*NURSING > STUDY GUIDE > Chamberlain College of Nursing - NR 602 MIDTERM study guide. Latest 2020/2021 (All)
Chamberlain College of Nursing - NR 602 MIDTERM study guide. Latest 2020/2021
Document Content and Description Below
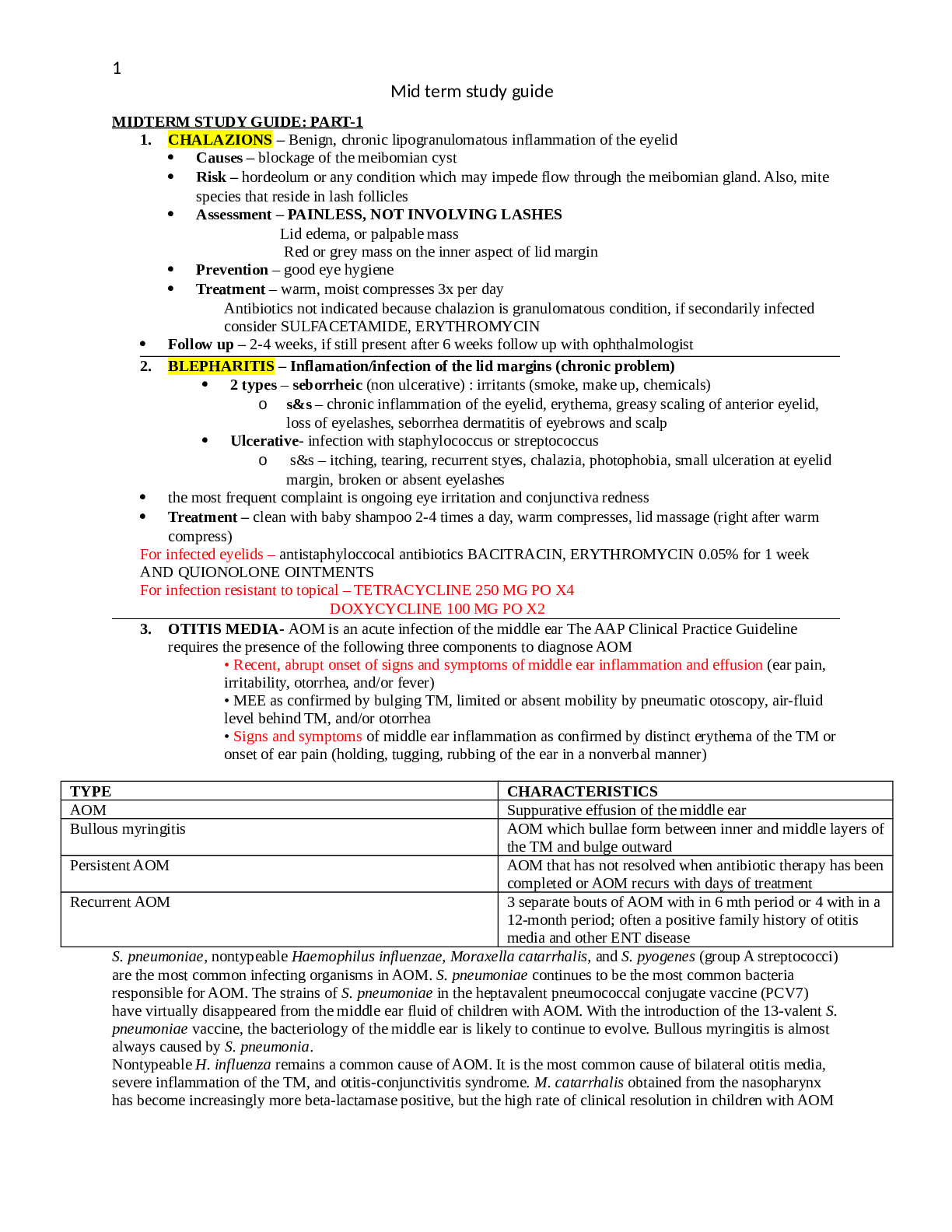
Mid term study guide 1 MIDTERM STUDY GUIDE: PART-1 1. CHALAZIONS – Benign, chronic lipogranulomatous inflammation of the eyelid Causes – blockage of the meibomian cyst Risk – hordeol... um or any condition which may impede flow through the meibomian gland. Also, mite species that reside in lash follicles Assessment – PAINLESS, NOT INVOLVING LASHES Lid edema, or palpable mass Red or grey mass on the inner aspect of lid margin Prevention – good eye hygiene Treatment – warm, moist compresses 3x per day Antibiotics not indicated because chalazion is granulomatous condition, if secondarily infected consider SULFACETAMIDE, ERYTHROMYCIN Follow up – 2-4 weeks, if still present after 6 weeks follow up with ophthalmologist 2. BLEPHARITIS – Inflamation/infection of the lid margins (chronic problem) 2 types – seborrheic (non ulcerative) : irritants (smoke, make up, chemicals) o s&s – chronic inflammation of the eyelid, erythema, greasy scaling of anterior eyelid, loss of eyelashes, seborrhea dermatitis of eyebrows and scalp Ulcerative- infection with staphylococcus or streptococcus o s&s – itching, tearing, recurrent styes, chalazia, photophobia, small ulceration at eyelid margin, broken or absent eyelashes the most frequent complaint is ongoing eye irritation and conjunctiva redness Treatment – clean with baby shampoo 2-4 times a day, warm compresses, lid massage (right after warm compress) For infected eyelids – antistaphyloccocal antibiotics BACITRACIN, ERYTHROMYCIN 0.05% for 1 week AND QUIONOLONE OINTMENTS For infection resistant to topical – TETRACYCLINE 250 MG PO X4 DOXYCYCLINE 100 MG PO X2 3. OTITIS MEDIA- AOM is an acute infection of the middle ear The AAP Clinical Practice Guideline requires the presence of the following three components to diagnose AOM • Recent, abrupt onset of signs and symptoms of middle ear inflammation and effusion (ear pain, irritability, otorrhea, and/or fever) • MEE as confirmed by bulging TM, limited or absent mobility by pneumatic otoscopy, air-fluid level behind TM, and/or otorrhea • Signs and symptoms of middle ear inflammation as confirmed by distinct erythema of the TM or onset of ear pain (holding, tugging, rubbing of the ear in a nonverbal manner) TYPE CHARACTERISTICS AOM Suppurative effusion of the middle ear Bullous myringitis AOM which bullae form between inner and middle layers of the TM and bulge outward Persistent AOM AOM that has not resolved when antibiotic therapy has been completed or AOM recurs with days of treatment Recurrent AOM 3 separate bouts of AOM with in 6 mth period or 4 with in a 12-month period; often a positive family history of otitis media and other ENT disease S. pneumoniae, nontypeable Haemophilus influenzae, Moraxella catarrhalis, and S. pyogenes (group A streptococci) are the most common infecting organisms in AOM. S. pneumoniae continues to be the most common bacteria responsible for AOM. The strains of S. pneumoniae in the heptavalent pneumococcal conjugate vaccine (PCV7) have virtually disappeared from the middle ear fluid of children with AOM. With the introduction of the 13-valent S. pneumoniae vaccine, the bacteriology of the middle ear is likely to continue to evolve. Bullous myringitis is almost always caused by S. pneumonia. Nontypeable H. influenza remains a common cause of AOM. It is the most common cause of bilateral otitis media, severe inflammation of the TM, and otitis-conjunctivitis syndrome. M. catarrhalis obtained from the nasopharynx has become increasingly more beta-lactamase positive, but the high rate of clinical resolution in children with AOM Mid term study guide 2 from M. catarrhalis makes amoxicillin a good choice for initial therapy. M. catarrhalis rarely causes invasive disease. S. pyogenes is responsible for AOM in older children, is responsible for more TM ruptures, and is more likely to cause mastoiditis. Although a virus is usually the initial causative factor in AOM, strict diagnostic criteria, careful specimen handling, and sensitive microbiologic techniques have shown that the majority of AOM is caused by bacteria or bacteria and virus together Clinical Findings History Rapid onset of signs and symptoms: • Ear pain with possible ear pulling in the infant; may interfere with activity and/or sleep • Irritability in an infant or toddler • Otorrhea • Fever Other key factors or symptoms: • Prematurity • Craniofacial anomalies or congenital syndromes associated with craniofacial anomalies • Exposure to risk factors • Disrupted sleep or inability to sleep • Lethargy, dizziness, tinnitus, and unsteady gait • Diarrhea and vomiting • Sudden hearing loss • Stuffy nose, rhinorrhea, and sneezing • Rare facial palsy and ataxia Physical Examination • Presence of MEE, confirmed by pneumatic otoscopy, tympanometry, or acoustic reflectometry, as evidenced by: • Bulging TM • Decreased translucency of TM • Absent or decreased mobility of the TM • Air-fluid level behind the TM • Otorrhea • Signs and symptoms of middle ear inflammation indicated by either: • Erythema of the TM (Amber is usually seen in otitis media with effusion [OME]; white or yellow may be seen in either AOM or OME or • Distinct otalgia that interferes with normal activity or sleep • In addition, the following TM findings may be present: • Increased vascularity with obscured or absent landmarks • Red, yellow, or purple TM (Redness alone should not be used to diagnose AOM, especially in a crying child.) • Thin-walled, sagging bullae filled with straw-colored fluid seen with bullous myringitis Diagnostic Studies Pneumatic otoscopy is the simplest and most efficient way to diagnose AOM. Tympanometry reflects effusion (type B pattern). Tympanocentesis to identify the infecting organism is helpful in the treatment of infants younger than 2 months old. In older infants and children, tympanocentesis is rarely done and is useful only if the patient is toxic or immunocompromised or in the presence of resistant infection or acute pain from bullous myringitis. If a tympanocentesis is warranted, refer the patient to an otolaryngologist for this procedure. Management Many changes have been made in the treatment of AOM because of the increasing rate of antibiotic-resistant bacteria related to the injudicious use of antibiotics. Ample evidence has been presented that symptom management may be all that is required in children with MEE without other symptoms of AOM Treatment guidelines are decided based on the child's age, illness severity, and the certainty of diagnosis. shows the recommendation for the diagnosis and subsequent treatment of AOM. 1. Pain management is the first principle of treatment. [Show More]
Last updated: 1 year ago
Preview 1 out of 48 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$14.00
Document information
Connected school, study & course
About the document
Uploaded On
Mar 01, 2021
Number of pages
48
Written in
Additional information
This document has been written for:
Uploaded
Mar 01, 2021
Downloads
0
Views
42