NURSING. > EXAM > NCSBN – Lesson 6A: Pharmacological & Parenteral Therapies Study Guide,100% CORRECT (All)
NCSBN – Lesson 6A: Pharmacological & Parenteral Therapies Study Guide,100% CORRECT
Document Content and Description Below
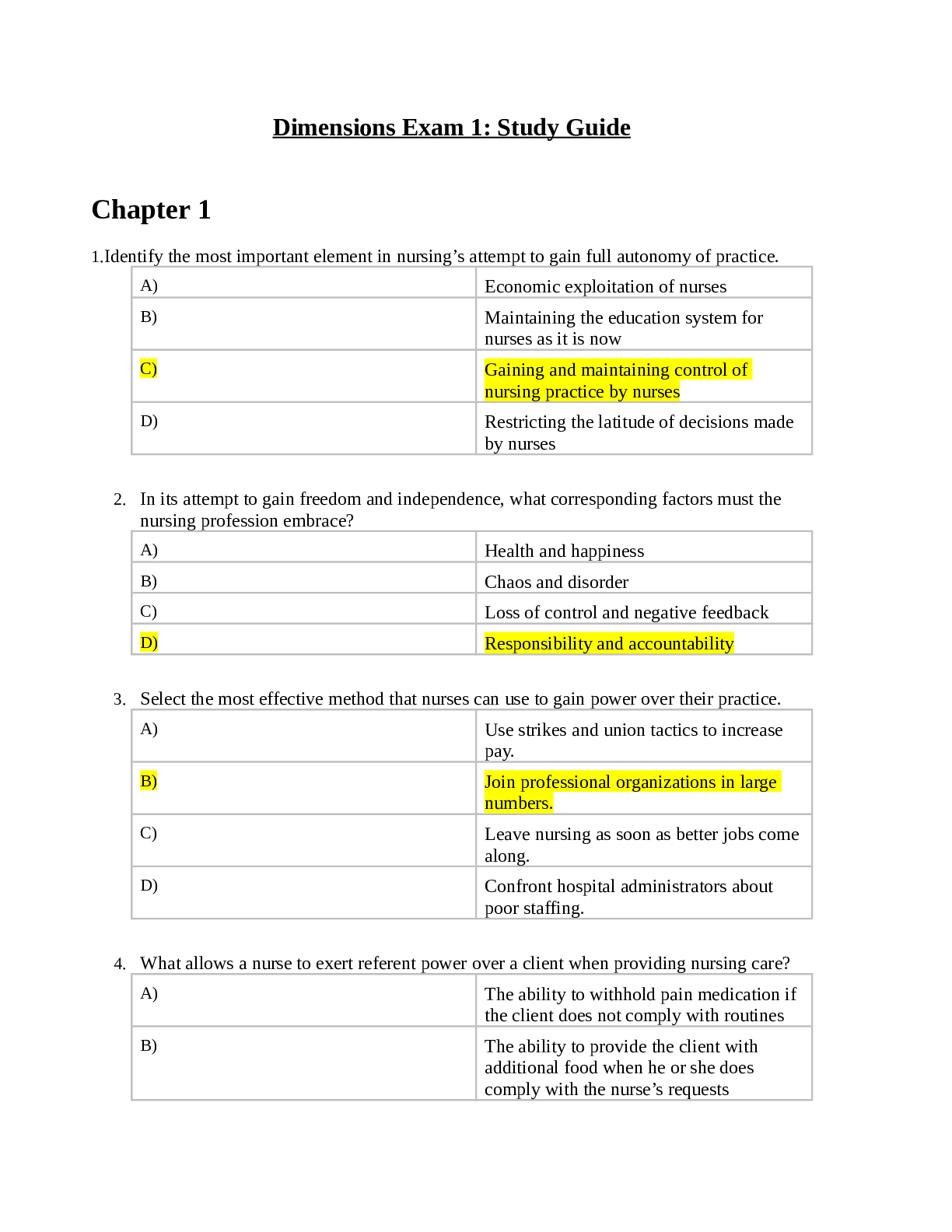
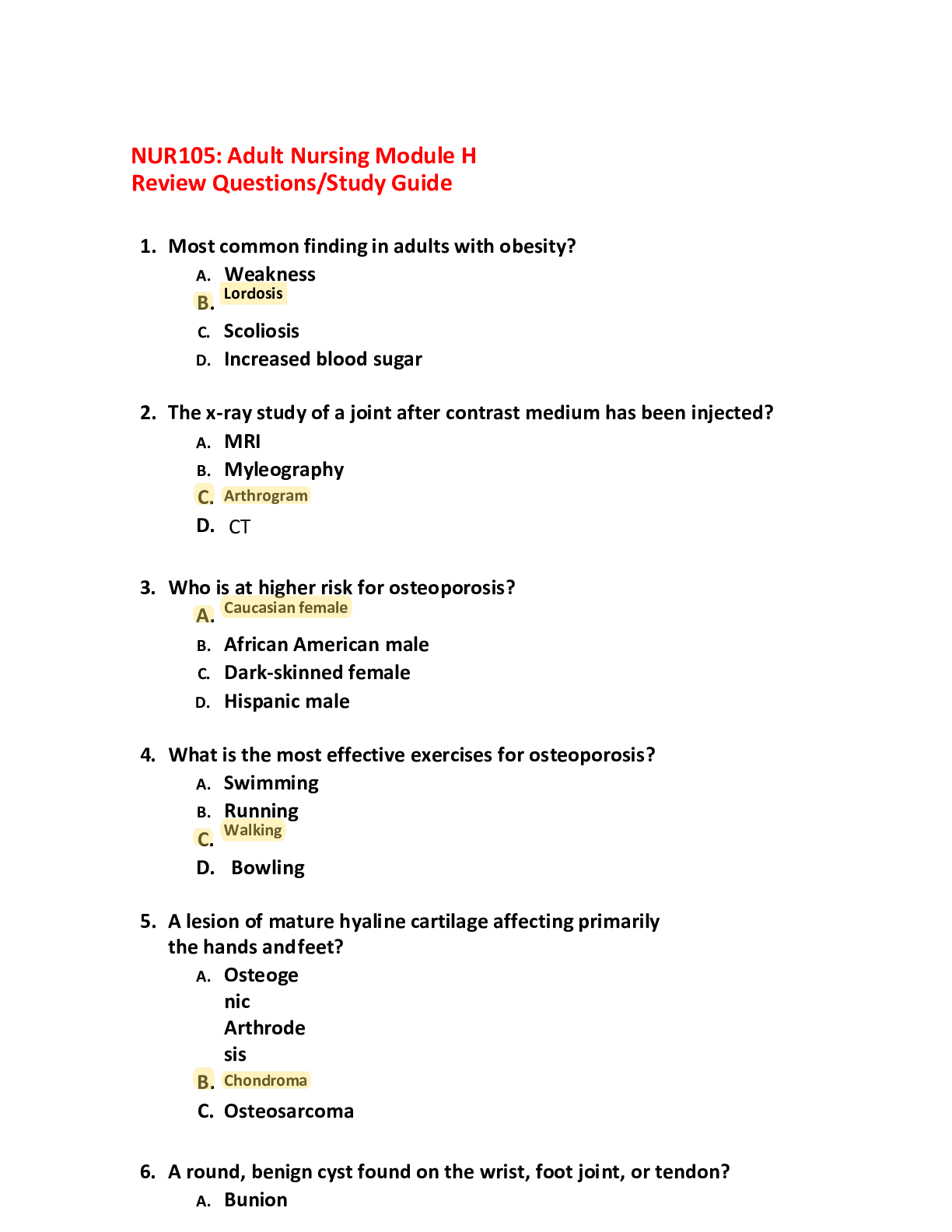
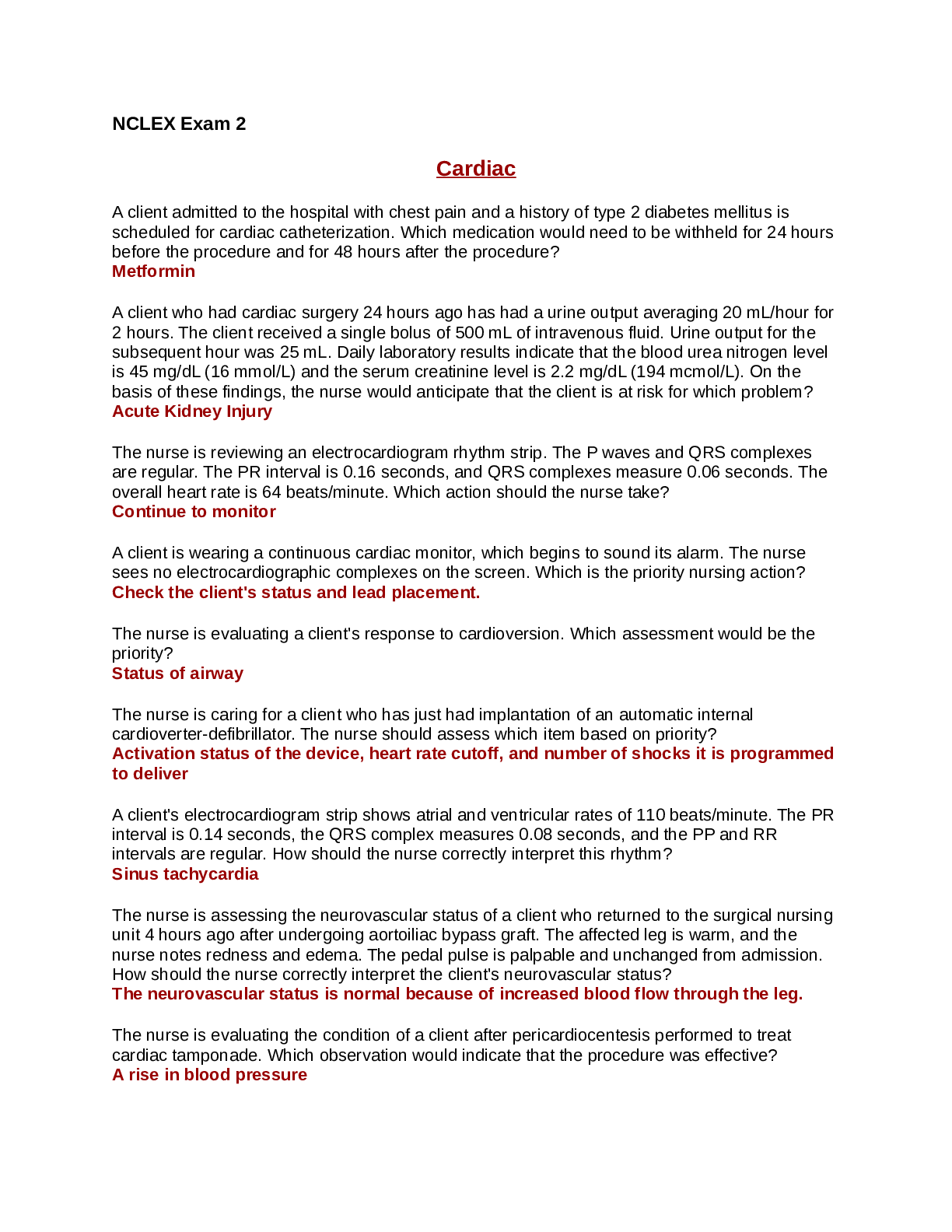
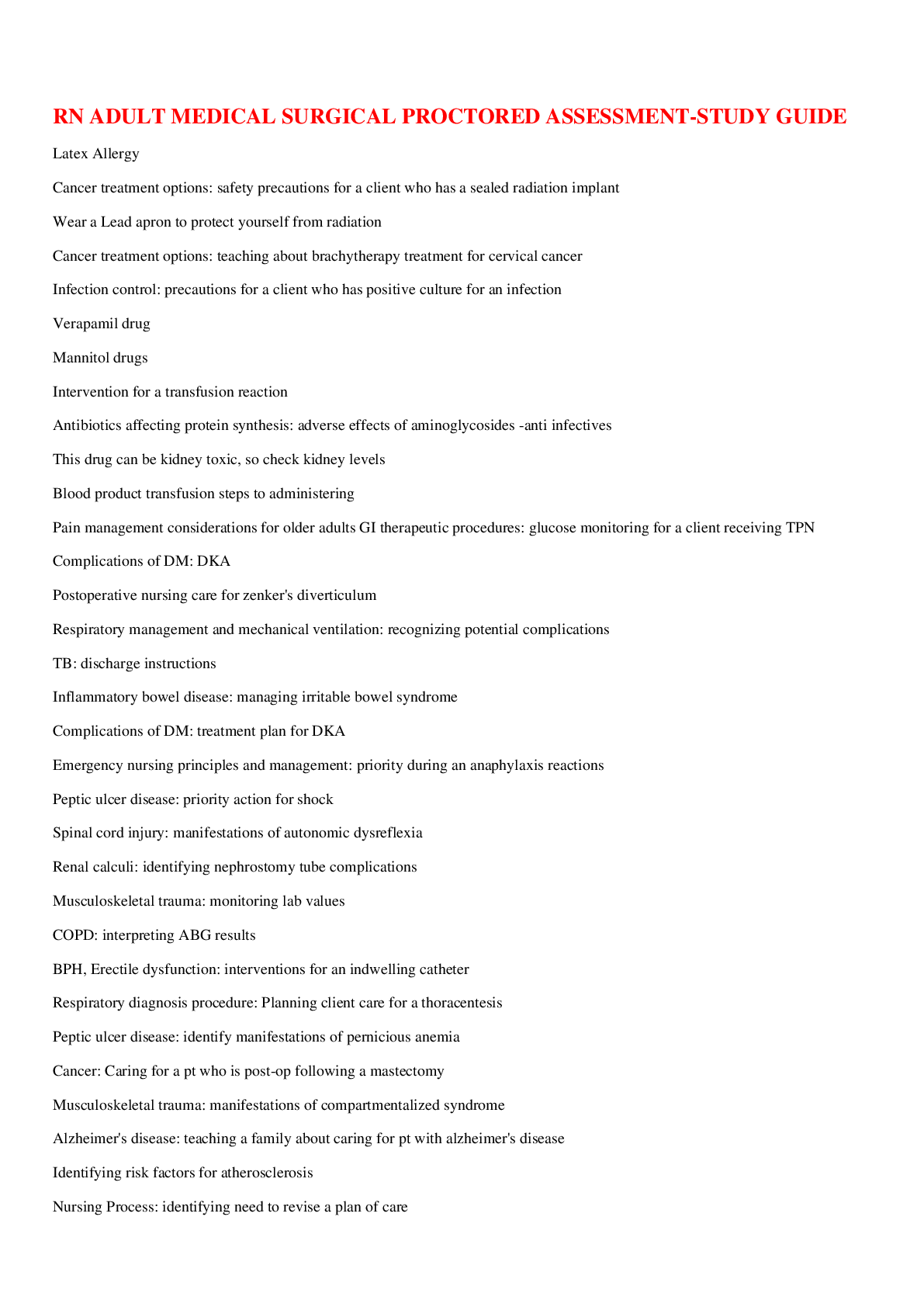
NCSBN – Lesson 6A: Pharmacological & Parenteral Therapies Study Guide Pharmacology Overview The nurse must have a general understanding of how medications are named, their pharmacodynamics and pha... rmacokinetics. Medication safety is a top priority and the nurse is expected to provide safe and proper medication adminstration. Generic drugs Nonproprietary drugs (i.e., not protected by a trademark). In the U.S., generic drugs are required to meet the same bioequivalency test as the original brand name drugs. Manufacturers of brand name drugs produce the majority of generic drugs and allow them to be sold without the original brand name. Generic and brand name drugs may experience manufacturing defects. Nearly half of all proprietary drugs available in the U.S. are also sold less expensively as generic drugs. Naming Medication • A medication's chemical name is the description of its chemical and molecular structure or composition. • A medication's generic name is the description assigned by the U.S. Adopted Name Council and is identified by lowercase letters. • A medication's trade (brand) name is the manufacturer's registered name; the name is capitalized and treated as a proper noun. • High-alert drugs are medications with a high potential to cause harm if administered incorrectly to the client. As a general rule, classes of drugs have the same generic "last" name: "PRILS" = ACE inhibitors (enalapril, lisinopril) "SARTANS" = angiotensin receptor blockers (losartan, valsartan) "TRIPTANS" = treatment of acute migraine headache "STATINS" = lower LDL cholesterol (simvastatin, rosuvastatin) "DIPINES" = calcium channel blockers (amlodipine, nifedipine) "PRAZOLES" = proton pump inhibitors (omeprazole) "AZOLES" = antifungals (miconazole) Pharmacodynamics Pharmacokinetics is how the body affects the medication. It consists of four processes: absorption, distribution, biotransformation (metabolism) and excretion. The factors affecting pharmacokinetics include a client's body mass index or growth and development factors, and drug-related factors such as the medication's route and administration, therapeutic ranges and side effects or tolerances. Medication Safety Nurses are responsible for providing safe, quality care in every patient setting. The complexity of the health care environment can contribute to prospective errors. Medication-related errors are the most common type of error and also help account for the increase in health care costs. Medication errors are responsible for over 7000 deaths annually (IOM, 2000). 10 Rights of Medication Administration The ten rights of medication administration • Right dose: o Check the medication's label against the client's administration record. • Right time: o Check the health care organization's policies for the right time to administer the drug (30 minutes before or 30 minutes after the ordered time is usually acceptable). • Right route: o Check the medication order to verify that the route is specified. • Right drug: o Check speed of infusion or push. o Verify accurate dosage calculations. • Right client: o Check the client's ID bracelet and verify the name and birth date; where available, include a bar code check of the ID bracelet. o Have the client state full name and birth date. o Verify information using the medication administration report (MAR). • Right documentation: o Immediately after giving the medication, the nurse will document on the MAR or electronic medical record (EMR), including the drug name, time, dose, route and signature. • Right assessment: o If necessary, the nurse must assess vital signs and check client data, such as lab values or other diagnostic studies before administrating medication. If the client needs to swallow their medication, the nurse must also assess the client's ability to do so. • Right education: o The client should be taught the indication for and maintenance of current medications. • Right evaluation: o Assess the client's response to an intervention. • Right to refuse medication: o The client has a right to refuse medication. The nurse must explore the client's reasoning for refusing the medication and then should explain complications associated with not taking the medication. Finally, the nurse must document the incident and notify the client's health care provider. Times to Double-check a Medication • When first taking the medication out of the container • Just before opening the medication package or pouring the dose • Just before replacing the container in the storage area or giving a unit dose to the client Medication Errors • Medication errors are often a result of poor communication. The most common nursing medication errors include administering the wrong dose, giving the medication at the wrong time or by the wrong route, and administering medications to the incorrect client. • Prescribing errors include mistakes made by the provider in prescribing drugs. This involves unsuitable drug choices, dosing errors, incompatibilities and contraindications. Preventing Medication Errors There are several steps you can follow to decrease medication errors. First, perform a medication reconciliation and avoid distractions while compiling the client's medications. Next, thoroughly check the Ten Rights of Medication Administration. Be sure to review the client's data and diagnostic tests prior to administration. Finally, read the medication labels three separate times and verify any medication allergies and contradictions. Use the acronym P.I.N.C.H. to remember some of the more commonly administered high alert medications. P = Potassium I = Insulin N = Narcotics C = Chemotherapy H = Heparin Client Teaching for All Prescribed Medications The nurse must discuss and verify the client's understanding of all drug information including the drug's name, dose, indication, administration guidelines, storage and adverse reactions (A harmful and undesired reaction resulting from the use of medication or other intervention, e.g., chemotherapy or surgery. An adverse effect is typically a function of dosage, drug levels, or drug interactions) and side effects. It is also important for the client to understand that they must consult with a provider if they would like to cut or crush a medication, or take over-the-counter (OTC) medications or herbal/vitamin supplements while on their prescribed medication. Finally, the nurse and client should create a current medication list for the client's reference. Blood Product Administration When administering blood products, the nurse is expected to understand the proper identification protocol for their health care organization, assess the client's venous access, evaluate client responses and document properly. • Blood Components 1. Packed Red Blood Cells (RBC) ▪ Packed RBC are given with 0.9% saline solution (NaCl) and typically administered over a 2-4 hour period. ▪ Use a standard blood filter and mix cells (squeeze bag) every 20-30 minutes. 2. Platelets ▪ Clients can experience a febrile reaction. ▪ Use 0.9% NaCl companion solution with a non-wettable filter. ▪ Give platelets as quickly as possible, typically four units/hour. 3. Plasma ▪ Clients can experience circulatory overload. ▪ Administer with a straight line set and give as quickly as possible. 4. Albumin ▪ Clients can experience circulatory overload. ▪ Use the administration set provided and give 25% albumin, 1 mL/min. Administer as quickly as possible if the client is in shock. 5. Prothrombin ▪ Clients can experience an allergic/febrile reaction. ▪ Hepatitis risk is also greater than with whole blood. ▪ Use a straight line set for administration. Nursing Procedure & Interventions • Guidelines for Blood Administration 1. The client must sign a consent form before the nurse administers blood. The nurse will retrieve the blood from the blood bank area. Working with another RN, the nurse will compare the blood and the crossmatch slip from the blood bank and compare data with the client's ID bracelet. The nurse will verify the client's name, ID number, blood type and Rh factors, and will also verify the donor number and expiration date on the blood container. 2. The nurse will establish baseline data and monitor the client, following the health care organization's policy for frequency and duration. Vital signs are typically the first to change during a transfusion reaction and it is critical to establish an accurate baseline. 3. The nurse will record the client's vital signs, oxygen saturation (SaO2) and skin condition after first 15 minutes of a transfusion, during administration (at an interval established by the health care organization's policy) and one hour post- transfusion. 4. The nurse will assess breath sounds, crackles, dyspnea and jugular vein distention. 5. The nurse will review the client's hemoglobin (Hgb) and hematocrit (HCT), urine output; serum potassium, calcium and creatinine. 6. Prime the intravenous tubing with normal saline for whole blood administration. Never use dextrose solutions, which may cause clumping of RBCs. Make sure the insertion site is patent. 7. Initiate the transfusion slowly for 15-20 minutes and remain at the bedside, monitoring the client's vital signs every five minutes (or at an interval established by organization policy). Frequently question the client about any unusual feelings. Most adverse reactions occur within the first 15 minutes. Benign hives may occur and the nurse can treat the client symptomatically per policy/orders. • Preventing Complications 1. To prevent complications, carefully verify documentation related to blood products and keep the blood product tags or identification intact. 2. Infuse the transfusion using an infusion control device, at the prescribed rate or the rate established by the organization's policy: ▪ Whole blood and packed RBC (about 250 mL/unit) should be infused within 2-4 hours. 20-gauge or larger needle/catheter is used to prevent hemolysis. ▪ Platelet concentration (about 300 mL/unit) should infuse within 15-30 minute/unit ▪ Fresh frozen plasma (about 200 mL/unit) should infuse within 30-60 minute/unit ▪ Albumin 5% (250-500 mL bottle) should infuse 1-10 mL/minute ▪ Albumin 25% (50-100 mL bottle) should infuse 4 mL/minute 3. Refrigerate the blood (as approved by the blood bank) and initiate the transfusion within 30 minutes of its removal from blood bank. 4. Collaborate with the health care provider to ensure safe administration: ▪ Use autologous blood or auto-transfusion and pre-medicate with a steroid or antihistamine ▪ Notify the blood bank of any transfusion reaction to increase scrutiny of crossmatch ▪ Administer 10% calcium gluconate for hypocalcemia, with continuous cardiac monitoring ▪ The nurse will consider the use of washed, filtered, irradiated, apheresis separated or leukocyte-poor blood products after a transfusion reaction • Client Teaching 1. The nurse will ensure that the client has signed an informed consent form and provide information to the client about contracting infections from the administered blood. Additionally, provide information on the method, monitoring, duration of transfusion, symptom recognition and to report symptoms such as chills, flushing, headache, chest and back pain, nausea, fever or tachycardia. Document any history of immunologic or non-immunologic transfusion reaction to the client database. • Blood Transfusion Reactions If a reaction occurs: 1. stop the transfusion immediately 2. take vital signs 3. Clamp the IV tubing and disconnect at the hub of the catheter. Return the entire administration set and blood bag to blood bank (or follow the health care institution's policy). 4. Do not allow additional blood to enter client's system and do not flush tubing with saline. 5. For findings of circulatory overload (cough, shortness of breath, crackles, hypertension, tachycardia or distended neck veins), place the client in high Fowler's position, administer a diuretic and oxygen as needed and monitor the intake and output (I/O). 6. For findings of sepsis (including rapid onset of chills and fever, vomiting, diarrhea, hypotension and shock), obtain blood cultures and send the blood transfusion bag for analysis. Treat sepsis with antibiotics, IV fluids, vasopressors and steroids. 7. The nurse will collaborate with the provider for pharmacologic treatment. Treatments may include supplemental oxygen, diuretics, antibiotics, antihistamines or glucocorticoids. In addition, monitor Hgb and HCT and complete a transfusion reaction form per the organization's policy. Total Parenteral Nutrition (TPN) Total Parenteral Nutrition (TPN) provides complete nutrients to the client via a parenteral/IV route. Its use is indicated for clients with severe burns and gastrointestinal (GI) conditions that require complete GI tract rest. Additionally, TPN is for clients with debilitating diseases. Nutritional Support Clinical uses of TPN include improving the nutritional status of clients whose GI tracts are unable to absorb nutrients, and correcting malnutrition due to anorexia, nausea or vomiting. TPN may also be used in clients with dysphagia, infection, multiple illness, trauma or substance abuse (Any use of drugs in a manner deviating from medically-approved or socially-acceptable patterns of use either on a single occasion or episodically.) . Clinical indicators of malnutrition include a low pre-albumin lab value, which indicates a protein deficiency - the primary indicator of malnutrition. Other lab values to consider include a low hemoglobin, transferrin, cholesterol and total lymphocytes. Additional assessments include reddened and open skin areas that are susceptible to infection, dull, dry eyes, nails, skin and hair. You may also see significant muscle wasting. Nursing Care For TPN Clients The TPN intravenous system is NOT to be used for central venous pressure monitoring or withdrawal of blood. Please refer to protocol for y-site compatibility of medications with parenteral nutrition. • Establish Baseline Data & Monitor o Prior to administering TPN, take the client's vital signs, SaO2, and right atrial pressure. o Blood urea nitrogen (BUN), creatinine, liver enzyme tests, and pH should also be evaluated. o Monitor the client's glucose at minimum once per shift, due to impairment of glucose metabolism. o Obtain and monitor the client's fluid volume status via weighing the client daily, measuring I/O every shift and assessing edema and breathing sounds. o Monitoring the client's nutritional status includes checking the skin, serum electrolytes, glucose, cholesterol and triglycerides. o Monitor for infection by measuring the client's temperature and white blood cell (WBC) count and assessing the insertion. o Assess the client's neurologic status according to your health care organization's policy. o Be aware of refeeding syndrome during the first 24-48 hours of therapy. The symptoms include bradypnea, lethargy, confusion and weakness. • Prevent Complications o To prevent rebound hypoglycemia ▪ withdraw TPN slowly. o To prevent a microemboli ▪ use a 0.2 µm-filter (except with lipid emulsion). ▪ Administer the solution at a constant rate and do not flush or irrigate the system. o Check the expiration date of the solution and always verify the TPN order. o To prevent hyperglycemia ▪ verify insulin coverage and check blood glucose frequently. o To prevent acidosis ▪ maintain a tight glycemic control and encourage coughing and deep breathing. o Refrigerate tubing until 30 minutes before using and change tubing daily. o The nurse can prevent fluid shifts, hypervolemia and osmotic diuresis by maintaining the infusion rate and glycemic control and verifying volume control with a time strip. o Start the infusion slowly and titrate to the client's tolerance. ▪ Administer 10% dextrose if TPN infusion is interrupted. o To prevent an air-emboli ▪ use Luer-Lok connections, cover the site with occlusive dressings and clamp the tubing when changing the solution or tubing. Parenteral/Intravenous Therapies The main purpose of intravenous therapy is to restore fluid and electrolyte balance. It also provides a route for medication, nutrition and blood components. • Intravenous Fluids o Isotonic ▪ IV Fluid • 0.9% NaCl • Lactated Ringer's ▪ Nursing Considerations • Macrodrip vs. microdrip • Maintain sterile technique • Monitor flow rate • Assess for infiltration • Assess for phlebitis • Change tubing/bag per your organization's policy o Hypotonic ▪ IV Fluid • 0.45% NaCl ▪ Nursing Consideration • Macrodrip vs. microdrip • Maintain sterile technique • Monitor flow rate • Assess for infiltration • Assess for phlebitis • Change tubing/bag per your organization's policy o Hypertonic ▪ IV Fluid • 10-15% dextrose in water or NaCl • Sodium bicarbonate 5% ▪ Nursing Considerations • Macrodrip vs. microdrip • Maintain sterile technique Complications • Monitor flow rate • Assess for infiltration • Assess for phlebitis • Change tubing/bag per your organization's policy • Circulatory Overload o Assessment ▪ Crackles, dyspnea ▪ Confusion ▪ Seizures o Nursing Care ▪ Reduce IV rate ▪ Assess vital signs and lab values ▪ Notify provider • Infiltration o Assessment ▪ Edema ▪ Pain ▪ Coolness in area ▪ Decrease in flow rate o Nursing Care ▪ Discontinue IV ▪ Apply warm compresses ▪ Apply sterile dressing ▪ Elevate arm • Phlebitis o Assessment ▪ Reddened, warm area around the insertion site or the path of the vein ▪ Tenderness and swelling o Nursing Care ▪ Discontinue IV ▪ Apply warm, moist compresses • Thrombophlebitis o Assessment ▪ Pain ▪ Swelling ▪ Redness and warmth around the insertion site or the path of the vein ▪ Fever ▪ Leukocytosis o Nursing Care ▪ Discontinue IV • Hematoma ▪ Apply warm compress ▪ Elevate the extremity o Assessment ▪ Ecchymosis ▪ Immediate swelling at site ▪ Leakage of blood at site o Nursing Care ▪ Discontinue IV ▪ Apply pressure with sterile dressing ▪ Apply cool compresses intermittently for 24 hours to the site, followed by warm compresses • Clotting o Assessment ▪ Decreased IV flow rate ▪ Back flow of blood into tubing o Nursing Care ▪ Discontinue IV ▪ Do not irrigate or milk tubing ▪ Do not increase the IV flow rate or hang the solution higher ▪ Do not aspirate clot from cannula Central Venous Access Devices Peripherally Inserted Central Catheter (PICC) The nurse must have a special certification to insert a PICC line. A PICC line can stay in place for as long as a year if properly maintained. The nurse must measure and document the external length of PICC with each dressing change and flush the unused ports with heparin. (Check your organization's policy for details.). Catheter should be flushed using a rapid push- pause technique to maintain patency of the PICC site after disconnecting from the site. Tunneled Central Venous Catheter (TCV) A tunneled central venous catheter (TCV) is encased in a subcutaneous tunnel. TCV catheters are used in frequent, long-term IV therapy. Types include the Broviac, Hickman and Groshong. The nurse must be certified to insert TCV, which is typically done as a sterile procedure at the bedside. Potential complications to assess include an arterial puncture, vasospasm or nerve damage, ventricular irritation or dysrhythmias. Implanted Port or Vascular Access Device (VAD) Implanted ports or vascular access devices (VAD) are surgically implanted and require needle insertion to access the port. A Huber (non-coring) needle must be used. The nurse must confirm placement prior to medication administration. A VAD requires flushing after each use. Perform a heparin flush monthly if unused. Check your organization's policy for guidelines. Solving Medication Problems The nurse must be able to perform calculations needed for medication administration and use clinical decision making when calculating dosages. Ratio & Proportion Used for calculating solid, liquid and injectable dosages: • Each side of the equation represents the same proportion, percentage or ratio • Both sides of the equation represent an equal relationship but are expressed with different quantities (the two sides match) Dimensional Analysis (DA) • A method for converting between units using ratios between different unit systems • Advantage – only one equation is used to solve for X Dosage Calculations The nurse is responsible for performing calculations as needed for medication administration. Unit Conversions • Length & Mass • Metric to Metric o Involves multiples of 10, 100 or 1000 o Grams : milligrams : micrograms (1 x 1000 x 1000) ▪ 1 gram (g) = 1000 milligrams (mg) ▪ 1 mg = 1000 micrograms (mcg) ▪ 1 g =1,000,000 mcg o Mcg : mg : grams (1 ÷ 1,000 ÷ 1,000) ▪ 1 mcg = 0.001 mg ▪ 1 mg = 0.001 gram ▪ 1 mcg = 0.000001 gram o Liters : milliliter (1 L = 1,000 mL) o Milliliter : liters (1 mL = 0.001 L) • Metric to Other o 2.5 cm = 1 inch o 1 kg = 2.2 lbs. o 30 mL = 1 ounce = 2 tablespoons • Temperature Directions & Example The nurse prepares vancomycin 500 mg IV in 250 mL of normal saline to infuse over two hours. What is the administration rate in mL/minute? Step 1 Set up the equation to determine concentration of drug (mg/mL) Step 2 Now determine the administration rate (mL/min) First determine volume for one hour: Now determine volume for one minute: Solution Report your answer to the nearest whole number [Show More]
Last updated: 1 year ago
Preview 1 out of 13 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 16, 2023
Number of pages
13
Written in
Additional information
This document has been written for:
Uploaded
Jun 16, 2023
Downloads
0
Views
39














.png)