*NURSING > CASE STUDY > Diana Humphries _ Diabetic Ketoacidosis (DKA) _ UNFOLDING Reasoning Case Study: STUDENT | Diabetic (All)
Diana Humphries _ Diabetic Ketoacidosis (DKA) _ UNFOLDING Reasoning Case Study: STUDENT | Diabetic Ketoacidosis _UNFOLDING Reasoning Case Study LATEST
Document Content and Description Below
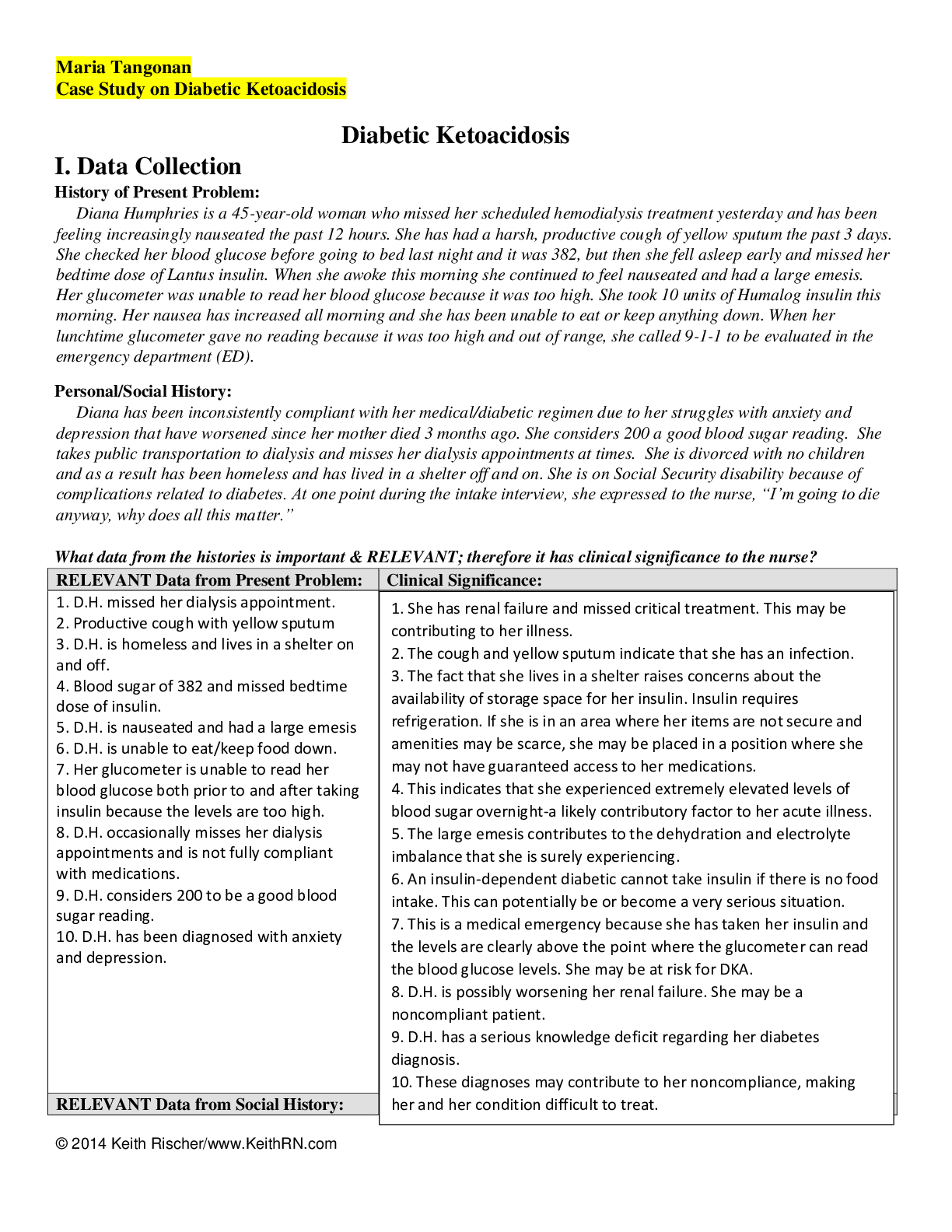
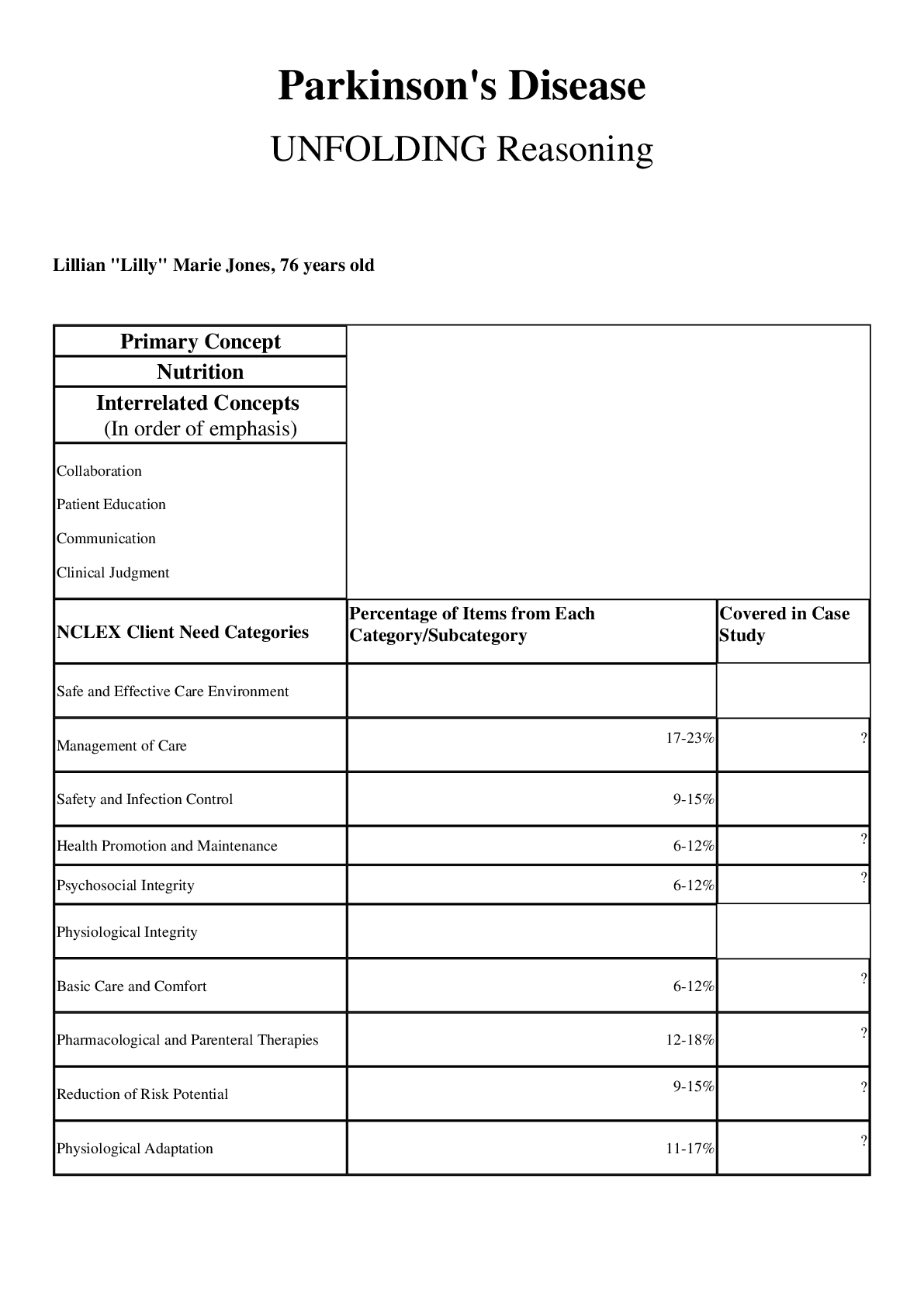
Diabetic Ketoacidosis (DKA) Diana Humphries, 45 years old Primary Concept Fluid and Electrolyte Balance Interrelated Concepts (In order of emphasis) 1. Acid-Base Balance ... 2. Glucose Regulation 3. Infection 4. Pain 5. Clinical Judgment 6. Patient Education 7. Communication 8. Collaboration UNFOLDING Reasoning Case Study: STUDENT Diabetic Ketoacidosis (DKA) History of Present Problem: Diana Humphries is a 45-year-old woman with chronic kidney disease stage III and diabetes mellitus type1 who checks her blood sugar daily, or whenever she feels like it. She has been feeling increasingly nauseated the past 12 hours. She has had a harsh, productive cough of yellow sputum the past three days. She checked her blood glucose before going to bed last night and it was 382, but then she fell asleep early and missed her bedtime dose of glargine (Lantus) insulin. When she awoke this morning, she had generalized abdominal pain and continued to feel nauseated and had a large emesis. Her glucometer was unable to read her blood glucose because it was too high. She took 10 units of lispro (Humalog) insulin this morning. Her nausea has increased all morning and she has been unable to eat or keep anything down despite having an increased thirst and appetite. She also has had increased frequency of urination. When her lunchtime glucometer gave no reading because it was too high and out of range, she called 9-1-1 to be evaluated in the emergency department (ED). Personal/Social History: Diana has been inconsistently compliant with her medical/diabetic regimen due to her struggles with anxiety and depression that have worsened since her mother died three months ago. She considers 200 a good blood sugar reading. She is divorced with no children and has been homeless and has lived in a shelter off and on the past month. She is on Social Security disability because of complications related to diabetes. At one point during the intake interview, she expressed to the nurse, “I’m going to die anyway, why does all this matter?” What data from the histories is RELEVANT and has clinical significance to the nurse? RELEVANT Data from Present Problem: Clinical Significance: Chronic Kidney Disease Type 1 Diabetes and checks blood sugar whenever she feels like it Blood Sugar 383 before bed and didn’t take her bedtime Lantus Generalized abdominal pain, nausea, emesis Increased thirst, appetite, urination Lunchtime glucometer gave no reading because too high Decreased function of the kidneys and if patient is in DKA there is an increased load on kidneys due to polyuria Puts her at risk for developing DKA especially since she doesn’t check her blood sugar regularly Blood sugar already high before bed so we know it was high for a while before she called 911 Signs and symptoms of hyperglycemia Signs and symptoms of hyperglycemia Severe hyperglycemia RELEVANT Data from Social History: Clinical Significance: Inconsistently compliant with her medical/diabetic regimen Anxiety and Depression from her mother’s death Divorced with no children Homeless Receives social security disability benefits Inability to comply with medications increases risk for complications. Doesn’t have emotional support Due to her current financial hardship, she is unable to comply with her medications and her diabetes regimen. What is the RELATIONSHIP of your patient’s past medical history (PMH) and current meds? (Which medication treats which condition? Draw lines to connect) PMH: Home Meds: Pharm. Classification: Expected Outcome: • Chronic Kidney disease stage III (diabetic nephropathy) • Anemia • Diabetes mellitus type 1 since age 12 • Diabetic retinopathy • Neuropathy in lower legs • Hyperlipidemia • Hypertension • Coronary artery disease • Gastroesophageal reflux disease (GERD) • Anxiety • Depression 1. Aspirin 81mg PO daily 2 .Lisinopril 10 mg PO daily 3. Lorazepam 1mg PO bid prn 4. Citalopram 40 PO mg daily 5. Zolpidem 10 mg PO at HS prn 6. Gabapentin 300 mg PO bid 7. Labetalol 200 mg PO bid 8. Omeprazole 20 mg PO daily 9 .Simvastatin 40 mg PO HS 10. Glargine insulin 50 units SQ at HS 11. Lispro insulin SQ sliding scale AC and HS Salicylates ACE inhibitors Benzodiazepine SSRI Sedative Analgesic adjunct Beta Blocker Antilipidemia Pancreatics Pancreatics Aspirin will help with the pain caused by her neuropathy. Lisinopril will help manage her hypertension and with her kidney disease. Lorazepam will help calm down the patient and make her less anxiety. Zolpidem will allow the patient to sleep better. Gabapentin will help with nerve pain caused by her neuropathy. Labetalol will help with her hypertension and decrease her heart rate decreasing stress on the heart. Omeprazole will decrease the stomach acid helping with her GERD. Simvastatin will help her cholesterol and lipids which will help with hyperlipidemia and coronary artery disease. Glargine is long acting insulin used to manage diabetes Lispro is rapid acting insulin used to manage diabetes - - - - - - - - - - Sodium: 125 Potassium: 5.1 Chloride: 106 CO2: 18 Glucose: 578 BUN: 50 Cr: 2.2 GFR: 24 Hyponatremia and hyperkalemia due to dehydration. Acidosis and BG above 400 are indications of DKA. Elevated BUN & Cr and low GFR due to impaired kidney function from CKD Stage 3. Worsening Improving Worsening Improving Improving Improving Improving Improving 12 Lead EKG: Interpretation: Sinus Rhythm Clinical Significance: Alterations in potassium can lead to cardiac dysrhythmias. Current VS: Most Recent: Current WILDA: T: 100.2 F/37.9 C (oral) T: 101.6 F/38.7 C (oral) Words: sharp P: 88 (regular) P: 114 (regular) Intensity: 2/10 R: 20 (regular) R 24 (regular) Location: Right chest BP: 124/70 BP: 102/66 Duration: Intermittent O2 sat: 94% 2 liters n/c O2 sat: 95% 2 liters n/c Aggravate: Alleviate: Coughing and deep breathing Not coughing and breathing shallow Current Assessment: GENERAL APPEARANCE: Resting comfortably, appears in no acute distress RESP: Breath sounds clear coarse crackles RLL, nonlabored respiratory effort CARDIAC: Pink, warm & dry, no edema, heart sounds regular with no abnormal beats, pulses strong, equal with palpation at radial/pedal/post-tibial landmarks NEURO: Alert & oriented to person, place, time, and situation (x4) GI: Abdomen soft/non-tender, bowel sounds audible per auscultation in all 4 quadrants, no nausea or abdominal pain GU: Urine clear and yellow. 250 mL the past 8 hours SKIN: Skin integrity intact, lips dry, but oral mucosa is moist 1. What clinical data is RELEVANT that must be recognized as clinically significant? RELEVANT VS Data: Clinical Significance: T: 100.2 F/37.9 C (oral) P:88 R:20 BP: 124/70 O2 Sat: 94% via 2L NC Vital signs are showing improvement RELEVANT Assessment Data: Clinical Significance: Resting comfortably with no acute distress Clear coarse crackles UO 250mL in last 8 hours Shows improvement Fluid excess probably due to pneumonia normal 2. Has the status improved or not as expected to this point? Shows improvement 3. Does your nursing priority or plan of care need to be modified in any way after this evaluation assessment? Remain the same 4. Based on your current evaluation, what are your nursing priorities and plan of care? Current nursing priorities are to monitor the patient for any changes in status. Continue medications and treatments as prescribed Watch labs closely for improving or worsening trend Effective and concise handoffs are essential to excellent care and if not done well can adversely impact the care of this patient. You have done an excellent job to this point, now finish strong and give the following SBAR report to the nurse who will be caring for this patient in ICU: Situation: Name/age: Diana Humphries, 45-year-old female BRIEF summary of primary problem: Patient presented to the emergency department due to highly elevated blood glucose. Day of admission/post-op #: Day 1 Background: Primary problem/diagnosis: DKA RELEVANT past medical history: CKD Stage III and Diabetes Mellitus Type I RELEVANT background data: Homeless, receives social security benefits, divorced and no children Assessment: Current vital signs:T: 100.2 F/37.9 C (oral), P: 88, R: 20, BP: 124/70 , and O2 Sat: 94% via 2L NC RELEVANT body system nursing assessment data: RESP: Breath sounds clear coarse crackles RLL, non-labored respiratory effort RELEVANT lab values: Sodium: 125, Potassium: 5.1, Chloride: 106, CO2: 18, Glucose: 578, BUN: 50, Cr: 2.2, GFR: 24 TREND of any abnormal clinical data (stable-increasing/decreasing): Stable How have you advanced the plan of? Administered fluid replacement and insulin. Patient response: Patients blood glucose is going down vital signs and vital signs and normalizing INTERPRETATION of current clinical status (stable/unstable/worsening): Stable Recommendation: Suggestions to advance plan of care: Monitor blood glucose, LOC, vital signs and strict I&Os. Monitor acid-base balance. Educate client how to prevent DKA. Education Priorities/Discharge Planning 1. What will be the most important discharge/education priorities you will reinforce with her medical condition to prevent future readmission with the same problem? Monitor blood sugar and take insulin as prescribed. Finish full course of antibiotics to treat pneumonia infection. 2. What are some practical ways you as the nurse can assess the effectiveness of your teaching with this patient? Have the patient summarize the teachings you provided. Ask questions to see if the patient understood teachings. Caring and the “Art” of Nursing 1. What is the patient likely experiencing/feeling right now in this situation? She might feel alone and maybe she doesn’t have motivation or anything to forward too. The patient’s mother recently passed away, she is divorced and has no children. 2. What can you do to engage yourself with this patient’s experience and show that he/she matters to you as a person? Build a connection with the patient by talking with her about things she likes. Regularly check up on the patient to see if there is anything she needs or something that I can do for her. Also provide physical touch to demonstrate that I care about her and provide comfort if she is okay with that. Use Reflection to THINK Like a Nurse Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention in the moment as the events are unfolding to make a correct clinical judgment. 1. What did I learn from this scenario? I learned how important it is for someone with diabetes to take care of themselves and how quickly it can go downhill. Also, dehydration, infection, inadequate insulin dose, and stress can all cause diabetic ketoacidosis 2. How can I use what has been learned from this scenario to improve patient care in the future? This will help in the future clinical setting by being able to identify those at risk of developing DKA. [Show More]
Last updated: 1 year ago
Preview 1 out of 22 pages
Instant download
 - Baptist Health College.png)
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Feb 21, 2021
Number of pages
22
Written in
Additional information
This document has been written for:
Uploaded
Feb 21, 2021
Downloads
0
Views
85



 Pneumonia Chronic Obstructive Pulmonary Disease Clinical Reasoning Case Study Medical surgical (NUR 201) Pneumonia-COPD case study solutions.png)