*NURSING > STUDY GUIDE > Rasmussen College: NUR 4323 /MDC4 Final Study Guide LATEST 2021/2022,100% CORRECT (All)
Rasmussen College: NUR 4323 /MDC4 Final Study Guide LATEST 2021/2022,100% CORRECT
Document Content and Description Below
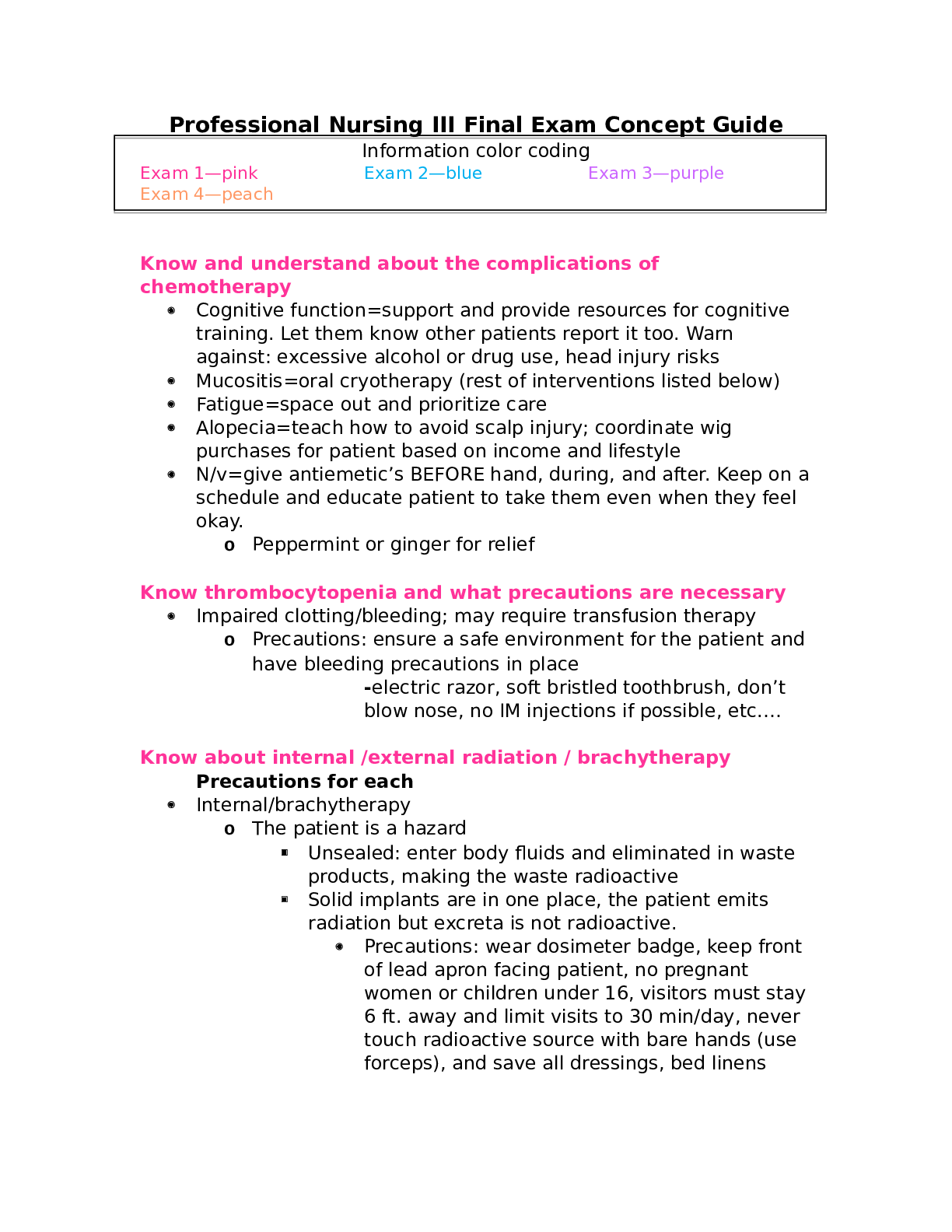
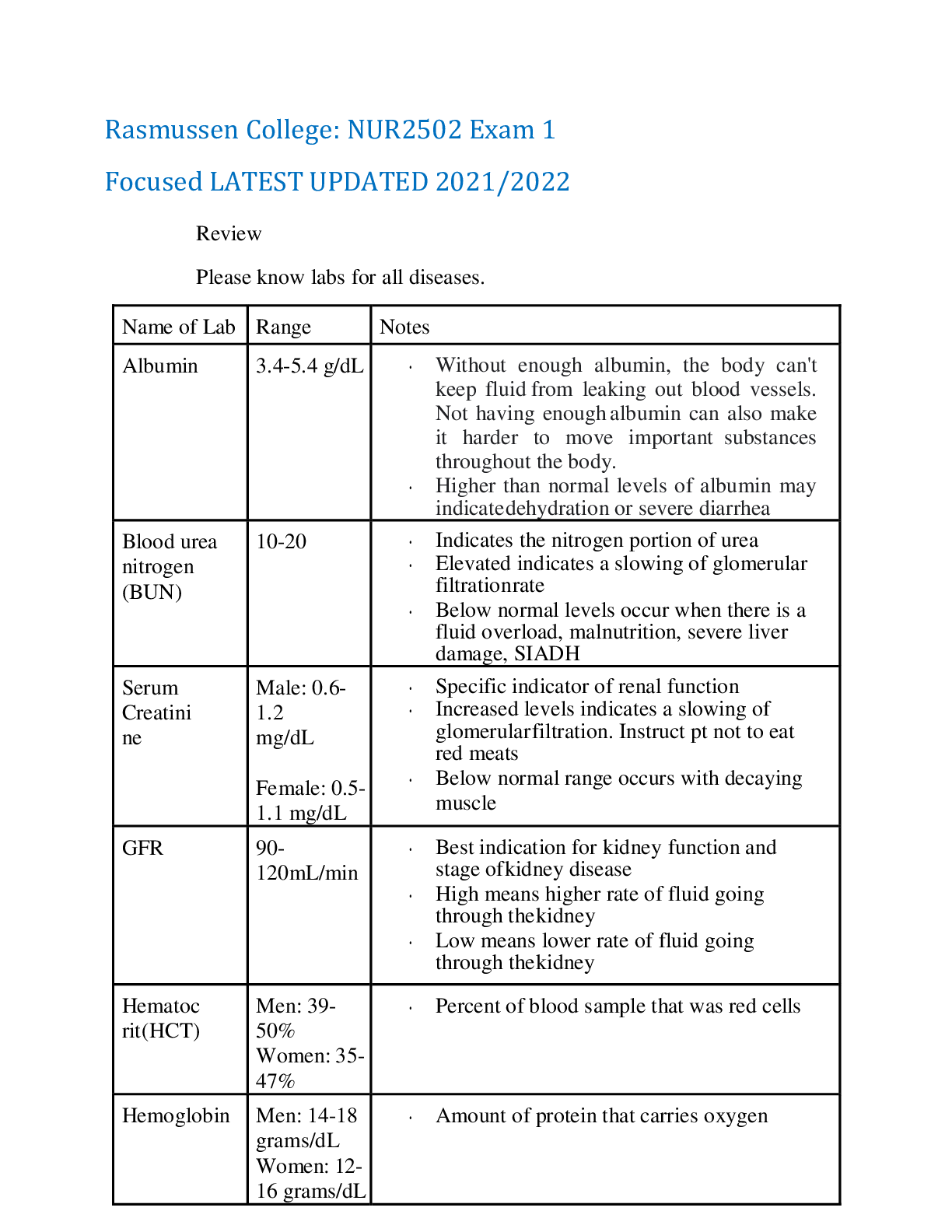
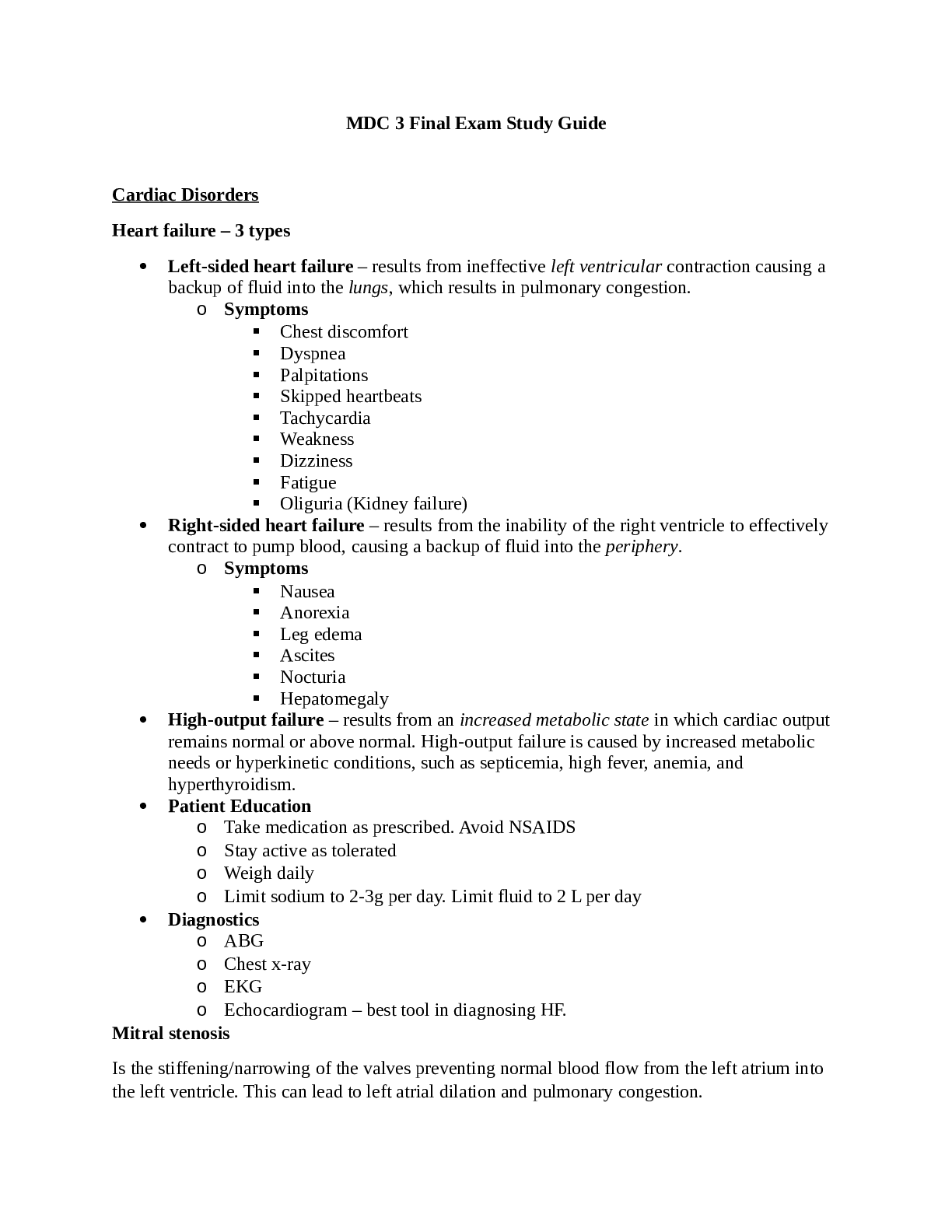
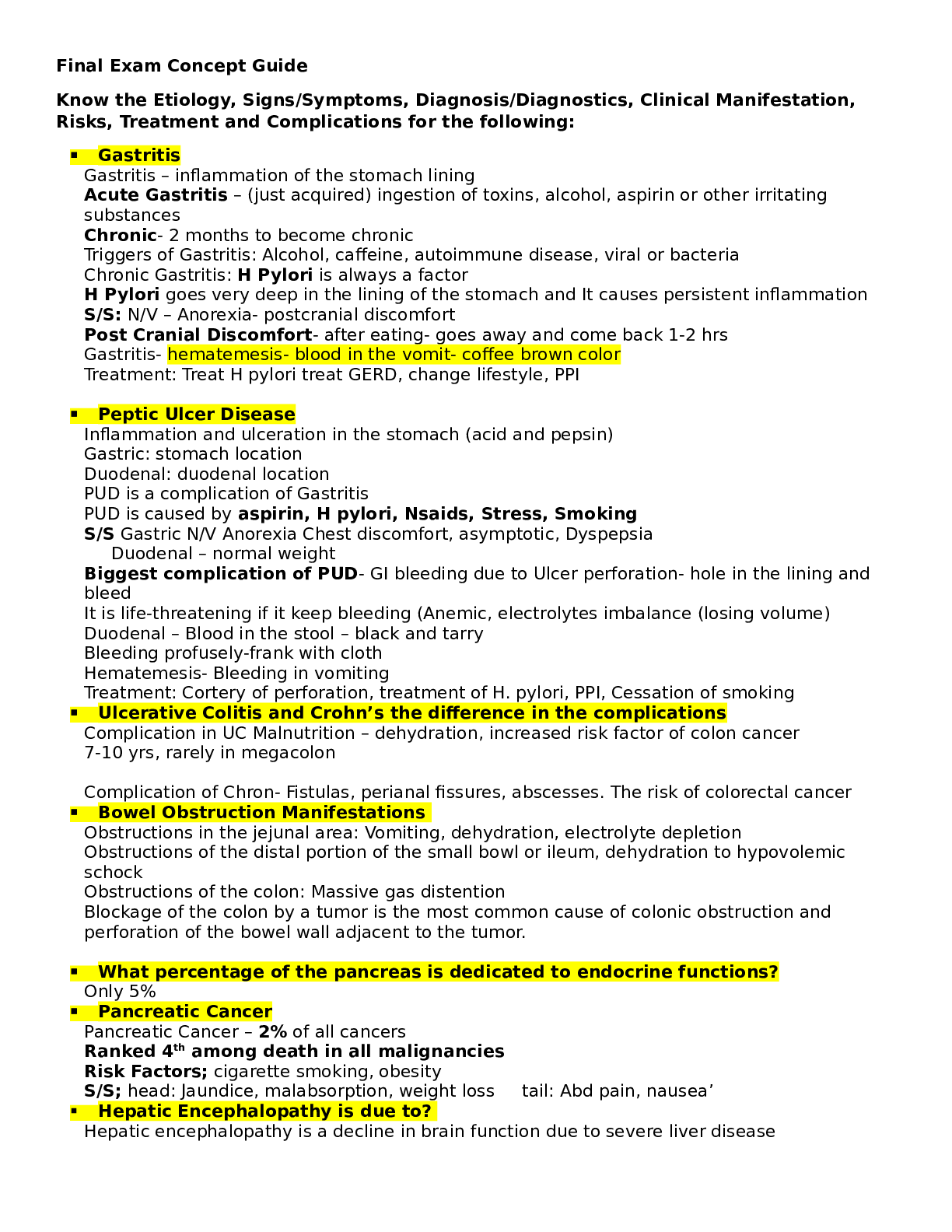
Rasmussen College: NUR 4323 /MDC4 Final Study Guide LATEST 2021/2022 Exam Notes MDC4 Final Parkland Formula a) 4ml x % BSA x weight (kg)= volume of fluid that needs to be infused b) ½ of the to... tal volume of fluid in first 8 hours c) Last half in 16 hours MAP Calculation a) MAP= 1/3 * SBP + 2/3 * DBP Treatment for frostbite a) Rewarming the skin a. Rewarm the area using a warm-water bath for 15 to 30 minutes b. Skin may turn soft and look red or purple c. You may be encouraged to gently move the affected area as it rewarms. b) Oral pain medicine a. The rewarming process can be painful c) Protecting the injury a. Once the skin thaws, loosely wrap the area with sterile sheets, towels, or dressing to protect the skin. b. May have to protect fingers and toes as they thaw by gently separating them from each other c. You may need to elevate the affected area to reduce swelling d) Debridement (removal of damaged tissue) a. To heal properly, frostbitten skin needs to be free of damaged, dead or infected tissue. e) Whirlpool therapy or physical therapy a. Hydrotherapy can aid healing by keeping skin clean and naturally removing dead tissue b. Pt may be encouraged to move the affected area f) Antibiotics a. If the skin or blisters appear to be infected, the doctor may prescribe oral antibiotics g) TPA a. IV injection of a drug that helps restore blood flow (thrombolytic) such as TPA. b. TPA lowers the risk of amputation c. These drugs can cause serious bleeding and are typically used only in the most serious situations and within 24 hours of exposure. h) Wound care i) Surgery a. Severe frostbite patients may need surgery or amputation to remove dead or decaying tissue. j) Hyperbaric oxygen therapy a. Some patients show improved symptoms after this therapy, but more study is needed. Treatment and differences of heat stroke and heat exhaustion a) Heat exhaustion a. Symptoms i. General weakness, increased heavy sweating, a weak but faster HR, N/V, possible fainting, pale/cold/clammy skin b. Treatment i. Stop physical activity, transfer to cool space ii. Cooling measures (ice water bath, mist skin with water, ice packs, special cooling blanket) iii. Rehydration therapy b) Heat stroke a. Symptoms i. Elevated body temperature above 103 F (39.4 C), rapid and strong HR, loss or change of consciousness, hot, red, dry, or moist skin b. Treatment i. Oxygen therapy, IV lines, urinary catheter, continuous cooling (Ice bath, mist skin with water, ice packs, special cooling blanket), benzodiazepine if shivering occurs, monitor for multi system organ dysfunction syndrome and electrolyte imbalances. Priority assessment in triage a) ABC’s Temperature reduction strategies a) Ice bath, mist skin with water, ice packs, special cooling blanket Skin injury related to frostbite a) Frostbite occurs in several stages: a. Frostnip i. Mild form of frostbite- does not permanently damage the skin ii. Continued exposure leads to numbness in the affected area iii. As the skin warms, the patient may feel pain and tingling. b. Superficial Frostbite i. Appears as reddened skin that turns white or pale ii. The skin may begin to feel warm- a sign of serious skin involvement iii. If you treat frostbite with rewarming at this stage, the surface of skin may appear mottled and you may notice stinging, burning, and swelling iv. Fluid-filled blisters may appear 12 to 36 hours after rewarming the skin c. Deep (Severe) Frostbite i. Skin turns white or bluish grey, and the patient may experience numbness, losing all sensation of cold, pain, or discomfort in the affected area. ii. Joints/muscles may no longer work iii. Large blisters form 24-48 hours after rewarming. Afterwards, the area turns black and hard as the tissue dies. Rationale for arrythmias in hypothermia a) The risk of cardiac arrest increases as the core temperature drops below 32°C, and increases substantially if the temperature reaches less than 28°C (Brown et al. 2012). At this level, a severe depression of critical body functions occurs Blunt chest injury assessment a) Primary assessment treatments a. Based on the mechanism of injury, consider manual stabilization of the cervical spine until a more complete spinal exam can be accomplished. Establish and maintain a patent airway while determining the patient's level of consciousness using the AVPU scale. If the patient is not fully awake or alert, manual airway positioning and basic airway adjuncts such as an OPA or NPA may be needed. Suctioning an airway filled with blood or emesis may be necessary. b) Seal chest wounds a. Any open chest wound should be sealed as soon as it is found, using the palm of a gloved hand at first, followed by an occlusive dressing. c) Relieve tension pneumothorax a. Tachypnea, hypopnea (shallow breathing) and accessory muscle use are key indicators of respiratory distress or failure. Expose the chest and auscultate lung fields immediately. Diminished sounds over one side may indicate a loss of lung capacity, either from a hemothorax, pneumothorax or both. b. Inspect the neck and chest area. Jugular venous distension may indicate greater than normal pressure within the chest cavity, possibly related to a developing tension pneumothorax. Hyperinflation of the chest over one side is another sign related to a tension pneumothorax. If the patient's mental status worsens and blood pressure falls, a decompression of the tension pneumothorax using a long, large gauge angiocatheter is needed to relieve the excessive pressure in the chest. d) Control hemorrhage a. Control any major external bleeding immediately with direct pressure. It will be difficult to create a pressure dressing, as is more commonly seen with extremity injuries. Manual pressure may be needed to stop the bleeding. Recognize that the chance of active bleeding inside the chest is significant and emergent transport to a trauma center is needed. e) Package for transport a. Unless there are clear signs of neurological deficit, avoid placing the patient with penetrating chest trauma in spinal precautions. Being supine may worsen respiratory distress and delay transport. b. In general, on-scene management of chest trauma should be done with BLS interventions, with the intent to begin transport to a trauma center as soon as feasible. With the exception of the needle decompression, other advanced level procedures are best done while en route. Addressing ventilator alarms a) Should never be turned off or ignored during mechanical ventilation b) The major alarms on the ventilator indicate either a high pressure or low exhaled volume c) If the alarm cannot be determined, ventilate the patient manually with a resuscitation bag until the problem is corrected by another health care professional Fractured ribs and flail chest a) Rib fracture a. Important info i. The most common cause is blunt trauma from a fall or car accident. Trauma can increase your risk for organ damage when your rib is fractured. ii. Older age, osteoporosis, or a tumor can increase your risk for rib fractures. iii. A stress fracture can happen in your upper or middle ribs. Stress fractures can happen when you have a forceful long-term cough. They can also be caused by forceful athletic movements, such as in golf, throwing, or rowing. iv. A condition called flail chest occurs if 3 or more of your ribs are broken in 2 or more places. This condition may make it hard for you to breathe. b. Signs and symptoms i. Chest wall pain that worsens when you breathe, move, or cough ii. Bruising or swelling near your injury iii. Shortness of breath or difficulty taking a deep breath c. Treatment i. Medications 1. NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. 2. Prescription pain medicine may be given. 3. Intercostal nerve block may be given to numb the injured area for about 6 hours. It is given as a shot between 2 of your ribs in the fractured area. You may need this if your pain continues or is getting worse even after you take oral pain medicines. ii. Surgery may be needed if your rib fracture is severe or several ribs are badly broken. Surgery is often needed for a flail chest. d. Management of symptoms i. Take deep breaths and cough 10 times each hour. This will decrease your risk for a lung infection. Hug a pillow on your injured side to decrease pain while you take deep breaths. Take a deep breath and hold it for as long as you can. Let the air out and then cough. Deep breaths help open your airway. You may be given an incentive spirometer to help you take deep breaths. Put the plastic piece in your mouth and take a slow, deep breath, then let the air out and cough. Repeat these steps 10 times every hour. ii. Rest and limit activity as directed. Do not pull, push, or lift objects. Start to do more as your pain decreases. iii. Apply ice on your chest near your fractured rib for 15 to 20 minutes every hour or as directed. Use an ice pack, or put crushed ice in a plastic bag. b) Flail chest Cover it with a towel. Ice helps prevent tissue damage and decreases swelling and pain. a. an injury that occurs typically following a blunt trauma to the chest. When three or more ribs in a row have multiple fractures within each rib, it can cause a part of your chest wall to become separated and out of sync from the rest of your chest wall. b. The chest moving unevenly between the separated part and rest of the chest is often the most definitive sign that you have a flail chest. The area of your chest that’s been traumatized will draw in when you breathe in, while the rest of your chest expands outward. When you breathe out, the affected area will expand out while the rest of your chest draws in. c. Treatment i. Your doctors will need to protect your lungs while ensuring that you can breathe adequately. They will give you an oxygen mask to assist your breathing and give you medication to help with your pain. ii. In more serious cases where there is associated underlying lung injury, you may need to be put on a mechanical ventilator in order to keep your chest cavity stable. It’s possible that surgery will be required, depending on the extent of injury and risks versus benefits of surgery. Chest injury a) Patients may be asymptomatic at first and can later develop various degrees of respiratory failure and possibly pneumonia b) These patients often have decreased breath sounds or crackles and wheezes over the affected area c) Other symptoms include bruising over the injury, dry cough, tachycardia, tachypnea, and dullness to percussion. d) At first the chest x ray may show no abnormalities but a hazy opacity in the lobes or parenchyma may develop over several days e) Management includes maintenance of ventilation and gas exchange Pneumothorax a) Collapsed lung b) Signs and symptoms a. sudden chest pain and shortness of breath. c) Causes a. Chest injury. i. Any blunt or penetrating injury to your chest can cause lung collapse. Some injuries may happen during physical assaults or car crashes, while others may inadvertently occur during medical procedures that involve the insertion of a needle into the chest. b. Lung disease. c. Ruptured air blisters. i. Small air blisters (blebs) can develop on the top of the lungs. These blebs sometimes burst — allowing air to leak into the space that surrounds the lungs. d. Mechanical ventilation. i. A severe type of pneumothorax can occur in people who need mechanical assistance to breathe. The ventilator can create an imbalance of air pressure within the chest. The lung may collapse completely. d) Diagnosis a. chest X-ray. In some cases, a computerized tomography (CT) scan may be needed to provide more-detailed images. Ultrasound imaging also may be used to identify a pneumothorax. e) Treatment a. Observation i. If only a small portion of your lung is collapsed, your doctor may simply monitor your condition with a series of chest X-rays until the excess air is completely absorbed and your lung has re-expanded. This may take several weeks. b. Needle aspiration or chest tube insertion c. Nonsurgical repair: i. Using a substance to irritate the tissues around the lung so that they'll stick together and seal any leaks. This can be done through the chest tube, but may be done during surgery. ii. Drawing blood from your arm and placing it into the chest tube. The blood creates a fibrinous patch on the lung (autologous blood patch), sealing the air leak. iii. Passing a thin tube (bronchoscope) down your throat and into your lungs to look at your lungs and air passages and place a one-way valve. The valve allows the lung to re-expand and the air leak to heal. d. Surgery: i. Sometimes surgery may be necessary to close the air leak. In most cases, the surgery can be performed through small incisions, using a tiny fiber-optic camera and narrow, long-handled surgical tools. The surgeon will look for the leaking area or ruptured bleb and close it off. ii. Rarely, the surgeon will have to make a larger incision between the ribs to get better access to multiple or larger air leaks. ARDs a) Overview a. Acute respiratory distress syndrome (ARDS) occurs when fluid builds up in the tiny, elastic air sacs (alveoli) in your lungs. The fluid keeps your lungs from filling with enough air, which means less oxygen reaches your bloodstream. This deprives your organs of the oxygen they need to function. b) Symptoms a. Severe shortness of breath b. Labored and unusually rapid breathing c. Low blood pressure d. Confusion and extreme tiredness c) Treatment a. Oxygen i. Supplemental oxygen. For milder symptoms or as a temporary measure, oxygen may be delivered through a mask that fits tightly over your nose and mouth. ii. Mechanical ventilation. Most people with ARDS will need the help of a machine to breathe. b. Fluids i. Carefully managing the amount of intravenous fluids is crucial. Too much fluid can increase fluid buildup in the lungs. Too little fluid can put a strain on your heart and other organs and lead to shock. c. Medication i. People with ARDS usually are given medication to: 1. Prevent and treat infections, Relieve pain and discomfort, Prevent blood clots in the legs and lungs, Minimize gastric reflux, and Sedate d. pulmonary rehabilitation. i. Many medical centers now offer pulmonary rehabilitation programs, which incorporate exercise training, education and counseling to help you learn how to return to your normal activities and achieve your ideal weight. Pulmonary Embolism a) Overview a. a blockage in one of the pulmonary arteries in your lungs. In most cases, pulmonary embolism is caused by blood clots that travel to the lungs from deep veins in the legs or, rarely, from veins in other parts of the body (deep vein thrombosis). b) Symptoms a. Common signs and symptoms include: i. Shortness of breath. This symptom typically appears suddenly and always gets worse with exertion. ii. Chest pain. You may feel like you're having a heart attack. The pain is often sharp and felt when you breathe in deeply, often stopping you from being able to take a deep breath. It can also be felt when you cough, bend or stoop. iii. Cough. The cough may produce bloody or blood-streaked sputum. b. Other signs and symptoms that can occur with pulmonary embolism include: i. Rapid or irregular heartbeat, Lightheadedness or dizziness, Excessive sweating, Fever, Leg pain or swelling, or both, usually in the calf caused by a deep vein thrombosis, and Clammy or discolored skin (cyanosis) c) Prevention a. Blood thinners (anticoagulants). i. These medications are often given to people at risk of clots before and after an operation — as well as to people admitted to the hospital with medical conditions, such as heart attack, stroke or complications of cancer. b. Compression stockings. i. Compression stockings steadily squeeze your legs, helping your veins and leg muscles move blood more efficiently. c. Leg elevation. i. Elevating your legs when possible and during the night also can be very effective. d. Physical activity. i. Moving as soon as possible after surgery can help prevent pulmonary embolism and hasten recovery overall. This is one of the main reasons your nurse may push you to get up, even on your day of surgery, and walk despite pain at the site of your surgical incision. e. Pneumatic compression. i. This treatment uses thigh-high or calf-high cuffs that automatically inflate with air and deflate every few minutes to massage and squeeze the veins in your legs and improve blood flow. d) Treatment a. Medications: i. Blood thinners (anticoagulants). These drugs prevent existing clots from enlarging and new clots from forming while your body works to break up the clots. Heparin is a frequently used anticoagulant that can be given through the vein or injected under the skin. It acts quickly and is often overlapped for several days with an oral anticoagulant, such as warfarin, until it becomes effective, which can take days. ii. Clot dissolvers (thrombolytics). While clots usually dissolve on their own, sometimes thrombolytics given through the vein can dissolve clots quickly. Because these clot-busting drugs can cause sudden and severe bleeding, they usually are reserved for life-threatening situations. b. Surgical and other procedures: i. Clot removal. If you have a very large, life-threatening clot in your lung, your doctor may suggest removing it via a thin, flexible tube (catheter) threaded through your blood vessels. ii. Vein filter. A catheter can also be used to position a filter in the body's main vein (inferior vena cava) that leads from your legs to the right side of your heart. This filter can help keep clots from going to your lungs. This procedure is typically reserved for people who can't take anticoagulant drugs or when they have had recurrent clots despite use of anticoagulants. Assessment of LOC Ways to minimize the risk of autonomic dysreflexia a) a syndrome that leads to a sudden onset of high blood pressure and can be accompanied by low heartbeats, is not uncommon. a. In fact, about fifty percent of individuals with a spinal cord injury get it. It is most common in individuals with spinal cord injuries, at, or above the thoracic (T6) nerves of the spine or above. b) When the skin or bladder is irritated, signals are sent to the spinal cord, which triggers a reflex action. This reflex tightens blood vessels below the injury, causing blood pressure to rise. c) Prevention a. Sit up when possible i. Sitting up helps blood move to lower parts of the body and helps ease blood pressure. b. Take off tight clothes i. At times, autonomic dysreflexia can be caused by skin conditions. c. Medications i. The most commonly used drugs are nifedipine (immediate release form) as well as nitrates. Other commonly used agents are prazosin, captopril, terazosin, mecamylamine, diazoxide, and phenoxybenzamine. d. Use the bathroom regularly i. While an individual's bladder will still store urine from their kidneys, their brain may not be able to control their bladder because of the injury. This can make patients more susceptible to urinary tract infections. e. Watch for bladder infection signs i. An autonomic dysreflexia episode that remains unexplained by most of the other causes can also be due to a urinary tract infection. Spinal shock injuries and how to assess a) characterized by the temporary reduction or loss of reflexes following a spinal cord injury. b) Symptoms a. Altered body temperature b. Skin color and moisture changes (such as dry and pale skin) c. Abnormal perspiration function (decreased or increased sweating, flushing) d. Increased blood pressure and slowed heart rate e. Irregularities in the musculoskeletal system f. Altered sensory response g. Unusual urinary bladder and GI tract functions (overflow and incontinence) h. Irregular vasomotor response i. Depressed genital reflexes Seizure care a) Mark the seizure start time. b) If a patient is standing, lay them to the ground and roll them to the side. If the patient is in bed, roll them to the side c) The patient can never swallow their tongue. Never place anything in patient mouth or try to open their mouth. This can compromise the airway or cause more harm to the patient. d) Never hold the patient down or try to stop their movements. This can cause injury to the patient. Instead, protect the patient from hitting hard surfaces with soft puddings like pillows. e) By rolling the patient to the sides, you may achieve a patent airway. f) Administer 100% oxygen g) Check oxygen saturation. It may be below 90 due to apnea. The patient may turn blue on the lips and fingers. Do not panic! h) Patient will have oral secretions. Suction at bedside to keep the airway patent. i) If help is available, establish an IV- line for possible IV medication administration if the seizure continues for a long time (Status epilepticus). You do not have to have a physician order to start an IV line in this case. j) Put the side rails up to prevent falls k) Pad the bed of any patient expected to get seizures. Injuries caused by unpadded bed can count against you. l) Your drug of choice during seizure is Ativan IV push. Homonymous hemianopsia and how to deal with deficit a) a condition in which a person sees only one side -- right or left -- of the visual world of each eye and results from a problem in brain function rather than a disorder of the eyes themselves. b) Treatment a. Strategies to improve reading ability: i. Use a straight edge to direct the eyes to the next line of text. ii. Work on willingly increasing the size of small eye movements as words are read along the line of text. The goal is to capture each word in the field of vision and to recognize it as a whole before reading it. iii. Place your hand at the edge of a page to make it easy to determine the margin of a page. iv. Hold the text at a 45- to 90-degree angle so that reading is done vertically rather than horizontally. People with a right hemianopsia should read down, while those with a left hemianopsia should read up. In each case, this will keep the next line of text within the available field of vision. b. Strategies to improve navigating the environment: i. When moving through the environment, learn to direct the eyes toward the good visual field. ii. When walking into a new environment, pause and move your head from one side to another. Observe where objects and people are located. Think about painting a picture of what you see in your brain. Practicing this, particularly in the 6 months after vision loss, can help train your brain to do this automatically. iii. When looking for objects in the blind field consciously make large eye movements to that side and then let the eyes come back to the object. iv. When walking, let a partner walk on the blind side and provide his or her arm for guidance. v. When in group situations, situate people in the good field of vision as much as possible. vi. When in a theater, sit far over to the blind side so that the action takes place in the normal visual field. vii. Play real-life (not computer-based) card games and do crossword puzzles to regain coordination between vision and touch. viii. Do word search or picture search puzzles to improve eye scanning at near distances. c. Other treatment i. Prisms on glasses may help to expand the area for central vision. A prism can displace images of objects into the field of vision. ii. Some makers of computer-assisted programs claim to promote recovery of the entire field of vision. However, there are no proven studies showing such programs are effective. In addition, they are very expensive. iii. Driving a motor vehicle is hazardous for many people with homonymous hemianopsia, particularly if other neurological problems are present. Practice on a driving simulator offers a chance to regain driving skills and allows an instructor to determine if the patient is able to drive again. Prevention of myasthenic and cholinergic crises a) Myasthenic crisis a. It is a complication of a condition known as myasthenia gravis, a chronic autoimmune disorder that is characterized by rapid fatigue and weakness of voluntarily controlled muscles. b. Symptoms i. weight loss, difficulty speaking or breathing, trouble chewing, trouble swallowing, a weak cough with increased secretions (saliva or mucus), weak tongue, feeling unrested during the day, daytime fatigue, frequent nighttime awakenings, morning headaches, and the skin around your neck, between your ribs, or on your abdomen pulls in when you breathe. c. Prevention i. Take anticholinesterase medication as prescribed ii. Avoid respiratory infections iii. Maintain strength and weight with proper nutrition iv. When exercising, plan intermittent rest periods v. Reduce emotional stress vi. All currently used medications should be disclosed to your doctor to help avoid medications that interfere with myasthenia gravis treatment b) Cholinergic crisis a. also referred to as mnemonic “SLUDGE syndrome,” is a clinical condition that occurs as a result of the overstimulation of muscarinic and nicotinic receptors at the neuromuscular synapses and junctions due to an excess of acetylcholine. b. Symptoms i. stimulation of skeletal muscle (due to nicotinic acetylcholine receptor stimulation), stimulation of the salivary glands, stimulation of the pupillary constrictor muscles, vomiting, smooth muscle tone changes causing gastrointestinal problems, like cramping, contraction of the detrusor muscles, relaxation of the internal sphincter muscle of urethra, stimulation of the lacrimal glands. c. Risks (Prevention= reducing the risks) i. sufferers after general anesthesia who received high doses of acetylcholinesterase inhibitors (a chemical which inhibits the acetylcholinesterase enzyme from breaking down acetylcholine) to reverse the effects of neuromuscular blocking agents ii. people with myasthenia gravis on the medical treatment with high dose acetylcholinesterase inhibitors. iii. exposure to a chemical substance that causes inactivation of acetylcholinesterase (the primary cholinesterase in the human body). Examples of such substances are nerve gas such as – tabun (the first nerve agent chemical weapon to be discovered), sarin (a highly toxic synthetic organophosphorus compound), soman and other organophosphates including insecticides and pesticides; Parkinson’s and mobility interventions a) nursing interventions a. Assess neurological status. b. Assess ability to swallow and chew. c. Provide high-calorie, high-protien, high-fiber soft diet with small, frequent feedings. d. Increase fluid intake to 2000 mL/day. e. Monitor for constipation. f. Promote independence along with safety measures. g. Avoid rushing the client with activities. h. Assist with ambulation and provide assistive devices. i. Instruct client to rock back and forth to initiate movement. j. Instruct the client to wear low-heeled shoes. k. Encourage the client to lift feet when walking and avoid prolonged sitting. l. Provide a firm mattress, and position the client prone, without a pillow, to facilitate proper posture. m. Instruct in proper posture by teaching the client to hold the hands behind the back to keep the spine and neck erect. n. Promote physical therapy and rehabilitation. o. Administer anticholinergic medications as prescribed to treat tremors and rigidity and to inhibit the action of acetylcholine. p. Administer antiparkinsonian medications to increase the level of dopamine in the CNS. q. Instruct the client to avoid foods high in vitamin B6 because they block the effects of antiparkinsonian medications. r. Instruct the client to avoid monoamine oxidase inhibitors because they will precipitate hypertensive crisis. Management of Guillain-Barre syndrome a) an autoimmune disease in which there is an acute inflammation of the spinal and cranial nerves manifested by motor dysfunction that predominates over sensory dysfunction. b) Symptoms a. often begins with tingling and weakness starting in your feet and legs and spreading to your upper body and arms b. Prickling, pins and needles sensations in your fingers, toes, ankles, or wrists c. Weakness in your legs that spreads to your upper body d. Unsteady walking or inability to walk or climb stairs e. Difficulty with facial movements, including speaking, chewing, or swallowing f. Double vision or inability to move eyes g. Severe pain that may feel achy, shooting or cramp like and may be worse at night h. Difficulty with bladder control or bowel function i. Rapid heart rate j. Low or high blood pressure k. Difficulty breathing c) Treatment a. Plasma exchange (plasmapheresis) i. The liquid portion of part of your blood (plasma) is removed and separated from your blood cells. The blood cells are then put back into your body, which manufactures more plasma to make up for what was removed. Plasmapheresis may work by ridding plasma of certain antibodies that contribute to the immune system's attack on the peripheral nerves. b. Immunoglobulin therapy i. Immunoglobulin containing healthy antibodies from blood donors is given through a vein (intravenously). High doses of immunoglobulin can block the damaging antibodies that may contribute to Guillain-Barre syndrome. c. medication to relieve pain, which can be severe and prevent blood clots, which can develop while you're immobile d) Therapy/PT a. Movement of your arms and legs by caregivers before recovery, to help keep your muscles flexible and strong b. Physical therapy during recovery to help you cope with fatigue and regain strength and proper movement c. Training with adaptive devices, such as a wheelchair or braces, to give you mobility and self-care skills e) Recovery a. After the first signs and symptoms, the condition tends to progressively worsen for about two weeks b. Symptoms reach a plateau within four weeks c. Recovery begins, usually lasting six to 12 months, though for some people it could take as long as three years Assessment signs for meningitis a) Signs and Symptoms a. Early symptoms will be similar to the flu, and they can develop over a matter of hours or even days. b. sudden high fever, stiff neck, severe headache, nausea or vomiting, confusion and difficulty concentrating, seizures, sleepiness or difficulty waking, sensitivity to light, no appetite or thirst, and skin rash b) Kernig’s sign a. To look for Kernig’s sign lie face up and flex your knee and hip in a 90˚ angle while someone else slowly extends your knee. i. If you feel either resistance or pain, see a doctor right away for treatment. c) Brudzinski sign a. To check for the Brudzinski sign, lie flat on your back. Your doctor will place one hand behind your head, and another on your chest to prevent you from rising. Then, your doctor will lift your head, bringing your chin to your chest. i. A positive Brudzinski sign occurs when this causes flexion of the hips. d) A third sign used to diagnose meningitis is called nuchal rigidity. Nuchal rigidity is an inability to flex the neck forward due to rigidity of the neck muscles. Post-operative breathing interventions a) cough and deep breathe every two to four hours. a. breathe deeply four times in a row and then coughing after the last deep breath in. b) incentive spirometer is a breathing toy used to exercise the lungs. a. Encourage to take slow, deep breaths when using the incentive spirometer. c) Encourage your child to be as active as allowed. a. Your child will be asked to move around in bed and to sit up as much as he/she can. The head of the bed can be raised to help your child breathe better. Turning your child from side to side helps to prevent secretions from staying in one place in the lungs. Sometimes chest physiotherapy (CPT) may be ordered for your child. d) Encourage your child to get out of bed and walk as soon as allowed by the doctor. Different types of wound drainage and wound assessment a) Types a. Serous Drainage i. A pale yellow or transparent fluid found most frequently inside the body’s cavities 1. Examples blisters, Seromucous inflammation, and Serous pulmonary alveolitis b. Sanguineous drainage i. involves solely blood that comes from a fresh wound. It usually is of a bright red color seen in partial -thickness and full-thickness wounds c. Serosanguineous drainage i. pink exudate d. Seropulent drainage i. It is also commonly named ‘’seropus’’ that is similar to serum when it comes to consistency but a bit more cloudier, yellowish in color. e. Purulent drainage i. It is often yellow, green or even brown in color, has unpleasing smell and is a sure sign that there is an infection b) Assessment a. Size, width, length and depth i. important to be measured and documented so that the progress of the wound can be measured over time. b. Undermining and tunnelling c. Wound bed tissue type i. A wound can consist of different tissue types, which can be categorized by name and/or colour. Record the percentages of the differing tissue types. d. Wound edge (margin) i. can indicate the stage of healing and provide information as to the wound aetiology. The margin type that is good to see is skin that is smooth and adheres firmly to the wound bed. Lab values of note: Sodium, Hgb, Platlet, Creatinine a) Sodium 135-145 a. Low: use of diuretics, diarrhea, adrenal insufficiency b. High: kidney disease, dehydration, Cushing’s syndrome b) Hgb F: 12.1-15.1 M: 13.8-17.2 a. Low: Iron, vit D3, or folate deficiency, bone marrow damage b. High: dehydration, kidney or heart disease c) Platelet 150,000-400,000 a. Low: viral infection, lupus, pernicious anemia (B12 deficiency), leukemia, chemo b. High: leukemia, bone marrow abnormalities, inflammatory conditions d) Creatinine 0.8-1.4 a. Low: low muscle mass, malnutrition b. High: low kidney function Understand the role of the Medical Reserve Corp a) a national network of volunteers, organized locally to improve the health and safety of their communities. b) MRC volunteers include medical and public health professionals, as well as other community members without healthcare backgrounds c) MRC units prepare for and respond to natural disasters, such as wildfires, hurricanes, tornados, blizzards, and floods, as well as other emergencies affecting public health, such as disease outbreaks. Understand the role of DMAT a) Disaster Medical Assistance Teams b) staffed with medical professionals and para-professionals who can help area health systems respond by providing expert patient care. c) members may be called on to help hospitals and healthcare facilities serve the needs of their patients, support medical sites and shelters, and more. Medication, use of Tagamet in burn injury a) pain medication, antibiotics, anti-anxiety medication, topical products for wound healing, such as bacitracin and silver sulfadiazine (Silvadene), and fluids for hydration b) tagamet increase cell immunity after injury Informed consent, know who can sign and who can sign if there is a change in capacity without an informed consent a) Doctor must explain the details of the procedure. The nurse can only clarify and watch the patient sign the informed consent after the doctor has spoke with the patient. Risk for those with latex allergies, who is at greatest risk? a) Risk factors a. People with spina bifida. The risk of latex allergy is highest in people with spina bifida — a birth defect that affects the development of the spine. People with this disorder often are exposed to latex products through early and frequent health care. b. People who undergo multiple surgeries or medical procedures. c. Health care workers. d. Rubber industry workers. e. People with a personal or family history of allergies. You're at increased risk of latex allergy if you have other allergies — such as hay fever or a food allergy — or they're common in your family. b) Certain fruits contain the same allergens found in latex. They include: a. Avocado, Banana, Chestnut, Kiwi, Passion fruit Pt positioning in surgery a) Goals: a. Maintain the patient's airway and circulation throughout the procedure b. Prevent nerve damage c. Allow surgeon accessibility to the surgical site as well as for anesthetic administration d. Provide comfort and safety to the patient e. Prevent soft tissue or musculoskeletal and other patient injury b) Fowler’s position a. also known as sitting position, is typically used for neurosurgery and shoulder surgeries. The beach chair position is often used for nasal surgeries, abdominoplasty, and breast reduction surgeries. c) High-fowler’s a. the patient is usually seated (Fowler's position) at the head end of the operating table. The upper half of the patient's body is between 60 degrees and 90 degrees in relation to the lower half of their body. The legs of the patient may be straight or bent. d) Supine a. Laying with face up to the ceiling b. Supine position is commonly used for the following procedures: intracranial, cardiac, abdominal, endovascular, laparoscopic, lower extremity procedures, and ENT, neck and face. e) Jackknife a. also known as Kraske, is similar to Knee-Chest or Kneeling positions and is often used for colorectal surgeries. f) Kidney position a. resembles lateral position, except the patient's abdomen is placed over a lift in the operating table that bends the body to allow access to the retroperitoneal space. A kidney rest is placed under the patient at the location of the lift. g) Prone a. Lying face down b. often used for spine and neck surgeries, neurosurgery, colorectal surgeries, vascular surgeries, and tendon repairs. h) Lithotomy a. the patient can be placed in either a boot-style leg holder or stirrup-style position. b. This position is typically used for gynecology, colorectal, urology, perineal, or pelvis procedures. i) Sims a. The Sims' position is a variation of the left lateral position. The patient is usually awake and helps with the positioning. The patient will roll to his or her left side. Body restraints are used to safely secure the patient to the operating table. Keeping the left leg straight, the patient will slide the left hip back and bend the right leg. This position allows access to the anus. j) Lateral a. A patient may be positioned in Lateral position during back, colorectal, kidney, and hip surgeries. It's also commonly used during thoracic and ENT surgeries, and neurosurgery. k) Trendelenburg a. typically used for lower abdominal, colorectal, gynecology, and genitourinary surgeries, cardioversion, and central venous catheter placement. b. In this position, the patient's arms should be tucked at their sides, and the patient must be secured to avoid sliding on the surgical table. l) Reverse Trendelenburg a. typically used for laparoscopic, gallbladder, stomach, prostrate, gynecology, bariatric and head and neck surgeries. Observations for same day surgical discharge a) must be met before the patient is discharged b) if the patient experiences ongoing issues related to unstable vital signs, poor gas exchange, excessive nausea and vomiting, or unmanageable alterations in comfort, admission to an cute care setting or extended-care facility may be necessary Surgical Drains a) Gravity drains such as the penrose and the T-tube drain directly through a tube from the surgical area. b) In closed=-wound drainage systems such as the JP and Hemovac drainage collects in a collecting vessel by means of compression and re-expansion of the system. Review Parkinson’s a) overview a. a progressive nervous system disorder that affects movement. b) Symptoms through stages a. c) Complications: a. Thinking difficulties. i. You may experience cognitive problems (dementia) and thinking difficulties. These usually occur in the later stages of Parkinson's disease. Such cognitive problems aren't very responsive to medications. b. Depression and emotional changes. i. You may experience depression, sometimes in the very early stages. You may also experience other emotional changes, such as fear, anxiety or loss of motivation. Doctors may give you medications to treat these symptoms. c. Swallowing problems. i. You may develop difficulties with swallowing as your condition progresses. Saliva may accumulate in your mouth due to slowed swallowing, leading to drooling. d. Chewing and eating problems. i. Late-stage Parkinson's disease affects the muscles in your mouth, making chewing difficult. This can lead to choking and poor nutrition. e. Sleep problems and sleep disorders. i. People with Parkinson's disease often have sleep problems, including waking up frequently throughout the night, waking up early or falling asleep during the day. People may also experience rapid eye movement sleep behavior disorder, which involves acting out your dreams. Medications may help your sleep problems. f. Bladder problems. i. Parkinson's disease may cause bladder problems, including being unable to control urine or having difficulty urinating. g. Constipation. i. Many people with Parkinson's disease develop constipation, mainly due to a slower digestive tract. h. Blood pressure changes. i. You may feel dizzy or lightheaded when you stand due to a sudden drop in blood pressure (orthostatic hypotension). i. Smell dysfunction. i. You may experience problems with your sense of smell. You may have difficulty identifying certain odors or the difference between odors. j. Fatigue. i. Many people with Parkinson's disease lose energy and experience fatigue, especially later in the day. k. Pain. l. Sexual dysfunction. i. Some people with Parkinson's disease notice a decrease in sexual desire or performance. d) Medications: a. Carbidopa-levodopa. Levodopa, the most effective Parkinson's disease medication, is a natural chemical that passes into your brain and is converted to dopamine. Levodopa is combined with carbidopa (Lodosyn), which protects levodopa from early conversion to dopamine outside your brain. This prevents or lessens side effects such as nausea. i. Side effects may include nausea or lightheadedness (orthostatic hypotension). ii. Also, you may experience involuntary movements (dyskinesia) after taking higher doses of levodopa. Your doctor may lessen your dose or adjust the times of your doses to control these effects. b. Inhaled carbidopa-levodopa. Inbrija is a new brand-name drug delivering carbidopa- levodopa in an inhaled form. It may be helpful in managing symptoms that arise when oral medications suddenly stop working during the day. c. Carbidopa-levodopa infusion. Duopa is a brand-name medication made up of carbidopa and levodopa. However, it's administered through a feeding tube that delivers the medication in a gel form directly to the small intestine. i. Duopa is for patients with more-advanced Parkinson's who still respond to carbidopa-levodopa, but who have a lot of fluctuations in their response. Because Duopa is continually infused, blood levels of the two drugs remain constant. d. Dopamine agonists. Unlike levodopa, dopamine agonists don't change into dopamine. Instead, they mimic dopamine effects in your brain. i. Dopamine agonists include pramipexole (Mirapex), ropinirole (Requip) and rotigotine (Neupro, given as a patch). Apomorphine (Apokyn) is a short- acting injectable dopamine agonist used for quick relief. 1. Some of the side effects of dopamine agonists are similar to the side effects of carbidopa-levodopa. But they can also include hallucinations, sleepiness and compulsive behaviors such as hypersexuality, gambling and eating. If you're taking these medications and you behave in a way that's out of character for you, talk to your doctor. e. MAO B inhibitors. These medications include selegiline (Zelapar), rasagiline (Azilect) and safinamide (Xadago). They help prevent the breakdown of brain dopamine by inhibiting the brain enzyme monoamine oxidase B (MAO B). This enzyme metabolizes brain dopamine. Selegiline given with levodopa may help prevent wearing-off. i. Side effects of MAO B inhibitors may include headaches, nausea or insomnia. When added to carbidopa-levodopa, these medications increase the risk of hallucinations. f. Catechol O-methyltransferase (COMT) inhibitors. Entacapone (Comtan) and opicapone (Ongentys) are the primary medications from this class. This medication mildly prolongs the effect of levodopa therapy by blocking an enzyme that breaks down dopamine. i. Side effects, including an increased risk of involuntary movements (dyskinesia), mainly result from an enhanced levodopa effect. Other side effects include diarrhea, nausea or vomiting. g. Anticholinergics. These medications were used for many years to help control the tremor associated with Parkinson's disease. Several anticholinergic medications are available, including benztropine (Cogentin) or trihexyphenidyl. i. However, their modest benefits are often offset by side effects such as impaired memory, confusion, hallucinations, constipation, dry mouth and impaired urination. h. Amantadine. Doctors may prescribe amantadine alone to provide short-term relief of symptoms of mild, early-stage Parkinson's disease. It may also be given with carbidopa-levodopa therapy during the later stages of Parkinson's disease to control involuntary movements (dyskinesia) induced by carbidopa-levodopa. i. Side effects may include a purple mottling of the skin, ankle swelling or hallucinations. e) Other important info a. Allow the patient time to perform ADL’s and mobility and provide assistance only as needed b. Implement interventions to prevent complications of impaired mobility such as constipation, pressure injuries, and contractures. c. Scheduled appointments and activities late in the morning to prevent rushing and allow adequate time d. A freezing gait and postural instability are major problems e. Nontraditional exercise programs such as yoga and tai chi may help improve mood and mobility early on f. Collaborate with PT and OT to plan a program. ROM, stretching, and out-of-bed activity g. Remind patient to not focus on feet while walking and implement fall precautions. Information on strokes a) Causes a. two main causes of stroke: a blocked artery (ischemic stroke) or leaking or bursting of a blood vessel (hemorrhagic stroke). Some people may have only a temporary disruption of blood flow to the brain, known as a transient ischemic attack (TIA), that doesn't cause lasting symptoms. b) Types a. Ischemic stroke i. This is the most common type of stroke. It happens when the brain's blood vessels become narrowed or blocked, causing severely reduced blood flow (ischemia). Blocked or narrowed blood vessels are caused by fatty deposits that build up in blood vessels or by blood clots or other debris that travel through your bloodstream and lodge in the blood vessels in your brain. b. Hemorrhagic i. occurs when a blood vessel in your brain leaks or ruptures. Brain hemorrhages can result from many conditions that affect your blood vessels. Factors related to hemorrhagic stroke include: 1. Uncontrolled high blood pressure, Overtreatment with blood thinners (anticoagulants), Bulges at weak spots in your blood vessel walls (aneurysms), Trauma (such as a car accident), Protein deposits in blood vessel walls that lead to weakness in the vessel wall (cerebral amyloid angiopathy), and Ischemic stroke leading to hemorrhage c. Transient ischemic i. sometimes known as a ministroke — is a temporary period of symptoms similar to those you'd have in a stroke. A TIA doesn't cause permanent damage. They're caused by a temporary decrease in blood supply to part of your brain, which may last as little as five minutes. ii. Like an ischemic stroke, a TIA occurs when a clot or debris reduces or blocks blood flow to part of your nervous system. c) Signs and symptoms a. Trouble speaking and understanding what others are saying. i. You may experience confusion, slur your words or have difficulty understanding speech. b. Paralysis or numbness of the face, arm or leg. i. You may develop sudden numbness, weakness or paralysis in your face, arm or leg. This often affects just one side of your body. Try to raise both your arms over your head at the same time. If one arm begins to fall, you may be having a stroke. Also, one side of your mouth may droop when you try to smile. c. Problems seeing in one or both eyes. i. You may suddenly have blurred or blackened vision in one or both eyes, or you may see double. d. Headache. A sudden, severe headache, which may be accompanied by vomiting, dizziness or altered consciousness, may indicate that you're having a stroke. e. Trouble walking. i. You may stumble or lose your balance. You may also have sudden dizziness or a loss of coordination. d) Treatment a. Ischemic stroke i. Emergency IV medication. 1. Therapy with drugs that can break up a clot has to be given within 4.5 hours from when symptoms first started if given intravenously. The sooner these drugs are given, the better. Quick treatment not only improves your chances of survival but also may reduce complications. 2. An IV injection of recombinant tissue plasminogen activator (tPA) — also called alteplase (Activase) — is the gold standard treatment for ischemic stroke. An injection of tPA is usually given through a vein in the arm with the first three hours. Sometimes, tPA can be given up to 4.5 hours after stroke symptoms started. a. This drug restores blood flow by dissolving the blood clot causing your stroke. By quickly removing the cause of the stroke, it may help people recover more fully from a stroke. Your doctor will consider certain risks, such as potential bleeding in the brain, to determine if tPA is appropriate for you. ii. Emergency endovascular procedures. Doctors sometimes treat ischemic strokes directly inside the blocked blood vessel. Endovascular therapy has been shown to significantly improve outcomes and reduce long-term disability after ischemic stroke. These procedures must be performed as soon as possible: 1. Medications delivered directly to the brain. Doctors insert a long, thin tube (catheter) through an artery in your groin and thread it to your brain to deliver tPA directly where the stroke is happening. The time window for this treatment is somewhat longer than for injected tPA, but is still limited. 2. Removing the clot with a stent retriever. Doctors can use a device attached to a catheter to directly remove the clot from the blocked blood vessel in your brain. This procedure is particularly beneficial for people with large clots that can't be completely dissolved with tPA. This procedure is often performed in combination with injected tPA. iii. Other procedures 1. Carotid endarterectomy. Carotid arteries are the blood vessels that run along each side of your neck, supplying your brain (carotid arteries) with blood. This surgery removes the plaque blocking a carotid artery, and may reduce your risk of ischemic stroke. A carotid endarterectomy also involves risks, especially for people with heart disease or other medical conditions. 2. Angioplasty and stents. In an angioplasty, a surgeon threads a catheter to your carotid arteries through an artery in your groin. A balloon is then inflated to expand the narrowed artery. Then a stent can be inserted to support the opened artery. a. Hemorrhagic stroke i. Emergency measures. 1. If you take blood-thinning medications to prevent blood clots, you may be given drugs or transfusions of blood products to counteract the blood thinners' effects. You may also be given drugs to lower the pressure in your brain (intracranial pressure), lower your blood pressure, prevent spasms of your blood vessels and prevent seizures. ii. Surgery. 1. If the area of bleeding is large, your doctor may perform surgery to remove the blood and relieve pressure on your brain. Surgery may also be used to repair blood vessel problems associated with hemorrhagic strokes. Your doctor may recommend one of these procedures after a stroke or if an aneurysm, arteriovenous malformation (AVM) or other type of blood vessel problem caused your hemorrhagic stroke: iii. Surgical clipping. 1. A surgeon places a tiny clamp at the base of the aneurysm, to stop blood flow to it. This clamp can keep the aneurysm from bursting, or it can keep an aneurysm that has recently hemorrhaged from bleeding again. iv. Coiling (endovascular embolization). 1. Using a catheter inserted into an artery in your groin and guided to your brain, your surgeon will place tiny detachable coils into the aneurysm to fill it. This blocks blood flow into the aneurysm and causes blood to clot. v. Surgical AVM removal. 1. Surgeons may remove a smaller AVM if it's located in an accessible area of your brain. This eliminates the risk of rupture and lowers the risk of hemorrhagic stroke. However, it's not always possible to remove an AVM if it's located deep within the brain, it's large, or its removal would cause too much of an impact on brain function. vi. Stereotactic radiosurgery. 1. Using multiple beams of highly focused radiation, stereotactic radiosurgery is an advanced minimally invasive treatment used to repair blood vessel malformations. Medication: Phenytoin and teaching a) Adverse effects a. Mild drowsiness and other CNS depressant effects b. Gingival hyperplasia, abnormal gum growth, is common in children and adolescents who take this drug c. It can occasionally cause a skin rash, which could indicate a serious side effect b) Interventions a. Monitor drowsiness and other CNS effects i. Excessive drowsiness may indicate toxicity b. Observe gums and monitor for rashes c) Administration a. Give with meals b. If through IV, push slow c. Therapeutic range should be between 10 and 20 mcg/ml i. If serum levels exceed this range, it can lead to nystagmus, ataxia, sedation, and blurred or double vision. d) Pt Instructions a. Avoid driving or participating in activities that require mental alertness if experiencing CNS effects such as sedation and drowsiness b. Obtain regular dental checkups c. Brush with a soft-bristled tooth brush, massage the gums, and floss d. Notify provider if rash occurs e. Do not stop taking abruptly e) Safety alerts a. Monitor for a rash that occurs after drug therapy starts, as epidermal necrolysis or Stevens-Johnsons syndrome can occur. Fever, damage to skin and organs, and sepsis can result. If this type of rash occurs, DC the drug immediately. b. This drug can reduce the effectiveness of oral contraceptives, so patients who wish to prevent pregnancy should find a different form. Understand the post-ictal phase of seizures a) refers to the period of time immediately following a seizure. The postictal phase can last for seconds, minutes, hours, and sometimes even days. It is commonly thought of as the time during which the brain recovers from a seizure. b) Symptoms a. Fatigue, Headache, Nausea, Sleepiness, Memory loss, Mental confusion or fogginess, Thirst, Weakness in part of all of the body, A strong urge to urinate, Difficulty walking, Speech or writing impairment b. Postictal migraines are a common complaint among people with epilepsy.2 One possible explanation for this is the cerebral edema (brain swelling) that can result from a seizure, causing increased intracranial pressure and pain. c. On the flip side, some people have postictal bliss, described as an excessively happy feeling, after a seizure. c) Postictal symptoms can sometimes help doctors determine the focus of the seizure—that is, where in the brain the seizure activity started. Understand the ictal phase a) The middle (ictal) stage of a seizure is called the ictal phase. It’s the time from the first symptom to the end of the seizure activity. It is during this time that intense electrical activity is occurring in the brain. b) Some common signs of this phase include: a. Loss of awareness, Memory lapse, Feeling confused, Difficulty hearing, Odd smells, sounds or tastes, Difficulty speaking or saying strange words, Twitching, Loss of muscle control, Repeated movements (such as lip smacking or chewing), Body convulsions, Racing heart, and Trouble breathing Decorticate vs Decerebrate Medication: Heparin Lab: PTT a) an anticoagulant (blood thinner) that prevents the formation of blood clots. b) You should not use heparin if you have uncontrolled bleeding or a severe lack of platelets in your blood. Do not use this medicine if you have ever been diagnosed with “heparin-induced thrombocytopenia,” or low platelets caused by heparin or pentosan polysulfate. c) PT Evaluates ability to clot a. 10-12 sec (not on blood thinners) d) INR ensures that results from a PT test are the same from one lab to another a. 1-2 (not on blood thinners) e) PTT determines if blood-thinning therapy is effective a. 30-45 seconds (not on blood thinners) i. Blood thinners will make blood take longer to clot, so a patient taking a blood thinner would be expected to have lab results that are higher (longer) than the ones listed here. Labs: WBC, Blood Glucose, Lactate(Know values and what happens when out of range) a) WBC4,500-10,000 a. Low: neutropenia, leukopenia, bone marrow failure, chemo, viral infection b. High: leukocytosis, intense exercise, stress corticosteroids b) BS 70-100 a. Low: excess insulin, liver disease, adrenal insufficiency b. High: excess glucose, diabetes, pancreatitis, hyperthyroidism c) Lactate 0.4-2 Triage prioritization a) the process of determining the priority of patients' treatments by the severity of their condition or likelihood of recovery with and without treatment. b) Priority is then given to patients most likely to deteriorate clinically and triage takes account of vital signs, pre-hospital clinical course, mechanism of injury and other medical conditions. Tag colors for triage a) Red emergent needing immediate attention (class I) b) Yellow can wait short time for care (class II) c) Green Non-urgent or “walking wounded” (class III) d) Black Expected to die or are dead (class IV) Assessment for those with CO poisoning a) The most common symptoms of CO poisoning are headache, dizziness, weakness, nausea, vomiting, chest pain, and altered mental status. b) The clinical presentation of CO poisoning is the result of its underlying systemic toxicity. Its effects are caused not only by impaired oxygen delivery but also by disrupting oxygen utilization and respiration at the cellular level, particularly in high-oxygen demand organs (i.e., heart and brain). c) Symptoms of severe CO poisoning: a. malaise, shortness of breath, headache, nausea, chest pain, irritability, ataxia, altered mental status, other neurologic symptoms, loss of consciousness, coma, and death. d) Signs: a. tachycardia, tachypnea, hypotension, various neurologic findings including impaired memory, cognitive and sensory disturbances; metabolic acidosis, arrhythmias, myocardial ischemia or infarction, and noncardiogenic pulmonary edema, although any organ system might be involved. e) The key to confirming the diagnosis is measuring the patient’s carboxyhemoglobin (COHgb) level. a. COHgb levels can be tested either in whole blood or pulse oximeter. b. It is important to know how much time has elapsed since the patient has left the toxic environment, because that will impact the COHgb level. If the patient has been breathing normal room air for several hours, COHgb testing may be less useful. Fire mgmt. RACE a) Rescue, Alarm, Contain and Extinguish when you first encounter a fire, and Pull, Aim, Squeeze and Sweep when using a fire extinguisher. [Show More]
Last updated: 1 year ago
Preview 1 out of 55 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 16, 2022
Number of pages
55
Written in
Additional information
This document has been written for:
Uploaded
Feb 16, 2022
Downloads
0
Views
26








.png)