*NURSING > QUESTIONS and ANSWERS > TEST BANK FOR MEDICAL SURGICAL CONCEPTS AND PRACTICE 3RD EDITION BY DEWIT 48 COMPLETE CHAPTERS DOWNL (All)
TEST BANK FOR MEDICAL SURGICAL CONCEPTS AND PRACTICE 3RD EDITION BY DEWIT 48 COMPLETE CHAPTERS DOWNLOAD TO SCORE A+
Document Content and Description Below
Chapter 01: Caring for Medical-Surgical Patients deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. Which statement accurately describes the primary purpose of the... state nurse practice act (NPA)? a. To test and license LPN/LVNs. b. To define the scope of LPN/LVN practice. c. To improve the quality of care provided by the LPN/LVN. d. To limit the LPN/LVN employment placement. ANS: B While improving quality of care provided by the LPN/LVN may be a result of the NPA, the primary purpose of the NPA of each state defines the scope of nursing practice in that state. PTS: 1 DIF: Cognitive Level: Comprehension REF: 2 OBJ: 3 TOP: NPA KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 2. The charge nurse asks the new vocational nurse to start an intravenous infusion, a skill that the vocational nurse has not been taught during her educational program. How should the vocational nurse respond? a. Ask a more experienced nurse to demonstrate the procedure. b. Look up the procedure in the procedure manual. c. Attempt to perform the procedure with supervision. d. Inform the charge nurse of her lack of training in this procedure. ANS: D The charge nurse should be informed of the lack of training to perform the procedure, and the vocational nurse should seek further training to gain proficiency. Although the other options might be helpful, they are not safe. PTS: 1 DIF: Cognitive Level: Application REF: 3 OBJ: 1 TOP: Providing Safe Care KEY: Nursing Process Step: N/A MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 3. Which patient statement indicates a need for further discharge teaching that the vocational nurse should address? a. “I have no idea of how this drug will affect me.” b. “Do you know if my physician is coming back today?” c. “Will my insurance pay for my stay?” d. “Am I going to have to go to a nursing home?” ANS: A Lack of knowledge at discharge about medication effects and side effects is a concern that should be addressed by the vocational nurse. The other concerns in the options are the responsibility of other departments to which the nurse might refer the patient. PTS: 1 DIF: Cognitive Level: Application REF: 2 OBJ: 1 TOP: Teaching KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 4. According to most state NPAs, the vocational nurse acting as charge nurse in a long-term care facility acts in which capacity? a. Working under direct supervision of an RN on the unit b. Working with the RN in the building c. Working under general supervision by the RN available on site or by phone d. Working as an independent vocational nurse ANS: C The vocational nurse in the capacity of the charge nurse in a long-term care facility acts with the general supervision of an RN available on site or by phone. PTS: 1 DIF: Cognitive Level: Comprehension REF: 2 OBJ: 1 TOP: Charge Nurse/Manager KEY: Nursing Process Step: N/A MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 5. The nurse is educating a patient that is a member of a health maintenance organization (HMO). Which information should the nurse include? a. Seek the opinion of an alternate health care provider. b. Obtain insurance approval for medical services prior to treatment. c. Provide detailed documentation of all care received for his condition. d. Wait at least 6 months to see a specialist. ANS: B Most HMOs require preprocedure authorization for treatment. Patients are not required to seek a second opinion, provide documentation of care, or wait a specific time period before visiting a specialist. PTS: 1 DIF: Cognitive Level: Application REF: 9 OBJ: 9 TOP: Charge Nurse/Manager KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 6. The patient complains to the nurse that he is confused about his “deductible” that he owes the hospital. Which statement accurately explains a deductible? a. An amount of money put aside for the payment of future medical bills b. A one-time fee for service c. An amount of money deducted from the bill by the insurance company d. An annual amount of money the patient must pay out-of-pocket for medical care ANS: D The deductible is the annual amount the insured must pay out-of-pocket prior to the insurance company assuming the cost. This practice improves the profit of the insurance company. PTS: 1 DIF: Cognitive Level: Comprehension REF: 7 OBJ: 9 TOP: Health Care Financing KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 7. The nurse compares the characteristics of a health maintenance organization (HMO) and a preferred provider organization (PPO). Which information should the nurse include about HMOs? a. HMOs require a set fee of each member monthly. b. HMOs allow the member to select his health care provider. c. HMOs permit admission to any facility the member prefers. d. HMOs offer unlimited diagnostic tests and treatments. ANS: A HMOs require a set fee from each member monthly (capitation). The patient will be treated by the HMO staff in HMO-approved facilities. Excessive use of diagnostic tests and treatments is discouraged by the HMO. PTS: 1 DIF: Cognitive Level: Application REF: 9 OBJ: 9 TOP: Managed Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 8. A patient asks the nurse what Medicare Part A covers. Which response is correct? a. Medicare Part A covers inpatient hospital costs. b. Medicare Part A covers reimbursement to the physician. c. Medicare Part A covers outpatient hospital services. d. Medicare Part A covers ambulance transportation. ANS: A Medicare Part A covers inpatient hospital expenses, drugs, x-rays, laboratory work, and intensive care. Medicare Part B pays the physician, ambulance transport, and outpatient services. PTS: 1 DIF: Cognitive Level: Comprehension REF: 7, Box 1-4 OBJ: 9 TOP: Government-Sponsored Health Insurance KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 9. Which is the main cost-containment component of diagnosis-related groups (DRGs)? a. Hospitals focus only on the specific diagnosis. b. Hospitals treat and discharge patients quickly. c. Reduced cost drugs are ordered for specific diagnoses. d. Diagnostic group classification streamlines care. ANS: B DRGs are a prospective payment plan in which hospitals receive a flat fee for each patient’s diagnostic category regardless of the length of time in the hospital. If hospitals can treat and discharge patients before the allotted time, hospitals get to keep the excess payment; cost is contained, and the patient is discharged sooner. PTS: 1 DIF: Cognitive Level: Comprehension REF: 8 OBJ: 9 TOP: Government-Sponsored Health Insurance KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 10. The nurse is assessing a group of patients. Which patient would most likely qualify for Medicaid? a. A 35-year-old unemployed single mother with diabetes b. A 70-year-old Medicare recipient with retirement income who needs to be in a long-term care facility c. An 80-year-old blind woman living in her own home who has inadequate private insurance d. A 67-year-old stroke victim with Medicare Part A and an income from investments ANS: A Medicaid is a joint effort of federal and state governments geared primarily for low-income people with no insurance. PTS: 1 DIF: Cognitive Level: Application REF: 8, Box 1-5 OBJ: 9 TOP: Government-Sponsored Health Insurance–Medicaid KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 11. Which area is the major focus of Healthy People 2020 and the primary mechanism through which to improve the health of Americans in the second decade of the century? a. Research funding b. Health information distribution c. Healthy lifestyle encouragement d. Health improvement program designs ANS: C Healthy People 2020 focuses on expanding ongoing programs to include support and information to reduce infant mortality, cancer, cardiovascular disease, and HIV/AIDS, and to increase effective immunizations, healthy eating habits, and healthy weight. PTS: 1 DIF: Cognitive Level: Comprehension REF: 6 OBJ: 7 TOP: Healthy People 2020 KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 12. Which term explains the type of care that addresses interventions for all dimensions of a patient’s life? a. Focused care b. General care c. Directed care d. Holistic care ANS: D Holistic care addresses the physiologic, psychological, social, cultural, and spiritual needs of the patient. PTS: 1 DIF: Cognitive Level: Comprehension REF: 6 OBJ: 8 TOP: Holistic Care KEY: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity: Coping and Adaptation 13. A patient furiously says, “My doctor was so busy giving me instructions that he didn’t hear what I was trying to ask him!” Which response is most empathetic? a. “When people ignore me, I really get mad.” b. “I’m sure that the doctor was rushed and unaware of your needs.” c. “I’ll bet that made you feel very frustrated.” d. “Take a deep breath and plan what you will say to him tomorrow.” ANS: C Empathy demonstrates that the nurse perceives the patient’s feelings but does not share the emotion. Belittling the patient’s feelings, showing sympathy, or defending the doctor makes the patient feel devalued. PTS: 1 DIF: Cognitive Level: Analysis REF: 10 OBJ: 10 TOP: Nurse–Patient Relationship KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 14. The nurse is explaining differences in a therapeutic relationship and a social relationship to a patient. Which information about therapeutic relationships is most important for the nurse to include in the explanation? a. Therapeutic relationships lack formal boundaries. b. Therapeutic relationships are goal directed. c. Therapeutic relationships meet the needs of each person in the relationship. d. Therapeutic relationships extend past the hospitalization period. ANS: B The therapeutic relationship is focused on the patient and is goal directed and designed to meet only the needs of the patient and does not extend past the period of hospitalization. PTS: 1 DIF: Cognitive Level: Comprehension REF: 9 OBJ: 10 TOP: Therapeutic Relationship KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 15. The long-term care facility nurse is caring for a newly admitted 80-year-old patient who is depressed. Which approach is best for the nurse to employ? a. Encourage the resident to engage in an activity. b. Remind the resident of reasons to be positive. c. Point out episodes of negative behavior. d. Present a bright and cheerful behavior. ANS: A Activity and social interaction are helpful to depressed patients. Presenting a cheery approach and pointing out negative behavior and reasons to be positive are not therapeutic at this stage of the relationship. PTS: 1 DIF: Cognitive Level: Analysis REF: 10 OBJ: 10 TOP: Depressed Behavior KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 16. The nurse is caring for a patient who has been on antidepressants for 3 days. The patient tearfully says, “I still feel terrible. I don’t think anything can help how I feel.” Which response is best? a. “I will tell the charge nurse how you are feeling.” b. “You just need to be patient and give your medicine some time to work.” c. “Look how much you have improved since you were admitted to the facility.” d. “It must be frustrating to be going through this difficult time.” ANS: D This response is an empathetic response that allows for further exploration of the patient’s feelings. The other responses will block communication with this patient. PTS: 1 DIF: Cognitive Level: Application REF: 9 OBJ: 10 TOP: Therapeutic Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 17. An overweight male patient rips off his hospital gown, throws it out the door, and shouts, “I’m not wearing this stupid gown! It is too small, too short, and exposes my backside to the world!” Which response is most appropriate? a. Remind patient of the need to wear the gown for convenience in care. b. Confer with the patient for methods to acquire a larger gown. c. Replace the torn gown with another. d. Inform the charge nurse of the hostile behavior. ANS: B Allowing hostile patients to make reasonable requests defuses the anger and allows patients to vent their feelings. PTS: 1 DIF: Cognitive Level: Application REF: 9 OBJ: 10 TOP: Hostile Behavior KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: Coping and Adaptation 18. The nurse is caring for a patient who states, “You are the only nurse who understands about my pain. Can’t you give me an extra dose of pain medication?” How should the nurse respond to the patient’s request? a. Explain that dosage schedules are by physician’s orders. b. Ignore the request. c. Tell the patient that his behavior is manipulative. d. Agree to give an extra dose of pain medication. ANS: A A matter-of-fact response to a manipulative request limits the effect of the manipulation, thereby helping the nurse to avoid becoming defensive or being swayed by flattery. PTS: 1 DIF: Cognitive Level: Application REF: 9 OBJ: 10 TOP: Manipulative Behavior KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 19. A female patient who has recently been diagnosed with an inoperable brain tumor asks the nurse, “Do you think God punishes us?” Which response demonstrates therapeutic communication? a. “What do you think?” b. “God loves you.” c. “Would like to speak with the chaplain?” d. “God will not give you more than you can bear.” ANS: A Sitting with the patient and offering oneself to listen to the patient’s concerns and encouraging reflection is the best approach rather than responding with a cliché or suggesting speaking with the chaplain. PTS: 1 DIF: Cognitive Level: Application REF: 10 OBJ: 10 TOP: Spiritual Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 20. The nurse is communicating with a patient who voices concern about an upcoming high-risk procedure. Which statement best demonstrates empathy? a. “Would you like to talk about your feelings regarding the procedure?” b. “My mother had the same procedure and did very well.” c. “I can’t imagine how you feel.” d. “It must be difficult preparing for the procedure; how are you feeling?” ANS: D This statement by the nurse displays empathy by trying to place oneself in the patient’s circumstance and validating the patient’s feelings. Simply asking patients if they would like to talk about their feelings does not show empathy and may elicit a “yes” or “no” response. Telling the patient one’s mother had the procedure or stating “I can’t imagine how you feel” does not show empathy toward the patient. PTS: 1 DIF: Cognitive Level: Application REF: 10 OBJ: 10 TOP: Nurse–Patient Relationship KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity MULTIPLE RESPONSE 21. Which of the following are sources of clear guidelines for upholding clinical standards for safe and competent care? (Select all that apply.) a. The state’s nurse practice act (NPA) b. The State Board of Nurse Examiners (BNE) c. The National Association for Practical Nurse Education and Service (NAPNES) d. Institutional policies e. The National Federation of Licensed Practical Nurses, Inc. (NFLPN) ANS: C, E NAPNES and the NFLPN give clear guidelines for clinical standards that can be used as a basis for court decisions. The NPA has broad guidelines, and institutional policies may not be complete. The BNE enforces the NPA. PTS: 1 DIF: Cognitive Level: Comprehension REF: 5 OBJ: 3 TOP: Upholding Clinical Standards KEY: Nursing Process Step: N/A MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 22. Which statement(s) accurately describes the role of the LPN/LVN regardless of employment placement? (Select all that apply.) a. Uphold clinical standards b. Educate patients c. Communicate effectively d. Collaborate with the health care team e. Initiate a care plan immediately after admission ANS: A, B, C, D The LPN/LVN has the accountability to uphold clinical standards, educate patients, communicate effectively, and collaborate with the health care team. Depending on the type of facility, initiation of a care plan is often the role of the registered nurse. PTS: 1 DIF: Cognitive Level: Comprehension REF: 2 OBJ: 3 TOP: Roles of LPN/LVNs KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 23. The newly licensed LPN/LVN demonstrates an understanding of employment opportunities when applying to a position in which area(s)? (Select all that apply.) a. An outpatient clinic b. A home health care agency c. An intravenous (IV) therapy team d. A long-term care facility e. An ambulatory care unit ANS: A, B, D, E With the exception of an IV therapy team, which requires postgraduate education and/or certification, the other options are open to newly graduated vocational nurses. PTS: 1 DIF: Cognitive Level: Application REF: 2 OBJ: 2 TOP: Employment Opportunities for LPN/LVNs KEY: Nursing Process Step: N/A MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 24. What factor(s) should the LPN/LVN consider when delegating a task to unlicensed assistive personnel (UAP)? (Select all that apply.) a. A need for the UAP to voluntarily accept the task delegated b. Continued accountability for the task by the LPN/LVN c. Assurance that the task requires no further need for supervision of the UAP d. An understanding that the task is in the job description of the UAP e. A transfer of authority to the UAP ANS: A, B, D, E Delegation is a considered act involving the condition of the patient and the competency of the UAP. Delegation requires that the UAP voluntarily accept the task, which is in the job description of the UAP. The vocational nurse has transferred authority for the completion of the task but is still accountable and should supervise. PTS: 1 DIF: Cognitive Level: Application REF: 3 OBJ: 1 TOP: Delegation KEY: Nursing Process Step: N/A MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 25. The LPN/LVN participates in an in-service about cost containment within the health care facility. Which action(s) demonstrate understanding of cost-containment principles? (Select all that apply.) a. Telling patients to limit their usage of supplies. b. Asking the UAP to ensure correct charges for patient care items. c. Only using necessary items for patient care. d. Charging for extra patient care items that the patient may take home upon discharge. e. Documenting supplies used for patients in their patient care record. ANS: B, C, E The UAP must correctly charge patients utilizing the facility’s charging system, only necessary supplies should be used for patient care, and documenting supplies used assists in reimbursement. It is inappropriate and not the patient’s responsibility to monitor their supply use, and excess charges would be incurred if items were given to the patient upon discharge. PTS: 1 DIF: Cognitive Level: Application REF: 6 OBJ: 8 TOP: Cost Containment KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Management of Care COMPLETION 26. When an insurance company directly reimburses a licensed health care provider for services, the form of financing is called ______________. ANS: fee for service Fee for service is the direct reimbursement by an insurance company to a health care provider. PTS: 1 DIF: Cognitive Level: Comprehension REF: 7 OBJ: 9 TOP: Health Care Financing KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 27. The nurse explains that the term _____________ refers to the severity of illness. ANS: acuity Acuity is the term referring to the severity of illness or condition of a patient. PTS: 1 DIF: Cognitive Level: Knowledge REF: 4 OBJ: 6 TOP: Acuity KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care Chapter 02: Critical Thinking and the Nursing Process deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. Which foundational behavior is necessary for effective critical thinking? a. Unshakable beliefs and values b. An open attitude c. An ability to disregard evidence inconsistent with set goals d. An ability to recognize the perfect solution ANS: B An open attitude not clouded by unshakable beliefs and values or preset goals allows the application of critical thinking. Acceptance that there may not be a perfect solution leaves the field open to new ideas. PTS: 1 DIF: Cognitive Level: Comprehension REF: 16, Box 2-1 OBJ: 2 (theory) TOP: Factors Influencing Critical Thinking KEY: Nursing Process Step: N/A MSC: NCLEX: Health Promotion and Maintenance 2. Which fundamental belief underscores the basis of the nursing process? a. Recognition that basic needs must be met by the individual without assistance. b. Acknowledgment that patients and families appreciate an efficient health care system that functions without their input. c. A focus on disease control as the most important aspect of patient care. d. Recognition that all people have worth and dignity. ANS: D The nursing process is based on the belief that all people have worth and dignity. Patient-centered care that is applied to all aspects of the patient’s health, and is not just disease oriented, is appreciated by the family and patient. Holistic care approach can support the patient to meet basic needs. PTS: 1 DIF: Cognitive Level: Comprehension REF: 17 OBJ: 5 (theory) TOP: Basic Beliefs Pertinent to the Nursing Process KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 3. The nurse is assessing a new patient who complains of his chest feeling tight. The patient displays a temperature of 100° F and an oxygen saturation of 89%, and expectorates frothy mucus. Which finding is an example of subjective data? a. Temperature b. Oxygen saturation c. Frothy mucus d. Chest tightness ANS: D Subjective data is information given by the patient that cannot be measured otherwise. The other data are considered objective data. Objective data are pieces of information that can be measured by the examiner. The nurse should avoid making judgments or conclusions when obtaining data. PTS: 1 DIF: Cognitive Level: Application REF: 18 OBJ: 8 (clinical) TOP: Assessment Data KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 4. The nurse is caring for a newly admitted patient who is describing his recent symptoms to the nurse. This scenario is an example of which type of source? a. Primary b. Objective c. Secondary d. Complete ANS: A The patient is the primary source of information. Objective refers to a type of data obtained by the nurse that is measured or can be verified through assessment techniques, secondary information is obtained from relatives or significant others, and information is not necessarily complete when the patient is the source. PTS: 1 DIF: Cognitive Level: Application REF: 19 OBJ: 8 (clinical) TOP: Sources of Information KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 5. The nurse is performing an intake interview on a new resident to the long-term care facility. The nurse detects the odor of acetone from the patient’s breath. Which term accurately describes this assessment? a. Inspection b. Observation c. Auscultation d. Olfaction ANS: D Olfaction is an assessment method of smells. Inspection and observation use the sense of vision. Auscultation refers to use of the sense of hearing. PTS: 1 DIF: Cognitive Level: Comprehension REF: 20 OBJ: 9 (clinical) TOP: Olfaction KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 6. During a morning assessment, the nurse observes that the patient displays significant edema of both feet and ankles. Which statement best documents these findings? a. Pitting edema present in both feet and ankles b. Edema in both feet and ankles approximately 4 mm deep c. 4 mm pitting edema quickly resolving d. Bilateral pitting edema in feet and ankles, 4 mm deep, resolving in 3 seconds ANS: D Edema should be recorded as to location, depth of pitting, and time for resolution. PTS: 1 DIF: Cognitive Level: Application REF: 20 OBJ: 9 (theory) TOP: Palpation KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 7. Which technique should the nurse employ to best assess skin turgor? a. Examine mucous membranes of the mouth. b. Compare limbs for similar color. c. Pinch a skinfold on chest to assess for tenting. d. Palpate the ankles for evidence of pitting edema. ANS: C Skin turgor can be assessed by tenting the skin on the chest and recording the speed at which the “tent” subsides. PTS: 1 DIF: Cognitive Level: Comprehension REF: 22 OBJ: 9 (clinical) TOP: Practical Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 8. Which example shows that the nursing student demonstrates compliance with the Health Insurance Portability and Accountability Act (HIPAA)? a. The student uses the patient’s full name only on clinical assignments submitted to the instructor. b. The student uses the facility printer to copy laboratory reports on an assigned patient. c. The student shreds any documents that contain identifying patient information before leaving the clinical facility. d. The student asks the patient for permission to copy laboratory and diagnostic reports for educational purposes. ANS: C HIPAA forbids any information used for educational purposes to have any identifying information; therefore, shredding documents would be appropriate. Full names on documents, printing copies of chart forms, and asking the patient for permission to copy forms would be violations of HIPAA regulations. PTS: 1 DIF: Cognitive Level: Comprehension REF: 26 OBJ: 4 (theory) TOP: HIPAA KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 9. The diabetic patient who had blood drawn for an HbA1c level says, “I don’t know why they want to look at my hemoglobin.” Which response is most appropriate for the nurse to make? a. “Diabetes increases your risk of bleeding.” b. “The HbA1c provides information relative to blood sugar levels for the last 2 to 3 months.” c. “Hemoglobin levels and blood sugar levels are closely related.” d. “The HbA1c tells if you have type 1 or type 2 diabetes.” ANS: B HbA1c evaluates the average blood glucose level for the last 2 to 3 months. By explaining the purpose of the common laboratory test (HgbA1c) and its relationship to diabetes, the nurse answers the patient’s question and clearly communicates relevant data. PTS: 1 DIF: Cognitive Level: Comprehension REF: 25, 27 OBJ: 8 (clinical) TOP: Diagnostic Studies KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 10. The nurse is caring for a patient with the problem statement/nursing diagnosis of Risk for Impaired Skin Integrity Related to Immobility. Which goal/outcome statement best correlates with this diagnosis? a. The patient will sit in chair at bedside for 15 minutes after each meal. b. The nurse will assist the patient to chair every shift. c. The nurse will assess skin and record condition every shift. d. The patient will change positions frequently. ANS: A The goal/outcome statement is directed at the etiology and should be patient oriented. The statement should be realistic and measurable and reflect what the patient will do. PTS: 1 DIF: Cognitive Level: Comprehension REF: 24 OBJ: 11 (clinical) TOP: Goals KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 11. The nurse who has recently moved from Louisiana to Texas is uncertain about the LPN/LVN’s role in applying the nursing process. Which source is most appropriate source for the nurse to consult? a. Hospital policies b. The Texas State Board of Nursing c. Rules and regulations of the Louisiana Nurse Practice Act d. The National Association of Practical Nurse Education and Service ANS: B Each state has different guidelines for areas of care planning, intravenous therapy, teaching, and delegation. The Texas State Board of Nursing is the most reliable source. PTS: 1 DIF: Cognitive Level: Comprehension REF: 17 OBJ: 4 (theory) TOP: Nursing Process KEY: Nursing Process Step: N/A MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 12. The nurse adds a nursing order to the care plan related to a patient with a problem statement/nursing diagnosis of altered nutrition/Nutrition: Less Than Body Requirements Related to Nausea and Vomiting. Which nursing order should the nurse include in the plan of care? a. Medicate with an antiemetic before each meal. b. Offer crackers and iced drink before each meal. c. Change diet to clear liquids. d. Give nothing by mouth until nausea subsides. ANS: B Offering crackers and iced drinks are within the scope of nursing; the other options would require a medical order to complete. PTS: 1 DIF: Cognitive Level: Application REF: 18 OBJ: 11 (clinical) TOP: Nursing Orders KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 13. After evaluating the nursing care plan, the nurse finds lack of progress toward the goal. What action should the nurse take next? a. Create a more accessible goal. b. Revise the nursing interventions. c. Change the problem statement/nursing diagnosis. d. Use a new evaluation plan. ANS: B When lack of progress to reach the goal is seen on evaluation, the interventions are reviewed and/or revised. PTS: 1 DIF: Cognitive Level: Application REF: 26 OBJ: 10 (clinical) TOP: Evaluation KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 14. During an intake interview, the nurse observes the patient grimacing and holding his hand over his stomach. The patient previously denied having any pain. What action should the nurse take next? a. Examine the history closely for etiology of pain. b. Ask the patient if he is experiencing abdominal pain. c. Record that patient seems to be having abdominal discomfort. d. Physically examine the patient’s abdomen. ANS: B The nurse should try to resolve any incongruence between body language and verbal responses. PTS: 1 DIF: Cognitive Level: Application REF: 20, Box 2-5 OBJ: 7 (clinical) TOP: Patient Interview KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 15. While conducting an admission interview, the nurse questions the patient about pain. The patient responds, “No. I’m pretty wobbly.” Which action should the nurse take next? a. Repeat the question about pain. b. Ask the patient to clarify his meaning. c. Record that the patient denied pain. d. Record that the patient stated he was wobbly. ANS: B The nurse should ask for clarification if unsure of what is meant by one of the patient’s responses. PTS: 1 DIF: Cognitive Level: Application REF: 20, Box 2-5 OBJ: 7 (clinical) TOP: Patient Interview KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 16. The nurse is caring for a patient with a goal/outcome statement of Patient will sleep for 5 hours uninterrupted each night. Which nursing intervention should the nurse include? a. Medicate with sedative each night. b. Offer warm fluids frequently. c. Arrange for a large meal at supper. d. Discourage daytime napping. ANS: D Discouraging daytime napping increases the probability of sleep. Giving medication is a collaborative intervention as it requires an order. Large meal and large fluid intakes may interrupt sleep. PTS: 1 DIF: Cognitive Level: Application REF: 25 OBJ: 11 (clinical) TOP: Nursing Intervention KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 17. The nursing team is prioritizing the problem statement/nursing diagnoses of an overweight hospital patient. Which problem statement/nursing diagnosis would be most important for this patient? a. Risk for dehydration related to vomiting. b. Activity intolerance related to shortness of breath. c. Knowledge deficit related to weight reduction diet. d. Altered self-image related to excessive weight. ANS: B Activity intolerance is the highest priority as it has to do with activities that are essential to life. The second is Knowledge deficit related to weight reduction diet, followed by Altered self-image related to excessive weight, and the last is Risk for dehydration related to vomiting. PTS: 1 DIF: Cognitive Level: Analysis REF: 23 OBJ: 11 (clinical) TOP: Setting Priorities KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 18. The nurse is explaining the components of a complete problem statement/nursing diagnosis. In addition to the NANDA stem and etiology, which other component should the diagnosis include? a. A time reference for meeting the need b. A designation of what the patient should do c. Signs and symptoms of the problem assessed d. A specifically worded medical diagnosis ANS: C A complete problem statement/nursing diagnosis must have a NANDA stem, etiology, and signs and symptoms (etiology) of the problem. PTS: 1 DIF: Cognitive Level: Knowledge REF: 23 OBJ: 4 (theory) TOP: Nursing Diagnosis KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 19. Which statement explains the reason for inclusion of potential problems in the nursing care plan? a. To alert nursing staff to prevent potential complications. b. To remind the family of potential problems. c. To broaden the assessment of the caregiver. d. To educate the patient to aspects of her health. ANS: A Addressing potential problems prevents complications by early action rather than waiting for a problem to materialize. PTS: 1 DIF: Cognitive Level: Comprehension REF: 23 OBJ: 7 (clinical) TOP: Potential Health Problems KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 20. The nurse is completing the medication reconciliation form for a patient. Which information is most important for the nurse to include? a. The patient reports taking Ginkgo biloba daily for the last 6 months. b. The patient reports having high hematocrit levels during his last hospital stay. c. The patient reports he has been diabetic for 10 years. d. The patient reports having a recent infection. ANS: A As part of the medication reconciliation form, all home medications (including herbal preparations like Gingko biloba) are listed and reviewed by the provider, pharmacist, and nurses. The information gathered during the completion of this form may impact care that the patient will receive. Abnormal lab work and history of chronic or acute illnesses are important components of the patient’s history but should not be part of the medication reconciliation form. PTS: 1 DIF: Cognitive Level: Application REF: 20 OBJ: 7 (clinical) TOP: Alternative Medicine KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 21. The LPN/LVN adheres to facility policy regarding core measures by performing which interventions during patient care? a. Administering the ordered amount of insulin to a patient with type 1 diabetes. b. Performing a thorough patient assessment upon admission to the health care facility. c. Documenting accurately and at appropriate intervals in the patient’s record. d. Providing patient teaching regarding proper diet for the patient diagnosed with renal failure. ANS: A Core measures are interventions that are based on scientifically researched, evidence-based standards of care, and are used to treat the majority of patients with a specific illness that often develops complications. Insulin administration for diabetics is evidence-based researched practice. The remaining options are good practice but are not considered core measures. PTS: 1 DIF: Cognitive Level: Analysis REF: 25 OBJ: 4 (theory) TOP: Core Measures KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Management of Care 22. The nurse is caring for a patient with pneumonia who complains of shortness of breath. Further assessment reveals an oxygen saturation of 89% on room air, 28 respirations/min with bilateral crackles in lung bases, blood pressure of 160/94, and a pulse rate of 102 beats/min. Which nursing diagnosis is priority for this patient? a. Activity Intolerance b. Impaired Gas Exchange c. Ineffective Cardiopulmonary Tissue Perfusion d. Self-Care Deficit: Bathing and Hygiene ANS: B While all nursing diagnoses may apply to this patient, impaired gas exchange is the highest priority because this is the underlying problem for the other nursing diagnoses, as well as physiologically the highest priority. PTS: 1 DIF: Cognitive Level: Analysis REF: 23 OBJ: 11 (clinical) TOP: Nursing Diagnosis KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Management of Care MULTIPLE RESPONSE 23. The nurse explains to the nursing student that the application of critical thinking to patient care involves which factor(s)? (Select all that apply.) a. Identification of a patient problem b. Setting priorities c. Concentrating on the patient rather than family needs d. Use of logic and intuition e. Expansion of thought beyond the obvious ANS: A, B, D, E Critical thinking as applied to nursing care requires setting priorities of patient problems and needs by using logic and intuition. Inclusion of the family in the care makes the approach family oriented. Critical thinking should go beyond the obvious. PTS: 1 DIF: Cognitive Level: Comprehension REF: 15 OBJ: 7 (clinical) TOP: Critical Thinking KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 24. Which statement(s) demonstrates application of the nursing process? (Select all that apply.) a. Performing a head-to-toe assessment. b. Updating the patient care plan on a weekly basis. c. Evaluating if patient goals have been met. d. Determining if nursing interventions need to be changed based on lack of patient progress toward meeting goals. e. Ensuring that all personnel caring for the patient are implementing the care plan and working toward the same goal. ANS: A, C, D, E The nursing care plan should be updated as necessary, not just on a weekly basis. Concepts of the nursing process are demonstrated by performing orderly, logical head-to-toe assessments, as well as ongoing evaluation of patient goals and interventions to meet those goals. PTS: 1 DIF: Cognitive Level: Comprehension REF: 17 OBJ: 8 (clinical) TOP: Nursing Process KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 25. Which example(s) demonstrate patient care that reflects knowledge of the National Patient Safety Goals? (Select all that apply.) a. Identifying the patient prior to medication administration by asking the patient to state his or her name. b. Reporting any sentinel event to the facility’s quality assurance team. c. Assessing the patient’s heartrate prior to administration of digoxin. d. Performing hand hygiene prior to performing a patient assessment. e. Documenting the appropriate time of medication administration. ANS: C, D, E Assessing the patient’s heart rate prior to administration of digoxin demonstrates knowledge of medication actions and prevention of adverse effects; hand hygiene is required before any patient care, including assessment; and documentation of the time of medication administration is necessary to prevent medication errors. To meet National Patient Safety Goals, the nurse must use at least two methods of patient identification prior to medication administration. Reporting a sentinel event is required but demonstrates that National Patient Safety Goals were not met. PTS: 1 DIF: Cognitive Level: Application REF: 4, 23 OBJ: 4 (theory) TOP: National Patient Safety Goals KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control COMPLETION 26. The nursing student demonstrates knowledge of the proper use of the ___________ when determining that it is safe to administer meperidine (Demerol) and promethazine (Phenergan) together. ANS: Medication Reconciliation Form The Medication Reconciliation Form tracks all medications the patient is taking as prescribed by different physicians and can identify overdoses or drugs that are not compatible. PTS: 1 DIF: Cognitive Level: Application REF: 20 OBJ: 8 (clinical) TOP: Medication Reconciliation Form KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 27. Shortness of breath due to emphysema would be a major component of the _________ care plan. ANS: interdisciplinary An interdisciplinary care plan involves all members of the health care team and is based on the medical diagnosis rather than a problem statement/nursing diagnosis. PTS: 1 DIF: Cognitive Level: Application REF: 26 OBJ: 8 (clinical) TOP: Interdisciplinary Care Plan KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance MATCHING Place the steps of the nursing process in their proper sequence. a. Evaluation b. Assessment c. Implementation d. Planning e. Problem statement/nursing diagnosis 28. Step 1 29. Step 2 30. Step 3 31. Step 4 32. Step 5 28. ANS: B PTS: 1 DIF: Cognitive Level: Comprehension REF: 17 OBJ: 4 (theory) TOP: Applying the Nursing Process KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 29. ANS: E PTS: 1 DIF: Cognitive Level: Comprehension REF: 17 OBJ: 4 (theory) TOP: Applying the Nursing Process KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 30. ANS: D PTS: 1 DIF: Cognitive Level: Comprehension REF: 17 OBJ: 4 (theory) TOP: Applying the Nursing Process KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 31. ANS: C PTS: 1 DIF: Cognitive Level: Comprehension REF: 17 OBJ: 4 (theory) TOP: Applying the Nursing Process KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 32. ANS: A PTS: 1 DIF: Cognitive Level: Comprehension REF: 17 OBJ: 4 (theory) TOP: Applying the Nursing Process KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance Chapter 03: Fluid, Electrolytes, Acid-Base Balance, and Intravenous Therapy deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse uses a diagram to demonstrate how in dehydration the water is drawn into the plasma from the cells by which process? a. Distillation b. Diffusion c. Filtration d. Osmosis ANS: D The process of osmosis accomplishes the movement of water from the cells into the plasma, causing dehydration. PTS: 1 DIF: Cognitive Level: Knowledge REF: 32 OBJ: 3 (theory) TOP: Dehydration KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. The nurse assessing a patient with vomiting and diarrhea observes that the urine is scant and concentrated. Which controlling factor is responsible for compensatory reabsorption of water? a. Osmoreceptors in the hypothalamus b. Antidiuretic hormone in the posterior pituitary c. Baroreceptors in the carotid sinus d. Insulin from the pancreas ANS: B The antidiuretic hormone controls how much water leaves the body by reabsorbing water in the renal tubules. PTS: 1 DIF: Cognitive Level: Comprehension REF: 30 OBJ: 2 (theory) TOP: Regulation of Body Fluids KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. The nurse uses a picture to show how ions equalize their concentration by which passive transport process? a. Osmosis b. Filtration c. Titration d. Diffusion ANS: D Diffusion is the process by which substances move back and forth across compartment membranes until they are equally divided. PTS: 1 DIF: Cognitive Level: Knowledge REF: 31 OBJ: 2 (theory) TOP: Diffusion KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. Which term describes the active transport process that moves sodium and potassium into or out of cells? a. Filtration b. Sodium pump c. Diffusion d. Osmosis ANS: B The sodium pump is the mechanism by which sodium and potassium are moved into or out of cells regardless of the concentration. PTS: 1 DIF: Cognitive Level: Knowledge REF: 32 OBJ: 2 (theory) TOP: Active Transport KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. The patient taking furosemide (Lasix) to correct excess edema shows a weight loss of 5.5 pounds in 24 hours. The nurse calculates that this weight loss is equivalent to how many liters (L) of fluid? a. 1 L b. 1.5 L c. 2.0 L d. 2.5 L ANS: D Each kilogram (2.2 pounds) of weight loss is equivalent to 1 liter of fluid. Therefore, 5.5 pounds ÷ 2.2 pounds = 2.5 liters. PTS: 1 DIF: Cognitive Level: Application REF: 33, Clinical Cues OBJ: 1 (clinical) TOP: Fluid Loss KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 6. The nurse is caring for a patient with a potassium level of 2.9 mEq/L. The nurse should carefully monitor the patient for which potential problem? a. Excessive urinary output b. Abdominal distention c. Increased reflexes d. Hyperactive bowel sounds ANS: B A potassium level lower than 3.5 mEq/L results in reduced urine output, cardiac dysrhythmia, muscle weakness, abdominal pain and distention, paralytic ileus, lethargy, and confusion. PTS: 1 DIF: Cognitive Level: Application REF: 41, Table 3-4 OBJ: 15 (clinical) TOP: Hypokalemia KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 7. While the nurse is washing the face of a patient in renal failure, the patient demonstrates a spasm of the lips and face. Which laboratory value corresponds with the nurse’s assessment findings? a. Potassium of 3.4 mEq/L b. Calcium of 7.9 mg/dL c. Sodium of 140 mEq/L d. Phosphorus of 2.8 mg/dL ANS: B Chvostek sign is a signal of hypocalcemia. It occurs when the facial nerve is tapped or stroked about an inch in front of the earlobe and results in unilateral twitching of the face. Hypocalcemia occurs when the calcium level drops below 8.4. A potassium level of 3.4 mEq/L and a sodium level of 140 mEq/L are findings within normal limits. A patient in renal failure is most likely to have a high phosphorus level rather than a low phosphorus level, and 2.8 mg/dL is within the range consistent with hypophosphatemia. PTS: 1 DIF: Cognitive Level: Analysis REF: 43, Table 3-4 OBJ: 4 (theory) TOP: Chvostek Sign KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 8. Which finding is most important for the nurse to confirm prior to hanging an intravenous (IV) bag containing potassium? a. Verify a blood pressure of at least 60 mm Hg diastolic. b. Check for urine output of at least 30 mL/hr. c. Ensure filter placement on the IV line. d. Verify a pulse of at least 50 beats/min. ANS: B An adequate urine output must be present prior to the administration of potassium to ensure adequate excretion of potassium, preventing hyperkalemia. PTS: 1 DIF: Cognitive Level: Application REF: 43, Safety Alert OBJ: 10 (theory) TOP: Administration of IV Potassium KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 9. Which statement demonstrates that the patient accurately understands the nurse’s teaching related to a low-sodium diet? a. “I can have all the dried fruits I want.” b. “I’m looking forward to a tall glass of tomato juice.” c. “I’m going to eat my favorite avocado and orange salad.” d. “I’m going to eat a cheeseburger with extra ketchup.” ANS: C Avocado and oranges have no significant sodium content. Dried fruits, tomato juice, cheese, and ketchup are foods with high sodium content that should be limited or avoided. PTS: 1 DIF: Cognitive Level: Application REF: 43, Nutrition Considerations OBJ: 4 (clinical) TOP: Low-Sodium Diet KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 10. The nurse is caring for an 80-year-old patient. Which finding is the best early indicator of dehydration in this patient? a. Reduced skin turgor b. Constipation c. Increased temperature d. Thirst ANS: B The nurse understands that this patient’s age places him at greater risk for dehydration. Constipation is the best early indicator of dehydration in the older adult. Older adults have age-related poor skin turgor. Increased temperature and thirst are later signs of dehydration. PTS: 1 DIF: Cognitive Level: Analysis REF: 33-34 OBJ: 5 (theory) TOP: Dehydration in the Older Adult KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 11. The patient with long-term obstructive pulmonary disease has a pH of 7, HCO3 – of 18 mEq/L, and a PaCO2 of 40 mm Hg. These laboratory values are consistent with which acid-base imbalance? a. Respiratory alkalosis b. Metabolic alkalosis c. Respiratory acidosis d. Metabolic acidosis ANS: D These results are indicative of metabolic acidosis. PTS: 1 DIF: Cognitive Level: Application REF: 46 OBJ: 15 (clinical) TOP: Respiratory Acidosis KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 12. The nurse is caring for a young patient with asthma. Which activity should the nurse encourage in order to help prevent respiratory acidosis? a. Engage in deep-breathing exercises every 2 hours. b. Drink 8 ounces of fluid every 4 hours. c. Ambulate for 15 minutes twice a day. d. Sleep with the head of the bed elevated 45 degrees. ANS: A Deep breathing blows off CO2, which reduces the acid ions, thus preventing respiratory acidosis. Drinking fluids prevents dehydration and keeps secretions moist and thin, and sleeping with the head of the bed elevated will ease breathing and improve gas exchange. Ambulating 15 minutes twice a day does not have an impact on respiratory acidosis. PTS: 1 DIF: Cognitive Level: Analysis REF: 46 OBJ: 8 (theory) TOP: Respiratory Acidosis KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 13. The patient who has had diarrhea for the last 3 days has blood gases of pH of 7.1, HCO3 - of 20 mEq/L, and PCO2 of 36 mm Hg. These laboratory values are consistent with which acid-base imbalance? a. Respiratory alkalosis b. Metabolic alkalosis c. Respiratory acidosis d. Metabolic acidosis ANS: D Metabolic acidosis shows a low pH, low HCO3 - , and normal CO2. PTS: 1 DIF: Cognitive Level: Application REF: 46 OBJ: 8 (theory) TOP: Metabolic Acidosis KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 14. The nurse is caring for a patient with metabolic acidosis. Which assessment finding reveals that the compensatory mechanism to correct this imbalance is in effect? a. Increased urinary output b. Reduced abdominal distention c. Kussmaul respirations d. Decreased blood pressure ANS: C Kussmaul respirations, or deep and rapid respirations, are blowing off carbon dioxide to reduce an acidotic state. PTS: 1 DIF: Cognitive Level: Application REF: 47 OBJ: 7 (theory) TOP: Metabolic Acidosis KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 15. The nurse assesses the patient’s IV insertion site and observes that the vein is hard, the skin is red and tender, and a blood return in the IV line. After removing the IV catheter, which action should the nurse take next? a. Obtain an arm board to properly secure the IV. b. Elevate the arm above the level of the heart. c. Clean the site with alcohol and apply cool compresses. d. Apply a warm moist pack. ANS: D These are signs and symptoms of phlebitis and should be treated with a warm moist pack to increase blood flow to the area. The IV has been discontinued, so an arm board for stabilization is unnecessary. Elevation of the arm would be helpful to reduce swelling. A cool compress would be indicated for other issues related to IV infusion problems, such as extravasation. PTS: 1 DIF: Cognitive Level: Application REF: 51 OBJ: 18 (clinical) TOP: Phlebitis KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 16. Because there are no IV pumps available for the immediate infusion of an IV medication, the nurse must calculate the flow rate for 500 mL to run for 4 hours, using a set that delivers 15 gtt/mL. Which flow rate is correct? a. 30 gtt/min b. 35 gtt/min c. 40 gtt/min d. 45 gtt/min ANS: A 500 mL to be given in 4 hours equals 125 mL/hr. 125 mL ÷ 60 minutes = 2 mL/min × 15 gtt/mL = 30 gtt/min. PTS: 1 DIF: Cognitive Level: Application REF: 53 OBJ: 12 (theory) TOP: Calculation of IV Flow Rate KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 17. The count of the solution in the IV container at the beginning of the shift is 800 mL. A new 1000-mL bag was hung during the shift and has 650-mL left at the end of the shift. What amount should the nurse record as the IV fluid intake for the shift? a. 1000 mL b. 1050 mL c. 1100 mL d. 1150 mL ANS: D 800 mL + 350 mL from second bag = 1150 mL. PTS: 1 DIF: Cognitive Level: Application REF: 53-54 OBJ: 12 (theory) TOP: Calculating IV Fluid Intake KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 18. After selecting an appropriate fluid, which action should the nurse take to correctly flush a PRN lock? a. Flush forcefully to clear the lumen. b. Use slow, gentle pressure to clear the lumen. c. Flush hard enough to clear resistance. d. Aspirate for blood return prior to flushing. ANS: B The standard of care utilizes slow, gentle pressure. The nurse should stop the flush if resistance is met. Resistance may indicate a clot and force would break the clot loose. Aspiration is not necessary. PTS: 1 DIF: Cognitive Level: Application REF: 54 OBJ: 18 (clinical) TOP: Flushing PRN Lock KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 19. The nurse is caring for a patient who has been on total parenteral nutrition (TPN) for 48 hours. Which action demonstrates effective nursing care? a. Checking the patient’s blood glucose level according to facility protocol. b. Increasing the infusion rate if the prescribed intake falls behind. c. Informing the patient that TPN can only be administered via a central line for 1 week. d. Monitoring the peripheral IV site of TPN infusion for signs of infiltration at least every 8 hours. ANS: A The hypertonic solution causes difficulty with glucose tolerance, so monitoring of blood glucose level is imperative. The infusion rate should never be increased to “catch up” because of the likelihood of fluid overload caused by the hypertonicity of the TPN. TPN can be administered for more than 1 week and it is almost always administered via a central line rather than a peripheral line. PTS: 1 DIF: Cognitive Level: Application REF: 55 OBJ: 19 (clinical) TOP: TPN KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 20. The nurse is assessing a patient with renal failure and notes fatigue, muscle cramps, confusion, and headache. Which laboratory abnormality corresponds with these findings? a. Potassium of 3.3 mEq/L b. Sodium of 129 mEq/L c. Calcium of 8.2 mg/dL d. Chloride of 105 mEq/L ANS: B The patient is demonstrating signs and symptoms of hyponatremia; therefore, the nurse should assess the patient’s sodium level. PTS: 1 DIF: Cognitive Level: Application REF: 40, Table 3-4 OBJ: 15 (clinical) TOP: Hyponatremia KEY: Nursing Process Step: Evaluation MSC: NCLEX: Safe, Effective Care Environment: Management of Care MULTIPLE RESPONSE 21. The nurse is assessing the hydration status of the patient. Which action(s) demonstrates knowledge of proper assessment? (Select all that apply.) a. Monitoring the patient’s daily weight. b. Assessing the patient’s skin turgor on the back of the hand. c. Checking the patient’s blood glucose level four times a day. d. Assessing for skin tenting on the patient’s forehead. e. Asking the patient if he is experiencing thirst. ANS: A, D, E The skin of the abdomen, forearm, sternum, forehead, and thigh can be “tented” as a test for skin turgor by gently pinching up a fold of skin and observing the delay in return to normal. Assessment of skin turgor is not reliable on the back of the hand. Weight and experiencing thirst can be indicators of hydration status, along with further assessment. The patient’s blood glucose level is not an assessment parameter for hydration status. PTS: 1 DIF: Cognitive Level: Application REF: 33 OBJ: 13 (clinical) TOP: Assessment Data: Skin Turgor KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 22. The nurse is caring for a patient that has a potassium level of 5.0. The nurse should carefully monitor the patient for which signs and symptoms? (Select all that apply.) a. Muscle weakness b. Cardiac dysrhythmias c. Decreased reflexes d. Urinary retention e. Hypotension ANS: A, B, E Normal potassium level is 3.5 to 5.0 mEq/L. Because the patient is on the highest end of normal, the nurse should monitor for signs of hyperkalemia. Muscle weakness, cardiac dysrhythmias, and hypotension are signs of hyperkalemia. Decreased reflexes and urinary retention are signs of hypokalemia. PTS: 1 DIF: Cognitive Level: Application REF: 43 OBJ: 15 (clinical) TOP: Hyperkalemia KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 23. The primary care provider writes an order for the patient to receive an IV of a solution that has the same osmotic pressure as intracellular fluid. The nurse would correctly question which IV order(s)? (Select all that apply.) a. 5% dextrose in water b. 0.45% sodium chloride c. 5% dextrose in 0.9% sodium chloride d. Lactated Ringer solution e. 0.9% sodium chloride ANS: B, C The solution being prescribed is an isotonic solution. 5% dextrose in water, lactated Ringer solution, and 0.9% sodium chloride are all isotonic solutions, whereas 0.45% sodium chloride is a hypotonic solution, and 5% dextrose in 0.9% sodium chloride is a hypertonic solution. PTS: 1 DIF: Cognitive Level: Analysis REF: 48-49 OBJ: 11 (theory) TOP: Isotonic Solutions KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 24. The nurse is caring for a newly admitted patient with uncontrolled nausea and vomiting. The patient has a history of alcoholism and diabetes. After receiving these orders from the health care provider, which order(s) should the nurse question? (Select all that apply.) a. Administer 10 mg prochlorperazine maleate (Compazine), IM every 4 to 6 hours for nausea and vomiting. b. Administer diphenoxylate atropine (Lomotil), two tabs, by mouth after first occurrence of nausea and vomiting. c. Administer furosemide (Lasix) 40 mg by slow IV push. d. Monitor the patient’s intake and output every 4 hours. e. Obtain patient’s weight every morning and record. ANS: A, B, C A primary concern in a patient with uncontrolled vomiting includes monitoring hydration status. Intake and output and daily weights are indicators of hydration status and should be assessed. Prochlorperazine maleate (Compazine) should not be given with alcohol intake. Because the patient has a history of alcoholism, it would be best to administer an antiemetic that is not contraindicated with possible alcohol intake. Diphenoxylate atropine (Lomotil) is an antidiarrheal, not an antiemetic. Lasix is a powerful loop diuretic that would exacerbate the patient’s volume depletion. PTS: 1 DIF: Cognitive Level: Analysis REF: 33, Box 3-2, 36, Table 3-2, 50, Table 3-6 OBJ: 13 (clinical) TOP: Hydration Status KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation COMPLETION 25. The nurse demonstrates knowledge of IV solutions by identifying that the IV solution which provides free water, as well as 340 calories/L, is ______________. ANS: 10% dextrose in water 10% dextrose in water provides free water with no electrolytes and 340 calories/L. PTS: 1 DIF: Cognitive Level: Comprehension REF: 50, Table 3-6 OBJ: 12 (theory) TOP: IV Fluids KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 26. The nurse explains to the 85-year-old patient with a temperature that, with each degree of fever, the body loses _____% of water. ANS: 10 With each degree of fever, the body has an insensible loss of 10% of its water. PTS: 1 DIF: Cognitive Level: Comprehension REF: 32 OBJ: 5 (theory) TOP: Insensible Loss KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 27. The nurse reminds the patient that the three body mechanisms that attempt to compensate to correct acid-base imbalances are the __________ system, the __________ system, and the __________. ANS: buffer; respiratory; kidneys buffer; kidneys; respiratory respiratory; buffer; kidneys respiratory; kidneys; buffer kidneys; respiratory; buffer kidneys; buffer; respiratory The buffer system, the respiratory system, and the kidneys contribute unique compensations to correct an acid-base imbalance. PTS: 1 DIF: Cognitive Level: Comprehension REF: 44 OBJ: 8 (theory) TOP: Acid-Base Compensatory Mechanisms KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation MATCHING The nurse explains that the chain of events that results in hypocalcemia for the patient in early renal failure occurs in which order? (Match the events to the proper sequence.) a. Loss of calcium ions b. Vitamin D not activated c. Bone loss d. Retention of phosphates e. Loss of absorption of calcium from the gastrointestinal tract 28. Step 1 29. Step 2 30. Step 3 31. Step 4 32. Step 5 28. ANS: D PTS: 1 DIF: Cognitive Level: Analysis REF: 43 OBJ: 4 (theory) TOP: Hypocalcemia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 29. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 43 OBJ: 4 (theory) TOP: Hypocalcemia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 30. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 43 OBJ: 4 (theory) TOP: Hypocalcemia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 31. ANS: E PTS: 1 DIF: Cognitive Level: Analysis REF: 43 OBJ: 4 (theory) TOP: Hypocalcemia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 32. ANS: C PTS: 1 DIF: Cognitive Level: Analysis REF: 43 OBJ: 4 (theory) TOP: Hypocalcemia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation Chapter 04: Care of Preoperative and Intraoperative Surgical Patients deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is caring for a patient who has received epoetin alfa (Epogen) 2 to 3 weeks prior to a scheduled surgery. Which statement best explains the goal for Epogen administration prior to surgery? a. The patient will only require a single antibiotic immediately prior to surgery. b. The patient will have greater numbers of white blood cells (WBCs) following surgery. c. The patient will not require a blood transfusion during surgery. d. The patient will maintain stable potassium levels during surgery. ANS: C Epoetin alfa (Epogen) is given to increase red blood cell production prior to surgery with the goal of having a bloodless surgery. Epoetin alfa (Epogen) will not affect the need for an antibiotic preoperatively, nor will it affect WBCs or serum potassium levels. PTS: 1 DIF: Cognitive Level: Application REF: 62 OBJ: 1 (theory) TOP: Bloodless Surgery KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 2. The nurse is performing a preoperative assessment on a patient scheduled for surgery today. The patient reports drinking two glasses of wine daily, smoking one pack of cigarettes daily ´ 20 years, completing a round of corticosteroids for asthma control 2 days ago, and taking a dose of passion flower extract yesterday. Which action should the nurse take next? a. Supply the patient with information on a smoking cessation class. b. Educate the patient regarding the dangers of drinking alcohol on a daily basis. c. Provide the patient with information regarding the dangers of using herbal medications. d. Notify the physician immediately regarding the patient’s recent use of corticosteroids. ANS: D The use of corticosteroids reduces the body’s response to infection and delays healing. Surgery may need to be delayed until the patient has been off the drug approximately 7 days. Providing the patient with information regarding smoking cessation is advisable but is not a priority at this time. Drinking two glasses of wine daily may not be a problem if not contraindicated by the patient’s health status. Passion flower extract does not interfere with the surgery and poses no apparent problems. PTS: 1 DIF: Cognitive Level: Analysis REF: 65, Table 4-2 OBJ: 2 (theory) TOP: Perioperative Management KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 3. The nurse is caring for a presurgical patient. The patient asks the nurse why her height and weight are recorded. How should the nurse respond? a. “This information helps us to correctly calculate the anesthesia dose.” b. “Height and weight are important predictors of blood loss.” c. “This information is used to assess respiratory volume.” d. “Height and weight help us anticipate your fluid needs.” ANS: A Height and weight are used to calculate anesthesia dosages. PTS: 1 DIF: Cognitive Level: Comprehension REF: 76 OBJ: 3 (theory) TOP: Presurgical Assessment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 4. The nurse is reviewing the presurgical patient’s laboratory reports and notes an elevated aspartate aminotransferase (AST) and bilirubin. The nurse understands that this patient is most at risk for which potential complication? a. Excessive bleeding during or after surgery b. An increased serum albumin level c. Postsurgical respiratory infection d. Delayed wound healing ANS: A The AST and bilirubin are liver studies. Elevated levels may indicate a dysfunctional liver. The liver is directly involved with clotting factors; therefore, this patient would be at risk for excessive bleeding. The serum albumin level would most likely be decreased if the liver is not functioning properly. Postsurgical wound infection and delayed wound healing risks are not directly related to liver function. PTS: 1 DIF: Cognitive Level: Analysis REF: 64, Box 4-2, 65, Table 4-2 OBJ: 2 (theory) TOP: Preoperative Lab Studies KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 5. The patient received a preoperative dose of lorazepam (Ativan) 20 minutes ago. Which safety precaution should the nurse take? a. Monitor respiratory status. b. Raise the bed rails. c. Elevate the head of the bed 30 degrees. d. Take seizure precautions. ANS: B Raising the bed rails is a safety precaution against the dizziness and hypotension caused by this drug. PTS: 1 DIF: Cognitive Level: Application REF: 71, Safety Alert OBJ: 12 (clinical) TOP: Preoperative Medication KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 6. The nurse is caring for an 82-year-old presurgical patient. Which abnormal finding is most important for the nurse to report immediately? a. Respiratory rate of 22 breaths/min b. Report of extreme thirst c. Dizziness d. Temperature of 99.8° F ANS: D When assessing the presurgical patient, any significant deviations from normal range should be brought to the attention of the surgeon. An elevated temperature might indicate an infection that would need to be brought under control before surgery. Respiratory status is important, but a rate of 22 breaths/min is minimally abnormal. Borderline tachypnea, thirst, and dizziness are not necessarily indicative of a larger underlying problem. PTS: 1 DIF: Cognitive Level: Analysis REF: 63 OBJ: 2 (theory) TOP: Assessment of Surgical Risk Factors KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 7. The patient refuses to take off her diamond wedding band prior to going to the operating room. What action should the nurse take first? a. Document the patient’s refusal to remove the jewelry. b. Tape the ring to finger, covering the ring. c. Request that the patient sign a waiver to release the hospital from responsibility. d. Alert the surgery team to the presence of the jewelry. ANS: B Taping the ring will protect the ring and secure it to the finger. Care must be taken not to wrap the tape too tightly. The nurse will also need to document the presence of the ring on the preoperative checklist or in the nurse’s notes. There is no need for a signature on a waiver. Most facilities have policies in which the patient signs a release of responsibility for valuables. There is no need to notify the surgical team of the presence of the ring. PTS: 1 DIF: Cognitive Level: Comprehension REF: 71 OBJ: 3 (theory) TOP: Immediate Preoperative Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 8. The nurse is caring for an Asian patient who received atropine as a preoperative drug. For which problem should the nurse should carefully monitor the patient? a. Oliguria b. Hyperventilation c. Hypotension d. Tachycardia ANS: D Asians often metabolize atropine differently from other populations. The drug can greatly accelerate the heart rate in the Asian patient. PTS: 1 DIF: Cognitive Level: Application REF: 71, Cultural Considerations OBJ: 2 (theory) TOP: Immediate Preoperative Care KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 9. Which patient statement indicates a need for further instruction about the emotional preparation for surgery? a. “I’m going to hug my surgeon tomorrow.” b. “My fate is in the hands of my surgeon. I’m frightened about the outcome.” c. “I’ll be ready for a cheeseburger when I get back.” d. “I know I may have some pain, but this gallbladder will be gone when I wake up.” ANS: B This response demonstrates the patient’s fear and insecurity, which warrant further discussion. Providing additional information or answering patient questions may help alleviate the patient’s emotional unpreparedness for surgery. The plan for a cheeseburger indicates a potential need to further review nutrition in the postoperative period. The other responses demonstrate positive statements regarding the upcoming postsurgical period. PTS: 1 DIF: Cognitive Level: Analysis REF: 69 OBJ: 3 (theory) TOP: Planning KEY: Nursing Process Step: Evaluation MSC: NCLEX: Psychosocial Integrity: Psychosocial Adaptation 10. Which action should the nurse take prior to administering the preoperative doses of Demerol and atropine? a. Ensure that a family member is present. b. Remove the patient’s underwear. c. Verify that a consent form is signed. d. Raise each of the bed rails. ANS: C Consent forms must be signed prior to giving any sedative or preoperative drug. Removal of underwear and the raising of the side rails can be done after the administration of the drug. The family member does not have to present. PTS: 1 DIF: Cognitive Level: Comprehension REF: 68 OBJ: 12 (clinical) TOP: Obtaining Consent KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 11. Which person is responsible for verifying that the consent form is signed and that the surgical site? a. The scrub nurse b. The surgeon c. The anesthesiologist d. The circulating nurse ANS: D The circulating nurse is responsible for confirming a signature on the consent form and marking the site for surgery. PTS: 1 DIF: Cognitive Level: Comprehension REF: 74, Box 4-4 OBJ: 7 (theory) TOP: Circulating Nurse Duties KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 12. The nurse warns the patient that, in order to retard the growth of microorganisms, the operating room temperature must be maintained in which range? a. 60 to 65° F b. 66 to 70° F c. 71 to 74° F d. 75 to 77° F ANS: B The operating suite is kept at a temperature of 66 to 70° F to discourage microbial growth. PTS: 1 DIF: Cognitive Level: Knowledge REF: 73 OBJ: 3 (theory) TOP: The Surgical Suite KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 13. The nurse is caring for a patient in the immediate preoperative period. Which action best demonstrates compliance with the National Patient Safety Goals protocol? a. The nurse accompanies the patient to the operating room. b. The nurse raises all side rails and elevates the head of the bed to 30 degrees. c. The nurse verifies and marks the surgical site. d. The nurse identifies all prosthetic devices before the time-out. ANS: C The National Patient Safety Goals require that the patient be identified, the surgical consent be signed and correct, and the surgical site be marked. PTS: 1 DIF: Cognitive Level: Application REF: 74, Box 4-4 OBJ: 3 (theory) TOP: Immediate Preoperative Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 14. The nurse clarifies the difference between regional anesthesia and procedural sedation anesthesia. Which statement about procedural sedation anesthesia is true? a. Procedural sedation anesthesia uses both intravenous (IV) sedation and regional anesthesia. b. Procedural sedation anesthesia uses both general anesthesia and IV sedation. c. Procedural sedation anesthesia uses both alternative medicine herbs and regional anesthesia. d. Procedural sedation anesthesia uses both IV sedation and local anesthesia. ANS: A Procedural sedation anesthesia uses both IV sedation and regional anesthesia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 75, Table 4-3 OBJ: 8 (theory) TOP: Types of Anesthesia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 15. During the course of surgery, a patient exhibits tachycardia, diaphoresis, and rising body temperature. Which is the circulating nurse’s priority intervention? a. Monitor the patient for any further changes in condition. b. Note the patient’s oxygen saturation and blood pressure. c. Ask the scrub nurse to verify the assessment findings. d. Alert the anesthesiologist and surgeon immediately. ANS: D These are signs of malignant hyperthermia, along with arrhythmias, muscle rigidity, and hypotension. The anesthesiologist and surgeon should be notified immediately because malignant hyperthermia is a medical emergency. The nurse should continue to monitor the patient. The nurse should verify the patient’s oxygen saturation and blood pressure in conjunction with the anesthesiologist and surgeon. PTS: 1 DIF: Cognitive Level: Analysis REF: 76 OBJ: 13 (clinical) TOP: Malignant Hyperthermia KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 16. The nurse is caring for a postsurgical patient whose surgical procedure lasted 3 hours. Which complication should the nurse anticipate? a. Thrombophlebitis b. Muscle spasms c. Joint pain d. Hyperthermia ANS: C Long-term immobility places the patient at risk for pressure damage to skin and underlying tissues. Joint complaints are common after a long surgery. Thrombophlebitis, muscle spasms, and hyperthermia are complications that are not expected to occur. PTS: 1 DIF: Cognitive Level: Application REF: 77 OBJ: 4 (theory) TOP: Intraoperative Complications KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 17. The nurse is caring for a patient who has just been given medication to reverse neuromuscular blocking agents. The nurse is aware that the patient is in which general anesthetic stage? a. Induction b. Introduction c. Emergence d. Maintenance ANS: C Emergence is the stage of surgery in which surgery is completed and the patient is prepared to return to consciousness, and neuromuscular blocking agents are reversed. PTS: 1 DIF: Cognitive Level: Comprehension REF: 76 OBJ: 8 (theory) TOP: Stages of General Anesthesia KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 18. The nurse is planning care for four postoperative patients. Which patient is most likely to develop postoperative complications? a. 36-year-old with a history of controlled diabetes b. 62-year-old with a history of hypothyroidism c. 49-year-old with a history of a myocardial infarction (MI) d. 76-year-old with mild osteoarthritis ANS: D Patients over the age of 75 are three times more likely to experience surgical complications. An older adult is less able to adjust and compensate for the stress of surgery, as physiologic reserves (cardiac, respiratory, and renal) have already declined with age. PTS: 1 DIF: Cognitive Level: Analysis REF: 62, Older Adult Care Points OBJ: 4 (theory) TOP: Postoperative Complications KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 19. The LPN/LVN is in the patient’s room while the charge nurse is obtaining the patient’s signature on the surgical consent form. The patient states, “I didn’t really understand what my surgeon explained, but I trust him completely.” How should the nurse respond? a. “I need to contact your surgeon so your questions can be answered.” b. “I can answer any questions that you might have regarding your surgery.” c. “As long as you are comfortable, then you may sign the consent form.” d. “Maybe we should call your surgeon to be sure it is okay to sign the consent.” ANS: A An informed consent means that the surgeon has supplied information regarding the procedure itself, as well as the risks and benefits, and that the patient understands this information. The nurse’s responsibility is witnessing the signing of the form and ensuring the patient understands what the surgeon has discussed, not providing information if the patient has no understanding of the procedure. PTS: 1 DIF: Cognitive Level: Application REF: 68 OBJ: 3 (theory) TOP: Informed Consent KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Management of Care MULTIPLE RESPONSE 20. The patient questions the nurse about robotics surgery. Which information should the nurse include? (Select all that apply.) a. “Robotics gives the surgeon greater magnification than the human eye.” b. “Robotics allows the surgeon to be more precise than normal.” c. “Robotics allows for a smaller incision.” d. “Robotics increases healing time.” e. “Robotics procedures generally cause less postoperative pain.” ANS: A, B, C, E Robotics have 12 times magnification of the operative site, steady “hands,” and use a smaller incision, which results in less postoperative pain. Healing time is decreased with robotics. PTS: 1 DIF: Cognitive Level: Comprehension REF: 60-62 OBJ: 1 (theory) TOP: Robotic Surgery KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 21. Which physiological change(s) explain why the older adult is at greater surgical risk? (Select all that apply.) a. Fewer physiologic reserves b. Greater probability of a chronic illness c. Greater vulnerability to fluid loss d. Less tolerance for pain e. Less psychological stamina ANS: A, B, C The older adult does have less physiologic reserves, more probability for a chronic illness, and more vulnerability to fluid loss. There is no indication that the older adult has less tolerance for pain or less psychological stamina. PTS: 1 DIF: Cognitive Level: Comprehension REF: 62, Older Adult Care Points OBJ: 4 (theory) TOP: Older Adult Surgical Patient KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 22. What are the purposes of preoperative medication? (Select all that apply.) a. To reduce anxiety b. To decrease mucus secretion c. To counteract nausea d. To synergize anesthesia e. To enhance ventilation ANS: A, B, C, D Preoperative medications are given to reduce anxiety, decrease mucus production, counteract nausea, and enhance anesthesia. Many preoperative medications depress ventilation. PTS: 1 DIF: Cognitive Level: Comprehension REF: 71 OBJ: 3 (theory) TOP: Preoperative Medication KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 23. Which responses indicate to the nurse that the patient understands preoperative teaching? (Select all that apply.) a. “I will need to sign a consent form before I am given my medications prior to my surgery.” b. “The surgeon will want me to ambulate as soon as possible after my surgery.” c. “My nurse will want me to take the deepest breaths I can tolerate following my surgery.” d. “I may experience some constipation if I am taking much pain medication after my surgery.” e. “The general anesthesia will prevent me from having pain for the first 24 hours after surgery.” ANS: A, B, C, D Consent forms must be signed before preoperative pain medications are administered; early ambulation is common with most surgeries; deep breaths prevent postoperative respiratory complications; and constipation is common with the use of narcotic analgesics. General anesthesia does not prevent pain 24 hours after surgery, so this statement demonstrates the need for further preoperative teaching. PTS: 1 DIF: Cognitive Level: Application REF: 66 OBJ: 5 (theory) TOP: Preoperative Teaching KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 24. Which factor(s) may contribute to hypothermia during surgery? (Select all that apply.) a. Warm atmosphere of the operating room b. Infusion of cool IV fluids c. Inhalation of cool anesthetic gases d. Exposure of body surfaces e. Lowered metabolism ANS: B, C, D, E The infusion of cool IV fluids, inhalation of cool anesthetic gases, exposure of body surfaces, and lowered metabolism predispose patients to hypothermia during surgery. The operating room is kept cool to inhibit growth of organisms. PTS: 1 DIF: Cognitive Level: Application REF: 76 OBJ: 3 (theory) TOP: Potential Intraoperative Complications KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 25. The nurse is providing preoperative teaching to a patient who is scheduled for a needle biopsy of the breast. Which statement(s) demonstrate(s) a need for further preoperative teaching? (Select all that apply.) a. “This procedure will help the doctor determine if I have breast cancer.” b. “I will most likely have general anesthesia since this is a painful procedure.” c. “The surgeon will need to perform this procedure within the next 24 to 48 hours.” d. “I will have less breast pain after having this procedure performed.” e. “I will not require any further treatment after this procedure is performed.” ANS: B, C, D, E A needle breast biopsy is a diagnostic procedure that is used to determine if cancer cells are present. This procedure typically requires only a local or regional anesthetic; procedures that must be performed within 24 to 48 hours are considered urgent procedures for immediate life-threatening conditions; indicating that less pain will be experienced describes a palliative procedure; and indicating that less breast pain will occur describes a curative procedure. PTS: 1 DIF: Cognitive Level: Application REF: 61, Table 4-1 OBJ: 5 (theory) TOP: Preoperative Teaching KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance COMPLETION 26. The nurse reminds the patient that in laparoscopic surgery, with the small incision and less tissue trauma, there is less pain because of the diminished ______________. ANS: inflammatory response There is less trauma, therefore less inflammatory response, which reduces pain. PTS: 1 DIF: Cognitive Level: Comprehension REF: 60 OBJ: 1 (theory) TOP: Laparoscopic Surgery KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 27. A(n) ________________ allows a patient to donate her own blood to be used during or after surgery. ANS: autologous transfusion An autologous transfusion is one in which the patient has donated her own blood to be used during or after surgery. PTS: 1 DIF: Cognitive Level: Comprehension REF: 62 OBJ: 1 (theory) TOP: Autologous Transfusion KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 28. The _____________functions within the sterile area of the operating room and maintains sterile technique. ANS: scrub nurse scrub person The scrub nurse is a licensed nurse or surgery technician who functions in the sterile area of the operating room and maintains sterility throughout the operative procedure. PTS: 1 DIF: Cognitive Level: Knowledge REF: 74, Box 4-3 OBJ: 7 (theory) TOP: Scrub Nurse Duties KEY: Nursing Process Step: N/A MSC: NCLEX: N/A Chapter 05: Care of Postoperative Patients deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The postanesthesia care unit (PACU) nurse determines that the patient’s Aldrete score is 9. Which statement correctly describes the meaning of this score? a. The patient is at an increased risk for postoperative respiratory complications. b. The patient’s condition warrants close monitoring. c. The patient is experiencing severe pain. d. The patient will soon be transferred to the postoperative unit. ANS: D The Aldrete scoring system is a method of determining readiness for a surgery patient to be transferred from PACU to the postoperative unit. Scores are given for activity, respiration, circulation, consciousness, skin color, and oxygen saturation. A score of 9 or 10 indicates readiness for transfer. PTS: 1 DIF: Cognitive Level: Application REF: 81 OBJ: 5 (clinical) TOP: Immediate Postoperative Care KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 2. The nurse is caring for a patient recovering in the PACU. The patient awakens confused and disoriented. What action should the nurse take first? a. Take the patient’s vital signs. b. Encourage the patient to return to sleep. c. Reorient and reassure the patient. d. Document that the patient is awake and disoriented. ANS: C The patient should be reoriented and assured when awaking from anesthesia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 81 OBJ: 1 (theory) TOP: Immediate Postoperative Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 3. The PACU nurse is caring for a semiconscious patient immediately following abdominal surgery. The nurse correctly places the patient in which position? a. Supine b. Semi-Fowler c. Lateral d. Trendelenburg ANS: C Aspiration is a high-risk complication during this phase of recovery and can best be prevented by placing the unconscious or semiconscious patient on the side with head turned to the side. PTS: 1 DIF: Cognitive Level: Application REF: 83 OBJ: 6 (clinical) TOP: Immediate Postoperative Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 4. The PACU nurse is caring for an unconscious patient. Assessment reveals diminished breath sounds bilaterally. Which action should the nurse take? a. Hyperventilate the patient with an Ambu bag. b. Increase bi-nasal oxygen to 3 L/min. c. Elevate the head of bed 45 degrees. d. Document “diminished breath sounds in both lower lobes.” ANS: D Mild atelectasis is an expected sign after anesthesia for the first 48 hours after surgery. This finding is considered a normal finding while the patient is in the PACU and would require no further intervention unless other signs and symptoms, such as decreased oxygen saturation, were present. PTS: 1 DIF: Cognitive Level: Application REF: 83, 91 OBJ: 4 (theory) TOP: Immediate Postoperative Care KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. The nurse is caring for a patient during the first postoperative day. Which goal works to prevent atelectasis and is most appropriate for the nursing care plan? a. Patient will turn, cough, and deep-breathe every 4 hours. b. Patient will “huff-cough” every 2 hours. c. Patient will use the incentive spirometer twice a day. d. Patient will resume diet as soon as possible. ANS: B Bi-hourly coughing will help prevent atelectasis. The patient should turn, cough, and deep-breathe every 2 hours, and the incentive spirometer should ideally be used every hour. Resuming diet does not prevent atelectasis, and as soon as possible is not a measurable amount. PTS: 1 DIF: Cognitive Level: Analysis REF: 91, Table 5-2 OBJ: 3 (theory) TOP: Maintenance of Ventilation KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 6. The nurse is caring for a 90-year-old postoperative patient whose oxygen saturation is frequently dropping below 90%. Which age-related change is most likely related to this finding? a. Prolonged use of a walker b. Poor fluid intake c. Weakened respiratory muscles d. Increased elasticity of costal cartilages ANS: C Age-related changes that interfere with respiration in the older adult are weakened respiratory muscles and calcified costal cartilages. PTS: 1 DIF: Cognitive Level: Application REF: 83, Older Adult Care Points OBJ: 4 (theory) TOP: Maintenance of Ventilation KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 7. Which assessment finding on a patient who had a right total knee replacement this morning should be reported to the charge nurse immediately? a. Pain level of 8 at operative site b. Capillary refill of right toe of 7 seconds c. Right foot warm to touch d. Swelling of right knee ANS: B Capillary refills should be brisk, less than 3 seconds. Pain and swelling are expected at this early postoperative time. A warm foot is a normal finding. PTS: 1 DIF: Cognitive Level: Application REF: 84 OBJ: 5 (clinical) TOP: Maintenance of Circulation KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 8. Anti-embolic stockings are in place on the obese postsurgical patient. Which statement accurately describes the standard of care in regard to anti-embolic stockings? a. The stockings should remain in place continually for the first 24 hours. b. The stockings should fit tightly at the knee and ankle. c. The stockings should be removed approximately 20 minutes every shift. d. The stockings should be removed when ambulating. ANS: C Stockings should be removed approximately 20 minutes each shift for skin care. PTS: 1 DIF: Cognitive Level: Knowledge REF: 84 OBJ: 1 (theory) TOP: Maintenance of Circulation KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 9. The nurse has been assigned to care for several postoperative patients. Which patient is most likely to develop thrombophlebitis? a. A patient status post outpatient cholecystectomy with a history of blood clots. b. A patient who is 6 days postoperative for total right hip replacement with a history of left-sided stroke. c. A patient who underwent major abdominal surgery and was dehydrated upon admission. d. A patient who is 2 days postoperative for hernia repair with a history of diabetes. ANS: B Although all of these patients are at varying degrees of risk for thrombophlebitis, the hip replacement surgery places a patient at high risk for thrombophlebitis due to limited mobility, especially after the fifth postoperative day. This patient is at even higher risk of thrombophlebitis because of a history of left-sided stroke. PTS: 1 DIF: Cognitive Level: Analysis REF: 84 OBJ: 5 (theory) TOP: Maintenance of Circulation KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 10. The patient’s initial vital signs immediately on return from surgery include: blood pressure (BP) of 140/90; pulse (P) of 80; respirations (R) of 14; and temperature (T) of 98° F. One hour later the vital signs are: BP of 130/84; P of 72; R of 16; and T of 96.8° F. What action should the nurse take next? a. Add a blanket for warmth to the patient. b. Notify the charge nurse of a probable hemorrhage. c. Raise the head of the bed 45 degrees. d. Document the assessment findings. ANS: D These findings are normal. The nurse should document the normal recovery assessment and continue to monitor. There is no indication of chilling, hemorrhage, or respiratory distress, which respectively would require blanket application, charge nurse notification, or raising the head of the bed. PTS: 1 DIF: Cognitive Level: Analysis REF: 82, Assignment Considerations OBJ: 5 (clinical) TOP: Immediate Postoperative Care KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 11. The nurse is caring for a patient who has had spinal anesthesia. The nurse correctly questions which order? a. Patient to lie flat for 6 to 8 hours. b. Resume diet as tolerated. c. Use incentive spirometer every hour while awake. d. Notify physician immediately if headache occurs. ANS: D One of the goals during the postoperative period is to prevent or treat spinal headache. The headache can be treated with nursing interventions such as keeping the patient flat if a headache is reported and increasing fluid intake. If the headache becomes severe or does not improve, the physician could be notified. Lying flat for 6 to 8 hours reduces the risk of spinal headache and allows time for feeling to return to the legs; full diets can usually be resumed; and an incentive spirometer will reduce the chance of respiratory complications resulting from spinal anesthetic effects. PTS: 1 DIF: Cognitive Level: Analysis REF: 85 OBJ: 6 (clinical) TOP: Prevention of Injury KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 12. The nurse is caring for a patient who had spinal anesthesia. Which drink is the best choice for the nurse to offer the patient? a. Tea b. Orange juice c. Milk d. Water ANS: A Caffeinated beverages like tea or coffee increase the vascular pressure and help seal the punctured area. Orange juice, milk, or water would not achieve the same goal. PTS: 1 DIF: Cognitive Level: Application REF: 85 OBJ: 5 (theory) TOP: Prevention of Injury KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 13. When caring for a 10-hour postabdominal surgery patient, which finding the nurse should report to the charge nurse? a. 20 mL of clear green emesis b. Pain level of 5/10 c. No urine output since surgery d. A weak cough ability ANS: C The postsurgical patient should void in 4 to 8 hours after surgery. Scant emesis, moderate pain, and a weak cough are expected findings after abdominal surgery and do not require immediate report to the charge nurse. PTS: 1 DIF: Cognitive Level: Application REF: 85 OBJ: 5 (clinical) TOP: Immediate Postoperative Care KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 14. The nurse is caring for a surgical patient who complains of excessive gas. Which action should the nurse take? a. Offer iced fluids. b. Arrange for large meal servings. c. Provide a straw for drinking fluids. d. Ambulate the patient in the hall. ANS: D Ambulation, eating small meals, drinking tepid drinks, and avoiding the use of straws help eliminate gas. PTS: 1 DIF: Cognitive Level: Application REF: 86 OBJ: 6 (clinical) TOP: Promotion of Gastrointestinal Function KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 15. The postoperative patient complains of pain only 1 hour after having been medicated with an opioid, which cannot be repeated for three more hours. What action should the nurse take? a. Give one-half of the prescribed dose now. b. Contact the prescriber. c. Ambulate the patient in the hall. d. Reposition the patient. ANS: D Repositioning the patient is the best initial remedy. PTS: 1 DIF: Cognitive Level: Application REF: 87 OBJ: 7 (clinical) TOP: Promotion of Comfort KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 16. Which action is most important for the nurse to take prior to ambulating the postsurgical patient for the first time? a. Raise the head of the bed. b. Dangle the patient’s legs over side of bed. c. Offer the patient some fluids. d. Apply a gait belt to the patient. ANS: A The initial intervention prior to the first ambulation is to raise the head of the bed to gradually change the patient’s posture. The nurse should then sit the patient on the side of the bed and allow the legs to dangle over the side with the feet on the floor of a footstool. After a few minutes, the nurse should slowly assist the patient to stand and then assist the patient to walk. The nurse should use a gait belt and request additional assistance if the patient is very weak. PTS: 1 DIF: Cognitive Level: Application REF: 87 OBJ: 5 (theory) TOP: Promotion of Rest and Activity KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 17. The nurse educates the postsurgical patient about which potential effect of smoking on postsurgical recovery? a. Increased probability of hemorrhage b. Increased blood pressure c. Delayed healing d. Increased need for pain medication ANS: C Smoking delays healing because it causes a decrease in hemoglobin; hemoglobin carries oxygen to cells and tissues, which is necessary for wound healing. PTS: 1 DIF: Cognitive Level: Comprehension REF: 88 OBJ: 4 (theory) TOP: Factors Interfering with Wound Healing KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 18. When the postoperative patient refuses to cough due to incisional pain, which action should the nurse take first? a. Encourage deep breathing instead of coughing. b. Splint the abdomen with a pillow. c. Explain the importance of controlled coughing. d. Administer pain medication. ANS: B Giving pain medication and explaining the importance of coughing may be effective, but the best initial action would be splinting the incision with a pillow. Deep breathing should be done in addition to, not in place of, coughing. PTS: 1 DIF: Cognitive Level: Application REF: 91, Table 5-2 OBJ: 7 (clinical) TOP: Maintenance of Ventilation KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 19. The nurse is educating the patient about vitamins and wound healing. The nurse explains that which vitamin will enhance wound healing the most? a. Vitamin A b. Vitamin B c. Vitamin C d. Vitamin E ANS: C Vitamin C helps with the production of collagen, which restores damaged tissues. PTS: 1 DIF: Cognitive Level: Comprehension REF: 88 OBJ: 6 (clinical) TOP: Promotion of Wound Healing KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 20. The nurse is caring for a patient following abdominal surgery. The patient asks the nurse when he will be able to eat a normal diet. Which response is best? a. “It will depend on how well you tolerate advancing from a clear liquid diet.” b. “We will have to wait until your surgeon orders a regular diet for you.” c. “Most patients are able to eat regular foods within 2 to 3 days following abdominal surgery.” d. “Once you have bowel sounds and are passing gas, you may have clear liquids, and your diet will be advanced based upon your tolerance.” ANS: D Although the diet order originates with the physician, the nurse must ensure that bowel sounds are present and the patient is able to pass flatus before any type of diet can be given to the patient. Most surgeons will write an order to advance the diet as tolerated once these findings occur. Every patient responds differently based upon their body and the type of surgery, so stating that most patients eat regular foods within 2 to 3 days is inaccurate. PTS: 1 DIF: Cognitive Level: Application REF: 86 OBJ: 3 (theory) TOP: Postoperative Diet KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation MULTIPLE RESPONSE 21. The nurse is performing a neurological assessment on a patient who was just transferred from the PACU following abdominal surgery. Which action(s) correctly demonstrate(s) knowledge of a neurological assessment? (Select all that apply.) a. Asking the patient to spell his name. b. Asking the patient to identify where he is. c. Noting if the patient can identify the sensation of touch. d. Asking the patient to move his arms and legs. e. Assessing the patient’s pupils for response to light. ANS: B, C, D, E The level of consciousness, orientation, sensory status, motor skills, and pupillary responses are all integral components of the neurological assessment. Asking the patient to spell his name is not an assessment of neurological status, particularly immediately following surgery. PTS: 1 DIF: Cognitive Level: Application REF: 80 OBJ: 5 (clinical) TOP: Neurologic Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 22. The nurse is performing the Aldrete scoring system. Which factor(s) must be assessed? (Select all that apply.) a. Activity b. Circulation c. Presence of wound drainage d. Level of consciousness e. O2 saturation ANS: A, B, D, E The Aldrete scoring system requires that the nurse assess activity, circulation, respiration, level of consciousness, and oxygen saturation. PTS: 1 DIF: Cognitive Level: Comprehension REF: 81 OBJ: 1 (theory) TOP: Aldrete Scoring System KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 23. Following an outpatient procedure for which the patient received general anesthesia, which finding(s) indicate(s) to the nurse that the patient is ready to be discharged? (Select all that apply.) a. The patient ambulates to the bathroom with minimal assistance. b. The patient cannot read and voice an understanding of discharge instructions. c. The patient has been awake for 2 hours. d. The patient is able to empty the bladder. e. The patient plans to drive home. ANS: A, D The criteria for discharge from day surgery are the ability to ambulate unassisted and to empty the bladder. Following general anesthetic, a responsible person may receive the discharge instructions and a written copy should be provided to the patient; being awake for 2 hours is not discharge criteria; and patients cannot drive any distance after general anesthesia. PTS: 1 DIF: Cognitive Level: Application REF: 81 OBJ: 5 (theory) TOP: Day Surgery KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 24. When providing written discharge instructions, which information should the nurse include? (Select all that apply.) a. When to resume normal activity b. Signs and symptoms to report c. A list of probable complications d. The telephone number of the surgeon’s office e. The need to delay driving and decision making ANS: A, B, D, E The discharge instructions should include information about when to resume activity, signs and symptoms to report, contact information about the surgeon, and the need to delay driving and decision making. PTS: 1 DIF: Cognitive Level: Comprehension REF: 95-96, Patient Teaching OBJ: 9 (clinical) TOP: Discharge Instructions KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 25. The nurse is caring for a patient 48 hours after mastectomy surgery. The nurse is teaching the nursing student about Core Measures. The nursing student correctly implements which Core Measure intervention(s)? (Select all that apply.) a. Administering prophylactic antibiotic therapy 48 hours following surgery. b. Encouraging the older patient to use the call light attached to her when ambulating to the bathroom. c. Asking the patient to rate her pain on a pain scale. d. Ensuring that anti-embolic stockings are removed during bathing. e. Assisting the patient with incentive spirometer every 4 hours. ANS: B, D Core Measures for postsurgical patients, issued by The Joint Commission, address prevention of falls and antithrombosis therapy, which are demonstrated by encouraging use of the call light and anti-embolic stockings that may be removed during skin care. Core Measures state that prophylactic antibiotics should be discontinued within 24 hours after surgery. The pain scale and incentive spirometer are not Core Measure guidelines. In addition, use of the incentive spirometry should occur more often than every 4 hours. PTS: 1 DIF: Cognitive Level: Application REF: 84 OBJ: 6 (clinical) TOP: Core Measures KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care COMPLETION 26. The nurse in the PACU performs postsurgical assessments on the newly admitted patient every _________ minutes. ANS: 15 fifteen The staff in PACU make postoperative assessments every 15 minutes on the newly admitted patient. PTS: 1 DIF: Cognitive Level: Knowledge REF: 82, Focused Assessment OBJ: 5 (theory) TOP: Immediate Postoperative Care KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 27. The nurse assesses the musty odor coming from the wound drainage as being indicative of an infection by a(n) ____________ organism, such as Pseudomonas or Staphylococcus. ANS: aerobic A musty odor from the wound drainage is indicative of an infection by an aerobic microorganism such as Pseudomonas or Staphylococcus. PTS: 1 DIF: Cognitive Level: Application REF: 89 OBJ: 4 (theory) TOP: Wound Infection KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 28. A postsurgical patient consumed a cup of ice chips filled to the 120-mL mark, 2 ounces of broth, and 120 mL of water. In addition, 750 mL of intravenous fluids were infused. The patient voided 650 mL and vomited 100 mL. What is the total intake for this patient? ________ mL What is the total output for this patient? ________ mL ANS: 990; 750 One cup of ice is equal to one-half cup of water. Therefore, 120 mL of ice is 60 mL of intake. One ounce is equal to 30 mL, so 2 ounces equals 60 mL. Therefore, the combined intake is 990 mL and the combined output is 750 mL. PTS: 1 DIF: Cognitive Level: Application REF: 86, Clinical Cues OBJ: 6 (clinical) TOP: Intake and Output KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance Chapter 06: Infection Prevention and Control deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is teaching a patient about infection prevention. The nurse points out that covering the mouth and nose with a tissue for a sneeze reduces the probability of infection spreading by which route? a. Droplet b. Airborne c. Direct contact d. Indirect contact ANS: A Infection from the droplet route requires the pathogens be expelled in droplets from the host and inhaled by another host. PTS: 1 DIF: Cognitive Level: Comprehension REF: 101 OBJ: 1 (theory) TOP: Disease-Producing Pathogens KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 2. The nurse is providing infection control teaching to a patient. Which patient statement warrants additional patient teaching? a. “It is important that I get my whooping cough vaccination as directed by my health care provider.” b. “Getting plenty of sleep each night will help my immune system.” c. “I should wash my hands before preparing my food.” d. “It is important that I take my antibiotic until my symptoms have completely resolved.” ANS: D Antibiotics must be completed in entirety. Partial completion of a protocol of prescribed antimicrobial medication can cause a pathogen to become resistant to that particular drug. Vaccinations, adequate rest, and proper hand hygiene are important infection control measures. PTS: 1 DIF: Cognitive Level: Application REF: 101, 113, Table 6-7 OBJ: 1 (theory) TOP: Infection Control Measures KEY: Nursing Process Step: Evaluation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 3. When the patient complains, “If this viral infection I have right now can’t be helped by antibiotics, why am I taking this expensive acyclovir?” How should the nurse respond? a. “Acyclovir is an antiviral drug that kills viruses.” b. “Acyclovir is given to many patients with viral infections.” c. “Acyclovir is an antiviral drug that prevents your infection from becoming worse.” d. “Acyclovir helps strengthen your immune system.” ANS: C The patient currently has a viral infection; acyclovir is an antiviral drug that will decrease the virulence of the infection if started in the early phase of the infection. The drug may not kill the virus and is not given frequently to patients with viruses. Acyclovir will not strengthen the immune system. PTS: 1 DIF: Cognitive Level: Application REF: 101 OBJ: 8 (theory) TOP: Viruses KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 4. The clinic nurse offers suggestions to a patient who is planning a trip to Mexico that will help prevent a protozoan infection. Which suggestion is most helpful? a. “Ask the doctor for a prophylactic prescription for an antiviral drug.” b. “Broad-spectrum antibiotics will be most helpful if you contract a protozoan infection.” c. “Be sure to practice good hand hygiene while on your vacation.” d. “It would be best if you drank bottled water while on your trip.” ANS: D Protozoa frequently live in the water and soil and cause infection by ingestion of the parasite. Water in many foreign countries contains protozoa, so drinking bottled water is the best suggestion. PTS: 1 DIF: Cognitive Level: Application REF: 101 OBJ: 1 (theory) TOP: Protozoa KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 5. While assessing an obese resident in a long-term care facility, the nurse finds a red, moist rash under the patient’s breasts, in the axilla, and in the inguinal fold. Based on this assessment, the nurse reports to the charge nurse that the resident probably has which type of infection? a. A fungal infection b. A bacterial infection c. An allergic reaction d. Contact dermatitis ANS: A Fungal infections thrive in warm, moist environments and most frequently affect the skin. PTS: 1 DIF: Cognitive Level: Comprehension REF: 102 OBJ: 1 (theory) TOP: Fungi KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 6. A frustrated patient with a fungal infection complains, “Why is the infection taking so long to heal?” Which response is most appropriate? a. “Fungal infections are essentially incurable.” b. “Fungi form spores, which make them difficult to kill.” c. “Fungi can be considered natural flora and are protected by the body.” d. “Fungi can alter the patient’s DNA and RNA.” ANS: B Fungi are capable of forming spores, which makes them resistant to antifungal agents. PTS: 1 DIF: Cognitive Level: Comprehension REF: 102 OBJ: 1 (theory) TOP: Fungi KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 7. The nurse explains to the patient who is using Prilosec (a proton pump inhibitor) that the drug reduces the amount of which natural protector in the stomach lining? a. Lactic acid b. Lysozyme c. Cilia d. Fatty acids ANS: B Lysozyme is found in the lining of the stomach and in the stomach acids. PTS: 1 DIF: Cognitive Level: Knowledge REF: 102 OBJ: 2 (theory) TOP: Chemical Barrier KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 8. How should the home health nurse advise the patient to treat a fever of 100° F? a. Take aspirin as needed. b. Take Tylenol every 4 to 6 hours. c. Bathe in cool water before bed. d. Do nothing at all. ANS: D Allowing reasonable levels of fever allows the body’s natural defenses to make a hostile environment to the pathogen through heat. PTS: 1 DIF: Cognitive Level: Application REF: 103 OBJ: 3 (theory) TOP: Fever KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 9. The home health nurse is providing dietary recommendations to keep the immune system healthy. The patient demonstrates understanding by increasing intake of which foods? a. Eggs and beans b. Celery and water c. Pasta and bread d. Olive oil and peanuts ANS: A Protein stores must be kept at an adequate level in order to produce antibodies, thus boosting the immune system. Eggs and beans are a good source of protein. Increasing intake of celery and water increases fluid. Pasta and bread are carbohydrate-rich foods. Olive oil and peanuts feature unsaturated fats. Fluids, carbohydrates, and unsaturated fats will not enhance the immune system. PTS: 1 DIF: Cognitive Level: Application REF: 103 OBJ: 8 (theory) TOP: Nutrition KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 10. The nurse is caring for several patients and determines which patient to be most at risk for developing an infection related to a decreased anti-inflammatory response? a. A patient who has been experiencing high levels of stress for the last 3 months. b. A patient with a glycosylated Hgb level of 6.7%. c. A patient with osteoarthritis who was recently diagnosed. d. A patient who is scheduled for laparoscopic cholecystectomy in 2 weeks related to gallstones. ANS: A The presence of increased levels of cortisol resulting from ongoing stress inhibits the anti-inflammatory response, thus making this patient most susceptible to developing an infection. A glycosylated Hgb level of 6.7% is normal; osteoarthritis and gallstones would not significantly increase a patient’s likelihood of developing an infection. PTS: 1 DIF: Cognitive Level: Application REF: 100, Box 6-1, 103 OBJ: 10 (clinical) TOP: Cortisol KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 11. To which entity should the home health nurse make a referral in order to supply a home-bound older adult with a daily meal? a. A community food bank b. The Salvation Army c. An agency supplying food stamps d. Meals on Wheels ANS: D Meals on Wheels provides a large, nutritious meal to home-bound people. A community food bank, the Salvation Army, and food stamps would not adequately assist a home-bound individual. PTS: 1 DIF: Cognitive Level: Comprehension REF: 103, Older Adult Care Points OBJ: 1 (clinical) TOP: Nutrition KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 12. The nurse uses a visual aid to demonstrate how which antibody attaches to the antigen to clear the pathogen from the body? a. IgA b. IgD c. IgG d. IgM ANS: D Immunoglobulin M (IgM) is the antibody that recognizes the foreign protein and attaches itself to it in order to clear the pathogen from the body. PTS: 1 DIF: Cognitive Level: Knowledge REF: 104, Table 6-2 OBJ: 2 (theory) TOP: Antibodies KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 13. The nurse explains that exposure to a pathogen stimulates the macrophages to migrate to the area of infection to ingest and destroy the pathogen. This statement describes which process? a. Pathogen neutralization b. Immune response c. Antibody action d. Phagocytosis ANS: D Phagocytosis is the process of the ingestion of a pathogen by macrophages. PTS: 1 DIF: Cognitive Level: Knowledge REF: 104 OBJ: 2 (theory) TOP: Phagocytosis KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 14. The patient complains of the unsightly swelling of her lip at the site of an infection. The nurse explains that the swelling is part of the inflammatory response and performs which action? a. Stores blood b. Acts as a compression wall c. Provides an antibody reservoir d. Produces leukocytes ANS: B The swelling of the inflammatory response acts as a compression wall to delay the spread of harmful agents to the rest of the body. PTS: 1 DIF: Cognitive Level: Comprehension REF: 106 OBJ: 2 (theory) TOP: Inflammatory Response KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 15. The nurse is providing infection control teaching to a group of patients. Which statement demonstrates that the patient understands the nurse’s teaching? a. “I should take an antibiotic at the first sign of an infection.” b. “Hand hygiene is one of the most effective ways I can prevent the spread of infection.” c. “Vaccinations only prevent a disease from becoming severe.” d. “If I eat a nutritious diet, it will be difficult for me to get an infection.” ANS: B Hand hygiene is the most effective single act that can reduce the spread of disease. Antibiotics should not be taken at the first sign of infection, especially if the infection is caused by a virus; vaccinations can also prevent diseases from occurring; a nutritious diet is only one component in the prevention of infection. PTS: 1 DIF: Cognitive Level: Application REF: 107 OBJ: 2 (theory) TOP: Hand Hygiene KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 16. The nurse discusses and demonstrates proper hand hygiene to an immunocompromised patient and his wife. Which statement indicates a need for additional teaching? a. “It is okay for my wife to wear artificial nails as long as she washes her hands properly.” b. “I should always wash my hands before I eat.” c. “Hand gels work as well as handwashing under most circumstances.” d. “I should use friction and wash my hands for about 20 seconds if I am using soap and water.” ANS: A Artificial nails harbor microorganisms regardless of good hand hygiene. Washing hands prior to eating is good practice, as well as using friction and washing for 15 to 30 seconds with soap and water. Hand gels are effective in most circumstances except for certain infections such as C. difficile and C. albicans. PTS: 1 DIF: Cognitive Level: Application REF: 107-108 OBJ: 2 (clinical) TOP: Hand Hygiene KEY: Nursing Process Step: Evaluation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 17. The nurse explains that a vaccination provides defense against infection via which type of immunity? a. Innate immunity b. The inflammatory response c. Antibody-mediated immunity d. Cell-mediated immunity ANS: C Vaccinations produce an antibody-mediated immunity by stimulating the host to develop specific antibodies against specific diseases. PTS: 1 DIF: Cognitive Level: Knowledge REF: 105, Table 6-3 OBJ: 2 (theory) TOP: Immune Response KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 18. The nurse is planning care for a patient and determines that Expanded Precautions are warranted when performing care for a patient with which infection? a. Active tuberculosis (TB) b. Bacterial pneumonia c. A urinary tract infection (UTI) caused by E. coli d. A fungal infection of the groin and axilla ANS: A Active TB can be spread by airborne pathogens. Masks and gowns, in addition to gloves, should be worn while caring for such patients. Standard Precautions would be used for patients with bacterial pneumonia, a UTI caused by E. coli, and a fungal infection of the groin and axilla. PTS: 1 DIF: Cognitive Level: Application REF: 109, Table 6-5 OBJ: 5 (theory) TOP: Expanded Precautions KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 19. The nurse is caring for a patient with C. difficile infection. Which action is most important for the nurse to take? a. Only use alcohol-based hand cleanser for hand hygiene. b. Always wear an impervious mask. c. Don proper eye protection before providing care. d. Notify housekeeping to use appropriate cleaning agents. ANS: D Notification of housekeeping to use alcohol-free cleaners is necessary in order to eradicate the pathogen. Soap and water must be used after contact with this organism because alcohol-based hand sanitizers do not adequately kill the microorganism. A mask and eye protection are not necessary. PTS: 1 DIF: Cognitive Level: Application REF: 113 OBJ: 9 (clinical) TOP: Prevention of Health Care–Associated Infections KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 20. The nurse is caring for a patient with general sepsis. Which finding should first alert the nurse to a potential complication that warrants immediate attention? a. Increased lethargy b. Sudden coughing c. Elevated blood pressure d. Cloudy urine ANS: A Increasing lethargy is an indicator of impending septic shock. Coughing and cloudy urine are not signs of impending septic shock. Decreased rather than increased blood pressure would indicate impending septic shock. PTS: 1 DIF: Cognitive Level: Application REF: 115 OBJ: 1 (theory) TOP: Septic Shock KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 21. The nurse who suffers an accidental needle stick following administration of an intramuscular injection to a patient anticipates that facility protocol will suggest immediate treatment with which type of immunotherapy? a. IgM b. IgD c. Ig A d. IgG ANS: D IgG is frequently given to provide passive immunity until the body’s own immune system can defend itself; therefore, it would most likely be a component of a health care facility’s initial treatment protocol for accidental needle sticks. IgM, IgD, and IgA would not be indicated. PTS: 1 DIF: Cognitive Level: Comprehension REF: 104, Table 6-2 OBJ: 1 (theory) TOP: Immunoglobulins KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 22. The nurse provides discharge teaching about antibiotic therapy. Which statement indicates that the patient requires additional teaching? a. “I should wait 3 days after my symptoms resolve before stopping my antibiotic.” b. “I should try to take my medication as evenly spaced apart as possible.” c. “If I start feeling worse, I should call my health care provider.” d. “I should not share my medication with anyone.” ANS: A The antibiotic should be taken until it is completely gone in order to ensure the infection has been adequately treated. Antibiotics are more effective if spaced evenly apart when taken. The patient should continue to improve if therapy is effective, so the health care provider should be notified if symptoms are not improving. Patients should never share any type of prescribed medication. PTS: 1 DIF: Cognitive Level: Application REF: 113, Table 6-7 OBJ: 8 (theory) TOP: Antimicrobial Therapy KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance MULTIPLE RESPONSE 23. The nurse instructs the nursing assistant in a long-term care facility regarding infection control measures. Which action(s) demonstrate(s) that the nursing assistant understands the nurse’s teaching? (Select all that apply.) a. Assisting residents with hand hygiene before meals. b. Cleaning incontinent residents as soon as possible. c. Administering prescribed antibiotics during meals to residents who require assistance with feeding. d. Inspecting residents’ skin for open areas during bathing. e. Assisting residents with hand hygiene after participating in group activities. ANS: A, B, D, E It is important for the nursing assistant to assist residents with hand hygiene prior to meals and after participating in group activities in order to help prevent the spread of infection. Cleaning incontinent residents as soon as possible prevents skin breakdown, which may lead to infection. While bathing residents, the nursing assistant should monitor for signs of skin breakdown and report any areas to the nurse. Nursing assistants are not permitted to administer medications. PTS: 1 DIF: Cognitive Level: Application REF: 121 OBJ: 10 (clinical) TOP: Infection Control Measures KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 24. Which areas of the body is/are protected by normal flora? (Select all that apply.) a. Skin b. Bladder c. Lower gastrointestinal (GI) tract d. Nose and throat e. Eye ANS: A, C, D, E Normal flora inhabit and protect the skin, lower GI tract, nose and throat, and eyes. The bladder does not have any natural flora for protection. PTS: 1 DIF: Cognitive Level: Comprehension REF: 100, Table 6-1 OBJ: 2 (theory) TOP: Natural Flora KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 25. The nurse is obtaining a health history on a newly admitted patient. Which information alerts the nurse that the patient is at increased risk for developing an infection? (Select all that apply.) a. The patient reports having unprotected heterosexual sex in three previous relationships. b. The patient is employed as a biochemist in a hospital. c. The patient’s income is considered middle-class level. d. The patient reports getting 4 to 5 hours of sleep per night. e. The patient is 21% over the suggested normal weight. ANS: A, D, E This patient’s lifestyle habits, insufficient sleep, and being obese increase the chance of developing an infection by the strain placed on the immune system. This patient’s occupation and income level would not increase the risk for infection. PTS: 1 DIF: Cognitive Level: Application REF: 100, Box 6-1 OBJ: 10 (clinical) TOP: Risk Factors KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance COMPLETION 26. The nurse explains that an infection occurring in the body represents an interrelationship between the __________, __________, and __________. ANS: host, agent, environment host, environment, agent agent, host, environment agent, environment, host environment, host, agent environment, agent, host A pathologic agent, upon entering the body, must attach to a host in order to multiply in a supportive environment. PTS: 1 DIF: Cognitive Level: Application REF: 100, Box 6-1 OBJ: 1 (theory) TOP: Infection Process KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 27. The bacteria that are rod-shaped are classified as _________. ANS: bacilli Bacilli are rod-shaped bacteria. PTS: 1 DIF: Cognitive Level: Knowledge REF: 101 OBJ: 1 (theory) TOP: Bacteria KEY: Nursing Process Step: N/A MSC: NCLEX: Health Promotion and Maintenance 28. The nurse explains that the four lines of defense the body employs to combat infection are inflammatory response, immune response, __________, and __________. ANS: skin, normal flora normal flora, skin The body is defended against infection by the skin, normal flora, and inflammatory and immune responses. PTS: 1 DIF: Cognitive Level: Comprehension REF: 102 OBJ: 2 (theory) TOP: Defense Against Infection KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation Chapter 07: Care of Patients with Pain deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. In order to provide the optimum nursing care, it is important for the nurse to know that the standard of pain and pain control is best determined by which person? a. Physician b. Nurse c. Patient’s family d. Patient ANS: D Only the patient knows when pain occurs and what remedy relieves it. PTS: 1 DIF: Cognitive Level: Knowledge REF: 127 OBJ: 1 (theory) TOP: Pain Theory KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 2. The nurse clarifies the basics of the gate theory of pain control. Which information should the nurse include? a. Pain is perceived as opening a “gate” to pain symptoms. b. The “gate” can be closed to pain by the use of nonpainful stimuli. c. The “gate” swings back and forth, first allowing pain, then blocking it. d. The patient can be trained to close the “gate” to pain. ANS: B The sensorineural “gate” can be closed by applying a number of nonpharmacologic stimuli so that the pain is not perceived. PTS: 1 DIF: Cognitive Level: Comprehension REF: 124 OBJ: 1 (theory) TOP: Gate Theory KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 3. When giving care to a 30-year-old Hispanic male, which action can most likely be attributed to the patient’s cultural beliefs about pain? a. The patient maintains a stoic affect about pain. b. The patient prefers a pill to an injection. c. The patient ignores somatic interventions such as heat and massage. d. The patient confesses to pain but refuses pain medication. ANS: A Hispanic males are frequently stoic regarding pain. They prefer injections to pills but may elect to use prayer, heat, or herbal remedies for pain relief. PTS: 1 DIF: Cognitive Level: Application REF: 131, Cultural Considerations OBJ: 4 (theory) TOP: Cultural Considerations KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 4. The nurse is caring for a patient who is having constant nociceptor pain. Which intervention best addresses the patient’s pain during the perception phase of pain? a. Administer nonsteroidal anti-inflammatory drugs (NSAIDs) for moderate pain. b. Ask the physician if an opioid could be ordered to treat the patient’s pain when severe. c. Engage the patient in conversation regarding his family, hobbies, and plans following discharge from the facility. d. Determine if the patient typically takes a neurotransmitter uptake blocker medication for pain control. ANS: C Nonpharmacologic interventions such as distraction and guided imagery are effective for pain relief during the perception phase. NSAIDs are most effective during the transduction phase of pain, opioids are most effective during the transmission phase, and drugs that block neurotransmitter uptake work best during the modulation phase. PTS: 1 DIF: Cognitive Level: Application REF: 125 OBJ: 3 (theory) TOP: Pain Perception KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 5. The patient is experiencing phantom pain following the amputation of her foot. Which type of pain is most associated with phantom pain? a. Nociceptive b. Mild c. Uncontrollable d. Neuropathic ANS: D Neuropathic pain is associated with a dysfunction of the nervous system that involves an abnormality in the processing of sensations such as phantom pain. Nociceptive pain is associated with pain stimuli from either somatic (body tissue) or visceral (organs) structures. Mild and uncontrollable refer to severity rather than classifications of pain. PTS: 1 DIF: Cognitive Level: Comprehension REF: 126, Table 7-1 OBJ: 1 (theory) TOP: Neuropathic Pain KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 6. The nurse explains that the pain threshold and pain tolerance are different. Which statement about the pain threshold is true? a. Pain threshold is the point at which pain is perceived. b. Pain threshold is the point at which the person responds to pain. c. Pain threshold is the point at which pharmacologic intervention is required. d. Pain threshold is the point at which signs such as grimacing or groaning are observed. ANS: A The pain threshold is the point at which the pain is perceived. PTS: 1 DIF: Cognitive Level: Knowledge REF: 127 OBJ: 1 (theory) TOP: Pain Threshold KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 7. The patient who had abdominal surgery this morning refuses the opioid pain medication for fear of addiction. How should the nurse respond? a. “Opioids are addictive, whereas nonsteroidal anti-inflammatory drugs (NSAIDs) are not.” b. “Addiction is mainly a matter of attitude.” c. “Fewer than 3% of people become addicted to drugs used for pain relief.” d. “Although addiction does occur, it is quickly reversed.” ANS: C Pain from abdominal surgery is acute pain. This patient is not experiencing chronic pain that will require ongoing pain medication, and addiction occurs in fewer than 3% of people who take pain medication. Any medication can be addictive. Addiction is often not merely a matter of attitude. Finally, addictions typically require long-term therapy. PTS: 1 DIF: Cognitive Level: Application REF: 134, Table 7-4 OBJ: 5 (theory) TOP: False Perception About Pain KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 8. Which student nurse’s note in the patient’s record features proper documentation of a pain assessment? a. Pt. complains of local sharp pain (4/5) in lower abdomen upon standing. b. Pt. complains of stomach pain after eating (3/5). c. Pt. reports standing makes his stomach hurt. d. Pt. reports sharp pain in stomach. ANS: A The recorded assessment should include location, characteristics, quantity, severity based on a pain scale, and pattern. PTS: 1 DIF: Cognitive Level: Comprehension REF: 134 OBJ: 8 (clinical) TOP: Pain Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 9. The nurse is educating the home health patient about indications for acetaminophen. Which information should the nurse include in the teaching plan? a. Take acetaminophen as frequently as needed. b. Take acetaminophen before pain becomes severe. c. Take acetaminophen when pain becomes unbearable. d. Take acetaminophen sparingly and with caution. ANS: B Taking medication before pain becomes severe controls pain best. Once taken, the medication should be taken on the prescribed schedule until pain is well controlled. Taking acetaminophen too frequently could lead to toxicity and liver problems. Waiting until the pain becomes unbearable will require larger amounts of analgesics to control the pain. Acetaminophen may be used as needed. PTS: 1 DIF: Cognitive Level: Application REF: 134, Patient Teaching OBJ: 6 (theory) TOP: Pain Medication KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 10. While bathing a patient, the nurse notes that a transdermal patch that was meant to be on the patient for 3 days is now gone on the second day. What action should the nurse take? a. Document the loss and apply a fresh patch to be replaced in 3 days. b. Report the loss to the charge nurse. c. Document the loss, replace the patch, and continue with the original schedule for replacement. d. Remind the patient that oral pain relief will be available until the patch is replaced in 24 hours. ANS: A The patch should be replaced after the loss is documented, and the schedule should be changed. There is no need for the patient to wait for a new patch to be applied in 24 hours. PTS: 1 DIF: Cognitive Level: Application REF: 136 OBJ: 6 (theory) TOP: Transdermal Patches KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 11. The patient on frequent doses of meperidine (Demerol) complains of constipation. Which initial intervention is best? a. Offer fruit such as prunes or apricots. b. Request an order for an enema. c. Report the condition to the charge nurse. d. Increase oral fluid intake. ANS: D Increasing fluid intake is the best initial approach because additional fluid allows the body to correct the problem naturally. Fruits can be offered, but increasing the fluid intake is the most effective and priority intervention. An enema is invasive and is not an early intervention for constipation. The nurse should be able to implement proper care without reporting the constipation to the charge nurse. PTS: 1 DIF: Cognitive Level: Application REF: 137 OBJ: 10 (clinical) TOP: Common Side Effects KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 12. Because of the threat of lowering the seizure threshold, the home health nurse would suggest that the 85-year-old patient limit the use of which pain medication? a. Ibuprofen (Motrin) b. Naproxen (Aleve) c. Tramadol (Ultram) d. Acetaminophen (Tylenol) ANS: C Tramadol (Ultram) is associated with a lowered seizure threshold in the older adult. PTS: 1 DIF: Cognitive Level: Comprehension REF: 138, Older Adult Care Points OBJ: 7 (theory) TOP: Common Side Effects KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 13. The home health nurse educates the 75-year-old patient about the warm compresses he is using on his swollen elbow. Which information is most important to include in the teaching plan? a. Apply the warm compress directly on the skin. b. Allow the compress to remain in place for 15 to 20 minutes. c. Take aspirin 30 minutes prior to applying the compress. d. Alternate the warm compress with an ice pack every 10 minutes. ANS: B Applications of heat should only be left in place for 15 to 20 minutes. The warm compress should not be applied directly on the skin. The warm compress does not need to be combined with pharmacologic therapy, and aspirin therapy may not be indicated. The nurse should consult with the health care provider before suggesting any medication. The compress works to offer mild pain relief by vasodilation; these effects would be negated by alternating the warm compress with ice. PTS: 1 DIF: Cognitive Level: Application REF: 138 OBJ: 10 (clinical) TOP: Nonpharmacologic Approaches KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 14. The hospitalized postsurgical patient is reluctant to take the opioid pain medication because of drowsiness. Which response is most informative for the nurse to make? a. “Mental stimulation after the medication will keep you more alert.” b. “Sleep and pain relief promote healing.” c. “Drowsiness is an undesirable side effect.” d. “The medication should be taken only before bedtime.” ANS: B Effective analgesia and adequate rest and sleep promote healing. Mental stimulation after taking an opioid will most likely not be effective for keeping the patient alert. Drowsiness is an expected effect. The medication should be taken as prescribed, not just before bedtime. PTS: 1 DIF: Cognitive Level: Application REF: 138 OBJ: 9 (clinical) TOP: Nonpharmacologic Approaches KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 15. To help with pain control, how should the nurse time the distraction activities for a patient? a. To coincide with mealtimes b. To bridge the time between administration and onset c. To occur just before bedtime d. To awaken the patient in the morning ANS: B Distraction is helpful with pain control between administration of the analgesia and its onset. Mealtimes, bedtime, and sleep should not be interrupted with distraction activities. PTS: 1 DIF: Cognitive Level: Comprehension REF: 139 OBJ: 10 (clinical) TOP: Nonpharmacologic Approaches KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 16. A patient reports pain relief after having received a placebo. Which conclusion is most accurate for the nurse to determine? a. The patient was not actually experiencing pain. b. The patient was relieved of the anxiety that there is no ready source of pain remedy. c. The patient was demonstrating “attention-seeking” behavior. d. The patient was being manipulative. ANS: B Much pain is associated with anxiety that there will be no pain remedy available. The delivery of a placebo relieves pain as it relieves the anxiety. PTS: 1 DIF: Cognitive Level: Comprehension REF: 134, Table 7-4 OBJ: 6 (theory) TOP: False Perception about Pain KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 17. The nurse is caring for a 45-year-old male Arab patient who is in pain. Which action can most likely be attributed to the patient’s cultural belief about pain? a. The patient never requests pain medication. b. The patient asks for pain relief to control pain. c. The patient becomes irritable and demanding when in pain. d. The patient hides pain from his family. ANS: B Individuals of Arab descent generally view pain as something to be controlled and will probably call for pain remedy frequently and expect prompt response. Arabs will express pain to their family. PTS: 1 DIF: Cognitive Level: Application REF: 131, Cultural Considerations OBJ: 4 (theory) TOP: Cultural Beliefs about Pain KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 18. The nurse is caring for a patient that is receiving intravenous morphine sulfate. The patient breaks out in hives and begins to itch. What should the nurse do first? a. Obtain the patient’s vital signs. b. Stop the infusion. c. Report the patient’s condition to the charge nurse. d. Give the prescribed antihistamine. ANS: B The drug should be stopped immediately so that the patient does not receive any more of the medication. After completing this priority intervention, the nurse should then obtain the patient’s vital signs, report all findings to the charge nurse, and administer the prescribed antihistamine. PTS: 1 DIF: Cognitive Level: Analysis REF: 137 OBJ: 9 (clinical) TOP: Allergy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 19. The nurse is planning to teach a family member about effective massage techniques. Which information is most important to include in the teaching plan? a. Use heat and a mild menthol cream for comfort. b. Pound painful areas with the sides of the hands. c. Gently and firmly massage of areas of inflammation. d. Use long, firm strokes while avoiding areas of inflammation. ANS: D Long, firm, and smooth strokes on areas that are not inflamed will direct the patient’s attention away from the painful area. Heat and menthol cream used together may cause a burn. PTS: 1 DIF: Cognitive Level: Application REF: 139 OBJ: 10 (clinical) TOP: Massage KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 20. The nurse explains that acupressure and acupuncture are effective pain relief modalities that focus on specific body areas. Which term best describes these therapies? a. Triangulation b. Hot spots c. Meridians d. Zones ANS: C The Asian therapies of acupuncture and acupressure use body areas called meridians. PTS: 1 DIF: Cognitive Level: Knowledge REF: 139 OBJ: 7 (theory) TOP: Acupuncture and Acupressure KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 21. The nurse is caring for a patient who is 1-day postoperative following a colon resection. The patient has degenerative joint disease and uses a pain medication patch to control this chronic pain. Which consideration is most important when planning care for this patient? a. Understand that the pain medication patch will control the postoperative pain. b. Realize that this patient will most likely require more pain medication than most patients undergoing a colon resection. c. Recognize that the patient will be afraid to ask for additional pain medication for fear of being viewed as addicted to pain medicine. d. Expect the patient to forget about the pain caused from the degenerative joint disease. ANS: B Patients who are being treated for chronic pain often require higher doses of pain medication to treat postoperative pain. The patient’s pain medication patch will not likely treat the postoperative pain. There is no indication that the patient will be afraid to ask for additional pain medication, and the patient is not likely to forget about the postoperative pain. PTS: 1 DIF: Cognitive Level: Application REF: 127, Clinical Cues OBJ: 6 (theory) TOP: Acute vs. Chronic Pain Management KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 22. The nurse is planning care plans for multiple patients. Which patient does the nurse anticipate will experience the highest level of pain? a. 28-year-old experiencing pain related to a metatarsal fracture b. 45-year-old experiencing pain following a laparoscopic cholecystectomy c. 67-year-old experiencing chronic back pain d. 79-year-old experiencing pain related to osteoarthritis ANS: D While pain is always dependent on the individual patient’s perception, the older adult tends to be less tolerant to pain due to factors such as having more than one chronic ailment and having fewer resources for tolerating pain. PTS: 1 DIF: Cognitive Level: Application REF: 127, Older Adult Care Points OBJ: 4 (theory) TOP: Pain in Older Adults KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort MULTIPLE RESPONSE 23. The nurse is using the gate theory as a guide to pain management. Which intervention(s) should the nurse plan to offer? (Select all that apply.) a. Massage b. Social activities c. Music d. Interactive distraction e. A quiet environment ANS: A, B, D Music is not effective as a gate closer. High levels of sensory stimulation are more effective for decreasing pain according to the gate theory. PTS: 1 DIF: Cognitive Level: Comprehension REF: 124 OBJ: 1 (theory) TOP: Gate Control Theory KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 24. What is/are the functions of endorphins? (Select all that apply.) a. Inhibition of unpleasant stimuli b. Diminished anxiety c. Relief of pain d. Feeling of euphoria e. Increased blood pressure ANS: A, B, C, D Endorphins are thought to diminish unpleasant stimuli and pain, reduce anxiety, and give feelings of euphoria. PTS: 1 DIF: Cognitive Level: Comprehension REF: 125 OBJ: 3 (theory) TOP: Endorphins KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 25. The nurse is caring for the patient with neuropathic pain. Which agents will most effectively control this patient’s pain? (Select all that apply.) a. Analgesics b. Opioids c. Antidepressants d. Anti-inflammatory agents e. Anticonvulsants ANS: C, D, E Neuropathic pain is best relieved by antidepressants, anti-inflammatory agents, and anticonvulsants. Analgesics and opioids generally do not alleviate neuropathic pain. PTS: 1 DIF: Cognitive Level: Comprehension REF: 126-127 OBJ: 3 (theory) TOP: Neuropathic Pain KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 26. Although the patient with a kidney stone denies pain, the nurse assesses cues that indicate that pain is perceived. Which assessments indicate that pain may be present? (Select all that apply.) a. Increased pulse rate b. Decreased respiratory rate c. Diaphoresis d. Muscle tension e. Nausea ANS: A, C, D, E The respiratory rate increases in patients in acute pain. PTS: 1 DIF: Cognitive Level: Comprehension REF: 128-129 OBJ: 8 (clinical) TOP: Assessment of Acute Pain KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort COMPLETION 27. Pain receptors in the skin, connective tissue, bone, joints, and muscles are classified as __________. ANS: nociceptors Pain receptors in the skin, connective tissue, bone, joints, and muscles are nociceptors. PTS: 1 DIF: Cognitive Level: Knowledge REF: 125 OBJ: 3 (theory) TOP: Nociceptor Receptors KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation MATCHING Arrange the sequence of nociceptive pain in the order in which the process occurs. a. Transmission b. Modulation c. Transduction d. Perception 28. Step 1 29. Step 2 30. Step 3 31. Step 4 28. ANS: C PTS: 1 DIF: Cognitive Level: Comprehension REF: 125, 126, Figure 7-2 OBJ: 3 (theory) TOP: Nociceptive Pain Perception KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 29. ANS: A PTS: 1 DIF: Cognitive Level: Comprehension REF: 125, 126, Figure 7-2 OBJ: 3 (theory) TOP: Nociceptive Pain Perception KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 30. ANS: D PTS: 1 DIF: Cognitive Level: Comprehension REF: 125, 126, Figure 7-2 OBJ: 3 (theory) TOP: Nociceptive Pain Perception KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 31. ANS: B PTS: 1 DIF: Cognitive Level: Comprehension REF: 125, 126, Figure 7-2 OBJ: 3 (theory) TOP: Nociceptive Pain Perception KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation Chapter 08: Care of Patients with Cancer deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The 40-year-old female who was diagnosed with a benign growth in her colon is concerned about the growth spreading. Which explanation best allays the patient’s anxiety? a. “Benign growths arrest their growth on their own.” b. “Benign growths never interfere with normal structures or functions.” c. “Benign growths are easily controlled with radiation.” d. “Benign growths are surrounded by fibrous tissue that prevents spread.” ANS: D Benign neoplasms are encapsulated with a fibrous membrane that interferes with their spreading. They do not self-limit their growth and may obstruct passages or impinge on an organ. They are not treated with radiation. PTS: 1 DIF: Cognitive Level: Application REF: 145 OBJ: 1 (theory) TOP: Physiology of Cancer KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 2. The 26-year-old patient with a malignant neoplasm has experienced a 10-pound weight loss in 3 weeks. To which factor is this patient’s rapid weight loss most likely related? a. Disinterest in eating food in general b. Changes in the nutritional content of the patient’s diet c. The malignancy’s high nutritional demand d. A self-imposed rigid diet regimen ANS: C Rapid cell growth of the malignancy robs nutrients from normal cells and results in weight loss. PTS: 1 DIF: Cognitive Level: Comprehension REF: 146 OBJ: 1 (theory) TOP: Physiology of Cancer KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 3. The nurse recognizes the staging T3, N2, M2 of the patient’s cancer. Which interpretation is correct? a. Small tumor with fewer than two lymph nodes involved. b. Large tumor that is localized. c. Small tumor with adjacent nodes involved. d. Large tumor with extensive lymph node involvement. ANS: D The staging means a large tumor (T3) with involvement in regional lymph nodes (N2) and metastasis to distant lymph nodes (M2). PTS: 1 DIF: Cognitive Level: Analysis REF: 147 OBJ: 1 (theory) TOP: TNM Staging KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 4. The nurse assesses several patients in the outpatient clinic. Which patient has the greatest risk for developing cancer? a. 23-year-old car repairman who repaints cars b. 30-year-old overweight certified public accountant in New York who has smoked for 4 years and rarely exercises c. 45-year-old farmer from Texas who has worked on his family’s cotton farm since the age of 12 d. 60-year-old ski instructor in Colorado ANS: C The cotton farmer in Texas has the most exposure to carcinogens. Chemicals, pesticides, and sun are the carcinogens that this farmer has been exposed to for at least 33 years. PTS: 1 DIF: Cognitive Level: Analysis REF: 148 OBJ: 4 (theory) TOP: Cancer Risk KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 5. The nurse recognizes that smoking is a “promoter” that, although not a carcinogen itself, allows cancer to occur faster in the patients. Which factor is also a promoter of cancer? a. Obesity b. Occupational hazards c. Cocaine abuse d. Heavy alcohol intake ANS: D Alcohol and smoking are “promoters” that facilitate the occurrence of cancer. Being overweight, occupational hazards, and abusing cocaine are not considered “promoters” in regard to cancer risk. PTS: 1 DIF: Cognitive Level: Application REF: 148 OBJ: 2 (theory) TOP: Causative Factors KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 6. The nurse is caring for an x-ray technician who wears a badge that is monitored frequently to measure the amount of radiation he has absorbed. The nurse advises the technician that he has the highest risk for developing which type of cancer? a. Bladder cancer b. Leukemia c. Melanoma d. Lung cancer ANS: B The blood cancer leukemia is associated with radiation exposure. Bladder, melanoma, and lung cancer are associated with other carcinogens. PTS: 1 DIF: Cognitive Level: Application REF: 148, Table 8-1 OBJ: 2 (theory) TOP: Causative Factors KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 7. The nurse is outlining a diet that would be helpful in the prevention of cancer. Which instructions should the nurse include? a. Eliminate all red meat. b. Use margarine instead of butter. c. Avoid foods with vitamin B complex. d. Eat a variety of citrus fruits. ANS: D Vitamin C helps combat the effects of nitrites. Fats should be no more than 30%, and both butter and margarine should be used sparingly. Vitamin B has neither been proven effective for cancer prevention nor deemed harmful. PTS: 1 DIF: Cognitive Level: Application REF: 150, Nutritional ConsiderationsOBJ: 3 (theory) TOP: Prevention of Cancer KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 8. The nurse is advising a young college student who wants a tan before spring break. Which method is safest for the student to use? a. Take advantage of morning sun while using sunscreen with an SPF of 30. b. Use a spray-on tanning solution. c. Use a sun lamp for a maximum of 20 minutes a day. d. Use a tanning salon for no more than 10 minutes per visit. ANS: B Spray-on tanning solution is the safest. All other options increase ultraviolet exposure, even with the use of sunscreen. PTS: 1 DIF: Cognitive Level: Application REF: 148, Table 8-1 OBJ: 3 (theory) TOP: Prevention of Cancer KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 9. The nurse is educating the 40-year-old female patient about the American Cancer Society (ACS) recommendations for early detection of cancer. Which information should she include when teaching? a. Obtain a Pap smear every year. b. Get an annual fecal occult blood examination. c. Plan a sigmoidoscopy every 5 years. d. Obtain a mammogram every year. ANS: D The ACS recommends that 40-year-old women have an annual mammogram and a Pap smear every 2 to 3 years. Yearly fecal occult blood studies and sigmoidoscopy are recommended beginning at age 50. PTS: 1 DIF: Cognitive Level: Comprehension REF: 156, Box 8-1 OBJ: 4 (theory) TOP: Prevention of Cancer KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 10. The nurse assesses a man who is scheduled for a prostate-specific antigen (PSA) test. The nurse understands that which situation could delay the test? a. The patient reports he ate shellfish 48 hours previously. b. The patient reports that he has a history of an enlarged prostate. c. The patient reports having a recent urinary tract infection (UTI). d. The patient’s temperature is 99.0° F. ANS: C The PSA test would be delayed in the event of a recent UTI. Other considerations include teaching about abstaining from sexual activity for 24 to 48 hours before the test and collecting the blood sample prior to the digital examination. Eating shellfish or having a slightly elevated temperature should not alter the test in any way. A history of an enlarged prostate is a good reason to perform a PSA test. PTS: 1 DIF: Cognitive Level: Application REF: 156, Box 8-2 OBJ: 4 (theory) TOP: Prostate-Specific Antigen Test (PSA) KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 11. The nurse is planning care for the patient who is on a protocol of bleomycin. Since bleomycin is an antitumor antibiotic, which intervention should the nurse add to the care plan? a. Assess hearing acuity. b. Measure urinary output. c. Weigh daily to assess fluid retention. d. Monitor for cardiac arrhythmias. ANS: D Bleomycin is cardiotoxic and can cause cardiac arrhythmias; therefore, this would be the highest priority intervention. Chemotherapies that are ototoxic would warrant a hearing test; urinary output and fluid retention should be assessed with most chemotherapy drugs, and especially for those that are nephrotoxic. PTS: 1 DIF: Cognitive Level: Analysis REF: 163, Table 8-4 OBJ: 5 (theory) TOP: Chemotherapy: Bleomycin KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 12. The nurse is caring for a patient with cancer who is receiving vincristine. Which precaution is most important for the nurse to take? a. Prevent the patient from getting chilled. b. Administer a stool softener as ordered. c. Offer the patient a soft toothbrush. d. Feed the patient a snack during the infusion. ANS: B Certain antineoplastic drugs, such as vincristine, vinblastine, and paclitaxel, cause constipation. Increasing fluids (as allowed), adding fiber to the diet, administering stool softeners and fiber laxatives, exercise, and monitoring vigilantly for the beginning signs of constipation are the usual measures taken. Suppositories or enemas may be necessary. Preventing chills does provide comfort but does not work to actively prevent constipation. Offering a soft tooth brush is an appropriate intervention for mediations that increase bleeding risk. Feeding the patient a snack during the infusion may exacerbate constipation. PTS: 1 DIF: Cognitive Level: Analysis REF: 164, Table 8-5 OBJ: 10 (clinical) TOP: Chemotherapy: Vincristine KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 13. The nurse is teaching a 50-year-old male patient who is taking estrogens as treatment of prostate cancer. The nurse should educate the patient about which expected side effect? a. Blurred vision b. Gynecomastia c. Enlarged gonads d. Acne ANS: B Men taking estrogen experience a redistribution of fat and develop enlarged breasts (gynecomastia). Estrogen should not result in blurred vision, enlarged gonads, or acne. PTS: 1 DIF: Cognitive Level: Application REF: 165 OBJ: 10 (clinical) TOP: Chemotherapy: Hormones KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 14. The nurse is instructing a patient who is on a biologic response modifier (BRM) colony-stimulating drug. The nurse teaches that about which desired action from this medication? a. Increased appetite b. Increased hair growth c. Enhanced recovery of bone marrow d. Decreased cholesterol ANS: C BRMs enhance and support the recovery of suppressed bone marrow resulting from radiation and chemotherapy. PTS: 1 DIF: Cognitive Level: Knowledge REF: 166 OBJ: 5 (theory) TOP: Chemotherapy: Biologic Response Modifiers KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 15. The patient on radiation therapy has developed diarrhea. Which food should the nurse suggest to help slow the diarrhea? a. Broccoli b. Cauliflower c. Cheese and crackers d. Apples and pears ANS: C Food low in fiber, such as cheese and crackers, will help slow diarrhea. Broccoli, cauliflower, apples, and pears are high-fiber foods that stimulate bowel evacuation. PTS: 1 DIF: Cognitive Level: Application REF: 168 OBJ: 6 (theory) TOP: Radiation Side Effects: Diarrhea KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 16. The nurse is constructing a teaching plan about fatigue management for a patient who is taking radiation treatments. Which information should the nurse include? a. Prioritize activities and alternate rest with periods of activity. b. Plan to spend at least 4 to 5 hours of the day in bed. c. Discontinue pain medications that may cause drowsiness. d. Avoiding snacking in between meals. ANS: A Prioritizing activities is essential to balance energy with expenditure. These patients should not spend long periods of daytime in bed, and they should increase fluids and plan between-meal snacks to keep energy up. PTS: 1 DIF: Cognitive Level: Application REF: 170 OBJ: 6 (theory) TOP: Radiation Side Effects: Fatigue KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 17. A 32-year-old mother is undergoing radiation from a sealed-source modality and has been isolated in a private room for 3 days. How should the nurse best prepare for the patient’s 8-year-old twins to visit? a. Instruct the children to visit at the bedside one at a time. b. Inform family that children cannot visit patients undergoing radiation. c. Put chairs in the hall for “long-distance” visitation. d. Allow visitation for no longer than 3 minutes without any physical contact. ANS: C Children and pregnant people should not visit at the bedside, but a visit from a safe distance or by phone helps relieve the boredom of isolation. PTS: 1 DIF: Cognitive Level: Application REF: 161, Box 8-3 OBJ: 11 (clinical) TOP: Radiation Care Problems KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 18. Which statement indicates to the nurse that the 50-year-old male recently diagnosed with early stage cancer of the prostate has begun to accept his diagnosis? a. “Well, I guess this just about cancels any plans for a second honeymoon.” b. “I need to call my lawyer in order to update my will.” c. “Do you have any current information on prostate cancer?” d. “My children should come home from college to visit.” ANS: C Well-adjusted patients should seek information on the disease and varied treatments. Joking is a form of denial. Gathering family and making final arrangements reflect loss of hope and do not coincide with the prognosis of early stage prostate cancer. Humor is a positive coping strategy, but requesting information about the disease is more indicative of acceptance. PTS: 1 DIF: Cognitive Level: Analysis REF: 172 OBJ: 11 (clinical) TOP: Acceptance of Diagnosis KEY: Nursing Process Step: Evaluation MSC: NCLEX: Psychosocial Integrity: Coping and Adaptation 19. Following a visit from his family, the 55-year-old male patient with terminal cancer tearfully says, “I am so afraid” and begins to cry. Which response is most supportive? a. “Would you like to have your pain medication now?” b. “Let’s talk about the things that make you afraid.” c. “Would you like for me to call the hospital chaplain.” d. “I will leave to give you some privacy.” ANS: B Verbalizing fears to a caring nurse is comforting. Offering medications, chaplains, and privacy is not helpful or supportive as a first nursing response in this situation. PTS: 1 DIF: Cognitive Level: Application REF: 158 OBJ: 12 (clinical) TOP: Fear KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: Coping and Adaptation 20. The family becomes distressed when the dying 85-year-old patient becomes delirious and laughs and talks with old friends who have long since died. Which intervention is most appropriate? a. Medicate the patient with the prescribed sedative. b. Encourage a family member to talk to the patient calmly. c. Stimulate and reorient the patient. d. Suggest the family to leave the patient for a while. ANS: B Delirious patients can still hear. A familiar voice is comforting. Medicating the patient with a sedative is not appropriate. Stimulating and trying to reorient the patient may cause the patient to become irritated. The family should remain with the patient. PTS: 1 DIF: Cognitive Level: Analysis REF: 175 OBJ: 12 (clinical) TOP: Delirium KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: Coping and Adaptation 21. The student nurse is teaching a community group about risk factors for colorectal cancer. Based on risk factors, which patient has the highest risk for developing colorectal cancer? a. 50-year-old male who has been exposed to arsenic in the workplace b. 45-year-old female with a doctorate degree in psychology who smokes occasionally c. 38-year-old female who had her first child 1 year ago d. 29-year-old male who has had Crohn disease since the age of 13 ANS: D Inflammatory diseases of the colon increase the risk of colorectal cancer. Arsenic exposure places the patient at risk for lung cancer. Women with a high level of education have been found to fall into the high-risk category for developing breast cancer, as well as having the first child after the age of 30. PTS: 1 DIF: Cognitive Level: Application REF: 156, Box 8-2 OBJ: 3 (theory) TOP: Risk Factors KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance 22. Which statement indicates that the patient understands teaching about diagnostic examinations for cancer? a. “I will have less scarring if my surgeon uses an incision to biopsy my breast.” b. “My CEA level will be low if my pancreatic cancer returns.” c. “The doctor will monitor my ovarian cancer remission with the CA-125 test.” d. “My colonoscopy results were great, so I won’t need another one for 5 years.” ANS: C The CA-125 is one of the tests the physician will monitor to detect the presence of ovarian cancer or recurrence of ovarian cancer after therapy. Fine-needle biopsy causes the least amount of scarring during breast cancer biopsy. The patient’s CEA level will rise if pancreatic cancer is present. Recommendations suggest a colonoscopy every 10 years if the examination is negative and there is no family history of colon cancer. PTS: 1 DIF: Cognitive Level: Application REF: 156 OBJ: 3 and 4 (theory) TOP: Diagnostics KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 23. The nurse is caring for a terminally ill cancer patient who is receiving palliative care. The patient’s wife asks how her husband’s pain will be controlled as he nears death. Which is the nurse’s best response? a. “Most of the time we can manage the pain with oral morphine and transdermal pain medication.” b. “We will probably have to start an IV to administer morphine to control the intense pain he may be experiencing.” c. “Dying patients typically do not have any pain, so this will not be an issue.” d. “I will have to check with your husband’s physician to see how he wants us to handle pain control.” ANS: A Oral and transdermal pain control methods are most often used for the terminally ill patient near death. An IV is not typically started on a patient near death who is receiving palliative care. Dying patients do experience pain. The plan of care should be in place for the patient receiving palliative care, so the physician would not be contacted for pain medication orders. PTS: 1 DIF: Cognitive Level: Application REF: 173 OBJ: 12 (clinical) TOP: Pain Control KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort MULTIPLE RESPONSE 24. Which description(s) is/are characteristic of a malignant neoplasm? (Select all that apply.) a. Very small nuclei b. Disorganization c. Altered DNA d. Invasion of nearby organs e. Travel through body fluid ANS: B, C, D, E Malignant neoplasms have large rather than small nuclei. Disorganization, altered DNA, invasion of nearby organs, and the ability to travel through body fluids are all characteristics of malignancies. PTS: 1 DIF: Cognitive Level: Comprehension REF: 145 OBJ: 1 (theory) TOP: Physiology of Cancer KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 25. Which categories are classifications of malignant neoplasms? (Select all that apply.) a. Carcinomas b. Lymphomas c. Fibromas d. Lipomas e. Sarcomas ANS: A, B, E The categories of malignancy are sarcomas, carcinomas, leukemias, and lymphomas. Fibromas and lipomas are benign. PTS: 1 DIF: Cognitive Level: Comprehension REF: 146 OBJ: 1 (theory) TOP: Classification of Tumors KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 26. The nurse explains that metastasis from the original site to a new site can occur in a variety of ways. Which mechanisms do malignant cells use to metastasize? (Select all that apply.) a. Traveling through tissues. b. “Transplantation” via surgical instruments during surgery. c. Entering a body cavity and attaching to an organ. d. Traveling through the lymphatic system. e. “Relocation” from contaminated gloves during surgery. ANS: B, C, D, E Traveling through blood rather than tissues is a common mechanism for metastasis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 146 OBJ: 1 (theory) TOP: MetastasisKEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 27. Which viruses are responsible for specific cancers? (Select all that apply.) a. Liver cancer from hepatitis B virus b. Burkitt lymphoma from Epstein-Barr virus c. Cervical cancer from human papillomavirus d. Lung cancer from measles virus e. Kaposi sarcoma from human immunodeficiency virus ANS: A, B, C, E Hepatitis B virus can cause liver cancer, Epstein-Barr virus can lead to Burkitt lymphoma, HPV can cause cervical cancer, and HIV can lead to Kaposi sarcoma. Measles do not cause lung cancer. PTS: 1 DIF: Cognitive Level: Comprehension REF: 149 OBJ: 2 (theory) TOP: Causative Factors KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 28. Which medications are biologic response modifier (BRM) drugs? (Select all that apply.) a. Interleukins b. Colony-stimulating factors c. Monoclonal antibodies d. Cyclosporines e. Gene therapies ANS: A, B, C, E Cyclosporines are drugs that are used to prevent tissue transplant rejection and are considered a carcinogen for non-Hodgkin lymphoma. In addition to the BRM listed, vaccines are also a BRM. PTS: 1 DIF: Cognitive Level: Comprehension REF: 166 OBJ: 5 (theory) TOP: Biologic Response Modifiers (BRMs) KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Pharmacological Therapies COMPLETION 29. The nurse cautions that stress over a long period of time can contribute to the risk for cancer as prolonged stress suppresses the ____________. ANS: immune system The immune system can be suppressed by prolonged stress. PTS: 1 DIF: Cognitive Level: Comprehension REF: 150 OBJ: 2 (theory) TOP: Causative Factors KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance Chapter 09: Chronic Illness and Rehabilitation deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The rehabilitation nurse describes a patient who is blind, works full time as a Spanish interpreter, and lives with his wife in a downtown apartment. How should the nurse classify this person? a. Impaired b. Disabled c. Handicapped d. Dependent ANS: A The blindness is an impairment of vision that does not inhibit the patient from performing his job or enjoying a normal life. PTS: 1 DIF: Cognitive Level: Comprehension REF: 178 OBJ: 1 (theory) TOP: Concepts of Rehabilitation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. A resident with advanced Parkinson disease stays in his wheelchair all day. He reports that he is too tired to walk and is fearful of falling. Which intervention to increase the patient’s mobility should the nurse add to the patient’s care plan? a. Instruct the resident in crutch walking. b. Assist the resident with ambulating in the hallway with a gait belt. c. Encourage the resident to rock back and forth in his wheelchair to off-load weight. d. Arrange for a walking cane. ANS: B Walking is the best exercise to prevent problems associated with immobility. The gait belt will make the resident more secure. Canes and crutches do not diminish the weakness or the fear of falling. PTS: 1 DIF: Cognitive Level: Application REF: 185, Box 9-5 OBJ: 2 (theory) TOP: Preventing Problems of Immobility KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 3. The nurse is caring for an obese resident with a pressure ulcer on her coccyx. The patient frequently lies on her back because it is difficult to turn due to her weight. Which intervention most effectively encourages independence? a. Instruct the staff turn the resident every 2 hours. b. Turn the patient on her side and use pillows to stabilize her. c. Arrange for short side rails to be used for positioning. d. Arrange for a trapeze so the patient can assist with positioning. ANS: D The trapeze allows for self-positioning and is less confining than are bed rails. Turning the patient on her side or using short rails for positioning do not foster independence. PTS: 1 DIF: Cognitive Level: Application REF: 187 OBJ: 2 (theory) TOP: Preventing Problems of Immobility KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 4. After assessing reddened heels on a bed-bound patient with a history of a stroke, which intervention should the nurse add to the care plan? a. Massage heels briskly. b. Apply socks to feet. c. Swab heels with alcohol. d. Elevate feet on pillows. ANS: D Elevation of the feet gets the weight off the heels and will allow them to heal. All other options are not helpful to damaged skin. Brisk massage may promote damage to the skin. Alcohol can be irritating and may further damage heel skin. PTS: 1 DIF: Cognitive Level: Application REF: 181, Nursing Care Plan 9-1 OBJ: 2 (theory) TOP: Preventing Problems of Immobility KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 5. The nurse is educating a 70-year-old patient who just had a cast removed from a broken arm. The nurse should teach the patient about which potential effect of immobility related to casting? a. Arthritis b. Phlebitis c. Frozen shoulder d. Painful swelling ANS: C Immobility can cause loss of strength and flexibility in the older adult. PTS: 1 DIF: Cognitive Level: Knowledge REF: 180, Table 9-1 OBJ: 3 (theory) TOP: Effects of Immobility: Joint Stiffness KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 6. The nurse is caring for an 85-year-old patient who has been on bed rest for a fractured hip. The nurse finds that the patient is flushed, has a temperature of 100° F, a pulse of 100, and respiratory rate of 24. What assessment should the nurse perform next? a. Obtain blood pressure (BP) b. Auscultate breath sounds c. Assess for abdominal distention d. Measure amount of urinary output in the last hour ANS: B The initial assessments are the cardinal signs of pneumonia. The breath sounds should be assessed next to determine the presence of any adventitious breath sounds. BP will also need to be assessed, but the breath sounds are more important with the signs and symptoms present. Abdominal distention is indicative of a gastrointestinal problem. Amount of urinary output is important to an ongoing assessment but not a priority in the present circumstances. PTS: 1 DIF: Cognitive Level: Analysis REF: 180, Table 9-1 OBJ: 3 (theory) TOP: Effects of Immobility: Hypostatic Pneumonia KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 7. The nurse is caring for a 76-year-old patient in a long-term care facility who sent his food tray back to the kitchen untouched for the second time today. Which intervention is most effective to increase nutrition? a. Offer to feed the patient. b. Ask the dietitian to talk with the patient about food preferences. c. Offer the patient a high-protein drink. d. Sit with the patient during meals. ANS: C Taking the high-energy drink meets the immediate challenge of inadequate nutritional intake. Referral to the dietitian and sitting with the patient may be helpful. Offering to feed from a rejected tray is not supportive. PTS: 1 DIF: Cognitive Level: Analysis REF: 183 OBJ: 4 (theory) TOP: Effects of Immobility: Anorexia KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 8. The nurse assesses a bed-bound resident, a reddened area over the coccyx that does not blanch is discovered. Which is the best intervention to prevent further skin damage? a. Cover the site with a transparent film dressing. b. Apply warm compresses each shift. c. Turn the patient every 2 hours. d. Continue to monitor the area. ANS: A Since this appears to be a stage 1 pressure area, the transparent film ensures the proper amount of moisture is present for healing while allowing monitoring of the area. A warm compress is not warranted. This patient will need to be turned every hour. Monitoring of the area should continue but does not meet the immediate need. PTS: 1 DIF: Cognitive Level: Analysis REF: 181, Nursing Care Plan 9-1 OBJ: 3 (theory) TOP: Effects of Immobility: Impaired Circulation KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 9. The LPN/LVN making care assignments to nursing assistants would not assign a patient who has which problem? a. Manipulative behavior b. An unstable condition c. A draining wound d. A communicable disease ANS: B Nursing assistants are not assigned to patients who have an unstable condition. Care of an unstable patient does not fall into the scope of practice of the unlicensed personnel. PTS: 1 DIF: Cognitive Level: Comprehension REF: 184, Assignment Considerations OBJ: 5 (theory) TOP: Assigning Personnel KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 10. Which statement describes the chief goal of a long-term care facility? a. To offer restorative services b. To promote individual independence c. To facilitate achievement of complete autonomy d. To manage medication protocols ANS: B Promotion of independence is the chief goal, not complete autonomy. Other options are services directed at achieving increased independence. PTS: 1 DIF: Cognitive Level: Comprehension REF: 187 OBJ: 4 (theory) TOP: Goal of Long-Term Care Facilities KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 11. The nurse educates the nursing assistant about the importance of locking the wheels of a wheelchair. Which statement indicates that the nursing assistant understands the nurse’s teaching? a. “The locks supply a stable support for a patient to lift himself.” b. “The locks keep patient in position at a table or bedside.” c. “The locks help to prevent falls.” d. “The locks keep the patient from moving himself. ANS: C Fall prevention is the purpose of locking the wheels of a wheelchair. PTS: 1 DIF: Cognitive Level: Application REF: 185, Box 9-5 OBJ: 7 (theory) TOP: Fall Prevention KEY: Nursing Process Step: Evaluation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 12. The long-term care facility nurse is discussing fall prevention measures with the charge nurse. Which replacement should the nurse suggest? a. Replacing canes with 4 feet with a single-footed cane. b. Replacing hard-soled shoes with soft-soled bedroom slippers. c. Replacing area rugs with a nonslip pad. d. Replacing plain carpet with a highly patterned carpet. ANS: C Loose area rugs should be replaced with nonslip carpets. PTS: 1 DIF: Cognitive Level: Application REF: 185, Box 9-5 OBJ: 11 (clinical) TOP: Fall Prevention KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 13. The nurse is instructing a family about chair selection for an older adult with Parkinson disease. Which information is most important for the nurse to include? a. Choose a chair that is very wide to allow for position changes. b. Choose a chair with sturdy arms to aid in rising. c. Choose a chair that is low to the ground to prevent falls. d. Choose a chair that is soft and deep for added comfort. ANS: B Sturdy arms assist in rising and sitting. Soft, low, and wide chairs cause a person to lean forward to rise and to “fall into” the chair to be seated. PTS: 1 DIF: Cognitive Level: Comprehension REF: 185, Box 9-5 OBJ: 10 (clinical) TOP: Fall Prevention KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 14. The charge nurse instructs the nursing assistants about the policy concerning call lights. The nurse teaches that patients taking which type of medication require especially prompt call light attention? a. Diuretics b. Antibiotics c. Proton pump inhibitors d. Nonsteroidal anti-inflammatory drugs (NSAIDs ) ANS: A People taking diuretics need to go to the bathroom frequently, and often urgently. Prompt attention to call lights will reduce the probability of the patient getting up unassisted. Diuretics may also cause orthostatic hypotension, which increases the risk for falling. PTS: 1 DIF: Cognitive Level: Application REF: 185, Box 9-5 OBJ: 11 (clinical) TOP: Fall Prevention KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 15. The nurse is caring for a resident who has a security device for safety purposes. What intervention should the nurse include in the plan of care? a. Visually check the resident every hour. b. Turn and reposition the resident every hour. c. Assess condition of the skin every 4 hours. d. Reassess the need for the security device every 4 to 8 hours. ANS: D The need for continuing the use of the security device must be assessed every 4 to 8 hours. The patient should be visually checked every 30 minutes, and turned and skin assessed every 2 hours. PTS: 1 DIF: Cognitive Level: Application REF: 185, Box 9-5 OBJ: 11 (clinical) TOP: Use of Security Devices KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 16. When the confused resident pours his cereal in a cup and “drinks” it, how should the nurse best respond? a. Put his cereal back in the bowl and hand the resident a spoon. b. Discard the cup with his cereal and bring fresh cereal in a bowl. c. Calmly instruct the resident that cereal is to be eaten from a bowl. d. Do nothing to interrupt the behavior. ANS: D While this method of eating cereal is not typical, it is not harmful and allows the patient to be independent. The nurse should leave the resident alone to feed himself independently. Staff should refrain from doing what the resident can do for himself, so transferring his cereal to another container, discarding the cereal, or telling the patient that he cannot eat the cereal in a certain way is not appropriate. PTS: 1 DIF: Cognitive Level: Application REF: 187 OBJ: 4 (theory) TOP: Long-Term Care Facility Goals: Autonomy KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 17. The nurse is planning a group TV activity in a long-term care facility. The nurse should select a channel that offers which type of program? a. Cartoons b. Travel documentaries c. Dramatic two-part mini-series d. Opera performances ANS: B Travel documentaries are colorful and do not have a plot to follow. Cartoons are juvenile, opera does not have universal appeal, and the two-part drama would require long attention spans and good short-term memory. PTS: 1 DIF: Cognitive Level: Application REF: 188 OBJ: 4 (theory) TOP: Long-Term Care Facility Goals: Autonomy KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 18. The nurse is seeking to motivate a frustrated patient who is learning to walk again after a stroke. Which intervention would be most effective? a. Show short movies on ambulation techniques. b. Observe the patient while in physical therapy. c. Arrange a visit with another stroke victim who has learned to ambulate. d. Encourage a 1-week break from therapy, which will help the resident come back refreshed. ANS: C Talking with someone who can truly understand the frustration is helpful. Showing a short movie on ambulation techniques may be an effective teaching tool, but it is not a motivational tool. Observing the resident is necessary but does not provide motivation. A 1-week break will interrupt progress that has been made, thus decreasing motivation. PTS: 1 DIF: Cognitive Level: Application REF: 189, Older Adult Care Points OBJ: 7 (theory) TOP: Goals for Rehabilitation: Motivation KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 19. The nurse is caring for a disoriented resident. Which intervention is most appropriate for the nurse to include when planning care for this patient? a. Ensure that activities are scheduled for the same time each day. b. Change care assignments for assistive personnel frequently to prevent burnout. c. Encourage autonomy by allowing the resident to choose clothes from the closet. d. Administer sedatives to calm the patient. ANS: A Keeping a routine leads to less confusion. Changing assistive personnel care assignments frequently is confusing for the resident. Choosing clothing from an entire closet is overwhelming for the confused resident; rather, giving the resident a few items to choose from encourages autonomy without increasing confusion. Sedatives should not be given to treat confusion. PTS: 1 DIF: Cognitive Level: Application REF: 186 OBJ: 4 (theory) TOP: Managing Confusion and Disorientation KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity MULTIPLE RESPONSE 20. Which treatment resource focuses on restorative care for people with chronic illness and disabilities? (Select all that apply.) a. Outpatient clinics b. Long-term health care facilities c. Home care d. Rehabilitation agencies e. Hospice agencies ANS: A, B, C, D Outpatient clinics, long-term care facilities, home care, and rehabilitation agencies are sources of rehabilitation for people with chronic illness or disability. Hospice agencies focus on care of the dying patient. PTS: 1 DIF: Cognitive Level: Knowledge REF: 189 OBJ: 1 (theory) TOP: Locus of Treatment for Chronic Illness KEY: Nursing Process Step: N/A MSC: NCLEX: Health Promotion and Maintenance 21. Which statement expresses a multi-focused goal of rehabilitation? (Select all that apply.) a. To promote new coping skills. b. To teach adaptive living skills. c. To focus on self-care for increased independence. d. To improve quality of life. e. To restore former level of function. ANS: A, B, C, D Restoring former level of function is not a goal of rehabilitation because this may be an impossible goal. New coping and adaptive skills, and self-care skills that improve the quality of life are all goals of rehabilitation. PTS: 1 DIF: Cognitive Level: Comprehension REF: 189 OBJ: 7 (theory) TOP: Goals of Rehabilitation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 22. The patient who has been in traction for bilateral femur fractures complains of constipation. Which action(s) should the nurse take? (Select all that apply.) a. Provide prune juice from the snack cart. b. Encourage increased fluid intake. c. Arrange for high-fiber foods such as cauliflower and broccoli. d. Administer prescribed stool softeners. e. Encourage intake of milk products. ANS: A, B, C, D Milk products are constipating. Prune juice, extra fluid, high-fiber foods, and stool softeners will combat constipation. PTS: 1 DIF: Cognitive Level: Application REF: 180, Table 9-1 OBJ: 3 (theory) TOP: Preventing Problems of Immobility KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 23. Which statement describes an impact of disability? (Select all that apply.) a. Unchanged family roles b. Life patterns centered around treatment or rehabilitation c. Grief over what has been lost d. Spiritual distress e. Sense of powerlessness ANS: B, C, D, E Family roles often change as a result of a disability. Life patterns will center around treatment and rehabilitation for at least the initial phase of incurring the disability, as well as grief, spiritual distress, and powerlessness. PTS: 1 DIF: Cognitive Level: Application REF: 194 OBJ: 4 (theory) TOP: Impact of Disability KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 24. Long-term health care facilities are the center of treatment for which type of patients? (Select all that apply.) a. Patients who are recovering after the most acute phase of their illness is over. b. Patients who are receiving rehabilitation after a joint replacement. c. Patients who are too weak from primary illness to care for themselves presently. d. Patients who are in need of a permanent home because of effects of a chronic condition. e. Patients who are under treatment for substance abuse. ANS: A, B, C, D Long-term health care facilities do not offer active treatment to substance abusers. Recovery from an acute illness, joint replacement rehabilitation, weakness from illness, and a permanent home for a chronic illness are common reasons individuals seek care from long-term care facilities. PTS: 1 DIF: Cognitive Level: Comprehension REF: 183 OBJ: 4 (theory) TOP: Purpose of Long-Term Health Care Facilities KEY: Nursing Process Step: N/A MSC: NCLEX: Health Promotion and Maintenance 25. Which role may the LPN/LVN perform in a long-term health care facility? (Select all that apply.) a. Charge nurse b. Designer of nursing care plans c. Administrator of medications d. Administrator of wound care e. Assignment delegator ANS: A, C, D, E The LPN/LVN does not design the nursing care plan but may contribute to the care plan. This is the responsibility of the RN. The LPN/LVN may act in the role of charge nurse while under the supervision of an RN. Administration of medications and wound care and delegation of care are commonly the LPN/LVN’s responsibility. PTS: 1 DIF: Cognitive Level: Comprehension REF: 183 OBJ: 5 (theory) TOP: LPN/LVN Role in Long-Term Health Care Facility KEY: Nursing Process Step: N/A MSC: NCLEX: Health Promotion and Maintenance 26. What action should the LPN/LVN take when delegating care to a nursing assistant? (Select all that apply.) a. Give specific instruction as to what is to be done. b. Instruct how the task is to be done. c. List information that needs to be reported. d. Be aware that the nurse is responsible for outcome of delegated care. e. Insist that the nursing assistant accept the responsibility. ANS: A, B, C, D In delegating to unlicensed assistive personnel, the LPN/LVN should first inquire if the nursing assistant is willing to take responsibility for the care assigned. PTS: 1 DIF: Cognitive Level: Comprehension REF: 184, Assignment Considerations OBJ: 5 (theory) TOP: Delegation KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 27. When can the LPN/LVN apply a physical restraint to a resident in a long-term care facility? (Select all that apply.) a. If an order for the restraint is obtained within 12 hours of application. b. If all other measures have been attempted and failed. c. If documentation is made on all failed attempts. d. If the family is unable to stay with the resident. e. If the least restrictive device is chosen. ANS: B, C, D, E The order for the restraint must be obtained within 24 to 48 hours after application of the device. The LPN/LVN who applies a physical restraint must have satisfied all of the other options. PTS: 1 DIF: Cognitive Level: Application REF: 186 OBJ: 2 (clinical) TOP: Use of Restraints KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 28. The student nurse is becoming familiar with Healthy People 2020 goals related to rehabilitation. The student nurse demonstrates understanding when identifying which goals? (Select all that apply.) a. Increase the proportion of adults with disabilities who participate in social activities. b. Increase the proportion of adults with disabilities who report satisfaction with life. c. Increase the proportion of people with disabilities who report not having the assistive devices and technology needed. d. Reduce the proportion of adults with disabilities who report feelings such as sadness, unhappiness, or depression that prevent them from being active. e. Reduce the proportion of people with disabilities who report environmental barriers to participation in home, school, work, or community activities. ANS: A, B, D, E One of the goals of Healthy People 2020 is to reduce, rather than to increase, the proportion of people with disabilities who report not having the assistive devices and technology needed. All other options are included as goals. PTS: 1 DIF: Cognitive Level: Comprehension REF: 191 OBJ: 7 (theory) TOP: Healthy People 2020 Goals KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance COMPLETION 29. The rehabilitation nurse makes the point that a dysfunction of a specific body part is termed __________. ANS: impairment Impairment is a dysfunction of an organ or a body part. PTS: 1 DIF: Cognitive Level: Comprehension REF: 178 OBJ: 1 (theory) TOP: Concepts of Rehabilitation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 30. The nurse working in a long-term care facility is aware that in order to comply with Medicare guidelines, documentation of assessment findings that measure physical, psychological, and psychosocial functioning are necessary using the _____________________. ANS: Minimum Data Set minimum data set MDS The Minimum Data Set (MDS) is a primary screening and assessment tool that is standard for all Medicare and Medicaid residents in a long-term care facility. PTS: 1 DIF: Cognitive Level: Application REF: 188 OBJ: 12 (clinical) TOP: Documentation KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Management of Care Chapter 10: The Immune and Lymphatic System deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is teaching about changes in the immune system that result from the aging process. Which change should the nurse include? a. Thickened skin b. Reduced ciliary action c. Thinned periosteum d. Reduced saliva ANS: B Reduced ciliary action in the respiratory and gastrointestinal tracts results in a decrease in the removal of harmful organisms. PTS: 1 DIF: Cognitive Level: Knowledge REF: 200 OBJ: 5 (theory) TOP: Aging Immune System KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. The nurse differentiates the humoral response from the cell-mediated response. Which statement about cell-mediated response is true? a. The sensitized lymphocytes attack the cell for which they were sensitized. b. Cells produce new antibodies. c. The response does not occur until the white blood cell (WBC) count rises. d. There is a systemic response of fever and malaise. ANS: A Cell-mediated response occurs when the specifically antigen-sensitized T lymphocytes attack whole cells, infectious organisms, and nonliving matter such as pollen and dust. PTS: 1 DIF: Cognitive Level: Comprehension REF: 201 OBJ: 1 (theory) TOP: Cell-Mediated Response KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 3. Which type of lymphocytes actually produces either sensitized lymphocytes or antibodies? a. B lymphocytes b. T cells c. Suppressor T cells d. Stem cells ANS: A The B-cells secrete immunoglobulins that are called antibodies. PTS: 1 DIF: Cognitive Level: Comprehension REF: 201 OBJ: 1 (theory) TOP: Production of Antibodies KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 4. The nurse explains to a patient with a painful toe that the pain is related to the inflammatory response. What process causes this discomfort? a. Swelling, which compresses nerves. b. Enzyme release, which irritates the area. c. Acidic waste from the destroyed cells. d. Heat of lysis, which affects the nerves. ANS: A The swelling brought on by the fluid that collects at the site compresses nerves, causing pain. PTS: 1 DIF: Cognitive Level: Application REF: 200 OBJ: 1 (theory) TOP: Inflammatory Process KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 5. The nurse is reviewing laboratory results of a patient who had surgery 2 days ago. The nurse notes that the C-reactive protein is elevated. What potential problem does this finding indicate? a. Impending infection b. Possible hemorrhage c. A drug allergic reaction d. Fluid deficit ANS: A Since inflammation is an early response to infection, an elevation of the C-reactive protein (which elevates with inflammation) is an indicator of possible impending infection. C-reactive protein is not directly related to hemorrhage, drug reaction, or fluid deficit. PTS: 1 DIF: Cognitive Level: Application REF: 210, Table 10-3 OBJ: 1 (clinical) TOP: C-Reactive Protein KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 6. The nurse is preparing a presentation on the inflammatory response. While preparing a cartoon picture of lysis, the nurse correctly draws which scenario? a. An antibody acting through the process of neutralization b. An individual’s arm that is red and swollen c. A phagocyte eating an antigen d. A cell that is originating in the bone marrow ANS: C Lysis is the result of phagocytosis. Phagocytes “gobble up” antigens. An antibody acting through the process of neutralization depicts production of an antitoxin. Redness and swelling of the skin surface are general characteristics of inflammation. The picture of the cell originating in the bone marrow is depicting lymphocytic cells, which are a specialized type of WBC that originates in the bone marrow. PTS: 1 DIF: Cognitive Level: Analysis REF: 202 OBJ: 3 (theory) TOP: Lysis KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 7. Which analogy best describes the action of killer T cells? a. A tiger slowly stalking an antigen to devour it. b. A mad hornet flying through circulating fluids seeking and killing antigens. c. A spider waiting in a web for an antigen to get caught in it. d. A bird dog pointing to an antigen so it can be attacked by phagocytes. ANS: B Killer T cells move around in body fluids and react wherever they encounter the antigen. PTS: 1 DIF: Cognitive Level: Analysis REF: 201, Figure 10-3 OBJ: 1 (theory) TOP: Lysis KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 8. The nurse is aware that unlike dogs, humans do not contract such diseases as distemper. Which type of immunity explains this protection? a. Passive immunity b. Acquired immunity c. Innate immunity d. Passive natural immunity ANS: C Innate immunity is based on the genetic makeup of a particular species that allows that species to be immune to specific diseases without having had the infection themselves. An example is humans don’t get distemper, but dogs do. Humans do not get hoofand-mouth disease, but cows do. PTS: 1 DIF: Cognitive Level: Comprehension REF: 204 OBJ: 4 (theory) TOP: Innate Immunity KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 9. The young father tells the industrial nurse at work that he is afraid he will give his 2-week-old baby his cold. The nurse can assure him that the baby is protected by which type of immunity? a. Acquired immunity b. Passive immunity c. Active immunity d. Passive natural immunity ANS: D Passive natural immunity is the immunity a baby gets from the mother, in utero or from breast milk, that lasts for the first several months of the baby’s life. PTS: 1 DIF: Cognitive Level: Comprehension REF: 204 OBJ: 4 (theory) TOP: Immunity KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 10. Which scenario explains how a patient can be protected by passive artificial immunity? a. Receiving an injection with immune globulin b. Receiving immunizations c. Contracting the disease d. Consuming sufficient antioxidants ANS: A Immunoglobulin contains antibodies against not just one but many infectious diseases. This type of immune globulin is used when a susceptible person is exposed to or contracts a communicable disease since it enhances the immune system. Immunizations are a form of active artificially acquired immunity. Contracting the disease initiates naturally acquired immunity. Antioxidants are thought to simply boost the immune system. PTS: 1 DIF: Cognitive Level: Application REF: 204 OBJ: 4 (theory) TOP: Passive Immunity KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 11. A vaccination or immunization gives a patient which type of immunity? a. Active acquired immunity b. Passive acquired immunity c. Passive immunity d. Natural immunity ANS: A An immunization gives the recipient a “tiny dose” of a disease, enough to stimulate the production of antibodies and is considered active artificially acquired immunity. PTS: 1 DIF: Cognitive Level: Comprehension REF: 204 OBJ: 4 (theory) TOP: Immunity KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 12. How does long-term alcohol abuse lead to alteration in the immune system? a. It alters the effectiveness of antibodies. b. It stimulates autoimmune activity. c. It impairs the ability of B lymphocytes to produce antibodies. d. It shortens the life of circulating antibodies. ANS: C Alcohol impairs the ability of B lymphocytes to produce antibodies. PTS: 1 DIF: Cognitive Level: Comprehension REF: 205 OBJ: 5 (theory) TOP: Impact of Alcoholism on Immune System KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 13. The industrial nurse should teach all middle-aged employees to receive a tetanus booster how often? a. Every 2 years b. Every 4 years c. Every 7 years d. Every 10 years ANS: D The Centers for Disease Control and Prevention (CDC) recommends that adults get a tetanus booster every 10 years. PTS: 1 DIF: Cognitive Level: Comprehension REF: 205 OBJ: 6 (theory) TOP: Tetanus Booster KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 14. The outpatient clinic nurse is collecting a health history on a 78-year-old patient who has a history of emphysema. Which annual immunization is most important for the patient to receive? a. Tetanus b. Influenza c. Pneumonia d. Hepatitis B ANS: B The CDC recommends that older adults, people with respiratory impairment, and health care workers acquire an annual influenza immunization. A pneumonia vaccination is important for this patient, but it is not given on a yearly basis. Tetanus and hepatitis B are recommended for most individuals but are not given annually. PTS: 1 DIF: Cognitive Level: Comprehension REF: 205-206 OBJ: 6 (theory) TOP: Influenza Immunization KEY: Nursing Process Step: N/A MSC: NCLEX: Health Promotion and Maintenance 15. The nurse is working in a flu immunization clinic. Which situation would require a postponement of immunization? a. A patient has a history of asthma. b. A patient takes herbal remedies such as valerian and Ginkgo biloba daily. c. A patient has a history of poorly controlled diabetes. d. A patient received immune globulin 2 weeks ago. ANS: D Immune globulin will decrease the immune response to the vaccine, rendering it useless. Asthma, Ginkgo biloba, and uncontrolled diabetes do not prevent an individual from receiving a flu immunization. PTS: 1 DIF: Cognitive Level: Application REF: 206 OBJ: 6 (theory) TOP: Postponement of Immunizations KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 16. After assessing a patient, the nurse suspects that the patient has an abscessed tooth. Which assessment finding confirms that the immune system is fighting the abscess? a. Anorexia b. Purulent expectorate c. Foul breath d. Enlarged cervical lymph node ANS: D The enlarged lymph node near to the actual infection is evidence that the B- and T-lymphocytes are making antibodies and the activity in the lymph node has caused it to enlarge. Anorexia, purulent expectorate, and foul breath are manifestations consistent with the presence of an abscess. PTS: 1 DIF: Cognitive Level: Analysis REF: 208 OBJ: 1 (clinical) TOP: Indicators of Immune System Function KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 17. The nurse is evaluating the patient’s understanding of his new diagnosis of rheumatoid arthritis. Which statement reflects an understanding of the disease process? a. “My body lacks an appropriate response to invading bacteria.” b. “My body produces an immune response to my own cells and tissues.” c. “My body immediately produces a protein that is specifically designed to fight off an antigen.” d. My body has a delayed response in which lymphocytes attack whole cells like bacteria.” ANS: B When a patient has an autoimmune disease such as rheumatoid arthritis, the body produces an immune response to a “self” cell or tissue. Lacking an appropriate response is characteristic of an immune deficiency. Immediate production of a protein (an antibody) to an antigen is a normal humoral immune response. The statement involving the delayed response of lymphocytes is referred to a cell-mediated response. PTS: 1 DIF: Cognitive Level: Application REF: 200-201, 205 OBJ: 5 (theory) TOP: Types of Immune Responses KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 18. The mother of a young child voices concern about immunizations for her child. Which response is best? a. “Immunization is generally a safe method of avoiding certain diseases and the complications that go along with these diseases.” b. “There are no risk factors associated with immunizations, so there is no reason to worry.” c. “I really don’t understand the thinking behind people not immunizing their children if it can prevent disease.” d. “Recommendations of Healthy People 2020 Goal 14 is to reduce or eliminate cases of vaccine-preventable diseases, so I strongly urge you to immunize your child.” ANS: A This is the best response since immunizations are generally safe and do help prevent certain diseases and complications of diseases. There are risk factors, such as allergic reaction to vaccinations, so this should be discussed with the mother. The nurse should not voice personal feelings about immunization. Although increasing immunizations is a goal of Healthy People 2020, this is not a helpful response to a parent. PTS: 1 DIF: Cognitive Level: Analysis REF: 205 OBJ: 6 (theory) TOP: Complement System of Proteins KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation MULTIPLE RESPONSE 19. Which mechanisms are ways in which antibodies can protect the body by either destroying or inactivating a particular antigen? (Select all that apply.) a. Mechanically harming the antigen b. Activating the complement system c. Releasing chemicals that alter the environment of the antigen d. Directly attacking the nucleus of the antigen e. Forming organic “chains” that sweep out the antigen ANS: A, B, C Antibodies destroy an antigen by mechanically harming it, activating the complement system, and releasing chemicals that alter the environment of the antigen. PTS: 1 DIF: Cognitive Level: Application REF: 202 OBJ: 3 (theory) TOP: Antibody Action KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 20. Which statements about passive immunity are true? (Select all that apply.) a. Passive immunity lasts for several years. b. Passive immunity stimulates the production of antibodies. c. Passive immunity prevents further tissue damage. d. Passive immunity provides temporary immunity from the disease. e. Passive immunity is given by vaccination. ANS: C, D Passive immunity prevents further damage when a disease is already present. Passive immunity provides the protection of antibodies made by someone else. Benefits of passive immunity are usually time limited as the antibodies provided only last for a specific period. Active artificial acquired immunity is achieved through immunizations. PTS: 1 DIF: Cognitive Level: Comprehension REF: 204 OBJ: 4 (theory) TOP: Passive Immunity KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 21. Techniques of testing for possible allergy include which of the following? (Select all that apply.) a. The scratch test b. Drinking diluted solution of antigen c. Intradermal injection d. Dropping solution in the eye e. Adhesive patches ANS: A, B, C, E Testing for allergy in the eye is no longer done. All other options will produce an inflammatory response from the application of the antigen. PTS: 1 DIF: Cognitive Level: Application REF: 207 OBJ: 1 (clinical) TOP: Allergy Testing KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 22. Which patient would the nurse consider to be immunosuppressed? (Select all that apply.) a. A patient on chemotherapy for cancer b. A patient using corticosteroids c. A patient pregnant at 28 weeks gestation d. A patient recovering from joint replacement e. A patient diagnosed with human immunodeficiency virus (HIV) ANS: A, B, D, E A woman at 28 weeks gestation is not considered immunocompromised. All of the other options represent people who are immunosuppressed. PTS: 1 DIF: Cognitive Level: Comprehension REF: 213 OBJ: 9 (clinical) TOP: Immunosuppressed People KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 23. The nurse is caring for an immunosuppressed patient. Which care considerations should the nurse include? (Select all that apply.) a. Increase fresh fruit intake. b. Adhere to Standard Precautions. c. Avoid bringing potted plants into the patient’s room. d. Employ reverse isolation. e. Use filters on air conditioner vents. ANS: B, C, D, E Patients who are immunosuppressed require extended precautions, which are included in the neutropenic precautions, reverse isolation, or protective isolation. Fresh fruit and potted plants should be avoided because bacteria and other substances that have the potential to cause harm may be present. PTS: 1 DIF: Cognitive Level: Application REF: 214 OBJ: 9 (clinical) TOP: Neutropenic Precautions KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control COMPLETION 24. The bone marrow produces a(n) _______ cell that can differentiate itself to acquire individual characteristics. ANS: stem Stem cells, which are produced by the bone marrow, are capable of differentiating themselves as they mature into different cells, such as liver cells and brain cells. PTS: 1 DIF: Cognitive Level: Knowledge REF: 197, 199, Table 10-1 OBJ: 1 (theory) TOP: Stem Cells KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 25. The nurse explains that the immediate response of a person’s body that produces an antibody is called the _____________. ANS: humoral response The humoral response is the immediate response of the immune system when it recognizes an antigen and then makes antibody. PTS: 1 DIF: Cognitive Level: Knowledge REF: 201 OBJ: 1 (theory) TOP: Humoral Response KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 26. Plasma cells are stimulated to produce large quantities of specific antibodies by ____________. ANS: memory cells Memory cells reactivate the plasma cells to make specialized antibodies for the antigen that the memory cells have detected. PTS: 1 DIF: Cognitive Level: Comprehension REF: 201 OBJ: 1 (theory) TOP: Memory Cells KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 27. Lymphoid tissue that is typically found in the ileum portion of the small bowel is called ____________. ANS: Peyer patches Peyer patches help defend against ingested pathogens. PTS: 1 DIF: Cognitive Level: Knowledge REF: 198 OBJ: 3 (theory) TOP: Organs and Structures KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation MATCHING Place the events of the complement system of proteins in the correct sequence. a. Antibodies attack the antigen. b. Break in cell wall allows salt to enter antigen cell. c. Antigen swells and bursts. d. Water enters the antigen cell. e. Proteins embed in cell wall of antigen. 28. Step 1 29. Step 2 30. Step 3 31. Step 4 32. Step 5 28. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 200 OBJ: 1 (theory) TOP: Complement System of Proteins KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 29. ANS: E PTS: 1 DIF: Cognitive Level: Analysis REF: 200 OBJ: 1 (theory) TOP: Complement System of Proteins KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 30. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 200 OBJ: 1 (theory) TOP: Complement System of Proteins KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 31. ANS: D PTS: 1 DIF: Cognitive Level: Analysis REF: 200 OBJ: 1 (theory) TOP: Complement System of Proteins KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 32. ANS: C PTS: 1 DIF: Cognitive Level: Analysis REF: 200 OBJ: 1 (theory) TOP: Complement System of Proteins KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation Chapter 11: Care of Patients with Immune and Lymphatic Disorders (with HIV and AIDS) deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is caring for a pediatric patient recently diagnosed with severe combined immunodeficiency (SCID) disease. The nurse determines that teaching has been effective after the parent makes which statement? a. “This disease is like a pediatric version of AIDS.” b. “My child must be careful not to fall to avoid bleeding.” c. “My child should not attend day care.” d. “This problem happened because of chemotherapy treatments.” ANS: C There are two forms of immune deficiency: primary and acquired. In primary immune deficiency disorders (PIDD), the cause is an inherited genetic mutation and some of PIDD are detected during infancy or early childhood. Patients with this type of disorder experience repeated infections that clearly increase their risk of morbidity and mortality as well as the cost of health care. AIDS is an example of acquired immune deficiency and affects pediatric patients as well as adults. Hemophilia is a disorder in which patients can suffer life-threatening bleeds from a fall. Chemotherapy recipients may develop an acquired immune disorder, but chemotherapy would not cause any type of immune disorder in the child. PTS: 1 DIF: Cognitive Level: Application REF: 217, Box 11-1 OBJ: 1 TOP: Primary Immune Deficiency KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 2. After an influenza immunization, the patient complains of shortness of breath, breaks out in hives, and begins to twitch. Which ordered medication should the nurse give first? a. Epinephrine injection b. Oxygen via mask at 5 L/min c. Corticosteroid injection d. Bronchodilators per nebulization ANS: A Epinephrine is the initial line of defense to reverse anaphylaxis, followed by high-flow oxygen, bronchodilators, and corticosteroid injection as necessary. PTS: 1 DIF: Cognitive Level: Application REF: 249 OBJ: 6 (clinical) TOP: Anaphylaxis KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 3. The nurse is educating a patient with systemic lupus erythematosus (SLE). Which information is most important for the nurse to include in the teaching plan? a. Train with weights to increase strength. b. Avoid glycerin-based soaps. c. Use an SPF 15 sunblock when outdoors. d. Apply fragrance-free lotions to dry areas twice daily. ANS: D Skin protection for patients with SLE is a top priority. The patient should be advised to liberally apply fragrance-free lotions to dry areas at least twice daily. Weight training could cause joint strain. SLE patients should choose a mild soap with a glycerin base and select sunscreen that features SPF of 30 or higher. PTS: 1 DIF: Cognitive Level: Application REF: 233, 237, Patient Teaching OBJ: 7 TOP: SLE Teaching KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 4. The nurse is educating a patient about his diagnosis of stage II Hodgkin disease. Which statement indicates that the nurse’s teaching has been successful? a. “The cancer has spread throughout my entire body.” b. “There is only one lymph node involved.” c. “The lymph nodes in both of my arms are affected.” d. “Two nodes in my left arm area are affected.” ANS: D Stage II indicates that there are two or more involved lymph nodes on the same side of the diaphragm (or body). The lymph nodes affected could be in any part of the lymphatic system. The disease spreading outside of the lymph system indicates stage IV. Single node involvement is stage I, and lymph involvement on both sides of the diaphragm or body is considered stage III. PTS: 1 DIF: Cognitive Level: Application REF: 238, Figure 11-5 OBJ: 8 TOP: Hodgkin Disease Node Staging KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 5. MOPP and ABVD therapy for the treatment of Hodgkin disease are treatment protocols that use which combination of factors? a. Multiple medications given concurrently b. Heat, exercise, and chemotherapy c. Alternating radiation and chemotherapy d. Chemotherapy and alternative herbal remedies ANS: A MOPP and ABVD are chemotherapy treatment protocols using a combination of four drugs given concurrently. MOPP is the acronym for the drugs mechlorethamine, vincristine (Oncovin), procarbazine, and prednisone. ABVD is the acronym for the drugs doxorubicin (Adriamycin), bleomycin, vinblastine, and dacarbazine. This treatment protocol is usually used for stages III and IV of the disease. PTS: 1 DIF: Cognitive Level: Application REF: 238 OBJ: 8 TOP: Treatment: Hodgkin Disease KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 6. The nurse caring for a patient with advanced AIDS. While collecting data, the nurse notes a weight loss of several pounds, poor food consumption, and complaint of no appetite. Based on these findings, the nurse should carefully monitor the patient for development of which problem? a. Lymphedema b. Hyperglycemia c. Hypertension d. Anasarca ANS: D Anasarca is generalized edema in the trunk, extremities, and around the eyes. It results in patients with advanced AIDS from a severe depletion of albumin when the patient has an insufficient nutritional intake, as is evident with this patient. Lymphedema is an abnormal collection of lymph fluid accumulated in the peripheral and periorbital areas, sometimes seen in AIDS patients. Hypoglycemia and hypotension are typically seen in patients with advanced AIDS who have poor nutritional and fluid intake. PTS: 1 DIF: Cognitive Level: Analysis REF: 226 OBJ: 3 (clinical) TOP: Advanced AIDS: Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 7. The nurse is caring for an immune compromised patient. The patient displays a low-grade fever and complains of a burning and shooting pain, along with itching and tingling, that progresses from the clavicle to the scapula. The nurse suspects that the patient will undergo evaluation for which infection? a. Hepatitis C b. Shingles c. Candidiasis d. Cryptococcosis ANS: B The immune compromised patient may experience opportunistic infections. Hepatitis C, bacterial infections, and cryptococcosis are all opportunistic infections, but the symptoms this patient is experiencing are consistent with shingles. PTS: 1 DIF: Cognitive Level: Application REF: 226, Table 11-5 OBJ: 6 (theory) TOP: Opportunistic Infection KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 8. The patient scheduled for a computed tomography (CT) scan with contrast medium questions the nurse why the technologist asked her if she had any food allergies. Which response by the nurse is correct? a. “The dye used for a CT scan is egg based, so egg allergies would prevent you from having the test.” b. “People who are allergic to dairy products are likely to be allergic to CT scan dye.” c. “Allergies to shellfish can be a problem because shellfish and CT scan dye are iodine based.” d. “Wheat is the preservative used in CT scan dye, so allergies to wheat may cause allergies to the dye.” ANS: C Allergies to seafood indicate intolerance to iodine. This means there is potential for an allergic reaction to iodine-based contrast agents used in radiologic imaging studies such as CT scans with contrast medium. PTS: 1 DIF: Cognitive Level: Application REF: 247, Clinical Cues OBJ: 10 (theory) TOP: Allergies KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 9. The nurse is performing an assessment on a patient admitted for diagnostic testing to rule out fibromyalgia. Which assessment finding indicates that the patient actually may have the disorder? a. A decreased response to painful stimuli b. A pain response to nonpainful stimuli c. Absent response to painful stimuli d. Numbness and tingling in response to painful stimuli ANS: B Allodynia, pain response to nonpainful stimuli, is one of the signs typically seen in the patient with fibromyalgia. Patients with fibromyalgia often experience hyperalgesia, which is a heightened response to painful stimuli. PTS: 1 DIF: Cognitive Level: Knowledge REF: 240 OBJ: 9 (theory) TOP: Fibromyalgia KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Management of Care 10. The nurse is working in a trauma unit and is accidentally stuck with an IV needle following venipuncture of the patient. What is the nurse’s first action? a. Immediately begin taking the two- or three-drug regimen. b. Report the stick to the charge nurse immediately so follow-up can be initiated. c. Wash the punctured area with soap and water. d. Complete an incident report so immediate testing of the patient and nurse can begin. ANS: C The area should first be cleansed in an attempt to flush any pathogenic organisms from the site, followed by reporting the incident to the charge nurse and completing an incident report. Appropriate treatment regimen will then be started. PTS: 1 DIF: Cognitive Level: Application REF: 231, Safety Alert OBJ: 9 (theory) TOP: HIV Exposure KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 11. The nurse has just administered a new antibiotic to a patient. Which manifestation is the best early indicator that the patient may be experiencing an anaphylactic reaction? a. Wheezing b. Shortness of breath c. Difficulty swallowing d. Angioedema ANS: D The appearance of hives (urticaria) or swelling beneath the skin (angioedema) may signal the onset of an anaphylactic episode. Wheezing, shortness of breath, and difficulty swallowing are later signs of anaphylaxis. PTS: 1 DIF: Cognitive Level: Application REF: 247 OBJ: 10 (theory) TOP: Anaphylaxis KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Management of Care 12. A patient with an immune deficiency disorder has been admitted to the medical unit due to a current infection and weight loss of 12% of his body weight. Which nutritional intervention is most appropriate for this patient? a. Fat b. Vitamin C c. Vitamin B12 d. Protein ANS: D Foods high in protein will not only help with increasing weight but will aid in synthesizing needed antibodies for this condition. Fats, vitamin C, and vitamin B12 will not address either the need for weight gain or antibody synthesis. PTS: 1 DIF: Cognitive Level: Application REF: 219 OBJ: 4 (theory) TOP: Immune Deficiency KEY: Nursing Process Step: Intervention MSC: NCLEX: Safe, Effective Care Environment: Management of Care 13. The nurse is caring for a patient who reports feeling very stressed about her new diagnosis of fibromyalgia. Which response is most beneficial in addressing the patient’s stress? a. “I can’t imagine how it must feel to have this disorder.” b. “What worries you the most about your fibromyalgia?” c. “Light exercise and relaxation techniques may really help alleviate your stress.” d. “You can talk to your doctor about your stress and ask him to prescribe some antianxiety medication.” ANS: B Although light exercise and relaxation techniques may be helpful in reducing stress, the nurse should first address concerns and provide information about the disorder. Providing necessary information is a major stress reducer. Stating only that the nurse “can’t imagine how you feel” provides no therapeutic value, and medications are not a first-line treatment for stress. PTS: 1 DIF: Cognitive Level: Analysis REF: 240 OBJ: 9 | 5 (clinical) TOP: Fibromyalgia KEY: Nursing Process Step: Intervention MSC: NCLEX: Psychosocial Integrity 14. The home care nurse is caring for a patient with a severe immune deficiency disorder. What information about infection prevention is most important for the nurse to include in the teaching plan? a. Check your temperature daily. b. Wash your hands frequently. c. Check daily for signs of infection. d. Seek medical advice at the first sign of infection. ANS: B In order to prevent infection, meticulous hand hygiene must be practiced. Monitoring the temperature, monitoring for signs of infection, and reporting signs of infection to the physician are not preventative measures but early intervention if infection occurs. PTS: 1 DIF: Cognitive Level: Analysis REF: 219, Patient Teaching OBJ: 2 (clinical) TOP: Immune Deficiency KEY: Nursing Process Step: Intervention MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 15. The nurse is educating a patient with lymphoma. Which statement indicates that the patient correctly differentiates Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL)? a. “Non-Hodgkin lymphoma is less predictable and can spread faster.” b. “The first sign of Hodgkin lymphoma is that a single lymph node on one side of the body gets bigger.” c. “People who are older than 60 years are at a bigger risk than younger people.” d. “I will have to have a lot of blood work drawn.” ANS: A NHL is less predictable and can spread faster than HL. Additionally, this statement features a comparison. NHL usually begins with unilateral, painless enlargement of a single lymph node. Expressing an understanding about implication of age as a risk factor or need for blood work does not differentiate specific details about either type of lymphoma. PTS: 1 DIF: Cognitive Level: Application REF: 239 OBJ: 8 (theory) TOP: Lymphoma: Diagnosis KEY: Nursing Process Step: Intervention MSC: NCLEX: Physiological Integrity 16. The nurse is caring for a patient with suspected Hodgkin’s lymphoma (HL). For confirmation of this diagnosis, the nurse understands that the patient’s blood work would reveal which type of abnormal cell? a. Abnormal B cells b. Abnormal T cells c. Cytotoxic T cells d. Reed-Sternberg (R-S) cells ANS: D If Reed-Sternberg (R-S) cells are present, the patient has Hodgkin’s lymphoma (HL). If the R-S cells are not present, the patient is diagnosed as having non-Hodgkin’s lymphoma (NHL). NHL is then identified as either B-cell or T-cell lymphoma. PTS: 1 DIF: Cognitive Level: Comprehension REF: 237 OBJ: 8 (theory) TOP: Lymphoma: Diagnosis KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 17. The nurse is assessing a patient’s lymph nodes. Which finding would alert the nurse to the possibility of the patient having non-Hodgkin’s lymphoma (NHL)? a. Enlarged lymph nodes that form an adjacent line of enlargement. b. Painful widespread enlarged lymph nodes. c. Noncontiguous enlarged lymph nodes. d. Enlarged lymph nodes primarily in the neck and axillary region. ANS: C NHL typically manifests as enlargement in one node, then one or more nodes are skipped, and then another node is affected (noncontiguous). These enlarged nodes are usually painless with NHL. PTS: 1 DIF: Cognitive Level: Comprehension REF: 239 OBJ: 8 (theory) TOP: Lymphoma: Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 18. The nurse is preparing to write a care plan for the patient with fibromyalgia. Which problem/nursing diagnosis best addresses this disorder? a. Fatigue b. Pain, Chronic c. Impaired Physical Mobility d. Activity Intolerance ANS: B Pain is the predominant symptom with fibromyalgia. The pain can lead to other problems, such as fatigue, impaired mobility, and activity intolerance; however, if the pain can be controlled, other health problems may be reduced. PTS: 1 DIF: Cognitive Level: Application REF: 240 OBJ: 16 (clinical) TOP: Fibromyalgia KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Management of Care 19. The nurse is providing teaching to a patient who has undergone a liver transplant. Which statement by the patient demonstrates the need for further patient teaching? a. “I will need to take medications to boost my immune system for the next year.” b. “I will need to be sure to avoid people that have infections.” c. “I will need to take immune suppression medications the rest of my life.” d. “I will need to be monitored to determine if my medications need adjusted.” ANS: A Immune suppression medications will need to be taken for the rest of the patient’s life in order to increase the chances of avoiding organ rejection. Boosting the patient’s immune system would lead to organ rejection. Individuals with infections should be avoided since the immune system is depressed. Doses of medications must be evaluated for necessary adjustments throughout the patient’s lifetime. PTS: 1 DIF: Cognitive Level: Application REF: 217 OBJ: 2 (theory) TOP: Preventing Transplant Rejection KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 20. The home health nurse is teaching the HIV-positive patient and his family members about infection control in the home. Which action indicates that the nurse’s teaching has been successful? a. Using only regular household cleaners to clean the bathroom b. Placing soiled laundry directly into a hamper c. Refusing visitors during certain months of the year d. Wearing gloves during household chores ANS: D The nurse should encourage always donning protective gloves when performing household tasks. After cleaning the bathrooms with a regular household cleaner, disinfect with a 1:10 bleach solution. Soiled laundry should be placed into a closed plastic bag before laundering, not left in an open hamper. It is not necessary to refuse visitors based on certain months of the year; infection control involves proper hand hygiene, avoiding actively ill individuals, and adequately disinfecting surfaces and substances that may have come into contact with contaminated body fluids. PTS: 1 DIF: Cognitive Level: Application REF: 219 OBJ: 2 (clinical) TOP: Infection Control in KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 21. A patient has been exposed to an allergen resulting in a hypersensitivity reaction. The nurse correctly recognizes that which immunoglobulin has been triggered? a. IgA b. IgB c. IgD d. IgE ANS: D On first contact with the allergen, the body’s immune system is triggered to produce immunoglobulin E (IgE) antibody to recognize the specific antigen. PTS: 1 DIF: Cognitive Level: Comprehension REF: 241 OBJ: 10 (theory) TOP: Allergy and Hypersensitivity KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation MULTIPLE RESPONSE 22. Which condition(s) that can cause acquired immune deficiency? (Select all that apply.) a. Chemotherapy b. Viral infections c. Smoking d. Malnutrition e. Bacterial infections ANS: A, B, C, D Bacterial infections do not cause immune deficiency. PTS: 1 DIF: Cognitive Level: Comprehension REF: 217 OBJ: 1 (theory) TOP: Conditions Causing Immune Deficiency KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 23. During assessment of the patient diagnosed with systemic lupus erythematosus (SLE), which sign(s) and symptom(s) would the nurse expect to find? (Select all that apply.) a. Hair loss b. Enlarged cervical lymph nodes c. Mouth sores d. Fatigue e. Rashes ANS: A, C, D, E The patient with SLE does not typically have enlarged lymph nodes. Hair loss, mouth sores, fatigue, and rashes are just a few of the symptoms present in a patient with SLE. PTS: 1 DIF: Cognitive Level: Comprehension REF: 233-234 OBJ: 7 (theory) TOP: SLE KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 24. The nurse is caring for a patient with systemic lupus erythematosus (SLE). The patient complains of severe fatigue, a butterfly rash, and joint pain. Which nursing intervention(s) is/are most appropriate for this patient? (Select all that apply.) a. Encourage the use of a sun lamp to help with the rash. b. Assess pain control measures that have helped the patient in the past. c. Assist the patient with planning rest periods throughout the day. d. Remind the patient to avoid contact with people who have an infection. e. Ensure the patient understands the importance of her medication regimen. ANS: B, C, D, E Any type of sunlight tends to worsen the rash of a patient with SLE and can cause a generalized flare-up of the disease. Pain control measures that have previously been effective should be continued; intense fatigue is a common problem with SLE, so planned rest periods are necessary; infections often exacerbate the disease, so it is important to decrease the chance of the patient with SLE from being exposed to others with infections; and the medication regimen for the SLE patient should be maintained in order to prevent flare-ups of the disease or other body systems from being affected by SLE. PTS: 1 DIF: Cognitive Level: Application REF: 233, 236, Nursing Care Plan 11-1 OBJ: 7 (theory) TOP: SLE KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Management of Care 25. The school nurse is instructing a group of high school sophomores in safe sex practices. Which practice(s) should the nurse include in her teaching? (Select all that apply.) a. Use a condom. b. Use a spermicide. c. Practice abstinence. d. Get vaccinated against HIV. e. Avoid unprotected orogenital sex. ANS: A, C, E HIV can be transmitted by sexual practices of not using a condom and through orogenital sex. Abstinence is the only way to ensure that HIV is not transmitted through sexual intercourse. Spermicides do not prevent HIV transmission, and there is no vaccination against HIV. PTS: 1 DIF: Cognitive Level: Application REF: 222-223 OBJ: 4 (theory) TOP: Safe Sex KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance 26. When collecting data from a patient suspected of having an immune deficiency, which factor(s) should be included? (Select all that apply.) a. Family history of immune disorders b. Age c. Weight gain d. Alcohol use e. Exposure to HIV ANS: A, B, D, E When an immune deficiency is suspected, information is gathered about the current physical status of the patient, such as her general state of health, infections she may have had recently, how the infections affected her, and how frequently they occur. It is also important to assess for risk behaviors such as intravenous drug use, multiple sexual partners, exposure to HIV, immunosuppressive drug therapy, alcohol consumption, and family history of genetic immune disorders. PTS: 1 DIF: Cognitive Level: Comprehension REF: 218-219 OBJ: 14 (clinical) TOP: Nursing Management Immune Deficiency KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation COMPLETION 27. The nurse stresses that the primary emphasis on controlling HIV is __________. ANS: prevention Prevention of HIV infections is the major key to controlling HIV infections. PTS: 1 DIF: Cognitive Level: Knowledge REF: 223 OBJ: 1 (theory) TOP: HIV Infection KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 28. The patient with AIDS voices concern over the amount of money it will cost to manage his disease. The nurse is aware that the estimated medications and laboratory testing cost is an average of $______ per year for the patient with AIDS. ANS: 25000 25,000 It is estimated that medications and laboratory testing for a patient with AIDS will cost at least $25,000. PTS: 1 DIF: Cognitive Level: Knowledge REF: 224 OBJ: 2 (theory) TOP: Diagnosis of AIDS KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Management of Care MATCHING Arrange the process of HIV invasion in the proper sequence. a. HIV attaches to CD4 receptor sites on T-helper cells. b. Opportunistic infection occurs. c. Infected cell replicates itself millions of times. d. T-helper cells fail to activate phagocytes. e. Immune system is unable to respond effectively. 29. Step 1 30. Step 2 31. Step 3 32. Step 4 33. Step 5 29. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 220 OBJ: 3 (theory) TOP: HIV Infection KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 30. ANS: C PTS: 1 DIF: Cognitive Level: Analysis REF: 220 OBJ: 3 (theory) TOP: HIV Infection KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 31. ANS: D PTS: 1 DIF: Cognitive Level: Analysis REF: 220 OBJ: 3 (theory) TOP: HIV Infection KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 32. ANS: E PTS: 1 DIF: Cognitive Level: Analysis REF: 220 OBJ: 3 (theory) TOP: HIV Infection KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 33. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 220 OBJ: 3 (theory) TOP: HIV Infection KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation Chapter 12: The Respiratory System deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. What is the purpose of mucus? a. To warm the air entering the lungs. b. To trap particles and bacteria. c. To protect the cilia. d. To clean the sinus cavity. ANS: B Mucus traps particles and bacteria that may be in the inspired air. PTS: 1 DIF: Cognitive Level: Knowledge REF: 252 OBJ: 1 (theory) TOP: Mucus KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. A patient with emphysema presents to the emergency room with severe dyspnea; O2 saturation is 74%, pulse is 120, and respirations are 26. The nurse positions the patient in high Fowler. What action should the nurse take next? a. Collect a sputum specimen. b. Coach the patient in pursed-lip breathing. c. Give oxygen at 5 L/min by nasal cannula. d. Ensure patent intravenous (IV) access. ANS: B Coaching in pursed-lip breathing will open the respiratory tree with negative pressure. Oxygen given at such a high concentration will cause an emphysemic patient to stop breathing. Collecting a sputum specimen and ensuring patent IV access are appropriate interventions that should be performed after the patient’s dyspnea is addressed. PTS: 1 DIF: Cognitive Level: Analysis REF: 268 OBJ: 7 (clinical) TOP: Oxygen Administration to Emphysemic Patient KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 3. The nurse explains that the mechanism that triggers rate and depth of respiration is based on which factor? a. Ease of respiration. b. Alveolar pressure. c. Patency of bronchi. d. Blood pH. ANS: D Chemoreceptors in the brainstem and carotid arteries measure hydrogen concentration, as well as CO2 and O2, to trigger respiration rate to correct the excessive CO2. PTS: 1 DIF: Cognitive Level: Comprehension REF: 254 OBJ: 2 (theory) TOP: Ventilation and Blood pH KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. When creating a visual aid to show the mechanics of inhaling, the nurse correctly illustrates which scenario? a. The diaphragm moves downward. b. The negative pressure of the lung converts to positive pressure. c. The muscles contract and pull the rib cage downward. d. The bronchi enlarge. ANS: A On inspiration, the diaphragm moves down, increasing the area of negative pressure, muscles pull the rib cage up, and the positive-pressure room air flows into the negative-pressure lungs. PTS: 1 DIF: Cognitive Level: Comprehension REF: 254 OBJ: 1 (theory) TOP: Mechanics of Inspiration KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. Which substance decreases the surface tension of the alveolar walls? a. Plasma b. Surfactant c. Cilia d. Mucus ANS: B Surfactant is the substance that reduces the surface tension of the walls of the alveoli, making gas exchange more effective. PTS: 1 DIF: Cognitive Level: Knowledge REF: 254 OBJ: 1 (theory) TOP: SurfactantKEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 6. Most of the inspired oxygen is carried to the tissues via which component of the body? a. Plasma b. Lymphatic system c. Red blood cells d. White blood cells ANS: C The red blood cells carry 97% of the oxygen to the cells, attached to hemoglobin. PTS: 1 DIF: Cognitive Level: Knowledge REF: 255 OBJ: 1 (theory) TOP: Oxygen Transport KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 7. The nurse is caring for a patient with an obstructive respiratory disorder. Which of these conditions is an example of an obstructive lung disorder? a. Atelectasis b. Lung cancer c. Guillain-Barré syndrome d. Chronic bronchitis ANS: D Obstructive lung disease is related to the reduced ability to move air in and out of the lungs. Asthma, emphysema, and chronic bronchitis are classified as obstructive disorders. Atelectasis, lung cancer, and Guillain-Barré syndrome are restrictive disorders. PTS: 1 DIF: Cognitive Level: Comprehension REF: 256 OBJ: 1 (theory) TOP: Obstructive Lung Disease KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 8. The nurse is caring for multiple patients. After reviewing the patients’ histories, the nurse determines that which patient possesses the highest risk of throat cancer? a. A male patient who drinks four cups of coffee per day b. A female patient who smokes a pack of cigarettes weekly c. A female patient who drinks three carbonated drinks per day d. A male patient who drinks four vodka tonics per day ANS: D The combination of alcohol and cigarettes increases the risk for throat cancer. However, males are four times more likely to develop throat cancer than women, and the male patient consuming vodka drinks is consuming significantly more alcohol than the female patient who smokes cigarettes. Coffee and carbonated drink consumption has not been found to increase the risk of throat cancer. PTS: 1 DIF: Cognitive Level: Analysis REF: 262, Older Adult Care Points OBJ: 2 (theory) TOP: Alcohol-Related Throat CancerKEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance 9. The nurse is preparing to administer the influenza immunization to four patients. Allergy to which substance should cause the nurse to question giving the immunization? a. Strawberries b. Ragweed c. Penicillin d. Eggs ANS: D The influenza vaccine is cultured in chicken embryos, making anyone allergic to eggs probably allergic to the immunization. PTS: 1 DIF: Cognitive Level: Application REF: 256 OBJ: 2 (theory) TOP: Influenza Immunization Allergy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 10. While performing an assessment, the nurse auscultates a coarse low-pitched sonorous rattling in the left lower lobe. Based on the presence of this adventitious lung sound, which action should the nurse take next? a. Instruct the patient to turn, cough, and deep-breathe. b. Administer the diuretic as ordered. c. Administer the bronchodilator as ordered. d. Instruct the patient to blow into the incentive spirometer. ANS: A Low-pitched sonorous wheezing sounds are caused by secretions accumulating in the larger airways. Patients with pneumonia or chronic bronchitis often present with low wheezes (rhonchi). Coughing may help to partially clear the secretions. High-pitched wheezes result from narrowing of air passages, and a bronchodilator would be beneficial. Crackles are produced by air passing through moisture in the smaller airways; diuretics are beneficial. Proper technique for the incentive spirometer directs the patient to inhale through the mouthpiece, as if the patient is pretending to drink a thick milk shake. PTS: 1 DIF: Cognitive Level: Application REF: 265 OBJ: 5 (clinical) TOP: Breath Sounds KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 11. When the nurse places the diaphragm of the stethoscope over one of the main bronchi, which expected normal breath sound should the nurse hear? a. Bronchovesicular sounds b. Bronchial sounds c. Sonorous sounds d. Vesicular sounds ANS: A Bronchovesicular sounds are moderate hollow sounds that are equal on inspiration and expiration. PTS: 1 DIF: Cognitive Level: Comprehension REF: 265 OBJ: 5 (clinical) TOP: Breath Sounds KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 12. The nurse is performing deep tracheal suctioning of a patient with a respiratory disorder. Which action demonstrates appropriate technique? a. The nurse maintains clean technique. b. The nurse places the patient in a side-lying position. c. The nurse suctions the patient for 10 to 15 seconds. d. The nurse reassures the patient that he will feel no discomfort. ANS: C The suctioning, which is done during extraction of the suction tip, should not last more than 10 to 15 seconds as it deprives the patient of oxygen. Deep tracheal suction requires sterile technique, and the patient should be positioned with the neck slightly extended to facilitate entrance into the trachea. Even though the procedure does not last for a long time, suctioning is uncomfortable for the patient. PTS: 1 DIF: Cognitive Level: Application REF: 268 OBJ: 5 (clinical) TOP: Suctioning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 13. The nurse is aware that the patient is in respiratory failure when the blood gas findings contain which values? a. PaO2 46 mm Hg; PaCO2 52 mm Hg b. PaO2 50 mm Hg; PaCO2 45 mm Hg c. PaO2 52 mm Hg; PaCO2 42 mm Hg d. PaO2 55 mm Hg; PaCO2 58 mm Hg ANS: A Respiratory failure is defined by ABGs: arterial oxygen (PaO2) is below 50 mm Hg and partial pressure of carbon dioxide (PaCO2) is equal to or greater than 50 mm Hg. PTS: 1 DIF: Cognitive Level: Comprehension REF: 269 OBJ: 3 (theory) TOP: Blood Gases KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 14. The nurse is caring for a patient who was recently admitted with a traumatic head injury. The nurse anticipates that the patient may display which type of respirations? a. Apneustic respirations b. Cheyne-Stokes c. Kussmaul d. Biot ANS: D Biot respirations are characterized by irregular periods of apnea followed by four to five breaths of identical depth. This pattern is associated with increased intracranial pressure, which is common with a traumatic head injury. Apneustic respirations are indicative of damage to the respiratory centers in the brain. Cheyne-Stokes respirations are often seen in patients in a coma resulting from a disorder affecting the central nervous system. Kussmaul respiration is an abnormal breathing pattern often seen in patients with diabetic acidosis and coma. PTS: 1 DIF: Cognitive Level: Application REF: 269, Figure 12-13 OBJ: 5 (clinical) TOP: Biot Respiration KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 15. The nurse is caring for a postoperative patient. After instructing the patient to cough and deep-breathe, what action should the nurse take next? a. Offer a warm drink. b. Perform mouth care. c. Deliver oxygen by mask. d. Take the patient’s temperature. ANS: B Mouth care should be offered after deep breathing and coughing to clear the mouth of unpleasant taste. PTS: 1 DIF: Cognitive Level: Comprehension REF: 270 OBJ: 5 (clinical) TOP: Mouth Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 16. A patient is admitted to the medical unit with an acute illness accompanied by a fever for the last 3 days. What will likely be the patient’s respiratory response? a. Hypercarbia b. Respiratory alkalosis c. Kussmaul respirations d. Respiratory acidosis ANS: B Respiratory alkalosis, or hypocapnia, results from the patient’s respiratory rate being elevated for a prolonged period due to the persistent fever. The patient blows off too much CO2 as a result. Hypercarbia and respiratory acidosis are the same and result from disorders that cause hypoventilation. Kussmaul respirations are an abnormal breathing pattern. PTS: 1 DIF: Cognitive Level: Application REF: 269 OBJ: 2 (theory) TOP: Hypocapnia KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 17. The nurse is caring for a patient with chronic obstructive pulmonary disorder (COPD) who has been in the hospital for several days. The patient complains of shortness of breath and asks the nurse to turn up his oxygen to compensate for his labored breathing. What is the best nursing response? a. Turn up the patient’s oxygen flow by 1 liter. b. Call the physician for an order to turn up the oxygen. c. Assess the patient in an attempt to identify the cause of the shortness of breath. d. Ask the patient what he usually keeps his oxygen set on at home. ANS: C The nurse should assess the patient for possible causes of the shortness of breath before calling the physician. The nurse may be able to implement nursing interventions, or may need to contact the physician for orders based on the assessment findings. Since the COPD patient’s respiratory drive is lowering levels of PO2, turning up the oxygen may take away his incentive to breathe. Asking the patient about his home oxygen is not helpful at this point. PTS: 1 DIF: Cognitive Level: Analysis REF: 263 OBJ: 7 (clinical) TOP: Respiration Control KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Management of Care MULTIPLE RESPONSE 18. The nurse clarifies that when interstitial edema occurs in the lung tissue, it inhibits ventilation by causing which problem(s)? (Select all that apply.) a. Thickening alveolar membranes b. Pus formation c. Alveoli filling with fluid d. Evaporating surfactant e. Gas failing to diffuse across membrane ANS: A, C, E Interstitial edema will cause problems that affect the alveoli: thickened walls and filling with fluid that obstructs gas exchange across the thickened walls. Pus formation is associated with infection. Surfactant decreases surface tension on the alveolar wall, allowing it to expand more easily with inspiration and preventing alveolar collapse on expiration. PTS: 1 DIF: Cognitive Level: Application REF: 254 OBJ: 2 (theory) TOP: Interstitial Edema KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 19. Which manifestation(s) are age-related changes that alter the respiratory system? (Select all that apply.) a. Weakened cough b. Kyphosis c. Increased ciliary movement d. Decrease in body fluid e. Muscle weakness ANS: A, B, D, E Age-related changes in the respiratory system include weakened cough, kyphosis, decreased bodily fluids, and increased muscle weakness. Age often decreases ciliary movement. PTS: 1 DIF: Cognitive Level: Comprehension REF: 255 OBJ: 2 (theory) TOP: Age-Related Changes That Affect Ventilation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 20. For which individual(s) does U.S. Public Health Service recommend the influenza immunization? (Select all that apply.) a. Physicians b. Compromised infants c. Older adults d. Chronically ill e. Nurses ANS: A, C, D, E Health care workers, older adults, and chronically ill individuals are at risk for contracting influenza and should be immunized. Compromised infants should not be immunized. PTS: 1 DIF: Cognitive Level: Comprehension REF: 256 OBJ: 4 (theory) TOP: Influenza Immunization KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 21. Which physical signs indicate labored breathing? (Select all that apply.) a. Grunting on expiration b. Elevating shoulders and ribs on inspiration c. Tensing neck and shoulder muscles d. Substernal retraction e. Productive cough ANS: A, B, C, D Labored breathing may be indicated by expiratory grunting, inspiratory elevation of shoulders and ribs, tensing neck and shoulder muscles, and substernal retraction. Productive cough is not a sign of labored breathing. PTS: 1 DIF: Cognitive Level: Application REF: 263 OBJ: 5 (clinical) TOP: Signs of Labored Breathing KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 22. The nurse is caring for a patient with a respiratory disorder who complains of anorexia. Which factor(s) may contribute to the patient’s anorexia? (Select all that apply.) a. Increased sense of taste b. Bad taste in mouth c. Fear of exacerbate coughing by eating d. Fatigue e. Altered sense of smell ANS: B, C, D, E Respiratory disorders may cause a bad taste in the mouth, fatigue, and an altered sense of smell; additionally, the patient may be wary that eating will exacerbate coughing. Sense of taste is not heightened by respiratory disorders. PTS: 1 DIF: Cognitive Level: Comprehension REF: 270 OBJ: 2 (theory) TOP: Anorexia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation COMPLETION 23. The nurse uses a visual aid to show the “hinged door” that helps prevent aspiration. This “hinged door” is the __________. ANS: epiglottis The epiglottis is the “hinged door” that closes upon swallowing and opens when breathing. PTS: 1 DIF: Cognitive Level: Knowledge REF: 252 OBJ: 1 (theory) TOP: Epiglottis KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 24. Rapid opening and closing of the glottis combined with movement of the mouth, lips, and tongue is what makes _____________. ANS: speech The rapid opening and closing of the glottis combined with the movement of the mouth, lips, and tongue is what makes speech. PTS: 1 DIF: Cognitive Level: Comprehension REF: 253 OBJ: 1 (theory) TOP: Speech KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 25. The nurse describes the ability of the lungs to respond to change in the volume and pressure of inhaled air by expanding as lung __________. ANS: compliance The lungs normal expansion in response to inhaled air is known as lung expansion. Lung compliance first increases and then decreases with age as the lungs become stiffer and the chest wall becomes more rigid. PTS: 1 DIF: Cognitive Level: Comprehension REF: 254 OBJ: 1 (theory) TOP: Lung Compliance KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation MATCHING Trace the route of a molecule of oxygen inhaled from room air to the point of gas exchange. a. Larynx b. Left and right bronchi c. Trachea d. Oxygen is inhaled through the nose e. Bronchioles f. Alveoli 26. Step 1 27. Step 2 28. Step 3 29. Step 4 30. Step 5 31. Step 6 26. ANS: D PTS: 1 DIF: Cognitive Level: Comprehension REF: 252-253 OBJ: 1 (theory) TOP: Inhalation Process KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 27. ANS: A PTS: 1 DIF: Cognitive Level: Comprehension REF: 252-253 OBJ: 1 (theory) TOP: Inhalation Process KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 28. ANS: C PTS: 1 DIF: Cognitive Level: Comprehension REF: 252-253 OBJ: 1 (theory) TOP: Inhalation Process KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 29. ANS: B PTS: 1 DIF: Cognitive Level: Comprehension REF: 252-253 OBJ: 1 (theory) TOP: Inhalation Process KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 30. ANS: E PTS: 1 DIF: Cognitive Level: Comprehension REF: 252-253 OBJ: 1 (theory) TOP: Inhalation Process KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 31. ANS: F PTS: 1 DIF: Cognitive Level: Comprehension REF: 252-253 OBJ: 1 (theory) TOP: Inhalation Process KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation Place in the appropriate sequence the steps of auscultation of the chest. a. Place diaphragm of stethoscope above clavicles. b. Listen in midaxillary line to level of diaphragm. c. Move stethoscope from side to side down midline of the chest. d. Place diaphragm of stethoscope above scapulae. e. Move stethoscope side to side on either side of the spine. 32. Step 1 33. Step 2 34. Step 3 35. Step 4 36. Step 5 32. ANS: A PTS: 1 DIF: Cognitive Level: Application REF: 264 OBJ: 5 (clinical) TOP: Auscultation KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 33. ANS: C PTS: 1 DIF: Cognitive Level: Application REF: 264 OBJ: 5 (clinical) TOP: Auscultation KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 34. ANS: D PTS: 1 DIF: Cognitive Level: Application REF: 264 OBJ: 5 (clinical) TOP: Auscultation KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 35. ANS: E PTS: 1 DIF: Cognitive Level: Application REF: 264 OBJ: 5 (clinical) TOP: Auscultation KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 36. ANS: B PTS: 1 DIF: Cognitive Level: Application REF: 264 OBJ: 5 (clinical) TOP: Auscultation KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease Chapter 13: Care of Patients with Disorders of the Upper Respiratory System deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. What is the contagion period of a cold? a. 2 days b. 3 days c. 4 days d. 7 days ANS: B The contagion period of a viral cold is about 3 days. PTS: 1 DIF: Cognitive Level: Knowledge REF: 275 OBJ: 1 (theory) TOP: Contagion of Colds KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 2. The nurse is caring for a patient who has had a cold for 1 week. The patient questions why the health care provider issued a prescription for an antibiotic. Which explanation is best? a. “The antibiotic will cure your cold.” b. “The antibiotic will help to reduce your symptoms.” c. “The antibiotic will treat the secondary bacterial infection that has developed.” d. “The antibiotic will decrease the amount of time for which you are contagious.” ANS: C If a cold persists for more than a week to 10 days without improvement, a bacterial infection is present and requires medical treatment. While the etiology of a cold is viral in nature, antibiotics are necessary to this secondary bacterial infection. No cure exists for a cold. Antibiotics will not reduce symptoms of a cold or decrease the contagion period for a cold. PTS: 1 DIF: Cognitive Level: Application REF: 275 OBJ: 1 (theory) TOP: Antibiotics KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 3. The nurse is caring for a patient with suspected sinusitis. Which assessment finding supports this diagnosis? a. Maxillary sinuses nontender on percussion. b. Generalized pain in the upper teeth. c. Clear drainage from the ear. d. Ear pain when lying dow ANS: B Sinusitis is an inflammation of the mucosal lining of the sinuses. Exudate accumulates in the sinuses and pressure builds, which causes pain. Symptoms include painful upper teeth, tenderness over the sinuses, purulent drainage from the nose, nasal obstruction, and sometimes a nonproductive cough. Drainage from the ear and ear pain when supine are findings likely consistent with an ear infection. PTS: 1 DIF: Cognitive Level: Application REF: 276 OBJ: 1 (theory) TOP: Sinusitis KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 4. The nurse is caring for a 20-year-old patient who recently underwent a tonsillectomy. The patient is fully awake and clearing his throat frequently but denies pain. Which action is most important for the nurse to take first? a. Place the patient in a side-lying position. b. Look in the patient’s mouth. c. Offer the patient a grape popsicle. d. Remove the straw from the patient’s tray. ANS: B Frequent swallowing or clearing of the throat may indicate bleeding. Further assessment is indicated, and the nurse should look in the patient’s mouth to assess for bleeding. The fully alert adult patient should be placed in semi-Fowler position to ensure adequate ventilation. Offering the patient a grape popsicle is an appropriate intervention once the nurse confirms that the patient is not bleeding. While removing the straw from the tray is an appropriate intervention to prevent bleeding that may result from sucking, the nurse should first ensure that the patient is not currently bleeding. PTS: 1 DIF: Cognitive Level: Analysis REF: 278 OBJ: 1 (theory) TOP: Positioning After Tonsillectomy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 5. The nurse is caring for a patient with sleep apnea. The patient complains that he is constantly fatigued. Which response is most appropriate for the nurse to make? a. “Patients with sleep apnea experience oxygen overloads, which lead to drowsiness.” b. “Patients with sleep apnea often wake frequently during the night.” c. “Patients with mild sleep apnea benefit from a small amount of red wine right before bed.” d. “All patients have difficulty sleeping properly in the hospital.” ANS: B Periods of apnea followed by abrupt intake of air frequently awaken the patient and reduce the amount of rapid eye movement (REM) sleep. Patients with sleep apnea experience oxygen deficiency. Mild apnea may be treated with conservative measures like avoiding alcohol 4 to 6 hours before bed. Telling the patient that all patients sleep poorly in the hospital ignores the patient’s concern and makes an overgeneralization based on the nurse’s bias. PTS: 1 DIF: Cognitive Level: Application REF: 279 OBJ: 1 (theory) TOP: Sleep Apnea KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 6. The nurse is caring for a patient during the immediate postoperative period following a rhinoplasty. Which finding is most concerning to the nurse? a. The patient complains of being cold and chilled. b. The patient complains of nausea. c. The nurse notices the patient is swallowing frequently. d. The nurse notices drainage on the nasal drip pad. ANS: C Frequent swallowing indicates bleeding that is trickling down the back of the throat. Feeling cold and chilly is a common symptom with surgery and is related to anesthetic and the cool surgical environment. Nausea may be experienced by some patients due to anesthetic. Drainage from the nose is expected. PTS: 1 DIF: Cognitive Level: Application REF: 280 OBJ: 2 (theory) TOP: Postoperative Care: Rhinoplasty KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 7. The nurse is caring for a patient who has a tracheostomy with a one-way valve box. The nurse explains to the CNA that this valve allows the patient to carry out which function? a. Drinking b. Eating c. Coughing d. Talking ANS: D A one-way tracheostomy valve box can be fitted into the tube opening. It allows air to be inhaled through the tracheostomy opening, but the valve closes when the patient exhales. This diverts the exhaled air through the larynx and enables the patient to speak. PTS: 1 DIF: Cognitive Level: Comprehension REF: 282 OBJ: 5 (theory) TOP: One-Way Valve Box KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 8. Which statement is most important for the nurse to make when caring for an anxious patient with a new tracheostomy? a. “I have cared for patients who were able to have the tracheostomy reversed.” b. “I will be efficient and give care quickly.” c. “I will wait until your tracheostomy heals before teaching.” d. “I understand that you might be apprehensive.” ANS: D Offering reassurance to a patient who cannot speak is essential. Care should be unhurried with teaching and conversation. Offering false reassurance or mentioning what other patients have done is inappropriate. Giving care quickly or with minimal conversation may cause further anxiety. Teaching cannot be delayed until the tracheostomy is healed. PTS: 1 DIF: Cognitive Level: Application REF: 285 OBJ: 5 (theory) TOP: Care of a Tracheostomy Patient KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 9. The nurse is caring for a patient who underwent a laryngectomy. Which need should the nurse address first? a. Pain control b. Family support c. Communication method d. Plan for long-term care ANS: C Pain control and family support are important, but the need of a method of communication is paramount for a new tracheostomy patient to allay anxiety, ensure accurate communication between the patient and the nurse, and make the patient comfortable that nursing staff are attentive. The need for long-term care may not be necessary. PTS: 1 DIF: Cognitive Level: Analysis REF: 284 OBJ: 4 (theory) TOP: Laryngectomy: Need for Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 10. The nurse is teaching a patient who underwent a laryngectomy. Which statement describes the correct technique for warming inspired air during cold weather? a. Cover the stoma with a clean hand. b. Cover the stoma with a scarf. c. Apply a moist dressing over the stoma. d. Carry a portable humidifier. ANS: B The fold of the scarf retains body heat and can warm air as the air passes through the scarf. PTS: 1 DIF: Cognitive Level: Comprehension REF: 286 OBJ: 4 (theory) TOP: Warming Inspired Air KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 11. When teaching a patient about esophageal speech, which technique should the nurse instruct the patient to use first? a. Coordinate lip and tongue movements with produced sound. b. Relax the diaphragm to allow air into the esophagus. c. Cough to express air. d. Swallow air and force it back up through the esophagus. ANS: D Many people are able to learn esophageal speech. First, the patient should master the art of swallowing air and then moving it forcibly back up through the esophagus. Next, the patient should learn to coordinate lip and tongue movements with the sound produced by the air passing over vibrating folds of the esophagus. The sounds may be somewhat hoarse, but are more natural than the sounds produced by an artificial larynx. Relaxing the diaphragm and coughing to express air are not methods to achieve esophageal speech. PTS: 1 DIF: Cognitive Level: Application REF: 286 OBJ: 4 (theory) TOP: Esophageal Speech KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 12. The nurse carefully applies suction prior to deflating the cuff on a cuffed tracheostomy in order to prevent which complication? a. Bleeding b. Excessive negative pressure c. Accidental dislodgement of the tube d. Aspiration ANS: D By suctioning prior to deflating the cuff, the oral liquids that are trapped above the balloon cannot be aspirated. Bleeding, negative pressure, and dislodgement of the tube are not related to cuff inflation. PTS: 1 DIF: Cognitive Level: Comprehension REF: 282, Skill 14-1 (on Evolve) OBJ: 5 (theory) TOP: Cuffed Tracheostomy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 13. When doing routine cleaning of a double-lumen tracheostomy tube, the nurse should include which action? a. Place the patient supine. b. Reinsert the inner cannula without touching the faceplate of the tracheostomy tube. c. Rinse the inner cannula in a basin of hydrogen peroxide. d. Clean the inner cannula with a pipe cleaner. ANS: D The inner cannula is cleaned with a pipe cleaner, the patient is put in the semi-Fowler position, and the inner cannula is rinsed in sterile saline or sterile water, rather than peroxide. PTS: 1 DIF: Cognitive Level: Comprehension REF: 282, Skill 14-2 (on Evolve) OBJ: 7 (clinical) TOP: Double-Lumen Tracheostomy Tube KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 14. The nurse is caring for a patient experiencing epistaxis. What action should the nurse take first? a. Obtain the patient’s vital signs. b. Firmly pack the nostrils with gauze. c. Apply a cold compress. d. Instruct the patient to sit forward and pinch the nose below the bone. ANS: D When epistaxis occurs, the patient should sit forward and apply direct pressure by pinching the nose just below the bone, close to the face for 10 to 15 minutes. This position prevents blood from running down the back of the throat. Cold compresses or ice may be applied to the nose to constrict the blood vessels. If there is still bleeding at the end of a 10- to 15-minute period, the process should be repeated. If bleeding continues, the nurse should obtain the patient’s vital signs and notify the provider. The provider may cauterize the bleeding vessels or solidly pack the nose. PTS: 1 DIF: Cognitive Level: Analysis REF: 276 OBJ: 6 (clinical) TOP: Epistaxis KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 15. The nurse is aware that the patient seeking antibiotic treatment for pharyngitis will only receive the desired medication if the condition is caused by what type of pathogen? a. Protozoa b. Bacteria c. A virus d. Fungi ANS: B Pharyngitis (sore throat) will be treated with an antibiotic only if the infection is deemed bacterial in etiology. Protozoa, viruses, and fungi do not respond to antibiotics. PTS: 1 DIF: Cognitive Level: Knowledge REF: 277 OBJ: 1 (theory) TOP: Pharyngitis KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Management of Care 16. The nurse is assisting the physician with the insertion of a new tracheostomy tube. The physician asks for the obturator. The nurse correctly hands the physician which device? a. The guide for the tracheostomy tube to be inserted b. The scalpel used to make the tracheostomy stoma c. A single-cannula tracheostomy tube d. A cuffed tracheostomy tube ANS: A The obturator is used during insertion of a tracheostomy tube as a guide to protect against scraping the sides of the trachea with the sharp edge of the tube. PTS: 1 DIF: Cognitive Level: Comprehension REF: 282 OBJ: 5 (theory) TOP: Types of Tracheostomy Tubes KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Management of Care MULTIPLE RESPONSE 17. Which action(s) may help to reduce the risk of transmitting a common cold? (Select all that apply.) a. Cover the mouth and nose when sneezing. b. Wash the hands frequently. c. Use saline nose sprays. d. Turn the head to the crook of the arm when coughing. e. Drink juices with vitamin C. ANS: A, B, D Covering the mouth and nose when sneezing and coughing as well as frequent washing of hands will reduce the risk of passing a cold to another. Using saline sprays and drinking juices with vitamin C are not helpful in containing a cold. PTS: 1 DIF: Cognitive Level: Comprehension REF: 287 OBJ: 1 (theory) TOP: Cold Contagion KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 18. Which organism(s) are common causative agents for sinusitis? (Select all that apply.) a. Pneumococci b. Pseudomonas c. Staphylococci d. Haemophilus influenzae e. Streptococci ANS: A, D, E The common organisms causing sinusitis are pneumococci, Haemophilus influenzae, and streptococci. PTS: 1 DIF: Cognitive Level: Knowledge REF: 276 OBJ: 1 (theory) TOP: Causes of Sinusitis KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 19. The nurse is teaching an adult post-tonsillectomy patient. Which dietary instructions are most important for the nurse to include? (Select all that apply.) a. Increase intake of citrus fruits. b. Avoid hot fluids. c. Avoid milk products. d. Avoid foods with red dye. e. Use a straw to drink liquids. ANS: B, D Avoiding red colored foods can help in distinguishing between ingested food and blood. Milk products are acceptable for posttonsillectomy patient. Citrus fruits should be avoided until the throat has completely healed. Hot fluids should be avoided until the throat completely heals. Straws are not used because sucking may cause bleeding. PTS: 1 DIF: Cognitive Level: Application REF: 278 OBJ: 2 (theory) TOP: Post-tonsillectomy Instruction KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 20. The nurse is assessing an older adult with a family tendency of developing laryngeal cancer. The nurse should ask the patient about which risk factors? (Select all that apply.) a. History of smoking b. Alcohol abuse c. Exposure to asbestos d. Occupational exposure to wood dust e. Infection with Streptococcus bacteria ANS: A, B, C, D Cigarette smoking, alcohol abuse, asbestos exposure, and wood dust exposure are risk factors linked to laryngeal cancer. Streptococcus bacteria are not considered a risk factor for laryngeal cancer; infection with human papillomavirus or Helicobacter pylori has been linked to increased incidence of cancer of the larynx. PTS: 1 DIF: Cognitive Level: Comprehension REF: 280 OBJ: 1 (theory) TOP: Risk Factors for Laryngeal Cancer KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 21. The nurse is performing discharge teaching for a patient who underwent a microlaryngoscopy with laser removal of polyps. Which instruction(s) should the nurse include? (Select all that apply.) a. Be alert for massive swelling. b. You can return to work in 3 days. c. Cough gently to expectorate blood. d. Observe 2 days of voice rest. e. Take opioids as needed for pain control. ANS: B, D Observation of voice rest for 2 days and return to work in 3 days are the basic instructions. There is minimal swelling or bleeding, and NSAIDs (not opioids) are used for pain control. PTS: 1 DIF: Cognitive Level: Application REF: 280 OBJ: 4 (theory) TOP: Postoperative Care: Microlaryngoscopy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 22. The nurse is setting up the environment for tracheal suction on a newly postoperative tracheostomy patient. Which action(s) should the nurse perform? (Select all that apply.) a. Auscultate lungs for retained secretions. b. Wash hands and open sterile suction kit. c. Don clean gloves and lift out catheter and connect to suction. d. Inform the patient about the procedure. e. Perform suction with sterile supplies. ANS: A, B, D, E The nurse should inform the patient about the procedure. The nurse should auscultate the lungs, wash hands, and open the sterile kit, and perform suction with sterile supplies. Sterile rather than clean gloves should be worn during the suctioning procedure. PTS: 1 DIF: Cognitive Level: Comprehension REF: 283, Nursing Care Plan 13-1, Skill 14-1 (on Evolve) OBJ: 7 (clinical) TOP: Tracheal Suction KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 23. The radical neck resection removes a large amount of tissue on the same side as the lesion. Which statement(s) about the tissue removed is/are correct? (Select all that apply.) a. The tissue includes all muscle, lymph nodes, and soft tissue from the lower edge of the mandible to the top of the clavicle. b. The tissue includes all muscle, lymph nodes, and soft tissue from the top of the trapezius to the midline. c. The tissue includes all muscle, lymph nodes, and soft tissue from the lower edge of the eye socket to the bottom of the maxilla, including the zygomatic arch. d. The tissue includes part of the tongue and parotid salivary glands. e. The tissue includes all lower lip to midline. ANS: A, B, C The tissue includes: all muscle, lymph nodes, and soft tissue from the lower edge of the mandible to the top of the clavicle; all muscle, lymph nodes, and soft tissue from the top of the trapezius to the midline; and all muscle, lymph nodes, and soft tissue from the lower edge of the eye socket to the bottom of the maxilla, including the zygomatic arch. The radical neck resection does not ordinarily include the tongue, parotid salivary glands, or lip. PTS: 1 DIF: Cognitive Level: Knowledge REF: 280 OBJ: 1 (theory) TOP: Radical Neck Resection KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 24. The nurse is teaching a patient with a newly resolved episode of epistaxis. Which information is important for the nurse to include? (Select all that apply.) a. Avoid sneezing. b. Rest for several hours until all threat of epistaxis is gone. c. Avoid rubbing the nose. d. Gently remove clotted blood from the occluded nostril. e. Blow the nose gently in small breaths. ANS: A, B, C The patient should avoid sneezing, rest for several hours, and avoid rubbing the nose. The patient should not attempt to remove clotted blood or blow the nose. PTS: 1 DIF: Cognitive Level: Application REF: 276 OBJ: 6 (clinical) TOP: Epistaxis KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 25. The clinic nurse is giving discharge instructions to the mother of a 10-year-old boy who has been diagnosed with a mild cold. Which statements indicate that the mother accurately understands the nurse’s instructions? (Select all that apply.) a. “I will be sure he takes the entire prescription of antibiotic.” b. “I will be sure he drinks plenty of apple and orange juice.” c. “If he runs a fever, I will give him two aspirin every 4 hours until his fever comes down.” d. “I will be sure he washes his hands well so he doesn’t pass this cold on to his younger sister.” e. “Since his cold symptoms just started, zinc lozenges may be helpful for him to take.” ANS: B, D, E Increasing fruit and citrus juice intake may decrease the duration or severity of a cold. Proper hand hygiene decreases the likelihood of transmission. According to Singh and Das (2013), if started with conjunction of symptom onset, zinc lozenges have proven effective in limiting a cold’s duration and severity. Antibiotics are not used for colds (because colds are viral in etiology) unless a secondary infection is present or there is an increased risk for a secondary infection. Aspirin should not be given to children under age 12 due an increased risk for Reye syndrome. PTS: 1 DIF: Cognitive Level: Application REF: 275 OBJ: 1 (theory) TOP: Treatment and Nursing Management: Colds KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort COMPLETION 26. The nurse encourages a patient with larynx cancer that the “near-total laryngectomy” is a new procedure that preserves the ability to __________ and to __________. ANS: speak; swallow swallow; speak The new technique does not rob the patients’ ability to speak or swallow, which makes rehabilitation easier. PTS: 1 DIF: Cognitive Level: Comprehension REF: 280 OBJ: 4 (theory) TOP: Near-total Laryngectomy KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity MATCHING Place the steps of abdominal thrusts in proper sequence. a. Wrap hand around fist. b. Squeeze and thrust five times. c. Make a fist. d. Check status of breathing. e. Position fist, thumb foremost, over umbilicus. 27. Step 1 28. Step 2 29. Step 3 30. Step 4 31. Step 5 27. ANS: D PTS: 1 DIF: Cognitive Level: Application REF: 278 OBJ: 3 (theory) TOP: Abdominal Thrusts KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 28. ANS: C PTS: 1 DIF: Cognitive Level: Application REF: 278 OBJ: 3 (theory) TOP: Abdominal Thrusts KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 29. ANS: E PTS: 1 DIF: Cognitive Level: Application REF: 278 OBJ: 3 (theory) TOP: Abdominal Thrusts KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 30. ANS: A PTS: 1 DIF: Cognitive Level: Application REF: 278 OBJ: 3 (theory) TOP: Abdominal Thrusts KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 31. ANS: B PTS: 1 DIF: Cognitive Level: Application REF: 278 OBJ: 3 (theory) TOP: Abdominal Thrusts KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance Chapter 14: Care of Patients with Disorders of the Lower Respiratory System deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The patient with acute bronchitis asks if antibiotics will be ordered for the condition. Which response is best for the nurse to make? a. “Antibiotics are the best treatment option.” b. “Antibiotics will not help a viral condition.” c. “Antibiotics will be given if the sputum culture indicates your bronchitis is caused by bacteria.” d. “Antibiotics will inhibit the inflammatory response of your body to the invasion of this infection.” ANS: C Bronchitis is treated symptomatically with humidification and cough medications. Antibiotics are only given if the sputum culture suggests it. PTS: 1 DIF: Cognitive Level: Comprehension REF: 290 OBJ: 1 (theory) TOP: Bronchitis: Treatment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 2. The nurse is assessing the patient with influenza. The patient reports having general malaise and aching muscles over the past 2 weeks. The nurse suspects that the patient may have developed which complication of influenza? a. Bronchitis b. Bacterial pneumonia c. Urinary infection d. Encephalitis ANS: B Bacterial pneumonia is a common complication of influenza and may present with atypical symptoms of only general malaise and muscle aches, making it difficult to recognize the symptoms of pneumonia. Bronchitis, urinary infections, and encephalitis are not common complications of influenza. PTS: 1 DIF: Cognitive Level: Application REF: 293 OBJ: 1 (theory) TOP: Complications of Influenza: Pneumonia KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 3. What is the purpose of treatment with amantadine (Symmetrel)? a. To prevent viral pneumonia if taken regularly. b. To prevent avian flu if taken at the first signs and symptoms of disease. c. To lessen the severity of type A flu symptoms if taken within 48 hours of exposure. d. To reduce irritation of bronchitis if taken weekly. ANS: C Amantadine (Symmetrel) is an antiviral medication that may be given within 48 hours of exposure or within 48 hours of the onset of influenza symptoms. It is not a drug that is taken regularly and will not stop the spread of the avian flu. PTS: 1 DIF: Cognitive Level: Knowledge REF: 291 OBJ: 1 (theory) TOP: Treatment: Amantadine KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 4. The nurse is caring for a patient with suspected bacterial pneumonia. Which finding supports the potential diagnosis? a. Elevated white blood cell (WBC) count b. Consolidation of lung tissue c. Interstitial inflammation d. Copious exudate ANS: C Viral pneumonia causes interstitial inflammation with attendant edema. White blood cell (WBC) count will not be elevated and no exudate is consolidating the lung as with bacterial pneumonia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 292 OBJ: 1 (theory) TOP: Pneumonia: Viral KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 5. The 79-year-old patient with bacterial pneumonia becomes increasingly restless, confused, and agitated. The patient’s temperature is 100° F, and his pulse, blood pressure, and respirations are elevated since the last assessment 6 hours ago. What action should the nurse take first? a. Auscultate the patient’s lungs. b. Assess the patient’s oxygen saturation. c. Administer the mild sedative as ordered. d. Administer an ordered analgesic for discomfort. ANS: B Outward signs of hypoxia vary in patients, but dyspnea, restlessness, and confusion are the most common signs. While blood gas analysis is the most reliable indicator, bedside assessment pulse oximetry is quick, noninvasive, and gives a snapshot of oxygen saturation. The nurse should auscultate the patient’s lungs after obtaining the oxygen saturation. Medications for sedation or discomfort do not address the patient’s current condition. PTS: 1 DIF: Cognitive Level: Analysis REF: 321 OBJ: 2 (theory) TOP: Hypoxia KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 6. The 75-year-old patient asks the nurse if the Pneumovax immunization he took when he was 65 is still protecting him. Which reply is most accurate? a. “Pneumovax protects you for your lifetime.” b. “Immunity afforded you by Pneumovax lasts only 2 years.” c. “Pneumovax protection varies according to your risk factors and living situation.” d. “After 6 years, you need a repeat dose of Pneumovax for full immunity.” ANS: D Pneumovax, an immunization that protects against 23 pneumococcal organisms, is repeated 6 years after the first dose. PTS: 1 DIF: Cognitive Level: Comprehension REF: 292 OBJ: 1 (theory) TOP: Pneumonia Immunization: Pneumovax KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 7. The 75-year-old patient presents to the emergency department with shortness of breath, fatigue, and a dry cough. When information leads the nurse to suspect that this patient should undergo workup for histoplasmosis? a. The patient reports drinking pond water. b. The patient lives on a farm and raises chickens. c. The patient recently went hunting in a wooded area. d. The patient owns a landscaping company. ANS: B Histoplasmosis is caused by a fungus that lives in bird droppings. Contact with chickens coupled with the characteristic signs of dry cough, shortness of breath, and fatigue warrants a workup for histoplasmosis. Legionellosis is a bacterial infection contracted from contaminated drinking water. Rocky Mountain spotted fever and lime disease are transmitted by ticks found in wooded areas. Coccidioidomycosis is contracted by people who engage in desert recreational activities or are working in occupations that require digging in the earth. PTS: 1 DIF: Cognitive Level: Application REF: 294 OBJ: 2 (theory) TOP: Fungal Infection: Histoplasmosis KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 8. The nurse is caring for a 30-year-old American Indian female who is taking Rifater, a drug containing rifampin, isoniazid, and pyrazinamide. The patient asks how long she will have to take the medication. Which response explains when the patient may discontinue the medication? a. When the sputum culture comes back negative b. When the medication has been taken for 9 months c. When three consecutive sputum cultures are negative d. When the tuberculin skin test (TST) is no longer positive ANS: C This drug is given to treat active tuberculosis (TB). The active TB patient is considered noncontagious when three consecutive sputum cultures are negative. Taking the medication for a given period of time does not make the patient noncontagious. The TST will always be positive. PTS: 1 DIF: Cognitive Level: Comprehension REF: 296 OBJ: 3 (theory) TOP: TB: Treatment KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 9. The nurse reading a tuberculin skin test (TST) on a new employee who lives in the Midwest, is 20-years-old, and has no known history of contact with any people with tuberculosis (TB). The nurse should interpret the reading as positive if the area around the injection site has an induration of how many millimeters? a. 0 mm b. 5 mm c. 10 mm d. 15 mm ANS: D All TSTs are read at 48 to 72 hours after the injection. A positive reading of a TST for a person who is low risk for exposure is an area of swelling 15 mm or more. For individuals who are at high risk for TB (such as recent immigrants from countries where TB is prevalent, medically underserved groups, and the homeless), swelling of more than 10 mm is considered positive. Individuals with a history of contact with infectious TB or who are immunocompromised are considered to have a positive TST if there is more than 5 mm of swelling. PTS: 1 DIF: Cognitive Level: Comprehension REF: 295 OBJ: 3 (theory) TOP: TB: TST KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 10. The nurse is assessing a patient with chronic obstructive pulmonary disease (COPD). Which assessment finding indicates a potential complication and requires the nurse’s immediate attention? a. Distended neck veins b. Left lower quadrant tenderness c. Urinary output of 40 mL/hr d. Excessive coughing ANS: A Cor pulmonale is enlargement of the right side of the heart as a result of pulmonary hypertension caused by constriction of the pulmonary vessels in response to hypoxia. Constant hypoxia stimulates erythropoiesis, with resulting polycythemia and increased viscosity of blood. Eventually, right-sided heart failure causes systemic venous congestion which manifests with distended neck veins. The patient would experience right upper quadrant tenderness from an engorged liver. Urinary output of 40 mL/hr is normal. Excessive coughing does not indicate an urgent complication. PTS: 1 DIF: Cognitive Level: Application REF: 300 OBJ: 2 (theory) TOP: COPD Complication: Cor Pulmonale KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 11. The patient with asthma is prescribed a leukotriene modifier drug, montelukast (Singulair). Which statement describes an advantage of this medication? a. Limited gastrointestinal (GI) side effects b. Bronchodilation and anti-inflammatory effects c. Stringent control of acute episodes of asthma d. Ability to replace all other asthma remedies ANS: B Singulair provides both bronchodilation and anti-inflammatory effects, but it has numerous GI side effects and is not effective in controlling acute asthmatic attacks. PTS: 1 DIF: Cognitive Level: Comprehension REF: 305, Table 14-4 OBJ: 3 (clinical) TOP: Asthma: Treatment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 12. After using a nasal cannula delivery system at 3 L/min, a patient with chronic airflow limitation (CAL) changes to a simple face mask. The nasal equipment oxygen was set at 3 L/min. How should the nurse adjust the oxygen flow for the new delivery system? a. Decrease it to 2 L. b. Keep it the same. c. Increase it to 4 L. d. Increase it to 6 L. ANS: D When changing to a mask from a nasal cannula, the oxygen should be increased by approximately 100% to get the same concentration. Simple face masks deliver approximately the same range of concentration of oxygen as the nasal cannula. However, the nasal cannula flow rates range from 1 to 6 L, delivering 24% to 44% oxygen, whereas the simple face mask delivers 35% to 50% oxygen which is achieved with flow rates from 6 to 12 L. PTS: 1 DIF: Cognitive Level: Application REF: 320, Table 14-5 OBJ: 1 (clinical) TOP: Oxygen Delivery Systems KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 13. The nurse is caring for a patient immediately postoperative after a left pneumonectomy. How should the nurse position the patient? a. In high Fowler position b. In semi-Fowler position c. In a right side-lying position d. In a left side-lying position ANS: D Postoperative positioning after a pneumonectomy is on the operated side to prevent the threat of tension pneumothorax with mediastinal shift and leakage from the amputated bronchial stump. The physician’s order should always be checked before turning the patient or raising the head of the bed. PTS: 1 DIF: Cognitive Level: Comprehension REF: 312 OBJ: 6 (theory) TOP: Pneumonectomy: Positioning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 14. The nurse is caring for a patient with a closed-chest drainage system with chest tubes. Which observation confirms that the system is intact and working? a. The water level in the water-seal chamber fluctuates. b. The level of fluid in the collection chamber rises. c. There are constant bubbles in the water-seal chamber. d. The suction has been attached. ANS: A If the level of the water in the water-seal chamber rises and falls with the patient’s respiration, the system is intact. Constant bubbles in the water-seal chamber indicate a leak in the system. The fluid in the collection container drains by gravity whether the closed-chest drainage system is intact or not. Suction is not significant with respect to whether the system is intact. PTS: 1 DIF: Cognitive Level: Comprehension REF: 314 OBJ: 6 (theory) TOP: Closed-Chest Drainage KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 15. The nurse is caring for a first-day postoperative thoracotomy patient. The nurse assesses that the level of drainage has not increased over the last 3 hours. After assessing the patient’s respiratory status, what should the nurse do next? a. Raise the system above the patient’s heart. b. Check the tubing for kinks. c. Reposition the patient. d. Notify the physician. ANS: B After assessing the patient’s respiratory status, the nurse should ensure that the tubing is not kinked or obstructed by the weight of the patient. The nurse should then check the apparatus; all connections should be taped, be intact, and remain airtight. The system must be below the level of the patient’s heart. The nurse should also double-check the physician’s order for patient position, and reposition as needed. Finally, the nurse should report the findings to the RN or physician. PTS: 1 DIF: Cognitive Level: Application REF: 313 OBJ: 6 (theory) TOP: Closed-Chest Drainage KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 16. The nurse is educating a patient who requires daily postural drainage treatments. Which statement indicates that the patient understands when and why treatments will be scheduled? a. “I will have treatments first thing in the morning to get rid of fluids that have built up over night.” b. “I will have my treatments after an hour after breakfast to make sure that I am fully alert.” c. “I will have treatments after lunch to prevent an unsafe drop in my blood sugar.” d. “I will have treatments right before bed to ensure that I breathe more easily at night.” ANS: A If the patient is to have postural drainage only once a day, drainage should be done in the morning to remove secretions that have accumulated during the night. Because there is likely to be some gagging during coughing episodes that take place during postural drainage, it is best to carry out the procedure before meals, when the stomach is relatively empty and vomiting is less likely. PTS: 1 DIF: Cognitive Level: Application REF: 318 OBJ: 2 (theory) TOP: Postural Drainage KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 17. The patient with sleep apnea is fitted with a continuous positive airway pressure (CPAP) mask and asks the nurse how this device will help. How should the nurse respond? a. “The device delivers constant positive pressure to keep your airway open.” b. “The device will require you to be intubated to open your airway.” c. “The device delivers oxygen only when you are apneic.” d. “The device delivers negative pressure to stimulate your respirations.” ANS: A The CPAP mask delivers a constant positive pressure to keep the airway open. CPAP does not require intubation and does not deliver negative pressure. PTS: 1 DIF: Cognitive Level: Comprehension REF: 323 OBJ: 6 (theory) TOP: CPAP Mask KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 18. When caring for a patient with acquired immune deficiency syndrome (AIDS), the nurse is aware that this patient is most at risk for developing which type of pneumonia? a. Hypostatic b. Streptococcus pneumoniae c. Atypical d. Pneumocystis jiroveci ANS: D Pneumocystis jiroveci (formerly known as Pneumocystis carinii) is commonly seen in AIDS patients. Hypostatic pneumonia is related to inadequate aeration of the lungs seen frequently with immobile patients. Streptococcus pneumoniae is the most common causative organism for bacterial pneumonia in the general population. Atypical pneumonia refers to pneumonia that does not present with the typical symptoms of pneumonia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 293 OBJ: 1 (theory) TOP: Pneumonia KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 19. The nurse is educating an asthma patient about proper use of the peak flowmeter. The nurse determines that the patient needs further teaching when observing which action? a. The patient repeats the procedure and obtains three readings. b. The patient breathes deeply through the mouthpiece. c. The patient stands while performing the test. d. The patient reports the highest reading on the peak flow sheet. ANS: B Peak flow should be monitored on a daily basis to determine if the asthma patient has adequate airflow. The reading helps determine if treatment should be adjusted. The patient should stand to achieve adequate chest expansion while taking a deep breath. The patient then blows as hard and fast as possible into the device with the mouthpiece in the mouth and the lips clamped firmly around it for a tight seal. The procedure should be performed three times with the highest reading recorded. PTS: 1 DIF: Cognitive Level: Comprehension REF: 306, Patient Teaching OBJ: 3 (clinical) TOP: Patient Teaching: Peak Flowmeter KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance MULTIPLE RESPONSE 20. Through which method(s) can influenza spread? (Select all that apply.) a. Direct contact b. Indirect contact c. Vector d. Blood-borne method e. Droplets ANS: A, B, E Influenza spreads through direct and indirect contact from droplets. Influenza is not spread by vectors or the blood-borne method. PTS: 1 DIF: Cognitive Level: Knowledge REF: 291 OBJ: 1 (theory) TOP: Influenza: Contagion KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 21. The home health nurse is making an initial call on a newly diagnosed tuberculosis (TB) patient. The patient lives with his wife and child. Which infection control instructions should the nurse include in the teaching plan? (Select all that apply.) a. Place contaminated tissues in sealable plastic bag. b. Take medications exactly as directed. c. Implement airborne precautions. d. Wash hands frequently. e. Wear a mask when in crowds. ANS: A, B, D, E Instructions should include information about disposing of contaminated materials in sealed bags, taking medications exactly as directed, utilizing frequent hand hygiene, and donning a mask when in crowds. Since the family has already been exposed, taking airborne precautions is unnecessary. PTS: 1 DIF: Cognitive Level: Comprehension REF: 297 OBJ: 3 (theory) TOP: TB: Prevention KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 22. The nurse is performing an occupational history as part of the respiratory assessment. Which occupation(s) place the patient at increased risk for an occupational lung disorder? (Select all that apply.) a. A firefighter b. A cotton gin worker c. A construction contractor d. A bartender e. A landscaper ANS: A, B, C Firefighters, cotton gin workers, and construction contractors all come into contact with occupational hazards that could increase risks for lung disorders. Coal dust, dust from hemp, flax, and cotton processing, and exposure to silica in the air all can cause work-related lung disorders. Asbestos exposure may cause mesothelioma and scarring of lung tissue. The other exposures cause obstruction of small airways or scarring and loss of elasticity and compliance. A bartender and landscaper are not at increased risk of occupational lung disorders. PTS: 1 DIF: Cognitive Level: Comprehension REF: 298 OBJ: 3 (theory) TOP: Occupational Lung Disorders KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 23. The nurse is caring for a patient with advanced emphysema. Which signs are manifestations of this disorder? (Select all that apply.) a. Productive cough b. Dyspnea c. Barrel chest d. Wheezing e. Cyanotic skin tone ANS: A, B, C, E Manifestations of late emphysema include a productive cough, dyspnea, a barrel chest, and cyanosis. (Coughing, mucus production, and cyanosis usually do not occur until late in the disease.) Wheezing usually does not occur in the emphysemic patient. PTS: 1 DIF: Cognitive Level: Comprehension REF: 300 OBJ: 2 (theory) TOP: Emphysema: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 24. The home health nurse is educating a 60-year-old patient with emphysema with a nutritional deficit. Which instructions should the nurse include in the teaching plan to address this problem? (Select all that apply.) a. Rest before eating. b. Avoiding gas-producing foods. c. Eat four to six small meals instead of three large meals. d. Lie down after eating. e. Take small bites and chew slowly. ANS: A, B, C, E The patient should rest before eating to prevent fatigue. Foods that cause gas or bloating can lead to a distended stomach, which can increase work of breathing. Eating four to six small meals a day rather than three regular meals decreases stomach fullness and reduces fatigue. Taking small bites and chewing food slowly may help combat shortness of breath. The patient should avoid lying down for an hour after eating. PTS: 1 DIF: Cognitive Level: Application REF: 300, Nutrition Considerations OBJ: 2 (theory) TOP: Emphysema: Anorexia KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 25. The nurse is caring for a patient on a mechanical ventilator that it is set on assist-control mode. Which statement(s) accurately describe this function? (Select all that apply.) a. The ventilator delivers a set tidal volume. b. The ventilator delivers a set number of breaths if the patient’s rate falls. c. The ventilator automatically cuts off if the patient is breathing independently. d. The ventilator delivers more oxygen at the end of an inspiration. e. The ventilator helps correct respiratory acidosis. ANS: A, B The assist-control mode delivers a set tidal volume on every respiration and will deliver a set number of breaths per minute should the patient’s rate drop. It does not cut off automatically or deliver more oxygen at the end of the inspiration, nor does it correct respiratory acidosis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 322 OBJ: 2 (clinical) TOP: Mechanical Ventilation: Assist-Control Mode KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 26. The nurse is preparing a presentation that highlights the benefits of annual influenza vaccination. The nurse correctly targets which groups? (Select all that apply.) a. Parents of children 3 to 6 months of age. b. Diabetics who are over 50 years old. c. Pregnant women. d. Home health aides. e. CNAs who work in long-term care facilities. ANS: B, C, D, E Children ages 6 to 59 months should receive the influenza vaccine, not children 3 to 6 months of age. The Advisory Committee on Immunization Practices also suggests that pregnant women, people over age 50, and people with certain chronic illnesses receive the vaccine. In addition, health care workers and those caring for people in homes who are at high risk for contracting influenza should receive the vaccine. PTS: 1 DIF: Cognitive Level: Comprehension REF: 291, Health Promotion OBJ: 1 (theory) TOP: Influenza Vaccination KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance MATCHING Place the events of an asthma attack in proper sequence. a. Mast cell–mediated inflammatory response in bronchi b. Mucus production c. Plugging of small airways d. Contact with precipitator e. Mucosal edema 27. Step 1 28. Step 2 29. Step 3 30. Step 4 31. Step 5 27. ANS: D PTS: 1 DIF: Cognitive Level: Application REF: 302, Concept Map 14-2 OBJ: 4 (theory) TOP: Asthma: Pathophysiology KEY: Nursing Process Step: N/A MSC: NCLEX: Health Promotion and Maintenance 28. ANS: A PTS: 1 DIF: Cognitive Level: Application REF: 302, Concept Map 14-2 OBJ: 4 (theory) TOP: Asthma: Pathophysiology KEY: Nursing Process Step: N/A MSC: NCLEX: Health Promotion and Maintenance 29. ANS: E PTS: 1 DIF: Cognitive Level: Application REF: 302, Concept Map 14-2 OBJ: 4 (theory) TOP: Asthma: Pathophysiology KEY: Nursing Process Step: N/A MSC: NCLEX: Health Promotion and Maintenance 30. ANS: B PTS: 1 DIF: Cognitive Level: Application REF: 302, Concept Map 14-2 OBJ: 4 (theory) TOP: Asthma: Pathophysiology KEY: Nursing Process Step: N/A MSC: NCLEX: Health Promotion and Maintenance 31. ANS: C PTS: 1 DIF: Cognitive Level: Application REF: 302, Concept Map 14-2 OBJ: 4 (theory) TOP: Asthma: Pathophysiology KEY: Nursing Process Step: N/A MSC: NCLEX: Health Promotion and Maintenance Chapter 15: The Hematologic System deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. Which organ releases the erythropoietin-stimulating factor that directs stem cells in the bone marrow to make blood cells? a. Brain b. Lung c. Kidney d. Liver ANS: C The kidney secretes the erythropoietin-stimulating factor to stimulate the stem cells to make blood cells. PTS: 1 DIF: Cognitive Level: Knowledge REF: 328 OBJ: 2 (theory) TOP: Erythropoiesis KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. What is the average life span of a red blood cell (RBC)? a. 30 days b. 90 days c. 100 days d. 120 days ANS: D RBCs live approximately 120 days. PTS: 1 DIF: Cognitive Level: Knowledge REF: 328 OBJ: 1 (theory) TOP: Life of RBCs KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 3. Which organ can help the body compensate in the event of a massive hemorrhagic episode by contracting and adding blood to the circulating volume? a. Spleen b. Liver c. Pancreas d. Bone marrow ANS: A The spleen has the ability to contract and add blood to the circulating volume in the event of massive hemorrhage. PTS: 1 DIF: Cognitive Level: Knowledge REF: 330 OBJ: 1 (clinical) TOP: Spleen KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. The nurse is reviewing laboratory reports for multiple patients. Which patient’s laboratory values require the nurse’s immediate attention? a. Hemoglobin (Hgb) of 7.1 g/dL; white blood cell (WBC) count of 4500 mL/mm3 b. Potassium of 5.5 mEq/L; WBC count of 7000 mL/mm3 c. Sodium of 129 mEq/L; WBC of 6000 mL/mm3 ; 13.2 g/dL d. Calcium of 8.8 mg/dL; WBC count of 8000 mL/mm3 ANS: A All of the WBC counts are normal. The nurse must then decide which other laboratory value requires the most urgent attention. The Hgb is critically low and requires immediate intervention (likely a transfusion). The low Hgb suggests possible anemia or blood loss. The normal Hgb range for adults is: females, 12.0 to 16.7 g/dL; males, 13.0 to 18.0 g/dL. The potassium of 5.5 mEq/L is at the top of the normal range and requires close monitoring for potential cardiac complications but is less urgent than the critical value. The sodium of 129 mEq/L is at the low end of the normal range and requires close monitoring but is less urgent than the critical value. The calcium level of 8.8 mg/dL is a normal value. PTS: 1 DIF: Cognitive Level: Analysis REF: 333, Table 15-1 OBJ: 5 (theory) TOP: Blood Counts KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 5. When the nurse notes a rise in the eosinophil count, which problem does she suspect? a. Bacterial infection b. Allergy c. Viral infection d. Blood dyscrasia ANS: B In the event of an allergy or the infestation of pinworms, the eosinophil count will rise. Bacterial infection stimulates the production of neutrophils and segmented neutrophils; lymphocytes are increased with viral infections. Blood dyscrasia refers to an imbalance in the numbers of types of cells or other pathologic conditions of the blood. PTS: 1 DIF: Cognitive Level: Comprehension REF: 329 OBJ: 5 (theory) TOP: Eosinophil Count KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 6. The nurse uses a visual aid to depict the several kinds of hemoglobin. Which hemoglobin changes the shape of the red blood cell RBC on which it resides? a. hemoglobin A b. hemoglobin A1c c. hemoglobin F d. hemoglobin S ANS: D Hemoglobin S is the abnormal hemoglobin seen in people with sickle cell anemia. The hemoglobin changes the shape of the RBC to a sickle shape. PTS: 1 DIF: Cognitive Level: Knowledge REF: 332 OBJ: 1 (theory) TOP: Hgb S KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 7. The nurse is caring for an 80-year-old African American patient. On assessment, the nurse observes yellow sclera. Which other finding would support the nurse’s suspicion that hemolysis is occurring? a. Koilonychia b. Circumoral cyanosis c. Tea colored urine d. Hemangioma ANS: C Jaundice, or a yellowing discoloration of the skin and sclera of the eyes, can occur as a result of excessive destruction of red blood cells (hemolysis). When red blood cells are ruptured, bilirubin is released. The pigment eventually finds its way into the bloodstream, where it causes jaundice. If hemolysis is occurring, the urine will often contain bilirubin, giving urine a brown tea color. Koilonychia are ridges in the fingernails associated with iron deficiency anemia. Circumoral cyanosis is a bluish tinge around the mouth that indicates respiratory deficiency. A hemangioma is a benign, strawberry-colored birthmark common in children. PTS: 1 DIF: Cognitive Level: Application REF: 336 OBJ: 7 (theory) TOP: Hemolysis KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 8. Jaundice results from excessive release of which substance into the bloodstream? a. Histamine b. Bilirubin c. Plasma d. Platelets ANS: B Excessive levels of bilirubin in the blood (hyperbilirubinemia) from the increased hemolysis of red blood cells are responsible for jaundice. PTS: 1 DIF: Cognitive Level: Knowledge REF: 336 OBJ: 7 (theory) TOP: Jaundice: Hyperbilirubinemia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 9. The nurse is caring for a patient with pernicious anemia. The patient asks the nurse why she experiences constant fatigue. Which response most accurately answers the patient’s question? a. “Your anemia causes inadequate oxygen delivery to your cells, which causes you to feel fatigue.” b. “Your anemia causes an enlarged spleen, which makes breathing difficult and leads to fatigue.” c. “Your anemia causes proliferation of white cells, which leads to fatigue.” d. “Your anemia causes excessive manufacture of red blood cells, which overworks your body and leads to fatigue.” ANS: A The fatigue experienced by people with anemia is related to the lack of oxygenation due to the lack of RBCs to carry the oxygen. PTS: 1 DIF: Cognitive Level: Comprehension REF: 337 OBJ: 3 (clinical) TOP: Fatigue Associated With Anemia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 10. If melena appears, a minimum of what amount of blood has been deposited into the gastrointestinal (GI) tract? a. 35 mL b. 50 mL c. 80 mL d. 100 mL ANS: B For the symptom of melena (dark, tarry stools) to appear, a minimum of 50 to 75 mL of blood must have entered the GI tract. PTS: 1 DIF: Cognitive Level: Knowledge REF: 339, Clinical Cues OBJ: 2 (clinical) TOP: Melena KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 11. The nurse is caring for a patient whose complete blood count reports an abnormal amount of “bands,” or immature granulocytes. Based on this finding, which problem does the nurse suspect? a. An ongoing bacterial infection b. An allergic reaction c. Impending anemia d. An overwhelming viral infection ANS: A Immature white blood cells are released when the more mature circulating cells have not been able to combat an ongoing bacterial infection. Eosinophils increase in response to allergic reactions, and red blood cells are associated with anemia. An increase in lymphocytes is seen with a viral infection. PTS: 1 DIF: Cognitive Level: Comprehension REF: 332, Clinical Cues OBJ: 5 (theory) TOP: Significance of Bands: Bacterial Infection KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 12. The nurse is caring for an older adult patient who is confused and irritable. The nurse reviews the patient’s history and notes that it is negative for dementia. Which potential underlying problem should the nurse suspect? a. Leukopenia b. Hypokalemia c. Hypoxia d. Hyperbilirubinemia ANS: C Confusion and irritability caused by hypoxia is often mistaken for Alzheimer’s dementia. Confusion and irritability are not common features of low white blood cell count, low potassium levels, or high bilirubin levels. PTS: 1 DIF: Cognitive Level: Application REF: 336, Older Adult Care Points OBJ: 5 (theory) TOP: Hypoxia versus Dementia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 13. The nurse is reviewing a patient’s assessment data upon admission to the acute care facility. Which finding best indicates iron deficiency anemia? a. Pulse of 90 beats/min b. Yellow sclera c. Tea-colored urine d. Pale conjunctivae ANS: D Pale conjunctivae are an indication of anemia. A pulse rate of 90 beats/min is within the higher limits of normal. Yellow sclera is indicative of jaundice. Tea-colored urine may indicate the presence of bilirubin or blood in the urine. PTS: 1 DIF: Cognitive Level: Application REF: 332 OBJ: 7 (theory) TOP: Signs of Anemia KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 14. The nurse is caring for a patient with pernicious anemia immediately following a bone marrow biopsy of the left posterior iliac crest. Which action should the nurse perform first? a. Inform the patient that he may feel pressure and sharp, brief pain. b. Check the pulses in the leg and foot distal to the puncture. c. Administer an ordered analgesic. d. Apply pressure to the site for 5 minutes with an ice pack. ANS: D The most immediate priority concern for this patient is bleeding. The nurse should apply pressure to the site to prevent a hematoma. The patient would feel pressure and sharp brief pain during the aspiration, not afterward. The nurse can assess pulses in the leg and foot, although this assessment would be most appropriate if the procedure involved an arterial stick. The nurse should administer the ordered analgesic after hemostasis is obtained. PTS: 1 DIF: Cognitive Level: Analysis REF: 335, Table 15-1 OBJ: 7 (clinical) TOP: Post-marrow Aspiration Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 15. The nurse is caring for a patient who is taking radiation treatments. The patient has a platelet count of 100,000/mm3 . Which action is most important for the nurse to add to the patient’s care plan? a. Instruct the patient to change positions slowly. b. Remove the clutter from the patient’s room. c. Remove the fresh orange from the patient’s meal tray. d. Limit the number of visitors in the room at a time. ANS: B This patient is thrombocytopenic (low platelet count) and is at an increased risk for bleeding. A cluttered room increases the risk for falls, and a fall could be particularly dangerous for this patient. Changing positions slowly is indicated in the patient with orthostatic hypotension. Removing the fresh orange from the patient’s tray and limiting visitors are infection control measures for the patient on neutropenic precautions. PTS: 1 DIF: Cognitive Level: Analysis REF: 331 OBJ: 2 (theory) TOP: Thrombocytopenia KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 16. What is the average life span of a platelet cell? a. 10 days b. 14 days c. 30 days d. 45 days ANS: A Platelets live only about 10 days. PTS: 1 DIF: Cognitive Level: Knowledge REF: 330 OBJ: 2 (theory) TOP: Platelets: Life Span KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 17. The nurse is caring for an older adult patient. A family member of the patient seems to frequently catch colds. Which response is best? a. “After the age of 60, the plasma volume decreases so there is less infection fighting ability.” b. “Bone marrow activity decreases by about 50% with aging, which lowers the immune response to infection.” c. “The older adult’s blood is more prone to clotting, so infection-fighting cells don’t get to the source of infection quickly.” d. “His antibody response to vaccines is overactive.” ANS: B The older adult patient is more prone to infection due to the decrease in bone marrow activity, which in turn reduces the immune response. Plasma volume does decrease after age of 60, but the concern is decreased blood reserve volume in case of blood loss, not infection. The older adult’s blood is more prone to clotting due to platelet aggregation and alterations in clotting activity; this increases the risk for problems related to thrombosis, not infection. Lastly, the older adult’s antibody response to vaccines is decreased. PTS: 1 DIF: Cognitive Level: Application REF: 330 OBJ: 3 (theory) TOP: Effects of Aging KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 18. Which statement about the hematologic system is accurate? a. “African Americans have the highest incidence of sickle cell disease.” b. “Iatrogenic blood disorders are congenital in origin.” c. “Folic acid is directly related to synthesis of hemoglobin.” d. “Bruising in the older adult patient is of great concern.” ANS: A African Americans do have the highest incidence of sickle cell disease. Iatrogenic blood disorders are brought on by medical treatment, such as bone marrow suppression. Iron, rather than folic acid, is directly related to hemoglobin synthesis; folic acid is related to RBC maturation. The older adult tends to bruise more due to the thinning of the skin and the increased fragility of the vessels; therefore, it is expected to see some bruising with these patients. Excessive bruising, however, in the older adult patient should be investigated. PTS: 1 DIF: Cognitive Level: Comprehension REF: 330, Cultural Considerations OBJ: 3 (theory) TOP: Hematologic System Characteristics KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation MULTIPLE RESPONSE 19. Which statement(s) describe functions of blood? (Select all that apply.) a. To absorb nutrients b. To transport blood gases c. To regulate pH by buffering d. To regulate fluid distribution e. To regulate body temperature ANS: B, C, D, E Blood transports blood gases, regulates pH through buffering, regulates fluid distribution, and regulates body temperature. Blood transports nutrients but does not absorb them. PTS: 1 DIF: Cognitive Level: Comprehension REF: 327 OBJ: 1 (theory) TOP: Blood: Function KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 20. Which organ(s) compose the lymphatic system? (Select all that apply.) a. Thymus b. Lymph nodes c. Kidneys d. Spleen e. Tonsils ANS: A, B, D The lymphatic system consists of the thymus gland, lymph nodes, lymph channels, the spleen, and the thymus gland (see Chapter 10). The tonsils and kidneys are not considered a part of the lymphatic system. PTS: 1 DIF: Cognitive Level: Knowledge REF: 330 OBJ: 2 (theory) TOP: Lymphatic System KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 21. Which age-related changes occur in the hematologic system? (Select all that apply.) a. Decreased blood volume b. Decreased bone marrow production c. Decreased rate of blood cell production d. Increased immune response e. Increased clotting time ANS: A, B, C, E Age-related changes of the hematologic system include decreasing blood volume, bone marrow production, and blood cell production rate, along with increasing clotting time. The immune response decreases with age. PTS: 1 DIF: Cognitive Level: Comprehension REF: 330 OBJ: 3 (theory) TOP: Blood: Age-Related Changes KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 22. Which assessment technique assures accuracy in daily abdominal girth measurement? (Select all that apply.) a. Place marks on the lateral sides of the abdomen where the tape is placed. b. Use the same tape every day. c. Measure girth with the tape placed 1 inch above the umbilicus. d. Measure the same area every day. e. Measure girth at the same time every day. ANS: A, B, D, E Place marks on the lateral aspects of the abdomen where the measuring tape is placed and measure at the umbilicus. Put the measuring tape in the same place each day at the same time. Girth is measured at the level of the umbilicus. PTS: 1 DIF: Cognitive Level: Comprehension REF: 336, Clinical Cues OBJ: 2 (clinical) TOP: Measurement of Girth KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 23. The nurse is assessing a patient with a dark complexion for cyanosis. To ensure the most accurate assessment, which locations should the nurse inspect? (Select all that apply.) a. Conjunctiva b. Gums c. Roof of the mouth d. Nail beds e. Palms of the hands ANS: B, C A person with a dark complexion can be assessed for cyanosis by examining the gums and the roof of the mouth. Cyanosis is not usually apparent in the conjunctiva or palms of the hands. The nail beds tend to be darker in dark-skinned individuals so this would not render an accurate assessment of cyanosis. PTS: 1 DIF: Cognitive Level: Application REF: 335, Focused Assessment OBJ: 2 (clinical) TOP: Assessment: Cyanosis KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 24. Which actions should the nurse take to help the severely anemic patient conserve energy? (Select all that apply.) a. Manage care to include frequent rest periods. b. Assist with activities of daily living (ADLs). c. Place personal care items close at hand. d. Arrange for small meals with between-meal snacks. e. Ensure that exercise sessions are planned during the morning. ANS: A, B, C, D Managing care and planning for rest, assisting with ADLs, placing personal care items nearby, and arranging for small meals are all actions that will spare the patient fatigue. Exercise sessions should not be implemented until the severe anemia improves. PTS: 1 DIF: Cognitive Level: Comprehension REF: 337, Table 15-2 OBJ: 3 (clinical) TOP: Fatigue KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort COMPLETION 25. The normal range of hemoglobin is from _____ g/dL to _____ g/dL. ANS: 12.0; 18.0 The normal range for hemoglobin is from 12.0 to 18.0 g/dL. PTS: 1 DIF: Cognitive Level: Knowledge REF: 328 OBJ: 2 (theory) TOP: Hgb: Normal Range KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 26. In making an assessment of a patient with a bleeding disorder who has a dark complexion, the nurse should check the palms of the hands and the soles of the feet for _____________. ANS: petechiae The small hemorrhages, petechiae, can be better assessed on people with a dark complexion by examining the palms of the hands and the soles of the feet. PTS: 1 DIF: Cognitive Level: Comprehension REF: 336 OBJ: 7 (theory) TOP: Assessment for Petechiae KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 27. A female patient being seen in an outpatient clinic states she is having excessive menstruation and reports saturating four peri-pads per day. The nurse estimates the blood loss for this patient as ______ mL per day. ANS: 200 The average amount of blood loss via menstruation is less than 80 mL. Each saturated pad or tampon is equal to about 50 mL of blood loss. Therefore, this patient is losing approximately 200 mL of blood per day. PTS: 1 DIF: Cognitive Level: Application REF: 331, Clinical Cues OBJ: 4 (theory) TOP: Menstruation Blood Loss KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential MATCHING The student nurse is drawing a diagram of the phases of the monocyte cell to present to the nursing class. The student correctly diagrams the phases in which order of occurrence? a. Becomes a phagocyte b. Becomes a macrophage c. Engulfs bacteria d. Migrates into tissues e. Becomes a monocyte f. Becomes a leukocyte 28. Step 1 29. Step 2 30. Step 3 31. Step 4 32. Step 5 33. Step 6 28. ANS: F PTS: 1 DIF: Cognitive Level: Analysis REF: 328-329 OBJ: 1 (theory) TOP: Monocyte Phases KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 29. ANS: E PTS: 1 DIF: Cognitive Level: Analysis REF: 328-329 OBJ: 1 (theory) TOP: Monocyte Phases KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 30. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 328-329 OBJ: 1 (theory) TOP: Monocyte Phases KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 31. ANS: D PTS: 1 DIF: Cognitive Level: Analysis REF: 328-329 OBJ: 1 (theory) TOP: Monocyte Phases KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 32. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 328-329 OBJ: 1 (theory) TOP: Monocyte Phases KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 33. ANS: C PTS: 1 DIF: Cognitive Level: Analysis REF: 328-329 OBJ: 1 (theory) TOP: Monocyte Phases KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance Chapter 16: Care of Patients with Hematologic Disorders deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is caring for a 79-year-old male who underwent a gastrectomy 1 month ago. The nurse recognizes that this patient is at the greatest risk for which type of anemia? a. Aplastic anemia b. Pernicious anemia c. Iron deficiency anemia d. Nutritional anemia ANS: B Pernicious anemia may result from the lack of the intrinsic factor found in the stomach lining. Without the intrinsic factor, the body is unable to absorb vitamin B12. Aplastic anemia is related to bone marrow suppression. Iron deficiency anemia is often related to a deficiency of iron in the diet. PTS: 1 DIF: Cognitive Level: Application REF: 345, Clinical Cues OBJ: 1 (theory) TOP: Pernicious Anemia: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. Iron deficiency anemia impacts adequate production of which component? a. Plasma b. White blood cells (WBCs) c. Hemoglobin d. Antibodies ANS: C Deficiency of iron causes reduced production of hemoglobin. PTS: 1 DIF: Cognitive Level: Comprehension REF: 345 OBJ: 1 (theory) TOP: Iron Deficiency Anemia KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. The nurse is caring for a patient with anemia who has a past medical history of diabetes, hypertension, chronic kidney disease, and acid reflux. The nurse is aware the patient’s anemia is likely related to which condition? a. Diabetes b. Hypertension c. Chronic kidney disease d. Acid reflux ANS: C The kidney makes most of the body’s erythropoietin stimulating factor, which then prompts the liver to release erythropoietin for erythrocyte production. Damaged kidneys produce decreased amounts of erythropoietin, which ultimately leads to decreased red blood cell production and anemia. Diabetes, hypertension, and acid reflux do not cause anemia. PTS: 1 DIF: Cognitive Level: Application REF: 344 OBJ: 1 (theory) TOP: Causes of Anemia KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. Which descriptions accurately characterize the appearance of red blood cells (RBCs) in iron deficiency anemia? a. Normochromic and normocytic b. Hypochromic and microcytic c. Hyperchromic and macrocytic d. Normochromic and microcytic ANS: B Iron deficiency anemia causes the RBCs to be smaller (microcytic) and have less color (hypochromic). PTS: 1 DIF: Cognitive Level: Comprehension REF: 345 OBJ: 1 (theory) TOP: Characteristics of RBCs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. The home health nurse is caring for a patient who is taking ferrous sulfate (Feosol). Which statement indicates that the patient requires additional teaching about this medication? a. “It tastes better when I take my medicine with milk.” b. “My wife says I should take my medicine with orange juice.” c. “I am always careful not to break open the capsule.” d. “I usually take my iron with my whole-grain toast during breakfast.” ANS: A Milk products inhibit the absorption of iron. Iron is better absorbed if vitamin C is in the gastrointestinal tract at the same time, so drinking orange juice with the ferrous sulfate is beneficial. Capsules and enteric-coated iron preparations should not be opened or crushed. Whole grains are not known as inhibitors of iron absorption. PTS: 1 DIF: Cognitive Level: Application REF: 347, Table 16-3 OBJ: 2 (clinical) TOP: Anemia Treatment: Feosol KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 6. The student nurse is preparing to administer an iron preparation via the intramuscular (IM) route. Which action indicates the need for further instruction? a. The student changes needles after drawing up the medication. b. The student administers 3 mL at the ventrogluteal site. c. The student chooses a 20-gauge needle. d. The student uses the Z-track technique when administering the injection. ANS: B Such intramuscular (IM) injections must not exceed 2 mL at each site, and the sites of injection should be rotated to allow for proper absorption and to minimize the hazards of local inflammation. When administering an IM iron preparation, it is important to change the needle after drawing up the medication and use a 19- to 20-gauge, 3-inch needle for injection since iron is irritating to the tissues. The Z-track technique for IM injection is recommended. PTS: 1 DIF: Cognitive Level: Application REF: 347, Table 16-3 OBJ: 2 (clinical) TOP: Absorption of Iron KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 7. The nurse is caring for a patient with aplastic anemia. Which actions are most important for the nurse to take? a. Alternate activity with periods of rest and provide magazines. b. Provide a soft toothbrush and decrease clutter in the room. c. Request an order for telemetry and limit intake of potassium-rich foods. d. Encourage the patient to reposition regularly and float heels on pillows. ANS: B Aplastic anemia can cause bleeding episodes. Priority nursing actions are directed toward preventing the episodes. Providing a soft toothbrush and decreasing clutter in the room are interventions to reduce risk of bleeding. While aplastic anemia can cause fatigue, and limiting activity and providing nontaxing entertainment can help, fatigue is a lesser priority than decreasing risk for bleeding. Requesting an order for telemetry and limiting intake of potassium-rich foods are indicated when monitoring highpotassium levels (which are not typical of aplastic anemia). Repositioning and floating heels are interventions helpful in preventing skin breakdown. PTS: 1 DIF: Cognitive Level: Analysis REF: 349 OBJ: 1 (theory) TOP: Aplastic Anemia: Infection KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 8. The nurse is caring for a 20-year-old female patient with sickle cell trait. Which statement accurately reflects this patient’s condition? a. The condition will evolve into sickle cell anemia as she ages. b. All of her children will have sickle cell anemia. c. The trait will be transmitted to male children only. d. The trait can be passed on to all children. ANS: D A person who has the trait can pass it on to male or female children, even if there are no symptoms. Fifty percent of the patient’s total hemoglobin may be affected. Age does not increase the chance of the trait evolving into the disease. PTS: 1 DIF: Cognitive Level: Comprehension REF: 350 OBJ: 3 (theory) TOP: Sickle Cell Trait KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 9. The nurse is caring for a patient with sickle cell anemia. Which intervention may best help prevent sickle cell crisis? a. Taking iron supplements daily b. Maintaining adequate fluid intake c. Engaging in daily exercise d. Eating leafy green vegetables ANS: B The maintenance of an adequate fluid intake keeps the circulating blood volume hydrated, which discourages clumping of the sickle cells. PTS: 1 DIF: Cognitive Level: Comprehension REF: 351 OBJ: 3 (theory) TOP: Sickle Cell Crisis: Prevention KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 10. The nurse is caring for a patient with sickle cell anemia. Based on the underlying pathophysiology of this disorder, the nurse should carefully perform which detailed assessment? a. Examination for skin breakdown b. Auscultation of lungs c. Abdominal girth measurement d. Palpation of radial pulses ANS: A Sickle cell anemia results in sluggish blood flow which increases the threat of stasis ulcers and makes it harder for existing wounds to heal. Careful assessment for skin breakdown is of priority importance in this patient. Lung auscultation, assessment of abdominal girth, and palpation of radial pulses do not directly correlate to sickle cell anemia. PTS: 1 DIF: Cognitive Level: Application REF: 352, Figure 16-3 OBJ: 3 (theory) TOP: Sickle Cell Anemia: Stasis Ulcers KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 11. The nurse is caring for a patient with sickle cell anemia. Which statement indicates that the patient requires further instruction? a. “I should not drink iced drinks.” b. “I miss drinking beer in the afternoon.” c. “I walk every day rather than doing other strenuous exercise.” d. “I am planning a trip to Colorado next month.” ANS: D People with sickle cell anemia should avoid cold temperatures and high altitudes, which can bring on a crisis due to thickening of the blood. Avoidance of iced drinks, alcohol, and strenuous exercise is beneficial. PTS: 1 DIF: Cognitive Level: Analysis REF: 351 OBJ: 3 (theory) TOP: Sickle Cell Anemia: Lifestyle Changes KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 12. The nurse is assessing a patient with polycythemia vera. Which finding is consistent with this disorder? a. Pallor b. Blood pressure (BP) of 100/60 c. Hemoglobin of 17 mg/dL d. Agitation ANS: C A patient with polycythemia vera will have high hemoglobin and hematocrit related to the large number of RBCs. The complexion is ruddy with blue lips; there is fatigue and weakness and high BP. PTS: 1 DIF: Cognitive Level: Application REF: 351 OBJ: 4 (theory) TOP: Polycythemia Vera: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 13. How often should a patient with polycythemia vera have phlebotomy to thin the blood? a. Every 2 to 3 weeks b. Monthly c. Every 2 to 3 months d. Semiannually ANS: C The phlebotomies are scheduled about every 2 to 3 months in order to thin the blood to reduce hypertension and threat of stroke. PTS: 1 DIF: Cognitive Level: Knowledge REF: 352 OBJ: 4 (theory) TOP: Polycythemia Vera: Treatment KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 14. The home health nurse is caring for a patient with polycythemia vera. Which focus is most important for the nurse to emphasize? a. Maintenance of high fluid intake b. Daily exercise to reduce weight c. Daily dose of anticoagulants d. Adequate intake of vitamin C ANS: A The major focus is maintaining a high fluid intake to keep the circulating fluid well hydrated. PTS: 1 DIF: Cognitive Level: Application REF: 352 OBJ: 4 (theory) TOP: Polycythemia Vera: Home Care KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 15. The patient with acute myelogenous leukemia (AML) asks why he is making more WBCs when he already has so many. Which statement clarifies the underlying pathophysiology related to the patient’s white blood cells (WBCs)? a. “The large number of leukemic white cells that you already have are not as effective as normal white cells.” b. “The large number of leukemic white cells that you already have protect against infection.” c. “The large number of leukemic white cells that you already have attempt to take over the functions of RBCs. d. “The large number of leukemic white cells that you already have are produced by the lymphatic system.” ANS: A The many leukemic white cells cannot function as normal WBCs do. The bone marrow “rushes” production of immature white cells (blasts) to try to create adequate protection. These cells do not protect against infection, nor do they take over the functions of the RBCs. AML originates in the bone marrow. PTS: 1 DIF: Cognitive Level: Application REF: 353, Table 16-5 OBJ: 5 (theory) TOP: AML: WBC Production KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 16. Which statement accurately describes induction therapy for acute lymphocytic leukemia (ALL)? a. Induction therapy is an intensive protocol of chemotherapy in high doses to achieve remission. b. Induction therapy is a long-term protocol with smaller doses of chemotherapy to achieve a cure. c. Induction therapy is a 2- to 5-year low-dose chemotherapy regimen to reduce painful symptoms. d. Induction therapy is a combination of chemotherapy and radiation to achieve remission. ANS: A A combination of several antileukemic drugs in high doses has been found to induce a remission. PTS: 1 DIF: Cognitive Level: Knowledge REF: 353 OBJ: 5 (theory) TOP: ALL: Treatment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 17. When caring for a patient with advanced multiple myeloma, the nursing staff must exercise extreme care to prevent which complication? a. Pain b. Hematomas c. Muscle spasms d. Pathologic fractures ANS: D Pathologic fractures of osteoporotic bones are an ongoing concern in the patient with multiple myeloma. PTS: 1 DIF: Cognitive Level: Comprehension REF: 357 OBJ: 1 (clinical) TOP: Multiple Myeloma: Safety KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 18. Blood infusions must be started within how many minutes of its arrival on the unit? a. 10 minutes b. 15 minutes c. 30 minutes d. 60 minutes ANS: C To reduce the risk of infection, the blood must be started within 30 minutes of its arrival on the unit. PTS: 1 DIF: Cognitive Level: Knowledge REF: 361 OBJ: 2 (theory) TOP: Transfusion: Starting Blood KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies MULTIPLE RESPONSE 19. A patient with a nutritional anemia may lack which nutrients? (Select all that apply.) a. Proteins b. Vitamin B1 c. Folic acid d. Zinc e. Iron ANS: A, C, E Nutritional anemia occurs due to the lack of proteins, folic acid, and iron. Deficiencies in vitamin B1 and zinc do not result in anemia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 344 OBJ: 1 (theory) TOP: Nutritional Anemia: Etiology KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 20. The nurse makes a visual aid differentiating between mild, moderate, and severe anemia. Which signs and symptoms are manifestations of mild anemia? (Select all that apply.) a. Hemoglobin of 14.4 g/dL b. Palpitations c. Dyspnea on exertion d. Pallor e. Fatigue ANS: B, C Palpitations and dyspnea on exertion are manifestations of mild anemia. Mild anemia is characterized by hemoglobin below 14 g/dL and does not result in pallor or abnormal levels of fatigue. PTS: 1 DIF: Cognitive Level: Comprehension REF: 345 OBJ: 1 (theory) TOP: Mild Anemia: Signs and Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 21. The nurse is caring for patient with iron deficiency anemia. The nurse should encourage intake of which food(s)? (Select all that apply.) a. Liver b. Lima beans c. Prune juice d. Cabbage e. Dried apricots ANS: A, B, C, E Iron-rich foods that can boost dietary iron intake include liver, lima beans, prune juice, and dried apricots. Cabbage is not high in iron. PTS: 1 DIF: Cognitive Level: Application REF: 364, Nutrition Considerations OBJ: 2 (theory) TOP: Iron Deficiency Anemia: Diet KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 22. Which medication(s) may cause aplastic anemia? (Select all that apply.) a. Antimetabolite cancer drugs b. Phenylbutazone (Butazolidin) c. Oral contraception drugs d. Chloramphenicol (Chloromycetin) e. Sulfonamides ANS: A, B, D, E Antimetabolite cancer drugs, phenylbutazone (Butazolidin), chloramphenicol (Chloromycetin), and sulfonamides may cause aplastic anemia. Oral contraceptives are not known to cause aplastic anemia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 349 OBJ: 1 (theory) TOP: Aplastic Anemia: Etiology KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 23. Which factor(s) may be causative for leukemia? (Select all that apply.) a. Radiation exposure b. Pesticides exposure c. Benzene exposure d. Frequent bacterial infections e. Virulent viral infections ANS: A, B, C Exposure to radiation, pesticides, and benzenes has been linked to potential causes of leukemia. Bacterial and viral infections are not considered to be causes of leukemia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 352 OBJ: 5 (theory) TOP: Leukemia: Etiology KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 24. The patient with AML has a platelet count of 95,000. What interventions should the nurse include in the patient’s care plan? (Select all that apply.) a. Observe for melena and hematuria. b. Instruct the patient to brush and floss at least twice daily. c. Measure abdominal girth daily. d. Apply ice and pressure to puncture sites. e. Instruct the patient to use an electric razor. ANS: A, C, D, E A low platelet makes the patient prone to excessive bleeding. The nurse should monitor for bleeding into the stool and urine. An increase in the abdominal girth will alert the nurse to the possibility of internal bleeding. Ice and pressure on puncture sites aid in stopping bleeding. An electric razor reduces the chance of the patient being cut during shaving. Soft toothbrushes will decrease the likelihood of the gums bleeding, and the patient should not floss too frequently or brush teeth aggressively. PTS: 1 DIF: Cognitive Level: Application REF: 355, Nursing Care Plan 16-1 OBJ: 5 (theory) TOP: Thrombocytopenic Precautions KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 25. The nurse is monitoring a patient who is receiving a blood transfusion. Which finding(s) would lead the nurse to stop the infusion? (Select all that apply.) a. Report of chills b. Headache c. Back pain d. Report of a rash e. Fever ANS: B, C, D, E Headache, back pain, rash, and fever are findings that indicate a reaction to the transfusion; the transfusion should be stopped. The nurse should then infuse saline solution into the line to keep the intravenous line patent. Report of chills correlates to the infusion of the chilled blood. The transfusion is not stopped; the patient is given a blanket. PTS: 1 DIF: Cognitive Level: Application REF: 362, Table 16-7 OBJ: 7 (theory) TOP: Transfusion: Complications KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential COMPLETION 26. The nurse is aware that bone marrow transplantation (BMT) is a treatment alternative for aplastic anemia for people under the age of ____________________. ANS: 45 forty-five People under the age of 45 are considered candidates for BMT. PTS: 1 DIF: Cognitive Level: Comprehension REF: 350 OBJ: 1 (clinical) TOP: Aplastic Anemia: Treatment KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 27. When assessing a complete blood count (CBC) of a patient with acute lymphocytic leukemia (ALL), the nurse would anticipate large numbers of immature white cells, called ____________________. ANS: blasts Immature white cells are released from the bone marrow in response to the body’s need for more effective WBCs. Immature WBCs are known as blasts. PTS: 1 DIF: Cognitive Level: Comprehension REF: 353 OBJ: 5 (theory) TOP: ALL: CBC KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 28. The patient with acute myelogenous leukemia (AML) has a volume of blood extracted by machine, white cells are extracted in the machine, and the blood is then returned to the patient. This process is called ____________________. ANS: leukapheresis Leukapheresis is a process by which blood is withdrawn from the patient by an extractor machine, the excess diseased WBCs are extracted, and the blood is returned to the patient. PTS: 1 DIF: Cognitive Level: Comprehension REF: 354 OBJ: 5 (theory) TOP: Leukapheresis KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 29. The nurse explains to a person who has undergone bone marrow transplantation (BMT) that engraftment takes up to ____________________ weeks. ANS: 5 five Engraftment takes from 2 to 5 weeks to begin to make stem cells. PTS: 1 DIF: Cognitive Level: Comprehension REF: 363 OBJ: 2 (clinical) TOP: BMT: Engraftment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation Chapter 17: The Cardiovascular System deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is educating a female patient with a family history of coronary artery disease (CAD) about risk factors and prevention of heart disease in women. Which information is most important for the nurse to include? a. Women should maintain a body mass index (BMI) of less than 28. b. Women should utilize estrogen supplementation to decrease risk of heart disease. c. Women should drink one alcoholic beverage daily. d. Women should incorporate stress reduction techniques into their daily lifestyle. ANS: D Increased stress is a risk factor for cardiovascular disease, especially in women. Women should incorporate stress reduction techniques into their daily lifestyle. Women should maintain a BMI of less than 25. Women should discontinue use of estrogen contraception/supplementation as soon as possible. Women should not consume more than one alcoholic drink per day, and abstaining from alcohol is beneficial. PTS: 1 DIF: Cognitive Level: Comprehension REF: 372-373 OBJ: 2 (theory) TOP: Heart Disease in Women KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 2. In a blood pressure of 120/80, what does the “80” indicate? a. Pulse pressure b. Pressure in the relaxed ventricles c. Relative ejection factor d. Stroke volume ANS: B The diastolic pressure of 80 mm Hg is the reading of the pressure during ventricular relaxation. PTS: 1 DIF: Cognitive Level: Knowledge REF: 371 OBJ: 1 (theory) TOP: Diastolic Pressure: Definition KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. The nurse is caring for a patient on lisinopril (Zestril). The patient asks how this medication affects blood pressure. Which response best explains the medication’s effects? a. “This medication blocks epinephrine and lowers the heart rate, which impacts blood pressure.” b. “This medication stimulates the release of sodium and water to be excreted.” c. “This medication lowers blood pressure by blocking an enzyme that causes blood vessels to constrict.” d. “This medication decreases cardiac output.” ANS: C Angiotensin-converting-enzyme (ACE) inhibitors are antihypertensive medications, or medications that lower blood pressure. ACE-inhibitors block angiotensin I from converting to angiotensin II and cause vasoconstriction. This action prevents blood pressure from increasing. PTS: 1 DIF: Cognitive Level: Comprehension REF: 371 OBJ: 1 (theory) TOP: Angiotensin: Effect on Circulatory System KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. The 85-year-old patient with a newly diagnosed heart murmur expresses concern that he has never been notified of this finding before. What is the most likely cause of this patient’s heart murmur? a. Hypertension b. Atherosclerosis c. Insufficient valves d. Weakened pacemaker ANS: C Systolic murmurs commonly appear in people over the age of 80. These murmurs are usually related to valvular dysfunction caused by thickening of the valves, especially the mitral and aortic valves. PTS: 1 DIF: Cognitive Level: Application REF: 372 OBJ: 2 (theory) TOP: Murmur in the Older Adult KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 5. The nurse is caring for an older adult patient. While auscultating the patient’s apical pulse, the nurse notices an irregular rhythm. The nurse suspects which causative factor for the patient’s dysrhythmia? a. Loss of cells in the sinoatrial (SA) nodes b. Increased peripheral resistance c. Hypertension d. Atherosclerosis ANS: A Loss of cells in the SA nodes via age-related changes is the most common cause of dysrhythmias in the older adult. This nurse should, however, document these findings and report the findings to the primary care provider. PTS: 1 DIF: Cognitive Level: Application REF: 372 OBJ: 2 (clinical) TOP: Dysrhythmia in the Older Adult KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 6. The nurse is assessing a female patient with a family history of coronary artery disease (CAD). Which report is most concerning to the nurse? a. “I get a little short of breath after climbing the three flights of stairs to my apartment.” b. “I stay tired all of the time, and it feels like my bra is too tight.” c. “I awaken frequently in the night, and my husband says that I snore.” d. “I notice wheezing after I dust or when I exercise.” ANS: B In addition to displaying a positive family history for CAD, report of fatigue and shoulder and back discomfort are most concerning to the nurse. Chest pain is often atypical in women and may manifest as pain in the shoulders, back, or abdomen. Mild shortness of breath after climbing three flights of stairs is consistent with exertion. Awakening frequently in the night and snoring are suspicious for obstructive sleep apnea. Wheezing in the presence of dust or with exercise are findings consistent with potential asthma. PTS: 1 DIF: Cognitive Level: Analysis REF: 374 OBJ: 9 TOP: Chest Pain in Women KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 7. The nurse is outlining a teaching program for diabetic patients. Which teaching point about heart disease prevention should the nurse emphasize most? a. Keep blood sugar below 100 mg/dL. b. Prevent infections. c. Eat meals at regular times. d. Use sterile technique in insulin injections. ANS: A The diabetic person who maintains the glucose level below 100 mg/dL will avoid the adverse effects of hyperglycemia on the vessels. Preventing infections, eating at regular times, and using sterile technique are all valid teaching points for the diabetic patient, but they do not specifically address prevention of heart disease. PTS: 1 DIF: Cognitive Level: Analysis REF: 373, Health Promotion, 374, Table 17-1 OBJ: 4 (theory) TOP: Prevention of Heart Disease: Diabetics KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 8. Which statement accurately describes the purpose of a Doppler flow study? a. To detect a clot in a coronary artery b. To visualize obstructions in leg vessels c. To assess efficiency of blood flow through heart chambers d. To detect a defective heart valve ANS: B The Doppler flow study detects obstructions in the vessels of the lower extremities. The Doppler study may also be performed in other areas of the body, such as the carotid arteries. PTS: 1 DIF: Cognitive Level: Comprehension REF: 377, Table 17-2 OBJ: 5 (theory) TOP: Doppler Flow Study KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 9. The nurse is caring for a patient who just returned from a transradial heart catheterization. Which action indicates the priority care for the postprocedure period? a. The nurse encourages the patient to increase fluid intake. b. The nurse checks the presence and strength of pedal pulses. c. The nurse places the pulse oximeter on the thumb or first digit of the affected hand. d. The nurse places the blood pressure cuff on the arm corresponding to the affected hand. ANS: C Priority postprocedure care involves carefully monitoring circulation checks to ensure adequate blood flow to the affected hand while maintaining adequate compression on the radial artery to prevent bleeding. The patient will return with a compression band over the radial puncture site. By placing the pulse oximetry probe on the thumb or first digit of the affected hand, the nurse can obtain a pulse oximetry reading that is specific to the radial artery. The nurse can compare this value to the patient’s baseline and ensure that the circulation is adequate. Increasing fluid intake helps flush dye out of the patient’s system, but it is a lesser priority than adequate perfusion and hemostasis. Presence and strength of pedal pulses are a priority assessment for a transfemoral heart cauterization. The nurse should avoid placing the blood pressure cuff on the same arm as the catheterization site because cuff inflation could induce bleeding or compromise circulation at the site. PTS: 1 DIF: Cognitive Level: Analysis REF: 379, Table 17-2 OBJ: 5 (theory) TOP: Transradial Heart Catheterization: Postprocedure Care KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 10. The nurse is caring for a patient who is scheduled to undergo a stress echocardiogram. Which statement indicates that the nurse’s teaching about preparation for the test has been successful? a. “I should eat a full meal to give me energy to walk on the treadmill.” b. “I will avoid smoking for fours before the test.” c. “I will have to move extremely quickly from the treadmill to the table.” d. “I should wear comfortable house shoes during the test.” ANS: C A stress echocardiogram combines exercise on a treadmill with an ultrasound (echocardiogram). Once an optimal heart rate is achieved, the patient must transfer extremely quickly from the treadmill to the table to ensure quality imaging. Patients should avoid eating a heavy meal, avoid smoking for 6 to 8 hours prior to the test, and wear comfortable walking shoes. House shoes are not appropriate footwear for treadmill exercise. PTS: 1 DIF: Cognitive Level: Application REF: 377, Table 17-2 OBJ: 5 (theory) TOP: Stress Echocardiogram: Preparation KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 11. The 65-year-old patient complains of leg pain that disappears at rest after having walked a short distance. The nurse recognizes that the patient’s symptoms are consistent with which problem? a. Muscle spasm b. Deep venous thrombosis c. Claudication d. Angiospasm ANS: C Intermittent claudication, or cramping pain in the calves, occurs in the presence of arterial insufficiency. This allows the muscles to build up lactic acid and cause pain. PTS: 1 DIF: Cognitive Level: Knowledge REF: 382 OBJ: 5 (theory) TOP: Claudication: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 12. While performing a focused cardiac assessment, the nurse auscultates an abnormal swooshing sound. Which action is most appropriate to clarify the nurse’s finding? a. The nurse uses the diaphragm of the stethoscope while asking the patient to take a deep breath. b. The nurse uses the bell of the stethoscope while asking the patient to lean forward. c. The nurse asks the patient about a history of heart stents. d. The nurse asks the patient about a history of cardiac dysrhythmias. ANS: B Heart murmurs usually generate a swooshing sound that results from turbulent blood flow (usually through damaged valves). The nurse should use the bell of the stethoscope and place it lightly on the skin. Leaning the patient forward may amplify or clarify the sound. Asking the patient about heart stents and abnormal heart rhythms does not clarify the presence or history of a heart murmur. PTS: 1 DIF: Cognitive Level: Application REF: 384 OBJ: 5 (theory) TOP: Auscultating for Murmur KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 13. When using a 0 to 4+ scale to grade pulse quality, how should the nurse record a normal volume pulse? a. 1+ b. 2+ c. 3+ d. 4+ ANS: C A 0 to 4+ scale for grading pulse quality is as follows: 0—Absent, +1—Weak, thready, +2—Light volume, +3—Normal volume, and +4—Full, bounding. The nurse should be aware of the type of scale used in different facilities. PTS: 1 DIF: Cognitive Level: Knowledge REF: 385, Box 17-2 OBJ: 5 (theory) TOP: Recording Pulse Quality KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 14. The nurse is caring for a patient with a blood pressure of 140/90, an apical pulse of 82, and a radial pulse of 76. Which value indicates that the nurse accurately calculated the patient’s pulse pressure? a. 6 b. 50 c. 82 d. 90 ANS: B The pulse pressure is the difference between the systolic and diastolic pressures (140-90 = 50). Pulse deficit is the difference between the radial and the brachial pulses. PTS: 1 DIF: Cognitive Level: Application REF: 371 OBJ: 5 (theory) TOP: Pulse Pressure KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 15. The nurse is caring for a 50-year-old patient who complains of tingling in his toes. Which other assessment finding would cause the nurse to suspect arterial insufficiency? a. Equal warmth in bilateral feet b. Shiny, hairless legs c. Thin, brittle toenails d. Pedal edema ANS: B To distinguish arterial insufficiency, instruct the patient to dangle the feet. In arterial insufficiency, feet display delayed color return, and if severe peripheral arterial disease is present, the dangling feet soon take on a dusky red color (rubor). The skin may be shiny, taunt, and hairless. Equal warmth indicates equal and sufficient blood flow to the extremities. The nails would be thick rather than thin with arterial insufficiency, and pedal edema is an indication of venous insufficiency. PTS: 1 DIF: Cognitive Level: Application REF: 386 OBJ: 5 (theory) TOP: Arterial Insufficiency: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 16. The nurse is caring for a patient with a history of hypertension. Which information is most important for the nurse to obtain? a. “Do you take a daily multivitamin?” b. “Do you use over-the-counter decongestants or diet pills?” c. “How often do you use laxatives?” d. “How often do you use antacids?” ANS: B Many over-the-counter (OTC) drugs can cause vasoconstriction and elevate blood pressure. Cold remedies, decongestants, and diet pills are particularly noted for having this effect. Patients sometimes do not consider OTC items as medications and do not report their use. PTS: 1 DIF: Cognitive Level: Comprehension REF: 382 OBJ: 5 (theory) TOP: Assessing for Causes of Hypertension KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 17. The patient asks if it is harmful for him to drink a glass of wine with dinner on a daily basis. Which is the nurse’s best response? a. “As long as it is okay with your physician, moderate alcohol intake can be beneficial to your cardiovascular health.” b. “Drinking wine on a daily basis may lead to you having issues with increased blood pressure.” c. “You may want to be careful because drinking wine with dinner may stimulate your appetite significantly.” d. “This practice may cause your triglyceride level to rise, so I would discourage it.” ANS: A Alcohol is a mild vasodilator when consumed in moderate amounts, which can be beneficial to heart health, depending on the patient’s condition. PTS: 1 DIF: Cognitive Level: Application REF: 393 OBJ: 2 (clinical) TOP: Vasodilation with Alcohol KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 18. Which layer of the heart contains muscle fibers that contract to pump blood? a. Myocardium b. Endocardium c. Epicardium d. Pericardium ANS: A The myocardium is the middle layer of muscle fibers of the heart that contract to pump blood. The endocardium is the lining of the inner surface of the heart chambers, the epicardium is the outer layer of the heart muscle, and the pericardium is the membranous sac that surrounds the heart. PTS: 1 DIF: Cognitive Level: Knowledge REF: 368 OBJ: 1 (theory) TOP: Structures of the Heart KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 19. The nurse is teaching a patient about the purpose of his telemetry. Which statement indicates that the nurse’s teaching has been successful? a. “I will need to stay in bed when the monitor is reading my heart waves.” b. “This test will help determine if I have a blockage in my arteries.” c. “If there is a problem with my heart valves, it will show up with telemetry.” d. “The nurses will be able to monitor my heart rate and rhythm.” ANS: D Telemetry provides monitoring of the heart’s rate and rhythm with the use of electrodes and wire leads from a bedside monitor or battery-operated transmitter unit. Patients may ambulate on the unit and still be monitored. Blockage of arteries is usually diagnosed with an arteriogram, and valvular problems may be diagnosed with echocardiography. PTS: 1 DIF: Cognitive Level: Application REF: 375 OBJ: 5 (theory) TOP: Diagnostic Tests and Procedures KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance MULTIPLE RESPONSE 20. Which preventative measure(s) may protect against development of cardiovascular disease? (Select all that apply.) a. Exercising regularly for at least 30 minutes a day b. Maintaining high-density lipoprotein (HDL) greater than 50 mg/dL c. Refraining from smoking d. Obtaining and maintaining a healthy weight e. Maintaining triglycerides above 150 mg/dL ANS: A, B, C, D Behaviors that may help to prevent CAD include: exercising regularly for at least 30 minutes a day, maintaining HDL greater than 50 mg/dL, refraining from smoking, and obtaining and maintaining a healthy weight. Triglycerides should be maintained below 150 mg/dL. PTS: 1 DIF: Cognitive Level: Comprehension REF: 373, Health Promotion OBJ: 4 (theory) TOP: Behaviors Preventing Cardiovascular Disease KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 21. Which factors may affect the volume of cardiac output? (Select all that apply.) a. Heart rate b. Peripheral pulses c. Preload d. Contraction strength e. Afterload ANS: A, C, D, E The amount of cardiac output depends on the heart rate, the amount of blood returning to the heart (venous return or preload), the strength of contraction, and the resistance to the ejection of the blood (afterload). Peripheral pulses are dependent on cardiac output. PTS: 1 DIF: Cognitive Level: Knowledge REF: 370 OBJ: 1 (theory) TOP: Cardiac Output KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 22. Which modifiable risk factors increase a patient’s risk for heart disease? (Select all that apply.) a. Smoking b. Race c. Obesity d. Sedentary lifestyle e. Age ANS: A, C, D Smoking, obesity, and sedentary lifestyle are modifiable risk factors that increase risk of CAD. Race and age are nonmodifiable risk factors for heart disease. PTS: 1 DIF: Cognitive Level: Comprehension REF: 374, Table 17-1 OBJ: 2 (theory) TOP: Modifiable Risks KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 23. Which disorder(s) is/are examples of congenital heart defects? (Select all that apply.) a. Arteriosclerosis b. Coarctation of the aorta c. Septal defects d. Valvular defects e. Atherosclerosis ANS: B, C, D Causes of cardiovascular disorders can be congenital or acquired. Narrowing of the aorta (coarctation), septal defects, or abnormal cardiac valve formation can occur congenitally. Acquired defects include narrowing or hardening of the blood vessels from arteriosclerosis (thickening and loss of elasticity) or atherosclerosis and aneurysms of the large vessels. PTS: 1 DIF: Cognitive Level: Knowledge REF: 373 OBJ: 1 (theory) TOP: Disorders of the Heart KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance COMPLETION 24. The nurse assessing the heart places the stethoscope between the fifth and sixth ribs at the mid-clavicular line to hear the point of _________. ANS: maximal impulse The placement of the stethoscope will allow the loudest beat at the point of maximal impulse (PMI). PTS: 1 DIF: Cognitive Level: Application REF: 369 OBJ: 1 (clinical) TOP: Auscultating the PMI KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 25. When the nurse uses the PQRST tool for pain assessment, the “R” prompts an inquiry about the __________ of the pain. ANS: radiation The tool prompts inquiries about Precipitating events, Quality of pain, Radiation of the pain, Severity of the pain, and Timing of the pain. PTS: 1 DIF: Cognitive Level: Comprehension REF: 383, Table 17-3 OBJ: 5 (theory) TOP: PQRST Assessment Tool KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 26. The nurse who uses a regular sized adult blood pressure cuff on a large adult will get a blood pressure reading that is falsely __________. ANS: elevated high The small cuff compresses the artery in a narrow local area and causes a greater compression than a cuff that is better suited. The result is a falsely high reading. PTS: 1 DIF: Cognitive Level: Comprehension REF: 385 OBJ: 5 (theory) TOP: Blood Pressure: False High KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 27. _________ is the acute symptom most experienced by African Americans when having a myocardial infarction (MI). ANS: Dyspnea Dyspnea is the most common symptom experienced by African Americans during an acute MI rather than the classic MI symptoms. This often causes the African American patient to delay seeking treatment. PTS: 1 DIF: Cognitive Level: Application REF: 383, Cultural Considerations OBJ: 5 (theory) TOP: Cultural Considerations KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential Chapter 18: Care of Patients with Hypertension and Peripheral Vascular Disease deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. Which blood pressure findings constitute a diagnosis of hypertension? a. 120/80 × 2, 2 weeks apart b. 140/90 × 2, 2 weeks apart c. 120/80 on 3 consecutive days d. 140/90 every day for a week ANS: B A diagnosis of hypertension is made if the systolic pressure is equal to or greater than 140 mm Hg and the diastolic pressure is equal to or greater than 90 mm Hg at least twice on two different occasions 2 weeks apart. PTS: 1 DIF: Cognitive Level: Comprehension REF: 396 OBJ: 10 (theory) TOP: Hypertension: Diagnosis KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 2. The nurse is educating an older adult patient who is taking antihypertensives with diuretics. Which information regarding safety precautions is most important for the nurse to include? a. Consider purchasing a home blood pressure monitor. b. Limit sodium intake in the diet. c. Sit on the side of the bed before standing. d. Keep an updated list of all medications. ANS: C Age-related changes (reduced baroreceptor sensitivity) and risk for fluid shifts related to diuretics predispose the older adult patient to orthostatic hypotension. In order to prevent falls, the patient should change positions slowly and cautiously, like taking time to sit on the edge of the bed before standing. While purchasing a home blood pressure monitor, limiting sodium in the diet, and keeping an updated list of medications may assist with management of hypertension, fall prevention and safety are most important for the older adult patient. PTS: 1 DIF: Cognitive Level: Analysis REF: 398, Older Adult Care Points OBJ: 5 (clinical) TOP: Orthostatic Hypotension KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 3. The home health nurse is caring for a patient with a blood pressure reading of 200/160. The patient denies any discomfort. The nurse should immediately contact the health care provider to report that the patient is experiencing which problem? a. Primary hypertension b. Hypertensive crisis c. Essential hypertension d. Secondary hypertension ANS: B The diastolic pressure rising to readings between 140 and 170 and the patient being asymptomatic indicates hypertensive crisis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 402 OBJ: 3 (theory) TOP: Malignant Hypertension KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. The nurse is caring for a patient who has a new prescription for a loop diuretic. Which nutritional intervention is most important for the nurse to add to the care plan? a. Increase intake of leafy green vegetables. b. Increase intake of bananas and potatoes. c. Avoid foods like canned soups and hot dogs. d. Limit caffeine intake. ANS: B Loop diuretics are potent, potassium-wasting diuretics. After talking with the health care provider, the patient should recommend that the patient increase intake of potassium-rich foods like bananas and potatoes to offset potassium depletion from the diuretic. Leafy green vegetables are rich in vitamin K and may increase clotting times. Sodium-rich foods like canned soups and hot dogs should be avoided to prevent excess water retention, but this intervention does not address the risk for potassium depletion with loop diuretics. Caffeine is a stimulant that causes vasoconstriction and may increase blood pressure. While avoiding caffeine may improve blood pressure, this intervention does not address the risk of potassium depletion with a loop diuretic. PTS: 1 DIF: Cognitive Level: Analysis REF: 403 OBJ: 3 (theory) TOP: Loop Diuretics KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 5. The patient has been prescribed a low-sodium diet. Which food choice indicates that the patient requires additional teaching? a. Fresh spinach b. Pickles c. Whole-grain pasta d. Grapefruit ANS: B High-sodium foods include pickled vegetables, canned soups, and processed meats. Fresh spinach, whole-grain pasta, and grapefruit are appropriate low-sodium choices. PTS: 1 DIF: Cognitive Level: Application REF: 403, Nutrition Considerations OBJ: 3 (theory) TOP: Low-Sodium Diet KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 6. Which medication is the most common and effective antiplatelet aggregation agent? a. Warfarin b. Aspirin c. Alteplase (Activase) d. Reteplase (Retavase) ANS: B Aspirin is the most common and effective antiplatelet agent. PTS: 1 DIF: Cognitive Level: Knowledge REF: 407 OBJ: 9 (theory) TOP: Antiplatelet Therapy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 7. The nurse is caring for a patient with a history of peripheral arterial disease. The patient complains of significant claudication, and findings of an ankle-brachial index are abnormal. The nurse anticipates that this patient will most likely require which type of procedure? a. Left heart catheterization b. Stress echocardiogram c. Percutaneous transluminal angioplasty (PTA) d. Nuclear medicine stress test ANS: C PTA may be done to open an artery to reduce claudication symptoms and improve extremity perfusion. PTS: 1 DIF: Cognitive Level: Knowledge REF: 408 OBJ: 10 (theory) TOP: PTA: Stents KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 8. The nurse is teaching a pregnant patient who works as a cashier in a grocery store about varicose vein prevention. Which instruction is most important for the nurse to include in the teaching plan? a. Add vitamin C to diet. b. March in place while standing at the counter. c. Avoid tight support hose. d. Wear supportive shoes. ANS: B Varicose veins are enlarged and tortuous veins that are distorted in shape by accumulations of pooled blood. Treatment of varicose veins includes exercising the legs and feet periodically throughout the day, like marching in place while standing at the counter, elevating the legs whenever possible, and wearing support hose. Supportive shoes and vitamin C do not prevent venous congestion. PTS: 1 DIF: Cognitive Level: Analysis REF: 415 OBJ: 5 (clinical) TOP: Varicose Veins: Prevention KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 9. An 86-year-old patient asks why her ankles have a brownish discoloration and the skin looks thick. Which response best addresses the patient’s concern? a. “The valves in the vessels in your legs aren’t working as well as they used to, which causes the discoloration and thickening of your skin.” b. “You probably aren’t getting enough iron in your diet. We should talk to your doctor about adding an iron supplement.” c. “How many years have you smoked? Nicotine will cause these changes in your skin.” d. “These are just normal changes seen in most older people.” ANS: A Hemosiderin leaks out of the trapped red blood cells in the dilated vessels of the feet and ankles, and stains the skin of people with venous insufficiency. In addition, fibrous tissue replaces subcutaneous tissue around the ankles and causes the skin to become thick and hardened. Iron and nicotine do not play a role in these skin changes with venous insufficiency, and these are not normal changes associated with aging. PTS: 1 DIF: Cognitive Level: Application REF: 419 OBJ: 3 (theory) TOP: Signs of Chronic Venous Insufficiency: Hemosiderin KEY: Nursing Process Step: Intervention MSC: NCLEX: Physiological Integrity: Physiological Adaptation 10. The nurse is caring for a patient who underwent endovenous laser treatment. Which statement indicates that the nurse’s teaching about postprocedure management has been successful? a. “I should wear compression stockings for 5 days.” b. “I should walk at least an hour every day for 2 weeks.” c. “I should massaging the legs to stimulate circulation.” d. “I should notify my doctor if my foot is warm to the touch.” ANS: B Endovenous occlusion using laser is done by placing a catheter within the vein under duplex ultrasound guidance. A laser heats the vessel, causing it to collapse and close off. Patients ambulate immediately after the procedure for 30 to 60 minutes and 1 to 2 hours per day for 1 to 2 weeks. The patient should wear compression stockings for 1 to 2 weeks. The patient should not massage the legs or notify the doctor of warm feet (a normal finding). PTS: 1 DIF: Cognitive Level: Application REF: 419 OBJ: 10 (theory) TOP: Endovenous Laser Treatment KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 11. The nurse is caring for a 75-year-old patient with a history of diabetes and peripheral vascular disease (PVD). The nurse observes an inflamed and excoriated area on the patient’s right shin. Which intervention should the nurse perform first? a. Document the findings. b. Review the patient’s diet. c. Notify the primary care provider. d. Cover with clear occlusive dressing. ANS: D The nurse should first cover the area with a clear, occlusive dressing to protect the area from scratching and infection. The nurse should then document the findings, notify the primary care provider, and review nutritional intake to confirm adequacy for wound healing. PTS: 1 DIF: Cognitive Level: Analysis REF: 420 OBJ: 2 (theory) TOP: PVD: Skin Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 12. The nurse is caring for a patient with a compression dressing. Which action indicates appropriate wound care? a. The nurse changes the compression dressing daily. b. The nurse uses an alcohol-based cleanser before applying the compression dressing. c. The nurse places a compression dressing over the wound dressing. d. The nurse dons a face mask before applying a compression dressing. ANS: C Compression therapy options include compression stockings, elastic tubular support bandages, intermittent compression devices, a paste bandage such as Unna boot, or placement of two to four layers of compression dressings to the affected area. Venous return is accomplished as the patient moves his leg and achieves pressure on the calf muscles. Compression dressings can be placed over wound dressings. The dressings help to reduce ulcer pain, keep the wound moist, and assist debridement. The dressing is changed from every 2 to 3 days to every few weeks depending on the type of dressing applied. An alcohol-based cleanser would be drying and harsh. Compression dressings do not necessitate use of a face mask. PTS: 1 DIF: Cognitive Level: Comprehension REF: 420 OBJ: 8 (theory) TOP: Venous Insufficiency: Compression Dressings KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 13. The nurse is caring for a patient with a deep venous thrombosis (DVT). Which finding requires the nurse’s immediate attention? a. Hematuria b. Decreased sensation in the affected leg c. Urine output of 35 mL in 1 hour d. Hemoptysis ANS: D The primary concern for a patient with a DVT is the potential for embolisms. Hemoptysis (coughing up rust colored sputum) is the cardinal sign of a pulmonary embolus and is a medical emergency. Hematuria (bloody urine) is a finding that requires additional assessment but is not the priority. Hematuria may occur from trauma from Foley catheter insertion, use of blood thinners to treat the DVT, or a variety of other causative factors. Decreased sensation in the affected leg is an expected abnormal finding. Urine output of 35 mL/hr is normal. PTS: 1 DIF: Cognitive Level: Analysis REF: 414, Clinical Cues OBJ: 2 (clinical) TOP: Pulmonary Embolus: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 14. The nurse is caring for a patient with a deep venous thrombosis (DVT). Which medication would likely be used for initial inpatient treatment? a. Dabigatran (Pradaxa) b. Heparin c. Warfarin (Coumadin) d. Edoxaban (Lixiana) ANS: B Inpatient medical treatment for DVT usually consists of intravenous (IV) heparin. Low-molecular-weight heparin (LMWH) such as enoxaparin (Lovenox) by injection may be used for inpatient management and is used more frequently for outpatient treatment. Fondaparinux (Arixtra), a Factor Xa inhibitor, may be used instead of enoxaparin. After initial IV or injection anticoagulation treatment oral anticoagulation is started with warfarin sodium (Coumadin), rivaroxaban (Xarelto), edoxaban (Lixiana), dabigatran (Pradaxa), or apixaban (Eliquis). Anticoagulation is continued for 3 to 6 months for the first episode of DVT and a year for recurrent episodes (Patel, 2014). PTS: 1 DIF: Cognitive Level: Knowledge REF: 414 OBJ: 9 (theory) TOP: DVT Treatment: Streptokinase KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 15. The nurse is teaching a patient who takes warfarin (Coumadin) about a coagulation monitoring device. Which blood clotting time should the device monitors? a. PT b. PTT c. INR d. ACT ANS: C A coagulation monitoring device measures the INR level for clotting time for a person on therapeutic doses of warfarin. PTS: 1 DIF: Cognitive Level: Comprehension REF: 417, Nursing Care Plan 18-1 OBJ: 9 (clinical) TOP: INR Standard KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 16. The student nurse is planning a community group presentation on hypertension. Which group of individuals should the student identify as having the highest incidence of hypertension? a. Muslims b. African Americans c. Whites d. Latinos ANS: B African Americans have a higher incidence of hypertension than any other minority group or whites. PTS: 1 DIF: Cognitive Level: Comprehension REF: 398, Cultural Considerations OBJ: 1 (clinical) TOP: Hypertension KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 17. The nurse is caring for a patient diagnosed with an abdominal aortic aneurysm who complains of sudden, intense abdominal pain and light-headedness. What action should the nurse take next? a. Monitor the patient’s blood pressure every 15 minutes. b. Contact the physician immediately. c. Notify the patient’s family of the change in condition. d. Continue to assess the patient’s pain. ANS: B The patient is most likely experiencing a ruptured aneurysm, which is a medical emergency requiring surgical repair. The nurse should contact the physician immediately. The vital signs may need to be measured more often than every 15 minutes. Notifying the family is not the priority intervention. Ongoing assessment of pain should continue, but after the physician is notified of the emergent status change. PTS: 1 DIF: Cognitive Level: Analysis REF: 410 OBJ: 6 (theory) TOP: AneurysmKEY: Nursing Process Step: Intervention MSC: NCLEX: Physiological Integrity: Physiological Adaptation 18. The nurse is caring for a patient with peripheral arterial disease who complains of 3/10 pain in the lower extremities. The nurse observes a 0.5 cm × 1 cm ulcer on the left lower leg, and the lower legs are shiny and hairless bilaterally. The nurse identifies which priority problem statement/nursing diagnosis? a. Injury related to loss of peripheral circulation. b. Acute pain related to ischemia to lower extremities. c. Altered skin integrity related to ulcers on lower extremities. d. Insufficient knowledge related to new diagnosis of hypertension. ANS: C Altered skin integrity is the priority problem statement/diagnosis in this situation. Acute pain is a nursing diagnosis, but the pain is 3/10 so it is not the priority since there is an open wound. Injury and insufficient knowledge could be problems, but there is not enough information to support these diagnoses. PTS: 1 DIF: Cognitive Level: Application REF: 406 OBJ: 9 (theory) TOP: Arterial Ulcer KEY: Nursing Process Step: Diagnosis MSC: NCLEX: Health Promotion and Maintenance MULTIPLE RESPONSE 19. Which problems are potential complications of uncontrolled hypertension? (Select all that apply.) a. Stroke b. Kidney failure c. Heart attack d. Congestive heart failure e. Deep vein thrombosis (DVT) ANS: A, B, C, D Uncontrolled hypertension may result in stroke, kidney failure, heart attack, and congestive heart failure. A DVT is not a potential complication of hypertension. PTS: 1 DIF: Cognitive Level: Comprehension REF: 404, Patient Teaching OBJ: 6 (theory) TOP: Hypertension: Complications KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 20. Which findings characterize peripheral vascular disease (PVD)? (Select all that apply.) a. Narrowed arteries b. Obstructed veins c. Involvement of all extremities d. Defective valve function e. Thrombophlebitis ANS: A, B, D, E Findings that characterize PVD include narrowed arteries, obstructed veins, deficient valvular function, and thrombophlebitis. PVD usually involves only the lower extremities. PTS: 1 DIF: Cognitive Level: Comprehension REF: 406, Table 18-4 OBJ: 6 (theory) TOP: PVD: Characteristics KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 21. Which factor(s) may be useful in preventing peripheral vascular disease (PVD)? (Select all that apply.) a. Stress relief b. Diabetes control c. Weight control d. Routine exercise e. Smoking cessation ANS: A, B, C, D, E All strategies are supportive of the prevention of PVD. PTS: 1 DIF: Cognitive Level: Knowledge REF: 406 OBJ: 5 (theory) TOP: PVD: Prevention KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 22. The nurse is caring for a patient with peripheral vascular disease (PVD). The nurse understands that which age-related changes may cause PVD? (Select all that apply.) a. Decreasing blood viscosity b. Loss of elasticity in vessel walls c. Atherosclerotic changes in vessels d. Sedentary practices e. Weakened leg muscles ANS: B, C, D, E Age-related changes that can lead to PVD include: loss of elasticity in vessel walls, atherosclerotic changes in vessels, sedentary practices, and weakened leg muscles. Blood viscosity increases with age. PTS: 1 DIF: Cognitive Level: Comprehension REF: 418,Older Adult Care Points OBJ: 2 (clinical) TOP: PVD: Prevention KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 23. Which intervention(s) is/are important for a patient with venous insufficiency? (Select all that apply.) a. Avoid swimming. b. Elevate feet to reduce edema. c. Wear tight clothing. d. Decrease fluid intake. e. Apply elastic compression wraps twice daily. ANS: B, E Elevating feet above heart level and wearing elastic compression support wraps decrease edema. (Wraps should be applied twice daily.) Swimming is encouraged as good exercise that encourages venous return. Tight clothing should be avoided. Reduction of fluid intake may increase blood viscosity and promote clotting. PTS: 1 DIF: Cognitive Level: Comprehension REF: 419 OBJ: 3 (clinical) TOP: PVD: Basic Care KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 24. Which words compose part of the “5 Ps” of arterial disease? (Select all that apply.) a. Pain b. Paresthesia c. Purulent d. Pooling e. Pallor ANS: A, B, E Five Ps of arterial disease are pain, pulselessness, pallor, paresthesias, and paralysis. PTS: 1 DIF: Cognitive Level: Knowledge REF: 422 OBJ: 3 (clinical) TOP: 6 Ps of Arterial Disease KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 25. The nurse is caring for an 80-year-old long-resident in a term care facility. Which intervention(s) should the nurse plan to enhance blood flow? (Select all that apply.) a. Apply light blankets over legs while sitting. b. Elevate legs frequently. c. Encourage walking. d. Avoid tight compression stockings. e. Maintain a warm environment. ANS: A, B, C, E Interventions that may enhance blood flow include using light blankets while sitting, elevating legs, encouraging exercise, and maintaining a warm environment. Compression stockings are beneficial. PTS: 1 DIF: Cognitive Level: Application REF: 409 OBJ: 3 (clinical) TOP: PVD: Maintenance KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 26. The nurse is caring for a patient with Raynaud disease who is employed as a construction worker, has hypertension, and smokes one-half to one pack of cigarettes per day. What teaching points should the nurse include in discharge instructions? (Select all that apply.) a. Wear gloves when handling cold items. b. Drink plenty of warm beverages, such as coffee. c. Wear insulated socks when working in cool weather. d. Attend a smoking program. e. Use a heating pad to stay warm. ANS: A, C, D, E The major nursing interventions for Raynaud disease involve teaching the patient to protect extremities and prevent injury. The patient should be taught to dress warmly when in cold environments. Clothing should be layered and nonrestrictive. The patient should wear protective clothing like hats, gloves, and warm socks. The patient should wear protective gloves when reaching into ovens and when handling extremely cold items. The patient should also manage stress and stop tobacco use. Caffeine intake should be limited. The patient should not use a heating pad for warmth due to risk for burns. PTS: 1 DIF: Cognitive Level: Application REF: 412 OBJ: 7 (theory) TOP: Raynaud Disease KEY: Nursing Process Step: Intervention MSC: NCLEX: Health Promotion and Maintenance COMPLETION 27. The patient who has a history of smoking and alcohol abuse is most likely to develop __________ hypertension. ANS: secondary Secondary hypertension results from other conditions or lifestyle choices. Primary hypertension is idiopathic or familial. PTS: 1 DIF: Cognitive Level: Comprehension REF: 397 OBJ: 1 (theory) TOP: Hypertension KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation Chapter 19: Care of Patients with Cardiac Disorders deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is caring for a patient with suspected right-sided heart failure. Which manifestation best supports this potential diagnosis? a. Wheezing b. Orthopnea c. Edema d. Pallor ANS: C Right-sided heart failure leads to edema from systemic backup. Wheezing, orthopnea, and pallor are indicative of left-sided failure. PTS: 1 DIF: Cognitive Level: Comprehension REF: 426, Table 19-2 OBJ: 1 (theory) TOP: Heart Failure: Right Side KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. The nurse is caring for a patient with a history of left-sided congestive heart failure (CHF). Which finding leads the nurse to suspect that the patient could be experiencing an acute exacerbation of this condition? a. The abdomen is tight and shiny. b. Wheezes are present during lung auscultation. c. The pupils react sluggishly to light. d. The heart rate is irregularly irregular. ANS: B Left-sided heart failure causes increased pressure on the lungs and may manifest in wheezing. A tight and shiny abdomen is consistent with ascites, a manifestation of right-sided CHF. Sluggish pupillary reaction is consistent with a neurologic problem, and an irregularly irregular heart rate is consistent with a cardiac arrhythmia like atrial fibrillation. PTS: 1 DIF: Cognitive Level: Application REF: 426, Table 19-2 OBJ: 1 (theory) TOP: CHF: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. The statement indicates that the nurse’s teaching about the purpose of an implanted cardioverter-defibrillator (ICD) has been successful? a. “The ICD will detect bad rhythms and shock my heart into normal rhythm.” b. “I should avoid handheld security devices at the airport.” c. “I should ask my doctor how often I should have my ICD checked.” d. “I should avoid working on the alternator of my boat.” ANS: A All statements are accurate, but the question asks about the purpose of the ICD. ICDs are devices indicated for patients with repeated episodes of life-threatening dysrhythmias and for some patients with cardiomyopathy. This device monitors the heartbeat and provides an electrical shock similar to that delivered in cardiac defibrillation or cardioversion when a life-threatening rhythm is detected. Most ICDs have the ability to pace as well as defibrillate. The patient is warned to avoid exposure to strong magnetic fields such as: microwave towers, transformers and electrical transmitters, electrical generators, handheld security devices at airports, and arc welding equipment. The patient should not lean over the alternator of a running car or boat motor. A magnetic field will temporarily inactivate the device. Moving away from the magnetic source will restore normal function. PTS: 1 DIF: Cognitive Level: Analysis REF: 441 OBJ: 2 (clinical) TOP: ICD KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 4. The nurse is caring for a patient with severe congestive heart failure (CHF) who denies pain and is fearful of taking prescribed morphine. Which explanation best works to alleviate the patient’s anxiety about risk of addiction? a. “Many people with CHF use morphine for pain control.” b. “We can treat your pain with aspirin or ibuprofen.” c. “Morphine has properties that help relieve air hunger in CHF patients.” d. “You can refuse to take it.” ANS: C The primary purpose of morphine is its relief of air hunger and anxiety. Nonsteroidal anti-inflammatory drugs do not have the same vasodilation properties as morphine. Telling the patient that many CHF patients take morphine provides a generalized statement that does not therapeutically address the patient’s anxiety or confusion about the medication. Telling the patient that he may refuse is a dismissive, nontherapeutic response. PTS: 1 DIF: Cognitive Level: Application REF: 427 OBJ: 4 (clinical) TOP: CHF Treatment: Morphine KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 5. The nurse is caring for a patient with congestive heart failure (CHF). Which intervention should the nurse include in the plan of care? a. Encourage intake of canned soups. b. Place the patient in a side-lying position to prevent venous pooling. c. Encourage large meals for increased nutritional impact. d. Alternate rest with activity. ANS: D Alternating rest with activity preserves the patient’s energy. Canned soups are high in sodium, and CHF patients are often placed on restricted-sodium diets. Patients are more comfortable in semi-Fowler position to ease breathing and should eat small meals that are easy to chew and use less energy. PTS: 1 DIF: Cognitive Level: Application REF: 432 OBJ: 1 (clinical) TOP: CHF: Nursing Care KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 6. The nurse is caring for a patient with a heart rate of 115 beats/min and complaints of shortness of breath. The nurse anticipates that these findings are most likely related which underlying problem? a. Pulmonary edema b. Decreased cardiac output c. Impending pneumonia d. Increasing anxiety ANS: B When the heart is beating rapidly, the stroke volume decreases. This diminishes the cardiac output, causing reduced oxygen to tissues and tissue hypoxia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 435 OBJ: 2 (clinical) TOP: Tachycardia: Complications KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 7. The nurse is teaching the patient with an arrhythmia. Which statement indicates that the patient requires further teaching? a. “I’ve cut my coffee from 10 cups to 2 cups a day.” b. “I don’t drink regular cola drinks anymore.” c. “I have given up drinking those high-energy drinks.” d. “I’ve switched from 5 cups of coffee to 5 cups of tea.” ANS: D The patient with an arrhythmia should decrease caffeine intake. Tea has as much caffeine as coffee does, or more. All other options will reduce the caffeine intake. PTS: 1 DIF: Cognitive Level: Comprehension REF: 435, Clinical Cues OBJ: 2 (clinical) TOP: Arrhythmias: Caffeine Reduction KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 8. The nurse is analyzing a patient’s telemetry strip and observes a sawtooth appearance with no P waves. How should the nurse document this finding? a. Premature ventricular contraction (PVC) b. Atrial flutter c. Ventricular tachycardia (VT) d. Premature atrial contraction (PAC) ANS: B Atrial flutter displays a sawtooth appearance generated from small ineffective contractions prior to the QRS complex. An abnormally shaped P wave appears on the electrocardiogram (ECG) before the QRS wave in PAC. PVC is seen as an early beat without a P wave and with a wide QRS complex. VT is seen as three or more PVCs in a row with a ventricular rate of greater than 100 beats/min. PTS: 1 DIF: Cognitive Level: Application REF: 437 OBJ: 2 (clinical) TOP: Arrhythmias: Atrial Flutter KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 9. The nurse is caring for a patient with atrial fibrillation who asks why she needs to take warfarin. Which statement best answers the patient’s question? a. Warfarin increases the ejection fraction. b. Warfarin prevents clots from forming in the atria. c. Warfarin keeps the atrial fibrillation from involving the ventricles. d. Warfarin increases the cardiac output. ANS: B Warfarin keeps clots from forming in the retained blood in the atria left there by the ineffective atrial contractions. PTS: 1 DIF: Cognitive Level: Comprehension REF: 437 OBJ: 3 (clinical) TOP: Arrhythmias: Warfarin KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 10. The nurse caring for a patient who is taking amiodarone (Cordarone). What side effect could this patient experience? a. Sudden increase in temperature b. Hypotension c. Bradycardia d. Depressed ventilation ANS: B Hypotension with the attendant fatigue is a side effect of amiodarone (Cordarone). PTS: 1 DIF: Cognitive Level: Analysis REF: 438, Table 19-4 OBJ: 4 (clinical) TOP: Amiodarone (Cordarone): Side Effects KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 11. Which disorganized ECG pattern is recognized as the most fatal of all arrhythmias? a. Ventricular fibrillation b. Premature ventricular beats c. Atrial fibrillation d. Ventricular tachycardia (VT) ANS: A Ventricular fibrillation is a disorganized pattern of totally ineffective contractions and no cardiac output. This is a medical emergency and, if not corrected, is fatal. PTS: 1 DIF: Cognitive Level: Knowledge REF: 439 OBJ: 2 (clinical) TOP: Arrhythmias: Ventricular Fibrillation KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 12. Which statement accurately explains how calcium channel blocker verapamil assists to correct an arrhythmia? a. The medication desensitizes the heart to the impulse to contract. b. The medication increases the strength of the impulse from the atrioventricular (AV) node. c. The medication alters the impulse from the sinoatrial (SA) node. d. The medication inhibits transmission of the impulse from the AV node. ANS: D Verapamil blocks calcium from the cardiac cells, inhibiting the transmission of the impulse from the AV node. PTS: 1 DIF: Cognitive Level: Knowledge REF: 438, Table 19-4 OBJ: 4 (clinical) TOP: Arrhythmias: Verapamil KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 13. Which potential hazard is most important for a patient with an automatic implantable cardioverter-defibrillator (AICD) to avoid? a. Static electricity from synthetic fabric b. Airport security detection devices c. Constricting clothing and belts d. High altitudes ANS: B Electronic wands at airport security check stations can alter the setting on the AICD. People with AICDs should have certification that they have the embedded device. High altitudes and clothing will not alter the settings. PTS: 1 DIF: Cognitive Level: Comprehension REF: 441 OBJ: 6 (clinical) TOP: AICD: Precautions KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 14. The nurse caring for a patient who requires a temporary transvenous pacemaker. Which statement indicates that the patient understands the nurse’s teaching? a. “I may experience uncomfortable muscle contractions.” b. “The procedure will use general anesthesia.” c. “I will be given a sedative after the procedure.” d. “This device may be left in place for 6 weeks.” ANS: A A temporary transvenous pacemaker is placed if a transient rhythm such as heart block develops after a myocardial infarction or drug toxicity. It is important that the patient understands the uncomfortable muscle contractions are normal. Transvenous pacemakers are inserted by fluoroscopy with local anesthesia, and the leads are attached to an external power source. Patient consent is required, and a sedative is given to the patient before the procedure. Epicardial pacemaker wires are often placed during cardiac surgery for quick use should the patient need to be “paced” in the postoperative period. The wires are brought through the chest wall and are attached to an external power source. When the need for the wires is past, the surgeon will pull them out. The device is a short-term solution and is only used until the problem resolved or a permanent device is inserted. PTS: 1 DIF: Cognitive Level: Application REF: 439 OBJ: 6 (clinical) TOP: Temporary Pacemakers KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 15. Which teaching point will the nurse include when providing discharge instructions to the patient with a new permanent pacemaker? a. “You will be able to have an MRI for diagnostic purposes.” b. “Avoid using microwave ovens.” c. “Avoid lifting heavy objects for as long as your physician prescribes.” d. “Airport screening devices may cause your pacemaker to fire incorrectly.” ANS: C The postoperative patient with a permanent pacemaker can assume normal activity when the physician prescribes. Using the arm for lifting and other activities may dislodge the leads from their positions. MRIs must be avoided since the large magnet can interfere with the pacemaker’s function. Microwaves and airport security devices do not affect the pacemaker. PTS: 1 DIF: Cognitive Level: Application REF: 440, Patient Teaching OBJ: 5 (clinical) TOP: Permanent Pacemaker: Postoperative Expectations KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 16. The nurse is caring for a patient who is taking digitalis. The patient complains of increased thirst, and the nurse observes dry mucous membranes. Which additional finding warrants the nurse’s immediate attention? a. Sudden, sharp knee pain b. Blurred vision c. Epistaxis d. Chills ANS: B Blurred vision, halos around lights, nausea, vomiting and diarrhea, and fatigue are all indicators of toxicity to digitalis. Assessment is especially important for the dehydrated patient because of the rising potassium level. PTS: 1 DIF: Cognitive Level: Analysis REF: 446 OBJ: 4 (clinical) TOP: Digitalis: Toxicity KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 17. The nurse is caring for several patients on a cardiac care unit. Which patient is most likely to have aortic stenosis? a. 35-year-old with a history of Raynaud disease b. 63-year-old with uncontrolled diabetes c. 73-year-old with a history of hypertension d. 86-year-old with a history of atherosclerosis ANS: D The older 86-year-old patient with atherosclerosis is most likely to have degenerative calcification of the valve. Risk for aortic stenosis increases with age, and congenital valve malformations and rheumatic fever are causes in younger patients. PTS: 1 DIF: Cognitive Level: Application REF: 444 OBJ: 3 (clinical) TOP: Cardiac Valve Disorders KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 18. The home health nurse is caring for a patient with congestive heart failure (CHF). Which assessment finding should the nurse report immediately to the physician? a. Moderate shortness of breath after walking down the hall b. A 3 pound weight gain over the course of a week c. Heart rate of 104 beats/min after ambulating to the bathroom d. Increase in urinary output to 50 mL in the last hour ANS: B A weight gain without an increase in caloric intake is indicative of fluid retention, which is an indication of worsening heart failure. Moderate shortness of breath after exercise and a mild increase in heart rate after activity are expected. A decrease in urinary output would be of concern. PTS: 1 DIF: Cognitive Level: Analysis REF: 430 OBJ: 8 (theory) TOP: Home Care Considerations: Heart Failure KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential MULTIPLE RESPONSE 19. The nurse is caring for a 60-year-old African American patient with hypertension. The patient is obese and a smoker. Which modifiable risk factors place this patient at an increased risk for heart disease? (Select all that apply.) a. Age b. Race c. Hypertension d. Obesity e. Smoking ANS: C, D, E Modifiable risk factors that increase the patient’s risk of heart disease include hypertension, obesity, and cigarette smoking. The patient could lessen his risk by strictly controlling blood pressure, losing weight with diet and exercise, and implementing a smoking cessation plan. Age and race are nonmodifiable risk factors for heart disease. PTS: 1 DIF: Cognitive Level: Comprehension REF: 424, 427 OBJ: 6 (clinical) TOP: Modifiable Risk Factors KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 20. The nurse is performing an initial assessment on a new patient with suspected right-sided heart failure. Which finding(s) is/are consistent with the patient’s potential diagnosis? (Select all that apply.) a. Clammy skin b. Splenomegaly c. Abdominal distention d. Wheezing e. Dyspnea ANS: B, C, E Signs and symptoms of right-sided CHF include fatigue, peripheral edema, gastrointestinal congestion and abdominal distention, ascites with liver congestion, splenomegaly, and dyspnea. Clammy skin and wheezing are symptoms of left-sided CHF. PTS: 1 DIF: Cognitive Level: Application REF: 426, Table 19-2 OBJ: 1 (theory) TOP: Heart Failure Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 21. The nurse in a skilled nursing facility is caring for an 80-year-old patient who develops a productive cough with pink, frothy sputum. Which independent interventions should the nurse implement immediately? (Select all that apply.) a. Limit the patient’s activity. b. Administer morphine. c. Administer lasix. d. Place the patient in high Fowler position. e. Weigh the patient daily. ANS: A, D Acute pulmonary edema (acute left ventricular failure) is a medical emergency that must be treated promptly. The patient with this condition has severe dyspnea; a cough productive of frothy, pink-tinged sputum; tachycardia; and moist, bubbling respirations with cyanosis. Nursing interventions for acute pulmonary edema include placing the patient in high Fowler position to relieve the dyspnea; administering oxygen, diuretics, morphine, and other prescribed drugs; limiting and monitoring activity; and assessing cardiopulmonary status. Limiting activity and placing the patient in high Fowler do not require a physician’s order and should be implemented immediately. Acute pulmonary edema is a medical emergency, and activity necessary to obtain a daily weight is not indicated at this time. Administering morphine and diuretics are dependent nursing interventions. PTS: 1 DIF: Cognitive Level: Analysis REF: 429 OBJ: 5 (clinical) TOP: Acute Pulmonary Edema: Independent Nursing Interventions KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 22. Which statement(s) accurately describe(s) characteristics of normal sinus rhythm (NSR)? (Select all that apply.) a. One atrial contraction (P wave) b. One ventricular contraction (QRS complex) c. One T wave d. Heart rate 60 to 100 e. P wave immediately follows the QRS complex ANS: A, B, C, D The P wave precedes the QRS complex. All other options are seen in NSR. PTS: 1 DIF: Cognitive Level: Knowledge REF: 434, Figure 19-5 OBJ: 1 (clinical) TOP: Normal Sinus Rhythm KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 23. Which factor(s) is/are potential causative agents for arrhythmias? (Select all that apply.) a. Hyperkalemia b. Valvular prolapse c. Infarct damage d. Properly functioning sinoatrial (SA) node e. Excess fluid ANS: A, B, C, E Electrolyte imbalances, especially a high-potassium level, valvular prolapse, heart damage after a heart attack, and fluid overload are all potential causative factors for abnormal heart rhythms. A properly functioning SA node results in normal sinus rhythm. PTS: 1 DIF: Cognitive Level: Comprehension REF: 435 OBJ: 5 (theory) TOP: Arrhythmias: Etiology KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 24. The nurse is educating a patient about cardiomyopathy. The nurse includes information that which circumstance(s) may increase risk for cardiomyopathy? (Select all that apply.) a. Systemic hypertension b. Chronic excessive alcohol consumption c. Pregnancy d. Diabetes e. Systemic infection ANS: A, B, C, E Cardiomyopathy is a group of disorders that result in enlargement of the heart and subsequent inefficient pumping action. Risk factors include systemic hypertension, chronic alcohol consumption, pregnancy, and certain systemic infections. Diabetes is not considered a risk factor for cardiomyopathy. PTS: 1 DIF: Cognitive Level: Comprehension REF: 443 OBJ: 3 (clinical) TOP: Cardiomyopathy KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential COMPLETION 25. The nurse expresses concern to the 80-year-old resident in a long-term care facility who is attempting to jog on a treadmill. The nurse is aware that the exceptional oxygen and metabolic demands brought on by the exercise might cause ____________. ANS: heart failure When the body makes excessive oxygenation and metabolic demands on an aging heart with low cardiac reserve, heart failure may result. PTS: 1 DIF: Cognitive Level: Application REF: 430, Older Adult Care Points OBJ: 1 (clinical) TOP: CHF: Older Adult KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 26. When the nurse assesses an apical pulse of 52, the nurse documents this arrhythmia as _________. ANS: bradycardia An apical pulse of less than 60 is considered to be bradycardia. PTS: 1 DIF: Cognitive Level: Knowledge REF: 434 OBJ: 1 (clinical) TOP: Bradycardia KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 27. The patient suffering from ventricular tachydysrhythmia may benefit from _________________ when medications are not effectively treating the disorder. ANS: radiofrequency catheter ablation This procedure destroys the irritable focus in the heart via heat and subsequent scarring, thus correcting the ventricular tachydysrhythmia when medication is not effective. PTS: 1 DIF: Cognitive Level: Analysis REF: 441 OBJ: 8 (theory) TOP: Home Care Considerations: Heart Failure KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential Chapter 20: Care of Patients with Coronary Artery Disease and Cardiac Surgery deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is caring for a patient with agina pectoris who asks what happens to make his body experience pain. The nurse explains that pain results from which underlying causative factor? a. Congestion that backs up into the lungs b. Inadequate blood flow and poor oxygen supply c. Edema from fluid overload d. Inflammation in the vessels ANS: B Angina pectoris (chest pain) occurs when blood supply to the heart is decreased or totally obstructed. Pain results from ischemia (inadequate blood and oxygen supply). PTS: 1 DIF: Cognitive Level: Comprehension REF: 450 OBJ: 2 (theory) TOP: CAD: Pain KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. How does a myocardial infarction (MI) alter the pumping efficiency of the heart? a. An MI reduces the impulse from the sinoatrial node. b. An MI causes myocardial necrosis. c. An MI shunts all myocardial blood flow to a specific cardiac region. d. An MI causes myocardial swelling and inflammation. ANS: B Myocardial necrosis (damaged or dead heart muscle tissue) cannot contract effectively, which decreases pumping efficiency (cardiac output). PTS: 1 DIF: Cognitive Level: Comprehension REF: 450 OBJ: 2 (theory) TOP: MI: Pathophysiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. The nurse is caring for a patient admitted with chest pain to rule out a myocardial infarction (MI). The nurse observes that the patient is experiencing electrocardiogram (ECG) changes and reviews new laboratory results. Which laboratory value should the nurse report immediately? a. Troponin of 2.4 mcg/L b. Potassium of 3.4 mEq/L c. Creatine phosphokinase of 134 IU/L d. Sodium of 133 mEq/L ANS: A The patient has a significantly elevated troponin. The abnormal troponin, along with ECG changes, indicates that the patient is likely experiencing an MI. (Elevated troponin levels are most indicative of an MI as these enzymes are specific to heart muscle damage.) While the nurse should report the abnormally low potassium of 3.4 (low normal) sodium, these findings are of lesser priority than the elevated troponin. PTS: 1 DIF: Cognitive Level: Analysis REF: 458 OBJ: 5 (theory) TOP: MI: Cardiac Enzymes KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. The nurse is caring for a post–myocardial infarction (MI) patient who has been started on daily simvastatin (Zocor) and a low-fat diet. Which statement best indicates that the nurse’s teaching has been successful? a. “I will need to have blood work every month while taking Zocor.” b. “I should take my Zocor with grapefruit juice to help absorption. c. “I should call my doctor if I experience unexplained muscle pain.” d. “I should take Zocor an hour before my biggest meal of the day.” ANS: C Statins can injure muscle tissue and are toxic to the liver in some patients. Patients should report any unexplained muscle tenderness or pain persisting for more than a few days. Laboratory tests for liver enzymes are recommended at the start of therapy and only when clinically indicated. Grapefruit juice interferes with drug metabolism and should be avoided to prevent increased risk of toxicity. Zocor can be taken without regard to meals. PTS: 1 DIF: Cognitive Level: Application REF: 454, Clinical Cues OBJ: 2 (clinical) TOP: Statins: Precaution KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 5. The nurse is educating a patient on a low-fat, low-cholesterol diet after a myocardial infarction (MI). Which food choice should the nurse recommend? a. “Avoid eating frozen foods.” b. “Replace a serving of red meat with a serving of fish.” c. “Use nondairy creamer in your decaffeinated coffee.” d. “Drink a serving of grapefruit juice each day.” ANS: B Fish have a high content of omega-3 fatty acids, which are helpful in reducing cholesterol. Not all frozen foods are unhealthy. Frozen vegetables with no sodium added are a good choice for a low-fat, low-cholesterol diet. Nondairy creamer is high in trans fat and saturated fat. Grapefruit juice often interferes with metabolism of a variety of medications. PTS: 1 DIF: Cognitive Level: Application REF: 454, Nutrition Considerations OBJ: 3 (clinical) TOP: Low-Fat Diet: Omega-3 KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 6. The nurse is caring for a male patient with angina who has a new prescription for sublingual nitroglycerin. What information is most important for the nurse to include in the teaching plan? a. Nitroglycerin tablets expire 3 months after the bottle is opened. b. Take a second tablet 15 minutes after the first dose and call the physician if pain persists. c. Store nitroglycerin tablets in a cool, dark location. d. Nitroglycerin may cause an unsafe drop in heart rate when combined with certain medications for erectile dysfunction. ANS: C Sublingual nitroglycerin tablets should be kept in a cool, dark place and should be carried by the patient at all times. If chest pain persists after the first dose, the patient should repeat the dose in 5 minutes. The patient should contact emergency services, not the physician. Nitroglycerin may cause an unsafe drop in blood pressure (BP) if combined with certain medications for erectile dysfunction. PTS: 1 DIF: Cognitive Level: Application REF: 457, Clinical Cues OBJ: 3 (clinical) TOP: Angina: Nitroglycerin Tablets KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 7. The nurse is explaining the difference between exertional angina and unstable angina. Which statement about unstable angina is accurate? a. Unstable angina occurs with moderate exercise. b. Unstable angina occurs when the blood pressure increases sharply. c. Unstable angina occurs when the body reacts to high stress levels. d. Unstable angina occurs unpredictably, even in sleep. ANS: D Unstable angina attacks are unpredictable and do not follow a pattern, as do stable angina attacks. Unstable angina can progress into a myocardial infarction (MI) and a medical emergency. PTS: 1 DIF: Cognitive Level: Knowledge REF: 451 OBJ: 3 (theory) TOP: Angina: Unstable Angina KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 8. The patient with angina asks the nurse how a daily dose of 81 mg of aspirin is helpful. Which reply is best? a. Low-dose aspirin helps reduce clotting. b. Low-dose aspirin helps dilate coronary vessels. c. Low-dose aspirin helps alleviates pain associated with angina. d. Low-dose aspirin helps lower cholesterol. ANS: A Daily doses of aspirin reduce clotting by prolonging clotting time, thus helping prevent clots that can cause an MI. PTS: 1 DIF: Cognitive Level: Comprehension REF: 460 OBJ: 4 (theory) TOP: Angina: Use of Aspirin KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 9. The nurse is caring for a female patient with a family history of heart disease who is undergoing a workup for cardiovascular disease. Which finding is most concerning to the nurse? a. Fainting b. Dry mouth c. Dizziness d. Fatigue ANS: D Women frequently experience fatigue with heart disease. Many women do not even experience chest pain. Fainting, dry mouth, and dizziness are not typical signs of heart disease in women. PTS: 1 DIF: Cognitive Level: Comprehension REF: 452, Box 20-1 OBJ: 2 (theory) TOP: CAD in Women KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 10. The patient states that he had a cardiac catheterization 10 years ago and wonders if any of the postprocedure care has changed. Which response by the nurse is most accurate? a. “We will only roll you to the same side as the catheter insertion site.” b. “You will lay flat for several hours, and we will place a sandbag over the dressing in the groin.” c. “You will most likely be able to ambulate within a few hours if your doctor uses an arterial closure device at the catheter insertion site.” d. “We will encourage you to flex and extend your legs when you return from the procedure to prevent a clot from forming at the insertion site.” ANS: C Most physicians use an arterial closure device at the puncture site, which enables the patient to be ambulatory within 2 hours after the cardiac catheterization procedure. The patient may be turned to either side. Sandbags were used in the past to prevent bleeding from the puncture site and the patient had to lay flat for several hours. Flexing and extending the legs immediately after the procedure would likely cause bleeding from the site. PTS: 1 DIF: Cognitive Level: Application REF: 459 OBJ: 4 (theory) TOP: Angiogram: Aftercare KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 11. The drug alteplase (t-PA) is given to the patient with a myocardial infarction (MI). Which statement accurately describes the purpose of this medication? a. “Alteplase (t-PA) dissolves the obstruction in the coronary artery.” b. “Alteplase (t-PA) dilates vessels to relieve pain.” c. “Alteplase (t-PA) strengthens cardiac contraction.” d. “Alteplase (t-PA) increases cardiac output.” ANS: A Alteplase (t-PA) is a thrombolytic drug that will dissolve the clot if given within 12 hours of the MI. PTS: 1 DIF: Cognitive Level: Comprehension REF: 460 OBJ: 2 (clinical) TOP: MI: t-PA KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 12. The nurse is caring for a patient with uncontrolled hypertension, diabetes, asthma, and gastroesophageal reflux disease (GERD). Which problem serves as a contraindication for a thrombolytic agent? a. Uncontrolled hypertension b. Diabetes c. Asthma d. GERD ANS: A Thrombolytic agents are contraindicated in people with uncontrolled hypertension, GI bleeds, recent intracranial or intraspinal surgery, or aneurysm because of threat of excessive bleeding. PTS: 1 DIF: Cognitive Level: Application REF: 460 OBJ: 2 (clinical) TOP: MI: Thrombolytic Agents KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 13. The nurse is caring for a post-myocardial infarction (MI) patient. The patient questions the reason for a stool softener and denies constipation. Which statement indicates that the patient accurately understands the nurse’s teaching? a. “Stool softeners help me keep from straining during bowel movements, which can lower my heart rate.” b. “Stool softeners help me to get rid of extra wastes that can harm my heart.” c. “Stool softeners help reduce swelling that can increase work on my heart.” d. “Stool softeners help to reduce discomfort from gas pains.” ANS: A Bearing down or straining at stool can stimulate the vagal nerve and induce bradycardia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 461 OBJ: 3 (clinical) TOP: MI: Aftercare KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 14. The nurse is caring for a patient who underwent a transfemoral cardiac catheterization with coronary angiography earlier in the day. The patient denies pain and no longer requires bed rest. The groin is soft with no palpable hematoma. Which postprocedure care is most important for the patient at this time? a. Encourage increased fluid intake. b. Administer pain medications as ordered. c. Obtain vital signs every 15 minutes. d. Assist the patient with ambulation. ANS: A The procedure uses a large volume of dye, which can be harmful to the kidneys. Increasing fluid intake is the priority focus for care at this time after hemostasis is obtained. Keeping the patient hydrated increases the rate of urine flow, dilutes the urine, and helps prevent kidney damage as the contrast is excreted. The patient denies pain. Vital signs are taken every 15 minutes for the first hour and are checked progressively less frequently unless there is evidence of bleeding or instability. The patient can now ambulate, but ambulation is a lesser priority than flushing out the hypertonic dye. PTS: 1 DIF: Cognitive Level: Analysis REF: 459, Safety Alert OBJ: 4 (theory) TOP: Cardiac Catheterization KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 15. The nurse assesses a friction rub in a patient who is 2 days post–myocardial infarction (MI). The nurse recognizes this finding indicates which problem? a. A recurrent MI b. Pleural effusion c. Pericarditis d. Angina ANS: C Friction rubs occur in pericarditis when the inflamed area of the infarct rubs the pericardium. PTS: 1 DIF: Cognitive Level: Comprehension REF: 460, Table 20-3 OBJ: 2 (theory) TOP: MI: Complications KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 16. The 60-year-old female in the post-coronary care unit confides to the nurse, “My life is over. I’ll never be able to care for my family, take a vacation, or work in my garden.” Which response is most supportive? a. “You are doing great! You can do all of those things in a few weeks.” b. “You may have to give up some things, but there are other activities you might enjoy.” c. “You are feeling a little blue today. Would you like medication to help your anxiety?” d. “You sound a little down. Tell me what you think is going to keep you from those activities; we might be able to address the problems.” ANS: D Helping patients identify and face depression is helpful in dispelling it, and talking about her concerns will open up conversation and address the concerns in a problem-solving approach. Telling her that she will be able to resume all activities may be instilling false hope. Medication is not warranted at this point. PTS: 1 DIF: Cognitive Level: Application REF: 462, 468 OBJ: 8 (theory) TOP: MI: Depression KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 17. A patient who presented to the emergency room with a myocardial infarction (MI) becomes pale, diaphoretic, and hypotensive. What action should the nurse take first? a. Notify the physician immediately. b. Ensure that the patient has patent IV access. c. Request assistance from respiratory therapy. d. Inform the patient’s family of the change in status. ANS: A If the left ventricle is badly damaged, cardiogenic shock may occur. Signs and symptoms are those that accompany decreased cardiac output, such as decreased BP, confusion, restlessness, diaphoresis, rapid and thready pulse, increased respiratory rate, cold and clammy skin, and diminishing urinary output to less than 20 mL/hr. This condition is a medical emergency that requires immediate notification of the physician. The nurse should then ensure that the IV is patent. Respiratory therapy assistance will likely be beneficial, especially if the patient’s condition further deteriorates. The nurse should finally notify the patient’s family about the change in status. PTS: 1 DIF: Cognitive Level: Analysis REF: 461 OBJ: 5 (theory) TOP: MI: Cardiogenic Shock KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 18. The nurse performs patient teaching about minimally invasive direct coronary artery bypass (MIDCAB). Which statement indicates that the patient needs further instruction? a. “It frightens me to think that my heart will be stopped for a long time during surgery.” b. “This surgery bypasses my artery that is blocked, and replaces it with sections of a vein or artery taken from another part of my body.” c. “This surgery will hopefully control my angina since nothing else we have tried has worked.” d. “I may come out of surgery with vessels removed from my legs.” ANS: A The MIDCAB procedure is less invasive than the traditional coronary artery bypass graft (CABG) procedure and does not require the patient be placed on the heart-lung machine due to stopping the heart for an extended period. Both procedures are used to treat angina that has not responded to more conservative treatment and utilize either the mammary artery or sections of the saphenous vein for the graft. PTS: 1 DIF: Cognitive Level: Application REF: 465 OBJ: 7 (theory) TOP: CABG and MIDCAB Surgery KEY: Nursing Process Step: Evaluation MSC: NCLEX: Safe, Effective Care Environment: Management of Care 19. The patient being evaluated for a heart transplant asks the nurse what the survival rate is. Which response is best for the nurse to make? a. “I’m not really sure. It is better if you ask your surgeon.” b. “Every patient has different circumstances, but the average 5-year survival rate is 79%.” c. “The survival rate is excellent. Almost all patients with a heart transplant live past 10 years.” d. “There are not any really good statistics for me to give you an accurate estimate.” ANS: B Identifying that individual cases vary while giving accurate statistics is the most helpful response. Stating “I’m not really sure” does not instill confidence in the nurse’s ability or knowledge. Although a significant number of patients live past 10 years following heart transplant, responding that almost all patients live past 10 years is inaccurate and instills false hope. PTS: 1 DIF: Cognitive Level: Application REF: 465 OBJ: 7 (theory) TOP: Heart Transplant KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity MULTIPLE RESPONSE 20. The nurse is caring for a 38-year-old African American patient with diabetes. The patient manages her diabetes with dietary control, takes oral contraceptives, and is a nonsmoker. Which characteristic(s) in this patient’s history increase the patient’s risk for coronary artery disease (CAD)? (Select all that apply.) a. Age b. Race c. Diabetes d. Nonsmoker status e. Use of oral contraceptives ANS: B, C, E African Americans have an ethnic tendency to CAD. Taking birth control pills and diabetes are both risk factors for CAD. Older patients are at increased risk for CAD, and a nonsmoking status decreases the likelihood of developing CAD. PTS: 1 DIF: Cognitive Level: Application REF: 450 OBJ: 1 (theory) TOP: CAD: Risk Factors KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 21. The nurse instructs a patient that the pain of angina is due to ischemia of the myocardium. Which factors are causative agents for angina? (Select all that apply.) a. Exertion b. Emotional excitement c. Eating heavy meals d. Exposure to cold e. Allergic reactions ANS: A, B, C, D Angina may be caused by exertion, emotional excitement, eating heavy meals, and exposure to cold. Angina is not brought on by allergy. PTS: 1 DIF: Cognitive Level: Comprehension REF: 457, Patient Teaching OBJ: 3 (theory) TOP: Angina: Precipitators KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 22. Which herbs and supplements lower cholesterol? (Select all that apply.) a. Garlic b. Bananas c. Oatmeal d. St. John’s wort e. Soy products ANS: A, C, E Garlic, whole-grain foods, and soy products are thought to decrease cholesterol. Bananas and St. John’s wort are not known to lower cholesterol. PTS: 1 DIF: Cognitive Level: Knowledge REF: 451, Complementary and Alternative Therapies OBJ: 3 (clinical) TOP: Hyperlipidemia: Herbal Remedies KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 23. The nurse is aware that a positive diagnosis of a myocardial infarction (MI) is based on which diagnostic test finding(s)? (Select all that apply.) a. Electrocardiographic (ECG) changes in the QRS complex b. Elevation of low-density lipoprotein (LDL) c. Elevation of troponin levels d. Elevated white blood cell (WBC) count e. Elevated bilirubin levels ANS: A, C Diagnosis of MI is made by patient history, ECG, and serum cardiac enzyme levels. Elevated LDL, WBC, or bilirubin levels are not indicative of an MI. PTS: 1 DIF: Cognitive Level: Knowledge REF: 458 OBJ: 1 (theory) TOP: MI: Diagnosis KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 24. The nurse clarifies that the MONA protocol for drug administration in the emergent stage of a myocardial infarction (MI) involves the use of which therapies? (Select all that apply.) a. Aspirin b. Morphine c. Nitrates d. Antibiotics e. Oxygen f. Anticoagulants ANS: A, B, C, E Morphine, oxygen, nitrates, and aspirin are the components of MONA therapy. Antibiotics are not part of the MONA protocol. PTS: 1 DIF: Cognitive Level: Comprehension REF: 459 OBJ: 2 (clinical) TOP: MONA Therapy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 25. The nurse encourages the patient who has had a myocardial infarction (MI) to enroll in the outpatient cardiac rehabilitation in order to receive which service(s)? (Select all that apply.) a. Nutritional counseling b. Supervised progressive exercise c. Stress reduction techniques d. Sexual counseling e. Administration of cardiotonic drugs ANS: A, B, C Cardiac rehab services include nutritional counseling, specialized exercise programs, and stress-reduction techniques. Sexual counseling and administration of medications are not services of cardiac rehab. PTS: 1 DIF: Cognitive Level: Comprehension REF: 461 OBJ: 3 (clinical) TOP: Cardiac Rehabilitation: Services KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 26. During the acute phase following a myocardial infarction (MI), the nurse anticipates that the patient may require a temporary pacemaker in which situation(s)? (Select all that apply.) a. The patient’s heart rate remains above 120 beats/min. b. The patient experiences worsening anginal pain. c. The patient experiences complete heart block. d. The patient’s systolic BP drops to 60. e. The patient’s pulse rate remains below 40 beats/min. ANS: C, E A temporary pacemaker is warranted when the patient’s pulse consistently remains below 40 beats/min and when the patient experiences complete heart block. Complete heart block means that the electrical impulse for contraction does not go through the atrioventricular node to the ventricles and the ventricles are not signaled to contract. Tachycardia, above 100, continued angina pain, and hypotension are not correct indications for a pacemaker. PTS: 1 DIF: Cognitive Level: Application REF: 461 OBJ: 6 (theory) TOP: Temporary Pacemaker KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Management of Care COMPLETION 27. The nurse uses a diagram to show how obstruction of an artery has caused an area of necrosis called a(n) _________. ANS: infarct infarction Tissue necrosis from arterial obstruction is referred to as an infarct. PTS: 1 DIF: Cognitive Level: Knowledge REF: 457 OBJ: 1 (theory) TOP: Infarct: Definition KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 28. The nurse is aware that the patient’s cardiac rehabilitation levels of physical activity are designated through ____________ units. ANS: metabolic equivalent MET One MET is the amount of oxygen needed by the body at rest. The patient’s rehabilitation program slowly progresses stepwise to higher energy expenditures over a period of months. PTS: 1 DIF: Cognitive Level: Comprehension REF: 462 OBJ: 4 (clinical) TOP: Cardiac Rehabilitation KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Management of Care MATCHING Place the events of arterial obstruction in proper sequence. a. Platelets adhere to plaque. b. Deposits of low-density lipoproteins (LDLs) accumulate. c. Fibrous plaque is laid down in vessel. d. Streaks of fatty material are laid down in arteries. e. Platelets clump. f. Platelets calcify. 29. Step 1 30. Step 2 31. Step 3 32. Step 4 33. Step 5 34. Step 6 29. ANS: D PTS: 1 DIF: Cognitive Level: Comprehension REF: 452, Figure 20-1 OBJ: 2 (theory) TOP: Thrombus Formation KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 30. ANS: B PTS: 1 DIF: Cognitive Level: Comprehension REF: 452, Figure 20-1 OBJ: 2 (theory) TOP: Thrombus Formation KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 31. ANS: C PTS: 1 DIF: Cognitive Level: Comprehension REF: 452, Figure 20-1 OBJ: 2 (theory) TOP: Thrombus Formation KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 32. ANS: A PTS: 1 DIF: Cognitive Level: Comprehension REF: 452, Figure 20-1 OBJ: 2 (theory) TOP: Thrombus Formation KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 33. ANS: E PTS: 1 DIF: Cognitive Level: Comprehension REF: 452, Figure 20-1 OBJ: 2 (theory) TOP: Thrombus Formation KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 34. ANS: F PTS: 1 DIF: Cognitive Level: Comprehension REF: 452, Figure 20-1 OBJ: 2 (theory) TOP: Thrombus Formation KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies Chapter 21: The Neurologic System deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is caring for the patient who has had an injury to the hypothalamus. Which intervention is most important for the nurse to implement? a. Closely control room temperature. b. Monitor for signs of hemorrhage. c. Protect the patient’s eyes from bright lights. d. Turn the patient hourly to maintain skin integrity. ANS: A The hypothalamus regulates body temperature; therefore, it is important to maintain adequate temperature control of the environment since the body’s ability to regulate the temperature will be affected by injury to the organ. Bleeding, photophobia, and skin integrity are not issues associated with the hypothalamus. PTS: 1 DIF: Cognitive Level: Application REF: 473, Table 21-1 OBJ: 6 (theory) TOP: Hypothalamus KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 2. The nurse differentiates the sympathetic from the parasympathetic nervous systems. Which statement about the sympathetic system is accurate? a. The sympathetic system provides energy for “fight or flight” in stressful situations. b. The sympathetic system slows the heart rate after a stressful situation. c. The sympathetic system supports deep sleep after large expenditures of energy. d. The sympathetic system relaxes blood vessels to counteract hypertension. ANS: A The sympathetic nervous system “gears up” the body for “fight or flight” situations with epinephrine that will raise the blood pressure (BP), reduce bowel motility, and energize the whole body to defend itself in a stressful situation. The parasympathetic system slows the heart rate after stress, supports deep sleep, and relaxes blood vessels. PTS: 1 DIF: Cognitive Level: Knowledge REF: 475, Table 21-3 OBJ: 2 (theory) TOP: Sympathetic Nervous System KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. The nurse is assessing an 80-year-old patient. The nurse correctly attributes the slowed knee jerk reflex with which agerelated change? a. Diminished brain cells b. Degeneration of myelin sheath c. Weakened muscles d. Irritation of nerve roots ANS: B In the peripheral nervous system (PNS), the motor nerve fibers and the myelin sheath degenerate with advancing age; reflexes may become diminished or absent with advanced age. PTS: 1 DIF: Cognitive Level: Comprehension REF: 484 OBJ: 2 (theory) TOP: PNS: Diminished Reflexes KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. A student nurse questions the nurse about the difference between a quadriplegic and a tetraplegic patient. Which statement correctly describes tetraplegia? a. Tetraplegic patients are capable of fewer fine motor movements. b. Tetraplegic patients can experience pain in paralyzed parts. c. Tetraplegic patients are more easily rehabilitated. d. Tetraplegia is the newer term for the old term quadriplegia. ANS: D Tetraplegia is the newer term for the old term quadriplegia. PTS: 1 DIF: Cognitive Level: Knowledge REF: 492 OBJ: 1 (theory) TOP: Tetraplegia vs. Quadriplegia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. The nurse is performing a neurologic assessment on a patient. Which action should the nurse take to adequately test the effectiveness for the hypoglossal nerve? a. Ask the patient to touch the tip of the tongue to each cheek. b. Check air movement through each nostril separately. c. Ask the patient to wrinkle the forehead. d. Ask the patient to shrug the shoulders. ANS: A Asking the patient to touch the tip of the tongue to each cheek (while the nurse palpates the outside of the cheek) tests the effectiveness of the hypoglossal nerve (CN XII: a cranial motor nerve responsible for tongue movement and articulation of speech). Checking air movement through each nostril separately evaluates the olfactory nerve (CN I). Asking the patient to wrinkle the forehead tests the facial nerve (CN VII). Asking the patient to shrug the shoulders tests the spinal accessory nerve (CN XI). PTS: 1 DIF: Cognitive Level: Application REF: 480, Table 21-5 OBJ: 5 (theory) TOP: Cranial Nerve Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 6. Which behavior causes the nurse to report a positive Romberg test? a. The patient cannot keep his eyes closed. b. The patient cannot touch his nose with eyes closed. c. The patient complains of dizziness. d. The patient sways from side to side. ANS: D Romberg test evaluates equilibrium. The patient stands with eyes closed and feet only slightly apart. Swaying from side to side during the Romberg test is a positive sign for impaired balance. PTS: 1 DIF: Cognitive Level: Comprehension REF: 480, Table 21-5 OBJ: 5 (theory) TOP: Romberg Test KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 7. While performing an assessment, the nurse taps a patient’s knee and observes that the quadriceps muscle reflexively contracts. How should the nurse document this finding? a. Patellar reflex 2/5 b. Patellar reflex 4/5 c. Achilles reflex 2/5 d. Achilles reflex 4/5 ANS: A This action describes a normal patellar reflex. The knee jerk, or patellar reflex, tests nerve pathways to and from the spinal cord at the level of the second through fourth lumbar nerves. When the knee is tapped, the nerve that receives this stimulus sends an impulse to the spinal cord, where it is relayed to a motor nerve. This causes the quadriceps muscle at the front of the thigh to contract and to move the leg upward. This reflex, or simple reflex arc, involves only two nerves and one synapse. The leg begins to jerk up while the brain is just becoming aware of the tap on the knee. Reflexes are graded as follows: 0/5 = absent; 1/5 = weak response; 2/5 = normal; 3/5 = exaggerated response; and 4/5 = hyperreflexia with clonus. PTS: 1 DIF: Cognitive Level: Application REF: 484 OBJ: 5 (theory) TOP: Reflex: Definition KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 8. The nurse interprets the physician’s finding of a grade of 2/5 on the Achilles tendon to mean what has occurred? a. Hyperreflexive response for the fifth and sixth cervical nerves b. Exaggerated response for the seventh and eighth cervical nerves c. Normal response for the first and second sacral nerves d. Weak response for the second through the fourth lumbar nerves ANS: C A score of 2/5 is a normal grade. The Achilles tendon reflex or ankle jerk reflex evaluates the first and second sacral nerves. PTS: 1 DIF: Cognitive Level: Comprehension REF: 484 OBJ: 5 (theory) TOP: Reflexes: Grading KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 9. Which reflex indicates an abnormality in the motor control pathways from the cerebral cortex? a. Babinski reflex b. Biceps reflex c. Brachioradialis reflex d. Knee jerk reflex ANS: A A positive Babinski reflex indicates an abnormality in the motor pathways from the cerebral cortex. PTS: 1 DIF: Cognitive Level: Knowledge REF: 484, Figure 21-7 OBJ: 1 (theory) TOP: Babinski Reflex KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 10. The nurse is caring for a patient with a head injury. Over a time span of 30 minutes, the nurse observes the following vital signs changes: temperature from 97° to 98° F; pulse from 86 to 78 beats/min; respirations from 18 to 14 breaths/min; and blood pressure from 140/86 to 150/82. Which action is most important for the nurse to take? a. Notify the physician immediately. b. Document the findings. c. Determine the patient’s Glasgow Coma Scale (GCS) score. d. Observe pupils for size, equality, and reactivity. ANS: A An increasing temperature, decreasing pulse and respirations, and a widening pulse pressure are indicative of increasing intracranial pressure (ICP). Any identified change must be reported to the provider promptly. The nurse should also observe the pupils for any changes, determine the patient’s GCS score, and document the findings. PTS: 1 DIF: Cognitive Level: Analysis REF: 485 OBJ: 6 (theory) TOP: Increasing ICP KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 11. The patient is caring for a patient who spontaneously opens his eyes, localizes pain, and carries out confused conversation. The nurse correctly documents which Glasgow Coma Scale (GCS) rating for this patient? a. 12 b. 13 c. 14 d. 15 ANS: B The GCS is used to evaluate a patient’s neurologic functioning and level of consciousness. Scores range from 3 to 15 points. The higher the score, the higher the level of consciousness. Spontaneous eye movement (4 points), localizing pain (5 points), and confused conversation (4 points) total a GCS rating of 13. PTS: 1 DIF: Cognitive Level: Application REF: 486, Table 21-7 OBJ: 3 (clinical) TOP: GCS KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 12. The nurse is caring for a patient who requires neurologic checks. When performing an assessment, how should the nurse best evaluate the patient’s thinking? a. Ask the patient to add three numbers together in his head. b. Ask the patient to identify the name of the present month. c. Ask the patient what he would do in the event of a fire. d. Ask the patient what the last major holiday was. ANS: A Thinking can be evaluated by asking the patient to add three numbers together; to count by 6s; or to solve a simple puzzle. Asking the patient to identify the name of the present month evaluates orientation. Asking the patient what he would do in a fire evaluates judgment. Asking the patient to name the last major holiday assesses for memory lapses. PTS: 1 DIF: Cognitive Level: Application REF: 486 OBJ: 5 (theory) TOP: Assessment of Thinking KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 13. The nurse is performing a neurologic assessment on a newly admitted patient with a head injury. Which sign best indicates that the patient may have experienced a brainstem injury? a. Nystagmus b. Decerebrate posturing c. Seizure activity d. Glasgow Coma Scale score of 3 ANS: B The appearance of decerebrate, as well as decorticate, posturing is an indicator of brainstem injury. Nystagmus, seizures, and a GCS score of 3 are not necessarily signs of brainstem injury. PTS: 1 DIF: Cognitive Level: Application REF: 487, Figure 21-10 OBJ: 6 (theory) TOP: Brainstem Injury: Decerebrate Posturing KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 14. The nurse is assessing muscle strength in a fully conscious patient as part of a neurologic assessment. Which technique should the nurse employ? a. Press down on the patient’s extended arms one at a time while the patient attempts to raise the arm. b. Apply pressure above the eye and push upward while the patient attempts to remove the hand. c. Pinch the trapezius muscle at the angle of the shoulder and neck while twisting the fingers slightly. d. Rub the sternum with fisted knuckles in a twisting motion while the patient attempts to remove the fist. ANS: A To test muscle strength, have the patient extend her arms in front of her, and press down on each arm one at a time, while asking her to try to raise her arm. Applying pressure above the eye, pinching the trapezius muscle, or employing a sternal rub tests the degree of unconsciousness in a patient (and does not include asking the patient to attempt to remove the hand). PTS: 1 DIF: Cognitive Level: Application REF: 487 OBJ: 2 (clinical) TOP: Neuro Check KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 15. When feeding a patient with dysphagia with a left-sided hemiplegia, how should the nurse position the patient? a. Side-lying on the right side b. Semi-Fowler c. High Fowler d. Upright at a table in a wheelchair ANS: C High Fowler is the most comfortable and safe position. Sitting upright at a table may prove stressful because of weakness and impaired balance. PTS: 1 DIF: Cognitive Level: Application REF: 494 OBJ: 6 (theory) TOP: Dysphagia KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 16. Bladder training begins with scheduling the patient’s toileting in what time increment? a. Every hour b. Every 2 hours c. Every 4 hours d. Every 6 hours ANS: B Bladder training begins with toileting the patient every 2 hours. PTS: 1 DIF: Cognitive Level: Knowledge REF: 494 OBJ: 6 (theory) TOP: Bladder Training KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 17. A patient is admitted to the hospital to rule out the possibility of bacterial meningitis. Which test will be most helpful in diagnosing this condition? a. Magnetoencephalography (MEG) b. Myelography c. Cerebral angiography d. Lumbar puncture for cerebrospinal fluid (CSF) analysis and culture ANS: D A lumbar puncture is performed to remove a sample of CSF to detect abnormalities that are indicative of specific neurologic problems and determine which organism is responsible for an infection such as bacterial meningitis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 480, Table 21-6 OBJ: 4 (theory) TOP: Diagnostic Testing: Lumbar Puncture KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation MULTIPLE RESPONSE 18. The patient scheduled for a PET (positron emission tomography) scan of the brain asks if there is any special preparation for the test. The nurse correctly responds with which statement(s)? (Select all that apply.) a. “There is no special preparation involved with this test since it is noninvasive.” b. “You should avoid any tranquilizers or sedatives the night before and the day of the test.” c. “You will need to sign a consent form for this test to be performed.” d. “You will have two IVs inserted for the examination.” e. “You should wait to empty your bladder once the test is completed.” ANS: B, C, D During a PET scan, radioactive material is given through an intravenous (IV) line and provides differing color in areas of cellular activity. A consent form is required because this is an invasive test, and tranquilizers and sedatives should be avoided because this PET scan is of brain activity. The test requires insertion of two IVs. Obviously, special preparation is indicated, and the patient should empty his bladder before the test begins. PTS: 1 DIF: Cognitive Level: Application REF: 483, Table 21-6 OBJ: 5 (theory) TOP: Diagnostic Tests: PET KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 19. The loss of neurons in the autonomic nervous system (ANS) of the older adult will cause the older adult to take longer to complete which action(s)? (Select all that apply.) a. Recuperate from an illness b. Apply brakes to stop a car c. Form words into sentences d. Climb stairs e. Learn new material ANS: A, B Recuperation and response times are lengthened with the loss of neurons from the ANS. Taking longer to form words into sentences and learn new material result from mentation loss, and taking longer to climb stairs results from decreased strength. PTS: 1 DIF: Cognitive Level: Application REF: 478 OBJ: 6 (theory) TOP: ANS: Age-Related Changes KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 20. Which statement(s) provide examples of ways in which individuals may be proactive in reducing neurologic injuries? (Select all that apply.) a. Refusing to start the car until all seat belts are buckled. b. Requiring children to wear bike helmets. c. Reminding swimmers to test water depth before diving. d. Encouraging use of hard hats at industrial sites. e. Discouraging recreational drug use. ANS: A, B, C, D, E All options would be supportive of the reduction of CNS injury. PTS: 1 DIF: Cognitive Level: Knowledge REF: 479, Health Promotion OBJ: 3 (theory) TOP: CNS Disorders: Prevention KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 21. The FOUR (Full Outline of UnResponsiveness) tool is based on the assessment of which components? (Select all that apply.) a. Eye response b. Motor response c. Brainstem response d. Respiratory function e. Reflex response ANS: A, B, C, D The FOUR outline evaluates eye response, motor response, brainstem response, and respiratory function. Reflex response is not part of the assessment tool. PTS: 1 DIF: Cognitive Level: Knowledge REF: 486 OBJ: 1 (theory) TOP: FOUR Assessment Tool KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 22. The nurse performs a reflex test on a newly admitted adult patient. The nurse runs a tongue blade along the sole of the foot and the patient responds with the great toe bending backward (upward) and the smaller toes fanning outward. These findings cause the nurse to suspect that the patient may have experienced which problem(s)? (Select all that apply.) a. Injury to the central nervous system (CNS) that resulted in an abnormality in the motor control pathways leading from the cerebral cortex b. Myocardial infarction that resulted in hypoxemia c. Influence of chemical substances d. Damage to the peripheral nervous system (PNS) e. Trauma to the hypothalamus ANS: A, C This response in the adult indicates a positive Babinski reflex, indicative of an abnormality in the motor control pathways leading from the cerebral cortex, or from the influence of chemical substances. Hypoxemia, damage to the PNS, and trauma to the hypothalamus would not cause a positive Babinski reflex. PTS: 1 DIF: Cognitive Level: Application REF: 484, Figure 21-7 OBJ: 6 (theory) TOP: Assessment: Babinski Reflex KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation COMPLETION 23. The component of the peripheral nervous system (PNS) that carries the impulse to the central nervous system (CNS) is the ____________ impulse. ANS: afferent The afferent impulse carries the impulse to the CNS from the PNS. PTS: 1 DIF: Cognitive Level: Knowledge REF: 472 OBJ: 1 (theory) TOP: PNS: Afferent Impulse KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 24. There are _______ cranial nerves that control the sensory and motor activities of the body. ANS: 12 twelve There are 12 cranial nerves that control the sensory and motor activities of the body. PTS: 1 DIF: Cognitive Level: Knowledge REF: 475, Table 21-2 OBJ: 5 (theory) TOP: Cranial Nerves KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 25. When documenting pupillary response that is normal, the acceptable abbreviation is _______. ANS: PERRLA perrla PERRLA (Pupils Equally Round and Reactive to Light with Accommodation) is an acceptable and recognizable abbreviation of an assessment of pupillary response. PTS: 1 DIF: Cognitive Level: Comprehension REF: 488 OBJ: 5 (theory) TOP: Pupillary Response: PERRLA KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 26. A neurologically damaged patient who cannot interpret communication directed to him is said to have ____________ aphasia. ANS: receptive The person who cannot interpret communication is said to have receptive aphasia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 496 OBJ: 6 (clinical) TOP: Receptive Dysphasia KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 27. During a physical assessment of the neurologic system, the nurse checks the patient’s __________, which is built into the nervous system and does not need the intervention of conscious thought to take place. ANS: reflex A reflex is an automatic response (an action or movement) that is built into the nervous system and does not need the intervention of conscious thought to take place. (The knee jerk is an example of the simplest type of reflex.) PTS: 1 DIF: Cognitive Level: Comprehension REF: 475 OBJ: 5 (theory) TOP: Assessment: Reflex KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation MATCHING The degree of consciousness in an otherwise unresponsive patient can be assessed by the use of progressive painful stimuli. Arrange the painful stimuli in the appropriate sequence of their application. a. Press on the orbital notch. b. Press the mandibular angle. c. Shake gently. d. Rub sternum. e. Pinch trapezius. 28. Step 1 29. Step 2 30. Step 3 31. Step 4 32. Step 5 28. ANS: C PTS: 1 DIF: Cognitive Level: Application REF: 487 OBJ: 5 (theory) TOP: Assessment: Painful Stimuli KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 29. ANS: A PTS: 1 DIF: Cognitive Level: Application REF: 487 OBJ: 5 (theory) TOP: Assessment: Painful Stimuli KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 30. ANS: E PTS: 1 DIF: Cognitive Level: Application REF: 487 OBJ: 5 (theory) TOP: Assessment: Painful Stimuli KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 31. ANS: B PTS: 1 DIF: Cognitive Level: Application REF: 487 OBJ: 5 (theory) TOP: Assessment: Painful Stimuli KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 32. ANS: D PTS: 1 DIF: Cognitive Level: Application REF: 487 OBJ: 5 (theory) TOP: Assessment: Painful Stimuli KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation Chapter 22: Care of Patients with Head and Spinal Cord Injuries deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse describes a concussion as a closed head injury in which: a. The brain tissue is bruised. b. No loss of consciousness occurs. c. There is amnesia related to the incident. d. There are no subsequent symptoms. ANS: C A concussion is a closed head injury in which there is a brief disruption of consciousness, amnesia, and subsequent headaches that may last for several weeks. PTS: 1 DIF: Cognitive Level: Comprehension REF: 501, Figure 22-1 OBJ: 1 (theory) TOP: Concussion: Pathophysiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. Why is the older adult more at risk for a cranial bleed following a head injury? a. The older adult’s brain is smaller, which allows for more movement inside the cranium. b. The older adult’s brain features fragile vessels more likely to rupture. c. The older adult’s brain contains less cerebrospinal fluid (CSF) to cushion the brain. d. The older adult’s brain has less flexible meninges to absorb impact. ANS: A The brain atrophies with age and does not take up as much space in the cranial vault. This change allows for more movement and more potential for torn vessels and contusions on the brain when an accident occurs that involves a head injury. PTS: 1 DIF: Cognitive Level: Comprehension REF: 501, Older Adult Care Points OBJ: 6 (theory) TOP: Cranial Bleed: Older Adult KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. The emergency room nurse is assessing a newly admitted patient with a head injury. The nurse observes clear drainage from the nose. Which action should the nurse perform first? a. Document the presence of rhinorrhea. b. Inform the physician of the assessment. c. Test the fluid with a Dextrostix. d. Tape a drip pad under the nose. ANS: C Head injury symptoms may include rhinorrhea (fluid from the nose) or otorrhea (fluid from the ear), among many others. Rhinorrhea and otorrhea should be tested to determine if there is a cerebrospinal fluid (CSF) leak. Testing with a Dextrostix will determine whether glucose is present; the presence of glucose indicates CSF. Documentation, informing the physician, and applying a drip pad under the nose are actions that should occur after confirmation of the fluid type. PTS: 1 DIF: Cognitive Level: Analysis REF: 502 OBJ: 1 (theory) TOP: Rhinorrhea KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 4. In assessing the patient with a significant right intracerebral hemorrhage, the nurse anticipates that the patient will demonstrate which signs? a. Left-sided hemiplegia with dilated right pupil b. Right-sided hemiplegia with brisk right pupil response c. Bilateral motor hemiplegia with bilaterally dilated pupils d. Left-sided hemiplegia and bilateral PERRLA ANS: A An acute intracerebral bleed causing hematoma formation is accompanied by unconsciousness, hemiplegia on the contralateral (opposite) side, and a dilated pupil on the ipsilateral (same) side. However, the symptoms indicating a slow buildup of pressure within the skull are more subtle and less easily detected. PTS: 1 DIF: Cognitive Level: Application REF: 502 OBJ: 2 (theory) TOP: Closed Head Injury: Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. The nurse is caring for an older adult patient who was admitted to the hospital following a closed head injury that resulted in a 5-minute period of unconsciousness. The nurse most carefully monitors the patient for which change? a. Increasing respiratory rate b. Decreasing heart rate c. Decreasing pulse pressure d. Decreasing level of consciousness (LOC) ANS: D Assessment of LOC provides the greatest amount of information about neurologic condition. A reduction in LOC may signal the onset of complications in the patient who has had a head injury. PTS: 1 DIF: Cognitive Level: Application REF: 501, Older Adult Care Points OBJ: 2 (theory) TOP: Epidural Hematoma: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 6. The patient with a suspected subdural hematoma is on an intravenous (IV) drip of mannitol infusing at 50 mL/hr. The nurse explains that the slow infusion rate is essential for what purpose? a. To ensure effectiveness of the drug. b. To avoid fluid overload. c. To maintain electrolyte balance. d. To maintain adequate blood pressure (BP). ANS: B The slow infusion rate will not cause fluid overload, which would add to the possibility of increased intracranial pressure (ICP). PTS: 1 DIF: Cognitive Level: Comprehension REF: 503 OBJ: 3 (theory) TOP: Diuretic Drip: Mannitol KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 7. Following a craniotomy to relieve increased intracranial pressure (ICP), which implementation should the nurse implement? a. Elevate the head of the bed 20 to 30 degrees. b. Place drip pad or cotton to absorb cerebrospinal fluid (CSF) drainage from the nose or ears. c. Stimulate the patient to better assess changing level of consciousness (LOC). d. Reposition the patient frequently for comfort. ANS: A A patent airway must be secured, and the head raised 20 to 30 degrees with the body in correct alignment. Elevation helps reduce ICP. Neurologic signs are monitored closely. An IV line is inserted for access for diuretic drugs, if needed, and for administration of fluid. IV fluids are infused very slowly to prevent fluid overload that would increase the ICP. Diuretics are used to decrease vascular volume and keep ICP as low as possible. Drip pads, patient stimulation, and changing positions frequently may increase ICP. PTS: 1 DIF: Cognitive Level: Application REF: 503 OBJ: 2 (theory) TOP: Cranial Surgery: Postoperative Care KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 8. The unconscious patient with a closed head injury is on mechanical ventilation. To improve brain perfusion through increased blood pressure, the carbon dioxide (CO2) should be maintained at what level? a. 10 to 15 mm Hg b. 15 to 20 mm Hg c. 20 to 25 mm Hg d. 25 to 30 mm Hg ANS: D The CO2 level is set to be maintained at 25 to 30 mm Hg to create vascular constriction, raise blood pressure, and perfuse the cerebrum. PTS: 1 DIF: Cognitive Level: Comprehension REF: 508 OBJ: 4 (theory) TOP: Carbon Dioxide Level on Mechanical Ventilation KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 9. The nurse is caring for a patient with a closed head injury. Which finding causes the nurse to suspect that the patient has developed diabetes insipidus (DI)? a. Increased lethargy b. Widening pulse pressure c. Copious pale urine output d. Increasing blood glucose levels ANS: C A large increase in urinary output of pale urine with a low specific gravity is the clue to the development of DI related to edema of the posterior pituitary. Antidiuretic hormone is released in inadequate amounts, resulting in polyuria, and the awake patient may complain of polydipsia (excessive thirst). IV vasopressin and fluid replacement are the preferred treatments. Lethargy and increased pulse pressure are not typical signs of DI. Increased serum glucose levels is a sign of diabetes mellitus, not DI. PTS: 1 DIF: Cognitive Level: Application REF: 509 OBJ: 1 (theory) TOP: Development of Diabetes Insipidus KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 10. Which position is best for an unconscious patient with a right-sided closed head injury? a. High Fowler b. Right side-lying c. Flat with small pillow under head d. Head of bed 20 to 30 degrees ANS: D Keeping the head of the bed 20 to 30 degrees with the body in good alignment will help reduce intracranial pressure and keep the airway patent. PTS: 1 DIF: Cognitive Level: Knowledge REF: 503 OBJ: 4 (theory) TOP: Closed Head Injury: Positioning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 11. The nurse is caring for a patient with a neurologic injury who is awake. On assessment, the patient displays mild disorientation to surroundings and time and needs additional verbal cues to stimulate response to commands. The nurse correctly documents the patient’s level of consciousness (LOC) by using which term? a. Alert b. Confused c. Lethargic d. Obtunded ANS: B The confused patient is awake, but slightly confused and needs coaching to respond to commands. Alert indicates appropriate response to questions and commands with little stimulation. Lethargic is described as the patient being drowsy, but easily aroused. Obtunded patients are more difficult to arouse and respond slowly to stimulation. PTS: 1 DIF: Cognitive Level: Application REF: 502, Box 22-1 OBJ: 2 (clinical) TOP: LOC Discrimination KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 12. The nurse is caring for an adolescent who has lower limb paralysis after sustaining a spinal injury yesterday. The patient’s anxious mother asks if the paralysis is permanent. Which response is most appropriate for the nurse to make? a. “It is possible that motor function may or may not return after spinal cord swelling has subsided.” b. “Motor function may improve, but there will always be a deficit.” c. “In all likelihood, the paralysis will be permanent.” d. “Have you asked the physician about your concerns?” ANS: A Until spinal cord edema has subsided, the extent or the permanency of the paralysis cannot be evaluated. It would be incorrect to indicate that there will definitely be a deficit or paralysis. Not addressing the question and suggesting only to talk to the physician will likely frighten the parent. PTS: 1 DIF: Cognitive Level: Application REF: 521 OBJ: 7 (theory) TOP: Spinal Cord Edema KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 13. The nurse is caring for a patient with flaccid paralysis after sustaining a spinal cord injury 3 days earlier. The family excitedly notifies the nurse that the patient has flexed his arm. Which response is best for the nurse to make? a. “I will give the doctor this wonderful news.” b. “Avoid directly touching the arm muscles so that you don’t cause more muscle spasms.” c. “This movement means that the spinal cord is adjusting to the injury.” d. “These muscles spasms are a type of involuntary movement that happens frequently in patients with spinal cord injuries.” ANS: D The patient is experiencing the spastic phases of paralysis that occurs as the cord adjusts to injury. The family members may interpret these spasms as a return of voluntary limb function and an indicator of impending complete recovery. First, the nurse should explain that this movement is not purposeful and an expected finding that often occurs in patients with spinal cord injuries. The nurse should not describe this finding as wonderful news. While it is important to avoid stimulating spasms when moving the patient and the technique involves avoiding direct contact with the muscles, the family could misunderstand the nurse’s teaching as an accusation that someone’s touch caused this movement. While the spinal cord is adjusting to injury, this statement is vague enough that the family may not realize that the movement is not purposeful. PTS: 1 DIF: Cognitive Level: Application REF: 514 OBJ: 8 (theory) TOP: SCI Patient: Muscle Spasms KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 14. The nurse is caring for a patient with spastic paralysis. Which technique is most appropriate for the nurse to use when moving the patient? a. Firmly grasp the muscles. b. Use the palms of hands to support the joints. c. Log roll the patient as a unit. d. Perform passive range-of-motion (ROM). ANS: B Spastic paralysis features involuntary skeletal muscle contractions. These muscle spasms may be violent enough to throw the patient from the bed or wheelchair and must be anticipated, and the patient must be secured so that accidents can be avoided. To avoid stimulating the muscles when moving the patient and thereby precipitating a spasm of the muscles, the nurse should avoid grasping the muscle itself. Instead, the nurse should use the palms of the hands to support the joints above and below the affected muscles. Firmly grasping the muscles, log rolling, and ROM may initiate spasms. PTS: 1 DIF: Cognitive Level: Application REF: 514 OBJ: 8 (theory) TOP: Muscle Spasm: Prevention KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 15. The nurse is caring for a patient with a spinal cord injury who develops autonomic dysreflexia (AD). Which action is most important for the nurse to take first? a. Elevate the head of the bed. b. Notify the charge nurse. c. Decrease the IV fluid rate. d. Administer antihypertensive medication. ANS: A AD (hyperreflexia) response is potentially dangerous to the patient, because it can produce vasoconstriction of the arterioles with an immediate elevation of blood pressure. Elevating the head of bed is the initial intervention to decrease the rising blood pressure. The nurse should notify the charge nurse and the physician. The IV fluids can be decreased but are not the most important intervention. The vital signs should be obtained and the cause of AD should be addressed before administering any hypertensive medication. PTS: 1 DIF: Cognitive Level: Analysis REF: 516 OBJ: 8 (theory) TOP: Autonomic Dysreflexia: Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 16. When turning the patient who is in Crutchfield tongs traction, the nurse should employ which technique? a. Turn the patient as a unit by log rolling. b. Release the weights to prevent injury while turning. c. Turn the patient quickly to avoid muscle spasms. d. Advise the patient to hold his breath and bear down during turning. ANS: A Turning the patient as a unit by log rolling with the weights in place immobilizes the affected vertebrae and maintains alignment. Releasing the weights or turning quickly will affect vertebrae and alignment. Deep breathing will decrease muscle tension. PTS: 1 DIF: Cognitive Level: Application REF: 513 OBJ: 8 (theory) TOP: Crutchfield Tongs: Turning KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 17. A patient presents to the health clinic with low back pain that radiates into the buttocks and below the knee. The nurse suspects which condition? a. Herniated disk b. Muscle spasm in lower back c. Spinal cord injury d. Sciatica ANS: A Herniated disks typically cause compression on the sciatic nerve and allow the pain to radiate into the buttocks and leg. Muscle spasm in the lower back will result in back pain. There is no indication of spinal cord injury. Pain from sciatica does not involve back pain. PTS: 1 DIF: Cognitive Level: Comprehension REF: 518 OBJ: 9 (theory) TOP: Herniated Disk: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 18. The student nurse is planning care for a patient with a recent spinal cord injury. Which intervention indicates that the student nurse requires further instruction regarding appropriate care for this patient? a. Keep the halo jacket fastened unless the patient is in a supine position. b. Monitor the bladder every 4 hours for signs of bladder distention. c. Instruct unlicensed assistive personnel (UAP) to turn and reposition the patient every 2 hours. d. Assess compression stockings for proper fit. ANS: C Moving or positioning the patient with neurologic injury or surgery should not be delegated to unlicensed personnel. Following proper instruction, the UAP can assist the nurse with moving or repositioning the patient. Halo jackets must be kept fastened unless the patient is in a supine position in order to prevent sudden head movement. Bladder distention should be avoided to prevent infection or autonomic dysreflexia. Compression stockings are used to prevent deep vein thrombosis. PTS: 1 DIF: Cognitive Level: Application REF: 517, Assignment Considerations OBJ: 3 (clinical) TOP: Spinal Cord Injury Care KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Management of Care MULTIPLE RESPONSE 19. The nurse uses a visual aid to demonstrate how a coup-contrecoup injures the brain. Which information should the nurse include? (Select all that apply.) a. These injuries allow the brain to twist on the brainstem. b. These injuries cause the brain to move forward to strike the anterior interior skull. c. These injuries allow the brain to compress on itself. d. These injuries cause the brain to strike the bony area opposite of the site of impact. e. These injuries cause the brain to lose small amounts of cerebrospinal fluid. ANS: B, D In a coup-contrecoup injury, the brain moves forward, striking the anterior interior wall of the cranium, and moves back, striking the bony area opposite the site of the impact, causing two areas of injury. PTS: 1 DIF: Cognitive Level: Application REF: 501, Figure 22-1 OBJ: 1 (theory) TOP: Coup-Contrecoup: Pathophysiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 20. After an older adult falls, the nurse suspects the development of a subdural hematoma based on which finding(s)? (Select all that apply.) a. Increasing irritability b. Complaint of a dull headache c. Frequent “nodding off” in chair during the day d. Focal seizures e. Staggering gait ANS: A, B, C Increasing irritability and complaint of headache as well as changing level of consciousness are signs of increasing intracranial pressure. Seizures and staggering gait are not specifically indicative of subdural hematoma. PTS: 1 DIF: Cognitive Level: Application REF: 501 OBJ: 2 (theory) TOP: Subdural Hematoma: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 21. The nurse documents which sign(s) of epidural hematoma in a patient with a closed head injury? (Select all that apply.) a. Mottling of extremities b. Periorbital ecchymosis c. Battle sign d. Nausea and vomiting e. PERRLA ANS: B, C, D Raccoon eyes (periorbital ecchymosis), bruising behind the ears (Battle sign), and nausea and vomiting are some of the typical signs of epidural hematoma. PTS: 1 DIF: Cognitive Level: Comprehension REF: 502 OBJ: 2 (theory) TOP: Epidural Hematoma: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 22. The nurse is aware that an epidural hematoma warrants immediate intervention based on which criteria? (Select all that apply.) a. An epidural hematoma is related to bleeding from arterial venous source. b. An epidural hematoma can increase intracranial pressure (ICP) quickly. c. An epidural hematoma changes overall condition quickly. d. An epidural hematoma can cause death. e. An epidural hematoma can cause irreversible brain damage. ANS: B, C, D, E An epidural hematoma can increase ICP quickly, changes overall condition quickly, and can cause death or irreversible brain damage. Bleeding is related to an arterial source. An epidural hematoma is a medical emergency. PTS: 1 DIF: Cognitive Level: Comprehension REF: 501 OBJ: 2 (theory) TOP: Epidural Hematoma: Complications KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 23. The nurse is caring for a patient with a complete transection of the cord at C7. The patient asks the nurse what functions he will be able to perform. The nurse responds that the patient will most likely be able to perform which activities? (Select all that apply.) a. Transferring himself b. Dressing himself c. Using a wheelchair with standard hand rims d. Feeding himself e. Typing using all digits ANS: A, B, C, D With physical and occupational therapy, the patient may be able to transfer himself, dress and feed himself, and use a wheelchair with standard hand rims. The patient with an injury at C7 does not have full control of all digits. The third finger is the most functional. PTS: 1 DIF: Cognitive Level: Application REF: 512, Table 22-1 OBJ: 8 (theory) TOP: Cord Injury: C7 KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 24. The nurse is caring for a patient with (AD). The nurse should assess the patient for which conditions or situations? (Select all that apply.) a. Distended bladder b. Constipation c. Increased fluid intake d. Wrinkles in bed linens e. Abrupt environmental temperature changes ANS: A, B, D, E Bladder distention, constipation, wrinkled bed linens, and temperature changes are potential triggers for AD that the nurse should assess for. This condition causes a rapid increase in blood pressure. Increased fluid intake is not relevant to AD. PTS: 1 DIF: Cognitive Level: Comprehension REF: 514 OBJ: 8 (theory) TOP: Autonomic Dysreflexia: Etiology KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 25. The nurse is evaluating the patient to determine if adequate learning has occurred regarding care of lower back pain. Which activities indicate that the patient adequately understands the nurse’s teaching? (Select all that apply.) a. The patient carries items away from the center of the body. b. The patient bends the knees, with the back straight, and crouches to lift an item off the floor. c. The patient uses a lumbar pillow or roll when sitting for long periods. d. The patient performs proper back exercises twice a day. e. The patient maintains proper body weight. ANS: B, C, D, E Bending the knees with a straight back while crouching to lift an item off the floor, using a lumbar pillow or roll when sitting for long periods, exercising twice a day, and maintaining proper body weight are actions that indicate correct lower back care. The patient should carry items close to the center of the body rather than away from the center of the body. PTS: 1 DIF: Cognitive Level: Application REF: 521, Patient Teaching OBJ: 4 (clinical) TOP: Low Back Pain: Self-Care Measures KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance COMPLETION 26. The nurse is aware that increasing intracranial pressure can cause _____________ of the brain, which results in the brain impinging on the brainstem. ANS: herniation When the brain is under unreduced pressure, it can herniate through the notch of the tentorium and impinge on the brainstem. PTS: 1 DIF: Cognitive Level: Knowledge REF: 506 OBJ: 5 (theory) TOP: Herniation: Etiology KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 27. If conservative measures are unsuccessful in treating a herniated disk, a(n) __________ may be necessary to remove the posterior arch of the vertebrae, along with the disk. ANS: diskectomy laminectomy A diskectomy or laminectomy is performed to decompress the nerve root when other, less invasive, methods of treatment are not successful. PTS: 1 DIF: Cognitive Level: Comprehension REF: 519 OBJ: 9 (theory) TOP: Herniated Disk KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation Chapter 23: Care of Patients with Disorders of the Brain deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is caring for a patient who recently suffered a cerebrovascular accident (CVA). Family members ask the nurse why their father had a seizure. Which response is best for the nurse to make? a. “The seizure was most likely caused by brain cells being deprived of oxygen due to a blood clot in the brain.” b. “The stroke generated a toxin that excites the brain cells.” c. “The stroke causes an alteration in the cells adjacent to the blood clot.” d. “The stroke causes an increase in the depolarization of the brain cells due to the clot formation.” ANS: A Thrombi from a CVA can occlude vessels, cutting off oxygen supply to cells of the brain and causing a seizure. PTS: 1 DIF: Cognitive Level: Comprehension REF: 524 OBJ: 2 (theory) TOP: Seizure: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. The nurse is providing teaching to a patient newly diagnosed with simple partial seizure disorder. Which statement by the nurse is most accurate? a. “Your seizures will typically only affect one side of your body.” b. “Simple partial seizures may result in an alteration of consciousness.” c. “The simple partial seizure may cause motor impairment to begin in all of your extremities.” d. “Simple partial seizures are not treatable.” ANS: A Simple partial seizures only involve one side of the brain and one side of the body. Complex partial seizures may or may not result in an alteration in level of consciousness. Generalized seizures affect both sides of the body. Simple partial seizures may respond to treatment. PTS: 1 DIF: Cognitive Level: Application REF: 525 OBJ: 1 (theory) TOP: Simple Partial Seizures KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. The nurse is caring for an anxious 20-year-old college student who just suffered his first seizure in his dorm room. The patient asks the nurse if he is now an epileptic. What is the nurse’s best response? a. “No. All other causes of seizure activity must be ruled out before the diagnosis of epilepsy is made.” b. “Yes, but you may never have another seizure since it has just now manifested itself.” c. “No, but you should see a physician to get a prescription for a preventative antispasmodic.” d. “Yes. All seizures are considered to be epilepsy.” ANS: A Epilepsy diagnosis is made after all other causes of seizure activity have proven negative. All seizures are not considered to be epilepsy. PTS: 1 DIF: Cognitive Level: Comprehension REF: 525 OBJ: 1 (clinical) TOP: Seizures vs. Epilepsy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 4. The nurse instructs a person taking phenytoin (Dilantin) that periodic blood tests will be necessary. The nurse explains that the laboratory checks will monitor for which potential medication-induced change? a. Potassium depletion b. Liver damage c. Increasing creatinine d. Increasing sedimentation rates ANS: B Periodic blood tests are recommended for people taking phenytoin to monitor for liver damage. PTS: 1 DIF: Cognitive Level: Comprehension REF: 549 OBJ: 1 (clinical) TOP: Phenytoin: Adverse Effects KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 5. The nurse is assessing a patient on intravenous (IV) phenytoin (Dilantin). Which assessment finding is most concerning to the nurse? a. Blood pressure (BP) 138/92 b. Frequent hiccups c. Irregular apical pulse d. Nausea and vomiting ANS: C IV phenytoin can cause cardiac arrhythmias and hypotension, especially if given faster than 50 mg/min. PTS: 1 DIF: Cognitive Level: Analysis REF: 527, Clinical Cues OBJ: 1 (theory) TOP: Phenytoin: Adverse Effects KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 6. The nurse is providing medication teaching to a patient with epilepsy who is taking phenytoin (Dilantin). Which statement best indicates that the nurse’s teaching has been successful? a. “I should decrease my alcohol intake to a single drink per day.” b. “I should visit the dentist every 3 to 6 months while taking this medication.” c. “I should take my antacid an hour after my Dilantin.” d. “This medication may turn my urine orange.” ANS: B Dilantin can cause gingival hyperplasia. The patient should brush teeth and floss regularly, and schedule dentist visits every 3 to 6 months. Alcohol interferes with the metabolism of anticonvulsants, increases lethargy, and may trigger seizures. The patient should not consume alcohol at all while taking Dilantin. The patient should not take antacids within 2 hours of taking Dilantin. Dilantin may turn the urine pink. PTS: 1 DIF: Cognitive Level: Application REF: 526, Box 23-1, 532, Table 23-1OBJ: 1 (theory) TOP: Phenytoin: Patient Teaching KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 7. The nurse reinforces the information given by the physician that endarterectomy as an intervention for stroke prevention is reserved for people who have carotid obstruction of greater than what percentage? a. 30% b. 40% c. 50% d. 60% ANS: D Endarterectomy is reserved for people with carotid obstruction of more than 60%. PTS: 1 DIF: Cognitive Level: Knowledge REF: 529 OBJ: 4 (theory) TOP: Endarterectomy: Guidelines KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 8. The dysarthric patient seated in the dining room of the long-term care facility yells, “Poon! Poon! Poon!” with increasing frustration. What is the nurse’s best response? a. “Slow down so that I can understand what you are saying.” b. “Are you asking for a spoon?” c. “Not being able to speak is frustrating.” d. “If you tell me what you want, I will get it.” ANS: B Attempting to interpret the dysarthric communication through questions that can be answered simply will reduce frustration. PTS: 1 DIF: Cognitive Level: Application REF: 533 OBJ: 4 (theory) TOP: Stroke: Dysarthria KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 9. The nurse is assisting a patient with agnosia after a CVA. Which intervention is most appropriate? a. Showing the patient a spoon while calling it by name and describing its purpose. b. Moving the patient’s hand with a toothbrush in repetitive motion to brush teeth. c. Describing the placement of food on the plate. d. Providing an adaptive fork to enhance self-feeding. ANS: A Identifying objects and their intended use is helpful to people with agnosia who can no longer recognize items. The other options are helpful to people with apraxia, hemianopsia, and altered coordination, respectively. PTS: 1 DIF: Cognitive Level: Application REF: 533 OBJ: 4 (theory) TOP: Agnosia: Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 10. Which nursing intervention best encourages self-feeding in a patient with right-sided paralysis after a CVA? a. Place finger foods on the left side of the plate. b. Support the right hand in holding an adaptive cup. c. Seat the patient in the dining room with other residents. d. Place large helpings of food in the center of the plate. ANS: A Finger foods on the nonparalyzed side encourage self-feeding. Privacy is more supportive to early efforts than being in a common dining room. Smaller helpings on the same side of the nonparalyzed limb are conducive to self-feeding. PTS: 1 DIF: Cognitive Level: Application REF: 540 OBJ: 4 (clinical) TOP: Stroke: Self-Feeding KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 11. Which symptom is a key sign of a brain tumor? a. Morning nausea b. Difficulty reading c. A headache that awakens patient d. Increasing blood pressure ANS: C A headache that awakens the patient is an early sign of a brain tumor. Morning nausea, difficulty reading, and increasing blood pressure are nonspecific findings that can be attributed to multifactorial causes. PTS: 1 DIF: Cognitive Level: Comprehension REF: 541 OBJ: 7 (theory) TOP: Brain Tumor: Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 12. The nurse is caring for a patient with brain tumor–related hydrocephalus who is scheduled to undergo placement of a ventriculoperitoneal (V-P) shunt. Which information is most important for the nurse to include when explaining the purpose of the procedure? a. A V-P shunt redirects the cerebrospinal fluid (CSF) from the ventricles to the peritoneum. b. A V-P shunt stimulates ventricles to reabsorb excess CSF. c. A V-P shunt channels excess CSF to the left atrium. d. A V-P shunt provides a port from which excess CSF can be aspirated. ANS: A Obstruction of CSF flow may require placing a shunt to reduce CSF pressure and prevent increased intracranial pressure (ICP). A shunt is a tube placed in a ventricle and attached to a small manual pump that moves excess CSF fluid from the ventricles to the peritoneal cavity or into the atrium of the heart, so that it may be absorbed. PTS: 1 DIF: Cognitive Level: Comprehension REF: 543 OBJ: 3 (clinical) TOP: Hydrocephalus: V-P Shunt KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 13. Following a craniotomy for the removal of a brain tumor, the patient exhibits nuchal rigidity, rash on the chest, headache, and a positive Brudzinski sign. What do these assessment findings indicate to the nurse? a. Intracranial bleeding b. Encephalitis c. Increasing intracranial pressure d. Meningitis ANS: D Nuchal rigidity, skin rash, headache, and a positive Brudzinski sign are indicative of meningitis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 543 OBJ: 10 (theory) TOP: Meningitis: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 14. The nurse is caring for a patient with bacterial meningitis. What interventions should the nurse include in the plan of care? a. Maintain a quiet environment with minimal stimulation. b. Provide all care using sterile technique. c. Limit intake of oral fluids. d. Provide magazines and other activities to reduce daytime naps. ANS: A The environment is kept quiet with minimal stimulation to reduce the possibility of seizure. The care is done with general precautions. Fluid intake is encouraged, as are daytime naps to preserve energy. PTS: 1 DIF: Cognitive Level: Application REF: 545 OBJ: 10 (theory) TOP: Meningitis: General Care KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 15. The patient reports intense intermittent headaches over the last 6 months that are preceded by specific symptoms. What symptom is the patient most likely experiencing? a. Nausea and vomiting b. Focal seizures c. Scotoma d. Fainting ANS: C The headaches are most likely migraines. Scotoma (spots before the eyes) is the typical prodromal symptom of a migraine headache. PTS: 1 DIF: Cognitive Level: Comprehension REF: 546 OBJ: 11 (theory) TOP: Migraine Headaches: Prodromal Symptoms KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 16. A patient was recently diagnosed as having Bell palsy. Which nursing intervention is most important for the nurse to include in the patient’s care plan? a. Administer pain medication as needed. b. Administer artificial tears and aclyclovir. c. Implement aspiration precautions. d. Offer the patient a small fan to cool the face. ANS: B Treatment consists of closing and patching the eye if it loses the blink reflex. Artificial tear eyedrops also are used to prevent dryness of the cornea. Corticosteroids are given if they can be started right after the beginning of symptoms. They are ineffective if delayed more than 7 days. Acyclovir may be prescribed as well, since herpes virus may be a causative organism. Bell palsy is usually a painless condition. Bell palsy does not pose a particular risk for aspirations. Cool air may trigger or exacerbate Bell palsy. PTS: 1 DIF: Cognitive Level: Application REF: 549 OBJ: 12 (theory) TOP: Bell Palsy KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 17. The nurse is writing the care plan for a cerebrovascular accident (CVA) patient who has partial left-sided paralysis and is experiencing ataxia. Which intervention is most beneficial for this patient? a. Encourage the patient to ambulate as much as possible when she feels the energy to do so. b. Ensure the patient receives pureed foods and thickened liquids. c. Place the patient’s call light on the right side of the patient and remind her to call for assistance before getting up. d. Encourage the patient to use a communication board. ANS: C The patient with ataxia has experienced a loss of balance or poor coordination; therefore, placing the call light on this patient’s right side and reminding her to call for help will best address her high risk for falling. Pureed foods and thickened liquids are necessary for the patient with dysphagia, and a communication board would assist a patient with dysarthria or aphasia. PTS: 1 DIF: Cognitive Level: Application REF: 533 OBJ: 4 (theory) TOP: Ataxia KEY: Nursing Process Step: Planning, Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 18. The nurse is caring for a stroke patient who is experiencing homonymous hemianopsia. The patient asks if he is going to have any limitations when discharged from the hospital. The nurse anticipates the patient will be restricted from what activity? a. Ambulating independently b. Cooking on a stove c. Reading a book d. Driving a vehicle ANS: D Homonymous hemianopsia is blindness in part of the visual field of both eyes. Driving a vehicle may be very dangerous for this patient. With proper occupational therapy, the patient should be able to ambulate independently, cook, and read. PTS: 1 DIF: Cognitive Level: Comprehension REF: 533 OBJ: 4 (theory) TOP: Homonymous Hemianopsia KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 19. A patient diagnosed with a primary brain tumor asks the nurse if this is a common disease. Which response is most appropriate for the nurse to make? a. “Brain tumors are very rare.” b. “About 40,000 people a year are diagnosed with a primary brain tumor.” c. “It doesn’t really matter. We are just concerned with helping you.” d. “Almost all primary brain tumors are malignant.” ANS: B About 200,000 new brain tumors are discovered each year in the United States with approximately 40,000 of those being primary tumors and the rest are metastatic tumors from a different site of origin. Many primary brain tumors are benign. Telling the patient his question doesn’t really matter is dismissive and nontherapeutic. PTS: 1 DIF: Cognitive Level: Application REF: 541 OBJ: 6 (theory) TOP: Brain Tumors KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Management of Care MULTIPLE RESPONSE 20. Which condition(s) may cause seizures? (Select all that apply.) a. Stroke b. Cerebral tumor c. Hyperpyrexia d. Epilepsy e. Metabolic toxicity ANS: A, B, C, D, E Stroke, cerebral tumors, hyperpyrexia, epilepsy, and metabolic toxicity are conditions that may all potentially cause seizures. PTS: 1 DIF: Cognitive Level: Knowledge REF: 550, Key Points OBJ: 2 (theory) TOP: Seizure: Etiology KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 21. The nurse is caring for an adult patient with a history of seizures. In the event of a seizure, the nurse should document which information? (Select all that apply.) a. Duration of seizure b. Location of initiation of seizure c. Description of movements d. Family’s reaction during the seizure e. Presence of incontinence ANS: A, B, C, E The nurse should document seizure duration, location of seizure initiation, description of unilateral or bilateral movement, and presence of incontinence. The family’s reaction to the seizure is not included in documentation of a seizure. PTS: 1 DIF: Cognitive Level: Comprehension REF: 527, Focused Assessment OBJ: 1 (theory) TOP: Seizure: Documentation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 22. The nurse is aware that absence (petit mal) seizures are difficult to detect for which reason(s)? (Select all that apply.) a. Lack of an aura b. Appearance as a brief moment of absentmindedness c. Brief loss of consciousness (LOC) d. Absence of patient memory of the event e. Absence of postictal signs ANS: A, B, D, E Factors that make petit mal seizures difficult to detect include lack of an aura and appearance as a brief moment of absentmindedness with no patient memory of the event or presence of postictal signs. Petit mal seizures do not result in LOC. PTS: 1 DIF: Cognitive Level: Application REF: 525 OBJ: 1 (theory) TOP: Absence Seizures: Characteristics KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 23. The nurse is caring for a patient admitted with a transient ischemic attack (TIA). A carotid ultrasound reveals a 40% obstruction. The nurse anticipates that the treatment will likely consist of which factor(s)? (Select all that apply.) a. Diet modification b. Lifestyle alteration c. Aspirin for antiplatelet aggregation d. Daily doses of nitrates e. Endarterectomy ANS: A, B, C Since the patient has a carotid obstruction below 60%, the patient will likely be treated conservatively with measures that include diet and lifestyle modification in conjunction with aspirin therapy. Nitrates and endarterectomy are not initial treatment options for carotid obstruction below 60%. PTS: 1 DIF: Cognitive Level: Comprehension REF: 529 OBJ: 4 (theory) TOP: TIA: Treatment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 24. To help prevent aspiration while feeding a patient who has a right-sided paralysis, the nurse should implement which intervention(s)? (Select all that apply.) a. Place the patient in high Fowler position. b. Instruct the patient to tilt the head and neck forward. c. Instruct the patient to drink liquids through a straw. d. Place food in the left side of the mouth. e. Avoid mixing foods with different textures. ANS: A, B, D, E To help prevent aspiration in this patient, the nurse should position the patient in high Fowler position, instruct the patient to tilt the head and neck forward, place food in the left side of the mouth, and avoid mixing foods with different textures. Drinking through a straw rather than sipping from a cup increases the risk for aspiration. PTS: 1 DIF: Cognitive Level: Application REF: 538, Nursing Care Plan 23-1 OBJ: 4 (clinical) TOP: Stroke: Prevention of Aspiration KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 25. The nurse is completing a care plan for a stroke patient who is at risk for impaired physical mobility. Which interventions should the nurse include in the care plan? (Select all that apply.) a. Assist the patient to stand. b. Remind the patient to ambulate as much as possible. c. Ensure that the call light is within reach. d. Coach the patient in active range-of-motion (ROM). e. Reinforce the use of a walker or cane. ANS: A, C, D, E Fall precautions important for this patient include helping the patient to stand, placing the call light within reach, coaching the patient in active ROM, and reinforcing the use of a walker or cane. Reminding the patient to ambulate as much as possible would potentially increase the risk of falls. PTS: 1 DIF: Cognitive Level: Application REF: 538, Nursing Care Plan 23-1 OBJ: 4 (theory) TOP: Stroke: Prevention of Falls KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 26. The nurse is educating a patient about his cluster headaches. The nurse includes information that cluster headaches may be accompanied by which signs or symptoms? (Select all that apply.) a. Reddened conjunctiva b. Nasal congestion c. Ptosis d. Lethargy e. Sensitivity to touch ANS: A, B, C, E Manifestations of cluster headaches may include severe unilateral orbital, supraorbital, or temporal pain along with one of the following: redness of the conjunctiva of the eye, tearing, nasal congestion, dripping nose, facial swelling, pupil constriction, ptosis (drooping) of the eyelid, and sensitivity to touch. Cluster headaches might cause restlessness (patients often pace), not lethargy. PTS: 1 DIF: Cognitive Level: Comprehension REF: 547-548 OBJ: 11 (theory) TOP: Cluster Headache: Signs and Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 27. The patient with a right-sided paralysis from a stroke becomes frustrated when attempting to self-feed. He throws the spoon at the nurse and begins to cry. What nursing action(s) is/are most appropriate at this time? (Select all that apply.) a. Retrieve the spoon and sit quietly for a few seconds. b. Touch the patient and inquire if he would rather have a high-protein milkshake for his meal. c. Remind the patient that such behavior is not acceptable. d. Add an intervention to the NCP for increased support with self-feeding. e. Complete an incident report. ANS: A, B, C, D Quietly retrieving the spoon, offering an alternative, reassuring the patient, and devoting new interventions related to the selffeeding deficit are appropriate nursing actions in this situation. Completing an incident report is not necessary unless the nurse or someone else was injured. PTS: 1 DIF: Cognitive Level: Application REF: 538, Nursing Care Plan 23-1, 540 OBJ: 4 (theory) TOP: Stroke: Lability KEY: Nursing Process Step: Planning, Implementation MSC: NCLEX: Psychosocial Integrity: Coping and Adaptation Chapter 24: Care of Patients with Peripheral Nerve and Degenerative Diseases deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is explaining Parkinson disease to the student nurse. Which statement indicates that the student nurse correctly understands the pathophysiology of the disease? a. “Regardless of the actual etiology, Parkinson disease is caused by depletion of dopamine and excess of acetylcholine.” b. “The pathophysiology of the disease is caused by the deterioration of the myelin sheath of the basal ganglia.” c. “Excess dopamine and deficient acetylcholine are the cause of Parkinson disease.” d. “When there is decreased dopamine uptake at receptors in brain cells, Parkinson disease results.” ANS: A The specific cause of Parkinson disease is unknown, but the basic pathophysiology is depletion of dopamine and excess of acetylcholine. PTS: 1 DIF: Cognitive Level: Comprehension REF: 553 OBJ: 1 (theory) TOP: Parkinson Disease: Pathophysiology KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. The nurse is assessing a patient with Parkinson disease. Which statement likely characterizes this patient’s tremors? a. Tremors occur constantly. b. Tremors decrease with voluntary movement. c. Tremors are absent when the body is at rest. d. Tremors are characterized by tonic/clonic muscle activity. ANS: B Tremors in Parkinson disease decrease with voluntary movement, are absent during sleep, and occur when the body is at rest. Parkinsonian muscle activity is that of “pill rolling.” Tonic/clonic movement is associated with seizures. PTS: 1 DIF: Cognitive Level: Comprehension REF: 554 OBJ: 1 (theory) TOP: Parkinson Disease: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. Which problem statement/nursing diagnosis is most appropriate for a person with Parkinson disease? a. Risk for falls related to unsteady gait. b. Ineffective airway clearance related to drooling. c. Risk for impaired skin integrity related to tremor. d. Nutrition: less than body requirements related to nausea. ANS: A Rigidity and impaired balance with the propulsive gait create a risk for falls. The tremor decreases with voluntary movement, making eating relatively trouble free. Drooling is not a threat for aspiration, and there is no characteristic nausea. PTS: 1 DIF: Cognitive Level: Application REF: 557, Nursing Care Plan 24-1 OBJ: 3 (theory) TOP: Parkinson Disease: Nursing Diagnoses KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 4. To enhance more erect posture in the patient with Parkinson disease, the nurse should encourage the patient to practice which activity? a. Imagine stepping over an object. b. Sleep in the prone position. c. Walk with a marching step. d. Limit exercise to increase joint mobility. ANS: B The nurse should teach the patient to consciously assume correct posture. Sleeping in the prone position without a pillow will help to improve erect posture. Imagining stepping over something helps prevent “freezing” when walking. Walking may also improve by having the patient think about imaginary lines across the pathway on which to walk. The patient should be encouraged to exercise; the physical therapist will institute an exercise program to help the patient maintain muscle function and promote joint mobility. PTS: 1 DIF: Cognitive Level: Application REF: 559 OBJ: 3 (theory) TOP: Parkinson Disease: Improving Posture KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. The caregiver of a patient with Parkinson disease is concerned with the patient’s recent weight loss. The home health nurse should suggest which modification to help the caregiver enhance the patient’s nutrition? a. Provide six mini-meals throughout the day. b. Be sure to increase milk and cheese daily in the diet. c. Limit fluid intake in order to increase the appetite. d. Prepare larger meals of fibrous foods. ANS: A Mini-meals can be eaten before food cools since it takes longer for the patient with Parkinson disease to eat. Large meals are overwhelming and may become unappetizing before they can be consumed. Reduced fluid and increased dairy products increase the threat of constipation. PTS: 1 DIF: Cognitive Level: Application REF: 559 OBJ: 3 (theory) TOP: Parkinson Disease: Nutrition KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 6. Which type of multiple sclerosis (MS) is the most common? a. Secondary progressive b. Primary progressive c. Relapsing-remitting d. Relapsing-progressive ANS: C Relapsing-remitting is the most common type of MS. PTS: 1 DIF: Cognitive Level: Knowledge REF: 560, Table 24-2 OBJ: 5 (theory) TOP: MS: Disease Types KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 7. Which factor(s) is/are most likely a potential cause(s) of multiple sclerosis (MS)? a. Environmental factors and genetic predisposition b. Allergic response to antiviral medications c. Hypersensitivity reaction attacking the myelin d. Bacterial infection of the myelin ANS: A The cause of MS is not known, but it is attributed to an environmental factor (bacteria, virus, or chemical) combining with a genetic predisposition for the disease. Current thought also includes the hypothesis that MS is an autoimmune disease where the immune system attacks healthy central nervous system tissues. PTS: 1 DIF: Cognitive Level: Knowledge REF: 560 OBJ: 4 (theory) TOP: MS: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 8. The home health nurse is caring for a patient with multiple sclerosis (MS) who complains of severe fatigue. What activity should the nurse suggest to diminish the effects of fatigue? a. Relaxing in a warm bath b. Performing deep-breathing exercises c. Scheduling rest periods during the day d. Including daily-dose multivitamins ANS: C Scheduling and observing rest periods during the day will reduce fatigue. Heat increases sense of fatigue. Muscular problems are associated with ineffective impulse transmission rather than muscle weakness related to nutritional deficiency. PTS: 1 DIF: Cognitive Level: Application REF: 562 OBJ: 5 (theory) TOP: MS: Reducing Fatigue KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 9. Which factors predominantly determine probable diagnosis of multiple sclerosis (MS)? a. Blood tests revealing identifiable MS markers b. Lumbar puncture results revealing inflammatory response c. Muscle biopsies revealing characteristic lesions d. Signs and symptoms assessed and reported by the patient ANS: D No laboratory test will definitively establish a diagnosis of MS, although most patients have elevated IgG levels in their cerebrospinal fluid (CSF), with the presence of oligoclonal bands (bands of IgG produced by electrophoresis of the CSF). An magnetic resonance imaging (MRI) study usually shows characteristic white matter lesions scattered through the spinal cord and/or brain, which confirms the diagnosis of MS. However, the clinical signs and symptoms presented by a patient usually are sufficient characteristics of the disorder to allow the neurologist to make a diagnosis that the patient possibly or probably has MS. PTS: 1 DIF: Cognitive Level: Comprehension REF: 561 OBJ: 4 (theory) TOP: MS: Diagnosis KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 10. Which drug therapy is indicated for an acute severe attack of multiple sclerosis (MS)? a. Intravenous (IV) methylprednisolone b. Intramuscular injections of interferon beta-1b c. Massive doses of antibiotics d. Muscle relaxants and opioids ANS: A IV methylprednisolone is the standard treatment for the severe acute attack of MS. Interferon is used to prevent attacks. PTS: 1 DIF: Cognitive Level: Knowledge REF: 561 OBJ: 5 (theory) TOP: MS: Treatment KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 11. The home health nurse is planning an exercise program for a patient with multiple sclerosis (MS). Which exercise would be most beneficial for this patient? a. Swimming b. Progressive walking c. Weight training d. Isometric exercises ANS: A An exercise program is very beneficial for the MS patient to relieve spasticity and improve coordination (Harmon, 2011). Because of fatigue, it is often difficult to convince MS patients to exercise. Swimming provides considerable benefits as exercising in water is less fatiguing than exercising out of water. PTS: 1 DIF: Cognitive Level: Comprehension REF: 561 OBJ: 5 (theory) TOP: MS: Exercise Program KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 12. The nurse is educating the family of a patient in the late stages of amyotrophic lateral sclerosis (ALS). Which information is most important for the nurse to include? a. Ability to move the upper limbs may be affected. b. Cognitive and mental capacities will most likely remain intact throughout the disease progression. c. Breathing should not be affected by the disease. d. Ability to swallow will remain intact. ANS: B Whereas the ability to move the upper limbs will likely be affected by the disease, it is important for families to remember that the patient’s cognitive and mental capacity stays intact as the motor activity rapidly declines. Breathing and swallowing are often significantly affected by ALS. PTS: 1 DIF: Cognitive Level: Application REF: 563 OBJ: 7 (theory) TOP: ALS: Retention of Mentation KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 13. The home care nurse is visiting a patient in the late stages of amyotrophic lateral sclerosis (ALS). Which example indicates that the patient accepts the grief associated with the condition and prognosis? a. The patient cries about his incapacity. b. The patient makes jokes about this approaching death. c. The patient talks with his family about his desires for his funeral. d. The patient begins to sleep for longer periods of time during the day. ANS: C Planning with family signals acceptance. Crying, joking, and sleeping are efforts at denial. PTS: 1 DIF: Cognitive Level: Application REF: 563 OBJ: 7 (theory) TOP: ALS: Acceptance of Death KEY: Nursing Process Step: Evaluation MSC: NCLEX: Psychosocial Integrity 14. Signs and symptoms of Guillain-Barré syndrome (GBS) usually appear within how many days after a viral infection? a. 2 to 3 days b. 7 days c. 10 to 21 days d. 30 days ANS: C The cause of GBS is not known, but it usually follows a viral respiratory infection or gastroenteritis in adults within 10 to 21 days. PTS: 1 DIF: Cognitive Level: Knowledge REF: 563 OBJ: 6 (theory) TOP: GBS: Etiology KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 15. The nurse is caring for a patient with Huntington disease. The patient asks if his disease will affect future children. Which reply is most appropriate? a. “Huntingdon disease does not have a genetic component.” b. “Male children would have Huntington disease and female children would be carriers.” c. “Huntington disease is caused by an autoimmune response.” d. “The genetic nature of the disease means that 50% of your children will inherit it.” ANS: D Huntington disease is an autosomal dominant disorder, meaning that 50% of the children of a person who has the disease will inherit it. If a child does not inherit the disease, the gene is not passed on to the next generation. Huntington disease has an autosomal link and can be passed on to 50% of the children of a person with the disease. PTS: 1 DIF: Cognitive Level: Comprehension REF: 565 OBJ: 7 (theory) TOP: Huntington Disease: Genetic Link KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 16. The nurse is assessing a patient with suspected myasthenia gravis. The nurse is aware that which assessment finding supports this diagnosis? a. Ptosis b. Hand tremors during voluntary movement c. Dizziness with sudden head movement d. Postural hypotension ANS: A Symptoms of myasthenia gravis include diplopia (double vision), difficulty chewing and swallowing, and ptosis. PTS: 1 DIF: Cognitive Level: Knowledge REF: 565 OBJ: 8 (theory) TOP: Myasthenia Gravis: Early Sign KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 17. The nurse is caring for a patient with myasthenia gravis. The patient asks the nurse if she can return to her normal job as a data entry specialist. Which symptom would most affect the patient’s ability to perform her job? a. Ptosis b. Diplopia c. Dysphagia d. Aphasia ANS: B A data entry specialist spends large amounts of time entering data in the computer. Ptosis, dysphagia, and aphasia are all symptoms associated with myasthenia gravis, but diplopia, or double vision, will cause the patient the most difficulty with using a computer. PTS: 1 DIF: Cognitive Level: Application REF: 565 OBJ: 8 (theory) TOP: Myasthenia Gravis: Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Management of Care 18. The nurse is planning care for a patient with Parkinson disease. Which problem statement/nursing diagnosis is most appropriate for the patient experiencing bradykinesia? a. Risk for falls b. Impaired swallowing c. Acute confusion d. Risk for suicide ANS: A Bradykinesia is a condition that is associated with Parkinson disease, characterized by slow speech and movement, which produces poor body balance, a characteristic shuffling gait, and difficulty initiating movement. This condition places the patient at risk for falling. PTS: 1 DIF: Cognitive Level: Application REF: 554 OBJ: 3 (theory) TOP: Parkinson Disease KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control MULTIPLE RESPONSE 19. The home health nurse assesses the patient with Parkinson disease who just started taking carbidopa-levodopa. The nurse should be alert for which side effect(s)? (Select all that apply.) a. Urinary retention b. Pruritis c. Diaphoresis d. Orthostatic hypotension e. Pink urine ANS: A, C, D Carbidopa-levodopa may cause urinary retention, diaphoresis, and orthostatic hypotension. The medication should not cause itching, and it may turn the urine dark. PTS: 1 DIF: Cognitive Level: Comprehension REF: 556, Box 24-1 OBJ: 2 (theory) TOP: Parkinson Disease Treatment: Carbidopa-Levodopa KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 20. The nurse is preparing a care plan for a person with late-stage Parkinson disease. The nurse should plan interventions to address which problem(s)? (Select all that apply.) a. Dysphagia b. Hallucinations c. Immobility d. Insomnia e. Urinary incontinence ANS: A, C, D, E The nurse should plan interventions to address dysphagia, immobility, insomnia, and urinary incontinence. Hallucinations are not part of the late Parkinson disease symptoms. PTS: 1 DIF: Cognitive Level: Comprehension REF: 557 OBJ: 3 (theory) TOP: Parkinson Disease: Complications KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 21. The nurse outlines nutritional needs for the patient with multiple sclerosis (MS). Which dietary instruction(s) is/are most important for the nurse to emphasize? (Select all that apply.) a. Maintain fluid intake of at 1500 mL each day. b. Include intake of high-fiber foods in the diet. c. Include high intake of carbohydrates. d. Add supplemental calcium and vitamin D to the diet. e. Increase intake of high-fat foods. ANS: A, B, D Fluids and high fiber in the diet will prevent constipation, and calcium and vitamin D will help in preventing osteoporosis. High levels of carbohydrates and fats are not emphasized in the diet for an MS patient. PTS: 1 DIF: Cognitive Level: Application REF: 562 OBJ: 5 (theory) TOP: MS: Nutrition KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 22. The nurse is caring for a patient with Guillain-Barré syndrome (GBS). Which area(s) should the care plan address? (Select all that apply.) a. Assessment of advancing paralysis b. Provision for ventilation support c. Maintenance of adequate nutrition d. Prevention of complications of immobility e. Assessment of hypertension ANS: A, B, C, D The nurse should include assessment of paralysis, provision for ventilation support, nutritional maintenance, and prevention of complications from immobility. The care plan should address assessment of hypotension rather than hypertension. PTS: 1 DIF: Cognitive Level: Comprehension REF: 564 OBJ: 6 (theory) TOP: GBS: Nursing Care KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 23. The student nurse is researching relapsing-progressive forms of multiple sclerosis (MS). What characteristic(s) is/are typical of this form of the disease? (Select all that apply.) a. Steadily worsens b. Partial remissions c. Clear, acute relapses d. Temporary minor improvements e. Long plateau periods ANS: A, C Steady worsening and clear acute relapses are the principle characteristics of relapsing-progressive MS. PTS: 1 DIF: Cognitive Level: Comprehension REF: 560, Table 24-2 OBJ: 2 (clinical) TOP: MS: Relapsing Progressive Type KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 24. The nurse is caring for a patient with Huntington chorea. Which symptom(s) is/are characteristic manifestation(s) of this disease? (Select all that apply.) a. Fidgeting b. Restlessness c. Constant movement d. Dementia e. Difficulty swallowing ANS: A, B, C, D Huntington chorea is a degenerative neurologic disorder characterized by abnormal movements (chorea). The disease begins with the patient being fidgety and progresses to constant movement and intellectual decline. Death usually occurs within 15 to 20 years after diagnosis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 565 OBJ: 7 (theory) TOP: Huntington Chorea: Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Management of Care COMPLETION 25. The triad of Parkinson disease is __________, __________, and __________. ANS: tremor; bradykinesia; rigidity bradykinesia; rigidity; tremor tremor; rigidity; bradykinesia bradykinesia; tremor; rigidity rigidity; tremor; bradykinesia rigidity; bradykinesia; tremor Tremor, bradykinesia, and rigidity are included in the triad of Parkinson disease. PTS: 1 DIF: Cognitive Level: Comprehension REF: 554 OBJ: 1 (theory) TOP: Parkinson Disease: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 26. Two viruses that are especially associated with the etiology of Guillain-Barré syndrome (GBS) are ___________ and ___________. ANS: cytomegalovirus; Epstein-Barr virus Epstein-Barr virus; cytomegalovirus Cytomegalovirus and Epstein-Barr virus are especially associated with the development of GBS. PTS: 1 DIF: Cognitive Level: Knowledge REF: 563 OBJ: 6 (theory) TOP: GBS: Etiology KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 27. The test for the diagnosis of myasthenia gravis in which muscle strength is increased within 1 minute of the injection is the __________ test. ANS: Tensilon An injection of Tensilon will increase muscle strength within 1 minute of injection and is a positive test for the diagnosis of myasthenia gravis. PTS: 1 DIF: Cognitive Level: Knowledge REF: 566 OBJ: 8 (theory) TOP: Myasthenia Gravis: Diagnosis KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance Chapter 25: The Sensory System: Eye and Ear deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. Which component in the eye refracts light rays to be directed to the lens? a. Pupil b. Cornea c. Retina d. Ciliary body ANS: B The cornea bends or refracts the light rays onto the retina. The pupil acts to regulate the entrance of light into the eye. The ciliary body helps to change the shape of the eye for far and near vision. The retina is the inner coat of the eyeball and is found in the posterior portion of it. The retina contains several layers. The layer with rods and cones acts as the receptor for light images. PTS: 1 DIF: Cognitive Level: Knowledge REF: 572 OBJ: 1 (clinical) TOP: Cornea: Function KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 2. A tonometer reading reflects the amount of pressure exerted by which component of the eye? a. Sclera b. Aqueous humor c. Vitreous humor d. Cornea ANS: B The tonometer reads the pressure exerted by the aqueous humor in the anterior chamber. The sclera is the part of the eyeball that is opaque white and covers the posterior portion of the eyeball. The vitreous humor is the substance found in the posterior chamber of the eye between the lens and the retina. The cornea is a transparent structure in the eye that allows light to hit the lens. It is involved in the bending of light rays. PTS: 1 DIF: Cognitive Level: Comprehension REF: 572, 577, Table 25-2 OBJ: 1 (theory) TOP: Optic Pressure KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 3. During examination of the fundus of the eye, the nurse assesses a choked disc. Which statement accurately explains the significant of this finding? a. The disc has an infarct. b. There is increased intracranial pressure (ICP). c. There is significant hypertension. d. The lens has become opaque. ANS: B Visualization of the optic disc provides information about the pressure within the eye and within the skull. When ICP gets higher, the optic disc appears “swollen” or “choked.” PTS: 1 DIF: Cognitive Level: Comprehension REF: 572 OBJ: 2 (theory) TOP: Fundus Assessment: Choked Disc KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 4. An office assistant tells the nurse his job requires him to work at his computer for 7 to 8 hours each day. Which statement indicates that the nurse’s teaching about preventing eyestrain has been successful? a. “I will wear protective goggles while working.” b. “I will eat more carrots and cooked spinach.” c. “I will close my eyes every few hours.” d. “I will instill artificial tears each hour while working.” ANS: C To prevent eyestrain, the patient should rest the eye muscles periodically when working at the computer or performing any activity that demands intensive visual effort. Resting the eye muscles every several hours helps prevent eye fatigue. Protective goggles do not help prevent eyestrain. Nutrients such as lutein and zeaxanthin are found in carrots and cooked spinach and are good for the eyes but do not reduce eyestrain. Overuse of artificial tears is not recommended, and proper usage works to combat dry eyes. PTS: 1 DIF: Cognitive Level: Application REF: 574 OBJ: 1 (clinical) TOP: Eye Rest KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 5. The nurse is reviewing the health history of a 26-year-old patient who denies corrective lenses. Which scenario indicates that the patient follows preventive eye examination recommendations? a. The patient has had annual eye examinations since age 18. b. The patient’s last eye examination occurred at age 10. c. The patient had a baseline eye examination at age 25. d. The patient has never had an eye examination. ANS: C Starting at age 25, adults should have an eye examination every 5 to 10 years until age 40, every 2 to 4 years from 40 to 54, and every 1 to 3 years from 55 to 64. After age 65, eyes should be examined by an eye specialist every 1 to 2 years (AHRQ, 2014). PTS: 1 DIF: Cognitive Level: Comprehension REF: 574-575 OBJ: 1 (theory) TOP: Periodic Eye Examination: Frequency KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 6. How often should eye cosmetics be discarded? a. Every 2 months b. Every 3 months c. Every 6 months d. Every year ANS: C Eye cosmetics should be discarded every 6 months to prevent infection. PTS: 1 DIF: Cognitive Level: Knowledge REF: 575 OBJ: 1 (theory) TOP: Eye Cosmetics: Source of Infection KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 7. The nurse is caring for a blind patient. Which action is most appropriate when entering the patient’s room? a. Touch the patient before speaking to allow her to locate the nurse’s position. b. Speak to the patient by name when entering the room to avoid startling her. c. Speak to the patient only when at bedside to increase orientation. d. Walk about in the room, carrying on conversation. ANS: B Speaking to the person by name allows the patient to know someone has entered the room and will avoid startling the patient. PTS: 1 DIF: Cognitive Level: Comprehension REF: 580 OBJ: 5 (theory) TOP: Visually Impaired: Orientation KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 8. The nurse is orienting a visually impaired patient to a meal plate. Which action is most appropriate? a. Identify the location of the plate. b. Hold the patient’s hand and direct it to the plate. c. Place eating utensil in the patient’s hand. d. Identify food according to an imaginary clock face. ANS: D Identifying food location by position on an imaginary clock face is helpful to the visually impaired patient. PTS: 1 DIF: Cognitive Level: Comprehension REF: 582 OBJ: 5 (theory) TOP: Visually Impaired: Self-Feeding KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 9. The visually impaired person has entered the outpatient clinic with a guide dog. What action is most appropriate for the nurse to take? a. Quietly greet the dog and pat it. b. Direct the patient and the dog to an area where the dog will not be distracted. c. Take the harness from the patient, and direct the dog and patient to a seat. d. Refrain from interacting with the patient and dog until the dog leads the patient to a seat. ANS: D The dog should not be distracted while it is working. The dog will seat the patient if possible; if not, the nurse can ask how best the patient can be directed. PTS: 1 DIF: Cognitive Level: Application REF: 582 OBJ: 5 (theory) TOP: Guide Dog Etiquette KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 10. The nurse is caring for a 40-year-old patient. How often should the nurse recommend that this patient undergo testing for glaucoma? a. Yearly b. Every 2 to 3 years c. Every 5 years d. Every 10 years ANS: C Glaucoma testing should be done every 2 to 3 years for people over age 40. PTS: 1 DIF: Cognitive Level: Knowledge REF: 582 OBJ: 1 (theory) TOP: Glaucoma Testing: Frequency KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 11. When assessing for macular degeneration, the nurse should use which assessment tool? a. Snellen eye chart b. Corneal reflex test c. Visual field test d. Amsler grid test ANS: D The Amsler grid test assesses the extent of macular degeneration by noting the patient’s perception of missing or wavy lines on the grid. The Snellen eye chart is used to assess visual acuity. Visual field assessments may be used to assess peripheral vision. PTS: 1 DIF: Cognitive Level: Knowledge REF: 578, Table 25-2 OBJ: 2 (clinical) TOP: Amsler Grid Test: Function KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 12. The nurse is caring for a patient who is experiencing diabetes-related visual changes. Which statement indicates that the patient accurately understands the nurse’s teaching about the cause of vision changes in diabetes? a. “Long-term exposure to high glucose levels can damage the blood vessels in my retina.” b. “Frequent injections of regular insulin damage the cornea.” c. “High glucose levels cause increase pressure in my eyes that leads to lens opacity. d. “Diabetes affects healing and causes frequent eye infections.” ANS: A Prolonged periods of hyperglycemia cause damage to the retina from bleeding. Insulin does not result in visual changes in the patient with diabetes. Lens opacity and corneal dryness will not promote vision-related complications in the patient with diabetes mellitus. PTS: 1 DIF: Cognitive Level: Application REF: 579 OBJ: 5 (theory) TOP: Diabetes: Retinal Damage KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 13. The nurse is assessing an 84-year-old patient. Which finding is consistent with aging? a. Thick cerumen b. Heightened perception of low-frequency sounds c. Outer ear canal pain d. Increased hair on the pinna ANS: A Thickened, hard cerumen collections in the outer ear can disrupt sound conduction and impair hearing. Age-related changes may include reduced perception of low-frequency sounds. Pain in the outer ear is not a normal change related to aging, nor is increased hair on the pinna. PTS: 1 DIF: Cognitive Level: Comprehension REF: 583 OBJ: 2 (clinical) TOP: Ear: Age-Related Changes KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 14. The patient is experiencing frequent attacks of vertigo. When planning care, which activity should the nurse encourage? a. Increase sodium in the diet. b. Consider a smoking cessation program. c. Increase daily fluid intake. d. Drink a glass of red wine before supper. ANS: B Cessation of smoking will decrease incidence of vertigo in the person with middle-ear disorders. Tobacco is vasoconstrictive and can affect the blood supply to the inner ear and nerves. When increased fluid pressure in the inner ear is suspected as the cause of dizziness, the provider may order a low-sodium diet and limit fluid intake. Alcohol intake does not combat vertigo. PTS: 1 DIF: Cognitive Level: Application REF: 592 OBJ: 5 (theory) TOP: Remedies to Reduce Vertigo KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 15. A patient tilts her head to the side while reading a pamphlet. The nurse recognizes that this action may be an attempt to compensate for which problem? a. Tinnitus b. Nystagmus c. Photophobia d. Diplopia ANS: D Tilting the head may indicate a visual disturbance such as double vision or that one eye is stronger than the other. Tilting the head to read would not affect tinnitus (ringing in the ears) or nystagmus (involuntary eye movements). Shading the eyes may be noted with photophobia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 579 OBJ: 2 (theory) TOP: Focused Assessment KEY: Nursing Process Step: Diagnosis MSC: NCLEX: Physiological Integrity: Physiological Adaptation 16. The nurse is teaching a group of schoolchildren about the relationship between diet and vision. The nurse encourages the ingestion of foods rich in vitamin A. Which food choice should the nurse recommend? a. Kale b. Cauliflower c. Strawberries d. Apples ANS: A Vitamin A protects against night blindness, slow adaptation to darkness, and glare blindness. The carotenoids are the precursors for vitamin A and are found in green leafy and yellow vegetables. PTS: 1 DIF: Cognitive Level: Application REF: 574, Nutritional ConsiderationsOBJ: 1 (theory) TOP: Nutrition Considerations KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Health Promotion/Disease Prevention 17. The nurse is caring for a patient who presents to the clinic a small, hard lesion on the eyelid. Which condition is consistent with these findings? a. Blepharitis b. Chalazion c. Hordeolum d. Conjunctivitis ANS: B Chalazion is an internal stye caused by infection of the meibomian gland. PTS: 1 DIF: Cognitive Level: Comprehension REF: 581, Table 25-4 OBJ: 2 (theory) TOP: Clinical Signs and Symptoms of Selected Eye Diseases, Medical Treatment, and Nursing Interventions KEY: Nursing Process Step: Diagnosis MSC: NCLEX: Physiological Integrity: Physiological Adaptation MULTIPLE RESPONSE 18. The student nurse is ambulating with a blind patient. Which technique(s) indicate(s) that the student nurse requires further instruction? (Select all that apply.) a. Holding the patient’s dominant arm b. Instructing the patient to put both hands on his shoulders c. Allowing the patient to hold the nurse’s arm d. Holding the patient’s hand e. Walking just behind the patient ANS: A, B, D, E The safest and most effective technique when ambulating a blind patient involves allowing the patient to hold the nurse’s arm, as the patient follows. The nurse should not hold the patient’s arm, instruct the patient to place his hands on the nurse’s shoulders, or hold the patient’s hand, so these actions would require additional teaching. PTS: 1 DIF: Cognitive Level: Application REF: 582 OBJ: 5 (theory) TOP: Ambulation of the Blind: Technique KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 19. The nurse assesses the age-related changes that occur in the eye. Which finding(s) is/are consistent with aging? (Select all that apply.) a. Subcutaneous fat increases. b. The cornea flattens and increases astigmatism. c. Water loss occurs from the lens. d. Presbyopia occurs. e. Ectropion occurs. ANS: B, C, D, E Age-related eye changes include corneal flattening, water loss from the lens, and occurrence of presbyopia and ectropion. Subcutaneous fat decreases with aging. PTS: 1 DIF: Cognitive Level: Comprehension REF: 573 OBJ: 3 (theory) TOP: Eye: Age-Related Changes KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 20. The nurse recalls that the Healthy People 2020 objectives for vision include directives for which goals? (Select all that apply.) a. Vision screenings for children 10 years of age and younger b. Reduction of uncorrected refractive errors c. Reduction of diabetic retinopathy d. Reduction of visual impairment related to cataracts e. Increased use of protective eyewear ANS: B, C, D, E Healthy People 2020 includes many objectives to prevent vision problems, including reduction of uncorrected refractive errors, diabetic retinopathy, and cataract-related visual impairment, along with increased use of protective eyewear. Vision screening for children should begin at age 5. PTS: 1 DIF: Cognitive Level: Comprehension REF: 574 OBJ: 1 (clinical) TOP: Healthy People 2020: Objectives for Vision KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 21. The nurse is teaching a patient about visual problems that require professional attention. Which symptom(s) indicate an underlying visual problem? (Select all that apply.) a. Eyes that tire easily b. Burning c. Itching d. Reddening with use e. Exophthalmos ANS: A, B, C, D Underlying visual problems may manifest with eyes that tire easily, burn, itch, or redden with use. Exophthalmos (protruding eyes) is not usually a visual problem, but a sign of a systemic problem such as hyperthyroidism. PTS: 1 DIF: Cognitive Level: Comprehension REF: 574 OBJ: 3 (clinical) TOP: Visual Disorders: Signs and Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 22. The nurse is assessing a patient’s visual field. Which action(s) demonstrate(s) correct technique? (Select all that apply.) a. The nurse faces the patient. b. The nurse covers her right eye while instructing the patient to cover his right eye. c. The nurse moves a finger from an area outside the line of peripheral vision into the line of vision. d. The nurse instructs the patient to read the smallest row on the Snellen chart. e. The nurse instructs the patient to look directly into her eyes. ANS: A, C, E To assess visual field, the examiner should face the patient and ask him to look directly into his eyes. The examiner covers the right eye while the patient covers the left eye. The examiner moves his finger from outside of the peripheral vision into the line of vision. The patient should detect the finger about the same time as the examiner. The test is repeated with the other eye covered. The Snellen chart is not used for a visual field test. PTS: 1 DIF: Cognitive Level: Comprehension REF: 577, Table 25-2 OBJ: 2 (clinical) TOP: Visual Field Evaluation: Technique KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 23. The nurse is caring for a patient with a frequent history of falls. The nurse notes that which problems in the patient’s history may contribute to frequent falls? (Select all that apply.) a. Diplopia b. Vertigo c. Tinnitus d. Cirrhosis e. Ataxia ANS: A, B, E Double vision affects visual acuity and depth perception, vertigo affects equilibrium and balance, and inability to control muscle movements leads to unsteady gait—all problems that may contribute to frequent falls. Ringing in the ears and cirrhosis do not overtly increase fall risk. PTS: 1 DIF: Cognitive Level: Application REF: 584 OBJ: 5 (theory) TOP: Inner Ear Disorders: Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 24. Which medication(s) may cause ototoxicity? (Select all that apply.) a. Vancomycin b. Furosemide c. Acetaminophen d. Ibuprofen e. Amoxicillin ANS: A, B, D Commonly administered drugs that can be ototoxic are many of the antibiotics, nonsteroidal anti-inflammatory drugs, chemotherapy agents, and potent diuretics, such as furosemide (Lasix) (Box 25-3). Acetaminophen and amoxicillin are not ototoxic. PTS: 1 DIF: Cognitive Level: Comprehension REF: 586, Box 25-3 OBJ: 5 (theory) TOP: Ototoxic Drugs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies COMPLETION 25. The nurse clarifies to the patient with an eye disorder that the fluid in the anterior chamber is called __________ humor, whereas the fluid in the posterior chamber is called __________ humor. ANS: aqueous; vitreous The fluid in the anterior chamber is aqueous humor and the fluid in the posterior chamber is vitreous humor. PTS: 1 DIF: Cognitive Level: Knowledge REF: 571 OBJ: 2 (clinical) TOP: Eye Chamber Fluids KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 26. The receptors of light and color in the eyeball are the __________ and the __________. ANS: rods; cones cones; rods The rods and cones are the receptors of light and color. PTS: 1 DIF: Cognitive Level: Knowledge REF: 571 OBJ: 2 (clinical) TOP: Rods and Cones: Function KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 27. The nurse interviewing a patient with macular degeneration will inquire about the patient’s habits, especially __________, which is a significant contributor to the disorder. ANS: smoking Smoking is a significant contributor to macular degeneration. PTS: 1 DIF: Cognitive Level: Comprehension REF: 574 OBJ: 2 (clinical) TOP: Macular Degeneration: Smoking KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance MATCHING Place the steps of instillation of eyedrops in appropriate order. a. Expose the conjunctival sac. b. Ask the patient to close the eyelids and move the eyes back and forth. c. Ask the patient to look up. d. Ask the patient to tilt the head toward the eye receiving the drops. e. Drop medication in the conjunctival sac. 28. Step 1 29. Step 2 30. Step 3 31. Step 4 32. Step 5 28. ANS: C PTS: 1 DIF: Cognitive Level: Comprehension REF: 581, Box 25-1 OBJ: 4 (theory) TOP: Eyedrop Instillation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 29. ANS: D PTS: 1 DIF: Cognitive Level: Comprehension REF: 581, Box 25-1 OBJ: 4 (theory) TOP: Eyedrop Instillation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 30. ANS: A PTS: 1 DIF: Cognitive Level: Comprehension REF: 581, Box 25-1 OBJ: 4 (theory) TOP: Eyedrop Instillation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 31. ANS: E PTS: 1 DIF: Cognitive Level: Comprehension REF: 581, Box 25-1 OBJ: 4 (theory) TOP: Eyedrop Instillation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 32. ANS: B PTS: 1 DIF: Cognitive Level: Comprehension REF: 581, Box 25-1 OBJ: 4 (theory) TOP: Eyedrop Instillation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort Chapter 26: Care of Patients with Disorders of the Eyes and Ears deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse notices that the patient must hold the newspaper at arm’s length and squint to read. The nurse understands that this finding is consistent with which eye problem? a. Myopia b. Hyperopia c. Presbyopia d. Astigmatism ANS: B The person with hyperopia is farsighted; the patient cannot see things up close and must change the distance from the eyes in order to focus. The person with myopia cannot see things in the distance. Presbyopia refers to the hardening of the ciliary bodies of the eyes. Astigmatism refers to a visual defect resulting from a warped lens or an irregular curvature of the cornea. PTS: 1 DIF: Cognitive Level: Comprehension REF: 597 OBJ: 1 (theory) TOP: Refraction Errors: Hyperopia KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. The nurse explains that a photorefractive keratectomy (PRK) is a very brief surgery that corrects myopia. Which statement indicates that the nurse’s teaching about the procedure has been successful? a. “This procedure uses a laser to remove a thin layer of the cornea.” b. “This procedure uses a laser to reshape the cornea, then replace the outer layer.” c. “This procedure makes tiny cuts in the cornea to flatten it.” d. “This procedure uses a laser to reshape the fundus.” ANS: A A PRK uses a laser to remove a thin layer of the cornea. The LASIK procedure uses a laser to reshape the cornea and replace the outer layer. Making tiny cuts in the cornea to flatten it refers to a radial keratotomy. PTS: 1 DIF: Cognitive Level: Comprehension REF: 598 OBJ: 4 TOP: PRK: Technique KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 3. The nurse is caring for a patient who has developed keratitis. When planning care, the nurse should implement which action to improve the patient’s comfort? a. Use eye shields. b. Instill artificial tears. c. Apply cold compresses. d. Apply warm compresses. ANS: B Keratitis is an inflammation of the cornea caused by irritation or infection. Artificial tears will reduce the irritation. Antibiotics can be given in the event of a bacterial infection. Eye shields and compresses are not indicated in the management of this condition. PTS: 1 DIF: Cognitive Level: Application REF: 599 OBJ: 4 TOP: Keratitis: Initial Remedy KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 4. The patient with a corneal transplant asks how long he must wear the eye shield at night. The nurse instructs the patient that he should wear the shield for at least what period of time? a. 1 month b. 2 months c. 6 months d. 1 year ANS: A Nightly wearing of the eye shield following a corneal transplant is recommended for 1 month following surgery. PTS: 1 DIF: Cognitive Level: Knowledge REF: 600, Box 26-1 OBJ: 2 TOP: Corneal Transplant: Eye Shield Use KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 5. The nurse is discussing the postoperative period with a patient with a corneal transplant. Which statement indicates that the patient displays realistic expectations about vision improvement? a. “I will have my full vision restored within 48 to 72 hours.” b. “It will take about 24 hours before I see improvement in my vision.” c. “My vision will show improvement in about 2 weeks.” d. “It may take about a month before my vision shows improvement.” ANS: C Increasing visual acuity may take up to 2 weeks before improvement in vision is noted. PTS: 1 DIF: Cognitive Level: Comprehension REF: 602 OBJ: 2 TOP: Corneal Transplant: Recovery Time KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 6. The patient who had a corneal transplant is taught that inflammatory changes (redness, swelling, and pain) in the corneal graft are best indicators of which complication? a. Graft rejection b. Allergy to graft c. Infection d. Revascularization ANS: A Inflammatory symptoms are indicative of graft rejection. PTS: 1 DIF: Cognitive Level: Comprehension REF: 600 OBJ: 2 TOP: Corneal Transplant: Graft Rejection KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 7. A patient presents to a walk-in clinic with a small piece of rock deeply embedded in his right eye. What should the nurse do first? a. Flush the eye with a continuous stream of warm water. b. Refer the patient to the emergency department. c. Irrigate the eye with cool water. d. Cover both eyes with a dressing. ANS: D If a foreign body is sticking out of the eye, no attempt to remove it should be made. Both eyes should be patched to prevent further eye movement, and then the patient should be referred to the emergency department or to an ophthalmologist. For foreign bodies not deeply embedded in the tissues of the eye, irrigation can easily remove them. Irrigation with clear, lukewarm water or sterile water or saline is used to remove a foreign body sticking to the cornea. PTS: 1 DIF: Cognitive Level: Analysis REF: 600 OBJ: 3 TOP: Eye Injury: Embedded Object KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 8. After teaching a patient about a new eye medication, the nurse observes the patient applying eye ointment. Which technique indicates that the nurse’s teaching has been successful? a. The patient applies the ointment from the inner to outer canthus. b. The patient applies the ointment in the center of the conjunctival sac. c. The patient applies the ointment liberally from the outer to inner canthus. d. The patient applies the ointment directly to the sclera. ANS: A A thin line of eye ointment should be applied from the inner canthus to the outer canthus along the lower eyelid inside the conjunctival sac. PTS: 1 DIF: Cognitive Level: Comprehension REF: 600 OBJ: 12 TOP: Eye Medications: Ointment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 9. The nurse is caring for a patient in the postoperative period after enucleation. Which intervention is most important? a. Provide emotional support. b. Educate the patient about permanent prosthesis placement. c. Resume diet as ordered. d. Educate the patient about postoperative medications. ANS: A Postoperatively, the nurse should observe for signs of complications such as excessive bleeding, swelling, increased pain, elevated temperature, or displacement of the implant. Losing an eye is a devastating experience even when there has been a long period of painful blindness preoperatively. Understanding of the emotional impact and support of the patient are prime nursing responsibilities. The permanent prosthesis is placed about 6 weeks after the surgery, and while it is important to teach the patient about prosthetic placement and medications, providing support is most important. PTS: 1 DIF: Cognitive Level: Analysis REF: 601 OBJ: 11 TOP: Enucleation: Preoperative Teaching KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 10. The patient with glaucoma is prescribed an Ocusert miotic. How often should the medication be replaced? a. Daily b. Semiweekly c. Weekly d. Biweekly ANS: C Eye medications that are delivered per Ocusert are replaced every week. PTS: 1 DIF: Cognitive Level: Comprehension REF: 606, Table 26-1 OBJ: 12 TOP: Ocusert: Replacement Frequency KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 11. The nurse is caring for a patient who is receiving dipivefrin (Propine). Which abnormal finding is an expected side effect of this medication? a. Blood pressure 80/50 b. Pulse 112 c. Respirations 8 d. Temperature 102.4 ANS: B Sympathomimetic drugs such as dipivefrin are used to reduce intraocular pressure by increasing aqueous outflow. They can cause tachycardia and hypertension. PTS: 1 DIF: Cognitive Level: Application REF: 607, Table 26-1 OBJ: 4 TOP: Sympathomimetic Drugs: Side Effects KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 12. Which manifestation is the classic early warning symptom of a detached retina? a. Tearing and swelling of the eye b. Flashing colored lights in the eye c. Bleeding into the anterior chamber d. Intense brow pain ANS: B Seeing flashing colored lights is an early warning symptom of retinal detachment. PTS: 1 DIF: Cognitive Level: Comprehension REF: 609 OBJ: 4 TOP: Retinal Detachment: Early Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 13. The nurse is teaching a patient who is scheduled to undergo surgery to manage glaucoma. Which statement indicates that the patient understands the nurse’s teaching about the procedure? a. “The surgery will increase outflow of aqueous humor.” b. “The surgery will reduce amount of vitreous humor.” c. “The surgery will widen my pupils.” d. “The surgery will reduce pain.” ANS: A Glaucoma is a condition that causes increased ocular pressure. Surgical management for the condition seeks to provide an increased outflow of aqueous humor. PTS: 1 DIF: Cognitive Level: Comprehension REF: 609 OBJ: 11 TOP: Glaucoma: Surgical Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 14. The nurse is caring for a patient with suspected macular degeneration. During the assessment the patient is asked to focus on an image. Which finding supports the diagnosis? a. The patient only sees disconnected pieces of the image. b. The patient sees a dark spot in the center of what is viewed. c. The patient sees nothing in the peripheral vision. d. The patient sees wavy lines and bright flashing lights. ANS: B The person with macular degeneration sees a dark spot in his central vision. Peripheral vision is not affected until later in the disease. PTS: 1 DIF: Cognitive Level: Application REF: 612 OBJ: 4 TOP: Macular Degeneration: Early Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 15. The nurse is caring for a patient with Ménière disease. Which action is most important for the nurse to take? a. Speak loudly and clearly into the affected ear. b. Restrict sodium intake. c. Encourage frequent ambulation. d. Encourage fluid intake. ANS: B Treatment of Ménière disease focuses on relieving symptoms; there is no cure for this condition, although the disorder does disappear spontaneously in some cases. To control edema and reduce pressure in the inner ear, the patient may be placed on a low-sodium diet. The patient’s fluid intake may be restricted, and diuretics may be ordered. The nurse should avoid turning on bright overhead lights, making loud noises, or having the patient reposition unnecessarily. PTS: 1 DIF: Cognitive Level: Comprehension REF: 617-618 OBJ: 8 TOP: Ménière Disease: Reduction of Nausea and Vomiting KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 16. The nurse is reviewing the plan of care for a patient following a tympanoplasty. Which intervention should the nurse implement in the immediate postoperative period? a. Keep the patient flat in bed. b. Encourage deep breathing and coughing. c. Reposition the patient quickly to reduce nausea and vomiting. d. Position the patient’s head with the affected ear touching the mattress. ANS: A Postoperative care involves keeping the patient quiet and flat in bed for at least 12 hours. Coughing and sneezing should be avoided, or if unavoidable, should be accomplished with the mouth open to decrease pressure in the ear. Position changes should be accomplished slowly. The head is turned so that the affected ear is uppermost. PTS: 1 DIF: Cognitive Level: Application REF: 618 OBJ: 14 TOP: Tympanoplasty: Immediate Postoperative Care KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 17. The nurse is caring for a patient who has come to the ambulatory care clinic after experiencing a chemical burn to the eye. The nurse should irrigate the patient’s eye with which solution? a. Normal saline b. Tap water c. Sterile water d. A mixture of half sterile water and half normal saline ANS: A The preferred solution for use when irrigating the eye is an intravenous bag of normal saline. In the event that normal saline is not available, the next option would be tap water. PTS: 1 DIF: Cognitive Level: Knowledge REF: 601 OBJ: 3 TOP: Removal of Foreign Bodies from the Eye KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 18. The nurse is caring for patient who presented to an ambulatory care clinic with a large amount of sand in his eyes following an all-terrain vehicle accident. After the nurse completes eye irrigation, the patient reports that his eyes still hurt and feel irritated. What action is most appropriate? a. Instruct the patient that these feelings are normal after an eye irrigation. b. Instruct the patient that the prescribed ointment will help to soothe the eye irritation. c. Repeat the eye irrigation with a solution of 50% sterile water and normal saline. d. Notify the physician. ANS: D The continued sensation of grittiness or irritation may signal the presence of a corneal abrasion. To prevent further injuries, the nurse should notify the physician. PTS: 1 DIF: Cognitive Level: Application REF: 600 OBJ: 3 TOP: Removal of Foreign Bodies from the Eye KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort MULTIPLE RESPONSE 19. The nurse is caring for a patient following a left corneal transplant. When positioning the patient, the nurse correctly assists the patient into which positions? (select all that apply.) a. Supine b. Supine with head on small pillow c. Left side-lying d. Right side-lying e. High Fowler ANS: A, B, D The patient may lie only on his back and nonoperative side postoperatively. Flat on his back, on his back with his head on a small pillow, and positioned on his nonoperative side are acceptable as all these positions place no undue pressure on the transplant. Allowing the patient to rest on the operative side or in high Fowler position would place excessive pressure on the operative site. PTS: 1 DIF: Cognitive Level: Application REF: 600 OBJ: 2 TOP: Corneal Transplant: Postoperative Positioning KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 20. A patient comes to the ambulatory care clinic after getting hay into the eyes while farming. Which action(s) should the nurse implement? (select all that apply.) a. Flush the eye with warm saline. b. Hold the eyelids open. c. Tilt the head back. d. Use a moistened sterile cotton swab. e. Ask the patient to rub the eyes with the lids closed to produce more tears. ANS: A, B, C, D If the foreign body is not deeply embedded in the tissues of the eye, it can easily be removed by irrigation. Irrigation with clear, lukewarm water or sterile water or saline is used to remove a foreign body sticking to the cornea. Have the patient tilt the head back. Hold the eyelids open to prevent blinking. Sometimes a speck of foreign matter on the cornea can be removed with a moistened, sterile cotton swab. The goals of treatment will be to remove the foreign objects from the eyes and to prevent further injury to the eye. Rubbing an irritated eye may cause a corneal abrasion. PTS: 1 DIF: Cognitive Level: Application REF: 600 OBJ: 3 TOP: Eye: Foreign Body Removal KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 21. Which manifestation(s) is/are symptoms of a cataract? (select all that apply.) a. Nystagmus b. Troubled by glare c. Increased myopia d. Color distortion e. Night blindness ANS: B, C, D, E A cataract is opacity of the lens that produces an effect similar to one a person would get when looking through a sheet of falling water. A cataract causes a blurring of vision because the lens, which is normally transparent, becomes cloudy and opaque. Nystagmus is not a symptom of a cataract. All other options are classic symptoms of a person with a developing cataract. PTS: 1 DIF: Cognitive Level: Comprehension REF: 602 OBJ: 4 TOP: Cataract: Classic Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 22. The nurse is performing postoperative teaching for a patient who underwent a left cataract removal. Which information should the nurse include in the teaching plan? (select all that apply.) a. Sleep on the right side. b. Take a stool softener to avoid straining during bowel movements. c. Bend at the waist and avoid stooping. d. Wash hands before instilling eyedrops. e. Follow the prescribed medication schedule exactly. ANS: A, B, D, E The patient should sleep on the unaffected side, use a stool softener to prevent straining, wash hands before instilling eyedrops, and follow the prescribed medication schedule exactly. The patient should not bend from the waist as the position increases intraocular pressure. PTS: 1 DIF: Cognitive Level: Application REF: 602-603, Nursing Care Plan 26-1 OBJ: 5 TOP: Cataract: Postoperative Teaching KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 23. Following a scleral buckling procedure, which intervention(s) should the nurse include in the postoperative care? (select all that apply.) a. Speak before touching the patient. b. Administer a laxative. c. Warn the patient that vision does not return immediately. d. Instruct the patient to wear an eye shield at night and while napping. e. Instruct the patient to change the eye patch twice daily. ANS: A, B, C, D The patient will return from the surgery with an eye patch in place. The nurse should speak before touching the patient so the patient is not startled. The nurse should administer a laxative to prevent straining during bowel movements. The nurse should warn the patient that vision does not return immediately and instruct the patient to wear an eye shield at night or when napping. This procedure does not require changing an eye patch twice daily. PTS: 1 DIF: Cognitive Level: Comprehension REF: 610 OBJ: 5 (theory) TOP: Scleral Buckling: Postoperative Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 24. The nurse has completed the assessment on a newly admitted patient. Which finding(s) is/are risk factor(s) in the development of cataracts? (select all that apply.) a. Cigarette smoking b. Completion of radiation therapy c. Hormone replacement therapy d. Long-term corticosteroid use e. History of gastroesophageal reflux disease (GERD) ANS: A, D Traumatic cataracts may occur from a physical blow, extreme heat, or chemical toxins. Cigarette smoking increases the risk of developing cataracts, and heavy drinking is also implicated. Chronic use of corticosteroids predisposes a patient to developing cataracts. Radiation therapy, hormone replacement therapy, and GERD are not risk factors for cataracts. PTS: 1 DIF: Cognitive Level: Comprehension REF: 601 OBJ: 4 TOP: Cataracts: Etiology KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance COMPLETION 25. Accommodation is accomplished through the interaction of the ciliary bodies and the _____. ANS: lens Ciliary muscles and ligaments change the shape of the lens to provide accommodation, which is the bending of light rays to focus on the retina. PTS: 1 DIF: Cognitive Level: Knowledge REF: 598 OBJ: 1 TOP: Accommodation: Physiology KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance MATCHING Place the steps of eye irrigation in appropriate sequence. a. Ask patient to turn head to affected side. b. Don gloves. c. Direct continuous stream of fluid from inner to outer canthus. d. Instruct patient to lie supine. e. Hold lids apart with thumb and finger. f. Have patient close eyes to move debris from upper eyelid to conjunctival sac. 26. Step 1 27. Step 2 28. Step 3 29. Step 4 30. Step 5 31. Step 6 26. ANS: D PTS: 1 DIF: Cognitive Level: Analysis REF: 601 OBJ: 12 TOP: Eye Irrigation: Technique KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 27. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 601 OBJ: 12 TOP: Eye Irrigation: Technique KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 28. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 601 OBJ: 12 TOP: Eye Irrigation: Technique KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 29. ANS: E PTS: 1 DIF: Cognitive Level: Analysis REF: 601 OBJ: 12 TOP: Eye Irrigation: Technique KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 30. ANS: C PTS: 1 DIF: Cognitive Level: Analysis REF: 601 OBJ: 12 TOP: Eye Irrigation: Technique KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 31. ANS: F PTS: 1 DIF: Cognitive Level: Analysis REF: 601 OBJ: 12 TOP: Eye Irrigation: Technique KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance Arrange the steps of the pathophysiologic process of open-angle glaucoma in the correct order. a. Intraocular pressure exceeding 25 mm Hg b. Optic nerve and retina damaged by ischemia c. Permanent and irreversible vision impairment d. Overproduction of aqueous humor e. Continued high intraocular pressure restricting blood flow to optic nerve and retina 32. Step 1 33. Step 2 34. Step 3 35. Step 4 36. Step 5 32. ANS: D PTS: 1 DIF: Cognitive Level: Application REF: 605 OBJ: 4 TOP: Glaucoma: Pathophysiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 33. ANS: A PTS: 1 DIF: Cognitive Level: Application REF: 605 OBJ: 4 TOP: Glaucoma: Pathophysiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 34. ANS: E PTS: 1 DIF: Cognitive Level: Application REF: 605 OBJ: 4 TOP: Glaucoma: Pathophysiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 35. ANS: B PTS: 1 DIF: Cognitive Level: Application REF: 605 OBJ: 4 TOP: Glaucoma: Pathophysiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 36. ANS: C PTS: 1 DIF: Cognitive Level: Application REF: 605 OBJ: 4 TOP: Glaucoma: Pathophysiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation Chapter 27: The Gastrointestinal System deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse cautions that constant stress can cause which alteration to the gastrointestinal (GI) system? a. Slowed GI mobility resulting in constipation b. Reversed peristalsis resulting in projectile vomiting c. Increased digestive juices resulting in a gastric ulcer d. Decreased digestive juices resulting in ineffective metabolism ANS: C Stress increases the gastric secretions, which irritate and finally ulcerate the gastric mucosal lining. PTS: 1 DIF: Cognitive Level: Comprehension REF: 627 OBJ: 2 (theory) TOP: Stress: Gastric Ulcer KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 2. The nurse is caring for multiple patients. The nurse determines that which patient has the highest risk for developing gallstones? a. A 37-year-old white man of normal weight on long-term corticosteroids for asthma. b. A 42-year-old African American man of normal weight who has smoked for 25 years. c. A 46-year-old Indonesian woman who is under normal weight and has recently had radiation treatments. d. A 50-year-old obese Mexican American woman who has type 1 diabetes. ANS: D Obesity, diabetes mellitus (DM), rapid weight loss, and Crohn disease increase the risk for the development of gallstones. Native Americans and Mexican Americans have an ethnic predisposition to gallstones. PTS: 1 DIF: Cognitive Level: Analysis REF: 628 OBJ: 1 (theory) TOP: Gallstones: Risk Factors KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 3. The home health nurse is caring for the patient with tuberculosis who is taking rifampin and isoniazid (INH). The nurse should carefully monitor the patient for which potential side effect? a. Gallstones b. Liver disorders c. Bleeding ulcers d. Esophagitis ANS: B Rifampin and INH are both hepatotoxic. PTS: 1 DIF: Cognitive Level: Application REF: 629 OBJ: 2 TOP: Liver Disorders: Etiology KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 4. The nurse is obtaining a history of a patient with hepatitis A. Which question is most appropriate for the nurse to ask? a. “If using drugs, do you share needles?” b. “Do you always practice safe sex?” c. “Have you traveled to Canada in the last month?” d. “Do you eat shellfish or oysters often?” ANS: D Shellfish and mollusks can be contaminated by living in feces-contaminated water. Drug use and unprotected sex are not part of the etiology of hepatitis A but are for hepatitis B. Travel to Canada is not associated with hepatitis A. PTS: 1 DIF: Cognitive Level: Application REF: 629, Health Promotion OBJ: 1 (clinical) TOP: Hepatitis A: Etiology KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 5. The nurse is caring for a patient who complains, “I don’t see why I can’t have a CT scan instead of the expensive MRI!” Which response is most appropriate for the nurse to make? a. “The MRI provides better contrast between normal and pathologic tissue.” b. “The MRI requires less analysis and is easier to read.” c. “The MRI produces a digital image that can be transmitted via e-mail.” d. “The MRI exposes the patient to less radiation.” ANS: A Magnetic resonance imaging (MRI) uses radiofrequency signals to determine how hydrogen atoms behave in the magnetic field. In addition, the MRI provides a better contrast than computed tomography (CT) between healthy tissues and pathologic tissues. PTS: 1 DIF: Cognitive Level: Comprehension REF: 631, Table 27-1 OBJ: 4 TOP: MRI: Advantages KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 6. The nurse is preparing to administer liquid laxative to a patient in preparation for a colonoscopy. Which action should the nurse take? a. Offer a small snack. b. Take the patient’s temperature. c. Mix the laxative with orange juice. d. Chill the laxative and pour it over ice. ANS: D Chilling the laxative or pouring it over ice makes the drink more palatable and easier to swallow. The nurse should not offer any food, as the accuracy of the test depends on adequate bowel prep. The laxative does not affect the patient’s temperature. Mixing the laxative with another substance can make it difficult to judge how much the patient actually consumed if any liquid is remaining. PTS: 1 DIF: Cognitive Level: Application REF: 629 OBJ: 4 TOP: Oral Laxative: Techniques of Administration KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 7. The nurse caring for an 80-year-old woman who is undergoing the extensive bowel preparation for a colonoscopy. The nurse should most closely monitor the patient for which potential complication? a. Diarrhea b. Metabolic acidosis c. Fatigue d. Dyspnea ANS: B The older patient is especially at risk for problems of electrolyte imbalance, fluid overload, or dehydration when undergoing preparation for diagnostic tests that require a fasting state and/or bowel cleansing. Metabolic acidosis can occur when there is a large volume loss of bowel content. Bowel preparation causes diarrhea and may cause fatigue; bowel preparation should not cause dyspnea. PTS: 1 DIF: Cognitive Level: Understanding REF: 629, Older Adult Care Points OBJ: 4 TOP: Bowel Preparation: Side Effects KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 8. The nurse is caring for a patient who returns to the floor at lunch time after undergoing an upper GI (UGI series). Which action is most important for the nurse to perform first? a. Administer a laxative. b. Educate the patient about the possibility of white stools. c. Offer the patient a small snack. d. Provide oral care. ANS: A The contrast media used in the series features barium that can harden and lead to an impaction. Patients should have a bowel movement quickly after the procedure to eliminate the medium from the body. While fluids and snacks or meal trays should be given as quickly as possible, patients should be educated about the possibility of white stools for several days postprocedure, and oral care should be provided, these interventions are of lesser importance since they do not directly work to quickly prevent a postprocedure complication. PTS: 1 DIF: Cognitive Level: Analysis REF: 630, Table 27-1 OBJ: 4 TOP: UGI Series: Aftercare KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 9. The nurse is assessing a patient’s bowel sounds. After auscultating each quadrant for 30 seconds, the nurse fails to hear any sounds. How should the nurse document this finding? a. Absent bowel sounds b. Hypoactive bowel sounds c. Active bowel sounds d. Hyperactive bowel sounds ANS: B Hypoactive bowel sounds can be noted in the medical record when no sounds are heard after listening in each of the four quadrants for 30 seconds. For bowel sounds to be considered absent, it is necessary to verify that no sounds are heard after listening in each of the four quadrants for 5 minutes. If hyperactive, high-pitched sounds are heard in one quadrant, and decreased sounds are heard in another quadrant, assess for nausea and vomiting, as the patient may have an intestinal obstruction. PTS: 1 DIF: Cognitive Level: Comprehension REF: 636, Clinical Cues OBJ: 1 (clinical) TOP: Bowel Sounds: Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 10. When assessing a patient’s bowel sounds, nurse auscultates loud bowel sounds in each quadrant every 3 seconds. The nurse understands that these findings could indicate that the patient is experiencing which condition? a. Diarrhea b. Paralytic ileus c. Vomiting d. Constipation ANS: A Loud, rapid bowel sounds are indicative of hypermobility, which could result in diarrhea. Absent bowel sounds are associated with paralytic ileus. Normal bowel sounds present as soft gurgles and clicks every 5 to 15 seconds. Hypoactive bowel sounds indicate decreased motility and could indicate that the patient is constipated? PTS: 1 DIF: Cognitive Level: Application REF: 636 OBJ: 1 (clinical) TOP: Bowel Sounds: Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 11. The nurse is reviewing a student nurse’s charting and notes that the student has documented absent bowel sounds. The nurse reminds the student that in order to document absent bowel sounds, one must auscultate each quadrant at what period of time? a. 30 seconds b. 1 minute c. 2 minutes d. 5 minutes ANS: D The criterion for the documentation of absent bowel sounds is that each quadrant is auscultated for 5 minutes. PTS: 1 DIF: Cognitive Level: Knowledge REF: 636 OBJ: 1 (clinical) TOP: Bowel Sounds: Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 12. The nurse is percussing a patient’s abdomen and hears a dull thud in the right upper quadrant. This sound indicates that nurse is percussing over which location? a. The liver b. The small intestine c. The stomach d. The lungs ANS: A Percussion is performed by placing the middle finger of one hand on the abdomen and striking the finger lightly below the knuckle and listening for the pitch of sound produced. A dull thud would be heard over the liver. Tympany would be heard over the stomach and intestines, and resonance would be heard over lung tissue. PTS: 1 DIF: Cognitive Level: Comprehension REF: 637 OBJ: 1 (clinical) TOP: Abdominal Assessment: Percussion KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 13. During a morning assessment, the nurse observes that a patient displays bulging flanks when supine with the knees flexed. Which action should the nurse take next? a. Measure the patient’s abdominal girth. b. Auscultate each quadrant of the abdomen for 5 minutes. c. Document the finding. d. Notify the charge nurse. ANS: A The nurse’s initial assessment indicates fluid accumulation. The nurse needs to obtain more information, first measuring abdominal girth. The nurse can then percuss from the umbilicus to the flanks to detect fluid shifts, and document all findings. The nurse will only auscultate bowel sounds for 5 minutes in each quadrant if bowel sounds are not heard before then. It is unnecessary to notify the charge nurse at this time. PTS: 1 DIF: Cognitive Level: Application REF: 637 OBJ: 7 TOP: Ascites: Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 14. The nurse is reviewing the laboratory results of an assigned patient. The serum bilirubin is 2.8 mg/dL. The nurse anticipates that the patient’s urine will display which finding? a. Dark color b. Low specific gravity c. Very scant amount d. Foul odor ANS: A Normal serum bilirubin is 0.1 to 1.2 mg/dL. Jaundice is present at readings above 2.5 mg/dL. The patient who is jaundiced will have dark, tea-colored urine. Specific gravity refers to the concentration of the urine. The amount and odor of urine will not be directly influenced by the bilirubin level. PTS: 1 DIF: Cognitive Level: Application REF: 637 OBJ: 7 TOP: Liver Disorder: Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 15. The nurse is caring for a patient who is complaining of postoperative gas pain. What intervention should nurse implement? a. Assist the patient with ambulation. b. Apply a cold compress on the abdomen. c. Offer a cup of coffee or tea. d. Offer chilled vegetable juice. ANS: A Ambulation is the most effective method for helping a patient expel gas. Hot or cold beverages and cold compresses will increase gas. PTS: 1 DIF: Cognitive Level: Comprehension REF: 640 OBJ: 4 TOP: Flatus: Interventions KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 16. The nurse is planning care for a patient who has experienced moderate diarrhea for 3 days. Which collaborative intervention is most important to include in the plan of care? a. Place the patient on NPO status. b. Limit the patient’s diet to clear liquids. c. Administer parenteral nutrition. d. Restrict the patient’s diet to soft foods only. ANS: B If diarrhea is moderate, only clear liquids are permitted by mouth. If the diarrhea is severe, nothing is given by mouth until it subsides. Severe, long-term diarrhea may require the use of total parenteral nutrition. When diarrhea is caused by infection, stool cultures and antibiotics may be necessary. As the condition improves, the diet is advanced. PTS: 1 DIF: Cognitive Level: Application REF: 641 OBJ: 5 TOP: Diarrhea KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 17. The nurse is talking with a patient who has been experiencing nausea and vomiting. The patient indicates an interest in using alternative therapies for the condition. Which product may aid in nausea management? a. Ginger b. Ginseng c. Chamomile d. Soy ANS: A Ginger has been used for centuries in Asia to combat nausea and vomiting, motion sickness, and dyspepsia. It is available candied in capsules, fluid extract, and tablets, and tincture or as fresh ginger root that can be grated and used to make tea. Ginger may decrease the action of histamine (H2) receptor antagonists and proton pump inhibitors and may increase absorption of medications taken orally. Ginger may decrease the effect of antidiabetic medications. It should not be used during pregnancy or lactation. PTS: 1 DIF: Cognitive Level: Comprehension REF: 639 OBJ: 9 TOP: Ginger for Nausea KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 18. The nurse is caring for a patient who has been experiencing severe diarrhea and can now resume solid foods. The nurse educates the patient about appropriate food choices. Which food choice indicates that the nurse’s teaching has been successful? a. Whole-grain rice b. Wheat toast c. Applesauce d. Grapes ANS: C When a patient has severe diarrhea and is allowed to resume solid foods, the foods should be slowly introduced in order to help thicken the stool. Foods such as applesauce, pretzels, bananas, white rice, white toast, and yogurt are beneficial. PTS: 1 DIF: Cognitive Level: Application REF: 641, Nutrition Considerations OBJ: 5 TOP: Nutrition Considerations: Foods That Thicken Stool KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 19. The nurse is performing preprocedure teaching for a patient scheduled to undergo a liver biopsy. After listening to the information, the patient states, “I am so scared. I just don’t know if I can do this procedure.” Which response is best? a. “The procedure will only last about 15 minutes.” b. “Most patients say it feels similar to a punch in the shoulder.” c. “You do not have to have the procedure.” d. “I understand that you are afraid. Tell me more about your concerns.” ANS: D The nurse should acknowledge the patient’s feelings and promote therapeutic communication. While all of the other statements are true, none of them investigate the underlying cause of the patient’s fear. Reassurance about the length of the procedure or the sensation that the patient might experience may be indicated after the patient explains more about specific concerns. While the patient can refuse to have the procedure, dismissing the patient is not an appropriate or therapeutic statement. PTS: 1 DIF: Cognitive Level: Analysis REF: 633, Table 27-1 OBJ: 8 TOP: Liver Biopsy KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity MULTIPLE RESPONSE 20. The nurse explains that the older adult is prone to digestive disorders related to which age-related change(s)? (select all that apply.) a. Decreased hydrochloric acid b. Increased enzyme levels c. Inadequate chewing d. Diminished intestinal motility e. Gastroesophageal sphincter incompetence ANS: A, C, D, E Age-related changes that predispose the older adult to digestive disorders include decreased hydrochloric acid, inadequate chewing, diminished intestinal motility, and gastroesophageal sphincter incompetence. Age does not increase digestive enzyme levels. PTS: 1 DIF: Cognitive Level: Comprehension REF: 626 OBJ: 6 TOP: Age-Related Changes to GI System KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 21. Which factor(s) increase the risk for developing pancreatic cancer? (select all that apply.) a. Obesity b. Jewish ethnicity c. Diabetes mellitus (DM) d. Hepatitis A e. Smoking ANS: A, C, E Pancreatic cancer incidence rises steadily with age. Although the cause of pancreatic cancer is not known, the incidence is higher in cigarette smokers. Obesity, chronic pancreatitis, and DM are also risk factors for this cancer. Jewish ethnicity and hepatitis are not contributory to the disease. PTS: 1 DIF: Cognitive Level: Comprehension REF: 629 OBJ: 2 TOP: Pancreatic Cancer: Risk Factors KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 22. Which action(s) should the nurse recommend to promote a patient’s bowel health? (select all that apply.) a. Exercise regularly. b. Include adequate bulk in the diet. c. Drink adequate water. d. Defecate at approximately the same time every day. e. Take a laxative to maintain a regular defecation pattern. ANS: A, B, C, D Daily exercise and intake of adequate bulk and water are contributions to bowel health. Heeding the need to defecate and defecating at the same time daily will help to keep the gastrocolic reflex healthy. Taking daily laxatives is not conducive to good bowel health. PTS: 1 DIF: Cognitive Level: Comprehension REF: 640 OBJ: 3 TOP: Bowel Health: Maintenance KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 23. The nurse is caring for a patient scheduled to have an MRI study. Which instruction(s) should the nurse include in the teaching? (select all that apply.) a. Radiation exposure is extremely minimal. b. All metal objects, including dental bridges, jewelry, and body piercings, must be removed. c. Do not eat or drink for 4 hours before the procedure. d. A radiopaque medium may be injected during the procedure. e. There may be a tingling sensation in metal alloy filling of the teeth. ANS: B, D, E The MRI places the patient in a magnetic field and uses radiofrequency signals to determine how hydrogen atoms behave in the field. All metal must be removed, contrast medium may be injected, and the patient may have a tingling sensation in the teeth with metal alloy fillings. There is no restriction on food or fluid intake in relation to the test. The test does not expose the patient to radiation. PTS: 1 DIF: Cognitive Level: Comprehension REF: 631, Table 27-1 OBJ: 4 TOP: MRI: Preparation and Teaching KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 24. The nurse is caring for a patient immediately following a liver biopsy. Which actions are appropriate for the nurse to take? (select all that apply.) a. Position the patient on the right side. b. Assess the patient’s pain. c. Monitor vital signs every 15 minutes for the first hour. d. Instruct patient to cough and deep-breathe. e. Assess for hematoma at puncture site. ANS: A, B, C, E The liver biopsy is performed under local or general anesthesia. Postprocedural care will include positioning on the right side for the first 2 hours, and assessing pain, vital signs and the puncture site. The patient should not cough as it increases intra-abdominal pressure and may stimulate bleeding. PTS: 1 DIF: Cognitive Level: Application REF: 633, Table 27-1 OBJ: 5 TOP: Liver Biopsy: Aftercare KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 25. The nurse is caring for a patient with anorexia nervosa. Which intervention(s) might the nurse use to stimulate appetite? (select all that apply.) a. Offer oral care after meals. b. Arrange for preferred foods to be served. c. Encourage family members to bring food from home. d. Suggest that family members or friends come and socialize during the meal. e. Allow ample time to eat and enjoy the meal. ANS: B, C, D, E Appetite depends on complex mental processes having to do with memory and mental associations that can be pleasant or extremely unpleasant. Appetite is stimulated by the sight, smell, and thought of food. The physical and social environment in which a person is eating stimulates appetite. The enjoyment of eating can be inhibited by unattractive or unfamiliar food, by unpleasant surroundings, and by emotional states such as anxiety, anger, and fear. By serving food based on patient’s preferences, encouraging positive interaction, and allowing ample times for meals, the nurse can stimulate appetite. Oral care should be offered before meals to aid in stimulating the appetite. PTS: 1 DIF: Cognitive Level: Comprehension REF: 638 OBJ: 3 TOP: Anorexia: Interventions KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 26. Before a nurse can document the presence of diarrhea, which criteria must be met? (select all that apply.) a. One loose stool in a 24-hour period b. Multiple liquid or semiliquid stools in a 24-hour period c. Hyperactive bowel sounds d. Cramping e. Fever ANS: B, C, D Multiple liquid or semiliquid stools in a 24-hour period with hyperactive bowel sounds with cramping are the criteria for diarrhea. Fever is not a diagnostic criteria for diarrhea, and a single loose stool is merely documented as such. PTS: 1 DIF: Cognitive Level: Comprehension REF: 640-641 OBJ: 5 TOP: Diarrhea: Criteria KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease COMPLETION 27. The nurse caring for the patient who has diarrhea from taking a protocol of oral amoxicillin will use __________ Precautions in the care. ANS: Standard standard The diarrhea caused by medications is not infectious and should be dealt with using Standard Precautions. PTS: 1 DIF: Cognitive Level: Comprehension REF: 641 OBJ: 5 TOP: Diarrhea: Standard Precautions KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control MATCHING Match each term with its correct definition. a. Absorption b. Peristalsis c. Metabolism d. Anabolism e. Catabolism 28. Rhythmic squeezing action of intestinal tract 29. Chemical process to make substances needed by the body 30. Repair of body tissue 31. Breaking down larger molecules into smaller molecules 32. Transfer of nutrients from intestine to bloodstream 28. ANS: B PTS: 1 DIF: Cognitive Level: Comprehension REF: 627 OBJ: 1 TOP: Terminology KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 29. ANS: C PTS: 1 DIF: Cognitive Level: Comprehension REF: 627 OBJ: 1 TOP: Terminology KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 30. ANS: D PTS: 1 DIF: Cognitive Level: Comprehension REF: 627 OBJ: 1 TOP: Terminology KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 31. ANS: E PTS: 1 DIF: Cognitive Level: Comprehension REF: 627 OBJ: 1 TOP: Terminology KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 32. ANS: A PTS: 1 DIF: Cognitive Level: Comprehension REF: 627 OBJ: 1 TOP: Terminology KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance Chapter 28: Care of Patients with Disorders of the Upper Gastrointestinal System deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse explains that the diagnosis of morbidly obese is reserved for people who exceed which percentage of their recommended weight? a. 50% b. 70% c. 90% d. 100% ANS: D Those people who weigh 100% over their recommended weight are considered morbidly obese. PTS: 1 DIF: Cognitive Level: Comprehension REF: 645 OBJ: 1 TOP: Obesity: Morbid Obesity KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 2. The nurse calculates the body mass index (BMI) of a man who is 6 feet tall and weighs 150 pounds. Which value is correct? a. 21.0 b. 25.0 c. 43.1 d. 66.3 ANS: A The formula to calculate BMI is: weight in kilograms divided by height in meters squared (68.1 kilograms ÷ 3.24 meters = 21.0). PTS: 1 DIF: Cognitive Level: Application REF: 645 OBJ: 1 TOP: BMI: Calculation KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 3. The nurse explains that the laparoscopic adjustable gastric banding surgery is best described as which type of bariatric surgery? a. Restrictive b. Malabsorptive c. Restrictive/malabsorptive d. Obstructive ANS: A The three types of bariatric surgery are restrictive, malabsorptive, and restrictive/malabsorptive. Laparoscopic adjustable gastric banding is performed by placing an inflatable band around the fundus of the stomach and is considered restrictive. This procedure may be performed laparoscopically. The band is inflated and deflated via a subcutaneous port to change the size of the stomach as the patient loses weight. PTS: 1 DIF: Cognitive Level: Comprehension REF: 646 OBJ: 1 TOP: Restrictive Procedures KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 4. The nurse is discussing bariatric surgery complications with a patient. Which statement indicates that the patient accurately understands the nurse’s teaching about common procedural side effects? a. “I understand that gastric ulcers frequently occur in patients who have bariatric surgery.” b. “Gallstones are a common occurrence in patients who have bariatric surgery.” c. “I know an umbilical hernia might happen after I have bariatric surgery.” d. “Unfortunately, I may experience gastritis after having bariatric surgery.” ANS: B Nutritional deficiencies caused by the banding result in the formation of gallstones in a large percentage of bariatric surgery patients. About a third of patients who undergo bariatric surgery develop gallstones. PTS: 1 DIF: Cognitive Level: Comprehension REF: 646 OBJ: 1 TOP: Bariatric Surgery: Side Effects KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. The nurse is caring for a patient with suspected dysphagia. Which action is most appropriate for the nurse to take? a. Encourage incentive spirometry use. b. Instruct the patient to take practice swallows before the meal. c. Encourage patient attempts to communicate, and pay attention to nonverbal cues. d. Encourage the patient to keep a food diary. ANS: B Dysphagia means difficulty in swallowing. The nurse should have the patient take some “practice swallows” before beginning the meal, and watch to see that the larynx rises with each swallow. Incentive spirometry usage is important or patients with dyspnea, or shortness of breath. Encouraging communication and paying attention to nonverbal cues is an effective intervention for aphasia (inability to use or understand words). Keeping a food diary may be useful in cases of polyphagia (extreme hunger), but it does not evaluate whether or not the patient can swallow effectively. PTS: 1 DIF: Cognitive Level: Application REF: 648 OBJ: 6 TOP: Dysphagia: Evaluation of the Swallow KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 6. A patient with a gastrostomy tube gets a bolus feeding of 200 mL every 4 hours. Before giving the bolus, the nurse aspirates a residual of 100 mL. Which action is most appropriate? a. Give the 200 mL feeding. b. Record the residual and give 100 mL of the feeding. c. Document the residual and hold the feeding. d. Position the patient in high Fowler position and give the feeding. ANS: C On finding a large residual, the nurse should return the residual to the patient, document the amount of the residual, and hold the feeding to avoid possible aspiration. PTS: 1 DIF: Cognitive Level: Application REF: 663 OBJ: 7 (theory) TOP: Gastrostomy Feeding: Evaluating Residual KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 7. Which causative agent is the primary cause of Barrett esophagus? a. Gastroesophageal reflux disease (GERD) b. Eating hot, spicy foods c. Anorexia nervosa d. Esophageal polyps ANS: A A major cause of Barrett esophagus is esophageal reflux. PTS: 1 DIF: Cognitive Level: Comprehension REF: 649 OBJ: 4 TOP: Barrett Esophagus: Etiology KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 8. The nurse is educating a patient with Barrett esophagus. Which statement indicates that the patient requires a need for further instruction? a. “I should eat smaller meals and avoid foods that cause reflux.” b. “I can still have a small glass of wine with dinner.” c. “I should consider switching to smokeless tobacco.” d. “I should stay upright after eating.” ANS: C Care of the patient with Barrett esophagus is focused on encouraging measures to prevent GERD and on regular checkups. Patients should be encouraged not to use tobacco products and not to indulge in heavy alcohol use. PTS: 1 DIF: Cognitive Level: Application REF: 649 OBJ: 4 TOP: Barrett Esophagus: Teaching Plan KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 9. The nurse is caring for a patient who is postoperative after esophageal resection. Shortly after the nurse starts a feeding, the patient suddenly becomes dyspneic and complains of substernal pain. What should the nurse do first? a. Stop the feeding. b. Ambulate the patient. c. Notify the charge nurse. d. Reassure the patient. ANS: A After esophageal resection, pain, increased temperature, and dyspnea may indicate leakage of the feeding into the mediastinum. The nurse should immediately discontinue the feeding, then notify the charge nurse and address any patient concerns. Ambulation is not indicated at this time; ambulation is an intervention to address gas pains. PTS: 1 DIF: Cognitive Level: Analysis REF: 649 OBJ: 11 TOP: Esophageal Resection: Complications KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 10. The nurse is educating a patient with a hiatal hernia. Which statement indicates that the patient understands the nurse’s teaching? a. “I should avoid tea and chocolate.” b. “I should wear an abdominal binder for added support. c. “I should sleep flat on a single pillow.” d. “I should not eat within an hour of going to bed.” ANS: A Hiatal hernia is diagnosed by an upper gastrointestinal (GI) series. Nutritional modification indicated in patients with hiatal hernias includes limiting intake of alcohol, chocolate, caffeine, and fatty food. Other treatment includes weight reduction, avoidance of tight-fitting clothes around the abdomen, administration of antacids, histamine (H2)-receptor antagonists, or proton pump inhibitors, and elevation of the head of the bed on 6- to 8-inch blocks. The patient is instructed not to eat within 3 hours of going to bed. PTS: 1 DIF: Cognitive Level: Application REF: 650 OBJ: 14 TOP: Hiatal Hernia: Education KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 11. The nurse is educating a patient who has gastroesophageal reflux disease (GERD) about dietary modification. Which information is most important for the nurse to include in the teaching plan? a. Avoid highly seasoned or spiced foods. b. Drink ginger ale or lemon lime soda rather than cola. c. Use a straw to drink all fluids. d. Eating three meals spaced evenly apart. ANS: A Avoiding highly seasoned or spicy food should be incorporated into diet changes for the patient with GERD. The avoidance of carbonated beverages with meals and the use of a straw do not reduce the impact of GERD. The frequency of dietary intake does not influence GERD. PTS: 1 DIF: Cognitive Level: Application REF: 653, Patient Teaching OBJ: 9 TOP: GERD: Diet Modification KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 12. The nurse is preparing a teaching plan for a patient with gastroesophageal reflux disease (GERD) who has been prescribed multi-drug therapy for treatment. Which information is most important for the nurse to obtain? a. “Can you identify triggers for your reflux?” b. “Can you commit to changing your diet?” c. “Do you understand how each type of medication works?” d. “Do you think you can afford these prescriptions?” ANS: D Drug therapy may include antacids, H2-receptor antagonists, proton pump inhibitors, and prokinetic drugs. Priorities related to education about medication include checking for possible drug interactions with other drugs the patient is taking and verifying that the patient can afford the drugs prescribed. (If the patient cannot afford the medications, compliance is an unrealistic expectation.) While it is important for the patient to attempt to identify triggers, commit to dietary and lifestyle modifications, and understand each medication, those are questions that can be answered over time. PTS: 1 DIF: Cognitive Level: Analysis REF: 650 OBJ: 9 TOP: GERD: Lifestyle Changes KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 13. The nurse is aware that patients who have chronic gastritis from renal failure may present with which first sign of this disorder? a. An increase in the white blood cell count b. Sudden massive hemorrhage c. Asthma-like symptoms d. Extreme dyspnea ANS: B Sudden massive GI hemorrhage may be the first indication of chronic gastritis. Many of these patients do not have any symptoms at all until the hemorrhage. PTS: 1 DIF: Cognitive Level: Comprehension REF: 654 OBJ: 5 TOP: Chronic Gastritis: Signs KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 14. For which patient should the nurse question an order for esomeprazole (Nexium)? a. A 55-year-old female who takes digoxin b. A 52-year-old male who is noncompliant c. A 38-year-old female who has asthma d. A 56-year-old male who has epistaxsis ANS: A Esomeprazole (Nexium) interferes with the absorption of digoxin, rabeprazole, and iron salts. In addition, the Food and Drug Administration (FDA) has issued a warning that long-term use of the proton pump inhibitors esomeprazole (Nexium) or omeprazole (Prilosec) may increase the risk of heart problems. PTS: 1 DIF: Cognitive Level: Application REF: 651, Table 28-1 OBJ: 5 (theory) TOP: Gastritis: Contraindications for Esomeprazole KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 15. The nurse is caring for a patient who is being treated for extensive burns. The nurse notes the presence of coffeeground material in the Salem sump catheter. The nurse correctly recognizes which factor as the likely cause? a. Esophagitis b. Perforated gastric ulcer c. Gastric irritation from the Salem sump tube d. A physiologic stress ulcer ANS: D Prolonged physiologic stress produces what is known as a physiologic stress ulcer, which is believed to be the result of unrelieved stimulation of the vagus nerves and decreased perfusion to the stomach. A stress ulcer is pathologically and clinically different from a chronic peptic ulcer. It is more acute and more likely to produce hemorrhage. Perforation occurs occasionally, and pain is rare. Stress ulcers are a hazard for patients who are severely ill and in intensive care units for prolonged periods. Patients with multiple trauma, burns, or multisystem disorders are subject to physiologic stress ulcers, which may produce blood that has been in contact with gastric juices. PTS: 1 DIF: Cognitive Level: Application REF: 655 OBJ: 7 TOP: Physiologic Stress Ulcer: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 16. The nurse is caring for a patient with a peptic ulcer. The patient also has a history of chronic bronchitis, diabetes, and arthritis. Which component of the patient’s history is the most likely contributing factor to the patient’s ulcer? a. The patient requires insulin to manage his diabetes. b. The patient uses a daily inhaler to decrease incidence of asthma attacks. c. The patient takes ibuprofen daily for arthritis pain. d. The patient takes a multivitamin daily. ANS: C About 4.5 million people in the United States have experienced a peptic ulcer. H. pylori infection is the major cause. Smoking and the continued use of nonsteroidal anti-inflammatory drugs (NSAIDs) are other causes. PTS: 1 DIF: Cognitive Level: Application REF: 654 OBJ: 6 TOP: NSAIDs: Etiology of Peptic Ulcer KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 17. The nurse documenting the presence of pain in a patient with possible gastric ulcer would anticipate that the pain would occur at which time? a. In the morning b. Erratically, without pattern c. At bedtime d. With meals ANS: C Pain occurs at bedtime because the stomach is empty, but the gastric juices are still high. Pain is absent in the morning when the digestive juices are low and when the stomach is filled with food. PTS: 1 DIF: Cognitive Level: Comprehension REF: 655 OBJ: 6 TOP: Gastric Ulcer: Pain Cycle KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 18. The nurse is caring for a patient with a Salem sump tube for decompression. The patient displays dyspnea and reports feeling full and nauseated. What action should the nurse take first? a. Increase suction from low to high. b. Notify the charge nurse. c. Irrigate the tube with normal saline. d. Withdraw the tube about three inches. ANS: C Irrigation of the tube to restore patency is the first intervention when assessment indicates inadequate decompression. The suction should remain on low. Withdrawing the tube may cause inappropriate placement. Notifying the charge nurse is not necessary at this time. Irrigating an obstructed sump tube is a standard of care. PTS: 1 DIF: Cognitive Level: Analysis REF: 662 OBJ: 3 (clinical) TOP: Salem Sump Tube: Obstruction KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 19. The nurse is caring for a patient who is being treated for a gunshot wound to the abdomen. The patient is receiving total parenteral nutrition (TPN), and the physician has prescribed insulin coverage on a sliding scale. The patient reports he has never had diabetes before. What response is best for the nurse to make? a. “It is likely you have developed diabetes as a result of your illness.” b. “Do you have a family history for diabetes?” c. “The TPN you are receiving has high amounts of glucose.” d. “Insulin is needed to manage your stomach’s inability to adequately metabolize food at this time.” ANS: C People on TPN are prone to hyperglycemia from the high glucose content of the solution. PTS: 1 DIF: Cognitive Level: Application REF: 665 OBJ: 8 TOP: TPN: Hyperglycemia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 20. A patient who had gastric bypass surgery 5 weeks ago calls the office to report feelings of nausea, sweating, and diarrhea shortly after eating meals. What response by the nurse is most appropriate? a. “This is common after the type of surgery you had.” b. “How much, if any, alcohol do you consume each day?” c. “Avoid large meals, limit sweets, and drink small amounts of liquids between meals.” d. “You may be experiencing a postoperative infection.” ANS: C Some patients who have had a gastrectomy experience a complication known as the “dumping syndrome.” The patient has nausea, weakness, abdominal pain, and diarrhea and may feel faint and perspire profusely or experience palpitations after eating. These sensations are caused by the rapid passage of large amounts of food and liquid into the jejunum. When a patient experiences dumping syndrome, instruction is given to avoid eating large meals and to drink a minimum of fluids during the meal. Fluids may be taken in small amounts later, between meals. If sweet foods seem to aggravate the condition—and they sometimes do—the patient should try to avoid them. Although this is not an uncommon manifestation after this type of surgery, informing the patient that this is common provides limited information to the patient and is not the best response. This problem is not connected to alcohol consumption and is not a symptom of a postoperative infection. PTS: 1 DIF: Cognitive Level: Analysis REF: 647 OBJ: 2 (clinical) TOP: Gastric Bypass: Complications KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 21. The nurse is caring for a patient who is suspected of having oral cancer. When reviewing the patient’s health history, which finding provides supportive data for the diagnosis? a. Presence of leukoplakia b. History of oral herpes simplex c. History of an oral yeast infection d. Reports of a dry oral cavity ANS: A Leukoplakia, a precancerous lesion, may occur on the tongue or mucosa. PTS: 1 DIF: Cognitive Level: Comprehension REF: 648 OBJ: 2 TOP: Oral Cancer: Risk Factors KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation MULTIPLE RESPONSE 22. The nurse correctly recognizes that esophageal cancer is associated with which risk factor(s)? (select all that apply.) a. Cigarette smoking b. Diabetes c. Hypertension d. Heavy alcohol use e. Smokeless tobacco ANS: A, D, E Cigarette smoking is a major cause of esophageal cancer in the United States. When combined with heavy alcohol consumption, the risk for esophageal cancer greatly increases. Both substances are irritants to the mucosa of the esophagus. Smokeless tobacco is also associated with esophageal cancer. Diabetes and hypertension do not increase the risk of developing esophageal cancer. PTS: 1 DIF: Cognitive Level: Comprehension REF: 649 OBJ: 2 TOP: Cancer of the Esophagus: Etiology and Pathophysiology KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 23. The nurse instructs the patient on the weight reduction drug Orlistat (Xenical, Alli) that he may experience which side effect(s)? (select all that apply.) a. Diarrhea b. Hypoglycemia c. Abdominal cramping d. Constipation e. Nausea ANS: A, C, E Medications that suppress appetite or block fat absorption may be used on a short-term basis. Orlistat (Xenical, Alli) inhibits lipase, causing fats to remain partially undigested and unabsorbed. Gastrointestinal side effects of orlistat include diarrhea (sometimes uncontrolled), abdominal cramping, and nausea. PTS: 1 DIF: Cognitive Level: Comprehension REF: 645 OBJ: 1 (theory) TOP: Appetite Suppressants: Side Effects KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 24. The nurse explains to an obese patient that initial medically supervised weight reduction includes which components(s)? (select all that apply.) a. General health assessment b. Specialized exercise program c. Participation in a support group d. Stress reduction e. Surgery ANS: A, B, C, D Dietary control and exercise are the main treatments for obesity. A general health assessment should be conducted before a patient is placed on a weight reduction diet. A provider will usually prescribe a lower-calorie diet and exercise. The patient is taught ways to change thinking about food and weight. Those with a BMI over 40 may have surgery to achieve weight reduction if they meet established criteria. Participation in a support group and behavior modification with some sort of reward for weight loss are part of the total treatment plan. Teaching stress reduction and alternate ways of coping are essential to success. Medications that suppress appetite or block fat absorption may be used on a short-term basis. Surgery would be a last resort. PTS: 1 DIF: Cognitive Level: Comprehension REF: 645 OBJ: 1 TOP: Weight Loss Programs: Characteristics KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 25. The nurse is presenting a program about bulimia nervosa to a group of student nurses. After the program, the participants correctly identify which method(s) of treatment? (select all that apply.) a. Appetite suppressants b. Antidepressant medications c. Psychotherapy d. Behavior modification e. Increased exercise ANS: B, C, D Bulimia nervosa is a psychological disorder. The bulimic patient consumes large quantities of food and then induces vomiting to get rid of it so that weight is not gained. Laxatives may be taken to purge the system after an eating binge. Treatment of bulimia includes psychotherapy, antidepressant medication, and behavior modification. Appetite suppressants and exercise are not part of treatment for bulimia nervosa. PTS: 1 DIF: Cognitive Level: Comprehension REF: 644 OBJ: 1 TOP: Bulimia Nervosa: Characteristics KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 26. To best assist a patient with dysphagia, the nurse should implement which action(s)? (select all that apply.) a. Encourage “practice swallowing” before the meal. b. Coach the patient to chew thoroughly. c. Assist the patient to sit upright with the head forward and chin tucked. d. Offer fluid during the meal. e. Give the patient thin liquids, such as water. ANS: A, B, C, D To assist a patient with dysphagia (trouble swallowing), the nurse should encourage practice swallows and visualize the larynx rising. Coaching the patient to chew thoroughly while sitting upright, and offering appropriate liquids are actions that decrease likelihood of aspiration. The nurse should administer thickened liquids. PTS: 1 DIF: Cognitive Level: Application REF: 648 OBJ: 6 TOP: Dysphagia: Techniques to Assist KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 27. The nurse is caring for a 70-year-old patient who was diagnosed with gastroenteritis after returning from a camping trip to Mexico. Which manifestation(s) is/are consistent with this diagnosis? (select all that apply.) a. Positive stool culture for Giardia or Shigella b. Abdominal cramping c. Fat in the stool d. Mucus in stool e. Blood in stool ANS: A, B, D, E Manifestations associated with gastroenteritis include a positive stool culture for Giardia or Shigella, abdominal cramping, and presence of mucus or blood in the stool. Fat in the stool is not symptomatic of gastroenteritis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 653 OBJ: 5 TOP: Gastroenteritis: Signs and Symptoms KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation COMPLETION 28. The nurse cautions that increased morbidity from hypertension and cardiac disease, even in children, is related to the modifiable risk factor of __________. ANS: obesity Obesity contributes to the morbidity of hypertension and cardiac disease. There are 300,000 deaths a year attributed to hypertension and cardiac diseases in the obese. PTS: 1 DIF: Cognitive Level: Comprehension REF: 644 OBJ: 1 TOP: Obesity: Morbidity KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 29. The nurse demonstrates that the person whose recommended weight is 150 pounds based on height, age, and body type would be considered obese if the person weighed a minimum of ______ pounds. ANS: 180 A person is considered obese if his or her weight exceeds 20% of the recommended weight for his or her height, age, and body type. (Recommended weight of 150 pounds × .20 is 30 pounds; 150 pounds + 30 pounds = 180 pounds.) PTS: 1 DIF: Cognitive Level: Application REF: 645 OBJ: 1 TOP: Obesity: Calculation KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance Chapter 29: Care of Patients with Disorders of the Lower Gastrointestinal System deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. Which type of hernia can lead to necrosis? a. Strangulated hernia b. Indirect hernia c. Direct hernia d. Irreducible hernia ANS: A The incarcerated hernia may become strangulated, which cuts off the blood supply and can lead to necrosis of the trapped bowel loop. Hernias are classified as reducible, which means the protruding organ can be returned to its proper place by pressing on the organ, and irreducible, which means that the protruding part of the organ is tightly wedged outside the cavity and cannot be pushed back through the opening. Another name for an irreducible hernia is incarcerated hernia. An indirect hernia protrudes through the inguinal ring. A direct hernia protrudes through the posterior inguinal wall. PTS: 1 DIF: Cognitive Level: Knowledge REF: 676 OBJ: 1 (theory) TOP: Incarcerated Hernia: Complications KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. The nurse is caring for patient with a history of a chronic incarcerated hernia. The patient suddenly complains of abdominal pain and vomits dark material with a fecal odor. The nurse recognizes these signs as indications of which complication? a. Complete intestinal obstruction b. Rupture c. Gastroenteritis d. Duodenal ulcer ANS: A The symptoms of intestinal obstruction vary according to the location of the obstruction. Fecal odor or material in the emesis suggests a complete intestinal obstruction. In this case, the incarcerated hernia has blocked the flow of bowel content. If there is a defect in the muscular wall of the abdomen, the intestine may break through the defect; his protrusion is called a hernia or a rupture. Gastroenteritis is inflammation of the stomach and intestines. A duodenal ulcer occurs in the small intestine (the duodenum). PTS: 1 DIF: Cognitive Level: Comprehension REF: 671 OBJ: 1 (theory) TOP: Incarcerated Hernia: Obstructions KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 3. The nurse explains that a hernioplasty is a surgery that involves which process? a. Reducing the hernia by manual pressure. b. Sewing synthetic mesh over the abdominal wall defect to reduce the hernia. c. Applying an individualized truss for the reduction of the hernia. d. Reducing the hernia and suturing the defect in the abdominal wall. ANS: B Hernioplasty is a surgical intervention in which the hernia is reduced and a synthetic mesh is sewn over the defect in the wall to prevent reoccurrence. PTS: 1 DIF: Cognitive Level: Comprehension REF: 676 OBJ: 1 (theory) TOP: Hernia Repair: Hernioplasty KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 4. The nurse is caring for a patient whose home medications include bismuth subsalicylate (Pepto Bismol). The nurse should educate the patient about which side effect of this medication? a. Pink urine b. Sunburn-like rash c. Stained teeth d. Black stools ANS: D This medication often turns the stool black. It does not cause a rash, or stain the urine or teeth. PTS: 1 DIF: Cognitive Level: Comprehension REF: 667, Table 29-1 OBJ: 2 (theory) TOP: Bismuth Subsalicylate: Side Effects KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 5. Which age-related change predisposes older adult patients to diverticula? a. Loss of bowel tone reduces motility. b. Chronic constipation increases intra-abdominal pressure and allows herniation. c. The diet may be deficient in bulk. d. Multipharmacy has altered bowel mucosa. ANS: B Most diverticula are asymptomatic, uncommon in people under age 50, and almost universal in those over 90. Increases in intraabdominal pressure from constipation and straining to defecate causes herniation of the mucosa through the bowel wall, causing a small pocket in the colon. PTS: 1 DIF: Cognitive Level: Comprehension REF: 670-671 OBJ: 3 (theory) TOP: Diverticula: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 6. The nurse is educating a patient with diverticulitis. Which statement indicates that the nurse’s teaching about the importance of seeking treatment has been successful? a. “If left untreated, the inflamed bowel could spread to the entire bowel.” b. “If left untreated, the inflamed bowel could cause ulcers.” c. “If left untreated, the inflamed bowel can perforate and cause peritonitis.” d. “If left untreated, the inflamed bowel can cause appendicitis.” ANS: C The term diverticulum refers to a small, blind pouch resulting from a protrusion of the mucous membranes of a hollow organ through weakened areas of the organ’s muscular wall. Diverticula occur most often in the intestinal tract, especially in the esophagus and colon. The infected diverticula can perforate through the bowel wall and cause peritonitis. Diverticulitis does not result in ulcers or appendicitis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 670 OBJ: 3 (theory) TOP: Diverticulitis: Complication KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 7. The nurse is teaching a group of patients about the process of a mechanical bowel obstruction. Which example should the nurse include in the teaching? a. A tumor obstructs the lumen of the bowel. b. A paralytic ileus causes cessation of peristalsis. c. The bowel is inflamed by diverticulitis. d. The bowel motility is slowed by antidiarrheal drugs. ANS: A Mechanical obstruction results in blockage of the lumen of the bowel. Examples include tumors, adhesions, strangulated hernia, twisting of the bowel (volvulus), telescoping of one part of the bowel into itself (intussusception), gallstones, barium impaction, and intestinal parasites. PTS: 1 DIF: Cognitive Level: Comprehension REF: 691 OBJ: 4 (theory) TOP: Bowel Obstruction: Mechanical KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 8. The nurse is aware that an unresolved intestinal obstruction can lead to which complications? a. Systemic infection and fever b. Intestinal rupture and shock c. Adhesions and pain d. Bloating and expelling gas ANS: B An unresolved intestinal obstruction can lead to rupture of the intestine, peritonitis, shock, and death. PTS: 1 DIF: Cognitive Level: Comprehension REF: 672 OBJ: 4 (theory) TOP: Bowel Obstruction: Complications KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 9. The nurse is aware that the person with ulcerative colitis is a risk factor for developing which disorder? a. Colon cancer b. Chronic urinary infections c. Intussusception d. Volvulus ANS: A Ulcerative colitis is an inflammation, with the formation of ulcers, of the mucosa of the colon. It is often a chronic disease, and the patient is usually free from symptoms between acute flare-ups. The person with ulcerative colitis is 10 to 15 times more likely to develop colon cancer than those who do not have the disease. PTS: 1 DIF: Cognitive Level: Knowledge REF: 681 OBJ: 5 (theory) TOP: Ulcerative Colitis: Risks KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 10. The nurse is educating a patient with inflammatory bowel disease (IBD) about recommended nutritional choices. Which statement indicates that the nurse’s teaching has been successful? a. “I should try to eat foods like white rice and lean poultry.” b. “I should avoid red meats and eat large amounts of whole grains.” c. “I should eat food that is mushy in consistency.” d. “I should increase my intake of green leafy vegetables.” ANS: A A low-fat, low-fiber, high-protein, high-calorie diet is recommended for the patient with IBD to make up for the loss of fluid and nutrients in the frequent stools. Low-fat, low-fiber, high-protein, high-calorie foods include foods like white grains or starches and lean, tender meats. Whole grains are extremely high in fiber and should be avoided. A soft diet is not indicated. Green leafy vegetables are a rich source not only of vitamin K, but also of fiber. PTS: 1 DIF: Cognitive Level: Application REF: 678 OBJ: 6 (theory) TOP: IBD: Diet KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 11. The nurse caring for a patient admitted with peritonitis who has developed a paralytic ileus. While auscultating bowel sounds, the nurse assesses flatus. What is the significance of this finding? a. Gas has formed in bowel contents. b. Flatus results from forceful vomiting. c. Flatus indicates returning peristalsis. d. Flatus indicates inadequate decompression. ANS: C Paralytic ileum is a common complication of peritonitis. The nurse should auscultate at least once a shift for the return of bowel sounds. If the patient passes flatus or feces rectally, it indicates return of peristalsis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 680 OBJ: 7 (theory) TOP: Peritonitis: Complication KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 12. The nurse explains to the patient receiving bevacizumab (Avastin) for a tumor in the colon that the drug slows cancer cell growth by which process? a. Changing the pH of the cell environment b. Reducing blood flow to the tumor c. Overhydrating cells of the tumor, causing them to burst d. Interfering with DNA of tumor cells ANS: B Bevacizumab (Avastin) is an antiangiogenesis medication that reduces blood flow to the growing tumor cells, depriving them of nutrients needed for replication. PTS: 1 DIF: Cognitive Level: Comprehension REF: 682 OBJ: 1 (clinical) TOP: Cancer: Treatment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 13. The nurse caring for the patient who is immediately postoperative with a new ileostomy. Which intervention is most important for the nurse to implement at this time? a. Change the ostomy pouch frequently. b. Provide emotional support. c. Administer a stool softener. d. Offer the patient frequent snacks. ANS: B Helping the patient adjust to the new ostomy is one of the highest priorities in the immediate postoperative period. In the immediate postoperative period, the pouch should not be changed any more than is necessary to avoid trauma to the skin. A stool softener is not indicated since stools are usually softer and more watery when coming from a stoma. Diet advancement is a gradual process that must coordinate with returning bowel function, and the patient may be NPO for a short time while bowl motility returns. PTS: 1 DIF: Cognitive Level: Application REF: 685 OBJ: 8 (clinical) TOP: Ileostomy: Post-Operative KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 14. The nurse explains which advantage benefits patients with a Kock pouch ileostomy? a. The patient can expel feces from the rectum in the normal fashion. b. The patient does not have to wear a collection device. c. The patient only has to evacuate the pouch once a day. d. The patient can have the pouch reanastomosed to the colon at a later time. ANS: B The major advantage of the Kock pouch is that the patient does not have to wear a collection device. The feces are collected in the pouch and emptied by the patient inserting a catheter into the pouch every 3 or 4 hours. PTS: 1 DIF: Cognitive Level: Comprehension REF: 678 OBJ: 15 TOP: Ileostomy: Kock Pouch KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 15. The nurse is caring for a patient 1-day postoperative after a transverse colostomy. When assessing the stoma, which finding requires the nurse’s immediate action? a. A wet, glistening stoma b. A stoma with scant marginal bleeding c. An edematous stoma d. A purplish-red stoma ANS: D The purple hue in the new stoma is an indication of reduced perfusion to the stoma and should be reported immediately. A new stoma should have a pink or beefy red color, be slightly edematous, and have some small bleeding around the stoma. PTS: 1 DIF: Cognitive Level: Application REF: 685 OBJ: 15 TOP: Stoma: Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 16. The nurse is caring for a patient with a 4-day-old ileostomy. The patient complains of cramping, the nurse notes a drop in the effluent for the ileostomy, and the bowel sounds are rapid with a “tinkling” sound. What action should the nurse take? a. Ambulate the patient to help expel gas. b. Irrigate the ileostomy with 500 mL of warm water. c. Notify the charge nurse immediately. d. Turn the patient on the left side to help drain the ileostomy. ANS: C Cramping and reduced effluent from a new ileostomy should be reported immediately as these are signs of obstruction, which could lead to perforation. Ileostomies are not irrigated except by the physician or an enterostomal therapist. PTS: 1 DIF: Cognitive Level: Application REF: 686 OBJ: 15 (theory) TOP: Ileostomy: Obstruction KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 17. A 36-year-old woman who had an ascending colostomy angrily declares, “I don’t want this hateful thing on my body! This nasty thing is not me.” Which response is most appropriate for the nurse to make? a. “The colostomy is part of you now.” b. “Let me change the collection bag so you don’t stay nasty.” c. “All ostomates feel this way at first. I’ll go get a list of support groups you may want to join.” d. “What about this colostomy concerns you the most?” ANS: D Asking the patient to name the specific concerns helps to conceptualize where the adjustment problem lies. All other options negate the patient’s feelings, reinforce the patient’s negative feelings, and do not offer any therapeutic response. PTS: 1 DIF: Cognitive Level: Application REF: 685 OBJ: 8 TOP: Altered Body Image: Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 18. The nurse is caring for an older adult patient diagnosed with diverticulitis. Which medication is the best choice to manage the patient’s pain? a. Meperidine (Demerol) b. Morphine c. Nalbuphine hydrochloride (Nubain) d. Naloxone (Narcan) ANS: B Morphine is acceptable for pain management and has fewer side effects than meperidine (Demerol). In earlier recommendations, Demerol was the drug of choice based on a theoretical risk not shown in studies. A metabolite of meperidine (Demerol) is toxic, and the older adult has difficulty metabolizing and eliminating it. The buildup of the toxin in the blood can cause seizures and other mental status changes such as acute confusion. Ask for an alternate analgesic for these patients. PTS: 1 DIF: Cognitive Level: Application REF: 670 OBJ: 2 TOP: Diverticulitis: Treatment and Nursing Management KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 19. The nurse is educating a group of patients about high-fiber dietary selections. Which patient menu selection indicates that the nurse’s teaching has been successful? a. Turkey sandwich on whole wheat toast, pears, and tea b. Grilled chicken, corn, and water c. Cheese pizza, salad, and milk d. Bacon, lettuce, and tomato sandwich on sourdough, blackberry compote, and orange juice ANS: A A high-fiber diet is encouraged for the patient with diverticular disease. Eating whole-grain cereals and breads, as well as fruits such as apples, seedless berries, peaches, and pears adds fiber. High-fiber vegetables—squash, broccoli, cabbage, and spinach— and legumes, including dried beans, peas, and lentils, provide bulk that decreases constipation and speeds the transit time in the intestine. The meal with a turkey sandwich on whole wheat bread and pears is the only meal choice with multiple high-fiber foods (bread and pears). PTS: 1 DIF: Cognitive Level: Application REF: 671, Nutritional ConsiderationsOBJ: 4 (clinical) TOP: Diverticulitis: Nutrition Considerations KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 20. The nurse is caring for a patient who has been diagnosed with Crohn disease. When providing education concerning dietary recommendations, which statement indicates that the nurse’s teaching has been successful? a. “I should try to eat as much fiber daily as I can.” b. “Reducing dietary fat and fiber will be helpful in managing my condition.” c. “I should not have lactose-containing products.” d. “Eating a larger breakfast and smaller lunch and dinner portions is recommended.” ANS: B The recommended diet in Crohn disease consists of low-fat, low-fiber foods that are high in protein and calories. Small frequent feedings are best. Lactose avoidance helps some patients. PTS: 1 DIF: Cognitive Level: Application REF: 678 OBJ: 5 TOP: Crohn Disease: Treatment KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort MULTIPLE RESPONSE 21. Which contributing factor(s) may lead to hernia development? (select all that apply.) a. Heavy lifting b. Chronic cough c. Straining with defecation d. Ascites e. Strenuous sexual activity ANS: A, B, C, D The most common contributing factors in the development of a hernia are straining to lift heavy objects, chronic cough, straining to void or pass stool, and ascites. Sexual activity is not usually a cause for herniation. PTS: 1 DIF: Cognitive Level: Comprehension REF: 675 OBJ: 3 TOP: Hernia: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 22. Which foods or beverages may trigger an attack of irritable bowel syndromes (IBS)? (select all that apply.) a. Coffee b. Yogurt c. Whole wheat bread d. White rice e. Orange juice ANS: A, B, C Stress, caffeine, and sensitivity to certain foods such as dairy and wheat products seem to trigger IBS in some people. White rice and orange juice are not considered to be triggers for IBS. PTS: 1 DIF: Cognitive Level: Application REF: 666 OBJ: 1 TOP: IBS: Triggers KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 23. The presence of which diagnostic criteria are used to confirm the diagnosis of irritable bowel syndrome (IBS)? (select all that apply.) a. Abdominal pain that increases with defecation b. Abdominal pain with a change in stool consistency c. Mucorrhea d. Clay colored stools that float e. Bloating ANS: B, C, E Diagnosis of IBS is based on clinical manifestations and ruling out the presence of organic bowel disease. Diagnostic criteria include abdominal pain with a change in stool consistency, mucus in the stool (mucorrhea), and abdominal bloating. IBS pain is relieved with defecation; clay colored stools are associated with problems with the gallbladder. PTS: 1 DIF: Cognitive Level: Comprehension REF: 667 OBJ: 1 TOP: IBS: Diagnostic Criteria KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 24. Conservative treatment of diverticulosis includes which management? (select all that apply.) a. Eating a low-fiber diet b. Increasing fluid intake c. Taking stool softeners d. Taking nonsteroidal anti-inflammatory drugs (NSAIDs) for discomfort e. Taking bulk laxatives ANS: B, C, D, E A high-fiber diet is indicated for the treatment of diverticulosis. All other options would be part of a conservative, nonsurgical approach to treatment. PTS: 1 DIF: Cognitive Level: Comprehension REF: 670 OBJ: 2 TOP: Diverticulosis: Treatment KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 25. The nurse preparing a teaching plan for a 20-year-old woman who is taking sulfasalazine (Azulfidine) for Crohn disease. Which information should the nurse include in the teaching plan? (select all that apply.) a. Avoid tanning beds or going outside during peak hours of sun while taking sulfasalazine (Azulfidine). b. If taking sulfasalazine (Azulfidine) while on oral contraceptives, use a backup method of birth control. c. Sulfasalazine (Azulfidine) decreases the effect of hypoglycemic agents. d. Be aware that sulfasalazine (Azulfidine) may turn the urine orange. e. Be aware that sulfasalazine (Azulfidine) may cause gastrointestinal (GI) upset. ANS: A, B, D, E Sulfasalazine (Azulfidine) causes increased photosensitivity, may interfere with effectiveness of oral contraceptives, can tint the urine orange, and may cause GI upset. Sulfasalazine (Azulfidine) increases the effect of hypoglycemic agents. PTS: 1 DIF: Cognitive Level: Application REF: 668, Table 29-1 OBJ: 5 (theory) TOP: Crohn Disease: Treatment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 26. The nursing is planning care for a patient with an acute exacerbation of inflammatory bowel disease (IBD). Which action(s) is/are most important for the nurse to include in the care plan? (select all that apply.) a. Assess number and character of stools. b. Auscultate bowel sounds. c. Obtain weights each shift. d. Encouraging periods of rest. e. Assess for internal bleeding. ANS: A, B, D, E For an acute attack of IBD, care includes monitoring the number and character of stools, periodic auscultation of bowel sounds, and checking for signs of internal bleeding, electrolyte imbalances, or anemia. The nurse should carefully monitor intake and output, but daily weights are sufficient. PTS: 1 DIF: Cognitive Level: Comprehension REF: 679 OBJ: 10 TOP: Nursing Care for IBD KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 27. The nurse is teaching a patient about peristomal skin care. Which information is most important for the nurse to include? (select all that apply.) a. Gently remove the faceplate of the appliance to avoid skin irritation. b. Washing the peristomal area with a scrubbing motion to rid the skin of fecal waste. c. Thoroughly rinse the skin. d. Apply a skin barrier to the peristomal area. e. Cut the faceplate to allow a -inch opening around the stoma. ANS: A, C, D The faceplate should be removed gently to avoid skin damage; rinsing and drying, and application of a skin barrier, is essential. Washing should be gentle; the patient should avoid scrubbing that could irritate the skin. The faceplate should allow a 1/8-inch opening around the stoma. PTS: 1 DIF: Cognitive Level: Application REF: 687 OBJ: 16 TOP: Peristomal Skin Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance COMPLETION 28. The mechanical bowel obstruction caused when the bowel twists on itself is known as _________. ANS: volvulus Volvulus, the bowel twisting on itself, causes a mechanical bowel obstruction that must be reduced immediately to prevent necrosis to the bowel from ischemia. PTS: 1 DIF: Cognitive Level: Knowledge REF: 671 OBJ: 4 TOP: Bowel Obstruction: Volvulus KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance MATCHING Match the types of ostomies with the expected type of effluent. a. Ascending colostomy b. Transverse colostomy c. Descending colostomy d. Ileostomy e. Continent ileostomy 29. Formed stool on relatively regular basis 30. Semiliquid stool at unpredictable times 31. Liquid and unformed stool 32. Extremely watery stool with concentrations of digestive enzymes 33. No effluent 29. ANS: C PTS: 1 DIF: Cognitive Level: Application REF: 682-684 OBJ: 15 TOP: Ostomies: Effluents KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 30. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 682-684 OBJ: 15 TOP: Ostomies: Effluents KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 31. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 682-684 OBJ: 15 TOP: Ostomies: Effluents KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 32. ANS: D PTS: 1 DIF: Cognitive Level: Analysis REF: 682-684 OBJ: 15 TOP: Ostomies: Effluents KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 33. ANS: E PTS: 1 DIF: Cognitive Level: Analysis REF: 682-684 OBJ: 15 TOP: Ostomies: Effluents KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance Chapter 30: Care of Patients with Disorders of the Liver, Gallbladder, and Pancreas deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is providing discharge teaching for a patient who underwent a laparoscopic cholecystectomy. Which statement indicates that the nurse’s teaching has been successful? a. “I should call my doctor if I have any pain.” b. “I should be able to go back to work tomorrow.” c. “I should avoid fatty foods for a few weeks.” d. “I should let these Steri-Strips fall off on their own.” ANS: D The nurse should teach the patient to remove the bandages from the puncture site(s) the day after surgery and shower, leaving the Steri-Strips intact. Steri-Strips will fall off in 7 to10 days. The patient should notify the physician in cases of severe abdominal pain that is not relieved by medication or is worsening. Return to work is probable at 1 week postsurgery. The patient should adhere to a low-fat diet for several weeks and slowly introduce fattier foods to determine if they cause unpleasant symptoms. PTS: 1 DIF: Cognitive Level: Application REF: 696 OBJ: 11 TOP: Cholecystectomy: PostOp Teaching KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 2. The nurse is caring for a patient who presents to the emergency department with severe nausea and vomiting with stomach pain that radiates to his right scapula. The patient has a temperature of 101.2° F. The nurse anticipates that this patient will undergo workup for which problem? a. Cholecystitis b. Hepatitis c. Pancreatitis d. Gastroenteritis ANS: A Nausea and vomiting, fever, and leukocytosis occur with cholecystitis. Pain may be referred to the right clavicle, scapula, or shoulder. Hepatitis causes liver dysfunction, including jaundice. Pancreatitis causes abdominal pain that is usually acute, but this can vary among individuals. The pain is steady and is localized to the epigastrium or left upper quadrant. Gastroenteritis causes nausea, vomiting, and diarrhea. PTS: 1 DIF: Cognitive Level: Application REF: 696 OBJ: 2 TOP: Cholecystitis: Signs and Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 3. The nurse is caring for a patient with cholelithiasis who is scheduled to undergo a cholescintigraphy (HIDA scan). Which statement accurately describes the purpose of the HIDA scan? a. To visualize the location of gallstones b. To assess amounts of inflammation and swelling c. To diagnose abnormal contraction of the gallbladder d. To assess composition of gallstones ANS: C The HIDA scan can diagnose abnormal contractions of the gallbladder, which occur in the presence of gallstones or a gallbladder that is not functioning properly. PTS: 1 DIF: Cognitive Level: Comprehension REF: 696 OBJ: 1 (theory) TOP: Cholelithiasis: HIDA Scan KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 4. The nurse is caring for a patient diagnosed with gallstones who requires a cholecystectomy. The patient is upset and asks the nurse why he cannot have lithotripsy instead. Which response is most appropriate for the nurse to make? a. “Is there a reason that you want to have lithotripsy?” b. “Your doctor decides which procedure will be best.” c. “Gallstones are usually treated with surgery. Tell me more about your concerns.” d. “I understand that you are upset. Would you like to speak with a chaplain?” ANS: C Lithotripsy, or “shock wave” therapy, is rarely used for gallstones. The treatment of choice is gallbladder removal. By explaining that surgery is the treatment of choice but also asking the patient to elaborate, the nurse provides information and uses an openended statement to acknowledge the patient’s feelings. Asking the patient to list the reasons that he wants lithotripsy is not therapeutic or effective since the patient requires a cholecystectomy. While the physician does choose which procedure is best indicated, the nurse should not dismiss the patient’s concerns or deflect them and suggest that he speak with someone else. PTS: 1 DIF: Cognitive Level: Application REF: 696 OBJ: 2 TOP: Cholecystectomy vs. Lithotripsy KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 5. A nurse is caring for a patient who is 4 hours postoperative after a laparoscopic cholecystectomy. The patient reports abdominal fullness and mild discomfort. After verifying that the patient’s vital signs are stable, what action is most important for the nurse to take next? a. Ambulate the patient. b. Notify the charge nurse. c. Position the patient in high Fowler. d. Administer the ordered PRN analgesic. ANS: A Retained carbon dioxide (CO2) used during a laparoscopic procedure causes “free air” pain, which may manifest as abdominal fullness and mild discomfort. Early and frequent ambulation helps the CO2 gas dissipate. The charge nurse does not require notification at this time. The nurse should position the patient upright after ambulation. If ambulation does not ease the patient’s discomfort, the nurse should then administer the PRN analgesic as ordered. PTS: 1 DIF: Cognitive Level: Analysis REF: 696 OBJ: 2 TOP: Laparoscopic Surgery: “Free Air” KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 6. The nurse is caring for a patient who underwent a cholecystectomy 3 days ago. Which assessment finding best indicates to the nurse that the bile flow is no longer obstructed from entering the bowel? a. Excessive flatus b. Dark brown stool c. Dark urine d. Increased appetite ANS: B Darkening of stools back to the normal color indicates that the bile has reached the duodenum. PTS: 1 DIF: Cognitive Level: Application REF: 697 OBJ: 1 (clinical) TOP: Assessment of Bile Flow: Dark Stool KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 7. The nurse is caring for a patient with hepatitis. The nurse explains that jaundice occurs in conjunction with hepatitis based on which underlying pathophysiology? a. Liver ischemia in hepatitis causes jaundice. b. Increased bile production by the enlarged Kupffer cells causes jaundice. c. The hepatitis virus destroys red blood cells and causes jaundice. d. Hepatitis causes liver congestion that obstructs bile flow. ANS: D Congestion from the inflammation obstructs the bile from entering the duodenum and keeps it in the circulating volume. PTS: 1 DIF: Cognitive Level: Comprehension REF: 697 OBJ: 4 TOP: Hepatitis: Jaundice KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 8. The nurse is caring for a patient admitted with suspected acute viral hepatitis. Which laboratory value would best support this diagnosis? a. Decreased aspartate aminotransferase (AST) b. Decreased alanine aminotransferase (ALT) c. Decreased gamma-glutamyl transpeptidase (GGT) d. Increased prothrombin time ANS: D During the acute phase of hepatitis, the patient will likely display prolonged prothrombin times. Levels of aspartate aminotransferase (AST), alanine aminotransferase and GGT will be elevated. PTS: 1 DIF: Cognitive Level: Comprehension REF: 700, Table 30-3 OBJ: 4 TOP: Hepatitis B: Diagnostic Tests KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 9. A 20-year-old college student who has not been immunized against hepatitis B virus (HBV) comes to the clinic and reports that he has been exposed to hepatitis B. The nurse anticipates that the health care provider will likely recommend which treatment? a. A prescription for a broad-spectrum antibiotic b. A prescription for an antiviral agent c. The first of the three immunizations for HBV d. An injection of hepatitis B immune globulin (HBIG) ANS: D HBIG will give immediate passive immunity. Immunization for HBV takes too long for immediate coverage. Oral medications are of little value at this stage. PTS: 1 DIF: Cognitive Level: Application REF: 702 OBJ: 3 TOP: HBV: Immune Globulin KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 10. In caring for a patient with hepatitis B, a nurse would employ which precautions? a. Standard Precautions b. Strict isolation c. Contact Precautions d. Surgical asepsis ANS: A Standard Precautions are needed to care for a patient with hepatitis B. Isolation and contact precautions are not indicated for this diagnosis unless this patient is experiencing active bleeding. Surgical asepsis is not required. PTS: 1 DIF: Cognitive Level: Comprehension REF: 702, Health Promotion OBJ: 3 TOP: HBV: Standard Precautions KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 11. The nurse is aware that a definitive diagnosis of cirrhosis is made based on the results of which diagnostic or laboratory test? a. Liver biopsy b. Elevated aspartate aminotransferase (AST) c. Elevated alanine aminotransferase (ALT) d. Elevated lactate dehydrogenase (LDH) ANS: A Liver biopsy is the definitive test. AST, ALT, and LDH tests will be elevated, but they are not specific for cirrhosis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 706 OBJ: 5 (theory) TOP: Cirrhosis: Diagnosis KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 12. The nurse is caring for a patient with cirrhosis. Which assessment finding warrants the nurse’s immediate attention? a. Shiny, tight abdomen b. Yellow sclera c. Confusion d. Paired horizontal bands on the fingernails ANS: C Mental confusion and coma result from hepatic encephalopathy. Encephalopathy occurs from liver failure that leads to circulating toxins. This finding is an indicator of deteriorating patient condition. Ascites and jaundice are expected findings in cirrhosis and do not necessarily indicate an urgent change in condition. Fingernails that feature horizontal bands in pairs that alternate with normal nail color occur due to hypoalbuminemia from cirrhosis; this finding does not indicate an urgent change in condition. PTS: 1 DIF: Cognitive Level: Analysis REF: 702 OBJ: 5 TOP: Cirrhosis: Signs of Deterioration KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 13. The nurse is caring for a patient with cirrhosis. The nurse is educating the patient about nutritional implications related to his diagnosis. Which statement indicates that the nurse’s teaching has been successful? a. “I should eat lots of sweet potatoes and carrots for vitamin A.” b. “I should choose proteins like cottage cheese and quinoa instead of chicken.” c. “I should eat oysters and shellfish for a good source of copper.” d. “I should eat red meat and dark, leafy vegetables to boost my iron stores.” ANS: B Traditionally, limitation of dietary protein intake was prescribed; however, this approach is being challenged and the current recommendation is to manage encephalopathy with medications rather than to restrict protein. Vegetable proteins are preferred because they do not contribute to encephalopathy. Substituting meat proteins for protein sources like quinoa and cottage cheese is a good dietary choice. Patients with liver inflammation or cirrhosis should avoid taking large doses of vitamins and minerals. Vitamin A, iron, and copper can worsen the liver damage, so this patient should not try to increase intake of these vitamins and minerals. PTS: 1 DIF: Cognitive Level: Application REF: 707 OBJ: 5 TOP: Cirrhosis: Nutritional Implications KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 14. The physician has prescribed rifaximin (Xifaxan) for a patient with cirrhosis. The patient questions why he must take this medication. Which response by the nurse is most appropriate? a. Rifaximin (Xifaxan) helps prevent infection. b. Rifaximin (Xifaxan) helps reduce straining during a bowel movement. c. Rifaximin (Xifaxan) kills intestinal flora. d. Rifaximin (Xifaxan) aids in reducing ascites. ANS: C Rifaximin (Xifaxan) decrease the bowel flora, colonic bacteria that breakdown protein. This treatment lowers the formation of ammonia. This medication may cause headaches or flatulence and is taken twice daily with food. PTS: 1 DIF: Cognitive Level: Application REF: 701, Table 30-4 OBJ: 5 (theory) TOP: Cirrhosis: Rifaximin (Xifaxan) KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 15. The nurse is caring for a patient with esophageal varices with a new order for vasopressin (Pitressin). The nurse reviews the patient’s history and notes that the patient’s comorbidities include coronary artery disease (CAD), type 2 diabetes, gastroesophageal reflux disease (GERD), and fibromyalgia. The nurse should immediately notify the physician about which component of the patient’s history? a. CAD b. Diabetes mellitus (DM) type 2 c. GERD d. Fibromyalgia. ANS: A Vasopressin (Pitressin) is a potent medication that causes vasoconstriction and stops bleeding of esophageal varices. With the use of potent vasoconstrictors such as vasopressin (Pitressin), which constricts all vessels, the possibility of it causing a myocardial infarction (MI) is a very real concern and should be used most cautiously with the patient with CAD. PTS: 1 DIF: Cognitive Level: Analysis REF: 701, Table 30-4, 711 OBJ: 5 (theory) TOP: Vasoconstrictors: Possible MI KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 16. The nurse caring for a patient with acute pancreatitis assesses a bluish tinge around the patient’s umbilicus. The nurse recognizes that this finding likely results from which underlying problem? a. Increased amylase b. Retroperitoneal hemorrhage. c. Inflammatory response to a pseudocyst d. Ascites ANS: B A bluish tinge around the umbilicus or in the flank area indicates a retroperitoneal hemorrhage. Increased amylase levels, inflammatory response to a pseudocyst, and ascites do not result in a bluish tinge around the belly button. PTS: 1 DIF: Cognitive Level: Comprehension REF: 713 OBJ: 10 (theory) TOP: Pancreatitis: Retroperitoneal Hemorrhage KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 17. The nurse is caring for a patient diagnosed with acute pancreatitis who complains of significant pain. Which nursing action holds the highest priority for this patient? a. Instruct the patient to sit and lean forward. b. Monitor intake and output. c. Monitor laboratory values and note changes. d. Check blood glucose values frequently. ANS: A Pancreatitis causes abdominal pain that is usually acute, steady, and localized to the epigastrium or left upper quadrant. As it progresses, it spreads and radiates to the back and flank. Sitting and leaning forward may ease the pain. The severity of the pain may slowly decrease after 24 hours. Eating makes the pain worse. While monitoring intake and output and laboratory values are important actions, none of these actions actively address the patient’s pain. PTS: 1 DIF: Cognitive Level: Analysis REF: 713-714 OBJ: 10 TOP: Hepatitis: Signs and Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 18. The nurse is caring for a patient being treated for new onset of gallstones. The patient asks the nurse if he will have to have surgery. How should the nurse respond? a. “You will have to have surgery if you continue to have gallstones.” b. “Tell me more about your concern.” c. “Treatment for gallstones may include diet modification and weight loss, medications, or surgery.” d. “You need to ask the doctor about your concerns.” ANS: C The patient should be aware that treatment varies according to severity and frequency of symptoms in conjunction with the patient’s response to various treatments. Conservative therapy includes low-fat diets and weight loss, along with restriction of alcohol intake. Oral medications may be given to dissolve gallstones. If the patient does not respond to this therapy, or if bile obstruction occurs, correction of the obstructed biliary tract is indicated. Gallbladder removal is indicated with patients with ongoing symptoms or complications. The nurse should not tell the patient that surgery is inevitable. The patient has already expressed his concern (whether he will require surgery). The nurse can address the patient’s concern and should not deflect them to the physician. PTS: 1 DIF: Cognitive Level: Comprehension REF: 696 OBJ: 1 (clinical) TOP: Gallbladder: Complications KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 19. A patient has reported to the clinic with concerns about contracting hepatitis A from her boyfriend. What response by the nurse is most appropriate? a. “If you are having unprotected sexual intercourse with your partner, there is a relatively high risk for hepatitis A.” b. “Hepatitis A is not transmitted as a result of close contact with an infected individual.” c. “Hepatitis A transmission is associated with contact with infected body fluids.” d. “Hepatitis A is relatively uncommon in our country and seen more in underdeveloped countries.” ANS: B Hepatitis A and hepatitis E viruses are transmitted primarily by the fecal-oral route. They are responsible for the epidemic forms of viral hepatitis. Hepatitis A virus can be transmitted by food handlers to customers or by mollusk shellfish from contaminated waters. Hepatitis B is transmitted via infected blood and body fluids. Hepatitis E virus infection is primarily seen in less developed countries. PTS: 1 DIF: Cognitive Level: Application REF: 699 OBJ: 3 (theory) TOP: Hepatitis: Etiology and Pathophysiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation MULTIPLE RESPONSE 20. The nurse is speaking with a patient who has concerns about the development of cholelithiasis. The nurse correctly includes which risk factors for the condition? (select all that apply.) a. Obesity b. Daily exercise regimen c. Diabetes mellitus (DM) d. Taking cholesterol-lowering drugs e. Mexican American ethnicity ANS: A, C, D, E Cholelithiasis is the presence of gallstones within the gallbladder or in the biliary tract. Obesity, DM, intake of cholesterollowering drugs, and Mexican American ethnicity are risk factors for the development of gallstones. A sedentary lifestyle is a risk factor for cholelithiasis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 694 OBJ: 1 (theory) TOP: Cholelithiasis: Risk Factors KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 21. The nurse points out to a patient recently diagnosed with hepatitis B virus (HBV) that the virus is found which type(s) of body fluid(s) or secretions? (select all that apply.) a. Semen b. Vaginal secretions c. Sweat d. Breast milk e. Human feces ANS: A, B, D, E HBV, hepatitis C virus (HCV), and hepatitis D virus (HDV) may cause chronic inflammation and necrosis of the tissue. HBV and HCV are transmitted by parenteral routes and sexually as they are present in semen, vaginal secretions, and saliva of carriers, as well as breast milk and human feces. HBV is not transmitted through sweat. Sexual partners of patients who are carriers of HBV and HCV are at high risk for contracting the virus. PTS: 1 DIF: Cognitive Level: Comprehension REF: 699 OBJ: 3 (theory) TOP: HBV: Body Fluids KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 22. The nurse is discussing the impact of cirrhosis on liver function with the family of a dying patient. The nurse explains that, when the damage caused by cirrhosis blocks the blood flow through the liver, it can lead to which complication(s)? (select all that apply.) a. Portal hypertension b. Decrease in metabolic processes of the liver c. Decrease in clotting factors d. Increase in ascites e. Decrease in aldosterone ANS: A, B, C, D Cirrhosis is a progressive, chronic disease of the liver. The destruction of normal hepatic structures and their replacement with necrotic tissue occur. Fibrous bands of connective tissue develop in the organ. The bands eventually constrict and partition the liver tissue into irregular nodules. If this process is halted before too much liver tissue is damaged, the liver tissue will regenerate. Late cirrhosis is considered irreversible. The outcomes of cirrhosis of the liver are failure of its cells to perform their functions and the development of portal hypertension. Aldosterone levels are increased rather than decreased. PTS: 1 DIF: Cognitive Level: Comprehension REF: 705 OBJ: 6 (theory) TOP: Cirrhosis: Pathophysiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 23. The nurse is planning skin care of the patient with ascites. Which actions should the nurse include? (select all that apply.) a. Bathe the patient in hot water. b. Apply emollients to decrease itching. c. Closely trim the patient’s fingernails. d. Change the patient’s position every 1 to 2 hours. e. Coach the patient in deep-breathing exercises. ANS: B, C, D Applying emollients, cutting the fingernails short, and changing the patient’s position frequently are appropriate interventions. The nurse should bathe the patient in tepid water. Deep breathing, although a good intervention in certain situations, has nothing to do with skin care. PTS: 1 DIF: Cognitive Level: Application REF: 704, Table 30-5 OBJ: 5 (theory) TOP: Cirrhosis: Skin Care KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 24. A patient with advanced cirrhosis develops esophageal varices. The nurse anticipates that this complication will be addressed by which type of medication(s)? (select all that apply.) a. Vasodilators b. Intravenous (IV) vasopressin (Pitressin) c. IV iron d. Beta blockers e. Vitamin K ANS: B, D, E Treatment options include administration of parenteral vasopressors such as vasopressin (Pitressin) to lower portal pressure, a beta blocker to lower blood pressure, and vitamin K to help rectify clotting factor deficiencies. Vasoconstrictors (not vasodilators) such as somatostatin (Zecnil) and octreotide (Sandostatin) are used to reduce portal blood flow, and iron may exacerbate liver failure. PTS: 1 DIF: Cognitive Level: Application REF: 711 OBJ: 5 (theory) TOP: Esophageal Varices: Treatment KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 25. The nurse caring for a patient recently admitted with acute pancreatitis. Which action(s) should the nurse include in the daily assessments? (select all that apply.) a. Auscultate bowel sounds. b. Carefully evaluate amount of food eaten each meal. c. Measure abdominal girth. d. Monitor for effectiveness of pain control. e. Monitor urine output. ANS: A, C, D, E The nurse should auscultate bowel sounds, measure abdominal girth to monitor for ascites, monitor for pain and evaluate effectiveness of pain control, and monitor urine output. In early acute pancreatitis, the patient should be kept NPO; measuring food is unnecessary. PTS: 1 DIF: Cognitive Level: Comprehension REF: 713 OBJ: 3 (clinical) TOP: Pancreatitis: Essential Assessments KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort COMPLETION 26. The nurse explains that bile salts deposited in the skin cause jaundice and also cause _____. ANS: pruritus Bile salts deposited in the skin cause both jaundice and pruritus. PTS: 1 DIF: Cognitive Level: Comprehension REF: 705 OBJ: 4 (theory) TOP: Jaundice: Pruritus KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 27. The nurse reinforces that the immunization for HBV is believed to provide _____ immunity. ANS: lifelong lifetime The vaccine for hepatitis B produces immunity in about 95% of vaccinated individuals and is administered in three or four doses for probable lifetime immunity (Buggs, 2012). PTS: 1 DIF: Cognitive Level: Comprehension REF: 702 OBJ: 3 (theory) TOP: HBV Immunization: Effectiveness KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance MATCHING Match the hepatitis virus (HV) with the characteristics that best describe it. a. HAV b. HBV c. HCV d. HDV e. HEV 28. Transmission by contact with blood and body fluids, perinatal transmission from mother to infant 29. Prevalent in less developed countries 30. Most likely to lead to cirrhosis 31. Coexists with HBV 32. Fecal-oral transmission, acute onset 28. ANS: B PTS: 1 DIF: Cognitive Level: Application REF: 698, Table 30-2 OBJ: 3 (theory) TOP: Hepatitis Differences KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 29. ANS: E PTS: 1 DIF: Cognitive Level: Application REF: 698, Table 30-2 OBJ: 3 (theory) TOP: Hepatitis Differences KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 30. ANS: C PTS: 1 DIF: Cognitive Level: Application REF: 698, Table 30-2 OBJ: 3 (theory) TOP: Hepatitis Differences KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 31. ANS: D PTS: 1 DIF: Cognitive Level: Application REF: 698, Table 30-2 OBJ: 3 (theory) TOP: Hepatitis Differences KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 32. ANS: A PTS: 1 DIF: Cognitive Level: Application REF: 698, Table 30-2 OBJ: 3 (theory) TOP: Hepatitis Differences KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance Chapter 31: The Musculoskeletal System deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is discussing actions that can be taken to best prevent osteoporosis with a patient. Which information should the nurse include? a. Take an extra calcium supplement. b. Eat a balanced diet. c. Exercise throughout life. d. Increase daily intake of milk products. ANS: C A lifetime of even mild daily exercise will delay or prevent osteoporosis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 720 OBJ: 4 (theory) TOP: Osteoporosis: Supplement KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 2. What does goniometry measure? a. Bone strength b. Muscle density c. Muscle strength d. Range-of-motion (ROM) ANS: D Goniometry measures joint mobility, described as the number of degrees that the joint can move from the 0-degree mark. PTS: 1 DIF: Cognitive Level: Comprehension REF: 721 OBJ: 2 (clinical) TOP: Goniometry: Joint Mobility KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 3. Positioning and range-of-motion (ROM) exercises most help the immobilized patient to prevent which complication? a. Increased pain b. Contractures c. Pressure ulcers d. Compromised circulation ANS: B Although positioning may help decrease pain and increase circulation, anatomical alignment and ROM exercises are most helpful in preventing contractures in the immobilized patient. Pressure ulcers are prevented by frequent position changes. PTS: 1 DIF: Cognitive Level: Analysis REF: 728 OBJ: 2 (clinical) TOP: Contractures: Prevention KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 4. The nurse adds interventions for range-of-motion (ROM) and isometric exercises for the new patient with a stroke. The nurse’s reasoning stems from her awareness that contracture formation may begin with how many days of immobilization? a. 1 day b. 2 days c. 3 days d. 10 days ANS: C Contracture-related muscle changes occur as early as 3 days of immobilization. PTS: 1 DIF: Cognitive Level: Comprehension REF: 731 OBJ: 2 (clinical) TOP: Process of Contracture Formation: Time Frame KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 5. If muscles are not regularly stretched and contracted, how will the muscles be effected? a. Muscles will become longer and flexed. b. Muscles will become fibrosed and spastic. c. Muscles will become shorter and less elastic. d. Muscles will become shorter and painful. ANS: C The formation of contractures (shortening of skeletal muscle tissue causing deformity), loss of muscle tone, and fixation of joints can be prevented in most cases by consistent nursing intervention. The major components of the intervention are gradual mobilization, an exercise program, proper positioning, and instruction of the patient and family. Within a matter of a few days, the structures of immobilized muscles and joints begin to undergo changes. If no effort is made to prevent these changes, the patient will become permanently disabled. PTS: 1 DIF: Cognitive Level: Comprehension REF: 731 OBJ: 2 (clinical) TOP: Immobility: Effect on Muscles KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 6. The nurse uses a visual aid to show the pathologic muscle tone changes that result in footdrop. Which changes should the nurse include? a. The stretching of calf muscles b. The stretching of flexor muscles c. The toes curl downward d. The thigh muscles contract ANS: B The most frequent contractures occurring in patients immobilized for long periods are “footdrop,” knee and hip flexion contractures, “wrist drop,” and contractures of the fingers and arms. Calf muscles contract and flexor muscles are stretched, allowing the unbraced foot to drop toward the surface of the bed. PTS: 1 DIF: Cognitive Level: Comprehension REF: 731 OBJ: 2 (clinical) TOP: Contractures: Pathophysiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 7. How often should range-of-motion (ROM) exercises be performed? a. Once a day b. Once in the morning and once in the afternoon c. Three to four times a day d. Four to six times a day ANS: C ROM exercises, both passive and active, are planned and carried out as soon as feasible after immobilization occurs as a result of disease, injury, or surgery. The exercises are done to maintain functional connective tissue within the joint and thereby ensure that every joint retains its function and mobility. ROM exercises should be done three to four times a day. PTS: 1 DIF: Cognitive Level: Comprehension REF: 731 OBJ: 2 (clinical) TOP: ROM Exercises: Frequency KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 8. The physician has prescribed isometric exercises for a patient. For which patient should the nurse question this order? a. A patient experiencing an acute exacerbation of congestive heart failure b. A patient with uncontrolled diabetes c. A patient with a urinary tract infection (UTI) d. A patient with resolving epistaxis ANS: A Isometric exercises are based on the energy of opposing muscles working against each other. Isometric exercise may be contraindicated in patients with hypertension, increased intracranial pressure, or congestive heart failure, as there is a significant increase in blood pressure and heart rate during isometric exercise PTS: 1 DIF: Cognitive Level: Analysis REF: 728 OBJ: 2 (clinical) TOP: Isometric Exercises: Concept KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 9. When the patient returns to the unit from having had an arthrogram, which intervention should the nurse perform first? a. Ambulate the patient in the room. b. Apply ice packs to the knee. c. Perform passive range-of-motion (ROM) exercises. d. Wrap the knee in an elastic bandage. ANS: B Ice packs applied to the knee will reduce swelling. The patient will ambulate at some point but not before the application of ice. There is not going to be a significant loss of mobility for the patient, so ROM exercises will not likely be included in the plan of care. There is no indication that an elastic bandage is needed. PTS: 1 DIF: Cognitive Level: Application REF: 723, Table 31-3 OBJ: 4 (clinical) TOP: Arthroscopy: Aftercare KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 10. The nurse encourages the patient to use the four-point crutch gait technique. Which statement indicates that the patient accurately understands the nurse’s teaching? a. “This way of walking takes weight off of one leg.” b. “This way of walking is the most stable gait.” c. “This way of walking mimics normal walking pattern.” d. “This way of walking allows the most rapid pace.” ANS: B The four-point crutch gait is the most stable, requires that there may be partial weight bearing on both legs, and does not mimic normal walking pattern. PTS: 1 DIF: Cognitive Level: Application REF: 729 OBJ: 5 (clinical) TOP: Four-Point Crutch Gait: Characteristics KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 11. The nurse is assessing the patient’s cane for appropriate length. Which observation affirms that an appropriate cane has been selected? a. The handgrip is at hip level. b. The elbow flexes at 45 degrees when weight is placed on the cane. c. The cane tip is placed touching outside the good foot. d. The rubber tip has been removed when measuring cane length. ANS: A The handgrip should be at hip level to allow for proper flexion of the arm to bear weight. The cane tip should be placed 6 inches from the good foot. The elbow angle should be 30 degrees. PTS: 1 DIF: Cognitive Level: Application REF: 730 OBJ: 5 (clinical) TOP: Cane: Measurement KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 12. The nurse is instructing the patient on quadriceps and gluteal muscle exercises. Which instructions should the nurse include? a. In a supine position, straighten the leg and tense leg muscles while raising heel. b. Flex the leg and hold it with the hands while pulling the leg back toward the hip. c. Straighten the legs while raising the head. d. Flex both legs and perform an abdominal crunch up toward the knees. ANS: A The quad setting exercise is to straighten the leg and tense the leg muscles while raising the heel. PTS: 1 DIF: Cognitive Level: Comprehension REF: 729, Patient Teaching OBJ: 2 (clinical) TOP: Quadriceps and Gluteal Muscle Exercises KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 13. What is the name for the anatomical structure that joins the bones of a joint together? a. A ligament b. A tendon c. A muscle d. Cartilage ANS: A Ligaments hold the bones of a joint together. Tendons are connective tissues that provide joint movement. Cartilage is a type of connective tissue in which fibers and cells are embedded in a semisolid gel material. PTS: 1 DIF: Cognitive Level: Knowledge REF: 718 OBJ: 1 (theory) TOP: Ligament: Function KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 14. Which bodily component constantly renews bone? a. Osteoblasts b. Stem cells c. Free circulating calcium ions d. Combination of phosphorus and vitamin D ANS: A Osteoblasts build bone as the old bone is reabsorbed into the body. PTS: 1 DIF: Cognitive Level: Knowledge REF: 720 OBJ: 1 (theory) TOP: Bone Regeneration KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 15. The patient’s plan of care includes using the continuous passive motion (CPM) machine. Which statement indicates the patient needs for further teaching? a. “I marched in the Marines for 20 years, and now I’m marching flat on my back!” b. “My new knee will be glad to rest at night.” c. “I can make my new knee stronger if I reset this thing to go faster and flex my knee more.” d. “I almost wish this CPM ran at night. The motor noise is soothing.” ANS: C The continuous passive motion (CPM) machine is used to provide movement to a joint in recovery. The apparatus is driven by a motor and requires no effort on the part of the patient or nurse to move the limb. It is usually left on all day and is discontinued at night while the patient sleeps. CPM is preset as to speed and the degree of flexion that is determined by the physician and should not be adjusted by the patient. PTS: 1 DIF: Cognitive Level: Application REF: 729 OBJ: 3 (clinical) TOP: CPM Machine KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 16. When preparing a patient for electromyography (EMG), which instructions should the nurse include? a. Cease smoking for 12 hours before the test. b. Refrain from caffeine drinks for 3 hours before the test. c. Take muscle relaxants before the test. d. Prepare for a lengthy testing time (usually about 2 hours). ANS: B Electromyography (EMG) is used to detect abnormal nerve transmission to the muscle and abnormal muscle function, and to assess the rehabilitation progress. Before the test, smoking and use of caffeine should be ceased for 3 hours. The test usually takes 1 hour. PTS: 1 DIF: Cognitive Level: Application REF: 723, Table 31-3 OBJ: 5 (theory) TOP: EMG: Preprocedure Instructions KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 17. The nurse is caring for an older adult patient. Which age-related factor increases this patient’s risk for falls? a. Multiple lines and tubes b. Increased postural sway c. Room clutter d. Pain medication ANS: B Approximately 30% to 40% of inpatient safety incidents are related to falls, and older adults are particularly vulnerable because of changes related to aging such as decreased strength, unsteady balance, loss of endurance, slow reflexes, gait disturbances, and increased postural sway, and chronic diseases such as arthritis. Lines and tubes, room clutter, and pain medications are risk factors for falls regardless of age. PTS: 1 DIF: Cognitive Level: Comprehension REF: 725, Older Adult Care Points OBJ: 4 (theory) TOP: Older Adult: Sense of Cold KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 18. The nurse is changing the position of a person with flaccid paralysis. Which action is most important? a. Change the patient’s joint position frequently. b. Refrain from footboard usage. c. Only move the patient from side to side, not supine. d. Refrain from using pillows to keep the patient in place. ANS: A Frequent changes in joint position reduce the incidence of ankylosis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 728 OBJ: 2 (clinical) TOP: Positioning: Flaccid Paralysis KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 19. The nurse is caring for a patient who has had an arthrocentesis. The nurse has completed discharge instructions. Which statement indicates the patient needs further instruction? a. “I should avoid moving my knee for at least 2 weeks.” b. “The steroids prescribed by my physician will reduce the inflammation in my knee.” c. “Some pain is anticipated.” d. “My elastic bandage will be worn for 2 to 3 days.” ANS: A The patient with the arthrocentesis will be instructed to avoid overuse of the joint; however, it may be moved in moderation. Steroids will be prescribed to limit inflammation. Pain is anticipated and analgesics will likely be prescribed. Elastic bandages are frequently worn for 2 to 3 days. PTS: 1 DIF: Cognitive Level: Application REF: 723, Table 31-3 OBJ: 5 (theory) TOP: Diagnostic Tests for the Musculoskeletal System KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 20. A patient is learning to use crutches on the stairs. Which action indicates that the patient needs further instruction? a. The patient places the good leg on the step to be climbed first. b. The patient places the affected leg on the step to be climbed first. c. The patient places the crutches on the floor and uses a swing-through method to get to the next step. d. The patient places the crutch on the affected side on the next step first. ANS: A When climbing stairs with crutches, the patient should first stand at the foot of the stairs with weight on the good leg and crutches, put weight on the crutch handles, and then lift the good leg up onto the first step of the stairs. Weight should be placed on the good leg to lift the injured leg and crutches up to that step. PTS: 1 DIF: Cognitive Level: Application REF: 729 OBJ: 5 (clinical) TOP: Patient Teaching: Special Maneuvers on Crutches KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 21. The nurse is assessing the patient’s crutches. Which observation confirms that the crutches are sized correctly? a. The crutches are the same height as the patient’s shoulders. b. The crutches are approximately 12 inches shorter than the patient’s shoulders. c. The crutches are approximately 16 inches shorter than the patient’s height. d. The crutches are tall enough to allow the patient’s arms to be fully extended when walking. ANS: C Crutches should be about 16 inches (40 cm) shorter than the patient’s height. When in the standing position with axillary crutches, the axillary bar should be two finger breadths below the axilla. The elbow should be flexed at a 30-degree angle when the palms of the hands rest on the handgrip. It is important that the patient not rest the body at the axilla on the top of the crutch; body weight should be borne by the arms on the hand rests of the crutches. If crutches are too long, pressure on the axilla will occur and can cause nerve and circulatory impairment. PTS: 1 DIF: Cognitive Level: Application REF: 730, Safety Alert OBJ: 5 (clinical) TOP: Patient Teaching: Special Maneuvers on Crutches KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 22. A patient at risk for the development of osteoporosis has reported plans to increase calcium intake. Which meal choice is most appropriate for this patient? a. Grilled salmon, green beans, and milk b. Hamburger patty on a wheat bun, baked chips, and milk c. Grilled chicken breast, tossed salad, and fruit punch d. Bacon, lettuce, and tomato sandwich on whole-grain bread, orange slices, and milk ANS: A In addition to dairy products, sources of calcium include canned sardines or salmon, tofu, figs, and green vegetables. PTS: 1 DIF: Cognitive Level: Application REF: 721, Nutrition Considerations OBJ: 4 (theory) TOP: Nutrition for Bone Growth and Density KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance MULTIPLE RESPONSE 23. Which component(s) is/are functions of the musculoskeletal system? (select all that apply.) a. Motion b. Fighting of infections c. Support d. Protection of organs e. Body shape ANS: A, C, D, E Musculoskeletal system functions include motion, support, organ protection, and retention of body shape. The musculoskeletal system does not fight infections. PTS: 1 DIF: Cognitive Level: Knowledge REF: 720 OBJ: 1 (theory) TOP: Bone Function KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 24. Which age-related change(s) occur(s) in the musculoskeletal system? (select all that apply.) a. Increased bone density b. Increased brittleness and fragility of bones c. Decreased healing times d. Decreased muscle mass e. Tendon sclerosis ANS: B, C, D, E Age-related musculoskeletal changes include increased fragility, decreased healing times and muscle mass, and tendon sclerosis. Bone density usually decreases with aging. PTS: 1 DIF: Cognitive Level: Knowledge REF: 720 OBJ: 1 (theory) TOP: Age-Related Changes in Musculoskeletal System KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 25. When the nurse plans for the progressive mobilization of a hemiplegic, the nurse will consider the patient’s ability to perform which function(s)? (select all that apply.) a. Move limbs b. Change position in bed independently c. Transfer self from bed to chair d. Perform all activities of daily living (ADLs) independently e. Walk ANS: A, B, C, E Progressive mobilization is assessing the patient’s ability to move their limbs, turn themselves in bed, transfer themselves from bed to chair and back again, and stand and walk. These measurable signs of independent movement represent various stages to which the patient can gradually progress. According to the Joint Commission’s National Patient Safety Goals, it is a nursing responsibility to recognize that these patients are at risk for falls while they are learning to regain mobility. Progressive mobilization does not require that the patient perform all ADLs independently. PTS: 1 DIF: Cognitive Level: Comprehension REF: 728 OBJ: 2 (clinical) TOP: Planning Progressive Mobilization: Considerations KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance COMPLETION 26. When a joint is obliterated by bony overgrowth, the joint is said to be _________. ANS: ankylosed Ankylosis occurs when the joint is overgrown with bony overgrowth. PTS: 1 DIF: Cognitive Level: Knowledge REF: 728 OBJ: 4 (theory) TOP: Ankylosis: Process KEY: Nursing Process Step: N/A MSC: NCLEX: Physiological Integrity: Physiological Adaptation 27. The canal system that runs through the bone and contains the blood and lymph vessels is called the ____________. ANS: haversian system The haversian system is the canal system that runs through the bone to carry blood and lymph vessels. PTS: 1 DIF: Cognitive Level: Knowledge REF: 718 OBJ: 1 (theory) TOP: Haversian System KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance MATCHING Arrange the instructions for a person on crutches to sit down. a. Transfer both crutches to the side of injury. b. With weight on good leg, reach back, and grasp chair arm. c. Sit back in chair. d. Turn slowly and touch backs of legs to seat of chair. e. Using crutch and chair arm for support, slowly sit on chair. 28. Step 1 29. Step 2 30. Step 3 31. Step 4 32. Step 5 28. ANS: D PTS: 1 DIF: Cognitive Level: Application REF: 730, Patient Teaching OBJ: 5 (clinical) TOP: Crutch Walker: Instructions to Sit in Chair KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 29. ANS: A PTS: 1 DIF: Cognitive Level: Application REF: 730, Patient Teaching OBJ: 5 (clinical) TOP: Crutch Walker: Instructions to Sit in Chair KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 30. ANS: B PTS: 1 DIF: Cognitive Level: Application REF: 730, Patient Teaching OBJ: 5 (clinical) TOP: Crutch Walker: Instructions to Sit in Chair KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 31. ANS: E PTS: 1 DIF: Cognitive Level: Application REF: 730, Patient Teaching OBJ: 5 (clinical) TOP: Crutch Walker: Instructions to Sit in Chair KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 32. ANS: C PTS: 1 DIF: Cognitive Level: Application REF: 730, Patient Teaching OBJ: 5 (clinical) TOP: Crutch Walker: Instructions to Sit in Chair KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential Chapter 32: Care of Patients with Musculoskeletal and Connective Tissue Disorders deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. A patient has come to the ambulatory care clinic with a sprain. The nurse correctly differentiates a grade 2 sprain from a grade 3 sprain with the assessment of which finding? a. Pain b. Swelling c. Bleeding into the joint d. Minor loss of function ANS: D The minor loss of function is the differentiating factor. Pain, swelling, and bleeding into the joint are true of both grade 2 and grade 3 sprains. A grade 3 sprain has loss of function of the joint. PTS: 1 DIF: Cognitive Level: Application REF: 735 OBJ: 1 (theory) TOP: Sprains: Grade 2 KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. An older adult has fallen and sprained his ankle in a local park. Which action should the responder perform first? a. Elevate the foot. b. Apply ice. c. Administer aspirin. d. Assist the patient with ambulation. ANS: A Elevation to reduce swelling is the most important initial intervention. Elevation may be done immediately. The responder will have to acquire the ice and pain medication, but should do so as quickly as possible. The responder should not attempt to ambulate the patient at this time. PTS: 1 DIF: Cognitive Level: Analysis REF: 735 OBJ: 1 (theory) TOP: Sprain: First Aid KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 3. When the clinic nurse starts to take the “air cast” off the grade 2 sprain, the patient asks why it is being removed since he still has pain. Which explanation is best? a. “Long-term immobilization can interfere with adequate circulation.” b. “Long-term immobilization may increase long-term edema.” c. “Long-term immobilization can cause permanent disability.” d. “This cast will be replaced with a heavier cast.” ANS: C Air casts, braces, or supports are used only until a joint has been strengthened. If a joint is immobilized too long and muscles are not exercised, muscle atrophy—which begins in a matter of days—can cause permanent disability PTS: 1 DIF: Cognitive Level: Application REF: 735 OBJ: 1 (theory) TOP: Splinted Sprain: Complications KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 4. Which statement indicates that the patient needs further instruction about application of ice to a sprain? a. “I know this ice will reduce the swelling.” b. “I will keep the ice on this knee for the rest of the day.” c. “I will use the ice as you have directed for 24 hours.” d. “I can elevate my leg and use ice to reduce swelling.” ANS: B Ice should be applied for 20 minutes of each hour for the first 24 hours. PTS: 1 DIF: Cognitive Level: Application REF: 735 OBJ: 1 (theory) TOP: Ice: Duration of Application KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 5. The industrial nurse examines an employee who complains of right shoulder pain on abduction. He points with one finger to the exact location of the pain and mentions that he won a racquetball tournament yesterday. The nurse suspects the employee is suffering from which problem? a. Rotator cuff tear b. Bursitis c. Dislocation d. Subluxation ANS: B Bursitis occurs after overuse, with pain in the joint on activity with no erythema and little, if any, swelling. Dislocations are very painful and the pain is spread all over the shoulder. The shoulder also looks misshapen in a dislocation. Rotator cuff tear would prevent the patient from abducting his shoulder. PTS: 1 DIF: Cognitive Level: Application REF: 737 OBJ: 1 (theory) TOP: Bursitis: Signs and Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 6. The nurse is caring for a patient who works as a legal secretary. The patient asks the nurse about ways to avoid developing carpal tunnel syndrome (CTS). Which action should the nurse suggest? a. “Exercise your wrists with repetitive flexion movements nightly.” b. “Wrap your wrists with elastic bandages.” c. “Acquire a pad to support your wrists while typing.” d. “Apply warm compresses to wrists every evening.” ANS: C Elevating the wrist with a firm support eliminates the need to keep the wrists flexed for long periods of time. This wrist support will help prevent CTS. Repetitive motion increases risk for carpal tunnel. Wrapping the wrists or applying warm compresses do not lessen risk of developing carpal tunnel. PTS: 1 DIF: Cognitive Level: Application REF: 737 OBJ: 1 (theory) TOP: CTS: Prevention KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 7. Carpal tunnel syndrome (CTS) is caused when the carpal tunnel compresses which location? a. Radial artery b. Brachial artery c. Median nerve d. Ulnar nerve ANS: C When the median nerve is compressed by the carpal tunnel to the point that numbness, pain, and tingling occur, the result is CTS. PTS: 1 DIF: Cognitive Level: Knowledge REF: 737 OBJ: 1 (theory) TOP: Carpal Tunnel Syndrome: Pathophysiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 8. Which vitamin is essential in treating osteoporosis? a. Vitamin A b. Vitamin D c. Vitamin B12 d. Vitamin C ANS: B Standard treatments for osteoporosis include vitamin D and calcium supplementation, along with weight-bearing exercise. Vitamins A, B12, and C are not included in the standard treatment regimen for osteoporosis. PTS: 1 DIF: Cognitive Level: Knowledge REF: 757 OBJ: 7 (theory) TOP: Osteoporosis: Treatment KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 9. The nurse is caring for a patient who just returned from surgical decompression of the carpal tunnel. Which finding requires the nurse’s immediate action? a. The patient’s fingers swollen and warm. b. The patient complains of generalized pain 5/10. c. The capillary refill time is 8 seconds. d. The patient’s fingers are pink and cool bilaterally. ANS: C A capillary refill of over 5 seconds is an indication of diminished perfusion. Pain and swelling are to be expected, and pink but cool fingers bilaterally do not indicate circulatory compromise. PTS: 1 DIF: Cognitive Level: Application REF: 737 OBJ: 1 (theory) TOP: Nerve Decompression: Aftercare KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 10. An 80-year-old man falls and suffers a compound fracture of the femur. Which immediate action is most appropriate? a. Position him flat on his back. b. Apply a tourniquet on the leg. c. Carefully splint the leg as it is. d. Carefully straighten the leg. ANS: C Any fracture, even a compound one, should be immobilized in position to avoid further injury to the soft tissue attached to the bones. Any other initial action may cause further injury. PTS: 1 DIF: Cognitive Level: Application REF: 738 OBJ: 2 (theory) TOP: Fracture: First Aid Splinting KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 11. Which major advantage is specific to external fixation devices? a. Faster healing time b. Allowance for immediate weight bearing c. Greater freedom of movement d. Pain reduction ANS: C The external device for fracture reduction allows greater freedom of movement, decreasing the problems of immobility. Healing time and pain are the same as with any other fracture reduction method. PTS: 1 DIF: Cognitive Level: Comprehension REF: 740 OBJ: 3 (theory) TOP: External Fixation Device: Advantages KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 12. The patient in a long arm cast (from below the shoulder to the wrist, with a 90-degree elbow flexion) complains of a burning sensation over the elbow. The nurse’s initial intervention should be: a. Elevate the casted arm on pillows. b. Check to see if the cast is properly supported. c. Notify the charge nurse of developing pressure ulcer. d. Cut a “window” in the cast. ANS: B The initial intervention should be to assess for adequate support to the cast, then elevate the limb for 30 minutes. If the pain has not diminished, document the intervention and notify the charge nurse. PTS: 1 DIF: Cognitive Level: Analysis REF: 744, Focused Assessment OBJ: 2 (clinical) TOP: Cast Care: Pain KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 13. The nurse is performing an assessment on the patient who is in bilateral Buck traction. Which finding indicates the need to reposition the patient? a. The patient’s heels are not touching the surface of the mattress. b. The elastic bandages need to be rewrapped. c. The patient’s feet are against the footboard. d. The weights are hanging free. ANS: C When the patient’s feet are against the footboard, the traction is ineffective. The heels should be off the surface of the mattress to reduce the threat of pressure ulcer. The weights should be hanging free. PTS: 1 DIF: Cognitive Level: Application REF: 741 OBJ: 5 (theory) TOP: Buck Traction KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 14. A patient in Russell traction with a Pearson attachment for a fracture of the tibia complains of intense pain at the fracture site. The nurse assesses a temperature of 102° F and increased swelling at the fracture site. Which complication do these findings suggest? a. Osteomyelitis b. Fat embolism c. Traction misalignment d. Nonunion of the fracture ANS: A Osteomyelitis is a bacterial infection of the bone. The causative organism is most often Staphylococcus aureus, which enters the bloodstream from a distant focus of infection, such as a boil or furuncle, or from an open wound, as in an open (compound) fracture. It is usually found in the tibia or fibula, in vertebrae, or at the site of a prosthesis. Osteomyelitis has a sudden onset with severe pain and marked tenderness at the site, high fever with chills, swelling of adjacent soft parts, headache, and malaise. These findings are not consistent with fat embolisms, traction misalignment, or nonunion of the fracture. PTS: 1 DIF: Cognitive Level: Application REF: 742 OBJ: 5 (theory) TOP: Osteomyelitis: Complications KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 15. The nurse is performing morning care for a patient who sustained a fractured pelvis and bilateral femur fractures yesterday in a motorcycle collision. The patient complains of shortness of breath. Assessment reveals audible wheezes and oxygen saturation of 76%. What action should the nurse take first? a. Establish a peripheral intravenous (IV) line. b. Inform the charge nurse. c. Explain the patient’s change in status to his family. d. Raise patient to high Fowler position. ANS: D Fat embolism is a rare but serious complication of a fracture of a bone that has an abundance of marrow fat (e.g., the long bones, pelvis, and ribs). In the early postinjury period, patients with multiple fractures resulting from severe trauma are at risk for this complication. Signs and symptoms of fat embolism include a change in mental status, respiratory distress, tachypnea, crackles and wheezes on auscultating the lungs, rapid pulse, fever, and petechiae (a fine red rash over the chest, neck, upper arms, or abdomen). The nurse should stay with the patient; put him in a high Fowler position, use a nonre-breather mask to give high-flow oxygen, and establish a peripheral IV line. The nurse should also summon the provider immediately as there is about an 80% mortality rate from this complication. Raising the patient to high Fowler position is the best initial intervention as it can be done immediately. The nurse should then verify patent IV access, notify the charge nurse and provider, and update the family on the patient’s status change. PTS: 1 DIF: Cognitive Level: Analysis REF: 742 OBJ: 2 (clinical) TOP: Fracture Complication: Fat Embolus KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 16. The nurse is instructing a patient with rheumatoid arthritis about a prescribed exercise program. Which information should the nurse include? a. Perform exercises every day, 3 to 10 times for every joint. b. Perform exercises even if inflammation is present. c. Perform exercises past the point of pain. d. Perform twice the number of exercises the next day if one day is missed. ANS: A Exercises are essential to preserve joint function and should be done every day 3 to 10 times per joint. Exercises should be omitted if there is inflammation present and should not be taken past the point of pain, or made up the next day. PTS: 1 DIF: Cognitive Level: Comprehension REF: 755 OBJ: 9 (theory) TOP: Rheumatoid Arthritis: Exercises KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 17. The patient with osteoporosis calls the nurse in the doctor’s office to report that she should have taken but has forgotten to take her weekly bisphosphonate (alendronate [Fosamax]) that was due 2 days ago. How should the nurse advise the patient? a. “Take the dose now with 8 ounces of water.” b. “Take two doses 3 days apart.” c. “Skip this week and pick up the schedule next week.” d. “Take two tablets now with a snack.” ANS: C If 2 or more days have passed since the regular dose time, this week’s dose should be skipped and the weekly schedule should be picked up next week. PTS: 1 DIF: Cognitive Level: Application REF: 758, Box 32-2 OBJ: 8 (theory) TOP: Osteoporosis: Treatment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 18. When caring for a patient who has an abductor wedge in place after a total hip replacement, for which finding should the nurse assess? a. Muscle spasms b. Alteration in peripheral circulation c. Compression fracture d. Appropriateness of the size of the wedge ANS: B Pressure from the abductor wedge can interrupt arterial blood supply and compress the peroneal nerve. PTS: 1 DIF: Cognitive Level: Application REF: 751, Safety Alert OBJ: 7 (theory) TOP: Care of a Total Hip Replacement KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential MULTIPLE RESPONSE 19. A patient presents to the emergency department immediately after an injury. An x-ray has been ordered for a suspected dislocation. Before confirmation by x-ray, which finding(s) support the potential diagnosis? (select all that apply.) a. History of forceful injury b. Purple-black hematoma over joint c. Severe pain, aggravated by motion d. Muscle spasm e. Abnormal appearance of joint ANS: A, C, D, E A dislocation will be evidenced by severe pain aggravated by motion, muscle spasm, and an abnormal-appearing joint after the history of a forceful injury. A hematoma, if it forms, will not be evident for a few hours. PTS: 1 DIF: Cognitive Level: Comprehension REF: 736 OBJ: 1 (theory) TOP: Dislocation: Signs and Symptoms KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 20. Soft-tissue injuries require the nurse to assist with or instruct about the importance of which components of care? (select all that apply.) a. Bed rest b. Pain control c. Immobilization d. Activity restrictions e. Prevention of recurrence ANS: B, C, D, E Pain control, immobilization, activity restrictions, and prevention of recurrence are part of the care to a patient with a soft-tissue injury. Bed rest is not warranted with this type of injury. PTS: 1 DIF: Cognitive Level: Comprehension REF: 736 OBJ: 1 (theory) TOP: Soft Tissue Injury: General Care KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 21. Which statement(s) accurately describe the advantage(s) of fiberglass casts? (select all that apply.) a. Lighter weight b. Allowance of weight bearing after 30 minutes c. Cheaper d. Dries more quickly e. Easily pliable f. Smooth surface that is less abrasive to skin ANS: A, B, D Fiberglass casts are lighter and dry quickly, allowing weight bearing in as little as 30 minutes. Fiberglass casts are very expensive and do not lend themselves to molding to body parts. The surface is very rough and often abrades the skin. PTS: 1 DIF: Cognitive Level: Application REF: 740 OBJ: 3 (theory) TOP: Fiberglass Casts: Advantages KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 22. The patient is returning to the unit with a wet long leg cast. To prevent damage to the wet cast, what action(s) should the nurse take? (select all that apply.) a. Determine the cast material. b. Prop the casted limb on a footboard and elevate it until the cast is dry. c. Support the cast with the palms of the hands rather than holding it with the fingers. d. Assess heat generated from the drying cast. e. Explain that the cast has dried when it acquires a grayish color. ANS: A, C, D Determining the cast material will inform the nurse of how quickly the cast can be expected to dry. The cast should be supported with the palms of the hands rather than holding it with the fingers. The heat of the drying cast should be evaluated to prevent skin irritation. A grayish color indicates that the cast is still wet. PTS: 1 DIF: Cognitive Level: Application REF: 740 OBJ: 3 (theory) TOP: Cast Care: Wet Cast KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 23. The nurse is educating a patient going home with a short arm synthetic cast. Which instructions should the nurse include in the teaching plan? (select all that apply.) a. Cover the cast with a plastic bag when taking a shower. b. Blow warm air into the cast to relieve itching. c. Observe skin at the edge of the cast for irritation or injury. d. Check circulation and sensation in the fingers frequently. e. Move and flex the fingers to stimulate circulation. ANS: A, C, D, E All options listed are important teaching points for cast care except blowing warm air into the cast. If itching occurs, cool air will be most helpful. PTS: 1 DIF: Cognitive Level: Application REF: 745 OBJ: 1 (clinical) TOP: Cast Care: Discharge Instruction KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 24. The nurse suspects compartment syndrome in a patient with a side arm cast and traction when observing which finding(s)? (select all that apply.) a. Warm, rosy fingers b. Intense pain in hand and fingers c. Edema of fingers d. Weak radial pulse e. Tingling and numbness ANS: B, C, D, E Compartment syndrome is a restriction of blood flow that occurs in one or more muscle compartments of the extremities. Compartment syndrome is caused by external or internal pressure. The main sign of compartment syndrome is severe, unrelenting pain that is out of proportion to the injury and unrelieved by narcotics. Decreased sensation, numbness and tingling, paleness of the skin, and weakness of the extremity are other signs. Warm, rosy fingers would be assessed as a sign of adequate perfusion. PTS: 1 DIF: Cognitive Level: Application REF: 743 OBJ: 4 (theory) TOP: Cast Complication: Compartment Syndrome KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential COMPLETION 25. The nurse explains that the “C” in the acronym RICE for sprain treatment stands for _______. ANS: compression RICE stands for Rest, Ice, Compression, and Elevation. PTS: 1 DIF: Cognitive Level: Knowledge REF: 735 OBJ: 1 (theory) TOP: Sprain Treatment: Acronym KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 26. The nurse uses a visual aid to show the difference between a complete dislocation and a partial dislocation, which is also called a(n) __________. ANS: subluxation A subluxation is a partial dislocation. PTS: 1 DIF: Cognitive Level: Comprehension REF: 736 OBJ: 1 (theory) TOP: Subluxation: Definition KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation MATCHING Match the fracture type to the description that characterizes it. a. Complete fracture b. Comminuted fracture c. Closed fracture d. Compound fracture e. Greenstick fracture 27. Bone is partially broken and partially bent 28. Fracture that has not broken through skin 29. Fracture bone end protruding through skin 30. Bone that is in two distinct pieces 31. Bone shattered in more than two pieces 27. ANS: E PTS: 1 DIF: Cognitive Level: Knowledge REF: 738, Box 32-1 OBJ: 2 (theory) TOP: Fractures: Types KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 28. ANS: C PTS: 1 DIF: Cognitive Level: Knowledge REF: 738, Box 32-1 OBJ: 2 (theory) TOP: Fractures: Types KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 29. ANS: D PTS: 1 DIF: Cognitive Level: Knowledge REF: 738, Box 32-1 OBJ: 2 (theory) TOP: Fractures: Types KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 30. ANS: A PTS: 1 DIF: Cognitive Level: Knowledge REF: 738, Box 32-1 OBJ: 2 (theory) TOP: Fractures: Types KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 31. ANS: B PTS: 1 DIF: Cognitive Level: Knowledge REF: 738, Box 32-1 OBJ: 2 (theory) TOP: Fractures: Types KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance Match the type of fracture stabilization with the characteristics that best describe it. (The options can be used once, more than once, or not at all.) a. Closed reduction b. Open reduction c. Internal fixation d. External fixation 32. Reduction of fracture through surgical incision 33. Metal appliances are used to stabilize pieces of fracture 34. Reduction of fracture and fixation to device that maintains alignment 35. Used with infected fractures that do not heal properly 36. Manual reduction and manipulation of bones into alignment 37. Used with older adults when brittle bones do not heal quickly 32. ANS: B PTS: 1 DIF: Cognitive Level: Comprehension REF: 739-740 OBJ: 3 (theory) TOP: Fracture Reduction Methods: Characteristics KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 33. ANS: C PTS: 1 DIF: Cognitive Level: Comprehension REF: 739-740 OBJ: 3 (theory) TOP: Fracture Reduction Methods: Characteristics KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 34. ANS: D PTS: 1 DIF: Cognitive Level: Comprehension REF: 739-740 OBJ: 3 (theory) TOP: Fracture Reduction Methods: Characteristics KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 35. ANS: D PTS: 1 DIF: Cognitive Level: Comprehension REF: 739-740 OBJ: 3 (theory) TOP: Fracture Reduction Methods: Characteristics KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 36. ANS: A PTS: 1 DIF: Cognitive Level: Comprehension REF: 739-740 OBJ: 3 (theory) TOP: Fracture Reduction Methods: Characteristics KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 37. ANS: C PTS: 1 DIF: Cognitive Level: Comprehension REF: 739-740 OBJ: 3 (theory) TOP: Fracture Reduction Methods: Characteristics KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance Place the steps of the process of fracture healing in proper order. a. Medullary canal is reconstructed. b. Mature bone cells form ossification. c. Callus is formed. d. Granulation tissue is formed. e. Hematoma is formed between broken ends of bone. 38. Step 1 39. Step 2 40. Step 3 41. Step 4 42. Step 5 38. ANS: E PTS: 1 DIF: Cognitive Level: Analysis REF: 739 OBJ: 2 (theory) TOP: Fracture Healing: Process KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 39. ANS: D PTS: 1 DIF: Cognitive Level: Analysis REF: 739 OBJ: 2 (theory) TOP: Fracture Healing: Process KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 40. ANS: C PTS: 1 DIF: Cognitive Level: Analysis REF: 739 OBJ: 2 (theory) TOP: Fracture Healing: Process KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 41. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 739 OBJ: 2 (theory) TOP: Fracture Healing: Process KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 42. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 739 OBJ: 2 (theory) TOP: Fracture Healing: Process KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance Chapter 33: The Urinary System deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. An 85-year-old patient who has been NPO since midnight last night for diagnostic testing just completed the procedure. Which intervention is most important? a. Inform the patient about the test results. b. Obtain the patient’s weight for comparison to the morning value. c. Turn the patient every 2 hours. d. Offer 4 ounces of water or juice every hour. ANS: D Offering small amounts of fluid every hour will rehydrate the older adult without resorting to intravenous fluids. The older adult has very little fluid reserve and has lost the ability to concentrate the urine; consequently, a long period without fluid intake can cause dehydration. The doctor should inform the patient about the test results. Weighing the patient again is unnecessary. While prevention of skin breakdown is important, there is no indication that the patient cannot reposition independently. PTS: 1 DIF: Cognitive Level: Application REF: 769, Older Adult Care Points OBJ: 1 (clinical) TOP: Dehydration in the Older Adult KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 2. The nurse cautions the diabetic patient that diabetes affects the blood flow through the kidney. Which statement indicates that the patient understands the nurse’s teaching? a. “Long-term high blood sugars provide an environment for bacteria to grow, which can damage my kidneys.” b. “Diabetes causes changes to blood vessels, which impacts blood flow to my kidneys.” c. “Diabetes causes an immune response and exposes my kidneys to antibody complexes.” d. “Long-term insulin use leads to scarring on the kidneys.” ANS: B The long-term effect of diabetes is generalized vasoconstriction, which leads many diabetic patients to renal insufficiency and renal failure. Diabetes can increase a patient’s risk for infection. Diabetes does not cause exposure to antibody complexes. Insulin usage does not scar the kidneys. PTS: 1 DIF: Cognitive Level: Application REF: 767 OBJ: 2 (theory) TOP: Renal Insufficiency Related to Diabetes Mellitus KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. The nurse explains that when the kidney suffers an autoimmune inflammatory reaction, the glomeruli lose their ability to function effectively. The nurse is describing the etiology of which problem? a. Glomerulonephritis b. Renal calculi c. Hydronephrosis d. Acute pyelonephritis ANS: A Glomerulonephritis occurs when the inflammatory process alters the effectiveness of the semipermeable membrane in the glomeruli. Renal calculi are kidney stones; causative factions include urinary infections, inadequate fluid intake, and sluggish urine flow. Hydronephrosis results when flow of urine from the kidney is obstructed, and the kidney dilates and fills with fluid. Acute pyelonephritis an infection of the kidneys thought to occur when bacteria (such as Escherichia coli) from a bladder infection travel up the ureters to infect the kidneys. PTS: 1 DIF: Cognitive Level: Comprehension REF: 767 OBJ: 2 (theory) TOP: Glomerulonephritis: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. The nurse is caring for a confused patient who requires bladder training. Which component of the bladder training program can the nurse safely delegate to the nursing assistant? a. Teaching the patient about a voiding diary b. Creating a schedule for voiding c. Creating a schedule for fluids d. Recording instances of linen changes and fluids offered ANS: D In planning and implementing a bladder training program for your confused patient, there are several ways in which the UAP can provide help. The nurse appropriately delegates reporting and recording any fluids offered and consumed, along with frequency of linen changes. The nurse should perform patient teaching about the diary, especially since the patient is confused; the nurse is responsible for determining the patient’s level of comprehension. The nurse should create the schedule for voiding and fluids, and once the schedule is established, the nursing assistant can help the patient to follow the schedule. PTS: 1 DIF: Cognitive Level: Analysis REF: 782, Assignment Considerations OBJ: 9 (theory) TOP: Bladder Training KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, and Effective Care Environment: Coordinated Care 5. When the patient asks why he has so many urinary tract infections (UTIs), the nurse informs the patient that his recurrent UTIs most likely result from which causative factor? a. Bacteria that colonize in the kidney b. Viral infections generating debris in the bladder c. Carelessness in handwashing d. Spicy foods irritating the bladder wall ANS: A The urinary tract is very vulnerable to bacterial infection. In the high volume of blood that is filtered by the kidney, there are some bacteria that can colonize in the kidney, causing an infection. Also, bacteria can easily enter the urinary tract through the urethra, and then the infection may spread up into the kidneys. Viral infections do not generate bladder debris. Recurrent UTIs are not likely the result of poor hand hygiene. Spicy foods do not irritate the bladder wall or lead to UTIs. PTS: 1 DIF: Cognitive Level: Comprehension REF: 767 OBJ: 2 (theory) TOP: UTI: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 6. How can nephrotoxic drugs such as doxycycline and rifampin cause kidney damage? a. Bacterial destruction of the nephrons b. Chemical alterations of glomeruli c. Necrosis of tubules from reduction of oxygenation d. “Clumping” of cellular debris from killed bacteria ANS: B Nephrotoxic drugs may chemically alter the glomeruli, which make them ineffective. PTS: 1 DIF: Cognitive Level: Knowledge REF: 767 OBJ: 2 (theory) TOP: Nephrotoxicity KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 7. In order to keep optimal flow through the urinary system, a person should have a minimum daily intake of how many mL of fluid? a. 1000 mL b. 1500 mL c. 2000 mL d. 4000 mL ANS: C Intake of a minimum of 2000 mL/day is adequate to maintain optimal flow through the urinary system. PTS: 1 DIF: Cognitive Level: Knowledge REF: 768 OBJ: 3 (theory) TOP: Optimum Fluid Intake KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 8. The nurse is caring for a patient who has been taking a sulfa drug for a urinary tract infection (UTI). Which intervention is most important for the nurse to add to the patient’s care plan? a. Ambulate the patient q shift. b. Ask the patient about a penicillin allergy. c. Weigh the patient daily. d. Increase fluid intake to 1.5 L/day. ANS: D With sulfa drugs, it is most important for the patient to maintain a fluid intake of at least 3000 mL (1.5 L) in order to prevent crystalluria and stone formation. Ambulation does not directly correlate to the sulfa drug in any way. Investigating an allergy is an assessment, not an intervention, and this action should occur prior to administering the first dose. Daily weights are important for tracking inputs and outputs, but it is not the priority intervention. PTS: 1 DIF: Cognitive Level: Analysis REF: 768 OBJ: 3 (theory) TOP: Sulfa Drugs: Increased Fluid Intake KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 9. The nurse reviewing laboratory reports for a patient admitted for acute pyelenophritis. Which finding is most concerning to the nurse? a. Blood urea nitrogen (BUN) of 10.5 mg/dL b. Sodium of 140 mEq/L c. Potassium of 5.0 mEq/L d. Creatinine of 2.0 mg/dL ANS: D A creatinine of 2.0 is abnormally high and indicates that kidney function negatively affected. The BUN, sodium, and potassium values are within normal limits. (Laboratory ranges include: BUN 10 to 20 mg/dL, creatinine 0.6 to 1.2 mg/dL, sodium 135 to 145 mEq/L, and potassium 3.5 to 5.5 mEq/L.) PTS: 1 DIF: Cognitive Level: Comprehension REF: 768, Clinical Cues OBJ: 3 (theory) TOP: Serum Reports: BUN and Creatinine KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 10. A patient is scheduled to undergo a cystogram. Which statement indicates that the patient accurately understands the nurse’s teaching about prevention of potential complications of the test? a. “I can have a clear liquid breakfast in the morning before the test.” b. “I will have to have a Foley catheter.” c. “The test uses radioactive fluid to help take special images of my bladder.” d. “I should drink plenty of fluids after the test is over.” ANS: D A radionuclide cystogram utilizes a sodium iodine solution to obtain images of the bladder. The patient should increase intake postprocedure to flush the solution out of the body quickly to limit potential for damage from the hypertonic solution. While the patient is allowed to have a clear breakfast the morning prior to the test and will require a Foley catheter during the procedure, neither of these actions prevent complications from the test. An understanding of the purpose of the test does not prevent potential complications from the procedure. PTS: 1 DIF: Cognitive Level: Application REF: 771, Table 33-2 OBJ: 1 (clinical) TOP: Radionuclide Cystogram: Complication Prevention KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 11. The nurse is caring for a woman suspected of having a vaginal fistula. Which finding supports the potential diagnosis? a. Pneumaturia b. Hematuria c. Oliguria d. Dysuria ANS: A Pneumaturia, or gas in the urine, can occur if there is an abnormal passage between the bladder and vagina. A fistula would not cause hematuria, oliguria, or dysuria. PTS: 1 DIF: Cognitive Level: Comprehension REF: 774 OBJ: 2 (clinical) TOP: Vaginal Fistula: Pneumaturia KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 12. When the nurse is caring for a patient who reports he has blood that begins when he initiates the urine stream and then abates. Based on underlying pathophysiology, the nurse concludes that the hematuria is occurring in which location? a. In the kidney b. Above the neck of the bladder c. In the neck of the bladder d. In the urethra ANS: D Gross hematuria indicates bleeding from some point in the urinary tract. If the blood is noticed as soon as voiding starts, it is likely that the blood is from somewhere in the urethra. Blood that appears at the end of urination probably comes from near the neck of the bladder. Bleeding throughout voiding indicates that the blood is coming from a site above the neck of the bladder because the blood has been well mixed with the urine in the bladder. PTS: 1 DIF: Cognitive Level: Comprehension REF: 774 OBJ: 3 (clinical) TOP: Hematuria: Location KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 13. The nurse is collecting data from a patient who complains of having urinary frequency. The nurse should inquire about which dietary habit? a. Red meat intake b. Caffeine intake c. Complex carbohydrate intake d. Tomato juice intake ANS: B Caffeine and other diuretics found in foods and drinks, as well as increased fluid intake of fluid, can increase the number of times a person must urinate. PTS: 1 DIF: Cognitive Level: Comprehension REF: 774 OBJ: 2 (theory) TOP: Urinary Frequency: Cause KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 14. The student nurse is attempting to irrigate an indwelling catheter. Which action best indicates that the student nurse accurately understands the correct procedure? a. The student nurse irrigates using a steady, gentle stream. b. The student nurse forces solution into the catheter to remove the obstruction. c. The student nurse pulls back on the plunger if fluid will not enter the catheter. d. The student nurse counts the amount of irrigation fluid as output. ANS: A When irrigating, use the correct amount of sterile solution (according to agency policy, or the amount of solution that may be determined by physician’s order for nephrostomy tubes, ureteral tubes, or catheters). When irrigating, use a steady, gentle stream to irrigate. Avoid exerting pressure that may traumatize or cause discomfort. Do not pull back forcefully on an irrigating syringe attached to a urinary catheter or tube as this creates negative pressure that may damage delicate tissues. The amount of irrigation fluid is counted as intake, not output. PTS: 1 DIF: Cognitive Level: Comprehension REF: 777, Box 33-3 OBJ: 3 (clinical) TOP: Irrigation of Indwelling Catheter KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 15. The patient confides that sneezing makes her “wet her pants.” The nurse recognizes this cardinal sign of which type of incontinence? a. Urge incontinence b. Stress incontinence c. Functional incontinence d. Overflow incontinence ANS: B Stress incontinence occurs when the urethral sphincter fails and there is an increase in intra-abdominal pressure, caused by things such as sneezing, laughing, coughing, or aerobic exercise. Urge incontinence is the involuntary loss of urine when there is a strong urge to urinate (urinary urgency). Functional incontinence is caused by cognitive inability to recognize the urge to urinate or self-care deficit caused by extreme depression. Inability to reach the bathroom due to restraints, side rails, or an out-of-reach walker can also result in functional incontinence. Overflow incontinence occurs when there is poor contractility of the detrusor muscle or obstruction of the urethra, as in prostate hypertrophy in the male or genital prolapse or abnormality in the female. PTS: 1 DIF: Cognitive Level: Comprehension REF: 778 OBJ: 4 (theory) TOP: Incontinence: Stress KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 16. The nurse is caring for a frustrated patient reports that she still involuntarily voids despite two surgeries to correct incontinence. Which statement indicates that the patient accurately understands the nurse’s teaching about incontinence management after surgery? a. “I will avoid wearing pads that can cause skin breakdown.” b. “I will talk to my health care provider about a pessary.” c. “I will have to have an indwelling catheter.” d. “I will have to have another surgery.” ANS: B When surgical measures do not solve the problem, incontinence may be managed by a variety of measures, including intermittent catheterization, indwelling urethral catheterization, suprapubic catheters, external collection systems (such as condom catheters), protective pads and garments, or pelvic organ support devices such as a pessary. The pessary may be useful in managing this patient’s stress incontinence. The patient should utilize protective pads and garments. An indwelling catheter may or may not be necessary for this patient. There is no indication that the patient will require another surgery, especially since the previous two surgeries have not eliminated episodes on incontinence. PTS: 1 DIF: Cognitive Level: Application REF: 780 OBJ: 4 (clinical) TOP: Incontinence: Voiding Diary KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 17. The nurse is instructing a patient about use of vaginal weight training. Which technique indicates that the patient accurately understands the nurse’s teaching? a. The patient inserts the largest cone and leaves it in place for 4-hour increments. b. The patient inserts the smallest cone and performs 10 Kegel exercises before removing it. c. The patient inserts the smallest cone and holds it in place with muscle tightening for 15 minutes before removing it. d. The patient inserts the largest cone and attempts to expel it with vaginal muscle tightening. ANS: C Vaginal weight training is done with a set of five small, cone-shaped weights that are used along with pelvic muscle exercise as a therapeutic option for incontinence. The lightest cone, which has a string attached, is inserted into the vagina and held in place by muscle tightening for 15 minutes twice a day. When there is no problem holding this cone in place, the next heaviest cone is used. This continues until the heaviest cone can be held in place for the 15-minute period. PTS: 1 DIF: Cognitive Level: Application REF: 779 OBJ: 4 (clinical) TOP: Incontinence: Vaginal Weight Training KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 18. A patient has just returned to the nursing unit after having a renal biopsy. Which intervention is most important to include in the patient’s nursing care plan? a. Keep the patient NPO for the first 4 hours after the procedure. b. Instruct the patient to avoid laughing and use a pillow to splint when sneezing. c. Report hematuria immediately. d. Teach the patient about the importance of limiting fluid intake. ANS: B Postprocedure care for the patient who has undergone a renal biopsy will include monitoring for bleeding, avoiding activities that could increase abdominal pressure, and keeping the patient flat for 6 to 24 hours. Laughing and sneezing increase abdominal pressure and should be avoided; splinting when sneezing will help to decrease abdominal pressure. Oral intake is encouraged. Bloody urine is expected for the first 24 hours after the biopsy. The patient should increase fluid intake unless otherwise contraindicated and drink at least 3000 mL of fluid to flush the urinary system. PTS: 1 DIF: Cognitive Level: Application REF: 769, Patient Teaching OBJ: 1 (clinical) TOP: Patient Teaching: Renal Biopsy KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 19. The nurse is caring for a patient who recently had abdominal surgery. Which assessment finding requires the nurse’s immediate attention? a. Bruising near the surgical incision site b. Report of constipation c. Abdominal pain of 4/10 d. Urine output of 20 mL in the last hour ANS: D Urine output of 20 mL in an hour is inadequate and could indicate that the patient is not perfusing properly. Bruising is a common occurrence after surgery, from small blood vessels leaking blood under the skin after an incision is made. Constipation is normal after abdominal surgery, as anesthesia, surgery, and pain medications slow bowl motility. Abdominal pain of 4/10 may require an analgesic but does not indicate an emergent or urgent finding. PTS: 1 DIF: Cognitive Level: Analysis REF: 777 OBJ: 2 (clinical) TOP: Intake and Output KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 20. The nurse is caring for a patient with deteriorating kidney function. Laboratory work indicates 900 mg of uric acid in 24 hours. In addition to administering prescribed medication, which dietary modification should the nurse address? a. Limit servings of beef to 3-ounce portions. b. Increase intake of avocados and liver. c. Avoid yogurt or skim milk. d. Limit intake of potatoes and pasta. ANS: A Uric acid is an end product of protein metabolism, and levels may be elevated in renal failure and associated with increased dietary intake of purine-containing foods. Normal findings are 250 to 750 mg/24 hr (normal diet). A value of 900 mg/24 hr indicates an elevated uric acid level. Sources of purines include beef, liver, and sardines. Purine-rich foods like beef should be limited to small portions or eliminated completely from the patient’s diet. Additionally, fatty foods like avocados aid the kidneys in retaining uric acid. Skim milk, yogurt, potatoes, and pasta are low-purine food choices that the patient can eat. PTS: 1 DIF: Cognitive Level: Application REF: 770, Table 33-2 OBJ: 1 (clinical) TOP: Diagnostic Tests for Urologic Disorders: Hyperuricemia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential MULTIPLE RESPONSE 21. Which statement(s) accurately describe the functions of the kidneys? (select all that apply.) a. Regulation of electrolytes b. Regulation of fluid volume c. Regulation of blood pressure d. Secretion of erythropoietin e. Transportation of urine ANS: A, B, C, D Kidney functions include regulation of electrolytes, fluid volume, and blood pressure, along with the secretion of erythropoietin. The ureters transport urine from the renal pelvis to the bladder. PTS: 1 DIF: Cognitive Level: Comprehension REF: 766 OBJ: 1 (theory) TOP: Kidney Function KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 22. Which age-related change(s) occur(s) in the urinary system? (select all that apply.) a. Prostate hypertrophy b. Decreased renin secretion c. Decreased bladder muscle tone d. Enlarged bladder. e. Increased ability to concentrate urine ANS: A, B, C As the urinary system ages, the prostate hypertrophies, renin secretion decrease, and bladder muscle tone decrease. Age-related changes also include shrinking bladder size and decreased ability to concentrate urine. PTS: 1 DIF: Cognitive Level: Comprehension REF: 767 OBJ: 2 (theory) TOP: Age-Related Changes in the Urinary System KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 23. When discussing bladder health with a patient, the nurse emphasizes the importance of regular voiding in a timely manner. Which statement(s) indicate(s) that the patient accurately understands the underlying rationale for this recommendation? (select all that apply.) a. “Urinating regularly will prevent prolonged exposure of the bladder wall to harmful wastes.” b. “Allowing my bladder to overfill causes the walls to overstretch.” c. “A full bladder can cause undue strain on the urinary sphincters.” d. “The characteristics of urine can change after being in the bladder for overly extended periods.” e. “Pressure from a distended bladder can cause excessive pressure on my colon.” ANS: A, B, C Urinating regularly helps to prevent prolonged exposure to toxins. Allowing the bladder to overfill can allow the walls to become hyperelastic. A full bladder may also strain the urinary sphincters. Urine does not change character in the bladder and does not press on the colon. PTS: 1 DIF: Cognitive Level: Comprehension REF: 768 OBJ: 2 (theory) TOP: Encouraging Voiding Frequency KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 24. While caring for a patient with an indwelling catheter, which intervention(s) is/are important for the nurse to include in the plan of care? (select all that apply.) a. Observe tube placement and note the level of urine in the collection bag. b. Keep the drainage bag even with the level of the bed. c. Avoid ambulation until the catheter is discontinued. d. Use a syringe to deflate the balloon before discontinuing the catheter. e. Clean the meatus and catheter with soap and water. ANS: A, D, E The nurse should observe tube placement and urine levels, utilize a syringe to deflate the balloon prior to removing the catheter, and perform catheter care with soap and water. The drainage bag should be kept lower than the bed to prevent backflow of urine into the bag (which could lead to an infection). As long as the bag position is maintained below catheter insertion site, the patient can ambulate unless otherwise contraindicated. PTS: 1 DIF: Cognitive Level: Application REF: 776-777 OBJ: 3 (clinical) TOP: Catheter Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 25. The nurse is caring for a patient with urinary retention. Which measure(s) should the nurse take when assisting the patient to void? (select all that apply.) a. Accompany the patient to the toilet. b. Offer the patient tea or soda. c. Provide a warm bath. d. Discourage the double void technique. e. Run water in the lavatory. ANS: B, C, E Acceptable interventions when assisting a patient to void include offering a caffeinated or carbonated beverage, and providing a warm bath or running water in the lavatory to stimulate urination. The patient should be given privacy and adequate time to void. The nurse should instruct the patient to utilize the double void technique (void, sit on the toilet for several minutes, and void again). PTS: 1 DIF: Cognitive Level: Application REF: 782 OBJ: 3 (theory) TOP: Urine Retention: Techniques to Relieve KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort COMPLETION 26. The basic functional unit of the kidney is the ________. ANS: nephron The nephron is the functional unit of the kidney, housing the glomerulus and the collecting tubules. Each kidney has approximately 1 million nephrons. PTS: 1 DIF: Cognitive Level: Knowledge REF: 765 OBJ: 1 (theory) TOP: Nephron: Definition KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 27. The nurse explains that the urge to void occurs when the bladder contain as little as ______ mL of urine. ANS: 150 The bladder will transmit the urge to void with a bladder content as little as 150 mL of urine. PTS: 1 DIF: Cognitive Level: Knowledge REF: 767 OBJ: 3 (theory) TOP: Voiding: Urge KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation MATCHING In order to communicate with the patient more effectively, the nurse clarifies the meanings of some urological terms. Match these terms with their correct definitions. a. Anuria b. Oliguria c. Polyuria d. Nocturia e. Hematuria 28. Diminished urine 29. Blood in the urine 30. Urination at night 31. High urinary output 32. Absence of urine 28. ANS: B PTS: 1 DIF: Cognitive Level: Knowledge REF: 775, Box 33-2 OBJ: 1 (theory) TOP: Definitions of Terms KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 29. ANS: E PTS: 1 DIF: Cognitive Level: Knowledge REF: 775, Box 33-2 OBJ: 1 (theory) TOP: Definitions of Terms KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 30. ANS: D PTS: 1 DIF: Cognitive Level: Knowledge REF: 775, Box 33-2 OBJ: 1 (theory) TOP: Definitions of Terms KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 31. ANS: C PTS: 1 DIF: Cognitive Level: Knowledge REF: 775, Box 33-2 OBJ: 1 (theory) TOP: Definitions of Terms KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 32. ANS: A PTS: 1 DIF: Cognitive Level: Knowledge REF: 775, Box 33-2 OBJ: 1 (theory) TOP: Definitions of Terms KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance Chapter 34: Care of Patients with Disorders of the Urinary System deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is caring for a 90-year-old resident in a long-term care facility who is becoming progressively confused and irritable. What should the nurse do next? a. Request an order for a urinalysis. b. Hold the patient’s antihypertensive medications. c. Assess the patient for fecal impaction. d. Notify the charge nurse. ANS: A Sudden confusion and irritability may indicate a urinary tract infection (UTI) in the older adult. There is no supportive information indicating issues with the patient’s antihypertensive medications or the presence of a fecal impaction. PTS: 1 DIF: Cognitive Level: Application REF: 786, Older Adult Care Points OBJ: 1 (theory) TOP: UTI in the Older Adult KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 2. While reviewing a patient’s medications, the nurse notes that a patient has been prescribed liquid nitrofurantoin (Furadantin). Which intervention should the nurse add to the nursing care plan? a. Administer nitrofurantoin on an empty stomach. b. Provide a straw and instruct the patient to rinse the mouth after taking nitrofurantoin. c. Administer nitrofurantoin early in the morning to avoid insomnia. d. Assess the urine for hematuria. ANS: B The liquid form of this drug will stain the teeth. The patient should use a straw and rise the mouth after taking this medication. The drug causes drowsiness and should be given at night. Hematuria is not a concern. PTS: 1 DIF: Cognitive Level: Application REF: 787, Table 34-1 OBJ: 1 (theory) TOP: Nitrofurantoin: Nursing Considerations KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 3. A 25-year-old woman comes to the emergency department with nonspecific urethritis. Which information is most important for the nurse to obtain? a. “How many servings of green vegetables do eat each day?” b. “How often, if any, do you consume alcohol?” c. “How often do you use bath salts or take bubble baths?” d. “Do you take a daily multivitamin?” ANS: C Urethritis refers to inflammation of the urethra. The use of bath salts, spermicidal jelly, body powders, and feminine hygiene sprays can cause irritation and lead to urethritis. Green vegetable intake, alcohol consumption, and multivitamin intake do not directly relate to causative factors for urethritis. PTS: 1 DIF: Cognitive Level: Application REF: 788 OBJ: 1 (theory) TOP: Urethritis: Signs and Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. A 25-year-old man comes to the college clinic with fever of 101° F, nausea, and flank pain that radiates into the thigh and genitals. The nurse anticipates that the patient will undergo workup for which infection? a. Urethritis b. Pyelonephritis c. Glomerulonephritis d. Cystitis ANS: B Acute pyelonephritis is an infection of the kidneys. It is thought to occur when bacteria (such as Escherichia coli) from a bladder infection travel up the ureters to infect the kidneys. A frequent cause of pyelonephritis is an obstruction, causing stasis of urine and stones that cause irritation of the tissue. Both situations provide an environment in which bacteria can grow. When bacteria enter the renal pelvis, inflammation and infection occur. Pyelonephritis causes nausea and vomiting, flank pain, temperature elevation with chills, headache, and malaise. Urethritis and cystitis often cause dysuria. Glomerulonephritis commonly occurs about 2 to 3 weeks after a group A beta-hemolytic streptococcal infection, such as “strep throat” or impetigo. The patient with acute glomerulonephritis usually becomes suddenly ill with fever, chills, flank pain, widespread edema, puffiness about the eyes, visual disturbances, and marked hypertension. PTS: 1 DIF: Cognitive Level: Comprehension REF: 788 OBJ: 1 (theory) TOP: Pyelonephritis: Signs and Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. The nurse is caring for a young man who has been prescribed ciprofloxacin (Cipro) for pyelonephritis. Which information should the nurse include in order to prevent recurrence? a. Take this medication with a full glass of water. b. Take antacids 2 hours after this medication. c. Take the entire prescription. d. Take this medication on an empty stomach. ANS: A The most important way to prevent recurrence is to take the entire course of antibiotic therapy. Cipro should be taken at least 2 hours prior to an antacid, but this action does not work to prevent recurrence. Cipro does have to be taken with a full glass of water and may be taken on a full or empty stomach. PTS: 1 DIF: Cognitive Level: Application REF: 788-789 OBJ: 1 (theory) TOP: Pyelonephritis KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 6. The nurse is reviewing a history and physical examination of a 22-year-old man hospitalized for acute glomerulonephritis. Which finding best alerts the nurse to a potential causative agent? a. A recent trip to Mexico b. Unprotected sexual activity c. A recent strep throat infection d. A recent protocol of ciprofloxacin (Cipro) ANS: C Glomerulonephritis is primarily seen in children and young adults, and affects males more often than females. It most commonly occurs about 2 to 3 weeks after a group A beta-hemolytic streptococcal infection, such as “strep throat” or impetigo; however, it can occur in response to bacterial, viral, or parasitic infections elsewhere in the body. It is an immunologic problem caused by an antigen-antibody reaction. International travel and unprotected sexual activity are not causative agents for glomerulonephritis. While recent cipro therapy does indicate a recent bacterial infection, it does not cause glomerulonephritis. PTS: 1 DIF: Cognitive Level: Application REF: 789 OBJ: 2 (theory) TOP: Acute Glomerulonephritis: Etiology KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 7. Which statement best indicates that the patient understands teaching about dietary restrictions in glomerulonephritis? a. “I should avoid canned soups and hot dogs.” b. “I should drink more water.” c. “I should eat more meat and cheeses.” d. “I should not eat fresh produce.” ANS: A Care of the patient with glomerulonephritis may include a sodium-restricted diet if edema is present. Canned soups and processed meats are high in sodium. Fluids may be limited if there is oliguria (diminished urine secretion in relation to intake) or anuria (absence of urine). A low-protein, high-carbohydrate diet also may be ordered, so the patient should not increase meat intake. Fresh produce is not contraindicated for this patient. PTS: 1 DIF: Cognitive Level: Analysis REF: 789 OBJ: 2 (theory) TOP: Glomerulonephritis: Sodium-Restricted Diet KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 8. A patient with glomerulonephritis has an order to undergo plasmapheresis. Which statement indicates that the patient accurately understands teaching about the procedure? a. “This procedure removes my affected plasma and gives me a clean replacement.” b. “This procedure will use the IV in my hand.” c. “I will need to lie very still while the pictures are taken.” d. “I should drink this contrast with a straw to keep it from staining my teeth.” ANS: A Plasmapheresis is a blood cleansing procedure used in autoimmune disorders, such as acute glomerulonephritis or myasthenia gravis (see Chapter 24). Much like hemodialysis, plasmapheresis uses a special filter to remove plasma and “wash” it to eliminate antibodies. If treatment is not successful, the disease will rapidly progress to kidney failure and death. The patient’s blood is accessed through a shunt or a CVC, not a peripheral intravenous (IV) line. This procedure does not involve imaging or contrast. PTS: 1 DIF: Cognitive Level: Application REF: 789 OBJ: 2 (theory) TOP: Glomerulonephritis: Plasmapheresis KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 9. The nurse is caring for a patient diagnosed with glomerulonephritis. The patient reports feeling “bored and caged,” and asks when he can resume normal activities. Which finding indicates that bed rest may be discontinued? a. The patient has been compliant with medication for 2 weeks. b. The serum sodium level is 140 mEq/L. c. The patient’s weight returns to preillness baseline. d. The patient’s blood pressure is 110/74. ANS: D Bed rest is enforced until the person with glomerulonephritis no longer exhibits hypertension and hematuria. PTS: 1 DIF: Cognitive Level: Application REF: 789 OBJ: 2 (theory) TOP: Glomerulonephritis: Need for Bed Rest KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 10. As chronic glomerulonephritis progresses, how is the kidney usually affected? a. The kidney swells. b. The kidney atrophies. c. The kidney develops “skip lesions.” d. The kidney develops multiple cysts. ANS: B Chronic glomerulonephritis may develop rapidly or progress slowly over 20 to 30 years or longer. The exact cause is unknown; however, in chronic glomerulonephritis, the kidney atrophies, functional nephrons decrease, and eventually the kidneys fail. The kidney does not swell, develop skip lesions, or multiple cysts. PTS: 1 DIF: Cognitive Level: Comprehension REF: 790 OBJ: 2 (theory) TOP: Chronic Glomerulonephritis: Pathophysiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 11. The nurse is caring for a patient with glomerulonephritis. Which finding best leads the nurse to suspect that the patient is developing nephrotic syndrome? a. Ascites b. Anorexia c. Pruritis d. Lethargy ANS: A Nephrotic syndrome sometimes occurs after the glomeruli have been damaged by glomerulonephritis or some other disease. This damage results in increased membrane permeability and excretion of protein and decreased serum albumin (hypoalbuminemia). Hypoalbuminemia causes fluid to shift out into the body tissues and the result is severe edema (ascites). Patients with nephrotic syndrome may also display lethargy and anorexia but are not hallmark symptoms. Nephrotic syndrome does not cause pruritus (itching), although patients with renal insufficiency with high phosphorus/calcium products may experience itching. PTS: 1 DIF: Cognitive Level: Application REF: 790 OBJ: 2 (theory) TOP: Nephrotic Syndrome: Manifestations KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 12. A patient has a kidney stone lodged in the ureter. He questions why it must be removed. What response is most appropriate? a. “If the stone is not promptly removed, you will continue to have blood in your urine.” b. “If the stone is not removed, it could block urine flow from the kidney and cause swelling within the kidney.” c. “Keeping the stone in your body may result in a condition called glomerulonephritis.” d. “You may experience scarring of the renal structures and a condition known as nephrotic syndrome may result.” ANS: B An obstructed ureter will cause urinary reflux into the renal pelvis, causing hydronephrosis and, ultimately, destruction of the kidney. PTS: 1 DIF: Cognitive Level: Comprehension REF: 790 OBJ: 2 (clinical) TOP: Hydronephrosis: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 13. The nurse is caring for a patient who underwent a right nephrostomy to relieve hydronephrosis. Which intervention is most important for this patient? a. Assist the patient with turning every 2 hours. b. Irrigate the nephrostomy tube once per shift. c. Assess urinary output from the left kidney. d. Keep the nephrostomy tube clamped. ANS: C The left kidney will take on increased renal metabolism and must be assessed constantly. While it is important for the patient to turn, positioning of the patient depends on the surgeon’s orders. Frequent turning and deep breathing may help prevent complications but monitoring the unaffected kidney is most important. A nephrostomy tube should never be irrigated or clamped without a specific provider’s order that defines the circumstances and the amount of irrigation fluid. PTS: 1 DIF: Cognitive Level: Analysis REF: 791 OBJ: 1 (clinical) TOP: Nephrostomy Tube: Nursing Responsibility KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 14. The nurse is caring for a 50-year-old female who presented to the emergency department after being involved in a motor vehicle collision. The patient displays marked tenderness and spasm in the suprapubic area and a nonpulsating mass. The nurse anticipates that this patient will undergo additional workup for which complication? a. Bladder trauma b. A damaged kidney c. A urethral tear d. Ruptured spleen ANS: A Bladder traumas signal themselves with pain, spasm, and a mass in the suprapubic area. These findings are not consistent with a damaged kidney, urethral tear, or splenic rupture. PTS: 1 DIF: Cognitive Level: Application REF: 794 OBJ: 1 (clinical) TOP: Bladder Injury: Signs and Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 15. The nurse is caring for patient who is postoperative after a bladder repair. The patient complains of pain. Which independent nursing intervention is best? a. Administer an analgesic medication. b. Apply a cold compress to the surgical site. c. Dim the lights in the room. d. Irrigate the drainage tube. ANS: B Cold application to the surgical site applies the best independent intervention. Dimming the lights may also help to create a more comfortable environment. Administering an analgesic and irrigating the drainage tube are interventions that require a physician’s order. PTS: 1 DIF: Cognitive Level: Analysis REF: 795 OBJ: 2 (clinical) TOP: Bladder Pain: Independent Interventions KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 16. The nurse is caring for a patient who received an instillation of doxorubicin (Adriamycin) into the bladder for treatment of cancer in situ. What should the nurse do next? a. Reposition the patient every 15 to 30 minutes. b. Unclamp the catheter. c. Educate the patient about the possibility of false positive tuberculin skin testing. d. Apply nonslip footwear for ambulation. ANS: A Doxorubicin (Adriamycin) has been found to help patients with bladder carcinoma in situ (site of origin) by reducing tumor recurrence and by eliminating residual malignant cells after surgery. The solution is instilled into the bladder via a urinary catheter. The patient should change position every 15 to 30 minutes, and the catheter is clamped for 2 hours. The nurse should not unclamp the catheter. While it is important to educate the patient about potential for positive PPD tests, education should be done at a time when the patient can focus on the information. Ambulation is not appropriate at this time. PTS: 1 DIF: Cognitive Level: Application REF: 795 OBJ: 1 (clinical) TOP: Intravesical Instillation: Nursing Management KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 17. The nurse is caring for a patient who is scheduled to undergo hemodialysis. Based on awareness of potential complications, the nurse correctly withholds which medication? a. Lisinopril (Zestril) b. Famotidine (Pepcid) c. Paroxetine (Paxil) d. Ciprofloxacin (Cipro) ANS: A Lisinopril is an ACE-inhibitor antihypertensive medication. Antihypertensive drugs are not given the morning of dialysis because they can cause severe hypotension during the treatment. Nitroglycerin (NTG) patches, digitalis, and anticoagulants also are held. The nurse should consult with the dialysis nurse to coordinate medication timing, but antacids (Pepcid), antianxeity agents (Paxil), and antibiotics (Cipro) do not need to be withheld. PTS: 1 DIF: Cognitive Level: Application REF: 806 OBJ: 4 (theory) TOP: Hemodialysis: Effect on Other Medications KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 18. The nurse is discussing alternative therapies with a patient who has cystitis. The patient asks the nurse if there are any dietary changes that might help. What response is most appropriate? a. “Drinking lots of water is the only dietary change that would help.” b. “Many rumors exist about dietary prevention of UTIs but none are proven at this time.” c. “Vitamin C may help decrease the frequency of cystitis.” d. “Increase the amount of leafy green vegetables in your daily diet.” ANS: C Vitamin C can help acidify the urine and decrease the frequency of cystitis. Drinking increased amount of water is very helpful, but it isn’t the only intervention to avoid a UTI. Evidence indicates that certain foods and drinks may be helpful preventative measures for UTI, like cranberries or cranberry juice. Leafy green vegetables are not considered a preventative food for UTIs. PTS: 1 DIF: Cognitive Level: Application REF: 788 OBJ: 1 (theory) TOP: Cystitis: Alternative and Complementary Therapies: Vitamin C KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Health Maintenance and Promotion 19. The nurse is assessing a patient who is being treated for acute pyelonephritis. When finding best indicates to the nurse that the patient is in the early stages of pyelonephritis? a. Smoky-colored urine b. Temperature of 99.4° F c. Weakness d. Flank pain ANS: D In the acute state of pyelonephritis, symptoms include pain in the flank (lateral abdomen) that radiates to the thigh and genitalia, fever (often 103° F+), chills, headache, malaise, and nausea and vomiting. The urine is cloudy with a foul odor as it is loaded with bacteria, blood, and pus. The chronic phase is often subtle, with low-grade fever, weakness, weight loss, and gradual scarring of the kidney tissues. PTS: 1 DIF: Cognitive Level: Analysis REF: 788 OBJ: 1 (theory) TOP: Pyelonephritis: Signs and Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 20. The nurse is caring for a child suspected of having acute glomerulonephritis. When reviewing the health history, which finding is most concerning to the nurse? a. Recent upper respiratory infection b. Recent outpatient surgery c. History of asthma d. Recent history of gastroenteritis ANS: A Glomerulonephritis is primarily seen in children and young adults, and affects males more than females. It most commonly occurs about 2 to 3 weeks after a group A beta-hemolytic streptococcal infection, such as “strep throat” or impetigo; however, it can occur in response to bacterial, viral, or parasitic infections elsewhere in the body. Outpatient surgery, asthma, and gastroenteritis are not risk factors for glomerulonephritis. PTS: 1 DIF: Cognitive Level: Application REF: 789 OBJ: 2 (theory) TOP: Acute Glomerulonephritis: Etiology and Pathophysiology KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation MULTIPLE RESPONSE 21. In which situation(s) should the nurse question an order for carbenicillin for a patient with a urinary infection? (select all that apply.) a. The patient is older than 80 years of age. b. The patient is allergic to penicillin. c. The patient takes warfarin daily. d. The patient takes oral contraceptives. e. The patient has a history of hypertension. ANS: B, C, D Carbenicillin is an extended-spectrum penicillin medication. It interferes with the effectiveness of oral birth control medication and warfarin and should not be given to people allergic to penicillin. Age and a history of hypertension are not contraindications to carbenicillin. PTS: 1 DIF: Cognitive Level: Application REF: 787, Table 34-1 OBJ: 1 (theory) TOP: Carbenicillin: Contraindications KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 22. The nurse is caring for patient with a urinary tract infection (UTI) who is to receive cefazolin (Ancef). The nurse should carefully monitor the patient for which side effect(s)? (select all that apply.) a. Vaginitis b. Decreased clotting time c. Arrhythmias d. Rash e. Confusion ANS: A, C, D, E Cefazolin (Ancef) may cause vaginitis, arrhythmias, a sunburn-like rash, and confusion. Cefazolin may increase clotting time. PTS: 1 DIF: Cognitive Level: Comprehension REF: 787, Table 34-1 OBJ: 1 (theory) TOP: UTI: Treatment with Ancef KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 23. A patient has been admitted to the acute care facility to rule out glomerulonephritis. Which assessment finding(s) is/are supportive of the potential diagnosis? (select all that apply.) a. Flank pain b. Hematuria c. Periorbital edema d. Decrease in blood urea nitrogen (BUN) and creatinine e. Hypertension ANS: A, B, C, E The patient with acute glomerulonephritis usually becomes suddenly ill with fever, chills, flank pain, widespread edema, puffiness about the eyes, visual disturbances, and marked hypertension. The urine may be smoky and will contain red blood cells and protein, and urine will have an increased specific gravity. Serum creatinine and BUN levels rise above normal rather than decrease. Diagnosis is based on physical findings. PTS: 1 DIF: Cognitive Level: Application REF: 789 OBJ: 2 (theory) TOP: Glomerulonephritis: Signs and Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 24. The nurse is caring for a patient who is undergoing plasmapheresis. The nurse should carefully monitor the patient for which potential complication(s)? (select all that apply.) a. An allergic reaction b. Bleeding at the puncture site c. A bruit at the shunt site d. Decreasing blood pressure e. Signs of hyperkalemia ANS: B, C, D, E Plasmapheresis is a therapy used in autoimmune disorders, such as acute glomerulonephritis or myasthenia gravis. It removes the autoantibodies causing the disease. This procedure can be done at the bedside by a trained technician with specialized equipment. The patient’s blood is accessed through a shunt or a central IV catheter and the blood components are separated from the plasma by filtration or centrifuge. Then, the cellular components are returned to the patient and the plasma is replaced with a fluid such as normal saline or albumin. Assessment for bleeding at puncture site, bruits, hypotension, and electrolyte imbalances is essential. Allergic reactions are not anticipated. PTS: 1 DIF: Cognitive Level: Application REF: 789 OBJ: 2 (theory) TOP: Plasmapheresis: Nursing Responsibility KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 25. The nurse is collecting the health history of a patient who has had multiple episodes of renal calculi formation. Which finding(s) increase(s) the patient’s risk for the development of renal calculi? (select all that apply.) a. Uric acid crystals in urine b. Frequent bacterial urinary infections c. Excessive fluid intake d. Prolonged bed rest e. Parathyroid gland tumor ANS: A, B, C, D, E Risk factors for development of renal calculi include uric acid crystals in urine, frequent bacterial urinary infections, prolonged immobility or bed rest, and a parathyroid gland tumor. Another risk factor includes inadequate fluid intake. PTS: 1 DIF: Cognitive Level: Application REF: 792 OBJ: 1 (clinical) TOP: Renal Calculi: Risks KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 26. The home health nurse is caring for a patient with chronic renal failure. Which assessment finding(s) indicate(s) that the patient is experiencing uremic syndrome? (select all that apply.) a. Restless legs b. Dry, scaly skin c. Crystals in the eyebrows d. Muscle cramps e. Hypotension ANS: A, B, C, D Uremia or uremic syndrome signs generally appear when blood urea nitrogen (BUN) concentration passes 100 mg/dL. Complaints about restless legs syndrome are frequent, and the leg discomfort may interfere with sleep. The skin becomes dry, scaly, and a pallid yellowish gray. Uremic frost (a late sign) appears as evaporated sweat leaves urea crystals on the eyebrows. Calcium is not absorbed from the intestinal tract, and this leads to the loss of calcium from the body and a corresponding drop in serum calcium. If the hypocalcemia is not corrected, the patient will eventually suffer from muscle cramps, twitching, and possibly seizures. The patient is usually hypertensive rather than hypotensive. PTS: 1 DIF: Cognitive Level: Application REF: 802 OBJ: 5 (clinical) TOP: Uremic Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 27. The nurse caring for a patient who has just had an arteriovenous (AV) access created in his right forearm. Which finding(s) is/are important for the nurse to assess? (select all that apply.) a. Presence of bruit on auscultation of the AV site b. Capillary refill in the left hand c. Blood pressure in the right arm d. Adequate elevation of the right arm e. Abdominal incision site ANS: A, B, D The nurse should auscultate for a bruit, assess capillary refill times in both hands, and ensure that the right arm is elevated properly. The nurse should not take the patient’s blood pressure in the affected (right) arm, and this procedure does not result in an abdominal incision. PTS: 1 DIF: Cognitive Level: Comprehension REF: 805 OBJ: 4 (theory) TOP: AV Access: Nursing Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort COMPLETION 28. The nurse is aware that 80% of UTIs in females are the result of contamination from __________. ANS: Escherichia coli E. coli Escherichia coli E. coli Proximity of the urethral meatus to the anus makes contamination with Escherichia coli a frequent cause of infections. PTS: 1 DIF: Cognitive Level: Knowledge REF: 785 OBJ: 1 (theory) TOP: UTI: Etiology KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease MATCHING The nurse associates the types of acute renal failure with their probable cause to enhance the patient’s understanding. Match the type of acute renal failure (ARF) with its probable cause: (The options can be used once, more than once, or not at all.) a. Prerenal ARF b. Intrarenal ARF c. Postrenal ARF 29. Hypovolemic shock 30. Vascular changes related to diabetes mellitus 31. Ureteral obstruction 32. Prostate hypertrophy 33. Cardiogenic shock 29. ANS: A PTS: 1 DIF: Cognitive Level: Comprehension REF: 799 OBJ: 4 (clinical) TOP: Types of Renal Failure: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 30. ANS: B PTS: 1 DIF: Cognitive Level: Comprehension REF: 799 OBJ: 4 (clinical) TOP: Types of Renal Failure: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 31. ANS: C PTS: 1 DIF: Cognitive Level: Comprehension REF: 799 OBJ: 4 (clinical) TOP: Types of Renal Failure: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 32. ANS: C PTS: 1 DIF: Cognitive Level: Comprehension REF: 799 OBJ: 4 (clinical) TOP: Types of Renal Failure: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 33. ANS: A PTS: 1 DIF: Cognitive Level: Comprehension REF: 799 OBJ: 4 (clinical) TOP: Types of Renal Failure: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance Chapter 35: The Endocrine System deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. Intake of which nutrients directly impacts thyroid hormone production? a. Protein and iodine b. Fats and vitamins c. Carbohydrates and minerals d. Sodium and potassium ANS: A The production of thyroid hormone is dependent on the intake of protein and iodine. PTS: 1 DIF: Cognitive Level: Comprehension REF: 821 OBJ: 2 (theory) TOP: Thyroid Hormone Production KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. Which hormone acts on bone to release calcium into the blood? a. Thyroxine (T4) b. Thyrocalcitonin c. Triiodothyronine (T3) d. Parathormone ANS: D Parathormone, or parathyroid hormone, is produced and secreted by the parathyroid glands. Low calcium levels will stimulate release of parathormone, which increases the plasma level of calcium. Parathormone acts on the renal tubules to increase the excretion of phosphorus in the urine and to stimulate the reabsorption of calcium. Parathormone also acts on bone, causing the release of calcium from the bone into the bloodstream. PTS: 1 DIF: Cognitive Level: Comprehension REF: 821 OBJ: 2 (theory) TOP: Parathormone: Function KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. Which gland secretes epinephrine and norepinephrine? a. Thyroid b. Pituitary c. Pancreas d. Adrenal medulla ANS: D The adrenal medulla secretes epinephrine and norepinephrine. PTS: 1 DIF: Cognitive Level: Knowledge REF: 821, Table 35-1 OBJ: 2 (theory) TOP: Adrenal Medulla: Secretions KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. Where in the body are mineralocorticoids and glucocorticoids produced? a. Adrenal cortex b. Adrenal medulla c. Pancreas d. Hypothalamus ANS: A Mineralocorticoids and glucocorticoids are the products of the adrenal cortex. PTS: 1 DIF: Cognitive Level: Knowledge REF: 821, Table 35-1 OBJ: 2 (theory) TOP: Adrenal Cortex: Secretions KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. Which gland secretes androgenic hormones? a. Adrenal cortex b. Hypothalamus c. Pancreas d. Pituitary ANS: A The adrenal cortex secretes the androgenic hormones. PTS: 1 DIF: Cognitive Level: Knowledge REF: 823 OBJ: 2 (theory) TOP: Androgenic Hormones: Origin KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 6. Which action describes a function of aldosterone? a. Conserve water b. Excrete sodium c. Constrict blood vessels d. Excrete phosphorus ANS: A Aldosterone is classified as a mineralocorticoid. It promotes conservation of water by acting on the kidneys to retain sodium in exchange for potassium, which is excreted in the urine. PTS: 1 DIF: Cognitive Level: Comprehension REF: 823 OBJ: 2 (theory) TOP: Aldosterone: Function KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 7. Which corticoid counteracts the inflammatory response? a. Thyroxine b. Cortisol c. Insulin d. Norepinephrine ANS: B Cortisol is the corticoid that counteracts the inflammatory process. Thyroxine is secreted by the thyroid gland. Insulin is secreted by the beta cells of the pancreas. It is responsible for regulation of blood glucose levels. Norepinephrine is secreted by the adrenal medulla in response to stimulation from the sympathetic nervous system. It functions as a pressor (causing blood vessel constriction) hormone to maintain blood pressure. PTS: 1 DIF: Cognitive Level: Comprehension REF: 824 OBJ: 2 (theory) TOP: Cortisol: Function KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 8. Which gland is the only gland that is both an endocrine gland and an exocrine gland? a. Thyroid b. Hypothalamus c. Pancreas d. Parathyroid ANS: C The pancreas acts as an endocrine gland, secreting insulin directly into the bloodstream, and an exocrine gland, secreting digestive enzymes through ducts. PTS: 1 DIF: Cognitive Level: Knowledge REF: 824 OBJ: 2 (theory) TOP: Pancreas KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 9. Which statement accurately describes endocrine glands? a. Endocrine glands release secretions directly into the bloodstream. b. Endocrine glands release secretions via a duct into the bloodstream. c. Endocrine glands hold secretions in a reservoir until needed. d. Endocrine glands can produce constantly for body needs. ANS: A Endocrine glands secrete directly into the bloodstream, whereas exocrine glands secrete via a duct. PTS: 1 DIF: Cognitive Level: Comprehension REF: 824 OBJ: 2 (theory) TOP: Endocrine vs. Exocrine KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 10. The nurse is caring for a patient who has been experiencing infertility. Which statement indicates that the patient understands the impact of inadequate luteinizing hormone (LH) levels? a. “Since luteinizing hormone maintains my secondary sex characteristics, low levels explain my small breasts.” b. “Low levels of luteinizing hormone cause the swelling I experience during my menstrual cycle.” c. “Low levels of luteinizing hormone cause my menstrual cycle irregularities.” d. “Since luteinizing hormone stimulates ovulation and progesterone production, low levels could cause infertility.” ANS: D LH is produced by the anterior pituitary gland. It targets the ovaries. LH stimulates ovulation and production of progesterone. LH does not affect maintenance of secondary sex characteristics, fluid retention, or menstrual cycle regularity. PTS: 1 DIF: Cognitive Level: Application REF: 820 OBJ: 2 (theory) TOP: LH: Function KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 11. The nurse is caring for an 80-year-old patient with a history of type 2 diabetes and hypothyroidism. The physician wants to evaluate the patient’s blood glucose levels and orders a fructosamine assay. Which factor best explains why the physician chose this laboratory test instead a glycosylated hemoglobin (HbA1c) test? a. The patient’s age b. Type 2 diabetes c. Hypothyroidism d. The tests’ costs ANS: B The fructosamine assay is a diagnostic test used to assess the degree of diabetic control of blood sugar over the preceding 2- to 3- week period. The fructosamine assay is a better tool for the older adult as it is less influenced by age. The fructosamine assay is not specific to type 1or type 2 diabetes. Its accuracy is not affected by hypothyroidism. While the fructosamine assay is simpler and cheaper than an HbA1c test, the accuracy of results for this patient takes priority. PTS: 1 DIF: Cognitive Level: Comprehension REF: 829, Table 35-3 OBJ: 4 (theory) TOP: Fructosamine Assay KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 12. The nurse is caring for a patient who is scheduled to undergo a glucose tolerance test next week. The patient’s daily medications include an antihypertensive, oral contraceptives, and over-the-counter (OTC) vitamin C and calcium supplements. The nurse should instruct the patient to withhold which medication before the test? a. Antihypertensive agent b. Oral contraceptive c. Vitamin C d. Calcium supplement ANS: B Birth control pills will affect the reliability of the glucose tolerance test and should be withheld. Antihypertensive agents, vitamin C, and calcium supplements do not affect the reliability of glucose screening tests. PTS: 1 DIF: Cognitive Level: Application REF: 829, Table 35-3 OBJ: 4 (theory) TOP: Glucose Tolerance Test: Preprocedure Instructions KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 13. The nurse is caring for a patient who has orders for a 17-ketosteroid (17-KS) test. Which preparation is most important for the nurse to make? a. Keep the patient NPO after midnight the night before the test. b. Ensure adequate space for the specimen container is available in the refrigerator. c. Withhold the patient’s metformin for 24 hours prior to the test. d. Request an order for an antacid. ANS: B The 17-KS test is used to determine the amount of androgen metabolites in the urine and requires a 24-hour urine collection. The urine collection container must be kept chilled, so the nurse should ensure that adequate space is available in the specimen refrigerator. This test does not require the patient to fast. The nurse should consult with the physician and laboratory regarding the patient’s medications but should not withhold any without orders. Antacids will not alter the test results. PTS: 1 DIF: Cognitive Level: Application REF: 828, Table 35-2 OBJ: 4 (theory) TOP: 17-KS Test KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 14. The nurse is caring for a long-term diabetic patient with a glycosylated hemoglobin (HbA1c) level of 5%. Which statement indicates that the patient understands this laboratory result? a. “My hemoglobin A levels are excellent.” b. “I am anemic and may need a blood transfusion.” c. “I should meet with the dietician to discuss better food choices.” d. “My glucose control has been excellent for the last few weeks.” ANS: D The hemoglobin A1c (A1C) test (formerly called the glycosylated hemoglobin test) measures blood glucose over a period of many weeks. Glucose in the bloodstream attaches itself to the hemoglobin A (red blood cell) molecule and remains there for the life span of the red blood cell. Physicians use A1C test results to prescribe adjustments to a patient’s treatment program for managing diabetes. Results of 4.9% to 6.7% are considered excellent results. Good results are between 7.6% and 8.5%. Fair results are between 9.4% and 10.0%. Poor control is considered between 12.1% and 13.0%. PTS: 1 DIF: Cognitive Level: Application REF: 828, Table 35-2 OBJ: 4 (theory) TOP: A1C Test Results KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 15. Which actual structural unit secretes insulin? a. Pancreas b. Islets of Langerhans c. Beta cell d. Alpha cell ANS: C The actual structural unit that secretes insulin is the beta cell. Beta cells are found on the islets of Langerhans, which are in the pancreas. PTS: 1 DIF: Cognitive Level: Knowledge REF: 819 OBJ: 1 (theory) TOP: Insulin: Source KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 16. The nurse is caring for a patient who is scheduled to have a thyroid panel drawn next week. After confirming with physician, which information is most important for the nurse to include in the patient instructions? a. Do not take aspirin for 2 days before the test. b. Take an OTC antacid 30 minutes before the test. c. Take the preprocedure diuretic 30 minutes before the test. d. Do not take any multivitamins for 2 days before the test. ANS: A Aspirin, iodine-containing medications, contrast media, and other drugs may affect result. To ensure an accurate test result, aspirin should be avoided for 2 days before testing. Birth control pills also will alter the test results. Antacids, diuretics, and multivitamins do not affect the results of a thyroid panel. PTS: 1 DIF: Cognitive Level: Comprehension REF: 826 OBJ: 1 (clinical) TOP: Thyroid Panel: Preprocedure Instructions KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 17. Although thyroid hormone levels decrease with advancing age, which mechanism offsets this output reduction? a. Decreased rate of thyroid hormone breakdown b. Increased level of calcium c. Increased level of phosphorus d. Decreased mineralocorticoids ANS: A The production of thyroid hormones decreases with age, but the decrease is offset by a matching decrease in the body’s breakdown of the hormone. Changes in thyroid hormone levels are not affected by calcium, phosphorus, or mineralocorticoid levels. PTS: 1 DIF: Cognitive Level: Comprehension REF: 825 OBJ: 2 (theory) TOP: Age-Related Changes: Thyroxine Level Decrease KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 18. The nurse is educating an older adult patient with reduced cortisol levels. Which statement indicates that the patient accurately understands the nurse’s teaching? a. “I should avoid crowds because low cortisol levels weaken my immune system.” b. “I should keep stress to a minimum because low cortisol levels make it harder for my body to deal with stress.” c. “I should avoid hot climates because low cortisol levels impact temperature regulation.” d. “I should avoid salty foods because low cortisol levels keep my body from processing sodium.” ANS: B Cortisol is a mineralocorticoid produced by the adrenal glands. Cortisol acts to increase glucose levels in the blood. Cortisol also helps counteract the inflammatory response. The reduced production of cortisol hinders the older adult in dealing with stress. PTS: 1 DIF: Cognitive Level: Application REF: 827, Table 35-2 OBJ: 2 (theory) TOP: Cortisol: Function KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 19. If an endocrine gland begins to hypersecrete, it usually causes which result? a. Hyperplasia b. Activation of the inflammatory process c. An allergic response d. An autoimmune response ANS: A Hyperplasia (increased cellular growth) is the usual cause of hypersecretion of an endocrine gland. PTS: 1 DIF: Cognitive Level: Knowledge REF: 825 OBJ: 2 (theory) TOP: Hypersecretion: Cause KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 20. The nurse is caring for a patient who is scheduled to undergo a computed tomography (CT) scan with contrast within the hour. Which statement requires the nurse’s immediate attention? a. “I forgot that I was not supposed to eat anything.” b. “I left my potassium supplements off of my home medication list.” c. “Did I tell you that I cannot eat lobster?” d. “I take my daily blood pressure medication at night.” ANS: C Before administering tests that involve contrast media, the nurse must ask about allergies to iodine or shellfish. An allergy to either of these may indicate that an individual is hypersensitive to contrast media. PTS: 1 DIF: Cognitive Level: Application REF: 827-828, Table 35-2 OBJ: 4 (clinical) TOP: Diagnostic Tests and Procedures KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 21. The physician has ordered cortisol level testing for a patient. Which statement indicates that the patient accurately understands the nurse’s teaching? a. “I should not eat or drink 6 hours before the procedure.” b. “I should exercise for at least 10 minutes during the test.” c. “I will have blood samples collected during the day and night.” d. “I should limit salty foods the day before the test.” ANS: C Cortisol levels are collected during both the day and night to take into account alterations associated with circadian rhythms. The laboratory test does not require the patient to be fasting. Increases in activity levels may promote stress and alter the test results. Dietary intake will not affect the test results. PTS: 1 DIF: Cognitive Level: Application REF: 827, Table 35-2 OBJ: 2 (clinical) TOP: Diagnostic Tests and Procedures of the Endocrine System KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 22. The nurse is caring for a patient undergoing the fluid deprivation test. This test is designed to confirm which condition? a. Diabetes insipidus b. Diabetes mellitus c. Hypothyroidism d. Hyperparathyroidism ANS: A The fluid deprivation test is used to assess for the presence of diabetes insipidus. PTS: 1 DIF: Cognitive Level: Knowledge REF: 828, Table 35-2 OBJ: 4 (theory) TOP: Diagnostic Tests and Procedures of the Endocrine System KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease MULTIPLE RESPONSE 23. Which hormone(s) does the anterior pituitary secrete? (select all that apply.) a. Growth hormone (GH) b. Thyroid-stimulating hormone (TSH) c. Antidiuretic hormone (ADH) d. Follicle-stimulating hormone (FSH) e. Luteinizing hormone (LH) ANS: A, B, D, E The anterior pituitary secretes GH, TSH, FSH, and LH. The posterior pituitary secretes ADH. PTS: 1 DIF: Cognitive Level: Knowledge REF: 820, Table 35-1 OBJ: 2 (theory) TOP: Anterior Pituitary Hormones KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 24. Which change(s) in endocrine function can be attributed to age? (select all that apply.) a. Pituitary enlargement b. Declining metabolism c. Rising blood glucose levels d. Decreasing epinephrine levels e. Decreasing thyroxine levels ANS: B, C, D, E Age-related endocrine functions include declining metabolism, rising blood glucose levels, and decreasing levels of epinephrine and thyroxine. Aging causes the pituitary gland to become smaller. PTS: 1 DIF: Cognitive Level: Comprehension REF: 824-825 OBJ: 3 (theory) TOP: Age-Related Changes in Endocrine Function KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 25. In which body process(es) is/are the endocrine system involved? (select all that apply.) a. Regulation of metabolism b. Growth rate c. Physical development d. Sexual function e. Reproductive process ANS: A, B, C, D, E All functions listed are affected or controlled by the pituitary gland. PTS: 1 DIF: Cognitive Level: Knowledge REF: 820-821, 825 OBJ: 2 (theory) TOP: Endocrine System: Functions KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 26. Which causative factor(s) may be responsible for primary endocrine disorders? (select all that apply.) a. Hormone overproduction b. Long periods of limited mobility c. Trauma d. Severe infection e. Effects of certain drugs ANS: A, D Endocrine disorders are caused by an imbalance in the production of hormone or by an alteration in the body’s ability to use the hormones produced. Primary endocrine dysfunction means that an endocrine gland is either oversecreting or undersecreting hormone(s). Tumor or hyperplasia of the endocrine gland may lead to hypersecretion. Infection, mechanical damage, or an autoimmune response may be an inflammatory response in a gland and lead to hyposecretion. Secondary endocrine dysfunction occurs from factors outside the gland itself. Medications, trauma, hormone therapy, and other factors may cause secondary dysfunction. Long periods of limited mobility do not cause endocrine disorders. PTS: 1 DIF: Cognitive Level: Comprehension REF: 825 OBJ: 2 (theory) TOP: Primary Endocrine Disorders: Etiology KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation COMPLETION 27. The nurse explains that, when the target tissue signals that the need for a specific hormone is satisfied, the endocrine gland inhibits the secretion. This process is called _____________. ANS: negative feedback Negative feedback is the process by which the target tissue signals the endocrine gland that the hormone supply is adequate. PTS: 1 DIF: Cognitive Level: Comprehension REF: 825 OBJ: 2 (theory) TOP: Negative Feedback: Process KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation Chapter 36: Care of Patients with Pituitary, Thyroid, Parathyroid, and Adrenal Disorders deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. Pituitary adenoma antagonizes insulin. This benign tumor results in which imbalance? a. Hyperinsulinism b. Hyperglycemia c. Hypopituitarism d. Hypoglycemia ANS: B The tumor interferes with the effectiveness of insulin, resulting in hyperglycemia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 855, Key Points OBJ: 1 (clinical) TOP: Pituitary Tumor: Effects KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. A patient who had a hypophysectomy 3 days ago begins to have 3000 mL of urine output every shift and complains of thirst and a dry mouth. Which problem does the nurse suspect? a. Overreaction to diuretics b. Diabetes insipidus (DI) c. Diabetes mellitus d. Glucose intolerance ANS: B DI is a complication of a hypophysectomy. The posterior lobe of the pituitary gland controls urinary output; when this portion of the pituitary is removed or damaged, there is no secretion of antidiuretic hormone to stop excessive urine output. PTS: 1 DIF: Cognitive Level: Application REF: 835 OBJ: 4 (clinical) TOP: Hypophysectomy: Complication KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 3. A patient with central diabetes insipidus (DI) likely has which occurrence as part of his health history? a. Brain surgery to remove a tumor b. A kidney disorder c. Water addiction d. A thyroid disorder ANS: A Central DI is caused by insult to the pituitary that results from a brain injury or invasive brain surgery. Kidney disorders, water addiction, and thyroid disorders do not cause central DI. PTS: 1 DIF: Cognitive Level: Comprehension REF: 837 OBJ: 6 (clinical) TOP: DI: Central Type KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. The nurse is aware that the severe dehydration associated with diabetes insipidus (DI) can lead which serious electrolyte imbalance? a. Hypercalcemia b. Hypernatremia c. Hypocalcemia d. Hyperkalemia ANS: B The loss of potassium in the large volume of urine depletes the compensatory mechanisms and hypernatremia results. PTS: 1 DIF: Cognitive Level: Comprehension REF: 837 OBJ: 6 (clinical) TOP: DI: Complication KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. The nurse is educating a patient with a simple goiter. Which statement indicates that the patient needs additional instruction? a. “The lump on my throat is my enlarged thyroid.” b. “Treatment stops enlargement of the goiter.” c. “I am aware this goiter could develop into cancer.” d. “I’m glad my treatment will make this thing go away.” ANS: D Treatment usually arrests the growth of the goiter but usually does not diminish the size of the growth unless diagnosis is made early in the disease before growth has become excessive. PTS: 1 DIF: Cognitive Level: Comprehension REF: 839-840 OBJ: 1 (theory) TOP: Goiter KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 6. The nurse is caring for a patient with a goiter. The nurse correctly uses which technique to administer potassium iodide solution? a. Pour the solution over ice to increase palatability. b. Dilute the solution and administer it through a straw. c. Administer the solution on an empty stomach. d. Mix the solution with an antacid to reduce gastric irritation. ANS: B The solution should be diluted and drunk through a straw to avoid staining of teeth. PTS: 1 DIF: Cognitive Level: Comprehension REF: 840 OBJ: 1 (theory) TOP: Iodine Solutions: Administration KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 7. The nurse is reviewing the health history of a patient. Which behavior is linked to increased probability of developing Grave disease? a. Smoking b. Long-term use of oral contraceptives c. Excessive alcohol consumption d. Use of St. John wort ANS: A Primary hyperthyroidism is also known as Grave disease or toxic goiter. Medications containing iodine, such as amiodarone (an antidysrhythmic heart medication), can predispose to hyperthyroidism. In addition, it has been discovered recently that people who smoke have nearly twice the risk of developing hyperthyroidism when compared with nonsmokers. PTS: 1 DIF: Cognitive Level: Comprehension REF: 840 OBJ: 1 (theory) TOP: Grave Disease: Risk Factors KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 8. The patient with hyperthyroidism is undergoing ablation therapy with radioactive iodine. Which precaution is most important for the nurse to employ? a. Take radioactive precautions with syringes and bedpans. b. Use Standard Precautions only. c. Enforce isolation for 3 days. d. Wear a mask and eye protectors when caring for patient. ANS: A Radioactive iodine (131I) circulates in the blood and is excreted by the kidneys, so radioactive precautions should be taken with any equipment contaminated with blood or urine. PTS: 1 DIF: Cognitive Level: Application REF: 841 OBJ: 1 (theory) TOP: Ablation Therapy: Care KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 9. The nurse is educating a patient who has a new prescription for methimazole (Tapazole). Which instruction is most important for the nurse to include? a. “Double the next medication dose if the previous dose is forgotten.” b. “Take the medication on a strict schedule.” c. “Ask the pharmacist for a less expensive generic substitute.” d. “The medication is approved for use in pregnant women.” ANS: B All replacement hormone drugs should be taken on a strict schedule. Doubling up and taking a substitute drug interfere with the effectiveness of the therapy. Pregnant women should not take this drug because of risk for fetal damage. PTS: 1 DIF: Cognitive Level: Application REF: 841 OBJ: 1 (theory) TOP: Antithyroid Drugs: Instructions KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 10. Which statement accurately describes a subtotal thyroidectomy? a. It allows the patient to take minimum amounts of antithyroid drugs. b. It allows continued production and release of thyroid hormones from the remainder of the gland. c. It reduces exophthalmos. d. It poses less postoperative risk than a total thyroidectomy. ANS: B Patients who do not respond well to antithyroid drug therapy, who are unable to take radioactive iodine, or who have greatly enlarged thyroid glands are candidates for a subtotal thyroidectomy. In the subtotal procedure, two thirds of the glandular mass is removed. The remaining portion of the gland is left intact so production and release of thyroid hormone can continue. There is no need for antithyroid drugs, and the operative risks are the same. PTS: 1 DIF: Cognitive Level: Comprehension REF: 842 OBJ: 5 (clinical) TOP: Thyroidectomy: Subtotal KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 11. The husband of a patient with Grave disease confides that he is frustrated with his wife’s emotional outbursts and wide mood swings. How should the nurse respond? a. “I understand how you feel.” b. “Antithyroid drugs usually help regulate mood swings after a few weeks.” c. “I’m afraid this behavior will continue. How are you coping with it now?” d. “Have you told her how you feel?” ANS: B Reassurance that the signs and symptoms will improve with medication is helpful. The nurse may or may not understand how the patient feels, and this dismisses the husband’s concern. The behavior may or may not continue, and asking how the husband is coping or if he has shared his feelings are examples of nontherapeutic communication. PTS: 1 DIF: Cognitive Level: Application REF: 842 OBJ: 1 (theory) TOP: Grave Disease: Lability KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: Coping and Adaptation 12. The nurse is performing preoperative thyroidectomy instruction for a patient with Graves’ disease. The patient begins to cry and says, “I am so nervous and can’t listen to you. Just get out!” What should the nurse do next? a. Give the patient written preoperative instructions. b. Inform the charge nurse or surgeon of the patient’s behavior. c. Remind the patient the preoperative information is important. d. Ask the family member to explain the preoperative instructions. ANS: B Informing the charge nurse or surgeon will alert them to possible ineffective control of the thyroid, which can cause thyroid crisis postoperatively. The patient is not ready to read or listen to any instructions at this time, and instruction should not be deferred to a family member. PTS: 1 DIF: Cognitive Level: Application REF: 842 OBJ: 3 (theory) TOP: Grave Disease: Complication KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 13. The nurse is caring for patient who is 8 hours postoperative after a total thyroidectomy. The patient complains of muscle cramps, and the nurse assesses a positive Chvostek sign. The nurse correctly interprets that these findings indicate which complication? a. Imminent convulsions b. Hypoparathyroidism c. Hyperkalemia d. Thyroid storm ANS: B Hypoparathyroidism results when the parathyroid glands are removed during a total thyroidectomy. Chvostek sign (muscle irritability when the facial nerve is gently tapped) is consistent with hypocalcemia that occurs secondary to the removal of the parathyroid glands. PTS: 1 DIF: Cognitive Level: Application REF: 847 OBJ: 3 (theory) TOP: Hypoparathyroidism KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 14. The nurse is caring for a patient who reports abruptly discontinuing his prescribed levothyroxine. The nurse should carefully monitor the patient for which complication? a. Seizures b. Extreme diarrhea c. Sudden hypertension d. Respiratory distress ANS: D Abruptly stopping hormone replacement can cause the patient to go into myxedema coma. Signs and symptoms of myxedema coma include dizziness, respiratory distress, low blood sugar, or hypothermia. Discontinuation of levothyroxine should not cause seizures, diarrhea, or sudden hypertension. PTS: 1 DIF: Cognitive Level: Application REF: 846 OBJ: 3 (clinical) TOP: Myxedema Coma: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 15. A nurse is teaching a patient with Addison disease who has a prescription for corticosteroids. Which statement is most important for the nurse to include in the teaching plan? a. Take the medication every day. b. Take the medication on an empty stomach. c. Stop the medication if gastrointestinal symptoms appear. d. Double the medication during stressful events. ANS: A Corticosteroids should be taken every day. Corticosteroids should be administered with food. The medications should not be abruptly discontinued. To provide appropriate serum medication levels, they are not to be doubled or altered without physician consultation. PTS: 1 DIF: Cognitive Level: Comprehension REF: 852 OBJ: 2 (clinical) TOP: Corticosteroids KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 16. The patient with Addison disease is receiving IV fluids for rehydration. The nurse should carefully monitor the patient for which potential problem? a. Hypotension b. Hyperglycemia c. Hypokalemia d. Hypernatremia ANS: A The patient with Addison disease is at risk for an addisonian crisis. During an addisonian crisis, decreased levels of cortisol result in decreased sensitivity of the blood vessels to sympathetic stimulation. It is the sympathetic stimulation that maintains vascular tone. Lack of vascular tone causes vasodilation, producing hypotension. Addisonian crisis requires immediate fluid replacement therapy in order to prevent irreversible shock. Intravenous hydrocortisone is given along with sodium, fluids, and dextrose until blood pressure becomes stable. The hydrocortisone is then tapered off slowly. Hyperkalemia must also be addressed with insulin, Kayexalate, and loop diuretics, and by monitoring arrhythmias and the patient’s intake and output. Hypoglycemia is treated with IV glucose and with glucagon as needed; blood glucose is monitored every hour. PTS: 1 DIF: Cognitive Level: Comprehension REF: 852 OBJ: 5 (theory) TOP: Addisonian Crisis: Nursing Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 17. The nurse is preparing a patient to undergo a dexamethasone suppression test. Which action is most appropriate? a. Instruct the patient to be NPO 6 hours before the test. b. Instruct the patient that urine levels will be assessed after a 24-hour collection period. c. Administer a steroid the morning of the test. d. Instruct the patient that a blood specimen will be collected in the morning. ANS: D When assessing for Cushing disease cortisol levels are evaluated. If elevated cortisol levels are noted, a dexamethasone suppression test should be ordered. In preparation for the test, the patient is given a steroid at night, and blood and urine cortisol levels are then measured in the morning. PTS: 1 DIF: Cognitive Level: Application REF: 853 OBJ: 5 (theory) TOP: Cushing Disease: Diagnosis KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 18. The nurse is caring for a patient scheduled for a thyroidectomy. Which instruction should be included in the preoperative care? a. Avoid salt for 2 weeks prior to surgery. b. Preoperative medications will include drugs to increase the vascularity of the gland. c. Keep a food diary for 2 weeks prior to surgery. d. Preoperative medications will be given 2 weeks before surgery to reduce the vascularity of the gland. ANS: D Iodine preparations may be given for a period of 10 to 14 days before surgery of the thyroid to reduce the vascularity of the gland, minimizing the danger of releasing large amounts of thyroid hormone into the bloodstream during surgery, and to decrease the risk of hemorrhage. PTS: 1 DIF: Cognitive Level: Comprehension REF: 841 OBJ: 3 (theory) TOP: Hyperthyroidism: Medication Safety Alert KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease MULTIPLE RESPONSE 19. Which manifestations occur with a benign pituitary adenoma? (select all that apply.) a. Gigantism in children b. Acromegaly in adults c. Muscle weakness d. Excessive hair growth e. Joint pain ANS: A, B, C, E A benign pituitary adenoma may cause gigantism in children, acromegaly in adults, muscle weakness, and joint pain. A benign pituitary adenoma does not cause excessive hair growth (hirsutism). PTS: 1 DIF: Cognitive Level: Comprehension REF: 835 OBJ: 1 (clinical) TOP: Pituitary Tumor: Effects KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 20. The nurse planning the postoperative instructions for the patient who will undergo a hypophysectomy. Which information is most important for the nurse to include? (select all that apply.) a. A drip pad will be placed under your nose. b. Avoid brushing your teeth. c. Avoid raising your arms above your head. d. Breathe through your mouth. e. Avoid blowing your nose. ANS: A, B, D, E Removal of the pituitary gland is most often done microsurgically. The usual approach is transsphenoidal via the nose or at the junction of the gums and upper lip, and a nasal drip pad is placed. After surgery it is important that the patient not brush his teeth, cough, sneeze, blow his nose, or bend forward, as these may interfere with the healing process. The patient is allowed to raise his arms above his head. PTS: 1 DIF: Cognitive Level: Application REF: 835 OBJ: 4 (clinical) TOP: Hypophysectomy: Postoperative Instructions KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 21. The nurse is planning care for a patient with diabetes insipidus (DI). Which outcomes are important for the nurse to include? (select all that apply.) a. Maintain fluid therapy. b. Conserve energy. c. Supporting dietary choices to reduce diarrhea. d. Assess for bradycardia. e. Encouraging exercise to reduce weight. ANS: A, B, D Goals for the patient with DI should include fluid therapy maintenance, energy conservation, and assessment for bradycardia. DI patients are often constipated and frail from weight loss. PTS: 1 DIF: Cognitive Level: Application REF: 837-838 OBJ: 1 (theory) TOP: DI: Signs and Symptoms KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 22. A tumor of the pituitary has caused the syndrome of inappropriate secretion of antidiuretic hormone (SIADH). Which interventions should the nurse plan? (select all that apply.) a. Assist with activities of daily living. b. Record accurate urine. c. Weigh the patient daily. d. Assess for changes in level of consciousness. e. Assess stools for occult blood. ANS: A, B, C, D The nurse should assist with activities of daily living because of weakness, record accurate urine output because of oliguria, weigh the patient daily to assess fluid volume status, and assess for changes in level of consciousness. There is no overt threat of a GI bleed with SIADH, so assessing stools for occult blood is not indicated. PTS: 1 DIF: Cognitive Level: Application REF: 838 OBJ: 1 (clinical) TOP: SIADH: Care KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 23. Which classic signs and symptoms are manifestations of hyperthyroidism? (select all that apply.) a. Tremulousness b. Bradycardia c. Exertional dyspnea d. Scanty menstruation e. Increased thirst and urination ANS: A, C, D, E Manifestations of hyperthyroidism include tremulousness, exertional dyspnea, scanty menstruation, and increased thirst and urination. Hyperthyroidism causes tachycardia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 840 OBJ: 1 (theory) TOP: Hyperthyroidism: Classic Signs and Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 24. Which interventions are indicated for the immediate postoperative care of a person after a thyroidectomy? (select all that apply.) a. Placing the patient in semi-Fowler position. b. Supporting the head with sandbags. c. Assess vital signs hourly. d. Assess the patient’s ability to swallow. e. Assess for bleeding. ANS: B, D, E Immediate postoperative care of a person who had a total thyroidectomy includes supporting the head with sandbags, and assessing the patient’s ability to swallow, and monitoring for bleeding. The patient should be placed in high Fowler position and vital signs should be assessed every 15 minutes. PTS: 1 DIF: Cognitive Level: Application REF: 842 OBJ: 5 (clinical) TOP: Thyroidectomy: Postoperative Care KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 25. On the first postoperative day following a total thyroidectomy, which finding(s) would lead the nurse to suspect that the patient may be developing a thyroid storm? (select all that apply.) a. Temperature of 101.8° F b. Pulse of 58 beats/min c. Brief attention span d. Apprehension and restlessness e. Respiratory rate of 12 breaths/min ANS: A, C, D Rising temperature, a brief attention span, and apprehension with restlessness would indicate a developing thyroid storm. Increasing pulse and respirations are other manifestations of thyroid storm. PTS: 1 DIF: Cognitive Level: Application REF: 847-848 OBJ: 3 (theory) TOP: Thyroid Storm: Signs and Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 26. The nurse is evaluating the laboratory results of a patient suspected of having hyperparathyroidism. Which finding(s) would be consistent with this condition? (select all that apply.) a. Anorexia b. Decreased serum phosphate levels c. Diarrhea d. Agitation e. Increased serum calcium levels ANS: A, B, E Hyperparathyroidism would result in anorexia, low serum phosphate, and increased serum calcium. Hyperparathyroidism would cause constipation rather than diarrhea and lethargy rather than agitation. PTS: 1 DIF: Cognitive Level: Analysis REF: 847 OBJ: 4 (theory) TOP: Comparison of Hyperparathyroidism and Hypoparathyroidism KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease COMPLETION 27. The nurse’s major contribution to the care of a patient with Cushing syndrome is that of __________ and __________. ANS: education; support support, education Patients with Cushing syndrome have a frustrating time dealing with their own lability and fatigue. They need support and education and referral for assistance. PTS: 1 DIF: Cognitive Level: Comprehension REF: 855 OBJ: 6 (theory) TOP: Cushing Syndrome KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort MATCHING The nurse associates the pathophysiology to the signs of the condition it causes in the adult. Match the hormonal change to the symptom it would produce. a. Decreased growth hormone b. Increased thyroid hormone c. Decreased follicle-stimulating hormone d. Decreased thyroid hormone e. Increased antidiuretic hormone 28. Pathologic fractures 29. Weight gain, fatigue, and lethargy 30. Hyponatremia, edema 31. High metabolism rate 32. Menstrual irregularities 28. ANS: A PTS: 1 DIF: Cognitive Level: Application REF: 836-838, 836, Table 36-1 OBJ: 1 (theory) TOP: Endocrine Disorders: Signs and Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 29. ANS: D PTS: 1 DIF: Cognitive Level: Application REF: 836-838, 836, Table 36-1 OBJ: 1 (theory) TOP: Endocrine Disorders: Signs and Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 30. ANS: E PTS: 1 DIF: Cognitive Level: Application REF: 836-838, 836, Table 36-1 OBJ: 1 (theory) TOP: Endocrine Disorders: Signs and Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 31. ANS: B PTS: 1 DIF: Cognitive Level: Application REF: 836-838, 836, Table 36-1 OBJ: 1 (theory) TOP: Endocrine Disorders: Signs and Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 32. ANS: C PTS: 1 DIF: Cognitive Level: Application REF: 836-838, 836, Table 36-1 OBJ: 1 (theory) TOP: Endocrine Disorders: Signs and Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation The nurse traces the closed loop of thyroid secretion. Place the events in appropriate order. a. Hypothalamus is activated. b. Pituitary releases thyroid-stimulating hormone (TSH). c. Drop in norepinephrine level. d. Thyroid releases thyroid hormone. e. Satisfaction of norepinephrine level signals hypothalamus in negative feedback. f. Thyrotropin-releasing hormone (TRH) is secreted. 33. Step 1 34. Step 2 35. Step 3 36. Step 4 37. Step 5 38. Step 6 33. ANS: C PTS: 1 DIF: Cognitive Level: Application REF: 836-838, 836, Table 36-1 OBJ: 1 (theory) TOP: Thyroid Hormone: Stimulation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 34. ANS: A PTS: 1 DIF: Cognitive Level: Application REF: 836-838, 836, Table 36-1 OBJ: 1 (theory) TOP: Thyroid Hormone: Stimulation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 35. ANS: F PTS: 1 DIF: Cognitive Level: Application REF: 836-838, 836, Table 36-1 OBJ: 1 (theory) TOP: Thyroid Hormone: Stimulation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 36. ANS: B PTS: 1 DIF: Cognitive Level: Application REF: 836-838, 836, Table 36-1 OBJ: 1 (theory) TOP: Thyroid Hormone: Stimulation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 37. ANS: D PTS: 1 DIF: Cognitive Level: Application REF: 836-838, 836, Table 36-1 OBJ: 1 (theory) TOP: Thyroid Hormone: Stimulation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 38. ANS: E PTS: 1 DIF: Cognitive Level: Application REF: 836-838, 836, Table 36-1 OBJ: 1 (theory) TOP: Thyroid Hormone: Stimulation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation Chapter 37: Care of Patients with Diabetes and Hypoglycemia deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is explaining the underlying pathophysiology of type 1 diabetes to a newly diagnosed patient. Which information accurately explains why the type 1 diabetic does not produce adequate insulin? a. A pituitary disorder inhibits beta cells. b. An allergic response alters beta cell responses to hyperglycemia. c. Alpha cells proliferated in the islets of Langerhans. d. The body’s immune system destroyed beta cells. ANS: D In type 1 diabetes mellitus (DM), the beta cells on the islets of Langerhans are destroyed by an autoimmune reaction. PTS: 1 DIF: Cognitive Level: Comprehension REF: 858 OBJ: 1 (clinical) TOP: Type 1 DM: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. Type 2 diabetes cases compose approximately what percentage of all known cases of diabetes? a. 70% b. 75% c. 80% d. 95% ANS: D Type 2 diabetics comprise 90% to 95% of all known cases. PTS: 1 DIF: Cognitive Level: Knowledge REF: 858 OBJ: 1 (theory) TOP: Type 2 DM: Incidence KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 3. The nurse is educating a patient with gestational diabetes. Which statement indicates that the patient needs additional teaching? a. “Gestational diabetes happens because of the hormonal changes of pregnancy.” b. “I should exercise regularly and lose weight to reduce my risk of becoming a diabetic.” c. “This problem goes away completely once I give birth.” d. “The baby will have to be monitored for hypoglycemia during my pregnancy.” ANS: C Giving birth does not automatically resolve gestational diabetes. Of the women who have gestational diabetes, 5% to 10% go on to develop type 2 diabetes. The patient correctly understands that gestational diabetes occurs because of hormonal changes in pregnancy, proper diet and regular exercise may help decrease the likelihood of developing type 2 diabetes, and the baby will require monitoring for hypoglycemia throughout the patient’s pregnancy. PTS: 1 DIF: Cognitive Level: Application REF: 858, Table 37-1, 859 OBJ: 2 (theory) TOP: Gestational Diabetes: Risks KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. A patient asks the nurse if stress can be a potential cause of type 2 diabetes. Which response is most appropriate for the nurse to make? a. “Stress decreases the number of alpha cells in the pancreas, and increases the workload on the beta cells.” b. “Periods of stress cause increases in glycogen production by the adrenal cortex.” c. “Stress is directly associated with decreased insulin tolerance.” d. “The inhibition of beta cells to glucose is increased in periods of stress.” ANS: B Stress stimulates the adrenal cortex to release glucocorticoids, which can cause hyperglycemia. PTS: 1 DIF: Cognitive Level: Application REF: 859 OBJ: 2 (theory) TOP: DM: Metabolic Risks KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. The nurse is counseling an overweight, noncompliant, 30-year-old female with type 2 diabetes. Which change is most important for the nurse to suggest? a. Begin an exercise program and lose weight. b. Obtain annual eye examinations. c. Keep a food diary. d. Inspect feet daily. ANS: A All of these changes are important, but exercise and weight loss are priority changes. In the type 2 diabetic, weight reduction and increased physical activity can restore blood glucose to normal levels and maintained it—hence the importance of diet and exercise in the management of type 2 diabetes. Annual eye examinations are important to detect onset of diabetic retinopathy. A food diary can help the patient to visualize food intake that may be subconscious otherwise. Diabetics are prone to foot problems and wounds and should inspect their feet daily. PTS: 1 DIF: Cognitive Level: Analysis REF: 859 OBJ: 2 (theory) TOP: DM: Modifiable Risks KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 6. The nurse is educating the patient about the significance of islet cell antibodies. Which statement accurately describes islet cell antibodies? a. Islet cell antibodies cause beta cells to quit producing insulin and lead to type 1 diabetes mellitus (DM). b. Islet cell antibodies protect beta cells from viral attack. c. Islet cell antibodies increase production of insulin from beta cells. d. Islet cell antibodies decrease the size of the pancreas. ANS: A The antibodies cause beta cells to quit production of insulin. PTS: 1 DIF: Cognitive Level: Understanding REF: 859 OBJ: 2 (theory) TOP: DM: Islet Cell Antibodies KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 7. The nurse is educating a 50-year-old patient about diabetes monitoring. Which statement reinforces the American Diabetes Association’s (ADA’s) recommendation? a. Obtain regularly scheduled fasting blood glucose levels. b. Strictly adhere to weight reduction diets. c. Exercise regularly in intervals lasting a minimum of 30 minutes. d. Use stress reduction techniques. ANS: A The ADA recommends screening with a fasting blood glucose. Adherence to a weight loss plan, regular exercise, and stress reduction techniques help control diabetes but do not monitor it. PTS: 1 DIF: Cognitive Level: Analysis REF: 859 OBJ: 4 (theory) TOP: ADA Recommendations: Screening KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 8. A patient recently diagnosed with type 1 diabetes mellitus (DM) asks why she is experiencing increased thirst. Which explanation is most appropriate? a. Diabetes results in a lack of protein absorption that decreases amino acids and causes increased thirst. b. High glucose levels in the blood pull cellular water into circulating volume and increase thirst. c. Thirst results from the body’s increased loss of fluids from frequent urination. d. Diabetes causes large amount of fluid to shut to the pancreas, which dehydrates the body. ANS: B Polydipsia is stimulated by cellular dehydration from the hyperglycemia pulling intracellular fluid into the circulating volume. PTS: 1 DIF: Cognitive Level: Comprehension REF: 859-860 OBJ: 2 (clinical) TOP: Polydipsia: Pathophysiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 9. The nurse is caring for a patient with ketosis. Which statement indicates that the patient correctly understands the phenomenon? a. “I took too much insulin to decrease my body’s glucose levels.” b. “The condition resulted when my body tried to break down and use my stores of fats.” c. “My blood glucose went over 150 mg/dL and caused this condition.” d. “I exercised too much reduced my blood glucose level too dramatically.” ANS: B People with type 1 diabetes are more prone to a serious complication, ketosis, associated with an excess production of ketone bodies, leading to ketoacidosis (metabolic acidosis). When the glucose level gets too high, the body attempts to metabolize fats for energy, and the result is a buildup of ketone bodies. PTS: 1 DIF: Cognitive Level: Comprehension REF: 860 OBJ: 5 (clinical) TOP: Ketosis: Etiology KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 10. The nurse is caring for a patient with type 1 diabetes who is diaphoretic and clammy. The patient complains of hunger but denies pain. The nurse performs a bedside blood glucose check. What should the nurse do next? a. Administer insulin as scheduled. b. Notify the charge nurse. c. Give 6 ounces of orange juice. d. Document the findings. ANS: C These findings are consistent with hypoglycemia; manifestations of hypoglycemia include tremulousness, hunger, headache, pallor, sweating, palpitations, blurred vision, and weakness. Management includes providing a source of quick-acting carbohydrate/glucose such as orange juice. The nurse should withhold the patient’s scheduled insulin at this time. The nurse should document the findings and then notify the charge nurse. PTS: 1 DIF: Cognitive Level: Analysis REF: 868, Table 37-6 OBJ: 3 (clinical) TOP: Hypoglycemia: Nursing Interventions KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 11. Which laboratory values are consistent with a patient in ketoacidosis? a. Blood urea nitrogen (BUN) of 35 mg/dL b. Carbon dioxide (CO2) of 40 mEq/L c. pH of 7.54 d. Blood glucose of 70 mg/dL ANS: A Diabetic ketoacidosis results when the body attempts to metabolize protein and fats, which results in high BUN readings. The CO2 should be normal or low depending on the effectiveness of Kussmaul respirations. The arterial pH will be low, and there will be high glucose, which the diabetic patient cannot use. PTS: 1 DIF: Cognitive Level: Analysis REF: 860 OBJ: 5 (clinical) TOP: Ketoacidosis: Laboratory Values KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 12. The patient comes to the emergency room complaining of abdominal pain. The nurse assesses dry, hot skin, fruity breath, and deep respirations. To which problem should the nurse attribute these findings? a. An insulin reaction b. Ketoacidosis c. Rebound hyperglycemia d. Hypoglycemia ANS: B Abdominal pain with dry, hot skin, fruity breath, and deep respirations is characteristic of ketoacidosis. Manifestations of an insulin reaction, or hypoglycemia, include tremulousness, hunger, headache, pallor, sweating, palpitations, blurred vision, and weakness. Rebound hyperglycemia, or the Somogyi effect, follows a period of hypoglycemia, often during sleep. When hypoglycemia occurs, the body secretes glucagon, epinephrine, growth hormone, and cortisol to counteract the effects of low blood sugar. The patient may report nightmares and night sweats along with morning elevated serum glucose; if the patient increases the insulin dose, it worsens the problem. PTS: 1 DIF: Cognitive Level: Comprehension REF: 868, Table 37-6 OBJ: 5 (clinical) TOP: Ketoacidosis: Indicators KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 13. Which reason best explains why diabetics are prone to infection? a. High glucose levels provide an environment conducive to bacterial growth. b. Atherosclerotic vascular changes decrease blood supply to tissues. c. Diabetics display abnormal phagocyte function. d. Diabetics display decreased leukocyte function. ANS: B The primary reason for increased risk of infection in diabetic patients is the hyperglycemic environment. Lesser risk factors include atherosclerotic vascular changes, abnormal phagocyte function, and decreased leukocyte function. PTS: 1 DIF: Cognitive Level: Application REF: 870 OBJ: 3 (theory) TOP: DM: Infections KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 14. The nurse notes that the HbA1c level of an assigned patient demonstrated a drop from 9.4% to 5.4%. What can the nurse infer from these findings? a. The patient’s blood glucose control has improved over the last several months. b. The patient has been less compliant with the prescribed treatment regimen. c. The patient is experiencing a reduction in insulin sensitivity. d. The patient has less need for insulin. ANS: A HbA1c is a diagnostic assessment used to review blood glucose levels retrospectively. A reduction in the value indicates improved glucose control by the patient. There is no evidence of insulin sensitivity. The need for insulin is not decreased in this patient. PTS: 1 DIF: Cognitive Level: Analysis REF: 860 OBJ: 4 (clinical) TOP: Type 1 DM: HbA1c KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 15. The nurse is caring for an older adult patient who is diabetic. The nurse cautions against the technique of “tight control” of hyperglycemia. Which statement explains why this management method is not recommended? a. Older adults may not accurately test and administer sliding-scale insulin. b. Older adults possess lower risk for hyperglycemia. c. Older adults may experience cardiovascular problems from hypoglycemia. d. Older adults possess an unstable metabolic rate. ANS: C One complication of the “tight control” method includes hypoglycemia. Older adults experience hypoglycemia more quickly than do younger people, and older adults are more prone to hypoglycemic episodes. The older adult may progress to dangerously low levels of blood glucose before signs and symptoms are obvious. Severe hypoglycemia in the older adult can precipitate myocardial infarction, angina, stroke, or seizures. For this reason, “tight control” may not be the best thing for the older adult. Older adults can accurately test and administer insulin, possess a higher risk for hypoglycemia, and do not possess an unstable metabolic rate. PTS: 1 DIF: Cognitive Level: Application REF: 860, Older Adult Care Points OBJ: 1 (clinical) TOP: Tight Control of Hyperglycemia: Older Adult KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 16. Which goal is the primary objective of a diabetic diet? a. Adequate nutrition with weight control b. Exclusion of all sweets c. Increased fat intake for greater energy d. Elimination of all fast foods ANS: A Currently, the diabetic diet is much less stringent than diets of years past. The primary goal of the current diabetic diet includes adequate nutrition with weight and cholesterol control. The newer diets allow for some sweets and some fast foods. Fats are not adequate sources of energy. Fat intake should be limited to reduce complications related to weight gain and cardiovascular concerns. PTS: 1 DIF: Cognitive Level: Comprehension REF: 861 OBJ: 1 (clinical) TOP: DM: Diet KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance 17. The patient takes his NovoLog 70/30 at 0700. When should the nurse suggest that the patient schedule exercise? a. 0730. b. 1000. c. 1300. d. Scheduling exercise is unnecessary. ANS: C Exercise should occur after peak action time to prevent hypoglycemia. NovoLog is a rapid-acting insulin that peaks 1 to 3 hours after administration. Since the insulin is administered at 70/30, scheduling exercise for 1300 would mean that it occurs after the peak insulin action. PTS: 1 DIF: Cognitive Level: Application REF: 861 OBJ: 1 (clinical) TOP: Exercise: Schedule KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 18. The nurse is discussing insulin administration with an assigned patient. The patient reports that she prefers to use only certain sites for insulin injections and questions the need to rotate sites. What response by the nurse is most appropriate? a. “Rotating injection sites helps reduce your risk of infection.” b. “Rotating injection sites helps enhance insulin absorption.” c. “Unsightly fatty tumors can develop when you do not adequately rotate injection sites.” d. “Rotating injection sites decreases your risk of an insulin reaction.” ANS: B Insulin injections are rotated within one body area to enhance absorption. Patients are given charts showing the places on the arms, legs, buttocks, and abdomen where insulin can be injected. Patients should be encouraged to keep a daily record of injection sites to help remember which sites have been used and to avoid the problem of altered or erratic absorption, which is a complication associated with overuse of a single site. The most important way to reduce the incidence of infection is to wash the hands before insulin administration and to avoid reusing syringes. Fatty tumors are not complications of overuse of a single injection site. The term insulin reaction refers to hypoglycemia, and hypoglycemia is not directly associated with the failure to rotate injection sites. PTS: 1 DIF: Cognitive Level: Application REF: 865 OBJ: 1 (clinical) TOP: Insulin Injection: Site Rotation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 19. A long-term diabetic patient reports that he has been diagnosed with early cardiovascular disease. How does diabetes predispose the patient to cardiovascular complications? a. Hyperglycemic periods cause thickening of the basement membrane in vessels, which causes atherosclerosis. b. Hypoglycemic periods increase cortisol release, which causes hypertension. c. Insulin constricts the cardiovascular vessels, which causes congestive heart failure. d. Diabetes decrease in the body’s ability to digest fats by the pancreas, which leads to increased coronary artery blockage. ANS: A Periods of hyperglycemia cause thickening of the vessels, chiefly the basement membrane (thin layer of connective tissue under the epithelium). The vessels of the retina, renal glomeruli, peripheral nerves, muscles, and skin are affected. Larger vessels are also affected, predisposing the patient to atherosclerosis and vascular occlusion. Two out of three people with diabetes die prematurely from heart attack or stroke. PTS: 1 DIF: Cognitive Level: Understanding REF: 869 OBJ: 3 (theory) TOP: Cardiovascular Complications: Etiology KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 20. The nurse is caring for a patient who struggles to maintain glycemic control at night and during early morning hours. Which statement correctly explains the reason for this problem? a. Counterregulatory hormones produce hyperglycemia. b. Hyperglycemia of dawn phenomenon does not react to insulin. c. Hypoglycemia quickly follows the dawn phenomenon. d. Food intake fails to change hyperglycemia of dawn phenomenon. ANS: A Dawn phenomenon is produced in the morning by the circadian release of growth hormones, epinephrine, and glucagon during the night. Rebound hyperglycemia, also known as the Somogyi effect, follows a period of hypoglycemia, often during sleep. When hypoglycemia occurs, the body secretes glucagon, epinephrine, growth hormone, and cortisol to counteract the effects of low blood sugar. The patient may report nightmares and night sweats along with morning elevated serum glucose; if the patient increases the insulin dose, it worsens the problem. The dawn phenomenon is characterized by elevated blood glucose in the morning and is caused by release of growth hormone, glucagon, and epinephrine during the night, as part of the body’s natural circadian rhythm. These hormones act to raise the body’s blood sugar. The dawn phenomenon is the reason why most people with diabetes do not tolerate carbohydrates well in the morning. The treatment is an intermediate-acting insulin at night. PTS: 1 DIF: Cognitive Level: Comprehension REF: 869 OBJ: 1 (clinical) TOP: DM: Dawn Phenomenon KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 21. A patient with type 1 diabetes mellitus (DM) is preparing for a moderate 30-minute exercise period. Which action best indicates that the patient understands condition management? a. The patient reduces insulin use during days when exercise periods are planned. b. The patient administers insulin after exercise rather than before exercise. c. The patient eats a high-carbohydrate snack before the exercise period. d. The patient consumes a simple carbohydrate snack after 30 minutes of activity. ANS: D During moderate exercise (such as brisk walking, bowling, or vacuuming), 5 g of simple carbohydrate should be consumed at the end of 30 minutes and at 30-minute intervals during the continued activity. (A food example with 5 g of simple carbohydrate is 1 tsp honey.) PTS: 1 DIF: Cognitive Level: Application REF: 862 OBJ: 1 (clinical) TOP: Increasing Food During Exercise KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 22. The nurse is reviewing the patient’s prescribed insulin regimen. The nurse notes that the physician has ordered a longlasting insulin. Which medication best meets this criteria? a. Lantus b. NovoLog c. Humalog d. Regular ANS: A Lantus is a long-lasting insulin. It may be administered only one time per day. NovoLog and Humalog are both rapid-onset insulin preparations. Regular insulin is classified as a short-acting insulin. PTS: 1 DIF: Cognitive Level: Knowledge REF: 864, Table 37-3 OBJ: 1 (clinical) TOP: Common Types of Insulin: Onset, Peak, and Duration of Action KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies MULTIPLE RESPONSE 23. Which genetic factor(s) increase(s) the risk of a person developing diabetes mellitus (DM)? (select all that apply.) a. Number of relatives with DM b. Body mass index (BMI) c. Sedentary lifestyle d. Genetic closeness of relatives with DM e. Race ANS: A, D, E Genetic factors that increase the risk of developing diabetes include the number and genetic closeness of relatives with diabetes, as well as race. BMI and sedentary lifestyle are not genetic factors. PTS: 1 DIF: Cognitive Level: Understanding REF: 859 OBJ: 2 (theory) TOP: DM: Genetic Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 24. Which factor(s) may cause diabetes mellitus (DM)? (select all that apply.) a. Genetic b. Microbiologic c. Metabolic d. Allogenic e. Immunologic ANS: A, B, C, E Genetic, microbiologic, metabolic, and immunologic factors influence the development of diabetes mellitus. Allogenic refers to cells or tissues that are from different individuals in the same species. PTS: 1 DIF: Cognitive Level: Comprehension REF: 859 OBJ: 2 (theory) TOP: DM: Etiology KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 25. Which statement(s) explain(s) a reason for weight loss in type 1 diabetics? (select all that apply.) a. Loss of body fluid b. Insulin intolerance c. Metabolization of body fats d. Stress of disease e. Altered diet ANS: A, C Weight loss in type 1 diabetics can be attributed to loss of body fluids and metabolization of fats. Insulin intolerance, stress of the disease, and altered diet are not reasons for weight loss in type 1 diabetes. PTS: 1 DIF: Cognitive Level: Application REF: 860 OBJ: 2 (clinical) TOP: DM: Weight Loss KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 26. Which requirement(s) is/are part of the criteria for “tight control” of hyperglycemia? (select all that apply.) a. Perform glucose testing twice daily. b. Administer insulin injections three times a day based on glucometer readings. c. Maintain fasting glucose within normal limits. d. Maintain normal weight for height and age. e. Maintain cholesterol within normal limits. ANS: B, C, D, E Patients attempting tight control follow an intensive therapy plan of blood glucose testing and insulin injections, three or more times a day, or they use an insulin pump. Maintaining a normal fasting glucose, weight for height and age, and cholesterol helps establish “tight control” of hyperglycemia. PTS: 1 DIF: Cognitive Level: Application REF: 860 OBJ: 1 (clinical) TOP: DM: “Tight Control” KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 27. When discussing exercise programs with the diabetic, which instruction(s) is/are important for the nurse to include? (select all that apply.) a. Delay exercise until glucose controlled. b. Check glucose immediately after exercising. c. Keep a quick source of glucose readily available while exercising. d. Begin slowly and build up to 30 to 45 minutes. e. Only use the abdominal injection site for insulin. ANS: A, C, D, E The patient should delay exercise until glucose is controlled, keep a quick source of glucose readily available, begin slowly and build, and use the abdominal injection site for insulin. The patient should check the glucose level before exercising. PTS: 1 DIF: Cognitive Level: Application REF: 861 OBJ: 1 (clinical) TOP: DM: Exercise KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 28. The nurse is caring for a patient suspected of having ketoacidosis. Which manifestation(s) is/are characteristic with early ketoacidosis? (select all that apply.) a. Fruity breath b. Polyuria c. Nausea d. Thirst e. Sunken eyes ANS: A, B, D Ketoacidosis is a complication associated with type 1 diabetes. Some of the earliest symptoms may be polyuria, fatigue, anorexia, abdominal pain, and a fruity smell to the breath. Later signs and symptoms include sunken eyes as a result of excessive dehydration. Nausea is not associated with ketoacidosis. PTS: 1 DIF: Cognitive Level: Application REF: 868, Table 37-6 OBJ: 4 (theory) TOP: Types of Diabetes: Characteristics KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 29. The nurse watches a patient perform an insulin injection. Which observation(s) indicate(s) that the patient needs additional instruction? (select all that apply.) a. The patient uses a 90-degree angle to administer the injection. b. The patient cleans the injection site with alcohol before the injection. c. The patient rubs the injection site after administration of the insulin injection. d. The patient draws up the cloudy insulin and then the clear insulin. e. The patient shakes the insulin bottle before administration. ANS: C, D, E The patient should not rub the injection site because it could alter absorption. When mixing two types of insulin, in order to prevent contamination of the second vial, the patient should withdraw clear insulin into the syringe first. Shaking the bottle can damage the solution; the patient should gently roll the bottle between the palms of the hands. Administering the injection at a 90- degree angle and cleaning the injection site prior to injection describe appropriate technique. PTS: 1 DIF: Cognitive Level: Analysis REF: 865 OBJ: 1 (clinical) TOP: Patient Teaching: Guidelines for Subcutaneous Insulin Injection KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies COMPLETION 30. The nurse explains that the three cardinal signs of type 1 diabetes mellitus (DM) are __________, __________, and __________. ANS: polydipsia, polyphagia, polyuria polydipsia, polyuria, polyphagia polyphagia, polyuria, polydipsia polyphagia, polydipsia, polyuria polyuria, polydipsia, polyphagia polyuria, polyphagia, polydipsia The three Ps—polydipsia, polyphagia, and polyuria—are the cardinal signs of diabetes. PTS: 1 DIF: Cognitive Level: Comprehension REF: 860 OBJ: 1 (theory) TOP: Type 1 DM: Cardinal Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation MATCHING The nurse associates the type of diabetes with the characteristics that may be seen with the specific disease. Match the type of diabetes with the symptoms that are associated with it. (The options may be used once, more than once, or not at all.) a. Type 1 b. Type 2 c. Gestational d. Prediabetes 31. Weight loss and exercise can delay onset of diabetes 32. Occurs during pregnancy 33. Adult onset 34. Little or no endogenous insulin 35. Threat of renal, retinal, and neurologic complications 36. Rarely develops ketosis 31. ANS: D PTS: 1 DIF: Cognitive Level: Analysis REF: 858, Table 37-1 OBJ: 1 (theory) TOP: Types of Diabetes: Characteristics KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 32. ANS: C PTS: 1 DIF: Cognitive Level: Analysis REF: 858, Table 37-1 OBJ: 1 (theory) TOP: Types of Diabetes: Characteristics KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 33. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 858, Table 37-1 OBJ: 1 (theory) TOP: Types of Diabetes: Characteristics KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 34. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 858, Table 37-1 OBJ: 1 (theory) TOP: Types of Diabetes: Characteristics KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 35. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 858, Table 37-1 OBJ: 1 (theory) TOP: Types of Diabetes: Characteristics KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 36. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 858, Table 37-1 OBJ: 1 (theory) TOP: Types of Diabetes: Characteristics KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance Chapter 38: Care of Women with Reproductive Disorders deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The patient complains to the nurse about a sharp pain in the lower quadrants every month at midcycle that lasts for several hours. This description is consistent with which underlying pathophysiological process? a. Round ligament stretching to support the uterus b. Mittelschmerz, a pain associated with ovulation c. Premenstrual uterine enlargement d. Endometrial changes ANS: B Mittelschmerz is a pain in either lower quadrant associated with ovulation. There is no stretching of the round ligaments during the midcycle period. Premenstrual uterine changes do not produce discomfort. PTS: 1 DIF: Cognitive Level: Knowledge REF: 883 OBJ: 3 (theory) TOP: Mittelschmerz: Definition KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. How does the body benefit from the normal acidic pH of the vaginal vault? a. Supported vaginal muscle tone b. Vaginal lubrication c. A hostile environment to sperm d. Protection against infection ANS: D The acidic pH of the vagina, provided by lactic acid, is a defense against infection. The low pH is a hostile environment for pathogens. Muscle tone in the vagina is not affected by the pH level. The vagina is not a hostile environment to the sperm. PTS: 1 DIF: Cognitive Level: Comprehension REF: 883 OBJ: 1 (theory) TOP: Vaginal pH: Purpose KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. The nurse is educating a speaking to a group of junior high girls about reproductive health. Which information is most important to include? a. Breasts may be tender in the middle of the cycle. b. Girls ages 12 or older who have not had a period should see a doctor. c. Irregular or missed periods are nothing to worry about. d. A normal period may last up to 2 weeks. ANS: A Hormonal changes during the midportion of the cycle may increase breast tenderness. The onset of the menstrual cycle completes puberty and usually occurs between ages 9 and 17. During the first year following menarche, the menstrual cycle may be somewhat irregular, but by the second year a regular cycle of approximately 28 days is normally established. Irregular periods may be a benign finding, but late or absent periods could also be a cause for concern (including a potential sign of pregnancy). Menstrual bleeding occurs about 14 days after ovulation and lasts between 2 and 8 days. PTS: 1 DIF: Cognitive Level: Comprehension REF: 884 OBJ: 3 (theory) TOP: Breast Tenderness: Timing KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. When does premenstrual syndrome (PMS) occur? a. The follicular phase of the ovarian cycle b. The luteal phase of the ovarian cycle c. The dismantling stage of the menstrual cycle d. The proliferative stage of the stage of the menstrual cycle ANS: B PMS occur during the luteal stage, which lasts from day 15 to day 28 of a 28-day cycle. The uterus prepares to receive a fertilized ovum during this phase. The follicular phase includes the first 14 days of a 28-day cycle. During this dismantling stage, the endometrial layer sloughs away and menstrual flow begins. During the proliferative stage of the menstrual cycle, the follicle grows and the egg matures. PTS: 1 DIF: Cognitive Level: Comprehension REF: 884 OBJ: 3 (theory) TOP: PMS: Etiology KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. The nurse is educating a patient with premenstrual dysphoric disorder (PMDD) about potential triggers. Which nutritional change should the nurse suggest to help reduce symptoms? a. Eat whole-grain bread instead of white bread. b. Drink 4 ounces of red wine once a week. c. Increase red meat intake to boost iron stores. d. Use sugar instead of artificial sweeteners. ANS: A Strategies for self-care of PMDD may include stress management exercises, some lifestyle changes, and maintaining a healthy diet rich in complex carbohydrates and fiber (like whole-grain breads and pastas or lentils). Alcohol, red meat, and sugar exacerbate the symptoms of PMDD. PTS: 1 DIF: Cognitive Level: Analysis REF: 884 OBJ: 3 (theory) TOP: PMDD: Self-Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: Coping and Adaptation 6. Unresolved primary dysmenorrhea may cause the young female to develop which negative perception? a. An exaggerated sense of symptom severity b. A distrust of medications c. A negative attitude toward her own sexuality d. An unhealthy tendency toward peer comparison ANS: C Unresolved dysmenorrhea in the young woman can cause negative attitudes related to sexuality and self-worth. PTS: 1 DIF: Cognitive Level: Comprehension REF: 884 OBJ: 3 (theory) TOP: Dysmenorrhea: Negative Attitude KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: Coping and Adaptation 7. Which change is a possible benefit of oral contraceptives? a. Decreased breast tenderness b. Weight loss c. Heightened sexual pleasure d. Decrease incidence of vaginitis ANS: A Decreased breast tenderness is a benefit of oral contraceptives. Oral contraceptives do not cause weight loss, heightened sexual pleasure, or decreased incidence of vaginitis. PTS: 1 DIF: Cognitive Level: Knowledge REF: 886 OBJ: 4 (theory) TOP: Oral Contraception: Benefits KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 8. The nurse is caring for an adolescent girl with primary dysmenorrhea. The girl’s mother reports that her daughter has been absent from school at least 1 day during her last four periods. She anticipates that the health care provider will likely prescribe which treatment? a. Aromatherapy b. Dietary modification c. Effleurage d. Oral contraceptive Sesonale ANS: D Seasonale is a popular oral contraceptive that provides delayed menstruation. Since this patient is accruing multiple short-term school absences over a period of months, Seasonale would provide longer periods of pain-free amenorrhea by allowing only four menstrual periods per year. Aromatherapy, dietary modification, and effleurage may also help relieve discomfort when present but extend pain-free intervals. PTS: 1 DIF: Cognitive Level: Application REF: 886 OBJ: 4 (theory) TOP: Contraception: Seasonale KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 9. Which statement indicates that the patient requires additional teaching related to emergency contraception? a. “I should take Uliprisal (Ella) within 5 days of unprotected sex.” b. “I should take an antiemetic before I take levonorgestrel.” c. “Plan B one-step is available over the counter.” d. “I should follow up with my doctor after taking any emergency contraception.” ANS: B The emergency contraceptive Uliprisal (Ella) requires a prescription. It prevents pregnancy by prolonging ovulation and can be taken up to 5 days after unprotected sex. The woman is advised to take an antiemetic prior to each dose to minimize nausea and vomiting. Antiemetics are not necessary before levonorgestrel. “Plan B one-step” is one tablet of levonorgestrel only, taken within 72 hours of unprotected sex; the tablet was approved in July 2009 and is available without prescription to women over 17 years of age. After using any emergency contraception, the patient should be referred for counseling and follow-up care. PTS: 1 DIF: Cognitive Level: Application REF: 890-891 OBJ: 4 (theory) TOP: Emergency Contraception KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 10. A copper intrauterine device (IUD) can be used as an emergency contraceptive measure if it is inserted within what time frame after unprotected sex? a. 12 hours b. 3 days c. 7 days d. 10 days ANS: C A copper IUD can be inserted up to 7 days after unprotected sexual intercourse to prevent implantation of the zygote in women who prefer long-term contraception. PTS: 1 DIF: Cognitive Level: Knowledge REF: 891 OBJ: 4 (theory) TOP: IUD: Emergency Contraception KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 11. The nurse educates a patient about differences between primary infertility and secondary infertility. Which statement accurately describes primary infertility? a. Inability to maintain a pregnancy past the first trimester. b. Inability to conceive after 1 year of active unprotected sex. c. Inability to deliver a viable infant after two pregnancies. d. Inability to conceive after using a follicle stimulator for 1 year. ANS: B Primary infertility is defined as inability to conceive after 1 year of active unprotected sex. Secondary infertility is the inability to conceive after having once conceived, or the inability to maintain a pregnancy long enough to deliver a viable infant. Approximately 10% to 20% of U.S. couples have infertility, and today more couples are seeking medical intervention. PTS: 1 DIF: Cognitive Level: Comprehension REF: 891 OBJ: 5 (theory) TOP: Primary Infertility: Definition KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 12. During a family planning session, a young couple confides that they are hoping to conceive. Which action should the nurse suggest to potentially enhance conception? a. Relax together in a sauna or hot tub. b. Stimulate the scrotum with a vibrator. c. Increased time spent in foreplay. d. Use water-soluble lubricant. ANS: D Water-soluble lubricant has no spermicidal properties as compared to other lubricants that may damage sperm and decrease chances of conception. Heat to the scrotum depresses spermatogenesis and could decrease chance of conception. Foreplay and vibrators do not increase spermatogenesis and will not increase the chances of conception. PTS: 1 DIF: Cognitive Level: Analysis REF: 891 OBJ: 5 (theory) TOP: Infertility: Techniques to Enhance Conception KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 13. An infertile couple considering zygote intrafallopian transfer (ZIFT) asks how it differs from in vitro fertilization (IVF). Which information about ZIFT is most important for the nurse to include? a. During ZIFT, fallopian tubes are artificially lined with material that nourishes the gamete. b. During ZIFT, the fertilized egg is placed in the fallopian tube. c. During ZIFT, fallopian tubes are cleared with injected air. d. During ZIFT, fallopian tube is implanted with unfertilized ova and sperm. ANS: B The ZIFT refers to the placement of the fertilized ovum into the fallopian tube at the zygote stage of development. During IVFET, the woman’s eggs are collected from the ovary, fertilized in the laboratory, and transferred into the uterus at the embryo stage of development. PTS: 1 DIF: Cognitive Level: Comprehension REF: 892 OBJ: 5 (theory) TOP: ZIFT vs. IVF KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 14. The nurse is caring for a female patient who reports using an estrogen cream as a lubricant for sexual intercourse. The nurse should caution the patient about which potential negative effect? a. Estrogen cream may damage latex condoms. b. Estrogen cream may exacerbate hot flashes. c. Estrogen cream may decrease elasticity of vaginal tissue. d. Estrogen cream may cause contact dermatitis for sexual partners. ANS: A Using estrogen cream as a lubricant for sexual intercourse is discouraged as the cream may damage latex condoms and require a backup method of contraception. Estrogen cream will not exacerbate hot flashes. Estrogen cream is used to increase vaginal tissue elasticity. While the partner can absorb estrogen from estrogen cream for sexual intercourse, contact dermatitis is not likely. PTS: 1 DIF: Cognitive Level: Comprehension REF: 892, Older Adult Care Points OBJ: 6 (theory) TOP: Estrogen Cream: Precaution KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 15. The nurse is caring for a patient taking long-term estrogen replacement for osteoporosis prevention. The nurse recommends that the patient undergo which type of examination annually? a. Pelvic examination b. Bone density study c. Liver scan d. Lower GI study ANS: A Estrogen therapy increases the incidence of endometrial cancer and breast cancer. An annual pelvic examination is recommended, as well as monthly breast self-examinations (BSE). PTS: 1 DIF: Cognitive Level: Application REF: 893, Older Adult Care Points OBJ: 6 (theory) TOP: Estrogen Therapy: Precautions KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 16. The nurse is caring for a menopausal patient who is experiencing hot flashes. The nurse suggests that the patient increase intake of which foods? a. Red meat and leafy greens b. Cherries and black beans c. Carrots and asparagus d. Yogurt and cheese ANS: B During menopause, decreasing estrogen levels may cause hot flashes. Cherries, yams, and black beans are foods rich in phytoestrogens, substances found in plants that may act like normally produced estrogen. Red meat and leafy greens are rich in iron, carrots, and asparagus are rich in beta carotene. Yogurt and cheese are rich in calcium. Iron, beta carotene, and calcium are not known to impact estrogen levels. PTS: 1 DIF: Cognitive Level: Application REF: 894, Nutritional Therapies OBJ: 6 (theory) TOP: Phytoestrogens: Sources KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 17. When should a patient conduct breast self-examinations (BSE)? a. The day after the onset of menses b. The day after menses stops c. 1 week after the onset of menses d. 1 week after menses stops ANS: C The examination should be performed 1 week after the period has begun, or on a specific date if menses has stopped. PTS: 1 DIF: Cognitive Level: Knowledge REF: 894 OBJ: 1 (clinical) TOP: BSE: Timing KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 18. After having a right total mastectomy, the patient confides that her husband has voiced concern about her “disfigurement.” Which response is most appropriate for the nurse to make? The nurse’s most therapeutic response would be: a. “What a terrible thing to say!” b. “Many husbands feel that way at first.” c. “His feelings will change over time.” d. “How did you respond to his statement?” ANS: D Using open-ended and matter-of-fact tactful questions will help the patient express feelings. Characterizing the husband’s statement as terrible renders an inappropriate judgment without exploring how the patient feels. Informing the patient about others’ feelings or offering empty reassurance that her husband will change over time is inappropriate and ineffective. PTS: 1 DIF: Cognitive Level: Application REF: 914 OBJ: 8 (theory) TOP: Mastectomy: Therapeutic Communication KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: Coping and Adaptation 19. Which statement accurately describes BRCA1 and BRCA2? a. BRCA1 and BRCA2 are genes involved with the inherited form of breast cancer. b. BRCA1 and BRCA2 are enzymes that are markers for breast cancer. c. BRCA1 and BRCA2 are particular proteins attached to the red blood cells indicating presence of breast cancer. d. BRCA1 and BRCA2 are laboratory tests performed on a breast biopsy to detect breast cancer. ANS: A BRCA1 and BRCA2 are genes that are involved in the inherited form of breast cancer. It should be noted that not all people who have a BRCA gene get cancer, and people without it may get cancer. PTS: 1 DIF: Cognitive Level: Comprehension REF: 894, 910 OBJ: 7 (theory) TOP: BRCA: Definition KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 20. The nurse is caring for a patient with a tentative diagnosis of polycystic ovarian syndrome (PCOS). When reviewing the patient’s health history, which finding supports this diagnosis? a. Cold intolerance b. Significant weight loss c. Menstrual periods every 33 days d. Elevated serum glucose levels ANS: D PCOS is a congenital condition in which many cysts develop on one or both ovaries and produce excess estrogen. High levels of testosterone and luteinizing hormone (LH) and low levels of follicle-stimulating hormone (FSH) occur. A manifestation of PCOS includes problems with glucose tolerance, which would result in elevated serum glucose levels. Other signs and symptoms include excessive body hair (hirsuitism), irregular menstruation, and infertility. Cold intolerance could be indicative of hypothyroidism, anemia, Raynaud syndrome, or other underlying medical issues. PTS: 1 DIF: Cognitive Level: Application REF: 903 OBJ: 10 (theory) TOP: PCOS KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 21. The nurse is caring for a patient diagnosed with toxic shock syndrome (TSS). Which statement best indicates the patient understands the causative factor of this disorder? a. “This problem likely resulted from an untreated sexually transmitted infection.” b. “This problem is linked to my ovarian cyst rupture.” c. “This problem could have resulted from using a diaphragm for birth control.” d. “Taking steroids is associated with this problem.” ANS: C TSS is a rare and potentially fatal disorder caused by strains of Staphylococcus aureus that produce toxins that cause shock, coagulation defects, and tissue damage if they enter the bloodstream. It is associated with the trapping of bacteria within the reproductive tract for a prolonged time. Risk factors include the prolonged use of high-absorbency tampons, cervical caps, or diaphragms. PTS: 1 DIF: Cognitive Level: Analysis REF: 907 OBJ: 10 (theory) TOP: TSS KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 22. The nurse is caring for a middle-aged woman who is not sexually active. The patient questions the nurse about the recommended frequency of Pap smears. Which response is best? a. Annual screening is recommended. b. Screening is not needed for women who are not sexually active. c. Screening in the woman who is not sexually active may be spaced every 5 to 7 years. d. In the woman with negative screenings, the Pap test may be repeated every 3 years. ANS: D Women with three consecutive negative screenings at age 30 should have repeated testing every 3 years until age 65, when testing of asymptomatic women is no longer necessary. American Congress of Obstetricians and Gynecologists (ACOG) recommends that cervical cancer screening should begin at age 21 and be repeated every 2 years between ages 21 and 29 in asymptomatic women. Women with three consecutive negative screenings at age 30 should have repeated testing every 3 years until age 65, when testing of asymptomatic women is no longer necessary. Women with cervical pathology or cancer should be screened annually for 20 years after treatment. PTS: 1 DIF: Cognitive Level: Application REF: 907 OBJ: 7 (theory) TOP: Cervical Cancer KEY: Nursing Process Step: Diagnosis MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential MULTIPLE RESPONSE 23. Which age-related change(s) occur(s) in the woman after menopause? (select all that apply.) a. Atrophy of uterus b. Vaginal dryness c. Decrease in bone mass d. Increase in vaginal elasticity e. Uterine prolapse ANS: A, B, C, E Age-related changes that occur in women after menopause include uterine atrophy, increased vaginal dryness, decreased bone mass, and uterine prolapse. Vaginal elasticity decreases after menopause. PTS: 1 DIF: Cognitive Level: Comprehension REF: 882 OBJ: 2 (theory) TOP: Age-Related Changes: Postmenopause KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 24. Which manifestation(s) is/are signals of premenstrual syndrome (PMS)? (select all that apply.) a. Bloating b. Irritability c. Depression d. Excessive energy e. Fear of losing control ANS: A, B, E Signs of PMS include bloating, irritability, fear of losing control, breast tenderness, appetite changes, fatigue, and mood swings. PMS does not include depression or excessive energy. PTS: 1 DIF: Cognitive Level: Comprehension REF: 884 OBJ: 3 (theory) TOP: PMS: Signs and Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 25. The nurse is caring for a patient who is suffering from dysmenorrhea. Which action(s) is/are ways in which pelvic rock exercise decreases pain? (select all that apply.) a. Releasing endorphins b. Generating abdominal heat c. Suppressing prostaglandins d. Making the uterus drop forward e. Relieving pelvic congestion ANS: A, C, E Pelvic rock exercise decreases pain by releasing endorphins, suppressing prostaglandins, and relieving pelvic congestion. Pelvic rock exercise does not generate heat nor does it make the uterus drop forward. PTS: 1 DIF: Cognitive Level: Comprehension REF: 884 OBJ: 3 (theory) TOP: Dysmenorrhea: Pelvic Rock Exercise KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 26. The nurse is caring for a patient with primary dysmenorrhea. Which food(s) should the nurse suggest that the patient include in her diet? (select all that apply.) a. Watermelon b. Buttermilk c. Broccoli d. Asparagus e. Cranberries ANS: A, D, E The patient will benefit from a balanced low-fat diet with foods that are natural diuretics, like cranberries, asparagus, and watermelon. Broccoli and buttermilk do not have diuretic properties. PTS: 1 DIF: Cognitive Level: Application REF: 884 OBJ: 3 (theory) TOP: Dysmenorrhea: Diet KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 27. The nurse describes the “morning-after” pill, levonorgestrel, as a multipurpose pill. Which statement(s) describe(s) a purpose of levonorgestrel? (select all that apply.) a. Ovulation prevention b. Immediate menses induction c. Fertilization interference d. Alteration of ova DNA e. Prevention of uterine implantation ANS: A, C, E Levonorgestrel, depending on where in the menstrual cycle the woman is when she takes it, can prevent ovulation, interfere with fertilization, and prevent uterine implantation. It does not immediately induce menses or alter ova DNA. PTS: 1 DIF: Cognitive Level: Comprehension REF: 890 OBJ: 4 (theory) TOP: Levonorgestrel KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 28. Which manifestation(s) is/are signs and symptoms of menopause? (select all that apply.) a. Hot flashes and flushes b. Cessation of estrogen production c. Vaginal dryness d. Night sweats e. Irregularity of menses ANS: A, C, D, E Signs and symptoms of menopause include hot flashes, flushes, increasing vaginal dryness, night sweats, and menstrual irregularity. Estrogen production reduces but does not cease. PTS: 1 DIF: Cognitive Level: Knowledge REF: 892 OBJ: 6 (theory) TOP: Menopause: Signs and Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 29. The nurse is caring for a patient who has been diagnosed with a cystocele. The patient is not a surgical candidate. The nurse should include information about which nonsurgical management technique(s) in the teaching plan? (select all that apply.) a. Kegel exercises b. Pessary insertion of a pessary c. Hormone therapy d. Vitamin B12 therapy e. Increased fluid intake ANS: A, B, C, E Nonsurgical management includes teaching the woman how to perform Kegel exercises in order to strengthen the pubococcygeal muscles that support the pelvic floor. A pessary (a hard rubber or plastic ring) can be fitted into the vagina by the health care provider to provide support to the pelvic structures. Hormone therapy may be prescribed. Lifestyle changes include increasing fluid intake and a high-fiber diet to avoid constipation, avoiding heavy lifting, and maintaining an optimum weight. Cystocele care and treatment does not include vitamin B12 therapy. PTS: 1 DIF: Cognitive Level: Application REF: 903 OBJ: 2 (theory) TOP: Cystocele: Nonsurgical Management KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort COMPLETION 30. The nurse explains that the portion of the menstrual cycle in which the ova are stimulated and matured is the ________ phase. ANS: follicular The ova are stimulated and matured during the follicular phase of the menstrual cycle. PTS: 1 DIF: Cognitive Level: Comprehension REF: 882 OBJ: 1 (theory) TOP: Menstrual Cycle: Follicular Stage KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation MATCHING The nurse outlines the characteristics of primary or secondary dysmenorrhea to help the patient understand her condition. Match the options with the symptoms. (Options can be used once, more than once, or not at all.) a. Primary dysmenorrhea b. Secondary dysmenorrhea 31. Uterine contraction causing cramps 32. Caused by uterine polyps 33. Occurs within first menstruation past menarche 34. Lower abdomen pain progressing to back and thighs 35. Pain lasts throughout menstrual flow 36. Caused by release of high levels of prostaglandins 31. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 884 OBJ: 3 (theory) TOP: Dysmenorrhea: Primary vs. Secondary KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 32. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 884 OBJ: 3 (theory) TOP: Dysmenorrhea: Primary vs. Secondary KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 33. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 884 OBJ: 3 (theory) TOP: Dysmenorrhea: Primary vs. Secondary KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 34. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 884 OBJ: 3 (theory) TOP: Dysmenorrhea: Primary vs. Secondary KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 35. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 884 OBJ: 3 (theory) TOP: Dysmenorrhea: Primary vs. Secondary KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 36. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 884 OBJ: 3 (theory) TOP: Dysmenorrhea: Primary vs. Secondary KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation Chapter 39: Care of Men with Reproductive Disorders deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. In counseling a man with erectile dysfunction about a prescription for sildenafil (Viagra), when should the nurse suggest a different treatment? a. The patient is over 50 years of age. b. The patient takes nitroglycerin for angina. c. The patient is more than 50 pounds overweight. d. The patient is a long-term diabetic. ANS: B Viagra is contraindicated if the patient is also taking nitrates because the combination can cause significant hypotension. Age, weight, and diabetes are not contraindications for the use of Viagra. PTS: 1 DIF: Cognitive Level: Application REF: 927, Table 39-2 OBJ: 2 (theory) TOP: Erectile Dysfunction: Viagra KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 2. The nurse reminds a 68-year-old man that a man of any age can reproduce if he is able to perform which function? a. Maintain an erection b. Ejaculate c. Maintain a high sperm count d. Participate in intercourse ANS: D If a man can participate in intercourse, he can still reproduce, even with a low sperm count. PTS: 1 DIF: Cognitive Level: Comprehension REF: 926, Older Adult Care Points OBJ: 1 (theory) TOP: Sperm Production KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. The nurse is educating a patient who has been given a prescription for tadalafil (Cialis). The nurse warns the patient about which potential complication? a. Priapism b. Obstructed urethra c. Hydronephrosis d. Urethritis ANS: A Cialis can cause priapism, a persistent erection that can develop into a urologic emergency as penile vessels may become thrombosed. Urethral obstruction is not associated with the use of tadalafil (Cialis). Hydronephrosis refers to dilation of the renal pelvis and is not associated with the use of tadalafil (Cialis). Urethritis refers to infection or inflammation of the urethra and is not associated with the use of tadalafil (Cialis). PTS: 1 DIF: Cognitive Level: Application REF: 928 OBJ: 2 (theory) TOP: Erectile Dysfunction: Cialis KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 4. The nurse is interviewing a patient who is seeking assistance at the urology clinic for erectile dysfunction. Which statement is the best way to open the interview? a. “When was the last time you were impotent?” b. “Do you attempt to have intercourse every week?” c. “What medications have you tried previously?” d. “What experiences have you had with erectile dysfunction?” ANS: D Asking open-ended questions will help the patient respond with information that can be used in a plan of care. PTS: 1 DIF: Cognitive Level: Application REF: 923 OBJ: 2 (theory) TOP: ED: Interview KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: Coping and Adaptation 5. The nurse understands that the clinical definition of infertility is failure to conceive after frequent, unprotected sex over what period of time? a. 6 months b. 12 months c. 18 months d. 24 months ANS: B A couple who, after 1 year of unprotected sex, has not conceived is considered to be infertile. PTS: 1 DIF: Cognitive Level: Comprehension REF: 926 OBJ: 3 (theory) TOP: Infertility: Definition KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 6. The nurse is aware that of the known infertility causes, approximately what percentage is due to male factors? a. 15% b. 25% c. 35% d. 45% ANS: B Of the known cases of infertility, 25% to 30% are due to male factors. PTS: 1 DIF: Cognitive Level: Comprehension REF: 926 OBJ: 3 (theory) TOP: Male Infertility KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 7. The nurse explains to a male patient undergoing infertility studies that his luteinizing hormone (LH) is low and his follicle-stimulating hormone (FSH) is high. Which statement accurately interprets these laboratory findings? a. The patient is making testosterone and has decreased spermatogenesis. b. The patient is not making testosterone and has decreased spermatogenesis. c. The patient is making testosterone and has high spermatogenesis. d. The patient is not making testosterone and has high spermatogenesis. ANS: A A low LH means there is adequate stimulation of testosterone. A high FSH means there is a low or decreased spermatogenesis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 924, Table 39-1 OBJ: 4 (theory) TOP: Infertility Tests: LH and FSH KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 8. When developing a teaching plan for a young man who is undergoing fertility studies, which information is most important for the nurse to include? a. Engage in intercourse in the evening when testosterone levels are highest. b. Relax in a hot bath or Jacuzzi nightly to relieve stress. c. Wear boxer shorts instead of jockey shorts. d. Only engage in intercourse during your partner’s fertile period. ANS: C The heat from close body contact from wearing jockey shorts reduces spermatogenesis. Sexual intercourse will not increase testosterone levels. Heat will reduce sperm count, not increase it. PTS: 1 DIF: Cognitive Level: Application REF: 927 OBJ: 3 (theory) TOP: Infertility: Teaching Plan KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 9. A young man who has been diagnosed as sterile says to the nurse, “I am not much of a man or a husband.” Which response is most therapeutic? a. “I know you feel awful, but you can always adopt.” b. “How do you feel about artificial insemination?” c. “What about this sterility diagnosis concerns you the most?” d. “Sterility isn’t the end of the world, is it?” ANS: C Use of open-ended questions demonstrates a caring attitude and a willingness to listen. Telling the patient that she “knows how he feels” is incorrect and will be viewed as insincere. The patient feels less masculine as a result of infertility. It is premature and inappropriate to discuss options for alternative means of conception. Telling the patient that the diagnosis is not the end of the world minimizes the patient’s concerns. PTS: 1 DIF: Cognitive Level: Application REF: 923, 927 OBJ: 8 (theory) TOP: Sterility: Self-Concept KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: Coping and Adaptation 10. When teaching a high school boys’ health class, which information about latex condoms is most important for the nurse to include? a. Use petroleum jelly as a lubricant. b. Leave room at the condom tip for a reservoir for semen. c. Discard condoms after three uses. d. Apply the condom immediately before ejaculation. ANS: B Leaving room at the tip of a condom guards against spillage of semen. Petroleum jelly deteriorates latex condoms. Only waterbased lubricants should be used. Condoms should be applied only one time. A condom should be applied with erection; sperm is secreted in pre-ejaculate. PTS: 1 DIF: Cognitive Level: Comprehension REF: 922 OBJ: 3 (theory) TOP: Contraception: Condoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 11. After a fall on a bicycle, a 15-year-old boy is brought to the emergency department complaining of nausea and sudden and acute scrotal pain. There is an absence of the cremasteric reflex. Which problem does the nurse suspect? a. Hydrocele b. Varicocele c. Prostatitis d. Testicular torsion ANS: D Torsion of the testicle often occurs after trauma and manifests in acute scrotal pain, absence of the cremasteric reflex, and nausea/vomiting. A hydrocele (fluid accumulation in the scrotum) is usually painless and causes scrotal enlargement. A variocele is a painful swelling that results when tributary vessels of the spermatic vein dilate and clump. Prostatitis, or inflammation of the prostate, occurs from an infectious agent or other causes. Symptoms include recurrent urinary infection, pelvic pain, and sexual dysfunction and are often mistaken for benign prostatic hyperplasia (BPH). PTS: 1 DIF: Cognitive Level: Comprehension REF: 928 OBJ: 6 (theory) TOP: Torsion: Signs and Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 12. The nurse is caring for an older male patient. Which patient statement would alert the nurse to a probable presence of benign prostatic hyperplasia (BPH)? a. “It takes a long time for me to be able to urinate.” b. “I feel a burning sensation when I urinate.” c. “I have a throbbing pain in my groin.” d. “I have noticed that my urine is very foamy.” ANS: A Difficulty urinating is the first symptom noticed by a person who has BPH. A burning sensation during urination is most consistent with urinary tract infection (UTI). A throbbing sensation in the groin is a nonspecific complaint that could indicate different underlying issues; the nurse should ask the patient additional questions to determine more data. Bubbly or foamy urine may indicate the presence of protein in the urine. PTS: 1 DIF: Cognitive Level: Comprehension REF: 929 OBJ: 6 (theory) TOP: BPH: Signs and Symptoms KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 13. The nurse is teaching a patient with BPH who has a new prescription for finasteride (Proscar). Which information is most important for the nurse to include? a. “It may take several months for this medication to work.” b. “This medication has multiple side effects. c. “This medication will reduce the size of the prostate.” d. “This medication is known as a 5-Alpha-reductase inhibitor (ARIs).” ANS: A The patient should be aware that finasteride (Proscar) is a steroid that may take several months to relieve symptoms. Otherwise, the patient may wrongly think that the medication is not working, which could affect compliance. The medication does have multiple side effects, but the nurse should be more specific about emergent and expected effects and direct the patient to consult the physician if questions arise. The nurse should inform the patient that the medication does reduce the size of the prostate and is known as an ARI, but this information is not most important. PTS: 1 DIF: Cognitive Level: Analysis REF: 929 OBJ: 7 (theory) TOP: BPH: Drug Therapy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 14. The nurse is caring for a patient who returns to the unit after undergoing a transurethral resection of the prostate (TURP). The nurse observes a few small clots and pieces of tissue returning in the indwelling catheter bag. What should the nurse do next? a. Document the finding. b. Notify the surgeon immediately. c. Adjust the bladder irrigation flow rate. d. Apply traction to the catheter. ANS: A Presence of blood clots tissue in the urinary collection is anticipated and normal, so the nurse should document the finding and continue to monitor the patient. These findings do not warrant immediate notification of the surgeon, adjustment of the irrigation rate, or application of traction to the catheter. PTS: 1 DIF: Cognitive Level: Analysis REF: 931 OBJ: 10 (theory) TOP: TURP: Post-Op KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 15. On the first postoperative day, a patient with a TURP complains of abdominal pain. The nurse finds that the bladder is greatly distended. What should the nurse do next? a. Inform the charge nurse. b. Irrigate the indwelling catheter with 20 to 30 mL of normal saline. c. Increase the continuous bladder irrigation flow rate. d. Turn the patient to the right side. ANS: B The patient most likely has a clot that is occluding the catheter and causing pressure on the bladder. Additional irrigation will dislodge the clot that is occluding the catheter. Increasing continuous bladder irrigation flow rate would add fluid to the bladder and increase pain. It is within the primary care nurse’s role to perform the intervention without notifying the charge nurse. Turning the patient to the right side does not offer benefit. PTS: 1 DIF: Cognitive Level: Analysis REF: 931 OBJ: 10 (theory) TOP: Prostatectomy: Occluded Catheter KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 16. The health care provider has recommended that a patient undergo transurethral microwave thermotherapy (TUMT). Which statement correctly explains this procedure? a. The doctor uses a surgical instrument called a resectoscope to trim away excess prostatic tissue. b. The doctor uses a probe with an antenna that releases microwave energy to heat and coagulate prostatic tissue. c. The doctor uses a cystoscope to guide using radiofrequency needles to coagulate prostate tissue. d. The doctor vaporizes and desiccates prostatic tissue. ANS: B The TUMT procedure uses heat to coagulate the prostatic tissue with a probe. A resectoscope trims excess tissue in a transurethral resection of the prostate (TURP) . A transurethral needle ablation (TUNA) uses a cystoscope to guide needles directly into the prostate. A transurethral electrovaporization of the prostate (TUVP) vaporizes and desiccates prostatic tissue. PTS: 1 DIF: Cognitive Level: Understanding REF: 931, Table 39-3 OBJ: 9 (theory) TOP: TUMT: Technique KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 17. A patient who is 3 days postoperative after suprapubic prostatectomy asks, “When can I get rid of this other catheter?” Which data best indicates that nurse can discontinue the suprapubic catheter as ordered? a. Pain is adequately controlled with acetaminophen. b. Urine in the urethral catheter bag is clear with a pink tinge. c. The patient consumed 80% of his lunch. d. The urine residual after voiding is 50 mL. ANS: D After a suprapubic prostatectomy, the patient will have a suprapubic catheter in addition to a urethral catheter. After the urethral catheter is removed (sometime after the third day), the suprapubic catheter is clamped, and the patient attempts to void. Residual urine is measured afterward by unclamping the suprapubic catheter. When there is no more than 60 mL of residual urine after voiding, the suprapubic catheter is removed. Adequate pain control and appetite are signs that the patient is progressing well but do not directly affect suprapubic catheter removal. The urethral catheter will need to be discontinued before the suprapubic catheter is removed. PTS: 1 DIF: Cognitive Level: Analysis REF: 934 OBJ: 3 (clinical) TOP: Suprapubic Prostatectomy: Suprapubic Catheter KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 18. The nurse is educating a patient about testicular self-examination. Which information is most important for the nurse to include? a. Report any lumps larger than a pea to the health care provider. b. Perform weekly self-examinations on the same day of the week. c. Perform self-examinations after bathing when scrotal skin is relaxed. d. Pinch skin for at least 5 seconds. ANS: C Testicular self-examinations are best done after a warm bath or shower when the scrotal skin is relaxed. The patient should report lumps of any size to the health care provider, perform monthly self-examinations, and roll each testicle between the thumb and fingers. PTS: 1 DIF: Cognitive Level: Application REF: 935 OBJ: 11 (theory) TOP: Testicular Self-Examination KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 19. A postoperative prostatectomy patient is discouraged that he is still dribbling and wearing a protective pad 1 month after surgery. Which action should the nurse suggest? a. Eat a low-residue diet to reduce urinary retention. b. Drink grapefruit juice to tighten the urinary sphincter. c. Acquire an indwelling catheter to prevent leakage. d. Practice Kegel exercises several times a day. ANS: D Kegel exercises increase the strength of the perineal floor muscle and will reduce dribbling. Changes in dietary intake, grapefruit juice consumption, or insertion of an indwelling catheter will not provide the restorative care that the patient needs to correct the problem. PTS: 1 DIF: Cognitive Level: Application REF: 934, 937 OBJ: 10 (theory) TOP: Dribbling: Kegel KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 20. The nurse has provided discharge instructions to a patient who underwent a vasectomy. Which statement indicates the patient understands the nurse’s teaching? a. “I can use a heating pad this evening for my discomfort.” b. “Taking aspirin every 4 hours will help with my pain.” c. “I should leave the compression dressing on for the first 24 hours.” d. “I should ice my scrotum once I get home.” ANS: D Instruct the patient to use ice applications and acetaminophen or ibuprofen for scrotal pain and swelling the first 12 to 24 hours postoperatively. The patient should wear jockey shorts or a scrotal support for comfort. Heat is not recommended during the first 24 hours postoperatively. Aspirin may promote bleeding. The patient will not have a compression dressing. PTS: 1 DIF: Cognitive Level: Application REF: 923 OBJ: 3 (theory) TOP: Permanent Contraception: Vasectomy KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 21. The nurse is caring for a patient in the initial hours after having surgery to manage an enlarged prostate. The patient’s postoperative care includes continuous bladder irrigation. Which statement indicates the patient understands the nurse’s teaching? a. “I will be discharged home in about 6 hours.” b. “My urine will likely be a dark tea color as a result of the blood it contains.” c. “I will need to have my bladder irrigated for the first 2 to 3 days.” d. “I should report any bladder spasm immediately because it may indicate a serious complication.” ANS: C The patient will require continuous bladder irrigation or approximately 2 to 3 days. The patient will stay in the hospital for several days. Bloody urine that is red, pink, or watermelon colored is normal during the initial postoperative period. Tea color urine is not associated with this surgical procedure. Bladder spasms are normal and do not necessarily signal complications. PTS: 1 DIF: Cognitive Level: Application REF: 932 OBJ: 11 (theory) TOP: Benign Prostatic Hyperplasia: Postoperative Care KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Physiological Adaptation MULTIPLE RESPONSE 22. The nurse is conducting a presentation to a health class for male high school students. A student questions the nurse about what semen “really is.” Which contents compose semen? (select all that apply.) a. A thick, fructose-filled fluid from seminal vesicles b. Prostaglandins for sperm motility c. Thin, milky secretions from the prostate gland d. Lubricating mucus from the bulbourethral gland e. Spermatozoa ANS: A, B, C, E Semen content includes a thick, fructose-filled fluid from seminal vesicles, prostaglandins for sperm motility, thin, milky secretions from the prostate gland, and spermatozoa. Mucus from the bulbourethral gland is not part of the semen. PTS: 1 DIF: Cognitive Level: Comprehension REF: 921 OBJ: 5 (theory) TOP: Semen: Contents KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 23. Which changes in the male reproductive tract result from age? (select all that apply.) a. Increasingly pendulous scrotum b. Enlarged prostate c. Decreased testosterone d. Increased ejaculate volume e. Shortened arousal time ANS: A, B, C Age-related changes in the male reproductive system include a more pendulous scrotum, an enlarged prostate, and decreased testosterone levels. Ejaculate volume decreases over time, while arousal time lengthens. PTS: 1 DIF: Cognitive Level: Knowledge REF: 922 OBJ: 1 (theory) TOP: Age-Related Changes KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 24. The nurse is planning discharge instruction for a patient who just had a vasectomy. Which information is most important for the nurse to include? (select all that apply.) a. Use a scrotal support for comfort. b. Apply an ice pack to the scrotum for the first 24 hours. c. Wait 3 days before resuming sexual intercourse. d. Use a backup birth control method until the sperm count is negative. e. Return for a follow-up sperm count in 6 months. ANS: A, B, D The patient should use a scrotal support for comfort, apply an ice pack to reduce swelling in the first 12 to 24 hours postprocedure, and use a backup birth control method until the sperm count is negative. The patient should delay intercourse for 1 week, and the follow-up visit should occur 1 year after the sperm count is negative to confirm that the vas deferens is not intact. PTS: 1 DIF: Cognitive Level: Application REF: 922-923 OBJ: 3 (theory) TOP: Vasectomy: Postprocedure Instruction KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 25. The patient considering a vasectomy tells the nurse he is afraid he will be impotent after the surgery. Which statement(s) accurately describe expected outcomes of the procedure? (select all that apply.) a. The procedure will cause sterility without changes in potency. b. The procedure will have a minor impact on libido. c. The procedure will not impact performance. d. The procedure will not impact ejaculate volume. e. The procedure will leave some sperm for several weeks. ANS: A, C, D, E Expected results of a vasectomy include sterility without changes in potency, performance, or ejaculate volume; residual sperm may remain for several weeks. The procedure should not impact libido. PTS: 1 DIF: Cognitive Level: Comprehension REF: 922-923 OBJ: 3 (theory) TOP: Vasectomy Outcomes KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 26. Which factor(s) increase a patient’s risk for developing benign prostatic hyperplasia (BPH)? (select all that apply.) a. Increasing age b. Smoking c. Functioning testes d. Infrequent ejaculation e. Neurogenic bladder ANS: A, C Major risk factors for BPH include increasing age in conjunction with functioning testes. Smoking, infrequent ejaculation, and neurogenic bladder are not significant risk factors for BPH. PTS: 1 DIF: Cognitive Level: Knowledge REF: 929 OBJ: 7 (theory) TOP: BPH: Risk Factors KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 27. Which possible complication(s) may result from benign prostatic hyperplasia (BPH)? (select all that apply.) a. Urinary tract infection (UTI) b. Bladder cancer c. Hydroureter d. Hydronephrosis e. Renal failure ANS: A, C, D, E BPH occurs when the prostate gland enlarges and extends into the bladder neck, causing obstruction of urine flow. UTIs can result from urinary stasis, as the retained urine acts as a medium for organism growth. Gradual dilation of the ureter (hydroureter) and kidneys (hydronephrosis) can occur. Nitrogen products can accumulate in the blood (azotemia) and cause renal failure if the urinary obstruction is not relieved. Bladder cancer is not a complication of BPH. PTS: 1 DIF: Cognitive Level: Comprehension REF: 929 OBJ: 10 (theory) TOP: Complication of BPH KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 28. The nurse is collecting data from a patient who has come to the ambulatory care clinic with complaints of erectile dysfunction. When reviewing the patient’s health history, which finding(s) would provide support for this condition? (select all that apply.) a. History of iron deficiency anemia b. History of treatment for irritable bowel syndrome (IBS) c. History of medications to manage hypertension d. History of insulin-dependent diabetic e. History of bipolar disorder ANS: C, D, E Medications and health conditions may predispose the patient to erectile dysfunction. Medications used in the management of hypertension may be associated with erectile dysfunction. Vascular changes experienced by the patient with diabetes may be associated with difficulty having and/or maintaining an erection. Depression may result in difficulty attaining an erection. Sickle cell anemia and not iron deficiency anemia is associated with erectile dysfunction. IBS does not heighten the risk for developing erectile dysfunction. PTS: 1 DIF: Cognitive Level: Understanding REF: 925 OBJ: 6 (theory) TOP: Erectile Dysfunction: Clinical Cues KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation MATCHING The nurse teaches helpful terminology related to male reproductive disorders to a patient. Match the condition with the characteristic that best describes it. a. Hydrocele b. Varicocele c. Priapism d. Peyronie disease e. Torsion 29. Prolonged erection associated with sickle cell anemia 30. Erection curving upward preventing vaginal penetration 31. Painless enlargement of the scrotum from fluid accumulation 32. Twisting of testes and spermatic cord 33. Painful left-sided scrotal edema from clumping and dilation of vessels of the spermatic vein 29. ANS: C PTS: 1 DIF: Cognitive Level: Knowledge REF: 928 OBJ: 6 (theory) TOP: Male Reproductive Disorders KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 30. ANS: D PTS: 1 DIF: Cognitive Level: Knowledge REF: 928 OBJ: 6 (theory) TOP: Male Reproductive Disorders KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 31. ANS: A PTS: 1 DIF: Cognitive Level: Knowledge REF: 928 OBJ: 6 (theory) TOP: Male Reproductive Disorders KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 32. ANS: E PTS: 1 DIF: Cognitive Level: Knowledge REF: 928 OBJ: 6 (theory) TOP: Male Reproductive Disorders KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 33. ANS: B PTS: 1 DIF: Cognitive Level: Knowledge REF: 928 OBJ: 6 (theory) TOP: Male Reproductive Disorders KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance Chapter 40: Care of Patients with Sexually Transmitted Infections deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is caring for a homosexual man with a rectal tear and inflamed rectal tissue. The nurse understands that these findings increase the patient’s risk for which disorder? a. An abscess b. Human immunodeficiency virus (HIV) infection c. Hemorrhoids d. Rectal hemorrhage ANS: B Open lesions and inflamed tissue increase the risk of HIV infection. PTS: 1 DIF: Cognitive Level: Comprehension REF: 941 OBJ: 7 (theory) TOP: Exposure to HIV KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 2. The nurse instructs a sexually active teenager that frequent douching can cause which infection? a. Syphilis b. Bacterial vaginosis c. Pelvic inflammatory disease (PID) d. Purulent vaginitis ANS: B Bacterial vaginosis is caused when frequent douching changes the pH of the vaginal vault and creates an environment conducive to bacterial invasion. Sexually transmitted infections (STIs) like syphilis are not transferred by douching. PID is a condition that most often results from an untreated infection. Vaginitis is an inflammatory condition that does not result from douching. PTS: 1 DIF: Cognitive Level: Comprehension REF: 942 OBJ: 9 (theory) TOP: Vaginosis: Douching KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 3. Why are women at a greater risk for contracting sexually transmitted infections (STIs) than men? a. Male secretions are in contact with female mucous membranes for longer periods of time. b. Estrogens increase susceptibility of vaginal membranes. c. Penile friction to the vaginal wall encourages STIs. d. Changing hormonal levels create a vaginal environment conducive to bacterial growth. ANS: A Male secretions are in contact with female mucous membranes longer than female secretions are in contact with the penis. Estrogen provides for vaginal lubrication and therefore reduces friction and tissue tearing. PTS: 1 DIF: Cognitive Level: Comprehension REF: 942 OBJ: 1 (theory) TOP: Female Incidence of STIs KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 4. The nurse is educating a sexually active female patient about infection prevention. Which change during the premenstrual period increases the patient’s risk of infection? a. Cervical secretions become more alkaline. b. The cervical mucous plug becomes more permeable. c. Higher estrogen levels increase vaginal lubrication. d. Lower antibody levels increase risk for infection. ANS: B The mucous plug in the cervix of women provides protection to the upper genital tract. The hormonal changes make it become more permeable around the menstrual period. This change can result in an increased risk for infections in the upper genital tract, such as pelvic inflammatory disease (PID). Oral contraceptives alter cervical secretions and result in a more alkaline environment. Vaginal lubrication does not increase risk of infection, and antibody levels do not lower during the premenstrual period. PTS: 1 DIF: Cognitive Level: Comprehension REF: 942 OBJ: 3 (clinical) TOP: PID: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 5. Which statement indicates that a patient needs additional education about the vaccine for human papillomavirus (HPV)? a. “I know I must have three doses of the vaccine.” b. “Girls as young as 9 years of age may be vaccinated.” c. “I am relieved that the vaccine protects me from all HPV infections.” d. “I know I should continue having regular Pap smears.” ANS: C The vaccine protects against the most prevalent infections, genital warts and precancerous cervical lesions, but not against all HPV infections. The remaining statements are correct. PTS: 1 DIF: Cognitive Level: Application REF: 943 OBJ: 3 (clinical) TOP: HPV: Vaccinations KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 6. During an assessment of an older adult patient, the nurse observes a red rash on the palms of the hands and the soles of the feet. What should the nurse do next? a. Notify the charge nurse. b. Float the patient’s heels on a pillow. c. Apply a prescribed emollient. d. Reposition the patient on the left side. ANS: A A red rash on the palms of the hands and the soles of the feet is consistent with the secondary phase of syphilis. The nurse should notify the charge nurse and health care provider to allow for further workup and treatment as indicated. Floating the patient’s heels or repositioning addresses prevention of skin breakdown, and emollients help decrease dry skin. PTS: 1 DIF: Cognitive Level: Application REF: 943 OBJ: 8 (theory) TOP: Syphilis: Skin Lesions KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 7. Once a diagnosis of syphilis is confirmed, the nurse understands that she must report the illness to which entity? a. The World Health Organization (WHO) b. The Centers for Disease Control and Prevention (CDC) c. The hospital infection control department d. The local public health agency ANS: D STIs are reported to the local public health agency for accumulation by the CDC. The local public health agency will get in touch with the sexual contacts of the patient and attempt to initiate treatment. PTS: 1 DIF: Cognitive Level: Application REF: 943 OBJ: 3 (clinical) TOP: Reporting STIs KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 8. A female patient comes to the emergency department with severe abdominal pain, a temperature of 101° F, and a foulsmelling, purulent vaginal discharge. The nurse recognizes that these findings are consistent with which infection? a. Pelvic inflammatory disease (PID) b. Gonorrhea c. Syphilis d. Vaginosis ANS: A Fever, abdominal pain, and purulent discharge are cardinal indicators of PID. Gonorrhea most often presents in females with vaginal discharge and burning with urination. The initial state of syphilis presents with chancre (hard, painless sore) on the mucous membrane of the mouth or genitals. Vaginosis most often presents with symptoms including a grayish-white discharge that has a fishy odor. PTS: 1 DIF: Cognitive Level: Application REF: 942 OBJ: 1 (theory) TOP: PID: Signs and Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 9. After being stained with crystal violet, how will a gram-positive gonococcus react? a. Fluoresce after counterstain is applied. b. Accept the counterstain. c. Retain the original stain after the counterstain is applied. d. Turn dark after the counterstain is applied. ANS: C Staining procedures differentiate organisms by using dyes that have been found to stain some bacteria in specific ways. An example of this would be a Gram stain, in which bacteria are first stained with crystal violet, then treated with a strong iodine solution, decolorized with ethanol or ethanol acetone, and then counterstained with contrasting dye. Those retaining the initial stain are considered gram positive; those losing the stain but accepting the counterstain are considered gram negative. PTS: 1 DIF: Cognitive Level: Application REF: 950 OBJ: 3 (theory) TOP: Gram Stain: Significance KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 10. When caring for a male patient with a suspected gonorrheal infection, which action is most important for the nurse to take? a. Report the infection to the local public health agency. b. Assess the patient’s temperature hourly. c. Administer antibiotics before cultures are drawn. d. Wait 1 hour after the patient voids to collect a urethral swab. ANS: D Since the urine will have flushed out the organisms, the nurse should wait at least 1 hour postvoid before collecting the specimen. The infection has not been confirmed, so no report should be made at this time. The patient’s temperature should be obtained each shift. Administering antibiotics before cultures are drawn may cause cultures to be negative even though the drug or the dose may not be sufficient to cure the infection. If possible, obtain cultures prior to administering antibiotics. PTS: 1 DIF: Cognitive Level: Application REF: 950 OBJ: 3 (theory) TOP: Gonorrhea Swab: Technique KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 11. The nurse is educating a young woman newly diagnosed with genital herpes. Which information is most important for the nurse to include in the teaching plain? a. Take the entire course of antibiotics. b. Increase fluid intake to dilute urine. c. Wash hands after applying topical ointment to lesions. d. Avoid all sexual contact until lesions completely resolve. ANS: D To prevent spreading genital herpes, the patient should avoid sex until all the lesions are gone. Genital herpes is a viral condition and symptoms can be managed by antiviral medication. Increasing fluid intake will help to dilute urine and can manage pain, but is of lesser importance than preventing the spread of genital herpes. The patient should don gloves when applying topical ointment. PTS: 1 DIF: Cognitive Level: Application REF: 951 OBJ: 1 (clinical) TOP: Herpes: Prevention of Contagion KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 12. The nurse is caring for a patient with genital herpes. Which manifestation alerts the nurse to a potential signal of an impending outbreak? a. Elevation in temperature b. Tingling sensation in the vagina c. Copious vaginal discharge d. Migraine-like headache ANS: B Many women with herpes can predict an outbreak because of tingling or burning in the vagina. Elevations in temperature, increased vaginal discharge, and headaches are not common precursors of a herpes outbreak. PTS: 1 DIF: Cognitive Level: Comprehension REF: 945 OBJ: 1 (clinical) TOP: Herpes: Warning of Outbreak KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 13. How long after exposure does the incubation period for gonorrhea last? a. 2 to 6 days b. 1 week c. 2 weeks d. 4 weeks ANS: A The incubation period is 2 to 6 days before symptoms may appear. PTS: 1 DIF: Cognitive Level: Knowledge REF: 946 OBJ: 6 (theory) TOP: Gonorrhea: Incubation Time KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 14. The nurse is aware that men with gonorrhea are more likely to seek medical attention because their symptoms are more visible than those of women. Which clinical manifestation is most consistent with symptoms of gonorrhea in men? a. Copious, purulent penile discharge b. Hematuria when initiating the stream of urine c. Penile ulcers with a foul odor d. Scaly scrotal lesions ANS: A Signs and symptoms of gonorrhea in men include purulent penal discharge and scrotal pain. Gonorrhea should not cause hematuria when urinating, penile ulcers with a foul odor, or scaly scrotal lesions. PTS: 1 DIF: Cognitive Level: Comprehension REF: 946 OBJ: 5 (theory) TOP: Gonorrhea: Male Signs KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 15. Which patient is exhibiting manifestations consistent with the primary stage of syphilis? a. A female patient with copious vaginal discharge b. A male patient with a generalized skin rash c. A female patient with a painless nodule on her vagina d. A male patient with a gumma ANS: C Syphilis has three stages. The chancre, or painless, hard nodule, is visible in the primary stage of syphilis and disappears within a few weeks. The secondary stage occurs approximately 6 weeks later; symptoms may include a generalized skin rash. In tertiary syphilis, spirochetes access to all body tissues and a gumma (a soft encapsulated tumor) may appear on any organ. PTS: 1 DIF: Cognitive Level: Comprehension REF: 948 OBJ: 8 (theory) TOP: Syphilis: Primary Stage KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 16. The nurse is caring for a patient with syphilis. Which manifestation indicates that the syphilis has progressed to the secondary stage? a. Foul-smelling penile discharge b. Positive serology c. Purulent skin rash d. Scrotal swelling ANS: B A positive serology will appear in the secondary stage of syphilis. Penile discharge is not associated with the secondary stage of syphilis. A generalized skin rash, not purulent, may be seen in the secondary stage of syphilis. Scrotal swelling is not associated with syphilis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 948 OBJ: 8 (theory) TOP: Syphilis: Secondary Stage KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 17. The nurse is educating a pregnant patient who is human immunodeficiency virus (HIV) positive. Which information is most important for the nurse to include in the teaching plan? a. Breast-feeding is always best. b. Talk with your doctor about a vaginal delivery. c. Engage in oral, rather than vaginal, sex. d. Remain on the medication protocol. ANS: D Remaining on medication is essential. Certain prescribed drug combinations may significantly reduce the transmission to the fetus. Patients with HIV should avoid breast-feeding and cesarean birth. HIV can be spread by oral sex. PTS: 1 DIF: Cognitive Level: Application REF: 947 OBJ: 2 (clinical) TOP: HIV: Preventive Actions KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 18. A patient has been diagnosed with chlamydia for the second time in a 5-month period. Data collection reveals that the patient was not compliant with the plan of treatment with the last infection. Which medication does the nurse anticipate that the provider will prescribe? a. Doxycycline b. Erythromycin c. Diflucan d. Azithromycin ANS: D Chlamydia is best treated with a single dose of azithromycin for patients having a compliance problem. Doxycycline requires a 7- day course of therapy and may not be best given this patient’s history. Erythromycin is indicated to manage the disease in pregnant women. Diflucan is an antifungal medication used in the management of candidiasis. PTS: 1 DIF: Cognitive Level: Comprehension REF: 944 OBJ: 4 (theory) TOP: Table 41-1 Common STIs KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 19. The nurse is collecting information from a patient during her annual pelvic examination. The patient reports that she has noted a strong vaginal odor after intercourse. Which condition may be present? a. Gonorrhea b. Bacterial vaginosis c. Chlamydia d. Syphilis ANS: C Chlamydia may cause a strong vaginal odor noted after sexual intercourse. Gonorrhea causes vaginal discharge and a difficulty voiding. Bacterial vaginosis is associated with a fishy vaginal odor and discharge. Syphilis causes a chancre sore. PTS: 1 DIF: Cognitive Level: Comprehension REF: 944 OBJ: 4 (theory) TOP: Table 41-1 STIs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation MULTIPLE RESPONSE 20. Which routes are ways in which sexually transmitted infections (STIs) are transmitted? (select all that apply.) a. Sexual intercourse b. Oral-genital route c. Contact with infected blood d. Placenta to infant e. Contact with infected body fluids ANS: A, B, C, D, E All options listed are possible transmission routes for STIs. PTS: 1 DIF: Cognitive Level: Application REF: 941 OBJ: 3 (clinical) TOP: STIs: Transmission KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 21. To which factor(s) can the rise in the number of sexually transmitted infections (STIs) be attributed? (select all that apply.) a. An increase in the number of sexually active teenagers b. An increase in the opportunity to have multiple partners c. A knowledge deficit about signs and symptoms of STIs d. Teenagers being reluctant to report diseases e. Young people’s increasing ability to acquire confidential health care ANS: A, B, C, D Rising numbers of STIs may be attributed to an increase in the number of sexually active teenagers, an increase in the opportunity to have multiple partners, a knowledge deficit about signs and symptoms of STIs, and teenagers being reluctant to report diseases. Young people are often unable to acquire confidential health care. PTS: 1 DIF: Cognitive Level: Comprehension REF: 941 OBJ: 1 (clinical) TOP: Increasing Incidence of STIs KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 22. How can the use of oral contraceptives increase the risk of acquiring a sexually transmitted infection (STI)? (select all that apply.) a. Oral contraceptives cause bone marrow suppression. b. Oral contraceptives cause an alkaline vaginal environment. c. Oral contraceptives may reduce the perception of the need for condom use. d. Oral contraceptives decrease the inflammatory response. e. Oral contraceptives must be taken regularly in order to be effective. ANS: B, C, E The use of oral contraceptive pills causes the vaginal vault to become alkaline from cervical secretions, which makes for a conducive environment for STIs. Oral birth control pills make the need for a condom redundant as pregnancy will be averted by the medication. Oral contraceptives do not cause bone marrow suppression, and while birth control must be taken regularly in order to be effective, this contributes to the risk of pregnancy, not an STI. PTS: 1 DIF: Cognitive Level: Application REF: 942 OBJ: 3 (clinical) TOP: Oral Contraceptive: Effect on Rising STI Incidence KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 23. Which sexually transmitted infections (STIs) must be reported? (select all that apply.) a. Vaginitis b. Gonorrhea c. Pelvic inflammatory disease. d. Chlamydia e. Lymphogranuloma ANS: B, C, D, E All STIs listed are reportable in all states except for vaginitis. Syphilis is also a reportable STI. However, each state may add others to that list. PTS: 1 DIF: Cognitive Level: Knowledge REF: 943 OBJ: 3 (clinical) TOP: Reportable STIs KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 24. Which factors indicate reasons why young patients are frequently reluctant to have their sexually transmitted infections (STIs) reported? (select all that apply.) a. Fear of parental reaction b. Embarrassment about their condition c. Fear of reprisal from identified contacts d. Fear of information becoming public e. Fear of rejection by peers ANS: A, B, C, D, E All options are realistic concerns about reporting contacts. PTS: 1 DIF: Cognitive Level: Analysis REF: 951 OBJ: 3 (clinical) TOP: Reporting STIs: Reasons for Reluctance KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 25. A patient who has been diagnosed with chlamydia is started on a protocol of doxycycline. Which information is important for the nurse to include in the teaching? (select all that apply.) a. The partner does not need treatment. b. Use a condom to protect partners from disease. c. Chlamydia can develop into pelvic inflammatory disease (PID). d. Take the entire prescription of antibiotics. e. Chlamydia can result in an ectopic pregnancy. ANS: B, C, D, E The patient should understand the importance of using condoms to protect her partner and taking the entire course of antibiotics to prevent resistance or relapse. The patient should also understand that chlamydia increases the risk of developing PID or an ectopic pregnancy. The patient’s partner should receive treatment as well. PTS: 1 DIF: Cognitive Level: Application REF: 944 OBJ: 3 (clinical) TOP: Chlamydia: Instructions KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 26. The nurse urges a female patient with gonorrhea to seek medical care. Which complication(s) can occur if gonorrhea is left untreated? (select all that apply.) a. Ppelvic inflammatory disease (PID) b. Sterility c. Obstructed fallopian tubes d. Ectopic pregnancy e. Ophthalmia neonatorum in the newborn ANS: A, B, C, D, E All options are possible complications from untreated gonorrhea. PTS: 1 DIF: Cognitive Level: Application REF: 946 OBJ: 6 (theory) TOP: Gonorrhea: Complications KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 27. The nurse is providing information to a patient who has recently been diagnosed with genital herpes. Which statements indicate the need for further instruction? (select all that apply.) a. “I am only contagious when I have open sores.” b. “The infection is limited to only my genital region.” c. “There is no permanent cure for this condition.” d. “I will need to contact my physician for antibiotic cream for the open lesions whenever I have an outbreak.” e. “I should wash my hands carefully to prevent introduction of bacteria to the area.” ANS: A, B, D The disease may be spread during outbreaks. It is possible to spread the infection with viral shedding between outbreaks. Herpes is a lifelong condition. There is no cure. The condition’s treatment can include the administration of antiviral medication. Antibiotics are not typically indicated unless a secondary bacterial infection develops. Proper hand hygiene is important to prevent both further spreading of the virus and introduction of bacteria to the affected area. PTS: 1 DIF: Cognitive Level: Application REF: 945 OBJ: 4 (theory) TOP: Table 41-1 Common STIs KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance COMPLETION 28. The nurse recommends that the newly diagnosed patient with herpes get current information about her disease from the local _______________. ANS: health department The health department has clinics and written information in several languages that would be helpful to the newly diagnosed person. PTS: 1 DIF: Cognitive Level: Application REF: 953 OBJ: 4 (theory) TOP: STIs: Information Source KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance Chapter 41: The Integumentary System deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. What underlying pathophysiology explains the gradual graying of an older adult’s hair? a. Reduced hair follicles b. Less sebaceous gland activity c. Loss of collagen fibers in dermis d. Decreased melanocytes at hair follicle ANS: D Reduction in melanocytes at the hair follicle is the cause of graying hair. A reduction in the number of hair follicles will result in thinning hair. Reduced sebaceous gland activity and collagen will result in drying. PTS: 1 DIF: Cognitive Level: Comprehension REF: 957 OBJ: 2 (clinical) TOP: Skin Assessment: Hair KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 2. An 80-year-old resident prefers to lie in bed on her left side. The nurse anticipates that the risk for skin breakdown is greatest over which area? a. Left buttock b. Left heel c. Left trochanter d. Left ribs ANS: C The areas that are most prone to break down in the immobile patient are over bony prominences. PTS: 1 DIF: Cognitive Level: Application REF: 963 OBJ: 5 (theory) TOP: Pressure Ulcer: Risk KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 3. Which chemical irritant causes the most damage to skin of the immobilized patient? a. Urine b. Topical medication c. Bath soap d. Laundry soap ANS: A Urine and feces are the most common chemical irritants that cause skin breakdown. PTS: 1 DIF: Cognitive Level: Comprehension REF: 957 OBJ: 5 (theory) TOP: Skin Injury: Chemical KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 4. The nurse observes the CNA who is changing a patient’s bed. Which action demonstrates that the CNA requires additional teaching? a. Lifting the patient on the draw sheet to the stretcher. b. Pulling the draw sheet out from under the patient. c. Rolling the patient to the side to change the draw sheet. d. Using the gait belt to lift the patient from the bed to a wheelchair. ANS: B Pulling linens out from under a patient instead of rolling or lifting the patient causes a shearing type of skin tear. Use of a lift sheet, rolling the patient from side to side, and the use of the gait belt are recommended. PTS: 1 DIF: Cognitive Level: Application REF: 959 OBJ: 5 (theory) TOP: Skin Injury: Shearing KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 5. When planning care for an 80-year-old African American woman, which intervention is most important for the nurse to include? a. Bathe the patient twice weekly. b. Use liberal amounts of soap and water. c. Use quick, brisk motions to dry the patient’s skin. d. Apply emollient to limbs and back. ANS: B People with dark complexions need to be bathed frequently due to the oiliness of their skin. Liberal amounts of water and soap are beneficial. Twice weekly bathing is insufficient for cleanliness. Friction and application of emollient are not conducive to skin health. PTS: 1 DIF: Cognitive Level: Application REF: 958, Older Adult Care Points OBJ: 4 (theory) TOP: Bathing: Dark Complexion Considerations KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 6. A 93-year-old resident eats only a few bites at meals and then refuses to eat more. Which intervention might the nurse use to help delay skin breakdown from diminished nutrition? a. Spoon-feed the resident. b. Request an order for a feeding tube. c. Inform the resident of the need to increase intake. d. Offer 4 ounces of fluid every hour. ANS: D Dehydration can cause loss of skin turgor and predisposes the skin to break down. Spoon-feeding and instructing about increased intake may only result in a power struggle with the resident. PTS: 1 DIF: Cognitive Level: Comprehension REF: 959 OBJ: 2 (theory) TOP: Skin Damage: Dehydration KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 7. The school nurse is advising a group of high school girls about ways to avoid permanent skin damage from sun exposure. Which information is most important to include in the teaching plan? a. Avoid using cosmetics that have sunscreen added. b. Consider a spray tan in the summer. c. Limit sunbathing times on a cloudy day. d. Wear light, loose clothing while in sun. ANS: B A spray-on tan is the safest method to acquire a tan. Cosmetics with added sunscreen are an easy way to remember to protect the face from the sun. Ultraviolet (UV) rays can penetrate clouds and loose clothing. PTS: 1 DIF: Cognitive Level: Application REF: 958 OBJ: 10 (theory) TOP: Avoiding UV Skin Damage KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 8. Which method is best to use for lotion application? a. Avoid shaking lotion to prevent bubble formation. b. Apply lotion heavily as the water from lotion evaporates. c. Wash off residue before applying fresh lotion. d. Apply a scant film of lotion on eyelids and in the nose. ANS: C The residue from previous applications should be removed before applying fresh lotion. Shaking lotion is not harmful, lotion should not be applied to damp skin, and application should be avoided on sensitive areas around the eyes and in the nose. PTS: 1 DIF: Cognitive Level: Application REF: 966, Box 41-3 OBJ: 3 (clinical) TOP: Lotion: Application KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 9. Which statement best describes a “shave biopsy” of a skin lesion? a. A removal of the central core of a lesion b. Excision of an entire lesion with a -inch border around it c. Removal of the top of a lesion that stands above the skin line d. Excision of a lesion down to the dermis ANS: C The shave biopsy removes the top level of the lesion, which stands above the skin line. Removal of a core from the center of the lesion is referred to as a punch biopsy. Excision of the entire lesion is an excisional biopsy. PTS: 1 DIF: Cognitive Level: Comprehension REF: 960 OBJ: 7 (theory) TOP: Shave Biopsy: Technique KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 10. Which intervention is most important for a person who is in a wheelchair for long periods? a. Reposition self every 2 hours. b. Lift weight on the arms of the chair every 15 minutes. c. Massage bony prominences of the buttocks and hips. d. Use a donut device to keep weight off of the buttocks. ANS: B Lifting or off-loading weight every 15 minutes while in a wheelchair will reduce the threat of pressure ulcer. Tissue anoxia can result in less than 2 hours. Movement to shift weight every 15 minutes is most effective. Massage can damage delicate tissues in the at-risk patient. The donut device reduces circulation to the area compressed and is contraindicated. PTS: 1 DIF: Cognitive Level: Application REF: 959 OBJ: 5 (theory) TOP: Pressure Ulcer: Prevention KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 11. The nurse is assessing an older adult patient’s hydration status. The nurse observes that a fold of skin on the upper chest returns to normal position. The nurse should conclude that hydration is adequate if the skin returns to normal position in how many seconds? a. 6 seconds b. 9 seconds c. 10 seconds d. 15 seconds ANS: A If the tented skinfold takes more than 8 seconds to return to normal position, the patient is considered to be dehydrated. PTS: 1 DIF: Cognitive Level: Knowledge REF: 962, Older Adult Care Points OBJ: 2 (clinical) TOP: Test for Dehydration KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 12. The nurse teaches the patient the “ABCD” technique for evaluating melanomas. What does the “D” in this memory prompt represent? a. Darkness b. Drainage c. Dimpling d. Diameter ANS: D The “D” stands for diameter. The “A” is for asymmetrical, the “B” is for border, and the “C” is for color change. PTS: 1 DIF: Cognitive Level: Comprehension REF: 962 OBJ: 1 (clinical) TOP: “ABCD” Guide to Melanoma Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 13. The student nurse is preparing to document a suspicious area over a bony prominence. Which description would be most appropriate? a. Reddened area on left hip b. Reddened, nonblanching area approximately 1 cm × 1 cm c. Suspicious area over left trochanter d. Nonblanching area over left trochanter 0.8 cm × 1.2 cm ANS: D The area should be described as to location, appearance, and exact measurement. PTS: 1 DIF: Cognitive Level: Application REF: 963 OBJ: 2 (clinical) TOP: Stage I Pressure Ulcer: Documentation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 14. A newly admitted 86-year-old patient has scratch marks in the groin and axilla and on her limbs. There are small, punctate red lesions that the patient says itch “like crazy.” Which nursing action is most appropriate? a. Employ skin tear precautions b. Employ Standard Precautions c. Employ use of emollient d. Employs focused assessment for cause ANS: B The patient is most likely suffering from scabies. The nurse should employ Standard Precautions in order to avoid the spread of infection. PTS: 1 DIF: Cognitive Level: Application REF: 960, 963 OBJ: 3 (theory) TOP: Scabies: Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 15. After a medicated bath, the patient is assisted from the tub. Which statement about lotion application is correct? a. Apply lotion immediately after drying the patient. b. Apply lotion in a thick layer to warm skin. c. Apply lotion after returning the patient to bed. d. Allow the patient to apply the lotion. ANS: A Medication is applied in a thin layer as soon as the patient has completed a bath. Applying the lotion in a thick layer, waiting to apply the lotion, or deferring the lotion application to the patient is not appropriate. PTS: 1 DIF: Cognitive Level: Application REF: 966 OBJ: 3 (clinical) TOP: Medicated Bath and Lotion KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 16. The nurse is caring for a patient with an order for an “open dressing.” Which action indicates that the nurse accurately understands the order? a. The nurse leaves the entire lesion open to air. b. The nurse changes wet compresses frequently enough to keep them wet. c. The nurse applies medicated ointment directly in the open wound. d. The nurse applies dressings to the perimeter of the wound while leaving the center of the wound open to air. ANS: B An open dressing is a wet dressing that is kept that way, but the dressed lesion is not covered with an occlusive dressing. The dressing should be changed with each application. PTS: 1 DIF: Cognitive Level: Application REF: 966 OBJ: 3 (clinical) TOP: Open Dressings KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 17. The nurse is providing discharge teaching of a patient. Which instructions should the nurse include to teach reduction of soap in bed linens and sleeping garments? a. Only use high-efficiency detergents. b. Use vinegar in the rinse water. c. Only wash clothing in hot water. d. Send linens to a professional laundry. ANS: B The use of vinegar in the rinse water will cut soap that may be irritating to the skin if left in bed linens or sleeping garments. The type of washing machine that the patient owns determines whether or not high-efficiency detergent is necessary. Not all clothing may be washed in hot water. Professional laundry services are not necessary. PTS: 1 DIF: Cognitive Level: Comprehension REF: 966 OBJ: 7 (theory) TOP: Laundry Precautions KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 18. The nurse is caring for a patient and during the assessment, observes a full-thickness 2 cm × 1 cm skin tear on the right buttock. How should the nurse stage this pressure ulcer? a. Category I b. Category II c. Category III d. Category IV ANS: C Category III skin tears have complete tissue loss in which the epidermal flap is missing. Category I skin tears do not have tissue loss. Category II skin tears reflect a partial tissue loss. There is no Category IV. PTS: 1 DIF: Cognitive Level: Comprehension REF: 959 OBJ: 2 (clinical) TOP: Skin Tears KEY: Nursing Process Step: Diagnosis MSC: NCLEX: Physiological Integrity: Physiological Adaptation 19. The nurse is teaching a group of teenagers about skin care and sun damage. Which statement by a participant indicates the need for further instruction? a. “Although I have a darker complexion, I am still at risk for sun damage.” b. “The safest time of day to engage in water sports and avoid sun damage is from 10 A.M. to noon.” c. “My sunscreen should ideally have SPF 30 or higher.” d. “It is important to apply sunscreen about 30 minutes before sun exposure.” ANS: B The rays of the sun are most damaging between 10 A.M. and 2 P.M. standard time. Individuals having darker complexions are still at risk for sun damage. The sunscreen should have a minimum of 30 SPF. The application of sunscreen 15 to 30 minutes before sun exposure is needed. PTS: 1 DIF: Cognitive Level: Application REF: 958, Health Promotion OBJ: 4 (theory) TOP: Health Promotion: Sun Exposure Precautions KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 20. The patient reports to the nurse that the physician has ordered a Wood light examination. The nurse correctly recognizes the physician is concerned that the patient may have which condition? a. Tinea corpus b. Scabies c. Herpes simplex d. Dermatitis ANS: A The Wood light is a specially designed ultraviolet (UV) light source. It is helpful in the diagnosis of fungal infections such as tinea corpus. PTS: 1 DIF: Cognitive Level: Comprehension REF: 957 OBJ: 6 (theory) TOP: Microscopic Tests KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 21. A skin biopsy has been scheduled on a patient to rule out the presence of a malignancy. Which instruction is most important for the nurse to include in patient teaching? a. General anesthesia will be used during the procedure. b. Change the bandage the day after the procedure and then weekly for 2 weeks. c. Sutures placed at the site of the biopsy will be removed in approximately 10 days. d. Do not eat or drink anything after midnight the night before the procedure. ANS: C A skin biopsy can be used to rule out a malignancy or to diagnose the causative organism in a lesion. Sutures will be removed in 10 to 14 days after the procedure. The procedure will be performed under local anesthesia, the bandage should be changed daily, and no preprocedure preparation is required. PTS: 1 DIF: Cognitive Level: Application REF: 960 OBJ: 6 (theory) TOP: Diagnostic Tests and Procedures: Skin Biopsy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential MULTIPLE RESPONSE 22. Which age-related change(s) occur(s) in the integumentary system? (select all that apply.) a. Elastic fibers and adipose tissue diminish. b. Skin thins and becomes transparent. c. Hair thickens as follicles decrease. d. Skin becomes dry. e. Thinned skin leads to cold intolerance. ANS: A, B, D, E With age, elastic fibers and adipose tissue diminish, skin thins and becomes transparent, skin becomes dry, and thinned skin leads to cold intolerance. Hair thins as follicles decrease. PTS: 1 DIF: Cognitive Level: Knowledge REF: 956-958 OBJ: 1 (theory) TOP: Age-Related Changes to Integument KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 23. The nurse is advising an older adult regarding age-appropriate bathing practices. Which instruction(s) is/are most important for the nurse to include? (select all that apply.) a. Using lotion-based soaps. b. Using hot water to stimulate skin. c. Towel skin dry with quick, brisk motions. d. Apply lotion twice a day. e. Apply talcum powder after bathing. ANS: A, D The nurse should suggest actions that help keep the skin moist, like using lotion-based soaps and applying lotion twice daily. Using hot water, vigorously towel-drying skin, and applying talcum powder are actions that increase skin dryness. PTS: 1 DIF: Cognitive Level: Application REF: 958, Older Adult Care Points OBJ: 2 (theory) TOP: Older Adult: Bathing KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 24. Which factor(s) could increase the risk for skin tears in a 90-year-old resident? (select all that apply.) a. Incontinence b. Bruised areas c. Obesity d. Prolonged use of corticosteroids e. History of congestive heart disease ANS: B, D, E Older adults have a high risk for the development of skin tears. Risk factors that will further increase the likelihood for developing tears include the presence of bruises, prolonged use of corticosteroids, and systemic conditions such as a history of congestive heart failure. Incontinence and obesity are associated with the incidence of pressure ulcers. PTS: 1 DIF: Cognitive Level: Application REF: 959, Box 41-1 OBJ: 2 (theory) TOP: Skin Tears: Risk Factors in the Elderly KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 25. An 86-year-old resident struck her forearm on a table, causing a category I L-shaped skin tear 6 cm × 2 cm. Which action(s) is/are appropriate for the nurse to take? (select all that apply.) a. Clean the tear with alcohol. b. Approximate the edges of the tear. c. Secure the skin flap with Steri-Strips. d. Cover with a nonadherent dressing. e. Assess closely for 5 days for signs of infection. ANS: B, C, D, E Alcohol would act as an irritant to the skin tear and should be avoided. Cleansing with normal saline is recommended. The remaining options are appropriate for the management of the skin tear. PTS: 1 DIF: Cognitive Level: Application REF: 959, Box 41-2 OBJ: 5 (theory) TOP: Skin Tears: Interventions KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential COMPLETION 26. The nurse reminds the junior high school health class that the first line of defense from pathogens for the body is the ____________. ANS: skin The intact skin is the first defense of the body from pathogens. PTS: 1 DIF: Cognitive Level: Knowledge REF: 957 OBJ: 1 (theory) TOP: Skin: First Line of Defense KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance MATCHING The nurse uses a picture to show the structure of the integument. Match the options with the characteristic that best describes them. (Each option may be used once, more than once, or not at all.) a. Epidermis b. Dermis c. Sebaceous glands d. Sweat glands 27. Squamous epithelium, no blood vessels 28. Contains vessels, nerves, and hair follicles 29. Keeps skin and hair pliable 30. Consists of dense connective tissue 31. Excretes water and salt 27. ANS: A PTS: 1 DIF: Cognitive Level: Knowledge REF: 955 OBJ: 1 (theory) TOP: Integumentary Structures and Function KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 28. ANS: B PTS: 1 DIF: Cognitive Level: Knowledge REF: 955 OBJ: 1 (theory) TOP: Integumentary Structures and Function KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 29. ANS: C PTS: 1 DIF: Cognitive Level: Knowledge REF: 955 OBJ: 1 (theory) TOP: Integumentary Structures and Function KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 30. ANS: B PTS: 1 DIF: Cognitive Level: Knowledge REF: 955 OBJ: 1 (theory) TOP: Integumentary Structures and Function KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 31. ANS: D PTS: 1 DIF: Cognitive Level: Knowledge REF: 955 OBJ: 1 (theory) TOP: Integumentary Structures and Function KEY: Nursing Process Step: N/A MSC: NCLEX: N/A The nurse clarifies the descriptive terms for skin disorders. Match each option with the characteristic that best describes it. a. Erythrasma b. Wheal c. Fungal infection d. Keratosis e. Keloid 32. Thick ridge of scar tissue 33. Fluoresces under Wood light 34. Chronic bacterial infection in skinfolds, especially axilla and between toes 35. Smooth, elevated area that is pale or reddened 36. Benign wartlike lesions on trunk, arms, and scalp 32. ANS: E PTS: 1 DIF: Cognitive Level: Comprehension REF: 962-963, Table 41-1 OBJ: 2 (clinical) TOP: Skin Lesions: Characteristics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 33. ANS: C PTS: 1 DIF: Cognitive Level: Comprehension REF: 962-963, Table 41-1 OBJ: 2 (clinical) TOP: Skin Lesions: Characteristics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 34. ANS: A PTS: 1 DIF: Cognitive Level: Comprehension REF: 962-963, Table 41-1 OBJ: 2 (clinical) TOP: Skin Lesions: Characteristics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 35. ANS: B PTS: 1 DIF: Cognitive Level: Comprehension REF: 962-963, Table 41-1 OBJ: 2 (clinical) TOP: Skin Lesions: Characteristics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 36. ANS: D PTS: 1 DIF: Cognitive Level: Comprehension REF: 962-963, Table 41-1 OBJ: 2 (clinical) TOP: Skin Lesions: Characteristics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A Chapter 42: Care of Patents with Integumentary Disorders and Burns deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse is bathing a patient with poison ivy. Which action is most appropriate? a. Bathe the patient with warm water. b. Maintain a room temperature of 78° to 80° F to prevent chills. c. Cover vesicles with gauze dressings. d. Pat skin dry. ANS: D Patting the skin dry will decrease irritation and will not break vesicles. Heat (both water and room temperatures) will exacerbate itching. Vesicles should not be covered with dressings. PTS: 1 DIF: Cognitive Level: Application REF: 971 OBJ: 1 (theory) TOP: Contact Dermatitis: Care Instruction KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 2. The nurse is educating a patient with acne rosacea that has facial erythema and telangiectases. Which information should the nurse include in the teaching plan? a. Drink 4 ounces of wine daily to promote vasodilation. b. Wash your face at least three times daily. c. Avoid direct sunlight. d. Apply tea bags to the affected areas. ANS: C Avoiding direct sunlight will reduce the symptoms. Factors that cause facial flushing precipitate worsening. Tea, coffee, alcohol (especially wine), caffeine-containing foods, spicy foods, sunlight, and emotional stress cause flare-ups. Washing the face too frequently can lead to skin irritation and dry skin. PTS: 1 DIF: Cognitive Level: Application REF: 971 OBJ: 5 (theory) TOP: Acne Rosacea: Exacerbation KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 3. For which patient would the nurse question an order for isotretinoin (Accutane)? a. A 20-year-old epileptic man with nodular acne and epilepsy b. A 22-year-old pregnant woman with severe acne c. A 46-year-old woman on oral contraceptive pills with cystic acne d. A 50-year-old hypertensive man with cystic acne ANS: B Accutane is considered a teratogen and can cause fetal malformations. Patients of childbearing age must be on a contraceptive. PTS: 1 DIF: Cognitive Level: Analysis REF: 972 OBJ: 5 (theory) TOP: Accutane: Contraindications KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 4. The nurse is advising a 20-year-old college sophomore with acne vulgaris. Which information is most important for the nurse to include in the teaching plan? a. Avoid all chocolate. b. Wash your face gently with mild soap. c. Scrub your face with a soft brush. d. Gently express clogged sebum from your pores. ANS: B The patient should keep his face clean and dry by washing with gently with mild soap and water. Although evidence exists that caffeine could potentially cause flare-ups, strict diet restrictions are no longer recommended. Scrubbing the face with a brush can cause irritation, and squeezing pustules can lead to infection. PTS: 1 DIF: Cognitive Level: Application REF: 972 OBJ: 5 (theory) TOP: Acne: Home Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 5. A patient with psoriasis is placed on PUVA therapy. What factors compose this therapy? a. Radiation and corticosteroids b. X-rays and methotrexate c. Artificial ultraviolet (UV) rays and a coal tar product d. Laser treatment and antimetabolites ANS: C PUVA is a combination of artificial UV rays and psoralen, a coal tar product. PTS: 1 DIF: Cognitive Level: Knowledge REF: 973 OBJ: 2 (theory) TOP: Psoriasis Treatment: PUVA KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 6. The nurse is educating a patient with psoriasis. Which information is most important for the nurse to include in the teaching plan? a. Liberally apply a lubricating cream three times daily. b. Use a humidifier at night. c. Use an alcohol-based cleanser in the morning. d. Take hot baths to reduce skin discomfort. ANS: B Skin should be kept as moist and pliable as possible. Humidifiers increase moisture in the environment. Use and application frequency of lubricating lotions and creams should be approved by the dermatologist before recommending. Drying solutions like alcohol and heat can increase discomfort of psoriasis. PTS: 1 DIF: Cognitive Level: Application REF: 973 OBJ: 2 (theory) TOP: Psoriasis: Increasing Comfort KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 7. An 84-year-old patient has had a low-grade fever for 2 days. This morning, the patient complains of burning, tingling hip pain that shoots down the leg. The nurse observes a small group of vesicles on the leg. These findings are consistent with which disorder? a. Herpes simplex b. Herpes zoster c. Syphilis lesions d. Furuncles ANS: B Herpes zoster (shingles) begins with vague symptoms of chills and low-grade fever and possibly some gastrointestinal disturbance. Discomfort along the nerve pathway is common. Small groups of vesicles appear on the skin, usually following the nerve pathways. PTS: 1 DIF: Cognitive Level: Application REF: 975 OBJ: 4 (theory) TOP: Herpes Zoster: Shingles KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 8. The patient with shingles has been on an antiviral medication since the vesicles appeared. The goal of early treatment is to prevent which complication? a. Postherpetic pain b. Outbreak of additional vesicles c. Lesions of the eye d. Transmission to health care workers ANS: A Early treatment may avoid postherpetic pain syndrome, but it cannot prevent additional vesicles, eye lesions, or transmission to another person. PTS: 1 DIF: Cognitive Level: Comprehension REF: 975 OBJ: 4 (theory) TOP: Shingles: Treatment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 9. The nurse is caring for a patient diagnosed with shingles who complains of constant pain along the sciatic nerve. What intervention best helps to provide pain relief? a. Distract the patient with conversation. b. Massage the area of pain. c. Move the affected leg through range-of-motion (ROM). d. Change the patient’s position frequently. ANS: A Distraction, guided imagery, and deep muscle relaxation may help reduce pain. Massage to the affected area will result in disruption in the vesicles of the disease. This disruption will delay healing and cause further discomfort. ROM and changing of positions are needed for patients with shingles in the event they are not mobile, but these actions will not reduce the discomfort. PTS: 1 DIF: Cognitive Level: Application REF: 976 OBJ: 4 (theory) TOP: Shingles: Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 10. The home health nurse is educating the family of a child with head lice. Which instructions are most important for the nurse to include? a. Lice cannot be transmitted to pets. b. Insects must be moving across the scalp to confirm diagnosis of head lice. c. Wash and dry all linens on the hottest setting. d. Apply a dime-sized amount of alcohol-based lotion to hair. ANS: C Washing in hot water with ordinary detergent and drying on the hottest cycle will kill lice. Lice can be transmitted to pets. Diagnosis of head lice occurs based on physical examination of lice or nits (eggs). Benzyl alcohol lotion 5% treatment amount varies based on the length of the hair and requires a second treatment in 7 days. PTS: 1 DIF: Cognitive Level: Comprehension REF: 977 OBJ: 1 (clinical) TOP: Pediculosis Capitis: Bed Linen Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 11. While bathing a patient, the nurse discovers a grayish black, nodular growth that resembles a blackberry in the middle of the patient’s back. What action should the nurse take? a. Report the findings to the patient’s health care provider. b. Teach the patient how to assess for changes in the growth. c. Document the finding of an actinic keratosis on the back. d. Inform the patient that he has a growth that is a melanoma. ANS: A These findings are consistent with a nodular malignant melanoma. This lesion should be evaluated by the physician and removed immediately once the diagnosis is confirmed. Teaching the patient to assess for changes is a lesser-priority action. Actinic keratoses are not consistent with these findings but instead appear on fair-skinned people as small, scaly, red, or grayish papules. Biopsy is required before any diagnosis can be confirmed, at which time the physician should disclose the results. PTS: 1 DIF: Cognitive Level: Analysis REF: 980 OBJ: 6 (theory) TOP: Skin Cancer: Malignant Melanoma KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 12. What is the primary purpose of a whirlpool bath given to the patient with a stage III pressure ulcer? a. To prevent infection b. To stimulate granulation tissue growth c. To improve circulation in surrounding skin d. To provide moisture to the ulcer ANS: B The whirlpool acts as a type of débridement. It gets rid of the necrotic debris and stimulates granulation tissue growth. PTS: 1 DIF: Cognitive Level: Application REF: 983 OBJ: 3 (clinical) TOP: Pressure Ulcers: Débridement KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 13. While bathing a patient, the nurse assesses a red, unblanchable area on the coccyx. Which type of dressing should the nurse apply? a. Transparent film b. Hydrocolloid c. Fluffy absorbent d. Wet-to-dry ANS: A A transparent film for a stage I pressure ulcer will protect it from shearing injury and will retain moisture. A hydrocolloid dressing would be appropriate for a larger, more advanced pressure ulcer. There is no discharge in a stage I pressure ulcer, making absorbent and wet-to-dry dressing options inappropriate. PTS: 1 DIF: Cognitive Level: Application REF: 982-983 OBJ: 8 (theory) TOP: Pressure Ulcers: Dressings KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 14. The nurse is caring for a patient with a stage III pressure ulcer that is not healing. Which statement accurately describes the goal of electrical stimulation of the pressure ulcer? a. To sterilize the wound b. To increase blood vessel growth c. To cause the ulcer to close by scabbing d. To coagulate the drainage ANS: B The electrical stimulation will increase blood supply by stimulating vessel growth. The voltage unit will not cleanse the wound, cause scabbing, or coagulation of drainage. PTS: 1 DIF: Cognitive Level: Application REF: 985 OBJ: 3 (clinical) TOP: Pressure Ulcers: Electrical Stimulation KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 15. In caring for a stage IV pressure ulcer, the nurse assesses creamy yellow drainage with a necrotic odor. Which type of bacteria most likely causes this exudate? a. Proteus b. Bacteroides c. Staphylococcus d. Pseudomonas ANS: C Creamy yellow drainage is usually caused by Staphylococcus infections. Proteus is associated with a beige discharge having a fishy odor. Brown discharge having a fecal odor is seen in Bacteroides. Pseudomonas-containing wounds produce a green-blue discharge with a fruity odor. PTS: 1 DIF: Cognitive Level: Comprehension REF: 986, Table 42-2 OBJ: 3 (clinical) TOP: Pressure Ulcers: Drainage KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 16. Which symptom is consistent with an inhalation burn? a. Full-thickness burns to chest b. Hypotension c. Agitation d. Persistent coughing ANS: D Persistent coughing, particularly if black mucus is coughed up, is an indicator of an inhalation burn. PTS: 1 DIF: Cognitive Level: Comprehension REF: 986, 989 OBJ: 9 (theory) TOP: Burns: Inhalation Burns KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 17. The nurse is providing fluid resuscitation for a burn victim according to the Parkland formula. The nurse determines that the patient requires 8000 mL in a 24-hour time period. The burn occurred at noon, and the present time is 1400. How many milliliters of fluid should infuse by 2000? a. 2000 mL b. 3000 mL c. 4000 mL d. 7000 mL ANS: C According to the Parkland formula, one half of the fluid resuscitation load should be infused within 8 hours from the time of the burn. The burn occurred at noon, so by 8:00 P.M., 4000 mL should have been infused of the 8000 mL calculated. PTS: 1 DIF: Cognitive Level: Application REF: 989 OBJ: 11 (theory) TOP: Burns: Fluid Resuscitation KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 18. Acceptable urine output for an adult is at least how many milliliters per hour? a. 10 mL b. 20 mL c. 30 mL d. 40 mL ANS: C The minimum acceptable urine output for an adult is 30 mL/hr. PTS: 1 DIF: Cognitive Level: Knowledge REF: 989 OBJ: 11 (theory) TOP: Burns: Urine Output KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 19. The nurse is caring for a burn patient. Which action best prevents contractures? a. Assist the patient with ambulation as soon as fluid shifts stabilize. b. Medicate the patient approximately 30 minutes prior to dressing changes. c. Ensure adequate hydration. d. Ensure adequate nutritional intake. ANS: A While each of these interventions is important for management of the patient with burns, only ambulation works to prevent contractures. Other interventions address pain management, adequate hydration, and adequate nutritional intake. PTS: 1 DIF: Cognitive Level: Understanding REF: 992 OBJ: 12 (theory) TOP: Burns: Prevention of Contractures KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 20. A 75-year-old patient questions the nurse about vaccination to prevent shingles. Which response is most appropriate? a. “The incidence of shingles in people your age is not overly common, so vaccination is unnecessary.” b. “The vaccination has not yet been approved for use in the older adults.” c. “Because of the incidence of shingles in your age group, you should consider taking the vaccination.” d. “The vaccination is expensive but will provide lifelong immunity.” ANS: C The vaccination should be considered by high-risk populations. About 50% of individuals over age 80 years will have the disease. The vaccination has been approved for use. The immunity provided is anticipated to last for 6 years. PTS: 1 DIF: Cognitive Level: Understanding REF: 975 OBJ: 13 (clinical) TOP: Herpes Zoster: Elder Care Points KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 21. The mother of a 4-year-old child reports concerns about how to completely rid her home of lice. Which response indicates that the mother needs further instruction? a. “I should wash all bedding in hot water.” b. “I should re-treat my child’s hair 1 week after the first application.” c. “I should discard my child’s stuffed animals.” d. “My children should not share hats or hairbrushes.” ANS: C For items that cannot be cleaned, such as some stuffed animals, sealing them in plastic bags with the air expelled for 14 days can be effective. Linens should be washed and dried on the hottest cycle. Application of alcohol-based lotion requires reapplication after 1 week. Sharing hats or hairbrushes increases the likelihood of lice transmission. PTS: 1 DIF: Cognitive Level: Application REF: 978 OBJ: 1 (theory) TOP: Pediculosis and Scabies: Patient Teaching KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 22. The nurse is caring for a patient with a stage III pressure ulcer. Which assessment findings are consistent with this stage of ulcer? a. A crater-like lesion b. Skin that does not blanch with fingertip pressure c. Presence of mottled skin d. Excoriation around the lesion ANS: A A stage III pressure ulcer presents as a crater-like ulcer and underlying subcutaneous tissue is involved in the destructive process. Skin that does not blanch with pressure or is mottled are findings consistent with a stage I pressure ulcer. Excoriation around the lesion is consistent with scratching or another abrasive force. PTS: 1 DIF: Cognitive Level: Comprehension REF: 983 OBJ: 3 (clinical) TOP: Pressure Ulcers KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation MULTIPLE RESPONSE 23. The home health nurse gives instructions to a patient in avoiding recurrence of athlete’s foot. Which information should the nurse include? (select all that apply.) a. Wear clean cotton socks. b. Wear shoes that allow ventilation. c. Use only clean towels. d. Wash and dry feet daily. e. Apply antibacterial medication to feet. ANS: A, B, C, D Tinea pedis is a common fungal infection. Wearing clean, breathable socks and shoes that allow ventilation are helpful in managing a recurrence, along with use of clean towels and careful attention to hygiene. An antibacterial ointment is not helpful in treating a fungal infection. PTS: 1 DIF: Cognitive Level: Comprehension REF: 977 OBJ: 3 (theory) TOP: Tinea Pedis: Home Care KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 24. Which interventions are appropriate for a burn patient newly admitted to the emergency department? (select all that apply.) a. Cover burns with sterile saline–saturated towels. b. Carefully remove clothing adhered to burned areas. c. Carefully avoid disturbing blisters. d. Remove jewelry from injured limbs. e. Determine the causative agent of the burn. ANS: C, D, E The nurse should carefully avoid disturbing blisters, remove jewelry from injured limbs, and determine the causative agent of the burn. Clothing that is stuck to burn areas is not removed until the patient is admitted to the hospital. The nurse should apply a sterile dry (not wet) dressing. PTS: 1 DIF: Cognitive Level: Comprehension REF: 987 OBJ: 10 (theory) TOP: Burns: Admission Interventions KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 25. The nurse is educating patients about dietary selections that will promote wound healing. Which menu options should the nurse include? (select all that apply.) a. Tofu b. White bread c. Lean beef d. Citrus fruits e. Leafy green vegetables ANS: A, C, D, E Protein, zinc, and vitamins A, C, and E are shown to reduce pressure ulcers in high-risk patients. Tofu and lean beef are sources of protein. Citrus fruits are high sources of vitamin C. Leafy green vegetables are sources of vitamin A. White bread is not a significant source of protein, zinc, or vitamins A, C, and E. PTS: 1 DIF: Cognitive Level: Application REF: 997 OBJ: 8 (theory) TOP: Pressure Ulcers: Wound and Wound Healing KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance COMPLETION 26. An adult male patient enters the emergency department with full- and partial-thickness burns on the entire right leg, front of the right arm, and one half of the front torso. The nurse, using the “rule of nines,” assesses the burn as ____%. ANS: 31 31.5 32 Right leg = 18%, front of arm = 4.5%, and half of front torso = 9%; 18 + 4.5 + 9 = 31.5%. PTS: 1 DIF: Cognitive Level: Application REF: 987, Figure 42-15 OBJ: 10 (theory) TOP: Burn Assessment: “Rule of Nines” KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 27. Using the Parkland formula, the fluid needed for a person weighing 140 pounds with a 25% burn would be _____ mL. ANS: 6360 4 mL × 25% (percentage burn) × 63.6 (weight in kilograms) = 6360 mL. PTS: 1 DIF: Cognitive Level: Application REF: 989 OBJ: 10 (theory) TOP: Burns: Fluid Resuscitation Calculation KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance MATCHING The nurse differentiates the various type of dermatitis. Match each option with the characteristics that best describe it. (Options may be used once, more than once, or not at all.) a. Contact dermatitis b. Atopic dermatitis c. Stasis dermatitis d. Seborrheic dermatitis 28. Cell-mediated immunity resulting in inflammatory response 29. Erythema and pruritus with scaling associated with phlebitis 30. Appearance of vesicular lesions following inflammatory response 31. Scaly lesions on scalp, ear canals, and eyebrows 32. Rash associated with poison ivy 33. Mast cell–stimulated release of histamine 34. Lesions may become ulcerated 28. ANS: A PTS: 1 DIF: Cognitive Level: Comprehension REF: 971 OBJ: 1 (theory) TOP: Skin Disorders: Cause KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 29. ANS: C PTS: 1 DIF: Cognitive Level: Comprehension REF: 971 OBJ: 1 (theory) TOP: Skin Disorders: Cause KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 30. ANS: A PTS: 1 DIF: Cognitive Level: Comprehension REF: 971 OBJ: 1 (theory) TOP: Skin Disorders: Cause KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 31. ANS: D PTS: 1 DIF: Cognitive Level: Comprehension REF: 971 OBJ: 1 (theory) TOP: Skin Disorders: Cause KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 32. ANS: A PTS: 1 DIF: Cognitive Level: Comprehension REF: 971 OBJ: 1 (theory) TOP: Skin Disorders: Cause KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 33. ANS: B PTS: 1 DIF: Cognitive Level: Comprehension REF: 971 OBJ: 1 (theory) TOP: Skin Disorders: Cause KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 34. ANS: C PTS: 1 DIF: Cognitive Level: Comprehension REF: 971 OBJ: 1 (theory) TOP: Skin Disorders: Cause KEY: Nursing Process Step: N/A MSC: NCLEX: N/A The nurse describes common complications that burn patients may experience. Match the burn complication with the description that best fits it. a. Edema b. Hyperkalemia c. Hypovolemia d. Tissue hypoxia e. Hypermetabolism 35. Potassium released from damaged cells 36. Increased viscosity of blood slowing blood flow to small vessels 37. Negative nitrogen balance 38. Inflammatory response causing fluid shift 39. Loss of fluid from vascular space 35. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 986 OBJ: 6 (theory) TOP: Burn Pathophysiology KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 36. ANS: D PTS: 1 DIF: Cognitive Level: Analysis REF: 986 OBJ: 6 (theory) TOP: Burn Pathophysiology KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 37. ANS: E PTS: 1 DIF: Cognitive Level: Analysis REF: 986 OBJ: 6 (theory) TOP: Burn Pathophysiology KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 38. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 986 OBJ: 6 (theory) TOP: Burn Pathophysiology KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 39. ANS: C PTS: 1 DIF: Cognitive Level: Analysis REF: 986 OBJ: 6 (theory) TOP: Burn Pathophysiology KEY: Nursing Process Step: N/A MSC: NCLEX: N/A The nurse describes several types of burn treatment. Match the burn treatment to the statement that best describes it. a. Open technique b. Closed technique c. Escharotomy d. Allograft e. Xenograft 40. Incision into subcutaneous tissue to increase circulation 41. Biologic dressing obtained from a cadaver 42. Wound covered with ointment, then covered with layers of gauze saturated with topical medication 43. Biologic dressing obtained from a pig 44. Wound covered with ointment, and additional environmental warmth provided 40. ANS: C PTS: 1 DIF: Cognitive Level: Analysis REF: 990-992 OBJ: 8 (theory) TOP: Burns: Treatments KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 41. ANS: D PTS: 1 DIF: Cognitive Level: Analysis REF: 990-992 OBJ: 8 (theory) TOP: Burns: Treatments KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 42. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 990-992 OBJ: 8 (theory) TOP: Burns: Treatments KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 43. ANS: E PTS: 1 DIF: Cognitive Level: Analysis REF: 990-992 OBJ: 8 (theory) TOP: Burns: Treatments KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 44. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 990-992 OBJ: 8 (theory) TOP: Burns: Treatments KEY: Nursing Process Step: N/A MSC: NCLEX: N/A Chapter 43: Care of Patients in Disasters or Bioterrorism Attack deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse explains differences between an emergency situation and a disaster to high school class. Which statement is true? a. An emergency consists of fewer than 50 people who require emergent treatment. b. In an emergency situation, the local emergency rooms can meet the need. c. An emergency situation lacks the need for a prearranged management plan. d. In an emergency situation, the community population is not affected by the event. ANS: B An emergency situation, such as a plane crash at a local airport, can be handled by community emergency departments. Each community has in place an emergency plan as to dispersal of people needing to be treated, law enforcement participation, and transportation. Communities are always affected when a large-scale emergency situation occurs. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1002 OBJ: 1 (theory) TOP: Disaster vs. Emergency Situation KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 2. Which agency requires emergency preparedness plans for accredited hospitals? a. American Red Cross (ARC) b. The Joint Commission (TJC) c. Federal Emergency Management Agency (FEMA) d. Office of Civil Defense (OCD) ANS: B TJC requires that all accredited facilities have a written emergency preparedness plan with designated roles and responsibilities. The ARC is a voluntary organization that traditionally provides the basic essentials of shelter, food, and first aid during a natural disaster. FEMA is an organization under the federal government. It is activated by the Department of Homeland Security. It acts when states require assistance in times of disaster. The Office of Civil Defense (OCD) is no longer in existence. It was a federal agency that acted in cases of large-scale disasters. It was replaced by FEMA. PTS: 1 DIF: Cognitive Level: Knowledge REF: 1003 OBJ: 2 (theory) TOP: Institutional Disaster Plans KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 3. How many times per year should accredited health care facilities test their emergency plans? a. Once b. Twice c. Three times d. Four times ANS: B Disaster drills should be conducted at least two times per year. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1003 OBJ: 2 (theory) TOP: Disaster Drills: Frequency KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 4. After a truck crashes into the dayroom of a long-term health care facility, many of the residents are injured, and noninjured residents are stunned and frightened. What action should the nurse take? a. Firmly instruct two CNAs to start wheeling residents to the dining room in their wheelchairs. b. Begin wheeling residents back to their rooms herself. c. Shout for everyone to hurry to the dining room. d. Begin treating the injured in the center of the dayroom. ANS: A The nurse should recognize that everyone is in the impact stage. In the impact stage, firm direction is needed to get people to a central place for safety and information. The nurse should not try to single-handedly correct the situation, shout and increase confusion, or treat patients in the middle of the chaotic environment. PTS: 1 DIF: Cognitive Level: Analysis REF: 1010 OBJ: 3 (theory) TOP: Psychological Response: Stage I KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 5. During a flood, the public water supply has been contaminated. Which action is most important for the nurse to take? a. Designate which commodes can be used for body waste. b. Gather a large pot, household bleach, and other supplies. c. Run cold water in sinks to have reservoirs of water. d. Reserve existing water for hand washing only. ANS: B The nurse will need to purify water and should gather supplies that are necessary to do so. Using any of the water for waste disposal is inappropriate. Using cold water pulls from the contaminated water supply. Contaminated water should not be used to wash hands, prepare food, make ice, or prepare baby formula. PTS: 1 DIF: Cognitive Level: Analysis REF: 1011 OBJ: 5 (theory) TOP: Flood: Water Provision and Protection KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 6. During a power failure, at what temperature should perishable food be maintained to prevent possibility of food poisoning? a. 40° F b. 45° F c. 50° F d. 55° F ANS: A To prevent spoilage, perishable foods should be kept at 40° F. PTS: 1 DIF: Cognitive Level: Knowledge REF: 1011 OBJ: 3 (clinical) TOP: Food Supply: Temperature KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 7. A freezer full of food at the time of the power failure will keep food to eat for what period of time? a. 8 hours b. 12 hours c. 24 hours d. 48 hours ANS: D Food frozen in a full freezer will keep the food safe for 48 hours. A partially filled freezer will keep food safe for 24 hours. PTS: 1 DIF: Cognitive Level: Knowledge REF: 1011, Box 43-1 OBJ: 3 (clinical) TOP: Food Supply: Preservation KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 8. A nurse is attempting to restore order to a group of people trapped in a building by rising flood waters. Which action is best for the nurse to take? a. Give each person a specific duty. b. Allow people to direct themselves to helpful tasks. c. Make a list of essential jobs and ask for volunteers. d. Compile all food in a central location and direct people to form a line to take what they need. ANS: A During the impact stage, firm direction is needed, and executing essential helpful jobs will help restore order. Asking for volunteers when there is a loss of order and control would be counterproductive and would lack the direction needed by those affected. Food will need to be rationed in the event there is no rescue for an extended period of time. The rationing should be performed with direction and should not allow the people to take whatever they wish. PTS: 1 DIF: Cognitive Level: Application REF: 1010 OBJ: 3 (clinical) TOP: Disaster: Establishing Order KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 9. The news reports that a train derailment 5 miles from a clinic spilled a large amount of liquid chlorine that has been vaporized by the atmosphere. Which finding indicates that the chlorine gas is an imminent threat to the clinic? a. Sighting of a low-lying green cloud. b. Smelling “almonds” or “burning feathers.” c. Onset of sudden nausea in multiple patients. d. Onset of skin blisters in multiple patients. ANS: A Chlorine gas can be seen as a low-lying green cloud. The smell of almonds is associated with cyanide. Nausea is a nonspecific finding. Skin blistering is the result of contact with liquid chlorine. PTS: 1 DIF: Cognitive Level: Application REF: 1013, Table 43-3 OBJ: 6 (theory) TOP: Chlorine Gas: Assessing Threat KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 10. During a tornado warning with sirens, the nursing staff are caring for 36 patients on the second floor medical-surgical unit. How should the staff protect the patients? a. Move all patients to the evacuation center across the street. b. Bring all patients into the hall and close doors and windows. c. Seal all patients in their bathrooms and cover windows with bed mattresses. d. Evacuate patients to the basement via the elevators. ANS: B Movement to the hall is the safest and fastest and does not expose the patients to being out of doors, in elevators, or near exterior windows. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1010 OBJ: 6 (theory) TOP: Tornado: Patient Evacuation KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 11. Which measurement best detects the daily amount of radiation to which a health worker is exposed? a. Radiation urinalysis b. Radiation badges c. Radiation spectrometer d. Radiation sputum analysis ANS: B Radiation detection badges are worn under protective clothing and are analyzed for the amount of radiation absorbed. PTS: 1 DIF: Cognitive Level: Knowledge REF: 1015 OBJ: 7 (theory) TOP: Monitoring for Radiation Exposure: Badges KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 12. If terrorists were to use category B agents that produce low death rates and moderate illness, by which route would the organisms likely be delivered? a. Vaporization b. Water sources c. Explosion d. Person-to-person contact ANS: B Category B agents are usually delivered via a water source. Category A agents may be transmitted without detection and can be easily spread from person to person. Category C agents are agents that have not yet been weaponized. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1016 OBJ: 8 (theory) TOP: Category B Agents: Delivery Mode KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 13. Why is a chelating agent administered after a person has been exposed to particulate radioactive material? a. To bind with radioactive material and allow it to be excreted b. To reduce radioactivity to nonharmful levels c. To form a protective coat in the gastrointestinal system d. To dissolve particulate material ANS: A Chelating agents bind with radioactive material, allowing it to be excreted without absorption. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1015 OBJ: 7 (theory) TOP: Radiation Exposure: Chelating Agents KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 14. In a terrorist attack, which period of time poses the greatest chance for inhalation of aerosolized anthrax? a. The day of the attack b. The day after the attack c. 2 days after the attack d. 1 week after the attack ANS: B Anthrax in an aerosolized form is most potent 1 day after the explosion. After that time, the organism dies very quickly and anthrax is not communicable from person to person. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1017, Table 43-5 OBJ: 8 (theory) TOP: Aerosolized Anthrax: Life Span of Organism KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 15. When can patients with plague who have been treated with appropriate antibiotics be released from respiratory droplet precautions? a. After resolution of all symptoms b. After three sputum samples are negative for blood c. After all lesions are dried d. After the patient receives 48 hours of antibiotic treatment ANS: D The patient with plague can be released from respiratory precautions 48 hours after initiation of antibiotic therapy. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1019 OBJ: 8 (theory) TOP: Plague: Respiratory Precautions KEY: Nursing Process Step: N/A MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 16. In a terrorist attack, introduction of the plague would most likely occur as an aerosolized weapon. The nurse understands that this organism is very vulnerable to exposure to which element? a. Temperature of 40° F b. Sunlight c. Strong chlorine solution d. Nitrogen gas ANS: B Plague organisms can be destroyed by exposure to sunlight. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1019 OBJ: 8 (theory) TOP: Plague: Fragility of Organism KEY: Nursing Process Step: Planning MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 17. After a terrorist attack with smallpox virus, the nurse assesses a newly admitted patient with large vesicles. The nurse understands that which assessment finding differentiates smallpox vesicles from chickenpox vesicles? a. Lesions on the face b. Lesions on mucous membranes c. Lesions on the soles of the feet d. Lesions in the axilla ANS: C The lesions of smallpox can be found on the palms of the hands and soles of the feet. The lesions of chickenpox do not appear there. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1019 OBJ: 8 (theory) TOP: Smallpox vs. Chickenpox KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 18. What is the purpose of debriefing after caring for victims of a disaster? a. To analyze the effectiveness of the disaster plan b. To assess the efficiency of the response c. To modify the disaster plan d. To help allay post-traumatic stress disorders ANS: D The debriefing is for the purpose of allowing the health professionals to ventilate about their experiences in an effort to allay long-term psychological problems. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1022 OBJ: 10 (theory) TOP: Debriefing: Purpose KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 19. A patient comes to the emergency department after exposure to a toxic chemical spill. Which action indicates that the nurse accurately understands proper management of this patient? a. Disinfecting contact lenses before reinserting them. b. Irrigating the patient’s eyes for 5 to 7 minutes with water. c. Using tongs to handle removed clothing. d. Placing the clothing in a metal receptacle for disposal. ANS: C Clothing and contact lenses are considered contaminated and should be removed and discarded. The nurse should use tongs to prevent touching the clothing directly. Contact lenses should be discarded, eyes should be irrigated for 10 to 15 minutes, and clothing should be placed in a plastic bag for disposal. PTS: 1 DIF: Cognitive Level: Application REF: 1014 OBJ: 5 (theory) TOP: Chemical Disaster: KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 20. The nurse is teaching community members about precautions related to a pandemic occurrence. Which information is most important for the nurse to include in the teaching plan? a. Be sure to cover your mouth when coughing. b. Be prepared to stay at home for at least 2 weeks. c. Dispose of tissues after using them. d. Avoid shaking hands. ANS: B The nurse should be sure to include information that differentiates pandemic flu occurrences from normal respiratory illness. The priority education about pandemic flu involves teaching people to be prepared to stay at home for at least 2 weeks. While covering the mouth when coughing or sneezing, tissue disposal, and avoiding handshakes are important, all of these considerations are precautions for prevention of any respiratory illness. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1021 OBJ: 3 (clinical) TOP: Pandemic Infections KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance MULTIPLE RESPONSE 21. Essential elements in a disaster plan include provision of which components? (Select all that apply.) a. Shelter for victims b. Transportation c. Communication d. Welfare of victims e. Food ANS: A, B, C, D, E All options are essential elements in a disaster plan. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1002 OBJ: 2 (theory) TOP: Disaster Plan: Essentials KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 22. The nurse is preparing a list of items that are needed in a disaster kit. Which items should the nurse include? (Select all that apply.) a. A 12-day supply of bottled water b. Nonperishable food items c. Prescription medications d. Portable radio e. Bedding f. First aid kit ANS: B, C, D, E, F Nonperishable food items, prescription medication, a portable radio, bedding, and a first aid kit are essential components of an adequate disaster kit. A water supply that will last 3 days is sufficient for a disaster kit. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1009 OBJ: 3 (clinical) TOP: Disaster Kits: Minimal Provisions KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 23. Local civil defense courses on disaster preparedness explain the roles of which people/entities? (Select all that apply.) a. State government b. Federal government c. Law enforcement agencies d. Individual service agencies e. Nurse as a volunteer ANS: A, B, C, D, E Civil defense courses should explain the role of all of these participants. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1003 OBJ: 2 (theory) TOP: Disaster Preparation: Courses KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 24. Which statement accurately describes how water can be rendered safe for drinking in the event of a disruption of service? (Select all that apply.) a. Allow water to sit for 24 hours before using. b. Boil water for 3 to 5 minutes. c. Add 1 mL (16 drops) of household bleach to a gallon of water and let it stand for 30 minutes. d. Drain water from hot water heaters. e. Pour water through several layers of cotton towels. ANS: B, C, D Water can be rendered safe for drinking by boiling, treating with household bleach, or removing from hot water heaters or commode tanks. Allowing water to sit for 24 hours or pouring water through layers of cotton towels does not adequately render the water safe to drink. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1011 OBJ: 2 (clinical) TOP: Preparing Safe Drinking Water: Techniques KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 25. Which category A organisms may be released in a bioterrorism attack because of high lethality? (Select all that apply.) a. Ebola b. Avian flu c. Botulism d. Smallpox e. Tularemia ANS: A, C, D, E Ebola, botulism, smallpox, and tularemia are category A organisms with high lethality. Avian flu (bird flu) is not on the category A list. PTS: 1 DIF: Cognitive Level: Knowledge REF: 1017 OBJ: 8 (theory) TOP: Bioterrorism: Organisms with High Lethality KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 26. The nurse is participating in an educational program concerning nuclear disasters. Which factor(s) determine(s) a victim’s level of exposure to radiation? (Select all that apply.) a. Age of the victim b. Body surface area of the victim c. Length of exposure d. Distance of the victim from the nuclear source e. Shielding of the victim from the nuclear source ANS: C, D, E The amount of damage to each person depends on the type of radiation, the dose received, the length of time of exposure, and the route of the exposure. Time, distance, and shielding are key to the quantity of radiation an individual will receive. The shorter the time of exposure, the farther away from the radiation source, and whether or not the person was shielded by materials that are impermeable to radiation are details pertinent to radiation risk. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1015 OBJ: 7 (theory) TOP: Nuclear Disaster KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance MATCHING Assign triage categories to the disaster victims that they best fit. (Options may be used once, more than once, or not at all.) a. Red tag: emergent b. Yellow tag: urgent c. Green tag: nonurgent d. Black tag: terminal 27. Compound fracture of both femurs, concussion 28. Crushed chest, paraplegia 29. Closed fracture of arm, head laceration 30. Toddler with partial-thickness burns on both legs 31. Woman in labor, pains 10 minutes apart 32. Sucking chest wound, fully conscious 33. Amputated arm, conscious, but in shock 27. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 1004, Table 43-1 OBJ: 3 (theory) TOP: Triage: Process KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 28. ANS: D PTS: 1 DIF: Cognitive Level: Analysis REF: 1004, Table 43-1 OBJ: 3 (theory) TOP: Triage: Process KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 29. ANS: C PTS: 1 DIF: Cognitive Level: Analysis REF: 1004, Table 43-1 OBJ: 3 (theory) TOP: Triage: Process KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 30. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 1004, Table 43-1 OBJ: 3 (theory) TOP: Triage: Process KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 31. ANS: C PTS: 1 DIF: Cognitive Level: Analysis REF: 1004, Table 43-1 OBJ: 3 (theory) TOP: Triage: Process KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 32. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 1004, Table 43-1 OBJ: 3 (theory) TOP: Triage: Process KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care 33. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 1004, Table 43-1 OBJ: 3 (theory) TOP: Triage: Process KEY: Nursing Process Step: Assessment MSC: NCLEX: Safe, Effective Care Environment: Coordinated Care Chapter 44: Care of Patients with Emergencies, Trauma, and Shock deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. A diving accident occurs at the community pool and the victim is conscious and in pain. Which intervention is most appropriate pending the arrival of emergency medical personnel? a. Position the patient on the side of the pool. b. Move the patient to the shallow end and cover with a towel c. Leave the patient in the pool and support with a large float. d. Leave the patient in the pool and attempt cardiopulmonary resuscitation (CPR). ANS: C Care should be taken to avoid movement of the patient and increasing injury to the spinal cord. Leaving the patient in the pool and supporting the patient on a float will not increase a possible spinal injury. Pulling the patient may cause further injury to the spine. CPR is not indicated as the patient is not experiencing cardiopulmonary arrest. PTS: 1 DIF: Cognitive Level: Application REF: 1026 OBJ: 2 (theory) TOP: Diving Injury: First Aid KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 2. A drowning victim is brought to shore and is semiconscious and breathing. The camp counselor recognizes that which positioning is the most appropriate for this victim? a. Supine to receive CPR b. Supine with knees flexed c. On the side in recovery position d. Prone with head turned to side ANS: C The patient who is breathing should be placed in the recovery position to allow the patient to vomit out water without danger of aspiration. CPR is not indicated as the patient is not experiencing the absence of cardiopulmonary activity. Lying supine or prone will not prevent aspiration in the event of vomiting. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1026 OBJ: 2 (theory) TOP: Near-Drowning: Positioning KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 3. In the memory prompt for emergency care, ABCDE, what does the “E” represent? a. End b. Execute c. Expedite d. Expose ANS: D The “E” stands for expose. This reminder is to assist the first responder to assess for other injuries that may be hidden under clothing. PTS: 1 DIF: Cognitive Level: Knowledge REF: 1029 OBJ: 2 (theory) TOP: ABCDE Memory Prompt: Definition KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 4. The nurse is teaching a CPR class. During the class, the nurse correctly includes which statement when discussing the Good Samaritan Law? a. The Good Samaritan Law only protects medical professionals from liability. b. The Good Samaritan Law protects all people from liability. c. The Good Samaritan Law limits the liability of a medical professional. d. The Good Samaritan Law defines specific situations in which no liability will occur. ANS: B The Good Samaritan Law is designed to protect passersby who render first aid so they will not be held liable for the outcome of emergency care. Individuals who choose to render care will be held to the standard consistent with their training. The law is not limited to medical personnel. It does not address limitations of liability. There is no definition of specific scenarios protected by the law. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1026-1027 OBJ: N/A TOP: Good Samaritan Law: Provisions KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 5. A victim of a knife fight is found lying in a parking lot with a loop of bowel protruding from an abdominal wound. What should the first responder do first? a. Attempt to replace the bowel back into the abdomen. b. Wrap the victim’s shirt tightly around his body. c. Cover the evisceration with a plastic shopping bag. d. Assist the victim to flex his thighs against his abdomen. ANS: C Covering evisceration with a nonadhesive covering will keep the bowel moist. Attempts to return the bowel into the abdomen may result in further injury. Tightly wrapping the shirt around the body may compromise circulation. Flexion of the thighs onto the abdomen may compress and cause further damage to the bowel. PTS: 1 DIF: Cognitive Level: Application REF: 1027 OBJ: 2 (theory) TOP: Evisceration: First Aid KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 6. A worker in a department store fell through a plate glass window, causing a deep laceration on the right mid-thigh that is pumping bright red arterial blood. Which initial action is most important for the first responder to take? a. Elevate the leg. b. Bunch up the worker’s shirt and press it against the wound. c. Press the palm of hand in the groin to compress the femoral artery. d. Tie the worker’s belt tightly around his upper thigh to stop bleeding. ANS: B A guideline published by the American College of Surgeons Committee on Trauma in 2014 recommends holding direct pressure on the bleeding area for prehospital control of bleeding. If this approach is impractical or ineffective, a tourniquet may be implemented. It is not always possible to compress the artery at the needed location, so this choice is not a first line intervention. Elevation of an injured extremity is no longer recommended. PTS: 1 DIF: Cognitive Level: Application REF: 1031 OBJ: 2 (theory) TOP: Arterial Bleed: Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 7. The nurse cautions that, when cooling down a victim of heatstroke, one must be careful to prevent shivering. Shivering can lead to which complication? a. A paralytic ileus b. Cardiac arrhythmias c. An increase in temperature d. A seizure ANS: C Shivering is a homeostatic activity that generates heat and increases body temperature. Shivering would not cause a paralytic ileus, cardiac arrhythmias, or seizures. PTS: 1 DIF: Cognitive Level: Analysis REF: 1034 OBJ: 3 (theory) TOP: Heatstroke: Cooling Technique KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 8. The nurse is teaching a group of CNAs about the fastest and simplest technique to reduce temperature in a patient with a fever. Which method should the nurse include in the teaching plan? a. Apply ice packs to the groin. b. Bathe the patient in tepid water. c. Remove clothing and bed linen. d. Give the patient chilled drinks. ANS: C Removing the patient’s clothing and bed linen covering the patient is a quick, simple, and usually effective way to reduce temperature. The application of ice packs may result in excessive cooling and result in shivering, which acts to increase metabolic rate. Bathing in tepid water is effective but requires more time and interaction than simply removing clothing and bed linens. Chilled drinks will not adequately reduce the total body temperature. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1034 OBJ: 3 (theory) TOP: Increased Temperature: Initial Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 9. A spectator at the Little League playoffs in August in Texas faints in the sun-drenched stands. His face is flushed and his skin is hot to the touch. What action should the first responder take? a. Lay the spectator down on the bleacher seat. b. Help the spectator drink a large iced drink. c. Seat the spectator upright and shield him from the sun with an umbrella. d. Move the responder to a shady area, and sprinkle his clothing with water. ANS: D The best action is to remove the victim from the sun and cool by evaporation until emergency medical personnel arrive. The spectator should not remain in the sun on the hot bleachers in any capacity. PTS: 1 DIF: Cognitive Level: Application REF: 1034 OBJ: 3 (theory) TOP: Heatstroke: First Aid KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 10. A student nurse is assisting with the care of a 50-year-old man who is being treated in the emergency department for hypothermia. The student asks the charge nurse why the patient is having his heart monitored. How should the nurse best respond? a. Infusing intravenous (IV) fluids rapidly raise blood pressure (BP) and heart rate. b. Adrenal output of epinephrine increases in response to cold stress. c. Lactic acid from pooled blood in the extremities shunts back to the heart. d. The warming process causes vasodilation. ANS: C Lactic acid in the blood that was pooled in the extremities while being exposed to cold will shunt back to the heart through systemic perfusion as the warming process becomes effective. The lactic acid can cause arrhythmias. PTS: 1 DIF: Cognitive Level: Application REF: 1035 OBJ: 3 (theory) TOP: Hypothermia: Arrhythmias KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 11. The nurse is caring for a patient with frostbite. Which assessment findings would lead the nurse to conclude that the patient has second-degree frostbite? a. Reddened skin with hard white plaques b. Waxy skin with sensory deficits c. Reddened skin with milky fluid-filled blisters d. Waxy skin with blood-filled blisters ANS: C Frostbite is categorized by degree of injury, much like burns. Second-degree injury is characterized by redness, swelling, and formation of blisters filled with clear or milky fluid that forms within 24 hours of injury. A first-degree injury includes reddened skin, swelling, waxy appearance, hard white plaques, and sensory deficit. Third-degree injury consists of blood-filled blisters followed by black eschar forming over several weeks. Fourth-degree injury involves full-thickness damage affecting muscles, tendons, and bone, resulting in tissue loss. PTS: 1 DIF: Cognitive Level: Application REF: 1035 OBJ: 3 (theory) TOP: Frostbite: Staging KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 12. The emergency department nurse is attempting to revive an unconscious, shivering person with extreme hypothermia (rectal temperature of 94° F). The nurse should be most alarmed with which change? a. The patient’s cold ears turn red. b. The patient stops shivering. c. The patient’s hands clench. d. The patient’s reflexes return. ANS: B Cessation of shivering indicates that the body’s homeostatic response to generate heat has ceased and the patient’s condition is deteriorating. Clenching hands are an insignificant finding. Reddened ears and returning reflexes would indicate warming. PTS: 1 DIF: Cognitive Level: Analysis REF: 1035 OBJ: 3 (theory) TOP: Hypothermia: Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 13. An 80-year-old woman is brought to the emergency department after being found unconscious in her garage sitting in her car. Which assessment finding is most concerning to the nurse? a. Temperature, 97.6° F; pulse, 98; and blood pressure, 110/60 b. Oxygen (O2) saturation of 78% c. Cherry red mucous membranes d. Cold extremities ANS: C The cherry red mucous membranes are classic signs of carbon monoxide poisoning; unfortunately, they are very late signs. The temperature, pulse, and blood pressure are within normal limits. An O2 saturation of 78% could be corrected if accurate, and O2 saturation measurements are inaccurate in cases of carbon monoxide poisoning. Cold extremities do not necessarily indicate an urgent problem. PTS: 1 DIF: Cognitive Level: Application REF: 1037 OBJ: 4 (theory) TOP: Carbon Monoxide Poisoning: Significant Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 14. A restaurant patron sitting at a next table begins to choke and cough. The patron yells, “I’m choking! I can’t breathe!” What action should the first responder take? a. Initiate the Heimlich maneuver immediately. b. Strike the victim sharply between the scapulae. c. Encourage the patient to cough and deep-breathe. d. Offer him a small sip of fluid. ANS: C Because the victim can cough and speak, the airway is not compromised and can make an effort to clear the foreign matter by coughing. The Heimlich maneuver can be initiated at such a time that the victim’s airway becomes occluded. The patron should not attempt to drink or eat until the foreign matter is cleared. PTS: 1 DIF: Cognitive Level: Application REF: 1040 OBJ: 7 (theory) TOP: Choking: Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 15. A delivery man comes to the emergency department with dog bites on his legs. He states that the dog ran away after the attack and could not be identified. After treating the bites, the nurse educates the man about which next step? a. Notification of Animal Control b. Receipt of immune globulin for passive immunity c. Receipt of the first of five rabies vaccination injections d. Infusion of IV fluids ANS: B The administration of immune globulin will build up his immediate defenses. As a delivery man, he would be considered to be in a high-risk group for animal bites and should be advised to acquire the vaccine, but the vaccine will not be of any use to him at this point. IV fluids are not likely indicated unless blood loss was severe. PTS: 1 DIF: Cognitive Level: Application REF: 1038 OBJ: 5 (theory) TOP: Animal Bite: Prophylaxis KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 16. The first responder to an automobile accident finds a victim with a sucking chest wound. What action should the responder take? a. Tightly bind the injury with a folded magazine and the patient’s belt. b. Place a plastic sandwich bag over the wound and tape on three sides to make a flutter dressing. c. Turn the patient to the affected side and instruct the patient to deep breathe. d. Place the patient’s hand over the wound and tell the patient to press down. ANS: B The flutter dressing will allow the air to leave the pleural space, but not allow any more air in. The collapsed lung will begin to reexpand. PTS: 1 DIF: Cognitive Level: Analysis REF: 1033 OBJ: 2 (theory) TOP: Sucking Chest Wound: First Aid Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 17. The nurse has arrived on the scene of an accident. The victim is conscious and has a large bleeding laceration on his thigh. The nurse uses an available towel to provide compression to the wound. What action should the nurse perform next? a. Turn the patient to his left side. b. Elevate the patient’s affected leg. c. Bend the affected leg at the knee. d. Use the patient’s belt as a tourniquet. ANS: D After holding direct pressure on the bleeding area, a tourniquet may be implemented. The nurse should immobilize the leg and avoid position changes that could exacerbate bleeding. Elevation of an injured extremity is no longer recommended. PTS: 1 DIF: Cognitive Level: Application REF: 1031 OBJ: 1 (theory) TOP: Control of Bleeding: Safety Alert KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 18. The nurse is reviewing the physician’s notes on a patient’s chart. The nurse notes that the patient demonstrated Cullen sign. The nurse correctly recognizes that this patient most likely had which manifestation? a. Sharp flank pain b. Pain in the upper right quadrant of the abdomen c. Pain with inspiration d. A bluish tinge around the umbilicus ANS: D Cullen sign refers to a bluish tinge around the umbilicus. It may be noted in the presence of internal abdominal hemorrhage. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1033 OBJ: 3 (theory) TOP: Abdominal Trauma KEY: Nursing Process Step: Diagnosis MSC: NCLEX: Physiological Integrity: Physiological Adaptation 19. The nurse is caring for a conscious patient who has symptoms consistent with hypoglycemia. After a serum glucose reading supports this diagnosis, which substance is preferred to initially increase the patient’s glucose level? a. A carbonated soda b. A teaspoon of white sugar c. A glass of milk d. IV glucose ANS: C When the patient is conscious, an oral glucose-containing substance is suggested. A glass of milk, glucose tablets, or hard candy is preferred. PTS: 1 DIF: Cognitive Level: Application REF: 1034 OBJ: 1 (theory) TOP: Hypoglycemia: Treatment KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential MULTIPLE RESPONSE 20. The nurse recognizes which indications of respiratory distress? (Select all that apply.) a. Gasping b. Wheezing c. Stridor d. Choking e. Stupor ANS: A, B, C, D All options except stupor are indicators of respiratory distress. PTS: 1 DIF: Cognitive Level: Knowledge REF: 1030, Focused Assessment OBJ: 6 (theory) TOP: Signs of Respiratory Distress: Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 21. In which situation(s) is moving a victim of an automobile accident necessary? (Select all that apply.) a. Presence of pooled gasoline b. Oncoming traffic c. Submersion in snow d. Request from the victim to be moved e. Exposure to hot pavement ANS: A, B, C, E A victim request to be moved is not a valid reason to do so if the victim is safe. The patient should be removed from pooled gasoline, oncoming traffic, submerging snow, and hot pavement. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1027 OBJ: 2 (theory) TOP: Moving an Accident Victim: Rationale KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control 22. The nurse counsels a group of young track athletes about heatstroke prevention. Which information should the nurse include? (Select all that apply.) a. Drink plenty of fluids with high sugar content. b. Wear lightweight, loose clothing. c. Practice in the early morning. d. Rest frequently in cool places. e. Wear dark-colored clothing to block sun rays. ANS: B, C, D Athletes should wear lightweight and loose clothing, practice in the morning to avoid peak heat hours, and rest frequently in the shade to prevent overheating. While athletes should drink plenty of fluids for hydration, liquids should be nonalcoholic, noncaffeinated, and low sugar; liquids with alcohol, caffeine, and sugar increase dehydration. Dark-colored clothing will absorb heat; athletes should wear light-colored clothing. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1034 OBJ: 3 (theory) TOP: Heatstroke: Prevention KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 23. The home health nurse in Wyoming gives instruction to an 80-year-old patient in the prevention of hypothermia. Which information should the nurse include? (Select all that apply.) a. Wear multiple layers of clothing. b. Wear a loose-fitting hat. c. Move about briskly. d. Drink warm fluids from a thermos. e. Wear gloves and earmuffs. ANS: A, C, D, E The patient should wear multiple layers of clothing, move about briskly, drink warm fluids, and wear ear and hand protection. The patient should also wear a hat, but it should fit snugly. PTS: 1 DIF: Cognitive Level: Application REF: 1035 OBJ: 3 (theory) TOP: Hypothermia: Prevention KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 24. Which physiological differences explain why the older adult is prone to hypothermia? (Select all that apply.) a. Decreasing appetite with less food intake b. Increasing subcutaneous fat c. Decreasing metabolism d. Increased likelihood of atherosclerosis e. Decreasing activity level ANS: A, C, D, E The older adult is prone to hypothermia because of less food intake, lower metabolism, possibility of atherosclerosis, decreased activity level, and less subcutaneous fat. PTS: 1 DIF: Cognitive Level: Application REF: 1034 OBJ: 3 (theory) TOP: Hypothermia: Older Adult KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 25. Treatment for frostbite includes which actions? (Select all that apply.) a. Chafing the hands and fingers gently to reestablish circulation. b. Immersion of hands and feet in warm water. c. Wrapping hands in mitten-like dressings to retain warmth. d. Administering opioids to reduce pain. e. Elevating affected limbs. ANS: A, B, E Gently chafing hands and fingers, immersing extremities in water, and elevating affected limbs are indicated treatments for hypothermia. Nonsteroidal anti-inflammatory drugs are the analgesic of choice, because opioids decrease function and delay circulatory recovery. Fingers should be wrapped individually, not touching each other. PTS: 1 DIF: Cognitive Level: Application REF: 1035 OBJ: 3 (theory) TOP: Frostbite: Treatment KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 26. The nurse is instructing a group of 25- to 35-year-old hikers about heatstroke prevention. Which participant drink selection indicates the need for further education? (Select all that apply.) a. Clear carbonated soda b. Diet caffeinated cola c. Water d. Beer e. Sugar-sweetened energy drinks ANS: A, B, D, E The wrong fluids can increase fluid loss. To aid in the prevention of heatstroke, the hiker should drink plenty of fluids that are nonalcoholic, caffeine free, and low in sugar content. Clear carbonated soda and sweetened energy drinks are high in sugar. Diet cola contains caffeine. PTS: 1 DIF: Cognitive Level: Analysis REF: 1034 OBJ: 4 (theory) TOP: Heatstroke: Prevention KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 27. The nurse is caring for a patient suspected of having heatstroke. Which findings are consistent with this diagnosis? (Select all that apply.) a. Bradycardia b. Tachycardia c. Irregular pulse patterns d. Visual disturbances e. Increased urinary output ANS: B, C, D Heatstroke may cause a weak, rapid, irregular pulse, and visual disturbances. Other manifestations may include decreased urinary output, an alteration in neurologic function, dizziness, and nausea. PTS: 1 DIF: Cognitive Level: Application REF: 1034 OBJ: 4 (theory) TOP: Heatstroke KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation COMPLETION 28. ________________ are the organisms most commonly associated with infections leading to sepsis and septic shock. ANS: Bacteria Bacteria are commonly associated with infections that lead to sepsis and septic shock. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1042, Table 44-3, 1046 OBJ: 4 (theory) TOP: Etiology of Types of Shock: Septic Shock KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Adaptation MATCHING The nurse differentiates the types of treatment that are appropriate for each type of shock. Match the type of shock with the type of treatment associated with it. a. Cardiogenic shock b. Hypovolemic shock c. Anaphylactic shock d. Neurogenic shock e. Insulin shock 29. Administration of epinephrine 30. Administration of vasoconstrictors 31. Administration of glucose orally or IV 32. Administration of fluids 33. Administration of inodilators 29. ANS: C PTS: 1 DIF: Cognitive Level: Analysis REF: 1042, Table 44-3 OBJ: 10 (theory) TOP: Types of Shock: Treatment KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 30. ANS: D PTS: 1 DIF: Cognitive Level: Analysis REF: 1042, Table 44-3 OBJ: 10 (theory) TOP: Types of Shock: Treatment KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 31. ANS: E PTS: 1 DIF: Cognitive Level: Analysis REF: 1042, Table 44-3 OBJ: 10 (theory) TOP: Types of Shock: Treatment KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 32. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 1042, Table 44-3 OBJ: 10 (theory) TOP: Types of Shock: Treatment KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 33. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 1042, Table 44-3 OBJ: 10 (theory) TOP: Types of Shock: Treatment KEY: Nursing Process Step: N/A MSC: NCLEX: N/A A neighbor is found slumped over the lawn mower and is unconscious. Arrange the interventions made by the first responder in appropriate order. a. Tell neighbor’s wife to call 911. b. Assess for heartbeat. c. Initiate CPR if no respiration or circulation can be assessed. d. Assess for signs of breathing. e. Shake patient and call name to assess for level of consciousness (LOC). 34. Step 1 35. Step 2 36. Step 3 37. Step 4 38. Step 5 34. ANS: A PTS: 1 DIF: Cognitive Level: Analysis REF: 1040 OBJ: 6 (theory) TOP: CPR: Preliminary Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 35. ANS: E PTS: 1 DIF: Cognitive Level: Analysis REF: 1040 OBJ: 6 (theory) TOP: CPR: Preliminary Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 36. ANS: D PTS: 1 DIF: Cognitive Level: Analysis REF: 1040 OBJ: 6 (theory) TOP: CPR: Preliminary Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 37. ANS: B PTS: 1 DIF: Cognitive Level: Analysis REF: 1040 OBJ: 6 (theory) TOP: CPR: Preliminary Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 38. ANS: C PTS: 1 DIF: Cognitive Level: Analysis REF: 1040 OBJ: 6 (theory) TOP: CPR: Preliminary Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential Chapter 45: Care of Patients with Anxiety, Mood, and Eating Disorders deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The nurse observes a coworker who is always behind because he checks and rechecks the accuracy of his medication dosages. Even after being reassured his dosages are correct, he checks them again. The nurse suspects her coworker suffers from which disorder? a. Perfectionism b. Phobic disorder c. Obsessive-compulsive disorder (OCD) d. General anxiety disorder ANS: C When a person has an OCD, he experiences an obsession, recurrent, or intrusive thoughts that he cannot stop thinking about, and these thoughts create anxiety. A compulsive act is an act that the person feels compelled to perform. For example, a person may experience anxiety and so performs repetitive handwashing in an attempt to reduce that anxiety. Time spent in these thoughts and rituals can become overwhelming to the point of interfering with normal life. PTS: 1 DIF: Cognitive Level: Application REF: 1055 OBJ: 3 (theory) TOP: OCD: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity 2. The nurse is helping a patient get dressed to go to her dialysis treatment. The patient bursts into tears and says, “I can’t go! I can’t stand another day in that awful place. I will die if I have to go!” Which intervention is best? a. Stop the dressing process and calmly ask the patient talk about her feelings. b. Continue to dress the patient and reassure her that she will feel better after her treatment. c. Stop the dressing process and remind the patient that missing a treatment can make her very sick. d. Continue dressing the patient and remind her that she must stay on task in order to be on time. ANS: A A calm and supportive attitude will help the patient identify feelings. The nurse should put the dressing process on hold so that the nurse can focus attention on a therapeutic response to the patient’s concerns. The nurse should then ask an open-ended question to give the patient freedom to express her concerns. Making a threatening statement about consequences of missed treatments only exacerbates the patient’s concern. Continuing to dress the patient while offering empty reassurance or changing the subject ignores the problem at hand. PTS: 1 DIF: Cognitive Level: Analysis REF: 1056, 1070 OBJ: 1 (theory) TOP: Moderate Anxiety: Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 3. The nurse is caring for a patient who was admitted with fractures sustained during an MVC (motor vehicle collision). The patient tearfully confesses that she relives the accident in her dreams and is afraid to sleep. The nurse recognizes that this scenario is consistent with which disorder? a. Post-traumatic stress disorder (PTSD) b. Phobic disorder c. obsessive-compulsive disorder (OCD) d. Panic level of anxiety disorder ANS: A Individuals with PTSD have endured one or more extreme life-threatening events, and the remembrance of these events now produces feelings of intense horror, with recurrent symptoms of anxiety and nightmares or flashbacks. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1055 OBJ: 4 (theory) TOP: PTSD: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity 4. The nurse explains that anxiety disorders differ from normal anxiety. Which statement accurately describes anxiety disorders? a. Anxiety disorders develop into suicidal tendencies. b. Anxiety disorders are seldom controlled. c. Anxiety disorders interfere with effective functioning. d. Anxiety disorders make maintenance of relationships impossible. ANS: C Anxiety disorders interrupt normal day-to-day functioning in the workplace and in family settings. PTS: 1 DIF: Cognitive Level: Knowledge REF: 1053 OBJ: 2 (theory) TOP: Normal Anxiety vs. Debilitating Anxiety KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 5. The nurse is caring for a patient with moderate anxiety. Which activity should the nurse encourage to best manage the patient’s anxiety? a. Taking a walk b. Learning a new game c. Watching an intense television show d. Reading a pamphlet about the negative effects of anxiety ANS: A To best manage moderate level anxiety, the nurse should help provide outlets for tension. These activities include walking, crying, and working at simple, concrete tasks. Learning something new, watching an intense TV show, or reading information about the negative effects of anxiety are activities that may exacerbate anxiety rather than relieve it. PTS: 1 DIF: Cognitive Level: Application REF: 1054, Table 45-1 OBJ: 4 (theory) TOP: Management of Moderate Anxiety KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 6. The nurse is educating a patient who has just been prescribed diazepam (Valium). The nurse cautions the patient that diazepam (Valium) may cause which problem? a. Dependency b. Urinary retention c. Severe dehydration d. Hallucinations ANS: A Valium can cause a physiologic and a psychological dependence. Valium should not cause urinary retention, severe dehydration, or hallucinations. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1056 OBJ: 3 (theory) TOP: Diazepam (Valium): Dependency KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 7. The nurse is educating a patient with generalized anxiety disorder (GAD) who has a new prescription for buspirone (BuSpar). Which information is most important for the nurse to include in the teaching plan? a. Use this medication as needed to manage your anxiety. b. Taper this medication before discontinuing. c. Allow 3 weeks before expecting any relief of symptoms. d. This medication poses a great risk of tolerance and dependence. ANS: B Patients should not stop taking BuSpar abruptly, but should taper this medication according to health care provider instructions. BuSpar is always given as a scheduled drug (never on an as-needed basis). The patient should allow 7 to 10 days for symptoms to subside. No evidence exists that BuSpar causes tolerance or physical dependence PTS: 1 DIF: Cognitive Level: Comprehension REF: 1056, 1057, Table 45-2 OBJ: 3 (theory) TOP: Buspirone (BuSpar) Teaching KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 8. A long-term care facility resident with generalized anxiety disorder (GAD) enters the dining room and discovers that a visitor is sitting in her regular seat. The resident becomes agitated and insists that she cannot eat unless she sits in her chair. Which response is most appropriate? a. Instruct the visitor to move. b. Reassure the resident that she can sit in her regular spot at supper. c. Remind the resident that she will be hungry if she does not eat. d. Insist that the resident eat. ANS: B A calm approach and reassurance will help the anxious patient to mimic the nurse’s behavior. Asking the visitor to move, telling the resident that she will go hungry, or insisting that the resident eat are not therapeutic and will not help in reducing the patient’s anxiety. PTS: 1 DIF: Cognitive Level: Analysis REF: 1054 OBJ: 4 (theory) TOP: Anxiety: Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 9. An older adult resident in a long-term care facility expresses multiple minor complaints at the nurse’s station and wanders about aimlessly in the hallway. The nurse examines the patient’s chart. Which newly prescribed drug may explain his behavior? a. Tylenol b. Theophylline c. Bisacodyl d. Lisinopril ANS: B The drug theophylline may make patients feel anxious and restless. Tylenol, bisacodyl, and lisinopril do not typically have this effect. PTS: 1 DIF: Cognitive Level: Analysis REF: 1058, Older Adult Care Points OBJ: 2 (theory) TOP: Anxiety vs. Drug Reaction KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 10. After having refused lunch and dinner because her “regular” chair was occupied at breakfast, the resident in a longterm care facility asks for a snack. How should the nurse respond? a. “You are hungry now. Is there something else you could have done earlier besides refusing to eat?” b. “Here is your snack. Maybe you won’t be so quick to refuse meals the next time you don’t get your way.” c. “Refusing meals is not the answer. You must eat.” d. “Tell me why you left the dining room without eating.” ANS: A After acute anxiety passes, the nurse should focus on helping the resident recognize the behavior that was exhibited and how to deal more effectively with the anxiety. Scolding the patient, attempting to induce guilt, or causing the patient to dwell on the trigger do not redirect the patient to consider different behaviors. PTS: 1 DIF: Cognitive Level: Analysis REF: 1058 OBJ: 4 (theory) TOP: Anxiety: Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 11. A resident in a long-term care facility has been in a manic stage for 2 days. He has not slept and cannot focus long enough to eat a meal. How should the nurse best enhance the resident’s nutrition? a. Insist he sit down and eat at the table. b. Spoon-feed him at the table at regular mealtimes. c. Offer him small glasses of high-protein drinks every hour. d. Make up a game about who can finish a meal first. ANS: C The patient displays an inability to concentrate and a decreased need for sleep or nutrients. Offering a small amount of highenergy foods and drinks every hour will support nutrition until the manic behavior is under control. Because of the manic patient’s abbreviated focus, eating an entire meal may not be possible. The nurse should not force the patient to sit and eat, demean him by spoon-feeding, or challenge him to process a new activity. PTS: 1 DIF: Cognitive Level: Application REF: 1060, 1071 OBJ: 6 (theory) TOP: Manic Behavior: Nutritional Support KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 12. The nurse is educating a patient with a new prescription for lithium carbonate. Which information is most important for the nurse to include in the teaching plan? a. It can take up to two weeks for Lithium to reach a therapeutic level in the body. b. Lithium is often given in conjunction with loop diuretics. c. Carefully restrict sodium intake to less than 1 gram/day. d. Take medication before breakfast for maximum effectiveness. ANS: A Lithium may take 7-14 days to reach therapeutic level in the body. Diuretics should be avoided while on Lithium therapy. Patients should not restrict sodium intake since low sodium levels could cause Lithium toxicity. Medication should be taken with meals to decrease gastric distress. PTS: 1 DIF: Cognitive Level: Knowledge REF: 1060, Table 45-3 OBJ: 6 (theory) TOP: Lithium Therapy KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 13. A patient has been taking lithium for 5 days. The nurse notes his gait is a little unsteady with a walker, and he complains of thirst and insomnia. Which finding is most important for the nurse to report? a. Manic behavior b. Unsteady gait c. Thirst d. Insomnia ANS: B While all findings should be reported, uncoordinated movement is a sign of lithium toxicity and the priority finding. The patient is likely taking lithium to treat manic behavior. Thirst and insomnia are expected side effects of lithium and not indicative of toxicity. PTS: 1 DIF: Cognitive Level: Analysis REF: 1060, Table 45-3 OBJ: 6 (theory) TOP: Lithium: Side Effects KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 14. The nurse is caring for an older adult patient with a history of anxiety. Which complaint could indicate that the patient may actually be experiencing emotional distress? a. Upset stomach b. Heightened tooth sensitivity c. Unpleasant taste in mouth d. Dizziness ANS: A The older adult population often expresses somatic complaints rather than openly verbalizing emotional distress. You may observe the anxious older adult complaining of an upset stomach, inability to sleep, fatigue, or increased need to urinate. PTS: 1 DIF: Cognitive Level: Application REF: 1058, Older Adult Care Points OBJ: 4 (theory) TOP: Anxiety in Elderly KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 15. The depressed patient who has been taking amitriptyline (Elavil) for the past 2 weeks complains of still feeling depressed and wants to abandon the drug. How should the nurse respond? a. “I will ask the physician about a new order for a different drug.” b. “You probably should quit taking Elavil if it is not helping you.” c. “Sometimes drinking a small glass of wine with meals helps.” d. “These drugs take several weeks to become effective.” ANS: D Tricyclics may take up to 4 weeks before patients experience symptom relief. The patient has not been taking the medication long enough to request a new order. The nurse should not encourage the patient to discontinue the medication. This medication should not be combined with alcohol. PTS: 1 DIF: Cognitive Level: Application REF: 1064, Table 45-4 OBJ: 6 (theory) TOP: Tricyclic Antidepressants: Delayed Effect KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 16. The nurse is caring for a suicidal patient who has been treated effectively with antidepressant therapy. The patient verbalizes that he feels better. The nurse is alert that the patient is most at risk for which potential complication? a. Increased risk of self-harm b. Increased emotional fragility c. Increased potential for weight gain d. Increased activity intolerance ANS: A The risk of suicide is greater now that the patient has increased energy to plan and complete the suicide. Effective antidepressant therapy should not cause an increase in emotional fragility, weight gain, or activity intolerance. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1067 OBJ: 7 (theory) TOP: Suicide: Increased Risk KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 17. What thought process underscores a patient’s anorexia nervosa? a. A desire to be attractive by staying slender. b. A desire to be involved with food preparation of food, but not eating it. c. A desire to punish self by denial of adequate nutrition. d. A desire to gain a sense of control by limiting food intake. ANS: D Anorexia nervosa is characterized by the patient’s refusal to maintain minimal body weight or eat adequate quantities of food. There is a disturbance in the perception of body shape and size and an extreme fear of becoming fat. The patient strives for perfection and control by controlling caloric intake. The person with anorexia nervosa gains a sense of control by limiting food intake. PTS: 1 DIF: Cognitive Level: Analysis REF: 1069 OBJ: 9 (theory) TOP: Anorexia Nervosa: Etiology KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 18. Which classic behavior characterizes bulimia? a. Bingeing and purging b. Refusal to eat c. Excessive exercising d. Hiding food to make it appear it was eaten ANS: A Patients with bulimia nervosa induce vomiting after consuming large quantities of food. This binge eating occurs in a frenzied state and usually in secrecy; afterward, the patient experiences feelings of shame and self-criticism. Laxatives may be taken to purge the system after the binge. Ninety percent of patients with bulimia are young women. PTS: 1 DIF: Cognitive Level: Knowledge REF: 1069 OBJ: 9 (theory) TOP: Bulimia: Classic Behavior KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity 19. The nurse is caring for a patient admitted with a diagnosis of serotonin syndrome. Which type of medication will most likely be included in the plan of treatment? a. Antihypertensive medications b. Intravenous (IV) therapy c. Antianxiety medications d. Sedatives ANS: B Serotonin syndrome is a potential life-threatening condition that could start 30 minutes to 48 hours after taking the medication. Symptoms include change of mental status, increase in pulse and fluctuation in blood pressure, loss of muscular coordination, and hyperthermia. Treatment includes stopping medication, administering IV fluids, and decreasing temperature. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1064, Medication Alert OBJ: 6 (theory) TOP: Medication Safety Alert: Serotonin Syndrome KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential MULTIPLE RESPONSE 20. Which signs and symptoms are consistent with general anxiety disorder (GAD)? (Select all that apply.) a. Heart rate of over 100 beats/min b. Restlessness c. Urinary retention d. Fatigue e. Muscular tension ANS: A, B, D, E A person who experiences persistent, unrealistic, or excessive worry about two or more life circumstances for 6 months or longer is exhibiting symptoms associated with GAD. GAD usually develops slowly and is chronic in nature. Dieresis rather than urinary retention is a commonly seen with GAD. All other options listed are characteristics of GAD. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1054, 1056 OBJ: 3 (theory) TOP: GAD: Signs and Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 21. The nurse outlines the treatment for a person with anxiety disorders, which include(s) which of the following? (Select all that apply.) a. Anxiolytic medication. b. Education about disorder. c. Individual therapy. d. Relaxation techniques. e. Stress management. ANS: A, B, C, D, E All options are aspects of the treatment of the person with anxiety disorders. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1056 OBJ: 3 (theory) TOP: Anxiety Disorders: Treatment KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 22. Which nursing considerations relate to the administration of lithium? (Select all that apply.) a. Administer the medication on an empty stomach. b. Restrict fluids to 1000 mL daily. c. Draw frequent blood levels. d. Teach the importance of contraception while taking the drug. e. Teach the importance of avoid caffeine while taking the drug. ANS: C, D, E Lithium should be taken with food, and fluids should be increased to 3000 mL daily. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1060, Table 45-3 OBJ: 6 (theory) TOP: Lithium: Nursing Considerations KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 23. Which signs and symptoms characterize a major depressive disorder? (Select all that apply.) a. Euphoria b. Psychomotor retardation c. Indecisiveness d. Sleep disturbances e. Suicidal ideation ANS: B, C, D, E Major depressive disorder is diagnosed when at least five symptoms characteristic of depression have been present for at least 2 weeks. These symptoms include an overwhelming feeling of sadness; inability to feel pleasure or experience interest in daily activities; weight gain or loss not attributed to dieting; sleep disturbances; fatigue or loss of energy; feelings of worthlessness; difficulty in making decisions or concentrating; and suicidal thoughts. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1063 OBJ: 6 (theory) TOP: Major Depressive Disorder: Diagnostic Criteria KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity 24. Which characteristic(s) increase(s) the probability of suicidal ideations in a depressed patient? (Select all that apply.) a. Owning a gun collection b. Living with wife and three children c. Being an active member of the local church d. Having a plan to shoot himself in a motel e. Having a brother that recently committed suicide ANS: A, D, E Suicidal risk increases if the patient has a plan, access to a weapon, and a recent loss. PTS: 1 DIF: Cognitive Level: Knowledge REF: 1067 OBJ: 7 (theory) TOP: Suicide: Assessment KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity 25. A patient is considering having electroconvulsive therapy (ECT) to treat his severe depression. Which statement(s) indicate(s) the patient understands the procedure? (Select all that apply.) a. “I will have treatments once every other month.” b. “The shock will cause me to have a short seizure.” c. “This treatment is often more successful than medications.” d. “I will have to be hospitalized the day before and after the treatments for observation.” e. “The treatments will be performed in the early morning hours.” ANS: B, C, E ECT is the oldest form of brain stimulation therapy used for severe depression. After several regimens of medication are unsuccessful, or if the patient is severely depressed or actively suicidal, ECT is considered. Evidence suggests that ECT is more effective than pharmacotherapy. ECT consists of electric shock delivered to the brain via electrodes applied to the temples. This shock artificially induces a grand mal seizure lasting 30 to 90 seconds. The patient typically receives 8 to 12 treatments spread over several weeks. ECT is frequently done on an outpatient basis in the early morning. PTS: 1 DIF: Cognitive Level: Application REF: 1064 OBJ: 6 (theory) TOP: ECT KEY: Nursing Process Step: Evaluation MSC: NCLEX: Health Promotion and Maintenance 26. The nurse is reviewing the medical history of a patient who is being evaluated for anorexia nervosa. Which characteristic(s) would be consistent with the condition? (Select all that apply.) a. Weight loss of 2 to 3 pounds in the past month b. Binge eating c. Frequent mood changes d. Absence of three consecutive menstrual periods e. Body weight less than 85% of what is expected for height and weight ANS: C, D, E Anorexia nervosa is characterized by the patient’s refusal to maintain minimal body weight or eat adequate quantities of food. There is a disturbance in the perception of body shape and size and an extreme fear of becoming fat. The patient strives for perfection and control by controlling caloric intake. Defining characteristics include frequent mood fluctuation, absence of three consecutive menstrual periods, and body weight less than 85% of what is expected for height and weight. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1068-1069 OBJ: 9 (theory) TOP: Anorexia Nervosa KEY: Nursing Process Step: Diagnosis MSC: NCLEX: Physiological Integrity: Physiological Adaptation COMPLETION 27. The nurse points out that a persistent irrational fear of a specific object or situation that causes anxiety that interferes with responsibilities is a(n) _________. ANS: phobia A phobia is an irrational fear of a specific object or situation that renders the person unable to fulfill responsibilities. PTS: 1 DIF: Cognitive Level: Knowledge REF: 1055 OBJ: 2 (theory) TOP: Phobia: Definition KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 28. The nurse takes into consideration that it is estimated that _____% of the population will have some form of anxiety disorder. ANS: 25 twenty-five One person out of four will have symptoms of an anxiety disorder in his or her lifetime. PTS: 1 DIF: Cognitive Level: Knowledge REF: 1053 OBJ: 1 (theory) TOP: Anxiety: Incidence KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance Chapter 46: Care of Patients with Substance Abuse Disorders deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. The alcoholic patient says to the nurse, “I am not an alcoholic. I can quit any time I want to.” The nurse recognizes that the patient is using which defense mechanism? a. Repression b. Denial c. Rationalization d. Intellectualization ANS: B Denial is ignoring reality in spite of hard evidence. Denial is a mechanism frequently used by substance abusers. Repression refers to unconsciously blocking an unwanted thought or memory from open expression. Rationalization attempts to justify a behavior or action by making an excuse or an explanation. Intellectualization is the excessive reasoning and logic to counter emotional distress. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1074 OBJ: 4 (theory) TOP: Alcoholism: Defense Mechanism KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: Coping and Adaptation 2. The wife of an alcoholic tells the nurse, “My husband only drinks on the weekends to relax. He has a very stressful job.” The nurse recognizes that the patient’s wife is using which defense mechanism? a. Repression b. Denial c. Rationalization d. Identification ANS: C Rationalization is a justification for an unreasonable act to make it appear reasonable. Rationalization is used by many families to allay their own anxiety about the substance abuse of a family member. Repression refers to unconsciously blocking an unwanted thought or memory from open expression. Denial is ignoring reality in spite of hard evidence. Denial is a mechanism frequently used by substance abusers. Identification refers to modeling behaviors after another individual. PTS: 1 DIF: Cognitive Level: Application REF: 1074 OBJ: 5 (theory) TOP: Family Reaction to Substance Abuse: Rationalization KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity 3. Which statement accurately explains the difference between an enabler and a co-dependent? a. A codependent covers up the substance abuser’s behavior. b. A codependent rationalizes the substance abuser’s behavior. c. An enabler uses the substance abuser’s behavior to build up his or her own self-esteem. d. An enabler is also a substance abuser. ANS: A The codependent “fixes” things by overcompensating to prevent the abuser from facing reality. Enabling refers to “helping” a person so that the person’s consequences from unhealthy behavior are less severe; thus enabling “helps” the unhealthy behavior to continue. PTS: 1 DIF: Cognitive Level: Application REF: 1075 OBJ: 5 (theory) TOP: Codependent vs. Enabler KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 4. How long does it take the body to metabolize a single can of beer? a. 20 minutes b. 30 minutes c. 40 minutes d. 60 minutes ANS: D The metabolization of any amount of alcohol takes approximately 1 hour. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1075 OBJ: 3 (theory) TOP: Alcohol: Metabolization Time KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. A person in jail for public intoxication has been without alcohol for 12 hours. Which finding indicates that the patient may be withdrawing from alcohol? a. Irritability b. Nausea and vomiting c. Hallucinations d. Seizures ANS: A Marked irritability is the early sign (6 to 12 hours after last drink) of alcohol withdrawal. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1075 OBJ: 6 (theory) TOP: Alcohol Withdrawal: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 6. An intoxicated patient is admitted to a treatment center for detoxification. The nurse understands that his withdrawal will be supported with which method? a. Psychotherapy support b. Large doses opioids to ensure sedation for 72 hours c. Symptomatic relief until the substance clears his symptoms d. Titrated amounts of alcohol until severe withdrawal resolves ANS: C The alcoholic in withdrawal is supported with symptomatic relief for nausea and vomiting, cramps, and possible seizure. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1076 OBJ: 6 (theory) TOP: Alcoholism: Detoxification KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 7. After detoxification from substance abuse, the patient says, “I feel better than I have in years! All I needed was some rest. I am not an alcoholic.” Which response is best for the nurse to make? a. “What were you doing that got you admitted to the detoxification center?” b. “Alcoholism has many definitions. What is yours?” c. “Admitting to alcoholism is hard.” d. “Alcoholism has ruined your life. How can you say you are not an alcoholic?” ANS: A Confronting denial and encouraging self-diagnosis is the point of the treatment phase after detoxification. Asking for the patient’s definition of alcoholism allows for the patient to intellectualize the problem. Stating that alcoholism is “hard” is a sympathetic and unhelpful response. “Alcoholism has ruined your life” is accusatory and counterproductive. PTS: 1 DIF: Cognitive Level: Analysis REF: 1076 OBJ: 6 (theory) TOP: Alcoholism: Post-detoxification KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 8. The nurse explains that an alternative to disulfiram (Antabuse) is the drug naltrexone (ReVia). Which information should the nurse include in the teaching plan? a. Naltrexone (ReVia) causes severe headaches if alcohol is consumed while using the drug. b. Naltrexone (ReVia) can cause a dependence on the medication itself if taken improperly. c. Naltrexone (ReVia) releases endorphin-like enzymes that mimic intoxication. d. Naltrexone (ReVia) blocks craving and prevents relapse. ANS: D Naltrexone (ReVia) can be used to block the craving for alcohol and to prevent relapse in the recovery phase. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1076 OBJ: 6 (theory) TOP: TreatmentKEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 9. The nurse encourages the recovering alcoholic to participate in group therapy. Which benefit is most important for the nurse to mention? a. Development of improved social skills b. Progression toward sobriety c. Provision of a sense of belonging d. Increasing self-discipline ANS: D The learning of the skill of self-discipline is the long-lasting benefit from group therapy. The other options are also benefits, but the major one is self-discipline, a skill a drug abuser must acquire for successful rehabilitation. PTS: 1 DIF: Cognitive Level: Analysis REF: 1076 OBJ: 1 (clinical) TOP: Group Therapy: Benefits KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 10. The nurse is aware that when Korsakoff syndrome is suspected from behavioral cues, the syndrome can be confirmed by which diagnostic test? a. Liver biopsy b. Brain scan c. Magnetic resonance imaging d. Spinal tap ANS: B The individual with Korsakoff syndrome has grossly impaired memory and gait disturbance. Confabulation (making up stories) frequently is seen as an attempt to communicate. A brain scan will show brain atrophy; currently there is no treatment to reverse the condition. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1078 OBJ: 3 (theory) TOP: Korsakoff Syndrome: Diagnosis KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 11. The nurse uses the CAGE challenge to alcoholics who persist in denial. What does the “G” in the set of questions from CAGE represent? a. Get: “Do you feel like you must get alcohol?” b. Go: “Do you go out to drink?” c. Gone: “Is memory of drinking episodes gone?” d. Guilty: “Do you feel guilty about your drinking?” ANS: D A commonly used screening tool for alcohol abuse is the CAGE assessment. Two or more “yes” answers have a 90% correlation with an alcohol abuse problem. The “G” stands as a reminder for the question, “Do you feel guilty about your drinking?” PTS: 1 DIF: Cognitive Level: Comprehension REF: 1083 OBJ: 3 (theory) TOP: CAGE Queries: Significance KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 12. The nurse is caring for a patient who was admitted for a lorazepam (Ativan) overdose. Which assessment finding indicates that the patient is experiencing withdrawal? a. Lethargy b. Urine output of 40 mL/hr c. Heart rate of 48 beats/min d. Blood pressure of 140/90 ANS: D Elevated blood pressure is consistent with withdrawal from a central nervous system (CNS) depressant like lorazepam (Ativan), a benzodiazepine. If an individual has been abusing drugs that depress the CNS and goes through withdrawal, other symptoms would include an elevation in pulse, nervousness, and heightened anxiety. The patient would likely be agitated rather than lethargic and tachycardic. Urine output of 40 mL/hr is a normal finding. PTS: 1 DIF: Cognitive Level: Analysis REF: 1078 OBJ: 3 (theory) TOP: Benzodiazepine: Withdrawal KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 13. The nurse is concerned about a coworker who she suspects is abusing amphetamines. Which behavior best validates the nurse’s concern? a. Frantic, excited speech b. Poor attention to detail c. Poor personal hygiene d. Insatiable hunger ANS: A Excited speech, euphoric behavior, increased alertness, and anorexia are indications of abuse of amphetamines. PTS: 1 DIF: Cognitive Level: Application REF: 1079, Table 46-3 OBJ: 3 (theory) TOP: Amphetamine Abuse: Signs KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity 14. Why do many people who abuse Cannabis (marijuana) rationalize their use? a. Cannabis sedates them. b. Cannabis expands their senses. c. Cannabis heightens sexual pleasure. d. Cannabis may be obtained legally for therapeutic purposes. ANS: B Many young people offer the increased sensitivity to sound, colors, and other environmental elements as a rationale for using the nonaddicting drug. PTS: 1 DIF: Cognitive Level: Analysis REF: 1082 OBJ: 3 (theory) TOP: Cannabis: Rationalization for Use KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 15. A patient is admitted after abusing an inhalant. Which safety precaution is most important for the nurse to take? a. Check the patient’s temperature hourly. b. Place the patient on seizure precautions. c. Monitor carefully for changes in urine output. d. Ensure that respiratory support equipment is present at the bedside. ANS: D Medical treatment and intervention for both hallucinogens and inhalants include provision of safety for the individual who may be experiencing a bad “trip.” Emergency measures may be necessary to provide respiratory support for an individual who has impaired gas exchange as a result of inhalants. PTS: 1 DIF: Cognitive Level: Application REF: 1083 OBJ: 3 (theory) TOP: Hallucinogen Abuse: Precautions KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 16. Which action best aids in successful rehabilitation from substance abuse? a. The patient and family members collaborate to develop treatment goals. b. The patient and family members accurately list signs of relapse. c. The patient and family members commit to discarding all drugs and paraphernalia. d. The patient and family members commit to a 12-step program. ANS: A Collaboration is basic for success of rehabilitation. The patient and family must be part of the decision-making process for the formulation of treatment goals. While it is important to be aware of signs of relapse and essential to discard any paraphernalia and a 12-step program could be helpful, it is most important for the patient and family members to be active participants in the treatment plan. PTS: 1 DIF: Cognitive Level: Analysis REF: 1084 OBJ: 5 (theory) TOP: Treatment: Goals KEY: Nursing Process Step: Planning MSC: NCLEX: Health Promotion and Maintenance: Prevention and Early Detection of Disease 17. Which action is most important for the nurse to take before providing care for substance abusers? a. Become familiar with self-help programs. b. Examine personal bias relative to substance abuse. c. Become knowledgeable about theories of addiction. d. Ensure consistency with each patient. ANS: B Nurses must first determine their own biases and attitude toward substance abuse and substance abusers before they can relate effectively with the patient. Familiarization with resources and knowledge about theories of addiction are tools of lesser importance. Consistency with patients occurs while providing care to substance abusers. PTS: 1 DIF: Cognitive Level: Analysis REF: 1082, Think Critically OBJ: 3 (theory) TOP: Nurse’s Bias: Evaluation KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 18. Shortly after receiving one dose of naloxone (Narcan) for an overdose of opiates, a patient experiences a change in level of consciousness and a decreased respiratory rate. What should the nurse do first? a. Inform the charge nurse. b. Repeat the Narcan. c. Notify the health care provider. d. Update family members. ANS: B Narcan has a short half-life, and opiate action may resume and cause respiratory depression. Narcan may be repeated, or the nurse can request a continuous intravenous infusion of the drug. PTS: 1 DIF: Cognitive Level: Analysis REF: 1077, Table 46-2 OBJ: 3 (theory) TOP: Narcan: Short Half-life KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 19. The nurse is caring for an undernourished alcoholic patient. The nurse is helping the patient to select items from the menu. What dietary goal should the nurse try to help the patient achieve? a. Construct a diet that consists of at least 30% protein. b. Limit all fat and cholesterol. c. Limit sodium intake to less than 1.5 grams. d. Construct a diet that consists of at least 50% carbohydrates. ANS: D The diet for the malnourished alcoholic patient should be high in protein and consist of at least 50% carbohydrates. There are no specific limitations for fat, cholesterol, or sodium. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1088, Nursing Care Plan 46-1 OBJ: 3 (theory) TOP: Nursing Care Plan 47-1: Care of the Patient with a Substance Abuse Disorder KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 20. The nurse is caring for a patient who is undergoing detoxification from alcohol. Which supplement can the nurse expect to be included in the prescribed medications? a. Potassium chloride b. Thiamine c. Riboflavin d. Folic acid ANS: B The treatment for the alcoholic undergoing detoxification includes the administration of large doses of thiamine (vitamin B1). Thiamine acts as a nerve insulator in the body and is absent in the diets of most chronic alcoholics. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1078 OBJ: 3 (theory) TOP: Alcoholism: Treatment KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 21. The nurse is caring for a patient who has a heightened risk for seizures during his alcohol detoxification. Which medication may be included in the patient’s care? a. Magnesium sulfate b. Chlordiazepoxide (Valium) c. Promethazine (Phenergan) d. Dicyclomine (Bentyl) ANS: A The person undergoing alcohol withdrawal is at risk for the development of seizures. Magnesium sulfate may be prescribed to prevent their onset. Chlordiazepoxide may be administered to reduce anxiety. Promethazine (Phenergan) and dicyclomine (Bentyl) may be used to reduce symptoms such as nausea and vomiting. PTS: 1 DIF: Cognitive Level: Application REF: 1076 OBJ: 6 (theory) TOP: Alcoholism: Treatment KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential MULTIPLE RESPONSE 22. Which actions describe diagnostic criteria for the diagnosis of substance abuse? (Select all that apply.) a. Failure to meet obligations b. Putting self and others in potential harm c. Experiencing conflict with law enforcement authorities d. Developing physical debilitation e. Denying existence of a problem ANS: A, B, C Physical debilitation and denial are not in the criteria established by the American Psychiatric Association for the diagnosis of substance abuse. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1073 OBJ: 2 (theory) TOP: Substance Abuse: Diagnostic Criteria KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 23. Which criteria are part of alcohol dependency diagnosis guidelines? (Select all that apply.) a. Identifiable withdrawal signs and symptoms b. Decreasing tolerance c. Altered family relationships d. Blackouts or amnesia pertinent to drinking episodes e. Altered occupational productivity ANS: A, C, D, E Identifiable withdrawal signs and symptoms, altered family relationships, blackouts or amnesia pertinent to drinking episodes, and altered occupational productivity are all part of the diagnostic guidelines for the diagnosis of alcohol dependency. Increasing tolerance is also part of the diagnostic criteria. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1073 OBJ: 3 (theory) TOP: Alcohol Dependence: Diagnostic Criteria KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 24. The nurse cautions the recovering alcoholic who is on disulfiram (Antabuse) should avoid even small exposure to alcohol. Which signs and symptoms are characteristic of a reaction of disulfiram (Antabuse) with alcohol? (Select all that apply.) a. Chest pain b. Nausea and vomiting c. Hypertension d. Blurred vision e. Blinding headache ANS: A, B, D Disulfiram (Antabuse) is a drug that causes unpleasant reactions if the patient decides to return to drinking anytime within 2 weeks after starting Antabuse. Even small quantities of alcohol that might be inhaled from shaving lotion could trigger serious reactions such as chest pain, nausea and vomiting, hypotension, weakness, blurred vision, and confusion. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1076 OBJ: 6 (theory) TOP: Antabuse: Effect KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 25. Which findings indicate that the recovering alcoholic may be developing Wernicke encephalopathy? (Select all that apply.) a. Confusion b. Hallucinations c. Verbally aggressive behavior d. Ataxia e. Seizures ANS: A, D A serious effect of chronic alcohol abuse is damage to brain cells. A condition that is reversible with treatment is Wernicke encephalopathy. This condition precedes Korsakoff syndrome (substance-induced persisting dementia), which is irreversible. If the individual has a history of alcohol use and displays the symptoms of confusion, ataxia, and significant memory loss, Wernicke encephalopathy is suspected. Verbal aggression, hallucinations, and seizures are not characteristic of Wernicke encephalopathy. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1078 OBJ: 3 (theory) TOP: Wernicke Encephalopathy: Signs and Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 26. In what ways do support groups benefit substance abusers? (Select all that apply.) a. Support groups provide healthy relationships. b. Support groups offer opportunities to practice new coping skills. c. Support groups decrease stress and anxiety. d. Support groups improve social skills. e. Provide cathartic opportunities. ANS: A, B, C, D, E All options are benefits of support groups. PTS: 1 DIF: Cognitive Level: Application REF: 1080 OBJ: 1 (clinical) TOP: Support Groups: Purpose KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 27. Patients who use inhalants and hallucinogens are likely to experience which negative effects? (Select all that apply.) a. Distortion of senses b. Intense pruritus c. Uncontrolled flashbacks d. Koilonychia e. Severely impaired judgment ANS: A, C, E Hallucinogens cause distortion of the senses, an inability to separate fact from fantasy, impaired sense of time, and severely impaired judgment. Users never know whether they will have a good “trip” or a bad one. Uncontrolled flashbacks (feelings and sensations associated with use despite being drug-free) can occur. This group of drugs is very dangerous because use is known to cause panic, paranoia, and death from extremely impaired judgment. Inhalants and hallucinogens are not known to cause intense itching (pruritus) or spoon-shaped nails (koilonychia). PTS: 1 DIF: Cognitive Level: Comprehension REF: 1082-1083 OBJ: 3 (theory) TOP: Hallucinogens: Effects KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 28. What actions does becoming substance free involve? (Select all that apply.) a. Committing to a lifestyle change. b. Developing new coping skills. c. Committing to honesty in communication. d. Gaining an awareness of possible periods of relapse. e. Completing a program in 12 months. ANS: A, B, C, D The limitation of 12 months is not part of the commitment. Rehabilitation may take several years or a lifetime. PTS: 1 DIF: Cognitive Level: Analysis REF: 1089 OBJ: 3 (clinical) TOP: Rehabilitation: Skills KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity MATCHING The nurse clarifies terms relative to substance abuse. Match the option with the definition. a. Abuse b. Psychological dependence c. Addiction d. Tolerance e. Withdrawal 29. Needs substance to prevent symptoms of withdrawal 30. Symptomatology related to cessation of drug 31. Needs substance to feel good 32. Uses psychoactive drugs in nontherapeutic manner 33. Needs increasing amounts of substance to achieve desired effect 29. ANS: C PTS: 1 DIF: Cognitive Level: Knowledge REF: 1079 OBJ: 2 (theory) TOP: Terms: Definition KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 30. ANS: E PTS: 1 DIF: Cognitive Level: Knowledge REF: 1075 OBJ: 2 (theory) TOP: Terms: Definition KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 31. ANS: B PTS: 1 DIF: Cognitive Level: Knowledge REF: 1073 OBJ: 2 (theory) TOP: Terms: Definition KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 32. ANS: A PTS: 1 DIF: Cognitive Level: Knowledge REF: 1073 OBJ: 2 (theory) TOP: Terms: Definition KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 33. ANS: D PTS: 1 DIF: Cognitive Level: Knowledge REF: 1073 OBJ: 2 (theory) TOP: Terms: Definition KEY: Nursing Process Step: N/A MSC: NCLEX: N/A Chapter 47: Care of Patients with Cognitive Disorders deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. Which percentage of the population that is 85 years of age and older has some stage of Alzheimer disease (AD)? a. 10% b. 20% c. 35% d. 50% ANS: D AD is the most common degenerative disease of the brain. Approximately 5.3 million Americans have AD (Alzheimer Association, 2010), and there is no known cause or cure. AD typically affects people over 65 years of age, but can also strike younger people. The 85-year-old and over age group is currently the fastest-growing age group in the United States. It is estimated that 50% of this age group have AD. PTS: 1 DIF: Cognitive Level: Knowledge REF: 1094 OBJ: 1 (theory) TOP: AD: Incidence KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 2. An 85-year-old man is admitted to the hospital with gastroenteritis and dehydration. He receives a dose of meclizine hydrochloride, an anticholinergic, for vomiting. He begins to hallucinate and talk to his wife, who has been dead for 10 years. Which explanation best describes this behavior? a. Dementia related to advanced age b. Delirium related to dehydration c. Dementia related to early Alzheimer’s disease (AD) d. Delirium related to side effect of anticholinergic ANS: D Anticholinergic drugs can cause sudden confusion in older adults. There is nothing in the history that suggests that the behavior would be related to AD or any other dementia as dementias progress slowly. Dehydration would increase the effect of the anticholinergic. PTS: 1 DIF: Cognitive Level: Analysis REF: 1093 OBJ: 2 (theory) TOP: Delirium: Etiology KEY: Nursing Process Step: Assessment MSC: NCLEX: Health Promotion and Maintenance 3. The nurse is aware that the older adult is at risk for drug-induced delirium. Which age-related change contributes to this risk? a. Slower bowel motility b. Reduced fluid intake c. Overall reduced metabolism d. Sedentary lifestyle ANS: C Slower renal and liver clearance of drugs allows the drugs to accumulate in the system of the older adult. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1093, Older Adult Care Points OBJ: 2 (theory) TOP: Drug-Induced Delirium: Older Adult KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 4. Memory lapses seen in early stages of Alzheimer disease (AD) are related to the pathophysiology of which condition? a. Frontal lobe atrophy b. Overproduction of neurotransmitters c. Pituitary disorders d. Inadequate clearance of metabolic toxins ANS: A Loss of neurons in the frontal and temporal lobes results in atrophy and the many signs of AD, memory deficits being one of the earliest. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1094 OBJ: 3 (theory) TOP: AD: Pathophysiology KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 5. The nurse notes that the newly admitted patient with Alzheimer disease (AD) has significant anomia. Which intervention is most appropriate for this problem? a. Frequently reorient the patient to his room location. b. Remind the patient about the names and uses for particular items. c. Assist the patient with all meals. d. Wait patiently for the patient to find the word he wants. ANS: D Anomia is the inability to recall a word. Waiting for the patient to remember the word or be able to substitute another is more supportive than supplying the word for him. PTS: 1 DIF: Cognitive Level: Analysis REF: 1094 OBJ: 3 (theory) TOP: Anomia: Intervention KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 6. The nurse is assisting the patient with middle-stage Alzheimer’s disease (AD) with dressing. Which action is most appropriate? a. Select clothes and dress the patient. b. Layout clothing and coach the patient to dress self. c. Ask the patient what he wants to wear. d. Open the closet and tell the patient to choose a shirt. ANS: B Coaching the patient to dress himself helps preserve dignity and function. Selecting clothes and dressing the patient does not allow the patient to actively participate in any way. Asking the patient what he wants to wear and telling him to choose a shirt could increase confusion and indecision. PTS: 1 DIF: Cognitive Level: Application REF: 1098, Nursing Care Plan 47-1 OBJ: 3 (theory) TOP: AD: Activities of Daily Living KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 7. The nurse differentiates vascular dementia from Alzheimer dementia. Which causative factor is responsible for vascular dementia? a. Cerebral atrophy b. Global reduction of cognition c. Hypertension d. Emboli in cerebral vessels ANS: D Vascular dementia occurs from brain tissue becoming hypoxic and necrotic in local areas due to small emboli. The deficits may be intellectual or loss of sensory function. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1100 OBJ: 2 (theory) TOP: Vascular Dementia vs. Alzheimer Dementia KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 8. In which situation should the nurse document that the patient with AD exhibited agnosia? a. The patient attempts to comb her hair with a fork. b. The patient struggles to express herself verbally. c. The patient appears unable to understand written language. d. The patient cannot feed herself, despite having adequate motor function. ANS: A Agnosia is the inability to recognize an object and use it as intended. Expressive aphasia is difficulty in expressing oneself. Alexia is the inability to recognize the written language. Apraxia is the inability to do an activity despite having the motor function to accomplish it. PTS: 1 DIF: Cognitive Level: Application REF: 1095 OBJ: 3 (theory) TOP: Agnosia: Behavior KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Physiological Adaptation 9. The patient with Alzheimer’s disease (AD) has been on donepezil (Aricept) for several weeks. In which situation would the nurse suspect an overdose? a. The patient hungrily eats meals and often searches for snacks between meals. b. The nurse assesses a radial pulse rate of 92 beats/min. c. The patient’s blood pressure is elevated after periods of exertion. d. The patient fails to grasp a glass tightly enough to prevent dropping it. ANS: D Inability to grasp the glass indicates muscle weakness, a cardinal indicator of overdose of Aricept. Other overdose signs are hypotension, nausea and vomiting, and bradycardia. Appetite changes are not consistent with the use of this medication. PTS: 1 DIF: Cognitive Level: Analysis REF: 1095, Table 47-1 OBJ: 4 (theory) TOP: Donepezil (Aricept): Overdose KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 10. How should the nurse speak when communicating with a patient with moderate Alzheimer dementia? a. Slowly b. Clearly c. Loudly d. Softly ANS: B Clarity is essential when communicating with a patient with Alzheimer dementia. Placing self directly in front of the patient and using pictures or symbols is helpful. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1097, Nursing Care Plan 47-1, 1105 OBJ: 1 (clinical) TOP: Communication: Technique KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 11. The nurse is caring for a patient with acquired immune deficiency syndrome (AIDS) dementia complex (ADC). Which factor places this patient at particular risk for injury? a. Manic behavior b. Numbness and muscle weakness c. Suicidal ideation d. Difficulty concentrating ANS: B Peripheral neuropathy results in numbness and muscle weakness that may contribute to falls and thermal skin injuries. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1100 OBJ: 1 (theory) TOP: ADC: Characteristics KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Physiological Adaptation 12. The nurse is caring for a patient with moderate Alzheimer disease (AD) in a long-term care facility who “sundowns.” The nurse understands that which action would be most beneficial for this patient? a. Scheduling social interaction activities in the morning. b. Darkening the bedroom to encourage sleep. c. Administering sedatives to enhance sleep initiation. d. Scheduling an exercise program after supper. ANS: A Sundowning occurs when a patient is completely oriented during the day but becomes disoriented and confused during the evening and night hours. Planning interactive activities when the resident is not confused is beneficial. Exercise programs at night would add to agitation and confusion. Sedatives also frequently cause confusion. Lights should be left on to assist with reorientation should the resident wake up at night. PTS: 1 DIF: Cognitive Level: Application REF: 1101 OBJ: 3 (theory) TOP: Sundowning: Interventions KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 13. The nurse is caring for a patient with Alzheimer disease (AD) who wakes up moaning and frightened in the middle of the night. She begs that her husband’s coffin be removed from her room. How should the nurse respond? a. Turn light on and say, “There is no coffin here. This is the dresser.” b. Leave the light off and shine a flashlight on the dresser and say, “See! No coffin!” c. Turn the light on, assist patient to the bathroom, and say, “This is your dresser.” d. Leave the light off and say, “You are in your room.” ANS: C Turning the light on helps reorient the patient. Distraction of going to the bathroom and identifying the dresser assist with reorientation after a frightening illusion. The other options would lead to greater confusion. PTS: 1 DIF: Cognitive Level: Analysis REF: 1093 OBJ: 3 (theory) TOP: Illusions: Interventions KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 14. The CNA approaches the older adult in the long-term care facility and says, “Oh, look! Your pretty dress is icky with food spots! Let’s change your clothes, sweetie.” The nurse identifies that the CNA is using which type of communication? a. Instruction for personal hygiene b. Encouragement for self-care c. Simplistic “elderspeak” d. Reorientation techniques ANS: C Elderspeak is a way of communicating with older adults that is infantile, oversimplistic, oversolicitous, and demeaning. It serves no therapeutic purpose. PTS: 1 DIF: Cognitive Level: Application REF: 1105, Older Adult Care Points OBJ: 4 (theory) TOP: Communication: Elderspeak KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 15. The home health nurse is counseling a family who will be caring for a relative with moderate-stage Alzheimer disease (AD). Which information is most important to include? a. Construct a consistent routine to provide structured environment. b. Try to make each day different to enhance attention span. c. Use multiple caregivers to decrease unhealthy attachment and prevent caregiver burnout. d. Place bright scatter rugs, flower arrangements, and wall decorations around the room to stimulate sensory perception. ANS: A A consistent routine—eating, resting, medication, hygiene—are all beneficial to the demented patient. Different caregivers and distracting environmental objects increase confusion. PTS: 1 DIF: Cognitive Level: Application REF: 1105 OBJ: 3 (theory) TOP: Home Care: Preparations KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Reduction of Risk Potential 16. An exhausted daughter is the sole caregiver to a patient with moderate Alzheimer disease (AD). She asks the nurse what respite care entails. Which statement indicates that the caregiver understands the nurse’s response? a. “My mom would stay in a long-term care facility for a short time while I rest.” b. “Home health aides would come to our home and help me with housework.” c. “A registered nurse would provide total care for my mom in 3 day intervals.” d. “I would be connected with a special support group to share stresses and communicate with other caregivers.” ANS: A Respite care is placing the patient temporarily in a long-term care facility (usually for no longer than a month) to give the family respite from the responsibility of 24/7 care. PTS: 1 DIF: Cognitive Level: Application REF: 1106 OBJ: 7 (theory) TOP: Respite Care: Definition KEY: Nursing Process Step: Evaluation MSC: NCLEX: Psychosocial Integrity 17. Donepezil (Aricept) has been prescribed for a patient with Alzheimer disease (AD). Which statement indicates that the patient and spouse understand teaching about the medication? a. “It is best to take the medication at bedtime.” b. “The medication will interact with dark leafy greens.” c. “Taking the medication with a citrus beverage should improve absorption.” d. “The medication should be taken with meals.” ANS: D Donepezil (Aricept) is used in the management of AD. It has been shown to elevate acetylcholine levels in the brain and will slow the progression of the condition. The medication should be taken with meals to reduce gastrointestinal distress. PTS: 1 DIF: Cognitive Level: Application REF: 1095, Table 47-1 OBJ: 4 (theory) TOP: Drugs Used to Treat Cognitive Disorders KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 18. A recently licensed nurse is orienting to the Alzheimer disease (AD) care unit. The nurse is caring for a patient who is transitioning from oral rivastigmine (Exelon) to the medication patch. Which action indicates an accurate understanding of the medication? a. The nurse instructs the patient to apply the patch 12 hours after the last oral medication dosage. b. The nurse instructs the patient to replace the patch every 36 hours. c. The nurse explains that the sites of application will need to be rotated. d. The nurse instructs the patient to avoid placing the patch on the trunk region of the body. ANS: C Rivastigmine (Exelon) is used to manage AD by elevating acetylcholine. The medication is available orally and transdermally. The patch should be applied 24 hours after the last oral dosage is given. The sites for application of the drug patches should be rotated. PTS: 1 DIF: Cognitive Level: Application REF: 1095, Table 47-1 OBJ: 4 (theory) TOP: Drugs Used to Treat Cognitive Disorders KEY: Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity: Pharmacological and Parenteral Therapies 19. The nurse is caring for a patient who has dementia and has been getting up out of bed at night. What action by the nurse is most therapeutic? a. The nurse raises all of the side rails. b. The nurse reassigns the patient to a room closer to the nurse’s station. c. The nurse obtains orders from the physician to apply restraints at night. d. The nurse places the mattress on the floor. ANS: D The patient poses a significant risk for falls and needs provisions to increase safety. Placing the mattress on the floor decreases the risk of injury from falling from a larger height. Moving the patient closer to the nurse’s station does not offer protection or ensure that the patient will be seen or heard. The use of side rails can be considered a restraint and it can present an additional safety hazard. Restraints are to be the last option when caring for patients. PTS: 1 DIF: Cognitive Level: Application REF: 1104 OBJ: 1 (theory) TOP: Alternatives to Restraints KEY: Nursing Process Step: Implementation MSC: NCLEX: Safe, Effective Care Environment: Safety and Infection Control MULTIPLE RESPONSE 20. Postmortem brain examinations of Alzheimer disease (AD) patients reveal which type of finding(s)? (Select all that apply.) a. Tangled nerve cells b. Abnormal buildup of proteins c. Hemorrhagic areas d. Occluded cerebral vessels e. Reduced white matter ANS: A, B Tangled nerve cells and abnormal buildup of protein in the brain have been found on postmortem brain examinations of people who have AD. PTS: 1 DIF: Cognitive Level: Knowledge REF: 1094 OBJ: 3 (theory) TOP: AD: Cerebral Changes KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 21. Which criteria must be established to assign a diagnosis of dementia? (Select all that apply.) a. Evidence of cognitive deficits. b. Evidence of aphasia, apraxia, or agnosia. c. Impairment in social function. d. Impairments of occupational function. e. Neurologic signs and symptoms, such as ataxic gait. ANS: A, B, C, D, E Dementia is characterized by several cognitive deficits, memory in particular, and tends to be chronic in nature. It is classified according to etiology (cause or origin of disease). All options are criteria for the diagnosis of dementia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1101 OBJ: 3 (theory) TOP: Diagnostic Criteria: Dementia KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance 22. What does the Mini-Mental Status Exam (MMSE) assess? (select all that apply) a. Orientation b. Judgment c. Memory d. Insight e. Ability to follow directions ANS: A, C, E The Mini-Mental Status Exam (MMSE) is a popular shortened version of the mental status examination that was developed by Folstein and colleagues in 1975. It can be used for patients who have cognitive disorders or thought disorders to assess orientation, memory, and ability to follow commands. It consists of 11 easily scored items and should take about 5 to 10 minutes to administer. The MMSE does not measure insight or judgment. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1100-1101 OBJ: 4 (theory) TOP: MMSE: Purpose KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity 23. Which strategy/strategies best benefit(s) a late-stage Alzheimer patient with global amnesia? (Select all that apply.) a. Reorientation sessions b. Music therapy c. Reminiscence therapy d. Pet therapy e. Looking at family scrapbooks ANS: B, D Global amnesia wipes out all memory. Orientation and family pictures will not be helpful. Activities that stimulate the senses, such as music, stroking an animal, or aroma therapy, can be pleasing. PTS: 1 DIF: Cognitive Level: Application REF: 1103, Box 47-3 OBJ: 3 (theory) TOP: Global Amnesia: Interventions KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 24. The home health nurse assesses caregivers for a person with a cognitive deficit. Which finding(s) is/are characteristic of exhaustion? (Select all that apply.) a. Irritability with other family members and the patient b. Report of sleep disturbances c. Anger at patient and self d. Depression e. Fatigue ANS: A, B, C, D, E All options are characteristics of exhaustion in caregivers to the cognitively impaired. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1106 OBJ: 7 (theory) TOP: Caregiver Fatigue: Signs and Symptoms KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity 25. The nurse is caring for a patient with memory deficits. The patient asks the nurse about foods that may help improve memory. Which food(s) is/are linked to enhanced memory? (Select all that apply.) a. Salmon b. Red meat c. Pork loin d. Leafy green vegetables e. Fruit ANS: A, D, E Studies show that fish and omega-3 polyunsaturated fats, fruits and vegetables, curcumin (curry spice), and the traditional Mediterranean diet may lower the risk for loss of cognitive function and/or Alzheimer disease (AD). PTS: 1 DIF: Cognitive Level: Comprehension REF: 1094, Health Promotion OBJ: 1 (clinical) TOP: Health Promotion: Diet and Memory KEY: Nursing Process Step: Implementation MSC: NCLEX: Health Promotion and Maintenance MATCHING The nurse clarifies terminology related to cognitive disorders. Match the options to the expected characteristics. (Options may be used more than once.) a. Cognition b. Dementia c. Delirium 26. An acute alteration in cognition 27. Characterized by slow onset 28. Experiences an illusion 29. Uses confabulation to cover memory gaps 30. Results from cerebrovascular accident 31. Processes of perception, memory, and judgment 26. ANS: C PTS: 1 DIF: Cognitive Level: Knowledge REF: 1092 OBJ: 1 (theory) TOP: Terms: Characteristics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 27. ANS: B PTS: 1 DIF: Cognitive Level: Knowledge REF: 1092 OBJ: 1 (theory) TOP: Terms: Characteristics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 28. ANS: C PTS: 1 DIF: Cognitive Level: Knowledge REF: 1092 OBJ: 1 (theory) TOP: Terms: Characteristics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 29. ANS: B PTS: 1 DIF: Cognitive Level: Knowledge REF: 1092 OBJ: 1 (theory) TOP: Terms: Characteristics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 30. ANS: C PTS: 1 DIF: Cognitive Level: Knowledge REF: 1092 OBJ: 1 (theory) TOP: Terms: Characteristics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A 31. ANS: A PTS: 1 DIF: Cognitive Level: Knowledge REF: 1101 OBJ: 1 (theory) TOP: Terms: Characteristics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A Chapter 48: Care of Patients with Thought and Personality Disorders deWit: Medical-Surgical Nursing: Concepts & Practice, 3rd Edition MULTIPLE CHOICE 1. Approximately what percentage of the U.S. population is affected with schizophrenia? a. 1% b. 2% c. 3% d. 4% ANS: A Schizophrenia is the most common thought disorder. It is estimated that 1.1% of the general population is affected with schizophrenia, and in the United States this represents 2.4 million Americans. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1109 OBJ: 1 (theory) TOP: Schizophrenia: Incidence KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 2. The nurse explains that depression is thought to be the result of a deficit of which neurotransmitter? a. Norepinephrine b. Serotonin c. Acetylcholine d. Dopamine ANS: B Serotonin is a neurotransmitter of the central nervous system. It is important in sleep, pain perception, and emotional states. Lack of serotonin can lead to depression. Norepinephrine and acetylcholine are neurotransmitters of the autonomic nervous system. Norepinephrine plays an important role in the fight-or-flight reaction (constriction of the blood vessels, dilation of the pupils, increased heart rate, increased awareness, and vigilance). Acetylcholine causes decreased heart rate and force of contraction and plays a role in the sleep-wake cycle. Dopamine is located mostly in the brainstem. It is thought to play a role in controlling complex movements, motivation, and cognition. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1110 OBJ: 3 (theory) TOP: Depression: Etiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Physiological Adaptation 3. Which statement causes the nurse to document a schizophrenic patient’s delusion of persecution? a. “Did you know that I own this hospital and pay all these people to work for me?” b. “My doctor talked to all the other patients, but not to me. He doesn’t want me to get well.” c. “The president’s speech tonight is going to give me a coded message.” d. “I am going to wait in front of the hospital this morning for my limousine to pick me up and take me to my private jet.” ANS: B Delusions can be either grandiose or persecutory. An individual who believes he owns the hospital or is planning to be picked up by a limousine or has a private jet is having delusions of grandeur. Individuals with delusions of persecution believe that they are being persecuted by agencies, by other people, or by supernatural beings. The patient who believes the president’s speech is coded is having an idea of reference. PTS: 1 DIF: Cognitive Level: Application REF: 1110 OBJ: 3 (theory) TOP: Delusions: Persecution KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity 4. The paranoid schizophrenic patient states that his whole family has conspired to have him put in the hospital and that the medical staff are part of the conspiracy. Which is the nurse’s most therapeutic response? a. “I promise that I want to help you.” b. “You know your family is concerned about you.” c. “I’m sorry you feel that way. I’ll be around if you want to talk about your feelings.” d. “The doctors are trying to help you feel better. They have your best interest in mind.” ANS: C Arguing with the paranoid patient, or defending self or others, reinforces the paranoia. Passively offering self to the patient to approach you rather than the other way around is helpful to the nurse–patient relationship. PTS: 1 DIF: Cognitive Level: Application REF: 1117, Nursing Care Plan 48-1 OBJ: 3 (theory) TOP: Paranoia: Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 5. The delusional patient has become agitated and angry. The patient reports that the cook put tacks in his cereal. He is pacing back and forth in the crowded dining room and cursing the cook. How should the nurse respond? a. Keep distance from the patient and ask, “Can we go to the dayroom and talk?” b. Touch the patient’s arm and say, “Calm down. I’m sure we can straighten this out.” c. Call experienced CNAs to restrain the patient. d. Stand calmly and say, “This behavior is unacceptable. Sit down and eat, Carl.” ANS: A Allowing the angry patient space is important. Encourage the patient to find a quieter place. Acknowledge the anger and demonstrate willingness to help. The agitated patient should not be touched without permission. Restraints are a last resort and will increase the patient’s anger and feelings of persecution. PTS: 1 DIF: Cognitive Level: Application REF: 1120, Box 48-2 OBJ: 2 (clinical) TOP: Agitation and Anger: Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 6. The manipulative patient approaches the nurse and says, “I know it’s too early to give me my pain medication, but you are the only one who seems to care. Could you give me my pain medication now?” Which response is best? a. “The charge nurse is very stringent about scheduled medications. She would be very angry with me if I gave you the medication now.” b. “I know how it is when you are in pain. I’ll give you your medication early.” c. “Your medication is due in 2 hours. I will be glad to give it to you on schedule.” d. “It makes me feel good to know you are appreciative of our care. Here is your medication.” ANS: C Setting clear limits is important when managing manipulative patients. Once limits are set, it is important to maintain them. Blaming the charge nurse provides incentive for further manipulative behaviors. The nurse telling the patient that they know what it is like when they are in pain is not accurate or therapeutic. Providing the medication early likely does not follow the prescribed plan. PTS: 1 DIF: Cognitive Level: Application REF: 1120, Box 48-2 OBJ: 3 (clinical) TOP: Manipulation: Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 7. The nurse observes a withdrawn schizophrenic. The patient is sitting alone and moving her lips as if she is talking, but there is no audible sound. The nurse speaks to the patient by name, but the patient does not seem to hear. What should the nurse do first? a. Hug the patient’s shoulders, refer to the patient by name, and ask if she’s praying. b. Document the patient’s nonresponsiveness and continued detached behavior. c. Sit down in the chair next to the patient, touch her arm, and speak softly. d. Touch the patient’s shoulder and then join another group of patients. ANS: C Sitting with the patient and touching her presents the reality of the nurse’s presence. Continued attention will make the patient feel safe. Feelings of safety are needed in the beginning of the nurse–patient relationship. Hugging the patient may invade the patient’s personal space. The nurse’s assessment will be documented but it is most appropriate to attempt an interaction with the patient. PTS: 1 DIF: Cognitive Level: Application REF: 1111 OBJ: 2 (theory) TOP: Withdrawal: Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 8. After signing a contract that he will no longer smoke in his room, the patient violates the contract. The contract consequences include confiscation of smoking materials and mandatory supervision for future smoke breaks. How should the nurse appropriately address the patient’s behavior? a. “Why are you smoking in your room when you know it is not allowed?” b. “The contract states that if you smoke in your room, you must give me your smoking materials. Let me have them, please.” c. “Okay, Larry, give me your cigarettes and lighter now.” d. “I am going to give you one more chance, Larry. Let’s see if you can live up to the contract.” ANS: B Reminding the patient of contract violation and the penalty attached should be done before taking the cigarettes. This approach is fair and puts the blame for the consequence on the offender. Providing the patient with the opportunity to “explain” the actions does not conform to the agreed-on contract. Providing additional opportunities for compliance does not support the contract and may encourage manipulative behavior. PTS: 1 DIF: Cognitive Level: Application REF: 1120, Box 48-2 OBJ: 2 (theory) TOP: Manipulation: Intervention KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 9. When receiving report, the nurse learns that a schizophrenic patient has been displaying waxy flexibility. Which behavior is consistent with this report? a. The patient sits and stares at the wall without speaking. b. The patient arranges himself in several seated postures on the couch. c. The patient marches stiffly up and down the center of the dayroom. d. The patient holds his arm over his head with his fist clenched for an hour. ANS: D Waxy flexibility refers to maintaining a limb in one position for a long time. The catatonic patient will exhibit a stuporous demeanor. It is associated with rigidity and unusual posturing. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1112, Table 48-1 OBJ: 2 (theory) TOP: Catatonia: Waxy Flexibility KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity: Coping and Adaptation 10. The nurse is caring for a schizophrenic patient who has been prescribed large doses of thioridazine (Mellaril). Which manifestation may signal an overdose of the medication? a. The patient walks with a shuffling gait and drooling. b. The patient is lethargic and takes frequent naps. c. The patient exhibits disorganized thought processes. d. The patient exhibits extreme excitability with periods of mania. ANS: A Extrapyramidal side effects of pseudo-parkinsonism with a shuffling gait, tremors, and excessive salivation are cardinal signs of overdose of neuroleptics. PTS: 1 DIF: Cognitive Level: Application REF: 1112, 1113, Figure 48-3 OBJ: 2 (theory) TOP: Extrapyramidal Side Effects: Pseudo-Parkinsonism KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 11. The nurse adds an intervention to the nursing care plan for a patient on neuroleptics. Which intervention is most appropriate? a. Increase fluid intake to compensate for the side effect of diarrhea. b. Encourage snacks to prevent weight loss. c. Monitor vital signs for hypertension. d. Assess urinary output for evidence of urinary retention. ANS: D Neuroleptics cause urinary retention, weight gain, constipation, and hypotension. Diarrhea is not associated with the administration of neuroleptics. Weight gain, and not weight loss, is associated with this type of medication. Hypertension is not associated with this type of medication. PTS: 1 DIF: Cognitive Level: Analysis REF: 1112 OBJ: 2 (theory) TOP: Neuroleptic Drugs: Side Effects KEY: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 12. The nurse has asked a catatonic patient, “Where is your hat?” Which response should cause the nurse to document episodes of echolalia? a. The patient excitedly says, “Hat, cat, rat, fat, scat, splat!” b. The patient tearfully says, “I had a hat when my mother drove her yellow car.” c. The patient repeatedly says, “Your hat, your hat, your hat.” d. The patient places his hands on his head and says, “Where is your hat?” ANS: D Echolalia is the repetition of words spoken to the patient by another person. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1112, Table 48-1 OBJ: 2 (theory) TOP: Catatonia: Echolalia KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity 13. A student nurse questions the nurse about the frequency of administration of antipsychotics, such as risperidone (Risperdal). Which advantage is true of newer antipsychotics like risperidone (Risperdal)? a. Decreased photosensitivity b. Fewer serious side effects c. Less expensive d. Decreased incidence of headaches ANS: B Risperidone (Risperdal) is a newer generation of “atypical” antipsychotic medications that is known for having fewer serious side effects, such as tardive dyskinesia, but they still have significant effects. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1113 OBJ: 2 (theory) TOP: Atypical Antipsychotics KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 14. The nurse is aware that interventions for the negative symptoms of schizophrenia are based on which factor? a. Establishment of trust b. Acceptance of medication protocols c. Support in interpersonal social activities d. Promotion of conversation with the patient ANS: A General nursing interventions for the negative symptoms include establishing trust and teaching the patient and family how to manage the signs and symptoms. An attitude of acceptance is necessary to promote trust. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1116 OBJ: 2 (theory) TOP: Negative Symptoms: Establish Trust KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 15. During report, the nurse is told that a patient has Cluster B group type of personality disorder. Which type of behavior can the nurse anticipate? a. Paranoia b. Avoidance c. Antisocial behavior d. Obsessive-compulsive behavior ANS: C The antisocial personality disorder is included in Cluster B: dramatic and erratic. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1120, 1121, Box 48-3 OBJ: 4 (theory) TOP: Cluster B: Dramatic and Erratic KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 16. The nurse is aware the patient with borderline personality disorder did not have a family visit this week and adds an intervention to address the patient’s probable perception of abandonment. Which intervention is most appropriate? a. Schedule the patient for pet therapy visit. b. Arrange for remote activity during next visiting time. c. Assess daily for evidence of self-mutilation. d. Assign a young CNA to his care. ANS: C Patients with borderline personality disorder have a deep fear of abandonment and react with intense, emotionally charge acts, such as suicide attempts or self-mutilation. PTS: 1 DIF: Cognitive Level: Application REF: 1121 OBJ: 4 (theory) TOP: Borderline Personality Disorder: Self-Mutilation KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 17. What effect does the nurse desire to achieve by using clear, direct communication with patients with borderline personality disorder? a. Avoid generating an intense reaction from the patient. b. Eliminate the possibility of manipulation. c. Decrease the probability of the patient reacting emotionally. d. Provide a role model for good communication. ANS: D Clear communication can model a communication style that allows a person to verbalize feelings and make thoughts and expectations known. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1116 OBJ: 4 (theory) TOP: Communication: Setting a Model KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Basic Care and Comfort 18. The nurse is changing the dressing on self-inflicted cigarette burns on a patient with borderline personality disorder. When providing the care, which action is most therapeutic? a. Change the dressings while being nurturing and caring to keep patient from feeling abandoned. b. Approach the dressing change with a matter-of-fact demeanor to decrease secondary gains of sympathy. c. Present a stern attitude to underscore the seriousness of the act. d. Interact in a professional and distant manner to diminish the opportunity for manipulation. ANS: B The person with borderline personality disorder will seek additional secondary gains in terms of attention about the manipulative act of self-mutilation. Nurturing will reinforce the effectiveness of the mutilation to gain attention. Stern and distant demeanors may appear confrontational to the patient and reduce the therapeutic aspects of the intervention. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1121 OBJ: 4 (theory) TOP: Borderline Personality Disorder: Use of Attitude KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 19. The nurse is talking with a patient who voices concerns about the incidence of schizophrenia in her family. The patient states that she is worried the condition will be inherited by her teenage daughter. What response by the nurse is most appropriate? a. “Unfortunately, schizophrenia does run in families.” b. “Although some familial factors exist, there is no exact known cause for schizophrenia.” c. “Your daughter would show some evidence of the condition by this point in her life, so there is no real reason to worry.” d. “As long as your home environment is warm and loving, she will be fine.” ANS: B The exact cause of schizophrenia is unknown; however, current research favors the theory that there is a neurologic basis with a genetic component. As with most chronic conditions, an unfavorable social environment contributes to a poor prognosis. Schizophrenia usually develops in late adolescence or the early twenties. PTS: 1 DIF: Cognitive Level: Application REF: 1109-1110 OBJ: 2 (theory) TOP: Schizophrenia: Etiology and Pathophysiology KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 20. The family of a patient being treated for a recent diagnosis of schizophrenia voices concerns to the nurse. They report the patient just told them that the pepper flakes on his potatoes were crawling bugs. What response by the nurse is most appropriate? a. “At this stage it is most important to humor him and agree that you see them as well.” b. “To reduce his stress, just throw out the food.” c. “It is important to tell him that you do not see the bugs.” d. “The best thing to do in this case is to confront him and let him know that he is mistaken.” ANS: C The patient is experiencing an illusion. It is most important to offer support but to attempt to provide reality orientation. Confronting him may cause anger or increased anxiety and should be avoided. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1110 OBJ: 2 (theory) TOP: Schizophrenia: Signs and Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 21. The nurse is caring for a patient with a recent diagnosis of schizophrenia. His wife asks how long it will be until her husband is cured. What response by the nurse is most appropriate? a. “Unfortunately, there is no cure, but the condition can be managed.” b. “It will take approximately 1 to 2 months of medication therapy to alleviate your husband’s symptoms.” c. “We cannot consider your husband cured until he has been symptom free for at least 1 year.” d. “There is no way to predict his outcome during his initial episode.” ANS: A Schizophrenia can be managed with therapy and medications. It cannot be permanently cured. Evidence suggests that early treatment for schizophrenia improves long-term prognosis. Patients who are treated for first episodes generally respond to the therapeutic effects and require lower doses of antipsychotic medications. After starting a medication, the patient should be monitored for 2 to 4 weeks for therapeutic response. PTS: 1 DIF: Cognitive Level: Application REF: 1112 OBJ: 2 (theory) TOP: Schizophrenia: Treatment KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity: Mental Health Concepts MULTIPLE RESPONSE 22. Which psychotic feature(s) is/are characteristic of schizophrenia? (Select all that apply.) a. Hallucinations b. Sexual dysfunction c. Delusions d. Disorganized speech e. Disorganized behavior ANS: A, C, D, E Sexual dysfunction is not a characteristic of schizophrenia. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1111 OBJ: 2 (theory) TOP: Schizophrenia: Characteristics KEY: Nursing Process Step: PlanningMSC: NCLEX: Health Promotion and Maintenance 23. Which characteristic(s) is/are an example of a negative symptom of schizophrenia? (Select all that apply.) a. Avolition b. Hallucination c. Psychomotor retardation d. Delusions e. Anhedonia ANS: A, C, E Negative symptoms are abilities or personal characteristics that are absent or lost to the patient. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1111 OBJ: 2 (theory) TOP: Schizophrenia: Negative Symptoms KEY: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 24. The nurse explains that neuroleptic drugs such as chlorpromazine (Thorazine) are very effective in treating specific symptoms of schizophrenia. Which effect(s) should chlorpromazine have? (Select all that apply.) a. Eliminating hallucinations b. Stimulating effective interpersonal relationships c. Enabling organized thought d. Increasing activity level e. Eliminating delusional systems ANS: A, C, E Hallucinations, disorganized thought, and delusional systems are the positive symptoms that respond to neuroleptics. Negative symptoms such as withdrawal and inactivity do not respond well to these drugs. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1112 OBJ: 2 (theory) TOP: Neuroleptic Drugs: Advantages KEY: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity: Pharmacological Therapies 25. Which characteristic(s) of personality disorders should the nurse consider? (Select all that apply.) a. Impaired cognition b. Maladaptive response to life’s events c. Inability to maintain relationships d. Poor impulse control e. Inappropriate emotional responses ANS: B, C, D, E There is no impaired cognition in the individual with a personality disorder. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1120 OBJ: 4 (theory) TOP: Personality Disorders: Characteristics KEY: Nursing Process Step: PlanningMSC: NCLEX: Psychosocial Integrity 26. Milieu therapy is a therapeutic application for people with personality disorders. What principle(s) underscore(s) the basis of this method? (Select all that apply.) a. Maintaining a structured environment b. Participating as a member of the structured environment c. Practicing appropriate social behavior d. Actively attempting to modify behavior e. Learning to modify feelings and emotional responses ANS: A, B, C, D, E Milieu therapy provides all these options for treating people with personality disorders. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1121 OBJ: 5 (theory) TOP: Milieu Therapy: Characteristics KEY: Nursing Process Step: N/A MSC: NCLEX: N/A COMPLETION 27. The delusional patient rushes up to the nurse and begins to brush her uniform with his hands, saying, “I must get the weegos off of you!” The nurse recognizes that the word “weegos” is a(n) ________. ANS: neologism A neologism is a word that the patient makes up to express his or her disorganized thinking. PTS: 1 DIF: Cognitive Level: Comprehension REF: 1116 OBJ: 2 (theory) TOP: Schizophrenia: Use of Neologisms KEY: Nursing Process Step: Assessment MSC: NCLEX: Psychosocial Integrity 28. The paranoid schizophrenic who is taking a neuroleptic is brought to the emergency department with acute muscle spasm of the face and neck with eyes that are fixed in an upward stare. The nurse recognizes the condition of ________. ANS: dystonia Overdoses of neuroleptics can cause muscle spasms of the face and neck called dystonia. PTS: 1 DIF: Cognitive Level: Application REF: 1112 OBJ: 2 (theory) TOP: Neuroleptic Drugs: Dystonia KEY: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity: Pharmacological Therapies [Show More]
Last updated: 8 months ago
Preview 1 out of 367 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 16, 2023
Number of pages
367
Written in
Additional information
This document has been written for:
Uploaded
Oct 16, 2023
Downloads
0
Views
62

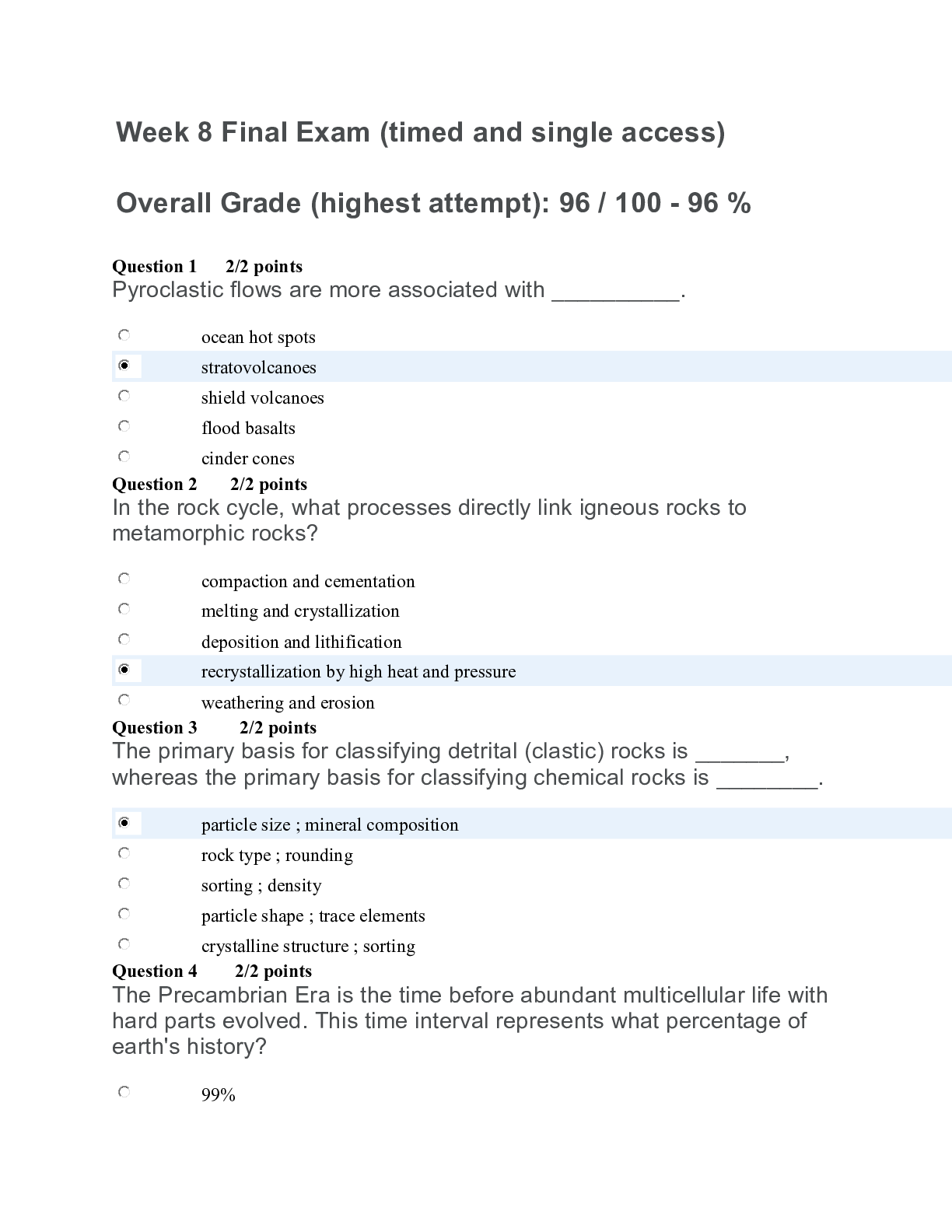
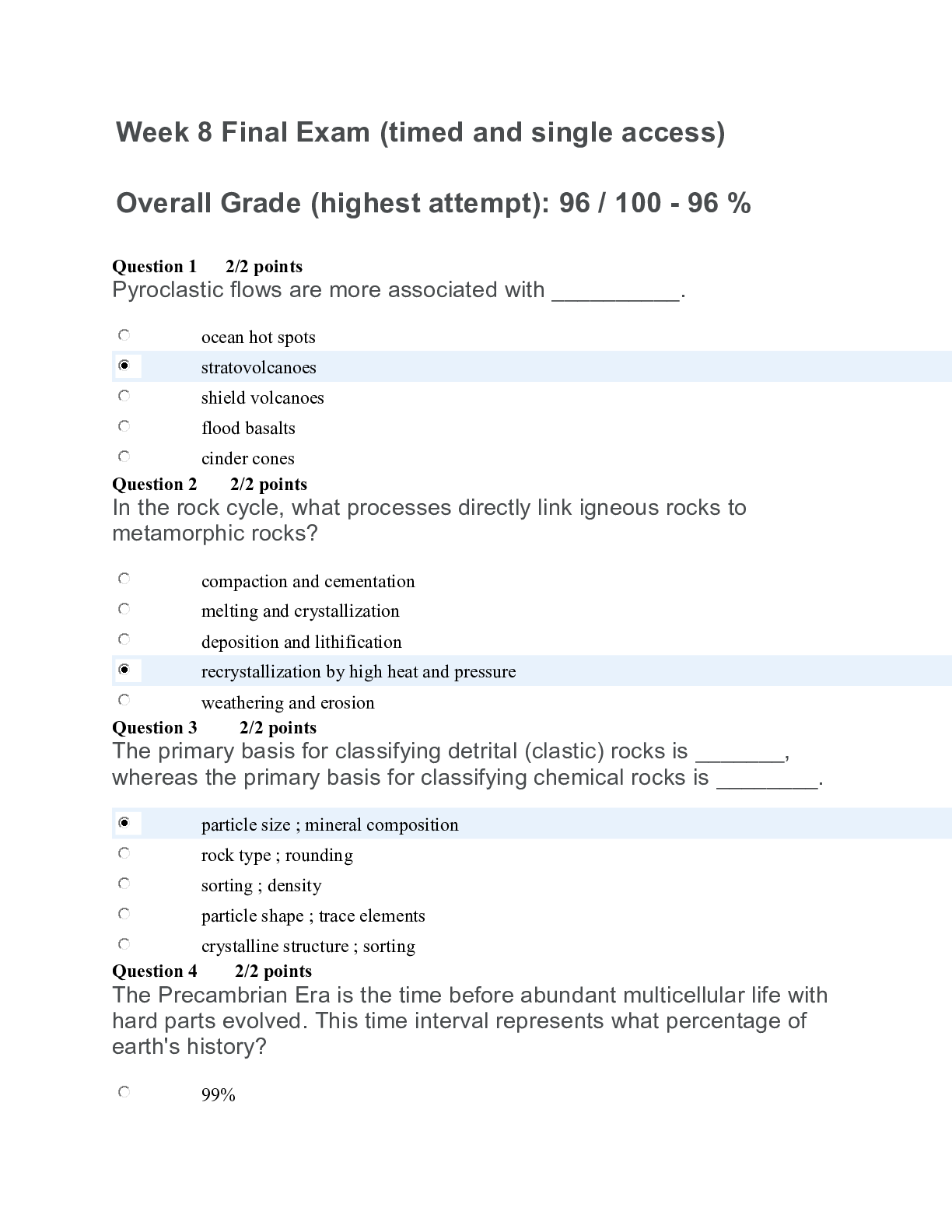
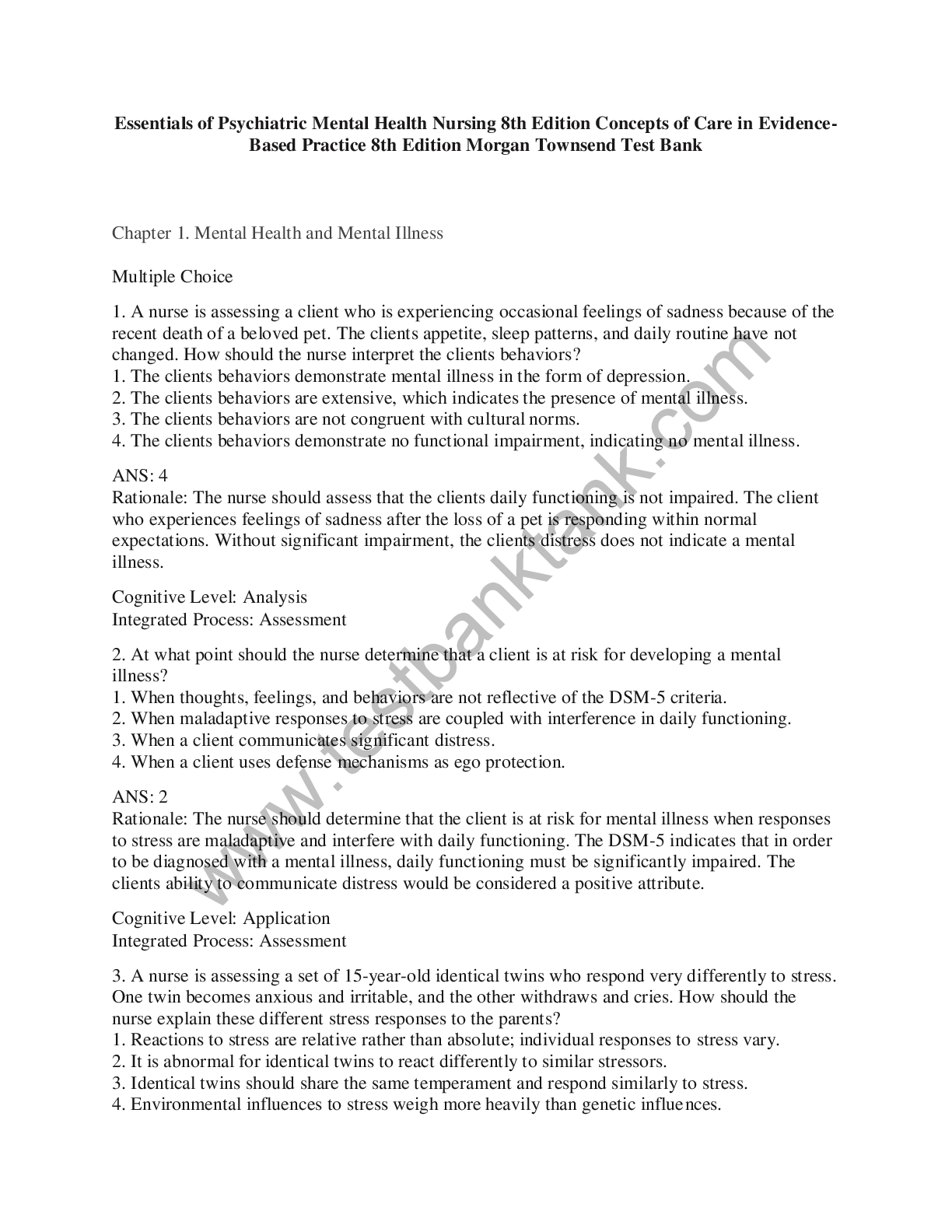
, (A Grade), Questions and Answers, All Correct Study Guide, Download to Score A.png)