*NURSING > EXAM PROCTORED > RN ADULT MEDICAL SURGICAL 2019 PROCTOR REMEDIATION,100% CORRECT (All)
RN ADULT MEDICAL SURGICAL 2019 PROCTOR REMEDIATION,100% CORRECT
Document Content and Description Below
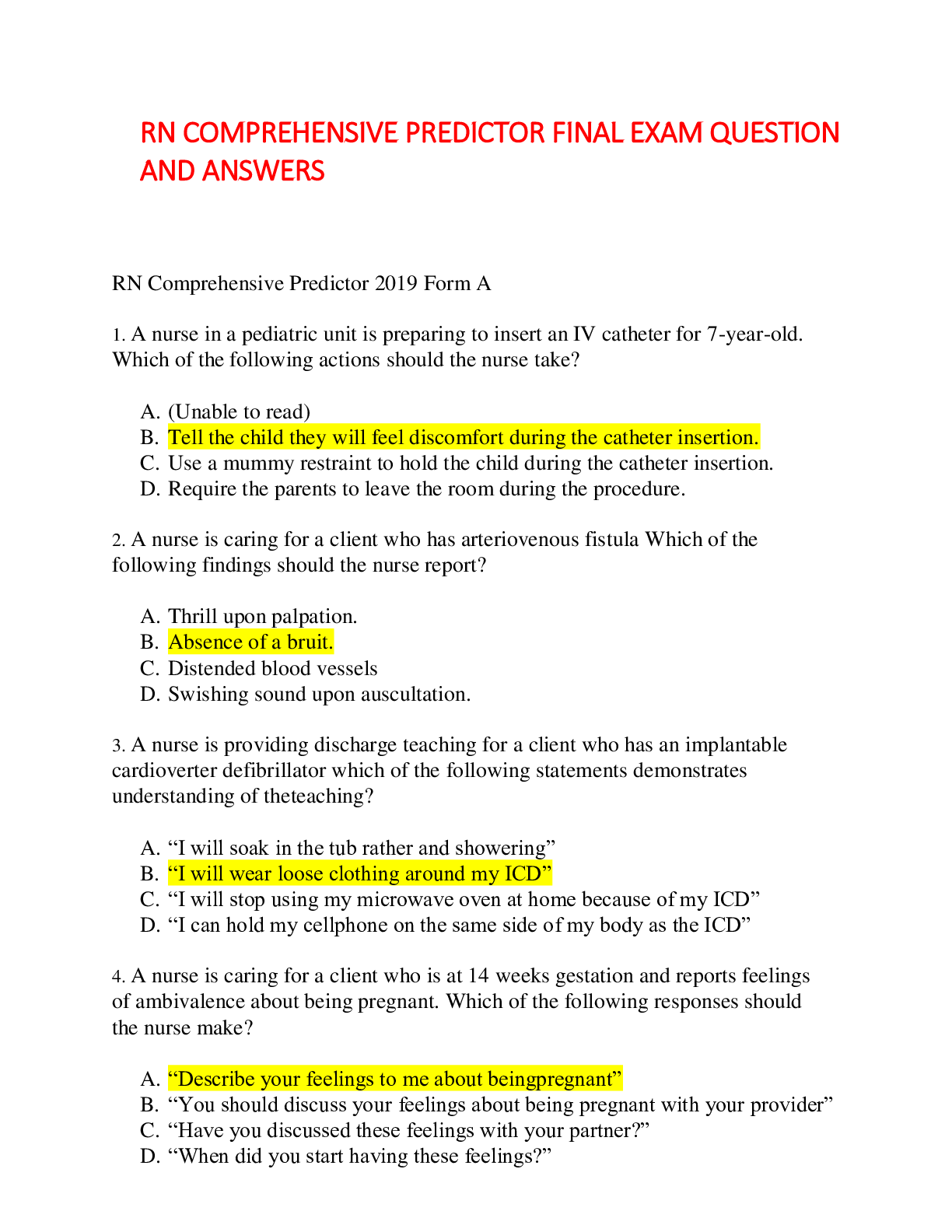
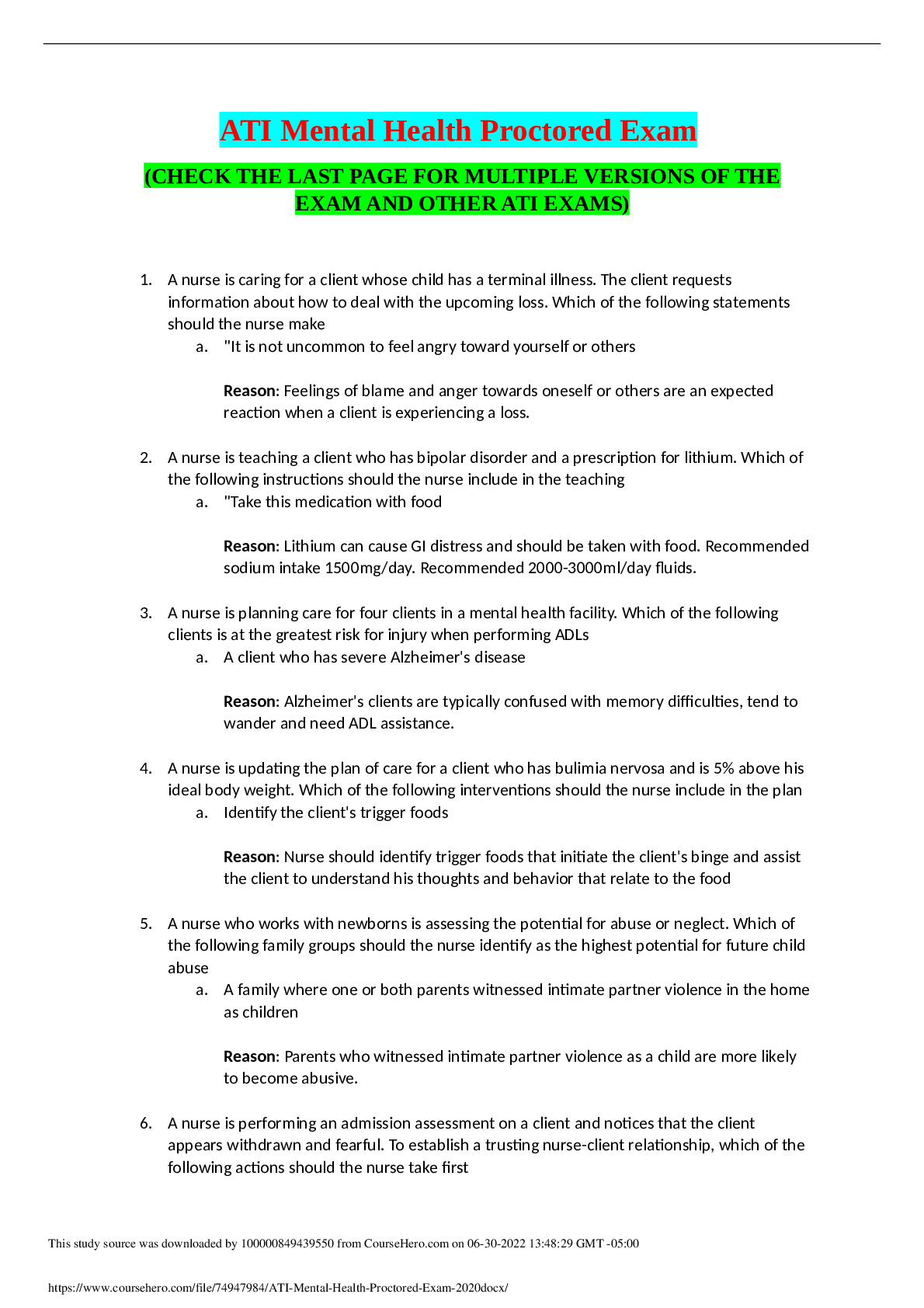
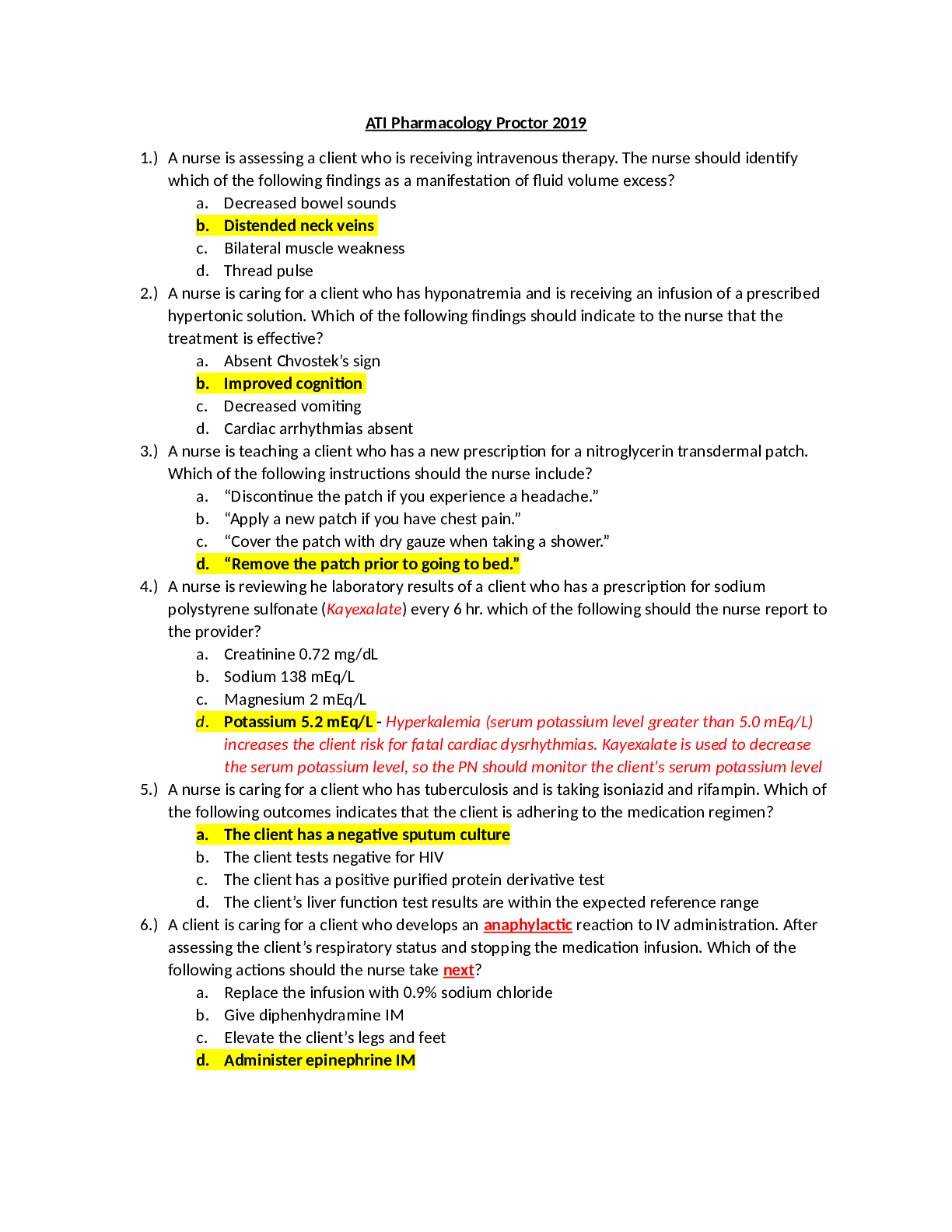
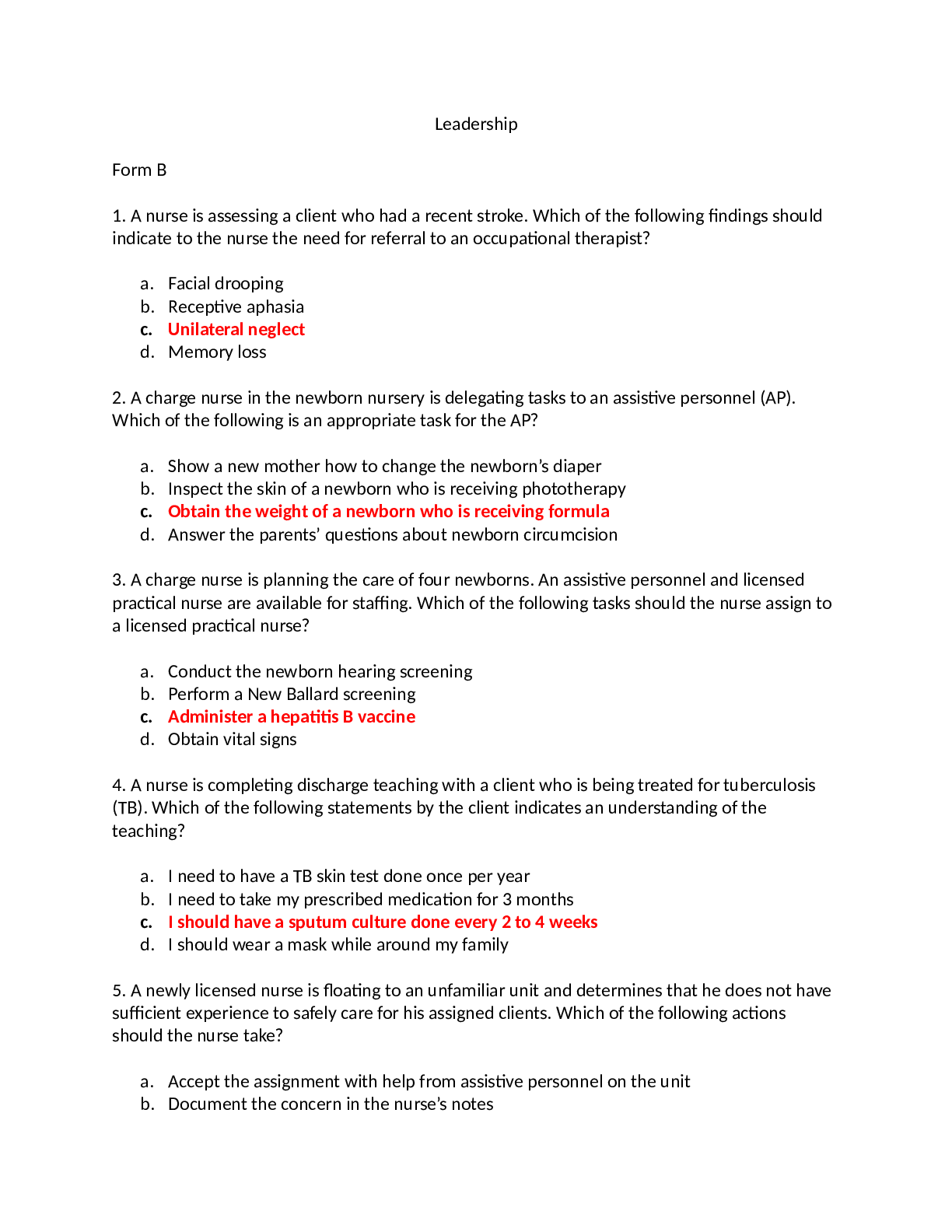
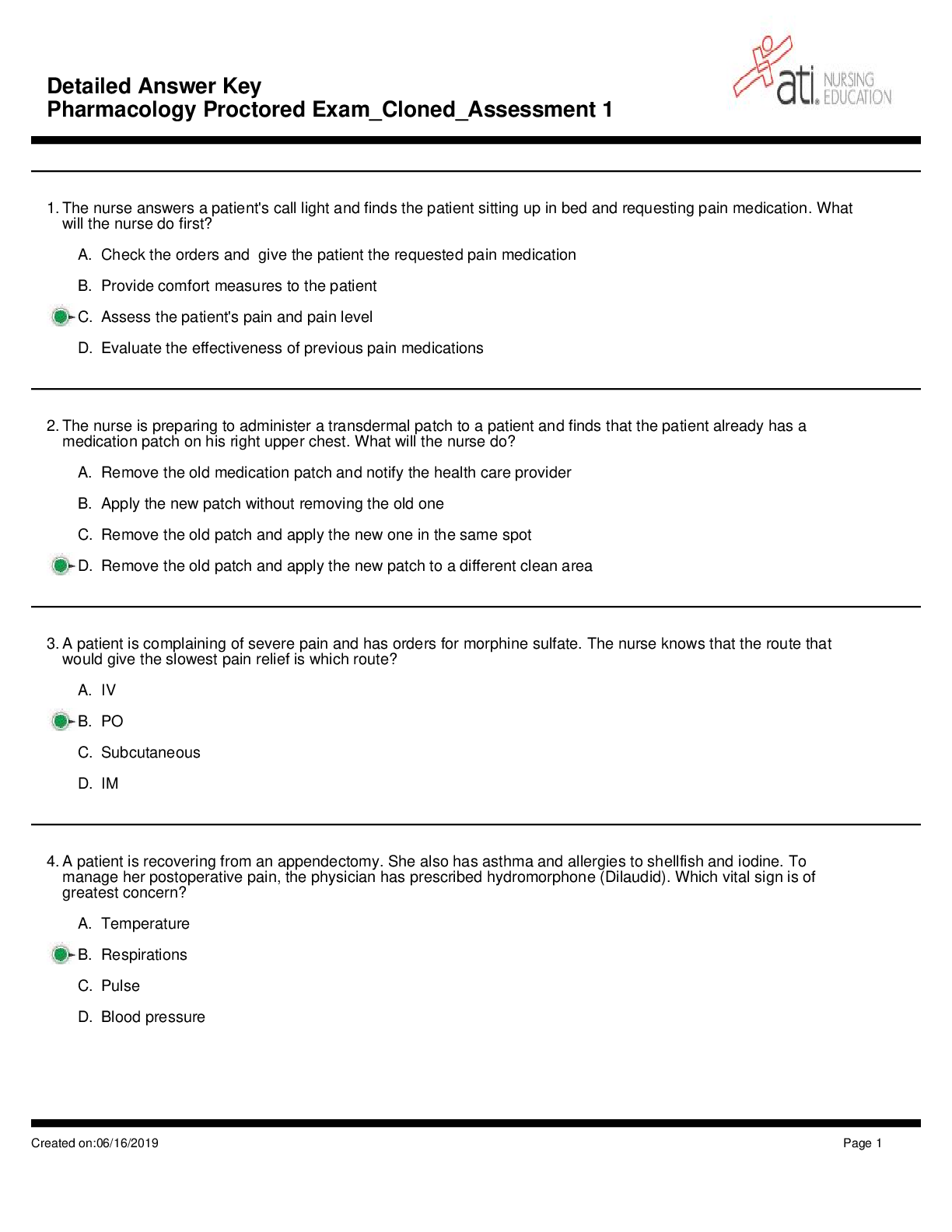
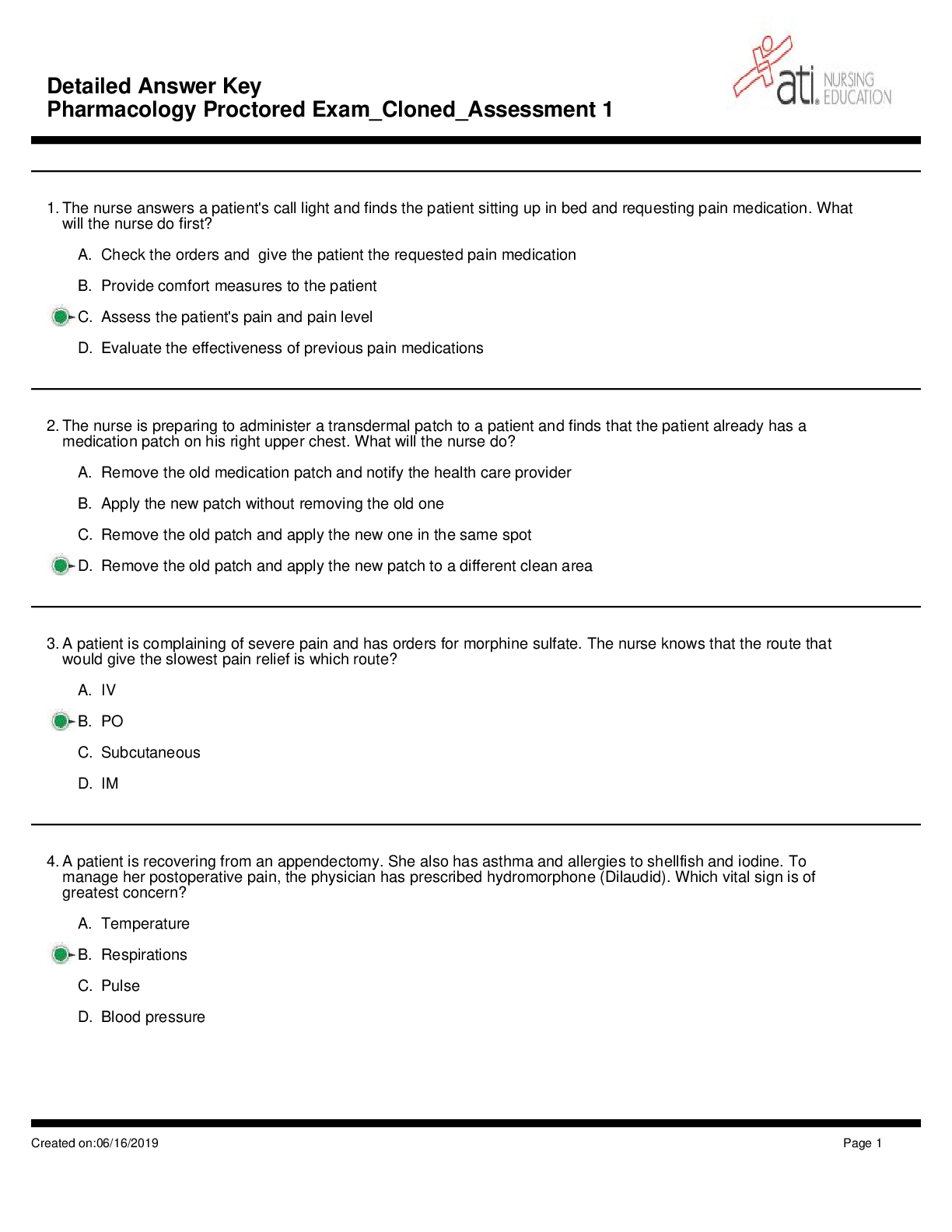
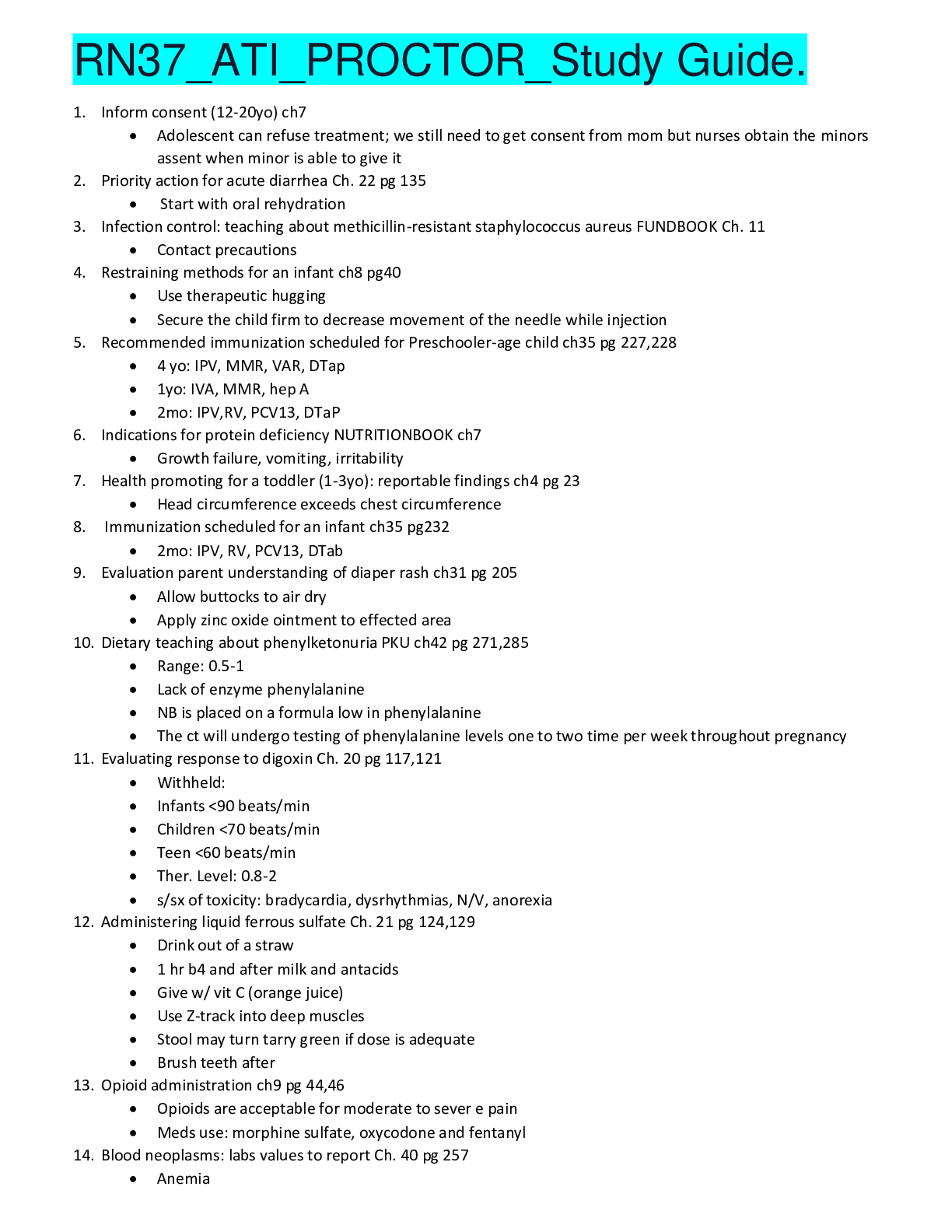
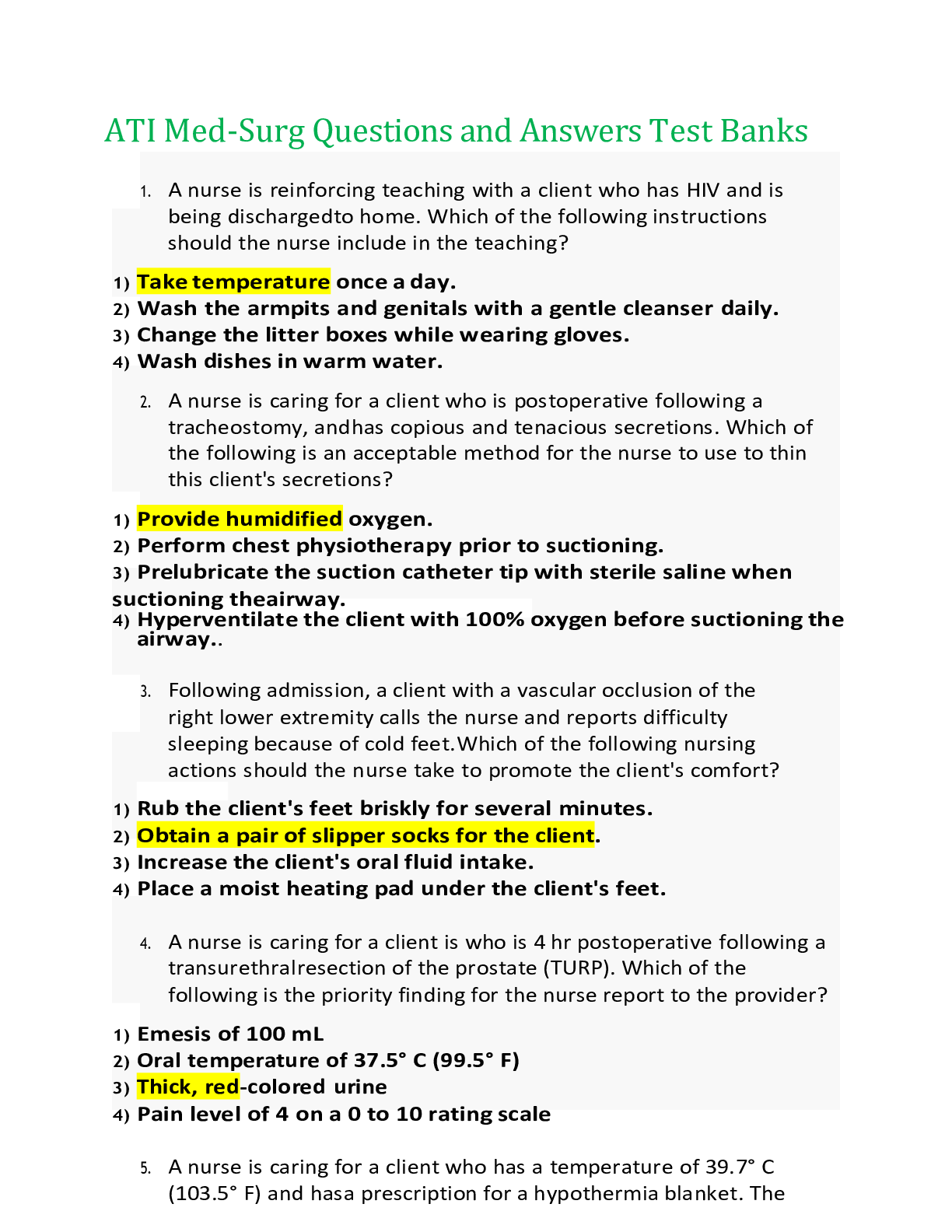
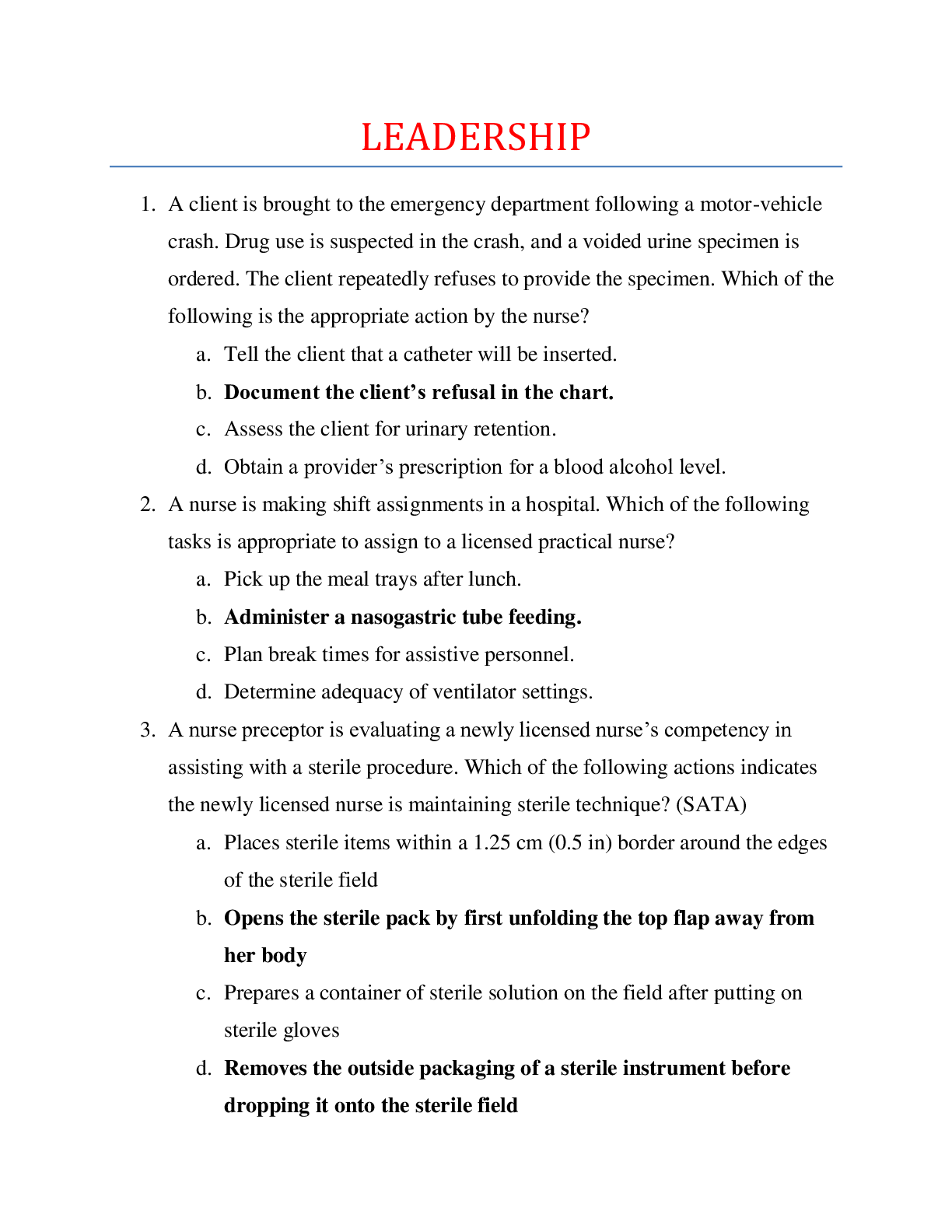
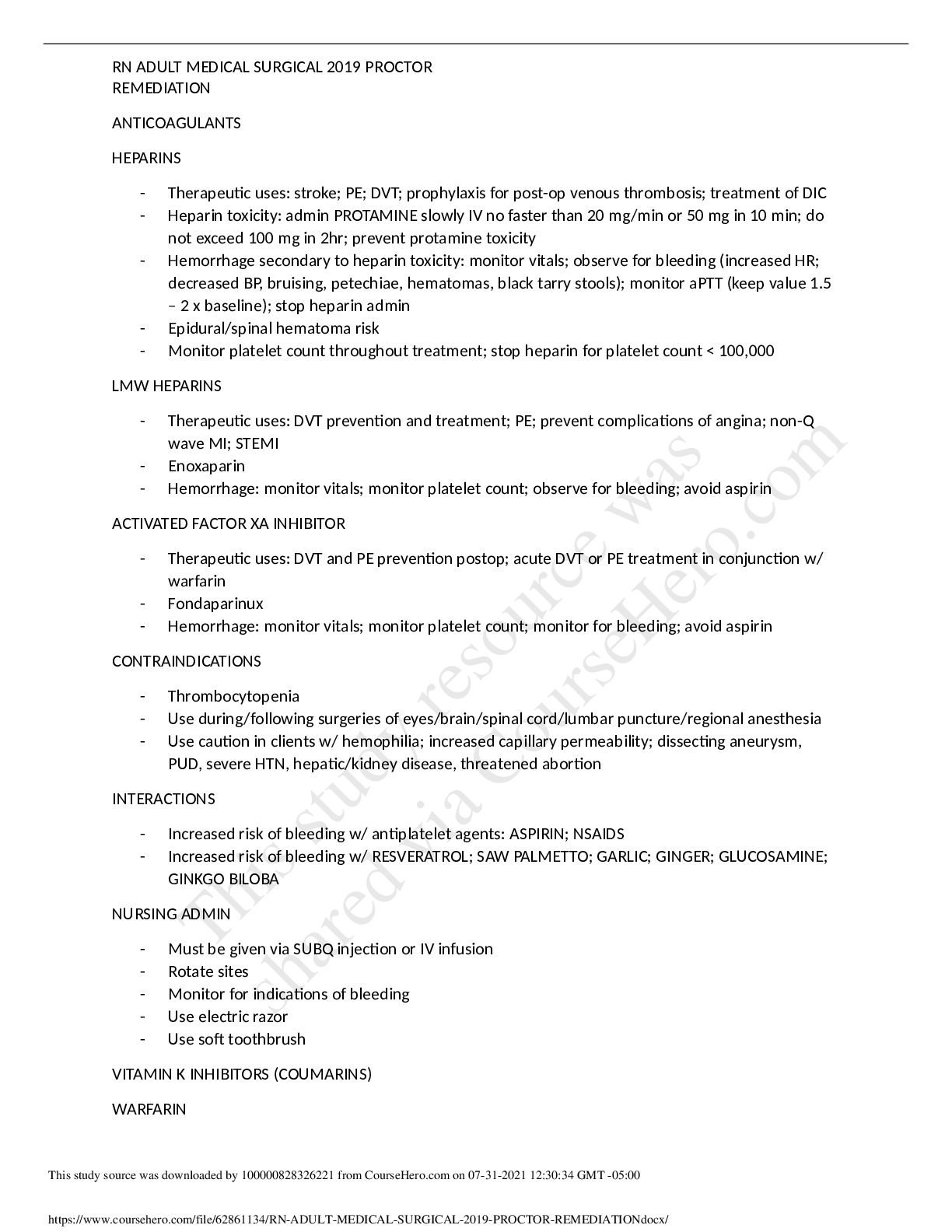
RN ADULT MEDICAL SURGICAL 2019 PROCTOR REMEDIATION ANTICOAGULANTS HEPARINS - Therapeutic uses: stroke; PE; DVT; prophylaxis for post-op venous thrombosis; treatment of DIC - Heparin toxicity: admin... PROTAMINE slowly IV no faster than 20 mg/min or 50 mg in 10 min; do not exceed 100 mg in 2hr; prevent protamine toxicity - Hemorrhage secondary to heparin toxicity: monitor vitals; observe for bleeding (increased HR; decreased BP, bruising, petechiae, hematomas, black tarry stools); monitor aPTT (keep value 1.5 – 2 x baseline); stop heparin admin - Epidural/spinal hematoma risk - Monitor platelet count throughout treatment; stop heparin for platelet count < 100,000 LMW HEPARINS - Therapeutic uses: DVT prevention and treatment; PE; prevent complications of angina; non-Q wave MI; STEMI - Enoxaparin - Hemorrhage: monitor vitals; monitor platelet count; observe for bleeding; avoid aspirin ACTIVATED FACTOR XA INHIBITOR - Therapeutic uses: DVT and PE prevention postop; acute DVT or PE treatment in conjunction w/ warfarin - Fondaparinux - Hemorrhage: monitor vitals; monitor platelet count; monitor for bleeding; avoid aspirin CONTRAINDICATIONS - Thrombocytopenia - Use during/following surgeries of eyes/brain/spinal cord/lumbar puncture/regional anesthesia - Use caution in clients w/ hemophilia; increased capillary permeability; dissecting aneurysm, PUD, severe HTN, hepatic/kidney disease, threatened abortion INTERACTIONS - Increased risk of bleeding w/ antiplatelet agents: ASPIRIN; NSAIDS - Increased risk of bleeding w/ RESVERATROL; SAW PALMETTO; GARLIC; GINGER; GLUCOSAMINE; GINKGO BILOBA NURSING ADMIN - Must be given via SUBQ injection or IV infusion - Rotate sites - Monitor for indications of bleeding - Use electric razor - Use soft toothbrush VITAMIN K INHIBITORS (COUMARINS) WARFARIN - Prevention of venous thrombosis and PE - Prevention of thrombotic events w/ a-fib or prosthetic heart valves - Reduce risk of recurrent TIA or MI COMPLICATIONS - Hemorrhage: monitor vitals; observe for bleeding; obtain baseline PT and INR - Warfarin toxicity: admin vitamin K1 - Hepatitis: monitor liver enzymes; assess for jaundice CONTRAINDICATIONS - Pregnancy/breastfeeding - Thrombocytopenia/uncontrollable bleeding - During/following surgeries of eyes; brain; spinal cord; lumbar puncture; regional anesthesia - Clients w/ vitamin K deficiencies; liver disorders; alcohol use disorder - Clients w/ hemophilia; dissecting aneurysm; PUD; severe HTN; threatened abortion INTERACTIONS - Concurrent use of HEPARIN; ASPIRIN; ACETAMINOPHEN; GLUCOCORTICOIDS; SULFONAMIES; PARENTERAL CEPHALOSPORINS, INCREASES RISK OF BLEEDING - Concurrent use of PHENOBARBITAL; CARBAMAZEPINE; PHENYTOIN; ORAL CONTRACEPTIVES; VITAMIN K - Foods high in vitamin K: dark green leafy vegetables, cabbage, broccoli, brussel sprouts, mayo, canola/soybean oil - RESVERATROL, SAW PALMETTO, FEVERFEW, GARLIC, GINGER, GLUCOSAMINE, GINKGO BILOBA NURSING ADMIN - Oral, once daily, same time each day - Baseline vitals - Monitor PT (18-24 sec); INR (2-3) - Baseline/monitor CBC, platelet count, Hct - Have vitamin K for warfarin toxicity - Wear medical alert bracelet - Soft bristle toothbrush and electric razor SKIN CANCER ABCDE TO EVALUATE MOLES - Asymmetry - Borders - Color - Diameter - Evolving AMPUTATIONS: PROVIDING SUPPORT - Allow client/family to grieve for loss of body part/change in body image - Feelings of depression, anger, withdrawal, grief - Asses psychosocial well-being of client; feelings of altered self-concept/self-esteem; willingness and motivation for rehab - Supportive environment BURNS: INDICATIONS OF HYPOVOLEMIC SHOCK - Inadequate perfusion, confusion, hypotension decreased urine output, increased cap refill time; decreased bowel sounds, DM MANAGEMENT: MEDICATION TO WITHOLD PRIOR TO CT SCAN W/ CONTRAST MEDIA - METFORMIN; stop for 24-48 hr before any test w/ contrast dye and restart 48 hr after; can cause lactic acidosis due to acute kidney injury HEARTH FAILURE AND PULMONARY EDEMA: INTERVENTIONS FOR FLUID VOLUME OVERLOAD - High fowlers positioning; O2 admin; rapid acting loop diuretics; medications to improve cardiac output; monitor I/O; daily weights; check abgs and electrolytes; restrict fluid intake; slow/discontinue IV fluids STROKE: ADMIN OF TPA - Give w/i 4.5 hr of initial manifestations for clients experiencing ischemic stroke due to embolic event as evidenced by CT scan results GI THERAPEUTIC PROCEDURES: FINDINGS TO REPORT FOR CLIENT RECEIVING TPN - Metabolic complications: hyperglycemia; hypoglycemia; vitamin deficiencies - Air embolism: sudden onset of dyspnea; chest pain; anxiety; hypoxemia - Infection: observe central line insertion site for infection (erythema; tenderness; exudate) - Fluid imbalance: crackles in lungs/respiratory distress POST OP NURSING CARE: CARING FOR CLIENT FOLLOWING APPENDECTOMY - Airway, breathing, circulation - Vital signs - Positioning - Response to anesthesia (sedation, nausea, vomiting) - Intake/Output - Surgical wound/incision site/dressing - Pain - Mentation NONINFLAMMATORY BOWEL DISORDERS: FINDINGS TO REPORT - HERNIA: report redness or swelling at incisional site - IRITABLE BOWEL SYNDROME: report constipation, fever, increased abdominal pain, fatigue, dark urine, bloody diarrhea, rectal bleeding - INTESTINAL OBSTRUCTION: Dehydration; persistent vomiting; metabolic disturbances; abdominal distention; absent bowel sounds LEGAL RESPONSIBILITIES: WITNESSING INFORMED CONSENT - Ensure provider gave client necessary information; client understood information and is competent to give informed consent; have client sign informed consent document; notify provider if client has more questions or appears not to understand any of the information; document questions client has/notification of provider/reinforcement of teaching/use of interpreter GI THERAPEUTIC PROCEDURES: DISCHARGE TEACHING FOR CLIENT W/ ILEOSTOMY - Foods that cause odor: fish, eggs, asparagus, garlic, beans, dark green leafy vegetables - Foods to decrease odor: buttermilk, cranberry juice, parsley, yogurt - Foods that cause gas: dark green leafy vegetables, beer, carbonated beverages, dairy products, corn, chewing gum, skipping meals, smoking - Foods to decrease gas: yogurt, crackers, toast - Avoid high-fiber foods for the first 2 months after surgery; chew food well; increase fluid intake, and evaluate for evidence of blockage when slowly adding high-fiber foods to diet - Proper fit and maintenance prevent odor when pouch is not open - Filters, deodorizers, or breath mint can be placed in pouch to minimize odor while pouch is open - Discuss feelings about ostomy and concerns about effect on life; look at / touch stoma; ostomy support group HEMODIALYSIS AND PERITONEAL DIALYSIS: MANIFESTATIONS OF PERITONITIS - Cloudy/opaque effluent ANEMIAS: MANIFESTATIONS OF ANEMIA - Pallor, fatigue, somnolence, headache, irritability, numbness/tingling of extremities, dyspnea on exertion, sensitivity to cold, pain/hypoxia (sickle cell crisis) - Shortness of breath/fatigue on exertion, tachycardia and palpitations, dizziness/syncope on standing or exertion, pallor of nail beds/mucous membranes, nail bed deformities (spoon- shaped nails), smooth/sore/bright-red tongue, paresthesia in hands/feet CARDIOVASCULAR AND HEMATOLOGIC DISORDERS: DIETARY TEACHING W/ CLIENT WHO HAS HF - Reduce sodium intake < 3000 mg per day for mild-mod HF, < 2000 mg per day for severe HF - Monitor fluid intake - Increase protein intake to 1.12 g/kg - Use small frequent meals that are soft/easy to chew HEART FAILURE AND POUMONARY EDEMA: TEACHING ABOUT LEFT-SIDED HF - Risk factors: hypertension, CAD, angina, MI, valvular disease - Findings: dyspnea, orthopnea, nocturnal dyspnea, fatigue, displaced apical pulse; S3 (gallop), pulmonary congestion, (dyspnea, cough, bibasilar crackles), frothy sputum, altered mental status, manifestations of organ failure (oliguria), nocturia HIV/AIDS: PRIORITY CLIENT TEACHING - Practice good/frequent hand hygiene - Avoid crowds and travel to countries w/ poor sanitation - Avoid raw foods/undercooked foods - Avoid cleaning pet litter boxes (toxoplasmosis) - Keep home environment clean - Wash dishes in hot water using dishwasher if available - Bathe daily using antimicrobial soap - Adhere to antiretroviral dosing schedules - Conduct frequent follow up monitoring of CD4 and viral load counts - Identify primary support systems - Perform constructive coping mechanisms - Report manifestations of infection immediately to provider BRAIN TUMORS: PHARMACOLOGICAL TREATMENT OF DIABETES INSIDPIDUS - Massive fluid replacement - Admin of synthetic vasopressin - Careful attn to lab values - Replacement of essential nutrients as indicated [Show More]
Last updated: 1 year ago
Preview 1 out of 5 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 19, 2021
Number of pages
5
Written in
Additional information
This document has been written for:
Uploaded
Mar 19, 2021
Downloads
0
Views
67