*NURSING > STUDY GUIDE > Care_of_Critically_ill_Patients_with_Respiratory_Problems_2020 | MED SURG 403 Care_of_Critically_ill (All)
Care_of_Critically_ill_Patients_with_Respiratory_Problems_2020 | MED SURG 403 Care_of_Critically_ill_Patients_with_Respiratory_Problems
Document Content and Description Below
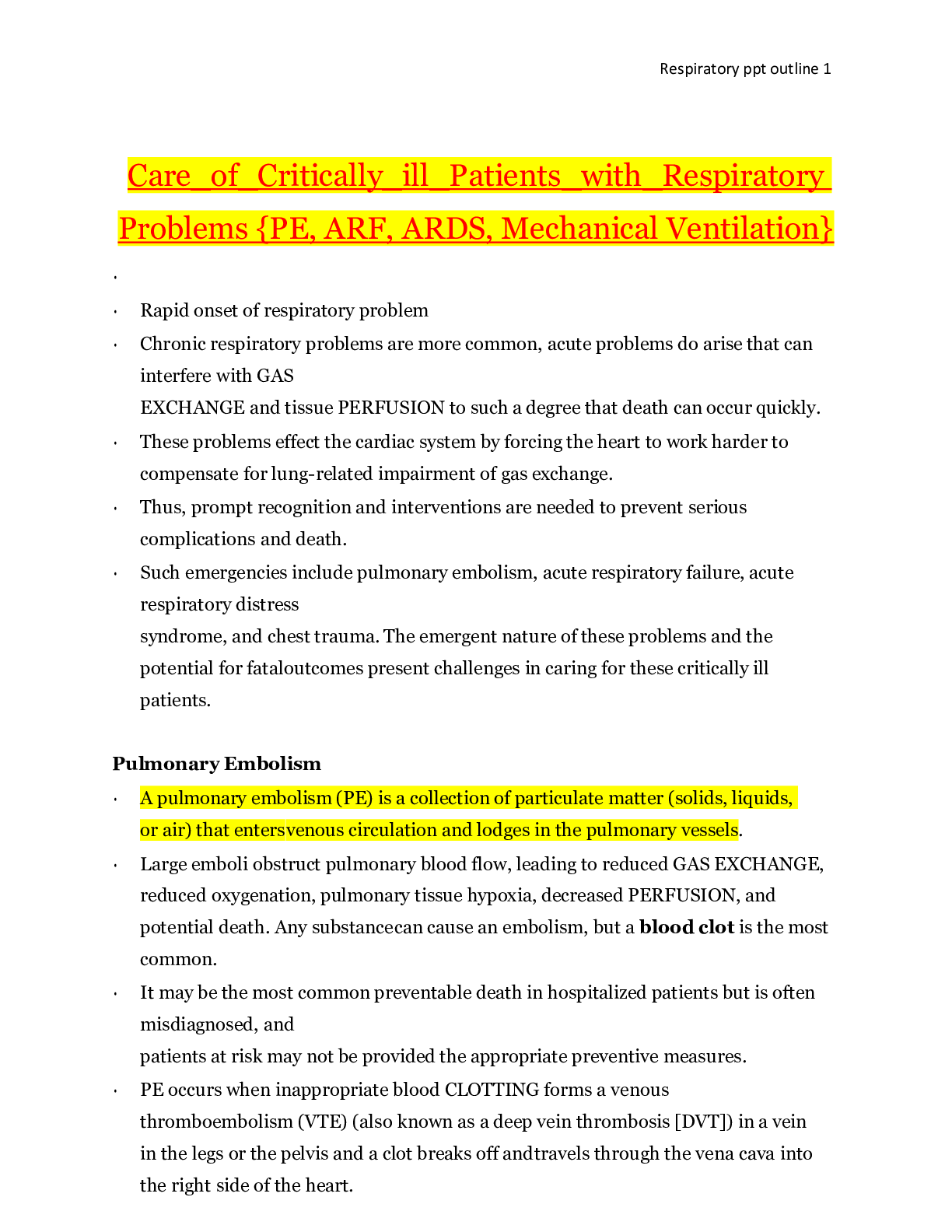
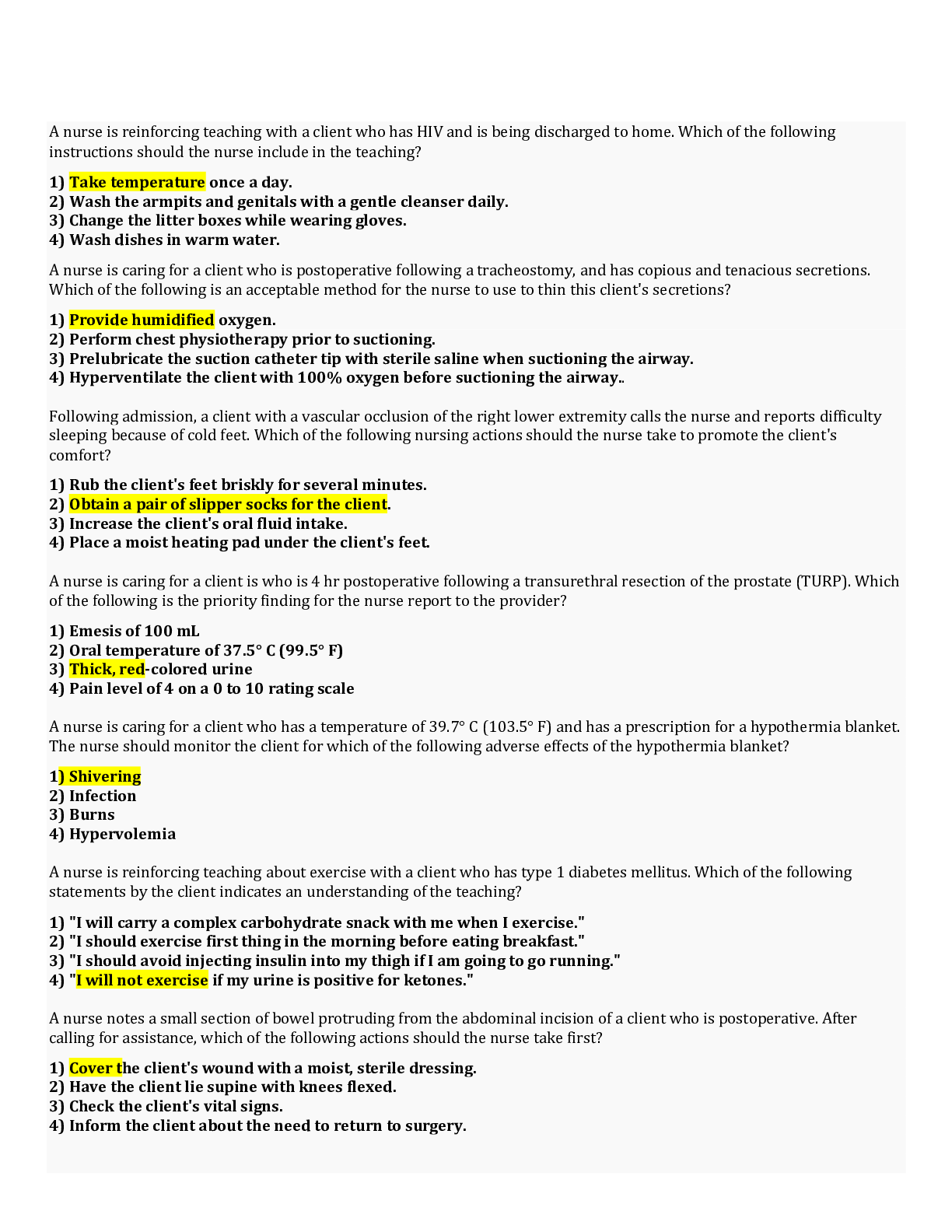
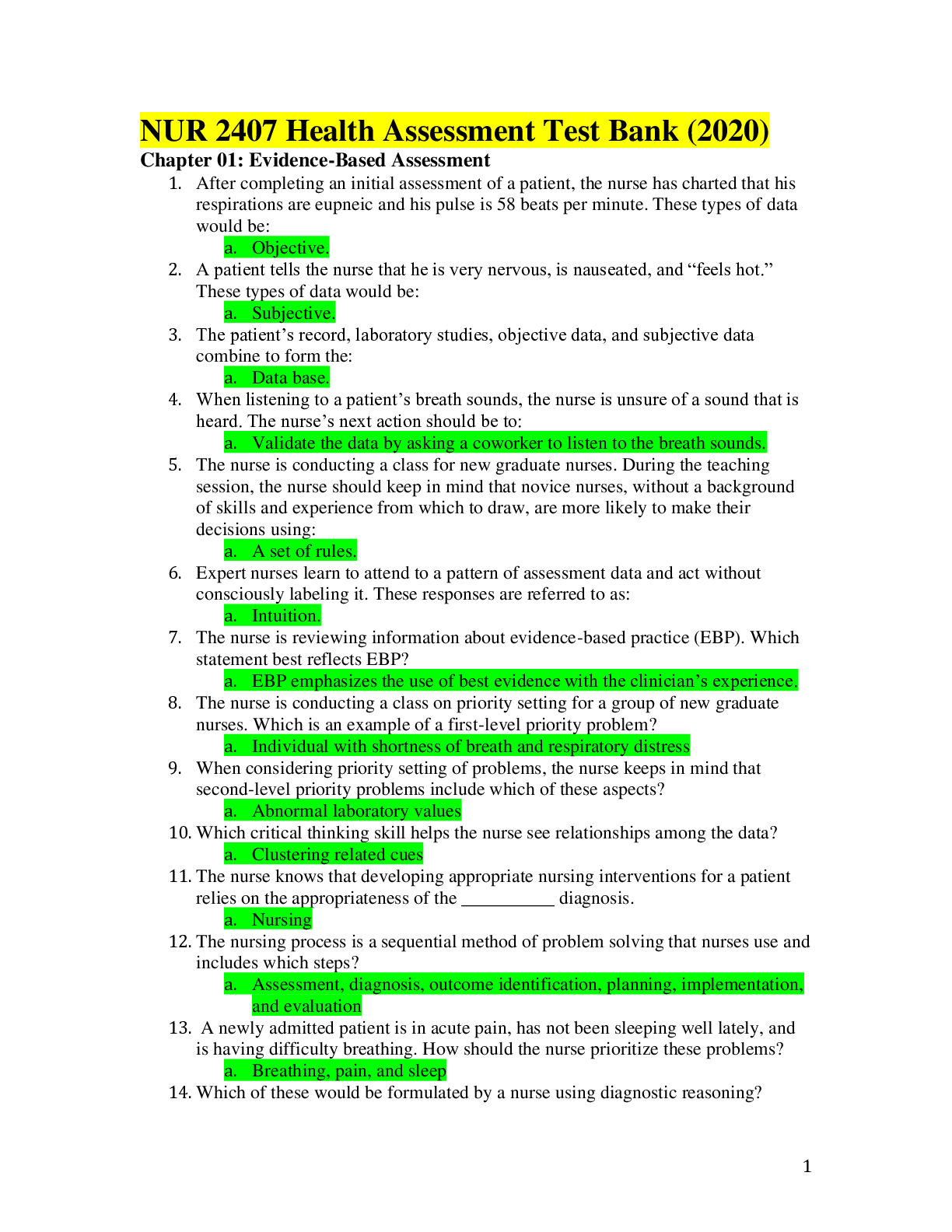
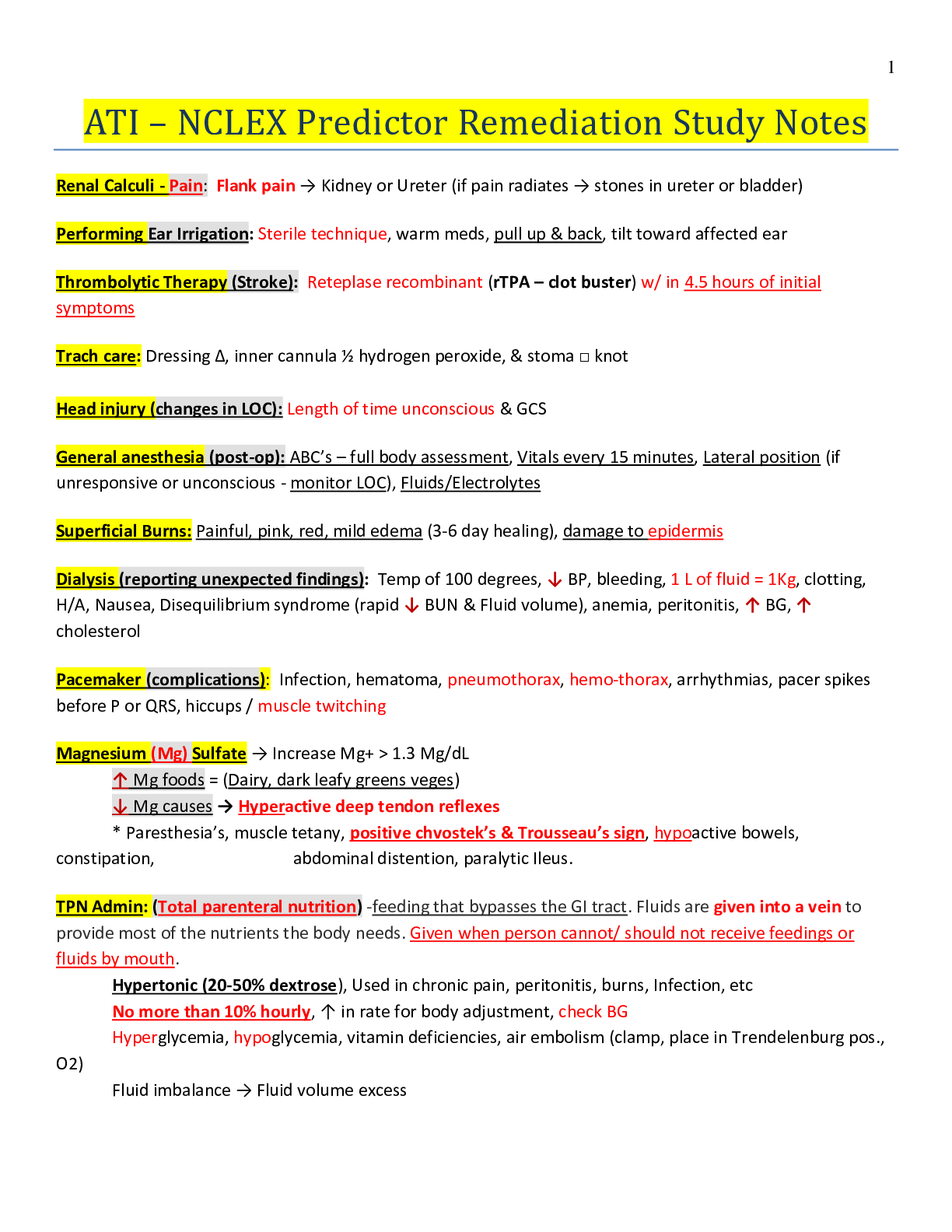
Care_of_Critically_ill_Patients_with_Respiratory Problems {PE, ARF, ARDS, Mechanical Ventilation} • • Rapid onset of respiratory problem • Chronic respiratory problems are more common, acute... problems do arise that can interfere with GAS EXCHANGE and tissue PERFUSION to such a degree that death can occur quickly. • These problems effect the cardiac system by forcing the heart to work harder to compensate for lung- related impairment of gas exchange. • Thus, prompt recognition and interventions are needed to prevent serious complications and death. • Such emergencies include pulmonary embolism, acute respiratory failure, acute respiratory distress syndrome, and chest trauma. The emergent nature of these problems and the potential for fatal outcomes present challenges in caring for these critically ill patients. Pulmonary Embolism • A pulmonary embolism (PE) is a collection of particulate matter (solids, liquids, or air) that enters venous circulation and lodges in the pulmonary vessels. • Large emboli obstruct pulmonary blood flow, leading to reduced GAS EXCHANGE, reduced oxygenation, pulmonary tissue hypoxia, decreased PERFUSION, and potential death. Any substance can cause an embolism, but a blood clot is the most common. • It may be the most common preventable death in hospitalized patients but is often misdiagnosed, and patients at risk may not be provided the appropriate preventive measures. • PE occurs when inappropriate blood CLOTTING forms a venous thromboembolism (VTE) (also known as a deep vein thrombosis [DVT]) in a vein in the legs or the pelvis and a clot breaks off and travels through the vena cava into the right side of the heart. • The clot then lodges in the pulmonary artery or within one or more of its branches. Platelets collect on the embolus, triggering the release of substances that cause blood vessel constriction. • Widespread pulmonary vessel constriction and pulmonary hypertension impair GAS EXCHANGE and tissue PERFUSION. • Deoxygenated blood moves into arterial circulation, causing hypoxemia (low arterial blood oxygen level). • Major risk factors for VTE leading to PE are: • Prolonged immobility, Central venous catheters, Surgery, Obesity, advancing age • Conditions that increase blood CLOTTING • History of thromboembolism • Smoking, pregnancy, estrogen therapy, heart failure, stroke, cancer (particularly lung or prostate), and trauma increase the risk for VTE and PE. • Fat, oil, air, tumor cells, amniotic fluid and fetal debris, foreign objects (e.g., broken IV catheters), injected particles, and infected clots can enter a vein and cause PE. • Fat emboli can occur with fracture of the femur, and oil emboli can occur from diagnostic procedures. • These have a mortality rate of about 10%. Fat emboli do not impede lung blood flow; instead, they injure blood vessels and cause acute respiratory distress syndrome (ARDS). Risks of PE • Lifestyle changes can help reduce the risk for PE. • Tobacco use narrows blood vessels and increases the risk for clot formation. • Hormone-based contraceptives also increase blood CLOTTING. • Urge patients to stop smoking cigarettes, especially women who use hormone-based contraceptives. • Reducing weight and becoming more physically active can reduce risk for PE. • Teach patients who are traveling for long periods to drink plenty of water, change positions often, avoid crossing their legs, and get up from the sitting position at least 5 minutes out of every hour to prevent stasis and clot formation. • For patients known to be at risk for PE, small doses of heparin or low-molecular-weight heparin (enoxaparin [Lovenox]), an indirect thrombin inhibitor, may be prescribed every 8 to 12 hours. • Oral direct thrombin inhibitors may be used instead of heparin for VTE prevention in patients who have nonvalvular atrial fibrillation. • For adults who have an ongoing risk for VTE and PE, prevention may include preoperative placement of a retrievable inferior vena cava (IVC) filter. • This placement occurs before any surgery in which the patient is expected to be confined to bed for more than just a few days and is retrieved when the patient is fully ambulatory. Prevention of Pulmonary Embolism • Start passive and active range-of-motion exercises for the extremities of immobilized and postoperative patients. • Ambulate patients soon after surgery. • Use anti-embolism and pneumatic compression stockings and devices after surgery. • Evaluate patient for criteria indicating the need for anticoagulant therapy. • Avoid the use of tight garters, girdles, and constricting clothing. • Prevent pressure under the popliteal space (e.g., do not place a pillow under the knee; instead, use alternating pressure mattress). • Elevate the affected limb 20 degrees or more above the level of the heart to improve venous return, as appropriate. • Change patient position every 2 hours or ambulate as tolerated • Prevent injury to the vessel lumen by preventing local pressure, trauma, infection, or sepsis. • Refrain from massaging leg muscles. • Instruct patient not to cross legs. • Administer prescribed prophylactic low-dose anticoagulant and antiplatelet drugs. • Administer prescribed drugs, such as stool softeners, that will prevent episodes of the Valsalva maneuver. • Teach the patient and family about precautions. (falls, bleeding, etc) • Encourage smoking cessation • Perform a comprehensive assessment of peripheral circulation Inter-collaborative Care of PE • The patient who has a pulmonary embolism (PE) is critically ill and at risk for life-threatening complications. Initial management occurs in an acute care environment, most often an ICU. • Some patients have ongoing issues or residual problems that impair GAS EXCHANGE and PERFUSION after the acute problems have resolved. These changes may be permanent. • Respiratory therapists assist with prescribed oxygen therapy and delivery needs. Physical therapists can help the patient maintain muscle conditioning. • Occupational therapists provide information and home set-up suggestions to help patients conserve energy when endurance is affected. • Registered dietitians assess patients' caloric and protein needs and plan personalized interventions to meet these needs. • Pastoral care workers and clergy may help patients who experience spiritual distress with this life- altering condition. • Social workers together with home care nurses determine which types of home modifications and durable supplies would be most helpful in maintaining functional ability for self-management of ADLs. • When significant lifestyle changes are needed, mental health professionals can help the patient and family cope with adjustments. Classical Symptoms of PE • Dyspnea, sudden onset • Sharp, stabbing chest pain • Apprehension, restlessness • Feeling of impending doom • Cough • Hemoptysis • Signs • Tachypnea • Crackles • Pleural friction rub • Pleural friction rub is an abnormal lung sound which is caused by inflammation of the pleural layer of the lungs rubbing together. Pleural friction rub is heard on inspiration and expiration and sounds like a low-pitch harsh/grating noise • Tachycardia • S3 or S4 heart sound • Diaphoresis • Fever, low-grade • Petechiae over chest and axillae • Decreased arterial oxygen saturation (SaO2) Cardiac Symptoms of PE • Cardiac symptoms related to decreased tissue PERFUSION include tachycardia, distended neck veins, syncope (fainting or loss of consciousness), cyanosis, and hypotension. • Systemic hypotension results from acute pulmonary hypertension and reduced forward blood flow. • Abnormal heart sounds, such as an S3 or S4, may occur. • Electrocardiogram (ECG) changes are nonspecific and transient. • T-wave and ST-segment changes may occur. • Right ventricular dysfunction and failure are extreme complications. The patient may have cardiac arrest or shock • Critical Thinking…. - - - - - Continued [Show More]
Last updated: 1 year ago
Preview 1 out of 48 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 18, 2021
Number of pages
48
Written in
Additional information
This document has been written for:
Uploaded
Mar 18, 2021
Downloads
0
Views
50



.png)
 Rasmussen College.png)