ATI NCLEX Exam and Assessments Review
Document Content and Description Below
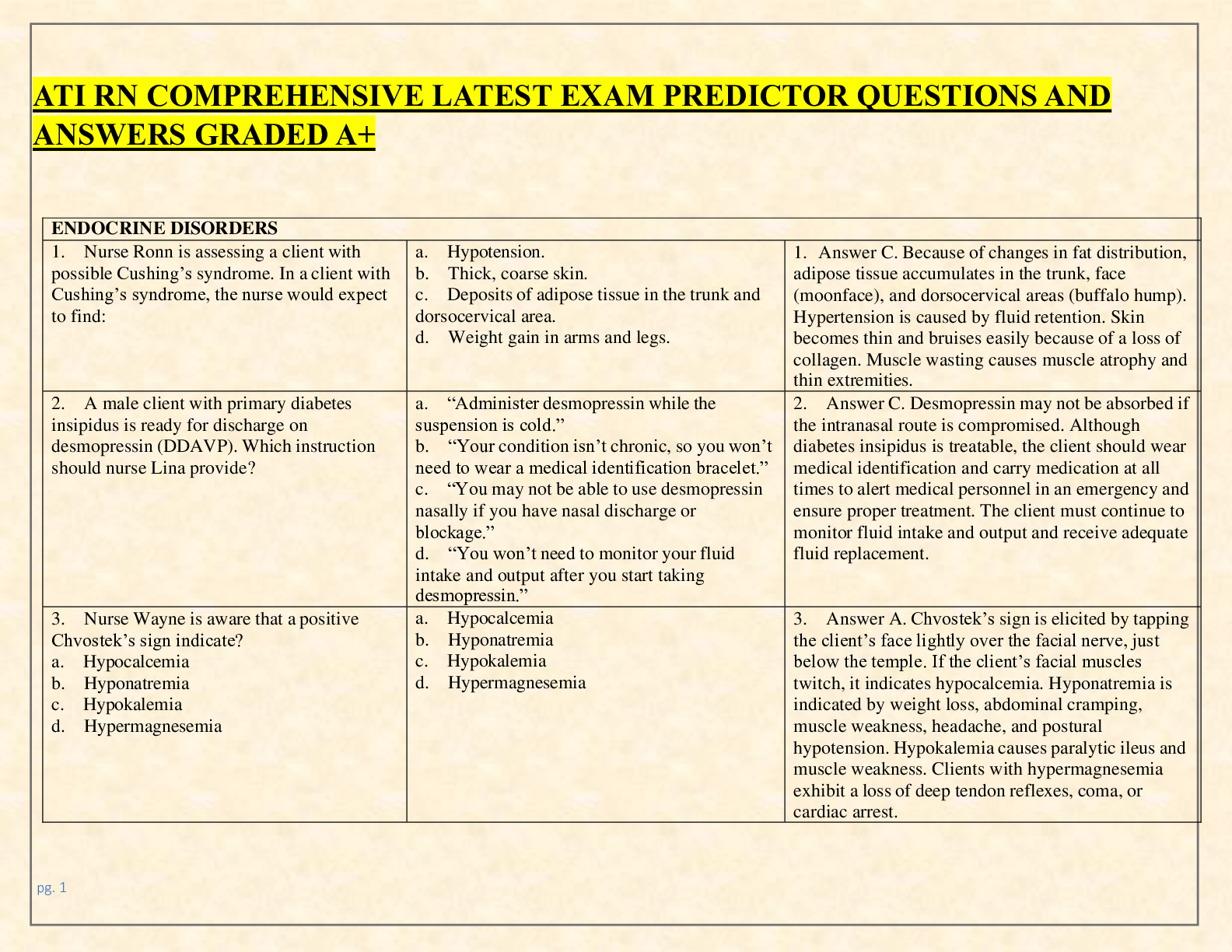
ATI NCLEX Exam and Assessments Review ATI NCLEX Exam and Assessments Review Acronyms to Remember • All People Eat Taco Meat o Aortic Regurgitation – listen to 2nd intercostal • VEAL CHO... P MINE o Variation deceleration cord compression Move patient side to side o Early deceleration head compression Identify Labor progress o Acceleration okay Nothing o Late deceleration placental insufficiency execute actions immediately • CWS (chips with salsa) o Cane weak then strong • COAL o Cane opposite of affected leg • If R is far from P, its first degree Heart Block • If Ps and Qs don’t agree, you have a 3rd degree Heart Block • RICE rest, ice, compression, elevate for tractions! o 2 common types ▪ skin or skeletal • For skeletal pin site care & manage weight ▪ Ice should be on for 30 min, then out of 30 min • 6 P’s o Pain o Paresthesia (pins and needles) o Pallor o Pressure o Paralysis o pulselessness Assessments to Remember • To check Mcburney’s point – lower right side of stomach for appendicitis • To asses for Liver Tenderness – palpate right upper quadrant • To assess for venous thrombolytic event (VTE) – assess dorsiflexion and extension of the foot o Homan’s sign Medication to Remember • Bronchodilator endings “terol” o Beta agonist o Promote beta system relax smooth muscles in body ▪ Causing bronchodilation & increased HR ▪ S/E increased myocardial • 3 step plan for pain management o Mild pain NSAIDs & acetaminophen (non-opioid) o Moderate pain opioids (hydromorphone [morphine]) & combo (Vicodin, Percocet) o Severe pain adjuvants (anti-seizure [Neurontin, gabapentin], SSRIs, marijuana) ▪ In this step, you are adding onto the pain regiment by trying to alternate the perception of pain • Opioid Agonist o Hydromorphone ▪ Use: pain ▪ SE: Respiratory depression, nausea (makes everything low and slow) • If RR depression occurs x<10 while on IV hydromorphone, stop hydromorphone & contact the provider. Might need naloxone • Insulins o Long acting insulin (Detemire, Lantus) ▪ Indication: DM1 & DM2 (usually for surgery since they are NPO for a long time) • Taken once a day at night, just like how pancreas does it ▪ SE: N/V, hypoglycemia o Give in between meal snack before peak, because then risk for hypoglycemic o Rapid Acting insulin (aspart) ▪ SE: hypoglycemia ▪ Give it 5-10 min prior to eating • Oral Anti-diabetic (Reglan, Metformin) o Indication: type 2 diabetic with good urinary system o SE: Anorexia, nausea, diarrhea ▪ Hypoglycemia not an expected effect unless combined with other medication ▪ Tip: For Metformin, hold 2 days before and 2 days after IV contrast • Risk for Lactic Acidosis [metabolic acidosis] o Lactic acid is a metabolic acid • If they have kidney problem, give Acetylcysteine (Mucomyst) • Ergot Alkaloid (Methylergonovine) o Indication: Postpartum bleeding (massive vasoconstrictors) o SE: Nausea, headache, hypertension (vasoconstriction causes BP to go up) ▪ Risk for postpartum hemorrhage (boggy uterus) retained placenta, full bladder, overstretched or overworked uterus (twins, many labor, long labor, injured), uterine atony, impaired maternal clotting • Intervention: fundal massage (Credes massage), check bladder and empty if necessary, give oxytocin (IV, IM, breast feeding) or methylergonovine o Do not give methylergonovine if they are hypertensive! o CHECK labs! prostaglandins (prost-) as it causes massive smooth muscle contracts like GI o Last resort, hysterectomy • Antineoplastic/Immunosuppressants (Methotrexate) o Indication: RA, cancer, psoriasis, Crohn’s ▪ Works on rapidly dividing cells & lowers inflammation by decreasing those WBC action • Anticonvulsant (Neurontin & pregablin) o Indication: Partial seizures, neuropathic pain o SE: Drowsiness, dizziness, fatigue ▪ Has short half-life so is given 3x a day (peak in 2-3 hours) o Pregablin ▪ Indication: neuralgia, partial seizure, fibromyalgia ▪ SE: dizziness, ataxia, confusion, weight gain ▪ How to assess pain in non-verbal patient? • Grimacing, guarding, restlessness • Organic nitrate (Nitroglycerin) o Indication: Angina o Route: patch, sublingual, paste, IV ▪ 1.5 in of paste if used as paste ▪ If IV, MUST BE ON PUMP • Narrow therapeutic because technically causing small shock o SE: headache, hypotension, tachycardia ▪ More vascular space = better profusion o Safety precaution: FALL risk ▪ Vasodilation causes dizziness ▪ Check BP constantly while giving Angina ▪ If BP is too low and losing consciousness due to too much organic nitrate, give LOTS OF FLUID (bolus) & put patient in severe Trendelenburg to profuse and massage legs. Put on oxygen on highest to increase oxygen carrying capacity • Talk to him to constantly check LOC • Uterine Simulant (oxytocin) o Indication: Induce or augment labor, postpartum hemorrhage o SE: tachysystole (fast contraction), uterine rupture, elevated BP, fetal hypoxia ▪ Oxytocin is Tocolysis • Tocolytic is stops contraction (opposite of oxytocin) o Ex: terbutaline, CCB, Magnesium (relaxes uterus muscle) • Proton pump inhibitor (-prazole like pantoprazole, esomeprazole) o Indication: GERD o SE: Diarrhea, osteoporosis, pneumonia ▪ Why is a client at risk for pneumonia when using pantoprazole? • Because we are altering the acidity of stomach acid and less stomach acid is killed o Alteration in GI flora ▪ Esomprazole taken 1 hour prior to eating to stop proton pumps ▪ Change in ph effect calcium absorption • So more diarrhea, and higher risk of osteoporosis • Atypical Antipsychotic (risperidone, Haldol) o Indication: schizo, acute bipolar mania, autism o SE: weight gain, dyslipidemia, diabetes ▪ ALL ANTIPSYCHOTIC cause agranulocytosis ▪ Atypical has less SE ▪ Monitor cholesterol and hyperglycemia because drug effects metabolism • Which causes weight gain • Glucocorticoid (methylprednisolone & prednisone [ –sone & -solone]) o Indication: inflammation o SE: euphoria, infection, cushing’s syndrome, ▪ Hyper- adrenal gland (Cushing’s syndrome) • = higher 3s sugar, salt, steroid o Where ever water goes, salt goes o Wound not healing well because of SE o High BP because retained fluid o Low potassium because high sodium ▪ Low calcium so risk for osteoporosis ▪ Hypo- adrenal gland (Addison’s because you need to add water) • = low 3s sugar, salt, steroid o bronzing color of skin o high potassium & high calcium because low salt o Low BP o Fluid deficit, weight loss & salt craving ▪ When taking fluticasone :prophylaxis for asthma; SE: candidiasis, hoarseness • Take it daily because its prophylaxis • Glucocorticoid/bronchodilator (budesonide/fortemolol) o Indication: prophylaxis in chronic restrictive airway diseases (asthma, COPD) o SE: GI upset, infection ▪ Risk for infection because it is an immunosuppression • Beta blocker (-olol) o Indication: HTN, angina o SE: bradycardia, AV heart block, heart failure, bronchoconstriction o Black box waning is will get exacerbation of angina/MI if abruptly discontinued ▪ MUST be tapered • Hypothyroidism Hormone (levothyroxine) o Give on empty stomach because absorbed the best then ▪ Increases metabolic rate and may cause interference with sleep o SE: tachycardia, nervousness, insomnia ▪ Stimulating hormone ▪ Hyper-thyroids • TIGGER! everything is moving fast, and always on the move o Unintentional weight loss, heat intolerance, high vital signs (high BP & RR), everything moves fast, insomnia, diarrhea ▪ Hypo-thyroidism • Eeyore everything is bad and sad o Cool, cyanotic, broken hair and nails, low HR, low BP, low RR, everything moves slow, constipation, urinary retention • Antibacterial (glycopeptide ) Vancomycin o Indication: c.diff, MRSA o SE: nephrotoxicity, “red man syndrome” ▪ Monitor BUN & Creatinine • Normal BUN = 10-20 • Creatinine = 0.6 – 1.2 • Cholinesterase inhibitor (donepezil) o Indication: mild to severe Alzheimer’s disease o SE: N/V, diarrhea, GI bleeding, anorexia, dizziness, bronchoconstriction o Take it at BEDTIME, may cause vivid unusual dreams so implement safety precaution • Platelet Aggregation Inhibitor (Clopidogrel) o Indication: prevent stenosis after cardiac stent placement, MI & CVA o SE: abdominal pain, dyspepsia, diarrhea, bleeding ▪ Platelet main goal is to stop bleeding so likes to stick to clots • Inhibiting it is like spraying cooking spray o Assess! ▪ Platelet count, H&H, epistaxis, bruising and bleeding • Mood Stabilizer (Lithium) o Indication: bipolar Disorder o SE: Anorexia, confusion, thirst ▪ Lithium competes with Sodium (inverse proportion) • Signs of Lithium Toxicity o Tremor, vomiting, diarrhea, drowsiness, slurred speech, o Levels: 1 is good, 2 is bad o Keep sodium level consistent (too much sodium will counter effect the lithium levels) • Lisinopril – htn hf, acute MI, SE: persistent dry cough, hyperkalemia, renal failure, angioedema • Rifampin – antibiotic; SE: hepatotox; body fluids orange; WATCH LFTs • Antipsychotic (Haloperidol) o Indication: Schizo, Acute psychosis, Tourette’s o SE: mild leukopenia, EPS, TD, laryngospasm, respiratory depression, NMS ▪ EPS: dystonia, tardive kinesis, ▪ Neuroleptic malignant syndrome (NMS) • Caused by too many neurotransmitter, like serotonin syndrome o Symptoms: rigidity, sudden high fever, blood pressure instability, headache • Adenosine o Indication: paroxysmal SVT (antidysrhythmic) o SE: bradycardia, dyspnea, hypotension, flushing, chest discomfort o PUSH it in fast & patient must be on heart monitor ▪ Should convert to normal sinus rhythm or atrial tach. • Sedative-hypnotic (Zolpidem) o Indication: Insomnia o SE: Daytime fatigue and drowsiness, dizziness o What changes in behavior and mental health may occur? ▪ Sleep complex behavior, depression ▪ ALL short term. No more than 14 days • High risk of dependence • Enoxaparin – anticoag, DVT prevention, ischemia, SE: bleeding, neuro injury • Anti-dysrhythmia (amiodarone, -rone) o Indication: a-fib, V-fib, V-tach o SE: pulmonary toxicity, liver injury, heart block ▪ Hard on body all around esp. for Ventricular dysrhythmia ▪ Avoid grapefruit because it changes the acidity of the stomach & influences the absorption o What findings indicate respiratory failure? ▪ Dyspnea, rales, friction rub etc. • Atypical antipsychotic (aripiprazole) o Indication: schizo, major depression, autism, bipolar o SE: anxiety, insomnia, agitation, EPS o What mental health safety concerns are associated with this med? ▪ Increased depression, suicidal ideation • Epoetin Alpha o Indication: anemia (CKD/Chemotherapy) o SE: HTN, thrombotic stroke, clotting of AV fistula o Hat labs should the nurse monitor? ▪ HY&H, CBC, potassium • Bisphosphonate (risedronate –dronate) o Indication: osteoporosis o SE: bone pain, leg cramps, colitis o Taken once a week for osteoporosis ▪ Stand up 30-1 hour and remain NPO after taking the med ▪ Take the med on empty stomach with full glass of water o Taken once a day for paget’s disease • Fentanyl – narcotic analgesic; SE: resp dep; patch worn for 72 hrs • Pain Scales o FLACC scale good for 2-7 years o Cries scale for 0-3 months o Wong baker good for non-communicant and child • Calcium Channel Blocker (Diltiazem & Verapamil) o Indication: HTN, angina, A-fib, A-flutter, SVT o S/S: Weight gain, edema, dyspnea • Smoking Cessation Aid (Varenicline) o Indication: helps with stopping smoking o SE: nausea, anorexia, unusual dreams, mood changes o Expect to take 12 weeks & take med 1 week before • Fluoroquinolone o Indication: pneumonia, sinusitis, skin infection o SE: tendonitis, photosensitivity o If patient has pain before giving the dose, hold the dose, place the patient on bed rest and notify the provider as it can be related to tendonitis! (tendonitis takes many months to heal) • Statin (Atorvastatin) o Indication: lower cholesterol & LDL level & raise HDL level o SE: rhabdomyolysis, hepatotoxicity ▪ Watch LFT closely! • Phosphodiesterase inhibitor (sildenafil –afil) o Indication: erectile dysfunction o SE: hypotension, priapism, flushing ▪ Major vasodilator, so do not take with NTF (nitroglycerine) • SSRI- sertraline`fe o Indication: depression, OCD, PTSD, panic attacks o SE: insomnia, agitation, weight gain, sexual dysfunction, suicidal thoughts o Should instruct to wait 2 weeks when stopping MAOI and starting sertraline ▪ Taper off, wait 2 weeks and then start the next drug ▪ Furosemide (Lasix)– loop for HF, renal/hepatic failure SE: hypokalemia, ototoxicity • Dutasteride o Indication: benign prostatic hypertrophy o Se: low ejaculate & libido o Cannot donate blood as it is a 5-alpha-reductase inhibitor & if it goes into women, high chance of birth defect ▪ Don’t touch the medicine! It is absorbed through the skin. Always absorb glove!! • Pheynytoin o Indication: seizure o SE: gingival hyperplasia, thrombocytopenia, ▪ Susceptible to Steven Johnson • Stop med and notify provider if they have flu likes S&S and skin rash • Avoid all CNS depressant & glucocorticoid • Digoxin o Class: cardiac glycoside, inotrope o Indication: HF & dysrhythmias o SE: dysrhythmias, anorexia, nausea, fatigue, yellow tinge to vision o Monitor dig. level, potassium and apical pulse ▪ Potassium & dig level work opposite! LABS • Potassium o Hypokalemia ▪ Caused by Diuretics, corticosteroids, diarrhea/GI suction • Lose GI fluid, then lose K* ▪ S&S • Skeletal muscle weakness shallow respiration • Dysrhythmias ▪ Intervention: • Replace K & treat underlying cause o DO NOT PUSH POTASSIUM (that is lethal injection) o Hyperkalemia ▪ Caused by renal failure, salt substitutes, packed RBCs, Addison’s disease ▪ S&S • Dysrhythmias peaked T-waves • Muscle weakness paralysis ▪ Intervention • Kayexalate or regular insulin • Calcium o Hypocalcemia ▪ Caused by • Hypoparathyroidism • Renal failure • Malabsorption ▪ S&S • Changes in HR, prolonged ST • Tetany • Change in LOC seizure ▪ Intervention: • Replace Ca or give Vitamin D o Hypercalcemia ▪ Caused by • Hyperparathyroidism • Excessive intake of Ca or Vitamin D ▪ S&S • Dysrhythmias cardiac arrest • Blood clots • Confusion coma ▪ Interventions • Increase mobility & dialysis Interventions to Remember • Pain that relieves when resting (doesn’t matter where it occurs) – intermitted blockage claudication o Artery that is not receiving enough oxygen ▪ Symptoms • Weak Pulse • Cool to touch • Shiny color • Pain when use o Position that area independently (V is for venous, legs up; A is for artery, legs down) • 4 blood transfusion type reaction o are hemolytic, febrile, mild allergic and anaphylactic o then, stop the transfusion! • Tracheostomy Intervention o Place an air humidifier at the bed side o Suctions intermittently for up to 10 seconds o Use tracheostomy gauze that is already pre-cut to put around the tracheostomy tube ▪ If cutting a 4x4 gauze, then possible for the bandage to get caught • Risk for aspiration and infection o Do not remove ties before cleaning the tracheostomy ▪ Cartilage not formed, so if patient coughs, trach will fall out • Cervical Spinal Cord Injury o No motor no urination, most likely no respiration, no movement o Use “ABC”s to prioritize • Triage o Fixed pupil low survival rate (CNS injury) o Agonal respiration low survival rate o Open fracture usually yellow tag, as it is not as emergent o Notify health department of infection disease ▪ Ex. Ebola (incubation period is 21 days) • Delegation o PN & LPN (practical nurse) ▪ Help with transfer to a rehab ▪ Take care of Stable Client ▪ Gather Data ▪ Contribute to Care Plan ▪ Reinforce Teaching ▪ Monitor IVFs and Blood Transfusion ▪ Administer Piggyback o RN ▪ Discharge teaching ▪ Take care of Unstable Clients ▪ All Assessment ▪ Initiate Care Plan (all Initiation) ▪ Teaching Blood Products ▪ IV fluids and IV push Medications o AP (assisted personnel) ▪ Stable Clients ▪ Obtain Vital Signs ▪ Gather Specific data ▪ Hygiene Care ▪ Bed Making ▪ Feeding ▪ Positioning ▪ Ambulation • Multiple Skeletal Fracture o When skeletal fracture occurs, fats are released ▪ Risk for Fat emboli ▪ Usually shown, couple hours before • Late sign is disorientation • Crutch Walking o Make sure the patient is tolerating upright position & not dizzy o Once patient is standing, have her place one crutch under each arm ▪ Crutch should be 6 in up and 6 in on the side of the feet o 4 point is for partial weight bearing (less stable & need more support) ▪ for light weakness like stoke ▪ Right crutch left foot left crutch right foot o 3 point for non-weighting bearing on one leg ▪ : . : o 2 Point for partial weight bearing on both leg ▪ left foot & right crutch forward right foot & left crutch forward o Swing-gait vs. Swing Through ▪ Swing gait is when you have stability ▪ Swing through is when you can bear weight on both leg and have good stability ▪ Swing-gait only swings to the level of crutches, while swing through in front of the crutches ▪ Nurse stands behind and to the side o Standing to Sitting ▪ Slide to the back until touching the bed ▪ Place both crutch on one side ▪ Lean as you sit o Stairs ▪ Going up • Step up with the good leg • Bring bad leg and the both crutches up beside the unaffected leg ▪ Going down • Place bad leg and the crutches down the stairs • Then, follow by good leg • Cane opposite of affected BUT Walker with the affected leg • Tet spell – Big Cardiac Issue o Squat and re-oxygenate & they get up and go again ▪ Because squatting increase the intravascular pressure o All because they have tetralogy of fallot ▪ Thick right ventricle and thin left ventricle (opposite of normal) ▪ So, deoxygenated blood is pumped • TPN o To prevent fluid volume deficit, monitor blood glucose every 4-6 hours ▪ If too much glucose, water imbalance will occur if glucose stays in intervascular space • Intracellular fluid volume depletion • Hyperglycemic water comes from the cell to dilute the outside • Management of Care (Most heavily focused area on NCLEX) o Nurse is negligent ONLY if she causes long-term harm to the patient ▪ Even if she administered the wrong dose, if there is not long-term harm, it is not negligence. • But, still need to report it in the matter of integrity o Conflict ▪ Competing win & lose ▪ Accommodating lose & lose ▪ Smoothing lose & lose ▪ Avoiding lose & lose ▪ Collaborating Win & Win o 5 rights of delegation ▪ Right person ▪ Right task ▪ Right Circumstance ▪ Right Communication ▪ Supervision • Determine assignment by acuity of client o To be fair • New Nurse should not often volunteer to help other team members to minimize interruption o Constant interruptions = higher risk for mistake Safety Control • Disaster Planning o Phases of Planning ▪ Disaster Preparedness ▪ Disaster Response ▪ Disaster Recovery o Includes ▪ First Responders ▪ Warning System ▪ Nursing Roles ▪ Chain of Command o ED Triage = treat most severely injured first o Disaster Triage = treat who can be saved ▪ Red = immediate ▪ Yellow = delayed ▪ Green = minor ▪ Black = expected to die • Nurses role when notified of disaster o Call in additional nurses o Identify who can be discharged to make room o Refer to facilities disaster planning • Placing Patient in Seclusion o Can’t be in seclusion if they have history like seizures or diabetic o Check up on them at least every 30 min until they are calm o Need order for seclusion • Radiation Implant o Save linens in client’s room o Assign client to private room o Limit each visitor to 30 mins a day o At least 6 ft. away o Place a caution sign on door o Put on shielding including thyroid protector and dosimeter and provide case asap ▪ Dosimeter measures how much radiation you’re exposed to o Pregnant staff cannot be assigned to the patient • Dressing Change o PICC line sterile o Gastrostomy tube clean o TPN via central line sterile o Even if sterile water was spilled on sterile field, you must start over! • Sterile Field o Open top flap away from body o Open side flaps o Turn last flap down toward body o Drop additional sterile supplies to center of field (open package and let it drop!) o Prepare to pour sterile solution into receptacle o Don sterile gloves • Don sterile loves o With the non-dominant hand grasp the inside of the dominant hand glove by the inside of the cuff o Pull the glove over the dominant hand o Slip the fingers of the dominant hand under the folded, sterile side of the cuff of the glove for the non-dominant hand o Slip the glove onto the non-dominant hand o Interlock fingers to fit the gloves onto each finger • Order of protection o Gown mask goggles gloves enter room • HIV transmission o Maintain standard precaution o Cover cuts and sores o Do not share personal items o Dispose of needles properly o Wear gloves for contact o Clean/disinfect surfaces • Meningitis o Very high mortality and morbidity rate o Nerve conduction malfunction o Diagnostic test spinal tap & blood culture ▪ Everything done BEFORE antibiotics are given o Prevention hand-hygiene, immunization and avoiding contact with secretion o Assessment Brzezinski’s sign & Kernig’s ▪ Brudzinski’s sign when you raise head, knee goes up ▪ Kerning’s sign if you bend the knee, head comes up ▪ Symptoms: headache, stiff neck, photophobia o Intervention: ▪ Antibiotic therapy ▪ Seizure precautions • Quite environment/private room • Less stimulant (answer alarms right away) • Dim lights • Padded railing • Premature Rupture of Membrane o Rupture of membranes one hour or more before onset of labor o Assessment ▪ Confirm fluid is amniotic ▪ VS Q4 hour ▪ Non-stress test • Monitor uterine contraction pattern and FHR o PPROM – rupture any time before 37 weeks gestation o Manage Care ▪ Antibiotic therapy ▪ Maintain bed rest ▪ Address psychosocial ▪ Biophysical profile ▪ Avoid vaginal exams • Sepsis/Septic Shock o What changes will you see? ▪ Tachycardia, Low BP, Vascular changes, more edematous, CNS alterations, renal, respiratory compromise o Interventions ▪ Broad spectrum antibiotics, progress oxygen, fluids, inotropic medication (dopamine), monitor GFR, bun, creatinine • Higher lactic acid = worse sepsis ▪ INCREASE vascular volume ▪ Trendelenburg & with legs up to move fluid to head and heart • Neonatal Sepsis (up to 30 days of life) o Expected signs and symptoms ▪ Temperature instability, poor feeding effort, tachypnea, low blood sugar, lethargy ▪ Normal Neonatal RR: 20 – 60 o Interventions ▪ Cultures ▪ Antibiotic Therapy ▪ Maintain Hydration ▪ Ventilator Support • Reportable Disease o Zika, Syphilis, Salmonella, Foodborne outbreaks, Giardai o Chlamydia, Gonorrhea, syphilis, HIV, hepatitis B, TB, meningitis, pertussis, Hep A & C, varicella, VRSA, Ebola, Lyme disease Basic • Blood Transfusion o 2 nurses verify blood with client ID o Informed consent o Baseline vital sings o 20 gauge (or larger) IV catheter o Administer with 0.9% NaCl only o After ▪ Stay with client for first 15 min. ▪ Compare next set of vital sings to baseline ▪ Begin infusion slowly ▪ Stop blood immediately if signs of transfusion reaction ▪ Complete infusion within 4 hours • Radiation o Symptoms: ▪ Impaired skin integrity ▪ Internal emits radiation ▪ Fatigue o Intervention: ▪ Skin care ▪ Protect others ▪ Energy conservation ▪ Frequent oral hygiene using soft bristle or oral swabs ▪ Radiation markings • Can be washed with soap & water • But no powder or lotion • Congenital & Pediatric Heart conditions o Ductus Arteriosus – skips lungs & connects pulmonary artery to aorta ▪ Symptoms • Displaced apical pulses • Murmur • Bounding pulses ▪ Interventions • Prepare to administer prostaglandins • Prepare for cardiac cath & surgical thoracoscopic repaired o Kawasaki’s disease ▪ S/S • High fever 5-14 days • Bright red non-blistering skin rash, strawberry red tongue, red eyes • Myocarditis ▪ Intervention • Prepare to administer gamma globulin and aspirin • IV hydration • Monitor cardiac status o Cardiac myopathy ▪ Symptoms • Tachydysrhythmias • Activity intolerance • Hypoxia and dyspnea • Clubbed fingers ▪ Interventions • Cluster activities for energy conservation • Monitor cardiac status • Monitor I&O o Pediatric Rheumatic Heart Disease ▪ Symptoms • Carditis • Polyarthritis • Subcutaneous nodules • Group A BH streptococcal pharyngitis recently ▪ Intervention • Rest • Antibiotics • Nutrition • Angina/Myocardial Infarction o Risk Factors ▪ Family history ▪ Hyperlipidemia ▪ Tobacco use ▪ Hypertension ▪ Diabetes mellitus ▪ Inactivity & obesity o Stable angina relieved by rest o Unstable is called pre-infarction o Prinz metal’s caused by coronary artery spasm o MONA, but prioritized is ONAM • Stroke o S&S ▪ Change in mental status • Earliest sign of increasing ICP ▪ Slurred speech and dysphagia ▪ Weakness on one side ▪ Visual disturbance ▪ Sudden severe Headache o Intervention o S & S ▪ Chest pain ▪ Dyspnea ▪ Fatigue ▪ Pallor ▪ Palpitation ▪ Nausea ▪ Baseline level of function and Glasgow coma scale ▪ Monitor for aspiration due to risk of dysphagia ▪ Establish means of communication ▪ Hemiparesis ▪ Hemiplegia: will cause safety issue • ECG interpretation o P-wave is atrial (atria contract due to functioning SA node) depolarization o QRS is ventricular (ventricle contract due to bundle of his) repolarization ▪ Sodium out & potassium in o T wave is o Normal ventricular rate is 20-40 o 5 question we ask every time ▪ Is there a p-wave? • Tells if the SA node is functioning ▪ Is there a QRS complex? • Tells me if the AV node is functioning • Narrow QRS means that the impulse comes from above the ventricle • If it is wide and bizarre, impulse comes from the ventricle ▪ What is the rate? • Count 15 blocks right before the first P wave, then count the R waves and multiply by 20 ▪ Is it regular or irregular? ▪ What does the P and QRS waves look like? o What can cause Sinus Tachycardia? ▪ Anemia because you don’t get enough oxygen ▪ DKA because you have too much O2 o What can cause Sinus bradycardia? ▪ Valsalva Maneuvers and Carotid massage • PICC line o After cleaning the site, withdraw 10 mL of blood and discard it o Never flush with sterile water. Only Normal Saline • Shock o Cardiogenic ▪ Result of direct pump failure ▪ Causes • MI, cardiac Arrest, cardiomyopathies ▪ Symptoms • Tachycardia, hypotension, pulmonary congestion, chest discomfort o Hypovolemic ▪ Low blood volume leads to inadequate tissue perfusion ▪ Causes • Surgery, trauma ▪ Symptoms • Increase in HR, decrease in pulse pressure, decrease in UO, mild acidosis o Urine output is an indirect, but accurate way of cardiac output o Distributive ▪ Blood is distributed to the interstitial tissues where it cannot perfuse organs ▪ Causes • Neurogenic neural induced pain • Anaphylactic • Septic capillary leak with burns, infection ▪ Symptoms • Decrease in MAP o Mean Arterial Pressure ▪ (systolic + 2* diastolic)/3 • Heart Sounds o Lub tricuspid and mitral o Dub aortic and pulmonic o S3 gallop ken-tuck-key as it doesn’t close on time • Right and Left Heart Failure o Right Side ▪ S&S • All things peripheral because fluid comes from the right side • JVD • Elevated CVP • Edema • Ascites • Weight gain o Left Side ▪ S&S • All things pulmonary since fluid comes from the lungs • Dyspnea • Fatigue • Frothy Sputum • Bibasilar Crackles • Elevated PAWP • S3 gallop o Interventions ▪ Respiratory – oxygen, fowler’s position, lung sounds ▪ Fluid management – I&O, fluid restriction, daily weights ▪ Cardiac – diuretic, ACE inhibitors, digitalis • Want to decrease afterload so there is no resistance • Dig • Diabetes Mellitus o Inotropic – squeeze harder o Chronotropic - slower o Hypoglycemia Symptoms ▪ Cool, clammy (needs some candy) ▪ Tired, restless ▪ Hunger ▪ Palpitations ▪ Confused ▪ Diaphoresis o Hyperglycemia Symptoms ▪ Polyuria ▪ Polydipsia ▪ Polyphagia ▪ Fruity Breath (like acetone) • When body burns fat, they produce ketone ▪ Kussmaul respiration ▪ Tachycardia o DKA is caused by LACK of insulin ▪ S/S Cirrhosis • Hyperglycemia • Dehydration • Acidosis ▪ Usually seen in type 1 DM o Hyperglycemic-hyperosmolar state (HHS) caused by insulin deficiency and profound dehydration ▪ Usually seen in type 2 DM o Long Term Issues ▪ Nephropathy, Neuropathy, retinopathy o Acute Complications ▪ Priority intervention is fluid & airway! • Think ABC! ▪ If you have high glucose and potassium, treat glucose first • Glucose and potassium will follow • Function o Protein metabolism ▪ Produces ammonium as by-product ▪ However, if you have cirrhosis, produces ammonia (deadly) o Produces Albumin o Vitamin synthesis (manage all of it) o Metabolize Medication o Produces clotting factors • S&S o Portal Hypertension o Esophageal Varices o Clotting abnormalities o Hepatic encephalopathy o Ascites/peritonitis o Altered Nutrient and vitamin metabolism • Nursing Intervention o Assess fluid balance o Assess o Limit Protein Intake Burn Care • Priority o 1. Secure airway o 2. Fluid replacement o 3. Maintain comfort o 4. Prevent infection o 5. Maintain body temperature o KNOW THE RULE OF NINES! Group B strep – might get early labor. Monitor Coombs test – if mom is Rh Ob procedure • Amnioinfusion – relieves umbilical cord compression that results in variable deceleration • Fetal scalp sampling – determines if fetus is getting enough oxygen during labor. Take blood from fetus’ head after water broke, then send it to lab to determine it • Chorionic Villus sampling – the client is instructed to fill the bladder prior to procedure. Done to test a genetic malformation. Done around 27 weeks. • Amniocentesis – withdrawing fluid and testing the chromosome to determine fetal lung maturity and chromosomal disorders • Non-stress test – performed 3rd trimester to evaluate fetal wellbeing by checking fetal heart monitoring Fetal Heart Monitoring • Early Deceleration good sign! Means that birth is getting closer o Decelerate earlier than contraction o Head compression o Mirror image of contraction o Variation of baseline • Late deceleration hypoxic baby! o Decelerate later than contraction o Begin at or after the peak of contraction o Due to inadequate fetal oxygenation (usually caused by placental deficiency) o Intervention ▪ Turn (left lateral) ▪ IV fluid bolus ▪ Oxygen ▪ Discontinue oxytocin (1st intervention) ▪ Provider notified ▪ Prepare for delivery Hypertension in Pregnancy • Preeclampsia o After 20 weeks o Recognized by hypertension and proteinuria o Interventions ▪ BP and daily weight ▪ Urine protein ▪ BUN ▪ Assess for edema • Eclampsia o Includes the onset of seizure activity o Intervention ▪ Maintain Patent Airway ▪ Pad Side rails ▪ Complete bed rest ▪ Decrease Stimuli ▪ Meds to maintain Hypertension and maintain blood pressure • CCB (main med for after first 24 hours), Mag for first 24 hours ABG • Rules of compensation o Uncompensated pH and 1 other not within expected range o Partially compensated all 3 values not within expected range o Fully compensated only pH within normal range • Examples o Pulmonary Embolus ▪ Would cause Respiratory Acidosis will have dyspnea and tachypnea • Restlessness and anxiety • Chest pain • Diaphoresis ▪ Can have more than one pulmonary emboli Sensory • Retinoblastoma o Intraocular tumor of childhood o S&S ▪ White eye reflex • Meniere’s ▪ Strabismus (cross eyed) ▪ Red and painful eyes o Abnormal inner ear fluid balance o S&S ▪ Episodic vertigo ▪ Tinnitus ▪ Fluctuating hearing loss o Intervention ▪ Low-sodium diet [Show More]
Last updated: 1 year ago
Preview 1 out of 27 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Nov 07, 2022
Number of pages
27
Written in
Additional information
This document has been written for:
Uploaded
Nov 07, 2022
Downloads
0
Views
33