*NURSING > EXAM > NR511 Midterm Exam_Chamberlain College Of Nursing: Verified Answers( Download To Score An A) (All)
NR511 Midterm Exam_Chamberlain College Of Nursing: Verified Answers( Download To Score An A)
Document Content and Description Below
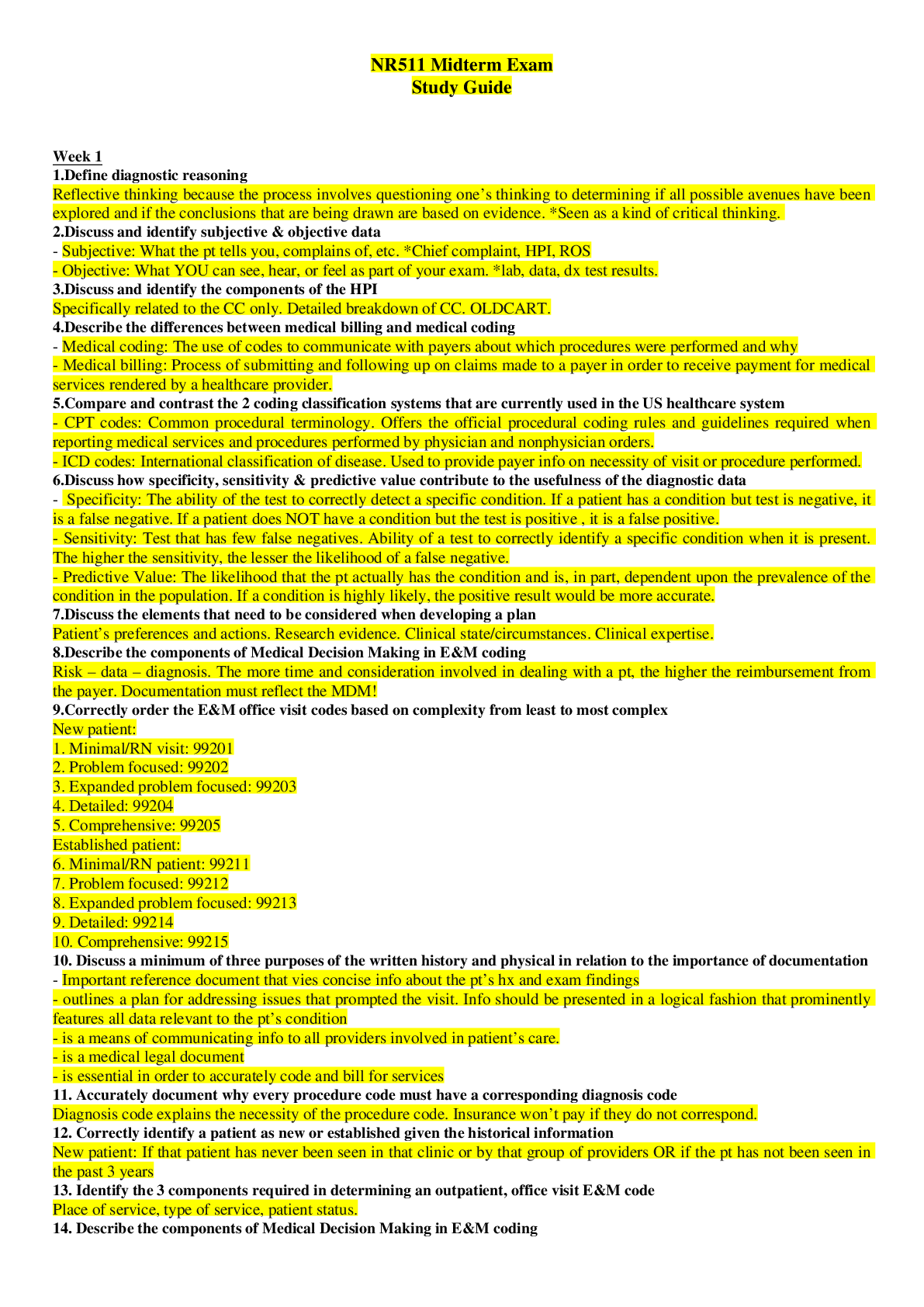
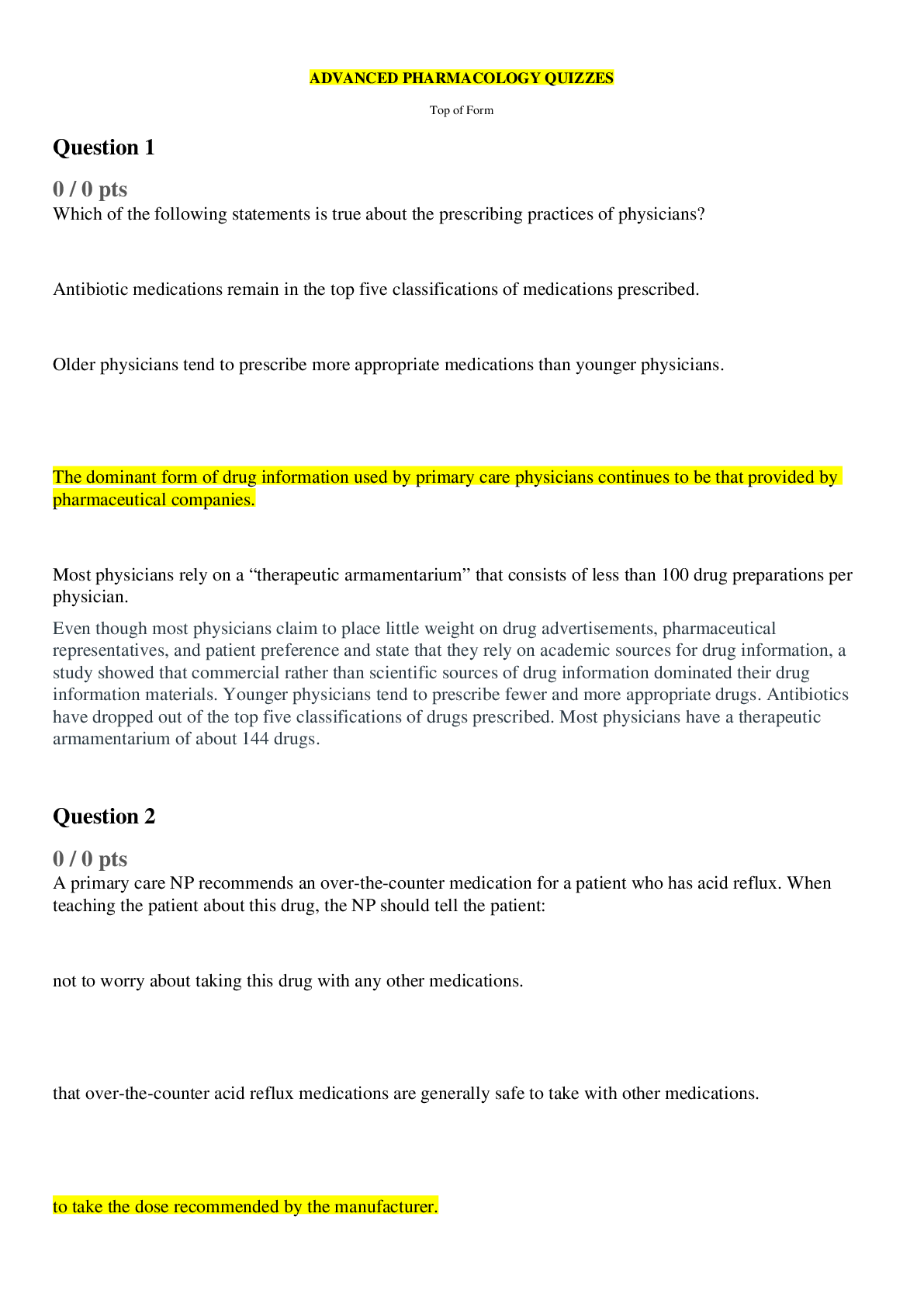
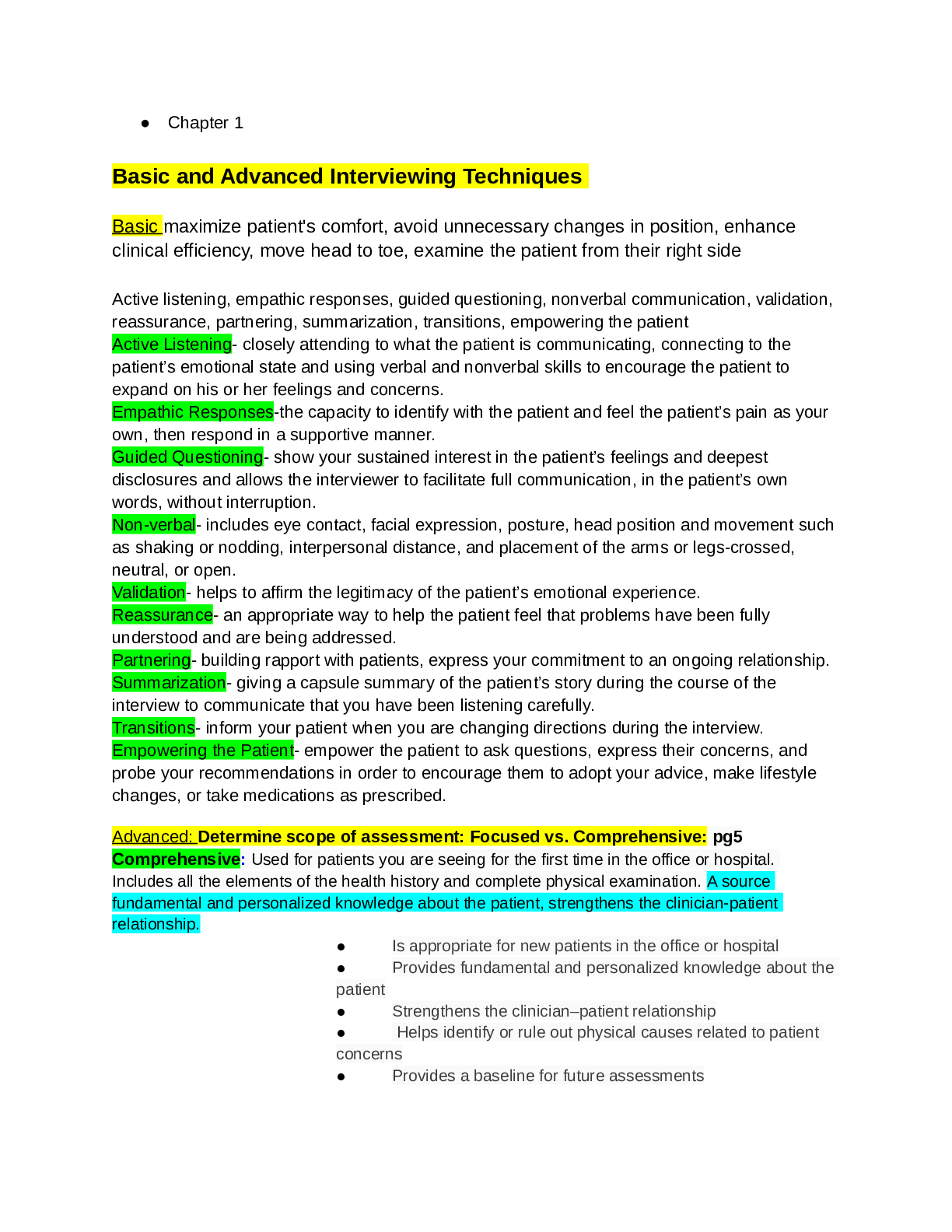
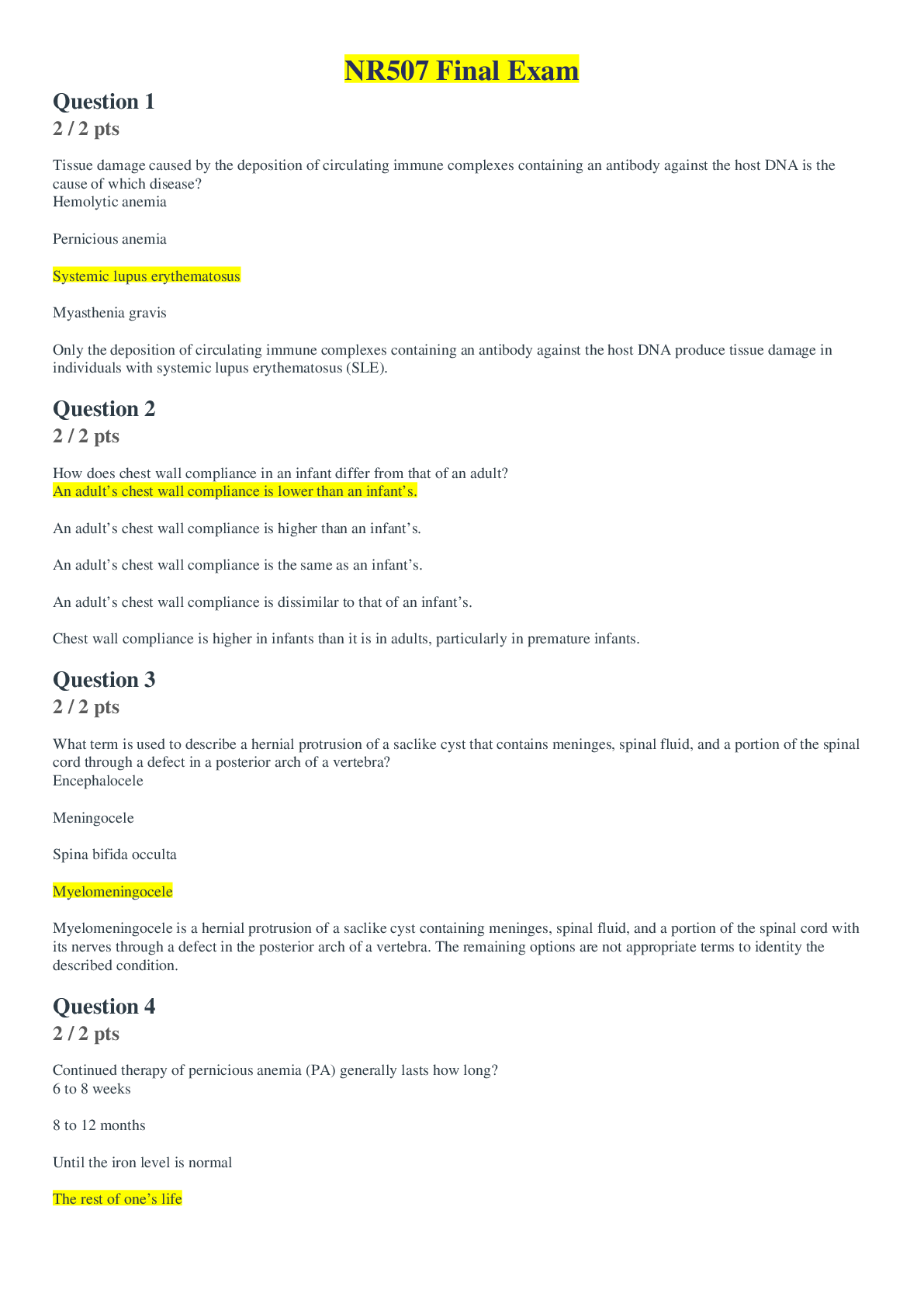
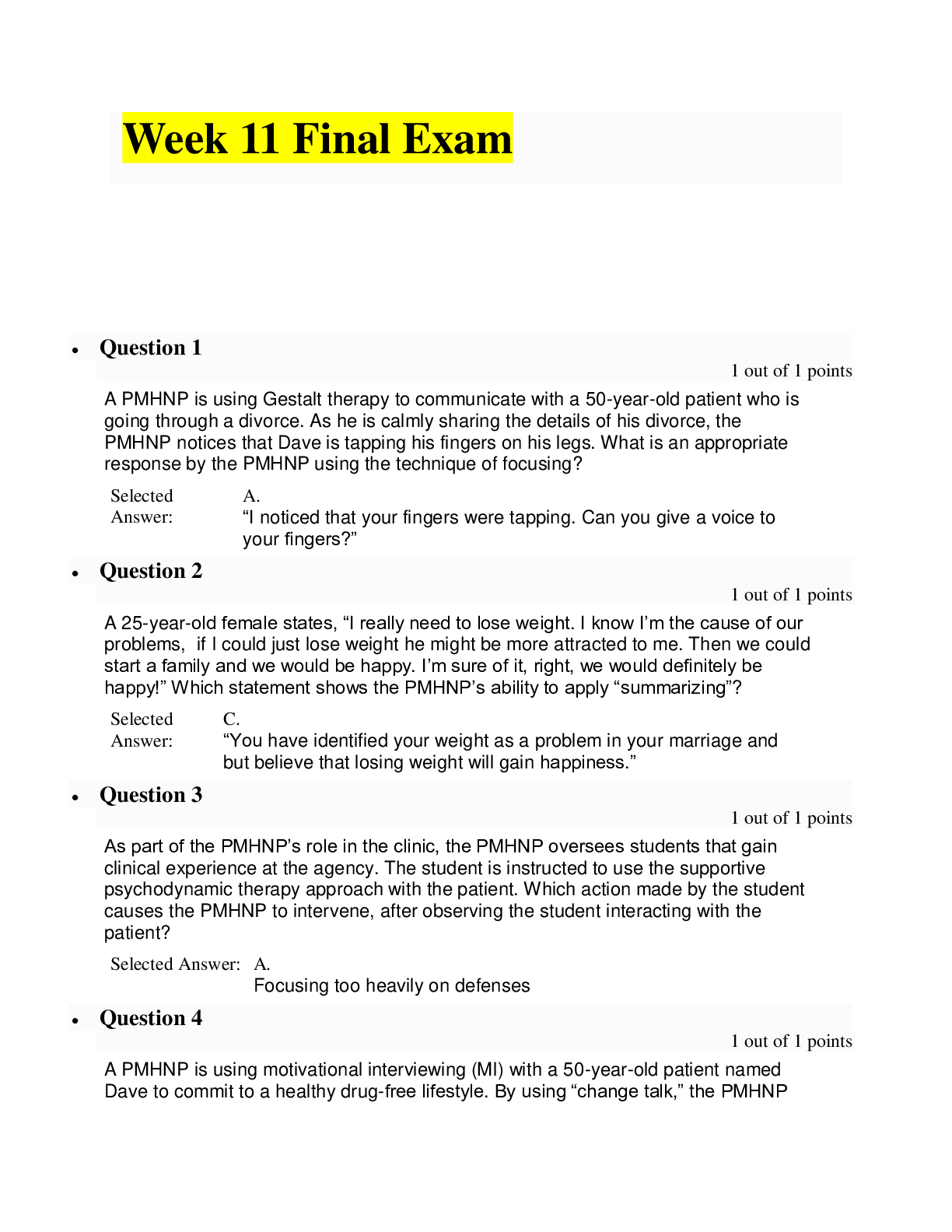
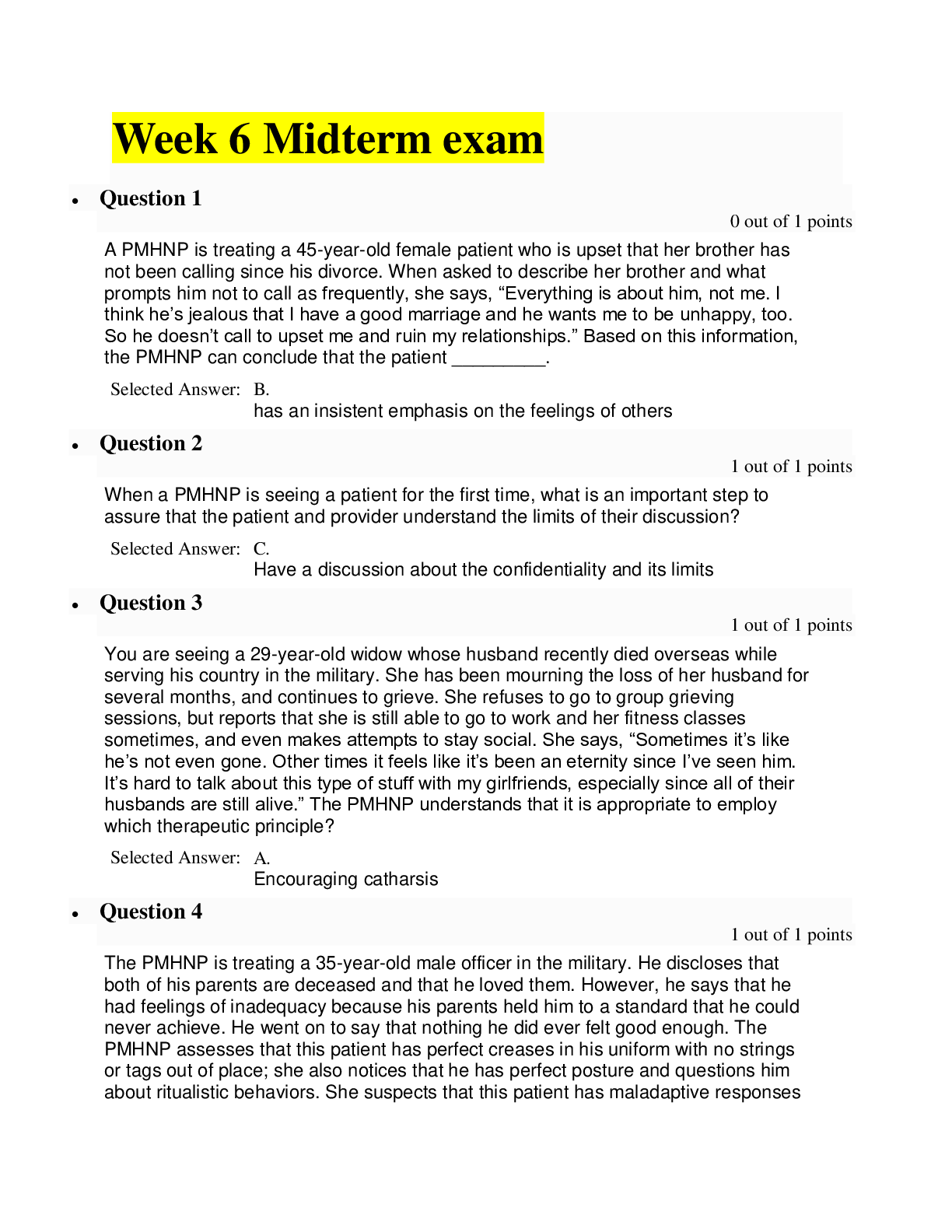
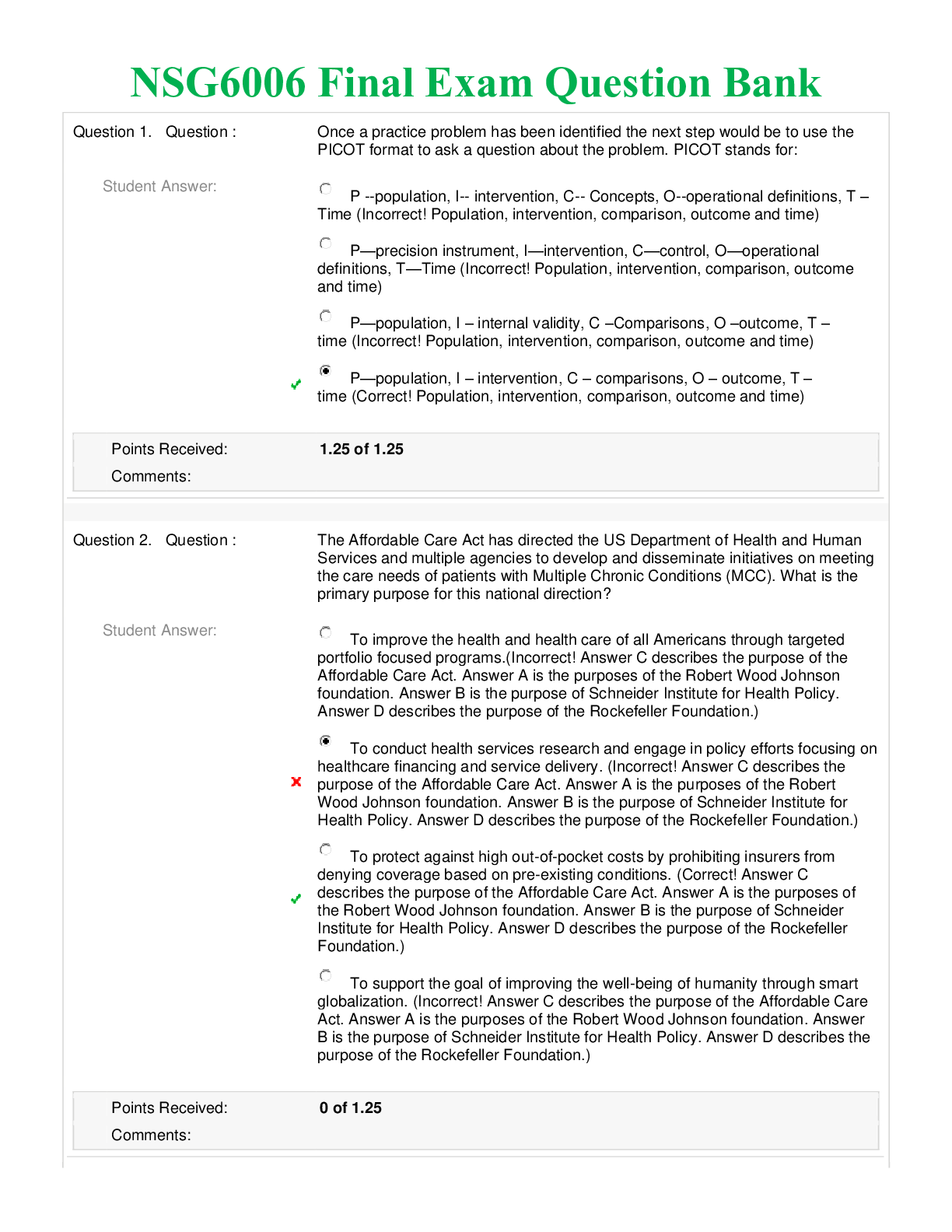
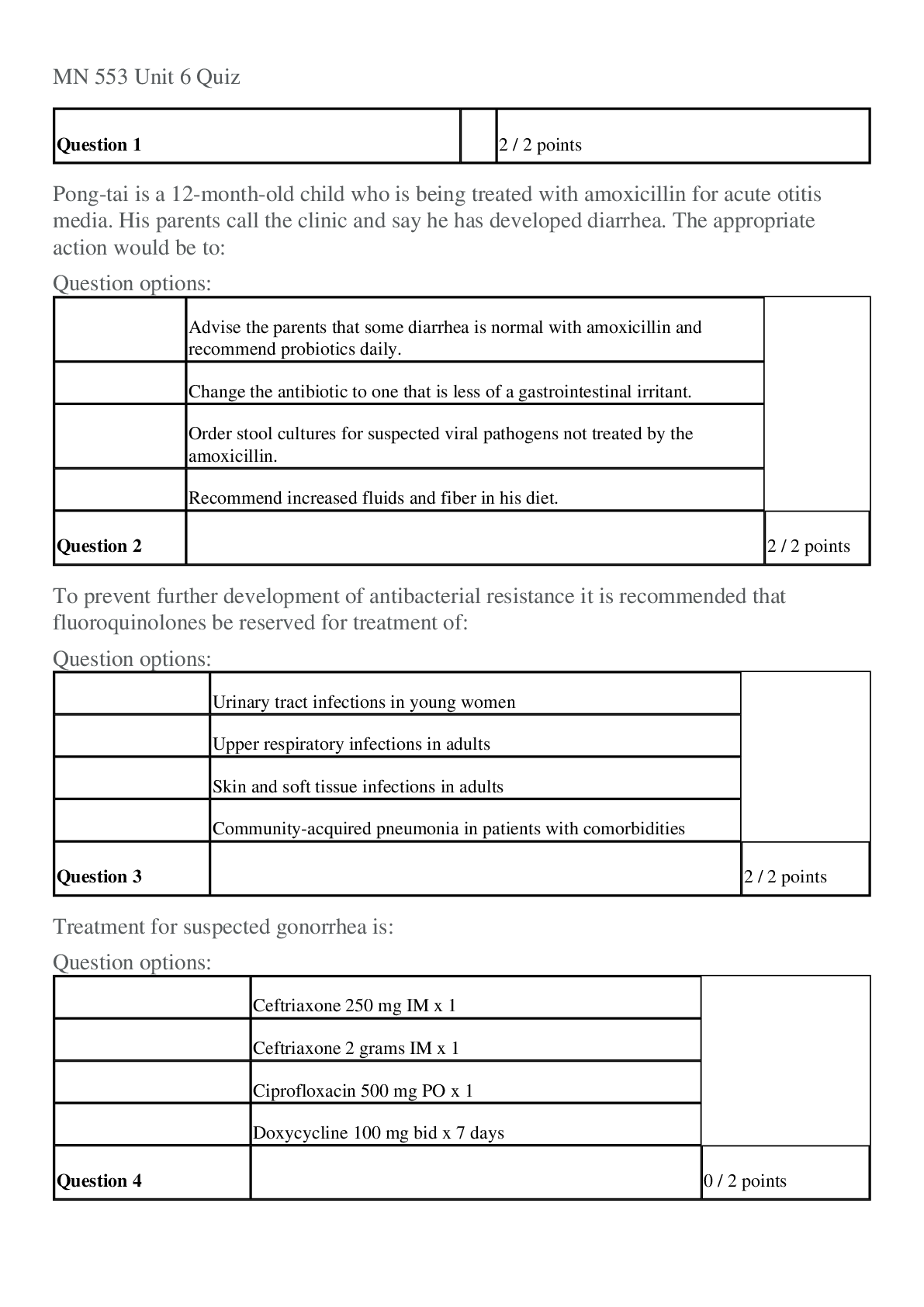
NR511 Midterm Exam Study Guide Week 1 1. Define diagnostic reasoning Reflective thinking because the process involves questioning one’s thinking to determining if all possible avenues have bee... n explored and if the conclusions that are being drawn are based on evidence. *Seen as a kind of critical thinking. 2. Discuss and identify subjective & objective data - Subjective: What the pt tells you, complains of, etc. *Chief complaint, HPI, ROS - Objective: What YOU can see, hear, or feel as part of your exam. *lab, data, dx test results. 3. Discuss and identify the components of the HPI Specifically related to the CC only. Detailed breakdown of CC. OLDCART. 4. Describe the differences between medical billing and medical coding - Medical coding: The use of codes to communicate with payers about which procedures were performed and why - Medical billing: Process of submitting and following up on claims made to a payer in order to receive payment for medical services rendered by a healthcare provider. 5. Compare and contrast the 2 coding classification systems that are currently used in the US healthcare system - CPT codes: Common procedural terminology. Offers the official procedural coding rules and guidelines required when reporting medical services and procedures performed by physician and nonphysician orders. - ICD codes: International classification of disease. Used to provide payer info on necessity of visit or procedure performed. 6. Discuss how specificity, sensitivity & predictive value contribute to the usefulness of the diagnostic data - Specificity: The ability of the test to correctly detect a specific condition. If a patient has a condition but test is negative, it is a false negative. If a patient does NOT have a condition but the test is positive , it is a false positive. - Sensitivity: Test that has few false negatives. Ability of a test to correctly identify a specific condition when it is present. The higher the sensitivity, the lesser the likelihood of a false negative. - Predictive Value: The likelihood that the pt actually has the condition and is, in part, dependent upon the prevalence of the condition in the population. If a condition is highly likely, the positive result would be more accurate. 7. Discuss the elements that need to be considered when developing a plan Patient’s preferences and actions. Research evidence. Clinical state/circumstances. Clinical expertise. 8. Describe the components of Medical Decision Making in E&M coding Risk – data – diagnosis. The more time and consideration involved in dealing with a pt, the higher the reimbursement from the payer. Documentation must reflect the MDM! 9. Correctly order the E&M office visit codes based on complexity from least to most complex New patient: 1. Minimal/RN visit: 99201 2. Problem focused: 99202 3. Expanded problem focused: 99203 4. Detailed: 99204 5. Comprehensive: 99205 Established patient: 6. Minimal/RN patient: 99211 7. Problem focused: 99212 8. Expanded problem focused: 99213 9. Detailed: 99214 10. Comprehensive: 99215 10. Discuss a minimum of three purposes of the written history and physical in relation to the importance of documentation - Important reference document that vies concise info about the pt’s hx and exam findings - outlines a plan for addressing issues that prompted the visit. Info should be presented in a logical fashion that prominently features all data relevant to the pt’s condition - is a means of communicating info to all providers involved in patient’s care. - is a medical legal document - is essential in order to accurately code and bill for services 11. Accurately document why every procedure code must have a corresponding diagnosis code Diagnosis code explains the necessity of the procedure code. Insurance won’t pay if they do not correspond. 12. Correctly identify a patient as new or established given the historical information New patient: If that patient has never been seen in that clinic or by that group of providers OR if the pt has not been seen in the past 3 years 13. Identify the 3 components required in determining an outpatient, office visit E&M code Place of service, type of service, patient status. 14. Describe the components of Medical Decision Making in E&M coding Risk – data – diagnosis 15. Correctly order the E&M office visit codes based on complexity from least to most complex • Repeat of #9? New patient: a. Minimal/RN visit: 99201 b. Problem focused: 99202 c. Expanded problem focused: 99203 d. Detailed: 99204 e. Comprehensive: 99205 Established patient: f. Minimal/RN patient: 99211 g. Problem focused: 99212 h. Expanded problem focused: 99213 i. Detailed: 99214 j. Comprehensive: 99215 16. Explain what a “well rounded” clinical experience means Includes seeing kids from birth through young adult visits for well child and acute visits as well as adults for wellness or acute/routine visits. Seeing a variety of patients including 15% of peds and 15% of women’s health of total time in the program. 17. State the maximum number of hours that time can be spent “rounding” in a facility No more than 25% of total practicum hours in the program 18. State 9 things that must be documented when inputting data into clinical encounter 1. Date of service 2. Age 3. Gender and Ethnicity 4. Visit E&M code 5. CC 6. Procedures 7. Tests performed and ordered 8. Dx 9. Level of involvement (mostly student, mostly preceptor, together, etc.) 19. Identify and explain each part of the acronym SNAPPS - Summarize: present the pt’s H&P findings - Narrow: based on the H&P findings, narrow down to the top 2-3 differentials - Analyze: analyze the differentials. Compare and contrast H&P findings for each of the differentials and narrow it down to the most likely one. - Probe: ask the preceptor questions of anything you are unsure of. - Plan: come up with a specific management plan - Self-directed learning: an opportunity to investigate more about any topics that you are uncertain of. Week 2 1. Identify the most common type of pathogen responsible for acute gastroenteritis Bacteria: Staphylococcus Viral: Norovirus (Norwalk virus) in adults and Rotavirus in Peds up to 2 yrs old. 2. Recognize that assessing for prior antibiotic use is a critical part of the history in patients presenting with diarrhea Due to Risk for C Diff infection 3. Describe the difference between Irritable Bowel Disease (IBS) and Inflammatory Bowel Disorder (IBD) IBS (Irritable Bowel Disease) ○ a disorder of bowel function, not from anatomic abnormality; ○ characterized by alternating bowel pattern, constipation and diarrhea; ○ associated symptoms include abdo pain relieved w/defecation, bloating, rectal urgency w/diarrhea; ○ Extra-intestinal symptoms: pain on intercourse or lack of libido, muscles aches&pain, fatigue, fibromyalgia syndrome, headache, back pain, urinary symptoms (urgency, hesitancy, bladder spasm); ○ Not associated with serious medical consequences; tend to live long; ○ Does not put stress on other organs (heart, liver, kidney) ○ Major problem of IBS: the quality of life that people suffer Inflammatory Bowel Disorder (IBD) ● A chronic immunological disease that manifests in intestinal inflammation. ● Characterized by exacerbations and remissions throughout lifetime. ● UC and CD -- most common 4. Discuss two common Inflammatory Bowel Diseases Ulcerative colitis (UC): ● the thinner mucosa of the rectum and sigmoid colon become inflamed, which results in friability, erosions, and bleeding. ● More in male (age 10-40) ● Involved in the rectosigmoid areas, crypt abscess development ● Sx: bleeding, cramping, urge to defecate d/t mucosa destruction ● Tenderness LLQ or across the entire abdomen, often accompanied by guarding and abdo distension; ● Stools --watery diarrhea w/ blood and mucus d/t loss of absorptive surface ○ Fecal leukocytes almost always present ○ Mild form < 4 BM per day, relieved w/defecation, no associated systemic sx ○ Moderate (4-6 BM/day), ↑ blood and mucus, systemic sx (tachy, fever, wt loss) ○ Severe -- (6-10/day), abdo tenderness, symptoms of anemia, hypovolemia, and impaired nutrition, --risk for perf colon Crohn’s disease (CD): ● An inflammatory process that begins in the submucosa of the intestine and gradually spreads to involve the mucosa and serosa. ● Can involve all or any layer of the bowel wall and portion of GI tract from mouth to anus (about 80% small bowel involvement and 20% of the colon). ● More in female (age 15-25, 50-80) ● Greater risk for colorectal cancer ● Skipped lesions --some haustral segments are affected while others are not. ● cobblestone appearance--inflamed tissue is surrounded by scar tissue. ● Transmural inflammation -- serosal inflammation cause bowel loops to adhere to one another leads to obstruction, fistulas, and shortening of the bowel. ● Tenderness RLQ or mass ● Sx: abdo cramping, fever, anorexia, weight loss, spasm, flatulence, ● Stools contain blood, mucus, and/or pus ● Symptoms tend to increase during stress or after meals consisting of poorly tolerated fatty, spicy, or dairy. ● Steatorrhea- fatty stools d/t insufficient absorption of bile salt ● 5. Discuss the diagnosis of diverticulitis, risk factors, and treatments - Diagnosis = occurs when a patient’s diverticulosis becomes inflamed and when the projection becomes eroded it can progress to the point of eruption causing left lower quad pain and tenderness, fever, change in bowel habits (usually diarrhea), N/V, mass, rebound tenderness with involuntary guarding and rigidity, occult blood. If there is a fistula, UA may show increased WBC and RBC, urine culture may be positive. - Risk Factors = low fiber diet, hypertrophy of the segments of the circular muscle of the colon, chronic constipation and straining, irregular and uncoordinated bowel contractions, obesity, and weakness of the bowel muscle brought on by aging. Directly related to the suspected causes of the disease: older than age 40, low-fiber diet, previous diverticulitis, and the number of diverticula present in the colon. - Treatments = metronidazole 500mg TID x 10-14 days along with Ciprofloxacin 500mg BID or trimethoprim/sulfamethoxazole DS 160/800 BID. Close office follow up should occur upon completion of abx therapy as complications such as abscess and perforation can occur. 6. Identify the significance of Barrett’s esophagus Thought to be caused by chronic GERD. Gastric contents are so irritating, an inflammatory response is established in the esophagus. Erosion occurs due to increased blood flow due to inflammation. As the erosion heals, the body replaces the normal squamous epithelium with metaplastic columnar epithelium (Barrett’s epithelium) containing goblet and columnar cells. These are more resistant to acid and support esophageal healing. Barrett’s epithelium is a premalignant tissue, and presents a 40 fold increased risk for esophageal adenocarcinoma. Fibrosis and scarring occur, leading to esophageal strictures. 7. Discuss the diagnosis of GERD, risk factors, and treatments o Clinical characteristics of GERD: • Heartburn, Regurgitation, Water brash (reflex salivation), Dysphagia, Sour taste in mouth in the morning, Odynophagia (painful swallowing), Belching, Coughing, Hoarseness, Wheezing usually at night, Substernal or retrosternal chest pain, Aggravating: reclining after eating, eating large meal, alcohol, chocolate, caffeine, fatty/spicy food, nicotine, constrictive clothes, heavy lifting, straining, bending over. Alleviating: antacids, sitting upright after meal, eating small meals o Treatment for GERD: • 1st line: life modification (elevate HOB, smoking cessation, avoid high fat/large meals, chocolate, ETOH, peppermint, caffeine, onions, garlic, citrus, tomatoes); don't sleep 3-4hrs after meal, avoid bedtime snack. Meds: avoid Ca blockers, beta blockers, alpha adrenergic agonists, theophylline, nitrates, some sedatives. Encourage wt loss for overweight/obese pts If lifestyle mods not working: step-up/down treatment guidelines for GERD. Mild, intermittent symptoms: trial for 4wks, if symptoms persist, step up: 1. Dietary/lifestyle mods 2. Antacid 3. OTC H2-RA: cimetidine (Tagamet), ranitidine (Zantac), famotidine (Pepcid), nizatidine (Axid) Trial above for 6wks, if symptoms persist, step up +referral to GI: 1. Continue dietary/life mods 2. H2-RA Rx dosage: cimetidine 800mg TID, ranitidine 150mg TID, nizatidine 150mg TID, famotidine 20mg TID. OR PPI: omeprazole 20mg, rabeprazole 20mg, lansoprazole 30mg, esomeprazole 20mg, or pantoprazole 40mg daily. Trial above for 8wks, if symptoms persist step up: 1. Diet/lifestyle mods: 2. PPI increase to 40mg daily Trial for 8wks, if symptoms persist, step up: 1. Diet/lifestyle mods: 2. Surgical intervention Characteristics of AGE (acute gastroenteritis): Nausea,Vomiting, Diarrhea, Fever, Abd pain/cramping, Fatigue, Malaise, Anorexia Tenesmus, Rectal burning d/t frequent diarrhea, Rectal abrasion, Rectal bleeding Passing stool w/blood and mucus, Severe dehydration, Increased HR, Dizziness Treatment for AGE: Fluid and diet PO pts: Pedialyte, gatorade, oral rehydration salts, sports drinks, diluted fruit juices, broths, soups. Boiled starches/cereals to facilitate enterocyte renewal Hosp pts: IV fluid Diarrhea: Pepto (can be used to treat acute diarrhea, but not as effective as loperamide; don't use w/abx in pts with HIV) Loperamide (Imodium): drug of choice for afebrile, nondysenteric cases of acute diarrhea Lomotil: Rx only, used in afebrile, nondysentery of acute diarrhea, has central opiate effects. Antibiotic treatments: Bacterial: C-diff (metronidazole/Flagyl 250mg x4 daily x10 days; vanc 125mg x4 daily x10 days). Vibrio cholerae (tetracycline 500mg PO q5hr x2 days; bactrim DS q12hr x2 days). Yersinia enterocolitica (tetracyclines 250-500mg q6hr x7-10days; cipro 500mg BID; tobramycin 3-5mg/kg q8h). Salmonella (Bactrim DS or quinoline, norfloxin 400mg or ofloxin 400mg x2 daily x7-10 days). Shigella (Bactrim DS BID x3 days) Viral: Rotavirus/norwalk virus: no treatment, treat symptoms 8. Discuss the differential diagnosis of acute abdominal pain, work-up and testing, treatments Abdominal pain is one of the most common complaints for which people seek medical attention The mechanism responsible for the abdominal pain is what gives certain characteristics to the pain. ● Visceral pain (poorly localized and is described as dull) and is caused by distention or spasm of a hollow viscus. ○ Distention of an organ capsule, such as Glisson’s capsule around the liver; vascular compromise; and mucosal irritations cause pain that is visceral in nature. ● Parietal pain, described as sharp and well localized, is caused by irritation of the peritoneum. ○ Appendicitis often causes this type of pain as the peritoneum becomes involved. ● Abdominal pain described as colicky, which simply means that it comes and goes ○ may result from gallstones or renal stones. ● Burning pain, caused by irritation of the gastric mucosa by gastric contents ○ associated with peptic ulcers and esophagitis. Differential Diagnosis Flowchart 11.1 presents selected causes of abdominal pain and their characteristics. Treatment of abdominal pain depends on the cause. (This flow chart is amazing and there is no way to copy it in here) All patients with abdominal pain should undergo rectal, genital, and pelvic evaluations. Blood found in the stool or intense pain on examination may indicate more serious conditions. Tests: A complete blood count, serum chemistries, liver function tests, urinalysis, pregnancy test, and abdominal films will help determine the acuity of the problem (Dunphy 505-509) 9. Discuss the difference between sensorineural and conductive hearing loss Conductive hearing loss: often reversible occurs when a change, obstruction, lesion in the outer or middle ear that impairs sound from the outer to the inner ear. Interference in air conduction. Can be caused by occlusion from cerumen, FB, tumors of CA in the middle or external ear (typically neuro changes), or ET tube dysfunction, OM, cholesteatoma (abnormal non cancerous skin growth), tympanosclerosis or otosclerosis (abnormal immobility of the stapes footplate from sclerotic bone; occurs in young adults 20-40), temporal bone fractures from trauma. S/S: diminished hearing, soft voice, py hears better in a noisy environment (paracusia willisiana) (McCance & Huether, 2013) Sensorineural: Often irreversible; Impairment/degeneration of hair cells in the organ of corti (inner ear), affecting CN 8; gradual or sudden. Causes: congenital, hereditary, noise exposure, menieres disease, AGE (presbycusis), ototoxicity, systemic disease (SLE, DM, syphilis, Paget disease), hypothyroidism, viral syndromes (mumps); congenital caused by maternal rubella, ototoxic drugs, prematurity, traumatic birth, erythroblastosis fetalis (dx with delayed speech for children). Presbycusis: age related sensorineural hearing loss and is most common type and cannot hear high frequencies and is gradual onset that eventually impacts low frequencies. Abx and lasix are linked to hearing loss and symptoms begin with tinnitus, hearing loss from this is permanent (McCance & Huether, 2013). Presentation: Hearing loss may be mixed, prevalence of hearing loss increases after 40 yo, men are likely than women, 90% of pts with hearing loss experience tinnitus (noises heard by pt when none present in environment). *use weber, rinne and schwabach tests to differentiate, assess ear/TM for abnormalities 10. Identify the triad of symptoms associated with Meniere's disease Tinnitus, Hearing loss, and vertigo fluctuating , unilateral, assoc with tinnitus and vertigo. 11. Identify the symptoms associated with peritonsillar abscess Tammy Tunis Almost always unilateral, located between tonsil and superior pharyngeal constrictor muscle Gradual onset of severe unilateral sore throat Odynophagia, Fever, Otalgia, Asymmetric cervical adenopathy, Pronounced trismus (hot potato voice) Toxic appearance (poor/absent eye contact, failure to recognize parents, irritability, inability to be consoled/distracted, drooling, severe halitosis, tonsillar erythema, exudates) Swelling above affected tonsil with a discrete bulge, deviation of soft palate/uvula 12. Identify the most common cause of viral pharyngitis Adenovirus: Mononucleosis (Epstein-Barr):HSV-1:RSV:Flu A&B: Coxsackie: Enteroviruses 13. Identify the most common cause of acute nausea & vomiting Acute gastroenteritis 14. Discuss the importance of obtaining an abdominal xray to rule out perforation or obstruction even though the diagnosis of diverticulitis can be made clinically All pt’s should get an abd xray to look for free air which indicates perforation, ileus, or obstruction. CT scan with oral or IV contrast would be accurate. Mild-moderate leukocytosis, WBC is usually normal. 15. Discuss colon cancer screening recommendations relative to certain populations Colon Cancer Screening Recommended by the American Cancer Society Risk Screening Recommendations Average risk Annual fecal occult blood (FOB) test Flexible sigmoidoscopy every 5 years beginning at age 50 or colonoscopy every 10 years High risk (general) Annual FOB testing Double-contrast barium enema OR Colonoscopy every 3–5 years starting at age 40 Specific High-Risk Groups Prior colorectal cancer Colonoscopy 1 year postfinding, then every 3 years Hereditary nonpolyposis colorectal cancers Colonoscopy screening must begin 10 years before the age at onset of the earliest affected family member OR Colonoscopy every 1–2 years beginning at age 20–25 and continuing until age 35 and then yearly Inflammatory bowel disease Annual colonoscopy beginning 8 years after onset of disease First-degree family history Colonoscopy every 3–5 years beginning 5 years before the age at onset of the youngest affected relative (Dunphy, p. 590) 16. Identify at least two disorders that are considered to be disorders related to conductive hearing loss Cerumen impaction,chronic otitis externa, middle ear effusion, AOM (acute otitis media), tympanic membrane rupture or perf 17. Identify the most common bacterial cause of pharyngitis : Group A Beta Hemolytic Streptococcus (GABHS) Identify treatment options for Group A B-hemolytic streptococcal pharyngitis o PCN is treatment of choice for GAS pharyngitis b/c of its efficacy, safety, narrow spectrum, and low cost. PCN is only abx that has been studied and shown to reduce rates of acute rheumatic fever. For most adult pts: Pen V 500mg BID-TID x10 days. For most kids: Pen V or amox. Alternatives for those with PCN allergies: 1st gen cephs, erythromycin, clinda, clarithromycin, azithromycin. 18. Identify the clinical findings associated with mononucleosis: Gradual onset of fever, MARKED MALAISE (The child doesn’t even want to get out of bed!). Severe sore throat, may have extensive tonsillitis, palatal petechiae/rash, anterior/posterior cervical adenopathy( FOR OUR BOARD EXAM REMEMBER THAT POSTERIOR CERVICAL NODE ENLARGEMENT IS CLASSIC). Splenic enlargement (NO CONTACT SPORTS). 19. Identify common characteristics in a rash caused be Group A Strep These turn into a fine pink-red rash that looks like sunburn. The skin feels rough when touched, like sandpaper. The rash spreads to the ears, neck, elbows, inner thighs and groin, chest, and other parts of the body (google, 2018 ;)). 20. Discuss that the diagnosis of streptococcal pharyngitis can be made clinically based on the Centor criteria: Fever greater than 38 Celsius, NO COUGH, tender anterior cervical lymphadenopathy, pharyngotonsillar exudate. The presence of FOUR strongly suggest GABHS infection. THREE or MORE present: Should empirically diagnose and treat without further testing. RAPID STREP TESTS ARE NOT CHEAP!! The treatment for GABHS is PCN V 500 mg BID-TID for 10 days. Alternatives if PCN allergic are Macrolides, Clinda, and 1st gen cephalosporins. 21. Describe an intervention for a patient with gastroenteritis - Avoid dehydration with fluid and electrolyte management (particularly with children, older adults, and immunocompromised patients). (From powerpoint lecture). - Oral rehydration: fluids with sodium content of 45-75 mEq/L (Pedialyte or Gatorade), broths, soups, fruit juices. IV rehydration: severe dehydration or patients with chronic diseases and are hypotensive. (from page 535-536). - Stool samples for prolonged diarrhea, fever >= 38.5C, bloody stools, or +leucocytes. (from powerpoint lecture). 22. Discuss an appropriate treatment for prophylaxis or treatment of traveler's diarrhea Patients traveling high risk areas are instructed to consume only safe food and beverages thre and on the airplaine leaving the area. Safe foods include acidic foods (unpeeled citrus food, dry foods( bread/cerea), steamed foods and beverages (coffee, tea, cooked vegetables), foods containing sugars (syrups, jellies, jams) bottled carbonated drinks (soda, beer). Not considered to safe to drink bottled water (unless from safe area) eat raw (salad). Patients with HIV infection or dilibilating illness should be encouraged to take prophylaxis antibiotics. 23. Identify at least one effective treatment for Irritable Bowel Syndrome (IBS) IBD treatment = 5-aminosalicylic acid agents, antidiarrheals (but not in UC!), steroid therapies such as prednisone or hydrocortisone if 5-asa do not work, immunomodulators such as azathioprine, methotrexate, and 6-mercaptopurine, anti-tumor necrosis factor therapy “biologics” include medications such as remicade, humira, and entyvio for mod-sever disease. (from powerpoint lecture). 24. Identify at least one prescription medication for the treatment of chronic constipation Linzess (linaclotide), trulance (plecanatide), Amitiza (lubiprostone). These work by acting locally on the atypical membrane of the GI tract to increase intestinal fluid secretion and improve fecal transabdominal pain caused by intestinal spasm and be controlled by antispasmodic agents (from powerpoint lecture). 25. Discuss at least one treatment for Meniere's disease Peripheral sensory disorder for both labyrinth and chochlea of inner ear. Resulting in vestibular (proprioceptive/balance) and auditory dysfunction ( tinnitus, vertigo, hearing loss). Risk factors: high in salt intake, exposure to high noise for periods. Inflammatory response of inner ear to variety of insults (trauma, viral infection, allergies, reduced/negative middle ear pressure, vascular/endocrine/lipid disorders).Tx: calm bedrest with closed eyes and protection from falling when acute attacks happen (< 4 hrs). Treatment is directed symptomatic relief since no medication known to affect this disease process. Low salt diet, mild diuretic ( chlorothiazide 500mg /day [Diuril]) with K supplement (---> reduces the endolymphatic pressure/volume (inner ear), No caffeine and tobacco cessation (to avoid vasoconstriction of labyrinthin system).Acute attacks are managed with combo of antimuscarinic or anticholinergics and vestibulosuppressive H 1 blockers. Meclizine, Promethazine, Dimenhydrinate, Diphenhydramine, or Metoclopramide are also advocated. Week 3 1. Discuss that the majority of dyspnea complaints are due to cardiac or pulmonary decompensation- The most common subjective dyspnea complaints are SOB, DIB, “can’t get enough air”, suffocation or smothering, air hunger and winded. The most common causes of cardiopulmonary decompensations are asthma, COPD, malignancy, Heart Failure, Interstitial Lung Disease, Pneumonia, Valve disorder, Intracardiac shunts, MI, Cardiomyopathies. 2. Explain the differences between intra-thorax and extra-thorax flow disorders Classifications of dyspnea disorders can be classified as Flow or Volume, either intra-thrax or extra-thorax. Flow/Intra-thorax- Obstruction of the distal airway. Flow/Extra-thorax- Obstruction of the proximal/larger airway. Volume/Intra-Thorax- Lung parenchyma disorders. Volume/Extra-thorax- Lung compliance disorders, respiratory center disorders. 3. Identify at least three examples of flow and volume disorders (intra and/or extra thorax) Flow/Intra-thorax- asthma, bronchiolitis, lymph node enlargement, solid foreign body aspiration- Causes expiratory effort in infants and children less than 5. Flow/Extra-thorax- rhinitis with nasal obstruction, cranial-facial malformation, sleep apnea, tonsil-adenoid hypertrophy, diphtheria, croup and epiglottitis- Causes inspiratory stridor in infants and children 5 and under. Volume/Intra-thorax (pulmonary)- pneumonia, atelectasis, pulmonary edema, near-drowning, sepsis- causes inspiratory effort. Volume/Extra-thorax (lung compliance)- neuromuscular disease, obesity, gastritis/peptic ulcer, ascites- causes inspiratory constraint. Volume/ Extra-thorax (pulmonary)- pneumothorax, cardiomegaly, heart failure, chest trauma such as rib fracture or lung contusion, thorax deformity such as pectus excavation or scoliosis- Causes inspiratory effort. Volume/Extra-thorax (Respiratory Center Disorders)- anemia, metabolic acidosis, meningitis, poisoning or salicylate or alcohol ingestion- Causes deep, rapid breathing. 4. Discuss diagnosis, risk factors and treatments for asthma-****needs completed**** Describe the classes of asthma and treatments for each category Diagnosis- Essential elements to consider- HX- cough (especially nocturnal), recurrent wheeze, recurrent episodic dyspnea, recurrent chest tightness Symptoms worsen in relation to specific factors- changes in weather, exercise, environmental allergens, GERD, Beta blockers, sensitivity to ASA, strong emotional expression To establish the diagnosis of asthma, episodic symptoms of airflow obstruction must be present, airflow obstruction must be at least partially reversible, and must rule out other diagnoses. Spirometry measurements are helpful in diagnosis & in evaluation of management The diagnosis is made by demonstrating the reversibility of the airway obstruction from the pre- and post- PFTs. Reversibility is defined as a 15% or greater increase in the FEV1 after 2 puffs of a beta-adrenergic agonist have been inhaled. When spirometry is non-diagnostic, bronchial provocation testing maybe useful with histamine, methacholine, or exercise. Risk Factors Family or personal history- allergic rhinitis, eczema/atopic diseases Residing in urban area Exposure to smoke or air pollution Cockroaches and dust Viral respiratory infections Cold air intolerance obesity Classifications of Asthma Severity Mild Intermittent Symptoms < 2 days per week OR < 2 nights per month. Exacerbations brief Mild Persistent Symptoms > 2 times per week, but not daily; OR 3-4 times per month at nighttime Moderate Persistent Daily symptoms OR >1 night per week but not nightly Severe persistent Symptoms throughout the day; often 7 nights per week Pharmacological Management *Short acting bronchodilator (albuterol) is a mainstay of treatment for ALL asthma patients Intermittent Short-acting bronchodilator (albuterol): for exacerbations (inhaled or nebulized) Mild Persistent Short acting bronchodilator + Preferred tx- Low-dose inhaled corticosteroids (fluticasone/Flovent, budesonide/Pulmicort, mometasone/asmanex Moderate Persistent Short acting bronchodilator + Preferred tx- low to medium dose inhaled corticosteroid AND Long acting inhaled bronchodilator (salmeterol/serevent, formoterol/Foradil) Alternative tx-low to med dose inh. Corticosteroid AND Either leukotriene blocker (Montelukast/singulair) OR theophylline Severe Persistent Short acting bronchodilator + High dose inhaled corticosteroids AND Long acting inhaled bronchodilator AND If needed, oral corticosteroids (2mg/kg/day, 60mg/day max) 5. Describe appropriate tests in the work up for dyspnea- Appropriate diagnostic tests should be ordered after medical history and physical exam have been completed. Chest X-Ray- Look for tumors, TB, pneumonia. CBC with diff- Rule out anemia or infection. Peak Expiratory Flow Test- determine degree of air flow in COPD and asthma. EKG- look at cardiac activity. Spirometry- Determine obstructive, reactive or mixed. 6. Discuss clinical findings and PFTs for asthma, chronic bronchitis, emphysema, and COPD chronic bronchitis. Characterized by excessive mucus secretion in bronchial tree Manifests by chronic or recurrent cough (with or without sputum), present on most days for minimum of 3mo of the year for at least 2 consecutive years. Pts usually use accessory muscles with respiration and have dyspnea with or whitout sheezing. Pts may have s/s of right HF (edema, cyanosis). FVC: normal to increased::RV: increased TLC: normal::EFR: normal to decreased::FEV1/FVC: decreased asthma. Chronic, inflammatory, obstructive disease in airways. May occur at any age and presents with wheezing (airway spasms), chest tightness, dyspnea, cough. Reversible hyperreactivity of bronchi and bronchioles to a variety of stimuli. FVC: normal::RV: normal, increased during attacks::TLC: normal to increased EFR: normal to decreased::FEV1/FVC: normal to decreased COPD. Progressive disease characterized by presence of airflow obstruction due to chronic bronchitis or emphysema. 3rd leading COD in US. Dz of lung parenchyma and small airways Pts may be asymptomatic for 10-20yrs except for frequent colds, persistent morning cough, URIs. Pts present with fatigue, SOB, cough, hyperinflation (barrel chest), wheezing, decreased breath sounds, hyperresonance. Stage 1 (mild): FEV >80%.:: Stage 2 (moderate): FEV 50-79% Stage 3 (severe): FEV 30-49%::Stage 4 (very severe): FEV <30% Emphysema 7. Differentiate between the following common rashes: rubeola, rubella, varicella, roseola, 5ths disease, pityriasis rosea, hand, foot and mouth disease and molluscum contagiosum. Rubeola-(measles, 9 day measles, 1st disease) Acute highly contagious viral characterized by fever, cough, coryza & conjunctivitis followed by maculopapular rash starts in face and spreads cephalocaudally (head) & centrifugally (trunk).Transmitted direct contact with droplets.Caused by Morbillivirus. RF: Children <5 & adults>20yrs, pregnant women, immunocompromised persons, malnutrition, Vit A deficiency,international travelers. Incubation 7-14 days from exposure. Rubella:German measles or 3-day measles.Caused by rubella virus.Rash may start 2wks after exposure, spread from respiratory droplets.Low-grade fever, HA, sore throat, rhinorrhea, malaise, eye pain, myalgia 2-5 days before rash (may last weeks after outbreak).Skin rash: rose-pink macules and papules, first on head, travel down body. Fades in 1-2 days in same order they appeared.Tx: symptomatic (apap, NSAIDs, rest). Rubella vaccination.Infectious 4-7 days before rash, can return to work/school after rash gone. Varicella: chicken pox.Very contagious.Caused by varicella zoster virus (VZV). Malaise, fever, chills, HA, arthralgia, then 1-2 days later urticarial erythematous macules and papules appear, quickly turning into vesicles and pustules. Rash starts on face/chest, spreads quickly over entire body. Blisters can be in ear canal or mouth. Dry up in 1wk.Tx: symptomatic (oral antihistamines, NSAIDs, cool compresses, oatmeal baths).Varicella vaccination.Contagious 2-3 days before rash, can return to work/school after lesions scabbed over Roseola: 6th disease Caused by human herpes virus types 6 and 7.Virus usually mild, common in children under age 2.Spread through saliva.Short-lived, 3-5 days.High fever, irritability, diarrhea, cough, cervical lymphadenopathy.Rash: light pink, erythematous macules and papules on face, neck, extremities. Usually resolves in 1-3 days.Dx based on clinical presentation and history.Tx: symptomatic.Contagious 1-2 days before fever, can return to work/school when fever, fatigue, cough, diarrhea gone. 5ths Disease: erythema infectiosum, human parvovirus.Spread through respiratory drops, blood products.3 stages: HA, fever/chills, possible cough, classic slapped cheek rash, bright red bilat cheeks (not forehead, nasal bridge, perioral area); pink lacy (reticulated) erythematous macules on all extremities and trunk (not palms, sole surfaces), may be itchy; 2-3wks of body rashDx can be made via blood test, but results not detected for 3wks after rash, so not valuable.Tx: symptomatic. Avoid heat (exacerbates rash).Contagious few days before rash, can return to work/school after initial s/s of HA, fever, chills are gone, even if rash still present. Pityruasis rosea: viral,difficult to confirm.Majority 10-35yo, more females than males. Common breakouts in spring.Solitary 2-4 patch/plaque on trunk ("herald patch"), starts 2-3wks before general rash. Rash is pink, erythematous, round to oval plaques/papules w/possible scaly borders. Resembles shape of a Christmas tree on the trunk. Usually not on face, palmar, sole surfaces. Can be itchy. Pt may have low-grade fever, HA, fatigue. Can last 1-2mo or longer.Dx made by H&P.Tx: antihistamines, sun (could help rash). Acyclovir for 1wk (may reduce severity).Contagious 7-14 days prior to rash. Returning to activities depend on symptoms, but by the time rash appears, pt is not contagious. Hand, foot & mouth: mostly occurring in young children.Caused by coxsackievirus A16 and enterovirus 71.Low-grade fever, fatigue, sore throat 1-2 days, then rash.Rash: vesicles on hands/feet w/mouth sores. Mouth sores are in almost 90% of cases, usually first sign. Hand vesicles appear with erythematous halos and appear mostly on soles/palms. Might appear on legs, butt, face. Usually resolve in 7 days.Dx made by H&P.Tx: symptomatic. Reassure parents that there will be no scarring.Contagious 4-6days prior to outbreak, can return to school when lesions are scabbed Molluscum contagiosum: from family of Poxviridae.Virus is encased in protective sac that prevents immune system from being triggered.Tiny pustules 2-5mm, some have slight depression in center of flesh-colored dome. Single or multiple lesions.Spread by contact, scratching, autoinocculation, shaving.Most common places in kids are thighs/arms.Most common places in adults are genital region.Never soles/palms. Sometimes erythematous papules/scaling from itching.Can last 8mo or longer. Dx by H&P, often misdiagnosed as genital warts.Tx: non-Rx OTC Zymaderm. Rx topical retinoids. PO Cimetidine (Tagamet) 40mg/kg/day x2mo. Cryosurgery w/liquid nitrogen (may be scarring or hypopigmentation).No single treatment better than another. Exclude from activities/sports until symptom-free or lesions are covered. 8. Differentiate between the following tineas: pedis, cruris, corporis and unguium and describe an appropriate treatment Tinea Pedis: athlete's foot. Mainly affects male teenage athlete/older adult. Usually painless unless infected.Most common cause T mentagrophytes.Presentation:macerated white skin between web of toes.Is pruritic,painful fissures (occasionally),unpleasant odour.Tx Topical antifungal (if severe oral itraconazole/terbinafine dly), moisture control, Burow’s solution for weeping areas ( Chapter 7 Dunphy). Tinea cruris:(jock itch).Rash presents on inner thighs, butt, groin. Well-demarcated erythematous/tan plaques with raised scaly borders.Tx: topical antifungal (itraconazole/terbinafine dly); if repetitive infections, OTC antifungal eg zeabsorb powder can help prevent breakout. Burow solution for weeping areas. Tx Itraconazole/terinafine. Tinea corporis (ringworm). Affects all age group. On the extremities or trunk. erythematous annular lesion with scaly macules and papules, well-defined edges.Pt/gaurdian reports lesion size increasing..May be itchy.Edge of lesion is raised, center of lesion is flattened. Can be small or cover large body surface area.Tx: antifungal topical cream or PO antifungal Itraconazole/Terbanafine (if severe). Tinea unguium: (onychomycosis).Fingernails or toenails.Very common in adults & elderly.Nail appearance may vary: yellow, green, black or white ridging w/possible cracking of nails.Diagnosed by fungal culture/potassium hydroxide (POH) exam.Tx: determined by severity and pt's age. Topical Ciclopirox nail laquer 8% applied daily for months at base of nail. PO Terbanafine 250mg daily x6wks (fingernails) X 12 wks (toenails,has high cure rate but pt has to have healthy liver (do CMP prior to initiation).Cure is VERY slow. 9. Identify the virus that causes warts Human papillomavirus (HPV). 10. Differentiate between atopic and contact dermatitis and give examples of each Contact: allergic reaction to substance that produces immune reaction in skin resulting in pruritic and erythemic rash. Common causes: nickel, abx creams, cosmetics, soaps, fragrances, jewelry, plants (poison ivy). Usually occurs in same area that was directly exposed to reaction within minutes to hours of exposure. Not contagious, cannot be spread from one area of body to another by touching. Tx: removal of substance causing reaction; mostly symptomatic; topical antihistamines; steroid creams; PO antihistamines to combat itching; mores severe cases or if reaction is on face, esp around eyes: taper dose of PO steroids. Can lead to secondary infection if area is repeatedly scratched. Atopic: disorder that is result of gene variation that affects skin's ability to retain moisture and protection from irritants. Often associated in people with asthma or hay fever. Patches of itchy, dry skin; red to brownish-gray; may have small raised vesicles that leak when scratched. Usually starts before age 5, persists into adulthood. Tx: symptomatic, much like contact derm. Topical steroid creams, PO antihistamines. Moisturize skin at least BID. Avoid triggers that worsen rash. 11. Identify common characteristics associated with blepharitis, chalazion and hordeolum Blepharitis: irritation, burning, itching, scales, redness. If lice is cause: reddish brown crust in lashes (not white or clear as typically seen). Chalzion: mass in mid-portion of upper lid away from margin. Usually not painful or tender. Slightly red, swollen. Hordeolum: usually on outside of lid, abscess on lid margin. Redness, swelling, painful. 12. Differentiate between viral, allergic, bacterial, toxic and HSV conjunctivitis (CH.8 & lecture) Viral- Benign, watery discharge, visual acuity is normal, itching present, mod/diffuse conjunctival abnormalities (bumps on the conjunctiva “follicles” hallmark sign), no pupillary involvement, mild photophobia (lecture), no photophobia (book),often has bilateral involvement, highly contagious, IOP normal, Preauricular nodes palpable, a URI usually present (adenovirus mainly), resolves on its own (few days-weeks), no firm guidelines when to return to work/school, AAO recommends when redness and tearing gone, treatment- no scratching, artificial tears, OTC anti-allergy drops may help, systemic antihistamines not helpful. HSV- HSV 1(above the waist) & 2 (below the waist), cause by direct contact with a person with visible lesions or shredding of lesions (predromal stage, before lesions appear), skin vesicles present, conjunctivitis, corneal infection w/ hallmark “dendrite” appearance (look at lecture for pic), referral to ophthalmology is necessary. Allergic- stringy/mucoid discharge, visual acuity normal, itching/burning present, mild/diffuse conjunctival abnormalities, no pupillary involvement, no photophobia, usually has bilateral involvement, IOP normal, preauricular nodes not palpable, other symptoms- rhinorrhea, sneezing, tearing, occurs in fall or spring. Bacterial- Contagious (24hrs w/ antibiotics before returning to work/school), purulent/thick discharge, crusted lids in the a.m, visual acuity normal, pain described as sandiness, Mod to heavy/diffuse conjunctival abnormalities, no pupillary abnormalities, no photophobia, begins unilateral, but may spread bilaterally, IOP normal, preauricular nodes not palpable, occurs in fall and winter, mainly caused by direct contact with infected person or one’s own bacteria. - May resolve w/o tx, but antibiotic drops can shorten duration(4x/day, 4-7 days). All antibiotic drops are pretty effective-choice depends on allergies, cost, and availability - Gonococcal infection- involves the cornea, hyper purulent discharge-send to ER Toxic- Caused by overuse of topical ocular meds (visine, antibiotics-longer than necessary), clear/watery discharge,red conjunctiva, TX- stop using offending agent 13. Discuss which chemical injury is associated with the most damage and highest risk to vision loss - Severity of injury depends on pH, volume, and duration, Alkaline agents are most damaging (ammonia, drain cleaner (lye), cement (lime), plaster mortar (sodium), air bags & fireworks (mag hydroxide), immediate irrigate (shower/hose), no eye wash or artificial tears, ambulance to ER - Acid injury -corneal abrasion that heals with little or no scarring - Epithelial and deep corneal layer damage - Poor prognosis 14. Recognize common eye emergency conditions that require emergency room evaluation Chemical burns, Gonococcal infection, complicated orbital cellulitis (can turn into meningitis), Eye led laceration, subconjunctival hemorrhage (severe or trauma)-check vision, foreign bodies, hyphema (blood is trapped b/w iris and cornea), ruptured globe (trauma, vision threatening, need surgery. 15. Discuss glaucoma, diagnosis and treatment -Progressive damage to the optic nerve, resulting in atrophy and blindness, most typically related to increase in IOP. - open-angle-most common, the chronic form, usually asymptomatic until loss of peripheral vision, good prognosis if treated early. Common in ages >40, but can occur at any age, African Americans have a higher incidence - closed-angle- sub-acute and chronic components, significant eye pain, redness, and acute visual loss, which if left untreated can rapidly lead to permanent blindness. Most common in ages 55-70. -congenital- seen in infants -or primary/secondary -the use of steroid therapy can increase IOP, antidepressant, anticholinergic, acute stress can contribute to an acute episode. Diagnostic: Tonometry reading for IOP, but not sensitive for glaucoma, no guidelines for glaucoma screening by the primary care provider. Refer to opthamologist (gonioscopy-measures ant chamber angle), appearance(color & contour) of optic nerve and visual fields most impt for diagnosis, size of the cup relative to optic nerve. Diagnosis is made on finding of characteristic degenerative changes in the optic disc and defects in visual fields. Tx: if nerve damage present-irreversible. Goal is to prevent progression- decrease IOP. Beta-blockers usually first-line, but prostaglandin analogs may be first-line or added soon after the beta-blocker. If medication does not work, then surgery is next (laser- (pressure may build back up after several years) or external trabeculectomy). Acute closed-angle requires emergency tx, medications( Diamox and IV mannitol) are used initially to lower IOP, so that surgical intervention can occur. Close and life-long F/U essential 16. Discuss diabetic retinopathy -noninflammatory disorder of the retina that develops in patients with diabetes. -stage 1: background diabetic retinopathy-microaneurysms, intraretinal hemorrhage, macular edema, and lipid deposits may be present -stage 2: preproliferative diabetic retinopathy-cotton-wool spots (infarctions), venous beading and dilation, edema and in some cases extensive retinal hemorrhage. -stage3: proliferative diabetic retinopathy- new blood vessel proliferation on retinal surface, optic nerve, and iris, laser surgery recommended, other tx cryoretinopexy (decrease neovascular stimulus), vitrectomy (severe proliferative) -diabetic patients-always refer to opthamologist -caused by uncontrolled hyperglycemia -patient will complain of visual changes, but asymptomatic in early stages -changes noted in funduscopic exam -risk is significantly increased in BG >200 - keep A1c <7% - in patients w/ HTN and diabetes-lisinopril shown slow progression -pt w/ diabetes- yearly opthamologist visit, and w/ known hx of retinopathy, Q 6 M, and if known hx of proliferative (stage 3) Q 3-4M, and if acute proliferative Q 8 wks. NOTES from Chapter 11 readings:( Please fill in any notes from your reading for any topics that have not listed down here)--This is where we can easily skim through the notes. Jaundice: Yellow of skin & mucous membrane, sclera; increase accumulation of bilirubin==need Emergency attention; Hyperbilirubinemia: result ↑production, ↓ uptake, ↓ conjugation, or ↓ excretion of bilirubin. DDx:Lab values: 1) Icterus not evident until bili level >2-3 mg/dl; (normal bili== 0.3 to 1.0 mg/dl) Most Bili—from heme portion, a break down of RBC; unconjugated bili (indirect bilirubin)-water insoluble and only bound to albumin; then conjugated by the liver (water soluble—direct bilirubin, found in urine) 2) AST and ALT==good indicators of hepatocyte damage; AST (in liver, skeletal muscle, brain, and heart); ALT --only in hepatocyte cytoplasm—more specific; AST and ALT with extreme elevation can be diagnostic, or otherwise <300U/L are nonspecific; AST >15 times indicate cholangitis; AST and ALT > 1,000 U/L—acute viral hepatitis; if ratio AST/ALT is high—severe hepatic necrosis (alcoholic hepatitis) 3) Alkaline phosphatase found in biliary canalicular membranes, useful in assessing cholestasis, (a condition where bile cannot flow from the liver to the duodenum). 4) GGT and 5-nucleotidase also increase in cholestasis. ↑ alkaline phosphatase with GGT== mechanical obstruction of the biliary system by a Tumor, stricture, or stone. 5) Alkaline Phosphatase is also found in bone without ↑ GGT==bone disorder. Sx: pruritus, anorexia, nausea, vomiting, fever, light-colored stools, weight loss, fatigue. Exam with RUQ pain and tenderness, dark urine, abdo distension. - Pruritus, dark urine, light-colored stools, jaundice indicate cholestasis d/t cholelithiasis, cirrhosis, or other biliary obstruction. [Show More]
Last updated: 1 year ago
Preview 1 out of 23 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
May 13, 2020
Number of pages
23
Written in
Additional information
This document has been written for:
Uploaded
May 13, 2020
Downloads
0
Views
35


.png)
.png)

