NCSBN – Lesson 2: Safety and Infection Control Study Guide,100% CORRECT
Document Content and Description Below
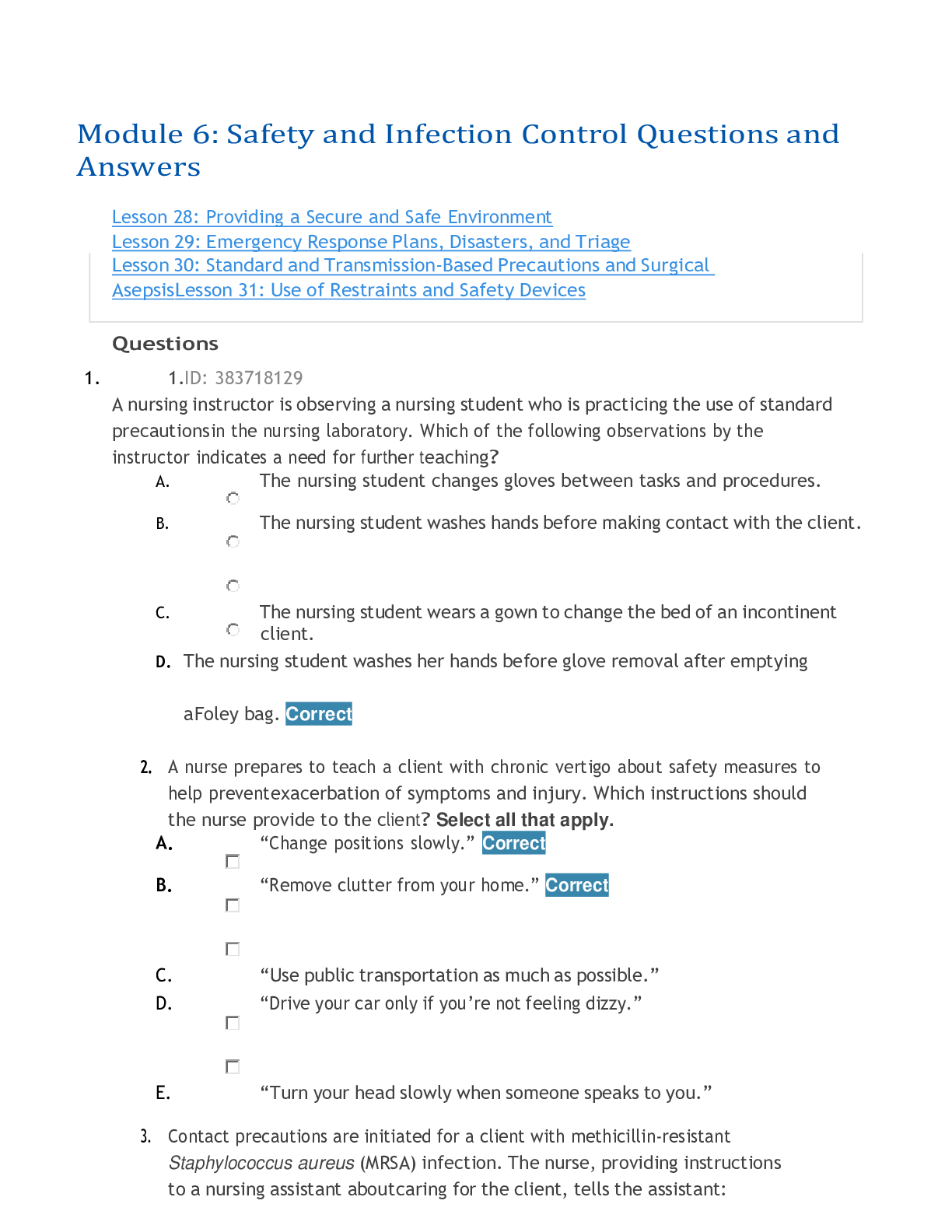
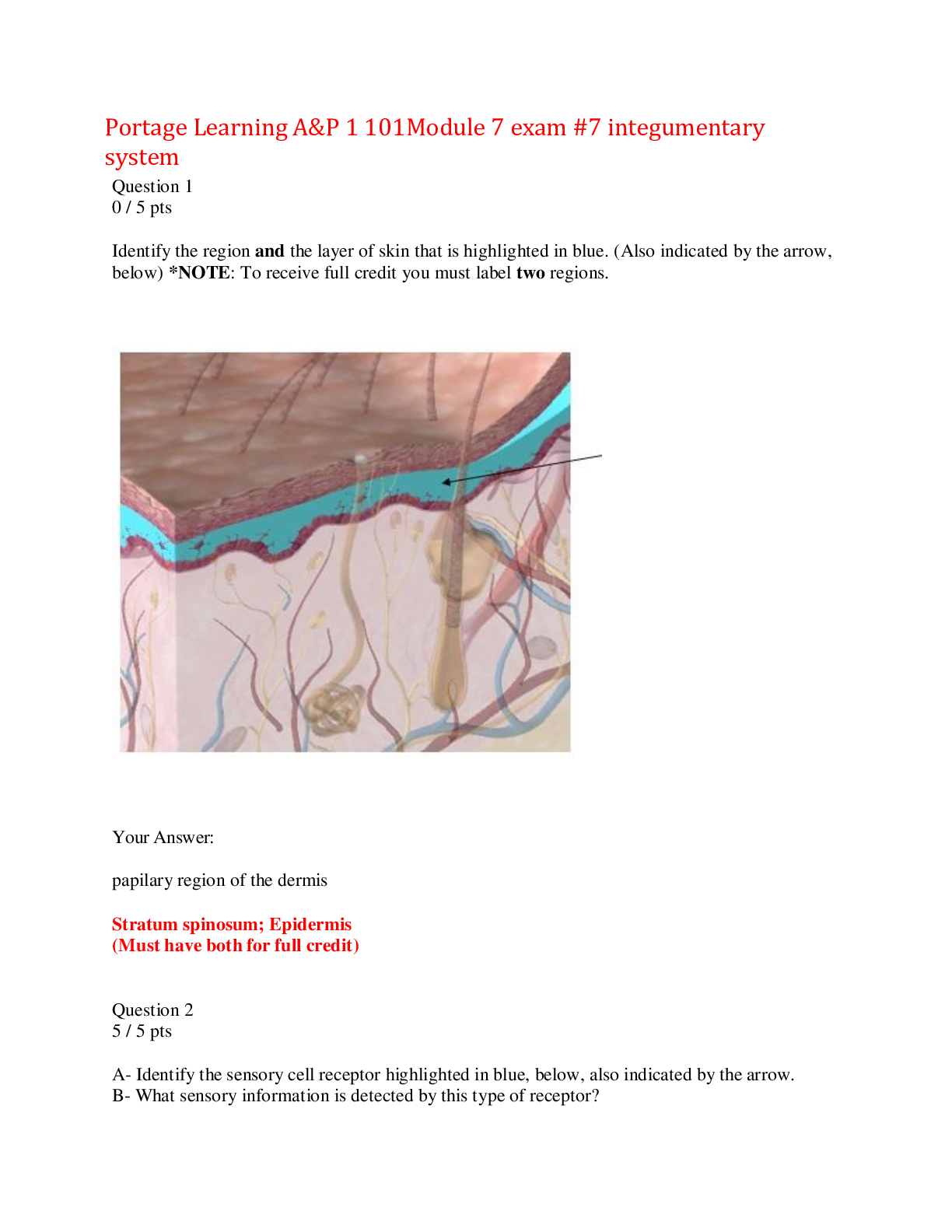
NCSBN – Lesson 2: Safety and Infection Control Study Guide Safety The goal of the Quality and Safety Education for Nurses (QSEN) project is to prepare future nurses who will have the knowledge, ... skills and attitudes (KSAs) necessary to minimize the risk of harm to patients and providers through both system effectiveness and individual performance. This includes knowing what knowledge and actions help promote fire, electrical and radiation safety. • Fire Safety o Location of fire alarms o Location of and how to use fire extinguishers o Location of fire exits • Electrical Safety o Health Care Settings ▪ All health care organizations have policies and procedures related to clients' use of any electrical equipment brought from home. ▪ For any equipment, inspect equipment for safety hazards. ▪ Always check the ground wire before plugging in a piece of electrical equipment. ▪ Remove malfunctioning equipment and report to appropriate personnel. o In the Home ▪ Assess the need for client home modifications, including lighting, handrails and/or a fire extinguisher in the kitchen. ▪ Check the wattage of light fixtures and lamps to make sure they are the correct wattage; incorrect wattage can cause overheating that can lead to a fire. ▪ Many avoidable electrical fires can be traced back to misuse of electric cords - overloading circuits, using extension cords and/or running cords under rugs. ▪ Use safety closures to "child-proof" electrical outlets. ▪ Educate/reinforce instructions on home safety issues and safe use of equipment. • Radiation Safety o Radiation exposure occurs in diagnostic X-rays/scans and radiopharmaceuticals. Clients undergoing implant therapy will have a sealed source of radioactive material (containing alpha or beta particles and/or gamma rays) placed inside a body cavity, close to the tumor. o Gamma rays have properties like X-rays and present a potential external hazard (they are the most penetrating type of radiation). o Alpha particles, which occur naturally in the environment, can be stopped by your skin and clothing. o An example of a treatment that emits both gamma rays and beta particles includes radioactive iodine-131 (I-131); I-131 has a half-life of eight days. o Use these simple techniques to reduce the hazards associated with gamma rays: ▪ Client • Mark the client's room with appropriate signage. • Place client in a private room. • Place wristband on client indicating that the client is receiving internal radiation therapy. ▪ Health Care Workers • Apply shoe covers and protective gloves before entering the client's room; remove equipment before exiting the room • Wear gloves • Plan care to minimize time at the client's bedside • Be efficient and courteous, but don't rush • Maintain the greatest distance possible from the client consistent with effective care • Restrict care to a maximum of one hour every eight hours • Prepare meal trays outside the room • Position items within the client's reach to facilitate as much self- care as possible • Schedule only one radioactive client to a nurse at a time • Ensure a long-handled forceps and a lead container are in the client's room in case of implant dislodgement • If a source becomes dislodged, notify the radiation oncologist • Do not attempt to handle the dislodged implant unless trained to do so • Wear a film badge (such as a dosimeter) while caring for the client to monitor exposure; have it checked per agency policy • No pregnant nurses, visitors, or children should be allowed near the client o To protect yourself, remember the three elements of radiation: o Time o Distance o Shielding Poison Control Basic therapy involves removing and/or neutralizing the poison. • Equipment needed for gastrointestinal (such as gastric lavage), cutaneous and ocular decontamination • Life support measures needed, including endotracheal intubation, assisted and control ventilation, parenteral fluid therapy, pharmacological treatment, cardiac pacing and defibrillation • Continuous cardiac and circulatory monitoring using ECG, blood pressure and other devices to monitor vital functions • X-rays • Laboratory analysis of acid-base balance, blood gases, electrolytes, blood glucose, liver and kidney function and coagulation • Initial and repeated specific toxicological analyses of body fluids of blood, urine and stomach contents • Possibly hemodialysis, peritoneal dialysis Do not induce vomiting for clients who have swallowed any substance containing an acid (such as toilet bowel cleaners and swimming pool cleaners) or corrosive alkalis (including oven cleaners, liquid drain cleaners, disk batteries, various household cleaners and dishwasher detergents). Vomiting these substance may cause irreversible upper respiratory damage. Antidotes An antidote is a substance or medication that counteracts forms of poisoning or symptoms of overdoses of certain medications. (The toxic substances are in bold). • Acetaminophen - N-acetylcysteine • Anticholinergics - physostigmine salicylate • Arsenic, gold, lead, copper or mercury - chelation therapy with dimercaprol (also known as British anti-Lewisite or BAL) • Benzodiazepines - flumazenil • Beta blockers - glucagon • Calcium channel blockers - glucagon, calcium chloride, calcium gluconate • Cholinergics - atropine, pralidoxime • Cyanide - amyl nitrate, followed by sodium nitrate, followed by sodium thiosulfate; hyperbaric oxygen chamber • Digitalis/digoxin - digoxin immune fab • Ethylene glycol - ethanol and fomepizole • Heparin - protamine sulfate • Iron - deferoxamine • Magnesium sulfate - calcium gluconate • Methanol - ethanol and fomepizole • Organophosphate nerve agent - atropine • Organophosphate or carbamate insecticide poisoning - atropine • Opioids (codeine, morphine) - naloxone • Snakes (rattlesnakes, copperheads, cottonmouths, coral snake) - antivenin (Micrurus fulvius) Crotalidae Polyvalent Immune Fab • Spiders (black widow) - Antivenin (Latrodectus mactans) • Vasopressor extravasation - phentolamine mesylate • Warfarin - phytonadione (vitamin K) Safety Risks Factors Infants • Burns and Falls Toddlers and Preschool • Burns and Choking • Falls • Playground/street related activities • Poisoning School-Age • Automobile-related injuries (for example, not wearing proper safety restraint devices) • Drowning • Sports-related injuries; may be due to not wearing proper equipment, such as bicycle helmets, knee pads, mouth guards Adolescence • Automobile accidents, including speeding, talking/texting while driving • Lifestyle choices, such as unprotected sex • Substance abuse Adults • Lifestyle habits, for example, sun exposure or not wearing car safety belts • Smoking • Stress-related illnesses • Substance abuse Older Adults • Automobile accidents • Burns • Falls Causes of Falls There are variety of reasons a client may fall. Age-related changes, diseases or health conditions, medications or the environment can contribute to an accidental fall. • Intrinsic Factors that Increase the Likelihood of Falling o Age-related Changes ▪ Vision • Decline in visual acuity • Decrease in color sensitivity • Decreased depth perception • Greater sensitivity to glare • Difficulty in detecting changes in shapes • Decreased acuity in low lighting • Decline in light sensitivity ▪ Balance/Gait • Decreased proprioception (sense of body position/movement) • Slower righting reflexes • Decreased muscle tone and strength • Changes in ambulation • Orthostatic hypotension (baroreceptor reflex decreases with age) • Fear of falling – leads to decrease in activities, deconditioning and loss of independence o Diseases or Health Conditions ▪ Cardiovascular • Changes in blood pressure, leading to orthostatic hypotension, lightheadedness and dizziness • Heart failure, which causes decreased muscle strength, lack of endurance and increased fatigue, leading to a change in gait • Edema, which can affect one's ability to maintain balance; increase of weight in legs causes a change in gait ▪ Neurologic/Cognitive • Alzheimer's disease and other neurocognitive disorders • Impaired judgment • Poor reasoning • Becoming lost (geographically) • Changes in perception • Behavioral changes, including aggression, agitation, restlessness, pacing • Parkinson's disease • Stroke ▪ Musculoskeletal • Muscle weakness • Arthritis • Disorders of the feet ▪ Gastrointentinal – any condition that requires an older adult to make multiple trips to the bathroom increases the risk of falling, such as: • Incontinence • Nocturia • Diarrhea ▪ Infections – a fall can be the first sign of a new illness or a chronic illness is getting worse o Medications ▪ Any medications that cause hypotension, dizziness, incontinence or fatigue: • Antihypertensives • Antidepressants • Diuretics • Hypoglycemics • Laxatives • Polypharmacy • Sedatives/hypnotics • Extrinsic Factors that Increase the Likelihood of Falling o Physical Environment ▪ Poor lighting ▪ Floors and stairs – (throw) rugs, handrails, (liquid/food) spills ▪ Bathroom ▪ Pets ▪ Beside table o Assistive Devices and Footwear ▪ Inappropriate use of canes, walkers or wheelchairs ▪ Improperly fitting shoes ▪ Shoes with slippery soles ▪ Wearing slippers instead of well-fitting shoes Fall Prevention Every client should be evaluated for risk of falling. A fall-assessment tool can help you to identify factors that may increase the likelihood of falling, such as previous history of falls, gait or balance disturbances, foot and leg problems, or any other physical or cognitive impairments. All staff should be alerted to fall precautions. Nurses must document all assessments and interventions. • All Clients o Health Care Settings ▪ Familiarize the client to the environment ▪ Have the client demonstrate how to use the call light ▪ Answer call lights promptly ▪ Keep client personal possessions within reach ▪ Have sturdy handrails in bathrooms, room and hallway ▪ Maintain bed in low position with wheels locked ▪ Wear non-slip, well-fitting footwear ▪ Maintain adequate day and night time lighting ▪ Keep floor surfaces clean and dry; wipe up spills promptly ▪ Provide supportive chairs with armrests ▪ Encourage clients to use grab bars in showers and bathtubs ▪ Verify that the client is appropriately using canes, walkers and other assistive devices for ambulation ▪ The nurse should regularly assess patients and modify the health record when needed. If a patient falls, the nurse should perform a post-fall analysis and incorporate findings into quality assurance and/or incident reporting programs. o In Home ▪ Home health nurses should also conduct a home safety check and, if necessary, recommend corrective actions. Patients and their families must be informed of potential risk factors and modification strategies to help ensure safety in the home. ▪ There is a greater risk of falling if a person: o Is older than age 80 o Has a history of falls o Lives alone o Needs to use stairs in the home (to access second-story bedroom and/or bathroom) • Restraints o Use the least restrictive form of restraint and/or safety device. o A restraint is a measure or condition that limits a client's movement. Restraints can also help keep a client from getting hurt or doing harm to others. A restraint or seclusion is used as a last resort and only when it is determined that it is clinically justified or warranted by client behavior that threatens the physical safety of the client, staff or others. o There are three categories of restraints: ▪ Chemical — Medications such as central nervous system depressants or paralytics. ▪ Physical — Manual methods (mechanical device, material or equipment) such as vest, wrist or ankle restraints. Raised side rails can be considered a form of restraint; however, one raised side rail that is used to facilitate mobility in and out of bed would not be considered a restraint. Additionally, if a client can easily remove a device, it doesn't qualify as a physical restraint. ▪ Seclusion — A client is held in a room involuntarily and prevented from leaving. This is only used for clients behaving violently. Using both a physical restraint and seclusion requires continuous nursing monitoring using both video and audio equipment that is in close proximity to the client. ▪ A physical restraint or safety device requires a signed, dated physician's order specifying the type of restraint or safety device and a time limit for its use. There can be no standing or as needed (PRN) orders for restraints. o A soft restraint can be implemented without a HCP orders to protect client from injury or harm. However, HCP must be contacted immediately. Only trained staff members should be allowed to intervene in a crisis. All staff who have direct contact with clients in restraints must go through training on how to monitor the physical and psychological needs of the person being restrained (measure vital signs, circulation and assess comfort). There should be documentation of all care, along with ongoing assessment of opportunities to use less restrictive methods or to discontinue the restraints. Medical Errors Breaches in standards or failure to perform by a health care provider that yields an unfavorable health result for a client. Have serious consequences in health care settings. "Actions to improve the culture of safety within health care is an essential component of preventing or reducing errors and improving overall health care quality" (ARHQ, 2017). To improve health outcomes for clients, nurses should: • Assess, identify and document/communicate allergies, including latex sensitivity and latex allergies. • Implement seizure precautions based on policy/protocol. • Ensure proper identification of client is used before providing care: o Use two identifiers prior to administering a medication; asking a client to state his or her full name and birthdate are common identifiers. o Use client wristband and barcode identification technology in conjunction with an electronic health record. • Verify appropriateness and/or accuracy of treatment orders. Chain of Infection Examples of incubation periods for specific diseases: • Mumps: 18 days • Varicella (chickenpox): 2 to 3 weeks Prodromal Stage Not all diseases have prodromal periods. For those that do, the prodromal stage is the time from onset of nonspecific findings, such as fatigue and malaise, to disease- specific findings. This is when the pathogen is multiplying, and the host is most contagious. Invasive Phase During the invasive phase, the person exhibits the specific findings of the disease: • Mumps: swelling of the parotid gland • Common cold: sore throat, congestion If the host cannot fight off an infection, such as pneumonia, influenza or a urinary tract infection (UTI), the invasive phase can progress to systemic complications such as septicemia and even death. Other diseases, such as varicella (chickenpox) virus can reactivate years later, causing shingles. Many of the preventable childhood diseases can cause (irreversible) complications: • Mumps: Can cause sterility • Measles: Can lead to pneumonia, encephalitis and permanent hearing loss • Polio: Can lead to temporary or permanent muscle paralysis, disability and deformities Convalescence • Convalescence is when the acute findings begin to disappear and the body returns to normal health. HAI & CAI Health care-associated infections (HAI) are associated with devices or procedures used to treat clients. HAIs are the most frequent adverse event in health care delivery worldwide, leading to significant mortality as well as financial losses for health systems. The most common healthcare-associated infection (HAI) is usually caused by a "staff" infection - one that is transmitted from a health care worker, or "staff," to a client. The more common HAIs include: • Central line-associated bloodstream infections (CLABSI) • Catheter-associated urinary tract infections (CAUTI) • Ventilator-associated pneumonia • Surgical site infections Infection Control Hand hygiene is the foundation of all infection control practices in health settings. The following information provides an overview of the various processes used to reduce or eliminate infections. Medical Asepsis Referred to as "clean technique," medical asepsis includes any therapy, protocol or medical procedure used to reduce the number and spread of microorganisms. • Hand hygiene — the single most effective and important way to prevent the spread of microorganisms: o Friction — loosens the microorganisms so they can be removed o Soap – non-antimicrobial soap and water or with antimicrobial soap and water if contact with spores, including Clostridium difficile or Bacillus anthracis • Disinfectants and antiseptics: o Disinfectant: a substance that reduces the number of microorganisms, including bleach solutions and Zephirin (or other quaternary ammonium compounds) o Antiseptic: a substance that can be applied to skin to reduce the number of microorganisms, including alcohol, povodine iodine solutions (such as Betadine®) and 2% chlorhexadine solution such as (ChloraPrep®) • Practices that interrupt transmission, such as the use of personal protective equipment Surgical Asepsis Surgical asepsis includes the practices that destroy all microorganisms and their spores, such as steam under pressure, gas, radiation and chemicals. Some very basic guidelines of surgical asepsis include: • Only sterile objects may be placed on a sterile field • Always hold your hands above the level of your elbows • Do not reach over the sterile field • The edges of a sterile field or container are considered contaminated (depending on the resource, this is approximately 1-2 inches surrounding the border) A sterile object will become contaminated under the following circumstances: • Sterile touching clean becomes... contaminated • Sterile touching contaminated becomes... contaminated • Sterile touching "questionable" is... contaminated • A sterile object or sterile field that is not in the range of vision is... contaminated • An object held below a person's waist is... contaminated • A sterile object that comes in contact with a wet, contaminated surface is… contaminated (through capillary action) • A sterile object becomes contaminated…with prolonged exposure to air Standard and Transmission-based Precautions Standard precautions are a set of infection control practices used to prevent the transmission of bloodborne and other pathogens from recognized and unrecognized sources. They are the basic level of infection control precautions that are used in the care of all clients. Standard Precautions • Wash hands with soap and water when visibly dirty or contaminated. • Wash hands or use an antiseptic handrub: o Immediately when there is direct contact with blood, body fluids, secretions, excretions or contaminated items o After contact with a person's intact skin, such as when taking a pulse or blood pressure, or moving or repositioning a client o After contact with inanimate objects, including medical equipment in the immediate vicinity of the client o After removing gloves o Between client contact • Wear gloves before touching anything wet or before performing invasive procedures • Use masks, goggles, face masks and other personal protective equipment (PPE) to protect mucous membranes of the eyes, nose and mouth when contact with blood and body fluids is likely Standard precautions also include respiratory hygiene/cough etiquette, safe injection practices and the use of masks for insertion of catheters or injection of material into spinal or epidural spaces via lumbar puncture procedures. Transmission-based Precautions • CONTACT PRECAUTIONS o Organisms can be transmitted by direct contact (from one infected person to another person) or by indirect contact, through a contaminated intermediate surface, object or vector (such as mosquitoes, flies, mites, fleas, ricks and rodents). o Epidemiologically important organisms for contact transmission: VRE (vancomycin-resistant enterococcus) and Clostridium difficile (C. difficile). o You should wear a gown and gloves for all interactions that may involve contact with the client or potentially contaminated areas in the client's environment. • DROPLET PRECAUTIONS o Respiratory droplets are generated when an infected person coughs, sneezes, talks or during procedures such as suctioning, endotracheal intubation, cough induction by chest physiotherapy and cardiopulmonary resuscitation. Transmission of these large particle droplets occurs when they come in contact with the conjunctivae or the mucous membranes of the nose or mouth of a susceptible person. o When close contact (typically within three feet or less) between the source client and a susceptible person is required, you should use a standard surgical mask. o Epidemiologically important organisms for infectious agents transmitted through the droplet route: group A Streptococcus (for the first 24 hours of antimicrobial therapy), adenovirus, rhinovirus, Neisseria meningitidis, pertussis, influenza virus. • AIRBORNE PRECAUTIONS o Airborne precautions are used when microorganisms dispersed through the air over long distances remain infective over time and distance. To prevent the spread of airborne pathogens, the client should be placed in a room with special airflow and ventilation systems (airborne infection isolation room or AIIR) and nurses should use respiratory protection with a NIOSH-certified N95 or higher level respirator when in the room. Epidemiologically important organisms for infectious agents transmitted through the airborne route: rubeola virus (measles), varicella-zoster virus (chickenpox), Mycobacterium tuberculosis. • NEUTROPENIC PRECAUTIONS o used to prevent infection in clients who have neutropenia (low white blood cell counts) or are immunocompromised. Which personal protective equipment (PPE) is used depends on the nature of interaction and the potential for exposure to blood, body fluids or infectious agents. o Usually visitors are restricted, and the client is in a private room. Protecting Nurses Injury is one of the hazards of direct nursing care. The physical demands of moving and repositioning clients can result in musculoskeletal injuries, especially back injuries. Needlestick injuries expose nurses to infection. Exposure to occupational chemicals and the potential for violence also have severe consequences for a nurse's health. • Turning and Repositioning Clients o To protect yourself and the client from injury, you must use your body correctly when turning and repositioning clients and when transferring clients to and from beds, chairs, wheelchairs, stretchers and toilets. o How you move or transfer a client will be based on: o The client's level of dependence, such as whether the client can bear weight or has upper body strength. o Whether the client is alert, oriented and cooperative. o Based on your assessment and documented information, you will also need to determine the amount of assistance needed and the type of equipment needed. Since manual lifting is unsafe for clients and caregivers, mechanical equipment such as ceiling- or Hoyer-type lifts should be used. You will need to know how the equipment works and match it to the needs of the client and limitations of the room/area before you move the client. Repositioning a client in bed is never a one person task. If possible, the bed should be flat, the height of the bed appropriate for staff safety (at the elbows). If possible, the client should flex the knees and push on the count of three; otherwise, you should use a slider board. You should take great care to reduce friction and shearing when moving a client in bed. • Needlesticks o If you are stuck by a needle or other sharp object or get blood or other potentially infectious materials in your eyes, nose, mouth, or on broken skin, you should immediately flood the exposed area with water and then clean any wound with soap and water or available skin disinfectant. You will then report the incident to your employer and seek further medical attention. • Chemical Occupational Exposure o Hazardous chemical exposure may include aerosols, gases and skin contaminants from cleaners and disinfectants, latex and pharmaceuticals. Medication administration, handling contaminated linens, exposure to human wastes or being involved in special procedures (such as administering antineoplastic drugs, exposure to anesthetic gases) can adversely affect a nurse's health. • Workplace Violence o Nurses and UAP are increasingly experiencing verbal or physical abuse – such as yelling, cursing, grabbing, scratching or kicking - from clients and visitors. Nurses are more vulnerable to violence since they are the ones who most frequently interact with clients and their families. Many nurses consider violence by clients as part of the job and that some clients cannot be held accountable for their violent actions, which is why many incidents of violence go unreported. However, nurses must report incidents of violence. Moreover, clients and visitors must be held accountable for their behavior. In fact, many states have enacted enforceable legislation that make it a felony to assault or batter nurses. Incident Reports Medication administration errors are one of the most common types of errors made by nurses. When you realize that you made an error, the first action should be to report the error to the first person in the chain of command (usually the charge nurse); the prescriber must also be contacted and orders implemented. After caring for the patient, you will need to complete an incident (or occurrence) report. By reporting errors, you are helping to improve processes or create new processes to minimize errors and risk of harm to patients. When to Complete an Incident Report In addition to reporting a medication administration error, an incident report (the written documentation of unusual incidents such as medication errors, acts of omission and commission, client falls and conflicts with clients and their families; also referred to as an occurrence report) should be filed whenever any unexpected event occurs. For example, an incident report is required for the following situations: • Any time a client makes a complaint. • A medical device malfunctions. • Anyone – clients, staff or visitors – is injured or involved in a situation with the potential for injury General Guidelines All organizations have specific guidelines for completing the report, you should always remember to stick to the facts and report the following information: • Date, time, and exact location of the occurrence (if the specific details are not known, document the date and time the error was discovered) • Names of persons involved in the incident and any witnesses • Direct quotes from the persons involved in the incident • Objective information describing the incident • Who was notified about the error • Orders received • If indicated, corrective actions taken Security Plans A written security plan is designed to protect clients, visitors and staff. The plan identifies security threats in all areas of a health care facility that could have an adverse impact on persons and property. Health care organizations are required to identify security-sensitive locations within the hospital that may require unique security protection, including mother-baby units, pediatric units, emergency department, (inpatient) psychiatry, radiation therapy, nuclear medicine, pharmacy, medical records, information services, human resources, food services and surgical services. Physical protection may include closed-circuit television or video surveillance, time delay locks and alarm systems, panic alarms, special locks, protective barriers, security presence and/or dedicated security patrols. Emergency Department Examples of security in the emergency department (ED): • All individuals may be screened when entering the unit • All personal items are screened with an X-ray unit • All interior and exterior doors leading to client care areas are equipped with electronic access control • The locked psychiatric unit within the ED are controlled by electronic access control and monitored via digital camera system Mother-baby Unit There are multiple tools and devices used to protect against infant abduction in the mother-baby unit: • All entrances have an electronic locking mechanism • All employees must use their badge to enter; guests must be cleared before entering • A digital surveillance system records activity 24/7 and stores data for a specific period of time (usually 30 days) • All ingress/egress doors are equipped with an infant protection system • Security measures for newborns (with matching devices for mother and father/support person) may include tamper-proof umbilical tags, cord clamps, wrist and ankle bracelets Emergency Preparedness Any emergency that is caused by a natural, accidental or intentional event can result in a mass casualty incident. A mass casualty incident includes any event that has the potential to overwhelm the available resources. The most common types of mass casualty incidents include terrorist attacks, air crashes, major fires, train derailments, building collapses, explosions, highway accidents, hazardous material releases (chemical and radiation), natural disasters and severe weather (floods, hurricanes, tornadoes, earthquakes and volcanoes) and recent disease outbreaks (ranging from Salmonella to Ebola). • Explosions Explosions or blasts can cause unique patterns of injury. Most injuries involve multiple penetrating injuries and blunt trauma. All bomb events have the potential for chemical and/or radiological contamination. Treatment overview: • Lung injuries o High flow oxygen sufficient to prevent hypoxemia via non-rebreather mask, CPAP or ET tube o Ensure tissue perfusion but avoid volume overload o Prompt decompression for clinical evidence of pneumothorax or hemothorax • Abdominal injury - clinical signs can be subtle at first; observe for acute abdomen or sepsis • Ear injuries may include tinnitus or deafness • Crush injuries - sudden release of a crushed extremity may result in reperfusion syndrome (acute hypovolemia, renal failure, metabolic abnormalities) o IV fluid replacement (up to 1.5 L/hour) o To help prevent renal failure - mannitol to maintain diuresis at least 300 mL/hour; dialysis may be needed o To treat acidosis - IV sodium bicarbonate until urine pH reaches 6.5 (to prevent myoglobin and uric acid deposition in the kidneys) o To treat hyperkalemia/hypocalcemia - calcium gluconate 10% 10 mL or calcium chloride 10% 5 mL IV over two minutes; sodium bicarbonate 1 mEq/kg IV push (slowly); regular insulin 5-10 units and D5O 1-2 ampules IV bolus; kayexalate 25-50 g with sorbitol 20% 100 mL PO or PR • Monitor injured areas for the five Ps: pain, paresthesia, paralysis, pulse and pallor • Monitor for sepsis • Injuries resulting in non-intact skin or mucous membrane exposure - hepatitis B immunization (within seven days) and tetanus toxoid vaccine o • Natural Disasters & Severe Weather o Clustered under this category are earthquakes, extreme heat, floods, hurricanes, tornadoes, tsunamis, volcanoes, wildfires, landslides/mudslides and winter weather. o Traumatic events following natural disasters are characterized by a sense of horror, helplessness, serious injury or the threat of serious injury or death. • Radiation Emergencies o Radiation emergencies can be caused by radioactive material that contaminates food and/or water and bombs (such a dirty bombs) or other weapons of mass destruction. o The severity of signs and symptoms of radiation sickness depends on how much radiation has been absorbed. o Mild radiation sickness (absorbed dose of 1-2 Gy): nausea and vomiting, headache, fatigue, weakness within 24 to 48 hours after exposure o Very severe radiation sickness (absorbed dose of 3.5-5.5 Gy): nausea and vomiting less than 30 minutes after exposure to radiation, dizziness, disorientation, hypotension; usually fatal o Treatment overview: ▪ Decontamination: • Remove clothing and shoes • Gently wash victim with soap and water ▪ For damaged bone marrow: • Filgrastim (Neupogen): a protein-based medication which promotes the growth of white blood cells • Pegfilgrastim (Neulasta): also increases white blood cells and prevents subsequent infections ▪ For internal contamination (chelating agents): • Potassium iodide (KI): used to prevent absorption of radioiodine in the thyroid gland • Prussian blue: a type of dye that binds to particles of radioactive elements (cesium and thallium) • Diethylenetriaminepentaacetic acid (DTPA): binds to particles of the radioactive elements’ plutonium, americium and curium ▪ Supportive treatment for infections, headache, fever, diarrhea and dehydration; also end-of-life care • Disease Outbreaks o The more common foodborne outbreaks include Salmonella, Listeria and E. coli. o Other recent outbreaks include Ebola virus disease, Avian influenza, Middle East respiratory syndrome coronavirus (MERS-CoV), H1N1 and Zika virus. o Recent vaccine-preventable disease outbreaks include mumps, measles, polio and pertussis (whooping cough). • Terrorism & Disease o The following list of agents and/or diseases that may be used in a terrorist attack. The list is divided into three categories (as suggested by the Centers for Disease Control and Prevention) based primarily on mortality rates. ▪ Category A • Biological agents with the highest probability of mass dissemination or person-to-person transmission and high mortality rates. o Anthrax (Bacillus anthracis) o Botulism (Clostridium botulinumtoxin) o Plague (Yersinia pestis) o Smallpox (Variola major) o Tularemia (Francisella tularensis) o Viral hemorrhagic fevers, including Ebola, Marburg and Lassa ▪ Category B • Second highest priority agents, mostly due to lower morbidity and mortality rates: o Brucellosis (Brucella species) o Epsilon toxin of Clostridium perfringens o Food safety threats (including Salmonella species, Escherichia coli O157:H7, Shigella) o Glanders (Burkholderia mallei) o Melioidosis (Burkholderia pseudomallei) o Psittacosis (Chlamydia psittaci) o Q fever (Coxiella burnetii) o Ricin toxin from Ricinus communis (castor beans) o Staphylococcal enterotoxin B o Typhus fever (Rickettsia prowazekii) o Viral encephalitis (alphaviruses) o Venezuelan equine encephalitis o Water safety threats (such as Vibrio cholerae, Cryptosporidium parvum) ▪ Category C • Third highest priority agents, including emerging pathogens that could be engineered for mass dissemination in the future: o Nipah virus o Hantavirus Triage and Mass Casualties An emergency response plan includes information used to determine which client(s) to recommend for discharge in a disaster situation and identify nursing roles in disaster planning. All employees participate in disaster planning activities and drills and nurses should understand their responsibility in implementing emergency response plans for internal and external disasters. Regardless of the triage system used, the primary goal is to quickly sort victims into categories and identify each of them, using a tag, tape or some other means. Triage is intended to do the greatest good for the greatest amount of people. A common triage system for a mass casualty event is the START triage system. This system uses a red, yellow, green, black tag system. Community Setting Victims are categorized based on the severity of the injury, the urgency of needed treatment and an available place for treatment: ▪ Treated first: individuals who have life-threatening injuries that are readily correctable. ▪ Treated last: o Individuals who have no injuries (noncritical injuries) and who are ambulatory. o Individuals who are dying or are dead. Health Care Settings Triage in the emergency department usually involves dividing those who need care into one of the following three categories: • Emergent – individuals who have life-threatening injuries and need immediate attention are given the highest priority • Urgent – individuals with non-life-threatening injuries • Nonurgent – individuals with no immediate complications and who can wait for treatment [Show More]
Last updated: 1 year ago
Preview 1 out of 20 pages
Instant download

Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 19, 2023
Number of pages
20
Written in
Additional information
This document has been written for:
Uploaded
Jun 19, 2023
Downloads
0
Views
140













.png)
.png)