NURSING. > STUDY GUIDE > NURS 2115 Neuro Meta Study Guide Questions with Answers,100% CORRECT (All)
NURS 2115 Neuro Meta Study Guide Questions with Answers,100% CORRECT
Document Content and Description Below
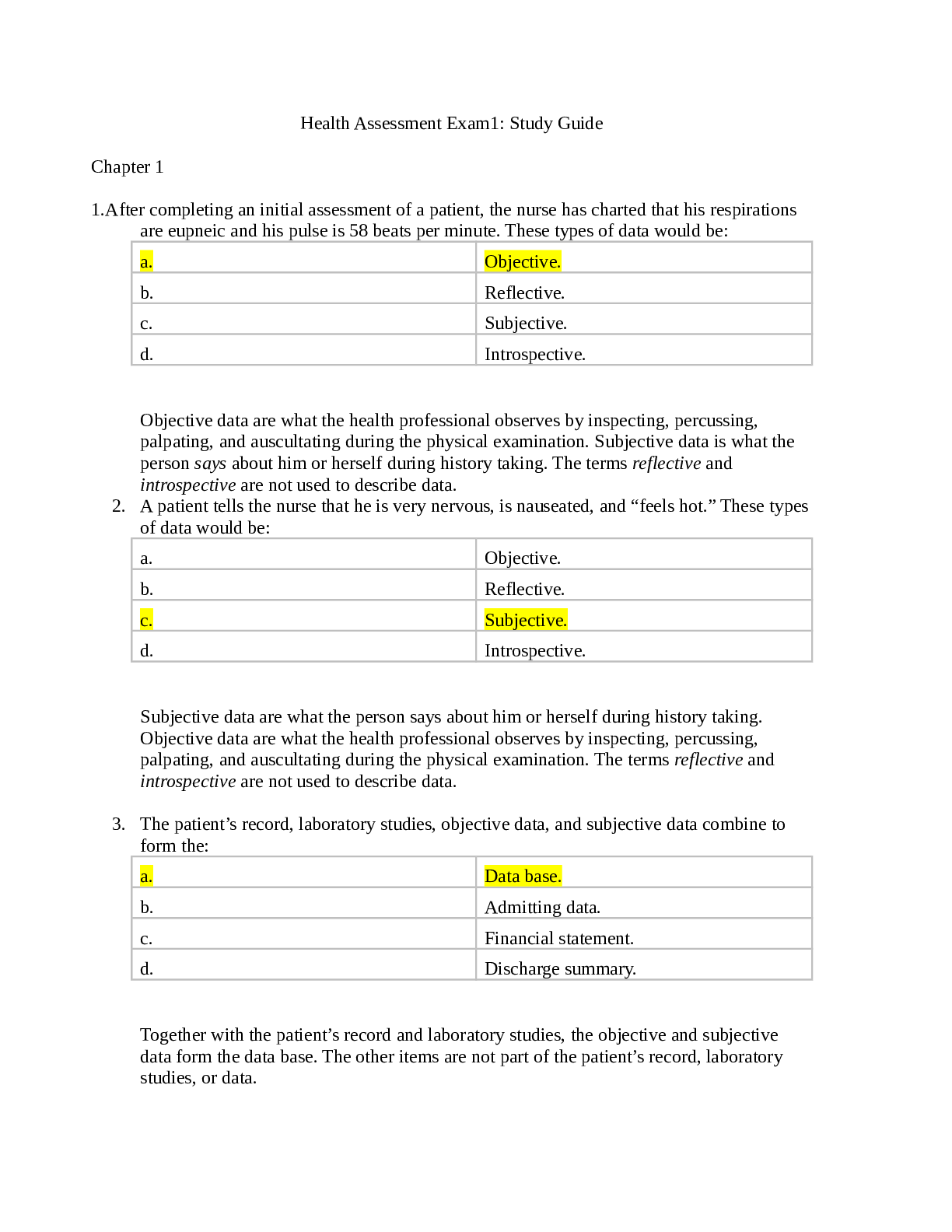
NURS 2115 Neuro Meta Study Guide Questions with Answers 1. What is the Glasgow Coma Scale? What are you assessing when using it? • Assessment tool to determine the patient’s LOC and response t... o tactile stimuli (unconscious) • 3 criteria: o Eye opening o Verbal response o Motor response • Scale of 3-15: 3 indicates coma, 15 indicates no neurological damage • Less than 8, intubate 2. What nursing interventions would you expect when caring for a patient with ineffective cerebral tissue perfusion? • Proper positioning: o Keep head midline, use a cervical collar if necessary, to promote venous drainage o Keep HOB at 30-45 degrees o Extreme rotation and flexion of the neck is avoided o Extreme hip flexion is avoided is also avoided because compression or distortion of the jugular veins increases • Valsalva maneuver: moderately forceful attempt to exhale against a closed airway o Produced by straining at defecation or moving in bed, raises ICP and is to be avoided ▪ Administer stool softeners ▪ High fiber diet o Maintain a patent airway o When moving or turning in bed, instruct the patient to exhale (which opens the glottis) to avoid the Valsalva maneuver • Mechanical ventilation: o Preoxygenate the patient before suctioning with 100% O2 o Do not suction for longer than 15 seconds o Caution with high levels of PEEP: decreased venous return to heart and decreased venous drainage from the brain through increased intrathoracic pressure • Activities that increase ICP, as indicated by changes in waveforms, should be avoided if possible o Space nursing interventions o During interventions, ICP should not increase above 25 mmHg • Avoid emotional stress and frequent arousal from sleep o Keep a calm environment o Minimize stimuli: noise, conversation, light • Brief periods of hyperventilation: CO2 around 35 3. What is significant about drainage from the ear or nose? How would you test the drainage for CSF? • Drainage could indicate a basal skull fracture when CSF escapes from the ears: otorrhea or rhinorrhea • It could also lead to meningeal infection if organisms gain access to the cranial contents • Testing: o halo test ▪ CSF separates from the blood and forms a yellow halo ▪ CSF should be clear and colorless o Glucose test: ▪ If drainage is only clear ▪ Snot does not have glucose 4. Describe the effects of secondary injuries associated with head injuries • Secondary injuries are any injury that happens after the initial insult • Insufficient blood flow • Intracranial hematoma • Cerebral edema • Hypotension • Increased ICP 5. Principles of the Monro-Kellie doctrine • Describes the dynamic of cranial contents • Because of the limited space for expansion within the skull, an increase in any one of the components causes a change in the volume of the others o Tissue, CSF, and blood • Under normal circumstances, minor changes in blood volume and CSF volume occur constantly as a result of alterations in intrathoracic pressure (coughing, sneezing, straining) posture, blood pressure, and systemic oxygen and CO2 levels 6. What are early signs of increased ICP? Late signs? • Early: o Earliest: change in LOC** o Subtle changes in behavior: quiet to restless o Changes in speech: slow or slurred o Changes in vitals: ▪ Increase or decrease in respirations ▪ Change in pattern: increased effort ▪ Increased temperature o Changes in reflexes or flaccid extremities o Changes in cranial nerves: 2, 4, 6 ▪ Pupillary changes and impaired extraocular movements o Headache that is constant ▪ Increases in intensity ▪ Aggravated by movement or straining • Late: o LOC continues to decrease ▪ GCS ≤ 8 o Cushing’s triad: ▪ Systolic HTN with widening pulse pressure ▪ Bradycardia ▪ Irregular respirations and change in respiratory pattern a. Cheyne Stokes: rhythmic waxing and waning of rate and depth of respirations, alternating with brief periods of apnea b. Ataxia: irregular breathing with a random sequence of deep and shallow breaths o Fixed and dilated pupils: ▪ Profound coma ▪ Indicates cerebral hemorrhage o Projectile vomiting o Posturing: ▪ Decorticate ▪ Decerebrate o Hemiplegia/hemiparesis o Facial paralysis o Bilateral flaccidity occurs before death o Loss of brainstem reflexes, including pupillary, corneal, gag, and swallowing reflexes 7. Decerebrate and decorticate posturing. Which is worse? What does each mean? • Abnormal posture response to stimuli • Decorticate: flexion of the upper extremities, internal rotation of the lower extremities, plantar flexion of the feet • Decerebrate: extension and outward rotation of the upper extremities, plantar flexion of the feet • Decerebrate is worse o Indicates increased ICP and decreased nutrition 8. What is normal ICP? How is it assessed? • Normal levels: 5-15 mmHg • Assessed by an ICP monitor o Maintain sterile technique to reduce infection o Transducer: ▪ Zero out ▪ Monitor wave forms 9. What nursing interventions would you expect for a patient who has had a craniotomy? • Supratentorial: above the tentorium (above eyebrow to middle ear, U shaped) o HOB at least 30 degrees o Neck in neutral alignment o Position on side or back ▪ Avoid positioning on operative side if large tumor removed) o Place only 1 pillow under the head • Infratentorial: below the tentorium, brainstem o Maintain neck in straight alignment o Avoid flexion of the neck to prevent possible tearing of the suture line o Position flat on either side, not back o Place 1 small, firm pillow under head • Transsphenoidal: sella turcica and pituitary region o Maintain nasal packing in place and reinforce as needed o Instruct patient to avoid blowing nose o Provide oral care o Keep HOB elevated to promote venous drainage and drainage from surgical site • Assessment: o Respiratory function: ▪ RR and pattern ▪ ABGs o Fluctuation in vitals are carefully monitored and documented o Temperature: hyperthermia o Neurologic checks ▪ Change in LOC or response to stimuli o Surgical dressing inspected for bleeding and CSF drainage o Monitor incision for redness, tenderness, bulging, separating, or foul odor o Obtain labs: ▪ Serum and urine electrolyte: sodium ▪ BUN ▪ Blood glucose ▪ Weight o I/O in view of losses associated with fever, respiration, and CSF drainage • Maintain cerebral tissue perfusion: o Monitor respiratory function o ETT is left in place until patient is awake and shows adequate spontaneous ventilation ▪ Obtain ABG’s o Reduce cerebral edema: ▪ Mannitol ▪ Dexamethasone a. IV q 6 h for 24-72 hr b. Change to oral ASAP c. Taper off over 5-7 days o Assess vitals and neurologic status every 15-60 minutes ▪ LOC and response to stimuli ▪ Pupillary and motor responses o Proper positioning o Turning: ▪ Body should be turned as a unit to prevent placing strain on the incision and possibly tearing the sutures ▪ Change position every 2 hours ▪ Turning sheet or lift sling is placed under the patient’s head to midthigh to make it easier • Regulate temp: o Monitor temp o Hyperthermia: ▪ Remove blankets ▪ Place ice packs ▪ Cooling blankets ▪ Admin antipyretics o Hypothermia: ▪ Rectal temps frequently ▪ Rewarm slowly to prevent shivering • Improve gas exchange: o Reposition every 2 hr o Yawn, sign, deep breathe, incentive spirometry o Increase room humidity • Coping with sensory deprivation: o Periorbital edema: black eye ▪ Elevate HOB ▪ Apply cold compresses ▪ Notify is increases significantly because it may indicate a post op clot, increasing ICP, or poor venous drainage o Announce when entering room • Monitor and manage complications: o Increased ICP, bleeding and hypovolemic shock, altered fluid and electrolyte imbalance (water intoxication and diabetes insipidus), infection, identification of CSF leaks, and seizures o Increased ICP: ▪ Align head in neutral position ▪ HOB 30 degreed ▪ Mannitol ▪ Possible paralytic agent o Fluid and electrolyte: ▪ Oral fluids resumed after 24 hr a. Assess gag reflex ▪ Hyperglycemia: a. corticosteroids can cause hyperglycemia b. Assess glucose every 4-6 hr c. admin H2 blockers to suppress secretion of gastric acid ▪ diabetes insipidus: a. excess urinary output, elevated serum osmolality, decreased urine osmolality, low USG, hypernatremia b. Measure USG hourly c. Fluid replacement compensate urine output d. Monitor serum potassium levels (hypokalemia) ▪ SIADH: a. Fluid retention, hyponatremia, decreased serum osmolality b. Measure I/O and specific gravity determinations of urine c. Monitor serum and urine electrolyte levels d. Fluid restriction o Infection prevention: ▪ Dressing stained with blood immediately post op a. Reinforced with sterile pads ▪ Report heavily stained or displaced dressing immediately ▪ Avoid coughing, sneezing, or blowing nose a. Can cause CSF leakage and increase risk for meningitis** ▪ Use aseptic technique for all dressings, drainage systems, and IV/ART lines o Monitor for seizure activity: ▪ Admin phenytoin (Dilantin) before and after surgery o Monitor other complications: ▪ VTE, pulmonary and urinary tract infection, pressure ulcers ▪ Change position, skin care ▪ Adequate suctioning or elimination of secretions ▪ Thrombosis prophylaxis ▪ Early removal of indwelling cath ▪ Early ambulation 10. What are expected findings of a patient with a traumatic brain injury? • Focal vs diffuse: o Focal: injury has a specific location ▪ Hematoma ▪ Contusion ▪ Laceration o Diffuse: does not have a specific location of injury ▪ Concussion ▪ Diffuse axonal injury • Concussion: temporary loss of neurologic function with complete recovery o Short stent of unconsciousness o Difficulty awakening or speaking o Confusion: typically a short amount of time but can be longer o Severe headache o Vomiting o Pulse changes o Unequal pupils o One sided weakness o Irritability • Contusion: bruised brain with possible surface hemorrhage o Unconscious for a longer period of time than concussion o Stupor o Confusion o Hemorrhage and edema 18-36 hrs after injury • Diffuse axonal injury: widespread shearing and rotational forces that produce damage throughout the brain (to axons) o Head moves forward and back with trauma o Unconscious, immediate coma (traumatic) o Decorticate and decerebrate posturing o CT scan is normal** o Later: CT scan shows significant cerebral edema o Poor prognosis o Midline shift: • Intracranial hemorrhage: o Epidural hematoma: ▪ Loss of consciousness, regain it, then lose it again o Subdural hematoma: ▪ Acute: a. Change in LOC b. Pupillary signs c. Hemiparesis d. Coma e. Increase BP f. Decrease HR and RR ▪ Chronic: a. Severe headache that comes and goes b. Alternating focal neurologic signs c. Personality changes d. Mental deterioration e. Focal seizures o Intracerebral hematoma: ▪ Development of neurologic deficits followed by headache • Skull fractures: o Persistent localized pain o Swelling may or may not occur o Basal: ▪ Bleeding and CSF leakage from the nose, pharynx, or ears ▪ Battle sign ▪ Raccoon eyes ▪ AMS, N/V ▪ Facial droop, hearing loss/tinnitus due to damage of cranial nerve 11. What is an epidural hematoma? • Epidural: bleeding/collection of blood between the dura and the inner surface of the skull o Typically involves the rupture of the middle meningeal artery ▪ Arterial bleed o Herniation occurs more often and faster ▪ More blood is building up faster which causes an increase in ICP faster, which can lead to a herniation faster ▪ Tool to remember: you give epi fast, epidural happens fast** • Subdural: collection of blood between the dura and the brain (space normally occupied by a thin cushion of fluid) o Typically a venous bleed o Herniation occurs slower o Can be acute, subacute, or chronic ▪ Acute: symptoms develop over 24-48 hrs ▪ Subacute: symptoms develop 2 days-2 weeks after injury ▪ Chronic: symptoms often resemble other conditions (stroke, UTI) and occur 3 weeks-months after injury o Risk factors: ▪ Age ▪ Blood thinners • Treatment: o Evacuate blood: craniotomy, burr holes o Decrease ICP o Stop bleeding 12. What nursing interventions would you expect for a patient with a suspected basal skull fracture? • Stabilize airway: ventilation and circulatory issues are the priority • Frequent assessment of neurological signs, ventilation and oxygenation • DVT and gastric ulcer prophylaxis • Heparin • Don’t suction or pack anything into the nose o Risk for infection o Increased ICP with packing • No NG/NT tube o Could enter the brain cavity instead of the pharynx • Conservative care 13. What would you expect/not expect patients with different levels of spinal injuries to be able to do or not do? • Respiratory dysfunction is related to the level of injury • C1: o Muscles contributing to respiration: ▪ C4: diaphragm ▪ T1-T6: intercostals ▪ T6-T12: abdominals o Injuries C4 or above: paralysis of the diaphragm ▪ Often require ventilator support o Injuries T12 and above: ▪ Respiratory dysfunction o Can: o Cannot: ▪ Little or no sensation or control of head and neck ▪ Control diaphragm, requires continuous ventilation ▪ Dress and eat ▪ Eliminate ▪ Mobility: limited, voice or sip-n-puff electric chair • C2-C3: o Can: ▪ Head and neck sensation, some control ▪ Breathe independently, mechanical ventilation for short periods o Cannot: ▪ Dress and eat ▪ Eliminate ▪ Mobility: limited voice or sip-n-puff electric chair • C4: • C5: o Can: ▪ Good head and neck sensation and motor control ▪ Some shoulder elevation ▪ Diaphragm movement ▪ Possibly eat with adaptive sling o Cannot: ▪ Dress and eat ▪ Eliminate ▪ Mobility: limited to voice, mouth, head, chin, or shoulder controlled electric chair o Can: ▪ Full head and neck control ▪ Shoulder strength ▪ Elbow flexion ▪ Dress and eat with assistance ▪ Eliminate with maximal assistance o Cannot: • C6: ▪ Mobility: electric or modified manual wheelchair, needs assistance with transfer o Can: ▪ Fully innervated shoulder ▪ Wrist extension and dorsiflexion ▪ Dress, eat and eliminate, or with minimal assistance ▪ Independent in transfers and wheelchair • C7-C8: o Can: ▪ Full elbow extension ▪ Wrist plantar flexion ▪ Some finger control ▪ Dress, eat, and eliminate ▪ Mobility: independent in manual wheelchair • T1-T5: o Can: ▪ Full hand and finger control ▪ Use of intercostal and thoracic muscles ▪ Dress, eat, and eliminate ▪ Mobility: independent in manual wheelchair • T6-T10: o Can: ▪ Abdominal muscle control, partial-good balance with trunk muscles ▪ Dress, eat, and eliminate ▪ Mobility: independent in manual wheelchair • T11-L5: o Can: ▪ L1-L3: hip flexors and abductors ▪ L2-L4: knee extension ▪ L4-L5: knee flexion and ankle dorsiflexion ▪ Dress, eat, and eliminate ▪ Short distance-full ambulation with assistance • S1-S5: o Can: ▪ Full leg, foot, and ankle control ▪ S2-S4: innervation of perineal muscles for bowel, bladder, and sexual function ▪ Dress and eat ▪ Eliminate ▪ Ambulate independently with or without assistance o Cannot: ▪ Impaired bowel and bladder function 14. What is spinal shock? What are the clinical manifestations? • Sudden depression of reflex activity in the spinal cord (areflexia) below the level of injury • Clinical manifestations: o The muscles innervated by the part of the spinal cord segment below the level of injury are without sensation, paralyzed, and flaccid, and the reflexes are absent o Decreased BP o Bradycardia o Paralytic ileus 15. What clinical manifestations would you expect the patient with an incomplete spinal cord lesion to exhibit at different levels? What is brown Sequard syndrome? • Cross sectional view of spine: o X: gray matter ▪ U in middle: upper extremity ▪ L on outside: lower extremity o Afferent: sensation ▪ Posterior portion of cord ▪ Dorsal column o Efferent: motor ▪ Anterior portion: action is in front of us** • Central cord: damages the center portion of the cord o Upper extremities lose all sensation and function o Lower extremities still function properly o AKA: walking paraplegic** • Posterior cord: damages the posterior portion of the cord o Loss of sensation below the level of injury o Motor function remains intact • Anterior cord: damages the anterior portion of the cord o Loss of motor function below the level of injury o Sensation remains intact • Brown-Sequard syndrome: damage one side of spinal cord completely while the other side is not damaged o Affected side of body: loss of motor o Unaffected side: loss of sensation 16. What is autonomic dysreflexia? What are the clinical manifestations? What would you expect to do for a patient experiencing it? • Exaggerated reflex response by the sympathetic nervous system due to an irritating stimulus below the SCI o Disconnect between the sympathetic and parasympathetic nervous systems • Causes: o 3 big B’s: ▪ Bladder: ** a. Kinked foley** (full, distended bladder) b. UTI ▪ Bowel: a. Hardened stool ▪ Breakdown of skin: a. Pressure ulcer b. Cut, infection • Clinical manifestations: o Only occurs in SCI above T6 o Headache o Increased BP: systolic 20-40 mmHg > baseline o Above injury: ▪ Diaphoresis ▪ Goosebumps (piloerection) ▪ Headache ▪ Flushed skin ▪ Dilated pupils ▪ Bradycardia ▪ Stuffy nose ▪ Anxiety o Below injury: ▪ Cool, clammy, pale skin • Nursing intervention: o Sit patient up quickly at 90 degrees to decrease BP temporarily o Call a rapid response team and doctor o Assess BP every 2-5 minutes o Remove binding devices or clothing o Investigate 3 big B’s and correct it o Nitropaste: topical administration ▪ Contraindicated in patients who have take a phosphodiesterase inhibitor in the last 24 hr (Sildenafil (viagara), tadalafil (Cialis)) o Nifedipine: calcium channel blocker ▪ Sublingual 17. What is Cushing’s triad? What are the clinical manifestations? • Late sign of increased ICP • Irregular respirations • Bradycardia • Systolic HTN (widening pulse pressure) 18. What is nursing care of a patient with an increased ICP? • Maintain patent airway: o Discourage coughing o Cautiously suction o Auscultate lungs every 8 hr o HPB 30-45 degrees • Achieve adequate breathing pattern • Optimizing cerebral tissue perfusion: o Initiate measures to prevent Valsalva maneuver o Maintain body temp within normal limits o Admin O2 to maintain PaO2 >90 mmHg o Maintain fluid balance with NS o Avoid noxious stimuli: ▪ Excessive suctioning ▪ Painful procedures o Administer sedation to reduce agitation o Maintain CPP of 50-70 mmHg 19. Neuro pharm: • Propofol: Michael Jackson drug o Used for medically induced coma after surgery to keep the patient sedated o Has a very short half life and can be paused to wake the patient up temporarily and assess their neuro • Ceftriaxone: Ceftriaxone (ceftriaxone sodium and dextrose) Injection is an antibacterial drug used to treat conditions such as lower respiratory tract infections, skin and skin structure infections, urinary tract infections, pelvic inflammatory disease, bacterial septicemia, bone and joint infections, and meningitis. o Brain abscesses • Cefotaxime: Cefotaxime is an antibiotic used to treat a number of bacterial infections. Specifically it is used to treat joint infections, pelvic inflammatory disease, meningitis, pneumonia, urinary tract infections, sepsis, gonorrhea, and cellulitis. It is given either by injection into a vein or muscle • Vancomycin: Vancomycin is used to treat an infection of the intestines caused by Clostridium difficile, which can cause watery or bloody diarrhea. It is also used to treat staph infections that can cause inflammation of the colon and small intestines. Oral vancomycin works only in the intestines. • Ciprofloxacin: Ciprofloxacin is a fluoroquinolone (flor-o-KWIN-o-lone) antibiotic that fights bacteria in the body. It is used to treat different types of bacterial infections, including skin infections, bone and joint infections, respiratory or sinus infections, urinary tract infections, and certain types of diarrhea. • Menactra: Menactra (meningococcal conjugate vaccine) is used to prevent infection caused by meningococcal bacteria Meningococcal conjugate vaccine contains four of the most common types of meningococcal bacteria (serogroups A, C, W, and Y). Meningococcal disease is a serious infection ... • Corticosteroids (decadron): Decadron (dexamethasone) is a corticosteroid, similar to a natural hormone produced by the adrenal glands, used to treat arthritis, skin, blood, kidney, eye, thyroid, intestinal disorders, severe allergies, and asthma. Decadron is also used to treat certain types of cancer and occasionally, cerebral edema. o Craniotomy o Increased ICP • H2 antagonists: H2 blockers are a group of medicines that reduce the amount of acid produced by the cells in the lining of the stomach. They are also called 'histamine H2- receptor antagonists' but are commonly called H2 blockers. They include cimetidine, famotidine, nizatidine and ranitidine, and have various different brand names. o Craniotomy o Acute pancreatitis • Mannitol: Mannitol is a diuretic that is used to reduce swelling and pressure inside the eye or around the brain. Mannitol is also used to help your body produce more urine. mannitol is used in people with kidney failure, to remove excess water and toxins from the body. o Decrease ICP • Barbiturates: Barbiturates are a group of drugs in the class of drugs known as sedative- hypnotics, which generally describes their sleep-inducing and anxiety-decreasing effects. o Barbiturates can be extremely dangerous because the correct dose is difficult to predict. Even a slight overdose can cause coma or death. Barbiturates are also addictive and can cause a life-threatening withdrawal syndrome. o Phenobarbital o Increased ICP • Phenytoin: (Dilantin) Phenytoin is an anti-epileptic drug, also called an anticonvulsant. Phenytoin works by slowing down impulses in the brain that cause seizures. Phenytoin is used to control seizures. It does not treat all types of seizures, and your doctor will determine if it is the right medicine for you o Increased ICP o Craniotomy before and after for seizure o Therapeutic 10-20 • Glucocorticoids: Glucocorticoids are powerful medicines that fight inflammation and work with your immune system to treat wide range of health problems. Your body actually makes its own glucocorticoids. These hormones have many jobs, such as controlling how your cells use sugar and fat and curbing inflammation. • Dextran: High-molecular weight dextran is a plasma volume expander made from natural sources of sugar (glucose). It works by restoring blood plasma lost through severe bleeding. Severe blood loss can decrease oxygen levels and can lead to organ failure, brain damage, coma, and possibly death. Plasma is needed to circulate red blood cells that deliver oxygen throughout the body. o Dextran is used to treat hypovolemia (decreased volume of circulating blood plasma), that can result from surgery, trauma or injury, severe burns, or other causes of bleeding. o Hepatic encephalopathy • Muscle relaxants (baclofen): Baclofen is a muscle relaxer and an antispasmodic agent. Baclofen is used to treat muscle symptoms; such as spasm, pain and stiffness; caused by multiple sclerosis, spinal cord injuries, or other spinal cord disorders. It is given intrathecally (directly into the spinal cord) or orally (by mouth) • Cholinergics (bethanechol): Bethanechol is a parasympathomimetic (cholinergic) used for the treatment of acute postoperative and postpartum nonobstructive (functional) urinary retention and for neurogenic atony of the urinary bladder with retention. o Autonomic dysreflexia • Heparin: Heparin is an anticoagulant (blood thinner) that prevents the formation of blood clots. Heparin is used to treat and prevent blood clots caused by certain medical conditions or medical procedures. It is also used before surgery to reduce the risk of blood clots • Hydralazine: Hydralazine (Apresoline) is an antihypertensive medication used to treat high blood pressure. It is a peripheral arterial vasodilator and causes relaxation of blood vessels which carry blood away from the heart and towards the organs and tissues. • Nitroglycerine: Nitroglycerin belongs to the group of medicines called nitrates. It works by relaxing the blood vessels and increasing the supply of blood and oxygen to the heart ... • Opioids: Opioids are a class of drugs that include the illegal drug heroin, synthetic opioids such as fentanyl, and pain relievers available legally by prescription, such as oxycodone (OxyContin®), hydrocodone (Vicodin®), codeine, morphine, and many others. Metabolic 1. Hepatitis A, B, and C. what are the causes? Risk factors? How are they transmitted? Tx? How long does it take after exposure to see s/s? immune globulins? Vaccines? What happens after an exposure, is there a vaccine an or immune globulin available. Nursing care/tx? Immunity? Cure? Hep Causes Risk factors Transmission Incubation immune globulins/ vaccines Nursing care/ treatment Immunity Cure Hep A Hep A virus (HAV) Highly contagio us Overcrowded areas Homosexual and HIV population Traveling out of country Poor sanitation Fecal-oral Sexual contact Contaminate d milk, H2O, and shellfish Greatest risk occurs before s/sp 2-7 weeks Infectious until 1-2 weeks after symptoms begin Pre exposure: Hep A Vaccine Post exposure: Gamma globulin Bed rest during acute phase Small freq feedings Patient ed Average: 30 days Homologo us Acute onset, usually mild Once it runs its course, it’s gone Flu like symptoms Hep B Hep B virus (HBV) Close contact with virus Frequent exposure to blood or fluids HCP IV/drug use Multiple sex partners Blood recipient Recent STI hx Blood* Body fluids: saliva, semen, vaginal sec Sexual contact Perinatal contact route 2-5 months Preexposure: Heb B vaccine Post exposure: Hep B Immune globulin Alpha- interferon Bedrest until symptoms subside Assess psychosocial issues and concerns Protein intake 1.2-1.5 g/kg/day Severity: severe Average: 70-80 days Homologo us Carrier: yes Chronic: yes Onset: insidious Hep C Hep C virus (HCV) Silent epidemic IV drug users Multiple sex partners Pt receiving frequent blood transfusions HCP Blood Sexual contact Perinatal contact route Can live on surfaces for up to 2 weeks 14-180 days No pre or post exposure treatment Antiviral Severity: moderate Average: 50 days Second attack may indicate weak immunity or infection with another agent Carrier: yes Chronic: yes 50-80% develop chronic infection Onset: insidious Hep D HBV Pt with Hep B IV drug use Blood Sexual contact Perinatal contact 3 weeks-3 months Preexposure: Hep B vaccine Post exposure: Immune Severity: can be severe and lead to fulminant Carrier: yes Chronic: yes Onset: acute Hemophiliacs globulin hepatitis • Clinical manifestations: related to specific stages o Preicteric: before jaundice o Icteric: jaundice occurs o Posticteric: begins as jaundice disappears • Diagnostic studies: o Hepatitis profile: establishes type o LFT indicates disease stage ▪ Increased ALT ▪ Increased AST o PT prolonged o Elevated serum bilirubin o WBC elevated o Liver biopsy 2. What is ascites? Nursing care for someone with ascites? Paracentesis? • Fluid in the peritoneal cavity • Patho: o Cirrhosis with portal HTN o Splanchnic arterial vasodilation o Decrease in circulating arterial blood volume o Activate of renin-angiotensin and sympathetic nervous system and ADH o Kidneys retain water and sodium o Hypervolemia o Persistent activation of system for retention of sodium and water; ascites and edema formation o Continued arterial underfilling; cycle repeats • Nursing care: o Assess and document I/O, abdominal girth, and daily weight o Monitor respiratory status o Monitor serum ammonia, creatinine, and electrolyte levels to assess electrolyte balance, response to therapy, and indication of hepatic encephalopathy • Treatment: o Dietary modifications ▪ Reduce sodium ▪ Don’t use salt substitute without talking to doctor ▪ Use powdered, low-sodium milk and products o Pharm therapy ▪ Spironolactone: first line ▪ Complications: hypovolemia, hypokalemia, hyponatremia, encephalopathy o Bed rest o Paracentesis ▪ Reserved for ineffective ventilation or abdominal pain ▪ Cell count, albumin and total protein levels, culture, and others ▪ Albumin o Shunt use 3. Hepatic encephalopathy: what is it? Signs and symptoms? Nursing care? Treatment? • Neuropsychiatric manifestation of hepatic failure associated with portal HTN and shunting of blood from the portal venous system into the systemic circulation • CNS dysfunction frequently associated with elevated ammonia levels that produce changes in mental status, altered LOC, and coma • Signs and symptoms: o Stage 1: ▪ Normal LOC with periods of lethargy and euphoria ▪ Reversal of sleep patterns ▪ Impaired writing and ability to draw line figures o Stage 2: ▪ Increased drowsiness ▪ Disorientation ▪ Inappropriate behavior ▪ Mood swings ▪ Agitation ▪ Asterixis: bird flap ▪ Abnormal EEG with generalized slowing o Stage 3: ▪ Stuporous ▪ Difficult to arouse ▪ Sleeps most of time ▪ Marked confusion ▪ Incoherent speech ▪ Asterixis: bird flap ▪ Increased DTR ▪ Rigidity of extremities ▪ EEG markedly abnormal o Stage 4: ▪ Comatose ▪ May not respond to painful stimuli ▪ Absence of asterixis ▪ Absence of DTR ▪ Flaccid extremities ▪ EEG markedly abnormal • Nursing care: o Minimize formation and absorption of toxins, principally ammonia o Daily protein: 1.2-1.5 g/kg/day o Avoid protein restriction is possible o Protein intolerant: amino acid supplement o Small, frequent meals and 3 small snacks, late-night snack before bed ▪ High calorie, high carb, low-mod fat diet o Encourage deep breathing and position changes to prevent development of atelectasis, pneumonia, and other complications o Monitor for watery diarrhea in patients taking lactulose: indicate med overdose • Treatment: o Identify and treat underlying cause o Protein restriction o Lactulose: given to reduce serum ammonia levels ▪ Traps and expels the ammonia in the feces ▪ 2-3 soft stools per day are desirable ▪ S/e intestinal bloating and cramps, subsides in a weeks ▪ Can dilute with fruit juice o IV admin of glucose to minimize protein breakdown o Neomycin, metronidazole (Flagyl), and rifaximin (Xifaxan): reduce ammonia- forming bacteria levels in the colon o Control GI bleeds o Liver transplant 4. Why is the liver such a significant organ? • Largest organ, only organ that can regenerate • Location • Encapsulated • Right and left lobes • Metabolic functions require large amounts of blood o Arterial and venous sources • Metabolic processing • Detoxification • Plasma protein synthesis • Storage of RBC’s • Activation of Vitamin D • Removal of bacteria and worn out RBC’s (Kupffer cells) • Excretion of bilirubin and cholesterol • Production of bile salts • Alter hormone function • Metabolizes glucose 5. Cirrhosis: what is it? Causes? Signs and symptoms? Nursing care? Treatment? Complications of end stage? • Chronic hepatic disease characterized by diffuse destruction and extensive degeneration • As necrotic tissue yields to fibrosis, it alters liver structure and normal vasculature, impairs blood and lymph flow, and ultimately causes hepatic insufficiency • 4 types and causes: o Alcoholic: chronic alcoholism and malnutrition, lack of protein ▪ Fat accumulation in liver ▪ > ½ of all US cases o Post necrotic: usually a complication of viral hepatitis ▪ Can be caused by toxins ▪ Most common worldwide o Biliary: results from prolonged bile duct obstruction or inflammation o Cardiac: caused by prolonged venous congestion in the liver in right sided HF • Signs and symptoms: o Early: ▪ GI disturbances: a. Anorexia, dyspepsia, flatulence, N/V, diarrhea or constipation ▪ Fever ▪ Slight weight loss ▪ Liver/spleen enlarged ▪ Palpable liver o Late: ▪ Severe ▪ Liver failure ▪ Portal HTN ▪ Jaundice, peripheral edema, ascites develop gradually ▪ Skin lesion ▪ Hematologic disorder ▪ Endocrine problems ▪ Peripheral neuropathies ▪ Small, nodular liver o Head to toe: ▪ Telangiectasias on the cheeks (busted capillaries) ▪ Spider angiomas on the face, neck, arms, and trunk ▪ Gynecomastia ▪ Umbilical hernia ▪ Distended abdominal blood vessels ▪ Ascites ▪ Testicular atrophy ▪ Palmar erythema ▪ Clubbed fingers ▪ Thigh and leg edema ▪ Ecchymosis ▪ Jaundice • Nursing care: o Promote rest o Improving nutritional status ▪ No complications: high protein, vitamin B, A, C, K ▪ Fatty stools: water soluble vitamin A, D, E o Provide skin care o Reducing risk of injury • Treatment: o Goal: remove or alleviate underlying cause, prevent further damage o Rest o Vitamin and nutritional supplement o Special caution with drug therapy o No alcohol o No ASA • Complications of end stage liver disease 6. Patient teaching for someone diagnosed with alcoholic cirrhosis • NO MORE ALCOHOL • Referral to AA, psych care, or counseling • Avoid consumption of raw shellfish • Sodium restriction • Rest • Lifestyle changes 7. Labs related to liver function • Serum bilirubin: 0.1-0.4 mg/dL • Urine bilirubin: 0.3-1 mg/dL • Total serum protein: 7-7.5 g/dL • Serum albumin: 3.5-5 g/dL • Albumin: 4-6 • PT: 11-12.5 seconds • Serum alkaline phosphatase: 30-120 • Serum aminotransferase: o AST: 10-40 o ALT: 8-40 • Ammonia: 15-45 mcg/dL • Cholesterol: < 200 o HDL: <100 o LDL: ▪ Male: 35-70 ▪ Female: 35-85 o Triglycerides: 8. Acute pancreatitis: what is it? Signs and symptoms? Nursing care? Treatment? • Self-digestion of the pancreas by its own proteolytic enzymes, trypsin, • Interstitial: characterized by a lack of pancreatic parenchymal necrosis with diffuse enlargement of the gland due to inflammatory edema • Signs and symptoms: o Severe abdominal pain** o Abdominal tenderness and back pain ▪ Increased tension in pancreatic capsule o Pain accompanied by: ▪ Abdominal distention ▪ Poorly defined, palpable abdominal mass ▪ Decreased peristalsis ▪ Vomiting o Abdominal guarding o Rigid, boardlike abdomen o Ecchymosis in the flank or around the umbilicus o Fever, jaundice, mental confusion, and agitation o Hypotension o Hypovolemia and shock o Respiratory distress and hypoxia • Nursing care: o Acute: ▪ NPO ▪ No odors ▪ NG suctioning to reduce N/V and abdominal distention and paralytic ileus ▪ Pain management a. Analgesia b. Opioids ▪ H2 antagonists: cimetidine and ranitidine ▪ PPIs: pantoprazole ▪ IV fluids ▪ TPN o Chronic: ▪ Oral feedings low in fat and protein after acute phase is over ▪ No caffeine or alcohol o Improving breathing pattern: ▪ Semi fowlers ▪ Frequent changes ▪ Pulmonary assessment: pulse ox and ABGs ▪ Cough and deep breathing o Improving nutritional status o Maintaining skin integrity • Treatment: o Prevent and relieve symptoms o Withhold oral intake o Enteral feedings o ICU: ▪ Insulin if hyperglycemia ▪ Correction of fluid and blood loss and low albumin levels ▪ Biliary drainage 9. Esophageal varices: what is it? Signs and symptoms? Nursing care? Treatment? • Esophagus vessels weaken and eventually rupture causing bleeding • Signs and symptoms: o Hematemesis o Melena o General deterioration in mental or physical status o History of alcohol abuse o Signs of shock • Nursing care: o Avoid bleeding o Avoid alcohol o Control cough • Treatment: o Treat URI promptly o Prophylactic treatment with beta blockers o Emergent treatment if bleeding o Possible blood transfusion o Vasopressin initially 10. Lactulose: synthetic sugar used to treat: • Constipation • Decrease ammonia levels in patients with liver disease • Side effects: o Diarrhea o N/V o Bloating o Gas, belching o Stomach pain or discomfort [Show More]
Last updated: 11 months ago
Preview 1 out of 29 pages
Instant download
Instant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 19, 2023
Number of pages
29
Written in
Additional information
This document has been written for:
Uploaded
Jun 19, 2023
Downloads
0
Views
103


.png)