Adult Health 1 Final.docx 2021 exam and answer
Document Content and Description Below
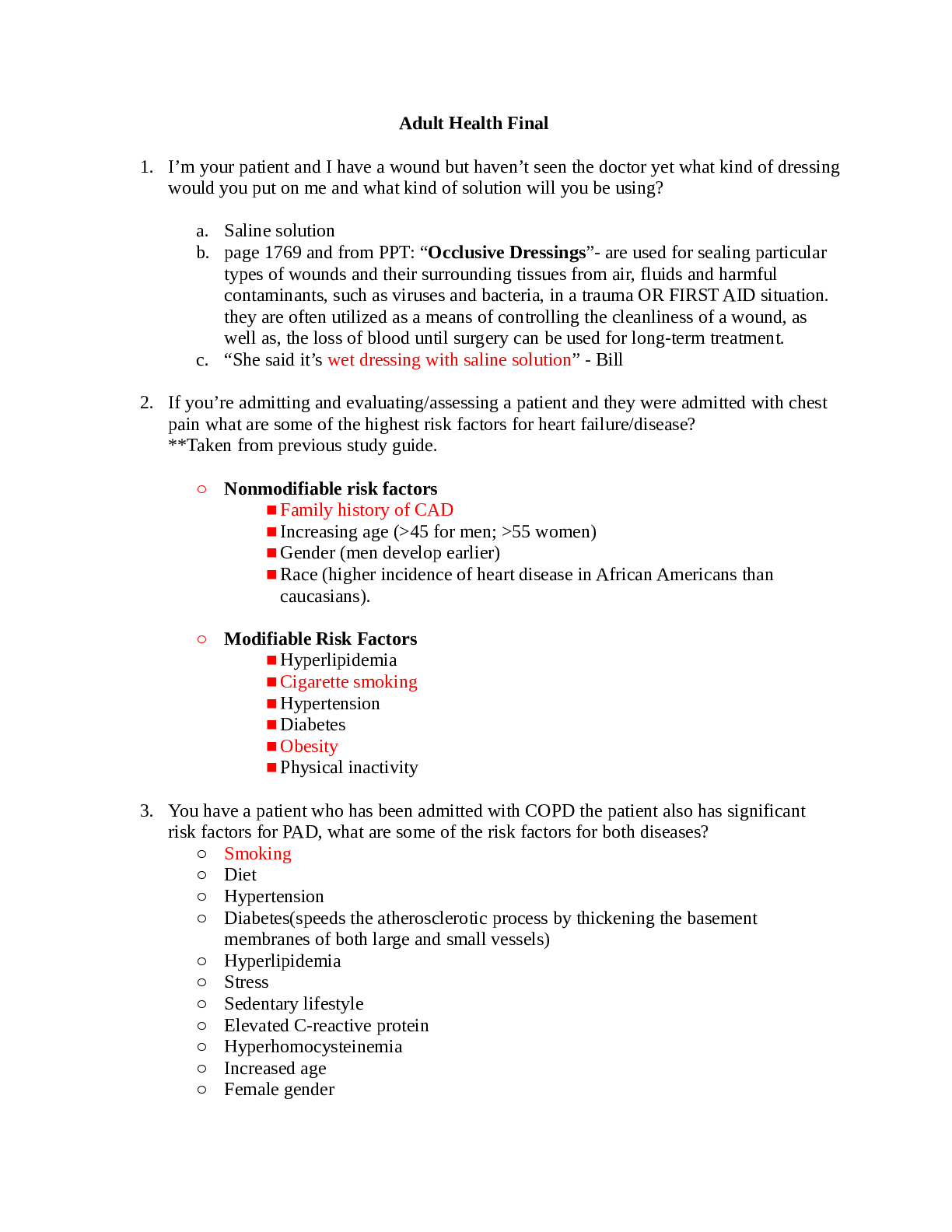
Adult Health 1 Final.docx 2021 exam and answer ⦁ I’m your patient and I have a wound but haven’t seen the doctor yet what kind of dressing would you put on me and what kind of solution will yo... u be using? ⦁ Saline solution ⦁ page 1769 and from PPT: “Occlusive Dressings”- are used for sealing particular types of wounds and their surrounding tissues from air, fluids and harmful contaminants, such as viruses and bacteria, in a trauma OR FIRST AID situation. they are often utilized as a means of controlling the cleanliness of a wound, as well as, the loss of blood until surgery can be used for long-term treatment. ⦁ “She said it’s wet dressing with saline solution” - Bill ⦁ If you’re admitting and evaluating/assessing a patient and they were admitted with chest pain what are some of the highest risk factors for heart failure/disease? **Taken from previous study guide. ⦁ Nonmodifiable risk factors ⦁ Family history of CAD ⦁ Increasing age (>45 for men; >55 women) ⦁ Gender (men develop earlier) ⦁ Race (higher incidence of heart disease in African Americans than caucasians). ⦁ Modifiable Risk Factors ⦁ Hyperlipidemia ⦁ Cigarette smoking ⦁ Hypertension ⦁ Diabetes ⦁ Obesity ⦁ Physical inactivity ⦁ You have a patient who has been admitted with COPD the patient also has significant risk factors for PAD, what are some of the risk factors for both diseases? ⦁ Smoking ⦁ Diet ⦁ Hypertension ⦁ Diabetes(speeds the atherosclerotic process by thickening the basement membranes of both large and small vessels) ⦁ Hyperlipidemia ⦁ Stress ⦁ Sedentary lifestyle ⦁ Elevated C-reactive protein ⦁ Hyperhomocysteinemia ⦁ Increased age ⦁ Female gender ⦁ Low-lifetime physical activity ⦁ Obesity ⦁ Hypercholesterolemia ⦁ Genetics ⦁ If your patient has high blood pressure, how are you diagnosing high BP? After one reading? ⦁ After several readings Two or more accurate blood pressure measurements (PP chapter 31) ⦁ Taken during two or more contacts with a healthcare provider under the same settings (PP chapter 31) ⦁ You are going to have a pic of a wound, need to know whether it’s going to be venous ulcer, arterial ulcer or diabetic ulcer. ⦁ Picture A and C- Venous Ulcers: located in medial lower leg, ankle, malleolar area. Foot and ankle will appear edematous. ⦁ Picture B- Arterial Ulcers: Typically are small, circular, deep ulcerations on the toes or tips of toes. “gangrene” ⦁ Picture D- Diabetic Ulcers: Located on plantar aspect of foot, under metatarsal heads, under heel and toes. Appear deep with surrounding callus and frequent cellulitis. D. ⦁ You’re going to have math questions, 5 of them, very similar to the 2nd exam ⦁ You need to know the difference between hyperthyroidism and hypothyroidism. ⦁ Hyperthyroidism = (hypermetabolic state) Overactivity of the thyroid gland and high levels of T4/T3, resulting in a rapid heartbeat and an increased rate of metabolism. ⦁ Sudden weight loss ⦁ Graves Disease ⦁ Anxiety ⦁ Irritability or moodiness (cannot sit quietly) ⦁ Nervousness, hyperactivity ⦁ Sweating or sensitivity to high temperatures ⦁ Hand trembling (shaking/tremors) ⦁ Hair loss ⦁ Missed or light menstrual periods (amenorrhea) ⦁ Rapid heartbeat (palpitations) ⦁ Fatigue, muscle weakness ⦁ Difficulty sleeping ⦁ Skin thinning ⦁ Fine, brittle hair ⦁ Flushed salmon colored skin in Caucasians (warm, soft, moist) ⦁ increased appetite and dietary intake ⦁ Bulging eyes (Exophthalmos) ⦁ Hypothyroidism = Abnormally low activity of the thyroid gland and low levels of T4/T3, resulting in retardation of growth and mental development in children and adults. Occurs most frequently in older women. ⦁ Fatigue ⦁ Myxedema (severe deficiency) ⦁ Weight gain ⦁ Numbness and tingling of fingers ⦁ loss of libido ⦁ Subnormal body temp and pulse rate ⦁ Voice may become husky/hoarse ⦁ Trouble sleeping * ⦁ Tiredness and Fatigue* ⦁ Difficulty concentrating* ⦁ Dry skin and hair* ⦁ Depression* ⦁ Sensitivity to cold temperature* ⦁ Frequent, heavy periods* ⦁ Joint and muscle pain* ⦁ Constipation* ⦁ If your patient has bulging eyes ⦁ Hyperthyroidism/Graves Disease ⦁ Thyroid dysfunction, what kind of questions would you ask a patient with thyroid dysfunction? Health history: Any changes in energy level Changes in tolerance to heat or cold Changes in weight or thirst Changes in frequency of urination Changes in fat or fluid distribution Any secondary sexual characteristics such as: Loss or growth of hair Menstrual cycle Memory / concentration Sexual dysfunction Changes in sleep pattern Changes in mood Visual changes Joint pain Physical Assessment: Vital signs Head to toe inspection Palpation of skin, hair and thyroid Physical changes Psychological changes Behavioral changes ⦁ What lab values would you look at for a patient with thyroid disease? Commonly Used Thyroid Tests: T4 by RIA (radioimmunoassay): ⦁ T4 reflects the amount of thyroxine in the blood. If the patient does not take any type of thyroid medication, this test is usually a good measure of thyroid function. ⦁ Thyroxine (T4) represents 80% of the thyroid hormone produced by the normal gland and generally represents the overall function of the gland. T3 by RIA (radioimmunoassay): ⦁ The other 20% is triiodothyronine measured as T3. Serum Thyroid-Stimulating Hormone (TSH): ⦁ Rise in TSH represents the pituitary gland’s response to a drop in circulating thyroid hormone (T3 & T4); it is usually the first indication of thyroid gland failure *according to the book TSH serum test is “the single best screening test of thyroid function because of its high sensitivity and ability to detect minute changes in serum” pg. 1472* ⦁ Blood test: levels of circulating hormones ⦁ Serum levels: specific hormone to determine the presence of hypo/hyper function of the endocrine system and site of dysfunction ⦁ Urine test: measure the amount of hormones excreted by the kidneys (one time 24-hour specimen) ⦁ Answer to 12 is going to be D (Cronk mentioned “PTU” which is Propylthiouracil given during a thyroid storm.*) ⦁ Patient is getting a blood transfusion and the patient is fine. 20 minutes after the infusion has been stopped, the patient has a reaction what’s the name of the reaction? ⦁ Acute hemolytic reaction ⦁ Febrile nonhemolytic reaction ⦁ Allergic reaction? Pg 894g ⦁ Hemolytic Transfusion Reaction p: 917 ⦁ Pick best nursing diagnosis ⦁ You’re giving a blood transfusion what’s hanging next to the blood? ⦁ 0.9% NaCl ⦁ What kind of tubing? ⦁ Y tubing ⦁ You have a patient in sickle cell crisis? What are some things you are going to take care of quickly? What is the main concern? pg. 913 ⦁ Control pain #1 ⦁ She also mentioned oxygen and airway (breath sounds/O2 sat/edema) ⦁ Fever and signs of infection ⦁ Assessment of fatigue ⦁ If I have anemia what are some of the things are you going to teach about the chronic illness? ⦁ For patients with anemia, medications or nutritional supplements are often prescribed to treat the condition. ⦁ Patients need to understand the purpose of the medication, how to take the medication and over what time period, and how to manage any side effects of therapy. (Infection symptoms, bruising and bleeding) ⦁ To enhance compliance, the nurse assist the patient to develop ways to incorporate the therapeutic plan into everyday activities rather than merely giving the patient a list of instructions. ⦁ For example, many patients have difficulty taking iron supplements because of related to GI effects. Rather than seeking assistance from a healthcare provider in managing the problem, some patients simply stop taking the iron: abruptly. (p 903- Promoting Compliance With Prescribed Therapy). ⦁ To prevent GI distress, start with one tablet per day and increase the dose gradually. PAGE: 902-903 ⦁ Increase Vitamin C intake because it enhances iron absorption. ⦁ Eat foods high in fiber. ⦁ Patients should avoid alcohol abuse, which can compromise the liver. ⦁ Teach patient how to manage fatigue (prioritize activities and and establish a balance between activity and rest.) ⦁ Maintain adequate nutrition (dietary sessions should be individualized, involve family members and include cultural aspects) ⦁ Maintain adequate perfusion (via IV fluids, blood products, supplemental O2) ⦁ Promote patient compliance: teach patient how to incorporate the therapeutic plan into everyday activities. DO NOT STOP TAKING MEDS ABRUPTLY. ⦁ Teach patient signs and symptoms of heart failure and to report to MD if they occur. (ie: paresthesias) ⦁ You’re going to be given a situation with orders for a patient, one of them you are going to question the provider, the one that has nothing to do with the situation ⦁ I have hemophilia, what lab work are you going to look at? Hemophilia = a medical condition in which the ability of the blood to clot is severely reduced, causing the sufferer to bleed severely from even a slight injury. The condition is typically caused by a hereditary lack of a coagulation factor, most often factor VIII. ⦁ Factor assays - shows the type of hemophilia and the severity ⦁ Fibrinogen test ⦁ Prothrombin Time (PT) test (12-14) sec ⦁ Activated Partial Thromboplastin Time (APTT) Test ⦁ Complete Blood Count (CBC) ⦁ Platelet count (150-400) x 10^3 ⦁ Hemoglobin ⦁ Hematocrit ⦁ Reticulocyte Counts ⦁ I have hemophilia, what is my best form of exercise? ⦁ Swimming ⦁ Nothing that is high impact or contact sports ⦁ I have iron deficiency anemia, what are some of the things you would teach? FOR WHEN THEY GO HOME. ⦁ Nutrition: Food sources high in iron include organ meats (beef or calf liver, chicken liver), other meats, beans (black, pinto, garbanzo), leafy green vegetables, raisins and molasses. ⦁ Taking iron rich foods with a source of vitamin C enhances the absorption of iron. ⦁ Take iron on an empty stomach ⦁ Remember that stools will become dark in color ⦁ To prevent GI distress, start with 1 tablet per day for a few days, then increase to 2 tablets per day, and so on allowing the body to adjust gradually to the iron ⦁ To prevent staining of teeth with a liquid preparation, use a straw or place a spoon at the back of the mouth to take the supplement. ⦁ Rinse mouth thoroughly afterward. ⦁ If I have herpes zoster(shingles) what would you take care of right away? Highest priority of treatment? ⦁ Pain ⦁ Granulation tissue what does it look like? ⦁ Bright red, pink and moist ⦁ Beefy red, puffy or mounded bubbly appearance ⦁ When you are looking at a wound what are some things you are going to assess about a wound? (Taken from ATI) APPEARANCE: ⦁ Note the color of open wounds.Red:Healthy regeneration of tissue. Yellow: Presence of purulent drainage and slough. Black:Presence of eschar that hinders healing and requires removal ⦁ Assess the length, width, and depth, and any undermining, sinus tracts or tunnels, and redness or swelling. Use a clock face with 12:00 toward the client’s head to document the location of sinus tracts. ⦁ Use the RYB color code guide for wound care: red (cover), yellow (clean), black (debride, removal of necrotic tissue). Closed wounds: Skin edges should be well-approximated. DRAINAGE (EXUDATE): ⦁ Is a result of the healing process and occurs during the inflammatory and proliferative phases of healing. ⦁ Note the amount, odor, consistency and color of drainage from a drain or on a dressing. ⦁ Note the integrity of the surrounding skin. ⦁ With each cleansing, observe the skin around a drain for irritation and breakdown. ⦁ For accurate measurement of drainage, weigh dressing FREQUENCY ⦁ document every dressing change -Preparation -Physical characteristics -Wound Measurement -Depth (tunneling and undermining: how deep and the direction) -Tissue Involvement -Tissue Types -Adherence of Tissue -Presence of Foreign bodies -Wound edges and margins -Surrounding tissue ⦁ 4 patients which one is at the highest risk of getting a Decubitus ulcers SOME FACTORS: ⦁ Immobility ⦁ Impaired sensory perception or cognition ⦁ Decreased tissue perfusion/edema ⦁ Prolonged pressure on tissue ⦁ Friction and shear forces ⦁ Altered skin moisture (too dry/too moist) ⦁ Incontinence of urine or feces ⦁ Trauma/burns ⦁ Patient with a surgical wound ⦁ Diabetics ⦁ Age-related skin changes ⦁ Malnutrition ⦁ Equipment: casts/traction/restraints ⦁ What factors ARE NOT included in documentation with a wound WHAT IS INCLUDED: ⦁ type of wound ⦁ correct anatomical location ⦁ measurement ⦁ tunneling/undermining ⦁ drainage ⦁ wound base tissue ⦁ wound edges ⦁ periwound: (intact, scaly, induration, edema, redness, warmth, color) ⦁ symptoms of infection ⦁ pain ⦁ patient fell six days ago -NOT ***TAKEN FROM WOUND DOCUMENT ASSESSMENT SHE POSTED. BAD documentation: “dressing change to foot ulcer. appears to be healing well. no ℅ voiced. DSD intact.” “patient has good pedal pulses and moves legs and feet well” the more specific documentation regarding the supplies used and the overall state of the wound and extremity affected is what should be documented. ⦁ Braden score, when do you do an interaction? What’s that number? ⦁ A score of 18 or less on the braden scale indicates a risk for developing a pressure ulcer. ⦁ Very High Risk: Total Score 9 or less ⦁ High Risk: Total Score 10-12 ⦁ Moderate Risk: Total Score 13-14 ⦁ Mild Risk: Total Score 15-18 ⦁ No Risk: Total Score 19-23 Braden Scale for Predicting Pressure Ulcer Risk: (Pg. 168) ⦁ Sensory Perception ⦁ Moisture ⦁ Activity ⦁ Mobility ⦁ Nutrition ⦁ Friction and Shear ⦁ Picture and be able to tell what kind of wound it is? ⦁ Is it herpes, shingles, scabies? *See #22 for Herpes Zoster Picture* ⦁ Picture is it stage 1 2 3 or 4? (Doc Sharing: wcei-pressure-ulcer-staging-guide) ⦁ Stage 1: Intact skin with nonblanchable redness of a localized area usually over a bony prominence. Darkly pigmented skin may not have visible blanching; its color may differ from the surrounding area. Further description: The area may be painful, firm, soft, warmer or cooler as compared to adjacent tissue. Stage I may be difficult to detect in individuals with dark skin tones. May indicate “at risk” persons (a heralding sign of risk) ⦁ Stage 2: Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough. May also present as an intact or open/ruptured serum-filled blister. Further description: Presents as a shiny or dry shallow ulcer without slough or bruising. Bruising indicates suspected deep tissue injury. This stage should not be used to describe skin tears, tape burns, perineal dermatitis, maceration or excoriation. ⦁ Stage 3:Full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscle are not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining and tunneling. Further description: The depth of a stage III pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have subcutaneous tissue and stage III ulcers can be shallow. In contrast, areas of significant adiposity can develop extremely deep stage III pressure ulcers. Bone/tendon is not visible or directly palpable. ⦁ Stage 4: Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often include undermining and tunneling. Further description: The depth of a stage IV pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have subcutaneous tissue and these ulcers can be shallow. Stage IV ulcers can extend into muscle and/or supporting structures (e.g., fascia, tendon or joint capsule) making osteomyelitis possible. Exposed bone/tendon is visible or directly palpable. ⦁ Question about insulin where you have this is your patient, accucheck, sliding scale, how much insulin are you going to give? ⦁ Need to know about Metformin. ⦁ Action = May increase the peripheral use of glucose, increase production of insulin, decrease hepatic glucose production, and alter intestinal absorption of glucose. ⦁ Indications = Adjunct to diet and exercise for the treatment of type 2 diabetics older than 10 years of age; extended release form for patients older than 17 years of age; adjunct treatment with polycystic ovary syndrome ⦁ Adverse Effects = Hypoglycemia, lactic acidosis, acute kidney failure, GI upset, nausea, anorexia, diarrhea, heartburn, and allergic skin reaction ⦁ Lab work that you do if your patient is a diabetic, what lab work would they do. What’s the scale that goes along with the lab work Hgb A1c less than 7% for people with diabetes (without: less than 6.5%) ⦁ Fasting lipid profile LDL: <100 mg/dL ⦁ Urinalysis (looking for ketones/ketonuria and glucosuria) glucose levels more than 240 mg/dl for two testing periods in a row) ⦁ Electrocardiogram ⦁ Serum creatinine level eGFR ≥60 mL/min/1.73 m2 ⦁ Accu-Chek (high> 100 or low <70) ⦁ Test for microalbuminuria ⦁ Oral Glucose Tolerance Test ⦁ Fasting blood glucose levels (NPO) (less 100 is normal, between 100-125 is pre, 126 or higher is considered within diabetic range) ⦁ Random Blood Glucose (200 or greater) ⦁ On PowerPoint with different lab values of diabetes, know that (?) Blood Glucose Targets are: 140-180 mg/dL ⦁ A1C: indicates your average blood sugar level for the past two to three months, measure the percentage of blood sugar attached to hemoglobin, the oxygen carrying protein in red blood cells ⦁ the higher your blood sugar levels, the more hemoglobin you’ll have with sugar attached ⦁ > 6.5% on two separate test indicated s that you have diabetes ⦁ 5.7% - 6.4% indicates prediabetes ⦁ < 5.7% = normal ⦁ Random blood glucose test: taken at random times, regardless of when you last ate or drank i. > 200 mg/dl suggests diabetes ⦁ Fasting blood glucose test: taken after an overnight fast ⦁ < 100 mg/dl = normal ⦁ 100 - 125 mg/dl = prediabetes ⦁ >126 on two separate tests = diabetes ⦁ Oral glucose tolerance test: Fast overnight, fasting glucose level completed, then you drink a sugary liquid and blood glucose levels are tested periodically for the next two hours ⦁ < 140 mg/dl = normal ⦁ 140 - 199 mg/dl = prediabetes ⦁ 200 mg/dl after 2 hours = diabetes ⦁ If I have diabetes what other lab work would you look at. Some of the complications that can set in so you have to look at other lab values ⦁ Fasting lipid profile LDL: <100 mg/dL ⦁ Urinalysis ⦁ Ketone bodies ⦁ Serum creatinine level ⦁ Low blood sugar/hypoglycemic what kind of medication would you give? ⦁ Immediate source of sugars such as candy/juice ⦁ Glucose elevating agents such as glucagon ⦁ Dextrose (D5) via IV ⦁ This is your patient’s type of insulin when would you see a reaction from the insulin? Know peak time- Know ONSET times ⦁ Need to know about how to reduce complications of diabetes. ⦁ Nutrition ⦁ Meal planning ⦁ Weight control ⦁ Increased activity/exercising ⦁ Monitoring blood glucose levels daily and A1C ⦁ Medications ⦁ Individualized treatment plans ⦁ Educate the patient! ⦁ Follow hospital insulin protocols or order sets that include standardized hypoglycemic treatment ⦁ Make guidelines available for glycemic goals and insulin dosing ⦁ Know the different signs/symptoms of hyper and hypoglycemia. Hyperglycemia ⦁ Extreme thirst ⦁ Frequent urination ⦁ Dry skin ⦁ Hunger ⦁ Blurred vision ⦁ Drowsiness ⦁ Nausea ⦁ Polydipsia, Polyuria, Polyphagia Hypoglycemia ⦁ Shaking ⦁ Fast heartbeat ⦁ Sweating ⦁ Cold ⦁ Clammy skin ⦁ May appear to be drunk ⦁ Dizziness ⦁ Anxious ⦁ Hunger ⦁ Impaired vision ⦁ Weakness fatigue ⦁ Headache ⦁ Irritable ⦁ Can induce seizure ⦁ Teaching how to give insulin how would you know they know how to self-administer their own insulin? ⦁ practice the skills with supervision by the nurse. ⦁ patient can identify the labels on the insulin vial. ⦁ checks appearance of insulin. ⦁ identifies where to purchase and store insulin. ⦁ can correctly use syringe for proper insulin administration. ⦁ can describe approximate time and course of insulin action. ⦁ can describe information about hypoglycemia. ⦁ can describe information about how to prevent hypoglycemia. ⦁ knows the type and dosage of own prescription and the timing of injections. ⦁ can describe site rotation and demonstrates injection with all appropriate anatomical areas to be used. ⦁ Evaluate patient’s literacy level and alter education to meet their levels of understanding. Determine how a patient learns best. ⦁ Go to sleep and stop breathing for 15-45 seconds, what do I have? ⦁ Sleep apnea ⦁ If I have to sleep and I have to put myself into a higher position, there’s a name for that where you have to sleep on pillows? ⦁ Orthopnea - refers to the need to sit upright to avoid feeling short of breath, including when sleeping. Patients use pillows to elevate their head or sleep sitting upright in a chair. ⦁ Paroxysmal nocturnal dyspnea - is sudden waking to shortness of breath due to reabsorption of fluid from dependent limbs, this fluid shift increases the preload and places increased demand on the heart, causing sudden pulmonary congestion. ⦁ pg 665 ⦁ Rhinitis what kind of drainage is coming from my nose? ⦁ Mucosal ⦁ Clear, watery, nasal discharge and nasal itching ⦁ Indications of endocrine disease, is a select all question (just to help know different endocrine diseases- from google- fyi more than we probably need to know) ⦁ Parathyroid, some of assessment findings, is also a select all (page 1487-1490) HYPERPARATHYROID findings: ⦁ diagnosed by persistent elevation of serum calcium levels ⦁ bone changes (detected by bone scans) ⦁ stones in one or both kidneys ⦁ apathy (lack of interest or concern) ⦁ fatigue ⦁ muscle weakness ⦁ N/V (Nausea/Vomiting) ⦁ constipation ⦁ HTN (Hypertension) ⦁ cardiac dysrhythmias. HYPOPARATHYROID findings: ⦁ Vitamin D deficiency ⦁ increased blood phosphate ⦁ decreased blood calcium ⦁ Tetany (seizures) ⦁ Graves’ disease, what lab work are you going to do? ⦁ TSH (normally low level if you have Graves’ disease) 0.5 to 5.0 normal range ⦁ T3 and T4 (usually high level if you have Graves’ disease) ⦁ Suppressed thyrotropin ⦁ Indicative of hyperthyroidism (goiter and exophthalmos) ⦁ If your patient is a diabetic what puts them at risk for a possible amputation? Select all. (Powerpoint Chapter 51 Slides: 25-26) ⦁ Neuropathy (Nerve Damage) in the feet or poor blood flow to the feet increases the risk of various foot complications such as amputation (Toes/feet). ⦁ Lower extremity amputation originates from: ⦁ Diabetic foot ulcers ⦁ Peripheral artery disease (PAD) ⦁ Peripheral vascular disease (PVD) ⦁ Peripheral neuropathy (furthest away from the heart) ⦁ Minor trauma ⦁ Deformity (Charcot) ⦁ Increased plantar pressure ⦁ Infection ⦁ Uncontrolled blood sugar levels ⦁ Another picture, what do you see in the picture, is it decubitus ulcer (around sacral, coccyx, greater trochanter, heels, ischial tuberosity, and lateral malleolus areas), diabetic ulcer (appears on plantar aspect of foot, under metatarsal heads, under heel and toes), varicose vein ulcer (typical to lower legs)? FYI: there is an awesome powerpoint Cronk posted in the last unit that has great images for different types of wounds :) Diabetic Foot Complication Diabetic Foot Complication- Wounds/Ulcers ^^CHARCOT FOOT ⦁ Patient is getting blood, what are you monitoring them for? ⦁ Allergic Reaction (acute hemolytic reaction) ⦁ Delayed hemolytic reaction (your body destroys red blood cells until your rbc level is very low) ⦁ Transfusion related acute lung injury ⦁ Febrile nonhemolytic reaction (fever, temperature) ⦁ Bacterial Contamination ⦁ Circulatory overload (Iron, blood pressure) ⦁ Disease acquisition ⦁ Complication of long term transfusion therapy. ⦁ Hypothermia ⦁ Difficulty breathing ⦁ Monitor BP/Pulse Rate/HR and Rhythm ⦁ Assess the IV site for infiltration reactions ⦁ You gave a blood transfusion and they are having an allergic reaction what are you going to do? Stop the transfusion, run the saline, what are you going to do with the blood? i. Send it back to the blood bank ⦁ Need to know about aplastic anemia, where is the anemia from? What are you going to look at to see if they have aplastic anemia? ⦁ Rare disease caused by a decrease in or damage to marrow stem cells, to the microenvironment within the marrow, and replacement of the marrow with fat. Stem cell damage is caused by the body’s T cells mediating an inappropriate attack against the bone marrow, resulting in bone marrow aplasia. ⦁ “markedly reduced hematopoiesis” ⦁ Significant neutropenia and thrombocytopenia occur. ⦁ Symptoms: “Infection-like”- fatigue, pallor, dyspnea, bruising (purpura), bleeding ⦁ CBC and hematologic evaluation should be performed. ⦁ If patient has repeated throat infections, cervical lymphadenopathies may be seen. As well as, splenomegaly. ⦁ A bone marrow aspirate would show extremely hypoplastic/aplastic marrow replaced with fat. ⦁ Patient is bedridden, and they are at a high risk for developing a decubitus ulcer (bedsore), what are you going to do to prevent it? ⦁ Change positions frequently ⦁ Keep skin clean and dry: decrease heat and moisture ⦁ Use pillows ⦁ Ensure no wrinkles on bed sheets “less is best” ⦁ Simple ROM exercises ⦁ Use higher specification foam mattresses ⦁ Evenly distribute pressure over large area ⦁ Monitor for skin breakdown frequently ⦁ You have a patient with diabetic ketoacidosis and elevated blood sugar. What kind of insulin are you going to give? ⦁ Insulin Glargine (long acting insulin) ⦁ How are you going to know if your patient is going to need more teaching by what comment do they make? It’s on diabetes ⦁ “ I’m a thug, I don’t need any insulin” I bet Gabe said this.... ⦁ “I will inject myself into my chest” ⦁ “I’m going to eat a lot of sugar, so I will give myself extra dose of insulin” ⦁ “I will drink my insulin before I eat” ⦁ Know about prednisone and diabetes. ⦁ Prednisone is a glucocorticoid that stimulates an increase in glucose levels for energy. ⦁ Caution should be used in patients with diabetes because the glucose-elevating effects disrupt glucose control ⦁ Use of steroids increases risk of infection, which puts a patient with diabetes at an even higher risk for developing foot ulcers. [Show More]
Last updated: 1 year ago
Preview 1 out of 21 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 13, 2021
Number of pages
21
Written in
Additional information
This document has been written for:
Uploaded
Mar 13, 2021
Downloads
0
Views
55

.png)



.png)