CNRN Practice Samples Exam 235 Questions with Verified Answers,100% CORRECT
Document Content and Description Below
CNRN Practice Samples Exam 235 Questions with Verified Answers Which of the following tumor types will have a higher incidence in pediatric populations and have a decreased incidence with age? A. ... Glioblastoma B. Pilocytic astrocytoma C. Central nervous system lymphoma D. Metastatic brain tumor - CORRECT ANSWER B Rationale: Both pilocytic astrocytoma and medulloblastoma brain tumors are more commonly found in the younger population. The incidence of these tumors will decrease with age. Glioblastomas are more frequently found in young adults. CNS lymphoma and metastasis will have an increased incidence with age. A patient presents with progressive neurological deficits and has a recent history of transient neurological attack. This patient is most likely experiencing which of the following types of stroke? A. Thrombotic stroke B. Embolic stroke C. Subarachnoid hemorrhage D. Vasospasms - CORRECT ANSWER A Rationale: Thrombotic strokes frequently present as a worsening neurological status over a short period of time. Patients may have experienced episodes of transient ischemic attacks (TIAs) before the onset of the ischemic strokes. Embolic strokes tend to have a more sudden onset without progression in symptoms. Subarachnoid hemorrhages (SAHs) are a sudden onset of headache without the history of transient neurological deficits. Vasospasms are associated with SAH, and symptoms occur most commonly between 7 and 10 days after the SAH. Which of the following best describes a coup injury? A. Injury occurs at the point of impact. B. Injury occurs on the contralateral side of impact. C. It is an acceleration injury. D. It is a deceleration injury. - CORRECT ANSWER A Rationale: A coup injury occurs at the point of impact, and a contracoup injury occurs on the contralateral side. The mechanism of injury for acceleration injuries is commonly defined as a moving object hitting a stationary head, whereas a deceleration injury involves a moving head hitting a stationary object. A patient is admitted to the ICU with persistent epileptic seizures lasting beyond 90 minutes. Which of the following best describes the seizure activity? A. Epileptic seizure B. Epilepsy C. Refractory seizure D. Nonepileptic seizure - CORRECT ANSWER C Rationale: An epileptic seizure, which persists for greater than 90 minutes despite administration of anticonvulsants is called a refractory seizure. An epileptic seizure indicates the presence of EEG wave changes during the seizure activity. Epilepsy refers to repetitive seizures without a reversible cause such as hyponatremia. Nonepileptic seizure is the presence of seizure activity without the EEG changes. Which of the following would be the best technique to use to assess for cerebrospinal fluid in bloody drainage from the nose following a traumatic brain injury? A. Glucose test B. Halo test C. Send to lab for hemoglobin level D. Litmus test - CORRECT ANSWER B Rationale: Halo test (a positive result produces a yellow ring) is more accurate than a glucose test, especially with the presence of bloody drainage. A glucose test has been used to distinguish between sinus drainage and cerebrospinal fluid (CSF) because CSF has glucose but sinus drainage does not. But in this scenario, the drainage was "bloody," and blood has glucose. Bloody drainage may give a false positive with a glucose test. Testing for hemoglobin in the drainage does not determine the presence of CSF. Litmus test is used to test a pH of a fluid and is not used to distinguish CSF from nasal drainage. Which of the following is the most common cause of an embolic stroke? A. Atrial septal defect B. Atrial fibrillation C. Calcified lesion D. Angioplasty - CORRECT ANSWER B Rationale: Atrial fibrillation (AF) is the most common cause of an embolic stroke. Atrial septic defect (ASD) and calcified lesions can also result in embolic strokes but are significantly less common than AF. A complication of angioplasty can be distal embolization but again is not the most common cause of an embolic stroke. Cranial nerve (CN) VII (facial nerve) is commonly involved with Bell's palsy. Where does this CN originate? A. Pons B. Medulla C. Midbrain D. Basal ganglia - CORRECT ANSWER A Rationale: Cranial nerve (CN) V (trigeminal nerve), VI (abducens nerve), VII (facial nerve), and VIII (acoustic nerve) originate from the pons. CNs IX (hypoglossal nerve), X (vagus), XI (spinal accessory nerve), and XII (hypoglossal nerve) originate from medulla. CNs III (oculomotor nerve) and IV (glossopharyngeal nerve) originate from the midbrain. No cranial nerves originate from the basal ganglia. Which of the following electrolyte abnormalities is LESS likely to result in a seizure? A. Hyponatremia B. Hyperkalemia C. Hypocalcemia D. Hypomagnesemia - CORRECT ANSWER B Rationale: Hyponatremia is one of the most common electrolyte abnormalities that can cause a seizure. Hypocalcemia and hypomagnesemia can also cause seizures. Potassium is more likely to affect the myocardial electrical system, resulting in arrhythmias. A patient in the ICU following a severe traumatic brain injury suddenly demonstrates profuse sweating, sustained tachycardia, hypertension, and fever. Which of the following is the most likely cause? A. Neurogenic fever B. Diencephalic seizure C. Paroxysmal sympathetic hyperactivity D. Cerebral salt wasting syndrome - CORRECT ANSWER C Rationale: Traumatic brain injury (TBI) patients can experience "sympathetic storms" called paroxysmal sympathetic hyperactivity. The symptoms include fever, tachycardia, hypertension, profuse sweating, agitation, and increase respiratory rate. The "storm" is thought to be due to intermittent stimulation of the sympathoexcitatory centers located in upper brainstem and diencephalon. Diencephalic seizure is an incorrect term for the symptoms because the EEG is negative. Neurogenic fevers can occur following TBI but is not associated with the other symptoms of hypertension and tachycardia. Cerebral salt wasting syndrome (CSWS) is the loss of sodium through the kidneys and results in hypovolemic hyponatremia. In severe cases of cerebral palsy, there may be a delay in growth and development. Which of the following conditions can occur in these cases? A. Coagulopathy B. Immunocompromise C. Failure to thrive D. Locked-in syndrome - CORRECT ANSWER C Rationale: Failure to thrive is a complication of moderate to severe cerebral palsy (CP). It can result in malnutrition and death. CP is not associated with immunocompromise or coagulopathies. CP involves abnormal motor movements associated with spasticity or flaccidity, but does not develop locked-in syndrome. Which of the following best describes the penumbra in an ischemic stroke? A. Irreversibly damaged tissue B. Normal healthy tissue C. Presence of vasogenic cerebral edema D. Reversible ischemic tissue - CORRECT ANSWER D Rationale: The penumbra is the area surrounding an infarction that is ischemic or reversible ischemic tissue. Irreversibly damaged tissue is the area of tissue infarction and is the core of the infarction. Vasogenic cerebral edema is an increase in interstitial edema or fluid and is typically found surrounding the penumbra. Normal, healthy tissue is the area of brain tissue not affected by the ischemia or injury. A patient is admitted to the trauma ICU following a traumatic brain injury due to vehicle rollover. The patient is hypotensive and tachycardic. Which of the following is the most accurate statement? A. Hypotension following traumatic brain injury (TBI) indicates presence of epidural hematoma. B. Hypotension is sign of blood loss but is not considered a sign of TBI. C. Scalp lacerations can be easily controlled with direct compression. D. Neurogenic shock following TBI results in hypotension. - CORRECT ANSWER B Rationale: Traumatic brain injury (TBI) patients can experience additional systemic injuries. Hypotension indicates hypovolemia from blood loss in trauma patients, but cerebral injury, even epidural hematoma, cannot account for the volume of blood loss. Scalp lacerations bleed profusely and may require sutures or staples to stop the bleeding. Neurogenic shock is associated with spinal cord injuries. Symptoms include hypotension and bradycardia (not tachycardia). Which of the following has been found to be the most effective in preventing embolic strokes due to atrial fibrillation? A. Aspirin B. Low-molecular-weight heparin C. Warfarin (Coumadin) D. Clopidogrel (Plavix) - CORRECT ANSWER C Rationale: Studies have shown warfarin is the best at preventing an embolic stroke but is associated with a greater risk of bleeding. Aspirin is also used in primary prevention of embolic strokes but has less efficacy in preventing embolic strokes. Aspirin has a lower risk of bleeding than anticoagulation therapy. Low-molecular-weight heparin (LMWH) and Plavix are not currently recommended in preventing embolic strokes. Which of the following scales are used to determine the overall prognosis in patients with a brain tumor? A. PedsQL B. Functional Independence Measure C. CHADS2 score D. Karnofsky Performance Status Scale - CORRECT ANSWER D Rationale: Karnofsky Performance Status Scale (KPS) is used to determine overall prognosis in patients with a brain tumor. It is used along with histopathology of the tumor, completeness of resection, presence of necrosis, and tumor size and location. CHADS2 score is used to determine the stroke risk of atrial fibrillation. Functional Independence Measure (FIM) is used to evaluate stroke patients in rehabilitation. PedsQL is a tool used to assess quality of life in pediatric patients with brain tumors but is not used for overall prognosis. Which of the following best describes a radiculopathy? A. Compression of the cord with central stenosis B. Inflammation of bone and cartilage of joint C. Compression of nerve roots with foraminal stenosis D. Symptomatic degenerative changes of osteoarthritis - CORRECT ANSWER C Rationale: Radiculopathy is compression of nerve roots due to the narrowing of foraminal processes. Osteoarthritis is the inflammation of bone and cartilage of the spinal joints. Myelopathy is compression of the spinal cord due to central stenosis. Spondylosis is the symptomatic degenerative change that occurs in osteoarthritis. Your patient presents with left upper extremity weakness and facial droop. Which of the following vessels is most likely involved in this stroke? A. Anterior cerebral artery B. Middle cerebral artery C. Posterior cerebral artery D. Basilar artery - CORRECT ANSWER B Rationale: The middle cerebral artery (MCA) supplies blood to the lateral portion of the cerebral cortex, which is where the motor strip for the upper extremities and face is located. The anterior cerebral artery (ACA) supplies blood to the medial portion of the cerebral cortex, which is where the motor strip for the lower extremities is located (results in lower-extremity weakness). The posterior cerebral artery (PCA) supplies blood to the occipital lobe, which results in visual deficits. The basilar artery is in the posterior circulation (brainstem) and may present with quadriplegia or "locked-in" syndrome. Your patient has sustained a traumatic brain injury and a basilar skull fracture. The physician has ordered a nasogastric tube (NG) be placed. Which of the following is your best response? A. Place the NG according to the physician's order. B. Discuss with the physician the need to place an enteral feeding tube. C. Insert the gastric tube orally. D. Ask the physician to place the NG. - CORRECT ANSWER C Rationale: Never place a gastric tube nasally in a patient with a basilar skull fracture. The nasogastric (NG) tube may go through the cribriform fracture and enter the brain. A gastric tube can be placed orally, just not nasally. An enteral feeding tube may not be indicated at this time. Having the physician place the NG tube is not appropriate because the tube should not be placed nasally. During a stroke assessment, the patient has been found to have a deviated gaze. Which of the following would be the most correct statement regarding the gaze? A. Dysconjugate gaze B. Upward gaze C. Gaze toward the affected side D. Gaze away from affected side - CORRECT ANSWER C Rationale: The gaze abnormality in a middle cerebral artery (MCA) stroke is deviated toward the affected side. Seizures result in gaze away from the affected side. A dysconjugate or upward gaze is frequently associated with cranial nerve abnormalities but not commonly associated with strokes. What type of seizure is an aura classified as? A. Simple partial B. Complex partial C. Generalized D. Nonconvulsive - CORRECT ANSWER A Rationale: An aura is a simple partial seizure typically involving somatosensory symptoms such as hallucinations. People are aware of the aura prior to having a generalized seizure. Complex partial seizures result in a loss of awareness and are frequently manifested as motor or automatism behavior. Generalized seizures occur across both hemispheres at once and are most frequently tonic-clonic. Nonconvulsive seizure patients have epileptic EEGs, but no physical signs of a seizure. Your patient presents with the diagnosis of Guillain-Barré syndrome. Which of the following is the priority of care for this patient? A. Assessment of vital capacity B. Reassurance of the patient C. Preparing for electromyography testing D. Obtaining CT scan of the spine - CORRECT ANSWER A Rationale: Airway and breathing are the priorities of care. The ascending loss of muscle contraction can include the diaphragm and respiratory muscles. Vital capacity is commonly used to assess the effectiveness of ventilation in neuromuscular disorders. Electromyogram (EMG) testing may be ordered; the patient should be reassured, but the priority of care is airway and breathing. A CT of the spine may be ordered to rule out cord compression, but is not a priority over assessment of ventilatory capability. A patient sustained cervical fractures at the C4 and C5 level from a motor vehicle collision. In the ED, initially he was moving all extremities equally. He suddenly became hemiplegic on the left side. Which of the following is the most likely cause for this neurological change? A. Carotid artery dissection B. Spinal cord injury C. Spinal epidural hematoma D. Cerebral edema - CORRECT ANSWER A Rationale: Carotid artery dissections are associated with traumatic injuries at the cervical level. The flexion/extension mechanism of injury that causes vertebral fractures and spinal cord injuries can also cause carotid and vertebral dissections. Carotid dissections can cause cerebral infarctions with symptoms of contralateral motor loss of upper and lower extremities. Spinal cord injury and epidural hematoma would result in paralysis bilateral. There is no justification within the scenario to suspect cerebral edema as the cause of the symptoms. Which of the following therapeutic interventions is frequently recommended to manage a cerebrospinal fluid (CSF) leak? A. Drain CSF with a lumbar drain. B. Administer mannitol. C. Limit fluid intake. D. Maintain head-of-the-bed elevation greater than 30 degrees. - CORRECT ANSWER A Rationale: Cerebrospinal fluid (CSF) leak is frequently managed by placing a lumbar drain to remove CSF. This lowers the CSF pressure and decreases the drainage. Mannitol is used to manage cerebral edema and increased intracranial pressure (ICP). Limiting fluid intake does not affect the CSF leak and is not recommended; head of the bed (HOB) is maintained flat, not elevated, to decrease the CSF leak. The mother of a 6-year-old girl just diagnosed with pilocytic astrocytoma asks the nurse what her child's prognosis is. Which of the following would be the best response by the nurse? A. This type of tumor has a good prognosis and can usually be managed with surgery. B. The tumor is malignant and frequently metastasizes to the spine. C. This tumor is associated with poor prognosis. I would encourage you to speak with a palliative care physician. D. The prognosis is not well known. She will probably require long-term chemotherapy. - CORRECT ANSWER A Rationale: The prognosis of pilocytic astrocytoma is good, with over a 90% survival rate in 10 years. It is commonly located in the cerebellum and can be surgically resected. It may not require follow-up radiotherapy if resection is complete. The tumor is not typically malignant. Which of the following cerebral arteries is most likely involved in the presentation of "locked-in" syndrome during a stroke? A. Anterior cerebral artery B. Posterior communicating artery C. Internal carotid artery D. Basilar artery - CORRECT ANSWER D Rationale: The basilar artery provides blood to the ventral portion of the pons. The basilar artery is involved in the stroke, resulting in locked-in syndrome. The internal carotid artery typically presents with unilateral paresis or paralysis. The posterior communicating artery or anterior cerebral artery does not present with quadriplegia. Following a minor brain injury (concussion), the patient may experience which of the following symptoms over the next 6 months? A. Periods of aphasia B. Swallowing deficits C. Difficulty concentrating D. Ataxia - CORRECT ANSWER C Rationale: Following a minor brain injury (concussion), patients may experience postconcussion syndrome. This is self-limiting, with neurological deficits that may last 6 months to a year after injury. Symptoms of postconcussion syndrome include (but not limited to) memory deficits, emotional outbursts, and difficulty concentrating. Periods of aphasia would be more likely transient ischemia attack. Swallowing deficit and ataxia are not associated with postconcussion syndrome and may indicate another neurological issue. A patient presents with signs of occipital headache and abnormal motor strength. The MRI found herniation of the cerebellar tonsils, vermis, and fourth ventricle. How would this Chiari malformation be classified? A. Type I B. Type II C. Type III D. Type IV - CORRECT ANSWER B Rationale: A type II Chiari malformation is the downward displacement of cerebellar tonsils and inferior vermis, fourth ventricle, choroid plexus, and medulla. The patient presents in the ED with expressive aphasia and paralysis of the right arm and leg. He has a decreased level of consciousness and rapid respiration. Which of the following is your priority of care? A. Obtain a STAT CT scan. B. Administer alteplase immediately. C. Perform a baseline National Institutes of Health Stroke Scale (NIHSS). D. Secure an airway and ensure ventilation. - CORRECT ANSWER D Rationale: Priority of care is always airway and breathing. Patients presenting with a decreased level of consciousness (LOC) may be unable to maintain an airway, requiring the airway to be secured. The patient will need a CT scan and a National Institutes of Health Stroke Scale (NIHSS) assessment and may be a candidate for thrombolytic therapy, but airway and breathing are the priorities of care. A patient presents with low-back pain. Upon review of the spinal radiographs, multiple levels of osteophytes are noted. Which of the following best describes an osteophyte? A. Inflammation of synovial joints B. Degeneration of vertebral body with increased bone formation C. Stenosis of the nerve root as exits lateral foramen D. Compression of lumbar disc - CORRECT ANSWER B Rationale: The degeneration of the vertebral body includes increased bone formation of the subchondral bone adjacent to endplate and is called sclerosis. It is less able to absorb loads and causes formation of osteophytes, bony projections also known as spurs. These may compress on neurological structures and cause symptoms. Synovitis is inflammation of synovial joints. Foraminal stenosis causes the compression of exiting nerve roots. Lumbar disc compression can cause symptoms but is not an osteophyte. Anticholinesterase agents are used to improve myasthenia gravis muscle function through which of the following actions? A. Increase secretion of acetylcholine. B. Prevent breakdown of acetylcholine. C. Increase sensitization postsynaptic receptors. D. Increase number of postsynaptic muscle receptors. - CORRECT ANSWER B Rationale: Anticholinesterase agents prevent the breakdown of acetylcholine by acetylcholinesterase. The effect of the anticholinesterase agents is to prolong the effect of the neurotransmitter acetylcholine. The agents do not increase secretion of the neurotransmitter acetylcholine or sensitize the receptors of acetylcholine. The postsynaptic muscle receptors are destroyed and cannot be regenerated. Which of the following diagnostic studies is considered the most reliable to identify spinal cord and soft-tissue injuries? A. Lateral cervical spine radiographs B. CT scan C. MRI D. Flexion/extension radiographs - CORRECT ANSWER C Rationale: The benefits of MRI in evaluating acute spinal cord injury (SCI) are its ability to identify cord compression, soft-tissue injuries such as herniated disc and epidural hematoma, ligament instability, and intramedullary hematomas. Lateral C-spine radiographic studies can identify vertebral fractures and can assess for misalignment of the cervical spine but cannot identify cord or soft-tissue injuries. CT scans are not considered as beneficial as MRI in identifying injury to the spinal cord, soft tissue, or ligaments. Flexion/extension radiographs are used in certain patients to identify misalignment of the spine (ligament injury) but are not able to identify actual injury to the cord, soft tissues, or ligaments. A patient reports he or she experiences irritability and mood changes days prior to a seizure. What is this period called? A. Preictal B. Aura C. Intraictal D. Postictal - CORRECT ANSWER A Rationale: The preictal state is the "warning" sign of an impending seizure that may occur days prior to the seizure. This may include feelings of general irritability or depression, mood changes, anxiety, headaches, lethargy, change in appetite, and light-headedness. An aura is the actual start of the seizure. Intraictal is the period of time during the seizure. Postictal is after the seizure. Which of the following secondary injuries would be the most important determinants of outcomes in patients following traumatic brain injuries? A. Hyponatremia and tachycardia B. Hypoxia and hypotension C. Hyperglycemia and hypothermia D. Hyperthermia and metabolic acidosis - CORRECT ANSWER B Rationale: Current research has found the two most important determinants of outcome following a traumatic brain injury are hypoxia and hypotension. They both are considered secondary injuries and determine cerebral perfusion. Hyperglycemia, hyperthermia, hyponatremia, and metabolic acidosis are secondary injuries and can affect outcomes but are not as severe as secondary injuries affecting cerebral perfusion. Which of the following would be a contraindication for administering a thrombolytic? A. Patient's home medications include Eliquis B. National Institutes of Health Stroke Scale score of 10 C. Patient on a daily aspirin D. Negative CT scan - CORRECT ANSWER A Rationale: Eliquis is classified as a novel anticoagulant. A National Institutes of Health Stroke Scale (NIHSS) score of 10 is not a contraindication for alteplase. Depending upon other criteria, it would be an indication. Antiplatelet agents, such as aspirin, are not a contraindication to alteplase in acute stroke. An acute ischemic stroke will have a negative CT scan initially. Your patient has a sudden loss of consciousness. An emergency CT is obtained and an intracerebral hemorrhage (ICH) is seen. Which of the following would be the LEAST common cause of an ICH? A. Anticoagulation therapy B. Hypertensive crisis C. Aneurysm rupture D. Vascular tumor - CORRECT ANSWER C Rationale: Aneurysm rupture results in subarachnoid hemorrhages (SAH) and intraventricular hemorrhage (IVH), not primarily intracerebral bleeds. Anticoagulated patients, hypertensive crisis, and vascular tumors will typically cause bleeding into the parenchyma and are called intracerebral hemorrhage (ICH). Which of the following statements is a true regarding cerebral palsy (CP)? A. CP is not preventable. B. CP is a disease found in children but can be cured. C. Most children with CP will die by the age of 10 years. D. CP has no cure. - CORRECT ANSWER D Rationale: There is no cure for cerebral palsy (CP). It is preventable in some cases such as those due to maternal infections (vaccinations) or Rh incompatibility (use of Rhogam). CP can be at birth or acquired at a very young age. CP may shorten life expectancy, but many children with CP live into adult ages. Plasmapheresis is treatment commonly used in managing Guillain-Barré. It involves the: A. Complete exchange of red blood cells B. Removal of antibodies with plasma exchange C. Washing of the white blood cells to clear allergens D. Filtering of the immunoglobulins - CORRECT ANSWER B Rationale: Guillain-Barré is an autoimmune disorder. Plasmapheresis involves the exchange of serum plasma to remove the antibodies. Plasmapheresis does not exchange red blood cells, wash white blood cells, or filter immunoglobulins. Which of the following best describes Moyamoya disease? A. Small, multiple aneurysms in the microcirculation B. Arteriovenous malformations C. Hyperlipidemia deposits of fat in the cerebral vessel wall D. Progressive occlusion of the intracranial internal carotid artery with collateral flow - CORRECT ANSWER D Rationale: Moyamoya disease is the progressive narrowing or occlusion of the internal carotid artery with the development of collateral circulation called Moyamoya vessels. Presence of multiple, small aneurysms in the microcirculation is called Charcot-Bouchard. Hyperlipidemia results in the formation of plaque and the narrowing of the vessel but is not called Moyamoya vessels. Arteriovenous malformations (AVMs) are congenital vascular anomalies in which the arteries feed directly into draining veins. When clearing a cervical spine injury in the acute period following a traumatic event, which of the following is NOT required? A. Maintain cervical immobilization until cleared of ligament injury B. Flexion/extension evaluation in an awake, asymptomatic patient C. Visualization of C1 through T1 on lateral cervical radiographs D. MRI of cervical spine - CORRECT ANSWER D Rationale: MRI of cervical spine can be used to clear a cervical spine injury (C-spine) in certain circumstances but is not required. Maintaining cervical immobilization until ligament injuries can be cleared is required to prevent subluxation and cord compression if an injury is present. Awake, asymptomatic patients require evaluation (radiographs or physical assessment) of flexion and extension capability to determine if potential ligament injury since plain radiographs cannot identify ligament unless some degree of subluxation is noted. Lateral C-spines require visualization of C1-C7 and the tip of T1 to clear the C-spine of bony fractures. Which of the following is a known risk factor for a brain tumor? A. Use of cellular phones B. Exposure to ionized radiation C. Consumption of fish with high mercury levels D. Use of microwaves - CORRECT ANSWER B Rationale: Overall, causes of brain tumors are unknown. Exposure to ionized radiation is a known risk factor, which can be modified. Cell phones produce a very low magnetic radiation and have not been found to increase the risk of brain tumor. Environmental risks such as ingestion of high mercury and food cooked in microwave have not been found to increase risk of brain tumors. Lobar intracerebral hemorrhage frequently presents with which neurological symptom? A. Cranial nerve deficits B. Decreased level of consciousness C. Pinpoint pupils D. Horner's syndrome - CORRECT ANSWER B Rationale: A decrease in level of consciousness is frequently associated with lobar intracerebral hemorrhage. A bleed within the brainstem frequently presents with cranial nerve deficits, pinpoint pupils, and Horner's syndrome. Patients with Mèniére's disease often complain of feelings of aural fullness accompanied by which of the following other symptoms? A. Worst headache of their lives B. Urinary incontinence C. Roaring sound in ears D. Frequent ear infections - CORRECT ANSWER C Rationale: A common complaint by patients is a "roaring" sound in their ears as well as aural fullness. Urinary incontinence is associated with normal-pressure hydrocephalus (NPH). Subarachnoid hemorrhage (SAH) presents with the "worst headache of their life." M`eniére's disease is not associated with frequent ear infections but can have hearing losses. A patient is experiencing a tonic-clonic seizure on the floor next to the bed. To prevent injury during the seizure, which of the following is the most appropriate intervention by the nurse? A. Move the bed and any other objects away from the patient to prevent injury. B. Just monitor the patient and do not attempt to make any interventions during the seizure. C. Move the patient away from the bed and to the middle of the floor. D. Restrain the patient to prevent injury. - CORRECT ANSWER A Rationale: The goal to prevent injury of the patient is to move objects that can potentially injure the patient away from the patient. Restraining or attempting to move the patient can cause injury to the patient. Just monitoring without attempting to protect the patient is incorrect and can cause great injury to the patient. Which of the following is NOT considered a cholinergic side effect of anticholinesterase medications used in managing myasthenia gravis? A. Diarrhea B. Nausea and vomiting C. Increased salivation D. Urinary retention - CORRECT ANSWER D Rationale: Cholinergic side effects of anticholinesterase medications include diarrhea, increased salivation, and nausea and vomiting. Urinary retention is not considered a side effect of anticholinesterase agents. Intracellular swelling in the brain occurred following an anoxic brain injury. What is this called? A. "Steal" phenomenon B. Neurogenic cerebral edema C. Vasogenic cerebral edema D. Cytotoxic cerebral edema - CORRECT ANSWER D Rationale: Cerebral edema is classified as vasogenic and cytotoxic. Cytotoxic cerebral edema involves intracellular swelling and is caused by hypoxic and/or anoxic brain injuries. Vasogenic cerebral edema is interstitial swelling and is usually caused direct trauma or injury to the brain tissue. The "steal" phenomenon involves inappropriate distribution of blood flow to areas of injury following traumatic brain injury. Neurogenic cerebral edema is not a classification of brain swelling. Which of the following frequently presents with nausea, vomiting, and ataxia? A. Cerebellar hemorrhage B. Thalamic hemorrhage C. Pituitary hemorrhage D. Frontal lobe hemorrhage - CORRECT ANSWER A Rationale: Cerebellar hemorrhage frequently presents with nausea, vomiting, and ataxia. Thalamic hemorrhage presents with loss motor and/or sensory. Headache and sudden loss of consciousness is sign of lobar (frontal lobe) hemorrhage. Pituitary hemorrhage causes sudden onset of headache and visual field deficits. Which of the following radiographs is best used to identify spinal segmental instability in an awake, nontraumatic patient? A. Cervical CT scan B. Diffusion-weighted imagery C. Myelogram D. Flexion extension x-rays - CORRECT ANSWER D Rationale: Cervical flexion extension radiographs are used to evaluate vertebral segmental stability. Diffusion weighted imagery is used to identify brain hypoperfusion in stroke patients. Myelogram is utilized to view central and lateral recesses and can visualize compression of individual nerve roots. Which of the following is a TRUE statement about rehabilitation with spinal cord-injured (SCI) patients? A. Rehabilitation begins after the patient is stabilized in the acute period. B. The goal of rehabilitation in SCI patients is to return the patient to his or her prior level of functioning. C. Preventing secondary injuries in SCI patients is a component of rehabilitation. D. It provides long-term assistance to patients with SCI. - CORRECT ANSWER C Rationale: Rehabilitation begins on admission into an acute care facility. A major component of rehabilitation is the prevention of secondary injuries that can adversely affect outcome. A goal of rehabilitation is to improve the patient's independence in activities of daily living, but it is not realistic to have the goal of returning to their prior level of function in spinal cord-injured (SCI) patients. Rehabilitation is to assist with reintegration of the patient into society with good resources, but it is not to provide long-term care and assistance to the patient. The cardinal feature of Guillain-Barré includes which of the following? A. Unilateral ascending paralysis B. Descending bilateral paresthesia C. Bilateral ascending paralysis D. Bilateral spasticity in upper extremities - CORRECT ANSWER C Rationale: The primary characteristic of paralysis in Guillain-Barré (GB) is bilateral, ascending paralysis. It may or may not involve ventilatory muscles and requirement for mechanical ventilation. It is bilateral, not unilateral, paralysis. GB presents in an ascending manner, not in a descending manner. Which of the following has been associated with a genetic increase in risk of brain tumor? A. Down syndrome B. Autoimmune disorders C. Glioblastoma gene D. Neurofibromatosis - CORRECT ANSWER D Rationale: Genetic syndromes, such as neurofibromatosis types I and II, have been associated with brain tumor risk in families. Glioblastoma has a less than 1% with a genetic predisposition. Allergies and immune disorders may protect against brain tumors. Down syndrome has a very low association with brain tumors. Which of the following is the priority of care of a patient following a seizure? A. Reorient the patient to place and time. B. Determine whether the patient has a recollection of the seizure. C. Maintain the patient's airway and breathing. D. Assess for the presence of Todd's paralysis. - CORRECT ANSWER C Rationale: Airway and breathing are always the priorities. Following a seizure, patients may have altered mentation and are unable to maintain airway. All of the other answers are interventions following a seizure, but the priority is airway. When assessing a patient with meningitis, you passively flex the patient's neck and his or her knees automatically flex upward. What is this called? A. Brudzinski's sign B. Romberg sign C. Kernig's sign D. Kehr's sign - CORRECT ANSWER A Rationale: Brudzinski's and Kernig's signs are both signs of meningeal irritation and can be present in patients with meningitis. The Brudzinski's sign is seen when the flexion of the neck causes knees to passively flex. The Kernig's sign is pain or hamstring spasm upon straightening the bent leg. Romberg's sign is found in patients with vertigo. Kehr's sign is found in splenic injuries. A patient presents to your unit with the diagnosis of an intracerebral hemorrhage. Which of the following blood pressure (BP) parameters orders would be expected? A. Keep systolic BP >220 mmHg. B. Maintain systolic BP <100 mmHg. C. Maintain systolic BP between 130 and 150 mmHg. D. Treat BP only if patient rebleeds. - CORRECT ANSWER C Rationale: The goal in a hemorrhagic stroke is to keep the systolic blood pressure (SBP) low to prevent a rebleed but high enough for perfusion of the brain tissue. Frequently, the BP will be ordered as a range such as between 130 and 150 mmHg. An SBP > 220 mmHg will increase incidence of rebleeding. Less than 100 mmHg will increase ischemic injury. The BP should be managed to prevent complications such as rebleeds, not to treat them only when they occur. Postoperative management of carotid endarterectomy (CE) includes monitoring of neurological assessment. Which of the following physiological changes is NOT considered a common cause for the neurological deterioration following the CE? A. Reperfusion injury with cerebral edema B. Embolic showers C. Cerebral ischemia D. Subdural hematoma - CORRECT ANSWER D Rationale: The procedure of carotid endarterectomy (CE) involves clamping of the carotid artery, which can lead to cerebral ischemia. Placing a catheter into the carotid artery to perform the CE can cause embolic showers. When the carotid artery is opened and perfusing, reperfusion hyperemia can predispose the patient to brain edema. Subdural hematoma is not a common complication of CE. Which of the following patients is LEAST likely to experience a chronic subdural hematoma? A. An 85-year-old male patient B. A patient with severe dementia C. Patient on anticoagulation therapy D. An alcoholic patient - CORRECT ANSWER C Rationale: The elderly, alcoholics, and dementia patients are prone to experiencing chronic subdural hematomas. These patient populations have atrophy of brain, resulting in a greater capacity to hold the volume of venous blood, delaying the onset of symptoms. Patients on anticoagulation are more likely to experience an intracerebral hemorrhage or an acute to subacute bleed. Which of the following types of headache may be accompanied by an aura? A. Cluster headaches B. Migraine headaches C. Stress headaches D. Daily headaches - CORRECT ANSWER B Rationale: An aura has been found to frequent migraine headaches. It is not associated with cluster, stress, or daily headaches. Which of the following is LESS meaningful when talking to the patient about the brain tumor pathology and prognosis? A. Malignant or benign B. Tumor growth C. Location of tumor D. Patient's comorbidities - CORRECT ANSWER A Rationale: A benign tumor in the brain may be more life-threatening than a malignancy due to several factors. The location is very important because the tumor may be benign but is present in an eloquent area of the brain or a difficult location to reach with surgery or radiation. Tumor behavior or growth is important to the development of symptoms. Patient's comorbidities, including health and age, play a significant role in outcomes with brain tumors. Aneurysms can be classified based on the shape, size, and origin of the aneurysm. Which of the following terms best describes an aneurysm with a neck? A. Saccular aneurysm B. Fusiform aneurysm C. Giant aneurysm D. Mycotic aneurysm - CORRECT ANSWER A Rationale: An aneurysm with a neck is called a saccular or berry aneurysm. A fusiform is more of an outpouching of the vessel wall. A giant aneurysm is based upon the size of the aneurysm, measuring greater than 2.5 cm in diameter. A mycotic aneurysm is classified based upon origin being an infectious source such as endocarditis. A patient is diagnosed with disc protrusion (propulsion). Which of the following best describes disc herniation? A. Occurs when nucleus ruptures through innermost fibers of the annulus fibrosus with no disruption to outer annular fibers. B. Rupture of nucleus distorts the outermost fibers of the annulus and causes bulge outward. C. Complete split of annulus allows nuclear material to leak out of surrounding spaces. D. Extruded nuclear substance is no longer attached to material remaining within the disc and fragments may float around the spinal canal. - CORRECT ANSWER B Rationale: Disc protrusion or propulsion involves the rupture of the outermost fibers of the annulus. This results in bulging outward of the disc. Disc nuclear herniation without protrusion involves injury to the inner annulus without disruption of the outer. Nuclear extension is the complete split of the annulus allowing nuclear material to leak into surrounding spaces, but protruded material remains attached. Extruded nuclear substances, which are not attached and float around the spinal cord, are called sequestered nuclei. A paraplegic patient is being taught in rehabilitation to prevent pressure ulcers while sitting in the wheelchair. Which of the following strategies is the MOST important to preventi pressure ulcers? A. Use air cushion pad at all times. B. Perform frequent shifts in the chair. C. Use a Hoyer lift to move in the chair. D. Massage skin frequently to improve skin circulation. - CORRECT ANSWER B Rationale: Paraplegic patients are taught to perform frequent chair shifting to prevent prolonged pressure and pressure ulcers (redistribution techniques). Cushions can be used in chair to lower the risk, but shifting frequently is more important. Hoyer lifts can be used, but paraplegic patients can usually shift themselves with their upper extremities. Massaging can improve circulation to skin but is not a technique to prevent pressure ulcers while sitting in the wheelchair. Hydrocephalus present in Chiari type II malformations is classified as which of the following? A. Communicating hydrocephalus B. Noncommunicating hydrocephalus C. Degenerative hydrocephalus D. Productive hydrocephalus - CORRECT ANSWER B Rationale: When there is an obstruction to cerebrospinal fluid (CSF) flow resulting in hydrocephalus, it is called noncommunicating hydrocephalus. Communicating hydrocephalus is a result of overproduction or decreased reabsorption of the CSF. Degenerative and productive hydrocephalus is not a classification of hydrocephalus. Which of the following autoimmune disorders is most commonly associated with trigeminal neuralgia? A. Lupus B. Multiple sclerosis C. Myasthenia gravis D. CREST syndrome - CORRECT ANSWER B Rationale: When trigeminal neuralgia (TN) is found in the younger population without other risk factors, they will frequently test for multiple sclerosis (MS). TN and MS are associated disorders, which frequently occur together. Lupus, crest syndrome, and myasthenia gravis are autoimmune disorders but are not frequently associated with TN. Which of the following aneurysms is caused by septic emboli associated with bacterial endocarditis? A. Charcot-Bouchard B. Giant aneurysm C. Ehler's aneurysm D. Mycotic aneurysm - CORRECT ANSWER D Rationale: Mycotic aneurysms are a result of a septic source such as endocarditis showering septic emboli. Charcot-Bouchard is the presence of multiple tiny aneurysms within the deep structures of the brain. A giant aneurysm measures greater than 2.5 cm in diameter. Ehlers-Danlos syndrome is a connective tissue disease resulting in formation of aneurysms throughout the vasculature. Hyperventilation with the lowering of PaCO2 causes which of the following physiological effects in the cerebral circulation? A. Cerebral vasodilation B. Cerebral vasoconstriction C. Increased intracranial pressure D. Cerebral edema - CORRECT ANSWER B Rationale: Carbon dioxide (CO2) is a potent vasodilator in the cerebral circulation. A decrease in PaCO2 causes cerebral vasoconstriction, thus lowering ICP. An increase in PaCO2 causes cerebral vasodilation resulting in an increase in the intracranial pressure (ICP). The lowering of the PaCO2 does not increase cerebral edema. Which of the following best describes the pain syndrome associated with trigeminal neuralgia? A. Dull, constant aching pain along the jaw line B. Constant, severe, knifelike facial pain occurs bilaterally C. Muscle spasms along the V1 and V2 branches, which result in cramping-like pain D. Shock-like sensations, intermittent or episodic facial pain that occurs unilaterally - CORRECT ANSWER D Rationale: The pain of trigeminal neuralgia (TN) is neuropathic pain. It is frequently described as shock-like or electrical pain, which comes in volleys, or episodes of pain. It usually occurs unilateral. It is not described as dull, constant, or a cramping-like pain. Which of the following is the most common result of an intracranial aneurysm rupture? A. Subarachnoid hemorrhage B. Epidural hematoma C. Subdural hematoma D. Intracerebral hemorrhage - CORRECT ANSWER A Rationale: Intracranial aneurysm rupture causes bleeding into the subarachnoid and intraventricular spaces. Epidural and subdural hematomas can be caused by trauma to the vascular but are not related to aneurysm rupture. Intracerebral hemorrhage (ICH) is bleeding into the brain parenchyma and is more likely caused by hypertension or anticoagulation. A vaccine has been developed for which of the following types of meningitis? A. Tuberculosis meningitis B. Meningococcal meningitis C. Haemophilus influenzae meningitis D. Listeria - CORRECT ANSWER B Rationale: Meningococcal meningitis is spread through an airborne route and can become an epidemic in close quarters. A vaccination has been developed against one strain of meningococcal meningitis and is recommended in people living in close quarters such as military barracks or college dorms. Which of the following neurotransmitters will inhibit seizure activity? A. Glutamine B. Dopamine C. Acetylcholine D. Gamma-aminobutyric acid - CORRECT ANSWER D Rationale: Gamma-aminobutyric acid is an inhibitory neurotransmitter in the brain and has been found to inhibit seizures. Glutamine is an excitatory neurotransmitter and has been found to stimulate seizures. Dopamine inhibits motor tone and is found to be diminished in Parkinson's disease. Acetylcholine is a neurotransmitter at the level of the neuromuscular junction and is required for muscular contraction. Which of the following types of tremor occur due to a fixed posture against gravity? A. Kinetic intentional tremor B. Postural tremor C. Magnetic gait tremor D. Ataxic tremor - CORRECT ANSWER B Rationale: A postural tremor occurs due to a fixed posture against gravity. Kinetic intentional tremor occurs during goal directed movement. Magnetic gait occurs with normal-pressure hydrocephalus (NPH). Ataxia is an abnormal balance or coordination and is not considered a tremor. When administering an osmotic diuretic, such as mannitol, which of the following laboratory values should be closely monitored? A. Calcium B. Creatinine C. Potassium D. Serum osmolality - CORRECT ANSWER D Rationale: Osmotic diuretics increase serum osmolality, resulting in hemoconcentration. As the serum osmolality increases greater than 320 mmol, neurological injury can occur. As the serum becomes hemoconcentrated, serum Na+ levels increase. Thus, monitoring of both serum osmolality and Na+ levels is recommended. Hgb, hct, Ca+, PO4+, creatinine, and blood urea nitrogen (BUN) may also be ordered but are not as greatly affected. Which of the following is the least severe or mildest form of spina bifida (SB)? A. Myelomeningocele B. SB occulta C. Syrinx D. Meningocele - CORRECT ANSWER B Rationale: Spina bifida occulta is just the identifiable gap between vertebral bodies found on radiographic studies. It does not involve injury to the spinal cord or spinal nerve roots. Meningocele and myelomeningocele are also forms of spina bifida and are more severe due to the involvement of the spinal cord and spinal nerve roots. Syrinx is the fluid accumulation within the central portion of the spinal cord and is not considered a form of spina bifida. Cerebral aneurysms can occur throughout the cerebral circulation. Which of the following is the most common location of a cerebral aneurysm? A. Anterior circulation B. Extracranial internal carotid artery C. Basilar artery D. Vertebral artery - CORRECT ANSWER A Rationale: About 80% of cerebral aneurysms occur within the anterior circulation, including the intracranial portion of the internal carotid artery (ICA), middle cerebral artery (MCA), and anterior cerebral artery (ACA). Of the vessels in the anterior circulation, the intracranial internal carotid artery (ICA) has the highest frequency. Injury to extracranial portion of the ICA is more commonly caused by a traumatic dissection versus an aneurysm formation. The basilar artery and vertebral arteries make up the posterior circulation and account for about 20% of the cerebral aneurysms. Which of the following brain tumors is classified as an extraaxial tumor? A. Oligodendrioglioma B. Astrocytoma C. Pituitary adenoma D. Ependymoma - CORRECT ANSWER C Rationale: An oligodendrioglioma, astrocytoma, and ependymoma all gliomas arise from glial cells. They are classified as intraaxial tumors because they are actually located in brain tissue. A pituitary adenoma is a tumor involving the pituitary gland in the brain but is not composed of brain tissue cells. This is classified as an extraaxial tumor. Trigeminal neuralgia is a type of neuropathic pain. The best treatment for neuropathic pain includes which of the following? A. An antiepileptic B. Opioid C. Nonsteroidal anti-inflammatory drug D. Benzodiazepine - CORRECT ANSWER A Rationale: Neuropathic pain is treated most effectively with antiepileptics (such as gabapentin) or tricyclic antidepressants. Nonsteroid anti-inflammatory drug (NSAID) can be a first-line treatment of neuropathic pain but is not as effective as antiepileptics. Neuropathic pain is not as responsive to opioids or anxiolytics in managing pain. The most common presentation for a subarachnoid hemorrhage is which of the following? A. Sudden development of paralysis B. Ascending bilateral paralysis C. Complaints of "worst headache" of one's life D. Expressive aphasia - CORRECT ANSWER C Rationale: The most common sign of a subarachnoid hemorrhage (SAH) is "the worst headache" of their life. They may also experience some focal neurological deficits and nausea and vomiting. Paralysis is not a common presenting sign of an SAH. Aphasia is more commonly associated with an ischemic stroke. Which of the following cranial nerves (CNs) is most commonly involved in long-term complications of bacterial meningitis? A. CN V (trigeminal nerve) B. CN I (olfactory nerve) C. CN IX (glossopharyngeal nerve) D. CN VIII (acoustic nerve) - CORRECT ANSWER D Rationale: CN VIII (acoustic) is the most commonly damaged cranial nerve (CN) as a result of bacterial meningitis. Hearing loss is a long-term complication of bacterial meningitis. Other CNs frequently injured in meningitis include CN III (oculomotor), IV (trochlear), and VI (abducens), which are involved in extraocular eye movement and CN II (optic). Which of the following would be the most appropriate method used to lower intracranial pressure? A. Elevate the head of the bed. B. Elevate the foot of the bed. C. Perform carotid massage. D. Place rolled towels on either side of the neck. - CORRECT ANSWER A Rationale: Elevating the head of the bed facilitates venous drainage, thus lowering volume and pressure in the intracranium. Elevating the foot of the bed may actually increase the intracranial pressure (ICP). Carotid massage can cause bradycardia but is not used to lower the ICP. Maintaining head alignment is appropriate to facilitate venous drainage, but a rolled towel is not as effective as a soft cervical collar. A patient has a seizure that is localized to the right upper extremity without impairment of consciousness. What is the classification of the seizure? A. Simple partial B. Complex partial C. Generalized seizure D. Nonepileptic seizure - CORRECT ANSWER A Rationale: Simple partial seizures are localized seizures to one area of the brain in which the patient maintains consciousness. Complex partial seizures are also localized seizures but with the loss of consciousness. Generalized seizures occur across both hemispheres at once and are associated with a loss of consciousness. Nonepileptic seizures may be caused by subclinical or psychological seizures. A patient is admitted with an acute ischemic stroke with a current history of sleep apnea. Which of the following would be the most appropriate intervention to improve outcomes? A. Continuous positive airway pressure B. Monitor end-tidal carbon dioxide levels C. Intubation and mechanical ventilation D. Place patient on ketogenic diet - CORRECT ANSWER A Rationale: Treatment of sleep apnea improves the outcomes of stroke patients with sleep apnea. Treatment of sleep apnea includes the use of continuous positive airway pressure. Intubation and mechanical ventilation is invasive management of an airway but is not indicated to treat sleep apnea. Monitoring EtCO2 can be used to assess for CO2 retention but is not an intervention to improve outcomes. A ketogenic diet is not a known therapy for sleep apnea. Neuroleptic agents are most commonly used to suppress symptoms of Tourette's syndrome. Which of the following is the most common neurological side effect of neuroleptic agents? A. Dystonic movements B. Weight loss C. Acute renal failure D. Angioedema - CORRECT ANSWER A Rationale: The most common neurological side effects of neuroleptic agents are dystonic movements (twisting or posturing), tremors, and involuntary movements. Weight loss is also a side effect of neuroleptic agents but it is not a neurological side effect. Acute renal failure and angioedema are not common side effects of neuroleptic agents. Which of the following pituitary adenomas is most amendable to medical management? A. Adrenocorticotropic-secreting adenoma B. Nonsecreting adenoma C. Growth hormone-secreting adenoma D. Prolactinoma - CORRECT ANSWER D Rationale: Prolactinoma is a pituitary adenoma, which secretes prolactin. Medical management is recommended to shrink the tumor. All of the other pituitary adenomas typically require surgical resection. Mechanism of hyperflexion of the neck during a trauma can result in which of the following patterns of injury? A. Disruption of anterior ligament with posterior vertebral fracture B. Central cord syndrome C. Brown-Sequard cord syndrome D. Disruption of the posterior ligament and fractures of the anterior vertebral body - CORRECT ANSWER D Rationale: A hyperflexion injury in the cervical region causes stretching of the posterior ligament with ligament disruption. The compressed area is anterior, causing anterior vertebral body fractures. Anterior ligament disruption with posterior vertebral body fracture is caused by cervical hyperextension injuries. Central cord injuries are usually a result of hyperextension and may not be associated with vertebral fractures. Brown-Sequard cord syndrome is caused by an injury resulting in hemisection of the spinal cord. Which of the following forms of spina bifida has the highest risk for experiencing complications from the time of birth? A. Meningocele B. Chiari malformation type I C. Spina bifida occulta D. Myelomeningocele - CORRECT ANSWER D Rationale: In myelomeningocele cases, the fetus's spinal canal remains open along several vertebrae in the low to middle back with protrusion of meninges and spinal cord. The cord compression and spinal nerve root injuries result in greater number and severity of complications over the other forms of spina bifida. Chiari malformation type I is not a form of spina bifida. A patient is admitted with the diagnosis of a Hunt and Hess scale grade III subarachnoid hemorrhage. You would expect the patient to have which of the following symptoms on neurological examination? A. Asymptomatic presentation B. Unresponsive with Glasgow Coma Scale score of 5 C. Abnormal posturing D. Drowsy or confused - CORRECT ANSWER D Rationale: A grade III subarachnoid hemorrhage (SAH) based upon the Hunt and Hess scale includes a patient presenting with an altered mental status, including being drowsy or confused. Asymptomatic presentation would be a grade 0, and the unruptured aneurysm may be found incidentally. Posturing is a grade IV, and unresponsive is a grade V. In benign essential tremor (BET), the tremor occurs when? A. During rest B. At night C. During intentional activity D. Only during stress - CORRECT ANSWER C Rationale: In benign essential tremor (BET), the tremors occur with intentional activity, not at rest. This is different than Parkinson's disease, in which tremors occur at rest and improve during intentional activity. Stress will worsen tremors, but it is not the only time when the tremors occur in BET. A burst fracture of the vertebral body is most commonly associated with which mechanism of injury? A. Hyperflexion B. Hyperextension C. Torsion injury D. Axial loading - CORRECT ANSWER D Rationale: Axial loading or vertical compression of the spine causes the vertebral body to burst. Hyperflexion injuries cause posterior ligament disruptions and anterior vertebral compression fractures. Hyperextension injuries cause fracture of posterior vertebral body components and disruption of anterior longitudinal ligament. Torsion injury is associated with sprain or muscle injury of the neck. Which of the following radiographic studies is considered the gold standard used to identify the location and characteristic of a central nervous system tumor? A. CT without contrast B. CT with contrast C. MRI D. Magnetic resonance arteriogram - CORRECT ANSWER C Rationale: MRI with and without contrast is considered the gold standard in diagnosing central nervous system tumors, including determining the location and characteristic of the tumor. CT with and without contrast is typically a screening and can identify mass lesions and shifts. Magnetic resonance angiography (MRA) is used more to identify vascular anomalies such as a cerebral aneurysm or arteriovenous malformation (AVM). Following an injury to the spinal cord, your patient exhibits the following symptoms: bilateral loss of motor function, pain, and temperature, but the patient maintains proprioception and light touch. Which of the following spinal cord syndromes does he or she exhibit? A. Anterior cord syndrome B. Central cord syndrome C. Brown-Sequard cord syndrome D. Complete cord injury - CORRECT ANSWER A Rationale: Anterior cord syndrome results in the loss of motor, pain, and temperature but spares some of the sensory tracts such as proprioception and light touch. Central cord syndrome results in greater upper-extremity than lower-extremity weakness. Brown-Sequard cord syndrome is a hemisection of the cord and results in ipsilateral loss of motor and contralateral loss of pain and temperature. A complete cord injury is a loss of all motor and sensory below the level of injury. Creutzfeldt-Jakob disease is a spongiform encephalopathy, which is considered a prion disease. Which of the following is a prion disease? A. Abnormal version of infectious protein B. Protozoa infection found in stagnant water C. Bovine tapeworm that invades brain tissue D. Tick-borne disease that infects meninges - CORRECT ANSWER A Rationale: A prion disease is an abnormal infectious protein. It results in a fatal encephalopathy. Prion diseases are not related to protozoa infections and tapeworm and are not transmitted by ticks. Which of the following is NOT classified as a simple partial seizure? A. Somatosensory seizure B. Psychogenic seizure C. Autonomic seizure D. Atonic seizure - CORRECT ANSWER D Rationale: Atonic seizures are classified as generalized seizures. The epileptic focus initiates throughout both hemispheres. Somatosensory, psychic, and autonomic seizures are classified as simple partial seizures due to epileptic focus occurring within a focal area of the brain. Which of the following may be a complication of a lumbar puncture in a patient with a subarachnoid hemorrhage? A. Herniation syndrome B. Development of aphasia C. Kernig's sign D. Brudizinski's sign - CORRECT ANSWER A Rationale: Following a lumbar puncture, herniation can occur if the patient has an increased intracranial pressure (ICP). The positive pressure in the brain can herniate brain structures following a negative pressure in the lumbar region caused by the lumbar puncture. Kernig's and Brudizinski's signs are associated with meningitis or meningeal irritation. Aphasia is associated more commonly with ischemic strokes. A patient requiring a posterior cervical fusion is placed in the prone position for a prolonged period of time and experiences significant blood loss and hypotension. Which of the following is the most likely complication of this scenario? A. Visual losses B. Mesenteric ischemia C. Acute kidney injury D. Intracerebral hemorrhage - CORRECT ANSWER A Rationale: Prone positioning for spine surgery puts one at a high risk for visual losses. The addition of the patient experiencing a significant blood loss and who is hypotensive increases the risk of visual losses. Blood loss and hypotension can cause mesenteric ischemia and acute kidney injury, but in this scenario with the patient being in the prone position for a prolonged period of time, it is more likely to cause visual losses. A complication would more likely be an ischemic versus a hemorrhagic stroke. Vasospasm is the focal narrowing of cerebral vessels. This is most likely to appear during which of the following time periods after the subarachnoid hemorrhage (SAH)? A. 2 to 3 days post SAH B. 14 days post SAH C. 7 to 10 days post SAH D. 3 months post SAH - CORRECT ANSWER C Rationale: Subarachnoid hemorrhage (SAH) complication of vasospasms has its highest incidence 7 to 10 days post SAH. Vasospasms are not typically seen before day 4 or after day 21 post SAH. Which of the following is most commonly used to manage the vasogenic cerebral edema surrounding a brain tumor? A. Corticosteroids B. Mannitol C. Hypertonic saline D. Hypothermia - CORRECT ANSWER A Rationale: Corticosteroids are commonly used to manage the vasogenic edema surrounding cerebral tumors. Dexamethasone (Decadron) is the drug of choice. In severe edema and increased intracranial pressure (ICP), osmotic diuretics (such as mannitol and hypertonic saline) may be used to lower the ICP. Therapeutic hypothermia is used in patients with cytotoxic cerebral edema caused by an anoxic brain injury (postresuscitation). Which of the following is a recognized management of vasospasm following subarachnoid hemorrhage? A. Hypervolemia B. Hypertension C. Hypothermia D. Hemodilution - CORRECT ANSWER B Rationale: Hypertension is used to provide perfusion to the brain tissue distal to the narrowed vessel experiencing vasospasm. Hypervolemia is no longer recommended due to situations of volume overload. It is recommended to optimize hemodynamic parameters and assure euvolemic status. Hypothermia is not recommended for subarachnoid hemorrhage (SAH) patients. Hemodilution is not recommended because of the effect on ability to carry oxygen to the tissues. The goal of medical treatment for benign essential tremor is best described as which of the following? A. Cessation of all tremor activity B. Decreasing the frequency of the tremors C. Decreasing the amplitude of the tremors D. Treating the emotional effects of the tremors - CORRECT ANSWER C Rationale: The treatment of benign essential tremor (BET) does not cure or stop the tremors. The goal of treatment is to decrease the amplitude of the tremors. Improvement of the emotional side may occur following the reduction in amplitude but is not the primary goal of treatment. A cerebrospinal fluid analysis of bacterial meningitis includes all of the following except? A. Elevated protein B. Elevated glucose C. Increased lactate D. Elevated neutrophils - CORRECT ANSWER B Rationale: In bacterial meningitis, cerebrospinal fluid (CSF) analysis results in elevated protein, elevated white blood cell (WBC) neutrophils, increased lactate, and low glucose. Bacterial meningitis causes low glucose, not high. Viral meningitis typically has a normal CSF glucose level. Which of the following can increase the risk of spina bifida during fetal development? A. Exercise B. Maternal trauma C. Vitamin C deficiency D. Exposure to high temperatures - CORRECT ANSWER D Rationale: Evidence suggests that increased body temperature in the early months of pregnancy may increase the risk of spina bifida (SB). Elevated core body temperature by about 2°C (about 3-4°F) above normal caused by fever or the use of saunas and hot tubs can result in development of SB. Vitamin B9 deficiency, not vitamin C, may increase the risk of SB. Maternal trauma is not as known of a risk for SB as for cerebral palsy. Exercise is not a risk for SB. Which of the following electrolyte abnormality most commonly follows subarachnoid hemorrhage? A. Hyperphosphatemia B. Hyponatremia C. Hyperkalemia D. Hypocalcemia - CORRECT ANSWER B Rationale: Hyponatremia is the most common electrolyte abnormality following subarachnoid hemorrhage. It can be due to cerebral salt wasting syndrome or syndrome of inappropriate antidiuretic hormone. A patient presents with neurological deficits lasting 20 minutes followed by complete resolution of symptoms. During the transient ischemic attack workup, the intracranial internal carotid artery was found to be 70% obstructed. Which of the following is NOT recommended at this time? A. Dual antiplatelet with clopidogrel (Plavix) and aspirin B. Maintain systolic blood pressure less than 140 mmHg C. Immediate angioplasty and stenting D. High intensity statins - CORRECT ANSWER C Rationale: It is currently not recommended for a patient with transient ischemic attack (TIA) to be immediately taken for angioplasty and stent placement. Medical management with dual antiplatelets, BP control, and high intensity statins is recommended as a first-line intervention. If TIA reoccurs or stroke occurs, then invasive management with stents or endarterectomy may be considered. Which of the following has been identified as a precipitating factor that can trigger the onset of Guillain-Barré syndrome? A. Hyperthyroidism B. Vaccinations C. Urinary tract infection D. Bacteremia - CORRECT ANSWER B Rationale: Flu vaccines can cause the onset of Guillain-Barré (GB). Other known causes include viral infections and trauma. Urinary tract infections (UTIs) are typically bacterial infections and are not associated with GB. Hyperthyroidism and bacteremia are not associated with triggering GB. A patient with Brown-Sequard cord syndrome would present with which of the following patterns of symptoms? A. Ipsilateral motor loss and contralateral pain and temperature loss B. Loss of both motor and sensory function below the level of injury C. Greater upper-extremity weakness verus lower-extremity weakness D. Loss of sensory function but maintains motor function bilaterally - CORRECT ANSWER A Rationale: Brown-Sequard cord syndrome involves the hemisection of the spinal cord. The resulting symptoms include ipsilateral loss of motor function and contralateral loss of pain and temperature control. In a complete cord injury, there is a complete loss of motor and sensory function below the level of injury. Central cord syndrome presents with greater loss of upper-extremity motor function than lower extremity motor function. A loss of sensory function without motor function is not indicative of Brown-Sequard syndrome. The larval stage of the pig tapeworm eventually enters through the gastrointestinal tract and moves into brain tissue. This larvae is acquired by which of the following? A. Swimming in stagnant water B. Tick bites C. Eating undercooked pork D. Mosquito bite - CORRECT ANSWER C Rationale: Neurocysticercosis involves pig tapeworm larvae entering the brain. Pig tapeworm larvae are acquired by eating undercooked pork or improper hand washing while preparing food of an infected person of tapeworm. Tick bites can cause Lyme disease. Swimming in stagnant water may expose children or immunosuppressed patients to protozoa, which results in severe cerebral edema and death. A mosquito bite can spread encephalitis. Which of the following brain tumor types is amendable to surgical gross resection and tumor biopsy? A. Frontal lobe glioblastoma B. Brainstem glioma C. Tumor located in Broca's area D. Vascular tumor - CORRECT ANSWER A Rationale: Deep, intraaxial tumors in the brainstem, vascular tumors, and tumors located in eloquent areas (i.e., Broca's area) are not amendable to surgical resection and biopsy due to the location or risk of hemorrhage. A glioblastoma located in the frontal lobe is a candidate for resection. Which of the following best describes cerebral palsy (CP)? A. CP is a progressive motor movement disorder. B. CP is always caused by hypoxic injuries during delivery. C. CP is a permanent injury that is nonprogressive. D. CP is a reversible ischemic injury. - CORRECT ANSWER C Rationale: Cerebral palsy (CP) is considered to be nonprogressive. The abnormal movement may change as the child matures but is not progressive. There are multiple causes and underlying etiologies besides just hypoxic injuries that can result in CP. CP is a permanent neurological disorder that is not reversible. Complementary medicine has been used to manage pain in trigeminal neuralgia. Which of the following would be the most appropriate treatment? A. Spinal manipulation B. Acupuncture C. Meditation D. Herbal supplements - CORRECT ANSWER B Rationale: The complementary medicine most commonly used to manage pain in trigeminal neuralgia (TN) is acupuncture. Spinal manipulation is not a pain management technique used in treating TN. Meditation can be an effective treatment for pain, but acupuncture is more effective in TN. Herbal supplements are not common for managing TN. Following spinal cord injury, the nurse needs to know complications that can occur at the different levels of spinal cord injury. At which level is the diaphragm innervated? A. C2 B. C4 C. C6 D. T1 - CORRECT ANSWER B Rationale: C4 is the level at which the diaphragm is innervated. Injury occurring at the level of C4 or above will affect the patient's ability to have spontaneous ventilation. C2 level injury, above the level of the diaphragm, results in a complete loss of ventilation, and the patient will become ventilator dependent. C6 and T1 injury level injuries occur below the level of diaphragm innervation and should be able to ventilate spontaneously once edema has resolved. A long-term complication of a subarachnoid hemorrhage includes which of the following: A. Vasospasm B. Cerebral edema C. Hydrocephalus D. Nausea and vomiting - CORRECT ANSWER C Rationale: All of the answers are complications of subarachnoid hemorrhage, but hydrocephalus is the only long-term complication and may even require the placement of a ventriculoperitoneal (VP) shunt. Vasospasms occur most frequently between day 7 and 10 post subarachnoid hemorrhage (SAH). Cerebral edema and nausea and vomiting commonly occur within the first 48 hours. Which of the following types of encephalopathy is described as an acute process, resulting in cerebral edema induced by rapid changes in serum osmolality? A. Septic encephalopathy B. Drug-induced delirium C. Hepatic encephalopathy D. Dialysis disequilibrium syndrome - CORRECT ANSWER D Rationale: Disequilibrium syndrome with hemodialysis is a sudden onset of cerebral edema caused by a rapid removal of blood urea nitrogen (BUN), resulting in a rapid decrease of serum osmolality. Septic encephalopathy is a result of sepsis and leukocytosis. Septic patients can develop altered mentation, but it is due more to the disruption of the blood-brain barrier. Drug-induced delirium is temporary due to the drug and resolves when the drug leaves the system. Hepatic encephalopathy is due to elevated ammonia levels and alterations of the blood-brain barrier. Your patient is experiencing a seizure. Upon recovery of the seizure, it was noted he had left arm paralysis. This is phenomenon is called? A. Postictal period B. Aura C. Todd's paralysis D. Electromechanical dissociation (EMD) - CORRECT ANSWER C Rationale: Todd's paralysis is a temporary neurological deficit following a seizure. It may include temporary loss of motor or sight. A postictal period is the time after a seizure in which the patient may be drowsy or lethargic. It does not involve a paralysis. An aura comes before the generalized seizure and is considered to be a simple partial seizure. Electromechanical dissociation is the physical presence of seizure activity without the electrical activity on EEG. Normal-pressure hydrocephalus (NPH) typically presents with all of the following except: A. Nausea and vomiting B. Gait disturbances C. Urinary symptoms D. Dementia - CORRECT ANSWER A Rationale: Normal-pressure hydrocephalus (NPH) presents as "wet," "wacky," and "wobbly." Wet is incontinence (urinary symptoms), wacky is dementia, and wobbly are the abnormal gait disturbances. Nausea and vomiting is a sign of increased pressure hydrocephalus, not in NPH. Which of the following tests is most commonly used to screen for fetal spina bifida during pregnancy? A. Maternal serum alpha-feto protein test B. Amniocentesis C. Estriol D. Human chorionic gonadotropin - CORRECT ANSWER A Rationale: Maternal serum alpha-fetoprotein (MSAFP) is the most commonly used screening test for spina bifida (SB). Estriol, human chorionic gonadotropin (HCG) and amniocentesis may be used if the MSAFP is positive for a high risk of the fetus having SB and confirmation is needed. The cervical region contains seven vertebral bodies. How many paired cervical nerve roots are found in the cervical region? A. Six B. Seven C. Eight D. Nine - CORRECT ANSWER C Rationale: There are seven vertebral bodies in the cervical region, but there are eight paired cervical nerve roots exiting the spinal cord. The spinal nerve roots exit above the corresponding vertebral body until the level of C7 in which the spinal nerve root changes to exit below the vertebral body. There are two sets of paired cervical spinal nerve roots at the level of C7. A fusiform aneurysm is best described as which of the following? A. Aneurysm with a neck B. Aneurysm measuring greater than 2.5 cm in diameter C. Tiny aneurysm in the microcirculation D. Aneurysm forms an outpouching of the vessel wall - CORRECT ANSWER D Rationale: A fusiform aneurysm is an outpouching of the vessel wall. A saccular or berry aneurysm has a neck. A giant aneurysm measures greater than 2.5 cm in diameter. Tiny, multiple aneurysms in microcirculation are called Charcot-Bouchard aneurysms. Which of the following statements best describes multiple sclerosis (MS)? A. MS is a demyelinating disorder characterized by relapses and remissions. B. MS affects the postsynaptic junction of the muscle. C. MS is a motor neuron disorder. D. MS presents as an ascending bilateral paralysis. - CORRECT ANSWER A Rationale: Multiple sclerosis (MS) is a demyelinating disorder of the central nervous system (CNS). The most common form of MS involves relapses and remissions. Myasthenia gravis (MG) affects the neuromuscular junction. Amyotrophic lateral sclerosis (ALS) is a pure motor neuron disorder. Guillain-Barré presents with the ascending paralysis bilateral. Which of the following commonly presents with visual changes, headaches, and depression? A. Viral encephalitis B. Meningioma C. Pseudotumor cerebri D. Normal-pressure hydrocephalus - CORRECT ANSWER C Rationale: Pseudotumor cerebri is considered a benign intracranial hypertension. It commonly presents with visual changes, headaches, nausea and vomiting, tinnitus, forgetfulness, and depression. Viral encephalitis commonly presents with altered mentation. Meningioma presentation may include headaches and visual changes (depending upon the location of the tumor) but is not typically associated with depression. Normal-pressure hydrocephalus (NPH) presents with gait abnormalities, incontinence, and dementia. Which of the following statements is most correct regarding the goal of brain tumor resection? A. The goal in all brain tumors is to resect the entire tumor to prevent reoccurrence. B. Resection of the tumor should only include enough brain tissue to send to pathology for tumor recognition. C. The goal is to resect to the greatest extent possible with the least amount of damage of eloquent areas. D. Chemotherapy and radiation are always preferred methods before surgical resection. - CORRECT ANSWER C Rationale: The goal of brain tumor resection is to remove as much tumor as possible without increasing morbidity or adversely affecting quality of life. Eloquent areas of the brain, such as the language and speech center, affect quality of life. If the goal was to always resect the complete tumor, areas of eloquence would be damaged and quality of life would be affected. It is recommended to resect as much of the tumor as feasible. Surgical resection is typically the first-line treatment followed by chemotherapy and/or radiation in primary brain tumors. Which of the following is NOT a common side effect of antiepileptic medications? A. Drowsiness B. Dizziness C. Nausea and vomiting D. Diplopia - CORRECT ANSWER C Rationale: Nausea and vomiting are not common side effects of most antiepileptics. Drowsiness, dizziness, and diplopia are common side effects of antiepileptics. Which of the following is the most accurate statement regarding strokes caused by central venous thrombosis (CVT)? A. CVT is due to a hypercoagulable state. B. Obstruction of a dural artery is the underlying cause of CVT. C. CVT presents as an ischemic stroke only. D. Thrombosis of the external jugular vein is the most commonly affected area of CVT. - CORRECT ANSWER A Rationale: Central venous thrombosis (CVT), like any other venous thrombotic events, is the result of a hypercoagulable state. The venous clot is occurring in the venous sinuses of the central nervous system (CNS). It is venous in nature, not arterial, so it does not involve the dural arterial system. CVT can present as an ischemic or hemorrhagic stroke and sometimes can be a combination of both. The venous sinuses (cavernous sinus, sagittal sinus, and lateral sinus) are the most common locations of the central venous thrombosis, not the external jugular vein. Which of the following statements is most correct about normal-pressure hydrocephalus (NPH)? A. To determine whether the hydrocephalus is of normal pressure, a ventriculostomy is inserted and the intracranial pressure is measured. B. All patients with NPH will improve with a ventriculoperitoneal (VP) shunt. C. Placement of a VP shunt will not improve symptoms but can slow the progression of the disease. D. Draining cerebrospinal fluid with lumbar drain trials may be used to evaluate patients for VP shunt placement. - CORRECT ANSWER D Rationale: Not all patients with normal-pressure hydrocephalus (NPH) will show significant improvement with the placement of a ventriculoperitoneal (VP) shunt. Typically, a test will be performed in which cerebrospinal fluid (CSF) is removed, and the patient is reevaluated to determine whether the procedure will be effective before the VP shunt is placed. This can include lumbar drain trials in a hospital setting or high-drainage test with a lumbar puncture. VP shunts can improve the symptoms in some patients. It is not recommended to place a ventriculostomy or intracranial pressure (ICP) monitor to determine the ICP while making the diagnosis of NPH. Lhermitte's sign may be present in multiple sclerosis. Which of the following best describes Llhermitte's sign? A. Paresthesia of arms B. Head tremors C. Electric-shock sensations D. Word-finding abnormalities - CORRECT ANSWER C Rationale: The Lhermitte's sign is a sign of neuropathy pain. It is described as an electric- shock sensation. It is not paresthesia, head tremors, or difficulty with word finding. Which of the following signs would be an indication of the presence of spinal shock following a spinal cord injury? A. Hyperspasticity B. Positive Babinski's reflex C. Loss of anal tone D. Hypertension - CORRECT ANSWER C Rationale: Spinal shock results in a loss of motor, sensory, and deep tendon reflexes. A loss of anal tone is a sign of loss of reflexes. Hyperspasticity, hyperreflexia, and hypertension occur after spinal shock has resolved, and the patient is at risk for autonomic hyperreflexia. A tumor in which of the following lobes of the brain is most likely to present with seizures? A. Frontal lobe B. Parietal lobe C. Temporal lobe D. Occipital lobe - CORRECT ANSWER C Rationale: Seizure risk is based upon location and the type of tumor. The temporal lobe is most susceptible to seizures and epilepsy. Tumors located in the temporal lobe commonly present with seizures. Which of the following is NOT considered a cause of central venous thrombosis? A. Malignancy B. Eye infections C. Factor VIII deficiency D. Pregnancy - CORRECT ANSWER C Rationale: A factor VIII deficiency would cause the patient to have a coagulopathy with a decreased ability to clot. The patient would not be at risk for central venous thrombosis (CVT). Malignancy, infections (especially, eyes, ears, and scalp), and pregnancy can all cause hypercoagulable states and are known risk factors for CVT. Which of the following time intervals for presentation of a stroke patient with a central venous thrombosis is most common? A. Acute (within 48 hours) B. Subacute (48 hours to 30 days) C. Chronic (greater than 30 days) D. Ultraacute (within 12 hours) - CORRECT ANSWER B Rationale: Venous thrombosis strokes are venous, not arterial. Arterial strokes most commonly present acutely, within hours of onset of the stroke symptoms. Venous strokes can present as acute, subacute, or chronic, but are most commonly subacute. Which of the following diagnostic exams can be used to assist in determining the severity of spina bifida in a fetus? A. Amniocentesis B. Maternal serum alpha-fetal protein test C. Ultrasonography D. CT - CORRECT ANSWER C Rationale: High levels of maternal serum alpha-fetoprotein (MSAFP) and amniocentesis measuring fetal alpha-protein are able to identify a fetus with spina bifida (SB), but advanced ultrasonography is the diagnostic examination used to visualize the spine and assist with determining the severity of the SB. Which of the following is NOT an appropriate instruction for a patient with cerebrospinal fluid leak following a transphenoidal approach to resect a pituitary tumor? A. Place packing in the nose. B. Avoid Valsalva maneuvers. C. Perform an open-mouth cough. D. Avoid nose blowing. - CORRECT ANSWER A Rationale: The Valsalva maneuver, nose blowing, sneezing, and coughing can cause a subsequent cerebrospinal fluid (CSF) leak. If the patient needs to cough, an open mouth cough or sneeze is recommended. Packing the nose with a CSF leak increases the risk of CNS infection. A patient presents in the ED following a witnessed seizure at home. She is awake and states she has been having headaches for the past 2 weeks. A CT scan identified a subacute ischemic stroke with some hemorrhagic components. Upon further diagnostic workup, she is diagnosed with a central venous thrombosis. Which of the following would most likely be the recommended treatment? A. Anticoagulation therapy B. Steroid therapy C. Decompressive craniotomy D. Statin therapy - CORRECT ANSWER A Rationale: Anticoagulation therapy is the recommended management of central venous thrombosis (CVT), even if there is a hemorrhagic component to the stroke. CVT is treated like other venous thromboembolisms (VTEs). Steroid therapy is not recommended in CVT. Decompressive craniotomy is reserved for severe cerebral edema and poor neurological function. This patient is awake and communicating. Statin therapy is not recommended due to the hemorrhagic stroke. Management of multiple sclerosis includes all of the following except? A. Steroid B. Acetylcholinesterase inhibitor C. Immunosuppressive D. Interferon - CORRECT ANSWER B Rationale: Multiple sclerosis (MS) is an autoimmune disorder and is frequently treated with immunosuppressant medications. Commonly ordered medications include steroids, immunosuppressive agents, and interferon. Acetylcholinesterase inhibitors are primarily used in myasthenia gravis (MG). Pseudotumor cerebri is most commonly linked with which of the following? A. Hyperlipidemia B. Obesity C. Hispanic population D. Pet dandruff - CORRECT ANSWER B Rationale: Obesity is the most common link associated with pseudotumor cerebri. A weight-loss program is often used in managing symptoms. Other associated risks include women greater than men, pregnant women, thyroid condition, and chronic kidney disease. Hyperlipidemia, Hispanic race, and exposure to pet dandruff are not considered higher risks for pseudotumor cerebri. A 35-year-old patient is admitted for new-onset right-sided weakness. He reports that playing football about 2 weeks ago, he developed a sore neck. He went to a chiropractor this morning, and the weakness started about 2 hours after his appointment. Which of the following would be the most likely cause of the patient's stroke? A. Basilar artery occlusion B. Extracranial vertebral dissection C. Intracranial internal carotid dissection D. Central venous thrombosis - CORRECT ANSWER B Rationale: Sudden twisting or head movements can cause vertebral or carotid dissections, but the most common location is extracranial. Extracranial vertebral would be more common with trauma and neck manipulations than an intracranial carotid dissection. The scenario is not likely to have resulted in a basilar artery occlusion or a central venous thrombosis (CVT). Ativan (lorazepam) is administered as a primary antiepileptic medication during an active seizure. What is the action of benzodiazepines in stopping a seizure? A. Blocks the Na+ channels. B. Enhances the inhibitory effects of gamma-aminobutyric acid (GABA). C. Overpaces the neurons. D. Induces a medical coma. - CORRECT ANSWER B Rationale: The benzodiazepines work to stop a seizure by enhancing the inhibitory effects of the neurotransmitter gamma-aminobutyric acid (GABA). Phenytoin works by blocking by sodium (Na+) channels and can be used to increase the seizure threshold. Vagal nerve stimulators are used like pacemakers in the heart. They can overdrive the neuronal impulses to control and inhibit the firing of the neurons. Barbiturates are used to induce a medical coma in a refractory seizure. Which of the following statements best describes trigeminal neuralgia (TN)? A. TN most commonly occurs bilaterally. B. TN most commonly affects the mandibular and maxillary divisions of the trigeminal nerve. C. Brain MRI is used to diagnose TN and rule out other causes of facial pain. D. Pain is constant and increases in intensity with progression. - CORRECT ANSWER B Rationale: Trigeminal neuralgia (TN) most commonly affects the mandibular and maxillary division of the trigeminal nerve and rarely affects the ophthalmic division only. TN is typically unilateral and difficult to diagnose. MRI does not typically identify the cause of TN. Pain is intermittent with paroxysmal attacks. It occurs in cycles with remissions. GS has a complete spinal cord injury at the level of C6. The patient complains of a headache and stuffy nose. Blood pressure (BP) is 210/120 mmHg. Which of the following is your first response in managing the patient? A. Immediately call the physician for a STAT CT scan. B. Elevate the head of the bed and remove the source of pain stimulus. C. Administer an antihypertensive. D. Continue to monitor the patient's BP. - CORRECT ANSWER B Rationale: Signs of autonomic hyperreflexia include hypertension, headache, and sensation of stuffy nose. Autonomic hyperreflexia results from an obnoxious stimulus below the level of injury. Putting the head of the bed (HOB) up will lower blood pressure (BP) due to orthostatic hypotension experienced by patients with spinal cord injuries. This allows time to find the painful source and remove it. Administering an antihypertensive initially will cause hypotension once the painful source is found and removed. Without treatment, the hypertension can be life-threatening. Which of the following is an incorrect statement regarding radiation treatment of a brain tumor? A. It affects tumor cells only. B. It causes brain tissue necrosis within area of radiation. C. Certain brain structures are more radiosensitive than others. D. Radiation effects are irreversible. - CORRECT ANSWER A Rationale: Radiation affects both normal and brain tumor cells. The mechanism of radiation to treat tumor cells is irreversible necrosis. Certain brain structures are more radiosensitive such as optic nerve and brainstem. A patient presents with unilateral ptosis, miosis, and anhydrosis on the ipsilateral face. Which of the following syndromes is the most likely cause of this patient's symptoms? A. Chagall's syndrome B. Duvet's syndrome C. Locked-in syndrome D. Horner's syndrome - CORRECT ANSWER D Rationale: Horner's syndrome includes ptosis (eyelid drooping), miosis (small pupils), and unilateral facial anhydrosis (inability to sweat). This is a result of injury to the sympathetic innervation of the face. Locked-in syndrome is a result of basilar artery occlusion. Duvet's syndrome does not result in the symptoms mentioned here. There is not a neurological disorder called Chagall's syndrome. A 1-year-old infant sustains a brain injury in a motor vehicle collision. The child develops abnormal motor movements. Which of the following is the most accurate statement? A. The abnormal movement is not considered to be cerebral palsy because the injury occurred after birth. B. This injury will always progress to mental retardation. C. The presentation of a motor movement abnormality caused by trauma during an early age can be classified as CP. D. Traumatic brain injuries do not cause abnormal motor movements. - CORRECT ANSWER C Rationale: Injury to the motor cortex during the maturation of the brain can result in cerebral palsy (CP). This injury can occur before birth, during the birthing process, or after birth during maturation of the motor cortex. CP is not always associated with mental delays or retardation. A patient with a spinal cord injury that occurred 10 years ago presents with hypertension and diaphoresis above the level of injury. Which of the following is the patient most likely experiencing? A. Spinal shock B. Neurogenic shock C. Autonomic hyperreflexia D. Lacunar stroke - CORRECT ANSWER C Rationale: Spinal cord-injured patients are at risk for the development of autonomic hyperreflexia. Symptoms of autonomic hyperreflexia include hypertension, headache, and diaphoresis above the level of injury. Spinal shock is a loss of motor and sensory below the level of injury in acute spinal cord-injured patients. Neurogenic shock occurs in acute spinal cord-injured patients and results in hypotension and bradycardia. Lacunar stroke is a type of ischemic stroke caused by chronic hypertension and is not related to spinal shock. Surgical instruments that have been used to biopsy brain tissue of a patient suspected of Creutzfeldt-Jakob disease should be: A. Autoclaved B. Destroyed C. Disinfected D. Washing - CORRECT ANSWER B Rationale: Abnormal infectious prions are not susceptible to normal disinfection agents or autoclaving. When instruments have been used on contaminated brain tissue, they need to be destroyed. Which of the following chemotherapy medications is most commonly used as first-line medical management of a glioblastoma? A. Doxorubicin (Adriamycin) B. Temozolomide (Temodar) C. Paclitaxel (Taxol) D. Bevacizumab (Avastin) - CORRECT ANSWER B Rationale: Temozolomide (Temodar) is a first-line chemotherapy treatment in a glioblastoma. It is used in brain tumors because it does cross the blood-brain barrier. Bevacizumab (Avastin) is used in treating several different types of cancer, including glioblastoma. It is used more often in recurring glioblastomas than as a first-line treatment. Doxorubicin (Adriamycin) is a chemotherapy drug commonly used to treat breast cancer. Paclitaxel (Taxol) is a chemotherapy drug used to treat lung cancer. Which of the following does NOT require surgical management? A. Myelomeningocele B. Chiari malformation type II C. Myelomeningocele D. Spina bifida occulta - CORRECT ANSWER D Rationale: Spina bifida occulta is a deformity in the closure of the vertebral bodies, but the spinal canal is intact. There is no spinal cord involvement and does not require surgery. Myelomeningocele and meningocele have opening in the spinal canal with protrusion of meninges and, in the severe cases, protrusion of the spinal cord. This does require surgery to replace the meninges and close the spine. Chiari malformations type II frequently require surgical management due to the severity of the herniation. Myasthenia gravis is a chronic autoimmune disorder that is commonly associated with which of the following disorders? A. Vaccinations B. Lyme disease C. Thyroid disorder D. Renal disease - CORRECT ANSWER C Rationale: Myasthenia gravis (MG) has been found to be associated with thyroid disorders. Thymectomy procedures have been shown to improve clinical function. Vaccinations have been associated with Guillain-Barré (GB). Lyme disease and renal disease are not associated with MG. Which of the following neurological complications is NOT associated with Ehlers-Danlos syndrome? A. Cerebral aneurysm B. Carotid dissection C. Arteriovenous malformation D. Vertebral dissection - CORRECT ANSWER C Rationale: Ehlers-Danlos is a connective tissue disease that causes a weakening of the medial layer within the vasculature. This places the person at a greater risk for arterial dissections (vertebral and carotid) and aneurysm formation (intracerebral). Arteriovenous malformation (AVM) is congenital and is present at birth. These are not commonly associated with Ehlers-Danlos. Which of the following diagnostic tests is considered the gold standard for diagnosing leptomeningeal tumor? A. CT scan B. PET scan C. Tumor biopsy D. Cerebrospinal fluid analysis - CORRECT ANSWER D Rationale: The cerebrospinal fluid (CSF) analysis is considered the gold standard for diagnosing leptomeningeal tumor. The presence of malignant tumor cells in the CSF is diagnostic. Neuroimaging can be used to assist with the diagnosis based upon the pattern of findings. The MRI would be a better imaging technique than the CT scan. PET scans are not used as often with identifying location of brain tumors. Rarely would a biopsy be indicated to diagnose a leptomeningeal tumor. A spinal cord-injured patient commonly experiences orthostatic hypotension when changing positions. Which of the following interventions may help prevent the hypotension? A. Abdominal binder B. Halo vest C. "Quad" cough D. Bowel stimulation - CORRECT ANSWER A Rationale: Orthostatic hypotension occurs in spinal cord-injured patients. Abdominal binders have been found to reduce incidence of orthostatic hypotension. A halo test is used to stabilize an unstable fracture but does not have an effect on orthostatic hypotension. A "quad" cough is performed to improve the effectiveness of the cough in spinal cord-injured patients with limited ventilatory effort. Bowel stimulation is a part of the bowel program in spinal cord-injured patients. Which of the following diagnostic radiographic tests is considered the gold standard for identifying cavernous malformations? A. Transcranial Doppler B. Cerebral angiogram C. Noncontrast CT scan D. Gradient echo MRI - CORRECT ANSWER D Rationale: Cavernous malformations frequently result in small hemorrhages separated by months to years. Gradient echo MRI is the best tool for identifying small hemorrhage and identifying various ages of the bleeds. Transcranial Doppler is used to identify focal narrowing of the cerebral arteries and does not contribute to the diagnosis of cavernous malformations. The vascular anomalies are low flow states and are not easily identified with cerebral angiogram. Noncontrast CT is not as specific as gradient echo MRI in identifying small areas of blood. Which of the following is the most common presenting symptom of Mèniére's disease? A. Dementia B. Vertigo C. Neuropathic pain syndrome of the face D. Facial numbness - CORRECT ANSWER B Rationale: Ménière's disease is characterized by episodes of vertigo. Symptoms include vertigo, nausea, and feeling of "fullness" in the ear. Ménière's disease is not associated with dementia and is not considered a sensory abnormality such as facial numbness or neuropathic pain syndrome of the face. Your patient had a tonic-clonic seizure. The physician has ordered you to load the patient on intravenous (IV) phenytoin (Dilantin). Which of the following is the most accurate statement regarding administering Dilantin via IV? A. Rapid intravenous push (IVP) B. Administer no faster than 50 mg/min C. Administer over 4 hours only D. Cannot be administered using the IV route - CORRECT ANSWER B Rationale: Phenytoin (Dilantin) should not be administered too rapidly intravenously (IV). Dilantin administered via IV too rapidly can cause cardiac arrest. The recommended rate of administration is no faster than 50 mg/minute. It should never be given rapid IV push. The bolus does not require 4 hours to administer. Dilantin is available and is frequently administered in the IV route. A patient presents with nonlocalized symptoms of muscle weakness and confusion. The EEG indicates encephalopathy. Which of the following studies is recommended to diagnose primary central nervous system vasculitis? A. Transcranial Doppler B. Cerebrospinal fluid drainage over 3 days C. Temporal artery biopsy D. MRI - CORRECT ANSWER C Rationale: Primary central nervous system (CNS) vasculitis is commonly diagnosed with bilateral temporal artery biopsy. Brain biopsy may be the gold standard but can have a higher risk. Transcranial Doppler is used to identify vasospasms following a subarachnoid hemorrhage. Cerebrospinal fluid drainage is a technique used to evaluate improvement in patients with normal-pressure hydrocephalus (NPH). MRI is not effective in identifying primary CNS vasculitis. Which of the following statements is most accurate regarding the presentation of myasthenia gravis? A. Causes hyperalgesia of lower extremities B. Bilateral ascending muscle weakness C. Progressive muscle weakness occurs with repetitive muscle activity D. Upper-extremity weakness greater than lower extremity - CORRECT ANSWER C Rationale: Myasthenia gravis (MG) is the result of muscle receptor sites being destroyed by antibodies, thus significantly limiting the number of receptor sites for acetylcholine. Repetitive movements begin to weaken the muscular contraction, resulting in weaker movement with repetitive activity. Testing large muscle repetitive muscles assist with determining the effectiveness of treatment. Which of the following types of central nervous system (CNS) tumor is most likely to benefit from intrathecal administration of chemotherapy medication? A. CNS lymphoma B. Pituitary tumor C. Glioma D. Leptomeningeal tumor - CORRECT ANSWER D Rationale: The leptomeningeal tumors are located in the meninges and subarachnoid space. Administration of a chemotherapy medication directly into the cerebrospinal fluid (CSF) (intrathecal) would assure that the medication more likely reaches the tumor bed. Central nervous system (CNS) lymphomas, gliomas, and pituitary tumors are not within the meninges or CSF and would not benefit from the intrathecal route. Following a stroke, the patient undergoes a cerebral angiogram. It is noted that the patient has "haze-like smoke puffs" bilaterally around the internal carotids. Which of the following would be the most likely diagnosis? A. Leptomeningeal fibrosis B. Neurofibromatosis C. Ehlers-Danlos disease D. Moyamoya disease - CORRECT ANSWER D Rationale: Moyamoya disease is the formation of abnormal collateral circulation due to the bilateral narrowing of the internal carotid and anterior cerebral arteries bilaterally. The gold standard for diagnosis is cerebral angiogram. When the contrast is injected, hazy, smoke-like puffs are seen in the carotid and anterior cerebral arteries bilateral. Leptomeningeal fibrosis is not a disease process. Neurofibromatosis can be a risk for Moyamoya but is not identified by the cerebral angiogram. Ehlers-Danlos disease is a connective tissue disease more commonly associated with vascular anomalies such as aneurysms and dissections. A patient presents with unilateral facial droop and paralysis. When assessing the patient, it is noted that the paralysis also involves the forehead. Which of the following would be the most likely cause? A. Lyme disease B. Bell's palsy C. Trigeminal neuralgia D. Ischemic stroke - CORRECT ANSWER B Rationale: Bell's palsy involves the terminal branches of the facial nerve (cranial nerve [CN] VII). It results in a loss of motor especially involving the muscles required for facial expressions. It is usually unilateral and will not spare the forehead muscles. Lyme disease is an encephalopathy. Trigeminal neuralgia is a pain syndrome, which involves the trigeminal nerve (CN V). Ischemic stroke causing facial droop and unilateral facial paralysis will not involve the forehead. Following administration of alteplase in an acute stroke, the patient is placed in the ICU. According to the American Heart Association/American Stroke Association guidelines, the systolic blood pressure be kept below what? A. 220 mmHg B. 180 mmHg C. 160 mmHg D. 140 mmHg - CORRECT ANSWER B Rationale: Following administration of alteplase in acute stroke patient, the American Heart Association/American Stroke Association (AHA/ASA) recommend maintaining the systolic blood pressure (BP) less than 180 mmHg and the diastolic BP less than 100 mmHg. If the patient did not receive alteplase and it is an ischemic stroke, the systolic BP is allowed to increase to 220 mmHg before treatment. Hemorrhagic strokes, not ischemic with alteplase administration, will have the systolic BP maintained below 160 mmHg. Which of the following is the best intervention to prevent spina bifida? A. Genetic testing B. Dietary supplement C. Maternal vaccinations D. Use of seatbelts - CORRECT ANSWER B Rationale: The most common cause of spina bifida (SB) is dietary deficiencies, especially of folic acid (vitamin B9). Fortifying or supplementing the diet with vitamin B and other required vitamins significantly lower the incidence SB. Genetic testing for abnormal variances is not consistent or reliable. Maternal vaccinations can help prevent cerebral palsy caused by maternal infections. Use of seatbelts is protective but does not prevent SB. Which of the following treatment plan would be indicated in a patient with one unprovoked seizure? A. Admit for video EEG monitoring. B. Initiate an antiepileptic agent. C. Avoid typical precipitants. D. Send home with no further follow-up. - CORRECT ANSWER C Rationale: The standard of care for a single unprovoked seizure is avoidance of typical precipitants such as alcohol and sleep deprivation. An anticonvulsant is not recommended unless the patient has risk factors for recurrence. Admission for video EEG monitoring is typically for patients with intractable episodes or to evaluate the etiology of the seizure. A patient with a seizure, even the first episode, should have follow-up with a neurologist. Which of the following is an indication for a decompressive craniectomy following a traumatic brain injury? A. Contusion in frontal lobe B. Organ donor following brain death determination C. Impending herniation D. Pediatric patient only - CORRECT ANSWER C Rationale: Decompressive hemicraniectomy is the surgical removal of a large portion of the skull to allow room for swelling. It is used to prevent herniation within the closed space or medically retractable increased intracranial pressure. Contusions are not an indication for decompressive craniectomy unless accompanied by increased intracranial pressure. Following brain death and while maintaining the patient for organ donor, a hemicraniectomy is not recommended. Adults and pediatric patients have been found to improve outcomes in certain circumstances. Following an ischemic stroke, the patient is in the progressive care unit (PCU). The following vital signs and laboratory data are obtained: blood pressure (BP) 190/92 mmHg, heart rate (HR) 84 beats/minute, respiratory rate (RR) 16 breaths/minute, temperature = 38.5°C, glucose = 130 mg/dL, Na+ 142 mEq/L. Which of the following interventions is recommended at this time based upon the patient's above findings? A. Administer antihypertensive. B. Administer acetaminophen for fever. C. Place patient on sliding scale insulin and administer insulin subcutaneous (SQ). D. Obtain a urine osmolality and urine specific gravity. answer - CORRECT ANSWER B Rationale: Hyperthermia can worsen outcomes in a patient following an ischemic stroke. Strict normothermia should be maintained, treating body temperature greater than 38˚C. Hyperglycemia can also worsen neurological outcomes but is not usually treated until greater than 140 mg/dl. A Na+ of 142 is normal, so obtaining urine osmolality and specific gravity to diagnose water imbalances is not required at this time. A common side effect of the anticholinergic drugs used to manage Mèniére's disease includes which of the following? A. Tachycardia B. Excessive drooling C. Blurred vision D. Nausea - CORRECT ANSWER C Rationale: Anticholinergics, which are used frequently to manage M`eniére's disease, may produce blurred vision. It decreases oral secretions and nausea and can cause bradycardia, not tachycardia. A patient is recently diagnosed with a grade II astrocytoma. The biopsy report was discussed with the patient, including that the tumor is considered to be benign. Which of the following statements would be most appropriate at this time? A. You are really lucky this is a benign tumor and easily managed. B. Even though the results are benign, this can be an invasive, progressive tumor. C. Benign means this is not cancer and will not require radiation or chemotherapy after surgical resection. D. An astrocytoma typically metastasizes to the lungs. You will need a routine chest x-ray to monitor for tumors. - CORRECT ANSWER B Rationale: Astrocytoma, even a low-grade "benign" tumor, can be very invasive, difficult to treat, and can progress to a higher grade "malignant" tumor. Brain tumor prognosis is based more upon the cell origin and location of the tumor than labeling the tumor benign or malignant. Astrocytoma typically requires follow-up treatment with either or both radiation and chemotherapy. Astrocytoma does not commonly metastasize to the lungs. Which of the following statements regarding the care of a patient after an ischemic stroke is most correct? A. Place all patients on supplemental oxygen to improve tissue oxygenation levels. B. Administer prophylactic antiepileptic medications to all patients. C. Antihypertensives should be administered to keep the systolic blood pressure less than 160 mmHg. D. A bedside swallow test should be obtained prior to administration of oral medications or oral intake on all patients. - CORRECT ANSWER D Rationale: A bedside swallow test should be performed on all stroke patients prior to any oral intake, including oral medications. If they fail a bedside swallow, they should remain NPO until speech therapy can evaluate them. Supplemental oxygen should be administered if the oxygen saturation is less than 94%. It is not recommended to administer to all stroke patients. Prophylactic anticonvulsants are not recommended in stroke patients. Following an ischemic stroke, permissive hypertension is recommended for perfusion unless the patient had received fibrinolytic agent. Systolic blood pressure (BP) may not be treated unless greater than 220 mmHg. Which of the following best describes the allodynia patients with cerebral palsy can experience? A. Inability to differentiate temperature changes B. Loss of pain sensation C. Inability to control body temperature D. Light touch can become painful - CORRECT ANSWER D Rationale: Allodynia is a sensory abnormality in which light touch can become painful. People with cerebral palsy (CP) may experience allodynia. The inability to control body temperature is not typically an issue with CP and is called poikilothermia. Following an unprovoked first seizure, which of the following findings would NOT increase the risk for a second seizure? A. Epileptiform abnormalities on EEG B. Partial-onset seizure C. Presence of hydrocephalus D. Generalized seizure - CORRECT ANSWER D Rationale: Partial-onset seizure carries a higher risk of recurrence than generalized seizures. Epileptiform or slowing on the EEG findings is associated with the highest risk of recurrence. Abnormal findings on MRI, including hydrocephalus, can increase the risk of reoccurrence of seizures. An ischemic stroke patient had passed a bedside swallow test prior to admission to the progressive care unit. While the nurse is administering an oral medication with a sip of water, she notes the patient coughs. Which of the following would be the most appropriate response? A. Continue to administer medications, the patient has passed the bedside swallow test. B. Hold oral medications, put the patient on nothing per os status, and consult speech therapy. C. Place a STAT order for a video endoscopic evaluation. D. Obtain a STAT chest x-ray and place the patient on supplemental oxygen. - CORRECT ANSWER B Rationale: Even though the patient may have passed the bedside swallow examination prior to admission, if a stroke patient begins to cough with oral intake, they should be place NPO and speech therapy are consulted for further swallow evaluations. Stroke patients with abnormal swallowing are at high risk for aspiration pneumonia. The speech therapist will evaluate the stroke patient and make a decision on the most appropriate follow-up diagnostic study. The patient does not require supplemental oxygen unless the oxygen saturations are less than 94%. A neurological patient develops polyuria with a urine output of 450 mL/hr. Which of the following would NOT be found in diabetes insipidus? A. Urine specific gravity <1.005 B. Serum osmolality <275 mOsm/L C. Urine osmolality <200 mOsm/L D. Na+ levels >145 dg/L - CORRECT ANSWER B Rationale: The diagnosis of diabetes insipidus (DI) is made when the urine is dilute (urine specific gravity <1.005 and urine osmolality <200 mOsm/L) and the serum is concentrated (serum Na+ >145 dg/L). Serum osmolality of <200 mOsm/L indicates a hypotonic serum. Which of the following treatments for cerebral edema and increased intracranial pressure is NOT recommended following severe traumatic brain injury? A. Hypertonic saline B. Mannitol C. Therapeutic hypothermia D. Cerebrospinal fluid drainage - CORRECT ANSWER C Rationale: There is very little research data supporting the use of therapeutic hypothermia in severe traumatic brain injury (TBI) and it is currently not a recommended treatment. Mannitol and hypertonic saline are both hyperosmolar agents that can lower the intracranial pressure (ICP) and are recommended to treat increased ICP in severe TBI patients. Cerebrospinal fluid (CSF) drainage is used to lower the CSF volume and decrease ICP. A stroke patient on warfarin (Coumadin) is being bridged with heparin infusion until the international normalized ratio (INR) meets goal. On day 7, the patient's platelet count decreased from 120,000 to 50,000. Which of the following is the most likely cause? A. Immune-mediated thrombocytopenia purpura B. Elevated INR affected the platelet count C. Heparin-induced thrombocytopenia D. Suppression of bone marrow production of platelets - CORRECT ANSWER C Rationale: Heparin is the most common cause for a drug-induced thrombocytopenia. The decrease in platelet count typically occurs between 5 and 10 days of being on heparin and is greater than a 50% decrease. The scenario had the patient on heparin, so heparin-induced thrombocytopenia (HIT) was more likely the cause over idiopathic thrombocytopenic purpura (ITP). An elevated INR does not cause platelet counts to decrease. Suppression of bone marrow production can decrease platelets, but there is no risk identified in the patient's scenario. Which of the following is NOT a known cause of trigeminal neuralgia? A. Aneurysm B. Tumor C. Multiple sclerosis D. Traumatic brain injury - CORRECT ANSWER D Rationale: Traumatic brain injury (TBI) is not considered a common cause of trigeminal neuralgia (TN). Compression of the trigeminal nerve by tumor or aneurysm is a known cause of TN. One of the first signs of multiple sclerosis (MS) is TN due to the demyelination of the cranial nerve. A brainstem glioma in the pons commonly presents with cranial nerve (CN) deficits. Which of the following CNs are most likely involved? A. CN I (olfactory nerve) and II (optic nerve) B. CN III (oculomotor nerve) and IV (trochlear nerve) C. CN V (trigeminal nerve), VI (abducens nerve), VII (facial nerve), and VIII (acoustic nerve) D. CN IX (glossopharyngeal) nerve, X (vagus nerve), and XII (hypoglossal nerve) - CORRECT ANSWER C Rationale: Of the 12 cranial nerves (CNs), 10 CNs originate from the brainstem. CN assessment is important with brainstem involvement. The pons originates in CN sV through VIII, so a tumor involved in the pons commonly presents with deficits in those CNs and those CNs should be assessed. CNs I and II originate from the cerebral cortex. CNs III and IV originate from the midbrain. And CNs IX, X, and XII originate from the medulla. A patient with an acute ischemic stroke states he is allergic to aspirin (acetylsalicylic acid [ASA]). Which of the following would be the most appropriate response? A. Call the pharmacy to check out ASA allergies. B. Explain to the patient that he needs the ASA and encourage him or her to take the ASA. C. Document the patient is refusing the ASA. D. Discuss with the physician changing the order to clopidogrel (Plavix) - CORRECT ANSWER D Rationale: If a patient is allergic to acetylsalicylic acid, the recommendation is to use clopidogrel (Plavix). The patient should receive an antithrombotic medication following an acute ischemic stroke. It would not be appropriate to encourage a patient to take a medicine that the patient states is an allergy. Documentation of the allergy (not that the patient is refusing the acetylsalicylic acid) is appropriate, but the best response to contact the physician for discussion about another antithrombotic agent. Calling the pharmacy about acetylsalicylic acid allergies may be for informational purposes but is not as appropriate as giving the best care to the patient. Upper motor neuron injury presents with which of the following symptoms? A. Flaccidity of muscles B. Significant muscle atrophy C. Hypertonicity of muscles D. Depressed deep tendon reflexes - CORRECT ANSWER C Rationale: The entral nervous system, including the brain and spinal cord, is an upper motor neuron (UMN). UMN injury results in symptoms of spasticity, increased muscle tone, increased deep tendon reflexes (DTRs), and less muscle atrophy. Lower motor neuron (LMN) injury results in flaccid paralysis with a decrease in muscle tone, decreased DTRs, and significant muscle loss. Which of the following terms best describes motor activity of sustained focal stiffening? A. Atonic B. Tonic C. Myoclonic D. Clonic - CORRECT ANSWER B Rationale: Tonic activity in motor seizures involves sustained focal stiffening. Atonicity is the focal loss of muscle tone. Myoclonic activity is irregular brief focal jerking movements. Clonic activity refers to the focal rhythmic jerking movement. It is more rhythmic than the myoclonic activity. An 8-year-old, previously diagnosed with attention deficit hyperactivity disorder, now presents to the neurologist with repetitive involuntary movements and vocalizations. Which of the following is the most likely cause? A. Tourette's syndrome B. Miller Fisher syndrome C. Absence seizures D. Dravet syndrome - CORRECT ANSWER A Rationale: Simple and complex involuntary motor movements and vocalizations are signs of Tourette's syndrome. Tourette's can be associated with attention deficit hyperactivity disorder (ADHD) and obsessive-compulsive behaviors. Miller Fisher syndrome is a variant presentation of Guillain-Barré. Absence seizures are found in children but are demonstrated by periods of blank stares, not involuntary movements. Dravet's syndrome is frequent and prolonged seizures in children within the first year of life. A patient is admitted to the trauma ICU following severe traumatic brain injury. An intracranial pressure (ICP) monitor is placed, and the patient is noted to have increased ICP. The following are the patient's data: K+ 4.2 mEq/L Na+ 130 mEq/L Serum osmolality = 280 mOsm/L Which of the following international normalized ratio results would be considered appropriate for a patient with an acute embolic stroke and atrial fibrillation? A. 1.8 B. 2.4 C. 3.1 D. 3.8 - CORRECT ANSWER B Rationale: The INR goal for ischemic stroke patients with atrial fibrillation is between 2 and 3. An international normalized ratio (INR) below 2 is too low and will increase their chance of another embolic event. An INR greater than 3 is too high and will increase the risk of bleeding. Which of the following would be the most likely ordered hyperosmolar agent to manage this patient's increased intracranial pressure? A. 3% saline B. Mannitol C. 7.5% saline D. Glycerol - CORRECT ANSWER B Rationale: The patient is hyponatremic (Na+ 130), and administration of hypertonic saline (3% or 7.5%) to treat an increased intracranial pressure (ICP) can be detrimental to hyponatremic patients. Sodium levels should be corrected slowly over 24 hours to prevent complications. Administration of hypertonic saline to treat increased ICP can change too rapidly the serum sodium. Mannitol is recommended over hypertonic saline in hyponatremic patients when treating an increased ICP. Glycerol is not commonly used to lower an ICP. Which of the following cranial nerves (CNs) is commonly affected by an acoustic neuroma? A. CN III (oculomotor nerve) B. CN VII (facial nerve) C. CN II (optic nerve) D. CN XII (hypoglossal nerve) - CORRECT ANSWER B Rationale: An acoustic neuroma involves a tumor invading the neural sheath surrounding cranial nerve (CN) VIII (acoustic). CNs VIII, VII (facial), and V (trigeminal) lie adjacent to each other, so damage to CN VII is commonly associated with acoustic neuroma. Focal seizures may demonstrate automatism. Which of the following best describes automatism behaviors? A. Motor arrest B. Hyperkinetic activity C. Irregular, brief focal jerking movement D. Purposeless repetitive motor activity - CORRECT ANSWER D Rationale: Automatism can be found in focal and absence seizures. It involves less coordinated, purposeless repetitive movements. Motor arrest is the cessation of motor movement and unresponsiveness. Hyperkinetic activity is an increase in activity such as pedaling or thrashing. Irregular, brief focal jerking movement is myoclonic activity. The neurologist ordered a statin for your acute ischemic stroke patient. Which of the following statements would be the most appropriate for patient education regarding the statin? A. If your urine turns "reddish, or cola colored," come to the ED. B. It is recommended to take the statin with grapefruit juice to improve absorption. C. This medication is ordered because diet alone will not lower your cholesterol. D. You will need to have your kidney function monitored closely while taking the statin. - CORRECT ANSWER A Rationale: A potential complication of statin administration includes rhabdomyolysis. Patient education regarding rhabdomyolysis, including the color change of urine, is recommended. It is actually recommended to avoid grapefruits and grapefruit juice due to the effect on drug levels. A statin may be ordered even if the patient has a normal cholesterol level. Liver function tests, not kidney function, are monitored when placed on a statin. Which of the following complications of mannitol should be monitored closely in multisystem trauma patients with severe traumatic brain injury? A. Hypokalemia B. Hypernatremia C. Increased serum osmolality D. Diuresis - CORRECT ANSWER D Rationale: Mannitol is effective in lowering intracranial pressure (ICP) and may be administered in severe traumatic brain injury (TBI), but the diuresis can result in hypovolemia and hypotension. This can be detrimental in multisystem trauma patients due to loss of blood. Hypertonic saline may be preferred in multisystem trauma patients over mannitol. Hypokalemia is a potential side effect of mannitol and does require treatment, but this is not specific to multisystem trauma patients. Increased serum osmolality and potentially some increase in sodium can occur but is not the concern with multisystem trauma patients as the diuresis, hypovolemia, and hypotension. Which of the following is a postoperative complication following a vestibular nerve resection? A. Cerebrospinal fluid leak B. Epidural hematoma C. Cushing's triad D. Cerebellar herniation - CORRECT ANSWER A Rationale: The approach for the decompression of the vestibular nerve is base skull surgery. This surgical approach is an increased risk for cerebrospinal fluid (CSF) leaks and central nervous system (CNS) infections. Epidural hematoma is not considered a potential complication of base skull surgeries. Cushing's triad is the symptoms of increased intracranial pressure and herniation. This is not a complication of vestibular nerve resection. Cerebellar herniation is the physiological effect of Chiari malformations. A patient is 24 hours postoperative following pituitary tumor removal by the transphenoidal route. The nurse taking care of the patient noted the urine output to have increased from to 400 mL/hr. Which of the following is the most likely cause for the increase in urine output? A. Shifting of fluids postoperatively B. Cerebral salt wasting syndrome C. Diabetes insipidus D. Syndrome of inappropriate antidiuretic hormone - CORRECT ANSWER C Rationale: Pituitary tumors and resections of the tumor by the transphenoidal route can affect the pituitary-hypothalamus axis, resulting in water imbalances postoperative. A sudden increase in urine output would more likely be due to a lack of production of antidiuretic hormone (ADH). Syndrome of inappropriate antidiuretic hormone (SIADH) is also a water imbalance associated with the pituitary gland but would result in a decrease in urine output and hyponatremia. Cerebral salt wasting syndrome (CSWS) is not associated with ADH and causes a hyponatremia. Fluids can shift from interstitial space back into the vascular space 24 to 48 hours postoperatively. This will increase the urine output due to an increase in circulating volume but would not typically cause the sudden increase in urine output within 1 hour. While providing education to a stroke patient, which of the following is considered to be the most important concept to ensure understanding? A. Document all education provided to the patient and family. B. Perform "teach back" by asking the patient to repeat the information in his or her own words. C. Use a variety of teaching methods. D. Provide a large amount of information during the short period of time the patient is hospitalized. - CORRECT ANSWER B Using the technique of "Teach Back" in which information is provided to the patient followed by the patient repeating the information back in his or her own words. This can be utilized to assess the patient's understanding of what is being taught. Documentation is important but is not used to determine the patient's understanding. It is recommended that a variety of methods are used to teach the patient, but it does not necessarily evaluate the understanding of the material being taught. Providing large amounts of information in a short period of time is not recommended due to the inability to take it all in and understand the information. Which of the following is the most powerful determinant of cerebral blood flow? A. PaO2 B. PaCO2 C. Arterial pH D. Bicarbonate - CORRECT ANSWER B PaCO2 is considered the most powerful determinant of cerebral blood flow (CBF) by controlling the cerebral vascular diameter. CBF responds in a linear fashion to the PaCO2 levels. As the PaCO2 decreases, so does CBF. PaO2 and pH also play a role in cerebral vascular diameter but is not as potent. Bicarbonate levels do not affect CBF. A patient presents to the ED with altered mentation. The patient then stiffens bilaterally followed by rhythmic movement and is not responding to external stimuli. Which of the following is the most correct description of the seizure? A. Tonic seizure B. Tonic-clonic seizure C. Atonic seizure D. Clonic seizure - CORRECT ANSWER B Rationale: In tonic-clonic seizures, the initial onset of the seizure involves muscle-stiffening (tonic) phase, which is followed by rhythmical motor activity, called clonic. A tonic seizure would begin and end with muscle stiffening and no other motor activity. Atonic seizure is a loss motor tone and is commonly associated with dropping or falling. Clonic seizure begins and ends with rhythmical motor activity. Which of the following is NOT a pediatric sign of meningitis? A. Lethargy B. Irritability C. Poor feeding D. Headache - CORRECT ANSWER D Rationale: Lethargy, irritability, and poor feeding are signs of meningitis in pediatric patients. Pediatric patients cannot complain of headaches, and it is not considered a sign of pediatric meningitis. When teaching about stroke recognition, the acronym used as a mnemonic, FAST, stands for which of the following except: A. F = facial drooping B. A = arm weakness C. S = speech difficulties D. T = tinnitus or ringing ears - CORRECT ANSWER D The "T" in the acronym of FAST stands for time to call 911, not tinnitus. The acronym of FAST is used to teach the public to recognize common symptoms of strokes. Which of the following areas of the brain is NOT easily identified as injured by using the National Institutes of Health Stroke Scale? A. Anterior cerebral artery B. Thalamic region C. Middle cerebral artery D. Posterior circulation - CORRECT ANSWER D Rationale: Posterior strokes, such as in the vertebral-basilar region, are not easily identified by using the National Institutes of Health Stroke Scale (NIHSS). The NIHSS is designed to identify anterior stroke syndromes such as middle cerebral and anterior cerebral artery territory. The thalamic infarction is more readily identified with the NIHSS than the posterior strokes. A brain tumor patient is experiencing nausea, vomiting, and headache from the cerebral edema. Which of the following would be the most appropriate initial treatment of the cerebral edema? A. Steroids B. Mannitol C. 3% saline D. Hyperventilation - CORRECT ANSWER A Rationale: The cerebral edema most commonly experienced by patients with brain tumors is focal, surrounding the tumor bed. The initial medical management includes steroids, such as dexamethasone. Mannitol and 3% saline can be used in patients with cerebral edema and increased intracranial pressure (ICP) but would not be the initial first-line therapy in brain tumor patients. Hyperventilation is not a recommended therapy for routine management focal edema. Which of the following neurological injuries is known to result in the development of normal-pressure hydrocephalus? A. Subarachnoid hemorrhage B. Epidural hematoma C. Subdural hematoma D. Parenchymal contusion - CORRECT ANSWER A Rationale: A subarachnoid hemorrhage (SAH) results in blood being introduced into the cerebral spinal fluid (CSF) causing obstruction to the reabsorption of CSF through the arachnoid villi. Damage to the arachnoid villi causes chronic hydrocephalus, resulting frequently in normal-pressure hydrocephalus (NPH). Epidural hematoma, subdural hematoma, and parenchymal contusions are not typically associated with NPH. Which of the following is NOT an educational stroke measure for stroke patients? A. Discharge medications for strokes B. Criteria for acute rehabilitation eligibility C. Signs and symptoms of stroke D. Personal risk factors for a stroke answer - CORRECT ANSWER B Rationale: It is important for patients and families of stroke patients to understand the eligibility and criteria for acute stroke rehabilitation but is not considered a measurement for strokes. Stroke measures for education include discharge medications, symptoms of stroke, and risk factors personalized to the patient. Following a severe traumatic brain injury, the patient is intubated, agitated, and has elevated intracranial pressures. A sedative is ordered. Which of the following side effects of the sedative would be the most concerning for the nurse at this time? A. Hypotension B. Respiratory depression C. Urinary retention D. Constipation - CORRECT ANSWER A Rationale: A sedative or analgesic can cause hypotension, which would adversely affect cerebral blood flow (CBF) and perfusion. Blood pressure must be monitored closely following administration. Respiratory depression can be a life-threatening side effect, but this patient is already intubated and being ventilated. Urinary retention or constipation is not an immediate concern at this time. Which of the following is a true statement regarding the use of steroids in traumatic brain-injured (TBI) patients? A. Steroids have been found to decrease cerebral edema following TBI. B. Steroids are recommended with severe TBI and require glucose monitoring. C. Steroids are not recommended in TBI patients. D. Steroids have been found to be more effective in minor brain injuries. - CORRECT ANSWER C Rationale: Steroids have not been found to decrease cerebral edema or improve outcomes in patients with traumatic brain injury (TBI). The use of steroids for TBI patients (minor or severe) is not recommended. High-dose steroids have been found to increase morbidity and mortality in severe TBI patients. A child was just diagnosed with cerebral palsy (CP), and the parents are asking whether this is genetic and can affect any future children they were planning on having. Which is the best response of the nurse? A. You will need to discuss this with your physician. B. You will need to have genetic counseling before considering getting pregnant again. C. Yes, it is genetic and is most likely to affect your future children. D. It is not genetic, and you are not likely to have more children with CP. - CORRECT ANSWER D Rationale: Cerebral palsy (CP) is not genetic. The chances a second child of the parents will have CP are unlikely unless exposed to the same situation during the pregnancy or delivery. Genetic counseling is not recommended following the diagnosis of CP. A 13-month-old child had sudden extension of both arms and flexion of the trunk. These seizures repeat in clusters. Which of the following is the most accurate description of the seizure? A. Infantile spasms B. Lennox-Gastaut syndrome C. Febrile seizure D. Myoclonic seizure - CORRECT ANSWER A Rationale: The term infantile is used because the spasms occur during infancy. The description provided of the seizure is typical of a spasm and can affect just legs or legs and body. Lennox-Gastaut syndrome usually begins between 3 and 5 years of age and commonly presents with myoclonic or abnormal absence seizures. Febrile seizures occur in infants and pediatric patients, but no temperatures or fever was provided in this scenario. Myoclonic seizure is more a rhythmical jerkin than spastic extension of arms or trunk. Which of the following is the most common visual deficit with patients presenting with pituitary tumors? A. Homonymous hemianopsia B. Scotoma C. Complete blindness unilateral D. Bitemporal hemianopsia - CORRECT ANSWER D Rationale: The pituitary gland is centrally located and adjacent to the optic chiasm. The lateral (temporal) vision crosses in the optic chiasm and travels through the contralateral optic nerve to the occipital lobe. A pituitary tumor can cause compression of the optic chiasm, resulting in bitemporal hemianopsia (loss of half vision in the peripheral in both eyes). This causes a "funnel" vision. A scotoma is a blind spot located anywhere within the visual field. Homonymous hemianopsia is the loss of half vision, medial (nasal) vision in one eye, and lateral (temporal) vision in the other. This commonly involves the occipital lobe. A complete loss of vision in one eye (unilateral) is typically caused by an injury that occurs before the optic chiasm. Which of the following feeding methods would best decrease the incidence of ventilator-associated pneumonia following a traumatic brain injury? A. Percutaneous endoscopic gastrostomy tube B. Transpyloric jejunal tube C. Orogastric tube D. Bolus gastric feeding - CORRECT ANSWER B Rationale: Early gastric feeding (percutaneous gastrostomy tube [PEG] or orogastric tube [OGT]) can pose the risk of delayed gastric emptying and an increase in gastric residuals and aspiration of gastric contents. This increases the risk of ventilator-associated pneumonia (VAP) or hospital-acquired pneumonia (HAP). Placing the feeding tube postpyloric or in the jejunum decreases gastric residuals and lowers the risk of VAP. After the physician left the patient's room, the family asked you to clarify what pseudoprogression means after receiving chemotherapy for a glioblastoma. What would be your best response? A. You will need to ask the physician the next time you meet with him. B. Chemotherapy is not an effective treatment for glioblastoma. C. The tumor appears to have worsened, but the tumor did not actually increase in size. D. This indicates that the tumor has become necrotic and progression will stop. - CORRECT ANSWER C Rationale: Following chemotherapy with temozolomide (TMZ), the glioblastoma tumor may appear to have worsened on radiographic studies, but the tumor progression has actually decreased. There is currently no noninvasive technique to determine pseudoprogression versus actual progression. Nurses should be familiar with management issues of brain tumors to clarify questions of the patients and family members. TMZ has been found effective in some glioblastoma tumors to increase life expectancy. The appearance of pseudoprogression may actually be a good prognosis, but because it cannot be differentiated from actual tumor growth, false reassurance is not recommended. The addition of "BE" to FAST (BE FAST) is to improve the recognition of which of the following types of strokes? A. Anterior strokes B. Embolic strokes C. Posterior strokes D. Subarachnoid hemorrhage - CORRECT ANSWER C Rationale: The use of FAST as an acronym used to remember signs of a stroke had been focused on anterior strokes. The addition of BE to the acronym is meant to improve the recognition of posterior stroke and stands for balance and eyes. Frequently, posterior strokes present with dizziness and visual deficits. An embolic stroke most often involves the middle cerebral artery and is considered an anterior stroke. This acronym is not as beneficial for recognizing a subarachnoid hemorrhage. A patient with a spinal cord lesion involving the spinal nerve root complains of severe pain. Which of the following medications is most appropriate for treating neuropathic pain? A. Hydromorphone (Dilaudid) B. Gabapentin (Neurontin) C. Ketamine D. Ketorolac (Toradol) - CORRECT ANSWER B Rationale: Neuropathic pain is most amendable to anticonvulsant medications, such as gabapentin. Other classes of medications used to manage neuropathic pain commonly include tricyclic antidepressant. Nonsteroidal medications, such as Toradol, can be used in the initial pain management but are not the most appropriate pain management for neuropathic pain. Opioids, such as Dilaudid, are not as effective in neuropathic pain and can lead to opioid addictions. Ketamine is an anesthetic with pain properties but is not recommended for the management of neuropathic pain. Which of the following is a true statement regarding amyotrophic lateral sclerosis (ALS)? A. ALS involves both motor and sensory abnormalities. B. ALS is sclerosis of the white matter in the frontal lobe. C. ALS involves both upper and lower motor neuron abnormalities. D. ALS affects the pons and results in locked-in syndrome. - CORRECT ANSWER C Rationale: Amyotrophic lateral sclerosis (ALS) involves both upper motor neurons and lower motor neurons. There is no sensory involvement in ALS. It is considered a pure motor neuron disease. It is not a sclerosing disorder of white matter. ALS does not affect the pons but can progress to similar paralysis like locked-in syndrome. Which of the following is the most significant complication of strict glycemic control (80-110 mg/dL) in patients following severe traumatic brain injuries? A. Worsening of the Glasgow Coma Scale score B. Increased cerebral edema C. Immunosuppression D. Hypoglycemia - CORRECT ANSWER D Rationale: Hyperglycemia is common following the severe stress, including in traumatic brain injury (TBI) patients. Hyperglycemia is thought to worsen outcomes, but strict glycemic control (range 80-110 mg/dL) results in frequent hypoglycemic episodes. Hypoglycemia can also negatively affect outcomes following neurological injury. Strict glycemic control itself does not cause a worsening of Glasgow Coma Scale (GCS) score unless periods of hypoglycemia (brain requires glucose and cannot store it). Immunosuppression and increased cerebral edema are not complications of insulin administration or strict glycemic control. Which of the following is NOT a true statement regarding cerebral palsy (CP)? A. CP is contagious. B. CP is not caused by a genetic abnormality or hereditary. C. CP is a chronic neurological disorder without a cure. D. CP is not always associated with mental impairment. - CORRECT ANSWER A CP is not contagious. It is chronic without a known cure. It is not related to a genetic abnormality and cannot be passed along generation to generation. It can be associated with mental impairment but not always. Which of the following is considered the single most important risk factor for a stroke? A. Hypertension B. Sedentary lifestyle C. Male gender D. Smoking - CORRECT ANSWER A Rationale: Hypertension is considered the single most important risk factor of both ischemic and hemorrhagic strokes. Sedentary lifestyle contributes to obesity and other known risk factors of stroke but is not the single most important risk factor. Male gender is a higher risk of most strokes than female, but both are at risk for strokes. Smoking is the most preventable risk for a stroke. Which of the following is the surgical management used to manage the symptoms of normal-pressure hydrocephalus? A. Skull base surgery B. Long-term intracranial pressure monitor C. Ventriculoperitoneal shunt D. Vagal nerve resection - CORRECT ANSWER C Rationale: A ventriculoperitoneal (VP) shunt may be placed to manage the symptoms of normal-pressure hydrocephalus (NPH) including patient's gait and urinary continence. Base skull surgeries and vagal nerve resections are not surgical procedures used to manage NPH. Intracranial pressure (ICP) monitors are not placed for long term or chronic use. A traumatic brain-injured patient in the ICU has an intracranial pressure (ICP) monitor and is noted to have the following: blood pressure = 140/60 mmHg, MAP = 80 mmHg, and ICP = 15 mmHg. Which of the following is the correct calculated cerebral perfusion pressure? A. 95 mmHg B. 125 mmHg C. 65 mmHg D. 75 mmHg - CORRECT ANSWER C Rationale: Cerebral perfusion pressures (CPPs) are calculated by subtracting the intracranial pressure (ICP) from the mean arterial pressure (MAP). So, MAP - ICP = CPP. This patient's MAP = 80 and ICP = 15. The CPP is 65 mmHg. Which of the following primary tumor locations most commonly metastasizes to the brain? A. Gastrointestinal tract B. Pancreas C. Lung D. Kidney - CORRECT ANSWER C Rationale: Tumors arising from the lungs commonly metastasize to the brain. Kidney and gastrointestinal tract tumors can also metastasize to the brain but not as commonly as lung. Pancreas is not as well known to metastasize to brain tissue. Which of the following presentations would most commonly be associated with autonomic seizures? A. Experiences of déjà vu B. Auditory hallucinations C. Feeling of being flushed and piloerection D. Repetitive movements - CORRECT ANSWER C Rationale: Autonomic seizures are commonly classified as simple partial or focal seizures with maintenance of awareness. Symptoms include feelings of being flush, piloerection (hair on the arms standing on end), pallor, and sweating. Auditory hallucinations and experiences of déjà vu occur in simple partial (focal) seizures but are commonly called somatosensory or psychic, respectively. Repetitive movements are called automatisms and are commonly found in complex partial seizures. Which of the following goals for blood pressure management is recommended for both primary and secondary prevention in a nondiabetic person? A. Maintain systolic blood pressure (SBP) <160 mmHg and diastolic <100 mmHg B. Do not treat unless SBP >220 mmHg or diastolic >120 mmHg C. Manage BP within a normal pressure of 110/80 mmHg D. Maintain SBP <140 mmHg and diastolic <90 mmHg - CORRECT ANSWER D Rationale: The recommendation by the American Heart Association/American Stroke Association (AHA/ASA) is to initiate blood pressure (BP) therapy with antihypertensive agents for a systolic BP > 140 mmHg and diastolic > 90 mmHg. There are no studies to support maintaining the BP less than 140/90 in nondiabetic patients. Not treating systolic BP unless greater than 220 mmHg and diastolic greater than 120 mmHg is only recommended in an acute stroke patient not eligible for thrombolytic therapy. It is not recommended for primary or secondary stroke prevention. What is a grade III astrocytoma called? A. Glioblastoma B. Neurofibromatosis C. Anaplastic D. Neuroblastoma - CORRECT ANSWER C Rationale: An anaplastic astrocytoma is a grade III astrocytoma. A glioblastoma is a grade IV astrocytoma. Neurofibromatosis is a familial tumor syndrome. Neuroblastoma is a solid tumor occurring on a peripheral nerve, commonly involving the sympathetic nervous system. Which of the following reflexes require the cervical spine to be cleared of injury before being tested? A. Bulbocavernosus reflex B. Babinski reflex C. Oculocephalic reflexes D. Oculovestibular reflexes - CORRECT ANSWER C Rationale: Moving the head side to side to assess for eye movement is performed to identify the presence of the oculocephalic reflex. Cervical spine should be cleared of injury prior to performing this reflex evaluation. Bulbocavernous reflex is used to evaluate spinal cord-injured patient and does not involve manipulating the neck. Running an object up the bottom of the foot tests Babinski reflex, assessing the movement of the toes. Oculovestibular reflex involves irrigation of iced cold water into the ear. This does not involve movement of the neck, and cervical injury does not need to be cleared before assessment. Both oculocephalic and oculovestibular reflexes are used to evaluate comatose patients for brain death. Assessment of oculovestibular reflex is safer in comatose patient. Ergotamine is used to manage benign headaches. Which of the following is a complication of this drug therapy? A. Liver toxicity B. Acute myocardial infarction C. Increased intracranial pressure D. Acute kidney injury - CORRECT ANSWER B Rationale: Ergotamine causes vasoconstriction in the cerebral circulation but also causes vasoconstriction in the coronary arteries. This coronary vasoconstriction may increase the risk of acute myocardial infarction. Liver toxicity, increased intracranial pressure, and acute kidney injury are not common complications found with the administration of ergotamine. An infant is born with a hypoplasia of the cerebellum. Which of the following is the correct classification of the Chiari malformation? A. Type I B. Type II C. Type III D. Type IV - CORRECT ANSWER D Rationale: The type IV Chiari malformation refers to a hypoplasia, which is an incomplete development of the cerebellum, or an aplasia, which is a lack of development of a portion of the cerebellum. These do not involve an actual herniation like the Chiari malformations type I and type II. Which of the following is NOT a route of exposure or cause of Creutzfeldt-Jakob disease? A. Sporadic B. Hereditary C. Exposure of infected person's tissue D. Casual contact - CORRECT ANSWER D Rationale: Creutzfeldt-Jakob disease (CJD) can be acquired through sporadic alteration of protein, hereditary, or exposure of the infected person's tissue. Casual contact is not a route of exposure to CJD. Which of the following would be considered a preventive intervention for cerebral palsy? A. Genetic counseling B. Administration of rubella vaccination prior to pregnancy C. Avoiding use of alcohol during pregnancy D. Participating in an exercise program during the pregnancy - CORRECT ANSWER B Rationale: One of the known causes for cerebral palsy (CP) is maternal infection, such as Rubella (German measles), during pregnancy. Prevention of CP includes vaccinations to prevent maternal infections. Genetic counseling is not considered preventive in CP. Avoiding alcohol and participating in exercise programs during pregnancy are always recommended for the health of the newborn but do not necessarily prevent CP to the degree of preventing maternal infections. Posttraumatic injury can involve cranial nerve (CN) injuries. Which of the following CNs is most commonly damaged with traumatic brain injury? A. CN I (olfactory nerve) B. CN V (trigeminal nerve) C. CN VII (facial nerve) D. CN VIII (acoustic nerve) - CORRECT ANSWER A Rationale: CN I, the olfactory cranial nerve, is commonly damaged due to shearing of the olfactory fibers at the cribriform plate during the trauma. This can result in loss of smell (amnosia) permanent, with some return and regeneration. CN V (trigeminal), CN VII (facial), and CN VIII (acoustic) are not commonly injured in traumatic brain injury (TBI). Which of the following should be stressed to the patient and family regarding best transportation to the hospital in case of a second stroke? A. EMS 9-1-1 B. Personal vehicle C. Taxi D. Next-door neighbor - CORRECT ANSWER A Rationale: Activating the EMS 9-1-1 system allows a more rapid transport to the hospital and allows for the prehospital identification of stroke symptoms, transport to designated stroke centers, and an early alert for the hospital to have the stroke team ready. Which of the following does NOT increase the risk of seizures following severe traumatic brain injury? A. Penetrating head trauma B. Decreased level of consciousness C. Depressed skull fracture D. Linear skull fracture - CORRECT ANSWER D Rationale: Linear skull fracture is associated with traumatic brain injury (TBI) but does not carry the high risk of seizures as in patients with penetrating head trauma, decreased level of consciousness, and depressed skull fractures. Other high risks for seizures include large parenchymal contusions and hematomas (epidural and subdural). What is a common complication of a pineal tumor? A. Hydrocephalus B. Visual field loss C. Hemiparesis D. Subarachnoid hemorrhage - CORRECT ANSWER A Rationale: Pineal tumors commonly cause the obstruction of cerebrospinal fluid, resulting in noncommunicating hydrocephalus. Visual field losses, hemiparesis, and subarachnoid hemorrhage are not commonly found in patients with pineal tumors. Which of the following would be considered a "simple" definition or explanation of what a stroke is? A. A stroke is an ischemic event causing cerebral injury. B. Stroke happens when there is a lack of blood flow to the brain due to an obstruction. C. A stroke is a permanent injury to the brain tissue and areas of ischemia, which may be reversible injury. D. Stroke occurs when the penumbra converts to an infarcted area. - CORRECT ANSWER B Rationale: Keep the definitions and explanations simple, at a fourth-grade level. Use common words and limit words with multiple syllables. Avoid medical jargon in definitions. However, you may develop a list of medical terms and definitions to assist the patient with medical jargon in the hospital. Cluster headaches may cause ipsilateral autonomic signs, which include all but which of the following? A. Nasal congestion B. Facial sweating C. Miosis D. Atrial fibrillation - CORRECT ANSWER D Rationale: Autonomic signs may be present with cluster headaches. These signs include nasal congestion, facial sweating, and miosis. Atrial fibrillation is not an autonomic sign. Which of the following is not considered a route of entry for bacterial meningitis? A. Direct B. Sinusitis C. Airborne, droplet spread D. Eating undercooked pork - CORRECT ANSWER D Rationale: Introduction of bacteria into the meninges can occur through the direct route such as a surgical site, sinusitis, and, in some type of meningitis, via an airborne or droplet route. Eating undercooked pork does not cause meningitis but can increase the risk of neurocysticercosis. At what age do most neonates develop seizures secondary to pyridoxine dependency? 1. Within the first 24 hours after birth 2. 24 to 48 hours after birth 3. 48 hours to 7 days after birth 4. 1 to 4 weeks after birth - CORRECT ANSWER 1. Within the first 24 hours after birth Pyridoxine dependency can be caused by glutamic acid decarboxylase activity impairment. This is a rare autosomal recessive condition. Seizures can start immediately after birth or later. Select the most common sleep disorder among the choices: 1. Obstructive sleep apnea 2. Narcolepsy 3. Periodic limb movement disorder 4. Delayed sleep phase syndrome - CORRECT ANSWER 1. Obstructive sleep apnea *Obstructive sleep apnea may affect up to ten to 15 percent of the population and is expected to increase as obesity increases. *Periodic limb movement disorder involves restless leg symptoms at night and affects one to five percent of the young and middle-aged but up to 20 percent of the elderly. *Narcolepsy only affects one in 4000 *In delayed sleep phase syndrome, the patient's circadian rhythm is delayed. It is most common in adolescents and young adults. A patient with multiple sclerosis had a urinary accident at night because he did not get to the bathroom in time. A bedside commode is suggested and immediately rejected. What could be the next step? 1. Ask the patient to take some time to think about the decision. 2. Provide a temporary commode. 3. Review the options and the consequence of each. 4. Drop the subject but include the exchanged in the progress note - CORRECT ANSWER 3. Review the options and the consequence of each. *Patients often have difficulty accepting change, especially when it involves admitting decline of skills or changes to the home. *When this occurs, the first step is to discuss the situation. *If the patient is still resistant, the other options are appropriate. Patients with spina bifida need special skin care. Which of the following would not be appropriate? 1. Patient and caregiver education for regular skin exam. 2. Frequent position changes 3. Avoidance of tight cloths 4. Deep and thick padding - CORRECT ANSWER 4. Deep and thick padding *Deep and thick padding can increase skin pressure. *There should only be enough padding for comfort. Which of the following is least likely to have elevated protein in the cerebrospinal fluid? 1. Guillain-Barre syndrome (GBS) 2. Chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) 3. Multifocal motor neuropathy (MMN) 4. Multiple sclerosis (MS) - CORRECT ANSWER 3. Multifocal motor neuropathy (MMN) *The CSF protein is multifocal motor neuropathy (MMN) can be normal or minimally elevated to <100 mg/dL. *In Chronic inflammaotry demyelinating polyradiculoneuropathy (CIDP), the CSF protein is elevated in 80 percent of patients with values from 50 to 200 mg/dL but often much higher *CSF protein is often >400 mg/dL in Guillain-Barre syndrome (GBS). *Multiple sclerosis (MS) can show CSF protein levels that are moderately elevated. Which of the following has been associated with cases of progressive multifocal leukoencephalopathy? 1. Rituximab 2. Natalizumab 3. Abciximab 4. Infliximab - CORRECT ANSWER 2 - Natalizumab *Natalizumab was initially related in 2004 for MS and was found to cause PML in patients when combined with other medications. *It was rerelated in 2006 with a strict program to treat MS and Chrohn disease as its benefits outweigh the risks. *Efalizumab was available in the market to treat psoriasis before June of 2009 but was withdrawn as of June 2009 because of potential risk to develop progressive multifocal leukoencephalopathy. Which of the following is the most common cause of a seizure in a full term infant less that 12 hours of age? 1. Sepsis 2. Inborn errors of metabolism 3. Hypoxemic encephalopathy 4. Intraventricular bleed - CORRECT ANSWER 3. Hypoxemic encephalopathy *The most common causes, in order, of neonatal seizures in the first 12 hours are hypoxic/ischemic encephalopthy, sepsis, meningitis, and subarachnoid hemorrhage Which classification of anoxic encephalopathy is associated with mostly theta wave? 1. Grade I 2. Grade II 3. Grade III 4. Grade IV - CORRECT ANSWER 2 - Grade II *Grade I of anoxic encephalopathy consists of mostly alpha waves. *Grade II of anoxic encephalopathy consists of mostly theta waves. *Grade III of anoxic encephalopathy consists of slow delta waves. *Grade IV of anoxic encephalopathy consists of low amplitude delta waves. A caregiver is approached by a colleague in the hall. The colleague wants to know how a hospitalized friend is doing and if his tests were improving. Which of the following is most appropriate? 1. Reassure the colleague that you are providing the best care possible. 2. Fill in the friend about the patient's condition 3. Decline to discuss the patient and encourage the colleague to visit him or her 4. report the colleague for violation of HIPAA - CORRECT ANSWER 3 - Decline to discuss the patient and encourage the colleague to visit him or her *Sharing any information about the patient is a violation of HIPPA *While asking the question is not appropriate, it is not a HIPPA violation *The best response is to encourage the colleague to visit the patient who can share as they see fit An obese patient needs to be transferred and the provider is not sure he can do it alone. What is the best solution? 1. Do not transfer the patient 2. Obtain help 3. Have a stronger provider do the transfer 4. Bend the knees, use a wide base of support, and keep the spine neutral - CORRECT ANSWER 2. Obtain help *It often takes 2 or more people to transfer morbidly obese patients *Sometimes the only option is a hydraulic lift *Trying to do so, even using proper body mechanics, can result in injury to the patient and/or the provider. Asking someone else to do the task is not professional Which of the following choices is not true of neuroblastoms? 1. They are masses which originate from the parasympathetic chain 2. They can present with an abdominal mass 3. Metastases to the lungs can occur with treatment is delayed 4. They can be difficult to differentiate from Wilms tumor on examination - CORRECT ANSWER 1. They are masses which originate from the parasympathetic chain *Neuroblastoms are tumors of the sympathetic chain and thus are comming in the adrenal gland and in other chromaffin cells. *These tumors are rare and can be difficult to differentiate from Wilms tumor on physical exam. When treatment is delayed, neuroblastomas can spread to the liver and lung How can you determine the vertebral level of a thoracic cord compression on a 24 cm field of view sagittal sequence? 1. Use the xiphoid process as a landmark. It is at the ninth thoracic level 2. Use the sternal notch as a landmark. It is at the T4-5 level 3. Take a single view lateral T-Spine radiograph. A vertebral collapse sufficient to cause cord compression should be evident. 4. Use the localizer's large field of view and count down from C2 - CORRECT ANSWER 4 Use the localizer's large field of view and count down from C2 *Although it is true that the xiphoid is typically at the T9 level and the sternal notch is typically at the T4-5 level, the best and most accurate method is to use the localizer's large field of view and count down from C2. *Using this technique also allows detection of fusion and other congenital anomalies that might lead to level numbering confusions at surgery. What percentage of seizures are caused by Lennox-Gastaut syndrome? 1. 57 2. 20 3. 13 4. 2 - CORRECT ANSWER 4 - 2 *Lennox-Gastaut syndrome is associated with about 2 percent of seizures. *It is also called childhood epileptic encephalopathy and has a poor prognosis with up to 75 percent of patients having mental retardation and treatment-resistant seizures What is the correct muscle strength grading in a patient with normal muscle movement? 1. 0 2. 1 3. 3 4. 5 - CORRECT ANSWER 4 - 5 *No muscle movement is a grade zero *Grade 3 motor strength is movement against only gravity. *Normal motor strength is grade 5 Select the condition that is not progressive myoclonic epilepsy? 1. Type I sialidosis 2. Neuronal ceroid lipofuscinosis 3. Juvenile myoclonic epilepsy 4. Myclonic epilepsy with ragged-red fibers - CORRECT ANSWER 3 Juvenile myoclonic epilepsy *Progressive myloclonic epilepsies are rare conditions that can show myoclonic or tonic clonic seizures *Some patients show progressive decline to death in early childhood while others show only mild neurologic impairment. *Other conditions that are considered progressive myoclonic epilepsy include Unverricht-Lundborg disease, and Lafora disease. Juvenile myoclonic epilepsy usually has onset a puberty. It is characterized by myoclonic jerks which often occur in the early morning hours. Patients with juvenile myoclonic epilepsy can also have absence-type seizures as well as generalized tonic-clonic seizures. [Show More]
Last updated: 8 months ago
Preview 1 out of 84 pages
Instant download
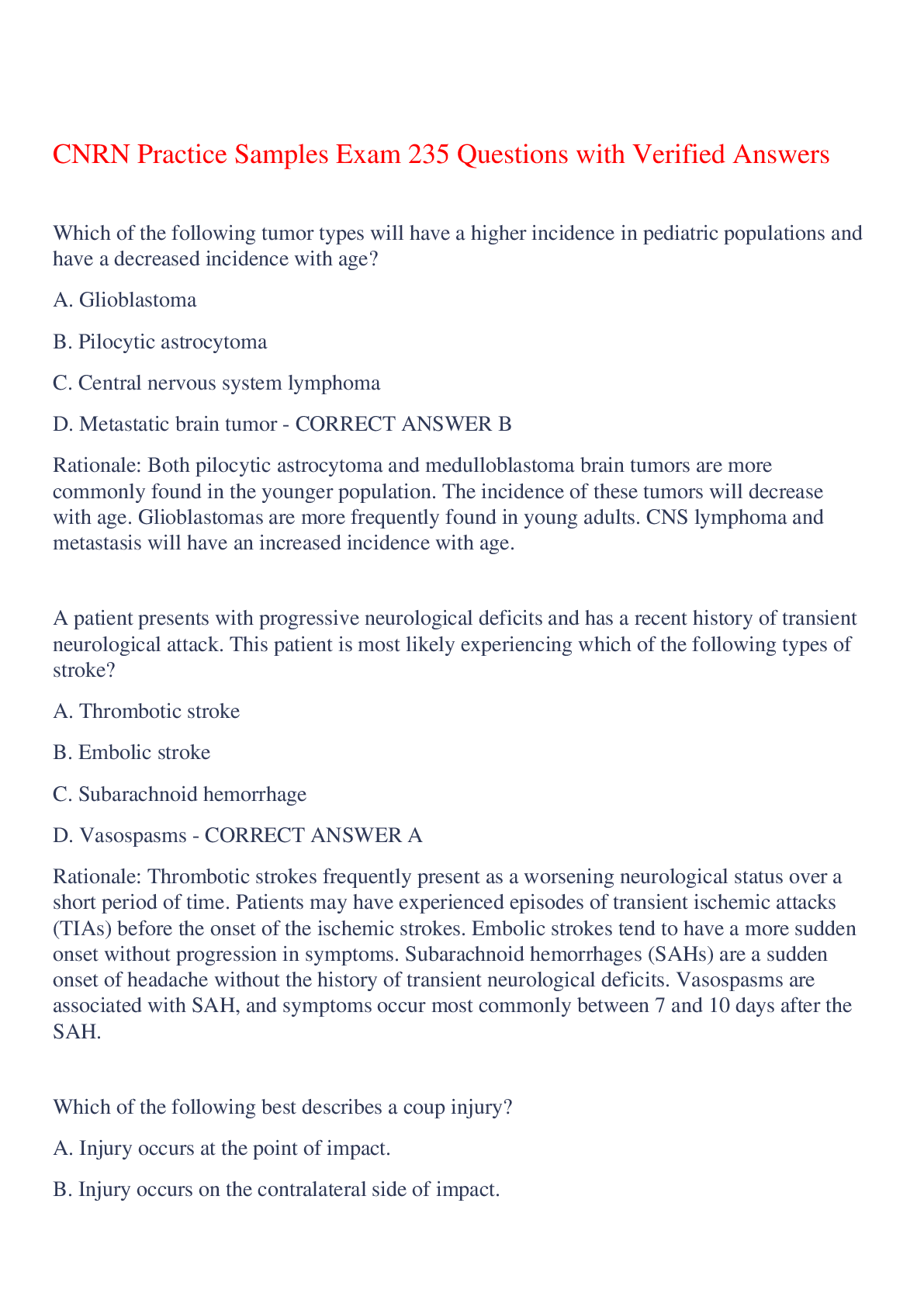
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 24, 2023
Number of pages
84
Written in
Additional information
This document has been written for:
Uploaded
Oct 24, 2023
Downloads
0
Views
38