Care Man 2 exam 1 study guide (Jazmin)
Document Content and Description Below
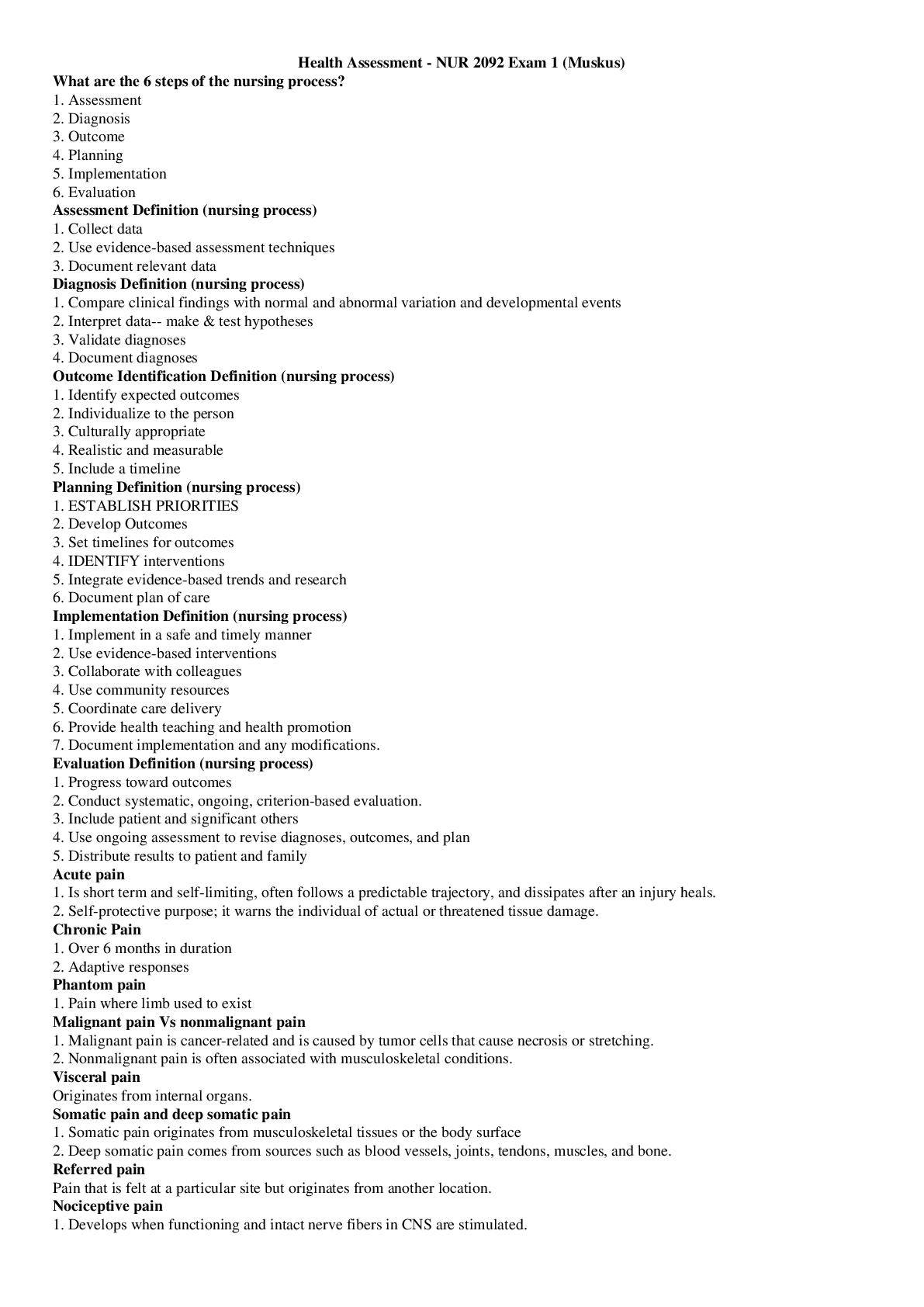
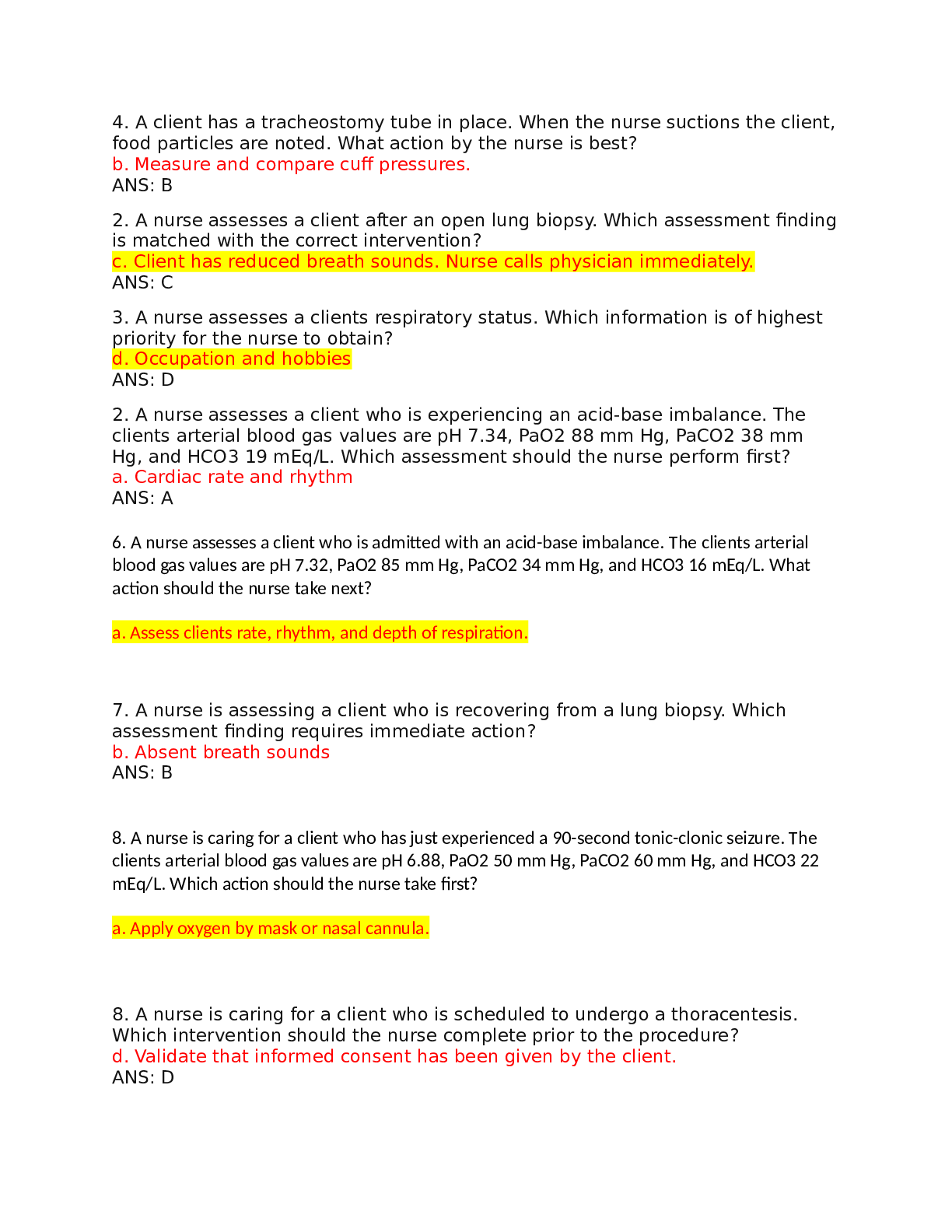
Care Man 2 exam 1 study guide (Jazmin) Exam 1 Weeks 1&2 Study Guide Chapter 4 Assessment and Care of Patients with Pain Concepts • The priority concept in this chapter is comfort • The in... terrelated concepts in this chapter are cognition sensory Perception Pain The Scope of the Problem • Pain is a major economic problem and a leading cause of disability that changes the lives of many people, especially older adults. • Chronic non-cancer pain such as osteoarthritis, rheumatoid arthritis, and diabetic neuropathy is the most common cause of long-term disability, affecting millions of Americans and others throughout the world. • Universal, complex personal experience • Is an impairment in comfort; major economic concern; leading cause of disability • Failure to manage pain is a worldwide health problem • Inter-professional pain initiatives help patients receive best treatment Definitions of Pain • Unpleasant sensory and emotional experience associated with actual or potential tissue damage • Whatever person experiencing it says it is; exists whenever person says it does • Self-report always most reliable indication of pain Categorization of Pain by Duration • Acute pain - Short-lived - Results from sudden, accidental trauma; surgery; ischemia; acute inflammation • Chronic (persistent) pain - Can last a person’s lifetime - Chronic cancer pain - Chronic non-cancer pain • Pain is treated inadequately in almost all health care settings. • Populations at the highest risk in medical-surgical nursing are older adults, patients with substance use disorder, and those whose primary language differs from that of the health care professional. • Older adults in nursing homes are at especially high risk because many residents are unable to report their pain. In addition, there often is a lack of staff members who have been educated to manage pain in the older-adult population. Acute Pain • Acts as warning sign • Activation of sympathetic nervous system • “Fight-or-flight” reactions - Increased vital signs - Sweating - Dilated pupils - Restlessness - Apprehension - Distress of varying degrees Acute Pain (Cont.) • Absence of physiologic and behavioral responses does not mean absence of pain • Usually temporary with sudden onset, and easily localized • Sensory perception of pain changes as injured area heals Chronic (Persistent) Pain • Lasts or recurs for indefinite period (more than 3 months) • Gradual onset • Character and quality often change over time • Serves no biological purpose • Can result in emotional, financial, and relationship burdens, as well as depression/hopelessness Chronic Cancer Pain • Usually result of tumor growth, nerve compression, tissue invasion, metastasis • Cancer treatment can also cause acute pain (e.g., procedures, surgery, toxicities from chemo and radiation) Chronic Non-Cancer Pain • Global health issue for people > 65 years old • Formerly called chronic nonmalignant pain • Neck, shoulder, low back • Over half of veterans of recent wars have this condition - Can cause depression, decreased sense of well-being Categorization of Pain by Underlying Mechanisms • Nociceptive pain - Somatic - Visceral • Neuropathic pain Pain Transmission • Painful stimuli often originate in extremities • If pain is not transmitted to the brain, person feels no pain • Two specific fibers transmit periphery pain: - A delta fibers - C fibers Assessment: Noticing • Patient’s self-report is “gold standard” for assessment • Nurse’s role - Accept patient self-report - Serve as advocate - Act promptly to relieve pain - Respect patient values and preferences Pain Assessment (Cont.) • Location • Intensity • Quality • Onset and duration • Aggravating and relieving factors • Effect of pain on function and quality of life • Comfort-function outcomes • Other information Psychosocial Assessment • Pain holds unique meaning for the person experiencing it. • Remain objective; advocate for proper pain control • Refer to resources such as “10-Step Program from Patient to Person” (as needed) Assessment Challenges • Patients who cannot self-report pain are at higher risk for under-treated pain - Hierarchy of Pain Measures - Checklist of Nonverbal Pain Indicators (CNPI) - Pain Assessment in Advanced Dementia Scale (PAINAD) Different Pain Types • Localized pain is confined to the site of origin. • Projected pain is diffuse around the site of origin and is not well localized. • Referred pain is felt in an area distant from the site of painful stimuli. • Radiating pain is felt along a specific nerve or nerves. • Intensity: Ask the patient to rate the severity of the pain using a reliable and valid assessment tool. • Various self-report scales have been developed to help patients communicate pain intensity. Teaching how to respond to a pain scale • Text book Table 4-4 Analgesic Groups • Non-opioid analgesics - Acetaminophen - NSAIDs Non-opioid Analgesics • Monitor patients taking acetaminophen for hepatotoxicity • Reduced daily dose may be appropriate for older adults on long-term therapy • Monitor patients taking NSAIDS for gastric side effects • NSAIDS carry risk for cardiovascular and renal adverse effects through prostaglandin inhibition Analgesics by Classification: Opioid Analgesics • Full or mu agonists - Morphine, fentanyl, hydromorphone, oxycodone, oxycodone, hydrocodone • Mixed agonists antagonists - Butorphanol, nalbuphine • Partial agonists - Buprenorphine Drug Formulation Terminology • Short acting, fast acting, immediate release (IR), normal release - Onset in about 30 minutes; short duration of 3 to 4 hours • Modified-release, extended release (ER), sustained release (SR), controlled release (CR) - Release over a prolonged period - Never crush, break, or have patients chew! Selected Opioid Analgesics • Morphine • Fentanyl - Teach patients to refrain from applying heat to patches • Hydromorphone • Oxycodone • Hydrocodone • Methadone Dual Mechanism Analgesics • Tramadol (Ultram) • Tapentadol (Nucynta) Opioids to Avoid • Meperidine • Codeine Intraspinal Analgesia • Analgesic administration via a needle or catheter in the epidural or intrathecal space • Placed by an anesthesia provider ……………………………..continued…………………………… [Show More]
Last updated: 1 year ago
Preview 1 out of 48 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jan 14, 2021
Number of pages
48
Written in
Additional information
This document has been written for:
Uploaded
Jan 14, 2021
Downloads
0
Views
53


.png)

.png)



