*NURSING > EXAM > BIO 669 Quiz 5 - Pulmonary Function Questions and Answers Latest updated 2022,100% CORRECT (All)
BIO 669 Quiz 5 - Pulmonary Function Questions and Answers Latest updated 2022,100% CORRECT
Document Content and Description Below
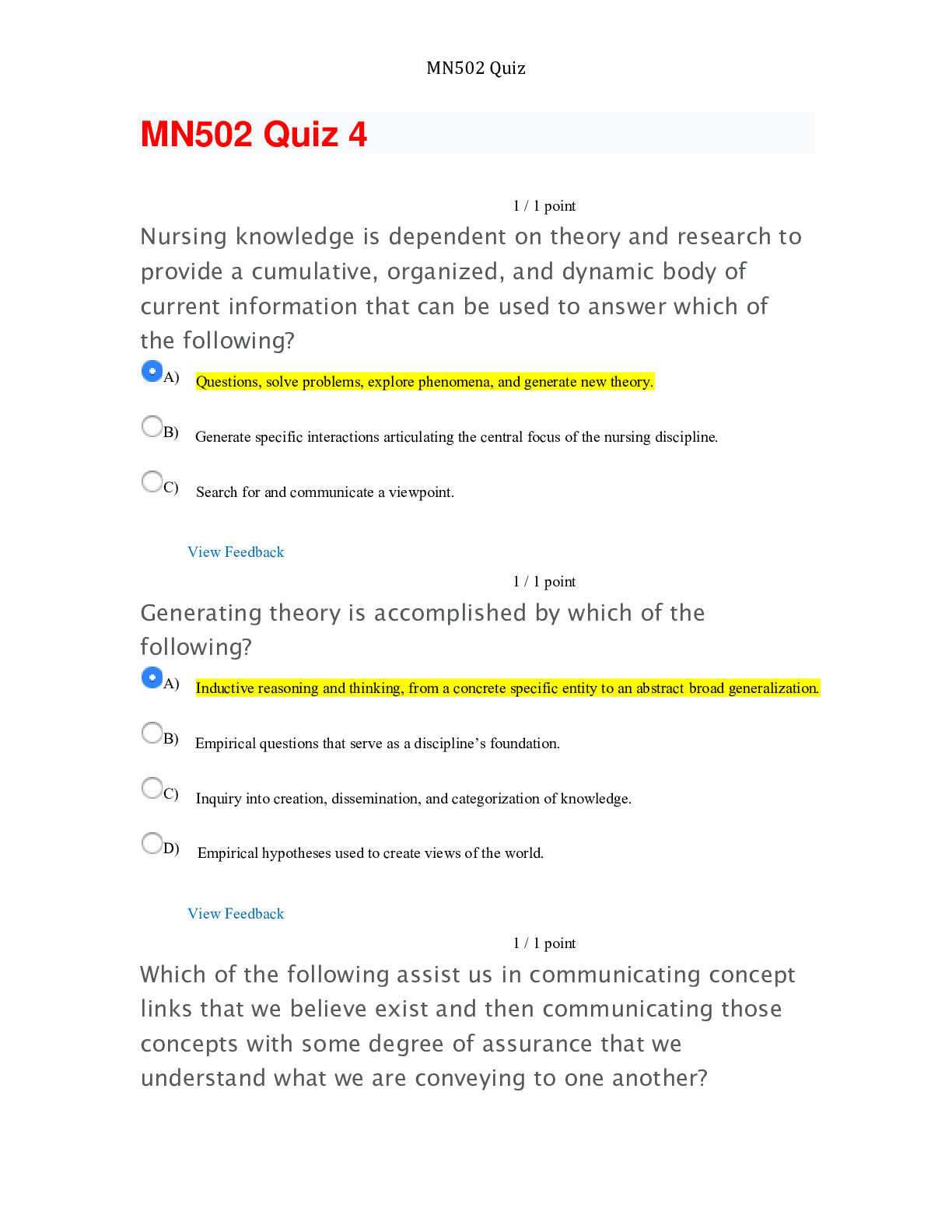
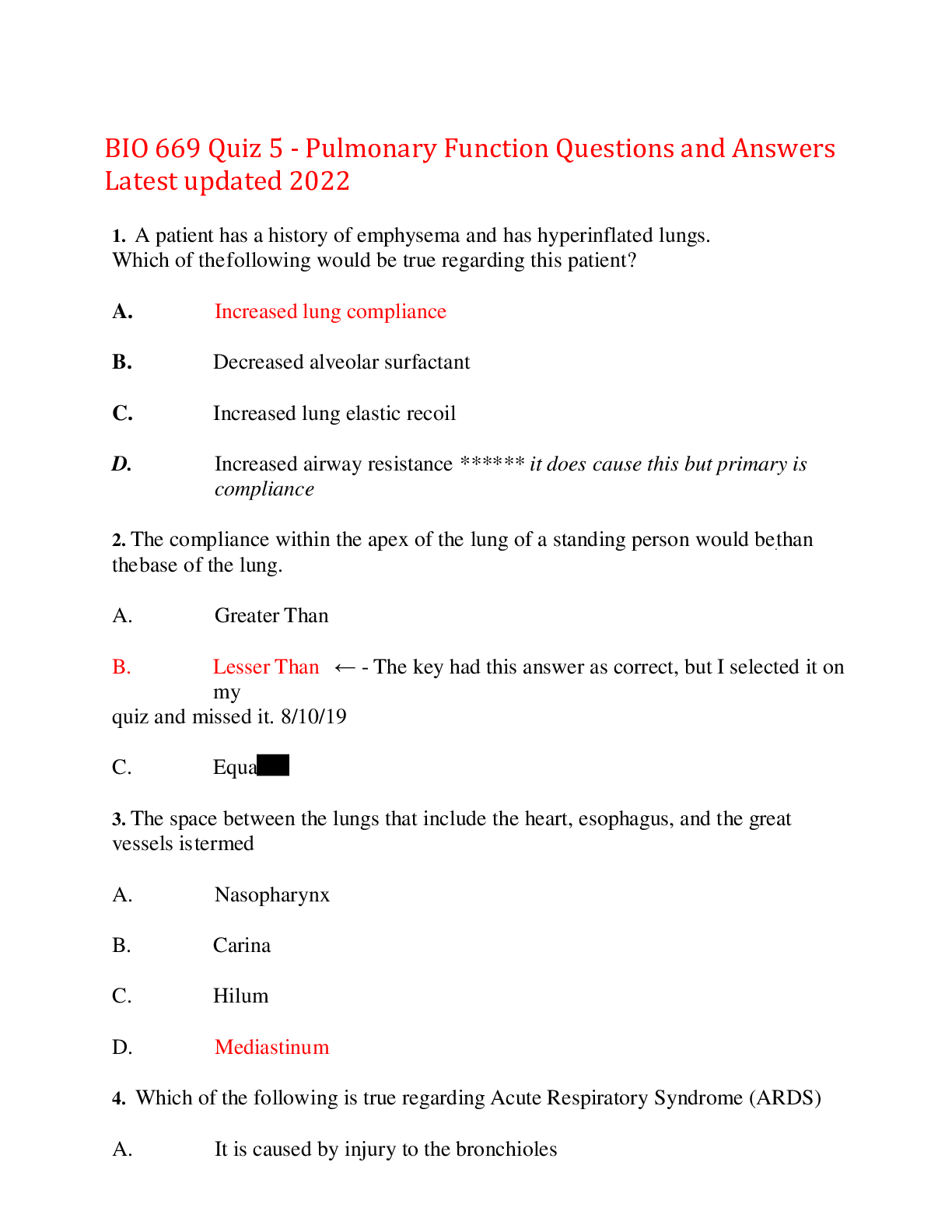
BIO 669 Quiz 5 - Pulmonary Function Questions and Answers Latest updated 2022 1. A patient has a history of emphysema and has hyperinflated lungs. Which of the following would be true regarding thi... s patient? A. Increased lung compliance B. Decreased alveolar surfactant C. Increased lung elastic recoil D. Increased airway resistance ****** it does cause this but primary is compliance 2. The compliance within the apex of the lung of a standing person would be than the base of the lung. A. Greater Than B. Lesser Than ← The key had this answer as correct, but I selected it on my quiz and missed it. 8/10/19 C. Equal 3. The space between the lungs that include the heart, esophagus, and the great vessels is termed A. Nasopharynx B. Carina C. Hilum D. Mediastinum 4. Which of the following is true regarding Acute Respiratory Syndrome (ARDS) A. It is caused by injury to the bronchioles B. It can cause severe pulmonary edema C. It is most commonly caused by exposure to inhaled irritants D. Macrophage and neutrophils are not involved in the response 5. Pulmonary fibrosis is most likely to result in all of the following except A. thickening of the alveolocapillary membrane B. Decreased diffusing capacity in the lungs C. Hypoxemia D. Oxygen toxicity 6. Emphysema results from A. A ruptured bleb B. An infected pleural effusion C. Persistent abnormal dilation of bronchi D. An excessive amount of fibrous or connective tissue in the lung 7. A reduced oxygenation of the blood is termed A. Hypoxemia B. Hypoxia C. Pneumoconiosis D. Asthma 8. Along with respiratory bronchioles, the is a thin walled balloon-liked structure that acts as the primary unit of gas exchange A. Alveolus B. Pore of Kohn C. Clara cell D. Bronchus 9. The most common feature as a result of hyperventilation is A. Acidosis B. Hypocapnia C. Hypercapnia D. Clubbing of the fingers 10. The pores of Kohn play a role in: a. Allowing plasma to leak from the capillary to the interstitium b. Connecting the right lung to the left lung c. Allowing blood flow to be evenly spread throughout the lungs d. Allowing air to pass from one alveoli to another, allowing equal distribution of air 11. What effect would acidemia at the alveolar level have on the pulmonary artery? a. Increased blood flow to that area (vasodilation) b. Decreased blood flow (vasoconstriction) to that area c. No effect of blood flow d. Vasodilation combined with decreased ventilation to the area **12. While most alveolar perfusion is under control of local humoral conditions, widespread decrease in PaO2 (alveolar O2) is likely to result in: a. Bronchoconstriction b. Pulmonary artery constriction (pulmonary hypertension) c. Increased blood flow to the lungs d. All of the above **13. A pulmonary embolus creating alveolar dead space will likely have which of the following effects? a. Shunt with very low V/Q ratio – WRONG b. Increased pulmonary compliance? c. High V/Q ratio d. Pulsus paradoxus 14. Severe bronchospasm not responsive to the normal measures (beta agonist bronchodilators) is best described as: a. Pulmonary fibrosis b. Pulsus paradoxus c. Air trapping d. Status asthmaticus 15. All of the following are findings consistent with pulmonary fibrosis EXCEPT: a. Increased lung compliance b. Chronic inflammation of the lung c. Decreased vital capacity? d. ? 16. Which of the following does NOT increase airway resistance (increase the work of breathing)? a. Bronchoconstriction b. Activation of the sympathetic nervous system effects on the airways c. … of the bronchial mucous d. Mucus collecting in the …. **17. The effect of H+ on oxygen binding to hemoglobin is termed the effect. 1. Haldane 2. Bohr 3. Bohrophil 4. Root 18. What happens to the functional residual capacity in COPD? A. It increases, resetting the TV to a higher volume B. It decreases, lowering the tidal volume level C. It is unchanged D. It increases in inspiration but decreases in expiration 19. Acidosis will the affinity of oxygen to hemoglobin and thus would be considered a shift in the oxyhemoglobin dissociation curve. A. Increase, right B. Increase, left C. Decrease, right D. Decrease, left 20. Which of the following is NOT part of Virchow’s triad in the development of thrombi and emboli? A. Hypercoagulability of blood B. Stasis of blood C. Endothelial damage D. Immune system activation 21. Which of the following statements is INCORRECT regarding tuberculosis? A. People who have been immunized with the BCG vaccine (as is common in Europe) will test positive on a tuberculin skin test (TST) B. macrophage are often unsuccessful in clearing the infection, rather they help to wall it off C. Tuberculosis typically presents as an acute onset and rapidly advancing disease process D. fatigue , weight loss, anorexia, low grade afternoon fever, and night sweats are common signs and symptoms of TB infection **22. Which of the following signs/symptoms best fits a patient presenting with chronic hypoxia as a result of pulmonary fibrosis? A. Cheyne-stokes breathing B. Hypoventilation C. Hypocapnia D. Clubbing of the fingers 23. The main neural control center coordinating ventilation during quiet breathing is the: 1. Apneustic center 2. Pneumotaxic center 3. Dorsal respiratory group - controls tidal volume 4. Ventral respiratory group - this is related to exercise 24. Vasoconstriction of a pulmonary artery serving an area of lung will have what effect? A. Decreased blood flow to that area B. Decrease ventilation to that area C. Increased airway resistance in that area D. Decrease in V/Q ratio 25. What effect would decreased compliance have on ventilation? A. It would not have any effect B. The increased stiffness would make inspiration more difficult C. The decreased compliance would make inflation easier and cause a barrel chest D. It would make breathing easier 26. What helps to keep the expansion forces of the chest wall and the contracting forces of the alveoli/lungs linked so that the lung does not collapse and the chest does not expand further? 1. The intercostal muscles 2. Surfactant 3. The carina 4. The negative pressure in the pleural cavity 27. Someone with a diminished ventilation to their alveoli as a result of respiratory disease is most likely to present with: 1. Pulmonary hypertension 2. Development of right sided heart failure over time if untreated 3. Jugular venous distention 4. All of the above 28. Atelectasis is cause by all of the following EXCEPT: 1. Compression by tumor, fluid, or air causing alveoli to collapse 2. Decreased or absent surfactant production 3. Blockage of or hypoventilated alveoli 4. All of the above can lead to atelectasis 29. Of the following types, which is responsible for secreting surfactant? 1. Type I alveolar cells 2. Type II alveolar cells 3. Clara cells 4. Goblet cells 30. Which of the following is NOT part of the conducting airways? a. Right mainstem bronchus b. Respiratory bronchioles c. Trachea d. Segmental bronchi **31. The amount of air remaining in the lungs after a complete, forceful exhalation is termed the: a. Functional residual capacity b. Residual volume c. Expiratory reserve volume d. Tidal volume 32. The amount of quiet inhalation/exhalation in a typical breath is termed the: a. Inspiratory reserve volume b. Expiratory reserve volume c. Tidal volume d. Residual volume 33. Fluid or solids replacing the air within the alveoli is best termed: a. Consolidation b. Cavitation c. Abscess d. Granuloma 34. The most common feature as a result of hyperventilation is: a. Hypocapnia b. Hypercapnia c. Clubbing of fingers 35. Your patient presents with a respiratory infection localized pain in the left side of the chest, combined with audible friction rub heard with your stethoscope that just began the past few days. Patient has decreased breath sounds and dullness to percussion to that area. A mediastinal shift was seen on the X-ray. Your most likely diagnosis is: a. Pericarditis b. A large pleural effusion c. Acute MI d. COPD 36. In response to low alveolar PO2 (pAO2): a. Bronchioles leading to that alveolus will constrict b. Vascular smooth muscle controlling flow that alveolus will constrict c. Central chemoreceptors will be activated. NOT THE ANSWER d. Both A and B (bronchoconstriction & vasoconstriction of that alveolus) 37. Surfactant is important to respiration because it: a. Vasodilator that promotes increased gas exchange in the alveolus b. An immune protein that helps to diminish inflammation at the alveolus c. An enzyme that promotes the conversion of carbon dioxide and water into bicarbonate and H+ ion d. Decreases surface tension and decreases the force favoring collapse of the alveolus 38. The structure that acts as a switching mechanism allowing food and fluid to go the esophagus rather than the trachea and is able to close and hold our breath is: a. Carina b. Hiking c. Larynx d. Nasopharynx 39. Which of the following statements regarding asthma is INCORRECT: a. Asthma is response to airway hyperresponsiveness to triggers b. Triggers can include exercise, allergens, pollution, smoke , and viral infections c. Increased allergen exposure and decreased exposure to certain infections in childhood are risk factors in asthma development d. Asthma is associated with pulsus paradoxus which is a rise in systolic pressure of >10 mmhg during inspiration. 40. Which of the following does not have cartilage as part of its structure? A. Right mainstem bronchus B. Respiratory bronchioles C. Trachea D. Segmental bronchi **41. Your patient presents with acute onset and worsening chest pain, dyspnea, mediastinal shift on x-ray and tachypnea. The most likely diagnostic fit for this patient's presentation is: A. Tuberculosis B. Tension pneumothorax C. Pneumoconiosis D. Asthma 42. Ventilations that increase in volume until a peak, followed by decreasing volumes until a period of apnea occurs, then repeats is best described as what breathing pattern? A. Cheyne-Stokes respirations B. Kussmaul breathing C. Orthopnea D. Exercise induced dyspnea 43. A 1 year old child present with tachypnea, labored breathing and wheezing following onset of what appears to be a cold/viral infection. The most likely diagnosis at this time is: A. Empyema B. Emphysema C. Pneumoconiosis D. Bronchiolitis 44. The ventilation-perfusion ratio is the same in the lung apex as the base in a standing, normal person A. True B. False 45. The experience of breathing discomfort, shortness of breath or air hunger upon laying flat in patients with heart failure is termed: a. Paroxysmal nocturnal dyspnea b. Orthopnea c. Dyspnea on exertion d. Kussmaul breathing **46. How is most of the CO2 transported in the blood? A. Dissolved in the plasma B. Bound to proteins such as hemoglobin C. As bicarbonate that can be converted back to CO2 D. The answer is different in arterial than in venous blood 47. Chronic inflammation of the bronchial wall, with destruction of the elastic and muscular components best describes A. Idiopathic pulmonary fibrosis B. Bronchiectasis C. Empyema D. Pleural effusion 48. In response to high alveolar PO2 (PaO2), which of the following will NOT occur? A. Pulmonary artery vasoconstriction B. Bronchiolar constriction to that alveolus C. Increased perfusion of that alveolus D. All of the above 49. Which of the following is TRUE regarding the pathophysiology of asthma? A. Ig A is a major factor B. There is decreased vascular permeability C. Inflammation results in hyperresponsiveness D. The inflammatory process is caused by the loss of bronchial smooth muscle spasm 50. Kussmaul breathing is best described as : A. Gasping upon waking from sleep B. Dyspnea upon lying flat in patients with heart failure C. Increasing volume of breath in consecutive breaths which peak and then diminish in volume until a period of apnea occurs, then repeat D. Slightly increased ventilatory rate with very large tidal volumes and no expiratory pause 51. The pulmonary disease most associated with permanent enlargement of acini due to loss of elastic tissue and inflammatory remodeling (without obvious addition of connective tissue) with air trapping is: (Hint: could also be a result of alpha 1-antitrypsin deficit) A. Pulmonary fibrosis B. Pleuritis (pleurisy) C. Asthma D. Emphysema 52. The vital capacity is comprised of all of the following volumes EXCEPT: a. Residual volume b. Tidal volume c. Inspiratory reserve volume d. Expiratory reserve volume 53. Which of the following is NOT part of the alveolar capillary membrane? a. Hyaline cartilage b. The alveolar wall c. The endothelial cells making up the capillary wall d. The fused basement membrane between the capillary and alveolar walls **54. Edema at the alveolar capillary membrane is a problem because a. Indicates cancerous changes b. Restricts perfusion of the alveolus c. It interferes with normal gas exchange d. It decreases airway resistance in that area 55. Which of the following is NOT associated with pulmonary edema? a. Pulmonary hypertension b. Pulmonary fibrosis c. Right-sided heart failure from tricuspid prolapse d. Acute respiratory distress syndrome **56. Which of the following statements about pneumonia is INCORRECT? a. Pneumonia is an upper respiratory tract infection b. Pneumonia is frequently preceded by a viral infection c. Pneumococcal (streptococcus pneumoniae) is the most common and lethal cause of pneumonia d. Signs and symptoms include tachypnea, tachycardia, decreased oxygenation and infiltrates on X-ray 57. Which of the following muscles is NOT associated with inspirations? a. Internal intercostals b. Diaphragm c. Sternocleidomastoid d. Scalene muscles **58. The effects of oxygen saturation on CO2 binding to hemoglobin is termed the effect A. Haldane B. Bohr C. Bohrophil D. Root 59. How is alveolar volume measured? A. Measuring tidal volume and breathing rate over the course of one minute (wrong) B. Measuring the total amount of air that can be held in the lungs C. Subtracting the residual volume from the total lung capacity D. Indirectly by measuring PaO2 or PaCO2. 60. Which of the following pulmonary conditions would not be considered as an Acute Lung Injury (ALI)/ acute respiratory distress syndrome (ARDS)? A. Sepsis leading to pulmonary dysfunction and hypoxemia B. Multiple traumas leading to pulmonary dysfunction/ hypoxemia C. Aortic stenosis leading to left sided heart failure and pulmonary dysfunction/hypoxemia D. Aspiration pneumonia leading to pulmonary dysfunction and hypoxemia [Show More]
Last updated: 1 year ago
Preview 1 out of 27 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Dec 20, 2022
Number of pages
27
Written in
Additional information
This document has been written for:
Uploaded
Dec 20, 2022
Downloads
0
Views
31