*NURSING > QUESTIONS & ANSWERS > NUR 4120Shock and Multiple Organ Dysfunction Syndrome. (All)
NUR 4120Shock and Multiple Organ Dysfunction Syndrome.
Document Content and Description Below
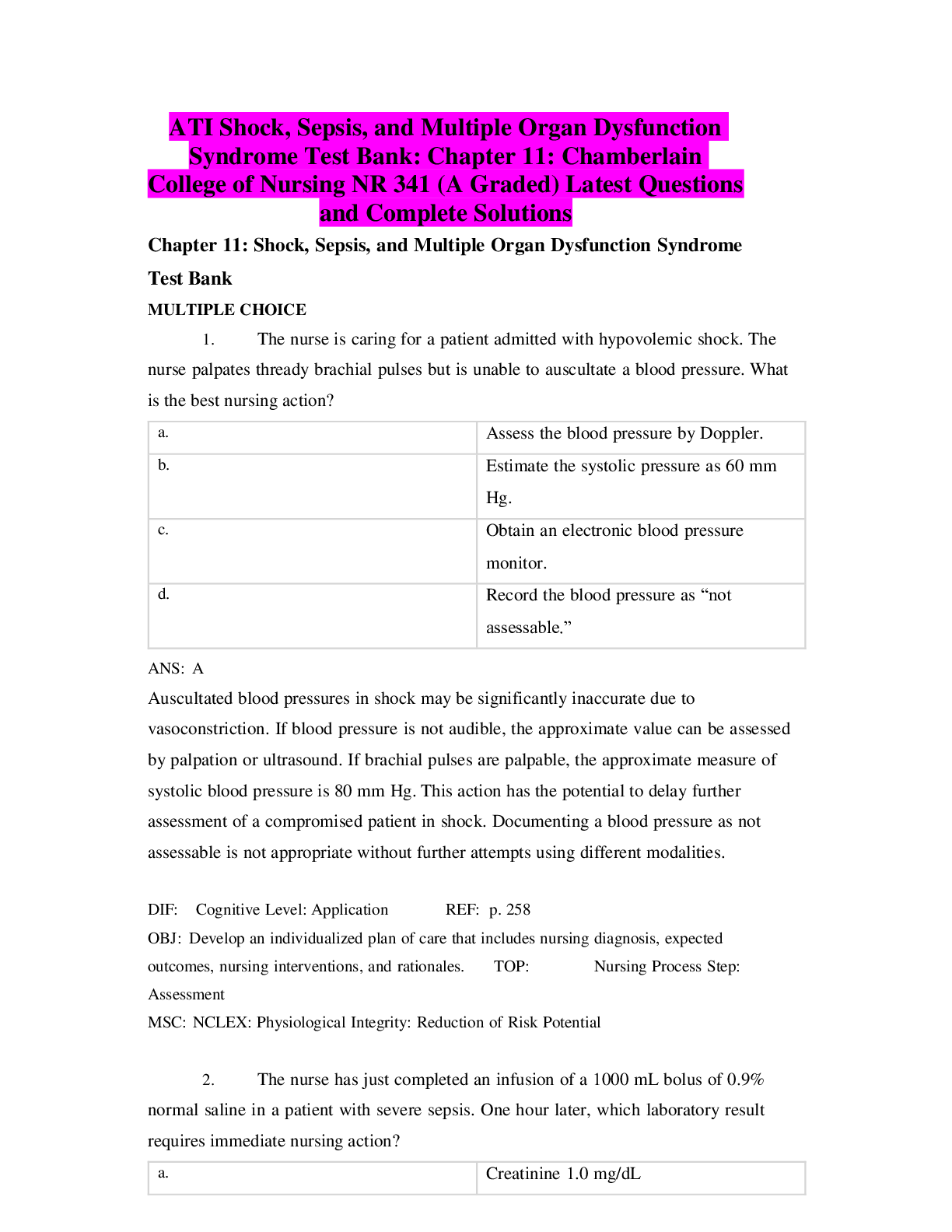
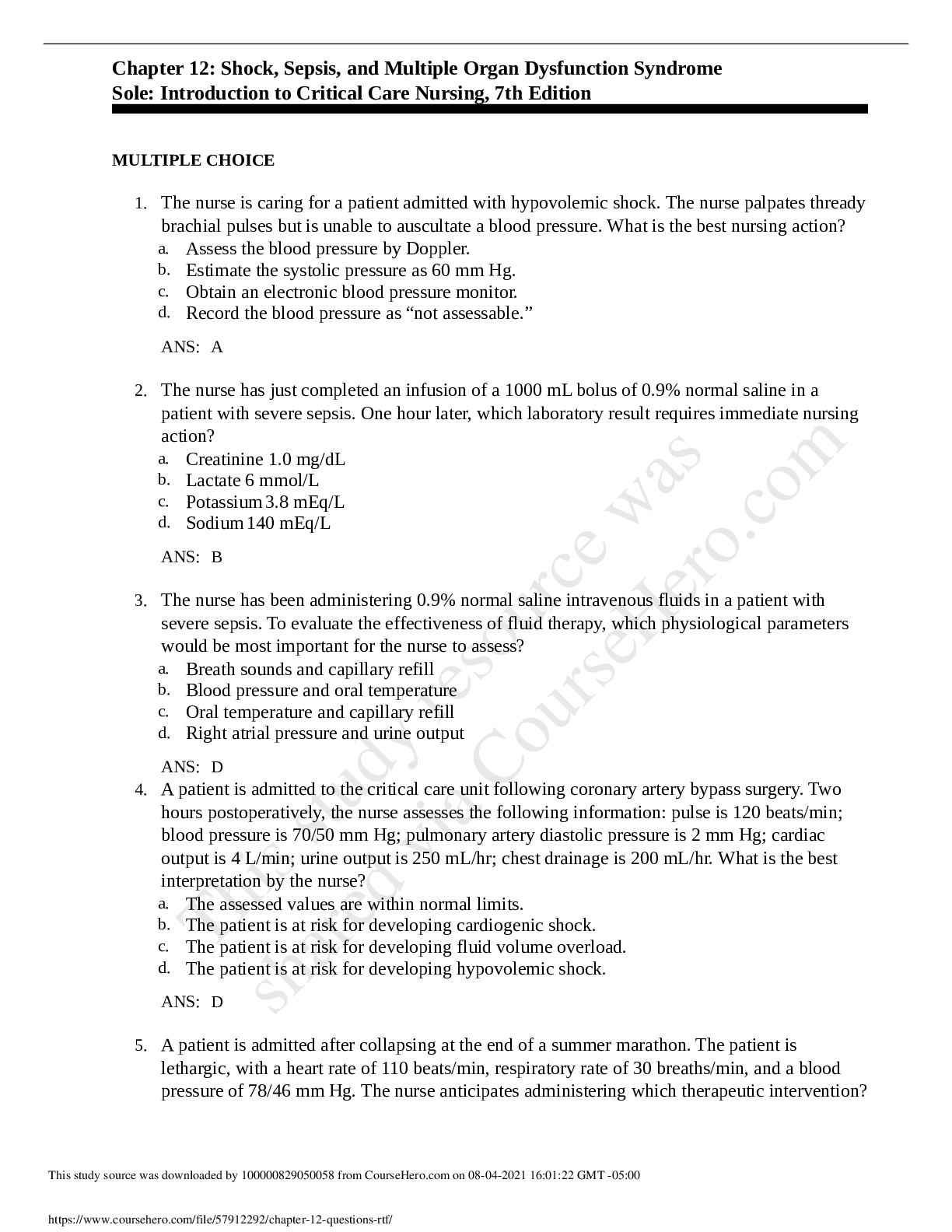
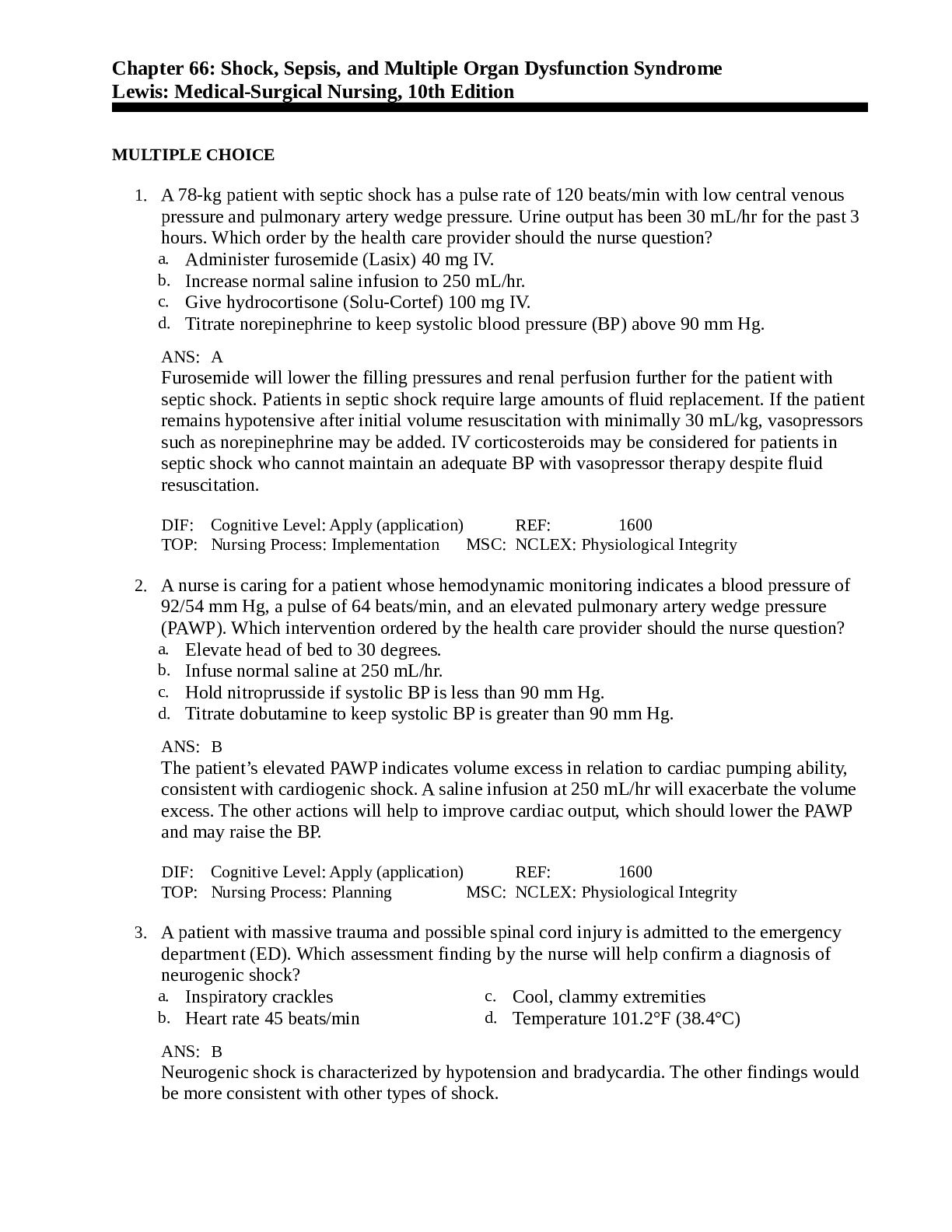
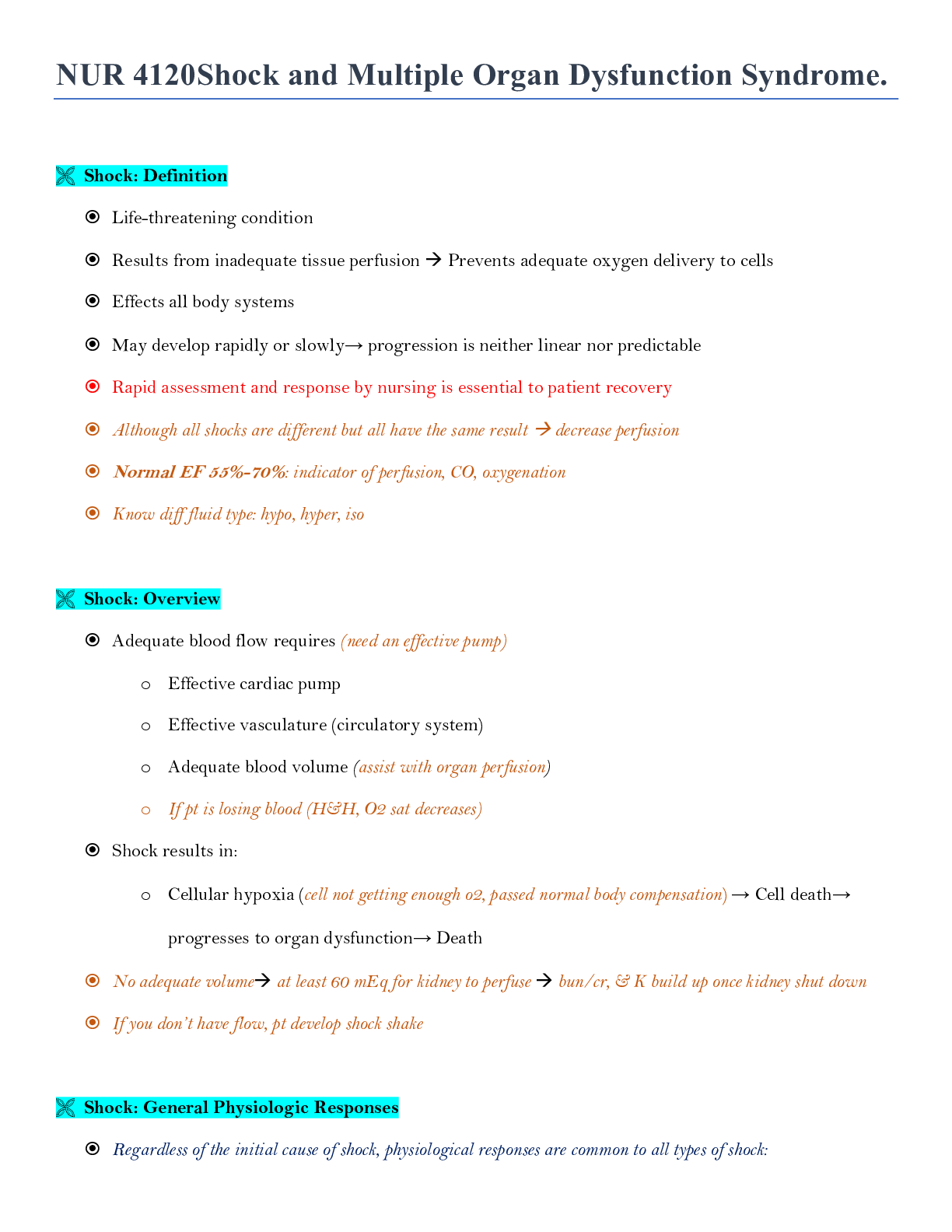
Medical Management of Septic Shock Identification and elimination of source of infection (goals are to id & tx within 3 hrs to increase pt outcome) Pan culture/Labs/Lactic acid (greater ... than 2)/ABG Remove infected lines/catheters then replace Fluid replacement through aggressive fluid resuscitation is key (monitor bp, CVP, fluid responsiveness w/ passive leg raise, u/o, serum lactate levels) Vasopressors (norepinephrine 1st line or dopamine to achieve MAP of >65; inotropic; PRBC to support O2 delivery; neuromuscular agent & sedation may be required to reduce metabolic demands & provide comfort; DVT plus SCD prophylactic, antacid [PPI]) Broad spectrum antibiotics; Change to appropriate antibiotics when cultures returned (do blood & urine culture prior; can take 24-36 hrs depend on labs) Nutritional Therapy (within 24-48 hrs in ICU to address hypermetabolic state; if not it will further impair pt’s resistance to infection enteral feeding if GI tract have good peristalsis) Nursing Management of Septic Shock Respiratory support Transfuse when Hgb < 7 g/dL Glucose control (< 180 mg/dL) DVT prophylaxis GI prophylaxis (antipeptic & protonic especially bc they on steroids) IV hydrocortisone Advanced planning If pt is hyperthermia: give acetaminophen or apply hypothermia blanket (avoid shivering) Patient & Family Support Anxiety Support of coping Patient, family education Communication End-of-life issues Grief processes Neurogenic Shock Pathophysiology Vasodilatation occurs as a result of a loss of balance between parasympathetic and sympathetic stimulation o Sympathetic stimulation: vascular smooth muscle constriction (in neurogenic state the SNS is not able to respond to body stressor) o Parasympathetic stimulation: vascular smooth muscle relaxation Parasympathetic stimulation is predominant Relative hypovolemia with adequate volume status Clinical Manifestations & Etiology (remember SNS is not able to function properly, so the s/s that will appear with neurogenic shock will be parasymptomatic signs) Causes bradycardia (slow HR), hypotension (low BP) & blood pooling Etiology o Spinal cord injury o Spinal anesthesia* o Nervous system damage o Depressant action of medications o Hypoglycemia/ lack of glc (insulin reaction) o Low bp, low HR, cyanosis, hypothermia, blank stare, Dry/warm skin Medical Management Restore sympathetic tone either by stabilization of a SCI or position pt properly Proper positioning Treat the cause! Pacemaker, atropine, vasopressor Nursing Management HOB up 30 degrees with epidural anesthesia Assess for DVT increase pooling of blood from vascular dilation (not able to feel anything if they have SCI daily check for lower extremity pain, redness, tenderness & warmth passive ROM of the immobile extremities help promote circulation early prevention includes SCD’s & antithrombotic agents [Lovenox]) Asses for signs/symptoms internal bleeding that could lead to hypovolemic shock Anaphylactic Shock Anaphylaxis Severe allergic reaction in patient who has already produced antibodies to an antigen Systemic antigen-antibody reaction o IgE mediated The antigen-antibodies reaction provokes mast cells to release potent vasoactive substance as histamine, bradykinin, inflammatory cytokines released o Widespread vasodilation and increased capillary permeability Common triggers o Food (peanuts) o Medication (ARB, ACE-I, ASA, NSAIDS, antibiotics, beta-blockers) o Insects (bee’s) o IV dye, iodine People who have been previous expose have worsened reaction to the 2 times, can occur in many year Clinical Manifestations 1. Acute onset of symptoms 2. Presence of two or more symptoms (resp compromise, reduce BP, GI distress & skin or mucosal tissues irritation) 3. Cardiovascular compromise from min (2-30 min) to hrs after exposure to antigen Headache, lightheaded N/V, acute abdominal pain or discomfort Pruritus, erythema, flushing & feeling of impending doom Laryngeal edema, bronchospasm Hypotension (due to trying to compensate) Cardiac dysrhythmia/arrest Characteristics of severe anaphylaxis usually include rapid onset of hypotension, neurologic compromise, resp distress & cardiac arrest Medical Management Remove the causative agent (such as d/c an antibiotic agent) Administering medications that restore vascular tone o IM Epinephrine (along with 50 mg IV of Benadryl to reverse histamine) o Albuterol (Proventil) may be given to reverse histamine-induced bronchospasm Emergency support Fluid management is critical, as massive fluid shifts can occur within min due to increase vascular permeability Medications (Reduce histamine) o Nebulizer treatments o Benadryl o Steroids Nursing Management Assess all patients for allergies or previous reactions to antigens (meds, blood product, food, contrast agent, latex) o Communicate existence of allergy to other team members (allergies to iodine or fish, previous contrast agent reaction) Prevent further exposure (bracelet) Observe for reactions while administering new medications (IV) Assess for reactions Be prepared for cardiac arrestperform CPR Multiple Organ Dysfunction Syndrome Altered organ function in acutely ill patients Requires medical intervention to support continued organ function Not always possible to predict Associated mortality rate as high as 75% ***High level antibiotic can increase BUN & Cr in pt w/o adequate fluid balance (whatever system pt have effected, know what doctor is on the case) Labs for liver issue: AST, ALT, albumin (s/s: jaundice, AMS, ascites) ***MODS mat be a complication of all form of shock but common in in pt w/ sepsis & result of inadequate tissues perfusion ***Organs failure usually begins in the lung & cardiovascular instability then liver, GI, renal, immunologic, & CNS follows Clinical Manifestations Hypotension Respiratory compromise (ALI or ARDS) requiring intubation & mechanical vent Hypermetabolic state o Hyperglycemia Lactic Acidosis o Hyper-lactic acidemia (excess lactic acid in the blood) Hepatic dysfunction elevated bilirubin & liver function test Renal dysfunction elevated cr & anuria Hematologic dysfunction: DIC, PT/INR, PTT Immunocompromise worsens Unstable cardiac system Neurologic compromised (unresponsive/coma) Systemic fulminant edema swelling everywhere electrolyte imbalance: d/r Medical & Nursing Management (Everything about MODS is about preventing it) Control the initiating event Promote adequate organ perfusion Provide nutritional support Nursing: supportive caremay be supportive end of life care Effective communication between nurse-patient and nurse-family Shock: Definition Life-threatening condition Results from inadequate tissue perfusion Prevents adequate oxygen delivery to cells Shock: Overview Adequate blood flow requires (need an effective pump) Shock: General Physiologic Responses Regardless of the initial cause of shock, physiological responses are common to all types of shock: Pathophysiology: Cellular Responses Cellular swelling occurs Pathophysiology: Cellular Responses Cellular changes that occur with shock: BP regulation requires adequate Pathophysiology: Coagulopathic Responses Pathophysiology: Inflammatory Responses 1. ) How is BP regulated? MAP= CO x PVR (peripheral vascular resistance) Blood Pressure Regulation: pressure Receptors Blood Pressure Regulation: RAA (kidney regulator, slowest system yet safest) 3 Stages of Shock Compensatory Stage of Shock SNS causes vasoconstriction, increased HR/increased heart contractility Inadequate tissue perfusion Progressive Stage of Shock Mechanisms that regulate BP can no longer compensate Progressive Stage of Shock Irreversible Stage of Shock (Refractory) At this point, organ damage so severe that patient does not respond to treatment, cannot survive (despite tx, BP remain low, resp system d/f prevent adequate oxygenation & ventilation despite mechanical vent support) o End-organ perfusion is decreased significantly o Organ damage is severe o Progresses to multiple organ dysfunction syndrome (MODS) Complete organ failure o Judgment that shock [Show More]
Last updated: 1 year ago
Preview 1 out of 27 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$9.00
Document information
Connected school, study & course
About the document
Uploaded On
Apr 22, 2020
Number of pages
27
Written in
Additional information
This document has been written for:
Uploaded
Apr 22, 2020
Downloads
0
Views
40

 Med Surg test Questions and Answers with Explanations, 100% Correct, Download to Score A.png)

 Correct Study Guide, Download to Score A.png)
, All Correct, Download to Score A.png)