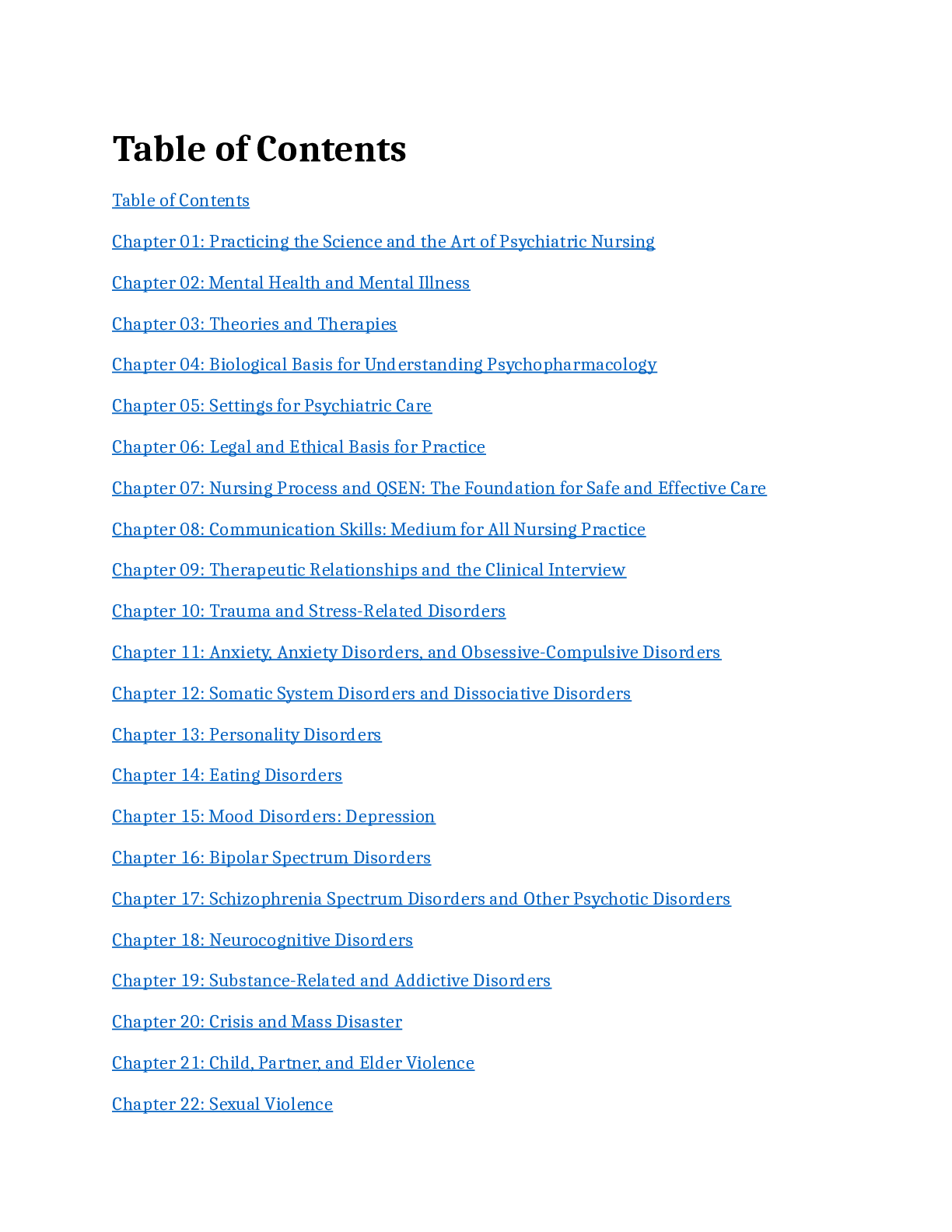
*NURSING > QUESTIONS and ANSWERS > Essentials of Psychiatric Mental Health Nursing 8th Edition Concepts of Care in Evidence- Based Prac (All)
Essentials of Psychiatric Mental Health Nursing 8th Edition Concepts of Care in Evidence- Based Practice 8th Edition Morgan Townsend Test Bank | Latest 2023
Document Content and Description Below
Essentials of Psychiatric Mental Health Nursing 8th Edition Concepts of Care in Evidence- Based Practice 8th Edition Morgan Townsend Test Bank Chapter 1. Mental Health and Mental Illness Multiple... Choice 1. A nurse is assessing a client who is experiencing occasional feelings of sadness because of the recent death of a beloved pet. The clients appetite, sleep patterns, and daily routine have not changed. How should the nurse interpret the clients behaviors? 1. The clients behaviors demonstrate mental illness in the form of depression. 2. The clients behaviors are extensive, which indicates the presence of mental illness. 3. The clients behaviors are not congruent with cultural norms. 4. The clients behaviors demonstrate no functional impairment, indicating no mental illness. ANS: 4 Rationale: The nurse should assess that the clients daily functioning is not impaired. The client who experiences feelings of sadness after the loss of a pet is responding within normal expectations. Without significant impairment, the clients distress does not indicate a mental illness. Cognitive Level: Analysis Integrated Process: Assessment 2. At what point should the nurse determine that a client is at risk for developing a mental illness? 1. When thoughts, feelings, and behaviors are not reflective of the DSM-5 criteria. 2. When maladaptive responses to stress are coupled with interference in daily functioning. 3. When a client communicates significant distress. 4. When a client uses defense mechanisms as ego protection. ANS: 2 Rationale: The nurse should determine that the client is at risk for mental illness when responses to stress are maladaptive and interfere with daily functioning. The DSM-5 indicates that in order to be diagnosed with a mental illness, daily functioning must be significantly impaired. The clients ability to communicate distress would be considered a positive attribute. Cognitive Level: Application Integrated Process: Assessment 3. A nurse is assessing a set of 15-year-old identical twins who respond very differently to stress. One twin becomes anxious and irritable, and the other withdraws and cries. How should the nurse explain these different stress responses to the parents? 1. Reactions to stress are relative rather than absolute; individual responses to stress vary. 2. It is abnormal for identical twins to react differently to similar stressors. 3. Identical twins should share the same temperament and respond similarly to stress. 4. Environmental influences to stress weigh more heavily than genetic influences. ANS: 1 Rationale: The nurse should explain to the parents that, although the twins have identical DNA, there are several other factors that affect reactions to stress. Mental health is a state of being that is relative to the individual client. Environmental influences and temperament can affect stress reactions. Cognitive Level: Application Integrated Process: Implementation 4. Which client should the nurse anticipate to be most receptive to psychiatric treatment? 1. A Jewish, female social worker. 2. A Baptist, homeless male. 3. A Catholic, black male. 4. A Protestant, Swedish business executive. ANS: 1 Rationale: The nurse should anticipate that the client of Jewish culture would place a high importance on preventative health care and would consider mental health as equally important as physical health. Women are also more likely to seek treatment for mental health problems than men. Cognitive Level: Application Integrated Process: Planning 5. A psychiatric nurse intern states, This clients use of defense mechanisms should be eliminated. Which is a correct evaluation of this nurses statement? 1. Defense mechanisms can be appropriate responses to stress and need not be eliminated. 2. Defense mechanisms are a maladaptive attempt of the ego to manage anxiety and should always be eliminated. 3. Defense mechanisms, used by individuals with weak ego integrity, should be discouraged and not eliminated. 4. Defense mechanisms cause disintegration of the ego and should be fostered and encouraged. ANS: 1 Rationale: The nurse should determine that defense mechanisms can be appropriate during times of stress. The client with no defense mechanisms may have a lower tolerance for stress, thus leading to anxiety disorders. Defense mechanisms should be confronted when they impede the client from developing healthy coping skills. Cognitive Level: Application Integrated Process: Evaluation 6. During an intake assessment, a nurse asks both physiological and psychosocial questions. The client angrily responds, Im here for my heart, not my head problems. Which is the nurses best response? 1. Its just a routine part of our assessment. All clients are asked these same questions. 2. Why are you concerned about these types of questions? 3. Psychological factors, like excessive stress, have been found to affect medical conditions. 4. We can skip these questions, if you like. It isnt imperative that we complete this section. ANS: 3 Rationale: The nurse should attempt to educate the client on the negative effects of excessive stress on medical conditions. It is not appropriate to skip physiological and psychosocial questions, as this would lead to an inaccurate assessment. Cognitive Level: Application Integrated Process: Implementation 7. An employee uses the defense mechanism of displacement when the boss openly disagrees with suggestions. What behavior would be expected from this employee? 1. The employee assertively confronts the boss. 2. The employee leaves the staff meeting to work out in the gym. 3. The employee criticizes a coworker. 4. The employee takes the boss out to lunch. ANS: 3 Rationale: The nurse should expect that the client using the defense mechanism displacement would criticize a coworker after being confronted by the boss. Displacement refers to transferring feelings from one target to a neutral or less-threatening target. Cognitive Level: Analysis Integrated Process: Assessment 8. A fourth-grade boy teases and makes jokes about a cute girl in his class. This behavior should be identified by a nurse as indicative of which defense mechanism? 1. Displacement 2. Projection 3. Reaction formation 4. Sublimation ANS: 3 Rationale: The nurse should identify that the boy is using reaction formation as a defense mechanism. Reaction formation is the attempt to prevent undesirable thoughts from being expressed by expressing opposite thoughts or behaviors. Displacement refers to transferring feelings from one target to another. Rationalization refers to making excuses to justify behavior. Projection refers to the attribution of unacceptable feelings or behaviors to another person. Sublimation refers to channeling unacceptable drives or impulses into more constructive, acceptable activities. Cognitive Level: Application Integrated Process: Assessment 9. Which nursing statement about the concept of neurosis is most accurate? 1. An individual experiencing neurosis is unaware that he or she is experiencing distress. 2. An individual experiencing neurosis feels helpless to change his or her situation. 3. An individual experiencing neurosis is aware of psychological causes of his or her behavior. 4. An individual experiencing neurosis has a loss of contact with reality. ANS: 2 Rationale: The nurse should define the concept of neurosis with the following characteristics: The client feels helpless to change his or her situation, the client is aware that he or she is experiencing distress, the client is aware the behaviors are maladaptive, the client is unaware of the psychological causes of the distress, and the client experiences no loss of contact with reality. Cognitive Level: Application Integrated Process: Assessment 10. Which nursing statement regarding the concept of psychosis is most accurate? 1. Individuals experiencing psychoses are aware that their behaviors are maladaptive. 2. Individuals experiencing psychoses experience little distress. 3. Individuals experiencing psychoses are aware of experiencing psychological problems. 4. Individuals experiencing psychoses are based in reality. ANS: 2 Rationale: The nurse should understand that the client with psychosis experiences little distress owing to his or her lack of awareness of reality. The client with psychosis is unaware that his or her behavior is maladaptive or that he or she has a psychological problem. Cognitive Level: Application Integrated Process: Assessment 11. When under stress, a client routinely uses alcohol to excess. Finding her drunk, her husband yells at the client about her chronic alcohol abuse. Which action alerts the nurse to the clients use of the defense mechanism of denial? 1. The client hides liquor bottles in a closet. 2. The client yells at her son for slouching in his chair. 3. The client burns dinner on purpose. 4. The client says to the spouse, I dont drink too much! ANS: 4 Rationale: The clients statement I dont drink too much! alerts the nurse to the use of the defense mechanism of denial. The client is refusing to acknowledge the existence of a real situation and the feelings associated with it. Cognitive Level: Application Integrated Process: Assessment 12. Devastated by a divorce from an abusive husband, a wife completes grief counseling. Which statement by the wife should indicate to a nurse that the client is in the acceptance stage of grief? 1. If only we could have tried again, things might have worked out. 2. I am so mad that the children and I had to put up with him as long as we did. 3. Yes, it was a difficult relationship, but I think I have learned from the experience. 4. I still dont have any appetite and continue to lose weight. ANS: 3 Rationale: The nurse should evaluate that the client is in the acceptance stage of grief because during this stage of the grief process, the client would be able to focus on the reality of the loss and its meaning in relation to life. Cognitive Level: Analysis Integrated Process: Evaluation 13. A nurse is performing a mental health assessment on an adult client. According to Maslows hierarchy of needs, which client action would demonstrate the highest achievement in terms of mental health?1. Maintaining a long-term, faithful, intimate relationship.2. Achieving a sense of self-confidence.3. Possessing a feeling of self-fulfillment and realizing full potential.4. Developing a sense of purpose and the ability to direct activities. ANS: 3 Rationale: The nurse should identify that the client who possesses a feeling of self-fulfillment and realizes his or her full potential has achieved self-actualization, the highest level on Maslows hierarchy of needs. Cognitive Level: Application Integrated Process: Assessment 14. According to Maslows hierarchy of needs, which situation on an in-patient psychiatric unit would require priority intervention by a nurse?1. A client rudely complaining about limited visiting hours.2. A client exhibiting aggressive behavior toward another client.3. A client stating that no one cares. 4. A client verbalizing feelings of failure. ANS: 2 Rationale: The nurse should immediately intervene when a client exhibits aggressive behavior toward another client. Safety and security are considered lower-level needs according to Maslows hierarchy of needs and must be fulfilled before other higher-level needs can be met. Clients who complain, have feelings of failure, or state that no one cares are struggling with higher-level needs such as the need for love and belonging or the need for self-esteem. Cognitive Level: Analysis Integrated Process: Evaluation 15. How would a nurse best complete the new DSM-5 definition of a mental disorder? A health condition characterized by significant dysfunction in an individuals cognitions, or behaviors that reflects a disturbance in the 1. psychosocial, biological, or developmental process underlying mental functioning. 2. psychological, cognitive, or developmental process underlying mental functioning. 3. psychological, biological, or developmental process underlying mental functioning. 4. psychological, biological, or psychosocial process underlying mental functioning. ANS: 3 Rationale: A health condition characterized by significant dysfunction in an individuals cognitions, or behaviors that reflects a disturbance in the psychological, biological, or developmental process underlying mental functioning, is the new DSM 5 definition of a mental disorder. Cognitive Level: Application Integrated Process: Assessment Multiple Response 16. A nurse is assessing a client who appears to be experiencing some anxiety during questioning. Which symptoms might the client demonstrate that would indicate anxiety? (Select all that apply.) 1. Fidgeting 2. Laughing inappropriately 3. Palpitations 4. Nail biting 5. Limited attention span ANS: 1, 2, 4 Rationale: The nurse should assess that fidgeting, laughing inappropriately, and nail biting are indicative of heightened stress levels. The client would not be diagnosed with mental illness unless there is significant impairment in other areas of daily functioning. Other indicators of more serious anxiety are restlessness, difficulty concentrating, muscle tension, and sleep disturbance. Cognitive Level: Application Integrated Process: Assessment Fill-in-the-Blank 17. is a diffuse apprehension that is vague in nature and is associated with feelings of uncertainty and helplessness. ANS: Anxiety Rationale: The definition of anxiety is a diffuse apprehension that is vague in nature and is associated with feelings of uncertainty and helplessness. Townsend considers this a core concept. Cognitive Level: Application Integrated Process: Assessment 18. is a subjective state of emotional, physical, and social responses to the loss of a valued entity. ANS: Grief Rationale: The definition of grief is a subjective state of emotional, physical, and social responses to the loss of a valued entity. Townsend considers this a core concept. Chapter 2. Biological Implications Multiple Choice 1. A depressed client states, I have a chemical imbalance in my brain. I have no control over my behavior. Medications are my only hope to feel normal again. Which nursing response is appropriate?1. Medications only address biological factors. Environmental and interpersonal factors must also be considered.2. Because biological factors are the sole cause of depression, medications will improve your mood.3. Environmental factors have been shown to exert the most influence in the development of depression.4. Researchers have been unable to demonstrate a link between nature (biology and genetics) and nurture (environment). ANS: 1 Rationale: The nurse should advise the client that medications address biological factors, but there are other factors that affect mood. The nurse should educate the client on environmental and interpersonal factors that can lead to depression. Cognitive Level: Analysis Integrated Process: Implementation 2. A client diagnosed with major depressive disorder asks, What part of my brain controls my emotions? Which nursing response is appropriate?1. The occipital lobe governs perceptions, judging them as positive or negative.2. The parietal lobe has been linked to depression.3. The medulla regulates key biological and psychological activities.4. The limbic system is largely responsible for ones emotional state. ANS: 4 Rationale: The nurse should explain to the client that the limbic system is largely responsible for ones emotional state. This system if often called the emotional brain and is associated with feelings, sexuality, and social behavior. The occipital lobes are the area of visual reception and interpretation. Somatosensory input (touch, taste, temperature, etc.) occurs in the parietal lobes. The medulla contains vital centers that regulate heart rate and reflexes. Cognitive Level: Application Integrated Process: Implementation 3. Which part of the nervous system should a nurse identify as playing a major role during stressful situations? 1. Peripheral nervous system 2. Somatic nervous system 3. Sympathetic nervous system 4. Parasympathetic nervous system ANS: 3 Rationale: The nurse should identify that the sympathetic nervous system plays a major role during stressful situations. The sympathetic nervous system prepares the body for the fight-or- flight response. The parasympathetic nervous system is dominant when an individual is in a nonstressful state. Cognitive Level: Comprehension Integrated Process: Assessment 4. Which client statement reflects an understanding of circadian rhythms in psychopathology?1. When I dream about my mothers horrible train accident, I become hysterical. 2. I get really irritable during my menstrual cycle.3. Im a morning person. I get my best work done before noon. 4. Every February, I tend to experience periods of sadness. ANS: 3 Rationale: By stating, I am a morning person, the client demonstrates an understanding that circadian rhythms may influence a variety of regulatory functions, including the sleep-wake cycle, regulation of body temperature, and patterns of activity. Most humans follow a 24-hour cycle that is largely affected by lightness and darkness. Cognitive Level: Analysis Integrated Process: Evaluation 5. Which types of adoption studies should a nurse recognize as providing useful information for the psychiatric community? 1. Studies in which children with mentally ill biological parents are raised by adoptive parents who were mentally healthy.2. Studies in which children with mentally healthy biological parents are raised by adoptive parents who were mentally ill. 3. Studies in which monozygotic twins from mentally ill parents were raised separately by different adoptive parents.4. Studies in which monozygotic twins were raised together by mentally ill biological parents. 5. All of the above. ANS: 5 Rationale: The nurse should determine that all of the studies could possibly benefit the psychiatric community. The studies may reveal research findings relating genetic links to mental illness. Adoption studies allow comparisons to be made of the influences of the environment versus genetics. Cognitive Level: Analysis Integrated Process: Evaluation 6. Six months after her husband and children were killed in a car accident, a client is diagnosed with ulcerative colitis. The nurse should recognize that this situation validates which study perspective? 1. Neuroendocrinology 2. Psychoimmunology3. Diagnostic technology4. Neurophysiology ANS: 2 Rationale: Psychoimmunology is the branch of medicine that studies the effects of social and psychological factors on the functioning of the immune system. Studies of the biological response to stress hypothesize that individuals become more susceptible to physical illness following exposure to stressful stimuli. Cognitive Level: Application Integrated Process: Evaluation 7. A withdrawn client, diagnosed with schizophrenia, expresses little emotion and refuses to attend group therapy. What altered component of the nervous system should a nurse recognize as being responsible for this behavior? 1. Dendrites2. Axons3. Neurotransmitters4. Synapses ANS: 3 Rationale: The nurse should recognize that neurotransmitters play an essential function in the role of human emotion and behavior. Neurotransmitters are targeted and affected by many psychotropic medications. Cognitive Level: Comprehension Integrated Process: Evaluation 8. An instructor is teaching nursing students about neurotransmitters. Which best explains the process of how neurotransmitters released into the synaptic cleft may return to the presynaptic neuron?1. Regeneration2. Reuptake3. Recycling4. Retransmission ANS: 2 Rationale: The nursing instructor should explain that the process by which neurotransmitters are released into the synaptic cleft and returned to the presynaptic neuron is termed reuptake. Reuptake is the process by which neurotransmitters are stored for reuse. Cognitive Level: Comprehension Integrated Process: Implementation 9. A nurse concludes that a restless, agitated client is manifesting a fight- or-flight response. The nurse should associate this response with which neurotransmitter?1. Acetylcholine2. Dopamine3. Serotonin4. Norepinephrine ANS: 4 Rationale: The nurse should associate the neurotransmitter norepinephrine with the fight-or- flight response. Norepinephrine produces activity in the sympathetic postsynaptic nerve terminal and is associated with the regulation of mood, cognition, perception, locomotion, and sleep and arousal. Cognitive Level: Comprehension Integrated Process: Assessment 10. A client is admitted to a psychiatric unit with the diagnosis of catatonic schizophrenia. Which of the clients neurotransmitters should a nurse expect to be elevated?1. Serotonin 2. Dopamine 3. Gamma-aminobutyric acid (GABA) 4. Histamine ANS: 2 Rationale: The nurse should expect that elevated dopamine levels might be an attributing factor to the clients current level of functioning. Dopamine functions include regulation of movements and coordination, emotions, and voluntary decision-making ability. Cognitive Level: Application Integrated Process: Assessment 11. A clients wife of 34 years dies unexpectedly. The client cries often and becomes socially isolated. The clients therapist encourages open discussion of feelings, proper nutrition, and exercise. What is the best rationale for the therapists recommendations? 1. The therapist is using an interpersonal approach.2. The client has an alteration in neurotransmitters. 3. It is routine practice to remind clients about nutrition, exercise, and rest.4. The client is susceptible to illness because of effects of stress on the immune system. ANS: 4 Rationale: The therapists recommendations should be based on the knowledge that the client has been exposed to stressful stimuli and is at an increased risk to develop illness because of the effects of stress on the immune system. The study of this branch of medicine is called psychoimmunology. Cognitive Level: Application Integrated Process: Planning 12. Which mental illness should a nurse identify as being associated with a decrease in prolactin hormone level? 1. Major depressive episode2. Schizophrenia 3. Anorexia nervosa4. Alzheimers disease ANS: 2 Rationale: Although the exact mechanism is unknown, there may be some correlation between decreased levels of the hormone prolactin and schizophrenia. Cognitive Level: Application Integrated Process: Evaluation 13. Which cerebral structure should a nursing instructor describe to students as the emotional brain?1. The cerebellum2. The limbic system3. The cortex4. The left temporal lobe ANS: 2 Rationale: The limbic system is often referred to as the emotional brain. The limbic system is largely responsible for ones emotional state and is associated with feelings, sexuality, and social behavior. Cognitive Level: Comprehension Integrated Process: Implementation 14. A nurse understands that the abnormal secretion of growth hormone may play a role in which illness?1. Acute mania2. Schizophrenia3. Anorexia nervosa4. Alzheimers disease ANS: 3 Rationale: The nurse should understand that research has found a correlation between abnormal levels of growth hormone and anorexia nervosa. The growth hormone is responsible for growth in children, as well as continued protein synthesis throughout life. Cognitive Level: Comprehension Integrated Process: Assessment 15. A client is admitted to an emergency department experiencing memory deficits and decreased motor function. What alteration in brain chemistry should a nurse correlate with the production of these symptoms? 1. Abnormal levels of serotonin2. Decreased levels of dopamine3. Increased levels of norepinephrine 4. Decreased levels of acetylcholine ANS: 4 Rationale: The nurse should correlate memory deficits and decreased motor function with decreased levels of acetylcholine. Acetylcholine is a major effector chemical of the autonomic nervous system. Functions of acetylcholine include sleep regulation, pain perception, the modulation and coordination of movement, and memory. Cognitive Level: Application Integrated Process: Assessment 16. A nurse should recognize that a decrease in norepinephrine levels would play a significant role in which mental illness?1. Bipolar disorder: mania2. Schizophrenia spectrum disorder3. Generalized anxiety disorder4. Major depressive episode ANS: 4 Rationale: The nurse should recognize that a decrease in norepinephrine level would play a significant role in the development of major depressive disorder. The functions of norepinephrine include the regulation of mood, cognition, perception, locomotion, cardiovascular functioning, and sleep and arousal. Cognitive Level: Application Integrated Process: Evaluation 17. A nurse should expect that an increase in dopamine activity might play a significant role in the development of which mental illness?1. Schizophrenia spectrum disorder2. Major depressive disorder3. Body dysmorphic disorder4. Parkinsons disease ANS: 1 Rationale: The nurse should expect that an increase in dopamine activity might play a significant role in the development of schizophrenia spectrum disorder. Functions of dopamine include regulation of emotions, coordination, and voluntary decision-making ability. Increased dopamine activity is also associated with mania. Cognitive Level: Application Integrated Process: Evaluation Multiple Response 18. Which of the following information should a nurse include when explaining causes of anorexia nervosa to a client? (Select all that apply.)1. There is a possible correlation between abnormal secretion of growth hormone and anorexia nervosa. 2. There is a possible correlation between antidiuretic hormone levels and anorexia nervosa. 3. There is a possible correlation between low levels of gonadotropin and anorexia nervosa. 4. There is a possible correlation between increased levels of prolactin and anorexia nervosa. 5. There is a possible correlation between altered levels of oxytocin and anorexia nervosa. ANS: 1, 3 Rationale: The nurse should explain to the client that there is a possible correlation between anorexia nervosa and decreased levels of growth hormones and gonadotropin. Anorexia nervosa has also been correlated with increased cortisol levels. Cognitive Level: Application Integrated Process: Implementation 19. Which of the following symptoms should a nurse associate with the development of increased levels of thyroid-stimulating hormone (TSH) in a newly admitted client? (Select all that apply.)1. Depression2. Fatigue3. Increased libido4. Mania5. Hyperexcitability ANS: 1, 2 Rationale: The nurse should associate depression and fatigue with increased levels of TSH. TSH is only increased when thyroid levels are low, as in the diagnosis of hypothyroidism. In addition to depression and fatigue, other symptoms, such as decreased libido, memory impairment, and suicidal ideation are associated with chronic hypothyroidism. Cognitive Level: Application Integrated Process: Assessment Fill-in-the-Blank 20. is the study of the biological foundations of cognitive, emotional, and behavioral processes. ANS: Psychobiology Rationale: Psychobiology is the study of the biological foundations of cognitive, emotional, and behavioral processes. In recent years, a greater emphasis has been placed on the study of the organic basis for psychiatric illness. Chapter 3. Ethical and Legal Issues Multiple Choice 1. In response to a students question regarding choosing a psychiatric specialty, a charge nurse states, Mentally ill clients need special care. If I were in that position, Id want a caring nurse also. From which ethical framework is the charge nurse operating? 1. Kantianism 2. Christian ethics 3. Ethical egoism 4. Utilitarianism ANS: 2 Rationale: The charge nurse is operating from a Christian ethics framework. The imperative demand of Christian ethics is that all decisions about right and wrong should be centered in love for God and in treating others with the same respect and dignity with which we would expect to be treated. Kantianism states that decisions should be made based on moral law and that actions are bound by a sense of moral duty. Utilitarianism holds that decisions should be made focusing on the end result being happiness. Ethical egoism promotes the idea that what is right is good for the individual. Cognitive Level: Analysis Integrated Process: Assessment 2. During a hiring interview, which response by a nursing applicant should indicate that the applicant operates from an ethical egoism framework? 1. I would want to be treated in a caring manner if I were mentally ill. 2. This job will pay the bills, and the workload is light enough for me. 3. I will be happy caring for the mentally ill. Working in med/surg kills my back. 4. It is my duty in life to be a psychiatric nurse. It is the right thing to do. ANS: 2 Rationale: The applicants comment reflects the ethical egoism framework. This framework promotes the idea that decisions are made based on what is good for the individual and may not take the needs of others into account. Cognitive Level: Analysis Integrated Process: Evaluation 3. Without authorization, a nurse administers an extra dose of narcotic tranquilizer to an agitated client. The nurses coworker observes this action but does nothing for fear of retaliation. What is the ethical interpretation of the coworkers lack of involvement? 1. Taking no action is still considered an unethical action by the coworker. 2. Taking no action releases the coworker from ethical responsibility. 3. Taking no action is advised when potential adverse consequences are foreseen. 4. Taking no action is acceptable, because the coworker is only a bystander. ANS: 1 Rationale: The coworkers lack of involvement can be interpreted as an unethical action. The coworker is experiencing an ethical dilemma in which a decision needs to be made between two unfavorable alternatives. The coworker has a responsibility to report any observed unethical actions. Cognitive Level: Analysis Integrated Process: Implementation 4. Group therapy is strongly encouraged, but not mandatory, in an inpatient psychiatric unit. The unit managers policy is that clients can make a choice about whether or not to attend group therapy. Which ethical principle does the unit managers policy preserve? 1. Justice 2. Autonomy 3. Veracity 4. Beneficence ANS: 2 Rationale: The unit managers policy regarding voluntary client participation in group therapy preserves the ethical principle of autonomy. The principle of autonomy presumes that individuals are capable of making independent decisions for themselves and that health-care workers must respect these decisions. Cognitive Level: Application Integrated Process: Implementation 5. Which is an example of an intentional tort? 1. A nurse fails to assess a clients obvious symptoms of neuroleptic malignant syndrome. 2. A nurse physically places an irritating client in four-point restraints. 3. A nurse makes a medication error and does not report the incident. 4. A nurse gives patient information to an unauthorized person. ANS: 2 Rationale: A tort, which can be intentional or unintentional, is a violation of civil law in which an individual has been wronged. A nurse who intentionally physically places an irritating client in restraints has touched the client without consent and has committed an intentional tort. Cognitive Level: Application Integrated Process: Evaluation 6. An involuntarily committed client is verbally abusive to the staff, repeatedly threatening to sue. The client records the full names and phone numbers of the staff. Which nursing action is most appropriate to decrease the possibility of a lawsuit? 1. Verbally redirect the client, and then refuse one-on-one interaction. 2. Involve the hospitals security division as soon as possible. 3. Notify the client that documenting personal staff information is against hospital policy. 4. Continue professional attempts to establish a positive working relationship with the client. ANS: 4 Rationale: The most appropriate nursing action is to continue professional attempts to establish a positive working relationship with the client. The involuntarily committed client should be respected and has the right to assert grievances if rights are infringed. Cognitive Level: Analysis Integrated Process: Implementation 7. Which statement should a nurse identify as correct regarding a clients right to refuse treatment? 1. Clients can refuse pharmacological but not psychological treatment. 2. Clients can refuse any treatment at any time. 3. Clients can refuse only electroconvulsive therapy (ECT). 4. Professionals can override treatment refusal by an actively suicidal or homicidal client. ANS: 4 Rationale: The nurse should understand that health-care professionals could override treatment refusal when a client is actively suicidal or homicidal. A suicidal or homicidal client who refuses treatment may be in danger or a danger to others. This situation should be treated as an emergency, and treatment may be performed without informed consent. Cognitive Level: Application Integrated Process: Evaluation 8. Which potential client should a nurse identify as a candidate for involuntarily commitment? 1. The client living under a bridge in a cardboard box 2. The client threatening to commit suicide 3. The client who never bathes and wears a wool hat in the summer 4. The client who eats waste out of a garbage can ANS: 2 Rationale: The nurse should identify the client threatening to commit suicide as eligible for involuntary commitment. The suicidal client who refuses treatments is in danger and needs emergency treatment. Cognitive Level: Application Integrated Process: Assessment 9. A client diagnosed with schizophrenia refuses to take medication, citing the right of autonomy. Under which circumstance would a nurse have the right to medicate the client against the clients wishes? 1. A client makes inappropriate sexual innuendos to a staff member. 2. A client constantly demands attention from the nurse by begging, Help me get better. 3. A client physically attacks another client after being confronted in group therapy. 4. A client refuses to bathe or perform hygienic activities. ANS: 3 Rationale: The nurse would have the right to medicate a client against his or her wishes if the client physically attacks another client. This client poses a significant risk to safety and is incapable of making informed choices. The clients refusal to accept treatment can be challenged, because the client is endangering the safety of others. Cognitive Level: Application Integrated Process: Implementation 10. A psychiatric nurse working on an inpatient unit receives a call asking if an individual has been a client in the facility. Which nursing response reflects appropriate legal and ethical obligations? 1. The nurse refuses to give any information to the caller, citing rules of confidentiality. 2. The nurse hangs up on the caller. 3. The nurse confirms that the person has been at the facility but adds no additional information. 4. The nurse suggests that the caller speak to the clients therapist. ANS: 1 Rationale: The most appropriate action by the nurse is to refuse to give any information to the caller. Admission to the facility would be considered protected health information (PHI) and should not be disclosed by the nurse without prior client consent. Cognitive Level: Application Integrated Process: Implementation 11. A client requests information on several medications in order to make an informed choice about management of depression. A nurse should provide this information to facilitate which ethical principle? 1. Autonomy 2. Beneficence 3. Nonmaleficence 4. Justice ANS: 1 Rationale: The nurse should provide the information to support the clients autonomy. A client who is capable of making independent choices should be permitted to do so. In instances when clients are incapable of making informed decisions, a legal guardian or representative would be asked to give consent. Cognitive Level: Application Integrated Process: Implementation 12. An inpatient psychiatric physician refuses to treat clients without insurance and prematurely discharges those whose insurance benefits have expired. Which ethical principle should a nurse determine has been violated based on these actions? 1. Autonomy 2. Beneficence 3. Nonmaleficence 4. Justice ANS: 4 Rationale: The nurse should determine that the ethical principle of justice has been violated by the physicians actions. The principle of justice requires that individuals should be treated equally, regardless of race, sex, marital status, medical diagnosis, social standing, economic level, or religious belief. Cognitive Level: Application Integrated Process: Evaluation 13. Which situation reflects violation of the ethical principle of veracity? 1. A nurse discusses with a client another clients impending discharge. 2. A nurse refuses to give information to a physician who is not responsible for the clients care. 3. A nurse tricks a client into seclusion by asking the client to carry linen to the seclusion room. 4. A nurse does not treat all of the clients equally, regardless of illness severity. ANS: 3 Rationale: The nurse who tricks a client into seclusion has violated the ethical principle of veracity. The principle of veracity refers to ones duty to always be truthful and not intentionally deceive or mislead clients. Cognitive Level: Application Integrated Process: Implementation 14. A client who will be receiving electroconvulsive therapy (ECT) must provide informed consent. Which situation should cause a nurse to question the validity of the informed consent? 1. The client is paranoid. 2. The client is 87 years old. 3. The client incorrectly reports his or her spouses name, date, and time of day. 4. The client relies on his or her spouse to interpret the information. ANS: 3 Rationale: The nurse should question the validity of informed consent when the client incorrectly reports the spouses name, date, and time of day. This indicates that this client is disoriented and may not be competent to make informed choices. Cognitive Level: Application Integrated Process: Assessment 15. A client diagnosed with schizophrenia receives fluphenazine decanoate (Prolixin Decanoate) from a home health nurse. The client refuses medication at one regularly scheduled home visit. Which nursing intervention is ethically appropriate? 1. Allow the client to decline the medication and document the decision. 2. Tell the client that if the medication is refused, hospitalization will occur. 3. Arrange with a relative to add the medication to the clients morning orange juice. 4. Call for help to hold the client down while the injection is administered. ANS: 1 Rationale: It is ethically appropriate for the nurse to allow the client to decline the medication and provide accurate documentation. The clients right to refuse treatment should be upheld, unless the refusal puts the client or others in harms way. Cognitive Level: Analysis Integrated Process: Implementation 16. Which situation exemplifies both assault and battery? 1. The nurse becomes angry, calls the client offensive names, and withholds treatment. 2. The nurse threatens to tie down the client and then does so, against the clients wishes. 3. The nurse hides the clients clothes and medicates the client to prevent elopement. 4. The nurse restrains the client without just cause and communicates this to family. ANS: 2 Rationale: The nurse in this situation has committed both the acts of assault and battery. Assault refers to an action that results in fear and apprehension that the person will be touched without consent. Battery is the touching of another person without consent. Cognitive Level: Analysis Integrated Process: Implementation 17. A geriatric client is confused and wandering in and out of every door. Which scenario reflects the least restrictive alternative for this client? 1. The client is placed in seclusion. 2. The client is placed in a geriatric chair with tray. 3. The client is placed in soft Posey restraints. 4. The client is monitored by an ankle bracelet. ANS: 4 Rationale: The least-restrictive alternative for this client would be monitoring by an ankle bracelet. The client does not pose a direct dangerous threat to self or others, so neither physical restraints nor seclusion would be justified. Cognitive Level: Application Integrated Process: Implementation 18. A brother calls to speak to his sister, who has been admitted to a psychiatric unit. The nurse connects him to the community phone, and the sister is summoned. Later the nurse realizes that the brother was not on the clients approved call list. What law has the nurse broken? 1. The National Alliance for the Mentally Ill Act 2. The Tarasoff Ruling 3. The Health Insurance Portability and Accountability Act 4. The Good Samaritan Law ANS: 3 Rationale: The nurse has violated the Health Insurance Portability and Accountability Act (HIPAA) by revealing that the client had been admitted to the psychiatric unit. The nurse should not have provided any information without proper consent from the client. Cognitive Level: Application Integrated Process: Implementation Multiple Response 19. After disturbing the peace, an aggressive, disoriented, unkempt, homeless individual is escorted to an emergency department. The client threatens suicide. Which of the following criteria would enable a physician to consider involuntary commitment? (Select all that apply.) 1. Being dangerous to others 2. Being homeless 3. Being disruptive to the community 4. Being gravely disabled and unable to meet basic needs 5. Being suicidal ANS: 1, 4, 5 Rationale: The physician could consider involuntary commitment when a client is dangerous to others, gravely disabled, or is suicidal. If the physician determines that the client is mentally incompetent, consent should be obtained from the legal guardian or court-approved guardian or conservator. A hospital administrator may give permission for involuntary commitment when time does not permit court intervention. Cognitive Level: Application Integrated Process: Assessment Fill-in-the-Blank 20. A valid, legally recognized claim or entitlement, encompassing both freedom from government interference or discriminatory treatment and an entitlement to a benefit or a service is defined as a . ANS: right Rationale: A right is a valid, legally recognized claim or entitlement, encompassing both freedom from government interference or discriminatory treatment and an entitlement to a benefit or a service. A right is absolute when there is no restriction whatsoever on the individuals entitlement. Cognitive Level: Application Integrated Process: Assessment 21. A branch of philosophy that addresses methods for determining the rightness or wrongness of ones actions is defined as . ANS: ethics Rationale: Ethics is a branch of philosophy that deals with systematic approaches to distinguishing right from wrong behavior. Bioethics is the term applied to these principles when they refer to concepts within the scope of medicine, nursing, and allied health. Chapter 4. Psychopharmacology MULTIPLE CHOICE 1. The nurse manager on the psychiatric unit was explaining to the new staff the differences between typical and atypical antipsychotics. The nurse correctly states that atypical antipsychotics: a. Remain in the system longer b. Act more quickly to reduce delusions c. Produce fewer extrapyramidal effects d. Are risk free for neuroleptic malignant syndrome (NMS) ANS: C Atypical antipsychotics produce less D2 blockade; thus movement disorders are less of a problem. No evidence suggests that the medication remains in the system longer nor that it acts more quickly to reduce delusions. The atypicals are not risk free for NMS. 2. The nurse would assess for neuroleptic malignant syndrome (NMS) if a patient on haloperidol (Haldol) develops a: a. 30 mm Hg decrease in blood pressure reading b. Respiratory rate of 24 respirations per minute c. Temperature reading of 104 F d. Pulse rate of 70 beats per minute ANS: C Increased temperature is the cardinal sign of NMS. This BP is not a significant feature of NMS. There are no significant findings to support the options related to respirations or pulse rate. 3. A patient taking fluphenazine (Prolixin) complains of dry mouth and blurred vision. What would the nurse assess as the likely cause of these symptoms? a. Decreased dopamine at receptor sites b. Blockade of histamine c. Cholinergic blockade d. Adrenergic blocking ANS: C Fluphenazine administration produces blockade of cholinergic receptors giving rise to anticholinergic effects, such as dry mouth, blurred vision, and constipation. 4. Which behavior displayed by a patient receiving a typical antipsychotic medication would be assessed as displaying behaviors characteristic of tardive dyskinesia (TD)? a. Grimacing and lip smacking b. Falling asleep in the chair and refusing to eat lunch c. Experiencing muscle rigidity and tremors d. Having excessive salivation and drooling ANS: A TD manifests as abnormal movements of voluntary muscle groups after a prolonged period of dopamine blockade. Movements may affect any muscle group, but muscles of the face, mouth, tongue, and digits are commonly affected. Falling asleep is reflective of the sedative effect of these medications. Muscle rigidity and drooling reflect EPS caused from imbalance between dopamine and acetylcholine. 5. When the nurse realizes that a patient diagnosed with schizophrenia is not taking the prescribed oral haloperidol (Haldol), which intervention would promote medication compliance? a. Instructing the patient to have friends monitor his medications b. Beginning administration of haloperidol (Haldol) decanoate c. Writing instructions in detail for the patient to follow d. Changing haloperidol to an atypical antipsychotic ANS: B Haloperidol decanoate is a depot medication, given intramuscularly every 2 to 4 weeks. It is unknown whether the patient has a support system. The patient probably received education, including written instructions prior to discharge. Changing to another classification of medication would not necessarily improve compliance. 6. When asked how tricyclic antidepressants affect neurotransmitter activity, the nurse should respond that they: a. Decrease available dopamine. b. Increase availability of norepinephrine and serotonin. c. Make available increased amounts of monoamine oxidase. d. Increase the effects of the chemical gamma-aminobutyric acid. ANS: B Tricyclic antidepressants block neurotransmitter uptake, increasing the amounts of norepinephrine and serotonin available. Decreasing dopamine is the action of typical antipsychotic medication. Increasing monoamine oxidase is not the action of tricyclics. Benzodiazepines, not tricyclics, increase the effects of GABA. 7. A severely depressed patient has been prescribed clomipramine (Anafranil). For which medication side effects should the patient be monitored? a. Excess salivation and drooling b. Muscle rigidity and restlessness c. Polyuria and coarse hand tremors d. Orthostatic hypotension and constipation ANS: D Alpha1 blockade produces orthostatic hypotension, and cholinergic blockade produces constipation. Mild tremors and urinary retention may occur. Drooling and excessive salvation may occur with SSRIs. Muscle rigidity and restlessness may occur with antipsychotics. 8. Which of these statements made by a patient taking the MAOI phenelzine (Nardil) would warrant further instruction? a. I often forget to wear sunscreen when I go outside. b. I need to restrict the amount of sodium in my diet. c. I should not use over-the-counter cold medications. d. I usually order liver and onions when my wife and I eat out. ANS: D MAOIs require patients to observe a tyramine-free diet to prevent hypertensive crisis. Liver is a food that contains large amounts of tyramine. The remaining options have no relevance for MAOI therapy. 9. Which patient complaint should receive priority from a patient who is taking the MAOI tranylcypromine (Parnate)? a. I havent had a bowel movement in 2 days. b. Will you take my temperature? I feel too warm. c. I get a headache when I drank several cups of coffee. d. My legs get stiff when I sit in the chair for any length of time. ANS: C Hypertensive crisis may occur if a patient taking a MAOI ingests certain food containing tyramine or drugs that cause blood pressure (BP) elevation. Headache is a warning sign of hypertensive crisis. The nurse should assess BP and inquire about other symptoms of hypertensive crisis. Stiffness is not related to MAOI therapy. Elevated temperature is not an initial sign of hypertensive crisis. Constipation is not a sign of hypertensive crisis. 10. Sertraline (Zoloft) has been prescribed for a patient with symptoms of a major depression. Which factor was probably most important in the physicians decision to use an SSRI? a. Good side-effect profile b. Less expense for the patient c. Increase in medication compliance d. Rapid rate of absorption from the GI tract ANS: A Compared to other antidepressant medication groups, SSRIs have the best side-effect profile. SSRIs are more costly. No studies have shown that SSRIs result in better compliance. These drugs are absorbed slowly from the GI tract. 11. Which statement made by a patient who will be maintained on lithium following discharge will require further instruction by the nurse? a. I will have my blood work done regularly. b. When I get home, I may go on a salt-free diet. c. I have learned not to restrict my intake of water. d. I understand some people gain weight on lithium. ANS: B This statement shows that the patient does not understand the relationship between lithium and sodium. The patient must be taught that changing dietary salt intake will affect lithium levels. Adding salt can cause lower levels; reducing salt can result in toxicity. The remaining options reflect correct information regarding lithium therapy. 12. To educate a patient regarding what to expect following the administration of a benzodiazepine, the nurse must understand that benzodiazepines: a. Have a rapid onset of peak action b. Reduce availability of GABA c. Generally diminish the activity of GABA d. Interact with serotonin to increase availability ANS: A Benzodiazepines do have a more rapid onset. There is no effect on the availability or function of GABA. Benzodiazepines do not diminish GABA activity; they enhance it. 13. A patient prescribed alprazolam (Xanax) for symptoms of anxiety shares with the nurse that, Im concerned about getting off this medication. Upon which fact will the nurse base the response to the patients concern? a. Long elimination half-life will result in a manageable withdrawal treatment plan. b. Rapid absorption and distribution to brain cells make withdrawal more difficult to manage. c. Sensitivity of the mesencephalic reticular activating system makes addiction unlikely. d. The combination of medication with an antidepressant often positively impacts withdrawal. ANS: B In general, shorter-acting benzodiazepines are more difficult to taper and potentially cause more problems with withdrawal. The remaining options are neither true nor relevant. 14. Which patient outcomes would be most applicable for the patient who has been taking benzodiazepines? Patient will state: a. That there are specific foods to avoid while on this medication b. An understanding of how to increase medication dosage c. That alcohol is a substance to avoid while on the medication d. An understanding that he or she can return to work while on this medication ANS: C Combining a benzodiazepine with alcohol or other CNS depressant is potentially fatal. No food restrictions exist. Dosage should not be changed without consultation with the physician. Patients may return to work unless experiencing sedation. In this case, they would be cautioned not to operate machinery. 15. Which person with mania is the least likely candidate to receive lithium? The patient who is: a. Six weeks pregnant b. Recovering from a hysterectomy c. Taking hormone replacement therapy d. Displaying symptoms of postpartum depression ANS: A Lithium is contraindicated during pregnancy because of teratogenic effects. The remaining options would not be contraindicative to lithium therapy. 16. An individual with poststroke depression is receiving an SSRI. What is the rationale for giving the medication at breakfast and again at midday? a. Prevent insomnia b. Prevent toxic reactions c. Decrease afternoon sleepiness d. Give an opportunity to monitor behavior closely ANS: A CNS stimulants may cause insomnia if given late in the day. Toxicity is a result of excessive medication in the system, not when it is administered. The drowsiness resulting from SSRI use would not be minimized if taken as described. There is no expectation that resulting behaviors will need to be so closely monitored. 17. A patient who has received lithium for 3 weeks to control acute mania has the following symptoms: coarse hand tremor, diarrhea, vomiting, lethargy, and mild confusion. The priority nursing action should be to: a. Administer prn Cogentin to relieve the symptoms. b. Provide reassurance that the symptoms are transient. c. Obtain a stat lithium level; hold lithium pending results. d. Assist the patient to decrease the sodium in their daily diet. ANS: C The symptoms the patient is experiencing are consistent with moderate lithium toxicity. The nurse should hold lithium, obtain a stat lithium level, and notify the physician. Cogentin is inappropriate; the symptoms are not EPS. The nurse may reassure the patient but cannot suggest that the symptoms will resolve over time. Minimizing salt would worsen lithium toxicity. 18. A patient with rapid cycling bipolar disorder is not responding well to lithium. The patient tells the nurse, It feels as though Ill never get well. I get better, and then I get worse. The reply that is based on knowledge of current therapy would be: a. Youre feeling very discouraged arent you? b. Its not all bad, is it? Sometimes you like being high. c. Another drug, valproic acid, is proving effective for rapid cycling. d. If your kidneys hold out, the lithium will eventually control the symptoms. ANS: C Valproic acid is a first-line agent for the treatment of bipolar disorder. It is particularly effective with rapid cycling. The other options are not responsive to the question stem, which asks for knowledge of current therapy. 19. Which statement by a patient with generalized anxiety disorder for whom lorazepam (Ativan) is prescribed as needed (prn) suggests the patient understands the purpose of the medication? a. I can talk with my therapist more easily after my medication takes effect. b. I wonder if I will have to take this medication for the rest of my entire life. c. Im embarrassed and dont want anyone to know Im on this kind of medication. d. Im going to ask for my prn dose so I can sleep instead of worrying about my kids. ANS: A The patient recognizes the therapeutic effects of the medication in assisting her to work effectively with the therapist. The remaining options show questions and inappropriate use of the medication. 20. A patient has been taking chlorpromazine (Thorazine) for the past 2 weeks. He drools, has hand tremors, and walks with a shuffling gait. The nurse would correctly attribute these behaviors to: a. Akinesia b. Tardive dyskinesia c. Pseudoparkinsonism d. Neuroleptic malignant syndrome ANS: C These are symptoms of pseudoparkinsonism associated with dopamine blockade. Tardive dyskinesia occurs after long-term therapy. The remaining options are not associated with the symptoms mentioned. 21. What intervention will the nurse request for a patient reporting gastrointestinal side effects related to valproate therapy? a. Mild laxative b. Low-fat diet c. Oral antacid d. Histamine-2 antagonist ANS: D Indigestion, heartburn, and nausea are common side effects of valproate therapy. The administration of a histamine-2 antagonist such as famotidine (Pepcid) is sometimes helpful. The other options would have no impact on the complaint. 22. A patients serum lithium level is reported as 1.9 mEq/L. The nurse should immediately: a. Restrict sodium and fluid intake. b. Assess for signs and symptoms of toxicity. c. Seek to have the patient transferred to ICU. d. Notify the patients physician immediately. ANS: B A serum lithium level this high suggests that the patient may be experiencing symptoms of lithium toxicity. Clinical assessment is essential to determine what, if any, signs and symptoms are present. After the clinical assessment has been made, the nurse can provide the physician with a complete picture. Restricting sodium and fluids would raise the serum level. Transferring may not be necessary and would require a physicians order. 23. To evaluate outcomes for a patient with schizophrenia receiving typical antipsychotic drug therapy, the nurse would look for improvement in: a. Affective mobility b. Positive symptoms c. Self-care activities d. Cognitive functioning ANS: B Typical antipsychotic medications produce improvement in the positive symptoms of schizophrenia such as hallucinations and delusions. Negative symptoms and cognitive functioning tend to show less improvement. 24. During a psychiatric emergency, IM ziprasidone (Geodon) is administered to an assaultive patient. During the next 2 hours, it is of primary importance that the nurse assess for: a. Tardive dyskinesia b. Anticholinergic effects c. Orthostatic hypotension d. Pseudoparkinsonism ANS: C The side effect most likely to appear is orthostatic hypotension related to alpha1 receptor blockade preventing peripheral blood vessels from automatically responding to positional change. Anticholinergic effects are of lesser concern. The remaining options are less likely to occur at this point in therapy. 25. A patient who began haloperidol (Haldol) therapy 24 hours ago tells the nurse that he feels jittery and unable to sit or stand still. The nurse can hypothesize that this report is related to: a. Dystonia b. Akathisia c. Serotonin syndrome d. Neuroleptic malignant syndrome ANS: B Akathisia, an extrapyramidal side effect, is characterized by restlessness, inability to sit still, and the need to pace. It usually occurs early in the course of treatment with a typical antipsychotic drug. The symptomology is not related or seen in the other options. Chapter 5. Relationship Development and Therapeutic Communication Multiple Choice 1. What is the most essential task for a nurse to accomplish prior to forming a therapeutic relationship with a client? 1. Clarify personal attitudes, values, and beliefs. 2. Obtain thorough assessment data. 3. Determine the clients length of stay. 4. Establish personal goals for the interaction. ANS: 1 Rationale: The most essential task for a nurse to accomplish prior to forming a therapeutic relationship with a client is to clarify personal attitudes, values, and beliefs. Understanding ones own attitudes, values, and beliefs is called self-awareness. Cognitive Level: Application Integrated Process: Implementation 2. If a client demonstrates transference toward a nurse, how should the nurse respond? 1. Promote safety and immediately terminate the relationship with the client. 2. Encourage the client to ignore these thoughts and feelings. 3. Immediately reassign the client to another staff member. 4. Help the client to clarify the meaning of the relationship, based on the present situation. ANS: 4 Rationale: The nurse should respond to a clients transference by clarifying the meaning of the nurse-client relationship based on the present situation. Transference occurs when the client unconsciously displaces feelings about a person from the past toward the nurse. The nurse should assist the client in separating the past from the present. Cognitive Level: Application Integrated Process: Implementation 3. What should be the priority nursing action during the orientation (introductory) phase of the nurse-client relationship? 1. Acknowledge the clients actions and generate alternative behaviors. 2. Establish rapport and develop treatment goals. 3. Attempt to find alternative placement. 4. Explore how thoughts and feelings about this client may adversely impact nursing care. ANS: 2 Rationale: The priority nursing action during the orientation phase of the nurse-client relationship should be to establish rapport and develop treatment goals. Rapport implies feelings on the part of both the nurse and the client, based on respect, acceptance, a sense of trust, and a nonjudgmental attitude. It is the essential foundation of the nurse-client relationship. Cognitive Level: Application Integrated Process: Implementation 4. Which client action should a nurse expect during the working phase of the nurse-client relationship? 1. The client gains insight and incorporates alternative behaviors. 2. The client establishes rapport with the nurse and mutually develops treatment goals. 3. The client explores feelings related to reentering the community. 4. The client explores personal strengths and weaknesses that impact behavioral choices. ANS: 1 Rationale: The nurse should expect that that the client will gain insight and incorporate alternative behaviors during the working phase of the nurse-client relationship. The client may also overcome resistance, problem-solve, and continually evaluate progress toward goals. Cognitive Level: Application Integrated Process: Planning 5. Which client statement should a nurse identify as a typical response to stress most often experienced in the working phase of the nurse-client relationship? 1. I cant bear the thought of leaving here and failing. 2. I might have a hard time working with you, because you remind me of my mother. 3. I really dont want to talk any more about my childhood abuse. 4. Im not sure that I can count on you to protect my confidentiality. ANS: 3 Rationale: The nurse should identify that the client statement, I really dont want to talk any more about my childhood abuse, reflects that the client is in the working phase of the nurse-client relationship. The working phase includes overcoming resistance behaviors on the part of the client as the level of anxiety rises in response to discussion of painful issues. Cognitive Level: Analysis Integrated Process: Evaluation 6. A mother who is notified that her child was killed in a tragic car accident states, I cant bear to go on with my life. Which nursing statement conveys empathy? 1. This situation is very sad, but time is a great healer. 2. You are sad, but you must be strong for your other children. 3. Once you cry it all out, things will seem so much better. 4. It must be horrible to lose a child, and Ill stay with you until your husband arrives. ANS: 4 Rationale: The nurses response, It must be horrible to lose a child, and Ill stay with you until your husband arrives, conveys empathy to the client. Empathy is the ability to see the situation from the clients point of view. Empathy is considered to be one of the most important characteristics of the therapeutic relationship. Cognitive Level: Application Integrated Process: Implementation 7. When an individual is two-faced, which characteristic essential to the development of a therapeutic relationship should a nurse identify as missing? 1. Respect 2. Genuineness 3. Sympathy 4. Rapport ANS: 2 Rationale: When an individual is two-faced, which means double-dealing or deceitful, the nurse should identify that genuineness is missing in the relationship. Genuineness refers to the nurses ability to be open and honest and maintain congruence between what is felt and what is communicated. When a nurse fails to bring genuineness to the relationship, trust cannot be established. Cognitive Level: Application Integrated Process: Assessment 8. On which task should a nurse place priority during the working phase of relationship development? 1. Establishing a contract for intervention 2. Examining feelings about working with a particular client 3. Establishing a plan for continuing aftercare 4. Promoting the clients insight and perception of reality ANS: 4 Rationale: The nurse should place priority on promoting the clients insight and perception of reality during the working phase of relationship development. Establishing a contract for intervention would occur in the orientation phase. Examining feelings about working with a client should occur in the pre-interaction phase. Establishing a plan for aftercare would occur in the termination phase. Cognitive Level: Application Integrated Process: Implementation 9. Which therapeutic communication technique is being used in the following nurse-client interaction? Client: My father spanked me often. Nurse: Your father was a harsh disciplinarian. 1. Restatement 2. Offering general leads 3. Focusing 4. Accepting ANS: 1 Rationale: The nurse is using the therapeutic communication technique of restatement. Restatement involves repeating the main idea of what the client has said. It allows the client to know whether the statement has been understood and provides an opportunity to continue. Cognitive Level: Application Integrated Process: Implementation 10. Which therapeutic communication technique is being used in the following nurse-client interaction? Client: When I am anxious, the only thing that calms me down is alcohol. Nurse: Other than drinking, what alternatives have you explored to decrease anxiety? 1. Reflecting 2. Making observations 3. Formulating a plan of action 4. Giving recognition ANS: 3 Rationale: The nurse is using the therapeutic communication technique of formulating a plan of action to help the client explore alternatives to drinking. The use of this technique may serve to prevent anger or anxiety from escalating. Cognitive Level: Application Integrated Process: Implementation 11. The nurse is interviewing a newly admitted psychiatric client. Which of the following nursing statements is an example of offering a general lead? 1. Do you know why you are here? 2. Are you feeling depressed or anxious? 3. Yes, I see. Go on. 4. Can you order the specific events that led to your admission? ANS: 3 Rationale: The nurses statement, Yes, I see. Go on, is an example of a general lead. Offering general leads encourages the client to continue sharing information. Cognitive Level: Application Integrated Process: Implementation 12. A nurse says to a client, Things will look better tomorrow after a good nights sleep. This is an example of which communication technique? 1. The therapeutic technique of giving advice 2. The therapeutic technique of defending 3. The nontherapeutic technique of presenting reality 4. The nontherapeutic technique of giving reassurance ANS: 4 Rationale: The nurses statement, Things will look better tomorrow after a good nights sleep, is an example of the nontherapeutic communication technique of giving reassurance. Giving reassurance indicates to the client that there is no cause for anxiety, thereby devaluing the clients feelings. Cognitive Level: Application Integrated Process: Implementation 13. A client diagnosed with post-traumatic stress disorder related to a rape is admitted to an inpatient psychiatric unit for evaluation and medication stabilization. Which therapeutic communication technique might a nurse use that is an example of broad openings? 1. What occurred prior to the rape, and when did you go to the emergency department? 2. What would you like to talk about? 3. I notice you seem uncomfortable discussing this. 4. How can we help you feel safe during your stay here? ANS: 2 Rationale: The nurses statement, What would you like to talk about? is an example of the therapeutic communication technique of a broad opening. Using broad openings allows the client to take the initiative in introducing the topic and emphasizes the importance of the clients role in the interaction. Cognitive Level: Application Integrated Process: Implementation 14. A nurse maintains an uncrossed arm and leg posture when communicating with a client. This nonverbal behavior is reflective of which letter of the SOLER acronym for active listening? 1. S 2. O 3. L 4. E 5. R ANS: 2 Rationale: The nurse should identify that maintaining an uncrossed arm and leg posture is nonverbal behavior that reflects the O in the active-listening acronym SOLER. The acronym SOLER includes sitting squarely facing the client (S), observing and open posture (O), leaning forward toward the client (L), establishing eye contact (E), and relaxing (R). Cognitive Level: Application Integrated Process: Implementation 15. An instructor is correcting a nursing students clinical worksheet. Which instructor statement is the best example of effective feedback? 1. Why did you use the clients name on your clinical worksheet? 2. You were very careless to refer to your client by name on your clinical worksheet. 3. Surely you didnt do this deliberately, but you breeched confidentiality by using names. 4. It is disappointing that after being told youre still using client names on your worksheet. ANS: 3 Rationale: The instructors statement, Surely you didnt do this deliberately, but you breeched confidentiality by using names, is an example of effective feedback. Feedback is method of communication for helping others consider a modification of behavior. Feedback should be descriptive, specific, and directed toward a behavior that the person has the capacity to modify and should impart information rather than offer advice. Cognitive Level: Application Integrated Process: Implementation 16. What is a nurses purpose for providing appropriate feedback? 1. To give the client good advice 2. To advise the client on appropriate behaviors 3. To evaluate the clients behavior 4. To give the client critical information ANS: 4 Rationale: The purpose of providing appropriate feedback is to give the client critical information. Feedback should not be used to give advice or evaluate behaviors. Cognitive Level: Application Integrated Process: Planning 17. A client exhibiting dependent behaviors says, Do you think I should move from my parents house and get a job? Which nursing response is most appropriate? 1. It would be best to do that in order to increase independence. 2. Why would you want to leave a secure home? 3. Lets discuss and explore all of your options. 4. Im afraid you would feel very guilty leaving your parents. ANS: 3 Rationale: The most appropriate response by the nurse is, Lets discuss and explore all of your options. In this example, the nurse is encouraging the client to formulate ideas and decide independently the appropriate course of action. Cognitive Level: Application Integrated Process: Implementation 18. A mother rescues two of her four children from a house fire. In an emergency department, she cries, I should have gone back in to get them. I should have died, not them. What is the nurses best response? 1. The smoke was too thick. You couldnt have gone back in. 2. Youre experiencing feelings of guilt, because you werent able to save your children. 3. Focus on the fact that you could have lost all four of your children. 4. Its best if you try not to think about what happened. Try to move on. ANS: 2 Rationale: The best response by the nurse is, Youre experiencing feelings of guilt, because you werent able to save your children. This response uses the therapeutic communication technique of restating what the client has said. This lets the client know whether an expressed statement has been understood or if clarification is necessary. Cognitive Level: Application Integrated Process: Implementation 19. A newly admitted client, diagnosed with obsessive-compulsive disorder (OCD), washes his hands continually. This behavior prevents unit activity attendance. Which nursing statement best addresses this situation? 1. Everyone diagnosed with OCD needs to control their ritualistic behaviors. 2. It is important for you to discontinue these ritualistic behaviors. 3. Why are you asking for help, if you wont participate in unit therapy? 4. Lets figure out a way for you to attend unit activities and still wash your hands. ANS: 4 Rationale: The most appropriate statement by the nurse is, Lets figure out a way for you to attend unit activities and still wash your hands. This statement reflects the therapeutic communication technique of formulating a plan of action. The nurse attempts to work with the client to develop a plan without damaging the therapeutic relationship. Cognitive Level: Application Integrated Process: Planning Multiple Response 20. Which of the following characteristics should be included in a therapeutic nurse-client relationship? (Select all that apply.) 1. Meeting the psychological needs of the nurse and the client 2. Ensuring therapeutic termination 3. Promoting client insight into problematic behavior 4. Collaborating to set appropriate goals 5. Meeting both the physical and psychological needs of the client ANS: 2, 3, 4, 5 Rationale: The nurse-client therapeutic relationship should include promoting client insight into problematic behavior, collaboration to set appropriate goals, meeting the physical and psychological needs of the client, and ensuring therapeutic termination. Meeting the nurses psychological needs should never be addressed within the nurse-client relationship. Cognitive Level: Application Integrated Process: Assessment 21. Which of the following individuals are communicating a message? (Select all that apply.) 1. A mother spanking her son for playing with matches 2. A teenage boy isolating himself and playing loud music 3. A biker sporting an eagle tattoo on his biceps 4. A teenage girl writing, No one understands me 5. A father checking for new e-mail on a regular basis ANS: 1, 2, 3, 4 Rationale: The nurse should determine that spanking, isolating, getting tattoos, and writing are all ways in which people communicate messages to others. It is estimated that about 70% to80% of communication is nonverbal. Cognitive Level: Application Integrated Process: Evaluation Fill-in-the-Blank 22. The term implies special feelings on the part of both the client and the nurse, based on acceptance, warmth, friendliness, common interest, a sense of trust, and a nonjudgmental attitude. ANS: rapport Rationale: Rapport implies special feelings on the part of both the client and the nurse, based on acceptance, warmth, friendliness, common interest, a sense of trust, and a nonjudgmental attitude. Establishing rapport may be accomplished by discussing non-health-related topics. Cognitive Level: Application Integrated Process: Assessment 23. refers to a nurses behavioral and emotional response to a client. These responses may be related to unresolved feelings toward significant others from the nurses past. ANS: Countertransference Rationale: Countertransference refers to a nurses behavioral and emotional response to a client. These responses may be related to unresolved feelings toward significant others from the nurses past or they may be generated in response to transference feelings on the part of the client. Chapter 6. The Nursing Process in Psychiatric/Mental Health Nursing Multiple Choice 1. Which statement is most accurate regarding the assessment of clients diagnosed with psychiatric problems? 1. Medical history is of little significance and can be eliminated from the nursing assessment. 2. Assessment provides a holistic view of the client, including biopsychosocial aspects. 3. Comprehensive assessments can be performed only by advanced practice nurses. 4. Psychosocial evaluations are gained by subjective reports rather than objective observations. ANS: 2 Rationale: The assessment of clients diagnosed with psychiatric problems should provide a holistic view of the client. A thorough assessment involves collecting and analyzing data from the client, significant others, and health-care providers, which may include the following dimensions: physical, psychological, sociocultural, spiritual, cognitive, functional abilities, developmental, economic, and lifestyle. Cognitive Level: Application Integrated Process: Assessment 2. Which statement regarding nursing interventions should a nurse identify as accurate? 1. Nursing interventions are independent from the treatment teams goals. 2. Nursing interventions are solely directed by written physician orders. 3. Nursing interventions occur independently but in concert with overall treatment team goals. 4. Nursing interventions are standardized by policies and procedures. ANS: 3 Rationale: The nurse should understand that nursing interventions occur independently but in concert with overall treatment goals. Nursing interventions should be developed and implemented in collaboration with other health-care professionals involved in the clients care. Cognitive Level: Application Integrated Process: Implementation 3. Within the nurses scope of practice, which function is exclusive to the advanced practice psychiatric nurse? 1. Teaching about the side effects of neuroleptic medications 2. Using psychotherapy to improve mental health status 3. Using milieu therapy to structure a therapeutic environment 4. Providing case management to coordinate continuity of health services ANS: 2 Rationale: The advanced practice psychiatric nurse is authorized to use psychotherapy to improve mental health. This includes individual, couples, group, and family psychotherapy. Education, case management, and milieu therapy can be provided by registered psychiatric mental health nurses. Cognitive Level: Application Integrated Process: Implementation 4. The nurse should recognize which acronym as representing problem-oriented charting? 1. SOAPIE 2. APIE 3. DAR 4. PQRST ANS: 1 Rationale: The acronym SOAPIE represents problem-oriented charting, which reflects the subjective, objective, assessment, plan, implementation, and evaluation format. Used in nursing, nursing diagnoses (problems) are identified on a written plan of care, with appropriate nursing interventions described for each. Cognitive Level: Comprehension Integrated Process: Implementation 5. Which tool would be appropriate for a nurse to use when assessing mental acuity prior to and immediately following electroconvulsive therapy (ECT)? 1. CIWA scale 2. GGT 3. MMSE 4. CAPS scale ANS: 3 Rationale: The MMSE, or mini mental status exam, would be the appropriate tool to use to assess the mental acuity of a client prior to and immediately following ECT. The CIWA scale, or clinical institute withdrawal assessment scale, would be used to assess withdraw from substances such as alcohol. The CAPS refers to the clinician-administered PTSD scale and would be used to assess signs and symptoms of PTSD. The GGT test is a blood test used to assess gamma- glutamyl transferase levels, which may be an indication of alcoholism. Cognitive Level: Application Integrated Process: Assessment 6. What is being assessed when a nurse asks a client to identify name, date, residential address, and situation? 1. Mood 2. Perception 3. Orientation 4. Affect ANS: 3 Rationale: The nurse should ask the client to identify name, date, residential address, and situation to assess the clients orientation. Assessment of the clients orientation to reality is part of a mental status evaluation. Cognitive Level: Application Integrated Process: Assessment 7. What is the purpose of a nurse gathering client information? 1. It enables the nurse to modify behaviors related to personality disorders. 2. It enables the nurse to make sound clinical judgments and plan appropriate care. 3. It enables the nurse to prescribe the appropriate medications. 4. It enables the nurse to assign the appropriate Axis I diagnosis. ANS: 2 Rationale: The purpose of gathering client information is to enable the nurse to make sound clinical judgments and plan appropriate care. The nurse should complete a thorough assessment of the client, including information collected from the client, significant others, and health-care providers. Cognitive Level: Application Integrated Process: Assessment 8. A nurse on an inpatient psychiatric unit implements care by scheduling client activities, interacting with clients, and maintaining a safe therapeutic environment. These actions reflect which role of the nurse? 1. Health teacher 2. Case manager 3. Milieu manager 4. Psychotherapist ANS: 3 Rationale: The milieu manager implements care by scheduling client activities, interacting with clients, and maintaining a safe therapeutic environment. Health teaching involves promoting health in a safe environment. Case management is used to organize client care so that outcomes are achieved. Psychotherapy involves conducting individual, couples, group, and family counseling. Cognitive Level: Application Integrated Process: Implementation 9. The following outcome was developed for a client: Client will list five personal strengths by the end of day one. Which correctly written nursing diagnostic statement most likely generated the development of this outcome? 1. Altered self-esteem R/T years of emotional abuse AEB self-deprecating statements 2. Self-care deficit R/T altered thought process 3. Disturbed body image R/T major depressive disorder AEB mood rating of 2/10 4. Risk for disturbed self-concept R/T hopelessness AEB suicide attempt ANS: 1 Rationale: The nurse should determine that altered self-esteem and self-deprecating statements would generate the outcome to list personal strengths by the end of day one. Self-care deficit, disturbed body image, and risk for disturbed self-concept would generate specific outcomes in accordance with specific needs and goals. The self-care deficit and risk for disturbed self-concept nursing diagnoses are incorrectly written. Cognitive Level: Application Integrated Process: Diagnosis 10. How should a nurse prioritize nursing diagnoses? 1. By the established goal of care 2. By the life-threatening potential 3. By the physicians priority of care 4. By the clients preference ANS: 2 Rationale: The nurse should prioritize nursing diagnoses related to their life-threatening potential. Safety is always the nurses first priority. Cognitive Level: Analysis Integrated Process: Diagnosis 11. A client has a nursing diagnosis of Insomnia R/T paranoid thinking AEB MNA, DFA, and daytime napping. Which is a correctly written and appropriate outcome for this client? 1. The client will avoid daytime napping and attend all groups. 2. The client will exercise, as needed, before bedtime. 3. The client will sleep seven uninterrupted hours by day four of hospitalization. 4. The clients sleep habits will improve during hospitalization. ANS: 3 Rationale: The outcome The client will sleep seven uninterrupted hours by day four of hospitalization is accurately written and an appropriate outcome for a client diagnosed with insomnia. Nursing outcomes should be derived from the diagnosis, measurable, and include a time estimate for attainment. The outcome must also be realistic for the clients capabilities. Cognitive Level: Analysis Integrated Process: Planning 12. The following NANDA-I nursing diagnostic stem was developed for a client on an inpatient unit: Risk for injury. What assessment data most likely led to the development of this problem statement? 1. The client is receiving ECT and is diagnosed with Parkinsonism. 2. The client has a history of four suicide attempts in adolescence. 3. The client expresses hopelessness and helplessness and isolates self. 4. The client has disorganized thought processes and delusional thinking. ANS: 1 Rationale: The nurse should identify that a client receiving ECT and who is diagnosed with Parkinsonism is at risk for injury. History of suicide, hopelessness, and disorganized thoughts would not lead the nurse to formulate a nursing diagnostic stem of Risk for injury. Cognitive Level: Application Integrated Process: Assessment 13. A student nurse asks an instructor how best to develop nursing outcomes for clients. Which response by the instructor most accurately answers the students question? 1. You can use NIC, a standardized reference for nursing outcomes. 2. Look at your clients problems and set a realistic, achievable goal. 3. With client collaboration, outcomes should be based on client problems. 4. Copy your standard outcomes from a nursing care plan textbook. ANS: 3 Rationale: Client outcomes are most realistic and achievable when there is collaboration among the interdisciplinary team members, the client, and significant others. Cognitive Level: Application Integrated Process: Planning 14. A client diagnosed with schizophrenia is exhibiting nonverbal behaviors indicating that the client is hearing things that others do not. Which nursing diagnosis, which was recently removed from the NANDA-I list, still accurately reflects this clients problem? 1. Disturbed thought processes 2. Disturbed sensory perception 3. Anxiety 4. Chronic confusion ANS: 2 Rationale: The nursing diagnosis disturbed sensory perception accurately reflects the clients symptoms of hearing things that others do not. The nursing diagnosis describes the clients condition and facilitates the prescription of interventions. Cognitive Level: Application Integrated Process: Diagnosis Multiple Response 15. Which of the following nursing interventions fall within the standards of psychiatricmental health clinical nursing practice for a nurse generalist? (Select all that apply.) 1. Assist the client to perform activities of daily living. 2. Consult with other clinicians to provide services for clients and effect system change. 3. Encourage the client to discuss triggers for relapse. 4. Use prescriptive authority in accordance with state and federal laws. 5. Educate the family about signs and symptoms of alcohol dependence and withdrawal. ANS: 1, 3, 5 Rationale: Assisting the client to perform daily living activities, encouraging the client to discuss triggers, and educating the family are nursing interventions that fall within the standards of psychiatric clinical nursing practice for a nurse generalist. Psychiatricmental health advanced practice registered nurses can consult with other clinicians and use prescriptive authority. Cognitive Level: Application Integrated Process: Implementation 16. Which of the following characteristics of accurately developed client outcomes should a nurse identify? (Select all that apply.) 1. Client outcomes are specifically formulated by nurses. 2. Client outcomes are not restricted by time frames. 3. Client outcomes are specific and measurable. 4. Client outcomes are realistically based on client capability. 5. Client outcomes are formally approved by the psychiatrist. ANS: 3, 4 Rationale: The nurse should identify that client outcomes should be specific, measurable, and realistically based on client capability. Outcomes should be derived from the diagnosis and should include a time estimate for attainment. Outcomes are most effective when formulated cooperatively by the interdisciplinary team members, the client, and significant others. Cognitive Level: Application Integrated Process: Planning Ordered Response 17. Number the following nursing interventions as they would proceed through the steps of the nursing process. Determine if an antianxiety medication is decreasing a clients stress. Measure a clients vital signs and review past history. Encourage deep breathing and teach relaxation techniques. Aim, with client collaboration, for a seven-hour nights sleep. Recognize and document the clients problem. ANS: The correct order is 5, 1, 4, 3, 2 Rationale: 1. Measuring a clients vital signs and reviewing past history is a nursing intervention that occurs in the assessment step of the nursing process. 2. Recognizing and documenting the clients problem occurs in the nursing diagnosis step. 3. Setting a goal with client collaboration, for a seven-hour nights sleep occurs in the planning step. 4. Encouraging deep breathing and teaching relaxation techniques occur in the implementation step. 5. Determining if an antianxiety medication is decreasing a clients stress occurs in the evaluation step. Cognitive Level: Analysis Integrated Process: Implementation Fill-in-the-Blank 18. A provides the basis for selection of nursing interventions to achieve outcomes for which the nurse has accountability. ANS: nursing diagnosis Rationale: Nursing diagnoses are clinical judgments about individual, family, or community experiences/responses to actual or potential health problems/life processes. A nursing diagnosis provides the basis for selection of nursing interventions to achieve outcomes for which the nurse has accountability. Chapter 7. Milieu Therapy - Therapeutic Community Multiple Choice 1. An angry client on an inpatient unit approaches a nurse stating, Someone took my lunch! People need to respect others, and you need to do something about this now! The nurses response should be guided by which basic assumption of milieu therapy? 1. Conflict should be avoided at all costs on inpatient psychiatric units. 2. Conflict should be resolved by the nursing staff. 3. On inpatient units, every interaction is an opportunity for therapeutic intervention. 4. Conflict resolution should only be addressed during group therapy. ANS: 3 Rationale: The nurses response should be guided by the basic assumption that every interaction is an opportunity for therapeutic intervention. The nurse can use milieu therapy to effect behavioral change and improve psychological health and functioning. Cognitive Level: Application Integrated Process: Implementation 2. A client on an inpatient unit angrily says to a nurse, Peter is not cleaning up after himself in the community bathroom. You need to address this problem. Which is the appropriate nursing response? 1. Ill talk to Peter and present your concerns. 2. Why are you overreacting to this issue? 3. You should bring this to the attention of your treatment team. 4. I can see that you are angry. Lets discuss ways to approach Peter with your concerns. ANS: 4 Rationale: The most appropriate nursing response involves restating the clients feeling and developing a plan with the client to solve the problem. According to Skinner, every interaction is an opportunity for therapeutic intervention to improve communication and relationship- development skills. Cognitive Level: Application Integrated Process: Implementation 3. A newly admitted client asks, Why do we need a unit schedule? Im not going to these groups. Im here to get some rest. Which is the most appropriate nursing response? 1. The purpose of group therapy is to learn and practice new coping skills. 2. Group therapy is mandatory. All clients must attend. 3. Group therapy is optional. You can go if you find the topic helpful and interesting. 4. Group therapy is an economical way of providing therapy to many clients concurrently. ANS: 1 Rationale: The nurse should explain to the client that the purpose of group therapy is to learn and practice new coping skills. The client owns his or her environment and can make decisions to attend group or not. Cognitive Level: Application Integrated Process: Implementation 4. A client diagnosed with schizophrenia functions well and is bright, spontaneous, and interactive during hospitalization but then decompensates after discharge. What does the milieu provide that may be missing in the home environment? 1. Peer pressure 2. Structured programming 3. Visitor restrictions 4. Mandated activities ANS: 2 Rationale: The milieu, or therapeutic community, provides the client with structured programming that may be missing in the home environment. The therapeutic community provides a structured schedule of activities in which interpersonal interaction and communication with others are emphasized. Time is also devoted to personal problems and focus groups. Cognitive Level: Application Integrated Process: Evaluation 5. To promote self-reliance, how should a psychiatric nurse best conduct medication administration? 1. Encourage clients to request their medications at the appropriate times. 2. Refuse to administer medications unless clients request them at the appropriate times. 3. Allow the clients to determine appropriate medication times. 4. Take medications to the clients bedside at the appropriate times. ANS: 1 Rationale: The psychiatric nurse promoting self-reliance would encourage clients to request their medications at the appropriate times. Nurses are responsible for the management of medication administration on inpatient psychiatric units, but nurses must work with clients to encourage self- reliance and responsibility, which may result in independent decision-making, leading to medication adherence. Cognitive Level: Application Integrated Process: Implementation 6. A nurse working on an inpatient psychiatric unit is assigned to conduct a 45-minute education group. What should the nurse identify as an appropriate group topic? 1. Dream analysis 2. Creative cooking 3. Paint by number 4. Stress management ANS: 4 Rationale: The nurse should identify that teaching clients about stress management is an appropriate education group topic. Nurses should be able to perform the role of client teacher in the psychiatric area. Nurses need to be able to assess a clients learning readiness. Other topics for education groups include medical diagnoses, side effects of medications, and the importance of medication adherence. Cognitive Level: Application Integrated Process: Planning 7. What is the best rationale for including family in the clients therapy within the inpatient milieu? 1. To structure a program of social and work-related activities 2. To facilitate discharge from hospitalization 3. To provide a concrete demonstration of caring 4. To encourage the family to model positive behaviors ANS: 2 Rationale: The nurse should include the clients family in therapy within the inpatient milieu to facilitate discharge from the hospital. Family members are invited to participate in some therapy groups and to share meals with the client in the communal dining room. Family involvement may also serve to prevent the client from becoming too dependent on the therapeutic environment. Cognitive Level: Application Integrated Process: Planning 8. How does a democratic form of self-government in the milieu contribute to client therapy? 1. By setting punishments for clients who violate the community rules 2. By dealing with inappropriate behaviors as they occur 3. By setting expectations wherein all clients are treated on an equal basis 4. By interacting with professional staff members to learn about therapeutic interventions ANS: 3 Rationale: A democratic form of self-government in the milieu contributes to client therapy by setting the expectation that all clients should be treated on an equal basis. Clients participate in the decision-making and problem-solving aspects that affect treatment setting. The norms, rules, and behavioral limits are established by the staff and clients. All individuals have input. Cognitive Level: Application Integrated Process: Evaluation 9. A client is to undergo psychological testing. Which member of the interdisciplinary team should a nurse consult for this purpose? 1. The psychiatrist 2. The psychiatric social worker 3. The clinical psychologist 4. The clinical nurse specialist ANS: 3 Rationale: The nurse should consult with the clinical psychologist to obtain psychological testing for the client. Clinical psychologists can administer, interpret, and evaluate psychological tests to assist in the diagnostic process. Cognitive Level: Application Integrated Process: Planning 10. In the role of milieu manager, which activity should the nurse prioritize? 1. Setting the schedule for the daily unit activities 2. Evaluating clients for medication effectiveness 3. Conducting therapeutic group sessions 4. Searching newly admitted clients for hazardous objects ANS: 4 Rationale: The milieu manager should search newly admitted clients for hazardous objects. Safety of the client and others always takes priority. Nurses are responsible for ensuring that the clients safety and physiological needs are met. Cognitive Level: Analysis Integrated Process: Evaluation Multiple Response 11. A nurse attends an interdisciplinary team meeting regarding a newly admitted client. Which of the following individuals are typically included as members of the interdisciplinary treatment team in psychiatry? (Select all that apply.) 1. Respiratory therapist and psychiatrist 2. Occupational therapist and psychologist 3. Recreational therapist and art therapist. 4. Social worker and hospital volunteer 5. Mental health technician and chaplain ANS: 2, 3, 5 Rationale: The interdisciplinary treatment team in psychiatry consists of a psychologist, occupational therapist, recreational therapist, art therapist, mental health technician, and chaplain. In addition, a psychiatrist, psychiatric nurse, psychiatric social worker, music therapist, psychodramatist, and dietitian also participate in the interdisciplinary treatment team. Respiratory therapists and hospital volunteers are not included in the interdisciplinary treatment team in psychiatry. Cognitive Level: Application Integrated Process: Assessment 12. Which of the following conditions promote a therapeutic community? (Select all that apply.) 1. The unit schedule includes unlimited free time for personal reflection. 2. Unit responsibilities are assigned according to client capabilities. 3. A flexible schedule is determined by client needs. 4. The individual is the sole focus of therapy. 5. A democratic form of government exists. ANS: 2, 5 Rationale: A therapeutic community is promoted when unit responsibilities are assigned according to client capability and a democratic form of government exists. Therapeutic communities are structured and provide therapeutic interventions that focus on communication and relationship-development skills. Cognitive Level: Application Integrated Process: Implementation Fill-in-the-Blank 13. A scientific structuring of the environment in order to effect behavioral changes and to improve the psychological health and functioning of the individual is defined as therapy. ANS: milieu Rationale: Milieu therapy is defined as a scientific structuring of the environment in order to effect behavioral changes and to improve the psychological health and functioning of the individual. The goal of milieu therapy is to manipulate the environment so that all aspects of the clients hospital experience are considered therapeutic. Chapter 8. Intervention in Groups Multiple Choice 1. During a therapeutic group, which nursing action demonstrates a laissez-faire leadership style? 1. The nurse mandates that all group members reveal an embarrassing personal situation. 2. The nurse asks for a show of hands to determine group topic preference. 3. The nurse sits silently as the group members stray from the assigned topic. 4. The nurse shuffles through papers to determine the facility policy on length of group. ANS: 3 Rationale: The nurse leader who sits silently and allows group members to stray from the assigned topic is demonstrating a laissez-faire leadership style. This style allows group members to do as they please with no direction from the leader. Group members often become frustrated and confused in reaction to a laissez-faire leadership style. Cognitive Level: Application Integrated Process: Implementation 2. During a community meeting, a nurse encourages clients to present unit problems and discuss possible solutions. Which type of leadership style is the nurse demonstrating? 1. Democratic 2. Autocratic 3. Laissez-faire 4. Bureaucratic ANS: 1 Rationale: The nurse who encourages clients to present problems and discuss solutions is demonstrating a democratic leadership style. Democratic leaders share information with group members and promote decision-making by the members of the group. The leader provides guidance and expertise as needed. Cognitive Level: Application Integrated Process: Implementation 3. Which situation should a nurse identify as an example of an autocratic leadership style? 1. The president of Sigma Theta Tau assigns members to committees to research problems. 2. Without faculty input, the dean mandates that all course content be delivered via the Internet. 3. During a community meeting, a nurse listens as clients generate solutions. 4. The student nurses association advertises for candidates for president. ANS: 2 Rationale: The nurse should identify that mandating decisions without consulting the group is considered an autocratic leadership style. Autocratic leadership increases productivity but often reduces morale and motivation owing to lack of member input and creativity. Cognitive Level: Application Integrated Process: Implementation 4. A single, pregnant teenager in a parenting class discloses her ambivalence toward the pregnancy and the subsequent guilt that these thoughts generate. A mother of three admits to having felt that way herself. Which of Yaloms curative group factors does this illustrate? 1. Imparting of information 2. Instillation of hope 3. Altruism 4. Universality ANS: 4 Rationale: The scenario is an example of the curative group factor of universality. Universality occurs when individuals realize that they are not alone in the problems, thoughts, and feelings they are experiencing. This realization reduces anxiety by the support and understanding of others. Cognitive Level: Analysis Integrated Process: Evaluation 5. A client diagnosed with alcohol use disorder experiences a first relapse. During an AA meeting, another group member states, I relapsed three times, but now have been sober for 15 years. Which of Yaloms curative group factors does this illustrate? 1. Imparting of information 2. Instillation of hope 3. Catharsis 4. Universality ANS: 2 Rationale: This scenario is an example of the curative group factor instillation of hope. This occurs when members observe the progress of others in the group with similar problems and begin to believe that personal problems can also be resolved. Cognitive Level: Analysis Integrated Process: Evaluation 6. During a group discussion, members freely interact with each other. Which member statement is an example of Yaloms curative group factor of imparting information? 1. I found a Web site explaining the different types of brain tumors and their treatment. 2. My brother also had a brain tumor and now is completely cured. 3. I understand your fear and will be by your side during this time. 4. My mother was also diagnosed with cancer of the brain. ANS: 1 Rationale: Yaloms curative group factor of imparting information involves group members sharing knowledge gained through formal instruction as well as advice and suggestions. Cognitive Level: Application Integrated Process: Assessment 7. Prayer group members at a local Baptist church are meeting with a poor, homeless family whom they are supporting. Which member statement is an example of Yaloms curative group factor of altruism? 1. Ill give you the name of a friend that rents inexpensive rooms. 2. The last time we helped a family, they got back on their feet and prospered. 3. I can give you all of my baby clothes for your little one. 4. I can appreciate your situation. I had to declare bankruptcy last year. ANS: 3 Rationale: Yaloms curative group factor of altruism occurs when group members provide assistance and support to each other that creates a positive self-image and promotes self-growth. Individuals gain self-esteem through mutual caring and concern. Cognitive Level: Application Integrated Process: Assessment 8. During an inpatient educational group, a client shouts out, This information is worthless. Nothing you have said can help me. These statements indicate to a nurse leader that the client is assuming which group role? 1. The group role of aggressor 2. The group role of initiator 3. The group role of gatekeeper 4. The group role of blocker ANS: 1 Rationale: The nurse should identify that the client is assuming the group role of the aggressor. The aggressor expresses negativism and hostility toward others in the group or to the group leader and may use sarcasm in an effort to degrade the status of others. Cognitive Level: Application Integrated Process: Assessment 9. During a group session, which client statement demonstrates that the group has progressed to the middle, or working, phase of group development? 1. Its hard for me to tell my story when Im not sure about the reactions of others. 2. I think Joes Antabuse suggestion is a good one and might work for me. 3. My situation is very complex, and I need professional, not peer, advice. 4. I am really upset that you expect me to solve my own problems. ANS: 2 Rationale: The nurse should recognize that group members have progressed to the working phase of group development when members begin to look to each other instead of to the leader for guidance. Group members in the working phase begin to accept criticism from each other and use it constructively to create change. Cognitive Level: Application Integrated Process: Evaluation 10. Which group leader activity should a nurse identify as being most effective in the final, or termination, phase of group development? 1. The group leader establishes the rules that will govern the group after discharge. 2. The group leader encourages members to rely on each other for problem solving. 3. The group leader presents and discusses the concept of group termination. 4. The group leader helps the members to process feelings of loss. ANS: 4 Rationale: The most effective intervention in the final, or termination, phase of group development would be for the group leader to help the members to process feelings of loss. The leader should encourage the members to review the goals and discuss outcomes, reminisce about what has occurred, and encourage members to provide feedback to each other about progress. Cognitive Level: Application Integrated Process: Assessment 11. A nursing instructor is teaching students about self-help groups like Alcoholics Anonymous (AA). Which student statement indicates that learning has occurred? 1. There is little research to support AAs effectiveness. 2. Self-help groups used to be the treatment of choice, but their popularity is waning. 3. These groups have no external regulation, so clients need to be cautious. 4. Members themselves run the group, with leadership usually rotating among the members. ANS: 4 Rationale: The student indicates an understanding of self-help groups when stating, Members themselves run the group, with leadership usually rotating among the members. Nurses may or may not be involved in self-help groups. These groups allow members to talk about feelings and reduce feelings of isolation, while receiving support from others undergoing similar experiences. Cognitive Level: Application Integrated Process: Evaluation 12. When planning group therapy, a nurse should identify which configuration as most optimal for a therapeutic group? 1. Open-ended membership; circle of chairs; group size of 5 to 10 members 2. Open-ended membership; chairs around a table; group size of 10 to 15 members 3. Closed membership; circle of chairs; group size of 5 to 10 members 4. Closed membership; chairs around a table; group size of 10 to 15 members ANS: 3 Rationale: The nurse should identify that the most optimal conditions for a therapeutic group is one in which the membership is closed and in which the group size is between 5 and 10 members, who are arranged in a circle of chairs. The focus of therapeutic groups is directed to relations within the group and the interactions among group members. Cognitive Level: Application Integrated Process: Planning 13. During the sixth week of a 10-week parenting skills group, a nurse observes as several members get into a heated dispute about spanking. As a group, they decide to create a pros-and- cons poster on the use of physical discipline. At this time, what is the role of the group leader? 1. The leader should referee the debate. 2. The leader should adamantly oppose physical disciplining measures. 3. The leader should redirect the group to a less-controversial topic. 4. The leader should encourage the group to solve the problem collectively. ANS: 4 Rationale: The role of the group leader is to encourage the group to solve the problem collectively. A democratic leadership style supports members in their participation and problem- solving. Members are encouraged to solve issues that relate to the group cooperatively. Cognitive Level: Application Integrated Process: Implementation 14. A 10-week, prenuptial counseling group composed of five couples is terminating. At the last group meeting, a nurse notices that the two most faithful and participative couples are absent. When considering concepts of group development, what might explain this behavior? 1. They are experiencing problems with termination, leading to feelings of abandonment. 2. They did not think any new material would be covered at the last session. 3. They were angry with the leader for not extending the length of the group. 4. They were bored with the material covered in the group. ANS: 1 Rationale: The nurse should determine that the clients absence from the final group meeting may indicate that they are experiencing problems with termination. The termination phase of group development may elicit feelings of abandonment and anger. Successful termination may help members develop skills to cope with future unrelated losses. Cognitive Level: Application Integrated Process: Evaluation 15. An experienced psychiatric registered nurse has taken a new position leading groups in a day treatment program. Which group is this nurse most qualified to lead? 1. A psychodrama group 2. A psychotherapy group 3. A parenting group 4. A family therapy group ANS: 3 Rationale: A psychiatric registered nurse is qualified to lead a parenting group. A parenting group can be classified as either a teaching group or therapeutic group. Psychodrama, psychotherapy, and family therapy are forms of group therapy and must be lead by qualified leaders who generally have advanced degrees in psychology, social work, nursing, or medicine. Cognitive Level: Application Integrated Process: Implementation 16. A nursing instructor is teaching about psychodrama, a specialized type of therapeutic group. Which student statement indicates that further teaching is necessary? 1. Psychodrama provides a safe setting in which to discuss painful issues. 2. In psychodrama, the client is the protagonist. 3. In psychodrama, the client observes actor interactions from the audience. 4. Psychodrama facilitates resolution of interpersonal conflicts. ANS: 2 Rationale: The nurse should educate the student that in psychodrama the client plays the role of him or herself in a life-situation scenario and is called the protagonist. During psychodrama, the client does not observe interactions from the audience. Other group members perform the role of the audience and discuss the situation they have observed, offer feedback, and express their feelings. Leaders of psychodrama must have specialized training to become a psychodramatist. Cognitive Level: Application Integrated Process: Evaluation Multiple Response 17. Which of the following behavioral skills should a nurse implement when leading a group that is functioning in the orientation phase of group development? (Select all that apply.) 1. Encourage members to provide feedback to each other about individual progress. 2. Ensure that group rules do not interfere with goal fulfillment. 3. Work with group members to establish rules that will govern the group. 4. Emphasize the need for and importance of confidentiality within the group. 5. Help the leader to resolve conflicts and foster cohesiveness within the group. ANS: 2, 3, 4 Rationale: During the orientation phase of group development, the nurse leader should work together with members to establish rules that will govern the group. The leader should ensure that group rules do not interfere with goal fulfillment and establish the need for and importance of confidentiality within the group. Members need to establish trust and cohesion in order to move into the working phase. Cognitive Level: Application Integrated Process: Implementation Ordered Response 18. Order the following leadership expectations that occur in the three phases of the group development process. The leader encourages members to provide feedback to each other about individual progress and to review goals and discuss outcomes. The leader promotes an environment of trust and ensures that rules established by the group do not interfere with fulfillment of the goals. The leader helps to resolve conflict and fosters cohesiveness, while ensuring that members do not deviate from the intended task. ANS: The correct order is 3, 1, 2 Rationale: 1. In the Initial, or Orientation, phase, the leader is expected to orient members to specific group processes, encourage members to participate without disclosing too much too soon, promote an environment of trust, and ensure that rules established by the group do not interfere with fulfillment of the goals. 2. In the Middle, or Working, phase, the role of leader diminishes and becomes more one of facilitator. Some leadership functions are shared by certain members of the group as they progress toward resolution. The leader helps to resolve conflicts and continues to foster cohesiveness among the members, while ensuring that they do not deviate from the intended task or purpose for which the group was organized. 3. In the Final, or Termination, phase, the leader encourages the group members to reminisce about what has occurred within the group, to review the goals and discuss the actual outcomes, and to encourage members to provide feedback to each other about individual progress within the group. The leader encourages members to discuss feelings of loss associated with termination of the group. Cognitive Level: Analysis Integrated Process: Implementation Fill-in-the-Blank 19. A is a collection of individuals whose association is founded on shared commonalities of interest, values, norms, or purpose. ANS: group Rationale: A group is a collection of individuals whose association is founded on shared commonalities of interest, values, norms, or purpose. Membership in a group is generally by chance (born into the group), by choice (voluntary affiliation), or by circumstance (the result of life-cycle events over which an individual may or may not have control). Chapter 9. Crisis Intervention Multiple Choice 1. A new mother is concerned about her ability to perform her parental role. She is quite anxious and ambivalent about leaving the postpartum unit. To offer effective client care, a nurse should be familiar with what information about this type of crisis? 1. This type of crisis is precipitated by unexpected external stressors. 2. This type of crisis is precipitated by preexisting psychopathology. 3. This type of crisis is precipitated by an acute response to an external situational stressor. 4. This type of crisis is precipitated by normal life-cycle transitions that overwhelm the client. ANS: 4 Rationale: The nurse should understand that this type of crisis is precipitated by normal life-cycle transitions that overwhelm the client. Reassurance and guidance should be provided as needed, and the client should be referred to services that can provide assistance. Cognitive Level: Application Integrated Process: Planning 2. A wife brings her husband to an emergency department after an attempt to hang himself. He is a full-time student and works 8 hours at night to support his family. He states, I cant function any longer under all this stress. Which type of crisis is the client experiencing? 1. Maturational/developmental crisis 2. Psychiatric emergency crisis 3. Anticipated life transition crisis 4. Traumatic stress crisis ANS: 2 Rationale: The nurse should determine that the client is experiencing a psychiatric emergency crisis. Psychiatric emergencies occur when crisis situations result in severe impairment, incompetence, or an inability to assume personal responsibility. Cognitive Level: Application Integrated Process: Assessment 3. A client comes to a psychiatric clinic experiencing sudden extreme fatigue and decreased sleep and appetite. The client works 12 hours a day and rates anxiety as 8/10 on a numeric scale. What long-term outcome is realistic in addressing this clients crisis? 1. The client will change his type A personality traits to more adaptive ones by one week. 2. The client will list five positive self-attributes. 3. The client will examine how childhood events led to his overachieving orientation. 4. The client will return to previous adaptive levels of functioning by week six. ANS: 4 Rationale: The nurse should identify that a realistic long-term outcome for this client is to return to previous adaptive levels of functioning. The nurse should work with the client to develop attainable outcomes that reflect immediacy of the situation. Cognitive Level: Application Integrated Process: Planning 4. A high school student has learned that she cannot graduate. Her boyfriend will be attending a college out of state that she planned to attend. She is admitted to a psychiatric unit after overdosing on Tylenol. Which is the priority nursing diagnosis for this client? 1. Ineffective coping R/T situational crisis AEB powerlessness 2. Anxiety R/T fear of failure 3. Risk for self-directed violence R/T hopelessness 4. Risk for low self-esteem R/T loss events AEB suicidal ideations ANS: 3 Rationale: The priority nursing diagnosis for this client is risk for self-directed violence R/T hopelessness. Nurses should prioritize diagnoses and outcomes based on potential safety risk to the client or others. Cognitive Level: Analysis Integrated Process: Diagnosis 5. After threatening to jump off of a bridge, a client is brought to an emergency department by police. To assess for suicide potential, which question should a nurse ask first? 1. Are you currently thinking about harming yourself? 2. Why do you want to harm yourself? 3. Have you thought about the consequences of your actions? 4. Who is your emergency contact person? ANS: 1 Rationale: The nurse should first assess the client for current harmful or suicidal thoughts to minimize risk of harm to the client and provide appropriate interventions. A suicidal client is experiencing a psychiatric emergency in which the crisis team should assess for client safety as a priority. Cognitive Level: Analysis Integrated Process: Assessment 6. An involuntarily committed client when offered a dinner tray pushes it off the bedside table onto the floor. Which nursing intervention should a nurse implement to address this behavior? 1. Initiate forced medication protocol. 2. Help the client to explore the source of anger. 3. Ignore the act to avoid reinforcing the behavior. 4. With staff support and a show of solidarity, set firm limits on the behavior. ANS: 4 Rationale: The most appropriate nursing intervention is to set firm limits on the behavior. Pushing food onto the floor should not warrant forced medication. This intervention may be too restrictive, considering the behavior. Exploring the source of anger may be more appropriate once the client has resolved the current emotion or in a therapeutic group setting. Ignoring the act may further upset the client and is not a method of teaching appropriate behavior. Cognitive Level: Application Integrated Process: Implementation 7. A college student who was nearly raped while jogging, completes a series of appointments with a rape crisis nurse. At the final session, which client statement most clearly suggests that the goals of crisis intervention have been met? 1. Youve really been helpful. Can I count on your for continued support? 2. I work out in the college gym rather than jogging outdoors. 3. Im really glad I didnt go home. It would have been hard to come back. 4. I carry mace when I jog. It makes me feel safe and secure. ANS: 4 Rationale: The nurse should evaluate that the client who has developed adaptive coping strategies has achieved the goals of crisis intervention. The final phase of crisis intervention involves evaluating the outcome of the crisis intervention and anticipatory planning. Cognitive Level: Analysis Integrated Process: Evaluation 8. A despondent client who has recently lost her husband of 30 years tearfully states, Ill feel a lot better if I sell my house and move away. Which nursing response is most appropriate? 1. Im confident you know whats best for you. 2. This may not be the best time for you to make such an important decision. 3. Your children will be terribly disappointed. 4. Tell me why you want to make this change. ANS: 2 Rationale: During crisis intervention, the nurse should guide the client through a problem- solving process. The nurse should help the individual confront the source of the problem, encourage the individual to discuss changes he or she would like to make, and encourage exploration of feelings about aspects of the crisis that cannot be changed. The nurse should also assist the client in determining whether any changes are realistic. Cognitive Level: Application Integrated Process: Implementation 9. An inpatient client with a known history of violence suddenly begins to pace. Which additional client behavior should alert a nurse to escalating anger and aggression? 1. The client requests prn medications. 2. The client has a tense facial expression and body language. 3. The client refuses to eat lunch. 4. The client sits in group with back to peers. ANS: 2 Rationale: The nurse should assess that tense facial expressions and body language may indicate that a clients anger is escalating. The nurse should conduct a thorough assessment of the clients history of violence and develop interventions for de-escalation. Cognitive Level: Application Integrated Process: Assessment 10. What is the best nursing rationale for holding a debriefing session with clients and staff after a take-down intervention has taken place on an inpatient unit? 1. Reinforce unit rules with the client population. 2. Create protocols for the future release of tensions associated with anger. 3. Process client feelings and alleviate fears of undeserved seclusion and restraint. 4. Discuss the situation that led to inappropriate expressions of anger. ANS: 4 Rationale: The nurse should determine that the purpose for holding a debriefing session with clients and staff after a take-down intervention is to discuss the situation that led to inappropriate behavior. It is important to determine the factors leading to the inappropriate behavior in order to develop future intervention strategies. It is also important to help clients and staff process feelings about the situation. Cognitive Level: Application Integrated Process: Implementation 11. An aggressive client has been placed in restraints after all other interventions have failed. Which protocol would apply in this situation? 1. An in-person evaluation by a physician or other licensed independent practitioner must be conducted within 1 hour of the initiation of the restraints. 2. An in-person evaluation by a physician or other licensed independent practitioner must be conducted within 2 hours of the initiation of the restraints. 3. An in-person evaluation by a physician or other licensed independent practitioner must be conducted within 3 hours of the initiation of the restraints. 4. An in-person evaluation by a physician or other licensed independent practitioner must be conducted within 4 hours of the initiation of the restraints. ANS: 1 Rationale: The Joint Commission (formerly the Joint Commission on Accreditation of Healthcare Organizations [JCAHO]) requires that an in-person evaluation by physician or other licensed independent practitioner be conducted within 1 hour of the initiation of restraint or seclusion. Cognitive Level: Application Integrated Process: Implementation 12. A combative adolescent client has been placed in seclusion after all other interventions have failed. Which protocol would apply in this situation? 1. The physician or other licensed independent practitioner must reissue a new order for restraints every 24 hours. 2. The physician or other licensed independent practitioner must reissue a new order for restraints every 8 hours. 3. The physician or other licensed independent practitioner must reissue a new order for restraints every 3 to 4 hours. 4. The physician or other licensed independent practitioner must reissue a new order for restraints every 1 to 2 hours. ANS: 4 Rationale: The physician or other licensed independent practitioner must reissue a new order for restraints every 4 hours for adults and every 1 to 2 hours for children and adolescents. Restraints should be used as a last resort, after all other interventions have been unsuccessful, and the client is clearly at risk of harm to self or others. Cognitive Level: Application Integrated Process: Implementation 13. A nursing instructor is teaching about the Roberts Seven-Stage Crisis Intervention Model. Which nursing action should be identified with Stage IV? 1. Collaboratively implement an action plan. 2. Help the client identify the major problems or crisis precipitants. 3. Help the client deal with feelings and emotions. 4. Collaboratively generate and explore alternatives. ANS: 3 Rationale: The following are the stages of the Roberts Seven-Stage Crisis Intervention Model: Stage I: Psychosocial and Lethality Assessment, Stage II: Rapidly Establish Rapport, Stage III: Identify the Major Problems or Crisis Precipitants, Stage IV: Deal with Feelings and Emotions, Stage V: Generate and Explore Alternatives, Stage VI: Implement an Action Plan, Stage VII: Follow-up. Cognitive Level: Application Integrated Process: Implementation Multiple Response 14. Which of the following nursing statements and/or questions represent appropriate communication to assess an individual in crisis? (Select all that apply.) 1. Tell me what happened. 2. What coping methods have you used, and did they work? 3. Describe to me what your life was like before this happened. 4. Lets focus on the current problem. 5. Ill assist you in selecting functional coping strategies. ANS: 1, 2, 3 Rationale: In the assessment phase, the nurse should gather information regarding the precipitating stressor and the resulting crisis. Focusing on the current problem and selecting functional coping strategies would not occur until after a complete assessment. Cognitive Level: Application Integrated Process: Assessment 15. Which of the following interventions should a nurse use when caring for an inpatient client who expresses anger inappropriately? (Select all that apply.) 1. Maintain a calm demeanor. 2. Clearly delineate the consequences of the behavior. 3. Use therapeutic touch to convey empathy. 4. Set limits on the behavior. 5. Teach the client to avoid I statements related to expression of feelings. ANS: 1, 2, 4 Rationale: The nurse should determine that, when working with an inpatient client with difficulty expressing anger appropriately, it is important to maintain a calm demeanor, clearly define the consequences, and set limits on the behavior. The use of therapeutic touch may not be appropriate and could increase the clients anger. Teaching would not be appropriate when a client is agitated. Cognitive Level: Application Integrated Process: Implementation 16. Which of the following are behavior assessment categories in the Broset Violence Checklist? (Select all that apply.) 1. Confusion 2. Paranoia 3. Boisterousness 4. Panic 5. Irritability ANS: 1, 3, 5 Rationale: The Broset Violence Checklist is a quick, simple, and reliable tool that can be used to assess the risk of potential violence. The behavior assessment categories include: confusion, irritability, boisterousness, physical threats, and verbal threats. Cognitive Level: Application Integrated Process: Implementation Ordered Response 17. Order the following stages of Roberts Seven-Stage Crisis Intervention Model. 1. Deal with feelings and emotions. 2. Generate and explore alternatives. 3. Rapidly establish rapport. 4. Psychosocial and lethality assessment. 5. Identify the major problems or crisis precipitants. 6. Follow up. 7. Implement an action plan. ANS: The correct order is 4, 5, 2, 1, 3, 7, 6 Rationale: The stages of Roberts Seven-Stage Crisis Intervention Model include: 1. Psychosocial and lethality assessment; 2. Rapidly establish rapport; 3. Identify the major problems or crisis precipitants; 4. Deal with feelings and emotions; 5. Generate and explore alternatives; 6. Implement an action plan; 7. Follow up. Cognitive Level: Analysis Integrated Process: Implementation Fill-in-the-Blank 18. A sudden event in ones life that disturbs homeostasis, during which usual coping mechanisms cannot resolve the problem, can be defined as a . ANS: crisis Rationale: A crisis is a sudden event in ones life that disturbs homeostasis, during which usual coping mechanisms cannot resolve the problem. Crises result in a disequilibrium, from which many individuals require assistance to recover. Chapter 10. The Recovery Model Multiple Choice 1. A nursing instructor is teaching about recovery as it applies to mental illness. Which student statement indicates that further teaching is needed? 1. The goal of recovery is improved health and wellness. 2. The goal of recovery is expedient, comprehensive behavioral change. 3. The goal of recovery is the ability to live a self-directed life. 4. The goal of recovery is the ability to reach full potential. ANS: 2 Rationale: The Substance Abuse and Mental Health Services Administration (SAMHSA) defines recovery from mental health disorders and substance use disorders as a process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential. Change in recovery is not an expedient process. It occurs incrementally over time. Cognitive Level: Application Integrated Process: Evaluation 2. Which situation presents an example of the basic concept of a recovery model? 1. The clients family is encouraged to make decisions in order to facilitate discharge. 2. A social worker, discovering the clients income, changes the clients discharge placement. 3. A psychiatrist prescribes an antipsychotic drug based on observed symptoms. 4. A client diagnosed with schizophrenia schedules follow-up appointments and group therapy. ANS: 4 Rationale: The basic concept of a recovery model is empowerment of the consumer. The recovery model is designed to allow consumers primary control over decisions about their own care. Cognitive Level: Analysis Integrated Process: Evaluation 3. A nursing instructor is teaching about the guiding principles of the recovery model, as described by the SAMHSA. Which student statement indicates that further teaching is needed? 1. Recovery occurs via many pathways. 2. Recovery emerges from strong religious affiliations. 3. Recovery is supported by peers and allies. 4. Recovery is culturally based and influenced. ANS: 2 Rationale: SAMHSA lists the following as guiding principles for the recovery model: recovery emerges from hope, recovery is person-driven, recovery occurs via many pathways, recovery is holistic, recovery is supported by peers and allies, recovery is supported through relationship and social networks, recovery is culturally based and influenced, recovery is supported by addressing trauma, recovery involves individual, family, and community strengths and responsibility, recovery is based on respect. Recovery emerges from hope but affiliation with any particular religion would have little bearing on the recovery process. Cognitive Level: Application Integrated Process: Evaluation 4. A client diagnosed with alcohol abuse disorder is referred to a residential care facility after discharge. According to the SAMHSA, which dimension of recovery is supporting this client? 1. Health 2. Home 3. Purpose 4. Community ANS: 2 Rationale: SAMHSA describes the dimension of Home as a stable and safe place to live. Cognitive Level: Application Integrated Process: Assessment 5. A client diagnosed with obsessive-compulsive disorder states, I really think my future will improve because of my successful treatment choices. Im going to make my life better. Which guiding principle of recovery has assisted this client? 1. Recovery emerges from hope. 2. Recovery is person-driven. 3. Recovery occurs via many pathways. 4. Recovery is holistic. ANS: 1 Rationale: The SAMHSA lists the following as guiding principles for the recovery model: recovery emerges from hope, recovery is person-driven, recovery occurs via many pathways, recovery is holistic, recovery is supported by peers and allies, recovery is supported through relationship and social networks, recovery is culturally based and influenced, recovery is supported by addressing trauma, recovery involves individual, family, and community strengths and responsibility, recovery is based on respect. This client has internalized hope. This hope is the catalyst of the recovery process. Cognitive Level: Application Integrated Process: Evaluation 6. A nurse maintains a clients confidentiality, addressed the client appropriately, and does not discriminate based on gender, age, race, or religion. Which guiding principle of recovery has this nurse employed? 1. Recovery is culturally based and influenced. 2. Recovery is based on respect. 3. Recovery involves individual, family, and community strengths and responsibility. 4. Recovery is person-driven. ANS: 2 Rationale: The SAMHSA lists the following as guiding principles for the recovery model: recovery emerges from hope, recovery is person-driven, recovery occurs via many pathways, recovery is holistic, recovery is supported by peers and allies, recovery is supported through relationship and social networks, recovery is culturally based and influenced, recovery is supported by addressing trauma, recovery involves individual, family, and community strengths and responsibility, recovery is based on respect. This nurse accepts and appreciates clients who are affected by mental health and substance use problems. This nurse protects the rights of clients and does not discriminate against them. Cognitive Level: Application Integrated Process: Implementation 7. A nurse on an inpatient unit helps a client understand the significance of treatments, and provides the client with copies of all documents related to the plan of care. This nurse is employing which commitment in the Tidal Model of Recovery? 1. Know that Change Is Constant 2. Reveal Personal Wisdom 3. Be Transparent 4. Give the Gift of Time ANS: 3 Rationale: Barker & Buchanan-Barker developed a set of essential values termed the The 10 Tidal Commitments upon which the Tidal Model is based. They include: Value the Voice, Respect the Language, Develop Genuine Curiosity, Become the Apprentice, Use the Available Toolkit, Craft the Step Beyond, Give the Gift of Time, Reveal Personal Wisdom, Know that Change Is Constant, and Be Transparent. This nurse is employing the Be Transparent commitment. Cognitive Level: Application Integrated Process: Implementation 8. Which is the priority focus of recovery models? 1. Empowerment of the health-care team to bring their expertise to decision-making 2. Empowerment of the client to make decisions related to individual health care 3. Empowerment of the family system to provide supportive care 4. Empowerment of the physician to provide appropriate treatments ANS: 2 Rationale: The basic concept of a recovery model is empowerment of the client. The recovery model is designed to allow clients primary control over decisions about their own care. Cognitive Level: Analysis Integrated Process: Assessment 9. A client experiences an exacerbation of psychiatric symptoms to the point of threatening self- harm. Which action step of the Wellness Recovery Action Plan (WRAP) model should be employed, and what action reflects this step? 1. Step 3: Triggers that cause distress or discomfort are listed. 2. Step 4: Signs indicating relapse are identified and plans for responding are developed. 3. Step 5: A specific plan to help with symptoms is formulated. 4. Step 6: Following client-designed plan, caregivers now become decision-makers. ANS: 4 Rationale: The WRAP recovery model is a step-wise process through which an individual is able to monitor and manage distressing symptoms that occur in daily life. The six steps include: Step 1. Develop a Wellness Toolbox; Step 2. Daily Maintenance List; Step 3. Triggers; Step 4. Early Warning Signs; Step 5. Things Are Breaking Down or Getting Worse; Step 6. Crisis Planning. In step 6 (Crisis Planning) clients can no longer care for themselves, make independent decisions, or keep themselves safe. Caregivers take an active role in this step on behalf of the client and implement the plan that the client has previously developed. All other actions presented require the client to be functionally capable. Cognitive Level: Analysis Integrated Process: Evaluation 10. A nursing instructor is teaching about components present in the recovery process as described by Andresen and associates that led to the development of the Psychological Recovery Model. Which student statement indicates that further teaching is needed? 1. A client has a better chance of recovery if he or she truly believes that recovery can occur. 2. If a client is willing to give the responsibility of treatment to the health-care team, they are likely to recover. 3. A client who has a positive sense of self and a positive identity is likely to recover. 4. A client has a better chance of recovery if he or she has purpose and meaning in life. ANS: 2 Rationale: In examining a number of studies, Andresen and associates identified four components that were consistently evident in the recovery process. These components are hope, responsibility, self and identity, and meaning and purpose. Under responsibility, this model tasks the client, not the health-care team, with taking responsibility for his or her life and well-being. Cognitive Level: Analysis Integrated Process: Evaluation 11. A client states, My illness is so devastating, I feel like my life is on hold. The nurse recognizes that this client is in which stage of the Psychological Recovery Model as described by Andersen and associates? 1. Moratorium 2. Awareness 3. Preparation 4. Rebuilding ANS: 1 Rationale: Andresen and associates have conceptualized a five-stage model of recovery called the Psychological Recovery Model. The stages include: Stage 1: Moratorium, Stage 2: Awareness, Stage 3: Preparation, Stage 4: Rebuilding, and Stage 5: Growth. The moratorium stage is identified by dark despair and confusion. It is called moratorium, because it seems that life is on hold. Cognitive Level: Analysis Integrated Process: Evaluation 12. A client states, I have come to the conclusion that this disease has not paralyzed me. The nurse recognizes that this client is in which stage of the Psychological Recovery Model as described by Andersen and associates? 1. Moratorium 2. Awareness 3. Preparation 4. Rebuilding ANS: 2 Rationale: Andresen and associates have conceptualized a five-stage model of recovery called the Psychological Recovery Model. The stages include: Stage 1: Moratorium, Stage 2: Awareness, Stage 3: Preparation, Stage 4: Rebuilding, and Stage 5: Growth. In the awareness stage, the individual comes to a realization that a possibility for recovery exists. Andresen and associates state, It involves an awareness of a possible self other than that of sick person: a self that is capable of recovery. Cognitive Level: Analysis Integrated Process: Evaluation 13. A psychiatrist who embraces the Psychological Recovery Model tells the nurse that a client is in the Growth stage. What should the nurse expect to fine when assessing this client? 1. A client feeling confident about achieving goals in life. 2. A client who is aware of the need to set goals in life. 3. A client who has mobilized personal and external resources. 4. A client who begins to actively take control of his or her life. ANS: 1 Rationale: Andresen and associates have conceptualized a five-stage model of recovery called the Psychological Recovery Model. The stages include: Stage 1: Moratorium, Stage 2: Awareness, Stage 3: Preparation, Stage 4: Rebuilding, and Stage 5: Growth. In the growth stage, the individual feels a sense of optimism and hope of a rewarding future. Skills that have been nurtured in the previous stages are applied with confidence, and the individual strives for higher levels of well-being. Cognitive Level: Analysis Integrated Process: Assessment Multiple Response 14. Which of the following has the SAMHSA described, as major dimensions of support for a life of recovery? (Select all that apply) 1. Health 2. Community 3. Home 4. Religious affiliation 5. Purpose ANS: 1, 2, 3, 5 Rationale: SAMHSA suggests that a life in recovery is supported by four major dimensions, which include health, home, purpose, and community. Religious affiliation is not included in the listed dimensions. Cognitive Level: Application Integrated Process: Assessment 15. A nurse uses the commitments of the Tidal Model of Recovery in psychiatric nursing practice. Which of the following nursing actions reflect the use of the Develop Genuine Curiosity commitment? (Select all that apply.) 1. The nurse expresses interest in the clients story. 2. The nurse asks for clarification of certain points. 3. The nurse encourages the client to speak his own words in his own unique way. 4. The nurse assists the client to unfold the story at his or her own rate. 5. The nurse provides the clients with copies of all documents relevant to care. ANS: 1, 2, 4 Rationale: Barker & Buchanan-Barker developed a set of essential values termed the The 10 Tidal Commitments, upon which the Tidal Model is based. They include: Value the Voice, Respect the Language, Develop Genuine Curiosity, Become the Apprentice, Use the Available Toolkit, Craft the Step Beyond, Give the Gift of Time, Reveal Personal Wisdom, Know that Change Is Constant, and Be Transparent. This nurse is employing the Develop Genuine Curiosity commitment, by expressing interest, asking for clarification, and assisting the client to unfold the story at his or her own rate. Cognitive Level: Application Integrated Process: Implementation Ordered Response 16. Order the six steps of The Wellness Recovery Action Plan(WRAP) Model as described by Copeland et al. 1. Daily Maintenance List 2. Things Are Breaking Down or Getting Worse 3. Crisis Planning 4. Develop a Wellness Toolbox 5 Early Warning Signs 6. Triggers ANS: The correct order is 2, 5, 6, 1, 4, 3 Rationale: The WRAP model is a step-wise process, through which an individual is able to monitor and manage distressing symptoms that occur in daily life. The six steps include: Step 1. Develop a Wellness Toolbox; Step 2. Daily Maintenance List; Step 3. Triggers; Step 4. Early Warning Signs; Step 5. Things Are Breaking Down or Getting Worse; Step 6. Crisis Planning. Cognitive Level: Analysis Integrated Process: Assessment Fill-in-the-Blank 17. from mental health disorders and substance use disorders is a process of change through which individuals improve their health and wellness, live a self- directed life, and strive to reach their full potential. ANS: Recovery Rationale: Recovery from mental health disorders and substance use disorders is a process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential. Recovery is the restoration to a former or better state or condition Chapter 11. Suicide Prevention MULTIPLE CHOICE 1. Which changes in brain biochemical function is most associated with suicidal behavior? a. Dopamine excess b. Serotonin deficiency c. Acetylcholine excess d. Gamma-aminobutyric acid deficiency ANS: B Research suggests that low levels of serotonin may play a role in the decision to commit suicide. The other neurotransmitter alterations have not been implicated in suicidal crises. 2. A college student failed two tests. Afterward, the student cried for hours and then tried to telephone a parent but got no answer. The student then gave several expensive sweaters to a roommate. Which behavior provides the strongest clue of an impending suicide attempt? a. Calling parents b. Excessive crying c. Giving away sweaters d. Staying alone in a dorm room ANS: C Giving away prized possessions may signal that the individual thinks he or she will have no further need for the items, such as when a suicide plan has been formulated. Calling parents and crying do not provide clues to suicide, in and of themselves. Remaining in the dormitory would be an expected behavior because the student has nowhere else to go. 3. A nurse uses the SAD PERSONS scale to interview a patient. This tool provides data relevant to: a. current stress level. b. mood disturbance. c. suicide potential. d. level of anxiety. ANS: C The SAD PERSONS tool evaluates 10 major risk factors in suicide potential: sex, age, depression, previous attempt, ethanol use, rational thinking loss, social supports lacking, organized plan, no spouse, and sickness. The tool does not have appropriate categories to provide information on the other options listed. 4. A person intentionally overdoses on antidepressant drugs. Which nursing diagnosis has the highest priority? a. Powerlessness b. Social isolation c. Risk for suicide d. Ineffective management of the therapeutic regimen ANS: C This diagnosis is the only one with life-or-death ramifications and is therefore higher in priority than the other options. 5. A person attempts suicide by overdose, is treated in the emergency department, and then hospitalized. What is the best initial outcome? The patient will: a. verbalize a will to live by the end of the second hospital day. b. describe two new coping mechanisms by the end of the third hospital day. c. accurately delineate personal strengths by the end of first week of hospitalization. d. exercise suicide self-restraint by refraining from gestures or attempts to kill self for 24 hours. ANS: D Suicide self-restraint relates most directly to the priority problem of risk for self-directed violence. The other outcomes are related to hope, coping, and self-esteem. 6. A college student who attempted suicide by overdose is hospitalized. When the parents are contacted, they respond, There must be a mistake. This could not have happened. Weve given our child everything. The parents reaction reflects: a. denial. b. anger. c. anxiety. d. rescue feelings. ANS: A The parents statements indicate denial. Denial or minimization of suicidal ideation or attempts is a defense against uncomfortable feelings. Family members are often unable to acknowledge suicidal ideation in someone close to them. The feelings suggested in the distractors are not clearly described in the scenario. 7. An adolescent tells the school nurse, My friend threatened to take an overdose of pills. The nurse talks to the friend who verbalized the suicide threat. The most critical question for the nurse to ask would be: a. Why do you want to kill yourself? b. Do you have access to medications? c. Have you been taking drugs and alcohol? d. Did something happen with your parents? ANS: B The nurse must assess the patients access to the means to carry out the plan and, if there is access, alert the parents to remove them from the home. The other questions may be important to ask but are not the most critical. 8. An adult attempts suicide after declaring bankruptcy. The patient is hospitalized and takes an antidepressant medication for five days. The patient is now more talkative and shows increased energy. Select the highest priority nursing intervention. a. Supervise the patient 24 hours a day. b. Begin discharge planning for the patient. c. Refer the patient to art and music therapists. d. Consider the discontinuation of suicide precautions. ANS: A The patient now has more energy and may have decided on suicide, especially considering the history of the prior suicide attempt. The patient is still a suicide risk; therefore, continuous supervision is indicated. 9. A nurse and patient construct a no-suicide contract. Select the preferable wording for the contract. a. I will not try to harm myself during the next 24 hours. b. I will not make a suicide attempt while I am hospitalized. c. For the next 24 hours, I will not kill or harm myself in any way. d. I will not kill myself until I call my primary nurse or a member of the staff. ANS: C The correct answer leaves no loopholes. The wording about not harming oneself and not making an attempt leaves loopholes or can be ignored by the patient who thinks, I am not going to harm myself, I am going to kill myself, or I am not going to attempt suicide, I am going to commit suicide. A patient may call a therapist and leave the telephone to carry out the suicidal plan. 10. A tearful, anxious patient at the outpatient clinic reports, I should be dead. The initial task of the nurse conducting the assessment interview is to: a. assess the lethality of a suicide plan. b. encourage expression of anger. c. establish a rapport with the patient. d. determine risk factors for suicide. ANS: C Establishing rapport will allow the nurse to obtain relevant assessment data such as the presence of a suicide plan, the lethality of a suicide plan, and the presence of risk factors for suicide. 11. Select the most helpful response for a nurse to make when a patient being treated as an outpatient states, I am considering suicide. a. Im glad you shared this. Please do not worry. We will handle it together. b. I think you should admit yourself to the hospital to get help. c. We need to talk about the good things you have to live for. d. Bringing this up is a very positive action on your part. ANS: D This response gives the patient reinforcement and validation for making a positive response rather than acting out the suicidal impulse. It gives neither advice nor false reassurance, and it does not imply stereotypes such as, You have a lot to live for. It uses the patients ambivalence and sets the stage for more realistic problem-solving strategies. 12. Which intervention should a nurse recommend for the distressed family and friends of someone who has committed suicide? a. Participating in reminiscence therapy b. Attending a self-help group for survivors c. Contracting for two sessions of group therapy d. Completing a psychological postmortem assessment ANS: B Survivors need outlets for their feelings about the loss and the deceased person. Self-help groups provide peer support while survivors work through feelings of loss, anger, and guilt. Psychological postmortem assessment would not provide the support necessary to work through feelings of loss associated with the suicide of a family member. Reminiscence therapy is not geared to loss resolution. Contracting for two sessions of group therapy would probably not provide sufficient time to work through the issues associated with a death by suicide. 13. Which statement provides the best rationale for why a nurse should closely monitor a severely depressed patient during antidepressant medication therapy? a. As depression lifts, physical energy becomes available to carry out suicide. b. Suicide may be precipitated by a variety of internal and external events. c. Suicidal patients have difficulty using social supports. d. Suicide is an impulsive act. ANS: A Antidepressant medication has the objective of relieving depression. The risk for suicide is greater as the depression lifts, primarily because the patient has more physical energy at a time when he or she may still have suicidal ideation. The other options have little to do with nursing interventions relating to antidepressant medication therapy. 14. A nurse assesses a patient who reports a 3-week history of depression and crying spells. The patient says, My business is bankrupt, and I was served with divorce papers. Which subsequent statement by the patient alerts the nurse to a concealed suicidal message? a. I wish I were dead. b. Life is not worth living. c. I have a plan that will fix everything. d. My family will be better off without me. ANS: C Verbal clues to suicide may be overt or covert. The incorrect options are overt references to suicide. The correct option is more veiled. It alludes to the patients suicide as being a way to fix everything but does not say it outright. 15. A depressed patient says, Nothing matters anymore. What is the most appropriate response by the nurse? a. Are you having thoughts of suicide? b. I am not sure I understand what you are trying to say. c. Try to stay hopeful. Things have a way of working out. d. Tell me more about what interested you before you began feeling depressed. ANS: A The nurse must make overt what is covert; that is, the possibility of suicide must be openly addressed. Often, patients feel relieved to be able to talk about suicidal ideation. 16. A nurse counsels a patient with recent suicidal ideation. Which is the nurses most therapeutic comment? a. Lets make a list of all your problems and think of solutions for each one. b. Im happy youre taking control of your problems and trying to find solutions. c. When you have bad feelings, try to focus on positive experiences from your life. d. Lets consider which problems are most important and which are less important. ANS: D The nurse helps the patient develop effective coping skills. He or she assists the patient to reduce the overwhelming effects of problems by prioritizing them. The incorrect options continue to present overwhelming approaches to problem solving. 17. When assessing a patients plan for suicide, what aspect has priority? a. Patients financial and educational status b. Patients insight into suicidal motivation c. Availability of means and lethality of method d. Quality and availability of patients social support ANS: C If a person has definite plans that include choosing a method of suicide readily available, and if the method is one that is lethal (i.e., will cause the person to die with little probability for intervention), the suicide risk is considered high. These areas provide a better indication of risk than the areas mentioned in the other options. 18. Which understanding about individuals who attempt suicide will help a nurse plan the care for a suicidal patient? Every suicidal person should be considered: a. mentally ill. b. intent on dying. c. cognitively impaired. d. experiencing hopelessness. ANS: D Hopelessness is the characteristic common among people who attempt suicide. The incorrect options reflect myths about suicide. Not all who attempt suicide are intent on dying. Not all are mentally ill or cognitively impaired. 19. Which statement by a patient during an assessment interview should alert the nurse to the patients need for immediate, active intervention? a. I am mixed up, but I know I need help. b. I have no one for help or support. c. It is worse when you are a person of color. d. I tried to get attention before I shot myself. ANS: B Lack of social support and social isolation increase the suicide risk. The willingness to seek help lowers the risk. Being a person of color does not suggest a higher risk; more whites commit suicide than do individuals of other racial groups. Attention seeking is not correlated with a higher risk of suicide. 20. The feeling experienced by a patient that should be assessed by the nurse as most predictive of elevated suicide risk is: a. hopelessness. b. sadness. c. elation. d. anger. ANS: A Of the feelings listed, hopelessness is most closely associated with increased suicide risk. Depression, aggression, impulsivity, and shame are other feelings noted as risk factors for suicide. 21. Four individuals have given information about their suicide plans. Which plan evidences the highest suicide risk? a. Jumping from a 100-foot-high railroad bridge located in a deserted area late at night b. Turning on the oven and letting gas escape into the apartment during the night c. Cutting the wrists in the bathroom while the spouse reads in the next room d. Overdosing on aspirin with codeine while the spouse is out with friends ANS: A This is a highly lethal method with little opportunity for rescue. The other options are lower lethality methods with higher rescue potential. 22. Which individual in the emergency department should be considered at the highest risk for completing suicide? a. An adolescent Asian-American girl with superior athletic and academic skills who has asthma b. A 38-year-old single African-American female church member with fibrocystic breast disease c. A 60-year-old married Hispanic man with 12 grandchildren who has type 2 diabetes d. A 79-year-old single white man with cancer of the prostate gland ANS: D High-risk factors include being an older adult, single, and male and having a co-occurring medical illness. Cancer is one of the somatic conditions associated with increased suicide risk. Protective factors for African-American women and Hispanic individuals include strong religious and family ties. Asian Americans have a suicide rate that increases with age. 23. A nurse answers a suicide crisis line. A caller says, I live alone in a home several miles from my nearest neighbors. I have been considering suicide for 2 months. I have had several drinks and now my gun is loaded. Im going to shoot myself in the heart. How would the nurse assess the lethality of this plan? a. No risk b. Low level c. Moderate level d. High level ANS: D The patient has a highly detailed plan, a highly lethal method, the means to carry it out, lowered impulse control because of alcohol ingestion, and a low potential for rescue. 24. A staff nurse tells another nurse, I evaluated a new patient using the SAD PERSONS scale and got a score of 10. Im wondering if I should send the patient home. Select the best reply by the second nurse. a. That action would seem appropriate. b. A score over 8 requires immediate hospitalization. c. I think you should strongly consider hospitalization for this patient. d. Give the patient a follow-up appointment. Hospitalization may be needed soon. ANS: B A SAD PERSONS scale score of 0 to 5 suggests home care with follow-up. A score of 6 to 8 requires psychiatric consultation. A score over 8 calls for hospitalization. 25. A patient recently hospitalized for two weeks committed suicide during the night. Which initial measure will be most helpful for staff members and other patients regarding this event? a. Request the public information officer to make an announcement to the local media. b. Hold a staff meeting to express feelings and plan the care for other patients. c. Ask the patients roommate not to discuss the event with other patients. d. Quickly discharge as many patients as possible to prevent panic. ANS: B Interventions should be aimed at helping the staff and patients come to terms with the loss and to grow because of the incident. Then, a community meeting should be scheduled to allow other patients to express their feelings and request help. Staff members should be prepared to provide additional support and reassurance to patients and should seek opportunities for peer support. The incorrect options will not control information or may result in unsafe care. Chapter 12. Caring for Patients with Mental Illness and Substance Use Disorders in General Practice Settings MULTIPLE CHOICE 1. When asked, What causes alcoholism? the nurses response will be based on the fact that: a. The response to alcohol is a result of a brain-based disorder. b. Alcoholism is believed to be an allergic response to the alcohol. c. Every individual has the same susceptibility for developing alcoholism. d. It is a physical response to alcohol but its etiology is not fully understood. ANS: A It has been determined that alcoholism is not an allergy but rather it is recognized as a partial brain-based disorder that some brains are more susceptible to than others. 2. Which patient response would support the conclusion that the patient has moved into the dark side of a narcotic addition? a. Ive been abusing drugs for at least 10 years. b. Drugs makes me feel good; that why I use them. c. I dont like the way I feel when I dont use drugs. d. Drugs are something that I can either take or leave ANS: C During beginning use (the light side), the feel good effects are dominant. As the individual becomes habituated to the drug, tolerance and withdrawal symptoms develop; this constitutes the dark side. The remaining options do not describe effects of drug use. 3. A substance use disorder (SUD) is a likely comorbid mental illness in which patient? a. The soldier diagnosed with posttraumatic stress disorder b. The teenager demonstrating symptoms of poor impulse control c. The older adult diagnosed with early stage Alzheimers disease d. The new mother exhibiting symptoms of postpartum depression ANS: A Posttraumatic stress disorder creates a risk for substance use or relapse. A total of 30% to 60% of persons with SUDs meet the criteria for comorbid posttraumatic stress disorder. The remaining options have not shown such a prevalence of comorbid relationship with SUDs. 4. Which group would be the target population for educational material on the dangers of binge drinking? a. Full-time college students b. Blue-collared young adults c. Older widows and widowers d. High school juniors and seniors ANS: A The highest prevalence of binge and heavy drinking is among young adults between the ages of 18 and 25 years, with the majority being full-time college students. 5. Which social factor has the greatest impact on the changing nature of alcohol abuse treatment? a. Development of new pharmaceutical treatment options b. Dramatic increase of alcoholism among young adult males c. Raising cost of both inpatient and outpatient treatment programs d. Womens substance abuse only recently acknowledge by society ANS: D The existence of an alcohol abuse problem among women has only been recently recognized and this has dramatically affected treatments and services being provided. Although the other options are true, they do not have the impact on treatment modalities as much as the correct option. 6. Which assessment data poses the greatest risk for injury in a patient who abuses alcohol? a. Takes a baby aspirin each morning b. Uses over-the-counter antihistamines for seasonal allergies c. Has been taking a tricyclic antidepressant for more than 2 years d. Took a narcotic for 1 week to manage postdental surgery pain ANS: C Tricyclic antidepressants are strictly contraindicated with alcohol consumption because of their potential effect on cardiac function. Although aspirin increases bleeding times and antihistamines and narcotics increase sedation, the outcome of combining alcohol and these drugs is not as dangerous as that of the correct option. 7. If an individual is admitted with a diagnosis of Wernicke-Korsakoffs syndrome, the nurse would expect to assess: a. Peptic ulcer b. Vivid illusions c. Cognitive deficits d. Auditory hallucinations ANS: C Wernicke-Korsakoffs syndrome includes a severe form of amnesia and an inability to learn new skills which reflects a cognitive impairment. The other options are not associated with the syndrome. 8. Which sociological aspect, vital to relapse prevention, is greatly affected when a patient is found to have a dual diagnosis of psychosis and alcoholism? a. Ability to afford the cost of outpatient services b. A supportive, reliable, accessible support system c. Protection from both physical and emotional abuse d. Access to reasonable housing and employment opportunities ANS: B Often individuals with this type of diagnosis have lost their support systems as a result of chronic mistreatment of their family and friends and an inability to maintain and recognize the importance of this aspect to their treatment plan. Although the remaining options impact relapse prevention, they are generally available when the patient is being supported appropriately. 9. Which nursing intervention best demonstrates an understanding of the relationship between confirmed intravenous drug abuse and specific infections? a. Screening the patient for hepatitis B virus (HBV) b. Assessing the patient for potentially infected injection sites c. Determining if the patient has ever been tested for human immunodeficiency virus (HIV) d. Evaluating the patients understanding of the increased risk for developing sexually transmitted diseases ANS: A Injecting drug users have one of the highest HBV rates among all risk groups and account for at least half of all new HCV cases, so screening for such infections demonstrates that the nurse understands the severity of the problem. Although the other options reflect potential infection risks, they are not as commonly seen in patients with this diagnosis. 10. Which assessment data would bring into question a patients statement that, I have only a few drinks on special occasions.? a. History of treatment for glaucoma b. Fasting serum blood glucose level of 182 mg/dL c. Patient reports numbness in hands and feet bilaterally d. Red rash observed over neck, shoulders, and upper chest ANS: C Peripheral nerve deterioration in both hands and feet result from chronic alcohol intake. Peripheral neuropathy occurs in about 10% of alcoholics after years of heavy drinking causing the nurse to question the patients statement. The remaining options do not reflect symptomology generally associated with alcoholism. 11. Which intervention has priority when a nurse suspects a staff member of providing patient care while being impaired by alcohol or drugs? a. Asking the staff member to explain their suspicious behavior b. Adjust the staff members assignment to minimize patient contact c. Providing the staff member with material regarding alcohol abuse and treatment d. Reporting the staff members suspicious behavior to the nursing supervisor on duty ANS: D It is a professional obligation to report suspected impaired practice. The remaining options do not have prior in this situation since the concern is patient safety. 12. Which nursing intervention demonstrates an understanding regarding the primary form of substance use disorder among older adults? a. Assessing the patients hands and feet for the presence of both numbness and tingling b. Having the patient, describe your relationship with you adult children, co- workers, and friends. c. Asking, Please identify for me all the medications both prescribed and over the counter you regularly take. d. Evaluate the patients understanding of the possible health risks that alcohol and medication abuse has on ones health ANS: C Misuse of prescription medications is the most common form of drug abuse among older adults. This population is especially vulnerable because of the multiple drugs that are often prescribed for medical conditions. The remaining options do not help identify the presence of multiple medications. 13. Which assessment demonstrates the nurses understanding of the relationship between substance abuse and the development of symptoms characteristic of delirium? a. Determining the patients age and gender b. Evaluating the patients food and fluid intake over the last 48 hours c. Observing the patient for fine tremors of the hands, especially the fingers d. Determining the amount of caffeine the patient ingested in the last 24 hours ANS: D Some people who ingest large amounts of caffeine develop delirium. The remaining options are not relevant to caffeine ingestion or the abuse of any other substance. 14. Which protocol should guide the nurse responsible for administering pharmacologic interventions for a patient who is experiencing alcohol intoxication? a. Medication interventions are based on the presence of withdrawal symptoms. b. Medications are prescribed at appropriate intervals for at least one full week. c. Symptoms are managed with medications for only the initial 24 hours of hospitalization. d. Medications are introduced to treat grand mal seizures that may accompany withdrawal symptoms. ANS: A The course of intoxication is usually self-limiting to approximately 24 hours, after which withdrawal symptoms can occur for a time period unique to each patient. Treatment is directed by the symptoms the patient is experiencing, which generally emerge during the withdrawal stage. Seizures are among several serious symptoms that can occur during the withdrawal stage. 15. A patient recently discharged from an alcohol rehabilitation program is brought to the hospital in a state of prostration with severe throbbing headache, tachycardia, a beet-red face, dyspnea, and continuous vomiting. The patients significant other states the patient got sick about 15 minutes after drinking a glass of wine. The nurse should be guided in assessment by the suspicion that the patient: a. Is having a stroke b. Has alcohol intoxication c. Is reacting to disulfiram (Antabuse) d. Is exhibiting symptoms of cross-dependence ANS: C The alcohol deterrent drug, Antabuse, commonly prescribed in recovering alcoholic treatment, causes this reaction when taken in combination with alcohol. Alcohol intoxication, stroke, and cross-dependence do not present with the listed prostration symptoms. 16. Which question is most appropriate when assessing a patient who is exhibiting symptoms of a systemic infection including a fever of unknown origin? a. Are you an intravenous drug user? b. Have you been told that you drink too much alcohol? c. Have you been diagnosed with an acute bacterial infection before? d. Are you familiar with an infection of the heart called endocarditis? ANS: A Intravenous drug users are at risk for subacute bacterial endocarditis and other circulatory compromise created by foreign substances introduced during the process of intravenous use. Regardless of the setting, nurses need to ask about intravenous drug use whenever a patient presents with fever of unexplained origin. Assessing the patients knowledge related to bacterial infections and endocarditis will not address the possible cause of the fever. Alcohol consumption is not relevant in this situation. 17. Which observation seen in a teenage patient supports the suspicion of anabolic steroid abuse? a. Lack of facial hair b. Ritualized hand washing c. Stealing and hiding a magazine belonging to another patient d. Throwing a chair when told it was time to turn off the television ANS: D For all individuals abusing anabolic steroids, extreme mood swings occur, and these may be accompanied by violent behaviors. Obsessive-compulsive behaviors and stealing are not generally associated with this disorder. The increased hormone presence would result not in a lack, but rather an increase, in facial hair. 18. A patients wife has chronic alcoholism, and the husband is concerned about the possibility that their children may develop the disease. He asks the nurse what the risk is. The nurses best response is: a. The risk for developing alcoholism is increased if there is a family history of alcoholism. b. Studies have confirmed that individuals with dependent personality traits are at high risk for this disease. c. Cultures that include alcohol as part of the ritualized behavior have a higher rate of alcoholism. d. Twin studies have indicated that the environment of a person is more important than the biologic influences of parents. ANS: A Problems with alcohol increase with the number of relatives with alcoholism. No unique personality profile is prone to addiction. Ritualized use of alcohol does not predispose to alcoholism and twin studies indicate a significant genetic contribution to susceptibility to alcoholism. 19. Which observation best supports the patients success with achieving long-term sobriety? a. Asking a family member to, get rid of all the alcohol before I come home b. Identifying all the problems alcoholism has caused the family over the years c. Being able to discuss the importance of attending a support group for alcoholics d. Promising to, stop the drinking so I can be a good parent and raise a good child ANS: B One of the most prominent factors that leads an individual to recovery is the patients recognition that substance use has caused or influenced his or her lifes problems and interrupted his or her functioning. The remaining options lack that element of self-reflection. 20. Which principle of recovery is the basis of the nurses response when a patient relapses and is hospitalized for alcohol detox treatment? a. Alcoholism requires a lifelong commitment to control. b. Most people who are serious about treatment achieve sobriety. c. Relapsing is an expected occurrence for the patient diagnosed with alcohol abuse. d. Rehabilitation generally involves several relapses before true sobriety is achieved. ANS: D Sobriety is the goal of complete abstention from drugs, alcohol, and addictive behaviors. Sobriety often involves several attempts, and many patients relapse 9 or 10 times before achieving and sustaining sobriety. This information is the basis for the physical and emotional support provided by the nurse. Although citing that a relapse is not a failure but an expected part of the recovery process, this option does not include the needed information of the frequency of the possible relapses. The remaining options are not focused on relapsing. Chapter 13. Neurocognitive Disorders Multiple Choice 1. A geriatric nurse is teaching the clients family about the possible cause of delirium. Which statement by the nurse is most accurate? 1. Taking multiple medications may lead to adverse interactions or toxicity. 2. Age-related cognitive changes may lead to alterations in mental status. 3. Lack of rigorous exercise may lead to decreased cerebral blood flow. 4. Decreased social interaction may lead to profound isolation and psychosis. ANS: 1 Rationale: The nurse should identify that taking multiple medications that may lead to adverse reactions or toxicity is a risk factor for the development of delirium in older adults. Symptoms of delirium include difficulty sustaining and shifting attention. The client with delirium is disoriented to time and place and may also have impaired memory. Cognitive Level: Application Integrated Process: Implementation 2. A husband has agreed to admit his spouse, diagnosed with Alzheimers disease (AD), to a long-term care facility. He is expressing feelings of guilt and symptoms of depression. Which appropriate nursing diagnosis and subsequent intervention would the nurse document? 1. Dysfunctional grieving; AD support group 2. Altered thought process; AD support group 3. Major depressive episode; psychiatric referral 4. Caregiver role strain; psychiatric referral ANS: 1 Rationale: The most appropriate nursing diagnosis and intervention for the husband is dysfunctional grieving; AD support group. Clients with AD are often at risk for trauma and have significant self-care deficits that require more care than a spouse may be able to provide. Cognitive Level: Analysis Integrated Process: Diagnosis/Implementation 3. A client diagnosed with vascular neurocognitive disorder (NCD) is discharged to home under the care of his wife. Which information should cause the nurse to question the clients safety? 1. His wife works from home in telecommunication. 2. The client has worked the nightshift his entire career. 3. His wife has minimal family support. 4. The client smokes one pack of cigarettes per day. ANS: 4 Rationale: The nurse should question the clients safety at home if the client smokes cigarettes. Vascular NCD is a clinical syndrome of NCD due to significant cerebrovascular disease. The cause of vascular NCD is related to an interruption of blood flow to the brain. Hypertension is a significant factor in the etiology. Cognitive Level: Application Integrated Process: Assessment 4. A client diagnosed with AD can no longer ambulate, does not recognize family members, and communicates with agitated behaviors and incoherent verbalizations. The nurse recognizes these symptoms as indicative of which stage of the illness? 1. Stage 4: Mild-to-Moderate Cognitive Decline 2. Stage 5. Moderate Cognitive Decline 3. Stage 6. Moderate-to-Severe Cognitive Decline 4. Stage 7. Severe Cognitive Decline ANS: 4 Rationale: The nurse should recognize that a client exhibiting these symptoms is in the severe cognitive decline, seventh stage, of AD. Cognitive Level: Application Integrated Process: Assessment 5. A client is diagnosed in stage seven of AD. To address the clients symptoms, which nursing intervention should take priority? 1. Improve cognitive status by encouraging involvement in social activities. 2. Decrease social isolation by providing group therapies. 3. Promote dignity by providing comfort, safety, and self-care measures. 4. Facilitate communication by providing assistive devices. ANS: 3 Rationale: The most appropriate intervention in the seventh stage of AD is to promote the clients dignity by providing comfort, safety, and self-care measures. Stage is characterized by severe cognitive decline in which the client is unable to recognize family members and is most commonly bedfast and aphasic. Cognitive Level: Application Integrated Process: Implementation 6. Which is the reason for the proliferation of the diagnosis of NCDs? 1. Increased numbers of neurotransmitters has been implicated in the proliferation of NCD. 2. Similar symptoms of NCD and depression lead to misdiagnoses, increasing numbers of NCD. 3. Societal stress contributes to the increase in this diagnosis. 4. More people now survive into the high-risk period for neurocognitive disorders. ANS: 4 Rationale: The proliferation of NCD has occurred because more people now survive into the high-risk period for neurocognitive disorder, which is middle age and beyond.. Cognitive Level: Application Integrated Process: Assessment 7. A client diagnosed recently with AD is prescribed donepezil (Aricept). The clients spouse inquires, How does this work? Will this cure him? Which is the appropriate nursing response? 1. This medication delays the destruction of acetylcholine, a chemical in the brain necessary for memory processes. Although most effective in the early stages, it serves to delay, but not stop, the progression of the disease. 2. This medication encourages production of acetylcholine, a chemical in the brain necessary for memory processes. It delays the progression of the disease. 3. This medication delays the destruction of dopamine, a chemical in the brain necessary for memory processes. Although most effective in the early stages, it serves to delay, but not stop, the progression of the disease. 4. This medication encourages production of dopamine, a chemical in the brain necessary for memory processes. It delays the progression of the disease. ANS: 1 Rationale: The most appropriate response by the nurse is to explain that donepezil delays the destruction of acetylcholine, a chemical in the brain necessary for memory processes. Although most effective in the early stages, it serves to delay, but not stop, the progression of the AD. Some side effects include dizziness, headache, gastrointestinal upset, and elevated transaminase. Cognitive Level: Application Integrated Process: Implementation 8. Which symptom should a nurse identify that differentiates clients diagnosed with NCDs from clients diagnosed with mood disorders? 1. Altered sleep 2. Altered concentration 3. Impaired memory 4. Impaired psychomotor activity ANS: 3 Rationale: The nurse should identify that impaired memory is a symptom that occurs in NCD and not in mood disorders. Neurocognitive disorder is classified in the DSM-5 as either mild or major, with the distinction primarily being one of severity of symptomatology. Cognitive Level: Application Integrated Process: Assessment 9. A client diagnosed with AD exhibits progressive memory loss, diminished cognitive functioning, and verbal aggression upon experiencing frustration. Which nursing intervention is most appropriate? 1. Organize a group activity to present reality. 2. Minimize environmental lighting. 3. Schedule structured daily routines. 4. Explain the consequences for aggressive behaviors. ANS: 3 Rationale: The most appropriate nursing intervention for this client is to schedule structured daily routines. A structured routine will reduce frustration and thereby reduce verbal aggression. Cognitive Level: Application Integrated Process: Implementation 10. After one week of continuous mental confusion, an older African American client is admitted with a preliminary diagnosis of AD. What should cause the nurse to question this diagnosis? 1. AD does not typically occur in African American clients. 2. The symptoms presented are more indicative of Parkinsonism. 3. AD does not develop suddenly. 4. There has been no T3- or T4-level evaluation ordered. ANS: 3 Rationale: The nurse should recognize that AD does not develop suddenly and should question this diagnosis. The onset of AD symptoms is slow and insidious. The disease is generally progressive and deteriorating. Cognitive Level: Application Integrated Process: Evaluation 11. A client diagnosed with AD has impairments of memory and judgment and is incapable of performing activities of daily living. Which nursing intervention should take priority? 1. Present evidence of objective reality to improve cognition. 2. Design a bulletin board to represent the current season. 3. Label the clients room with name and number. 4. Assist with bathing and toileting. ANS: 4 Rationale: The priority nursing intervention for this client is to assist with bathing and toileting. A client who is incapable of performing activities of daily living requires assistance in these areas to ensure health and safety. Cognitive Level: Application Integrated Process: Implementation 12. A client diagnosed with major NCD is exhibiting behavioral problems on a daily basis. At change of shift, the clients behavior escalates from pacing to screaming and flailing. Which action should be a nursing priority? 1. Consult the psychologist regarding behavior-modification techniques. 2. Medicate the client with prn antianxiety medications. 3. Assess environmental triggers and potential unmet needs. 4. Anticipate the behavior and restrain when pacing begins. ANS: 2 Rationale: The priority nursing action is to first medicate the client to avoid injury to self or others. It is important to assess environmental triggers and potential unmet needs in order to address these problems in the future, but interventions to ensure safety must take priority. Because of the cognitive decline experienced in clients diagnosed with this disorder, communication skills and orientation may limit assessment and teaching interventions. Cognitive Level: Analysis Integrated Process: Implementation 13. A client with a history of cerebrovascular accident (CVA) is brought to an emergency department experiencing memory problems, confusion, and disorientation. Based on this clients assessment data, which diagnosis would the nurse expect the physician to assign? 1. Delirium due to adverse effects of cardiac medications 2. Vascular neurocognitive disorder 3. Altered thought processes 4. Alzheimers disease ANS: 2 Rationale: The nurse should expect that the client will be diagnosed with vascular NCD, which is caused by significant cerebrovascular disease. Vascular NCD often has an abrupt onset. Progression of this disease often occurs in a fluctuating pattern. Cognitive Level: Application Integrated Process: Assessment 14. An older client has recently moved to a nursing home. The client has trouble concentrating and socially isolates. A physician believes the client would benefit from medication therapy. Which medication should the nurse expect the physician to prescribe? 1. Haloperidol (Haldol) 2. Donepezil (Aricept) 3. Diazepam (Valium) 4. Sertraline (Zoloft) ANS: 4 Rationale: The nurse should expect the physician to prescribe sertraline to improve the clients social functioning and concentration levels. Sertraline is an selective serotonin reuptake inhibitor (SSRI) antidepressant. Depression is the most common mental illness in older adults and is often misdiagnosed as a neurocognitive disorder. Cognitive Level: Application Integrated Process: Assessment 15. A client diagnosed with NCD is disoriented and ataxic and wanders. Which is the priority nursing diagnosis? 1. Disturbed thought processes 2. Self-care deficit 3. Risk for injury 4. Altered health-care maintenance ANS: 3 Rationale: The priority nursing diagnosis for this client is risk for injury. The client who is ataxic suffers from motor coordination deficits and is at an increased risk for falls. Clients that wander are at a higher risk for injury. Cognitive Level: Analysis Integrated Process: Diagnosis 16. Which statement accurately differentiates mild NCD from major NCD? 1. Major NCD involves disorientation that develops suddenly, whereas mild NCD develops more slowly. 2. Major NCD involves impairment of abstract thinking and judgment, whereas mild NCD does not. 3. Major NCD criteria requires substantial cognitive decline from a previous level of performance, and mild NCD requires modest decline. 4. Major NCD criteria requires decline from a previous level of performance in three of the listed domains, and mild NCD requires only one. ANS: 3 Rationale: The progression of the disorder is not a criterion for determining the severity of an NCD. Abstract thinking and judgment can be affected in both mild NCD and major NCD. Major NCD criteria requires substantial cognitive decline, and mild NCD requires modest decline. Both major and mild NCD classifications require decline from a previous level of performance in only one of the listed domains. Cognitive Level: Analysis Integrated Process: Assessment 17. Which statement accurately differentiates NCD from pseudodementia (depression)? 1. NCD has a rapid onset, whereas pseudodementia does not. 2. NCD symptoms include disorientation to time and place, and pseudodementia does not. 3. NCD symptoms improve as the day progresses, but symptoms of pseudodementia worsen. 4. NCD causes decreased appetite, whereas pseudodementia does not. ANS: 2 Rationale: NCD has a slow progression of symptoms, whereas pseudodementia has a rapid progression of symptoms. NCD symptoms include disorientation to time and place, and pseudodementia does not. NCD symptoms severity worsens as the day progresses, whereas in pseudodementia, symptoms improve as the day progresses. In NCD the appetite remains unchanged. whereas in pseudodementia, the appetite diminishes. Cognitive Level: Analysis Integrated Process: Assessment Multiple Response 18. Which of the following conditions have been known to precipitate delirium in some individuals? (Select all that apply.) 1. Febrile illness 2. Seizures 3. Migraine headaches 4. Herniated brain stem 5. Temporomandibular joint syndrome ANS: 1, 2, 3 Rationale: Delirium most commonly occurs in individuals with serious medical, surgical, or neurological conditions. Some examples of conditions that have been known to precipitate delirium in some individuals include the following: systemic infections; febrile illness; metabolic disorders, such as hypoxia, hypercarbia, or hypoglycemia; hepatic encephalopathy; head trauma; seizures; migraine headaches; brain abscess; stroke; postoperative states; and electrolyte imbalance. A herniated brain stem would most likely result in death, not delirium. Temporomandibular joint syndrome is marked by limited movement of the joint during chewing, not delirium. Cognitive Level: Application Integrated Process: Assessment 19. Which of the following medications that have been known to precipitate delirium? (Select all that apply.) 1. Antineoplastic agents 2. H2-receptor antagonists 3. Antihypertensives 4. Corticosteroids 5. Lipid-lowering agents ANS: 1, 2, 3, 4 Rationale: Medications that have been known to precipitate delirium include anticholinergics, antihypertensives, corticosteroids, anticonvulsants, cardiac glycosides, analgesics, anesthetics, antineoplastic agents, antiparkinson drugs, H2-receptor antagonists (e.g., cimetidine), and others. There have been no reports of delirium ascribed to the use of lipid-lowering agents. Cognitive Level: Application Integrated Process: Assessment Fill-in-the-Blank 20. Major NCD constitutes what was previously described as in the DSM-5-TR. ANS: dementia Rationale: NCD is classified in the DSM-5 as either mild or major, with the distinction primarily being one of severity of symptomatology. Major NCD constitutes what was previously described as dementia in the DSM-5-TR. Chapter 14. Substance Use and Addictive Disorders Multiple Choice 1. What should be the priority nursing diagnosis for a client experiencing alcohol withdrawal? 1. Risk for injury R/T central nervous system stimulation 2. Disturbed thought processes R/T tactile hallucinations 3. Ineffective coping R/T powerlessness over alcohol use 4. Ineffective denial R/T continued alcohol use despite negative consequences ANS: 1 Rationale: The priority nursing diagnosis for a client experiencing alcohol withdrawal should be risk for injury R/T central nervous system stimulation. Alcohol withdrawal may include the following symptoms: course tremors of hands, tongue, or eyelids; nausea or vomiting; malaise or weakness; tachycardia; sweating; elevated blood pressure; anxiety; depressed mood; hallucinations; headache; and insomnia. Cognitive Level: Analysis Integrated Process: Diagnosis 2. A nurse evaluates a clients patient-controlled analgesia (PCA) pump and notices 100 attempts within a 30-minute period. Which is the best rationale for assessing this client for substance addiction? 1. Narcotic pain medication is contraindicated for all clients with active substance use disorders. 2. Clients who are addicted to alcohol or benzodiazepines may develop cross-tolerance to analgesics and require increased doses to achieve effective pain control. 3. There is no need to assess the client for substance addiction. There is an obvious PCA malfunction, because these clients have a higher pain tolerance. 4. The client is experiencing alcohol withdrawal symptoms and needs accurate assessment. ANS: 2 Rationale: The nurse should assess the client for substance addiction, because clients who are addicted to alcohol or benzodiazepines may have developed cross-tolerance to analgesics and require increased doses to achieve effective pain control. Cross-tolerance is exhibited when one drug results in a lessened response to another drug. Cognitive Level: Application Integrated Process: Evaluation 3. On the first day of a clients alcohol detoxification, which nursing intervention should take priority? 1. Strongly encourage the client to attend 90 Alcoholics Anonymous (AA) meetings in 90 days. 2. Educate the client about the biopsychosocial consequences of alcohol abuse. 3. Administer ordered chlordiazepoxide (Librium) in a dosage according to protocol. 4. Administer vitamin B1 to prevent Wernicke-Korsakoff syndrome. ANS: 3 Rationale: The priority nursing intervention for this client should be to administer ordered chlordiazepoxide in a dosage according to protocol. Chlordiazepoxide is a benzodiazepine and is often used for substitution therapy in alcohol withdrawal to reduce life-threatening complications. Cognitive Level: Application Integrated Process: Implementation 4. Which client statement indicates a knowledge deficit related to a substance use disorder? 1. Although its legal, alcohol is one of the most widely abused drugs in our society. 2. Tolerance to heroin develops quickly. 3. Flashbacks from LSD use may reoccur spontaneously. 4. Marijuana is like smoking cigarettes. Everyone does it. Its essentially harmless. ANS: 4 Rationale: The nurse should determine that the client has a knowledge deficit related to substance use disorders when the client compares marijuana to smoking cigarettes and claims it to be harmless. Cannabis is the second most widely abused drug in the United States. Cognitive Level: Application Integrated Process: Evaluation 5. A lonely, depressed divorce has been self-medicating with small amounts of cocaine for the past year. Which term should a nurse use to best describe this individuals situation? 1. Psychological addiction 2. Physical addiction 3. Substance induced disorder 4. Social induced disorder ANS: 1 Rationale: The nurse should use the term psychological addiction to best describe the clients situation. A client is considered to be psychologically addicted to a substance when there is an overwhelming desire to use a drug in order to produce pleasure or avoid discomfort. Cognitive Level: Application Integrated Process: Assessment 6. Which term should a nurse use to describe the administration of a central nervous system (CNS) depressant during the substance induced disorder of alcohol withdrawal? 1. Antagonist therapy 2. Deterrent therapy 3. Codependency therapy 4. Substitution therapy ANS: 4 Rationale: Various medications have been used to decrease the intensity of symptoms in an individual who is withdrawing from, or who is experiencing the effects of excessive use of, alcohol and other drugs. This is called substitution therapy and may be required to reduce the life-threatening effects of alcohol withdrawal. Cognitive Level: Application Integrated Process: Assessment 7. A client diagnosed with chronic alcohol addiction is being discharged from an inpatient treatment facility after detoxification. Which client outcome, related to AA, would be most appropriate for a nurse to discuss with the client during discharge teaching? 1. After discharge, the client will immediately attend 90 AA meetings in 90 days. 2. After discharge, the client will rely on an AA sponsor to help control alcohol cravings. 3. After discharge, the client will incorporate family in AA attendance. 4. After discharge, the client will seek appropriate deterrent medications through AA. ANS: 1 Rationale: The most appropriate client outcome for the nurse to discuss during discharge teaching is attending 90 AA meetings in 90 days after discharge. AA is a major self-help organization for the treatment of alcohol addiction. It accepts alcohol addiction as an illness and promotes total abstinence as the only cure. Cognitive Level: Application Integrated Process: Implementation 8. A client with a history of heavy alcohol use is brought to an emergency department (ED) by family members who state that the client has had nothing to drink in the last 48 hours. When the nurse reports to the ED physician, which client symptom should be the nurses first priority? 1. Hearing and visual impairment 2. Blood pressure of 180/100 mm Hg 3. Mood rating of 2/10 on numeric scale 4. Dehydration ANS: 2 Rationale: The nurse should recognize that high blood pressure is a symptom of alcohol withdrawal syndrome and should promptly report this finding to the physician. Complications associated with alcohol withdrawal syndrome may progress to alcohol withdrawal delirium in about the second or third day following cessation of prolonged alcohol use. Cognitive Level: Analysis Integrated Process: Implementation 9. Which client statement demonstrates positive progress toward recovery from a substance use disorder? 1. I have completed detox and therefore am in control of my drug use. 2. I will faithfully attend Narcotic Anonymous (NA) when I cant control my cravings. 3. As a church deacon, my focus will now be on spiritual renewal. 4. Taking those pills got out of control. It cost me my job, marriage, and children. ANS: 4 Rationale: A client who takes responsibility for the consequences of substance use disorder or substance addiction is making positive progress toward recovery. This would indicate completion of the first step of a 12-step program. Cognitive Level: Application Integrated Process: Evaluation 10. A nurse holds the hand of a client who is withdrawing from alcohol. What is the nurses rationale for this intervention? 1. To assess for emotional strength 2. To assess for Wernicke-Korsakoff syndrome 3. To assess for tachycardia 4. To assess for fine tremors ANS: 4 Rationale: The nurse is most likely assessing the client for fine tremors secondary to alcohol withdrawal. Withdrawal from alcohol can also cause headache, insomnia, transient hallucinations, depression, irritability, anxiety, elevated blood pressure, sweating, tachycardia, malaise, and coarse tremors. Cognitive Level: Analysis Integrated Process: Assessment 11. A client presents with symptoms of alcohol withdrawal and states, I havent eaten in three days. A nurses assessment reveals BP 170/100 mm Hg, P 110, R 28, and T 97F (36C) with dry mucous membranes and poor skin turgor. What should be the priority nursing diagnosis? 1. Knowledge deficit 2. Fluid volume excess 3. Imbalanced nutrition: less than body requirements 4. Ineffective individual coping ANS: 3 Rationale: The nurse should assess that the priority nursing diagnosis is imbalanced nutrition: less than body requirements. The client is exhibiting signs and symptoms of malnutrition as well as alcohol withdrawal. The nurse should consult a dietitian, restrict sodium intake to minimize fluid retention, and provide small, frequent feedings of nonirritating foods. Cognitive Level: Analysis Integrated Process: Diagnosis 12. A clients wife has been making excuses for her alcoholic husbands work absences. In family therapy, she states, His problems at work are my fault. Which is the appropriate nursing response? 1. Why do you assume responsibility for his behaviors? 2. I think you should start to confront his behavior. 3. Your husband needs to deal with the consequences of his drinking. 4. Do you understand what the term enabler means? ANS: 3 Rationale: The appropriate nursing response is to use confrontation with caring. The nurse should understand that the clients wife may be in denial and enabling the husbands behavior. Codependency is a typical behavior of spouses of alcoholics. Partners of clients with substance addiction must come to realize that the only behavior they can control is their own. Cognitive Level: Application Integrated Process: Implementation 13. Which medication orders should a nurse anticipate for a client who has a history of benzodiazepine withdrawal delirium? 1. Haloperidol (Haldol) and fluoxetine (Prozac) 2. Carbamazepine (Tegretol) and donepezil (Aricept) 3. Disulfiram (Antabuse) and lorazepan (Ativan) 4. Chlordiazepoxide (Librium) and phenytoin (Dilantin) ANS: 4 Rationale: The nurse should anticipate that a physician would order chlordiazepoxide and phenytoin for a client who has a history of benzodiazepine withdrawal delirium. It is common for long-lasting benzodiazepines to be prescribed for substitution therapy. Phenytoin is an anticonvulsant used to prevent seizures. Cognitive Level: Application Integrated Process: Assessment 14. A nurse is interviewing a client in an outpatient addiction clinic. To promote success in the recovery process, which outcome should the nurse expect the client to initially accomplish? 1. The client will identify one person to turn to for support. 2. The client will give up all old drinking buddies. 3. The client will be able to verbalize the effects of alcohol on the body. 4. The client will correlate life problems with alcohol use. ANS: 4 Rationale: The nurse should expect that the client would initially correlate life problems with alcohol addiction. Acceptance of the problem is the first part of the recovery process. Cognitive Level: Application Integrated Process: Planning 15. A nurse is reviewing the stat laboratory data of a client in the emergency department. At what minimum blood alcohol level should a nurse expect intoxication to occur? 1. 50 mg/dL 2. 100 mg/dL 3. 250 mg/dL 4. 300 mg/dL ANS: 2 Rationale: The nurse should expect that 100 mg/dL is the minimum blood alcohol level at which intoxication occurs. Intoxication usually occurs between 100 and 200 mg/dL. Death has been reported at levels ranging from 400 to 700 mg/dL. Cognitive Level: Application Integrated Process: Evaluation 16. A client diagnosed with major depressive episode and substance use disorder has an altered sleep pattern and demands that a psychiatrist prescribe a sedative. Which rationale explains why a nurse should encourage the client to first try nonpharmacological interventions? 1. Sedative-hypnotics are potentially addictive, and their effectiveness will be compromised owing to tolerance. 2. Sedative-hypnotics are expensive and have numerous side effects. 3. Sedative-hypnotics interfere with necessary REM (rapid eye movement) sleep. 4. Sedative-hypnotics are known not to be as effective in promoting sleep as antidepressant medications. ANS: 1 Rationale: The nurse should recommend nonpharmacological interventions to this client because sedative-hypnotics are potentially addictive, and their effectiveness will be compromised owing to tolerance. The effects of central nervous system depressants are additive with one another, capable of producing physiological and psychological addiction. Cognitive Level: Application Integrated Process: Implementation 17. A client diagnosed with a gambling disorder asks the nurse about medications that may be ordered by the clients physician to treat this disorder. The nurse would give the client information on which medications? 1. Escitalopram (Lexapro) and clozapine (Clozaril) 2. Citalopram (Celexa) and olanzapine (Zyprexa) 3. Lithium carbonate (Lithobid) and sertraline (Zoloft) 4. Naltrexone (ReVia) and ziprasidone (Geodon) ANS: 3 Rationale: The SSRIs and clomipramine have been used successfully in the treatment of pathological gambling as a form of obsessive-compulsive disorder. Lithium, carbamazepine, and naltrexone have also been shown to be effective. The antipsychotic medications clozapine, olanzapine, and ziprasidone are not treatments of choice for this disorder. Cognitive Level: Application Integrated Process: Implementation 18. A nurse is assessing a pathological gambler. What would differentiate this clients behaviors from the behaviors of a non-pathological gambler? 1. Pathological gamblers have abnormal levels of neurotransmitters, whereas non-pathological gamblers do not. 2. Pathological gambling occurs more commonly among women, whereas non-pathological gambling occurs more commonly among men. 3. Pathological gambling generally runs an acute course, whereas non-pathological gambling runs a chronic course. 4. Pathological gambling is not related to stress relief, whereas non-pathological gambling is related to stress relief. ANS: 1 Rationale: There is a correlation between pathological gambling and abnormalities in the serotonergic, noradrenergic, and dopaminergic neurotransmitter systems. This is not the case with non-pathological gambling. For a pathological gambler, the preoccupation with and impulse to gamble intensifies when the individual is under stress. This is not the case with non- pathological gambling. Pathological gambling occurs more commonly among men not women and generally runs a chronic not acute course. Cognitive Level: Analysis Integrated Process: Assessment 19. A nursing instructor is teaching about the impaired nurse and the consequences of this impairment. Which statement by a student indicates that further instruction is needed? 1. The state board of nursing must be notified with factual documentation of impairment. 2. All state boards of nursing have passed laws that, under any circumstances, do not allow impaired nurses to practice. 3. Many state boards of nursing require an impaired nurse to successfully complete counseling treatment programs prior to a return to work. 4. After a return to practice, a recovering nurse may be closely monitored for several years. ANS: 2 Rationale: Several state boards of nursing have passed diversionary laws that allow impaired nurses to avoid disciplinary action by agreeing to seek treatment. This may require successful completion of inpatient, outpatient, group, or individual counseling treatment program(s); evidence of regular attendance at nurse support groups or 12-step program; random negative drug screens; and employment or volunteer activities during the suspension period. When a nurse is deemed safe to return to practice, he or she may be closely monitored for several years and required to undergo random drug screenings. Cognitive Level: Application Integrated Process: Assessment Multiple Response 20. Which of the following nursing statements exemplify the cognitive process that must be completed by a nurse prior to caring for clients diagnosed with a substance-related disorder? (Select all that apply.) 1. I am easily manipulated and need to work on this prior to caring for these clients. 2. Because of my fathers alcoholism, I need to examine my attitude toward these clients. 3. I need to review the side effects of the medications used in the withdrawal process. 4. Ill need to set boundaries to maintain a therapeutic relationship. 5. I need to take charge when dealing with clients diagnosed with substance disorders. ANS: 1, 2, 4 Rationale: The nurse should complete a cognitive process prior to caring for clients diagnosed with substance-abuse disorders. It is important for nurses to identify potential areas of need within their own cognitions that may affect their relationships with clients diagnosed with this problem. Cognitive Level: Application Integrated Process: Implementation 21. A nursing instructor is teaching nursing students about cirrhosis of the liver. Which of the following statements about the complications of hepatic encephalopathy should indicate to the nursing instructor that further student teaching is needed? (Select all that apply.) 1. A diet rich in protein will promote hepatic healing. 2. This condition results from a rise in serum ammonia, leading to impaired mental functioning. 3. In this condition, an excessive amount of serous fluid accumulates in the abdominal cavity. 4. Neomycin and lactulose are used in the treatment of this condition. 5. This condition is caused by the inability of the liver to convert ammonia to urea. ANS: 1 Rationale: The nursing instructor should understand that further teaching is needed if the nursing student states that a diet rich in protein will promote hepatic healing. The treatment of hepatic encephalopathy requires abstention from alcohol and temporary elimination of protein from the diet. Cognitive Level: Application Integrated Process: Evaluation 22. A clinic nurse is about to meet with a client diagnosed with a gambling disorder. Which of the following symptoms and/or behaviors is the nurse likely to assess? (Select all that apply.) 1. Stressful situations precipitate gambling behaviors. 2. Anxiety and restlessness can only be relieved by placing a bet. 3. Winning brings about feelings of sexual satisfaction. 4. Gambling is used as a coping strategy. 5. Losing at gambling meets the clients need for self-punishment. ANS: 1, 2, 4, 5 Rationale: In gambling disorder, the preoccupation with and impulse to gamble intensifies when the individual is under stress. Many impulsive gamblers describe a physical sensation of restlessness and anticipation that can only be relieved by placing a bet. Winning brings feelings of special status, power, and omnipotence, not sexual satisfaction. The gambler increasingly depends on this activity to cope with disappointments, problems, and negative emotional states. Cognitive Level: Application Integrated Process: Assessment 23. A nursing supervisor is about to meet with a staff nurse suspected of diverting client medications. Which of the following assessment data would lead the supervisor to suspect that the staff nurse is impaired? (Select all that apply.) 1. The staff nurse is frequently absent from work. 2. The staff nurse experiences mood swings. 3. The staff nurse makes elaborate excuses for behavior. 4. The staff nurse frequently uses the restroom. 5. The staff nurse has a flushed face. ANS: 2, 3, 4, 5 Rationale: A number of clues for recognizing substance impairment in nurses have been identified. They are not easy to detect and will vary according to the substance being used. There may be high absenteeism if the persons source is outside the work area, or the individual may rarely miss work if the substance source is at work. Some other possible signs are irritability, mood swings, tendency to isolate, elaborate excuses for behavior, unkempt appearance, impaired motor coordination, slurred speech, flushed face, inconsistent job performance, and frequent use of the restroom. Cognitive Level: Application Integrated Process: Assessment 24. A nursing supervisor is offering an impaired staff member information regarding employee assistance programs. Which of the following facts should the supervisor include? (Select all that apply.) 1. A hotline number will be available in order to call for peer assistance. 2. A verbal contract detailing the method of treatment will be initiated prior to the program. 3. Peer support is provided through regular contact with the impaired nurse. 4. Contact to provide peer support will last for one year. 5. One of the program goals is to intervene early in order to reduce hazards to clients. ANS: 1, 3, 5 Rationale: The peer assistance programs strive to intervene early, to reduce hazards to clients, and increase prospects for the nurses recovery. Most states provide either a hotline number that the impaired nurse may call or phone numbers of peer assistance committee members, which are made available for the same purpose. Typically, a written, not verbal, contract is drawn up, detailing the method of treatment, which may be obtained from various sources, such as employee assistance programs, Alcoholics Anonymous, Narcotics Anonymous, private counseling, or outpatient clinics. Peer support is provided through regular contact with the impaired nurse, usually for a period of two years, not one year. Cognitive Level: Application Integrated Process: Assessment 25. A nursing counselor is about to meet with a client suffering from codependency. Which of the following data would further support the assessment of this dysfunctional behavior? (Select all that apply.) 1. The client has a long history of focusing thoughts and behaviors on other people. 2. The client, as a child, experienced overindulgent and overprotective parents. 3. The client is a people pleaser and does almost anything to gain approval. 4. The client exhibits helpless behaviors but actually feels very competent. 5. The client can achieve a sense of control only through fulfilling the needs of others. ANS: 1, 3, 5 Rationale: The codependent person has a long history of focusing thoughts and behavior on other people and is able to achieve a sense of control only through fulfilling the needs of others. Codependant clients are people pleasers and will do almost anything to get the approval of others. They usually have experienced abuse or emotional neglect as a child. They outwardly appear very competent, but actually feel quite needy, helpless, or perhaps nothing at all. Cognitive Level: Application Integrated Process: Assessment Ordered Response 26. Order the following stages of the codependency recovery process according to Cermak. The Core Issues Stage The Reintegration Stage The Survival Stage The Reidentification Stage ANS: The correct order is 3, 4, 1, 2 Rationale: Cermak in 1986 identified four stages in the recovery process for individuals with codependent personality: During the survival stage, the codependent must begin to let go of denial. During the reidentification stage, the individual begins to glimpse their true selves. During the core issues stage, the individual must face the fact that relationships cannot be managed by force or will. During the reintegration stage, control is achieved through self- discipline and self-confidence. 1. The Survival Stage 2. The Reidentification Stage 3. The Core Issues Stage 4. The Reintegration Stage Cognitive Level: Analysis Integrated Process: Assessment Fill-in-the-Blank 27. The concept of arose out of a need to define the dysfunctional behaviors that are evident among members of the family of a chemically dependent person. ANS: codependency Rationale: The concept of codependency arose out of a need to define the dysfunctional behaviors that are evident among members of the family of a chemically dependent person. The term has been expanded to include all individuals from families that harbor secrets of physical or emotional abuse, other cruelties, or pathological conditions. Chapter 15. Schizophrenia Spectrum and Other Psychotic Disorders Multiple Choice 1. A paranoid client presents with bizarre behaviors, neologisms, and thought insertion. Which nursing action should be prioritized to maintain this clients safety? 1. Assess for medication nonadherance. 2. Note escalating behaviors and intervene immediately. 3. Interpret attempts at communication. 4. Assess triggers for bizarre, inappropriate behaviors. ANS: 2 Rationale: The nurse should note escalating behaviors and intervene immediately, to maintain this clients safety. Early intervention may prevent an aggressive response and keep the client and others safe. Cognitive Level: Analysis Integrated Process: Implementation 2. A client diagnosed with schizoaffective disorder is admitted for social skills training. Which information should be included in the nurses teaching? 1. The side effects of medications 2. Deep breathing techniques to decrease stress 3. How to make eye contact when communicating 4. How to be a leader ANS: 3 Rationale: The nurse should plan to teach the client how to make eye contact when communicating. Social skills, such as making eye contact, can assist clients to communicate needs and to establish relationships. Cognitive Level: Application Integrated Process: Implementation 3. A 16-year-old client diagnosed with schizophrenia spectrum disorder experiences command hallucinations to harm others. The clients parents ask a nurse, Where do the voices come from? Which is the appropriate nursing response? 1. Your child has a chemical imbalance of the brain, which leads to altered perceptions. 2. Your childs hallucinations are caused by medication interactions. 3. Your child has too little serotonin in the brain, causing delusions and hallucinations. 4. Your childs abnormal hormonal changes have precipitated auditory hallucinations. ANS: 1 Rationale: The nurse should explain that a chemical imbalance of the brain leads to altered perceptions. Hallucinations, or false sensory perceptions, may occur in all five senses. The client hearing voices is experiencing an auditory hallucination. Cognitive Level: Application Integrated Process: Implementation 4. Parents ask a nurse how they should reply when their child, diagnosed with schizophrenia spectrum disorder, tells them that voices command him to harm others. Which is the appropriate nursing response? 1. Tell him to stop discussing the voices. 2. Ignore what he is saying, while attempting to discover the underlying cause. 3. Focus on the feelings generated by the hallucinations and present reality. 4. Present objective evidence that the voices are not real. ANS: 3 Rationale: The most appropriate response by the nurse is to instruct the parents to focus on the feelings generated by the hallucinations and present reality. The parents should accept that their child is experiencing the hallucination but should not reinforce this unreal sensory perception. Cognitive Level: Application Integrated Process: Implementation 5. A nurse is assessing a client diagnosed with schizophrenia spectrum disorder. The nurse asks the client, Do you receive special messages from certain sources, such as the television or radio? The nurse is assessing which potential symptom of this disorder? 1. Thought insertion 2. Paranoid delusions 3. Magical thinking 4. Delusions of reference ANS: 4 Rationale: The nurse is assessing for the potential symptom of delusions of reference. A client that believes he or she receives messages through the radio is experiencing delusions of reference. These delusions involve the client interpreting events within the environment as being directed toward him- or herself. Cognitive Level: Application Integrated Process: Assessment 6. A client diagnosed with schizophrenia spectrum disorder states, Cant you hear him? Its the devil. Hes telling me Im going to hell. Which is the most appropriate nursing response? 1. Did you take your medicine this morning? 2. You are not going to hell. You are a good person. 3. The voices must sound scary, but the devil is not talking to you. This is part of your illness. 4. The devil only talks to people who are receptive to his influence. ANS: 3 Rationale: The most appropriate nursing response is to reassure the client while not reinforcing the hallucination. Reminding the client that the voices are a part of the illness is a way to help the client accept that the hallucinations are not real. It is also important for the nurse to connect with the clients fears and inner feelings. Cognitive Level: Application Integrated Process: Implementation 7. A client diagnosed with schizophrenia spectrum disorder tells a nurse about voices commanding him to kill the president. Which is the priority nursing diagnosis for this client? 1. Disturbed sensory perception 2. Altered thought processes 3. Risk for violence: directed toward others 4. Risk for injury ANS: 3 Rationale: The nurse should prioritize the diagnosis risk for violence: directed toward others. A client who hears voices commanding him to kill someone is at risk for other-directed violence. Other risk factors for violence include aggressive body language, verbal aggression, catatonic excitement, and rage reactions. Cognitive Level: Analysis Integrated Process: Diagnosis 8. Which nursing intervention would be most appropriate when caring for an acutely agitated paranoid client diagnosed with schizophrenia spectrum disorder? 1. Provide neon lights and soft music. 2. Maintain continual eye contact throughout the interview. 3. Use therapeutic touch to increase trust and rapport. 4. Provide personal space to respect the clients boundaries. ANS: 4 Rationale: The most appropriate nursing intervention is to provide personal space to respect the clients boundaries. Providing personal space may serve to reduce anxiety and thus reduce the clients risk for violence. Cognitive Level: Application Integrated Process: Implementation 9. Which nursing behavior will enhance the establishment of a trusting relationship with a client diagnosed with schizophrenia spectrum disorder? 1. Establishing personal contact with family members 2. Being reliable, honest, and consistent during interactions 3. Sharing limited personal information 4. Sitting close to the client to establish rapport ANS: 2 Rationale: The nurse can enhance the establishment of a trusting relationship with a client diagnosed with schizophrenia spectrum disorder by being reliable, honest, and consistent during interactions. The nurse should also convey acceptance of the clients needs and maintain a calm attitude when dealing with agitated behavior. Cognitive Level: Application Integrated Process: Implementation 10. A paranoid client diagnosed with schizophrenia spectrum disorder states, My psychiatrist is out to get me. Im sad that the voice is telling me to stop him. What symptom is the client exhibiting, and what is the nurses legal responsibility related to this symptom? 1. Magical thinking; administer an antipsychotic medication. 2. Persecutory delusions; orient the client to reality. 3. Command hallucinations; warn the psychiatrist. 4. Altered thought processes; call an emergency treatment team meeting. ANS: 3 Rationale: The nurse should determine that the client is exhibiting command hallucinations. The nurses legal responsibility is to warn the psychiatrist of the potential for harm. Clients demonstrating a risk for violence could potentially be physically, emotionally, and/or sexually harmful to others or to self. Cognitive Level: Application Integrated Process: Assessment 11. A client is diagnosed with schizophrenia spectrum disorder. A physician orders haloperidol (Haldol) 50 mg bid, benztropine (Cogentin) 1 mg prn, and zolpidem (Ambien) 10 mg HS. Which client behavior would warrant the nurse to administer benztropine? 1. Tactile hallucinations 2. Tardive dyskinesia 3. Restlessness and muscle rigidity 4. Reports of hearing disturbing voices ANS: 3 Rationale: The symptom of tactile hallucinations and reports of hearing disturbing voices would be addressed by an antipsychotic medication such as haloperidol. Tardive dyskinesia, a potentially irreversible condition, would warrant the discontinuation of an antipsychotic medication such as haloperidol. An anticholinergic medication such as benztropine would be used to treat the extrapyramidal symptoms of restlessness and muscle rigidity. Cognitive Level: Application Integrated Process: Implementation 12. A nurse is caring for a client who is experiencing a flat affect, paranoid delusions, anhedonia, anergia, neologisms, and echolalia. Which statement correctly differentiates the clients positive and negative symptoms of schizophrenia? 1. Paranoid delusions, anhedonia, and anergia are positive symptoms of schizophrenia. 2. Paranoid delusions, neologisms, and echolalia are positive symptoms of schizophrenia. 3. Paranoid delusions, anergia, and echolalia are negative symptoms of schizophrenia. 4. Paranoid delusions, flat affect, and anhedonia are negative symptoms of schizophrenia. ANS: 2 Rationale: The nurse should recognize that positive symptoms of schizophrenia include, but are not limited to, paranoid delusions, neologisms, and echolalia. The negative symptoms of schizophrenia include, but are not limited to, flat affect, anhedonia, and anergia. Positive symptoms reflect an excess or distortion of normal functions. Negative symptoms reflect a diminution or loss of normal functions. Cognitive Level: Application Integrated Process: Evaluation 13. A 60-year-old client diagnosed with schizophrenia spectrum disorder presents in an ED with uncontrollable tongue movements, stiff neck, and difficulty swallowing. Which medical diagnosis and treatment should a nurse anticipate when planning care for this client? 1. Neuroleptic malignant syndrome treated by discontinuing antipsychotic medications 2. Agranulocytosis treated by administration of clozapine (Clozaril) 3. Extrapyramidal symptoms treated by administration of benztropine (Cogentin) 4. Tardive dyskinesia treated by discontinuing antipsychotic medications ANS: 4 Rationale: The nurse should expect that an ED physician would diagnose the client with tardive dyskinesia and discontinue antipsychotic medication. Tardive dyskinesia is a condition of abnormal involuntary movements of the mouth, tongue, trunk, and extremities that can be a side effect of typical antipsychotic medications. Cognitive Level: Application Integrated Process: Planning 14. After taking chlorpromazine (Thorazine) for 1 month, a client presents to an ED with severe muscle rigidity, tachycardia, and a temperature of 105oF (40.5C). Which medical diagnosis and treatment should a nurse anticipate when planning care for this client? 1. Neuroleptic malignant syndrome treated by discontinuing Thorazine and administering dantrolene (Dantrium) 2. Neuroleptic malignant syndrome treated by increasing Thorazine dosage and administering an antianxiety medication 3. Dystonia treated by administering trihexyphenidyl (Artane) 4. Dystonia treated by administering bromocriptine (Parlodel) ANS: 1 Rationale: The nurse should expect that an ED physician would diagnose the client with neuroleptic malignant syndrome and treat the client by discontinuing chlorpromazine and administering dantrolene. Neuroleptic malignant syndrome is a potentially fatal condition characterized by rigidity, fever, altered consciousness, and autonomic instability. The use of typical antipsychotics is largely being replaced by atypical antipsychotics because they have fewer side effects and present a lower risk. Cognitive Level: Application Integrated Process: Planning 15. A client diagnosed with schizophrenia spectrum disorder takes an antipsychotic agent daily. Which assessment finding should a nurse prioritize? 1. Respirations of 22 beats/minute 2. Weight gain of 8 pounds in 2 months 3. Temperature of 104F (40C) 4. Excessive salivation ANS: 3 Rationale: When assessing a client diagnosed with schizophrenia spectrum disorder who takes an antipsychotic agent daily, the nurse should immediately address a temperature of 104F (40C). A temperature this high may indicate neuroleptic malignant syndrome, a life-threatening side effect of antipsychotic medications. Cognitive Level: Analysis Integrated Process: Assessment 16. An aging client diagnosed with schizophrenia spectrum disorder takes an antipsychotic and a beta-adrenergic blocking agent for hypertension. Understanding the combined side effects of these drugs, which statement by a nurse is most appropriate? 1. Make sure you concentrate on taking slow, deep, cleansing breaths. 2. Watch your diet and try to engage in some regular physical activity. 3. Rise slowly when you change position from lying to sitting or sitting to standing. 4. Wear sunscreen and try to avoid midday sun exposure. ANS: 3 Rationale: The most appropriate statement by the nurse is to instruct the client to rise slowly when changing positions. Antipsychotic medications and beta blockers cause a decrease in blood pressure. When given in combination, the additive effect of these drugs places the client at risk for developing orthostatic hypotension. Cognitive Level: Application Integrated Process: Implementation 17. A client diagnosed with schizophrenia spectrum disorder is prescribed clozapine (Clozaril). Which client symptoms, related to the side effects of this medication, should prompt a nurse to intervene immediately? 1. Sore throat, fever, and malaise 2. Akathisia and hypersalivation 3. Akinesia and insomnia 4. Dry mouth and urinary retention ANS: 1 Rationale: The nurse should intervene immediately if the client experiences signs of an infectious process, such as a sore throat, fever, and malaise, when taking the atypical antipsychotic drug clozapine. Clozapine can have a serious side effect of agranulocytosis, in which a potentially fatal drop in white blood cells can occur, leading to infection. Cognitive Level: Application Integrated Process: Evaluation 18. During an admission assessment, a nurse assesses that a client diagnosed with schizophrenia spectrum disorder has allergies to penicillin, prochlorperazine (Compazine), and bee stings. Based on this assessment data, which antipsychotic medication would be contraindicated? 1. Haloperidol (Haldol), because it is used only in older patients 2. Clozapine (Clozaril), because it is incompatible with desipramine 3. Risperidone (Risperdal), because it exacerbates symptoms of depression 4. Thioridazine (Mellaril), because of cross-sensitivity among phenothiazines ANS: 4 Rationale: The nurse should know that thioridazine would be contraindicated because of cross- sensitivity among phenothiazines. Prochlorperazine and thioridazine are both classified as phenothiazines. Cognitive Level: Application Integrated Process: Assessment 19. A client has been assigned an admission diagnosis of brief psychotic disorder. Which assessment information would alert the nurse to question this diagnosis? 1. The client has experienced impaired reality testing for a 24-hour period. 2. The client has experienced auditory hallucinations for the past 3 hours. 3. The client has experienced bizarre behavior for 1 day. 4. The client has experienced confusion for 3 weeks. ANS: 2 Rationale: This disorder is identified by the sudden onset of psychotic symptoms that may or may not be preceded by a severe psychosocial stressor. These symptoms last at least 1 day but less than 1 month. Cognitive Level: Application Integrated Process: Assessment 20. A nurse is assessing a client diagnosed with substance induced psychotic disorder (SIPD). What would differentiate this clients symptoms from the symptoms of a client diagnosed with brief psychotic disorder (BPD)? 1. Clients diagnosed with SIPD experience delusions, whereas clients diagnosed with BPD do not. 2. Clients diagnosed with BPD experience hallucinations, whereas clients diagnosed with SIPD do not. 3. Catatonic features may be associated with SIPD, whereas BPD has no catatonic features. 4. Catatonic features may be associated with BPD, whereas SIPD has no catatonic features. ANS: 3 Rationale: The diagnosis of SIPD is made when symptoms are directly attributable to substance intoxication or withdrawal. The symptoms are more excessive and more severe than those usually associated with the intoxication or withdrawal syndrome. Hallucinations and delusions are associated with both SIPD and BPD. Catatonic features may be associated with SIPD, whereas BPD has no catatonic features. Cognitive Level: Analysis Integrated Process: Assessment 21. A nurse prepares to assess a client using the Abnormal Involuntary Movement Scale (AIMS). Which side effect of antipsychotic medications led to the use of this assessment tool? 1. Dystonia 2. Tardive dyskinesia 3. Akinesia 4. Akathisia ANS: 2 Rationale: The AIMS is a rating scale that was developed in the 1970s by the National Institute of Mental Health to measure involuntary movements associated with tardive dyskinesia. Cognitive Level: Application Integrated Process: Assessment Multiple Response 22. Which of the following components should a nurse recognize as an integral part of a rehabilitative program when planning care for clients diagnosed with schizophrenia spectrum disorder? (Select all that apply.) 1. Group therapy 2. Medication management 3. Deterrent therapy 4. Supportive family therapy 5. Social skills training ANS: 1, 2, 4, 5 Rationale: The nurse should recognize that group therapy, medication management, supportive family therapy, and social skills training all play an integral part of rehabilitative programs for clients diagnosed with schizophrenia spectrum disorder. Schizophrenia results from various combinations of genetic predispositions, biochemical dysfunctions, physiological factors, and psychological stress. Effective treatment requires a comprehensive, multidisciplinary effort. Cognitive Level: Application Integrated Process: Planning 23. A nurse is administering risperidone (Risperdal) to a client diagnosed with schizophrenia spectrum disorder. Which of the following client symptoms would most likely decrease because of the therapeutic effect of this medication? (Select all that apply.) 1. Somatic delusions 2. Social isolation 3. Gustatory hallucinations 4. Flat affect 5. Clang associations ANS: 1, 3, 5 Rationale: The nurse should expect that risperidone would be effective treatment for the positive symptoms of somatic delusions, gustatory hallucinations, and clang associations. Risperidone is an atypical antipsychotic that has been effective in the treatment of the positive symptoms of schizophrenia and in maintenance therapy to prevent exacerbation of schizophrenic symptoms. Cognitive Level: Application Integrated Process: Assessment 24. Laboratory results reveal decreased levels of prolactin in a client diagnosed with schizophrenia spectrum disorder. Which of the following client symptoms would a nurse expect to observe during assessment? (Select all that apply.) 1. Apathy2. Social withdrawal3. Anhedonia4. Auditory hallucinations 5. Delusions ANS: 1, 2, 3 Rationale: The nurse should expect that a client with decreased levels of prolactin may experience apathy, social withdrawal, and anhedonia. Decreased levels of prolactin can cause depression, which could result in these symptoms. Cognitive Level: Application Integrated Process: Evaluation 25. The diagnosis of catatonic disorder associated with another medical condition is made when the clients medical history, physical examination, or laboratory findings provide evidence that symptoms are directly attributed to which of the following? (Select all that apply.) 1. Hyperthyroidism2. Hypothyroidism 3. Hyperadrenalism 4. Hypoadrenalism 5. Hyperaphia ANS: 1, 2, 3, 4 Rationale: The diagnosis of catatonic disorder associated with another medical condition is made when the symptomatology is evidenced from medical history, physical examination, or laboratory findings to be directly attributable to the physiological consequences of a general medical condition. Types of medical conditions that have been associated with catatonic disorder include metabolic disorders (e.g., hepatic encephalopathy, hypo- and hyperthyroidism, hypo- and hyperadrenalism, and vitamin B12 deficiency) and neurological conditions (e.g., epilepsy, tumors, cerebrovascular disease, head trauma, and encephalitis). Hyperaphia is an excessive sensitivity to touch. Cognitive Level: Application Integrated Process: Evaluation Ordered Response 26. Order the spectrum of schizophrenic and other psychotic disorders as described by the DSM- 5 on a gradient of psychopathology from least to most severe. Delusional disorder Schizotypal personality disorder Schizophrenia Brief psychotic disorder Psychotic disorder associated with another medical condition Catatonic disorder associated with another medical condition Schizoaffective disorder Schizophreniform disorder Substance-induced psychotic disorder ANS: The correct order is 2, 1, 9, 3, 5, 6, 8, 7, 4 Rationale: A spectrum of schizophrenic and other psychotic disorders has been identified in the DSM-5. These include (on a gradient of psychopathology from least to most severe): schizotypal personality disorder, delusional disorder, brief psychotic disorder, substance-induced psychotic disorder, psychotic disorder associated with another medical condition, catatonic disorder associated with another medical condition, schizophreniform disorder, schizoaffective disorder, and schizophrenia. 1. Schizotypal personality disorder 2. Delusional disorder 3. Brief psychotic disorder 4. Substance-induced psychotic disorder 5. Psychotic disorder associated with another medical condition 6. Catatonic disorder associated with another medical condition 7. Schizophreniform disorder 8. Schizoaffective disorder 9. Schizophrenia Cognitive Level: Analysis Integrated Process: Assessment Fill-in-the-Blank 27. disorder is manifested by schizophrenic behaviors, with a strong element of symptomatology associated with the mood disorders (depression or mania). ANS: Schizoaffective Rationale: Schizoaffective disorder is manifested by schizophrenic behaviors, with a strong element of symptomatology associated with the mood disorders (depression or mania). The decisive factor in the diagnosis of schizoaffective disorder is the presence of hallucinations and/or delusions that occur for at least 2 weeks in the absence of a major mood episode. Cognitive Level: Application Integrated Process: Assessment 28. are false sensory perceptions not associated with real external stimuli and may involve any of the five senses. ANS: Hallucinations Rationale: Hallucinations are false sensory perceptions not associated with real external stimuli and may involve any of the five senses. Types of hallucinations include auditory, visual, tactile, gustatory, and olfactory. Chapter 16. Depressive Disorders Multiple Choice 1. A nurse discovers a clients suicide note that details the time, place, and means to commit suicide. What should be the priority nursing action, and why? 1. Administer lorazepam (Ativan) prn, because the client is angry about plan exposure. 2. Establish room restrictions, because the clients threat is an attempt to manipulate the staff. 3. Place client on one-to-one suicide precautions, because specific plans likely lead to attempts. 4. Call an emergency treatment team meeting, because the clients threat must be addressed. ANS: 3 Rationale: The priority nursing action should be to place this client on one-to-one suicide precautions, because the more specific the plan, the more likely the client will attempt suicide. Cognitive Level: Analysis Integrated Process: Implementation 2. In planning care for a suicidal client, which correctly written outcome should be a nurses first priority? 1. The client will not physically harm self. 2. The client will express hope for the future by day three. 3. The client will establish a trusting relationship with the nurse. 4. The client will remain safe during hospital stay. ANS: 4 Rationale: The nurses first priority should be that the client will remain safe during the hospital stay. Client safety should always be the nurses first priority. Outcomes should be client-centered, specific, realistic, measureable, and must also include a time frame. Cognitive Level: Analysis Integrated Process: Planning 3. A nurse administers 100% oxygen to a client during and after electroconvulsive therapy treatment (ECT). What is the rationale for this procedure? 1. To prevent increased intracranial pressure resulting from anoxia. 2. To prevent decreased blood pressure, pulse, and respiration owing to electrical stimulation. 3. To prevent anoxia resulting from medication-induced paralysis of respiratory muscles. 4. To prevent blocked airway, resulting from seizure activity. ANS: 3 Rationale: The nurse administers 100% oxygen during and after ECT to prevent anoxia resulting from medication-induced paralysis of respiratory muscles. Cognitive Level: Application Integrated Process: Implementation 4. Immediately after electroconvulsive therapy (ECT), in which position should a nurse place the client? 1. On his or her side, to prevent aspiration 2. In high Fowlers position, to prevent increased intracranial pressure 3. In Trendelenburgs position, to promote blood flow to vital organs 4. In prone position, to prevent airway blockage ANS: 1 Rationale: The nurse should place a client who has received ECT on his or her side, to prevent aspiration. Cognitive Level: Application Integrated Process: Implementation 5. A client is diagnosed with major depressive episode. Which nursing diagnosis should a nurse assign to this client, to address a behavioral symptom of this disorder? 1. Altered communication R/T feelings of worthlessness AEB anhedonia 2. Social isolation R/T poor self-esteem AEB secluding self in room 3. Altered thought processes R/T hopelessness AEB persecutory delusions 4. Altered nutrition: less than body requirements R/T high anxiety AEB anorexia ANS: 2 Rationale: A nursing diagnosis of social isolation R/T poor self-esteem AEB secluding self in room addresses a behavioral symptom of major depressive episode. Other behavioral symptoms include psychomotor retardation, virtually nonexistent communication, curled-up position, and no attention to personal hygiene and grooming. Cognitive Level: Analysis Integrated Process: Diagnosis 6. A client diagnosed with major depressive episode hears voices commanding self-harm. Which should be the nurses priority intervention at this time? 1. Obtaining an order for locked seclusion until client is no longer suicidal. 2. Conducting 15-minute checks to ensure safety. 3. Placing the client on one-to-one observation while continuing to monitor suicidal ideations. 4. Encouraging client to express feelings related to suicide. ANS: 3 Rationale: The nurses priority intervention when a depressed client hears voices commanding self-harm is to place the client on one-to-one observation while continuing to monitor suicidal ideations. By providing one-to-one observation, the nurse will be able to interrupt any attempts at suicide. Cognitive Level: Analysis Integrated Process: Implementation 7. A nurse assesses a client suspected of having the diagnosis of major depressive episode. Which client symptom would rule out this diagnosis? 1. The client is disheveled and malodorous. 2. The client refuses to interact with others and isolates self in room. 3. The client is unable to feel any pleasure. 4. The client has maxed-out charge cards and exhibits promiscuous behaviors. ANS: 4 Rationale: The nurse should assess that a client who has maxed-out credit cards and exhibits promiscuous behavior is exhibiting signs of mania. The DSM-5 criteria state that there must never have been a manic episode or a hypomanic episode to meet the criteria for the diagnosis of major depressive episode. Cognitive Level: Application Integrated Process: Assessment 8. A client with a history of suicide attempts has been taking fluoxetine (Prozac) for one month. The client suddenly presents with a bright affect, rates mood at 9 out of 10, and is much more communicative. Which action should be the nurses priority at this time? 1. Give the client off-unit privileges as positive reinforcement. 2. Encourage the client to share mood improvement in group. 3. Increase the level of this clients suicide precautions. 4. Request that the psychiatrist reevaluate the current medication protocol. ANS: 3 Rationale: The nurse should be aware that a sudden increase in mood rating and change in affect could indicate that the client is at risk for suicide. Suicide risk may occur early during treatment with antidepressants. The return of energy may bring about an increased ability to act out self- destructive behavior. Cognitive Level: Analysis Integrated Process: Implementation 9. A nurse reviews the laboratory data of a client suspected of having the diagnosis of major depressive episode. Which lab value would potentially rule out this diagnosis? 1. Thyroid-stimulating hormone (TSH) level of 25 U/mL 2. Potassium (K+) level of 4.2 mEq/L 3. Sodium (Na+) level of 140 mEq/L 4. Calcium (Ca2+) level of 9.5 mg/dL ANS: 1 Rationale: A diagnosis of major depressive episode may be ruled out if the clients lab results reveal a TSH level of 25 U/mL. Normal levels of TSH range from 2 to 10 U/mL. High levels of TSH indicate low thyroid function. The clients high TSH value may indicate hypothyroidism, which can lead to depressive symptoms. The DSM-5 criteria for the diagnosis of major depressive episode states that this diagnosis must not be attributable to the direct physiological effects of another medical condition. Cognitive Level: Analysis Integrated Process: Evaluation 10. A depressed client reports to a nurse a history of divorce, job loss, family estrangement, and cocaine abuse. Which theoretical principle best explains the etiology of this clients depressive symptoms? 1. According to psychoanalytic theory, depression is a result of negative perceptions. 2. According to object-loss theory, depression is a result of overprotection. 3. According to learning theory, depression is a result of repeated failures. 4. According to cognitive theory, depression is a result of anger turned inward. ANS: 3 Rationale: The nurse should assess that, according to learning theory, this clients depressive symptoms may have resulted from repeated failures. The learning theory is a model of learned helplessness in which multiple life failures cause the client to abandon future attempts to succeed. Cognitive Level: Application Integrated Process: Assessment 11. What is the rationale for a nurse to perform a full physical health assessment on a client admitted with a diagnosis of major depressive episode? 1. The attention during the assessment is beneficial in decreasing social isolation. 2. Depression can generate somatic symptoms that can mask actual physical disorders. 3. Physical health complications are likely to arise from antidepressant therapy. 4. Depressed clients avoid addressing physical health and ignore medical problems. ANS: 2 Rationale: The nurse should determine that a client with a diagnosis of major depressive episode needs a full physical health assessment, because depression can generate somatic symptoms that can mask actual physical disorders. Cognitive Level: Application Integrated Process: Implementation 12. A nurse is planning care for a 13 -year-old who is experiencing depression. Which medication is approved by the Food and Drug Administration (FDA) for the treatment of depression in adolescents? 1. Paroxetine (Paxil) 2. Sertraline (Zoloft) 3. Citalopram (Celexa) 4. Escitalopram (Lexipro) ANS: 4 Rationale: Fluoxetine (Prozac) has been approved by the FDA to treat depression in children and adolescents, and escitalopram was approved in 2009 for treatment of depression in adolescents aged 12 to 17 years. All antidepressants carry an FDA warning for increased risk of suicide in children and adolescents. Cognitive Level: Application Integrated Process: Planning 13. A nurse admits an older client with memory loss, confused thinking, and apathy. A psychiatrist suspects a depressive disorder. What is the rationale for performing a mini-mental status exam? 1. To rule out bipolar disorder 2. To rule out schizophrenia 3. To rule out neurocognitive disorder 4. To rule out personality disorder ANS: 3 Rationale: A mini-mental status exam should be performed to rule out neurocognitive disorder. The client may be experiencing reversible dementia, which can occur as a result of depression. Cognitive Level: Application Integrated Process: Evaluation 14. A nurse recently admitted a client to an inpatient unit after a suicide attempt. A health-care provider orders amitriptyline (Elavil) for the client. Which intervention, related to this medication, should be initiated to maintain this clients safety upon discharge? 1. Provide a 6-month supply of Elavil to ensure long-term compliance. 2. Provide a 1-week supply of Elavil, with refills contingent on follow-up appointments. 3. Provide pill dispenser as a memory aid. 4. Provide education regarding the avoidance of foods containing tyramine. ANS: 2 Rationale: The health-care provider should provide no more than a 1-week supply of amitriptyline, with refills contingent on follow-up appointments, as an appropriate intervention to maintain the clients safety. Antidepressants, which are central nervous system depressants, can be used to commit suicide. Also these medications can precipitate suicidal thoughts during the initial use period. Limiting the amount of medication and monitoring the client weekly would be appropriate interventions to address the clients risk for suicide. Cognitive Level: Application Integrated Process: Implementation 15. An older client has recently been prescribed sertraline (Zoloft). The clients spouse is taking paroxetine (Paxil). A nurse assesses that the client is experiencing restlessness, tachycardia, diaphoresis, and tremors. Which complication should a nurse suspect, and why? 1. Neuroleptic malignant syndrome; caused by ingestion of two different seratonin reuptake inhibitors (SSRIs) 2. Neuroleptic malignant syndrome; caused by ingestion of an SSRI and a monoamine oxidase inhibitor (MAOI) 3. Serotonin syndrome; possibly caused by ingestion of an SSRI and an MAOI 4. Serotonin syndrome; possibly caused by ingestion of two different SSRIs ANS: 4 Rationale: The nurse should suspect that the client is suffering from serotonin syndrome; possibly caused by ingesting two different SSRIs (sertraline and paroxetine). Symptoms of serotonin syndrome include confusion, agitation, tachycardia, hypertension, nausea, abdominal pain, myoclonus, muscle rigidity, fever, sweating, and tremor. Cognitive Level: Application Integrated Process: Assessment 16. A client who has been taking fluvoxamine (Luvox) without significant improvement asks a nurse, I heard about something called a monoamine oxidase inhibitor (MAOI). Cant my doctor add that to my medications? Which is an appropriate nursing response? 1. This combination of drugs can lead to delirium tremens. 2. A combination of an MAOI and Luvox can lead to a life-threatening hypertensive crisis. 3. Thats a good idea. There have been good results with the combination of these two drugs. 4. The only disadvantage would be the exorbitant cost of the MAOI. ANS: 2 Rationale: The nurse should explain to the client that combining an MAOI and fluvoxamine, an SSRI, can lead to a life-threatening hypertensive crisis. Symptoms of hypertensive crisis include severe occipital and/or temporal pounding headaches, with occasional photophobia, sensations of choking, palpitations, and a feeling of dread. Cognitive Level: Application Integrated Process: Implementation 17. A number of assessment rating scales are available for measuring severity of depressive symptoms. Which scale would a nurse practitioner use to assess a depressed client? 1. Zung Depression Scale 2. Hamilton Depression Rating Scale 3. Beck Depression Inventory 4. AIMS Depression Rating Scale ANS: 2 Rationale: A number of assessment rating scales are available for measuring severity of depressive symptoms. Some are meant to be clinician administered, whereas others may be self- administered. Examples of self-rating scales include the Zung Self-Rating Depression Scale and the Beck Depression Inventory. One of the most widely used clinician-administered scales is the Hamilton Depression Rating Scale. The Abnormal Involuntary Movement Scale (AIMS) is a rating scale that measures involuntary movements associated with tardive dyskinesia. Cognitive Level: Application Integrated Process: Assessment 18. The severity of depressive symptoms in the postpartum period varies from a feeling of the blues, to moderate depression, to psychotic depression or melancholia. Which disorder is correctly matched with its presenting symptoms? 1. Maternity blues (lack of concentration, agitation, guilt, and an abnormal attitude toward bodily functions) 2. Postpartum depression (irritability, loss of libido, sleep disturbances, expresses concern about inability to care for baby) 3. Postpartum melancholia (overprotection of infant, expresses concern about inability to care for baby, mysophobia) 4. Postpartum depressive psychosis (transient depressed mood, agitation, abnormal fear of child abduction, suicidal ideations) ANS: 2 Rationale: The symptoms of the maternity blues include tearfulness, despondency, anxiety, and subjectively impaired concentration appearing in the early puerperium. Symptoms of postpartum depression are associated with fatigue, irritability, loss of appetite, sleep disturbances, loss of libido, and expressions of great concern about her inability to care for her baby. Both postpartum melancholia and postpartum depressive psychosis are characterized by a lack of interest in, or rejection of, the baby, or a morbid fear that the baby may be harmed. Other symptoms include depressed mood, agitation, indecision, lack of concentration, guilt, and an abnormal attitude toward bodily functions. Cognitive Level: Application Integrated Process: Assessment 19. A staff nurse is counseling a depressed client. The nurse determines that the client is using the cognitive distortion of automatic thoughts. Which client statement is evidence of the automatic thought of discounting positives? 1. Its all my fault for trusting him. 2. I dont play games. I never win. 3. She never visits because she thinks I dont care. 4. I dont have a green thumb. Any old fool can grow a rose. ANS: 4 Rationale: Examples of automatic thoughts in depression include: Personalizing: Im the only one who failed. All or nothing: Im a complete failure. Mind reading: He thinks Im foolish. Discounting positives: The other questions were so easy. Any dummy could have gotten them right. Cognitive Level: Application Integrated Process: Assessment 20. A client, who is taking transdermal selegiline (Emsam) for depressive symptoms, states, My physician told me there was no need to worry about dietary restrictions. Which would be the most appropriate nursing response? 1. Because your dose of Emsam is 6 mg in 24 hours, dietary restrictions are not recommended. 2. You must have misunderstood. An MAOI like Emsam always has dietary restrictions. 3. Only oral MAOIs require dietary restrictions. 4. All transdermal MAOIs do not require dietary modifications. ANS: 1 Rationale: Selegiline is a Monoamine Oxidase Inhibitor (MAOI). Hypertensive crisis, caused by the ingestion of foods high in tyramine, has not shown to be a problem with selegiline transdermal system at the 6 mg/24 hr dosage, and dietary restrictions at this dose are not recommended. Dietary modifications are recommended, however, at the 9 mg/24 hr and 12 mg/24 hr dosages. Cognitive Level: Application Integrated Process: Implementation 21. After 6 months of taking imipramine (Tofranil) for depressive symptoms, a client complains that the medication doesnt seem as effective as before. Which question should the nurse ask to determine the cause of this problem? 1. Are you consuming foods high in tyramine? 2. How many packs of cigarettes do you smoke daily? 3. Do you drink any alcohol? 4. Are you taking St. Johns wort? ANS: 2 Rationale: Imipramine is a tricyclic antidepressant. Smoking should be avoided while receiving tricyclic therapy. Smoking increases the metabolism of tricyclics, requiring an adjustment in dosage to achieve the therapeutic effect. Alcohol potentiates the effects of antidepressants. Tyramine is only an issue when MAOI medications are prescribed. Concomitant use of St. Johns wort and SSRIs, not tricyclics, increases, not decreases the effects of the drug. Cognitive Level: Application Integrated Process: Implementation Multiple Response 22. A nursing home resident has a diagnosis of dysthymic disorder. When planning care for this client, which of the following symptoms should a nurse expect the client to exhibit? (Select all that apply.) 1. Sad mood on most days 2. Mood rating of 2 out of 10 for the past 6 months 3. Labile mood 4. Sad mood for the past 3 years after spouses death 5. Pressured speech when communicating ANS: 1, 4 Rationale: The nurse should anticipate that a client with a diagnosis of dysthymic disorder would experience a sad mood on most days for more than two years. The essential feature of dysthymia is a chronically depressed mood, which can have an early or late onset. Cognitive Level: Application Integrated Process: Planning 23. An individual experiences sadness and melancholia in September continuing through November. Which of the following factors should a nurse identify as most likely to contribute to the etiology of these symptoms? (Select all that apply.) 1. Gender differences in social opportunities that occur with age 2. Drastic temperature and barometric pressure changes 3. A seasonal increase in social interactions 4. Variations in serotonergic functioning 5. Inaccessibility of resources for dealing with life stressors ANS: 2, 3, 4 Rationale: The nurse should identify drastic temperature and barometric pressure changes, a seasonal increase in social interactions, and/or variations in serotonergic functioning as contributing to the etiology of the clients symptoms. A number of studies have examined seasonal patterns associated with mood disorders and have revealed two prevalent periods of seasonal involvement: spring (March, April, May) and fall (September, October, November). Cognitive Level: Application Integrated Process: Evaluation 24. A client is prescribed phenelzine (Nardil). Which of the following statements by the client should indicate to a nurse that discharge teaching about this medication has been successful? (Select all that apply.) 1. Ill have to let my surgeon know about this medication before I have my cholecystectomy. 2. I guess I will have to give up my glass of red wine with dinner. 3. Ill have to be very careful about reading food and medication labels. 4. Im going to miss my caffeinated coffee in the morning. 5. Ill be sure not to stop this medication abruptly. ANS: 1, 2, 3, 5 Rationale: The nurse should evaluate that teaching has been successful when the client states that phenelzine should not be taken in conjunction with the use of alcohol or foods high in tyramine and should not be stopped abruptly. Phenelzine is an MAOI that can have negative interaction with other medications. The client needs to tell other physicians about taking MAOIs, because of the risk of drug interactions. Cognitive Level: Application Integrated Process: Implementation 25. A nursing instructor is teaching about the new DSM-5 diagnostic category of disruptive mood dysregulation disorder (DMDD). Which of the following information should the instructor include? (Select all that apply.) 1. Symptoms include verbal rages or physical aggression toward people or property. 2. Temper outbursts must be present in at least two settings (at home, at school, or with peers). 3. DMDD is characterized by severe recurrent temper outbursts. 4. The temper outbursts are manifested only behaviorally. 5. Symptoms of DMDD must be present for 18 or more months to meet diagnostic criteria. ANS: 1, 2, 3 Rationale: The APA has included a new diagnostic category in the Depressive Disorders chapter of the DSM-5. This childhood disorder is called disruptive mood dysregulation disorder. Criteria for the diagnosis include, but are not limited to, the following. Verbal rages or physical aggression toward people or property; temper outbursts must be present in at least two settings (at home, at school, or with peers). DMDD is characterized by severe recurrent temper outbursts. The temper outbursts are manifested both behaviorally and/or verbally. Symptoms of DMDD must be present for 12, not 18 or more months to meet diagnostic criteria. Cognitive Level: Application Integrated Process: Implementation Ordered Response 26. Order the depressive disorders and their predominant affective symptoms according to level of severity. Dysthymic disorder (pessimistic outlook, low self-esteem) Grief (feelings of anger, anxiety, guilt, helplessness) Major depressive episode (despair, worthlessness, flat affect, apathy, anhedonia) Transient depression (sadness, dejection, feeling downhearted, having the blues) ANS: The correct order is 3, 2, 4, 1 Rationale: Symptoms of transient depression are not necessarily dysfunctional. Affective symptoms include sadness, dejection, feeling downhearted, having the blues. Symptoms at the mild level of depression are identified by those associated with uncomplicated grieving. Affective symptoms include denial of feelings, anger, anxiety, guilt, helplessness, hopelessness, sadness, despondency. Dysthymic disorder, which is an example of moderate depression, represents a more problematic disturbance. Affective symptoms include feelings of sadness, dejection, helplessness, powerlessness, hopelessness; gloomy and pessimistic outlook; low self- esteem; difficulty experiencing pleasure in activities. Severe depression is characterized by an intensification of the symptoms described for moderate depression. Examples of severe depression include major depressive episode. Affective symptoms include feelings of total despair, hopelessness, and worthlessness; flat (unchanging) affect, appearing devoid of emotional tone; prevalent feelings of nothingness and emptiness; apathy; loneliness; sadness; inability to feel pleasure. 1. Transient depression (sadness, dejection, feeling downhearted, having the blues) 2. Grief (feelings of anger, anxiety, guilt, helplessness) 3. Dysthymic disorder (pessimistic outlook, low self-esteem) 4. Major depressive episode (despair, worthlessness, flat affect, apathy, anhedonia) Cognitive Level: Analysis Integrated Process: Assessment Fill-in-the-Blank 27. is a pervasive and sustained emotion that may have a major influence on a persons perception of the world. ANS: Mood Rationale: Mood is a pervasive and sustained emotion that may have a major influence on a persons perception of the world. Examples of mood include depression, joy, elation, anger, and anxiety. Affect is described as the emotional reaction associated with an experience. Chapter 17. Bipolar and Related Disorders Multiple Choice 1. A highly agitated client paces the unit and states, I could buy and sell this place. The clients mood fluctuates from fits of laughter to outbursts of anger. Which is the most accurate documentation of this clients behavior? 1. Rates mood 8/10. Exhibiting looseness of association. Euphoric. 2. Mood euthymic. Exhibiting magical thinking. Restless. 3. Mood labile. Exhibiting delusions of reference. Hyperactive. 4. Agitated and pacing. Exhibiting grandiosity. Mood labile. ANS: 4 Rationale: The nurse should document that this clients behavior is Agitated and pacing. Exhibiting grandiosity. Mood labile. The client is exhibiting mood swings from euphoria to irritability. Grandiosity refers to the attitude that ones abilities are better than everyone elses. Cognitive Level: Application Integrated Process: Evaluation 2. A client diagnosed with bipolar disorder is distraught over insomnia experienced over the last 3 nights and a 12-pound weight loss over the past 2 weeks. Which should be this clients priority nursing diagnosis? 1. Knowledge deficit R/T bipolar disorder AEB concern about symptoms 2. Altered nutrition: less than body requirements R/T hyperactivity AEB weight loss 3. Risk for suicide R/T powerlessness AEB insomnia and anorexia 4. Altered sleep patterns R/T mania AEB insomnia for the past 3 nights ANS: 2 Rationale: The nurse should identify that the priority nursing diagnosis for this client is altered nutrition: less than body requirements R/T hyperactivity AEB weight loss. Because of the clients rapid weight loss, the nurse should prioritize interventions to ensure proper nutrition and physical health. Cognitive Level: Analysis Integrated Process: Diagnosis 3. A nurse is planning care for a client diagnosed with bipolar disorder: manic episode. In which order should the nurse prioritize the client outcomes in the exhibit? Client Outcomes: 1. Maintains nutritional status 2. Interacts appropriately with peers 3. Remains free from injury 4. Sleeps 6 to 8 hours a night 1. 2, 1, 3, 4 2. 4, 1, 2, 3 3. 3, 1, 4, 2 4. 1, 4, 2, 3 ANS: 3 Rationale: The nurse should order client outcomes based on priority in the following order: Remains free of injury, maintains nutritional status, sleeps 6 to 8 hours a night, and interacts appropriately with peers. The nurse should prioritize the clients safety and physical health as most important. Cognitive Level: Analysis Integrated Process: Planning 4. A client diagnosed with bipolar disorder: depressive episode intentionally overdoses on sertraline (Zoloft). Family members report that the client has experienced anorexia, insomnia, and recent job loss. Which nursing diagnosis should a nurse prioritize? 1. Risk for suicide R/T hopelessness 2. Anxiety: severe R/T hyperactivity 3. Imbalanced nutrition: less than body requirements R/T refusal to eat 4. Dysfunctional grieving R/T loss of employment ANS: 1 Rationale: The priority nursing diagnosis for this client should be risk for suicide R/T hopelessness. The nurse should always prioritize client safety. This client is at risk for suicide because of his or her recent suicide attempt. Cognitive Level: Analysis Integrated Process: Diagnosis 5. A client diagnosed with bipolar I disorder: manic episode refuses to take lithium carbonate (Lithobid) because of excessive weight gain. In order to increase adherence, which medication should a nurse anticipate that a physician may prescribe? 1. Sertraline (Zoloft) 2. Valproic acid (Depakote) 3. Trazodone (Desyrel) 4. Paroxetine (Paxil) ANS: 2 Rationale: The nurse should anticipate that the physician may prescribe valproic acid in order to increase this clients medication adherence. Valproic acid is an anticonvulsant medication that can be used to treat bipolar disorder. One of the side effects of this medication is weight loss. Cognitive Level: Application Integrated Process: Planning 6. A client diagnosed with bipolar I disorder is exhibiting severe manic behaviors. A physician prescribes lithium carbonate (Eskalith) and olanzapine (Zyprexa). The clients spouse questions the Zyprexa order. Which is the appropriate nursing response? 1. Zyprexa in combination with Eskalith cures manic symptoms. 2. Zyprexa prevents extrapyramidal side effects. 3. Zyprexa increases the effectiveness of the immune system. 4. Zyprexa calms hyperactivity until the Eskalith takes effect. ANS: 4 Rationale: The nurse should explain to the clients spouse that olanzapine can calm hyperactivity until the lithium carbonate takes effect. Lithium carbonate may take 1 to 3 weeks to begin to decrease hyperactivity. Monotherapy with the traditional mood stabilizers like lithium carbonate, or atypical antipsychotics like olanzapine, has been determined to be the first-line treatment for bipolar I disorder. Cognitive Level: Application Integrated Process: Implementation 7. A client began taking lithium carbonate (Lithobid) for the treatment of bipolar disorder approximately 1 month ago. The client asks if it is normal to have gained 12 pounds in this time frame. Which is the appropriate nursing response? 1. Thats strange. Weight loss is the typical pattern. 2. What have you been eating? Weight gain is not usually associated with lithium. 3. Weight gain is a common, but troubling, side effect. 4. Weight gain only occurs during the first month of treatment with this drug. ANS: 3 Rationale: The nurse should explain to the client that weight gain is a common side effect of lithium carbonate. The nurse should educate the client on the importance of medication adherence and discuss concerns with the prescribing physician if the client does not wish to continue taking the medication. Cognitive Level: Application Integrated Process: Implementation 8. A client diagnosed with bipolar disorder has been taking lithium carbonate (Lithobid) for one year. The client presents in an emergency department with a temperature of 101F (38C), severe diarrhea, blurred vision, and tinnitus. How should the nurse interpret these symptoms? 1. Symptoms indicate consumption of foods high in tyramine. 2. Symptoms indicate lithium carbonate discontinuation syndrome. 3. Symptoms indicate the development of lithium carbonate tolerance. 4. Symptoms indicate lithium carbonate toxicity. ANS: 4 Rationale: The nurse should interpret that the clients symptoms indicate lithium carbonate toxicity. The initial signs of toxicity include ataxia, blurred vision, severe diarrhea, nausea and vomiting, and tinnitus. Lithium levels should be monitored monthly with maintenance therapy to ensure proper dosage. Cognitive Level: Application Integrated Process: Evaluation 9. What tool should a nurse use to differentiate occasional spontaneous behaviors of children from behaviors associated with bipolar disorder? 1. Risky Activity tool 2. FIND tool 3. Consensus Committee tool 4. Monotherapy tool ANS: 2 Rationale: The nurse should use the FIND tool to differentiate occasional spontaneous behaviors of children from behaviors associated with bipolar disorder. FIND is an acronym that stands for frequency, intensity, number, and duration and is used to assess behaviors in children. Cognitive Level: Application Integrated Process: Assessment 10. A nursing instructor is discussing various challenges in the treatment of clients diagnosed with bipolar disorder. Which student statement demonstrates an understanding of the most critical challenge in the care of these clients? 1. Treatment is compromised when clients cant sleep. 2. Treatment is compromised when irritability interferes with social interactions. 3. Treatment is compromised when clients have no insight into their problems. 4. Treatment is compromised when clients choose not to take their medications. ANS: 4 Rationale: The nursing student is accurate when stating that the most critical challenge in the care of clients diagnosed with bipolar disorder is that treatment is often compromised when clients choose not to take their medications. Clients diagnosed with bipolar disorder feel most productive and creative during manic episodes. This may lead to purposeful medication nonadherence. Symptoms of bipolar disorder will reemerge if medication is stopped. Cognitive Level: Application Integrated Process: Evaluation 11. A client is diagnosed with bipolar disorder: manic episode. Which nursing intervention would be implemented to achieve the outcome of Client will gain 2 lb by the end of the week? 1. Provide client with high-calorie finger foods throughout the day. 2. Accompany client to cafeteria to encourage adequate dietary consumption. 3. Initiate total parenteral nutrition to meet dietary needs. 4. Teach the importance of a varied diet to meet nutritional needs. ANS: 1 Rationale: The nurse should provide the client with high-calorie finger foods throughout the day to help the client achieve the outcome of gaining 2 lb by the end of the week. Because of the hyperactive state, the client will have difficulty sitting still to consume large meals. Cognitive Level: Application Integrated Process: Implementation 12. A nursing instructor is teaching about bipolar disorders. Which statement differentiates the DSM-5 diagnostic criteria of a manic episode from a hypomanic episode? 1. During a manic episode, clients may experience an inflated self-esteem or grandiosity, and these symptoms are absent in hypomania. 2. During a manic episode, clients may experience a decreased need for sleep, and this symptom is absent in hypomania. 3. During a manic episode, clients may experience psychosis, and this symptom is absent in hypomania. 4. During a manic episode, clients may experience flight of ideas and racing thoughts, and these symptoms are absent in hypomania. ANS: 3 Rationale: Three or more of the following symptoms may be experienced in both hypomanic and manic episodes: Inflated self-esteem or grandiosity, decreased need for sleep (e.g., feels rested after only 3 hours of sleep), more talkative than usual or pressure to keep talking, flight of ideas and racing thoughts, distractibility, increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation, excessive involvement in pleasurable activities that have a high potential for painful consequences (e.g., the person engages in unrestrained buying sprees, sexual indiscretions, or foolish business investments). If there are psychotic features, the episode is, by definition, manic. Cognitive Level: Analysis Integrated Process: Assessment 13. A client has been diagnosed with major depressive episode. After treatment with fluoxetine (Prozac), the client exhibits pressured speech and flight of ideas. Based on this symptom change, which physician action would the nurse anticipate? 1. Increase the dosage of fluoxetine. 2. Discontinue the fluoxetine and rethink the clients diagnosis. 3. Order benztropine (Cogentin) to address extrapyramidal symptoms. 4. Order olanzapine (Zyprexa) to address altered thoughts. ANS: 2 Rationale: A full manic episode emerging during antidepressant treatment (medication, electroconvulsive therapy, etc.), but persisting beyond the physiological effect of that treatment is sufficient evidence for a manic episode and, therefore, a Bipolar I diagnosis. Cognitive Level: Analysis Integrated Process: Assessment 14. Which is the basic premise of a recovery model used to treat clients diagnosed with bipolar disorder? 1. Medication adherence 2. Empowerment of the consumer 3. Total absence of symptoms 4. Improved psychosocial relationships ANS: 2 Rationale: The basic premise of a recovery model is empowerment of the consumer. The recovery model is designed to allow consumers primary control over decisions about their own care and to enable a person with a mental health problem to live a meaningful life in a community of his or her choice while striving to achieve his or her full potential. Cognitive Level: Application Integrated Process: Assessment Multiple Response 15. Which of the following instructions regarding lithium therapy should be included in a nurses discharge teaching? (Select all that apply.) 1. Avoid excessive use of beverages containing caffeine. 2. Maintain a consistent sodium intake. 3. Consume at least 2,500 to 3,000 mL of fluid per day. 4. Restrict sodium content. 5. Restrict fluids to 1,500 mL per day. ANS: 1, 2, 3 Rationale: The nurse should instruct the client taking lithium to avoid excessive use of caffeine, maintain a consistent sodium intake, and consume at least 2,500 to 3,000 mL of fluid per day. The risk of developing lithium toxicity is high because of the narrow margin between therapeutic doses and toxic levels. Fluid or sodium restriction can impact lithium levels. Cognitive Level: Application Integrated Process: Implementation 16. A nurse is assessing an adolescent client diagnosed with cyclothymic disorder. Which of the following DSM-5 diagnostic criteria would the nurse expect this client to meet? (Select all that apply.) 1. Symptoms lasting for a minimum of two years 2. Numerous periods with manic symptoms 3. Possible comorbid diagnosis of a delusional disorder 4. Symptoms cause clinically significant impairment in important areas of functioning 5. Depressive symptoms that do not meet the criteria for major depressive episode ANS: 4, 5 Rationale: The following are selected criteria for the diagnosis of cyclothymic disorder. For at least one year in children and adolescents there have been numerous periods with hypomanic, not manic symptoms that do not meet criteria for hypomanic episode and numerous periods with depressive symptoms that do not meet the criteria for a major depressive episode. The symptoms are not better accounted for by schizoaffective disorder and are not superimposed on schizophrenia, schizophreniform disorder, delusional disorder, or psychotic disorder not elsewhere classified. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. Cognitive Level: Application Integrated Process: Implementation 17. Which of the following rationales by a nurse explain to parents why is it difficult to diagnose a child or adolescent exhibiting symptoms of bipolar disorder? (Select all that apply.) 1. Bipolar symptoms mimic attention deficit-hyperactivity disorder symptoms. 2. Children are naturally active, energetic, and spontaneous. 3. Neurotransmitter levels vary considerably in accordance with age. 4. The diagnosis of bipolar disorder cannot be assigned prior to the age of 18. 5. Genetic predisposition is not a reliable diagnostic determinant. Nursing Process: Assessment Client Need: Psychological Integrity ANS: 1, 2 Rationale: It is difficult to diagnose a child or adolescent with bipolar disorder, because bipolar symptoms mimic attention deficit-hyperactivity disorder symptoms and because children are naturally active, energetic, and spontaneous. Symptoms may also be comorbid with other childhood disorders, such as conduct disorder. Cognitive Level: Application Integrated Process: Assessment Fill-in-the-Blank 18. is an alteration in mood that is expressed by feelings of elation, inflated self-esteem, grandiosity, hyperactivity, agitation, and accelerated thinking and speaking. ANS: Mania Rationale: Mania is an alteration in mood that is expressed by feelings of elation, inflated self- esteem, grandiosity, hyperactivity, agitation, and accelerated thinking and speaking. Mania can occur as a biological (organic) or psychological disorder, or as a response to substance use or a general medical condition. Chapter 18. Anxiety, Obsessive-Compulsive, and Related Disorders Multiple Choice 1. A nursing instructor is teaching about specific phobias. Which student statement indicates to the instructor that learning has occurred? 1. These clients recognize their fear as excessive and frequently seek treatment. 2. These clients have a panic level of fear that is overwhelming and unreasonable. 3. These clients experience symptoms that mirror a cerebrovascular accident (CVA). 4. These clients experience the symptoms of tachycardia, dysphagia, and diaphoresis. ANS: 2 Rationale: The nursing instructor should evaluate that learning has occurred when the student knows that clients with phobias have a panic level of fear that is overwhelming and unreasonable. Phobia is fear cued by a specific object or situation in which exposure to the stimuli produces an immediate anxiety response. Even though the disorder is relatively common among the general population, people seldom seek treatment unless the phobia interferes with ability to function. Cognitive Level: Application Integrated Process: Evaluation 2. Which nursing statement to a client about social anxiety disorder versus schizoid personality disorder (SPD) is most accurate? 1. Clients diagnosed with social anxiety disorder can manage anxiety without medications, whereas clients diagnosed with SPD can only manage anxiety with medications. 2. Clients diagnosed with SPD are distressed by the symptoms experienced in social settings, whereas clients diagnosed with social anxiety disorder are not. 3. Clients diagnosed with social anxiety disorder avoid interactions only in social settings, whereas clients diagnosed with SPD avoid interactions in all areas of life. 4. Clients diagnosed with SPD avoid interactions only in social settings, whereas clients diagnosed with social anxiety disorder tend to avoid interactions in all areas of life. ANS: 3 Rationale: Clients diagnosed with social anxiety disorder avoid interactions only in social settings, whereas clients diagnosed with SPD avoid interactions in all areas of life. Social anxiety disorder is an excessive fear of situations in which a person might do something embarrassing or be evaluated negatively by others. Cognitive Level: Analysis Integrated Process: Implementation 3. What symptoms should a nurse recognize that differentiate a client diagnosed with panic disorder from a client diagnosed with generalized anxiety disorder (GAD)? 1. GAD is acute in nature, and panic disorder is chronic. 2. Chest pain is a common GAD symptom, whereas this symptom is absent in panic disorders. 3. Hyperventilation is a common symptom in GAD and rare in panic disorder. 4. Depersonalization is commonly seen in panic disorder and absent in GAD. ANS: 4 Rationale: The nurse should recognize that a client diagnosed with panic disorder experiences depersonalization, whereas a client diagnosed with GAD would not. Depersonalization refers to being detached from oneself when experiencing extreme anxiety. Cognitive Level: Analysis Integrated Process: Assessment 4. Which treatment should a nurse identify as most appropriate for clients diagnosed with generalized anxiety disorder (GAD)? 1. Long-term treatment with diazepam (Valium) 2. Acute symptom control with citalopram (Celexa) 3. Long-term treatment with buspirone (BuSpar) 4. Acute symptom control with ziprasidone (Geodon) ANS: 3 Rationale: The nurse should identify that an appropriate treatment for clients diagnosed with GAD is long-term treatment with buspirone. Buspirone is an anxiolytic medication that is effective in 60% to 80% of clients diagnosed with GAD. Buspirone takes 10 to 14 days for alleviation of symptoms but does not have the dependency concerns of other anxiolytics. Cognitive Level: Application Integrated Process: Evaluation 5. Which symptoms should a nurse recognize that differentiate a client diagnosed with obsessive- compulsive disorder (OCD) from a client diagnosed with obsessive-compulsive personality disorder? 1. Clients diagnosed with OCD experience both obsessions and compulsions, and clients diagnosed with obsessive-compulsive personality disorder do not. 2. Clients diagnosed with obsessive-compulsive personality disorder experience both obsessions and compulsions, and clients diagnosed with OCD do not. 3. Clients diagnosed with obsessive-compulsive personality disorder experience only obsessions, and clients diagnosed with OCD experience only compulsions. 4. Clients diagnosed with OCD experience only obsessions, and clients diagnosed with obsessive-compulsive personality disorder experience only compulsions. ANS: 1 Rationale: A client diagnosed with OCD experiences both obsessions and compulsions. Clients with obsessive-compulsive personality disorder exhibit a pervasive pattern of preoccupation with orderliness, perfectionism, mental and interpersonal control, but do not experience obsessions and compulsions. Cognitive Level: Analysis Integrated Process: Evaluation 6. A cab driver, stuck in traffic, becomes lightheaded, tremulous, diaphoretic, tachycardic and dyspneic. A workup in an emergency department reveals no pathology. Which medical diagnosis should a nurse suspect, and what nursing diagnosis should be the nurses first priority? 1. Generalized anxiety disorder and a nursing diagnosis of fear 2. Altered sensory perception and a nursing diagnosis of panic disorder 3. Pain disorder and a nursing diagnosis of altered role performance 4. Panic disorder and a nursing diagnosis of anxiety ANS: 4 Rationale: The nurse should suspect that the client has exhibited signs and symptoms of a panic disorder. The priority nursing diagnosis should be anxiety. Panic disorder is characterized by recurrent, sudden-onset panic attacks in which the person feels intense fear, apprehension, or terror. Cognitive Level: Analysis Integrated Process: Diagnosis 7. A client diagnosed with panic disorder states, When an attack happens, I feel like I am going to die. Which is the most appropriate nursing response? 1. I know its frightening, but try to remind yourself that this will only last a short time. 2. Death from a panic attack happens so infrequently that there is no need to worry. 3. Most people who experience panic attacks have feelings of impending doom. 4. Tell me why you think you are going to die every time you have a panic attack. ANS: 1 Rationale: The most appropriate nursing response to the clients concerns is to empathize with the client and provide encouragement that panic attacks only last a short period. Panic attacks usually last minutes but can, rarely, last hours. When the nurse states that Most people who experience panic attacks the nurse depersonalizes and belittles the clients feeling. Cognitive Level: Application Integrated Process: Implementation 8. A nursing instructor is teaching about the medications used to treat panic disorder. Which student statement indicates that learning has occurred? 1. Clonazepam (Klonopin) is particularly effective in the treatment of panic disorder. 2. Clozapine (Clozaril) is used off-label in long-term treatment of panic disorder. 3. Doxepin (Sinequan) can be used in low doses to relieve symptoms of panic attacks. 4. Buspirone (BuSpar) is used for its immediate effect to lower anxiety during panic attacks. ANS: 1 Rationale: The student indicates learning has occurred when he or she states that clonazepam is a particularly effective treatment for panic disorder. Clonazepam is a type of benzodiazepine in which the major risk is physical dependence and tolerance, which may encourage abuse. It can be used on an as-needed basis to reduce anxiety and the related symptoms. Cognitive Level: Application Integrated Process: Evaluation 9. A family member is seeking advice about an older parent who seems to worry unnecessarily about everything. The family member states, Should I seek psychiatric help for my mother? Which is an appropriate nursing response? 1. My mother also worries unnecessarily. I think it is part of the aging process. 2. Anxiety is considered abnormal when it is out of proportion to the stimulus causing it and when it impairs functioning. 3. From what you have told me, you should get her to a psychiatrist as soon as possible. 4. Anxiety is a complex phenomenon and is effectively treated only with psychotropic medications. ANS: 2 Rationale: The most appropriate response by the nurse is to explain to the family member that anxiety is considered abnormal when it is out of proportion and impairs functioning. Anxiety is a normal reaction to a realistic danger or threat to biological integrity or self-concept. Cognitive Level: Application Integrated Process: Implementation 10. A client is experiencing a severe panic attack. Which nursing intervention would meet this clients physiological need? 1. Teach deep breathing relaxation exercises. 2. Place the client in a Trendelenburg position. 3. Have the client breathe into a paper bag. 4. Administer the ordered prn buspirone (BuSpar). ANS: 3 Rationale: The nurse can meet this clients physiological need by having the client breathe into a paper bag. Hyperventilation may occur during periods of extreme anxiety. Hyperventilation causes the amount of carbon dioxide (CO2) in the blood to decrease, possibly resulting in lightheadedness, rapid heart rate, shortness of breath, numbness or tingling in the hands or feet, and syncope. If hyperventilation occurs, assist the client to breathe into a small paper bag held over the mouth and nose. Six to twelve natural breaths should be taken, alternating with short periods of diaphragmatic breathing. Cognitive Level: Application Integrated Process: Implementation 11. A college student is unable to take a final exam owing to severe test anxiety. Instead of studying, the student relieves stress by attending a movie. Which priority nursing diagnosis should a campus nurse assign for this client? A. Non-adherence R/T test taking B. Ineffective role performance R/T helplessness C. Altered coping R/T anxiety D. Powerlessness R/T fear ANS: C Rationale: The priority nursing diagnosis for this client is altered coping R/T anxiety. The nurse should assist in implementing interventions that will improve the clients healthy coping skills and reduce anxiety. Cognitive Level: Analysis Integrated Process: Diagnosis 12. A client living in a beachfront community is seeking help with an extreme fear of bridges, which is interfering with daily functioning. A psychiatric nurse practitioner decides to try systematic desensitization. Which explanation of this treatment should the nurse provide? 1. Using your imagination, we will attempt to achieve a state of relaxation. 2. Because anxiety and relaxation are mutually exclusive states, we can attempt to substitute a relaxation response for the anxiety response. 3. Through a series of increasingly anxiety-provoking steps, we will gradually increase your tolerance to anxiety. 4. In one intense session, you will be exposed to a maximum level of anxiety that you will learn to tolerate. ANS: 3 Rationale: The nurse should explain to the client that when participating in systematic desensitization he or she will go through a series of increasingly anxiety-provoking steps that will gradually increase tolerance. Systematic desensitization was introduced by Joseph Wolpe in 1958 and is based on behavioral conditioning principles. Cognitive Level: Application Integrated Process: Implementation 13. A client diagnosed with obsessive-compulsive disorder is admitted to a psychiatric unit. The client has an elaborate routine for toileting activities. Which would be an appropriate initial client outcome during the first week of hospitalization? 1. The client will refrain from ritualistic behaviors during daylight hours. 2. The client will wake early enough to complete rituals prior to breakfast. 3. The client will participate in three unit activities by day three. 4. The client will substitute a productive activity for rituals by day one. ANS: 2 Rationale: An appropriate initial client outcome is for the client to wake early enough to complete rituals prior to breakfast. The nurse should also provide a structured schedule of activities and begin to gradually limit the time allowed for rituals. Cognitive Level: Application Integrated Process: Planning 14. A nurse is providing discharge teaching to a client taking a benzodiazepine. Which client statement would indicate a need for further follow-up instructions? 1. I will need scheduled blood work in order to monitor for toxic levels of this drug. 2. I wont stop taking this medication abruptly because there could be serious complications. 3. I will not drink alcohol while taking this medication. 4. I wont take extra doses of this drug because I can become addicted. ANS: 1 Rationale: The client indicates a need for additional information about taking benzodiazepines when stating the need for blood work to monitor for toxic levels. This intervention is used when taking lithium (Eskalith) for the treatment of bipolar disorder. The client should understand that taking extra doses of a benzodiazepine may result in addiction and that the drug should not be taken in conjunction with alcohol. Cognitive Level: Application Integrated Process: Evaluation 15. A client diagnosed with an obsessive-compulsive disorder spends hours bathing and grooming. During a one-on-one interaction, the client discusses the rituals in detail but avoids any feelings that the rituals generate. Which defense mechanism should the nurse identify? 1. Sublimation 2. Dissociation 3. Rationalization 4. Intellectualization ANS: 4 Rationale: The nurse should identify that the client is using the defense mechanism of intellectualization when discussing the rituals of obsessive-compulsive disorder in detail while avoiding discussion of feelings. Intellectualization is an attempt to avoid expressing emotions associated with a stressful situation by using the intellectual process of logic, reasoning, and analysis. Cognitive Level: Application Integrated Process: Assessment 16. A client is newly diagnosed with obsessive-compulsive disorder and spends 45 minutes folding clothes and rearranging them in drawers. Which nursing intervention would best address this clients problem? 1. Distract the client with other activities whenever ritual behaviors begin. 2. Report the behavior to the psychiatrist to obtain an order for medication dosage increase. 3. Lock the room to discourage ritualistic behavior. 4. Discuss the anxiety-provoking triggers that precipitate the ritualistic behaviors. ANS: 4 Rationale: The nurse should discuss with the client the anxiety-provoking triggers that precipitate the ritualistic behavior. If the client is going to be able to control interrupting anxiety, he or she must first learn to recognize precipitating factors. Attempting to distract the client, seeking medication increase, and locking the clients room are not appropriate interventions, because they do not help the client gain insight. Cognitive Level: Application Integrated Process: Implementation 17. A nursing student questions an instructor regarding the order for fluvoxamine (Luvox) 300 mg daily for a client diagnosed with obsessive-compulsive disorder (OCD). Which instructor response is most accurate? 1. High doses of tricyclic medications will be required for effective treatment of OCD. 2. Selective serotonin reuptake inhibitor (SSRI) doses, in excess of what is effective for treating depression, may be required for OCD. 3. The dose of Luvox is low because of the side effect of daytime drowsiness. 4. The dose of this selective serotonin reuptake inhibitor (SSRI) is outside the therapeutic range and needs to be questioned. ANS: 2 Rationale: The most accurate instructor response is that SSRI doses in excess of what is effective for treating depression may be required in the treatment of OCD. SSRIs have been approved by the Food and Drug Administration for the treatment of OCD. Common side effects include headache, sleep disturbances, and restlessness. Cognitive Level: Application Integrated Process: Implementation 18. A client is prescribed alprazolam (Xanax) for acute anxiety. What client history should cause a nurse to question this order? A. History of alcohol use disorder B. History of personality disorder C. History of schizophrenia D. History of hypertension ANS: A Rationale: The nurse should question a prescription of alprazolam for acute anxiety if the client has a history of alcohol use disorder. Alprazolam is a benzodiazepine used in the treatment of anxiety and has an increased risk for physiological dependence and tolerance. A client with a history of substance use disorder may be more likely to abuse other addictive substances. Cognitive Level: Application Integrated Process: Evaluation 19. During her aunts wake, a four-year-old child runs up to the casket before a mother can stop her. An appointment is made with a nurse practitioner when the child starts twisting and pulling out hair. Which nursing diagnosis should the nurse practitioner assign to this child? A. Complicated grieving B. Altered family processes C. Ineffective coping D. Body image disturbance ANS: C Rationale: Ineffective coping is defined as an inability to form a valid appraisal of the stressors, inadequate choices of practiced responses, and/or inability to use available resources. This child is coping with the anxiety generated by viewing her deceased aunt by pulling out hair. If this behavior continues, a diagnosis of hair-pulling disorder, or trichotillomania, may be assigned. Cognitive Level: Analysis Integrated Process: Diagnosis 20. A nursing instructor is teaching about the symptoms of agoraphobia. Which student statement indicates that learning has occurred? 1. Onset of symptoms most commonly occurs in early adolescence and persists until midlife. 2. Onset of symptoms most commonly occurs in the 20s and 30s and persists for many years. 3. Onset of symptoms most commonly occurs in the 40s and 50s and persists until death. 4. Onset of symptoms most commonly occurs after the age of 60 and persists for at least 6 years. ANS: 2 Rationale: The onset of the symptoms of agoraphobia most commonly occurs in the 20s and 30s and persists for many years. Cognitive Level: Application Integrated Process: Assessment Multiple Response 21. A college student has been diagnosed with generalized anxiety disorder (GAD). Which of the following symptoms should a campus nurse expect this client to exhibit? (Select all that apply.) 1. Fatigue 2. Anorexia 3. Hyperventilation 4. Insomnia 5. Irritability ANS: 1, 4, 5 Rationale: The nurse should expect that a client diagnosed with GAD would experience fatigue, insomnia, and irritability. GAD is characterized by chronic, unrealistic, and excessive anxiety and worry. Cognitive Level: Application Integrated Process: Assessment 22. A nurse is discussing treatment options with a client whose life has been negatively impacted by claustrophobia. Which of the following commonly used behavioral therapies for phobias should the nurse explain to the client? (Select all that apply.) 1. Benzodiazepine therapy 2. Systematic desensitization 3. Imploding (flooding) 4. Assertiveness training 5. Aversion therapy ANS: 2, 3 Rationale: The nurse should explain to the client that systematic desensitization and imploding are the most common behavioral therapies used for treating phobias. Systematic desensitization involves the gradual exposure of the client to anxiety-provoking stimuli. Imploding is the intervention used in which the client is exposed to extremely frightening stimuli for prolonged periods of time. Cognitive Level: Application Integrated Process: Implementation 23. A nurse has been caring for a client diagnosed with generalized anxiety disorder (GAD). Which of the following nursing interventions would address this clients symptoms? (Select all that apply.) 1. Encourage the client to recognize the signs of escalating anxiety. 2. Encourage the client to avoid any situation that causes stress. 3. Encourage the client to employ newly learned relaxation techniques. 4. Encourage the client to cognitively reframe thoughts about situations that generate anxiety. 5. Encourage the client to avoid caffeinated products. ANS: 1, 3, 4, 5 Rationale: Nursing interventions that address GAD symptoms should include encouraging the client to recognize signs of escalating anxiety, to employ relaxation techniques, to cognitively reframe thoughts about anxiety-provoking situations, and to avoid caffeinated products. Avoiding situations that cause stress is not an appropriate intervention, because avoidance does not help the client overcome anxiety and because not all situations are easily avoidable. Cognitive Level: Application Integrated Process: Implementation 24. An attractive female client presents with high anxiety levels because of her belief that her facial features are large and grotesque. Body dysmorphic disorder (BDD) is suspected. Which of the following additional symptoms would support this diagnosis? (Select all that apply.) 1. Mirror checking 2. Excessive grooming 3. History of an eating disorder 4. History of delusional thinking 5. Skin picking ANS: 1, 2, 5 Rationale: The DSM-5 lists preoccupation with one or more perceived defects or flaws in physical appearance that are not observable or appear slight to others as a diagnostic criteria for the diagnosis of BDD. Also listed is that at some point during the course of the disorder, the person has performed repetitive behaviors, such as mirror checking, excessive grooming, skin picking, or reassurance seeking. Cognitive Level: Application Integrated Process: Assessment Fill-in-the-Blank 25. Traits associated with schizoid, obsessive-compulsive, and personality disorders are commonly seen in clients with the diagnosis of body dysmorphic disorder. ANS: narcissistic Rationale: Traits associated with schizoid, obsessive-compulsive, and narcissistic personality disorders are not uncommon in clients with the diagnosis of BDD. Cognitive Level: Application Integrated Process: Assessment 26. Antianxiety drugs are also called and minor tranquilizers. ANS: anxiolytics Rationale: Antianxiety drugs are also called anxiolytics and minor tranquilizers. Antianxiety agents are used in the treatment of anxiety disorders, anxiety symptoms, acute alcohol withdrawal, skeletal muscle spasms, convulsive disorders, status epilepticus, and preoperative sedation. Chapter 19. Trauma- and Stressor-Related Disorders Multiple Choice 1. A nursing instructor is teaching about trauma and stressor-related disorders. Which student statement indicates that further instruction is needed? 1. The trauma that women experience is more likely to be sexual assault and child sexual abuse. 2. The trauma that men experience is more likely to be accidents, physical assaults, combat, or viewing death or injury. 3. After exposure to a traumatic event, only 10 percent of victims develop post-traumatic stress disorder (PTSD). 4. Research shows that PTSD is more common in men than in women. ANS: 4 Rationale: Research shows that PTSD is more common in women than in men. This student statement indicates a need for further instruction. Cognitive Level: Application Integrated Process: Evaluation 2. Which factors differentiate the diagnosis of PTSD from the diagnosis of adjustment disorder (AD)? 1. PTSD results from exposure to an extreme traumatic event, whereas AD results from exposure to normal daily events. 2. AD results from exposure to an extreme traumatic event, whereas PTSD results from exposure to normal daily events. 3. Depressive symptoms occur in PTSD and not in AD. 4. Depressive symptoms occur in AD and not in PTSD. ANS: 1 Rationale: PTSD results from exposure to an extreme traumatic event, whereas AD results from exposure to normal daily events, such as divorce, failure, or rejection. Depressive symptoms can occur in both PTSD and AD. Cognitive Level: Analysis Integrated Process: Assessment 3. Which client would a nurse recognize as being at highest risk for the development of an AD? 1. A young married woman 2. An elderly unmarried man 3. A young unmarried woman 4. A young unmarried man ANS: 3 Rationale: Adjustment disorders are more common in women, unmarried persons, and younger people. Although more common in the young, it can occur at any age. Cognitive Level: Application Integrated Process: Assessment 4. A nursing instructor is explaining the etiology of trauma-related disorders from a learning theory perspective. Which student statement indicates that learning has occurred? 1. How clients perceive events and view the world affect their response to trauma. 2. The psychic numbing in PTSD is a result of negative reinforcement. 3. The individual becomes addicted to the trauma owing to an endogenous opioid response. 4. Believing that the world is meaningful and controllable can protect an individual from PTSD. ANS: 2 Rationale: Learning theorists view negative reinforcement as behavior that leads to a reduction in an aversive experience, thereby reinforcing and resulting in repetition of the behavior. Psychic numbing decreases or protects an individual from emotional pain and, therefore, the learned response is the repetition of this behavior. Cognitive Level: Application Integrated Process: Evaluation 5. As the sole survivor of a roadside bombing, a veteran is experiencing extreme guilt. Which nursing diagnosis would address this clients symptom? 1. Anxiety 2. Altered thought processes 3. Complicated grieving 4. Altered sensory perception ANS: 3 Rationale: The clients survivor guilt is disrupting the normal process of grieving. Although the client may also experience anxiety, the symptom presented in the question is extreme guilt. There is no evidence presented in the question to indicate altered thought or altered sensory perception. Cognitive Level: Analysis Integrated Process: Diagnosis 6. A client has been assigned a nursing diagnosis of complicated grieving related to the death of multiple family members in a motor vehicle accident. Which intervention should the nurse initially employ? 1. Encourage the journaling of feelings. 2. Assess for the stage of grief in which the client is fixed. 3. Provide community resources to address the clients concerns. 4. Encourage attending a grief therapy group. ANS: 2 Rationale: Prior to implementing all other nursing interventions presented, the nurse must assess the stage of grief in which the client is fixed. Appropriate nursing interventions are always based on accurate assessments. Cognitive Level: Application Integrated Process: Implementation 7. Which clinical presentation is associated with the most commonly diagnosed adjustment disorder (AD)? 1. Anxiety, feelings of hopelessness, and worry 2. Truancy, vandalism, and fighting 3. Nervousness, worry, and jitteriness 4. Depressed mood, tearfulness, and hopelessness ANS: 4 Rationale: AD with depressed mood is the most commonly diagnosed adjustment disorder. The clinical presentation is one of predominant mood disturbance, although less pronounced than that of major depression. The symptoms, such as depressed mood, tearfulness, and feelings of hopelessness, exceed what is an expected or normative response to an identified stressor. Cognitive Level: Analysis Integrated Process: Assessment 8. Both situational and intrapersonal factors most likely contribute to an individuals stress response. Which factor would a nurse categorize as intrapersonal? 1. Occupational opportunities 2. Economic conditions 3. Degree of flexibility 4. Availability of social supports ANS: 3 Rationale: Intrapersonal factors that might influence an individuals ability to adjust to a painful life change include social skills, coping strategies, the presence of psychiatric illness, degree of flexibility, and level of intelligence. Cognitive Level: Application Integrated Process: Assessment 9. A client diagnosed with AD has been assigned the nursing diagnosis of anxiety R/T divorce. Which correctly written outcome addresses this clients problem? 1. Rates anxiety as 4 out of 10 by discharge. 2. States anxiety level has decreased by day one. 3. Accomplishes activities of daily living independently. 4. Demonstrates ability for adequate social functioning by day three. ANS: 1 Rationale: An outcome statement must be client-centered, specific, measurable, and contain a time frame, so that it can be evaluated effectively. A decrease in anxiety is vague rather than specific, and expecting an anxiety decrease by day one may also be unrealistic. Accomplishing activities of daily living independently and demonstrating the ability for adequate social functioning do not address the anxiety nursing diagnosis. Cognitive Level: Application Integrated Process: Planning 10. Eye movement desensitization and reprocessing (EMDR) has been empirically validated for which disorder? 1. Adjustment disorder 2. Generalized anxiety disorder 3. Panic disorder 4. Post-traumatic stress disorder ANS: 4 Rationale: EMDR has been used for depression, adjustment disorder, phobias, addictions, generalized anxiety disorder, and panic disorder. However, at present, EMDR has only been empirically validated for trauma-related disorders such as PTSD and acute stress disorder. Cognitive Level: Application Integrated Process: Evaluation 11. After a teaching session about grief, a client says to the nurse, I seem to be stuck in the anger stage of grieving over the loss of my son. How would the nurse assess this statement, and in what phase of the nursing process would this occur? 1. Assessment phase; nursing actions have been successful in achieving the objectives of care. 2. Evaluation phase; nursing actions have been successful in achieving the objectives of care. 3. Implementation phase; nursing actions have been successful in achieving the objectives of care. 4. Diagnosis phase; nursing actions have been successful in achieving the objectives of care. ANS: 2 Rationale: In the evaluation phase of the nursing process, reassessment is conducted to determine if the nursing actions have been successful in achieving the objectives of care. The implementation of client teaching has enabled the client to verbalize an understanding of the grief process and his or her position in the process. Therefore, the nurses actions can be evaluated as successful. Cognitive Level: Analysis Integrated Process: Evaluation 12. By which biological mechanism does EMDR achieve its therapeutic effect? 1. EMDR achieves its therapeutic effect, but the exact biological mechanism is unknown. 2. EMDR achieves its therapeutic effect by causing a decrease in imagery vividness. 3. EMDR achieves its therapeutic effect by causing an increase in memory access. 4. EMDR achieves its therapeutic effect by decreasing trauma associated anxiety. ANS: 1 Rationale: Some studies have indicated that eye movements cause a decrease in imagery vividness and distress, as well as an increase in memory access. EMDR is thought to relieve anxiety associated with the traumatic event. However, the exact biological mechanisms by which EMDR achieves its therapeutic effects are unknown. Cognitive Level: Application Integrated Process: Evaluation 13. A client receiving EMDR therapy says, After only two sessions of my therapy, I am feeling great. Now I can stop and get on with my life. Which of the following nursing responses is most appropriate? 1. I am thrilled that you have responded so rapidly to EMDR. 2. To achieve lasting results, all eight phases of EMDR must be completed. 3. If I were you, I would complete the EMDR and comply with doctors orders. 4. How do you feel about continuing the therapy? ANS: 2 Rationale: Clients often feel relief quite rapidly with EMDR. However, to achieve lasting results, it is important that each of the eight phases be completed. The nurses most appropriate response should be to give information to correct the clients misconceptions about the therapy. In answer 3 the nurse is subjectively giving advice rather than providing objective information. Cognitive Level: Application Integrated Process: Implementation 14. A nurse would recognize which treatment as most commonly used for AD and its appropriate rationale? 1. Psychotherapy; to examine the stressor and confront unresolved issues 2. Fluoxetine (Prozac); to stabilize mood and resolve symptoms 3. Eye movement desensitization therapy; to reprocess traumatic events 4. Lorazepam (Ativan); a first-line treatment to address symptoms of anxiety ANS: 1 Rationale: Psychotherapy is the most common treatment used for AD. AD is not commonly treated with medications. Anxiolytic and antidepressant medications may be prescribed as adjuncts to psychotherapy but should not be given as the first line of treatment. Eye movement desensitization and reprocessing therapy is not used to treat adjustment disorders. Cognitive Level: Application Integrated Process: Implementation 15. A nurse has been caring for a client diagnosed with PTSD. Which realistic goal should be included in this clients plan of care? 1. The client will have no flashbacks. 2. The client will be able to feel a full range of emotions by discharge. 3. The client will not require zolpidem (Ambien) to obtain adequate sleep by discharge. 4. The client will refrain from discussing the traumatic event. ANS: 3 Rationale: Obtaining adequate sleep without zolpidem by discharge is a goal that should be included in the clients plan of care. Having no flashbacks and experiencing a full range of emotions by discharge are unrealistic goals. Clients are encouraged, not discouraged, to discuss the traumatic event. Cognitive Level: Application Integrated Process: Planning 16. A client diagnosed with PTSD is receiving paliperidone (Invega). Which symptoms should a nurse identify that would warrant the need for this medication? 1. Flat affect and anhedonia 2. Persistent anorexia and 10 lb weight loss in 3 weeks 3. Flashbacks of killing the enemy 4. Distant and guarded in relationships ANS: 3 Rationale: The nurse should identify that a client who has flashbacks of killing the enemy may need paliperidone. Paliperidone is an antipsychotic medication that will address the symptoms of psychosis. Cognitive Level: Application Integrated Process: Assessment 17. A client, who recently delivered a stillborn baby, has a diagnosis of adjustment disorder unspecified. The nurse case manager should expect which client presentation that is characteristic of this diagnosis? 1. The client worries continually and appears nervous and jittery. 2. The client complains of a depressed mood, is tearful, and feels hopeless. 3. The client is belligerent, violates others rights, and defaults on legal responsibilities. 4. The client complains of many physical ailments, refuses to socialize, and quits her job. ANS: 4 Rationale: The diagnosis of adjustment disorder unspecified is assigned when the maladaptive reaction is not consistent with any of the other categories. Manifestations may include physical complaints, social withdrawal, or work or academic inhibition, without significant depressed or anxious mood. Cognitive Level: Application Integrated Process: Assessment 18. A client has been extremely nervous ever since a person died as a result of the clients drunk driving. When assessing for the diagnosis of AD, within what time frame should the nurse expect the client to exhibit symptoms? 1. To meet the DSM-5 criteria for adjustment disorder, the client should exhibit symptoms within one year of the accident. 2. To meet the DSM-5 criteria for adjustment disorder, the client should exhibit symptoms within three months of the accident. 3. To meet the DSM-5 criteria for adjustment disorder, the client should exhibit symptoms within six months of the accident. 4. To meet the DSM-5 criteria for adjustment disorder, the client should exhibit symptoms within nine months of the accident. ANS: 2 Rationale: According to the DSM-5 diagnostic criteria for adjustment disorders, the development of emotional or behavioral symptoms in response to an identifiable stressor occurs within three months of the onset of the stressor. Cognitive Level: Application Integrated Process: Assessment 19. A 20-year-old client and a 60-year-old client have had drunk driving accidents and are both experiencing extreme anxiety. From a psychosocial theory perspective, which of these clients would be predisposed to the diagnosis of adjustment disorder? 1. The 60-year-old, because of memory deficits. 2. The 60-year-old, because of decreased cognitive processing ability. 3. The 20-year-old, because of limited cognitive experiences. 4. The 20-year-old, because of lack of developmental maturity. ANS: 4 Rationale: Research indicates that there is a predisposition to the diagnosis of adjustment disorder when there is limited developmental maturity. By comparison, the 20-year-old does not have the developmental maturity, life experiences, and coping mechanisms that the 60-year-old might possess. Cognitive Level: Analysis Integrated Process: Evaluation Multiple Responses 20. A client diagnosed with an adjustment disorder says to the nurse, Tell me about medications that will cure this problem. Which of the following are appropriate nursing responses? (Select all that apply.) 1. Medications can interfere with your ability to find a more permanent problem solution. 2. Medications may mask the real problem at the root of this diagnosis. 3. Adjustment disorders are not commonly treated with medications. 4. Psychoactive drugs carry the potential for physiological and psychological dependence. 5. Psychoactive drugs will be prescribed only if your problems persist for more than three months. ANS: 1, 2, 3, 4 Rationale: Adjustment disorders are not commonly treated with medications because of temporary effects, masking the real problem, interfering with finding a permanent solution, and the potential for addiction. Cognitive Level: Application Integrated Process: Implementation 21. A nurse is admitting a client who has been diagnosed with PTSD. Which of the following symptoms might the nurse expect to assess? (Select all that apply.) 1. Feelings of guilt that precipitate social isolation 2. Aggressive behavior that affects job performance 3. Relationship problems 4. High levels of anxiety 5. Escalating symptoms lasting less than one month ANS: 1, 2, 3, 4 Rationale: Characteristic symptoms of PTSD include re-experiencing the traumatic event, a sustained high level of anxiety or arousal, general numbing of responsiveness, nightmares, inability to remember certain aspects of the traumatic event, depression, guilt feelings, substance abuse, anger, and aggressive behaviors. The full-symptom picture must present for more than one month and cause significant interference with social, occupational, and other areas of functioning. Cognitive Level: Application Integrated Process: Assessment 22. A family asks the nurse why their son was diagnosed with PTSD and others in the accident were not. Which of the following information should the nurse offer? (Select all that apply.) 1. An individuals religious affiliation can affect response to trauma. 2. Responses are affected by how an individual handled previous trauma. 3. Protectiveness of family and friends can help an individual deal with trauma. 4. Control over the possibility of recurrence can affect the response to trauma. 5. The time in which the trauma occurred can affect the individuals response. ANS: 2, 3, 4, 5 Rationale: Variables that affect whether an individual exposed to massive trauma develops trauma-related disorders are grouped into characteristics of (1) the traumatic experience, (2) the individual, and (3) the recovery environment. All information presented falls under one of these groups. Spiritual beliefs, which can be considered a cultural influence, can affect the individuals response, however, an individuals specific religious affiliation should have no bearing or influence. Cognitive Level: Application Integrated Process: Assessment 23. A nurse would recognize which of the following as the best predictors of PTSD in Vietnam veterans? (Select all that apply.) 1. The severity of the stressor 2. The degree of ego strength 3. The degree of psychosocial isolation in the recovery environment 4. The attitudes of society regarding the experience 5. The presence of preexisting psychopathology ANS: 1, 3 Rationale: In research with Vietnam veterans, it was shown that the best predictors of PTSD were the severity of the stressor and the degree of psychosocial isolation in the recovery environment. Cognitive Level: Analysis Integrated Process: Assessment 24. A client diagnosed with PTSD states, Why did my doctor prescribe an antidepressant rather than an antianxiety drug for me? Which of the following are the most appropriate nursing responses? (Select all that apply.) 1. Im not sure, because antianxiety drugs have been approved by the FDA for PTSD. 2. Antidepressants are now considered first-line treatment choice for PTSD. 3. Many people have adverse reactions to antianxiety drugs. 4. Because of their addictive properties, antianxiety drugs are less desirable. 5. There have been no controlled studies on the effect of antianxiety drugs on PTSD. ANS: 2, 4, 5 Rationale: Antidepressants are now considered the first-line treatment of choice for PTSD. There has been an absence of controlled studies demonstrating the efficacy of benzodiazepines for the treatment of PTSD. Their addictive properties make them less desirable than other medications used in the treatment of PTSD. Paroxetine and sertraline (antidepressant drugs), not antianxiety drugs, have been approved by the FDA for the treatment of PTSD. Adverse reactions can occur with the use of anxiolytic drugs, but these reactions are not common. Cognitive Level: Application Integrated Process: Implementation Ordering 25. Order the eight-phase process of eye movement desensitization and reprocessing (EMDR). Instillation Body scan Closure Reevaluation Preparation History and treatment planning Desensitization Assessment ANS: The correct order is 5, 6, 7, 8, 2, 1, 4, 3 Rationale: EMDR is an integrative psychotherapy approach with a theoretical model that emphasizes the brains information processing system and memories of disturbing experiences as the basis of pathology. EMDR has been shown to be an effective therapy for PTSD and other trauma-related disorders. 1. History and Treatment Planning 2. Preparation 3. Assessment 4. Desensitization 5. Instillation 6. Body scan 7. Closure 8. Reevaluation Cognitive Level: Analysis Integrated Process: Assessment Fill-in-the-Blank 26. An extremely distressing experience that causes severe emotional shock and may have long- lasting psychological effects is called . ANS: trauma Rationale: An extremely distressing experience that causes severe emotional shock and may have long-lasting psychological effects is called trauma. PTSD can occur following exposure to an identifiable stressor or to an extreme traumatic event. Chapter 20. Somatic Symptom and Dissociative Disorders Multiple Choice 1. A client diagnosed with somatic symptom disorder (SSD) is most likely to exhibit which personality disorder characteristics? 1. Experiences intense and chaotic relationships with fluctuating attitudes toward others. 2. Socially irresponsible, exploitative, guiltless, and disregards rights of others. 3. Self-dramatizing, attention seeking, overly gregarious, and seductive. 4. Uncomfortable in social situations, perceived as timid, withdrawn, cold, and strange. ANS: 3 Rationale: The nurse should anticipate that a client diagnosed with SSD would be self- dramatizing, attention seeking, and overly gregarious. It has been suggested that, in somatic symptom disorder, there may be some overlapping of personality characteristics and features associated with histrionic personality disorder. These symptoms include heightened emotionality, impressionistic thought and speech, seductiveness, strong dependency needs, and a preoccupation with symptoms and oneself. Cognitive Level: Analysis Integrated Process: Assessment 2. A nurse is working with a client diagnosed with SSD. What criteria would differentiate this diagnosis from illness anxiety disorder (IAD)? 1. The client diagnosed with SSD experiences physical symptoms in various body systems, and the client diagnosed with IAD does not. 2. The client diagnosed with SSD experiences a change in the quality of self-awareness, and the client diagnosed with IAD does not. 3. The client diagnosed with SSD disorder has a perceived disturbance in body image or appearance, and the client diagnosed with IAD does not. 4. The client diagnosed with SSD only experiences anxiety about the possibility of illness, and the client diagnosed with IAD does not. ANS: 1 Rationale: Individuals experiencing somatic symptoms without corroborating pathology are considered to have SSD, and those with minimal or no somatic symptoms would be diagnosed with IAD, a diagnosis new to the DSM-5. Clients diagnosed with IAD have minimal or no somatic complaints, but present with intense anxiety and suspiciousness of the presence of an undiagnosed, serious medical illness. Cognitive Level: Analysis Integrated Process: Assessment 3. Which would be considered an appropriate outcome when planning care for an inpatient client diagnosed with SSD? 1. The client will admit to fabricating physical symptoms to gain benefits by day three. 2. The client will list three potential adaptive coping strategies to deal with stress by day two. 3. The client will comply with medical treatments for physical symptoms by day three. 4. The client will openly discuss physical symptoms with staff by day four. ANS: 2 Rationale: The nurse should determine that an appropriate outcome for a client diagnosed with SSD would be for the client to list three potential adaptive coping strategies to deal with stress by day two. Because the symptoms of SSD are associated with psychosocial distress, increased coping skills may help the client reduce symptoms. Cognitive Level: Application Integrated Process: Planning 4. Which are examples of primary and secondary gains that clients diagnosed with SSD: predominately pain, may experience? 1. Primary: chooses to seek a new doctor; Secondary: euphoric feeling from new medications 2. Primary: euphoric feeling from new medications; Secondary: chooses to seek a new doctor 3. Primary: receives get-well cards; Secondary: pain prevents attending stressful family reunion 4. Primary: pain prevents attending stressful family reunion; Secondary: receives get-well cards ANS: 4 Rationale: The nurse should identify that primary gains are those that allow the client to avoid an unpleasant activity (stressful family reunion) and that secondary gains are those in which the client receives emotional support or attention (get-well cards). Cognitive Level: Analysis Integrated Process: Evaluation 5. A nursing instructor is teaching about the etiology of IAD from a psychoanalytical perspective. What student statement about clients diagnosed with this disorder indicates that learning has occurred? 1. They tend to have a familial predisposition to this disorder. 2. When the sick role relieves them from stressful situations, their physical symptoms are reinforced. 3. They misinterpret and cognitively distort their physical symptoms. 4. They express personal worthlessness through physical symptoms, because physical problems are more acceptable than psychological problems. ANS: 4 Rationale: The nurse should understand that from a psychoanalytical perspective, IAD occurs because physical problems are more acceptable than psychological problems. Psychodynamicists view IAD as a defense mechanism. Cognitive Level: Application Integrated Process: Evaluation 6. An inpatient client is newly diagnosed with dissociative identity disorder (DID) stemming from severe childhood sexual abuse. Which nursing intervention takes priority? 1. Encourage exploration of sexual abuse. 2. Encourage guided imagery. 3. Establish trust and rapport. 4. Administer antianxiety medications. ANS: 3 Rationale: The nurse should prioritize establishing trust and rapport when beginning to work with a client diagnosed with DID. DID was formerly called multiple personality disorder. Trust is the basis of every therapeutic relationship. Each personality views itself as a separate entity and must be treated as such to establish rapport. Cognitive Level: Analysis Integrated Process: Implementation 7. A client diagnosed with DID switches personalities when confronted with destructive behavior. The nurse recognizes that this dissociation serves which function? 1. It is a means to attain secondary gain. 2. It is a means to explore feelings of excessive and inappropriate guilt. 3. It serves to isolate painful events so that the primary self is protected. 4. It serves to establish personality boundaries and limit inappropriate impulses. ANS: 3 Rationale: The nurse should anticipate that a client who switches personalities when confronted with destructive behavior is dissociating in order to isolate painful events so that the primary self is protected. The transition between personalities is usually sudden, dramatic, and precipitated by stress. Cognitive Level: Application Integrated Process: Assessment 8. A client is diagnosed with DID. What is the primary goal of therapy for this client? 1. To recover memories and improve thinking patterns. 2. To prevent social isolation. 3. To decrease anxiety and need for secondary gain. 4. To collaborate among sub-personalities to improve functioning. ANS: 4 Rationale: The nurse should anticipate that the primary therapeutic goal for a client diagnosed with DID is to collaborate among sub-personalities to improve functioning. Some clients choose to pursue a lengthy therapeutic regimen to achieve integration, a blending of all the personalities into one. The goal is to optimize the clients functioning and potential. Cognitive Level: Application Integrated Process: Planning 9. According to the DSM-5 diagnostic criteria for dissociative amnesia (DA), what symptom would be essential to meet the criteria for the subcategory of dissociative fugue? 1. An inability to recall important autobiographical information 2. Clinically significant distress in social and occupational functioning 3. Sudden unexpected travel or bewildered wandering 4. Blackouts related to alcohol toxicity ANS: 2 Rationale: An inability to recall important autobiographical information and clinically significant distress in social and occupational functioning are basic criteria for the diagnosis of DA. A specific subtype of dissociative amnesia is with dissociative fugue. Dissociative fugue is characterized by a sudden, unexpected travel away from customary place of daily activities, or by bewildered wandering, with the inability to recall some or all of ones past. The DSM-5 also states that symptoms cannot be attributable to the direct physiological effects of a substance (e.g., alcohol, a drug of abuse, a medication). Cognitive Level: Application Integrated Process: Assessment 10. Which situation is an example of selective amnesia? 1. A client cannot relate any lifetime memories. 2. A client can describe driving to Ohio but cannot remember the car accident that occurred. 3. A client often wanders aimlessly after sunset. 4. A client cannot provide personal demographic information during admission assessment. ANS: 2 Rationale: Three types of disturbance in recall are identified in the DSM-5: localized, selective, and generalized. Localized and selective amnesia are related to a specific stressful event that has occurred. In selective amnesia, the individual can recall only certain incidents associated with a stressful event for a specific period after the event. In the generalized type, the individual has amnesia for his or her identity and total life history. Cognitive Level: Application Integrated Process: Assessment 11. Neurological tests have ruled out pathology in a clients sudden lower-extremity paralysis. Which nursing care should be included for this client? 1. Deal with physical symptoms in a detached manner. 2. Challenge the validity of physical symptoms. 3. Meet dependency needs until the physical limitations subside. 4. Encourage a discussion of feelings about the lower-extremity problem. ANS: 1 Rationale: The nurse should assist the client in dealing with physical symptoms in a detached manner. This client should be diagnosed with a conversion disorder in which symptoms affect voluntary motor or sensory functioning with or without apparent impairment of consciousness. Examples include paralysis, aphonia, seizures, coordination disturbance, difficulty swallowing, urinary retention, akinesia, blindness, deafness, double vision, anosmia, and hallucinations. Cognitive Level: Application Integrated Process: Implementation 12. Which combination of diagnoses and appropriate pharmacological treatments are correctly matched? 1. SSD: predominantly pain; treated with venlafaxine (Effexor) 2. IAD; treated with cefadroxil (Duricef) 3. Conversion disorder; treated with cyclobenzaprine (Flexeril) 4. Depersonalization-derealization disorder; treated with mometasone (Elocom) ANS: 1 Rationale: The nurse should anticipate that the diagnosis of SSD: predominantly pain can be effectively treated with venlafaxine. Antidepressants are often used with somatic symptom disorder when the predominant symptom is pain. They have been shown to be effective in relieving pain, independent of influences on mood. Cognitive Level: Analysis Integrated Process: Implementation 13. A nurse is reviewing progress notes on a newly admitted client. One progress note reveals that the client purposefully inserted a contaminated catheter into urethra, leading to a urinary tract infection. The nurse recognizes this behavior as characteristic of which mental disorder? 1. Illness anxiety disorder 2. Factitious disorder 3. Functional neurological symptom disorder 4. Depersonalization-derealization disorder ANS: 2 Rationale: Factitious disorders involve conscious, intentional feigning of physical or psychological symptoms. Individuals with factitious disorder pretend to be ill in order to receive emotional care and support commonly associated with the role of patient. Individuals become very inventive in their quest to produce symptoms. Examples include self-inflicted wounds, injection or insertion of contaminated substances, manipulating a thermometer to feign a fever, urinary tract manipulation, and surreptitious use of medications. Cognitive Level: Application Integrated Process: Assessment 14. A nursing instructor is teaching about the DSM-5 diagnosis of depersonalization- derealization disorder (D-DD). Which student statement indicates a need for further instruction? 1. Clients with this disorder can experience emotional and/or physical numbing and a distorted sense of time. 2. Clients with this disorder can experience unreality or detachment with respect to their surroundings. 3. During the course of this disorder, individuals or objects are experienced as dreamlike, foggy, lifeless, or visually distorted. 4. During the course of this disorder, the client is out of touch with reality and is impaired in social, occupational, or other areas of functioning. ANS: 4 Rationale: D-DD is characterized by a temporary change in the quality of self-awareness, which often takes the form of feelings of unreality, changes in body image, feelings of detachment from the environment, or a sense of observing oneself from outside the body. Depersonalization (a disturbance in the perception of oneself) is differentiated from derealization, which describes an alteration in the perception of the external environment. The DSM-5 states that during the depersonalization and/or derealization experiences, reality testing remains intact. This student statement indicates a need for further instruction. Cognitive Level: Application Integrated Process: Evaluation Multiple Response 15. A client is diagnosed with IAD. Which of the following symptoms is the client most likely to exhibit? (Select all that apply.) 1. Obsessive-compulsive behaviors 2. Pseudocyesis 3. Anxiety 4. Flat affect 5. Depression ANS: 1, 3, 5 Rationale: The nurse should expect that a client diagnosed with IAD would exhibit obsessive- compulsive behaviors, anxiety, and depression. Hypochondriasis involves an unrealistic or inaccurate interpretation of physical symptoms or sensations that can lead to preoccupation and fear of having a serious disease. Cognitive Level: Application Integrated Process: Assessment 16. A client is diagnosed with functional neurological symptom disorder (FNSD). Which of the following symptoms is the client most likely to exhibit? (Select all that apply.) 1. Anosmia 2. Anhedonia 3. Akinesia 4. Aphonia 5. Amnesia ANS: 1, 3, 4 Rationale: FNSD can also be termed conversion disorder. Conversion symptoms affect voluntary motor or sensory functioning suggestive of neurological disease. Examples include paralysis, aphonia, seizures, coordination disturbance, difficulty swallowing, urinary retention, akinesia, blindness, deafness, double vision, anosmia, loss of pain sensation, and hallucinations. Cognitive Level: Application Integrated Process: Assessment 17. A client is exhibiting symptoms of generalized amnesia. Which of the following questions should the nurse ask to confirm this diagnosis? (Select all that apply.) 1. Have you taken any new medications recently? 2. Have you recently traveled away from home? 3. Have you recently experienced any traumatic event? 4. Have you ever felt detached from your environment? 5. Have you had any history of memory problems? ANS: 1, 3, 5 Rationale: The nurse should assess the client for possible causes of amnesia, which may include side effects of new medications, experiencing a traumatic event, or having a history of memory problems. Three types of disturbance in recall are identified in the DSM-5: localized, selective, and generalized. In the generalized type, the individual has amnesia for his or her identity and total life history. Cognitive Level: Application Integrated Process: Assessment Fill-in-the-Blank 18. The DSM-5 diagnosis of functional neurological symptom disorder can also be identified as disorder. ANS: conversion Rationale: The DSM-5 diagnosis of functional neurological symptom disorder can also be identified as conversion disorder. Conversion disorder is a loss of or change in body function that cannot be explained by any known medical disorder or pathophysiological mechanism. There is most likely a psychological component involved in the initiation, exacerbation, or perpetuation of the symptom, although it may or may not be obvious or identifiable. Chapter 21. Eating Disorders Multiple Choice 1. Family dynamics are thought to be a major influence in the development of anorexia nervosa. Which statement regarding a clients home environment should a nurse associate with the development of anorexia nervosa? 1. The home environment maintains loose personal boundaries. 2. The home environment places an overemphasis on food. 3. The home environment is overprotective and demands perfection. 4. The home environment condones corporal punishment. ANS: 3 Rationale: The nurse should assess that a home environment that is overprotective and demands perfection may be a major influence in the development of anorexia nervosa. In adolescence, distorted eating patterns may represent a rebellion against the parents viewed by the child as a means of gaining and remaining in control. Cognitive Level: Application Integrated Process: Assessment 2. A clients altered body image is evidenced by claims of feeling fat, even though the client is emaciated. Which is the appropriate outcome criterion for this clients problem? 1. The client will consume adequate calories to sustain normal weight. 2. The client will cease strenuous exercise programs. 3. The client will perceive personal ideal body weight and shape as normal. 4. The client will not express a preoccupation with food. ANS: 3 Rationale: The nurse should identify that the appropriate outcome for this client is to perceive personal ideal body weight and shape as normal. Additional goals include accepting self based on self-attributes instead of appearance and to realize that perfection is unrealistic. Cognitive Level: Application Integrated Process: Planning 3. A nurse is counseling a client diagnosed with bulimia nervosa about the symptom of tooth enamel deterioration. Which explanation for this complication of bulimia nervosa, should the nurse provide? 1. The emesis produced during purging is acidic and corrodes the tooth enamel. 2. Purging causes the depletion of dietary calcium. 3. Food is rapidly ingested without proper mastication. 4. Poor dental and oral hygiene leads to dental caries. ANS: 1 Rationale: The nurse should explain to the client diagnosed with bulimia nervosa that his or her teeth will eventually deteriorate, because the emesis produced during purging is acidic and corrodes the tooth enamel. Excessive vomiting may also lead to dehydration and electrolyte imbalance. Cognitive Level: Application Integrated Process: Implementation 4. A nurse is teaching a client diagnosed with an eating disorder about behavior-modification programs. Why is this intervention the treatment of choice? 1. It helps the client correct a distorted body image. 2. It addresses the underlying client anger. 3. It manages the clients uncontrollable behaviors. 4. It allows clients to maintain control. ANS: 4 Rationale: Behavior-modification programs are the treatment of choice for clients diagnosed with eating disorders, because these programs allow clients to maintain control. Issues of control are central to the etiology of these disorders. Behavior modification techniques function to restore healthy weight. Cognitive Level: Application Integrated Process: Implementation 5. A potential Olympic figure skater collapses during practice and is hospitalized for severe malnutrition. Anorexia nervosa is diagnosed. Which client statement best reflects insight related to this disorder? 1. Skaters need to be thin to improve their daily performance. 2. All the skaters on the team are following an approved 1200-calorie diet. 3. The exercise of skating reduces my appetite but improves my energy level. 4. I am angry at my mother. I can only get her approval when I win competitions. ANS: 4 Rationale: The client reflects insight when referring to feelings toward family dynamics that may have influenced the development of the disease. Families who are overprotective and perfectionistic can contribute to the development of anorexia nervosa. Cognitive Level: Application Integrated Process: Evaluation 6. The family of a client diagnosed with anorexia nervosa becomes defensive when the treatment team calls for a family meeting. Which is the appropriate nursing response? 1. Tell me why this family meeting is causing you to be defensive. All clients are required to participate in two family sessions. 2. Eating disorders have been correlated to certain familial patterns; without addressing these, your childs condition will not improve. 3. Family dynamics are not linked to eating disorders. The meeting is to provide your child with family support. 4. Clients diagnosed with anorexia nervosa are part of the family system, and any alteration in family processes needs to be addressed. ANS: 2 Rationale: The nurse should educate the family on the correlation between certain familial patterns and anorexia nervosa. Families engaging in conflict avoidance and struggling with issues of power and control may contribute to the development of anorexia nervosa. Cognitive Level: Application Integrated Process: Implementation 7. A client diagnosed with bulimia nervosa has been attending a mental health clinic for several months. Which factor should a nurse identify as an appropriate indicator of a positive client behavioral change? 1. The client gained two pounds in one week. 2. The client focused conversations on nutritious food. 3. The client demonstrated healthy coping mechanisms that decreased anxiety. 4. The client verbalized an understanding of the etiology of the disorder. ANS: 3 Rationale: The nurse should identify that a client who demonstrates healthy coping mechanisms to decrease anxiety indicates a positive behavioral change. Stress and anxiety can increase bingeing, which is followed by inappropriate compensatory behavior. Cognitive Level: Application Integrated Process: Evaluation 8. A morbidly obese client is prescribed an anorexiant medication. The nurse should expect to teach the client about which medication? 1. Phentermine (Mirapront) 2. Dexfenfluramine (Redux) 3. Sibutramine (Meridia) 4. Pemoline (Cylert) ANS: 1 Rationale: The nurse should teach the client that phentermine is an anorexiant medication prescribed for morbidly obese clients. Phentermine works on the hypothalamus to stimulate the adrenal glands to release norepinephrine, a neurotransmitter that signals a fight-or-flight response, reducing hunger. Dexfenfluramine has been removed from the market because of its association with serious heart and lung disease. Several deaths have been associated with the use of sibutramine by high-risk clients. Based on pressure from the FDA, the manufacturer issued a recall of the drug in October 2010. Withdrawal from anorexiants can result in rebound weight gain, lethargy, and depression. Cognitive Level: Application Integrated Process: Implementation 9. A nurse is attempting to differentiate between the symptoms of anorexia nervosa and the symptoms of bulimia. Which statement delineates the difference between these two disorders? 1. Clients diagnosed with anorexia nervosa experience extreme nutritional deficits, whereas clients diagnosed with bulimia nervosa do not. 2. Clients diagnosed with bulimia nervosa experience amenorrhea, whereas clients diagnosed with anorexia nervosa do not. 3. Clients diagnosed with bulimia nervosa experience hypotension, edema, and lanugo, whereas clients diagnosed with anorexia nervosa do not. 4. Clients diagnosed with anorexia nervosa have eroded tooth enamel, whereas clients diagnosed with bulimia nervosa do not. ANS: 1 Rationale: The nurse should understand that clients diagnosed with anorexia nervosa experience nutritional deficits, whereas clients diagnosed with bulimia do not. Anorexia is characterized by a morbid fear of obesity and often results in low caloric and nutritional intake. Bulimia is characterized by episodic, rapid consumption of large quantities of food followed by purging. Cognitive Level: Application Integrated Process: Assessment 10. A client diagnosed with a history of anorexia nervosa comes to an outpatient clinic after being medically cleared. The client states, My parents watch me like a hawk and never let me out of their sight. Which nursing diagnosis would take priority at this time? 1. Altered nutrition less than body requirements 2. Altered social interaction 3. Impaired verbal communication 4. Altered family processes ANS: 4 Rationale: The nurse should determine that once the client has been medically cleared, the diagnosis of altered family process should take priority. Clients diagnosed with anorexia nervosa have a need to control and feel in charge of their own treatment choices. Behavioral-modification therapy allows the client to maintain control of eating. Cognitive Level: Analysis Integrated Process: Diagnosis Multiple Response 11. A nurse should identify topiramate (Topamax) as the drug of choice for which of the following conditions? (Select all that apply.) 1. Binge eating with a diagnosis of obesity 2. Bingeing and purging with a diagnosis of bulimia nervosa 3. Weight loss with a diagnosis of anorexia nervosa 4. Amenorrhea with a diagnosis of anorexia nervosa 5. Emaciation with a diagnosis of bulimia nervosa ANS: 1, 2 Rationale: The nurse should identify that topiramate is the drug of choice when treating binge eating with a diagnosis of obesity or bingeing and purging with a diagnosis of bulimia nervosa. Topiramate is an anticonvulsant that produces a significant decline in binge frequency and reduction in body weight. Cognitive Level: Application Integrated Process: Assessment 12. A nursing instructor is teaching about the DSM-5 criteria for the diagnosis of binge-eating disorder. Which of the following student statements indicates that further instruction is needed? (Select all that apply.) 1. In this disorder, binge eating occurs exclusively during the course of bulimia nervosa. 2. In this disorder, binge eating occurs, on average, at least once a week for three months. 3. In this disorder, binge eating occurs, on average, at least two days a week for six months. 4. In this disorder, distress regarding binge eating is present. 5. In this disorder, distress regarding binge eating is absent. ANS: 1, 3, 5 Rationale: According to the DSM-5 criteria for the diagnosis of binge-eating disorder, binge eating should not occur exclusively during the course of anorexia nervosa or bulimia nervosa. The new time frame criteria in the DSM-5 states that binge eating must occur, on average, at least once a week for three months not two days a week for six months. The DSM-5 criteria states that distress regarding binge eating would be present. Cognitive Level: Application Integrated Process: Assessment 13. Which of the following would contribute to a clients excessive weight gain? (Select all that apply.) 1. A hypothalamus lesion 2. Hyperthyroidism 3. Diabetes mellitus 4. Cushings disease 5. Low levels of serotonin ANS: 1, 3, 4 Rationale: Lesions in the appetite and satiety centers in the hypothalamus may contribute to overeating and lead to obesity. Hypothyroidism, not hyperthyroidism, is a problem that interferes with basal metabolism and may lead to weight gain. Weight gain can also occur in response to the decreased insulin production of diabetes mellitus and the increased cortisone production of Cushings disease. New evidence also exists to indicate that low levels of the neurotransmitter serotonin may play a role in compulsive eating. Cognitive Level: Application Integrated Process: Assessment Fill-in-the-Blank 14. The diagnosis of includes the symptoms of gross distortion of body image, preoccupation with food, and refusal to eat. ANS: anorexia nervosa Rationale: Anorexia nervosa is characterized by a morbid fear of obesity. Symptoms include gross distortion of body image, preoccupation with food, and refusal to eat. Cognitive Level: Application Integrated Process: Assessment 15. The episodic, uncontrolled, compulsive, rapid ingestion of large quantities of food over a short period of time is termed . ANS: bingeing Rationale: The episodic, uncontrolled, compulsive, rapid ingestion of large quantities of food over a short period of time is termed bingeing. Bingeing is a classic symptom of the eating disorder defined as bulimia nervosa. Cognitive Level: Application Integrated Process: Assessment 16. To rid the body of excessive calories, a client diagnosed with bulimia nervosa may engage in behaviors, which include self-induced vomiting, or the misuse of laxatives, diuretics, or enemas. ANS: purging Rationale: To rid the body of excessive calories, a client diagnosed with bulimia nervosa may engage in purging behaviors, which include self-induced vomiting or the misuse of laxatives, diuretics, or enemas. In addition to these behaviors, other inappropriate compensatory behaviors, such as fasting or excessive exercise may be noted. Chapter 22. Personality Disorders Multiple Choice 1. During an assessment interview, a client diagnosed with antisocial personality disorder spits, curses, and refuses to answer questions. Which is the appropriate nursing response to this behavior? 1. You are very disrespectful. You need to learn to control yourself. 2. I understand that you are angry, but this behavior will not be tolerated. 3. What behaviors could you modify to improve this situation? 4. What anti-personality disorder medications have helped you in the past? ANS: 2 Rationale: The appropriate nursing response is to reflect the clients feeling while setting firm limits on behavior. Clients diagnosed with antisocial personality disorder have a low tolerance for frustration, see themselves as victims, and use projection as a primary ego defense mechanism. Cognitive Level: Application Integrated Process: Implementation 2. At 11:00 p.m. a client diagnosed with antisocial personality disorder demands to phone a lawyer to file for a divorce. Unit rules state that no phone calls are permitted after 10:00 p.m. Which nursing response is most appropriate? 1. Go ahead and use the phone. I know this pending divorce is stressful. 2. You know better than to break the rules. Im surprised at you. 3. It is after the 10:00 p.m. phone curfew. You will be able to call tomorrow. 4. A divorce shouldnt be considered until you have had a good nights sleep. ANS: 3 Rationale: The most appropriate response by the staff is to restate the unit rules in a calm, assertive manner. The nurse can encourage the client to verbalize frustration while maintaining an accepting attitude. The nurse may also help the client to identify the true source of frustration. Cognitive Level: Application Integrated Process: Implementation 3. A client diagnosed with paranoid personality disorder becomes violent on a unit. Which nursing intervention is most appropriate? 1. Provide objective evidence that reasons for violence are unwarranted. 2. Initially restrain the client to maintain safety. 3. Use clear, calm statements and a confident physical stance. 4. Empathize with the clients paranoid perceptions. ANS: 3 Rationale: The most appropriate nursing intervention is to use clear, calm statements and to assume a confident physical stance. A calm attitude provides the client with a feeling of safety and security. It may also be beneficial to have sufficient staff on hand to present a show of strength. Cognitive Level: Application Integrated Process: Implementation 4. A client diagnosed with borderline personality disorder brings up a conflict with the staff in a community meeting and develops a following of clients who unreasonably demand modification of unit rules. How can the nursing staff best handle this situation? 1. Allow the clients to apply the democratic process when developing unit rules. 2. Maintain consistency of care by open communication to avoid staff manipulation. 3. Allow the client spokesman to verbalize concerns during a unit staff meeting. 4. Maintain unit order by the application of autocratic leadership. ANS: 2 Rationale: The nursing staff can best handle this situation by maintaining consistency of care by open communication to avoid staff manipulation. Clients with borderline personality disorder can exhibit negative patterns of interaction, such as clinging and distancing, splitting, manipulation, and self-destructive behaviors. Cognitive Level: Application Integrated Process: Implementation 5. Which nursing approach should be used to maintain a therapeutic relationship with a client diagnosed with borderline personality disorder? 1. Being firm, consistent, and empathic, while addressing specific client behaviors 2. Promoting client self-expression by implementing laissez-faire leadership 3. Using authoritative leadership to help clients learn to conform to society norms 4. Overlooking inappropriate behaviors to avoid providing secondary gains ANS: 1 Rationale: The best nursing approach when working with a client diagnosed with borderline personality disorder is to be firm, consistent, and empathetic while addressing specific client behaviors. Individuals with borderline personality disorder always seem to be in a state of crisis and can often have negative patterns of interaction, such as manipulation and splitting. Cognitive Level: Application Integrated Process: Implementation 6. Which adult client should a nurse identify as exhibiting the characteristics of a dependent personality disorder? 1. A physically healthy client who is dependent on meeting social needs by contact with 15 cat 2. A physically healthy client who has a history of depending on intense relationships to meet basic needs 3. A physically healthy client who lives with parents and depends on public transportation 4. A physically healthy client who is serious, inflexible, perfectionistic, lacks spontaneity, and depends on rules to provide security ANS: 3 Rationale: A physically healthy adult client who lives with parents and depends on public transportation exhibits signs of dependent personality disorder. Dependent personality disorder is characterized by a pervasive and excessive need to be taken care of that leads to submissive and clinging behaviors. Cognitive Level: Application Integrated Process: Assessment 7. A client expresses low self-worth, has much difficulty making decisions, avoids positions of responsibility, and has a behavioral pattern of suffering in silence. Which statement best explains the etiology of this clients personality disorder? 1. Childhood nurturance was provided from many sources, and independent behaviors were encouraged. 2. Childhood nurturance was provided exclusively from one source, and independent behaviors were discouraged. 3. Childhood nurturance was provided exclusively from one source, and independent behaviors were encouraged. 4. Childhood nurturance was provided from many sources, and independent behaviors were discouraged. Ans: 2 Rationale: The behaviors presented in the question represent symptoms of dependent personality disorder. Nurturance provided from one source and discouragement of independent behaviors can contribute to the development of this personality disorder. Dependent behaviors may be rewarded by a parent who is overprotective and discourages autonomy. Cognitive Level: Analysis Nursing Process: Assessment 8. Family members of a client ask the nurse to explain the difference between schizoid and avoidant personality disorders. Which is the appropriate nursing response? 1. Clients diagnosed with avoidant personality disorder desire intimacy but fear it, and clients diagnosed with schizoid personality disorder prefer to be alone. 2. Clients diagnosed with schizoid personality disorder exhibit delusions and hallucinations, while clients diagnosed with avoidant personality disorder do not. 3. Clients diagnosed with avoidant personality disorder are eccentric, and clients diagnosed with schizoid personality disorder are dull and vacant. 4. Clients diagnosed with schizoid personality disorder have a history of psychosis, while clients diagnosed with avoidant personality disorder remain based in reality. Ans: 1 Rationale: The nurse should educate the family that clients diagnosed with avoidant personality disorder desire intimacy but fear it, while clients diagnosed with schizoid personality disorder prefer to be alone. Schizoid personality disorder is characterized by a profound deficit in the ability to form personal relationships. Clients diagnosed with schizoid personality disorder may exhibit odd and eccentric behaviors but not to the extent of psychosis. Cognitive Level: Analysis Nursing Process: Assessment 9. Which nursing diagnosis should a nurse identify as appropriate when working with a client diagnosed with schizoid personality disorder? 1. Altered thought processes R/T increased stress 2. Risk for suicide R/T loneliness 3. Risk for violence: directed toward others R/T paranoid thinking 4. Social isolation R/T inability to relate to others ANS: 4 Rationale: An appropriate nursing diagnosis when working with a client diagnosed with schizoid personality disorder is social isolation R/T inability to relate to others. Clients diagnosed with schizoid personality disorder appear cold, aloof, and indifferent to others. They prefer to work in isolation and are not sociable. Cognitive Level: Analysis Integrated Process: Diagnosis 10. Looking at a slightly bleeding paper cut, the client screams, Somebody help me quick! Im bleeding. Call 911! A nurse should identify this behavior as characteristic of which personality disorder? 1. Schizoid personality disorder 2. Obsessive-compulsive personality disorder 3. Histrionic personality disorder 4. Paranoid personality disorder ANS: 3 Rationale: The nurse should identify this behavior as characteristic of histrionic personality disorder. Individuals with this disorder tend to be self-dramatizing, attention seeking, over gregarious, and seductive. Cognitive Level: Analysis Integrated Process: Evaluation 11. When planning care for a client diagnosed with borderline personality disorder, which self- harm behavior should a nurse expect the client to exhibit? 1. The use of highly lethal methods to commit suicide 2. The use of suicidal gestures to elicit a rescue response from others 3. The use of isolation and starvation as suicidal methods 4. The use of self-mutilation to decrease endorphins in the body ANS: 2 Rationale: The nurse should expect that a client diagnosed with borderline personality disorder may use suicidal gestures to elicit a rescue response from others. Repetitive, self-mutilating behaviors are common in borderline personality disorders that result from feelings of abandonment following separation from significant others. Cognitive Level: Application Integrated Process: Planning 12. A nurse tells a client that the nursing staff will start alternating weekend shifts. Which response should a nurse identify as characteristic of clients diagnosed with obsessive-compulsive personality disorder? 1. You really dont have to go by that schedule. Id just stay home sick. 2. There has got to be a hidden agenda behind this schedule change. 3. Who do you think you are? I expect to interact with the same nurse every Saturday. 4. You cant make these kinds of changes! Isnt there a rule that governs this decision? ANS: 4 Rationale: The nurse should identify that a client with obsessive-compulsive personality disorder would have a difficult time accepting changes. This disorder is characterized by inflexibility and lack of spontaneity. Individuals with this disorder are very serious, formal, over-disciplined, perfectionistic, and preoccupied with rules. Cognitive Level: Application Integrated Process: Assessment 13. Which reaction to a compliment from another client should a nurse identify as a typical response from a client diagnosed with avoidant personality disorder? 1. Interpreting the compliment as a secret code used to increase personal power 2. Feeling the compliment was well deserved 3. Being grateful for the compliment but fearing later rejection and humiliation 4. Wondering what deep meaning and purpose is attached to the compliment ANS: 3 Rationale: The nurse should identify that a client diagnosed with avoidant personality disorder would be grateful for the compliment but would fear later rejection and humiliation. Individuals diagnosed with avoidant personality disorder are extremely sensitive to rejection and are often awkward and uncomfortable in social situations. Cognitive Level: Application Integrated Process: Evaluation 14. Which factors differentiate a client diagnosed with social phobia from a client diagnosed with schizoid personality disorder? 1. Clients diagnosed with social phobia are treated with cognitive behavioral therapy, whereas clients diagnosed with schizoid personality disorder need medications. 2. Clients diagnosed with schizoid personality disorder experience anxiety only in social settings, whereas clients diagnosed with social phobia experience generalized anxiety. 3. Clients diagnosed with social phobia avoid attending birthday parties, whereas clients diagnosed with schizoid personality disorder would isolate self on a continual basis. 4. Clients diagnosed with schizoid personality disorder avoid attending birthday parties, whereas clients diagnosed with social phobia would isolate self on a continual basis. ANS: 3 Rationale: A client diagnosed with schizoid personality disorder exhibits a profound deficit in the ability to form personal relationships. Clients diagnosed with schizoid personality disorder prefer being alone to being with others and avoid social situations, social contacts, and activities. Cognitive Level: Analysis Integrated Process: Assessment 15. Which client symptoms should lead a nurse to suspect a diagnosis of obsessive-compulsive personality disorder? 1. The client experiences unwanted, intrusive, and persistent thoughts. 2. The client experiences unwanted, repetitive behavior patterns. 3. The client experiences inflexibility and lack of spontaneity when dealing with others. 4. The client experiences obsessive thoughts that are externally imposed. ANS: 3 Rationale: The nurse should suspect a diagnosis of obsessive-compulsive personality disorder when a client experiences inflexibility and lack of spontaneity. Individuals with this disorder are very serious, formal, and have difficulty expressing emotions. They are perfectionistic and preoccupied with rules. Cognitive Level: Application Integrated Process: Assessment 16. Which client is a nurse most likely to admit to an inpatient facility for self-destructive behaviors? 1. A client diagnosed with antisocial personality disorder 2. A client diagnosed with borderline personality disorder 3. A client diagnosed with schizoid personality disorder 4. A client diagnosed with paranoid personality disorder ANS: 2 Rationale: The nurse should expect that a client diagnosed with borderline personality disorder would be most likely to be admitted to an inpatient facility for self-destructive behaviors. Clients diagnosed with this disorder often exhibit repetitive, self-mutilating behaviors. Most gestures are designed to elicit a rescue response. Cognitive Level: Application Integrated Process: Assessment 17. When planning care for clients diagnosed with personality disorders, what should be the goal of treatment? 1. To stabilize the clients pathology by using the correct combination of psychotropic medications 2. To change the characteristics of the dysfunctional personality 3. To reduce personality trait inflexibility that interferes with functioning and relationships 4. To decrease the prevalence of neurotransmitters at receptor sites ANS: 3 Rationale: The goal of treatment for clients diagnosed with personality disorders should be to reduce inflexibility of personality traits that interfere with functioning and relationships. Personality disorders are often difficult and, in some cases, seem impossible to treat. There are no psychotropic medications approved specifically for the treatment of personality disorders. Cognitive Level: Application Integrated Process: Planning 18. Which client situation would reflect the impulsive behavior that is commonly associated with borderline personality disorder? 1. As the day-shift nurse leaves the unit, the client suddenly hugs the nurses arm and whispers, The night nurse is evil. You have to stay. 2. As the day-shift nurse leaves the unit, the client suddenly hugs the nurses arm and states, I will be up all night if you dont stay with me. 3. As the day-shift nurse leaves the unit, the client suddenly hugs the nurses arm, yelling, Please dont go! I cant sleep without you being here. 4. As the day-shift nurse leaves the unit, the client suddenly shows the nurse a bloody arm and states, I cut myself because you are leaving me. Ans: 4 Rationale: The client who states, I cut myself because you are leaving me reflects impulsive behavior that is commonly associated with borderline personality disorder. Repetitive, self- mutilating behaviors are common in clients diagnosed with borderline personality disorders that result from feelings of abandonment following separation from significant others. Cognitive Level: Application Nursing Process: Evaluation 19. Which nursing diagnosis should be prioritized when providing nursing care to a client diagnosed with paranoid personality disorder? 1. Risk for violence: directed toward others R/T paranoid thinking 2. Risk for suicide R/T altered thought 3. Altered sensory perception R/T increased levels of anxiety 4. Social isolation R/T inability to relate to others Ans: 1 Rationale: The priority nursing diagnosis for a client diagnosed with paranoid personality disorder should be risk for violence: directed toward others R/T paranoid thinking. Clients diagnosed with paranoid personality disorder have a pervasive distrust and suspiciousness of others that result in a constant threat readiness. They are often tense and irritable, which increases the likelihood of violent behavior. Cognitive Level: Analysis Nursing Process: Diagnosis 20. From a behavioral perspective, which nursing intervention is appropriate when caring for a client diagnosed with borderline personality disorder? 1. Seclude the client when inappropriate behaviors are exhibited. 2. Contract with the client to reinforce positive behaviors with unit privileges. 3. Teach the purpose of anti-anxiety medications to improve medication compliance. 4. Encourage the client to journal feelings to improve awareness of abandonment issues. Ans: 2 Rationale: The most appropriate nursing intervention from a behavioral perspective is to contract with the client to reinforce positive behaviors with unit privileges. Behavioral strategies offer reinforcement for positive change. Cognitive Level: Application Nursing Process: Implementation 21. A highly emotional client presents at an outpatient clinic appointment and states, My dead husband returned to me during a sance. Which personality disorder should a nurse associate with this behavior? 1. Obsessive-compulsive personality disorder 2. Schizotypal personality disorder 3. Narcissistic personality disorder 4. Borderline personality disorder ANS: 2 Rationale: The nurse should associate schizotypal personality disorder with this behavior. The behaviors of people diagnosed with schizotypal personality disorder are odd and eccentric but do not decompensate to the level of schizophrenia. Cognitive Level: Application Integrated Process: Assessment 22. A nursing instructor is teaching students about clients diagnosed with histrionic personality disorder and the quality of their relationships. Which student statement indicates that learning has occurred? 1. Their dramatic style tends to make their interpersonal relationships quite interesting and fulfilling. 2. Their interpersonal relationships tend to be shallow and fleeting, serving their dependency needs. 3. They tend to develop few relationships because they are strongly independent but generally maintain deep affection. 4. They pay particular attention to details, which can interfere with the development of relationships. ANS: 2 Rationale: The instructor should evaluate that learning has occurred when the student describes clients diagnosed with histrionic personality disorder as having relationships that are shallow and fleeting. These types of relationships tend to serve their dependency needs. Cognitive Level: Application Integrated Process: Evaluation 23. During an interview, which client statement should indicate to a nurse a potential diagnosis of schizotypal personality disorder? 1. I dont have a problem. My family is inflexible, and relatives are out to get me. 2. I am so excited about working with you. Have you noticed my new nail polish, Ruby Red Roses? 3. I spend all my time tending my bees. I know a whole lot of information about bees. 4. I am getting a message from the beyond that we have been involved with each other in a previous life. ANS: 4 Rationale: The nurse should assess that a client who states that he or she is getting a message from beyond indicates a potential diagnosis of schizotypal personality disorder. Individuals with schizotypal personality disorder are aloof and isolated and behave in a bland and apathetic manner. The person experiences magical thinking, ideas of reference, illusions, and depersonalization as part of daily life. Cognitive Level: Application Integrated Process: Assessment 24. Which nursing diagnosis should be prioritized when providing nursing care to a client diagnosed with avoidant personality disorder? 1. Risk for violence: directed toward others R/T paranoid thinking 2. Risk for suicide R/T altered thought 3. Altered sensory perception R/T increased levels of anxiety 4. Social isolation R/T inability to relate to others ANS: 4 Rationale: The priority nursing diagnosis for a client diagnosed with avoidant personality disorder should be social isolation R/T inability to relate to others. These clients avoid close or romantic relationships, interpersonal attachments, and intimate sexual relationships. Cognitive Level: Analysis Integrated Process: Diagnosis Multiple Response 25. A nurse is admitting a client with a new diagnosis of a personality disorder. Which of the following would make the nurse question this diagnosis? (Select all that apply.) 1. The client has been diagnosed with sickle cell anemia. 2. The client has an inflated self-appraisal and feels a sense of entitlement. 3. The client has a history of a substance use disorder. 4. The client is odd and eccentric but not delusional. 5. The client has an intellectual developmental disorder. ANS: 1, 3, 5 Rationale: The DSM-5 states that impairments in personality functioning and the individuals personality trait expression are not better understood as normative for the individuals developmental stage or sociocultural environment. The impairments in personality functioning and the individuals personality trait expression are not solely due to the direct physiological effects of a substance (e.g., a drug of abuse, medication) or a general medical condition (e.g., severe head trauma). The nurse would question the diagnosis of a personality disorder in a client with sickle cell anemia, substance use disorder, or an intellectual developmental disorder. Cognitive Level: Application Integrated Process: Evaluation 26. Which statements represent positive outcomes for clients diagnosed with narcissistic personality disorder? (Select all that apply.) 1. The client will relate one empathetic statement to another client in group by day two. 2. The client will identify one personal limitation by day one. 3. The client will acknowledge one strength that another client possesses by day two. 4. The client will list four personal strengths by day three. 5. The client will list two lifetime achievements by discharge. ANS: 1, 2, 3 Rationale: The nurse should determine that appropriate outcomes for a client diagnosed with narcissistic personality disorder include relating empathetic statements to other clients, identifying one personal limitation, and acknowledging one strength in another client. Narcissistic personality disorder is characterized by an exaggerated sense of self-worth, a lack of empathy, and exploitation of others. Cognitive Level: Application Integrated Process: Planning 27. A nurse is caring for a client diagnosed with antisocial personality disorder. Which factors should the nurse consider when planning this clients care? (Select all that apply.) 1. This client has personality traits that are deeply ingrained and difficult to modify. 2. This client needs medication to treat the underlying physiological pathology. 3. This client uses manipulation, making the implementation of treatment problematic. 4. This client has poor impulse control that hinders compliance with a plan of care. 5. This client is likely to have secondary diagnoses of substance abuse and depression. ANS: 1, 3, 4, 5 Rationale: The nurse should consider that individuals diagnosed with antisocial personality disorders have deeply ingrained personality traits, use manipulation, have poor impulse control, and often have secondary diagnoses of substance abuse or depression. Cognitive Level: Application Integrated Process: Planning 28. A client is being assessed for antisocial personality disorder. According to the DSM-5, which of the following symptoms must the client meet in order to be assigned this diagnosis? (Select all that apply.) 1. Ego-centrism and goal setting based on personal gratification. 2. Incapacity for mutually intimate relationships. 3. Frequent feelings of being down miserable and/or hopeless. 4. Disregard for and failure to honor financial and other obligations. 5, Intense feelings of nervousness, tenseness, or panic. ANS: 1, 2, 4 Rationale: The essential features of a personality disorder are impairments in personality (self and interpersonal) functioning and the presence of pathological personality traits. Pathological personality traits of antagonism and disinhibition must occur in order to meet the criteria for the diagnosis of antisocial personality disorder. Frequent feelings of being down, miserable, and/or hopeless and intense feelings of nervousness, tenseness, or panic are characteristics of the pathological personality trait domain of negative affectivity. This domain is listed by the DSM-5 for the diagnosis of borderline personality disorder, not antisocial personality disorder. Cognitive Level: Application Integrated Process: Assessment Fill-in-the-Blank 29. personality disorder is characterized by a profound defect in the ability to form personal relationships or to respond to others in any meaningful emotional way. ANS: Schizoid Rationale: Persons diagnosed with schizoid personality disorder have a profound defect in the ability to form personal relationships or to respond to others in any meaningful emotional way. These individuals display a life-long pattern of social withdrawal, and their discomfort with human interaction is apparent. Cognitive Level: Application Integrated Process: Assessment 30. personality disorder is characterized by colorful, dramatic, and extraverted behavior in excitable, emotional people. ANS: Histrionic Rationale: Histrionic personality disorder is characterized by colorful, dramatic, and extraverted behavior in excitable, emotional people. They have difficulty maintaining long-lasting relationships, although they require constant affirmation of approval and acceptance from others. Cognitive Level: Application Integrated Process: Assessment 31. personality disorder is characterized by a pervasive and excessive need to be taken care of that leads to submissive and clinging behavior and fears of separation. ANS: Dependent Rationale: Dependent personality disorder is characterized by a pervasive and excessive need to be taken care of that leads to submissive and clinging behavior and fears of separation. These characteristics are evident in the tendency to allow others to make decisions, to feel helpless when alone, to act submissively, to subordinate needs to others, to tolerate mistreatment by others, to demean oneself to gain acceptance, and to fail to function adequately in situations that require assertive or dominant behavior. Cognitive Level: Application Integrated Process: Assessment 32. personality disorder is a pervasive distrust and suspiciousness of others, such that their motives are interpreted as malevolent. ANS: Paranoid Rationale: Paranoid personality disorder is a pervasive distrust and suspiciousness of others such that their motives are interpreted as malevolent. This disorder begins in early adulthood and presents in a variety of contexts. Chapter 23. Children and Adolescents Multiple Choice 1. Which developmental characteristic should a nurse identify as typical of a client diagnosed with severe intellectual developmental disorder (IDD)? 1. The client can perform some self-care activities independently. 2. The client has more advanced speech development. 3. Other than possible coordination problems, the clients psychomotor skills are not affected. 4. The client communicates wants and needs by acting out behaviors. ANS: 4 Rationale: The nurse should identify that a client diagnosed with severe IDD may communicate wants and needs by acting out behaviors. Severe IDD indicates an IQ between 20 and 34. Individuals diagnosed with severe IDD require complete supervision and have minimal verbal skills and poor psychomotor development. Cognitive Level: Application Integrated Process: Assessment 2. Which nursing intervention related to self-care would be most appropriate for a teenager diagnosed with moderate IDD? 1. Meeting all of the clients self-care needs to avoid injury to the client 2. Providing simple directions and praising clients independent self-care efforts 3. Avoid interfering with the clients self-care efforts in order to promote autonomy 4. Encouraging family to meet the clients self-care needs to promote bonding ANS: 2 Rationale: Providing simple directions and praise is an appropriate intervention for a teenager diagnosed with moderate IDD. Individuals with moderate mental retardation can perform some activities independently and may be capable of academic skill to a second-grade level. Cognitive Level: Application Integrated Process: Implementation 3. A child has been diagnosed with autistic spectrum disorder. The distraught mother cries out, Im such a terrible mother. What did I do to cause this? Which nursing response is most appropriate? 1. Researchers really dont know what causes autistic spectrum disorder, but the relationship between autistic disorder and fetal alcohol syndrome is being explored. 2. Poor parenting doesnt cause autistic spectrum disorder. Research has shown that abnormalities in brain structure or function are to blame. This is beyond your control. 3. Research has shown that the mother appears to play a greater role in the development of autistic spectrum disorder than the father. 4. Lack of early infant bonding with the mother has shown to be a cause of autistic spectrum disorder. Did you breastfeed or bottle-feed? ANS: 2 Rationale: The most appropriate response by the nurse is to explain to the parent that autistic spectrum disorder is believed to be caused by abnormalities in brain structure or function, not poor parenting. Autism occurs in approximately 11.3 per 1,000 children and is about 4.5 times more likely to occur in boys than girls. Cognitive Level: Application Integrated Process: Implementation 4. In planning care for a child diagnosed with autistic spectrum disorder, which would be a realistic client outcome? 1. The client will communicate all needs verbally by discharge. 2. The client will participate with peers in a team sport by day four. 3. The client will establish trust with at least one caregiver by day five. 4. The client will perform most self-care tasks independently. ANS: 3 Rationale: The most realistic client outcome for a child diagnosed with autistic spectrum disorder is for the client to establish trust with at least one caregiver. Trust should be evidenced by facial responsiveness and eye contact. This outcome relates to the nursing diagnosis impaired social interaction. Cognitive Level: Application Integrated Process: Planning 5. After an adolescent diagnosed with attention deficit-hyperactivity disorder (ADHD) begins methylphenidate (Ritalin) therapy, a nurse notes that the adolescent loses 10 pounds in a 2-month period. What is the best explanation for this weight loss? 1. The pharmacological action of Ritalin causes a decrease in appetite. 2. Hyperactivity seen in ADHD causes increased caloric expenditure. 3. Side effects of Ritalin cause nausea, and, therefore, caloric intake is decreased. 4. Increased ability to concentrate allows the client to focus on activities rather than food. ANS: 1 Rationale: The pharmacological action of Ritalin causes a decrease in appetite, which often leads to weight loss. Methylphenidate is a central nervous symptom stimulant that serves to increase attention span, control hyperactive behaviors, and improve learning ability. Cognitive Level: Comprehension Integrated Process: Evaluation 6. A nurse assesses an adolescent client diagnosed with conduct disorder who, at the age of 8, was sentenced to juvenile detention. How should the nurse interpret this assessment data? 1. Childhood-onset conduct disorder is more severe than the adolescent-onset type, and these individuals likely develop antisocial personality disorder in adulthood. 2. Childhood-onset conduct disorder is caused by a difficult temperament, and the child is likely to outgrow these behaviors by adulthood. 3. Childhood-onset conduct disorder is diagnosed only when behaviors emerge before the age of 5, and, therefore, improvement is likely. 4. Childhood-onset conduct disorder has no treatment or cure, and children diagnosed with this disorder are likely to develop progressive oppositional defiant disorder. ANS: 1 Rationale: The nurse should determine that childhood-onset conduct disorder is more severe than adolescent-onset type. These individuals are likely to develop antisocial personality disorder in adulthood. Individuals with this subtype are usually boys and frequently display physical aggression and have disturbed peer relationships. Cognitive Level: Application Integrated Process: Analysis 7. Which finding should a nurse expect when assessing a child diagnosed with separation anxiety disorder? 1. The child has a history of antisocial behaviors. 2. The childs mother is diagnosed with an anxiety disorder. 3. The child previously had an extroverted temperament. 4. The childs mother and father have an inconsistent parenting style. ANS: 2 Rationale: The nurse should expect to find a mother diagnosed with an anxiety disorder when assessing a child with separation anxiety. Some parents instill anxiety in their children by being overprotective or by exaggerating dangers. Research studies speculate that there is a hereditary influence in the development of separation anxiety disorder. Cognitive Level: Comprehension Integrated Process: Assessment 8. A child has been recently diagnosed with mild IDD. What information about this diagnosis should the nurse include when teaching the childs mother? 1. Children with mild IDD need constant supervision. 2. Children with mild IDD develop academic skills up to a sixth-grade level. 3. Children with mild IDD appear different from their peers. 4. Children with mild IDD have significant sensory-motor impairment. ANS: 2 Rationale: The nurse should inform the childs mother that children with mild IDD develop academic skills up to a sixth-grade level. Individuals with mild IDD are capable of independent living, capable of developing social skills, and have normal psychomotor skills. Cognitive Level: Application Integrated Process: Teaching/learning 9. A nursing instructor is teaching about the developmental characteristics of clients diagnosed with moderate intellectual developmental disorder (IDD). Which student statement indicates that further instruction is needed? 1. These clients can work in a sheltered workshop setting. 2. These clients can perform some personal care activities. 3. These clients may have difficulties relating to peers. 4. These clients can successfully complete elementary school. ANS: 4 Rationale: The nursing student needs further instruction about moderate IDD, because individuals diagnosed with moderate IDD are capable of academic skill up to a second-grade level. Moderate IDD reflects an IQ range of 35 to 49. Cognitive Level: Application Integrated Process: Evaluation 10. A preschool child is admitted to a psychiatric unit with the diagnosis autistic spectrum disorder. To help the child feel more secure on the unit, which intervention should a nurse include in this clients plan of care? 1. Encourage and reward peer contact. 2. Provide consistent caregivers. 3. Provide a variety of safe daily activities. 4. Maintain close physical contact throughout the day. ANS: 2 Rationale: The nurse should provide consistent caregivers as part of the plan of care for a child diagnosed with autistic spectrum disorder. Children diagnosed with autistic spectrum disorder have an inability to trust. Providing consistent caregivers allows the client to develop trust and a sense of security. Cognitive Level: Application Integrated Process: Implementation 11. A preschool child diagnosed with autistic spectrum disorder has been engaging in constant head-banging behavior. Which nursing intervention is appropriate? 1. Place client in restraints until the aggression subsides. 2. Sedate the client with neuroleptic medications. 3. Hold clients head steady and apply a helmet. 4. Distract the client with a variety of games and puzzles. ANS: 3 Rationale: The most appropriate intervention for head banging is to hold the clients head steady and apply a helmet. The helmet is the least restrictive intervention and will serve to protect the clients head from injury. Cognitive Level: Application Integrated Process: Implementation 12. When planning care for a client, which medication classification should a nurse recognize as effective in the treatment of Tourettes syndrome? 1. Neuroleptic medications 2. Anti-manic medications 3. Tricyclic antidepressant medications 4. Monoamine oxidase inhibitor medications ANS: 1 Rationale: The nurse should recognize that neuroleptic (antipsychotic) medications are effective in the treatment of Tourettes syndrome. These medications are used to reduce the severity of tics and are most effective when combined with psychosocial therapy. Cognitive Level: Application Integrated Process: Planning 13. Which behavioral approach should a nurse use when caring for children diagnosed with disruptive behavior disorders? 1. Involving parents in designing and implementing the treatment process 2. Reinforcing positive actions to encourage repetition of desirable behaviors 3. Providing opportunities to learn appropriate peer interactions 4. Administering psychotropic medications to improve quality of life ANS: 2 Rationale: The nurse should reinforce positive actions to encourage repetition of desirable behaviors when caring for children diagnosed with disruptive behavior disorder. Behavior therapy is based on the concepts of classical conditioning and operant conditioning. Cognitive Level: Application Integrated Process: Implementation 14. A child diagnosed with severe autistic spectrum disorder has the nursing diagnosis disturbed personal identity. Which outcome would best address this client diagnosis? 1. The client will name own body parts as separate from others by day five. 2. The client will establish a means of communicating personal needs by discharge. 3. The client will initiate social interactions with caregivers by day four. 4. The client will not harm self or others by discharge. ANS: 1 Rationale: An appropriate outcome for this client is to name own body parts as separate from others. The nurse should assist the client in the recognition of separateness during self-care activities, such as dressing and feeding. The long-term goal for disturbed personal identity is for the client to develop an ego identity. Cognitive Level: Application Integrated Process: Planning 15. A nursing instructor presents a case study in which a three-year-old child is in constant motion and is unable to sit still during story time. She asks a student to evaluate this childs behavior. Which student response indicates an appropriate evaluation of the situation? 1. This childs behavior must be evaluated according to developmental norms. 2. This child has symptoms of attention deficit-hyperactivity disorder. 3. This child has symptoms of the early stages of autistic disorder. 4. This childs behavior indicates possible symptoms of oppositional defiant disorder. ANS: 1 Rationale: The students evaluation of the situation is appropriate when indicating a need for the client to be evaluated according to developmental norms. The DSM-5 indicates that emotional problems exist if the behavioral manifestations are not age-appropriate, deviate from cultural norms, or create deficits or impairments in adaptive functioning. Cognitive Level: Application Integrated Process: Evaluation 16. A client has an IQ of 47. Which nursing diagnosis best addresses a client problem associated with this degree of IDD? 1. Risk for injury R/T self-mutilation 2. Altered social interaction R/T non-adherence to social convention 3. Altered verbal communication R/T delusional thinking 4. Social isolation R/T severely decreased gross motor skills ANS: 2 Rationale: The appropriate nursing diagnosis associated with this degree of IDD is altered social interaction R/T non-adherence to social convention. A client with an IQ of 47 would be diagnosed with moderate intellectual developmental disorder and may also experience some limitations in speech communications. Cognitive Level: Analysis Integrated Process: Analysis 17. A physician orders methylphenidate (Ritalin) for a child diagnosed with ADHD. Which information about this medication should the nurse provide to the parents? 1. If one dose of Ritalin is missed, double the next dose. 2. Administer Ritalin to the child after breakfast. 3. Administer Ritalin to the child just prior to bedtime. 4. A side effect of Ritalin is decreased ability to learn. ANS: 2 Rationale: The nurse should instruct the parents to administer Ritalin to the child after breakfast. Ritalin is a central nervous system stimulant and can cause decreased appetite. Central nervous system stimulants can also temporarily interrupt growth and development. Cognitive Level: Application Integrated Process: Implementation 18. Which should be the priority nursing intervention when caring for a child diagnosed with conduct disorder? 1. Modify environment to decrease stimulation and provide opportunities for quiet reflection. 2. Convey unconditional acceptance and positive regard. 3. Recognize escalating aggressive behavior and intervene before violence occurs. 4. Provide immediate positive feedback for appropriate behaviors. ANS: 3 Rationale: The priority nursing intervention when caring for a child diagnosed with conduct disorder should be to recognize escalating aggressive behavior and to intervene before violence occurs. This intervention serves to keep the client as well as others safe, which is the priority nursing concern. Cognitive Level: Application Integrated Process: Implementation 19. A mother questions the decreased effectiveness of methylphenidate (Ritalin), prescribed for her childs ADHD. Which nursing response best addresses the mothers concern? 1. The physician will probably switch from Ritalin to a central nervous system stimulant. 2. The physician may prescribe an antihistamine with the Ritalin to improve effectiveness. 3. Your child has probably developed a tolerance to Ritalin and may need a higher dosage. 4. Your child has developed sensitivity to Ritalin and may be exhibiting an allergy. ANS: 3 Rationale: The nurse should explain to the mother that the child has probably developed a tolerance to Ritalin and may need a higher dosage. Methylphenidate is a central nervous system stimulant, and tolerance can develop rapidly. Physical and psychological dependence can also occur. Cognitive Level: Application Integrated Process: Implementation 20. After studying the DSM-5 criteria for oppositional defiant disorder (ODD), which listed symptom would a student nurse recognize? 1. Arguing and annoying older sibling over the past year 2. Angry and resentful behavior over a three-month period 3. Initiating physical fights for more than 18 months 4. Arguing with authority figures for more than six months ANS: 4 Rationale: The DSM-5 rules out the diagnosis of ODD when only siblings are involved in argumentative interactions. Angry and resentful behavior over more than six months, not three months, would be considered a symptom of ODD. Initiating physical fights is a symptom of conduct disorder, not ODD. Arguing with authority figures for more than six months is listed by the DSM-5 as a symptom for the diagnosis of ODD. Cognitive Level: Application Integrated Process: Evaluation Multiple Response 21. Which of the following risk factors, if noted during a family history assessment, should a nurse associate with the development of IDD? (Select all that apply.) 1. A family history of Tay-Sachs disease 2. Childhood meningococcal infection 3. Deprivation of nurturance and social contact 4. History of maternal multiple motor and verbal tics 5. A diagnosis of maternal major depressive disorder ANS: 1, 2, 3 Rationale: The nurse should recognize a family history of Tay-Sachs disease, childhood meningococcal infections, and deprivation of nurturance and social contact as risk factors that would predispose a child to IDD. There are five major predisposing factors of IDD: hereditary factors, early alterations in embryonic development, pregnancy and perinatal factors, medical conditions acquired in infancy or childhood, and environmental influences and other mental disorders. Cognitive Level: Application Integrated Process: Assessment 22. Which of the following findings should a nurse identify that would contribute to a clients development of ADHD? (Select all that apply.) 1. The clients father was a smoker. 2. The client was born 7 weeks premature. 3. The client is lactose intolerant. 4. The client has a sibling diagnosed with ADHD. 5. The client has been diagnosed with dyslexia. ANS: 2, 4 Rationale: The nurse should identify that premature birth and having a sibling diagnosed with ADHD would predispose a client to the development of ADHD. Research indicates evidence of genetic influences in the etiology of ADHD. Studies also indicate that environmental influences, such as lead exposure and diet, can be linked with the development of ADHD. Cognitive Level: Application Integrated Process: Assessment Fill-in-the-Blank 23. The DSM-5 criteria for ODD specifies that: A persistent pattern of angry/irritable mood, argumentative/defiant behavior, or vindictiveness must be evident and last at least months. ANS: six Rationale: A persistent pattern of angry/irritable mood, argumentative/defiant behavior, or vindictiveness must be evident and last at least six months according to the DSM-5 criteria for the diagnosis of ODD. Chapter 24. The Aging Individual Multiple Choice 1. A client has recently been placed in a long-term care facility, because of marked confusion and inability to perform most activities of daily living (ADLs). Which nursing intervention is most appropriate to maintain the clients self-esteem? 1. Leave the client alone in the bathroom to test ability to perform self-care. 2. Assign a variety of caregivers to increase potential for socialization. 3. Allow client to choose between two different outfits when dressing for the day. 4. Modify the daily schedule often to maintain variety and decrease boredom. ANS: 3 Rationale: The most appropriate nursing intervention to maintain this clients self-esteem is to allow the client to choose between two different outfits when dressing for the day. The nurse should also provide appropriate supervision to keep the client safe, maintain consistency of caregivers, and maintain a structured daily routine to minimize confusion. Cognitive Level: Application Integrated Process: Implementation 2. A son, who recently brought his extremely confused parent to a nursing home for admission, reports feelings of guilt. Which is the appropriate nursing response? 1. Support groups are held here on Mondays for children of residents in similar situations. 2. You did what you had to do. I wouldnt feel guilty if I were you. 3. Support groups are available to low-income families. 4. Your parent is doing just fine. Well take very good care of him. ANS: 1 Rationale: The most appropriate response by the nurse is to offer support to the son by presenting available support groups. Caregivers can often experience negative emotions and guilt. Release of these emotions can serve to prevent caregivers from developing psychopathology such a depression. Cognitive Level: Application Integrated Process: Implementation 3. A family asks why their father is attending activity groups at the long-term care facility. The son states, My father worked hard all of his life. He just needs some rest at this point. Which is the appropriate nursing response? 1. Im glad we discussed this. Well excuse him from the activity groups. 2. The groups benefit your father by providing social interaction, sensory stimulation, and reality orientation. 3. The groups are optional. Only clients at high functioning levels would benefit. 4. If your father doesnt go to these activity groups, he will be at high risk for developing cognitive problems. ANS: 2 Rationale: The most appropriate nursing response is to educate the family that the purpose of activity groups is to provide social interaction, sensory stimulation, and reality orientation. Groups can also serve to increase self-esteem and reduce depression. Cognitive Level: Application Integrated Process: Implementation 4. A nursing instructor is teaching about reminiscence therapy. What student statement indicates that learning has occurred? 1. Reminiscence therapy is a group in which participants create collages representing significant aspects of their lives. 2. Reminiscence therapy encourages members to share both positive and negative significant life memories to promote resolution. 3. Reminiscence therapy is a social group where members chat about past events and future plans. 4. Reminiscence therapy encourages members to share positive memories of significant life transitions. ANS: 2 Rationale: Reminiscence therapy encourages members to share both positive and negative significant life memories to promote resolution. Stimulation of life memories serve to help older clients work through their losses and maintain self-esteem. Reminiscence therapy can take place in one-on-one or group settings. Cognitive Level: Application Integrated Process: Evaluation 5. A couple both reside in a long-term care facility. The husband is admitted to the psychiatric unit after physically abusing his wife. He states, My wife is having an affair with a young man, and I want it investigated. Which is the appropriate nursing response? 1. Your wife is not having an affair. What makes you think that? 2. Why do you think that your wife is having an affair? 3. Your wife has told us that these thoughts have no basis in fact. 4. I understand that you are upset. We will talk about it. ANS: 4 Rationale: The most appropriate response by the nurse is to empathize with the client and encourage the client to talk about the situation. The nurse should remain nonjudgmental and help maintain clients orientation, memory, and recognition. Cognitive Level: Application Integrated Process: Implementation 6. A student nurse asks the instructor, Which psychiatric disorder is most likely initially diagnosed in the elderly? Which instructor response gives the student accurate information? 1. Schizophrenia is most likely diagnosed later in life. 2. Major depressive disorder is most likely diagnosed later in life. 3. Phobic disorder is most likely diagnosed later in life. 4. Dependent personality disorder is most likely diagnosed later in life. ANS: 2 Rationale: Major depressive disorder is most likely to be identified later in life. Depression among older adults can be increased by physical illness, functional disability, cognitive impairment, and loss of a spouse. Cognitive Level: Application Integrated Process: Assessment 7. An older client attending an adult day care program suddenly begins reporting dizziness, weakness, and confusion. What should be the initial nursing intervention? 1. Implement complete bedrest. 2. Advocate for a complete physical exam. 3. Address self-esteem needs. 4. Advocate for individual psychotherapy. ANS: 2 Rationale: The initial nursing intervention should be to advocate for a complete physical exam. Sudden onset of dizziness, weakness, and confusion could indicate a problem with the clients cardiovascular or respiratory symptoms. Physical symptoms should be thoroughly assessed prior to attributing symptoms to psychological causes. Cognitive Level: Application Integrated Process: Implementation 8. An older client who lives with a caregiver is admitted to an emergency department with a fractured arm. The client is soaked in urine and has dried fecal matter on lower extremities. The client is 6 feet tall and weighs 120 pounds. Which condition should the nurse suspect? 1. Inability for the client to meet self-care needs 2. Alzheimers disease 3. Abuse and/or neglect 4. Caregiver role strain ANS: 3 Rationale: The nurse should expect that this client is a victim of elder abuse or neglect. Indicators of elder physical abuse include bruises, fractures, burns, and other physical injury. Neglect may be manifested as hunger, poor hygiene, unattended physical problems, or abandonment. Cognitive Level: Application Integrated Process: Assessment 9. An older, emaciated client is brought to an emergency department by the clients caregiver. The client has bruises and abrasions on shoulders and back in multiple stages of healing. When directly asked about these symptoms, which type of client response should a nurse anticipate? 1. The client will honestly reveal the nature of the injuries. 2. The client may deny or minimize the injuries. 3. The client may have forgotten what caused the injuries. 4. The client will ask to be placed in a nursing home. ANS: 2 Rationale: The nurse should anticipate that the client may deny or minimize the injuries. The older client may be unwilling to disclose information, because of fear of retaliation, embarrassment about the existence of abuse in the family, protectiveness toward a family member, or unwillingness to bring about legal action. Cognitive Level: Application Integrated Process: Assessment 10. A client in the middle stage of Alzheimers disease has difficulty communicating because of cognitive deterioration. Which nursing intervention is appropriate to improve communication? 1. Discourage attempts at verbal communication owing to increased client frustration. 2. Increase the volume of the nurses communication responses. 3. Verbalize the nurses perception of the implied communication. 4. Encourage the client to communicate by writing. ANS: 3 Rationale: The most appropriate nursing intervention is to verbalize the nurses perception of the implied communication. The nurse should also keep explanations simple, use face-to-face interaction, and speak slowly without shouting. Cognitive Level: Application Integrated Process: Implementation 11. An older client is exhibiting symptoms of major depressive disorder. A physician is considering prescribing an antidepressant. Which physiological problem should make a nurse question this medication regime? 1. Altered cortical and intellectual functioning 2. Altered respiratory and gastrointestinal functioning 3. Altered liver and kidney functioning 4. Altered endocrine and immune system functioning ANS: 3 Rationale: The nurse should question the use of antidepressant medication in a client with altered liver and kidney function. Antidepressant medication should be administered with consideration for age-related physiological changes in absorption, distribution, elimination, and brain receptor sensitivity. Because of these changes, medications can reach high levels despite moderate oral dosage. Cognitive Level: Application Integrated Process: Implementation 12. An older client has met the criteria for a diagnosis of major depressive disorder. The client does not respond to antidepressant medications. Which therapeutic intervention should a nurse anticipate will be ordered for this client? 1. Electroconvulsive therapy (ECT) 2. Neuroleptic therapy 3. An antiparkinsonian agent 4. An anxiolytic agent ANS: 1 Rationale: The nurse should anticipate that ECT will be ordered to treat this clients symptoms of depression. ECT remains one of the safest and most effective treatments for major depression in older adults. The response to ECT may be slower in older clients, and the effects may be of limited duration. Cognitive Level: Application Integrated Process: Planning 13. A nurse is charting assessment information about a 70-year-old client. According to the U.S. Census Bureau, what term would the nurse use to describe this client? 1. The nurse should document using the term older. 2. The nurse should document using the term elderly. 3. The nurse should document using the term aged. 4. The nurse should document using the term very old. ANS: 2 Rationale: The U.S. Census Bureau classifies a 70-year-old individual as elderly. The U.S. Census Bureau has developed a system for classification of older Americans: older: 5564; elderly: 6574; aged: 7584; very old: 85 years and older. Cognitive Level: Application Integrated Process: Assessment 14. Which individual is most likely to be below the poverty level in the United States? 1. A 70-year-old Hispanic woman living alone 2. A 72-year-old African American man living alone 3. A 68-year-old Asian American woman living with family 4. A 75-year-old Latino American man living with family ANS: 1 Rationale: Approximately 3.5 million persons age 65 or older were below the poverty level in 2010. Older women had a higher poverty rate than older men, and older Hispanic women living alone had the highest poverty rate. Cognitive Level: Application Integrated Process: Assessment 15. According to Reichard, Livson, and Peterson, which classification of the personalities of older men describe passive-dependent individuals who are content to lean on others for support, to disengage, and to let most of lifes activities pass them by? 1. Mature men personalities 2. Armored men personalities 3. Self-haters personalities 4. Rocking chair personalities ANS: 4 Rationale: In a classic study by Reichard, Livson, and Peterson, the personalities of older men were classified into five major categories according to their patterns of adjustment to aging. Rocking chair personalities are found in passive-dependent individuals who are content to lean on others for support, to disengage, and to let most of lifes activities pass them by. Cognitive Level: Application Integrated Process: Assessment 16. According to Reichard, Livson, and Peterson, a client is classified as an armored man. Which personality description led to this classification? 1. Rigid and stable, presenting a strong silent front 2. Passive-dependent individuals who lean on others for support 3. Aggressiveness is common, as is suspicion of others 4. Animosity is turned inward on themselves ANS: 1 Rationale: In a classic study by Reichard, Livson, and Peterson, the personalities of older men were classified into five major categories according to their patterns of adjustment to aging. Armored men have well-integrated defense mechanisms, which serve as adequate protection. Rigid and stable, they present a strong silent front and often rely on activity as an expression of their continuing independence. Cognitive Level: Application Integrated Process: Assessment Multiple Response 17. According to genetic theory, aging is an involuntarily inherited process that operates over time to alter cellular or tissue structures. Which of the following findings support this theory? (Select all that apply.) 1. Decreased amounts of adrenocorticotropic hormone, resulting in less-efficient stress response 2. The development of collagen 3. The development of lipofuscin 4. The increased frequency in the occurrence of cancer 5. The increased frequency in the occurrence of autoimmune disorders ANS: 2, 3, 4, 5 Rationale: According to genetic theory, aging is an involuntarily inherited process that operates over time to alter cellular or tissue structures. This theory suggests that life span and longevity changes are predetermined. The development of free radicals, collagen, and lipofuscin in the aging body, and an increased frequency in the occurrence of cancer and autoimmune disorders, provide some evidence for this theory and the proposition that error or mutation occurs at the molecular and cellular level. Decreased amounts of adrenocorticotropic hormone, resulting in less-efficient stress response is part of the normal aging process of the endocrine system. Cognitive Level: Application Integrated Process: Assessment Fill-in-the-Blank 18. The discipline of is the branch of clinical medicine specializing in psychopathology of the elderly population. ANS: geropsychiatry Rationale: The discipline of geropsychiatry is the branch of clinical medicine specializing in psychopathology of the elderly population. Chapter 25. Survivors of Abuse and Neglect Multiple Choice 1. A kindergarten student is frequently violent toward other children. A school nurse notices bruises and burns on the childs face and arms. What other symptom should indicate to the nurse that the child may have been physically abused? 1. The child shrinks at the approach of adults. 2. The child begs or steals food or money. 3. The child is frequently absent from school. 4. The child is delayed in physical and emotional development. ANS: 1 Rationale: The nurse should determine that a child who shrinks at the approach of adults in addition to having bruises and burns may be a victim of abuse. Maltreatment is considered, whether or not the adult intended to harm the child. Cognitive Level: Application Integrated Process: Assessment 2. A woman presents with a history of physical and emotional abuse in her intimate relationships. What should this information lead a nurse to suspect? 1. The woman may be exhibiting a controlled response pattern. 2. The woman may have a history of childhood neglect. 3. The woman may be exhibiting codependent characteristics. 4. The woman may be a victim of incest. ANS: 4 Rationale: The nurse should suspect that this client may be a victim of incest. Many women who are battered have low self-esteem and have feelings of guilt, anger, fear, and shame. Women in abusive relationships often grew up in an abusive home. Cognitive Level: Application Integrated Process: Assessment 3. A nursing instructor is developing a lesson plan to teach about domestic violence. Which information should be included? 1. Power and control are central to the dynamic of domestic violence. 2. Poor communication and social isolation are central to the dynamic of domestic violence. 3. Erratic relationships and vulnerability are central to the dynamic of domestic violence. 4. Emotional injury and learned helplessness are central to the dynamic of domestic violence. ANS: 1 Rationale: The nursing instructor should include the concept that power and control are central to the dynamic of domestic violence. Battering is defined as a pattern of coercive control founded on physical and/or sexual violence or threat of violence. The typical abuser is very possessive and perceives the victim as a possession. Cognitive Level: Application Integrated Process: Planning 4. A client is brought to an emergency department after being violently raped. Which nursing action is appropriate? 1. Discourage the client from discussing the rape, because this may lead to further emotional trauma. 2. Remain nonjudgmental while actively listening to the clients description of the violent rape event. 3. Meet the clients self-care needs by assisting with showering and perineal care. 4. Probe for further, detailed description of the rape event. ANS: 2 Rationale: The most appropriate nursing action is to remain nonjudgmental and actively listen to the clients description of the event. It is important to also communicate to the victim that he/she is safe and that it is not his/her fault. Nonjudgmental listening provides an avenue for catharsis, which contributes to the healing process. Cognitive Level: Application Integrated Process: Implementation 5. A raped client answers a nurses questions in a monotone voice with single words, appears calm, and exhibits a blunt affect. How should the nurse interpret this clients responses? 1. The client may be lying about the incident. 2. The client may be experiencing a silent rape reaction. 3. The client may be demonstrating a controlled response pattern. 4. The client may be having a compounded rape reaction. ANS: 3 Rationale: This client is most likely demonstrating a controlled response pattern. In the controlled response pattern, the clients feelings are masked or hidden, and a calm, composed, or subdued affect is seen. In the expressed response pattern, feelings of fear, anger, and anxiety are expressed through crying sobbing, smiling, restlessness, and tension. Cognitive Level: Application Integrated Process: Assessment 6. A client who is in a severely abusive relationship is admitted to a psychiatric inpatient unit. The client fears for her life. A staff nurse asks, Why doesnt she just leave him? Which is the nursing supervisors most appropriate response? 1. These clients dont know life any other way, and change is not an option until they have improved insight. 2. These clients have limited cognitive skills and few vocational abilities to be able to make it on their own. 3. These clients often have a lack of financial independence to support themselves and their children, and most have religious beliefs prohibiting divorce and separation. 4. These clients are paralyzed into inaction by a combination of physical threats and a sense of powerlessness. ANS: 4 Rationale: The nursing supervisor is accurate when stating that clients who are in abuse relationships are paralyzed into inaction by a combination of physical threats and a sense of powerlessness. Women often choose to stay with an abusive partner: for the children, for financial reasons, for fear of retaliation, for lack of a support network, for religious reasons, or because of hopefulness. Cognitive Level: Application Integrated Process: Evaluation 7. A woman comes to an emergency department with a broken nose and multiple bruises after being beaten by her husband. She states, The beatings have been getting worse, and Im afraid, next time, he will kill me. Which is the appropriate nursing response? 1. Leopards dont change their spots, and neither will he. 2. There are things you can do to prevent him from losing control. 3. Lets talk about your options so that you dont have to go home. 4. Why dont we call the police so that they can confront your husband with his behavior? ANS: 3 Rationale: The most appropriate response by the nurse is to talk with the client about options so that the client does not have to return to the abusive environment. It is essential that clients make decisions on their own without the nurse being the rescuer. Imposing judgments and giving advice is nontherapeutic. Cognitive Level: Application Integrated Process: Implementation 8. A college student was sexually assaulted when out on a date. After several weeks of crisis intervention therapy, which client statement should indicate to a nurse that the student is handling this situation in a healthy manner? 1. I know that it was not my fault. 2. My boyfriend has trouble controlling his sexual urges. 3. If I dont put myself in a dating situation, I wont be at risk. 4. Next time I will think twice about wearing a sexy dress. ANS: 1 Rationale: The client who realizes that sexual assault was not her fault is handling the situation in a healthy manner. The nurse should provide nonjudgmental listening and communicate statements that instill trust and validate self-worth. Cognitive Level: Application Integrated Process: Evaluation 9. A client asks, Why does a rapist use a weapon during the act of rape? Which is the most appropriate nursing response? 1. To decrease the victimizers insecurity. 2. To inflict physical harm with the weapon. 3. To terrorize and subdue the victim. 4. To mirror learned family behavior patterns related to weapons. ANS: 3 Rationale: The nurse should explain that a rapist uses weapons to terrorize and subdue the victim. Rape is the expression of power and dominance by means of sexual violence. Rape can occur over a broad spectrum of experience, from violent attack to insistence on sexual intercourse by an acquaintance or spouse. Cognitive Level: Application Integrated Process: Implementation 10. When questioned about bruises, a woman states, It was an accident. My husband just had a bad day at work. Hes being so gentle now and even brought me flowers. Hes going to get a new job, so it wont happen again. This client is in which phase of the cycle of battering? 1. Phase I: The tension-building phase 2. Phase II: The acute battering incident phase 3. Phase III: The honeymoon phase 4. Phase IV: The resolution and reorganization phase ANS: 3 Rationale: The client is in the honeymoon phase of the cycle of battering. In this phase, the batterer becomes extremely loving, kind, and contrite. Promises are often made that the abuse will not happen again. Cognitive Level: Application Integrated Process: Evaluation 11. Which information should the nurse in an employee assistance program provide to an employee who exhibits symptoms of domestic physical abuse? 1. Have ready access to a gun and learn how to use it. 2. Research lawyers that can aid in divorce proceedings. 3. File charges of assault and battery. 4. Have ready access to the number of a safe house for battered women. ANS: 4 Rationale: The nurse should provide information about the accessibility of safe houses for battered women when working with a client who has symptoms of domestic physical abuse. Many women feel powerless within the abusive relationship and may be staying in the abusive relationship out of fear. Cognitive Level: Application Integrated Process: Implementation 12. A survivor of rape presents in an emergency department crying, pacing, and cursing her attacker. A nurse should recognize these client actions as which behavioral defense? 1. Controlled response pattern 2. Compounded rape reaction 3. Expressed response pattern 4. Silent rape reaction ANS: 3 Rationale: The nurse should recognize that this client is exhibiting an expressed response pattern. In the expressed response pattern, feelings of fear, anger, and anxiety are expressed through crying, sobbing, smiling, restlessness, and tension. In the controlled response pattern, the clients feelings are masked or hidden, and a calm, composed, or subdued affect is seen. Cognitive Level: Application Integrated Process: Evaluation 13. Which assessment data should a school nurse recognize as a sign of physical neglect? 1. The child is often absent from school and seems apathetic and tired. 2. The child is very insecure and has poor self-esteem. 3. The child has multiple bruises on various body parts. 4. The child has sophisticated knowledge of sexual behaviors. ANS: 1 Rationale: The nurse should recognize that a child who is often absent from school and seems apathetic and tired may be a victim of neglect. Other indicators of neglect are stealing food or money, lacking medical or dental care, being consistently dirty, lacking sufficient clothing, or stating that there is no one home to provide care. Cognitive Level: Application Integrated Process: Assessment 14. A client diagnosed with an eating disorder experiences insomnia, nightmares, and panic attacks that occur before bedtime. She has never married or dated, and she lives alone. She states to a nurse, My father has recently moved back to town. What should the nurse suspect? 1. Possible major depressive disorder 2. Possible history of childhood incest 3. Possible histrionic personality disorder 4. Possible history of childhood physical abuse ANS: 2 Rationale: The nurse should suspect that this client may have a history of childhood incest. Adult survivors of incest are at risk for developing post-traumatic stress disorder, sexual dysfunction, somatization disorders, compulsive sexual behavior disorders, depression, anxiety, eating disorders, and substance abuse disorders. Cognitive Level: Application Integrated Process: Assessment Multiple Response 15. In planning care for a woman who presents as a survivor of domestic abuse, a nurse should be aware of which of the following data? (Select all that apply.) 1. It often takes several attempts before a woman leaves an abusive situation. 2. Substance abuse is a common factor in abusive relationships. 3. Until children reach school age, they are usually not affected by abuse between their parents. 4. Women in abusive relationships usually feel isolated and unsupported. 5. Economic factors rarely play a role in the decision to stay. ANS: 1, 2, 4 Rationale: When planning care for a woman who is a survivor of domestic abuse, the nurse should be aware that it often takes several attempts before a woman leaves an abusive situation, that substance abuse is a common factor in abusive relationships, and that women in abusive relationships usually feel isolated and unsupported. Children can be affected by domestic violence from infancy, and economic factors often play a role in the victims decision to stay. Cognitive Level: Application Integrated Process: Planning 16. Which of the following nursing diagnoses are typically appropriate for an adult survivor of incest? (Select all that apply.) 1. Low self-esteem 2. Powerlessness 3. Disturbed personal identity 4. Knowledge deficit 5. Non-adherence ANS: 1, 2 Rationale: An adult survivor of incest would most likely have low self-esteem and a sense of powerlessness. Adult survivors of incest are at risk for developing post-traumatic stress disorder, sexual dysfunction, somatization disorders, compulsive sexual behavior disorders, depression, anxiety, eating disorders, and substance abuse disorders. Cognitive Level: Application Integrated Process: Assessment 17. A nursing instructor is teaching about intimate partner violence. Which of the following student statements indicate that learning has occurred? (Select all that apply.) 1. Intimate partner violence is a pattern of abusive behavior that is used by an intimate partner. 2. Intimate partner violence is used to gain power and control over the other intimate partner. 3. Fifty-one percent of victims of intimate violence are women. 4. Women ages 25 to 34 experience the highest per capita rates of intimate violence. 5. Victims are typically young married women who are dependent housewives. ANS: 1, 2, 4 Rationale: Intimate partner violence is a pattern of abusive behavior that is used by an intimate partner. It is used to gain power and control over the other intimate partner. Women ages 25 to 34 experience the highest per capita rates of intimate violence. Eighty-five percent of victims of intimate violence are women. Battered women represent all age, racial, religious, cultural, educational, and socioeconomic groups. They may be married or single, housewives or business executives. Cognitive Level: Application Integrated Process: Assessment Ordered Response 18. Order the description of the progressive phases of Walkers model of the cycle of battering? This phase is the most violent and the shortest, usually lasting up to 24 hours. In this phase, the mans tolerance for frustration is declining. In this phase, the batterer becomes extremely loving, kind, and contrite. ANS: The correct order is 2, 1, 3 Rationale: In her classic studies of battered women and their relationships, Walker identified a cycle of predictable behaviors that are repeated over time. The behaviors can be divided into three distinct phases that vary in time and intensity both within the same relationship and among different couples. 1. Tension building phase. In this phase, the mans tolerance for frustration is declining. 2. Acute battering incident phase. This phase is the most violent and the shortest, usually lasting up to 24 hours. 3. Honeymoon phase. In this phase, the batterer becomes extremely loving, kind, and contrite. Cognitive Level: Analysis Integrated Process: Assessment Fill-in-the-Blank 19. A pattern of coercive control founded on and supported by physical and/or sexual violence or threat of violence of an intimate partner is termed . ANS: battering Rationale: Battering is a pattern of behavior used to establish power and control over another person with whom an intimate relationship is or has been shared through fear and intimidation, often including the threat or use of violence. Battering happens when one person believes they are entitled to control another. Cognitive Level: Application Integrated Process: Assessment 20. Physical of a child includes refusal of or delay in seeking health care, abandonment, expulsion from the home or refusal to allow a runaway to return home, and inadequate supervision. ANS: neglect Rationale: Physical neglect of a child includes refusal of or delay in seeking health care, abandonment, expulsion from the home or refusal to allow a runaway to return home, and inadequate supervision. Children are vulnerable and relatively powerless, and the effects of maltreatment are infinitely deep and long lasting. Chapter 26. Community Mental Health Nursing Multiple Choice 1. A nursing instructor is teaching about the Community Health Centers Act of 1963. What was a deterring factor to the proper implementation of this act? 1. Many perspective clients did not meet criteria for mental illness diagnostic-related groups. 2. Zoning laws discouraged the development of community mental health centers. 3. States could not match federal funds to establish community mental health centers. 4. There was not a sufficient employment pool to staff community mental health centers. ANS: 3 Rationale: A deterring factor to the proper implementation of the Community Mental Health Centers Act of 1963 was that states could not match federal funds to establish community mental health centers. This act called for the construction of comprehensive community mental health centers to offset the effect of deinstitutionalization, the closing of state mental health hospitals. Cognitive Level: Application Integrated Process: Evaluation 2. A nurse is implementing care within the parameters of tertiary prevention. Which nursing action is an example of this type of care? 1. Teaching an adolescent about pregnancy prevention 2. Teaching a client the reportable side effects of a newly prescribed neuroleptic medication 3. Teaching a client to cook meals, make a grocery list, and establish a budget 4. Teaching a client about his or her new diagnosis of bipolar disorder ANS: 3 Rationale: The nurse who teaches a client to cook meals, make a grocery list, and establish a budget is implementing care within the parameters of tertiary prevention. Tertiary prevention consists of services aimed at reducing the residual effects that are associated with severe and persistent mental illness. It is accomplished by preventing complications of the illness and promoting rehabilitation that is directed toward achievement of maximum functioning. Cognitive Level: Application Integrated Process: Implementation 3. A nursing instructor is teaching about case management. What student statement indicates that learning has occurred? 1. Case management is a method used to achieve independent client care. 2. Case management provides coordination of services required to meet client needs. 3. Case management exists mainly to facilitate client admission to needed inpatient services. 4. Case management is a method to facilitate physician reimbursement. ANS: 2 Rationale: The instructor evaluates that learning has occurred when a student defines case management as providing coordination of services required to meet client needs. Case management strives to organize client care so that specific outcomes are achieved within allotted time frames. Cognitive Level: Application Integrated Process: Evaluation 4. A client at the mental health clinic tells the case manager, I cant think about living another day, but dont tell anyone about the way I feel. I know you are obligated to protect my confidentiality. Which case manager response is most appropriate? 1. The treatment team is composed of many specialists who are working to improve your ability to function. Sharing this information with the team is critical to your care. 2. Lets discuss steps that will resolve negative lifestyle choices that may have increased your suicidal risk. 3. You seem to be preoccupied with self. You should concentrate on hope for the future. 4. This information is secure with me because of client confidentiality. ANS: 1 Rationale: The most appropriate response by the case manager is to explain that sharing the information with the treatment team is critical to the clients care. This case managers priority is to ensure client safety and to inform others on the treatment team of the clients suicidal ideation. Cognitive Level: Application Integrated Process: Implementation 5. When intervening with a married couple experiencing relationship discord, which nursing action reflects an intervention at the secondary level of prevention? 1. Teaching assertiveness skills in order to meet assessed needs 2. Supplying the couple with guidelines related to marital seminar leadership 3. Teaching the couple about various methods of birth control 4. Counseling the couple related to open and honest communication skills ANS: 4 Rationale: Counseling the couple related to open and honest communication skills is a reflection of a nursing intervention at the secondary level of prevention. Secondary prevention aims at minimizing symptoms and is accomplished through early identification of problems and prompt initiation of effective treatment. Cognitive Level: Application Integrated Process: Implementation 6. A school nurse provides education on drug abuse to a high school class. This nursing action is an example of which level of preventive care? 1. Primary prevention 2. Secondary prevention 3. Tertiary prevention 4. Primary intervention ANS: 1 Rationale: Providing nursing education on drug abuse to a high school class is an example of primary prevention. Primary prevention services are aimed at reducing the incidence of mental health disorders within the population. Cognitive Level: Application Integrated Process: Implementation 7. A newly admitted homeless client diagnosed with schizophrenia states, I have been living in a cardboard box for two weeks. Why did the government let me down? Which is an appropriate nursing response? 1. Your discharge from the state hospital was done prematurely. Had you remained in the state hospital longer, you would not be homeless. 2. Your premature discharge from the state hospital was not intended for patients diagnosed with chronic schizophrenia. 3. Your discharge from the state hospital was based on firm principles; however, the resources were not available to make the transition a success. 4. Your discharge from the state hospital was based on presumed family support, and this was not forthcoming. ANS: 3 Rationale: The most accurate nursing response is to explain to the client that the resources were not available to make transitioning out of a state hospital a success. There are several factors that are thought to contribute to homelessness among the mentally ill: deinstitutionalization, poverty, lack of affordable housing, lack of affordable health care, domestic violence, and addiction disorders. Cognitive Level: Application Integrated Process: Implementation 8. An instructor is teaching nursing students about the difference between partial and inpatient hospitalization. In what way does partial hospitalization differ from traditional inpatient hospitalization? 1. Partial hospitalization does not provide medication administration and monitoring. 2. Partial hospitalization does not use an interdisciplinary team. 3. Partial hospitalization does not offer a comprehensive treatment plan. 4. Partial hospitalization does not provide supervision 24 hours a day. ANS: 4 Rationale: The instructor should explain that partial hospitalization does not provide supervision 24 hours a day. Partial hospitalization programs generally offer a comprehensive treatment plan formulated by an interdisciplinary team. They have proved to be an effective method of preventing hospitalization. Cognitive Level: Application Integrated Process: Evaluation 9. When a home health nurse administers an outpatients injection of haloperidol decanoate (Haldol decanoate), which level of care is the nurse providing? 1. Primary prevention level of care 2. Secondary prevention level of care 3. Tertiary prevention level of care 4. Case management level of care ANS: 3 Rationale: When administering medication in an outpatient setting, the nurse is providing a tertiary prevention level of care. Tertiary prevention services are aimed at reducing the residual effects that are associated with severe and persistent mental illness. It is accomplished by preventing complications of the illness and promoting rehabilitation that is directed toward achievement of maximum functioning. Cognitive Level: Application Integrated Process: Implementation 10. A client diagnosed with schizophrenia is hospitalized owing to an exacerbation of psychosis related to non-adherence with antipsychotic medications. Which level of care does the clients hospitalization reflect? 1. Primary prevention level of care 2. Secondary prevention level of care 3. Tertiary prevention level of care 4. Case management level of care ANS: 2 Rationale: The clients hospitalization reflects the secondary prevention level of care. Secondary prevention aims at minimizing symptoms and is accomplished through early identification of problems and prompt initiation of effective treatment. Cognitive Level: Application Integrated Process: Implementation 11. When attempting to provide health-care services to the homeless, what should be a realistic concern for a nurse? 1. Most individuals that are homeless reject help. 2. Most individuals that are homeless are suspicious of anyone who offers help. 3. Most individuals that are homeless are proud and will often refuse charity. 4. Most individuals that are homeless relocate frequently. ANS: 4 Rationale: A realistic concern in the provision of health-care services to the homeless is that individuals who are homeless relocate frequently. Frequent relocation confounds service delivery and interferes with providers efforts to ensure appropriate care. Cognitive Level: Application Integrated Process: Planning 12. A homeless client comes to an emergency department reporting cough, night sweats, weight loss, and blood-tinged sputum. Which disease, which has recently become more prevalent among the homeless community, should a nurse suspect? 1. Meningitis 2. Tuberculosis 3. Encephalopathy 4. Mononucleosis ANS: 2 Rationale: The nurse should suspect that the homeless client has contracted tuberculosis. Tuberculosis is a growing problem among individuals who are homeless, owing to being in crowded shelters, which are ideal conditions for the spread of respiratory tuberculosis. Prevalence of alcoholism, drug addiction, HIV infection, and poor nutrition also impact the increase of contracted cases of tuberculosis. Cognitive Level: Analysis Integrated Process: Assessment Multiple Response 13. Which of the following clients should a nurse recommend for a structured day program? (Select all that apply.) 1. An acutely suicidal teenager 2. A chronically mentally ill woman who has a history of medication non-adherence 3. A socially isolated older individual 4. A depressed individual who is able to contract for safety 5. A client who is hearing voices that tell the client to harm others ANS: 2, 4 Rationale: The nurse should recommend a structured day program for a chronically mental ill woman who has a history of medication non-adherence and for a depressed individual who is able to contract for safety. Day programs (also called partial hospitalizations) are designed to prevent institutionalization or to ease the transition from inpatient hospitalization to community living. Cognitive Level: Application Integrated Process: Implementation 14. Which of the following are characteristics of a Program of Assertive Community Treatment (PACT), as described by the National Alliance on Mental Illness (NAMI)? (Select all that apply.) 1. PACT offers nationally based treatment to people with serious and persistent mental illnesses. 2. PACT is a type of case-management program. 3. The PACT team provides services 24 hours a day, 7 days a week, 365 days a year. 4. The PACT team provides highly individualized services directly to consumers. 5. PACT is a multidisciplinary team approach. ANS: 2, 3, 4, 5 Rationale: NAMI defines PACT as a service-delivery model that provides comprehensive, locally, not nationally, based treatment to people with serious and persistent mental illnesses. PACT is a type of case-management program that provides highly individualized services directly to consumers. It is a team approach and includes members from psychiatry, social work, nursing, substance abuse, and vocational rehabilitation. The PACT team provides these services 24 hours a day, 7 days a week, 365 days a year. Cognitive Level: Application Integrated Process: Assessment 15. Which of the following have been assessed as the most common types of mental illness identified among homeless individuals? (Select all that apply.) 1. Schizophrenia 2. Body dysmorphic disorder 3. Antisocial personality disorder 4. Neurocognitive disorder 5. Conversion disorder ANS: 1, 3, 4 Rationale: A number of studies have been conducted, primarily in large, urban areas, which have addressed the most common types of mental illness identified among homeless individuals. Schizophrenia is frequently described as the most common diagnosis. Other prevalent disorders include bipolar disorder, substance abuse and dependence, depression, personality disorders, and neurocognitive disorders. Cognitive Level: Application Integrated Process: Assessment Ordered Response 16. Order the goals of the levels of prevention as they progress through the public health model set forth by Gerald Caplan. Interventions aimed at minimizing early symptoms of psychiatric illness and directed toward reducing the prevalence and duration of the illness Services aimed at reducing the residual defects that are associated with severe and persistent mental illness Services aimed at reducing the incidence of mental disorders within the population ANS: The correct order is 2, 3, 1 Rationale: The premise of the model of public health is based largely on the concepts set forth by Gerald Caplan (1964) during the initial community mental health movement. They include primary prevention, secondary prevention, and tertiary prevention. 1. Primary prevention is aimed at reducing the incidence of mental disorders within the population. 2. Secondary prevention is aimed at minimizing early symptoms of psychiatric illness and directed toward reducing the prevalence and duration of the illness. 3. Tertiary prevention is aimed at providing services that reduce the residual defects that are associated with severe and persistent mental illness. Cognitive Level: Analysis Integrated Process: Planning Fill-in-the-Blank 17. The movement closed state mental hospitals and caused the discharge of individuals with mental illness. ANS: deinstitutionalization Rationale: The deinstitutionalization movement closed state mental hospitals and caused the discharge of individuals with mental illness. Congress passed the Mental Retardation Facilities and Community Mental Health Centers Construction Act (often called the Community Mental Health Centers Act) in 1963. This act called for the construction of comprehensive community health centers, the cost of which would be shared by federal and state governments. Unfortunately, many state governments did not have the capability to match the federal funds required for the establishment of these mental health centers. Chapter 27. The Bereaved Individual Multiple Choice 1. A client is diagnosed with terminal cancer. Which situation represents Kbler-Rosss grief stage of anger? 1. The client registers for an iron-man marathon to be held in 9 months. 2. The client is a devout Catholic but refuses to attend church and states that his faith has failed him. 3. The client promises God to give up smoking if allowed to live long enough to witness a grandchilds birth. 4. The client gathers family in order to plan a funeral and make last wishes known. ANS: 2 Rationale: The nurse should assess that the client is in the anger stage of grieving when the client refuses to attend church and states that his faith has failed him. Anger is the second stage of Kbler-Rosss grief process, in which the reality of the situation is realized, and the individual has feelings of sadness, guilt, shame, helplessness, and hopelessness. Cognitive Level: Application Integrated Process: Assessment 2. A nurse is caring for an Irish client who has recently lost his wife. The client tells the nurse that he is planning an elaborate wake and funeral. According to George Engel, what purpose would these rituals serve? 1. To delay the recovery process initiated by the loss of the clients wife 2. To facilitate the acceptance of the loss of the clients wife 3. To avoid dealing with grief associated with the loss of the clients wife 4. To eliminate emotional pain related to the loss of the clients wife ANS: 2 Rationale: The nurse should anticipate that the purpose of these rituals is to facilitate the acceptance of the loss of the clients wife. Resolution of the loss is the fourth stage in Engels grief process, in which the bereaved experiences a preoccupation with the loss, which gradually decreases over time. Cognitive Level: Application Integrated Process: Evaluation 3. A nurse discharges a female client to home after delivering a stillborn infant. The client finds that neighbors have dismantled the nursery that she and her husband planned. According to Worden, how could this intervention affect the womans grieving task completion? 1. This intervention may hamper the woman from continuing a relationship with her infant. 2. This intervention would help the woman forget the sorrow and move on with life. 3. This intervention communicates full support from her neighbors. 4. This intervention would motivate the woman to look to the future and not the past. ANS: 1 Rationale: The nurse should anticipate that this intervention could hinder the woman from continuing a relationship with her infant. The first task in Wordens grief process is to accept the reality of the loss. It is common for individuals to refuse to believe that the loss has occurred. Behaviors may include misidentifying an individual in the environment as their loved one, retaining possessions of the lost loved one, and removing all reminders of the loved one in order to avoid reality. Cognitive Level: Application Integrated Process: Evaluation 4. A teenager has recently lost a parent. Which grieving behavior should a school nurse expect when assessing this client? 1. Denial of personal mortality 2. Preoccupation with the loss 3. Clinging behaviors and personal insecurity 4. Acting-out behaviors, exhibited in aggression and defiance ANS: 4 Rationale: The school nurse should anticipate that the teenager will exhibit aggression and acting out. Adolescents have the ability to understand death on an adult level yet have difficulty tolerating the intense feelings associated with the death of a loved one. It is often easier for adolescents to talk with peers about feelings than with other adults. Cognitive Level: Application Integrated Process: Assessment 5. What term should a nurse use when assessing a response to grieving that includes a sudden physical collapse and paralysis, and which cultural group would be associated with this behavior? 1. Falling out in the African American culture 2. Body rocking in the Vietnamese American culture 3. Conversion disorder in the Jewish American culture 4. Spirit possession in the Native American culture ANS: 1 Rationale: The nurse should use the term falling out to describe a sudden physical collapse and paralysis in the African American culture. The individuals may also experience an inability to see or speak yet maintain hearing and understanding. Cognitive Level: Application Integrated Process: Assessment 6. Which grieving behaviors should a nurse anticipate when caring for a Navajo client who recently lost a child? 1. Celebrating the life of a deceased person with festivities and revelry 2. Not expressing grief openly and reluctance to touch the dead body 3. Holding a prayerful vigil for a week following the persons death 4. Expressing grief openly and publicly and erecting an altar in the home to honor the dead ANS: 2 Rationale: The nurse should identify that a Navajo client who recently lost a child would not express grief openly and would be reluctant to touch the dead body. Navajo Indians do not bury the body of a deceased person for four days after death, and they conduct a cleaning ceremony prior to burial. The dead are buried with their shoes on the wrong feet and rings on their index fingers. Cognitive Level: Application Integrated Process: Assessment 7. A nursing instructor is teaching about the typical grieving behaviors of Chinese Americans. Which student statement would indicate that more instruction is necessary? 1. In this culture, the color red is associated with death and is considered bad luck. 2. In this culture, there is an innate fear of death. 3. In this culture, emotions are not expressed openly. 4. In this culture, death and bereavement are centered on ancestor worship. ANS: 1 Rationale: The nursing instructor should evaluate that more instruction is needed if a student states that the color red is associated with death and bad luck in the Chinese culture. Chinese Americans consider the color white as associated with death and is considered bad luck. Red is the ultimate color of luck in this culture. Chinese Americans also avoid purchasing insurance because of the fear that they may be inviting death. Cognitive Level: Application Integrated Process: Evaluation 8. A nurse assigns a client the nursing diagnosis of complicated grieving. According to Bowlby, which long-term outcome would be most appropriate for this nursing diagnosis? 1. The client will accomplish the recovery stage of grief by year one. 2. The client will accomplish the acceptance stage of grief by year one. 3. The client will accomplish the reorganization stage of grief by year one. 4. The client will accomplish the emotional relocation stage of grief by year one. ANS: 3 Rationale: The nurse should identify that, according to Bowlby, an appropriate long-term outcome for this client is to accomplish the reorganization stage of grief by year one. Until the client can recognize and accept personal feelings regarding the loss, grief work cannot progress. The reorganization stage of grieving is the final stage in which the individual accepts the loss and new goals and patterns are established. Cognitive Level: Application Integrated Process: Planning 9. A nurse assesses a woman whose husband died 13 months ago. She isolates herself, screams at her deceased spouse, and is increasingly restless. According to Bowlby, this widow is in which stage of the grieving process? 1. Stage I: Numbness or protest 2. Stage II: Disequilibrium 3. Stage III: Disorganization and despair 4. Stage IV: Reorganization ANS: 3 Rationale: The nurse should identify that this client is in the third stage of Bowlbys grief process, called disorganization and despair. This stage is characterized by feelings of despair in response to the realization that the loss has occurred. The individual experiences helplessness, fear, and hopelessness. Perceptions of visualizing or being in the presence of the lost one may occur. Cognitive Level: Application Integrated Process: Assessment 10. Which is the most accurate description of the nursing diagnosis of dysfunctional grieving? 1. Inability to form a valid appraisal of a loss and to use available resources 2. The experience of distress, with accompanying sadness, which fails to follow norms 3. A perceived lack of control over a current loss situation 4. Aloneness perceived as imposed by others and as a negative or threatening state ANS: 2 Rationale: The nurse should define dysfunctional grieving as the experience of distress, with accompanying sadness, which fails to follow norms. Three types of pathological grief reactions are delayed or inhibited grief, distorted (exaggerated) grief response, and chronic or prolonged grieving. One crucial difference between normal and dysfunctional grieving is the loss of self- esteem marked my feelings of guilt or worthlessness that may precipitate depression. Cognitive Level: Application Integrated Process: Assessment Multiple Response 11. A nurse is leading a bereavement group. Which of following members of the group should the nurse identify as being at high risk for complicated grieving? (Select all that apply.) 1. A widower who has recently experienced the death of two good friends 2. A man whose wife died suddenly after a cerebrovascular accident 3. A widow who removed life support after her husband was in a vegetative state for a year 4. A woman who had a competitive relationship with her recently deceased brother 5. A young couple whose child recently died of a genetic disorder ANS: 1, 2, 4, 5 Rationale: The nurse should identify that individuals are at a high risk for complicated grieving when the bereaved person was strongly dependent on the lost entity, the relationship with the lost entity was highly ambivalent, the individual experienced a number of recent losses, the loss is that of a young person, the individuals physical or psychological health is unstable, and the bereaved person perceived responsibility for the loss. Having a year to process grief while her husband was in a vegetative state would reduce the widows risk for the problem of complicated grieving. Cognitive Level: Application Integrated Process: Evaluation 12. An instructor is teaching nursing students about Wordens grief process. According to Worden, which of the following client behaviors would delay or prolong the grieving process? (Select all that apply.) 1. Refusing to allow oneself to think painful thoughts 2. Indulging in the pain of loss 3. Using alcohol and drugs 4. Idealizing the object of loss 5. Recognizing that time will heal ANS: 1, 3, 4 Rationale: The nurse should identify that refusing to allow oneself to think painful thoughts, using alcohol and drugs, and idealizing the object of loss will delay or prolong the grieving process. Task II of Wordens grief process is working through the pain or grief. Pain must be acknowledged and processed in order to move on. Cognitive Level: Application Integrated Process: Evaluation 13. Which of the following types of care should the interdisciplinary team of hospice provide? (Select all that apply.) 1. Physical care available on a 24/7 basis 2. Counseling on the addictive properties of pain-management medications 3. Discussions related to death and dying 4. Explorations of new aggressive treatments 5. Assistance with obtaining spiritual support and guidance ANS: 1, 3, 5 Rationale: The nurse should identify that the interdisciplinary team of hospice provides physical care available on a 24/7 basis, discussions related to death and dying, and assistance with obtaining spiritual support and guidance. Hospice is a program that provides palliative and supportive care to meet the needs of people who are dying and their families. Cognitive Level: Application Integrated Process: Implementation Ordered Response 14. Order the stages of normal grief, according to John Bowlby. Reorganization Disequilibrium Disorganization and despair Numbness/protest ANS: The correct order is 4, 2, 3, 1 Rationale: John Bowlby hypothesized four stages in the grief process. He implies that these behaviors can be observed in all individuals who have experienced the loss of something or someone of value, even in babies as young as 6 months of age. 1. Numbness/Protest 2. Disequilibrium 3. Disorganization and despair 4. Reorganization Cognitive Level: Analysis Integrated Process: Assessment 15. Order the stages of normal grief, according to J. William Worden. Finding an enduring connection with the lost entity in the mist of embarking on a new life Accepting the reality of the loss Adjusting to a world without the lost entity Processing the pain of grief ANS: The correct order is 4, 1, 3, 2 Rationale: Worden views the bereaved person as active and self-determining rather than a passive participant in the grief process. He proposes that bereavement includes a set of tasks that must be reconciled in order to complete the grief process. 1. Accepting the reality of the loss 2. Processing the pain of grief 3. Adjusting to a world without the lost entity 4. Finding an enduring connection with the lost entity in the mist of embarking on a new life Cognitive Level: Analysis Integrated Process: Assessment Fill-in-the-Blank 16. grieving is the experiencing of the feelings and emotions associated with the normal grief response before the loss actually occurs. ANS: Anticipatory Rationale: Anticipatory grieving is the experiencing of the feelings and emotions associated with the normal grief response before the loss actually occurs. Anticipatory grieving may serve as a defense for some individuals to ease the burden of loss when it actually occurs. Chapter 28. Military Families Multiple Choice 1. Approximately two million American children have experienced the deployment of a parent to Iraq or Afghanistan. How many of these children either lost a parent or have a parent who was wounded in these conflicts? 1. 48,000 2. 26,000 3. 11,000 4. 8,000 ANS: 1 Rationale: More than 48,000 children have either lost a parent or have a parent who was wounded in Iraq or Afghanistan. Cognitive Level: Application Integrated Process: Assessment 2. Research has shown that an adolescent (13 to18 years) would typically exhibit which behavior as a reaction to parental military deployment? 1. May exhibit regressive behaviors and assume blame for parents departure. 2. May become sullen, tearful, throw temper tantrums, or develop sleep problems. 3. May participate in high-risk behaviors, sexual acting out, and drug or alcohol abuse. 4. May respond to schedule disruptions with irritability and/or apathy and weight loss. ANS: 3 Rationale: Infants (birth to 12 months) may respond to schedule disruptions with irritability and/or apathy and weight loss. Toddlers (1 to 3 years) may become sullen, tearful, throw temper tantrums, or develop sleep problems. Preschoolers (3 to 6 years) may regress in areas such as toilet training, sleep, separation fears, physical complaints, or thumb sucking and may assume blame for parents departure. School age children (6 to 12 years) are more aware of potential dangers to parent. May exhibit irritable behavior, aggression, or whininess. May become more regressed and fearful about parents safety. Adolescents (13 to 18 years) may be rebellious, irritable, or more challenging of authority. Parents need to be alert to high-risk behaviors, such as problems with the law, sexual acting out, and drug or alcohol abuse. Cognitive Level: Application Integrated Process: Assessment 3. What is the expected feeling and/or behavior experienced by military families during the sustainment cycle of deployment, as described by Pincus and associates? 1. Feelings alternate between denial and anticipation of loss. 2. Feelings alternate between excitement and apprehension associated with homecoming. 3. Feelings focus on the establishment of new support systems and new family routines. 4. Feelings focus on the struggle to take charge of the details of the new family structure. ANS: 3 Rationale: In the pre-deployment cycle, feelings alternate between denial and anticipation of loss. In the redeployment cycle, feelings alternate between excitement and apprehension associated with homecoming. In the sustainment cycle, families establish new support systems and new family routines. In the deployment cycle, the spouse struggles to take charge of the details of living without his or her partner. Cognitive Level: Application Integrated Process: Assessment 4. A nursing instructor is teaching about suicide among active duty military. Which fact should the instructor include in the lesson plan? 1. On average, two suicides a day occur in the U.S. military. 2. From 2005 to 2009, relationship distress factored in more than 25% of Army suicides. 3. Statistically, in 2012, suicide rates of service members surpassed the number killed in combat. 4. Military suicides are associated with a narcissistic personality disorder diagnosis. ANS: 3 Rationale: On average, one not two suicides a day occur in the U.S. military. From 2005 to 2009, relationship distress factored in more than 50% not 25% of Army suicides. Military suicides are associated with the diagnoses of substance use disorder, major depressive disorder, PTSD, and TBI, not narcissistic personality disorder. Statistically, in 2012, suicide rates of service members surpassed the number killed in combat. Cognitive Level: Application Integrated Process: Planning Multiple Response 5. A nursing instructor is preparing a lesson plan related to the history of the diagnosis of post- traumatic stress disorder (PTSD). Which of the following facts would be appropriate to include? (Select all that apply.) 1. Between 1950 and 1970, little was written about PTSD. 2. During the 1970s and 1980s, there was a major increase in research on PTSD. 3. During the 1970s and 1980s, much research was related to World War II veterans. 4. PTSD did not appear until the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III). 5. PTSD did not appear until the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). ANS: 1, 2, 4 Rationale: Very little was written about PTSD during the years between 1950 and 1970. This absence was followed in the 1970s and 1980s with an explosion in the amount of research and writing on the subject. During this time, much research was related to Vietnam not World War II veterans. PTSD did not appear until the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III). Cognitive Level: Application Integrated Process: Assessment 6. Which of the following should a nurse identify as stressors in the lives of military spouses and children? (Select all that apply.) 1. Frequent moves 2. School credit transfer issues 3. Complications of spousal employment 4. Spousal loneliness 5. Loss of military privileges during spousal deployment ANS: 1, 2, 3, 4 Rationale: The lives of military spouses and children are clearly affected when the service- members active duty assignments require frequent family moves. These include, among others, school credit transfer issues, complications of spousal employment, and spousal loneliness. Military privileges are not lost during spousal deployment. Cognitive Level: Application Integrated Process: Assessment 7. Owing to the unique challenges experienced by children of active duty military, which of the following fears would a nurse most likely identify? (Select all that apply.) 1. Fear of not being accepted in new schools 2. Fear of being behind academically 3. Fear of not making friends in new schools 4. Fear of losing athletic standing 5. Fear of discrimination from new school faculty ANS: 1, 2, 3, 4 Rationale: Military children face unique challenges. They fear not being accepted, being behind academically, not making friends, and losing athletic standing as they move from one school to another. Fear of discrimination from new school faculty has not been shown as a realistic fear in this population. Cognitive Level: Application Integrated Process: Assessment 8. After reporting a sexual assault, a female soldier is diagnosed with a personality disorder. Which of the following consequences may result? (Select all that apply.) 1. Court-martial proceedings 2. Loss of health-care benefits 3. Loss of service-related disability compensation 4. Stigma of a psychiatric diagnosis 5. Service discharge ANS: 2, 3, 4, 5 Rationale: Some military women who report their sexual assaults are discharged with a psychiatric diagnosis of personality disorder or adjustment disorder. Some of the consequences of this diagnosis are loss of health-care benefits, loss of service-related disability compensation, and the stigma of a psychiatric diagnosis. The report of a sexual assault would not lead to courtmartial proceedings for the victim. Cognitive Level: Application Integrated Process: Evaluation Fill-in-the-Blank 9. Members of various components of the National Guard and U.S. Military Reserves are classified as the / . ANS: Ready Reserve Rationale: More than 1 million men and women make up the U.S. Military Ready Reserve, who are members of various components of the National Guard and U.S. Military Reserves. Cognitive Level: Application Integrated Process: Assessment 10. An association between Parkinsons disease and combat-related traumatic brain injury (TBI) has been established. This disorder may develop years after TBI as a result of damage to the / . ANS: basal ganglia Chapter 29. Concepts of Personality Development Multiple Choice 1. A jilted college student is admitted to a hospital following a suicide attempt and states, No one will ever love a loser like me. According to Eriksons theory of personality development, a nurse should recognize that this patient has a deficit in which developmental stage?1. Trust versus mistrust2. Initiative versus guilt3. Intimacy versus isolation4. Ego integrity versus despair ANS: 3 Rationale: The nurse should recognize that the client who states, No one will ever love a loser like me has not adequately completed the intimacy versus isolation stage of development. The intimacy versus isolation stage is presumed to occur in young adulthood between the ages of 20 and 30 years. The major developmental task in this stage is to establish intense, lasting relationships or commitment to another person, cause, institution, or creative effort. Cognitive Level: Application Integrated Process: Assessment 2. A nurse observes a 3-year-old client willingly sharing candy with a sibling. According to Peplau, which psychological stage of development should the nurse determine that this child has completed?1. Learning to count on others2. Learning to delay satisfaction3. Identifying oneself4. Developing skills in participation ANS: 2 Rationale: The nurse should determine that this client has completed the learning to delay satisfaction stage of development, according to Peplaus interpersonal theory. This stage typically occurs in toddlerhood when one learns the satisfaction of pleasing others. Cognitive Level: Application Integrated Process: Assessment 3. A 9-month-old child screams every time his mother leaves and will not tolerate anyone else changing his diaper. The nurse should determine that, according to Mahlers developmental theory, this childs development was arrested at which phase?1. The autistic phase2. The symbiotic phase3. The separation-individuation phase 4. The rapprochement phase ANS: 2 Rationale: The nurse should understand that this clients development was halted in the symbiotic phase of Mahlers developmental theory, which usually occurs between 1 and 5 months of age. The child has not entered into the separation-individuation phase of development, in which a child establishes the understanding of being separate from the mother. Cognitive Level: Application Integrated Process: Evaluation 4. According to Peplau, a nurse who provides an abandoned child with parental guidance and praise following small accomplishments is serving which therapeutic role?1. Technical expert2. Resource person3. Surrogate4. Leader ANS: 3 Rationale: The nurse who provides an abandoned child with parental guidance and praise is serving the role of the surrogate, according to Peplaus interpersonal theory. A surrogate serves as a substitute for another personin this case, the childs parent. Cognitive Level: Application Integrated Process: Implementation 5. When assessing clients, a psychiatric nurse should understand that psychoanalytic theory is based on which underlying concept? 1. A possible genetic basis for the clients problems2. The structure and dynamics of the personality3. Behavioral responses to stressors4. Maladaptive cognitions ANS: 2 Rationale: The nurse should understand that psychoanalytic theory is based on the underlying concepts of the structure and dynamics of personality. Psychoanalytic theory was developed by Sigmund Freud and explains the structure of personality in three different components: the id, the ego, and the superego. Cognitive Level: Application Integrated Process: Assessment 6. Which underlying concept should a nurse associate with interpersonal theory when assessing a client? 1. The effects of social processes on personality development 2. The effects of unconscious processes and personality structures 3. The effects on thoughts and perceptual processes 4. The effects of chemical and genetic influences ANS: 1 Rationale: The nurse should associate interpersonal theory with the underlying concept of effects of social process on personality development. Sullivan developed stages of personality development based on his theory of interpersonal relationships and their effect on personality and individual behavior. Cognitive Level: Application Integrated Process: Assessment 7. A physically healthy, 35-year-old, single client lives with parents, who provide total financial support. According to Eriksons theory, which developmental task should a nurse assist the client to accomplish?1. Establishing the ability to control emotional reactions2. Establishing a strong sense of ethics and character structure3. Establishing and maintaining self-esteem 4. Establishing a career, personal relationships, and societal connections ANS: 4 Rationale: The nurse should assist the client in establishing a career, personal relationships, and societal connections. According to Erikson, nonachievement of the generativity versus stagnation stage results in self-absorption, including withdrawal from others and having no capacity for giving of the self to others. Cognitive Level: Application Integrated Process: Assessment 8. A 1-month-old infant is left alone for extended periods, has little physical stimulation, and is malnourished. Based on this infants situation, in which phase of development, according to Mahlers theory, should a nurse expect to see a potential deficit?1. The symbiotic phase 2. The autistic phase3. The consolidation phase 4. The rapprochement phase ANS: 2 Rationale: The nurse should expect that a 1-month-old infant who is left alone, has little physical stimulation, and is malnourished would not meet the autistic phase of development. The autistic phase of development usually occurs from birth to 1 month, at which time the infants focus is on basic needs and comfort. Cognitive Level: Application Integrated Process: Evaluation 9. A 6-year-old boy uses his fathers flashlight to explore his 3-year-old sisters genitalia. According to Freud, in which stage of psychosocial development should a nurse identify this behavior as normal? 1. Oral2. Anal3. Phallic4. Latency ANS: 3 Rationale: The nurse should identify this behavior as normal, because the 6-year-old client who focuses on genital organs is in the phallic stage of Freuds psychosexual stages of development. Children in the phallic stage of development focus on genital organs and develop a sense of sexual identity. Identification with the same-sex parent also occurs at this stage. Cognitive Level: Application Integrated Process: Assessment 10. A married, 26-year-old client works as a schoolteacher. She and her husband have just had their first child. A nurse should recognize that this client is successfully accomplishing which stage of Eriksons developmental theory? 1. Industry versus inferiority2. Identity versus role confusion3. Intimacy versus isolation4. Generativity versus stagnation ANS: 3 Rationale: The nurse should recognize that a 26-year-old client who is married and has a child has successfully accomplished the intimacy versus isolation stage of Eriksons developmental theory. The intimacy versus isolation stage of young adulthood involves forming lasting relationships. Achievement of this task results in the capacity for mutual love and respect. Cognitive Level: Application Integrated Process: Assessment 11. A 10-year-old child wins the science fair competition and is chosen as a cheerleader for the basketball team. A nurse should recognize that this child is in the process of successfully accomplishing which stage of Eriksons developmental theory?1. Industry versus inferiority2. Identity versus role confusion3. Intimacy versus isolation4. Generativity versus stagnation ANS: 1 Rationale: The nurse should recognize that a 10-year-old child who is successful in school both academically and socially has effectively accomplished the industry versus inferiority developmental stage of Eriksons psychosocial theory. The industry versus inferiority stage of development usually occurs between 6 and 12 years of age, at which time individuals achieve a sense of self-confidence by learning, competing, performing successfully, and receiving recognition from others. Cognitive Level: Application Integrated Process: Assessment 12. A client has flashbacks of sexual abuse by her uncle. She had not had these memories until recently, when she became sexually active with her boyfriend. A nurse should identify this experience as which part of Sullivans concept of the self-system?1. The good me2. The bad me3. The not me4. The bad you ANS: 3 Rationale: The nurse should identify a client remembering sexual abuse when becoming sexually active with her boyfriend as experiencing the not me part of the personality. According to Sullivan, the not me part of the personality develops in response to situations that produced intense anxiety in childhood. Cognitive Level: Application Integrated Process: Evaluation 13. According to Freud, which statement should a nurse associate with predominance of the superego? 1. No one is looking, so I will take three cigarettes from Moms pack.2. I dont ever cheat on tests; it is wrong.3. If I skip school, I will get into trouble and fail my test.4. Dad wont miss this little bit of vodka. ANS: 2 Rationale: The nurse should associate the statement I dont ever cheat on tests; it is wrong as indicative of the predominance of the superego. Freud described the superego as the part of the personality that internalizes the values and morals set forth by primary caregivers. The superego can be referred to as the perfection principle. Cognitive Level: Application Integrated Process: Evaluation 14. A female complains that her husband only satisfies his sexual needs and never her needs. According to Freud, which personality structure should a nurse identify as predominantly driving the husbands actions? 1. The id 2. The superid3. The ego4. The superego ANS: 1 Rationale: The nurse should identify that the husbands actions are driven by the predominance of the id. According to Freud, the id is the part of the personality that is identified as the pleasure principle. The id is the locus of instinctual drives. Cognitive Level: Application Integrated Process: Evaluation 15. A father of a 5-year-old demeans and curses his child for disobedience. In turn, when upset, the child uses swear words at kindergarten. A school nurse recognizes this behavior as unsuccessful completion of which stage of development, according to Peplau? 1. Learning to count on others2. Learning to delay satisfaction3. Identifying oneself4. Developing skills in participation ANS: 3 Rationale: The nurse should identify that the child using swear words in kindergarten has not successfully completed the identifying oneself stage, according to Peplaus interpersonal theory. During this stage of early childhood, a child learns to structure self-concept by observing how others interact with him or her. Cognitive Level: Application Integrated Process: Evaluation 16. A nurse is caring for a hospitalized client who is quarrelsome, opinionated, and has little regard for others. According to Sullivans interpersonal theory, the nurse should associate the clients behaviors with a previous deficit in which stage of development?1. Infancy2. Childhood3. Early adolescence4. Late adolescence ANS: 2 Rationale: The nurse should associate the clients behavior with a deficit in the childhood stage of Sullivans interpersonal theory. The childhood stage in Sullivans interpersonal theory typically occurs from 18 months to 6 years of age, during which the child learns to experience a delay in personal gratification without undue anxiety. Cognitive Level: Application Integrated Process: Evaluation Multiple Response 17. Which of the following concepts should a nurse identify as being included in Black and Andreasens definition of personality? (Select all that apply.) 1. Personality is the characteristic way in which a person thinks, feels, and behaves.2. Personality is the ingrained pattern of behavior that each person evolves, both consciously and unconsciously. 3. Personality is developed in sporadic stages that vary from person to person and experience to experience.4. Personality has to do with a persons style of life or way of being. 5. Personality is inborn and cannot be influenced by developmental progression. ANS: 1, 2, 4 Rationale: Black and Andreasen (2011) define personality as the characteristic way in which a person thinks, feels, and behaves; the ingrained pattern of behavior that each person evolves, both consciously and unconsciously, as his or her style of life or way of being. Cognitive Level: Application Integrated Process: Assessment Fill-in-the-Blank 18. It is never right to take something that doesnt belong to you. According to Sigmund Freud, this statement reflects the predominance of the structure of the personality. ANS: superego Rationale: According to Sigmund Freud, the statement It is never right to take something that doesnt belong to you reflects the predominance of the superego structure of the personality. Freud organized the structure of personality into three major components: the id, the ego, and the superego, which are distinguished by their unique functions and different characteristics. The superego is the perfection principle, in which the values and morals set forth by primary caregivers are internalized. Chapter 30. Complementary and Psychosocial Therapies Multiple Choice 1. A nursing instructor is teaching about complementary therapies. Which student statement indicates that learning has occurred? 1. Complementary therapies view all humans as being biologically similar. 2. Complementary therapies view a person as a combination of multiple, integrated elements. 3. Complementary therapies focus on primarily the structure and functions of the body. 4. Complementary therapies view disease as a deviation from a normal biological state. ANS: 2 Rationale: The nurse should understand that complementary therapies view a person as a combination of multiple, integrated elements. A complementary therapy is an intervention that is used in conjunction with, but is different from, traditional medicine. Cognitive Level: Application Integrated Process: Evaluation 2. A client reports taking St. Johns wort for major depressive episode. The client states, Im taking the recommended dose, but it seems like if two capsules are good, four would be better! Which is an appropriate nursing response? 1. Herbal medicines are more likely to cause adverse reactions than prescription medications. 2. Increasing the amount of herbal preparations can lead to overdose and toxicity. 3. FDA does not regulate herbal remedies, therefore, ingredients are often unknown. 4. Certain companies are better than others. Always buy a reputable brand. ANS: 2 Rationale: The nurse should advise the client that increasing the amount of herbal preparations can lead to overdose and toxicity. The use of herbal medicines, such as St. Johns wort, should be approached with caution and responsibility. This herb is generally recognized as safe when taken at recommended dosages (900 mg/day). Cognitive Level: Application Integrated Process: Implementation 3. A client with chronic lower back pain says, My nurse practitioner told me that acupuncture may enhance the effect of the medications and physical therapy prescribed. What type of therapy is the nurse practitioner recommending? 1. Alternative therapy 2. Physiotherapy 3. Complementary therapy 4. Biopsychosocial therapy ANS: 3 Rationale: The nurse practitioner is recommending a type of complementary therapy. Acupuncture is a healing technique based on ancient Chinese philosophies that has gained wide acceptance in the United States by both patients and physicians. Cognitive Level: Application Integrated Process: Implementation 4. A client diagnosed with chronic migraine headaches is considering acupuncture. The client asks a clinic nurse, How does this treatment work? Which is the best response by the nurse? 1. Western medicine believes that acupuncture stimulates the bodys release of pain-fighting chemicals called endorphins. 2. Im not sure why he suggested acupuncture. There are a lot of risks, including HIV. 3. Acupuncture works by encouraging the body to increase its development of serotonin and norepinephrine. 4. Your acupuncturist is your best resource for answering your specific questions. ANS: 1 Rationale: The most appropriate response by the nurse is to educate the client on the medical philosophy that acupuncture stimulates the bodys release of endorphins. Acupuncture has been found to be effective in the treatment of asthma, insomnia, anxiety, depression, and many other conditions. Cognitive Level: Application Integrated Process: Implementation 5. Alternative approaches refer to interventions that are used instead of conventional treatment. A client asks a nurse to explain the difference between alternative and complementary medicine. Which is an appropriate nursing response? 1. Alternative medicine is a more acceptable practice than complementary medicine. 2. Alternative and complementary medicine are terms that essentially mean the same thing. 3. Complementary medicine disregards traditional medical approaches. 4. Complementary therapies partner alternative approaches with traditional medical practice. ANS: 4 Rationale: The nurse should explain to the client that complementary therapies partner alternative approaches with traditional medicine. More than $33 billion a year is spent on complementary and alternative therapies. Cognitive Level: Application Integrated Process: Implementation 6. A lethargic client is diagnosed with major depressive disorder. After taking antidepressant therapy for 6 weeks, the clients symptoms have not resolved. Which nutritional deficiency should a nurse identify as potentially contributing to the clients symptoms? 1. Vitamin A deficiency 2. Vitamin C deficiency 3. Iron deficiency 4. Folic acid deficiency ANS: 3 Rationale: The nurse should identify that an iron deficiency could contribute to depression. Iron deficiencies can result in feelings of chronic fatigue. Iron should be consumed by eating meat, fish, green leafy vegetables, nuts, eggs, and enriched bread and pasta. Cognitive Level: Application Integrated Process: Assessment 7. A client inquires about the practice of therapeutic touch. Which nursing response best explains the goal of this therapy? 1. The goal is to improve circulation to the body by deep, circular massage. 2. The goal is to re-pattern the bodys energy field by the use of rhythmic hand motions. 3. The goal is to improve breathing by increasing oxygen to the brain and body tissues. 4. The goal is to decrease blood pressure by body toxin release. ANS: 2 Rationale: The nurse should explain that the goal of the practice of therapeutic touch is to re- pattern the bodys energy field by the use of rhythmic hand motions. Therapeutic touch is based on the philosophy that the human body projects fields of energy that become blocked when pain or illness occurs. Therapeutic touch practitioners use this method to correct the blockages and relieve discomfort and improve health. Cognitive Level: Application Integrated Process: Planning 8. A nursing student, having no knowledge of alternative treatments, states, Arent these therapies bogus and, like a fad, will eventually fade away? Which is an accurate nursing response? 1. Like nursing, complementary therapies take a holistic approach to healing. 2. The American Nurses Association is researching the effectiveness of these therapies. 3. It is important to remain nonjudgmental about these therapies. 4. Alternative therapy concepts are rooted in psychoanalysis. ANS: 1 Rationale: The nurse is accurate when comparing complementary therapies to the holistic approach of nursing. The complementary therapies, as well as nursing process, view the person as consisting of multiple, integrated elements. Diagnostic measures are not based on one aspect, but include a holistic assessment of the person. Cognitive Level: Application Integrated Process: Implementation 9. Herbs and plants can be useful in treating a variety of conditions. Which treatment should a nurse determine is appropriate for a client experiencing frequent migraine headaches? 1. Saint Johns wort combined with an antidepressant 2. Ginger root combined with a beta-blocker 3. Feverfew, used according to directions 4. Kava-kava added to a regular diet ANS: 3 Rationale: The nurse should determine that the appropriate treatment for a client experiencing frequent migraine headaches is the herb feverfew. Feverfew is effective in either fresh leaf or freeze-dried form. It is considered to be safe in reasonable doses. Cognitive Level: Application Integrated Process: Evaluation 10. A nurse teaches a client about alternative therapies for back pain. When a practitioner corrects subluxation by manipulating the vertebrae of the spinal column, what therapy is the practitioner employing? 1. Allopathic therapy 2. Therapeutic touch therapy 3. Massage therapy 4. Chiropractic therapy ANS: 4 Rationale: Chiropractic therapy involves the correction of subluxations by manipulating the vertebrae of the spinal column. The theory behind chiropractic medicine is that energy flows from the brain to all parts of the body through the spinal cord and spinal nerves. Cognitive Level: Application Integrated Process: Assessment Multiple Response 11. Which of the following practices should a nurse describe to a client as being incorporated during yoga therapy? (Select all that apply.) 1. Deep breathing 2. Meridian therapy 3. Balanced body postures 4. Massage therapy 5. Meditation ANS: 1, 3, 5 Rationale: Yoga therapy involves deep breathing, balanced body postures, and meditation. The objective of yoga is to integrate the physical, mental, and spiritual energies to enhance health and well-being. Cognitive Level: Application Integrated Process: Implementation 12. A client inquires about pet therapy. Which of the following nursing responses provides the client with accurate information? (Select all that apply.) 1. Pet therapy allows the therapist to assess the clients social relationships. 2. Pet therapy decreases blood pressure. 3. Pet therapy enhances client mood. 4. Pet therapy improves sensory functioning. 5. Pet therapy mitigates the effects of loneliness. ANS: 2, 3, 5 Rationale: Pet therapy has been found to decrease blood pressure, enhance client mood, and mitigate the effects of loneliness. Evidence has shown that animals can directly influence a persons mental and physical well-being. Cognitive Level: Application Integrated Process: Implementation 13. A client who prefers to use St. Johns wort and psychotherapy in lieu of antidepressant therapy asks for tips on using herbal remedies. Which of the following teaching points should a nurse provide? (Select all that apply.) 1. Select a reputable brand. 2. Increasing dosage does not lead to improved effectiveness. 3. Monitor for adverse reactions. 4. Gradually increase dosage to gain maximum effect. 5. Most herbal remedies are best absorbed on an empty stomach. ANS: 1, 2, 3 Rationale: When educating a client on the use of herbal remedies, the nurse should advise the client to select a reputable brand. The nurse should also advise the client to monitor for adverse reactions and to take the recommended dose, because increasing the dose does not lead to improved effectiveness. Herbal remedies are classified as dietary supplements by the Food and Drug Administration (FDA) and, therefore, they are not subject to FDA approval and lack uniform standards of quality control. Cognitive Level: Application Integrated Process: Implementation 14. Which of the following statements reflect current attitudes toward complementary and alternative therapies? (Select all that apply.) 1. Some health insurance companies are beginning to cover treatments such as acupuncture and massage therapy. 2. The majority of third-party payers do not cover chiropractic client treatments. 3. A large number of U.S. medical schools, among them Harvard and Yale, now offer coursework in holistic methods 4. The AMA encourages members to be better informed regarding alternative medicine. 5. Interest in holistic health care is decreasing worldwide. ANS: 1, 3, 4 Rationale: Some health insurance companies and health maintenance organizations (HMOs) appear to be bowing to public pressure by including providers of alternative therapies in their networks of providers for treatments such as acupuncture and massage therapy. Chiropractic care has been covered by some third-party payers for many years. Interest in holistic health care is increasing worldwide. A large number of U.S. medical schoolsamong them Harvard, Yale, Johns Hopkins, and Georgetown Universitiesnow offer coursework in holistic methods. The American Medical Association encourages its members to become better informed regarding the practices and techniques of alternative or unconventional medicine. Cognitive Level: Application Integrated Process: Evaluation 15. Which of the following are included in the U.S. Departments of Agriculture and Health and Human Services guidelines to promote health and prevent disease. (Select all that apply.) 1. Increase physical activity and reduce time spent in sedentary behaviors. 2. Limit total calorie intake to 2,000 mg per day. 3. Reduce daily sodium intake to 3,000 mg per day. 4. Consume less than 10 percent of calories from saturated fatty acids. 5. Limit alcohol consumption to one drink per day for women and two drinks per day for men. ANS: 1, 4, 5 Rationale: The U.S. Departments of Agriculture and Health and Human Services guidelines to promote health and prevent disease include, but are not limited to, the following: Increase physical activity and reduce time spent in sedentary behaviors. Consume less than 10 percent of calories from saturated fatty acids. Limit alcohol consumption to one drink per day for women and two drinks per day for men. Control total calorie intake to manage body weight. For people who are overweight or obese, this will mean consuming fewer calories from foods and beverages. There is no specific daily calorie limit recommended. Reduce daily sodium intake to less than 2,300 mg, not 3,000 mg, and further reduce intake to 1,500 mg among persons who are 51 and older and those of any age who are African American or have hypertension, diabetes, or chronic kidney disease. Cognitive Level: Application Integrated Process: Assessment Fill-in-the-Blank 16. Interventions that are different from, but used in conjunction with, traditional or conventional medical treatment are termed medicine. ANS: complementary Rationale: Interventions that are different from, but used in conjunction with, traditional or conventional medical treatment are termed complementary medicine. Some individuals do not completely abandon conventional medicine for alternative therapies. Instead, they may choose to complement the conventional methods with the addition of alternative strategies. Chapter 31. Cultural and Spiritual Concepts Relevant to Psychiatric Mental Health Nursing Multiple Choice 1. An African American youth, growing up in an impoverished neighborhood, seeks affiliation with a black gang. Soon he is engaging in theft and assault. What cultural consideration should a nurse identify as playing a role in this youths choices? 1. Most African American homes are headed by strong, dominant father figures. 2. Most African Americans choose to remain within their own social organization. 3. Most African Americans are uncomfortable expressing emotions and seek out belonging. 4. Most African Americans have few religious beliefs, which contributes to criminal activity. ANS: 2 Rationale: The nurse should identify that a tendency to remain within ones own social organization may have played a role in the youths choice to join a black gang. African Americans who have assimilated into the dominant culture are likely to be well educated and future focused. Those who have not assimilated may be unemployed or have low-paying jobs and view their future as hopeless, given their previous encounters with racism and discrimination. Cognitive Level: Application Integrated Process: Assessment 2. Northern European Americans value punctuality, hard work, and the acquisition of material possessions and status. A nurse should recognize that these values may contribute to which form of psychopathology? 1. Dissociative disorders 2. Alzheimers dementia 3. Stress-related disorders 4. Schizophrenia-spectrum disorders ANS: 3 Rationale: The nurse should correlate many Northern European American values, such as punctuality, hard work, and acquisition of material possessions, with stress-related disorders. Psychopathology may occur when individuals fail to meet the expectations of the culture. Cognitive Level: Application Integrated Process: Assessment 3. A community health nurse is planning a health fair at a local shopping mall. Which middle- class socioeconomic cultural group should the nurse anticipate would most value preventive medicine and primary health care? 1. Northern European Americans 2. Native Americans 3. Latino Americans 4. African Americans ANS: 1 Rationale: The community health nurse should anticipate that Northern European Americans, especially those who achieve middle-class socioeconomic status, place the most value on preventative medicine and primary health care. This value is most likely related to this groups educational level and financial capability. Many members of the Native American, Latino American, and African American subgroups value folk medicine practices. Cognitive Level: Application Integrated Process: Planning 4. Which rationale by a nursing instructor best explains why it is challenging to globally classify the Asian American culture? 1. Extremes of emotional expression prevent accurate assessment of this culture. 2. Suspicion of Western civilization has understandably resulted in minimal participation in cultural research. 3. The small size of this subpopulation makes research virtually impossible. 4. The Asian American culture includes individuals from Japan, China, Vietnam, Korea, and other countries. ANS: 4 Rationale: The nursing instructors best explanation is that the Asian American culture is difficult to classify globally because of the number of countries that identify with this culture. The Asian American culture includes peoples and descendents from Japan, China, Vietnam, the Philippines, Thailand, Cambodia, Korea, Laos, India, and the Pacific Islands. Within this culture there are vast differences in values, religious practices, languages, and attitudes. Cognitive Level: Application Integrated Process: Assessment 5. A Latin American woman refuses to participate in an assertiveness training group. Which cultural belief should a nurse identify as most likely to affect this clients decision? 1. Future orientation causes the client to devalue assertiveness skills. 2. Decreased emotional expression makes it difficult to be assertive. 3. Assertiveness techniques may not be aligned with the clients definition of the female role. 4. Religious prohibitions prevent the clients participation in assertiveness training. ANS: 3 Rationale: The nurse should identify that the Latin American womans refusal to participate in an assertiveness training group may be affected by the Latin American cultural definition of the female role. Latin Americans place a high value on the family, which is male dominated. The father usually possesses the ultimate authority. Cognitive Level: Application Integrated Process: Evaluation 6. A Latin American man refuses to acknowledge responsibility for hitting his wife, stating instead, Its the mans job to keep his wife in line. Which cultural belief should a nurse associate with this clients behavior? 1. That families are maledominated, with clear male-female role distinctions. 2. That religious tenets support the use of violence in a marital context. 3. That the nuclear family is female-dominated and the mother has ultimate authority. 4. That marriage dynamics are controlled by dominant females in the family. ANS: 1 Rationale: The nurse should associate the cultural belief that families are maledominated, with clear male-female role distinctions with the clients abusive behavior. The father in the Latin American family usually has the ultimate authority. Cognitive Level: Application Integrated Process: Evaluation 7. When working with clients of a particular culture, which action should a nurse avoid? 1. Making direct eye contact 2. Assuming that all individuals who share a culture or ethnic group are similar 3. Supporting the client in participating in cultural and spiritual rituals 4. Using an interpreter to clarify communication ANS: 2 Rationale: The nurse should avoid assuming that all individuals who share a culture or ethnic group are similar. This action constitutes stereotyping and must be avoided. Within each culture, many variations and subcultures exist. Clients should be treated as individuals. Cognitive Level: Application Integrated Process: Implementation 8. To effectively plan care for Asian American clients, a nurse should be aware of which cultural factor? 1. Obesity and alcoholism are common problems. 2. Older people maintain positions of authority within the culture. 3. Tai and chi are the fundamental concepts of Asian health practices. 4. Asian Americans are likely to seek psychiatric help. ANS: 2 Rationale: To effectively care for Asian American clients, the nurse should be aware that older people in this culture maintain positions of authority. Obesity and alcoholism are low among Asian Americans. The balance of yin and yang is the fundamental concept of Asian health practices. Psychiatric illness is often believed to be out-of-control behavior and would be considered shameful to individuals and families. Cognitive Level: Application Integrated Process: Planning 9. A Native American client is admitted to an emergency department (ED) with an ulcerated toe, secondary to uncontrolled diabetes mellitus. The client refuses to talk to a physician unless a shaman is present. Which nursing intervention is most appropriate? 1. Try to locate a shaman that will agree to come to the ED. 2. Explain to the client that voodoo medicine will not heal the ulcerated toe. 3. Ask the client to explain what the shaman can do that the physician cannot. 4. Inform the client that refusing treatment is a clients right. ANS: 1 Rationale: The most appropriate nursing intervention would be to try to locate a shaman that will agree to come to the ED. The nurse should understand that in the Native American culture, religion, and health-care practices are often intertwined. The shaman, a medicine man, may confer with physicians regarding the care of a client. Research supports the importance of both health-care systems in the overall wellness of Native American clients. Cognitive Level: Application Integrated Process: Implementation 10. When planning client care, which folk belief that may affect health-care practices should a nurse identify as characteristic of the Latino American culture? 1. The root doctor is often the first contact made when illness is encountered. 2. The yin and yang practitioner is often the first contact made when illness is encountered. 3. The shaman is often the first contact made when illness is encountered. 4. The curandero is often the first contact made when illness is encountered. ANS: 4 Rationale: The nurse should understand that it is characteristic of Latin American culture for a client to contact a curandero when illness is initially encountered. The curandero is the folk healer who is believed to have a gift from God for healing the sick. Treatments often include supernatural rituals, prayers, magic, practical advice, and indigenous herbs. Cognitive Level: Application Integrated Process: Planning 11. In what probable way should a nurse expect an Asian American client to view mental illness? 1. Mental illness relates to uncontrolled behaviors that bring shame to the family. 2. Mental illness is a curse from God related to immoral behaviors. 3. Mental illness is cured by home remedies based on superstitions. 4. Mental illness is cured by hot and cold herbal remedies. ANS: 1 Rationale: The nurse should except that many Asian Americans are most likely to view mental illness as uncontrolled behavior that brings shame to the family. In addition, it is often more acceptable for mental distress to be expressed as physical ailments. Cognitive Level: Application Integrated Process: Assessment 12. Which cultural considerations should a nurse identify as reflective of Western European Americans? 1. They are present-time oriented and perceive the future as Gods will. 2. They value youth, and older adults are commonly placed in nursing homes. 3. They are at high risk for alcoholism, because of a genetic predisposition. 4. They are future oriented and practice preventive health care. ANS: 1 Rationale: The nurse should identify that most Western European Americans are present oriented and perceive the future as Gods will. Older adults are held in positions of respect and are often cared for in the home instead of in nursing homes. Cognitive Level: Application Integrated Process: Assessment 13. A nurse should recognize that clients who have a history of missed or late medical appointments are most likely to come from which cultural group? 1. African Americans 2. Asian Americans 3. Native Americans 4. Jewish Americans ANS: 3 Rationale: The nurse should recognize that Native American clients might have a history of missed or late medical appointments. Many Native Americans are not ruled by the clock. The concept of time is casual and focused on the present. Cognitive Level: Application Integrated Process: Assessment Multiple Response 14. When interviewing a client of a different culture, which of the following questions should a nurse consider? (Select all that apply.) 1. Would using perfume products be acceptable? 2. Who may be expected to be present during the client interview? 3. Should communication patterns be modified to accommodate this client? 4. How much eye contact should be made with the client? 5. Would hand shaking be acceptable? ANS: 2, 3, 4, 5 Rationale: When interviewing a client from a different culture, the nurse should consider who might be with the client during the interview, modifications of communication patterns, amount of eye contact, and hand-shaking acceptability. Given that cultural influences affect human behavior, its interpretation, and another persons response, it is important for nurses to understand the effects of these cultural influences to work effectively with diverse populations. Cognitive Level: Application Integrated Process: Implementation 15. A female nurse is caring for an Arab American male client. When planning effective care for this client, the nurse should be aware of which of the following cultural considerations? (Select all that apply.) 1. Limited touch is acceptable only between members of the same sex. 2. Conversing individuals of this culture stand far apart and do not make eye contact. 3. Devout Muslim men may not shake hands with women. 4. The man is the head of the household, and women take on a subordinate role. 5. Men of this culture are responsible for the education of their children. ANS: 1, 3, 4 Rationale: When planning effective care for this client, the nurse should be aware that limited touch in this culture is acceptable only between members of the same sex, that devout Muslim men may not shake hands with women, and that women are subordinate to the man, who is the head of household. Conversing individuals of this culture stand close together and maintain eye contact. Arab American women are responsible for the education of children. Cognitive Level: Application Integrated Process: Planning 16. In which of the following cultural groups should a nurse expect to find assessment of mood and affect most challenging, owing to the characteristics of the groups? (Select all that apply.) 1. Arab Americans 2. Native Americans 3. Latino Americans 4. Western European Americans 5. Asian Americans ANS: 2, 5 Rationale: The nurse should expect that both Native Americans and Asian Americans may be difficult to assess for mood and affect. In both cultures, expressing emotions is difficult. Native Americans are encouraged to not communicate private thoughts. Asian Americans may have a reserved public demeanor and may be perceived as shy or uninterested. Cognitive Level: Application Integrated Process: Assessment 17. A nursing instructor is developing a lesson plan to teach about the Northern European American culture. Which of the following information should be included? (Select all that apply.) 1. About half of first marriages end in divorce in this cultural group. 2. This cultural group does not use preventive medicine and primary health care. 3. Punctuality and efficiency are highly valued in this cultural group. 4. This cultural group tends to be future oriented. 5. A typical diet of this cultural group includes rice, vegetables, and fish. ANS: 1, 3, 4 Rationale: With the advent of technology and widespread mobility, less emphasis has been placed on the cohesiveness of the family in the Northern European American culture. Data on marriage, divorce, and remarriage in the United States show that about half of first marriages end in divorce. Northern European Americans, particularly those who achieve middle-class socioeconomic status, value preventive medicine and primary health care. Punctuality and efficiency are highly valued in the culture that promoted the work ethic, and most within this cultural group tend to be future oriented. A typical diet for many Northern European Americans is high in fats and cholesterol and low in fiber. Cognitive Level: Application Integrated Process: Assessment 18. The United States, viewed as a melting pot of multiple worldwide ethnic groups, has its own unique culture that impacts the health and care of individuals. Which of the following are characteristics common to the U.S. culture? (Select all that apply.) 1. The culture values independence, self-reliance, and determining ones life. 2. There is a strong emphasis on achievement in jobs, sports, and physical beauty. 3. Constructive criticism is considered personally offensive. 4. The culture favors structured and formal behaviors, speech, and relationships with others. 5. Overconsumption of food in this culture leads to increased obesity and decreased health. ANS: 1, 2, 5 Rationale: Independence, self reliance, and determining ones life describes the characteristic of individuality. Strong emphasis on achievement in jobs, sports, and physical beauty describes the characteristic of perfectionism. Constructive criticism is considered helpful for others in the U.S. culture. General behaviors, speech, and relationships with others are informal. There is common use of first names when addressing others. The overconsumption of food, leading to increased obesity and decreased health relates to the characteristic of consumerism. Cognitive Level: Application Integrated Process: Assessment Fill-in-the-Blank 19. exists within each individual, regardless of belief system, and serves as a force for interconnectedness between the self and others, the environment, and a higher power. ANS: Spirituality Rationale: Spirituality exists within each individual, regardless of belief system, and serves as a force for interconnectedness between the self and others, the environment, and a higher power. Spirituality is the human quality that gives meaning and sense of purpose to an individuals existence. Chapter 32. Issues Related to Human Sexuality and Gender Dysphoria Multiple Choice 1. A 52-year-old client states, My husband is upset because I dont enjoy sex as much as I used to. Which priority client data should a nurse initially collect? 1. History of hysterectomy 2. Date of last menstrual cycle 3. Use of birth control methods 4. History of thought disorder ANS: 2 Rationale: The nurse should assess the clients last menstrual cycle to determine if the client is experiencing the onset of menopause. Menopause usually occurs around the age of 50. The decrease in estrogen can result in multiple symptoms, including a decrease in biological drives and sexual activity. Cognitive Level: Application Integrated Process: Assessment 2. In the course of an assessment interview, a female client reveals a history of bisexual orientation. Which action should the nurse initially implement when working with this client? 1. Self-assess personal attitudes toward homosexuality. 2. Review clients possible childhood sexual abuse history. 3. Encourage discussion of aversion to heterosexual relationships. 4. Explore clients family history of homosexuality. ANS: 1 Rationale: The nurse should initially self-assess personal attitudes toward homosexuality. The nurse must be able to recognize when negative feelings compromise care. Unconditional acceptance of each individual is an essential component of compassionate nursing. Cognitive Level: Application Integrated Process: Assessment 3. A widower reports a fear of intimacy because of an inability to achieve and sustain an erection. He has become isolative, has difficulty sleeping, and has lost weight over the past year. Which nursing diagnosis should be a priority for this client? 1. Risk for situational low self-esteem AEB inability to achieve an erection 2. Sexual dysfunction R/T dysfunctional grieving AEB inability to experience orgasm 3. Social isolation R/T low self-esteem AEB refusing to engage in dating activities 4. Disturbed body image R/T penile flaccidity AEB client statements ANS: 2 Rationale: The nurse should prioritize the nursing diagnosis sexual dysfunction R/T dysfunctional grieving AEB inability to experience orgasm. The nurse should assess the clients mood and level of energy, because depression and fatigue can decrease desire for participation in sexual activity. Cognitive Level: Analysis Integrated Process: Diagnosis 4. A nurse is assessing a client diagnosed with pedophilic disorder. What would differentiate this sexual disorder from a sexual dysfunction? 1. Symptoms of sexual dysfunction include inappropriate sexual behaviors, whereas symptoms of a sexual disorder include impairment in normal sexual response. 2. Symptoms of a sexual disorder include inappropriate sexual behaviors, whereas symptoms of sexual dysfunction include impairment in normal sexual response. 3. Sexual dysfunction can be caused by increased levels of circulating androgens, whereas levels of circulating androgens do not affect sexual disorders. 4. Sexual disorders can be caused by decreased levels of circulating androgens, whereas levels of circulating androgens do not affect sexual dysfunction. ANS: 2 Rationale: The nurse should identify that pedophilic disorder is a sexual disorder in which individuals partake in inappropriate sexual behaviors. Sexual dysfunction involves impairment in normal sexual response. Pedophilic disorder involves having sexual urges, behaviors, or sexually arousing fantasies involving sexual activity with a prepubescent child. Cognitive Level: Analysis Integrated Process: Assessment 5. A female client on an inpatient unit enters the common area for visiting hours dressed in a see- through blouse. Which intervention should be a nurses first priority? 1. Discuss with the client the inappropriateness of her attire. 2. Avoid addressing her attention-seeking behavior. 3. Lead the client back to her room and assist her with a change of clothing. 4. Restrict client to room until visiting hours are over. ANS: 3 Rationale: The most appropriate intervention by the nurse is to lead the client back to her room and assist her with a change of clothing. The client could be exhibiting symptoms of exhibitionistic disorder, which is characterized by urges to expose oneself to unsuspecting strangers. Cognitive Level: Analysis Integrated Process: Implementation 6. A nurse is working with a client diagnosed with pedophilic disorder. Which client outcome is appropriate for the nurse to expect during the first week of hospitalization? 1. The client will verbalize an understanding of the importance of follow-up care. 2. The client will implement several relapse-prevention strategies. 3. The client will identify triggers for inappropriate behaviors. 4. The client will attend aversion therapy groups. ANS: 3 Rationale: During the first week of hospitalization, identifying triggers for inappropriate behaviors is an appropriate outcome for a client diagnosed with pedophilic disorder. Pedophilic disorder involves intense sexual urges, behaviors, or fantasies involving sexual activity with a prepubescent child. Cognitive Level: Application Integrated Process: Planning 7. When planning care for a client diagnosed with female sexual interest/arousal disorder, what should a nurse document as an expected outcome of senate focus exercises? 1. To initiate immediate orgasm 2. To reduce anxiety by eliminating physical touch 3. To focus on touching breasts and genitals 4. To reduce goal-oriented demands of intercourse ANS: 4 Rationale: Female sexual interest/arousal disorder is characterized by a reduced or absent frequency or intensity of interest or pleasure in sexual activity. Senate focus exercises are highly structured touching activities designed to help overcome performance anxiety and increase comfort with physical intimacy. The expected outcome of senate focus exercises is to reduce goal-oriented demands of intercourse. The reduction in demands reduces performance pressures and anxiety associated with possible failure. Cognitive Level: Application Integrated Process: Planning 8. A newly married woman comes to a gynecology clinic reporting anorexia, insomnia, and extreme pain during intercourse that has affected her intimate relationship. What initial intervention should the nurse expect a physician to implement? 1. A thorough physical, including gynecological examination 2. Referral to a sex therapist 3. Assessment of sexual history and previous satisfaction with sexual relationships 4. Referral to the recreational therapist for relaxation therapy ANS: 1 Rationale: The nurse should expect the physician to implement a thorough physical, including a gynecological examination to assess for any physiological causes of the clients symptoms. If no pathology exists the client may be diagnosed with genito-pelvic pain/penetration disorder. In this disorder, the individual experiences considerable difficulty with vaginal intercourse and attempts at penetration. Pain is felt in the vagina, around the vaginal entrance and clitoris, or deep in the pelvis. There is fear and anxiety associated with anticipation of pain or vaginal penetration. A tensing and tightening of the pelvic floor muscles occurs during attempted vaginal penetration. Cognitive Level: Application Integrated Process: Implementation 9. A nurse is instructing a client diagnosed with sexual female sexual interest/arousal disorder. Which symptom and treatment of this disorder should the nurse describe to the client? 1. Avoidance of all genital sexual contact treated by sensate focus exercises 2. Avoidance of all genital sexual contact treated by medicating with tadalafil (Cialis) 3. Anorgasmia treated by vardenafil (Levitra) 4. Anorgasmia treated by systematic desensitization ANS: 1 Rationale: The nurse should explain to the client that female sexual interest/arousal disorder is characterized by a reduced or absent frequency or intensity of interest or pleasure in sexual activity. Senate focus exercises are highly structured touching activities designed to help overcome performance anxiety and increase comfort with physical intimacy. Cognitive Level: Application Integrated Process: Implementation 10. A psychiatric nursing instructor is teaching about the psychological effects of the diagnosis of a sexually transmitted disease (STD). Which student statement indicates that further instruction is needed? 1. STDs carry strong connotations of illicit sex and considerable social stigma. 2. STDs can cause insanity. 3. AIDS can generate hopelessness and helplessness. 4. Antibiotics administered in the early stages can cure all STDs. ANS: 4 Rationale: The instructor should identify the need for further instruction if a student states that antibiotics can cure all STDs. STDs refer to infections that are contracted primarily through sexual activities or intimate contact. Antibiotics are ineffective in the treatment of the STD human immunodeficiency virus (HIV). Cognitive Level: Application Integrated Process: Evaluation 11. A nurse is counseling a client diagnosed with gender dysphoria. What criteria would differentiate this disorder from a transvestic disorder? 1. Clients diagnosed with transvestic disorder are dissatisfied with their gender, whereas clients diagnosed with gender dysphoria are not. 2. Clients diagnosed with gender dysphoria are dissatisfied with their gender, whereas clients diagnosed with transvestic disorder are not. 3. Clients diagnosed with gender dysphoria avoid all forms of sexual intercourse, whereas clients diagnosed with transvestic disorder do not. 4. Clients diagnosed with transvestic disorder avoid all forms of sexual intercourse, whereas clients diagnosed with gender dysphoria do not. ANS: 2 Rationale: The nurse should identify that clients diagnosed with gender dysphoria are dissatisfied with their gender, whereas clients diagnosed with transvestic disorder experience intense sexual arousal from dressing in the clothes of the opposite gender but are not dissatisfied with their gender. Clients diagnosed with either of these disorders do not avoid all forms of sexual intercourse. Cognitive Level: Analysis Integrated Process: Implementation 12. A nurse is assessing a client diagnosed with sexual masochistic disorder. What would differentiate this paraphilic disorder from sexual sadistic disorder? 1. Symptoms of sexual masochistic disorder are chronic acts of humiliation, whereas symptoms of sexual sadistic disorder are acute. 2. Symptoms of sexual sadistic disorder are chronic acts of humiliation, whereas symptoms of sexual masochistic disorder are acute. 3. Masochistic acts can be performed alone, whereas sadistic acts must have a consenting or non- consenting partner. 4. Sadistic acts can be performed alone, whereas mascochistic acts must have a consenting or non-consenting partner. ANS: 3 Rationale: The identifying feature of sexual masochistic disorder is recurrent and intense sexual arousal when being humiliated, beaten, bound, or otherwise made to suffer. These masochistic activities may be fantasized and may be performed alone (e.g., self-inflicted pain) or with a partner. The identifying feature of sexual sadistic disorder is the recurrent and intense sexual arousal from the physical or psychological suffering of another individual. Both sexual masochistic and sadistic disorders are chronic in nature. Cognitive Level: Analysis Integrated Process: Assessment 13. A nurse is assessing a client diagnosed with fetishistic disorder. What would differentiate this paraphilic disorder from frotteuristic disorder? 1. To derive sexual excitement, fetishistic disorder involves the use of nonliving objects, whereas frotteuristic disorder involves touching and rubbing against non-consenting people. 2. To derive sexual excitement, frotteuristic disorder involves the use of nonliving objects, whereas fetishistic disorder involves touching and rubbing against non-consenting people. 3. Clients diagnosed with frotteuristic disorder are heterosexual cross-dressing males, whereas Clients diagnosed with fetishistic disorder are homosexual cross-dressing males. 4. Clients diagnosed with fetishistic disorder are heterosexual cross-dressing males, whereas Clients diagnosed with frotteuristic disorder are homosexual cross-dressing males. ANS: 1 Rationale: Fetishistic disorder involves recurrent and intense sexual arousal from the use of either nonliving objects or specific nongenital body part(s). Frotteuristic disorder is the recurrent and intense sexual arousal involving touching and rubbing against a non-consenting person. Transvestic disorder involves recurrent and intense sexual arousal from dressing in the clothes of the opposite gender. Cognitive Level: Analysis Integrated Process: Assessment Multiple Response 14. Which of the following characteristics should a nurse identify as normal in the development of human sexuality for an 11-year-old child? (Select all that apply.) 1. The child experiments with masturbation. 2. The child may experience homosexual play. 3. The child shows little interest in the opposite sex. 4. The child shows little concern about physical attractiveness. 5. The child is unlikely to want to undress in front of others. ANS: 1, 2, 5 Rationale: The nurse should identify that experimenting with masturbation and homosexual play and not wanting to undress in front of others are characteristics that are normal in the development of human sexuality in an 11-year-old child. Interest in the opposite sex usually increases, and children often become self-conscious about their bodies. Cognitive Level: Application Integrated Process: Assessment 15. A nursing instructor is teaching about the various categories of paraphilic disorders. Which categories are correctly matched with expected behaviors? (Select all that apply.) 1. Exhibitionistic disorder: Mary models lingerie for a company that specializes in home parties. 2. Voyeuristic disorder: John is arrested for peering in a neighbors bathroom window. 3. Frotteuristic disorder: Peter enjoys subway rush-hour female contact that results in arousal. 4. Pedophilic disorder: George can experience an orgasm by holding and feeling shoes. 5. Fetishistic disorder: Henry masturbates into his wifes silk panties. ANS: 2, 3, 5 Rationale: Categories of paraphilic disorders include voyeuristic disorder (observing unsuspecting people, who are naked, dressing, or engaged in sexual activity), frotteuristic disorder (touching or rubbing against a non-consenting person), and fetishistic disorder (using nonliving objects in sexual ways). Exhibitionistic disorder is a paraphilic disorder but involves the urge to show ones genitals to unsuspecting strangers. Other categories include sexual masochism disorder, sexual sadism disorder, and transvestic disorder. Cognitive Level: Analysis Integrated Process: Implementation 16. A client is diagnosed with erectile disorder. Which of the following medications would address this condition, and what is the therapeutic action of the drug? (Select all that apply.) 1. Phentolamine (Oraverse); increases blood flow to the penis. 2. Apomorphine (Apokyn); acts directly on the dopamine receptors in the brain. 3. Vardenafil (Levitra); blocks the action of phosphodiesterase-5 (PDE5). 4. Goserelin (Zoladex); inhibits the production of gonadotropins. 5. Sildenafil (Viagra); blocks the action of phosphodiesterase-5 (PDE5). ANS: 1, 2, 3, 5 Rationale: Sildenafil (Viagra), tadalafil (Cialis), and vardenafil (Levitra) have been approved by the FDA for the treatment of erectile disorder. These newer impotence agents block the action of phosphodiesterase-5 (PDE5), an enzyme that breaks down cyclic guanosine monophosphate (cGMP), a compound that is required to produce an erection. Phentolamine has been used in combination with papaverine in an injectable form that increases blood flow to the penis, resulting in an erection. Apomorphine acts directly on the dopamine receptors in the brain. This mode of stimulating dopamine in the brain is thought to enhance the sexual response. Zoladex is a treatment for prostate cancer, not erectile dysfunction. Cognitive Level: Application Integrated Process: Evaluation 17. A nurse is planning care for a child diagnosed with gender dysphoria. Which of the following nursing diagnoses could potentially document this clients problems? (Select all that apply.) 1. Low self-esteem R/T rejection by peers 2. Self-care deficit R/T isolative behaviors 3. Disturbed personal identity R/T parenting patterns 4. Impaired social interactions R/T socially unacceptable behaviors 5. Activity intolerance R/T fatigue ANS: 1, 3, 4 Rationale: Based on the data collected during a nursing assessment, possible nursing diagnoses for the child with gender dysphoria may include the following: Disturbed personal identity related to biological factors or parenting patterns that encourage culturally unacceptable behaviors for assigned gender, impaired social interaction related to socially and culturally unacceptable behaviors, and low self-esteem related to rejection by peers. Self-care deficit and activity intolerance do not address the typical problems of clients diagnosed with gender dysphoria. Cognitive Level: Analysis Integrated Process: Diagnosis Fill-in-the-Blank 18. is the constitution and life of an individual relative to characteristics regarding intimacy. ANS: Sexuality Rationale: Sexuality is the constitution and life of an individual relative to characteristics regarding intimacy. It reflects the totality of the person and does not relate exclusively to the sex organs or sexual behavior. [Show More]
Last updated: 7 months ago
Preview 1 out of 86 pages
Instant download
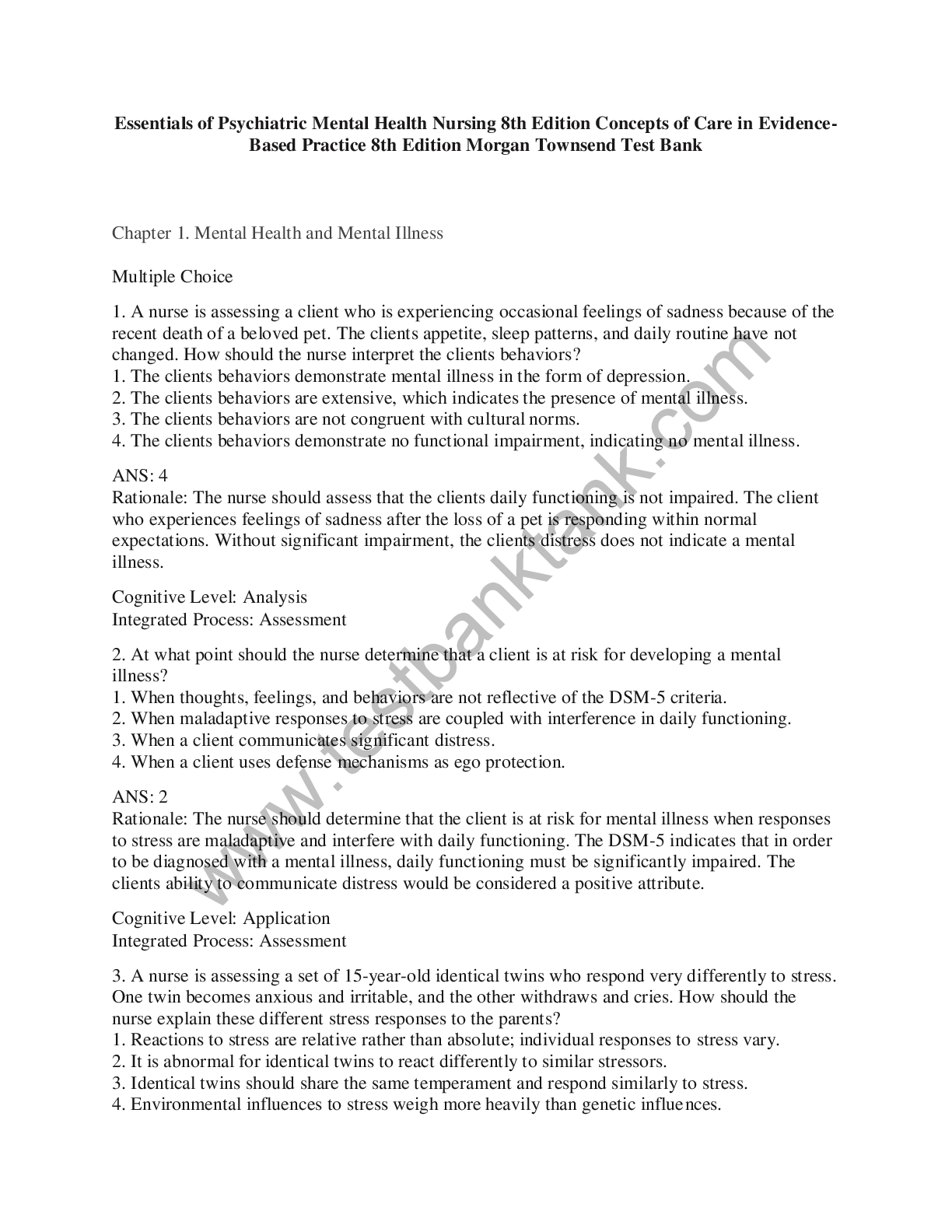
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 16, 2023
Number of pages
86
Written in
Additional information
This document has been written for:
Uploaded
Oct 16, 2023
Downloads
0
Views
62