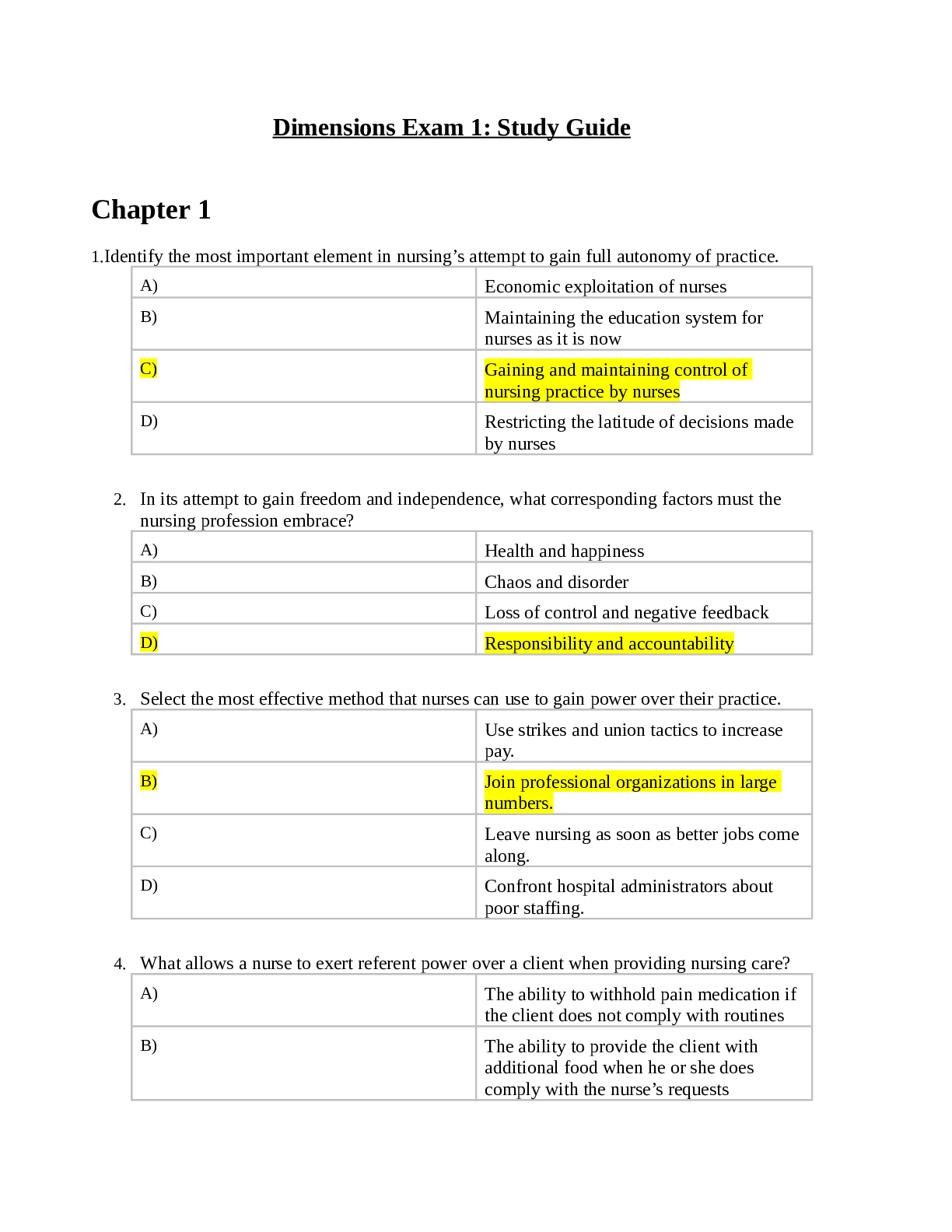
NURSING. > EXAM > Albany State University Nursing Division NURS 2115 Spring 2017 Metabolic Disorder Study Guide,100% C (All)
Albany State University Nursing Division NURS 2115 Spring 2017 Metabolic Disorder Study Guide,100% CORRECT
Document Content and Description Below
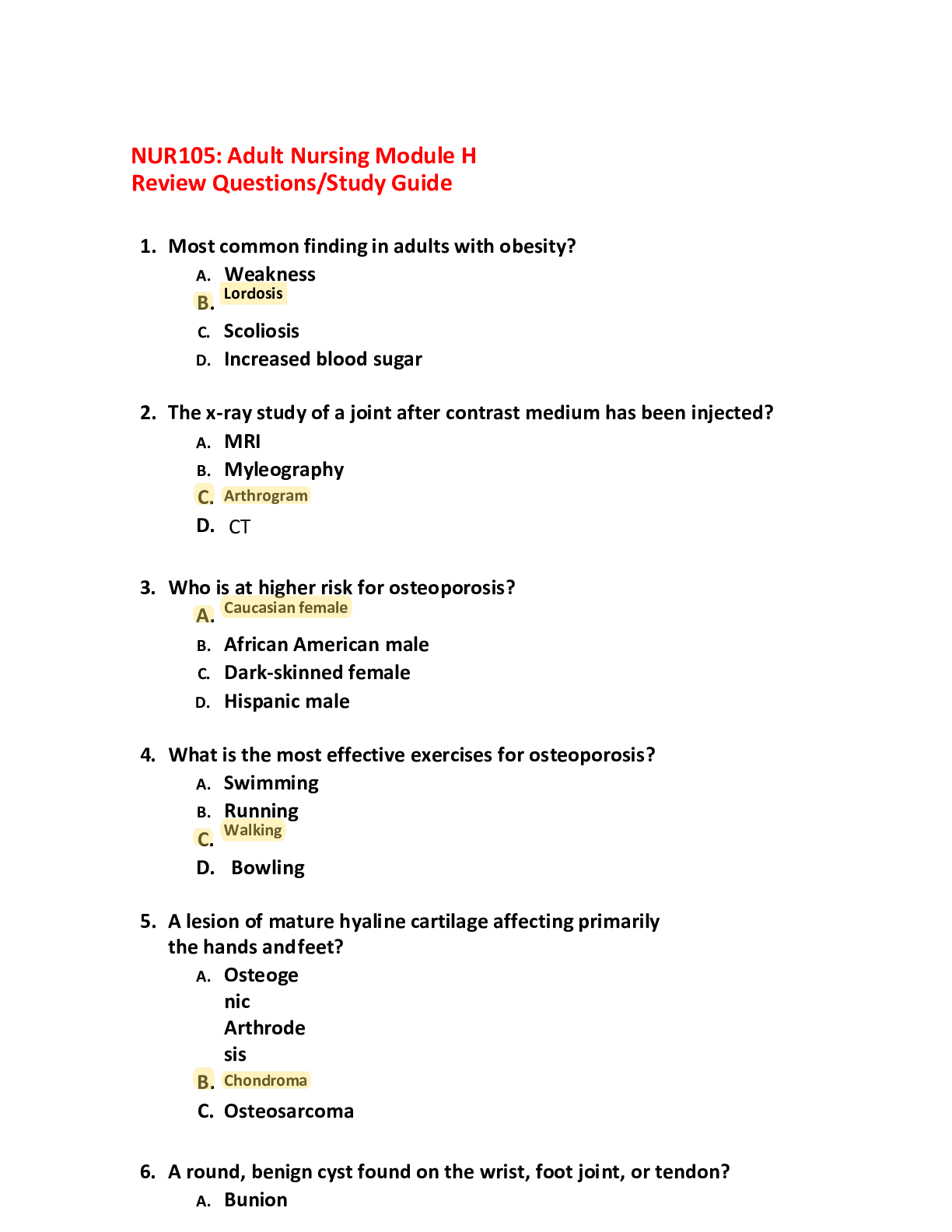
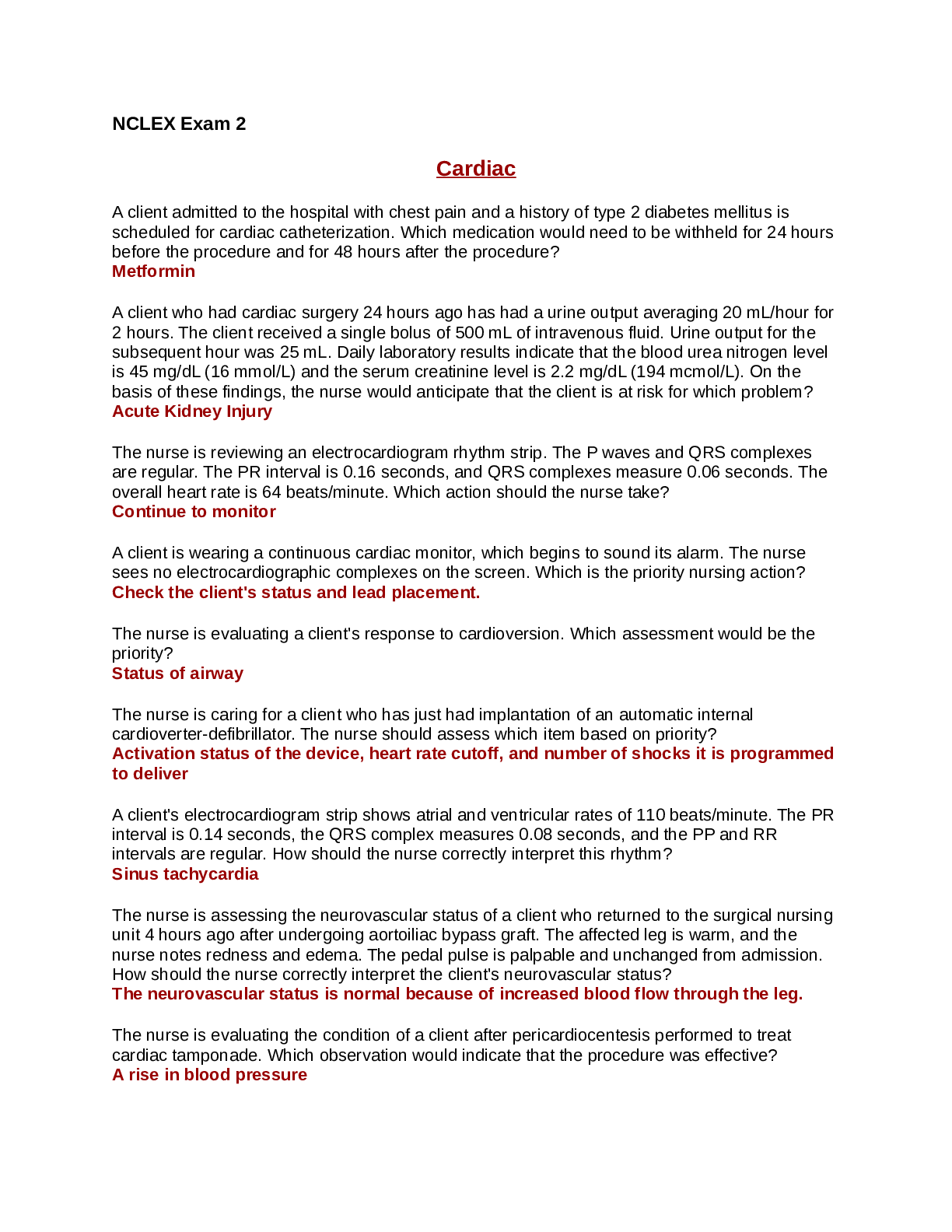
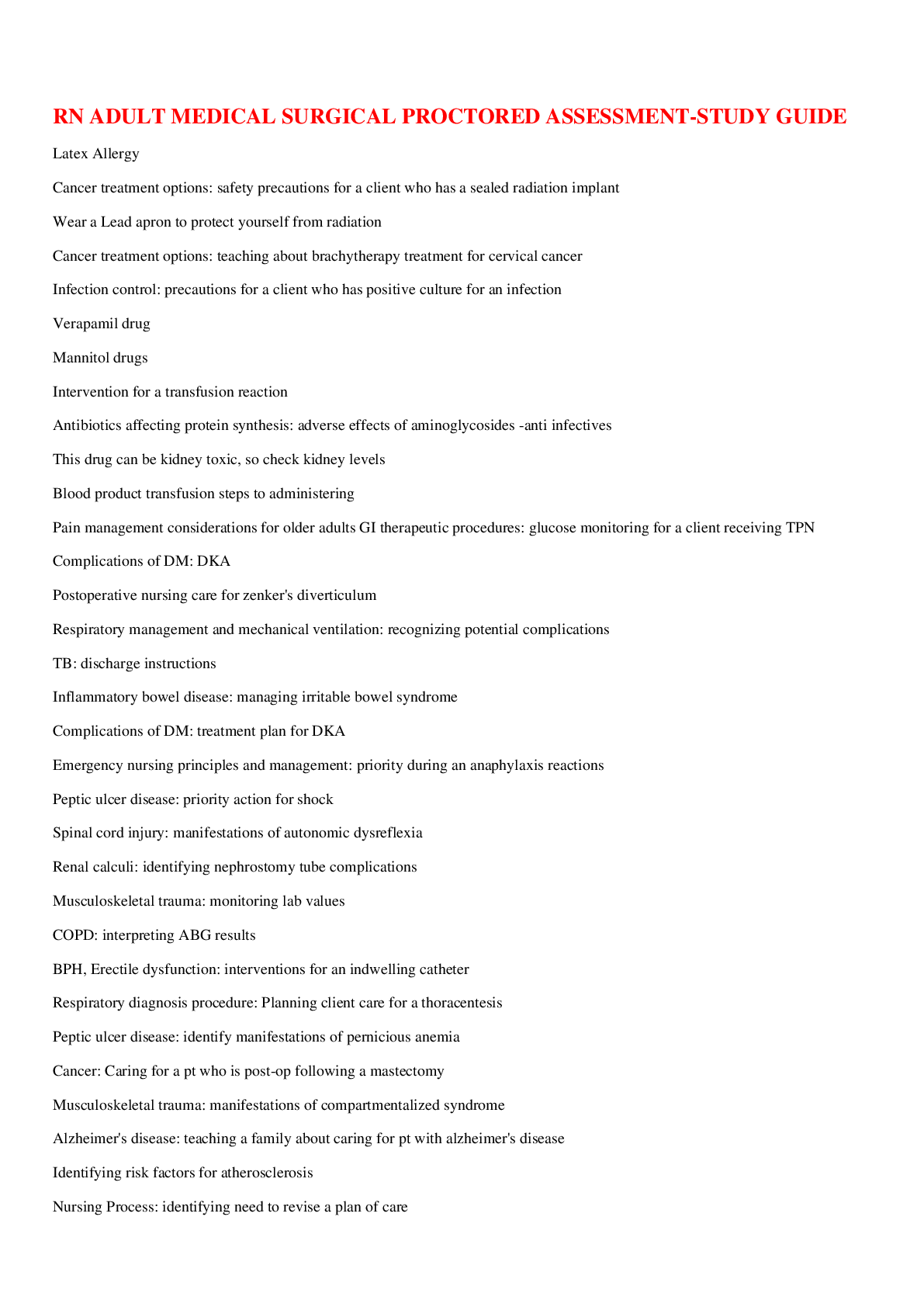
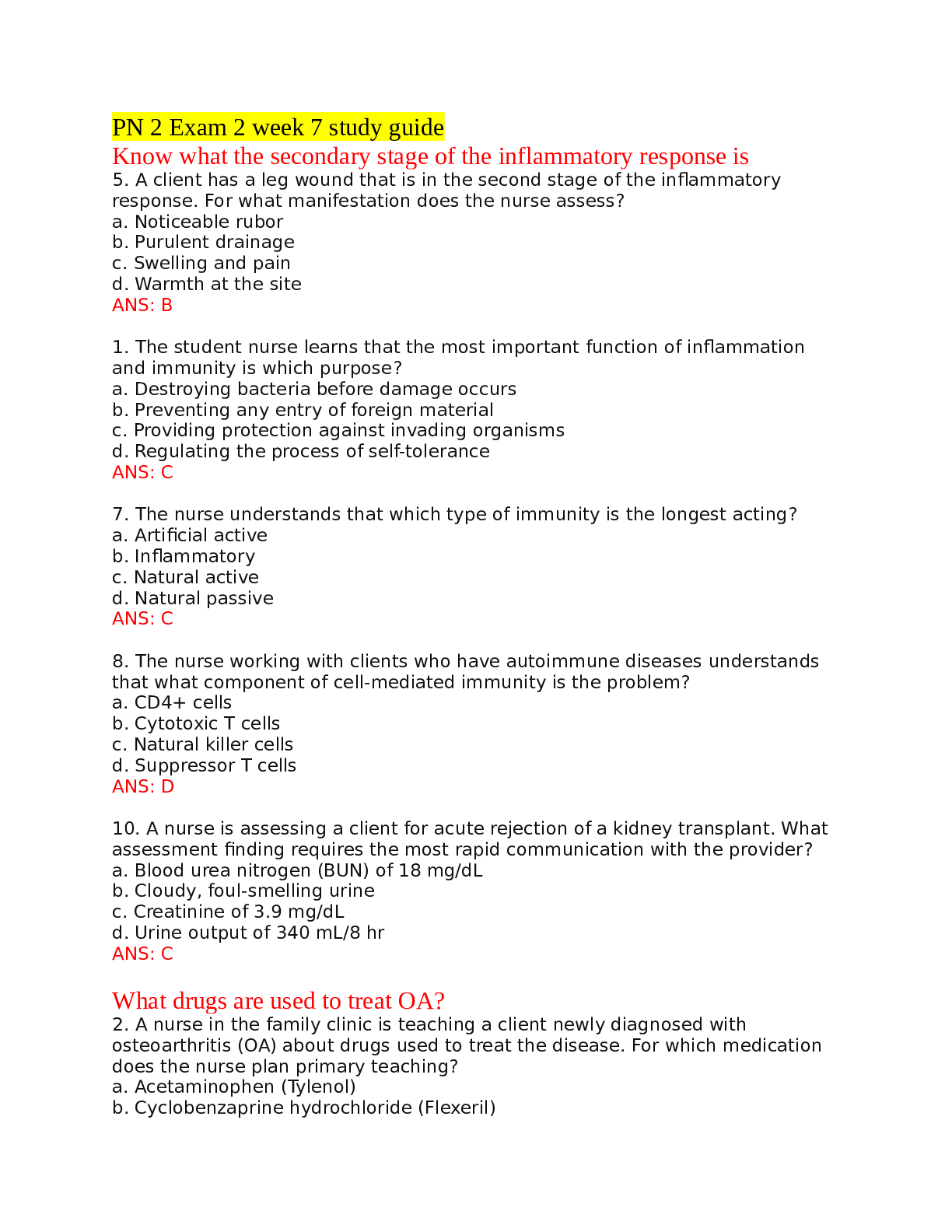
Albany State University Nursing Division NURS 2115 Spring 2017 Metabolic Disorder Study Guide The guide is meant to help focus on study topics. Liver disorders will be half of the metabolic items o... n the test. The emphasis will be on nursing care and decision- making. 1. Know the difference between legal and ethical action in nursing. 2. Examine cultural considerations when treating client conditions. 3. Understand the difference between active and passive immunity. Give an example of passive immunity in adults. ❖ Active Immunity ➢ immunologic defenses developed by the persons own body. ➢ Last many years or even a lifetime ➢ Creates memory B cells make antibodies when exposed to an antigen you were previously exposed to ➢ Examples ▪ Get sick and body makes antibodies ▪ Immunizations and vaccinations ❖ Passive Immunity ➢ Immunity transmitted from a source outside the body that has developed immunity through previous disease or immunization. ➢ Temporary immunization ➢ Examples ▪ Mother to fetus through placenta ▪ Mother to newborn through breastmilk ▪ IV immunoglobulins (Passive Immunoglobulins) this way the body doesn’t have to create the immunoglobulins ▪ Blood transfusion from someone who was previously infected or vaccinated 4. Discuss the signs and symptoms of liver disorders. ❖ Integumentary changes ➢ Jaundice ▪ When the bilirubin concentration in the blood is abnormally elevated , all of the bodies tissues, including the sclera and skin, become tinged yellow or greenish yellow. (pg 1342) ▪ This becomes clinically evident when the bilirubin levels exceed 2.5mg/dL ▪ Increased levels may result from impairment of hepatic uptake, conjugation of bilirubin, or excretion of bilirubin into the biliary system. ▪ Different types of jaundice • Hemolytic jaundice (Pg. 1343) ◆ Is the result of increased destruction of red blood cells which rapidly floods the plasma with bilirubin to the extent that a normally working liver cannot excrete the bilirubin as quickly as it is formed. ◆ Patients with this kind of jaundice, unless extreme, do not experience symptoms or complications other than jaundice but prolonged jaundice will predispose the formation of pigment stones in the gallbladder • Hepatocellular Jaundice (pg. 1344) ◆ Caused by the inability of the damaged liver cells to clear normal amounts of bilirubin from the blood. ◆ Liver cell damage can be caused by hepatitis, other viruses (Epstein Barr), chemical toxins, or alcohol. ◆ These patients may be mildly or severely ill with lack of appetite, nausea, malaise, fatigue, weakness, and possible weight loss. • Obstructive Jaundice (Pg. 1344) ◆ Cause by extrahepatic or intrahepatic obstruction ➢ Extrahepatic obstruction is caused by occlusion of the bile duct from a gallstone, an inflammatory process, a tumor or pressure from enlarged organ. ➢ Intrahepatic obstruction is caused by stasis and inspissation (Thickening) of the bile with in the canaliculi. ◆ Both cause bile to be unable to flow normally into the intestine causing it to back up in the liver where it is reabsorbed and carried out into the entire body, staining the skin, mucosa, and sclera. It is also excreted through urination causing urine to become deep orange and foamy. Stools will also become clayed colored because of lack of bile in intestine. Pts skin will also itch intensely. • Hereditary Hyperbilirubinemia (Pg.1344) ◆ Results from inherited disorders such as Gilbert’s syndrome, Dublin-Johnson syndrome, and Rotor’s syndrome ❖ Portal HTN (Pg., 1344) ➢ Results from obstruction of blood flow into and through a damaged liver. ➢ Commonly associated w/hepatic cirrhosis. ❖ Ascites (Pg. 1344 – 1349) ➢ Caused ▪ by failure if the liver to metabolize aldosterone increases sodium and water retention by the kidneys. Na and h2o retention, increased intravascular fluid volume, increased lymphatic flow, and decreased albumin synthesis by the damaged liver contributes to the fluid shift into the peritoneal space. Large amounts of this albumin rich fluid, 20L or more, accumulates in the peritoneal cavity as ascites. ➢ Manifestations ▪ Increased abdominal girth, rapid weight gain, SOB, Uncomfortable from enlarged abdomen, striae and distended veins over abdominal wall. Umbilical hernias occur freq. Also will present with some fluid and electrolyte imbalances. ➢ Assessment ▪ Palpation, Percussion and fluid wave test. ➢ Management ▪ Nutritional • Goal is a negative sodium balance to reduce fluid retention. • Table salt, salty foods, salted butter, canned foods, and frozen foods not specifically prepared for low sodium diet should be avoided. ▪ Pharmacological • Diuretics ➢ Spironolactone is first line therapy. When used with other diuretics it helps prevent potassium loss. ➢ Furosemide may be added but use with caution b/c long term use can lead to hyponatremia. ➢ Daily weight loss should not exceed 1-2kg (2.2-4.4lb) ◆ Complications ➢ Avoid use of ammonium chloride and acetazolamide because these drugs can precipitate hepatic coma. ➢ Diuretic complications are fluid and electrolyte imbalances and encephalopathy cause by dehydration • Bed Rest ◆ Patient needs to be in an upright posture to activate renin- angiotensin- aldosterone system. • Paracentesis ◆ Is the removal of fluid from the peritoneal cavity through a puncture or small surgical incision through the abdominal wall under sterile conditions . ◆ Large volume (5-6L) paracentesis has been shown a safe method for treating patients with severe ascites. ◆ Only provides temporary removal of fluid. ◆ Nursing Care for patient undergoing paracentesis ➢ Pre-procedure ▪ Check signed consent form, educate, instruct pt to void, gather materials, place patient in upright position on edge of bed or in a chair with feet supported by a stool. Fowlers position for pt confined to bed. Place a sphygmomanometer cuff around pts arm ➢ Procedure ▪ Help pt maintain position, measure and record BP at frequent intervals, monitor pt for signs of vascular collapse (pallor, increased pulse, decreased BP) ➢ Post Procedure ▪ Place pt in comfortable position, measure, describe and record fluid collected, send sample to lab, monitor VS q15 mins for 1hr, then q30 mins for 2 hours, then q1hr for 2hrs, and then q4hrs. Measure pts temp, assess for fluid volume problems, check puncture site for leakage during VS. educate pt on importance of watching for bleeding and to avoid straining and heavy lifting, change positions slowly, and monitor for fever. ❖ Esophageal Varices (Pg. 1349 – 1354) ➢ Pathophysiology • Esophageal varices are dilated, tortuous veins that are usually found in the submucosa of the lower esophagus but may develop higher in the esophagus and into the stomach. They are almost always caused by portal HTN, which results from obstruction of the portal venous circulation within a damaged liver. • These are present in 30% of pts with compensated cirrhosis and 60% of pts with decompensated cirrhosis. • Overall mortality rate associated with bleeding varices is 10 – 40%. • Factors that can contribute to bleeding ◆ Muscular exertion from heavy lifting, straining at stool, sneezing, coughing, or vomiting, esophagitis, irritation of vessels by poorly chewed foods or irritating fluids (Alcohol), and reflux of stomach contents. ➢ Clinical Manifestations • Hematemesis, melena (Black tarry feces), or general deterioration of mental and physical status (pts usually have Hx of alcohol abuse). • Watch for S&S of shock induced by bleeding also (cool clammy skin, hypotension, tachycardia) ➢ Assessment and Dx findings ▪ Endoscopy • B/c varices are present in 50% of pts with cirrhosis it is recommended that pts dx with cirrhosis undergo screening endoscopies. If no varices are detected a follow up will be in 2-3 years, if small varices are detected the test should be repeated 1-2yrs. • Immediate endoscopy is indicated to identify the cause and site of bleeding. Appx 40% of pts are actually bleeding from another source. • Care during and after examination: ◆ During procedure the nurse should support and carefully monitor to detect early signs of cardiac dysrhythmias, perforation, and hemorrhage. ◆ After examination hold fluids until gag reflex is present, lozenges and gargles may be used to comfort sore throat. ➢ If pt is actively bleeding oral intake will not be permitted b/c further test will be needed. ▪ Portal HTN measurements • Indirect measurement of hepatic vein pressure is most common. This is done by inserting a catheter w/balloon into the antecubital or femoral vein to the hepatic vein. Once in position the balloon is filled with fluid and a wedge pressure is obtained. • Direct measurement includes a Laparotomy that consist of a needle being introduced into the spleen taking a manometer reading, greater than 20 ml is abnormal. ➢ Medical Management • Pharmacologic, endoscopic, and surgical are used to treat bleeding esophageal varices, but none are ideal and most have considerable risk. • Nonsurgical tx of bleeding varices is preferred b/c of the high mortality rate of emergency surgery and b/c of the poor physical condition typical of a pt with severe liver disease. ▪ Volume Resuscitation • b/c pts w/bleeding varices have intravascular volume depletion and are subject to electrolyte imbalances, IV fluids, electrolytes, and volume expanders are provided to restore volume. • Blood transfusion may also be required. • * Caution has to be taken with volume resuscitation so that over hydration does not occur b/c this will raise the portal pressure and increase the bleeding you are trying to control. • Indwelling catheter is also in place during this to monitor urine output. ▪ Pharmacological Tx ◆ * in suspected variceal bleeding vasoactive drugs need to be given ASAP and BEFORE endoscopy. • Octreotide (Sandostatin) ◆ Preferred tx regimen for immediate variceal bleeding b/c it lacks the vasoconstrictive effects of vasopressin. ◆ These meds cause selective splanchnic vasoconstriction by inhibiting glucagon release and are used mainly in the management of active hemorrhage. • Vasopressin ◆ Only used in urgent situations. ◆ Contraindicated for pts with CAD b/c of coronary vasoconstriction effects but can be given with nitroglycerine to counteract those effects. ◆ Has to be administered with close monitoring b/c of side effects. • Beta-Blockers (propranolol & nadolol) ◆ Used as a prophylactic to decrease portal pressure in pts to prevent a first bleeding episode or to prevent recurrent bleeding episodes ◆ They should not be used in acute variceal hemorrhages. • Isosorbide ◆ Used in conjunction with LOLs b/c of their venodilation effect and decreases cardiac output that lowers portal pressure. ▪ Balloon Tamponade (Pg. 1351) • Complications ◆ Asphyxiation by displacement of the tube, inflation of tube in oropharynx, and rupture of the balloon. ➢ Nurse Intervention ▪ Inflate balloon before insertion to ensure balloon can handle the required pressure without rupture ▪ **Keep scissors at bedside to cut tube in an emergency ◆ Aspiration, especially in stuporous or comatose pts. ➢ Intubation may be required to ensure the pts airway is protected ◆ Ulceration and necrosis of the nose, the mucosa of the stomach, or the esophagus may occur if the tube is left in place to long, inflated to long, or inflated at too high of a pressure ➢ Nursing intervention ▪ Frequent mouth and nasal care, oral suctioning. ▪ Endoscopic Variceal Ligation (EVL) (Banding) (pg 1352) • Is a method of placing a band around the varices to cause necrosis, ulceration, and eventually sloughing of the variceal. • EVL is the Tx of choice to treat varices b/c it significantly reduces re- bleeding rates, mortality, procedure related complications, and reduces the number of sessions needed to eradicate varices. • Complications ◆ Superficial ulceration and dysphagia, transient chest discomfort, and rarely esophageal strictures. • Recommended for pts who have experienced bleeding while receiving beta-blocker therapy or those who cannot tolerate beta therapy ▪ Endoscopic Sclerotherapy (pg 1352) • Is a method of injecting a sclerosing agent into or adjacent to the bleeding varices to promote thrombosis and eventual sclerosis. • Not recommended for prevention of first or subsequent variceal bleeding episodes. • After TX ◆ Observe for bleeding, perforation of esophagus, aspiration pneumonia, and esophageal stricture. ◆ Antacids and h2 antagonist may be given to counteract the effects of sclerosing agent on esophagus and for reflux associated with procedure ▪ Trans-jugular Intrahepatic Portosystemic Shunt (TIPS) (Pg. 1352) • Used to divert blood flow and reduce portal HTN • Is indicated for tx of an acute episode of uncontrolled variceal bleeding refractory to pharm or endoscopic therapy. • In 10-20% of pts whom urgent band ligation or sclerotherapy and medications did not stop bleeding, TIPS procedure can effectively control acute variceal hemorrhage. • Complications ◆ Bleeding, sepsis, HF, organ perforation, shunt thrombosis, and progressive liver failure. ❖ Hepatic Encephalopathy and Coma (Pg. 1354) ➢ Pathophysiology ▪ Hepatic insufficiency may result in encephalopathy b/c of the inability of the liver to detoxify toxic by-products of metabolism ▪ Portosystemic shunting, in which collateral vessels develop as a result of portal HTN, allows elements of the portal blood (which contains toxins b/c the liver didn’t filter the blood yet) to enter the systemic circulation. ▪ Ammonia is one of the toxic by-products of metabolism that helps lead to encephalopathy. • Largest source of ammonia is from the digestion of dietary and blood proteins in the GI tract. Ammonia increases as a result from GI bleeding (bleeding esophageal varices, chronic GI bleeding), High protein diet, bacterial infection (which would convert more urea to ammonia) or uremia (high levels of waste). • Ways to decrease serum ammonia ◆ Elimination of protein in the diet so less protein is metabolized, admin of antibiotic so bacteria in the GI is reduce. ▪ Other factors that lead to encephalopathy • Excessive diuresis, dehydration, infections, surgery, fever and some medications. ➢ Clinical Manifestations ▪ Stage 1 • Normal LOC w/periods of lethargy and euphoria. Sleep pattern reversed • Asterixis (involuntary flapping of hand), impaired writing and ability to draw line figures. • Normal EEG. ▪ Stage 2 • Increased drowsiness, disorientation, inappropriate behavior (Mood swings and agitation) • Asterixis, fetor hepaticus (musty, sweetish odor on breath), • Abnormal EEG with generalized slowing ▪ Stage 3 • Stuporous (difficult to arouse), sleeps most of time, marked confusion, incoherent speech • Asterixis, increased deep tendon reflexes, rigidity to extremities • EEG marked abnormally ▪ Stage 4 • Comatose, may not respond to painful stimuli • Absence of asterixis, absent deep tendon reflexes, flaccidity in extremities, • EEG marked abnormally ➢ Medical Management ▪ Focuses on eliminating the precipitating cause such as ammonia lowering therapy, minimizing potential medical complications of cirrhosis and depressed consciousness, and reversing underlying liver disease. ▪ Correction of reason for deterioration such as bleeding, electrolyte abnormalities, sedation, or azotemia (high levels of nitrogen containing compounds in the blood) is essential. ➢ Pharmacological Management ▪ Lactulose • Used to reduce serum ammonia levels by trapping and expelling ammonia in feces. • Two or three soft stools per day indicates that lactulose is preforming as intended ◆ Watery diarrhea stools indicate medication overdose! • Side Effects include intestinal bloating and cramps. • Other laxatives are not prescribed during lactulose therapy. • May be admin via NG tube or enema for comatose pts or for those who oral admin is contraindicated • Pt teaching ◆ If sweet taste is dislike pt can dilute with fruit juice. ▪ IV glucose is given to minimize protein breakdown ▪ Vitamins to correct deficiencies and electrolyte imbalances ▪ Antibiotic to decrease ammonia forming bacteria in the colon. • No benefit has been shown for long term antibiotic tx ▪ Discontinue sedatives, tranquilizers, and analgesic medications ➢ Nutritional Management ▪ Low protein diet w/small frequent meals and snacks, substitute veggie proteins for animal proteins. ➢ Nursing Management ▪ Assess neuro freq, keep daily record of handwriting and arithmetic performance, I&O and body weight recorded daily, assess peritoneum and lungs for infection each day, monitor ammonia levels. ▪ Maintain safe environment, encourage deep breathing and position changes, communicate with family about pt status, and explain procedures and txs that are a part of care. 5. Describe physical assessments of liver function. ❖ Inspection ➢ Liver is normally not visualized so if you can see a liver in the upper right quadrant there should be suspicion of disease ❖ Palpation ➢ Palpated in the upper right quadrant to assess size and to detect any tenderness. ➢ This is done by placing one hand under the lower right rib cage and pressing downward during inspiration with the other had at the lower right rib cage. (Bimanual Technique) ➢ Palpable liver presents as a firm sharp ridge with a smooth surface. ▪ If palpable nurse notes and records size, consistency, any tenderness and whether its outline is regular or irregular. ❖ Percussion ➢ Used to determine size and tenderness ➢ To note size, the examiner percusses the upper and lower boarders of the liver and marks them so they can be measured in cm. (Normal Size 6-12 cm) ➢ If tenderness is suspected, tapping the lower right thorax briskly may elicit tenderness. For comparison preform the same on the opposite side. 6. Know lab tests used to examine liver function. What are the normal values for each test? Apply lab results to patient situations. ❖ Alanine Aminotransferase (ALT) ➢ Normal 5-35 units ➢ Used to identify liver disease, especially Cirrhosis and Hepatitis, caused by alcohol, drugs or viruses ➢ Used to keep track of medications effects on the liver. ➢ Also used to identify whether jaundice is cause by blood disorder or from liver disease ❖ Aspartate Aminotransferase (AST) ➢ Normal 10-40 units\ ➢ Used for the same as ALT ❖ Gamma Glutamyl Transferase (GGT) ➢ Normal 10-48 IU/L ➢ Used to detect some liver disease and bile duct obstructions ➢ Used also to screen for chronic alcohol abuse, Elevated in ETOH (Alcohol) abuse. ❖ Alkaline Phosphate (ALP) ➢ Normal 20-140 IU/L ➢ Sensitive to biliary obstruction ❖ Ammonia ➢ Normal 10-65 umg/dl ➢ Elevated in severe liver disease ➢ Used to help diagnose hepatic encephalopathy ❖ Albumin ➢ Normal 4-5.5 g/dl ➢ Affected in cirrhosis, chronic hepatitis, edema and ascites. ❖ Total Bilirubin ➢ Normal < 0.9 mg/dl ➢ Abnormal in liver and biliary tract disease ❖ Prothrombin Time (PT) ➢ Normal 12-16 seconds ➢ Prolonged in liver disease and will no return to normal w/K+ in severe liver damage. 7. Describe procedures used to diagnose and treat liver disorders, and related nursing actions. Discuss nursing actions and interventions related to procedures. ❖ Liver Biopsy ➢ The removal of a small amount of liver tissue, usually through needle aspiration, to examine liver cells. ➢ Main complication is peritonitis ➢ Pre-Procedure ▪ Check coagulation studies, if abnormal you must treat before the procedure because pts are at risk for bleeding and make sure compatible donor blood is available. ▪ Confirm signed consent/ allergies and identify pt using 2 identifiers, NPO 6-8hrs ▪ VS immediately before procedure ▪ Describe sensations expected, steps, after effect sensations in advance ➢ During Procedure ▪ Expose the right side of the pts upper abdomen ▪ Instruct the pt to inhale and exhale deeply several times, then to exhale and hold breath at the end of expiration. The dr. introduces the needle into the liver then aspirates and withdrawls. ▪ Instruct pt to resume breathing ➢ Post-procedure ▪ Immediately after assist pt to turn to right side, place a pillow under the coastal margin and caution pt to remain in this position, recumbent and immobile for several hours and to avoid coughing or straining ▪ Measure VS q10-15mins for the first hour, then q30mins for the next 1-2 hrs or until the pt stabilizes ▪ If pt is discharged teach to avoid heavy lifting and strenuous activity for 1 week. 8. Discuss treatments for liver disorders, including medications. Know indications, actions, side effects, and nursing considerations for medications. ❖ Cirrhosis (Pg, 1366) ➢ Pathophysiology ▪ Alcoholic Cirrhosis (Laennc’s) • The most common type, cause by chronic alcoholism • Characterized by episodes of necrosis involving the liver cells. The destroyed liver cells are gradually replaced by scar tissue and eventually the amount of scar tissue exceeds that of functioning tissue. • Women are at greater risk for development of alcohol induced liver disease ▪ Postnecrotic Cirrhosis • Characterized by broad bands of scar tissue which is a late result of a previous bout of acute viral hepatitis ▪ Biliary Cirrhosis • In which scarring occurs in the liver around the bile ducts. • Usually the result from chronic biliary obstruction and infection (cholangitis) • Much less common ➢ Clinical Manifestations ▪ Two Categories by severity (Compensated and Decompensated • Compensated cirrhosis is less severe and has vague symptoms that are usually discovered secondary to a routine physical examination. • These symptoms include: ◆ Intermittent mild fever, vascular spiders, palmar erythema (reddened palms), unexplained epistaxis, ankle edema, vague morning indigestion, flatulent dyspepsia (swelled stomach, felling full w/o eating), abdominal pain, firm enlarged liver, and splenomegaly. • Decompensated Cirrhosis results from failure of the liver to synthesize proteins, clotting factors, and other substances and manifestations of portal HTN. • Symptoms of Decompensated: ◆ Ascites, jaundice, weakness, muscle wasting, weight loss, continuous mild fever, clubbing of fingers, purpura (rash of purple spots), spontaneous bruising, epistaxis, hypotension, sparse body hair, white nails, gonadal atrophy. ▪ Other manifestations • Liver enlargement ◆ Early stages the liver is large, firm and sharp on palpation, abdominal pain because of the liver being stretched. ◆ Later stages the liver decreases in size because of fibrous tissue and if palpable will be nodular • Portal Obstruction and Ascites ◆ Late manifestations cause by failure of liver function and by obstruction of portal circulation • Infection and Peritonitis ◆ May develop in pts with cirrhosis and ascites in the absence of intra-abdominal source of infection or abscess ◆ Translocation of intestinal flora is believed to be the cause • Gastrointestinal Varices ◆ Caused by shunting of blood from the portal vessels into blood vessels with lower pressures which causes these vessels to distend and form varices or hemorrhoids depending on location. • Edema ◆ Liver failure causes a reduced plasma albumin concentration which predisposes the pt to edema mainly in the lower extremities, upper extremities and the presacral area. • Vitamin deficiency and Anemia ◆ B/c the damaged liver is no longer able to create, use or store the vitamins. ◆ Chronic gastritis and impaired GI function, together with inadequate diet and liver function, account for the anemia associated with cirrhosis • Mental Deterioration ➢ Assessment and Dx ▪ Diagnosis is confirmed by liver biopsy ➢ Medical Management ▪ Antacids or H2 antagonist are prescribed to decrease gastric distress and minimize possibility of bleeding ▪ Vitamins and nutritional supplements promote healing of damaged liver cells and improve pts general nutrition status ▪ Potassium-sparing diuretics such as spironolactone or triamterene may be indicated to decrease ascites. These diuretics are preferred b/c they minimize the fluid and electrolyte changes seen with others ▪ Thistle is used for its healing and regenerative properties ▪ SAM-e improves outcomes by improving liver function and enhancing antioxidant function. ➢ Nursing Management ▪ Promote Rest • Measure I&O and weight daily, position the client for maximal respiratory efficiency, oxygen therapy to oxygenate damaged cells and prevent further cell destruction ▪ Improving Nutritional Status • Pt w/cirrhosis w/o ascites, edema, or signs of hepatic coma should receive nutritious, high protein diet with supplemental vitamins of b complex and A, C, and K, • If ascites is present small frequent meals are better tolerated ➢ Providing Skin Care ▪ Change positions frequently and apply lotion to sooth irritated skin to help minimize scratching by the pt ➢ Reduce Risk of Injury ▪ Protect from falls, side rails should be up and padded just in case the pt becomes agitated, orientate pt so they don’t become agitated, tell pt to ask for help when getting out of bed, evaluate injuries to make sure there is no internal bleeding, use electric razor and soft bristled tooth brush because of risk for bleeding 9. Understand nursing considerations for client safety using devices and when participating in diagnostic procedures. 10. Differentiate Hepatitis A, B, C, D, E, and G including time of onset, symptoms, treatments, sequelae, and measures to prevent. Focus on hepatitis A, B, and C. ❖ Hepatitis A (HAV) (pg1358) ➢ Overveiw ▪ Caused by a RNA virus of the enterovirus family ▪ Transmitted via the fecal-oral route, by ingesting food or liquids infected w/the virus • Poor hygiene, hand-to-mouth contact, infected food handler, consuming water or shellfish from sewage contaminated waters, sexual contact (mainly oral-anal, anal intercourse) are other ways it can be spread. • Rarely spread by blood transfusions ▪ Incubation period of 2-6 weeks (Avg. 4 weeks or 30 days), can be prolonged and last 4-8 weeks. Last longer and is more severe in those over 40 years ▪ No carrier state exists and no chronic hepatitis is associated with HAV ▪ HAV confers immunity against itself, but the person can still contract other forms of hepatitis. ➢ Clinical Manifestations ▪ Pts can be anicteric (w/o jaundice) and symptomless, but when they do appear they resemble a mild flu w/low-grade fever, anorexia (early and sometimes severe symptom). As the virus progresses jaundice and dark urine appear, indigestion, vague epigastric distress, nausea, heartburn, and flatulence can occur. ▪ Some pts have a strong aversion to the taste of cigarettes or the presence of cigarette smoke. ▪ Symptoms tend to clear as so as the jaundice reaches it peak at about 10 days ➢ Assessment and Dx ▪ Hep A antigen may be found in stool 7-10 days before illness and for 2-3 weeks after symptoms appear ➢ Prevention ▪ Good hygiene, safe water supplies, proper sewage disposal, protected sex, safe preparation and dispensing of food, ect ▪ HAV vaccines • Havrix and Vaqta are safe and 95-100% effective after 2-3 doses ◆ Two dose vaccine for adults 18 and older, with the second dose given 6-12 months after first. Protection develops several weeks after the first dose ◆ Children and adolescents 2-18 yrs receive 3 doses, second dose is given 1 month after first and the 3rd dose is given 6-12 months later. • Recommended for: ◆ People who travel to unsanitary places, homosexual men, IV or injection drug users, staff of day care centers, and health care personnel. • IM Globulin if given w/in 2 weeks of exposer can prevent HAV in a person who had previously not been vaccinated. This provides 6-8 weeks of passive immunity. The HAV exposure will provide immunity to subsequent episodes of the virus • Immune Globulin is also recommended for house hold members and sexual contacts of people with HAV. • Caution is required when anyone who has previously had angioedema, hives, or other reactions is treated w/any human immune globulin. Epinephrine should be available in case of allergic reaction. ➢ Medical Management ▪ Bed rest, nutritious diet, if pt is experiencing anorexia give small frequent feedings, supplement IV fluids and glucose if necessary. Ambulate but not until fatigued ➢ Nursing Management ▪ Educate family and patient the importance of avoiding alcohol, sanitation, follow-up blood work, and to seek additional health care of symptoms worsen ❖ Hepatitis B (HBV) (Pg. 1360) ➢ Overview ▪ DNA virus, incubation avg. 75 days ▪ Transmitted primarily through blood. ▪ Can be found in blood, saliva, semen, and vaginal secretions and can be transmitted through mucous membranes and breaks in the skin. ▪ Can also be transmitted from mother to baby during birth and the close contact afterwards • Not passed to child through the umbilical vein ▪ Most people recover spontaneously on 6 months and develop antibodies. ▪ 10% infected progress to carrier state or develop chronic hepatitis which remains a major worldwide cause of cirrhosis. ➢ Risk Factors (chart 49-9 pg 1361) ▪ Freq exposure to blood & body fluids, health care workers, hemodialysis staff, male homosexual and bisexual activity, IV/injection drug use, close contact w/carrier, Mother-child transmission, travel to or reside in area w/uncertain sanitary conditions, recent hx of STI, receive blood or blood products, tattooing. ➢ Clinical Manifestations ▪ Closely resembles HAV but the incubation period is much longer (1-6 months) ▪ Pts may have arthralgia (Joint pain) and rashes, loss of appetite, dyspepsia, abdominal pain, generalized aching, malaise, and weakness. If jaundice occurs light stools and dark urine accompanies it ▪ Liver may be enlarged 12-14cm vertically. ➢ Assessment and Dx ➢ Prevention ▪ Preventing Transmission • Screening of blood donors for HBV • Use of disposable syringes, needles, and lancets and use of needleless Iv administration • Clinical and hemodialysis units disinfected daily • Proper protective equipment worn when handling all blood and body fluids. (Always use std precautions) • Avoid multi-dose medicine vials ▪ Active Immunization: Hep B Vaccine • Yeast-Recombinant hepatitis B vaccine (Recombivax HB ) ◆ Used to provide active immunity and has shown rates of protection greater than 90% ◆ Recommended for people who are at high risk for HBV and for people with HCV or other chronic liver diseases. ◆ Immunologic memory may remain intact for at least 5-10 years and may become undetectable. Measurable amounts of HBV antibodies are not needed for protection but it is recommended that immunocompromised people get a booster dose. ◆ Administered IM in 3 doses. 2nd and 3rd doses are given 1-6months after 1st, 3rd dose is important because it provides the prolonged immunity]. Given in the deltoid muscle for adults. ◆ Provides no protection against other types. ▪ Passive immunity: Hep B Immune Globulin (HBIG) • HBIG is indicated for those who have never had HBV or have never received HBV vaccine and became exposed to HBV. • Specific Indications ◆ Inadvertent exposure of HBV by needle stick ◆ Sexual contact with person positive for HBV ◆ Perinatal exposure by positive mother (newborn should receive HBIG within 12hrs after delivery) • Prompt Immunization w/ HBIG (w/in hours to a few days after exposure) increases the likely hood of protection. ➢ Medical Management ▪ Goal are to minimize inflammation, infectivity, and decrease symptoms ▪ Alpha-Interferon • Single modality that offers the most promise • Doses are 5 million U daily or 10 million U 3 times a week weekly for 16-24 weeks ◆ Is method results in remission of disease in one third of patients infected • Administered by injection and has significant side effects which are: ◆ Fever, chills, anorexia, nausea, myalgia (muscle pain), and fatigue ◆ Delayed side effects are more serious and may require lower doses or discontinuation, these are bone marrow suppression, thyroid dysfunction, alopecia, and bacterial infections. • A recombinant form of interferon is peginterferon alfa-2a and has once weekly dosing ( has largely replaced standard interferon) ▪ Oral Antivirals used are lamivudine and adefovir • Used for chronic hepatitis B and reduces progressing to cirrhosis. • Can also be used for pts with decompensated cirrhosis who are awaiting a new liver. ▪ Bedrest and Adequate nutrition are also helpful ❖ Hepatitis C (HCV) (Pg. 1365) ➢ Overveiw ▪ Most common blood born infection, incubation avg. is 50 days, chronic carrier state is common, increased risk of chronic liver disease. ➢ Risk ▪ Contaminated needles, children born by infected mothers, multiple sex partners and unprotected sex, recipient of blood products ➢ Tx ▪ Anti-viral meds are ledipasvir-sofosbuvir ▪ Interferon alfa-2b • Tx is longer with more side effects than antiviral ▪ Liver transplant ❖ Hepatitis D ➢ Must have HBV first ➢ Likely chronic, carrier and cirrhosis ➢ NO VACCINE ❖ Hepatitis E ➢ Similar to HAV ➢ NO VACCINE ❖ Hepatitis G ➢ Causes persistent infection for up to 9 years ➢ Co-Infection often w/ HBV, HCV, and HIV ➢ NO VACCINE 11. Discriminate between hypo and hyperthyroidism, including signs, symptoms, treatments, and nursing care. ❖ Hypothyroidism (pg. 1474) ➢ Higher incidence in elderly and women over 50 ➢ Causes ▪ Most common cause is autoimmune thyroiditis, in which the immune system attacks the thyroid gland ▪ Other are atrophy b/c of aging, therapy of hyperthyroidism (Radioactive iodine and thyroidectomy), meds (lithium, iodine compounds, antithyroid meds), radiation of head and neck, infiltration diseases, and iodine deficiency or excess. ➢ Clinical Manifestations ▪ Extreme fatigue, Alopecia, hoarseness, menstrual disturbances (menorrhagia, amenorrhea, and loss of libido), weight gain, cold in warm environment, subdued emotion, slowed speech, tongue enlarges, hands and feet increase in size, respiratory weakness. ▪ Severe hypothyroidism pts are hypothermic and are abnormally sensitive to sedative, opioid and anesthetic agents (Administer with CAUTION) ▪ Myxedema Coma is a rare life-threating manifestation that causes the pt to become hypothermic and unconscious. • Cause by undiagnosed hypothyroidism pts who are undergoing surgery, infection or other systemic disease, or by uses of sedatives or opioid analgesics. • Pt initially shows signs of depression, diminished congnative status, lethargy, and somnolence. • Respiratory drive is depressed resulting in alveolar hypoventilation, carbon dioxide retention, necrosis, and coma. ➢ Medical Management ▪ Synthetic Levothyroxine • Give early (2hrs befor breakfast) ▪ Monitor for s&s of acute coronary syndrome (ACS), must be aggressively treated to avoid morbid complications, if angina or dysrhythmias occur thyroid administration should be discontinued immediately. ➢ Nursing Care ▪ VS, Orientate, Provide stimulation, Extra clothing/blankets (pts will loose heat), space out activities to promote rest, monitor bowel function, high fiber diet ❖ Hyperthyroidism (Pg. 1478) ➢ Causes ▪ Graves disease is most common, others are toxic multinodular goiter, and excessive ingestion of thyroid hormone. ▪ May appear after emotional shock, stress, or infection ▪ Affects women 8 times more than mean ➢ Clinical Manifestations ▪ Presenting symptom is usually nervousness. ▪ Pts often hyper-excitable, irritable and apprehensive. ▪ Rapid pulse and rest and exertion 90-160 ▪ Poor tolerance to heat, excessive perspiration, flushed ▪ Exophthalmos (protrusion of eye balls) ▪ Increase appetite, weight loss, diarrhea ▪ Periods of remission and exacerbations ➢ Assessment ▪ Thyroid gland is enlarged, soft and may pulsate (thrill or bruit) ▪ Increases serum thyroxine and increased 123I or 125I uptake (Iodine uptake) ➢ Medical management ▪ Radioactive Iodine • Most common tx • Iodine concentrates in the thyroid and destroys thyroid cells w/out compromising other radiosensitive tissues • Contraindicated in pregnant women, pregnancy test is given 48hrs before administration, should not conceive for up to 6 months following tx, and iodine should not be admin until 6 weeks after lactation stops • Pretreat high risk patients w/antithyroid meds • Watch for thyroid storm ▪ Anti-thyroid Meds • Methimazole (MMI), propylthiouracil (PTU) ◆ Used until pt is euthyroid (neither hypo or hyper) ◆ Take each morning on empty stomach 30 mins before meals ◆ May take several weeks until relief of symptoms ◆ With any sign of infection stop medication and contact provider ◆ Pregnant women should discontinue PTU after first trimester and switch to MMI for the remainder of pregnancy. ◆ Discontinuation of meds before complete usually leads to relapse w/in 6 months ➢ Surgical Management (Thyroidectomy) ▪ Reserved for pts allergic to meds, pts with large goiters, ▪ Pre-op • Give antithyroid meds to promote euthyroid state • Teach client to support neck with hands behind head • Scar will be thin • Calcium gluconate at bedside and trach tray ▪ Post-op • Risk of hypothyroidism • Risk of damage to parathyroids • Monitor calcium, chvosteks sign, calcium gluconate • Tetany may be 1-7 days later ▪ Complications • Airway compromise, trach tray at bedside, and risk for hemorrhage. ❖ Thyroid Storm (Thyrotoxic Crisis) (pg. 1480) ➢ Untreated is almost always fatal ➢ Causes ▪ Usually precipitated by stress from injury, infection, thyroid or nonthyroid surgery, tooth extraction, insulin reaction, DKA, pregnancy, digitalis intoxication, abrupt w/drawl of antithyroid meds, vigorous palpation of thyroid. ➢ S&S ▪ High fever, extreme tachycardia (>130 bpm), exaggerated symptoms of hyperthyroidism, altered neuro and mental state ➢ Management ▪ Reduce temperature ▪ Humidified O2 ▪ IV fluids containing dextrose ▪ PTU or MMI administered ▪ Hydrocortisone to treat shock ▪ Iodine is administered to decrease output of T4 12. Discuss parathyroidism and the physiologic effects of over and under production of parathyroid hormones. Explain medical and nursing treatments. ❖ Hyperparathyroidism (Pg. 1487) ➢ Caused by over production of parathyroid hormone and is characterized by bone decalcifications and renal calculi containing calcium ➢ Clinical Manifestations ▪ Kidney stones, due to increase urinary excretion of calcium and phosphorus. ▪ Skeletal pain and tenderness, pain of weight bearing, pathologic fractures, deformities, and shirting of body stature cause by demineralization of bones or by bone tumors ➢ Assessment ▪ Dx by persistent elevation of serum calcium and elevated concentration of parathyroid hormone ➢ Medical Management ▪ Parathyroidectomy • Recommended tx for symptomatic pts and recommended for asymptomatic pts who meet following criteria: ◆ Younger than 50 years old ◆ Unable or unlikely to participate in follow up care ◆ Serum calcium level more than 1mg/dL above normal reference range ◆ Urinary calcium level > 400 mg/day ◆ 30 % or greater decrease in kidney function ▪ Hydration Therapy • Daily fluid intake of 2,000 mL is recommended to prevent calculous formation. • Thiazide diuretics are avoided b/c they decrease the excretion of calcium ➢ Complications: Hypercalcemic Crisis ▪ Associated with serum calcium levels greater than 13 mg/dL that result in neurologic, cardiovascular, and kidney symptoms ▪ Treatment • Rapid, large volumes of IV isotonic saline fluids to maintain urine output of 100-150 ml/hr • Combined with calcitonin to promote renal excretion of excess calcium and reduce bone resorption. ❖ Hypoparathyroidism (Pg. 1489) ➢ Most common cause is near-total removal of the thyroid gland ➢ Inadequate secretion of parathyroid hormone results in increase blood phosphate and decreases blood calcium ➢ Clinical Manifestations ▪ Mostly cause by the hypocalcemia • Tetant (tremors), cramps, and seizures ➢ Assessment ▪ Positive Chvostek’s Sign • When a sharp tap close to the ear causes a spasm or twitching of the mouth, nose, and eye. ▪ Positive Trousseau’s Sign • When carpopedal spasm (hand and fingers draw in) is induced by occluding blood flow for 3 mins with a blood pressure cuff. ➢ Medical Management ▪ Oral calcium and vitamin D to increase calcium to normal levels ➢ Nursing management ▪ Keep IV calcium gluconate available for emergency ▪ Administer slowly and cautiously 13. Discriminate between DKA and HHNS. Explain the pathophysiology, signs and symptoms, treatments and expected nursing and medical care for each. ❖ Diabetic Ketoacidosis (DKA) (Pg. 1443 Text & Pg. 927 in ATI book) ➢ Acute life threating condition characterized by hyperglycemia greater than 250 mg/dL, resulting in the breakdown of body fat for energy and an accumulation of ketones in the blood and urine. Ketones are acidic and build- up of these lead to metabolic acidosis. ➢ Rapid onset ➢ Risk/Precipitating Factors ▪ Lack of sufficient insulin related to undiagnosed or untreated type 1 DM or nonadherence of Tx. ▪ Reduced or missed insulin doses ▪ Any condition that increases carb metabolism such as physical or emotional stress, illness, infection (No.1 cause) surgery or trauma. ➢ Clinical Manifestations (Only ones found in DKA) ▪ Polyphagia (Increase appetite), Weight loss, Nausea, Vomiting and abdominal pain, Acetone breath (Fruity), Kussmaul respirations (deep rapid respirations), Metabolic Acidosis. ➢ Assessment ▪ Plasma glucose > 250 mg/Dl ▪ Arterial Ph < 7.3 ▪ Presence of ketonemia or ketonuria. ➢ Management of DKA ▪ Fluid Replacement • 1-3L of 0.9% NS first hour, then I L per hour until euvolemic. • Once euvolemic swap to 0.45% NS till stable • Then switch to D5W when blood glucose reaches 180-250 mg/dl ▪ Insulin • Start after fluid resuscitation is in progress due to possibility of low K+ (about 1 hr) • IV regular insulin (Only one that can be given IV) at a slow continuous rate (0.1 U/kg/h) • Hourly BG levels must be drawn so make sure the BG isnt dropping faster than 100mg/dl/hr. • Once BG at 180-250 mg/dl stop insulin to avoid hypoglycemia ▪ Electrolytes (K+) • Potassium levels decrease during fluid Tx of DKA so potassium may be infused even if levels are normal. • Give 20-40 mEq/L of potassium with each liter of fluid once the potassium level is less than 5.5 mEq/L ➢ Nursing care ▪ Strict I&O ▪ Assess for fluid over load ❖ Hyperglycemic Hyperosmolar Syndrome (HHS) (Pg. 1445 Text & Pg. 927 ATI) ➢ Characterized by profound hyperglycemia greater than 600 mg/dl, hyperosmolarity that leads to dehydration and absence of ketosis. ➢ Onset is gradual, over a few days ➢ Risk Factors ▪ Type 2 Dm in older adults ▪ Inadequate fluid intake with older adults ▪ Older adults with kidney problems that do not excrete excess glucose into urine ▪ Medical conditions such as MI, cerebral vascular injury, or sepsis ▪ Infection or stress ➢ Clinical Manifestations ▪ 4 primary features – Hyperglycemia (>600 mg/dl), absence of ketones, profound dehydration (causes Polydipsia “thirst”), and neurological changes (Seizures) ▪ Can mimic stroke ➢ Treatment ▪ Similar to DKA with fluid and insulin ▪ DVT prophylaxis ▪ Poor outcome 40% mortality rate 14. Explain the pathophysiology of pancreatitis. Explain why shock, hemorrhage, hyperglycemia, and pulmonary involvement are major concerns for the disease. Discuss signs and symptoms, medical interventions, and nursing care. ❖ Acute Pancreatitis (Pg. 1401) ➢ Ranges from mild, self-limiting disorder to a severe, rapidly fatal disease that does not respond to treatment. ▪ Has a mortality rate of 10-15% ➢ Pathophysiology ▪ 80% of pts w/acute pancreatitis have a biliary tract disease such as gallstones or have a long term Hx of alcohol abuse. ▪ Gallstones cause this by entering the common bile duct and become lodged which obstructs the flow of pancreatic juices or causes reflux of bile from the common duct back into the pancreatic duct, which then activates the enzymes w/in the pancreas. ▪ Activation of enzymes can lead to vasodilation, increased vascular permeability, necrosis, erosion, and hemorrhage. ▪ Activated enzymes in the pancreas will begin to digest the pancreas itself which is referred to as auto-digestion. ▪ Auto-digestion of the pancreas sets off a massive inflammatory response leading to third spacing of fluid, hypotension and shock ▪ If these pancreatic enzymes are released through the pancreatic vasculature into the blood stream they can damage the aveolar capillary membrane and cause ARDS. ➢ Clinical Manifestations ▪ Onset 24-48hrs after heavy meal or ETOH intake. ▪ Acute epigastric pain ▪ Vomiting unrelieved by treatment. ▪ ** bruising around umbilicus (Cullen’s Sign) is a severe sign ▪ ** bruising around flank (Grey Tunner Sign) is a severe sign ▪ Hypotension due to third spacing which and lead to shock and acute renal failure ▪ Respiratory distress and hypoxia ▪ Hypocalcemia which can cause tetany that can cause paralysis and make it hard to breath ➢ Assessment ▪ Elevated Lipase 70-200 U/L (3x normal in pancreatitis) ▪ Elevated Amylase 58-70 U/L ▪ Elevated WBC ➢ Complications ▪ Acute pancreatitis is a serious medical condition ▪ If severe requires an admission to the ICU b/c complications can occur rapidly: • These are shock, GI bleed, renal failure, respiratory failure, treatment is supportive and to prevent further complications such as infection. ➢ Medical and Nursing Care ▪ NPO – to inhibit stimulation of the pancreas and its secretion of enzymes. • Enteral feedings should be started early • Parenteral nutrition can be used to meet nutritional needs if the person cannot tolerate enteral feedings. • H2 antagonist (cimetidine or ranitidine) can be used to decrease pancreatic enzyme activity • No sight or smell of food so pt doesn’t salivate and secrete enzymes ▪ Pain Relief • May require perenteral opioids such as morphine, fentanyl, or hydromorphone. ▪ Monitor blood glucose ▪ Symptomatic treatment of symptoms 15. Differentiate Cushing syndrome from other metabolic diseases. Explain each of the symptoms, especially hyperglycemia, hypertension, peptic ulcer, and diminished immunity occur. Discuss signs and symptoms, medical interventions, and nursing care. ❖ Cushing Syndrome (Pg. 1496) ➢ Most common cause is the use of corticosteroids and is infrequently the result of excessive corticosteroid produnction secondary to hyperplasia of the adrenal cortex. ➢ Adrenal over production. ➢ Clinical Manifestations ▪ Weight gain in midsection and upper back (Buffalo Hump), fatigue, muscle weakness, Moon face, facial flushing, Pink and purple stretch marks (striae), thin fragile skin, slow healing of cuts, depression, anxiety, and irritability, thicker and more visible body and facial hair (hirsutism), acne, irregular or absent menstral periods, erectile dysfunction in males, high B/P ➢ Medical Management ▪ Surgical Removal (Transsphenoidal Hypophysectomy ) • This is the removal of a pituitary tumor that may be causing symptoms • 80% success rate ▪ Radiation • Also very successful but does take several month to control symptoms ▪ Adrenalectomy • Tx of choice in pts w/ primary adrenal hypertrophy • If one adrenal gland is removed temporary hydrocortisone replacement may be needed until the other begins producing enough adrenal hormones needed for the body • If both adrenal glands are removed the patient will be on lifetime replacement of adrenal cortex hormones ▪ Adrenal Enzyme Inhibitors (Metyrapone & Mitotane) • These may be used if the cause is ectopic ATCH secretion by a tumor that cannot be removed ▪ Reduction of Corticosteroids • If cause is result of these meds an attempt will be made to reduce or taper the medication to the minimum dose needed to treat underlying disease process. • Going from once a day to Alternate day therapy usually tends to decrease cushing symptoms. ➢ Ways to Prevent Complications of Exogenous Corticosteroids (Cortisone, Budesonide, other end in “One”) ▪ Education • Take before 9am, Space multiple doses, taper high dose and long term therapy, arrange for higher doses when pt subject to unusual stressors, no live virus vaccines, antacids and take with food if GI upset occurs, freq follow up visits, wear medical alert bracelet. ▪ Side effects • Increased appetite, weight gain, heart burn/indigestion, susceptible to infection, poor wound healing, muscle weakness and fatigue ➢ Nursing interventions ▪ Decrease risk of injury because of delayed wound healing ▪ Decrease risk for infection and monitor pt for subtle signs of infection because corticosteroids mask inflammatory response to infections ▪ Encourage rest and activity to prevent complications of immobility and promote increased self-esteem ▪ Promote skin integrity, b/c pt skin is fragile nurses shouldn’t use adhesive tape and should assist pt to change positions frequently ▪ Improvement of body image can be promoted by discussion of the unwanted physical changes that will disappear in time, and help pt modify diet to decrease weight gain and edema ▪ Monitor for potential complications such as Addisonian Crisis which is caused by a rapid decreasing of adrenal hormones, b/c of surgery or abrupt cessation of corticosteroid agents. • S&S of crisis is Hypotension, cyanosis, fever, nausea, vomiting, and the other classic signs of shock. • Immediate tx is directed toward combating circulator shock by IV corticosteroids (Hydrocortisone), Fluid replacement w/ 5% dextrose in NS, and Vasopressors if Hypotension persist. Monitor VS and place pt in recumbent position with legs elevated ▪ Check Stool for occult blood which will indicate GI bleed from ulcer formation ➢ Other Discharge instructions ▪ Do not stop taking med abruptly and always keep adequate supply 16. Discuss teaching points for each of the conditions discussed. 17. Prioritize nursing actions when caring for clients with metabolic disorders. 7-12-15 sw Rev 3-28-17sw [Show More]
Last updated: 1 year ago
Preview 1 out of 23 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$14.50
Document information
Connected school, study & course
About the document
Uploaded On
Jun 14, 2023
Number of pages
23
Written in
Additional information
This document has been written for:
Uploaded
Jun 14, 2023
Downloads
0
Views
46














.png)