*NURSING > SHADOW HEALTH > NR_509_Abdominal_Pain_Documentation - Electronic Health Record | Abdominal Pain Physical Assessment (All)
NR_509_Abdominal_Pain_Documentation - Electronic Health Record | Abdominal Pain Physical Assessment Assignment Results | Completed
Document Content and Description Below
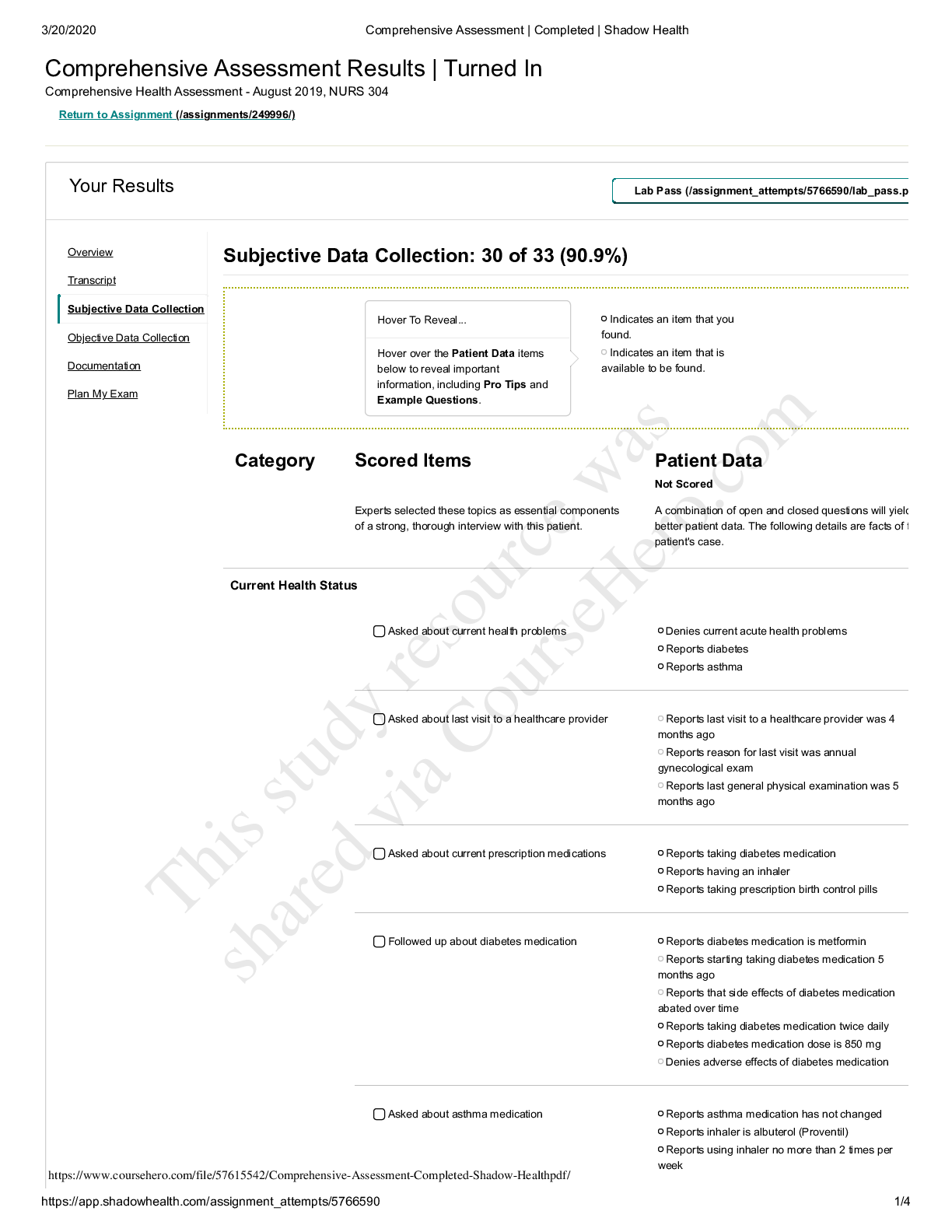
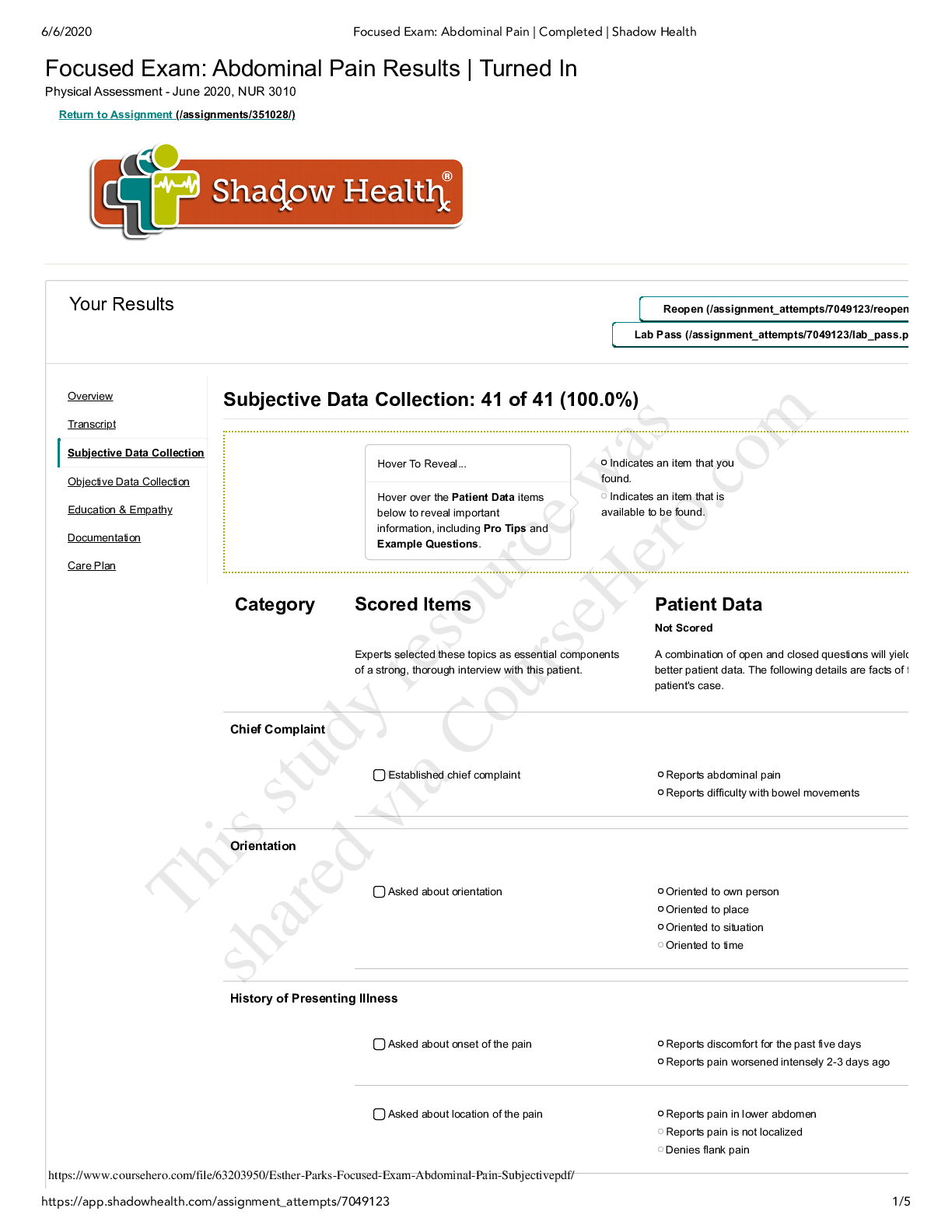
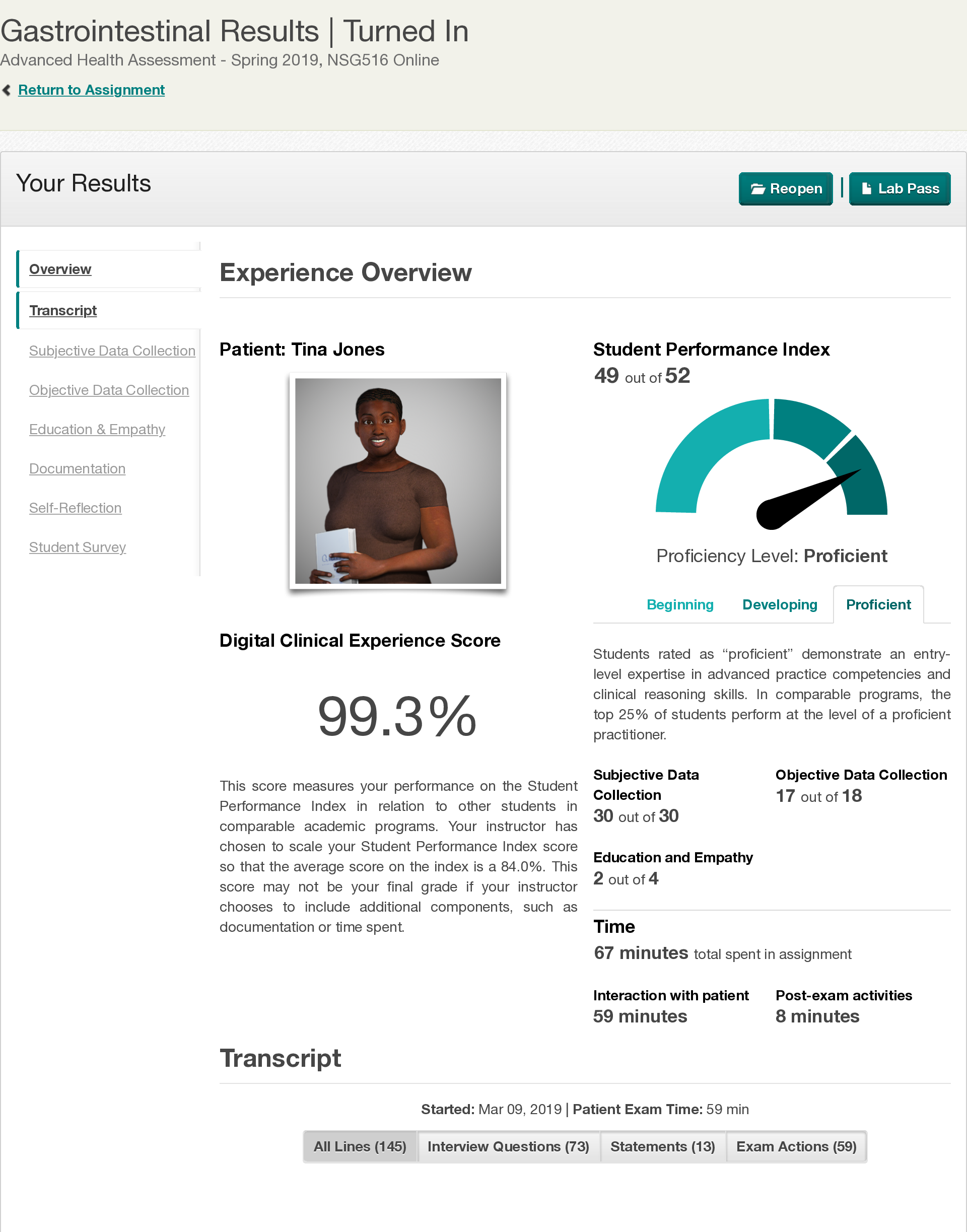
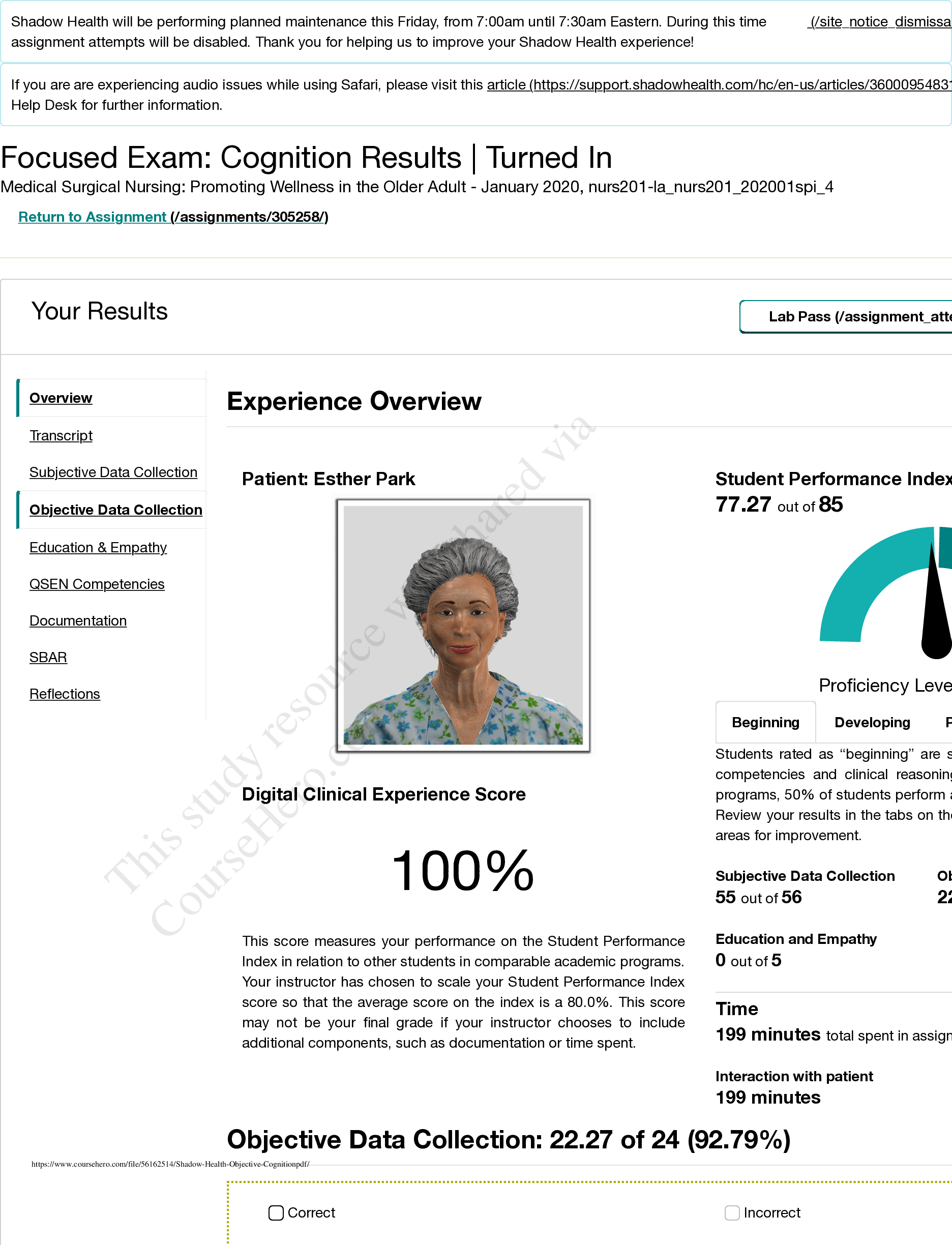
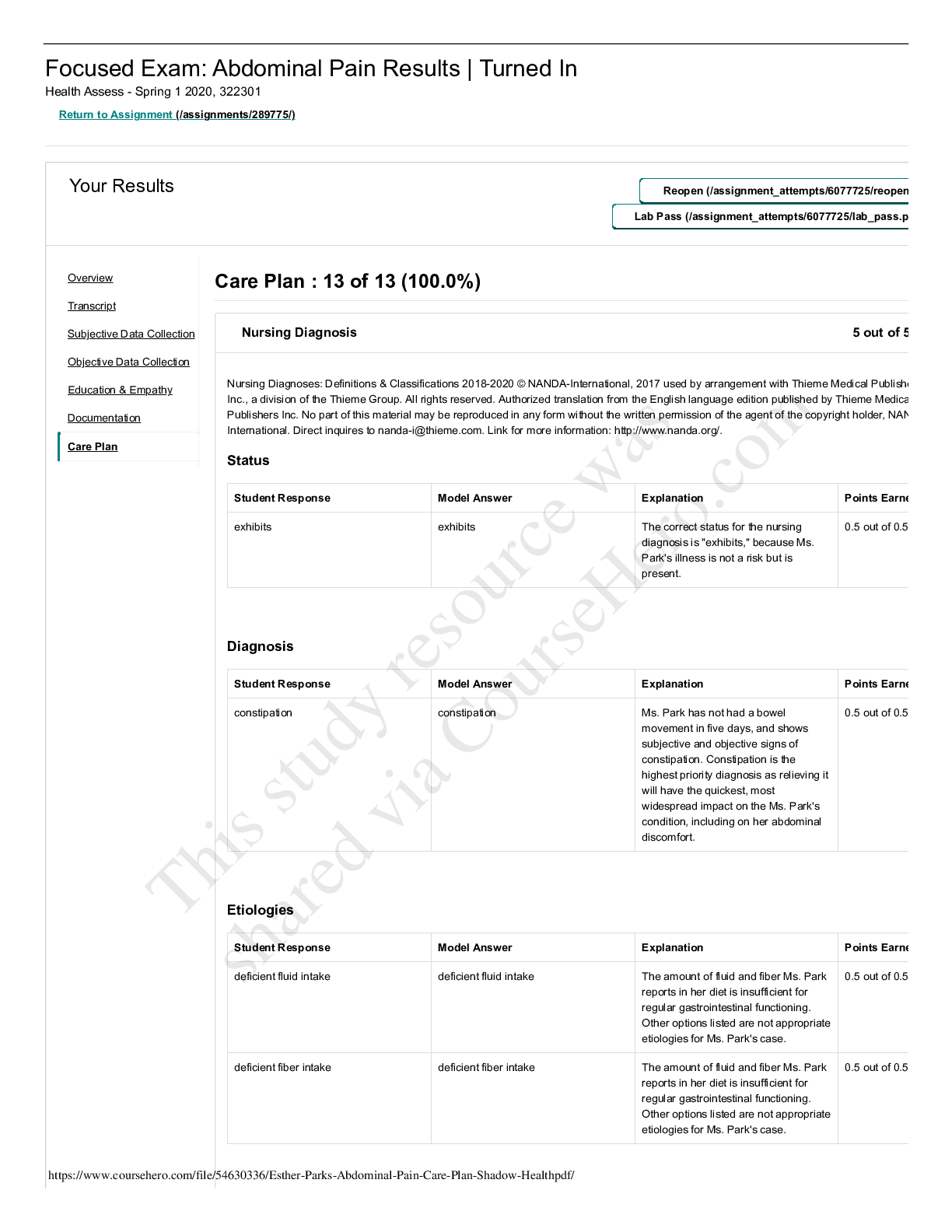
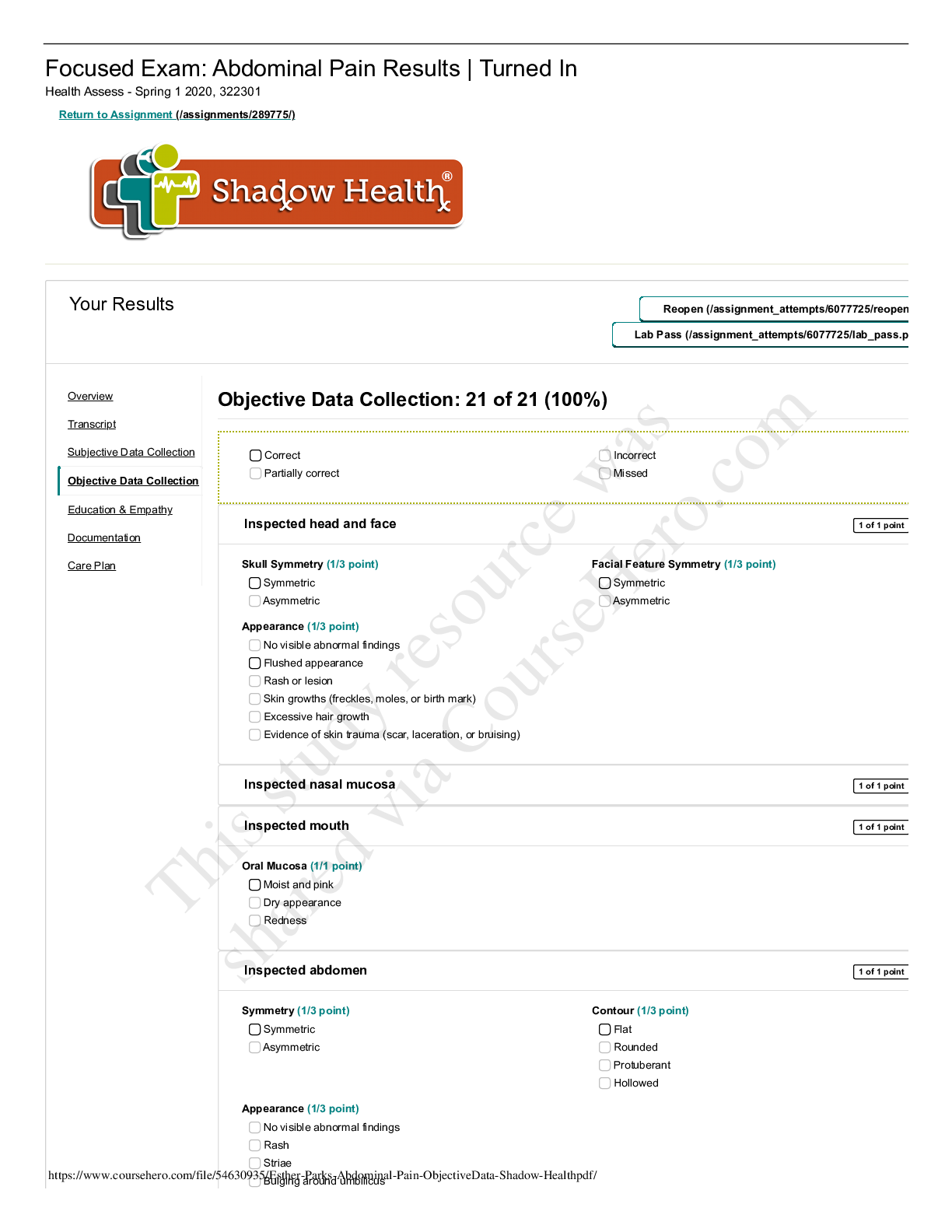
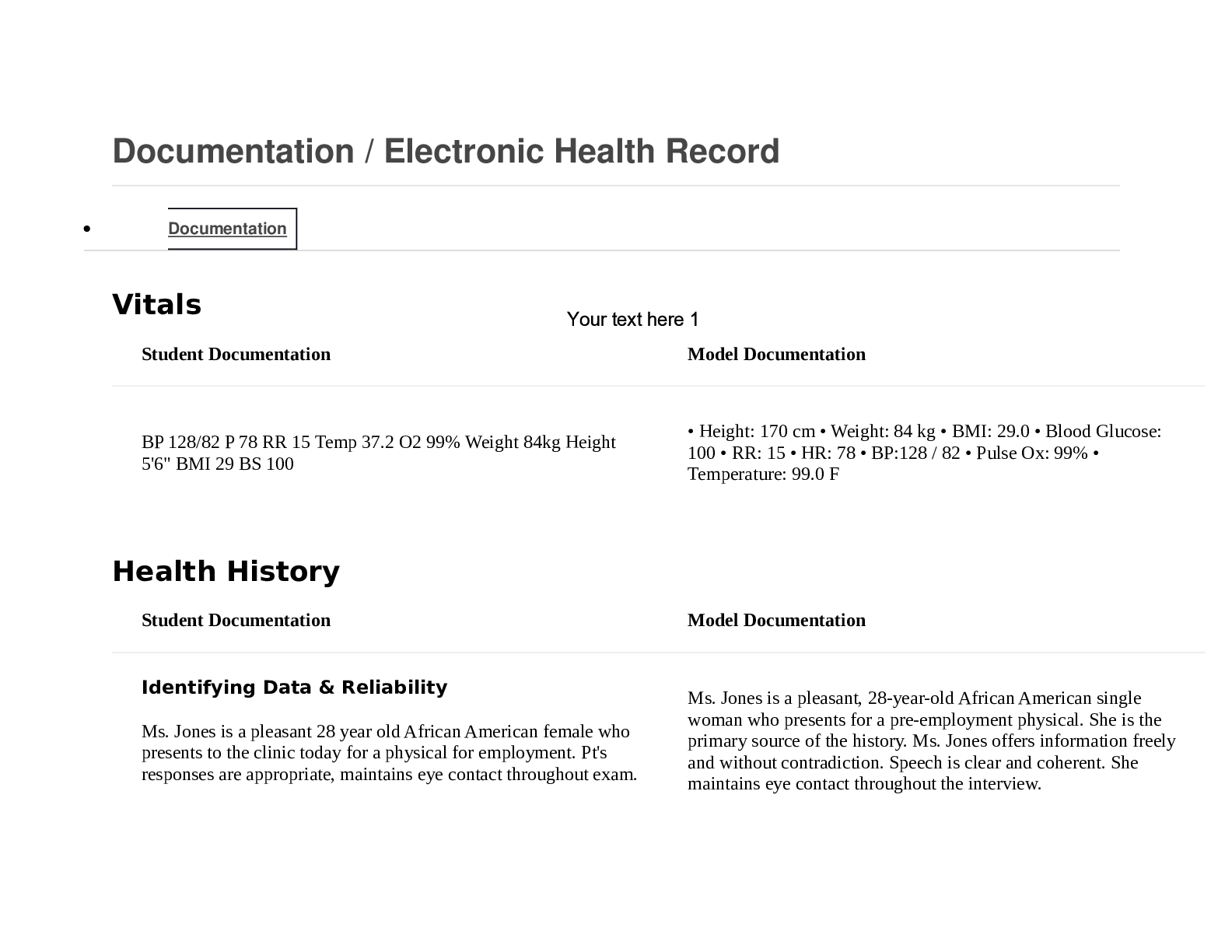
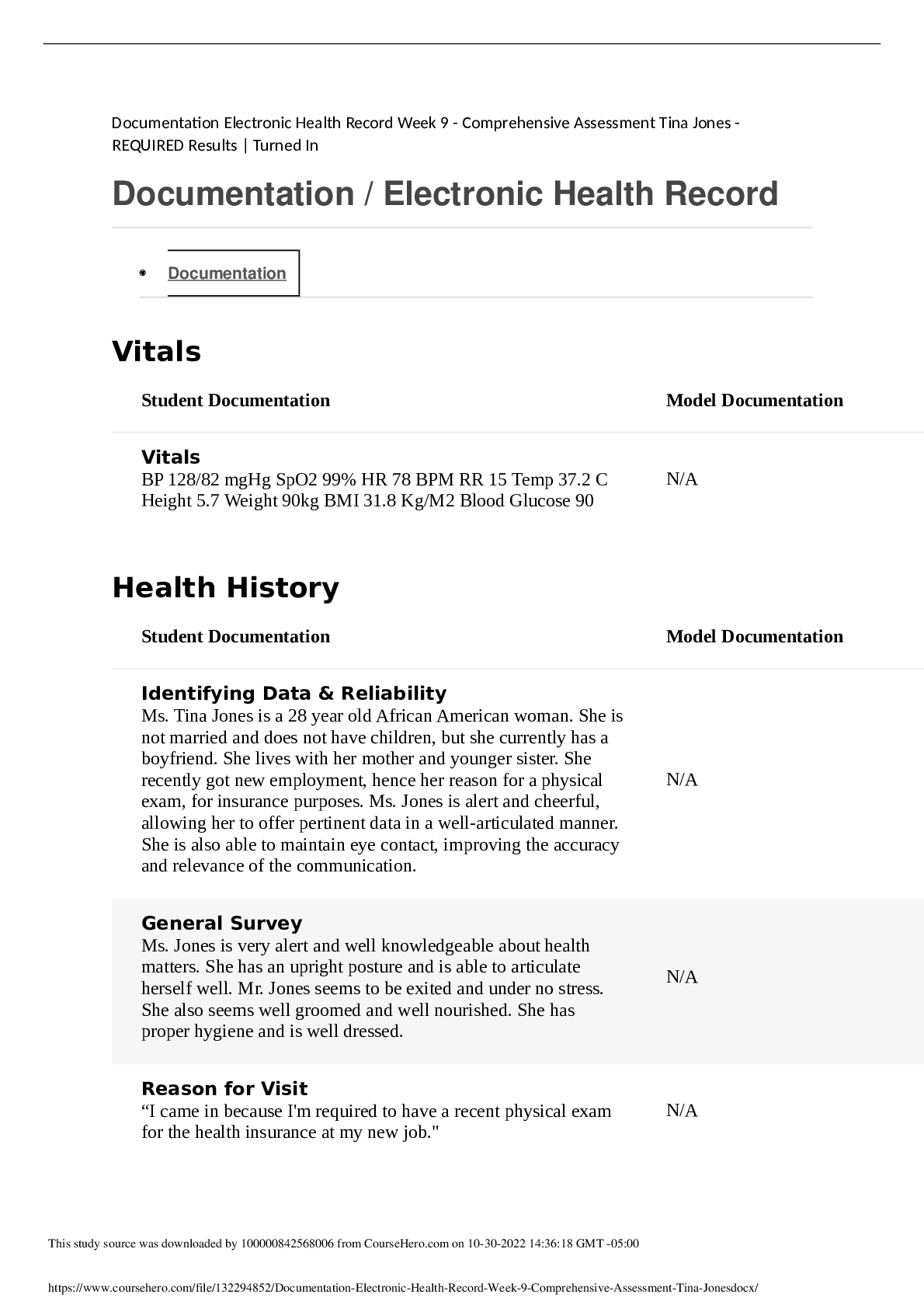
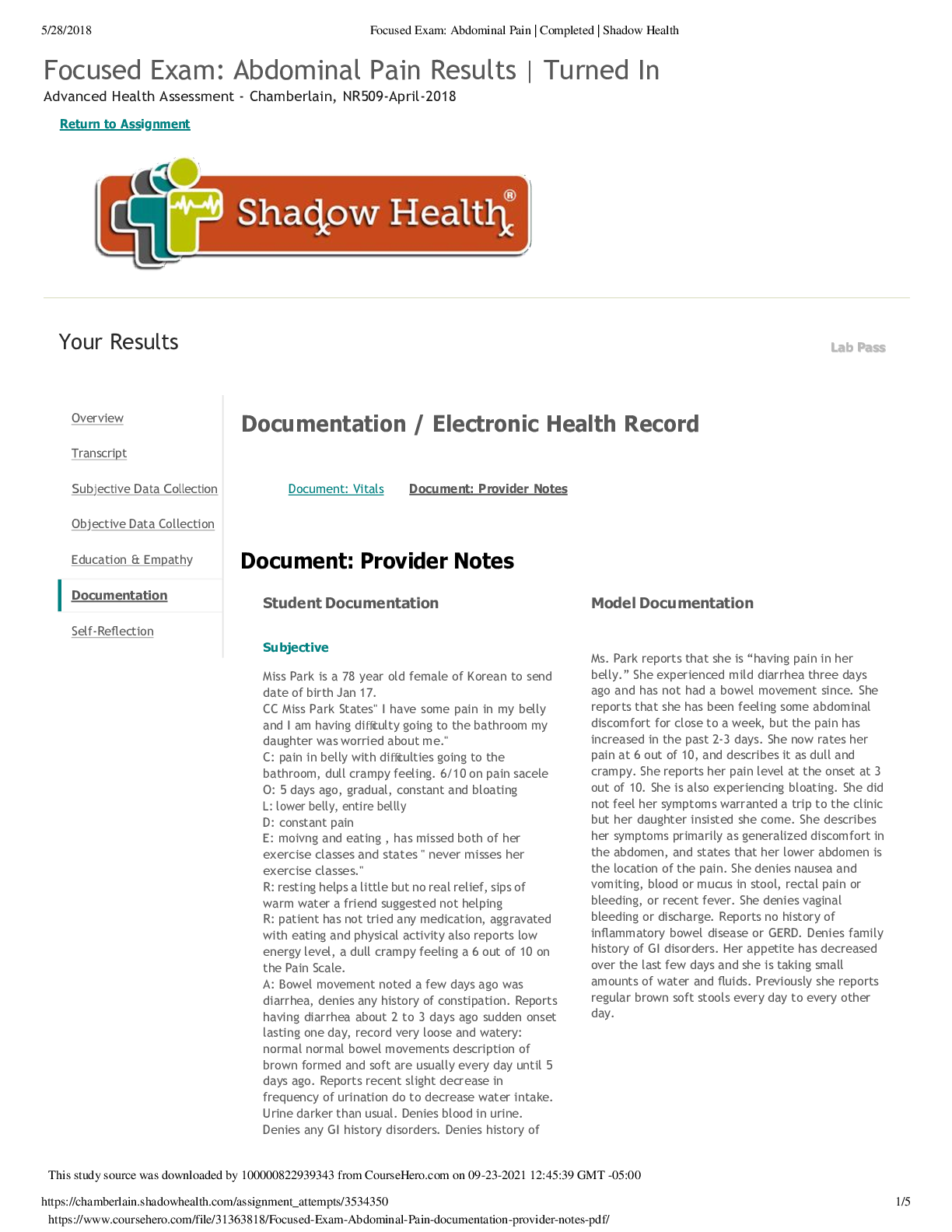
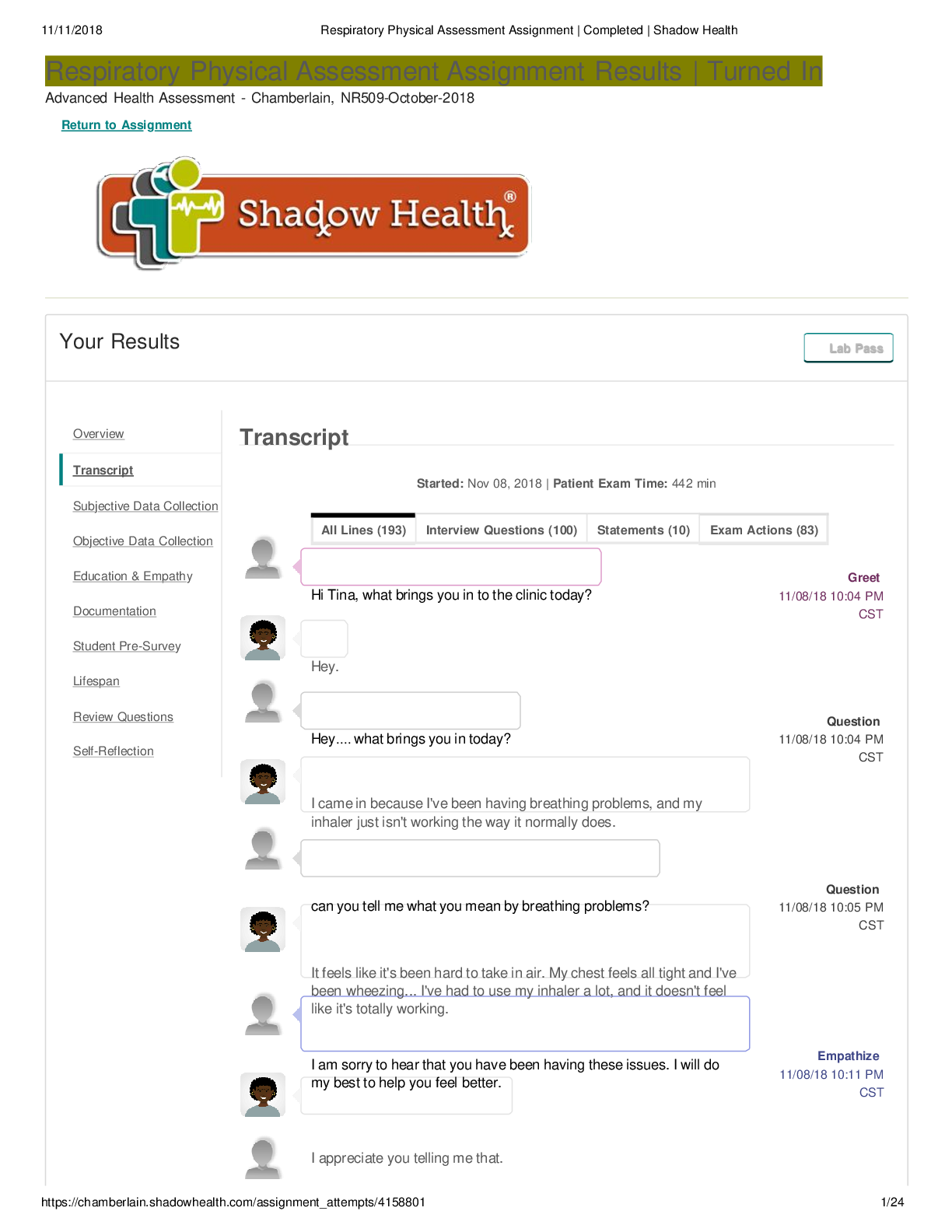
Abdominal Pain Physical Assessment Assignment Results | Completed Advanced Health Assessment - Chamberlain, NR509-October-2018 Return to Assignment Your Results T Turn In urn In Lab Pass Lab Pass ... Document: Vitals Document: Provider Notes Document: Provider Notes Student Documentation Model Documentation Subjective Patient Info: Esther Park, 78 years, Asian female CC: Patient states that they are "having pain in her belly" and that she is having trouble "going to the bathroom." HPI: The patient, Ms. Park, came into the office complaing of abdominal pain and not being able to have a bowel movement. She states that this pain started 5 days ago and has gotten worse over the past 2 to 3 days. The pain is in the lower abdomen and does not radiate. She does not have pain anywhere else. She states that her current abdominal pain could be rated a 6 out of 10. She describes the pain as "dull and crampy." She states that it does get worse sometimes, especially after physical activity or eating. She states that resting does help, but the only treatment she has pursued is "taking small sips of warm water," a method her friend infromed her of. This has not been an effective treatment. She states that she is not being able to go about her normal daily activities due to the pain. She also reports a low energy level. She is currently constipated, and issue that she has no history of. She has been constipated for about 5 days, but has not pursued any treatment. She had a bout of diarrhea about 3 days ago that she described as "loose and watery." It lasted for one day. Before the onset of the abdominal pain 5 days ago, the patient states that they had normal bowel habits, but has not had a movement in 3 days. No mucus or blood in stool. Patient states that the frequency of her Ms. Park reports that she is “having pain in her belly.” She experienced mild diarrhea three days ago and has not had a bowel movement since. She reports that she has been feeling some abdominal discomfort for close to a week, but the pain has increased in the past 2-3 days. She now rates her pain at 6 out of 10, and describes it as dull and crampy. She reports her pain level at the onset at 3 out of 10. She is also experiencing bloating. She did not feel her symptoms warranted a trip to the clinic but her daughter insisted she come. She describes her symptoms primarily as generalized discomfort in the abdomen, and states that her lower abdomen is the location of the pain. She denies nausea and vomiting, blood or mucus in stool, rectal pain or bleeding, or recent fever. She denies vaginal bleeding or discharge. Reports no history of inflammatory bowel disease or GERD. Denies family history of GI disorders. Her appetite has decreased over the last few days and she is taking small amounts of water and fluids. Previously she reports regular brown soft stools every day to every other day. Overview Transcript Subjective Data Collection Objective Data Collection Education & Empathy Documentation Self-Reflection Documentation / Electronic Health Record https://www.coursehero.com/file/36352067/NR-509-Abdominal-Pain-Documentation-Shadowpdf/ This study resource was shared via CourseHero.com12/10/2018 Abdominal Pain Physical Assessment Assignment | Completed | Shadow Health https://chamberlain.shadowhealth.com/assignment_attempts/4238251 2/5 Student Documentation Model Documentation urination has had a small decrease, as well as a darker yellow color. There is no blood in her urine. Current Meds: Patient takes Accupril 10mg daily for hypertension. She does not take any over the counter medication. Allergies: Patient has a latex allergy. No food, medication, or environmental allergies noted. Past Medical: Patient does have hypertension. Patient has no history of gastro issues, heartburns, or ulcers. She has not had appendicitis. She did have Cholecystectomy at 42 and a caesarean section at 40. No other major medical issues or hospitilizations. Patient is up to date on vaccines except for her seasonal flu shot. - - - - - - - - - Continued [Show More]
Last updated: 1 year ago
Preview 1 out of 5 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 06, 2021
Number of pages
5
Written in
Additional information
This document has been written for:
Uploaded
Mar 06, 2021
Downloads
0
Views
82