upon palpation. What assessment data are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Assessment Data: Clinical Significance: • Pt physically uncomfortable and holding abdomen • Respiration labored, but clear airway • A/Ox4 • FHR approaching 160 • Minimal variability with late decelerations • Frequent contractions • Hard uterus • Patient focus is on abdomen/fetus – will need to give support • Airway is patent; oxygenation source is viable • Pt alertness will help in comprehension of situation and decision making • All FHR information is non-reassuring and requires intervention • Uterine tension indicates internal bleeding Fetal Monitoring Strip: Interpretation: FHR baseline between 110-160, minimal variation with constant late decelerations. Category 3 Contractions are frequent and generally constant with rest periods being equal to duration of contraction Clinical Significance: Late decels are indicating placental oxygenation insufficiency Repositioning of mother and oxygenation are indicated Need to maintain monitoring for changes Medical Management: Rationale for Treatment and Expected Outcomes Care Provider Orders: Rationale: Expected Outcome: Prepare for immediate cesarean section in operating room (OR) Oxygen 10 liters/minute via nonrebreather Continuous fetal monitoring Strict I&O Insert urinary catheter Lactated Ringers (LR) 1000 mL bolus Type and screen for “maternal pack” that includes 6 units PRBCs, 4 units FFP, 1 apheresis pack of platelets. This ratio can be repeated as needed • Internal bleeding is apparent w/ fetal distress and poor oxygenation • To maintain maternal oxygen levels • To quickly identify any worsening of condition and take appropriate action • Pt needs to maintain fluid balance - I/O, catheter, LR • To be prepared for possible blood transfusion if needed • Successful delivery of healthy fetus • Maximum oxygenation of placenta/fetus • Fetal safety will be maintained • Pt will avoid adverse metabolic conditions • Pt will be able to void • Pt will maintain adequate supply of blood PRIORITY Setting: Which Orders Do You Implement First and Why? Care Provider Orders: Order of Priority: Rationale: • Oxygen -10 liters/minute vis non-rebreather • Continuous fetal monitoring • Insert urinary catheter with urometer for hourly I and O • Lactated Ringers (LR) IV 1000 mL bolus • Type and screen for “maternal pack” that includes 6 units PRBCs, 4 units FFP, 1 apheresis pack of platelets. This ratio can be repeated as needed based on labs (Drawn per policy, usually every 4 hours for 24). 1. O2 2. LR 3. Catheter 4. FM 5. Type/Screen • Need to maintain adequate oxygenation to both mother/fetus • LR/Cath required to maintain fluid balance • Fetal monitoring required to ID any further distress/change of conditions that require immediate action • In case of c/s and transfusion needed Lab Results: Complete Blood Count (CBC:) (Pregnancy Values) Current: High/Low/WNL? Previous: WBC (5,000 – 15,000 mm 3) 15.1 H 14.8 Hgb (11.5-14 g/dL) 9.5 L 11.2 Platelets (150-350 x103/µl) 101 L 122 What lab results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: • Hgb = 9.5 • Platelets = 101 • Both factors indicated bleeding and possible hemorrhage • Worsening trend Coags: Current: High/Low/WNL? PT/INR (0.9–1.1 nmol/L): 1.7 H PTT (29-35 seconds): 45 H Fibrinogen (<80 mg/dL): 44 L Kleihauer-Betke test (Positive if >0.01 mL of fetal blood in the maternal circulation) Positive What lab results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: • PT/INR = 1.7 • PTT = 45 • Fibrinogen = 44 • All clotting factors are at levels that reduce clotting abilities and put the mother at risk for hemorrhage • Worsening trend Urine Analysis (UA:) Current: WNL/Abnormal? Previous: Color (yellow) Dark amber Abnormal Clear yellow Protein (neg) Neg Normal Neg Glucose (neg) Neg Normal Neg What lab results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: 1. Urine = Dark Amber 1. Color indicates dehydration issues • Worsening trend Lab Planning: Creating a Plan of Care with a PRIORITY Lab: Lab: Normal Value: Clinical Significance: Nursing Assessments/Interventions Required: Kleihauer- Betke Positive Critical Value: Clinical Reasoning Begins… 1. What is the primary problem that your patient is most likely presenting with? Abruptio Placentae 2. What is the underlying cause/pathophysiology of this primary problem? Abruptio Placentae occurs when the placenta is partially or fully separated from the uterus, which if not addressed can progress to hemorrhage and death. 3. What nursing priority (ies) will guide your plan of care? (if more than one-list in order of PRIORITY) Hemorrhage, safe fetal delivery 4. What interventions will you initiate based on this priority? Nursing Interventions: Rationale: Expected Outcome: 1. Continual Monitor of all VS 2. Continually assess blood loss, amount, and any changes to content 3. Monitor pt A/O 4. Continue to palpate uterus To monitor for any changes that indicate a progressing negative trend Pt will not experience significant hemorrhage or go into shock 5. What psychosocial needs will this patient and/or family likely have that will need to be addressed? Support resources. Pt has limited support network and will need appropriate community referrals 6. How can the nurse address these psychosocial needs? Supply support and financial community resources for single mothers. Provide emotional support and education 7. What body system(s) will you assess most thoroughly based on the primary/priority concern? Cardio/respiratory and reproductive 8. What is the worst possible/most likely complication to anticipate? Death of fetus, mother or both 9 What nursing assessments will identify this complication EARLY if it develops? VS, Fluid/blood loss 10. What nursing interventions will you initiate if this complication develops? Administer fluids, assist to c/s delivery, blood transfusion if necessary 11. If the worst possible/most likely complication was recognized by the nurse, when would you decide to notify rapid response team to evaluate further? Significant increase of blood loss, further change to fetal VS/heart tracings, LOC Evaluation: Sixty minutes later… Michelle delivered a viable baby boy at 29 weeks gestation, via emergency Cesarean Section. Her quantitative blood loss was 1500 mL. What data are RELEVANT and must be interpreted as clinically significant by the nurse? RELEVANT Data from Present Problem: Clinical Significance: • c/s delivery @29wks • blood loss = 1500mL • blood transfusion required Initial Assessment: GENERAL APPEARANCE: 29 weeks gestation. Dusky with weak respiratory effort. RESP: Weak respiratory effort with grunting and sternal/intercostal retractions CARDIAC: Heart rate above 100 with no murmur. Weak pulses NEURO: Responds to stimuli, moves all extremities GI: Abdomen soft and flat, umbilical cord clamped SKIN: No lanugo,1/3 of foot has plantar creases, vessels visible under skin INFANT-Initial APGAR (1 minute): 0 Points 1 Point 2 Points Activity: X some flexion Pulse: X 110 Grimace: X gag Appearance: X dusky Respiration: X weak Total: 5 Current Assessment: GENERAL APPEARANCE: 29 weeks gestation. Marked acrocyanosis with weak respiratory effort. Central cyanosis noted. RESP: Weak respiratory effort with grunting, nasal flaring and retractions CARDIAC: Heart rate above 100 with no murmur. Weak pulses NEURO: Responds to stimuli, moves all extremities GI: Abdomen soft and flat, umbilical cord clamped SKIN: No lanugo, vessels visible APGAR: 5 Minutes: 0 Points 1 Point 2 Points Activity: X some flexion Pulse: x130 Grimace: X with stimulation Appearance: X marked acrocyanosis Respiration: X weak cry Total: 7 What assessment data are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Assessment Data: Clinical Significance: • APGAR: 51, 75 • c/s @29wks • acrocyanosis • respiration • Intervention needed • Developmental expectations • Acrocyanosis/respiration need to be addressed right away to increase perfusion INFANT: Umbilical Cord Arterial Arterial Blood Gas: Current: High/Low/WNL? pH (7.35–7.45) 7.29 L pCO2 (35–45) 55 H pO2 (80–100) 76 L HCO3 (18–26) 18 WNL O2 sat (>92%) 91% L Interpretation: What lab results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Lab(s): Clinical Significance: • pH: L • pCO2: H • pO2: L • O2 sat: L • At risk for uncompensated respiratory acidosis The baby has been transferred to the NICU and is receiving respiratory support through CPAP at this time. Michelle has just been admitted to her room from PACU. MOTHER Assessment Data: Current VS: Most Recent: Current PQRST: T: 99.1 F/37.3 C (oral) T: 98.5 F/ 36.9 C (oral) Provoking/Palliative: Movement/Lying still P: 102 (regular) P: 122 (regular) Quality: ache R: 16 (regular) R: 20 (regular) Region/Radiation: Incision BP: 110/74 MAP: 86 BP: 102/64 MAP: 77 Severity: 2/10 O2 sat: 94 % room air O2 sat: 96% room air Timing: Ongoing Current Assessment: GENERAL APPEARANCE: Resting quietly, pale RESP: Breath sounds clear with equal aeration bilaterally, non-labored respiratory effort CARDIAC: Pale, clammy, no edema, heart sounds regular with no abnormal beats, equal with palpation at radial/pedal/post-tibial landmarks. Pulse is thready. NEURO: Alert and oriented to person, place, time, and situation (x4) BUBBLE BREAST: Lactating; soft, non-tender with evidence of colostrum UTERUS: Boggy and several quarter sized clots expressed with massage BLADDER: 25 mL in last hour, dark amber BOWELS: Abdomen tender; bowel sounds audible per auscultation in all four quadrants LOCHIA: 50 mL blood on peri pad in last 30 minutes EPISIOTOMY: Perineum intact; abdomen with surgical dressing on abdomen which is clean, dry, and intact 1. What VS data are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT VS Data: Clinical Significance: • T: 99.1 • BP: 110/74 • O2 sat: 94% • With rising T/BP – keep close eye for s/s of infection • Needs O2 to bring up sat level RELEVANT Assessment Data: Clinical Significance: • Uterus – boggy w/ clots • Bladder – insufficient void • Lochia – 50mL blood in 30min • Pt in danger of hypovolemic shock • Needs fluids 2. Has the status improved or not as expected to this point? Though most signs are good, the overall trend indicate status is not improved 3. Does your nursing priority or plan of care need to be modified in any way after this evaluation assessment? Same plan should address the issues of concern 4. Based on your current evaluation, what are your nursing priorities and plan of care? Continue to monitor for s/s of unusual bleeding and continue fluid management It is now time to transfer your patient. Effective and concise handoffs are essential to excellent care and if not done well can adversely impact the care of this patient. You have done an excellent job to this point, now finish strong and give the following SBAR report to the nurse who will be caring for this patient: Situation: Name/age: Michelle Moore / 38yrs BRIEF summary of primary problem: Pt presented w/ severe uterine pain w/ bright read vaginal bleeding Day of admission/post-op #: 18 Nov 2020 Background: Primary problem/diagnosis: Abruptio Placentae RELEVANT past medical history: Hx of premature birth (35wks) and abruptio placentae RELEVANT background data: Insufficient support network, Employment: long off hours on feet, poor nutrition, active smoker Assessment: Vital signs: T: 99.1, P: 102 (regular), R: 16 (regular), BP: 110/74, O2 sat: 94% on rm air, Pain: 2/10 ache RELEVANT body system nursing assessment data: Uterus: Boggy and several quarter sized clots expressed with massage; Bladder: 25 mL in last hour, dark amber; 50 mL blood on peri pad in last 30 minutes; Perineum intact; abdomen with surgical dressing on abdomen which is clean, dry, and intact RELEVANT lab values: UA: dark amber color TREND of any abnormal clinical data (stable-increasing/decreasing): INTERPRETATION of current clinical status (stable/unstable/worsening): Pt status is on a worsening trend and @risk of fluid loss, infection Recommendation: Suggestions to advance plan of care: Continue fluid monitor/management, have PCP eval for pharm intervention of blood loss, monitor VS Education Priorities/Discharge Planning 1. What will be the most important discharge/education priorities you will reinforce with his/her medical condition to prevent future readmission with the same problem? • When pregnant again, start prenatal care earlier • Find employment opportunities that get her off her feet • Smoking cessation • Improve diet – nutrition • Importance of developing a support network 2. What are some practical ways you as the nurse can assess the effectiveness of your teaching with this patient? • Have her teach back the purpose of each topic covered • Follow up care (social worker, etc) Caring and the “Art” of Nursing 1. What is the patient likely experiencing/feeling right now in this situation? • Anxiety of current downward trending condition • Worry for baby 2. What can you do to engage yourself with this patient’s experience, and show that he/she matter to you as a person? • Praise for coming through the situation • Development of therapeutic relationship • Help with contacting appropriate referrals and making f/u appointments at the appropriate time • Listen to any concerns she may have and take action to help as able/appropriate Use Reflection to THINK Like a Nurse Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention in the moment as the events are unfolding to make a correct clinical judgment. 1. What did I learn from this scenario? • The timeliness of action necessary when a suspected hemorrhage is in play and all the moving parts that need to be addressed simultaneously – maternal, fetal, medical, AND psychosocial 2. How can I use what has been learned from this scenario to improve patient care in the future? • Being aware and knowing all the s/s of potential hazards and heading them off before they develop or get worse if they are in place. I also really need to understand how DIC develops in a case like this. [Show More]
Last updated: 1 year ago
Preview 1 out of 12 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 13, 2022
Number of pages
12
Written in
Additional information
This document has been written for:
Uploaded
Oct 13, 2022
Downloads
0
Views
59





 2021.png)