Health Care > EXAM > NUR 265 EXAM 2: latest Updated: Guaranteed A+ Score Guide (All)
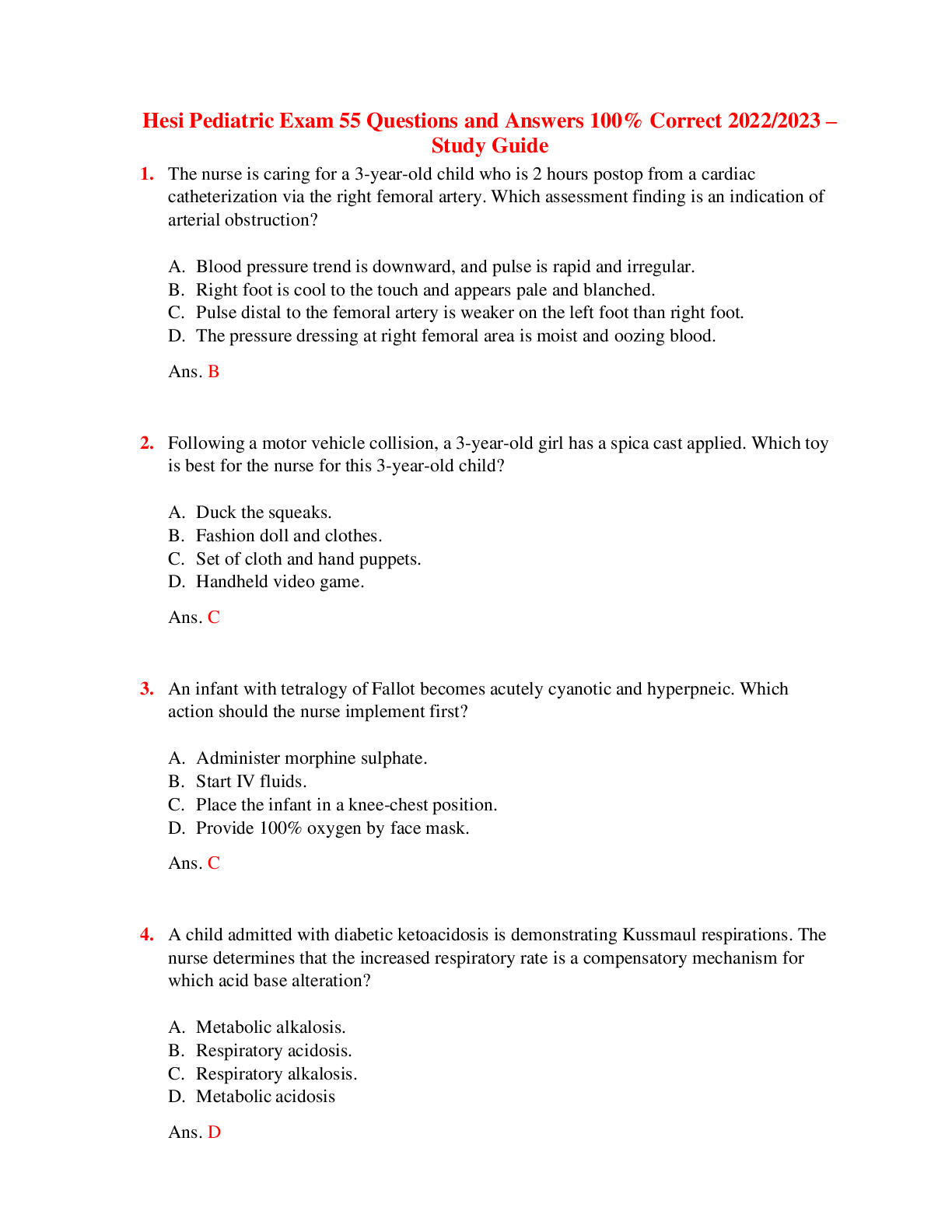
NUR 265 EXAM 2: latest Updated: Guaranteed A+ Score Guide
Document Content and Description Below
● Pulmonary embolism: clot that travels to the lungs ○ Risk factors ■ Prolonged immobility ■ Central venous catheter surgery ■ Obesity ■ Advancing age ■ Conditions that increase bl... ood clotting (DIC) ■ Distort of thromboembolism ■ Smoking ■ Pregnancy ■ Hormonal birth control (estrogen therapy) ■ Heart failure ■ Stroke ■ Cancer ■ Trauma ■ Afib ○ S/s: ■ Dyspnea - SUDDEN ONSET ■ Pleuritic chest pain (sharp, stabbing type pain on inspiration) ■ Crackles ■ Wheezes ■ Apprehension ■ Anxiety ● Give O2 ■ Restlessness ■ Impending doom ■ Cough (productive or dry) ■ Tachypnea ■ Pleural friction rub ■ S3 or s4 heart sound ■ Diaphoresis ■ Low grade fever ■ Petechiae (fat embolism , does not impede blood flow, causes actual damage to the blood vessels) over chest and a axillae ■ If really big you can see EKG changes ■ hemoptysis - bloody sputum ■ Decreased Sao2 ■ Sudden dyspnea and chest pain= immediately notify rapid response team ○ Labs: ■ Hyperventilation (caused from pain and hypoxia) = respiratory alkalosis (low paco2 <35, high PH >7.45) = blood shunting from right side to left ○ Dx: side without picking up O2 from the = respiratory acidosis (high paco2 >45, low PH <7.35)= build up of lactic acid = metabolic acidosis (low HCO3 <22, low PH <7.35) ■ D-dimer rises (positive) ■ Pulmonary angiography = gold standard ● Only if stable ● Inject dye, use imaging ■ CT ■ Chest X-ray ■ Doppler ultrasound ○ Nursing intervention: ■ Call rapid ■ O2 - use pulse ox ● Nasal cannula ● Mask ● Mechanical ventilation ■ Tele ■ IV access ■ Monitor VS. lung sounds and cardiac/ respiratory status Q1-2hrs ● Assess for and document increasing dyspnea, dysrhythmias, JVD, pedal or sacral edema, crackles, cyanosis ■ CTPA, pulmonary angiography ■ Bleeding precautions ● Monitor and record amount of bleeding ● Asses Q2 hours ■ Measure abdominal girth Q8 Hours ■ Monitor labs daily ● Monitor CBC to watch for blood loss ○ Blood loss= RBC, plasma ○ Monitor platelet count = decreased platelet count = HIIT ■ Drug therapy ■ Make sure antidote is on the floor ● Anticoagulants - keep clots from getting bigger ○ Unfractionated heparin ■ Check PTT (normal 20-30) before administering (range between 1.5-2.5 times the control) (therapeutic 46-70) (>75 = complication) ■ 5-10 days (for 24 hours) ■ Protamine sulfate = antidote ○ Then transferred to oral warfarin ■ Monitor INR (2.0-3.0) ■ Vitamin K = antidote ○ Heparin 5-10 days, most patients started on warfarin on day 1-2, both are continued together until the INR reaches 2-3, heparin will be continued for 24 hours after INR is >2 ● ○ Heparin induced thrombocytopenia ■ Body creates antibodies to the heparin = increased thrombin - prothrombin = increased clotting ■ Risk factors include: ● Duration of heparin use longer than 1 week ● Exposure to unfractionated heparin ● Post surgical prothrombin prophylaxis ● Being female ■ S/s: ● DVT ● PE ● Thrombocytopenia (hallmark sign) = platelets <150,000 ● Can through thrombus ■ Treatment: ● Argatroban and lepirudin (direct thrombin inhibitors) ● Inferior vena cava filtration - bedside procedure ○ Filter that catches things before it gets to the lungs ● Mechanical ventilation for respiratory acidosis + pao2 <60 = respiratory failure ● ● TPA ○ Antidote = clotting factors, frozen plasma, aminocaproic acid ● Mechanical ventilation ○ Mode: ■ A/C : assistive control ventilation ● Most restrictive - vent takes control of breathing completely ● Complications: ○ Hyperventilation ○ Respiratory alkalosis ( paco2 <35, ph >7.45) ● Resting mode: to try to allow patient to breath on their own, if not working then the vent takes over and breathing pattern is established ■ SIMV: synchronized intermittent mandatory ventilation ● Can be used as a main ventilator or as a weaning method ● Allows for spontaneous breathing at patients own rate ■ CPAP: continuous positive airway pressure ○ Rate ○ Fractionated inspired O2 (FiO2) ○ Tidal volume (Vt) ○ Positive end expirations pressure (PEEP) ■ Keep alveoli open longer ■ Complications: ● Pneumothorax ● Decreased pre load ○ Mechanical ventilator care ■ Lung assessment ■ Frequent VS ■ Pulmonary hygiene ■ Monitor ABG ■ ETT cuff/ pilot balloon ■ NPO ■ Skin care ■ I&O / Foley catheter ■ VTE prophylaxis ○ Pneumonia ■ Remove water from circuits ■ HOB up 30 degrees ■ Turn Q2hrs ■ Suction ■ Oral care ■ Lip moisturizer ■ Percussion ○ High pressure alarms ■ Blocked airway ■ Biting tube ■ Kinks ■ Coughing ■ Tension pneumothorax ■ Pulmonary edema ■ Psychomotor agitation ■ Pain ○ Low pressure alarms ■ Not getting enough air in or out ■ Air leak in the cuff ■ Disconnect tubing ■ Patient not breathing ● Acute respiratory distress syndrome (ARDS): stiffness= things in alveoli= refractory hypoxemia ○ Causes respiratory tissue to become inflamed which becomes stiff and then allows debri and other things into the alveoli - things that should not be in pockets ■ Gas exchange happens in the alveoli ■ Acute in onset, results from lung injury ○ Subtle changes in early stages (s/s) ■ Refractory hypoxemia : when a pt is given O2 and they remain hypoxemia - 100% O2 and still hypoxia = ARDS ■ Decreased PAO2 (80-100) ■ Hyperpnea ● Increased work effect ● Noisy respiration ■ Hypoxia ■ Cyanosis ■ Pallor ■ Intercostal and substernal retractions ■ Diaphoresis ■ Clear lung sounds early - abnormal lung sounds are not heart on auscultation because the edema occurs first in the interstitial spaces not in the airways ● Late signs = crackles ● Dysrhythmias ○ Common causes: ■ Shock ■ Trauma ■ Pancreatitis ■ Fat/ amniotic fluid emboli ■ Sepsis ■ Aspiration - especially stomach contents ■ Pneumonia ■ Inhaling toxic fumes ■ Drug ingestion (heroine, opioids, aspirin) ■ Hemolytic disorders ■ Cardiopulmonary bypass ■ Multiple blood transfusions ● Usually within 6 hours of transfusion ■ Water aspiration from submersion ● Especially fresh water ■ COVID ■ Nervous system injury ■ Fat embolism ■ Amniotic fluid emboli ○ Requires immediate intervention ○ Difficult to diagnose ■ ABG ● Low PAO2 ● Sputum cultures ● Chest X-ray ○ Will show ground glass appearance “whited out” ● Hemodynamic monitoring is ****** waiting for an answer! ○ PAP and PCWP ○ May lead to complications ■ SIRS ■ Multi organ failure ■ Respiratory failure - respiratory acidosis (ph 7.28, Co2 55) and a PAO2 of <60, respiratory rate goes up, oxygen saturation goes down [Show More]
Last updated: 1 year ago
Preview 1 out of 26 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 02, 2023
Number of pages
26
Written in
Additional information
This document has been written for:
Uploaded
Feb 02, 2023
Downloads
0
Views
38