*NURSING > STUDY GUIDE > Medical Surgery (Chapter 41)- Assessment of the Nervous System | 100% COMPLETE STUDY GUIDE (All)
Medical Surgery (Chapter 41)- Assessment of the Nervous System | 100% COMPLETE STUDY GUIDE
Document Content and Description Below
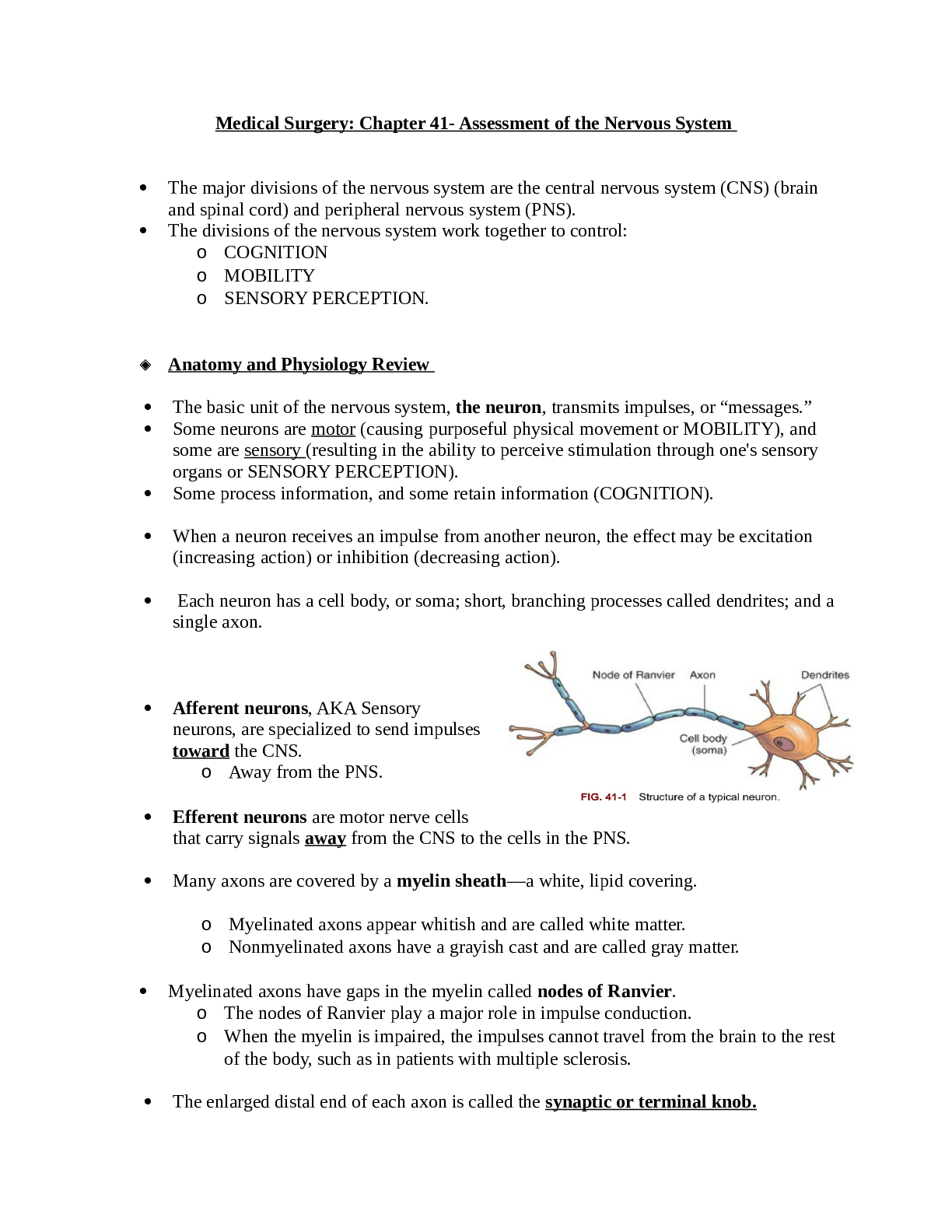
Medical Surgery: Chapter 41- Assessment of the Nervous System • The major divisions of the nervous system are the central nervous system (CNS) (brain and spinal cord) and peripheral nervous sys... tem (PNS). • The divisions of the nervous system work together to control: o COGNITION o MOBILITY o SENSORY PERCEPTION. ◆ Anatomy and Physiology Review • The basic unit of the nervous system, the neuron, transmits impulses, or “messages.” • Some neurons are motor (causing purposeful physical movement or MOBILITY), and some are sensory (resulting in the ability to perceive stimulation through one's sensory organs or SENSORY PERCEPTION). • Some process information, and some retain information (COGNITION). • When a neuron receives an impulse from another neuron, the effect may be excitation (increasing action) or inhibition (decreasing action). • Each neuron has a cell body, or soma; short, branching processes called dendrites; and a single axon. • Afferent neurons, AKA Sensory neurons, are specialized to send impulses toward the CNS. o Away from the PNS. • Efferent neurons are motor nerve cells that carry signals away from the CNS to the cells in the PNS. • Many axons are covered by a myelin sheath—a white, lipid covering. o Myelinated axons appear whitish and are called white matter. o Nonmyelinated axons have a grayish cast and are called gray matter. • Myelinated axons have gaps in the myelin called nodes of Ranvier. o The nodes of Ranvier play a major role in impulse conduction. o When the myelin is impaired, the impulses cannot travel from the brain to the rest of the body, such as in patients with multiple sclerosis. • The enlarged distal end of each axon is called the synaptic or terminal knob. o Within the synaptic knobs are the mechanisms for manufacturing, storing, and releasing a transmitter substance. • Each neuron produces a specific neurotransmitter chemical (acetylcholine and serotonin) that can either enhance or inhibit the impulse, but cannot do both. • Impulses are transmitted to their eventual destination through synapses, or spaces between neurons. There are two distinct types of synapses: 1. Neuron to neuron 2. Neuron to muscle (or gland). • Between the terminal knob and the next cell is a small space called the synaptic cleft. • The Knob, the cleft, and the portion of the cell to which the impulse is being transmitted make up the synapse. • Neuroglia cells, which vary in size and shape, provide protection, structure, and nutrition for the neurons. They are classified into four types: 1. Astroglial cells 2. Ependymal cells 3. Oligodendrocytes 4. Microglial cells. - These cells are also part of the blood-brain barrier and help regulate cerebrospinal fluid (CSF). ◆ CNS: Structure & Function o The central nervous system (CNS) is composed of the brain & spinal cord. ▪ The brain directs the regulation and function of the nervous system and all other systems of the body. ▪ The spinal cord, starts reflex activity and transmits impulses to and from the brain. ◆ Brain o The meninges form the protective covering of the brain and the spinal cord. o The outside layer: Dura mater. o Middle Layer: Arachnoid. o The subdural space is located between the dura mater and the middle layer, the arachnoid. o The pia mater is the most inner layer. ▪ Situated between the arachnoid and pia mater is the subarachnoid space, -Where CSF circulates. CSF is in the Subarachnoid space (btw. Arachnoid & pia mater). o A potential space, referred to as the epidural space, is located between the skull and the outer layer of the dura mater. ▪ This area also extends down the spinal cord and is used for the delivery of epidural analgesia and anesthesia. • The dura mater also lies between the cerebral hemispheres and the cerebellum and is called: the tentorium. o The tentorium helps decrease or prevents the transmission of force from one hemisphere to another and protects the lower brainstem when head trauma occurs. ◆ Major Parts of the Brain o The brain consists of three main areas—the forebrain, the cerebellum, and the brainstem. o The forebrain lies above the brainstem and cerebellum and is the most advanced in function complexity. ▪ This area of the brain is further divided into three areas—the diencephalon, the cerebrum, and the cerebral cortex. • The diencephalon (forebrain) which lies below the cerebrum, includes the thalamus, hypothalamus, and epithalamus. o The thalamus is the major “relay station,” or “central switchboard,” for the CNS. o The hypothalamus plays a major role in autonomic nervous system control (controlling temperature and other functions) and COGNITION. o The epithalamus connects the pathways to regulate emotion and contribute to smooth voluntary motor function. • The cerebrum is the largest part of the brain and controls intelligence, creativity, and memory. o The “gray matter” of the cerebrum is the central cortex—the center that receives information from the thalamus and all the lower areas of the brain. o The cerebrum consists of two halves, referred to as the right hemisphere and the left hemisphere, which are joined by the corpus callosum. o The left hemisphere is the dominant hemisphere in most people (even in many left-handed people). o Within the deeper structures of the cerebrum are the right and left lateral ventricles. o At the base of the cerebrum near the ventricles is a group of neurons called the basal ganglia, which help regulate motor function. • The cerebral cortex is part of the cerebrum and is involved with almost all of the higher functions of the brain. o This part of the brain processes and communicates all information coming from the peripheral nervous system (PNS). It also translates the impulses into understandable feelings and thoughts. o The cerebral cortex is so complex that it is further divided into four lobes: the frontal lobe, parietal lobe, temporal lobe, and occipital lobe. • The cerebellum receives immediate and continuous information about the condition of the muscles, joints, and tendons. Cerebellar function enables a person to: - Keep an extremity from overshooting an intended target - Move from one skilled movement to another in an orderly sequence - Predict distance or gauge the speed with which one is approaching an object - Control voluntary movement - Maintain equilibrium o Unlike the motor cortex, cerebellar control of the body is ipsilateral (situated on the same side). ▪ The right side of the cerebellum controls the right side of the body, and the left cerebellum controls the left side of the body. • The brainstem includes the midbrain, pons, and medulla. o Throughout the brainstem are special cells that constitute the reticular activating system (RAS), which controls awareness and alertness. o For example, this tissue awakens a person from sleep when presented with a stimulus such as loud noise or pain or when it is time to awaken. ◆ Circulation in The Brain • Circulation in the brain originates from the carotid and vertebral arteries. • The internal carotid arteries branch into the anterior cerebral artery (ACA) and middle cerebral artery (MCA), the largest ones. • The two posterior vertebral arteries become the basilar artery, which then divides into two posterior cerebral arteries. • The anterior, middle, and posterior cerebral arteries are joined together by small communicating arteries to form a ring at the base of the brain known as the circle of Willis. • The blood-brain barrier (BBB) seems to exist because the endothelial cells of the cerebral capillaries are joined tightly together. • This barrier keeps some substances in the bloodstream out of the cerebrospinal circulation and out of brain tissue. • Substances that can pass through the BBB include: o Oxygen o Glucose o Carbon dioxide o Alcohol o Anesthetics o Water. • Cerebrospinal fluid (CSF) also circulates, surrounds, and cushions the brain and spinal cord. • While moving through the subarachnoid space, the fluid is continuously produced by the choroid plexus, reabsorbed by the arachnoid villi, and then channeled into the superior sagittal sinus. • Expanded areas of subarachnoid space, where there are large amounts of CSF, are called cisterns. o The largest one is the lumbar cistern, the site of lumbar puncture, from the level of the second lumbar vertebra to the second sacral vertebra (L2-S2). ◆ Spinal Cord • The spinal cord controls MOBILITY; regulates organ function; processes SENSORY PERCEPTION information from the extremities, trunk, and many internal organs; and transmits information to and from the brain. • It contains H-shaped gray matter (neuron cell bodies) that is surrounded by white matter (myelinated axons). o Groups of cells in the white matter (ascending and descending tracts) carry impulses from the spinal cord to the brain (ascending tracts, such as the spinothalamic tract) or from the brain to the spinal cord (descending tracts, such as the corticospinal tract). o Because o The spinal cord ends between L1 and L2, the axons of the lumbar and sacral cord extend downward before exiting at the appropriate intervertebral foramen. ◆ Peripheral NS • The peripheral nervous system (PNS) is composed of the spinal nerves, cranial nerves, and autonomic nervous system. o There are 31 pairs of spinal nerves (8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal) exiting from the spinal cord. o Each of the nerves has a posterior and an anterior branch. o The posterior branch carries SENSORY PERCEPTION information to the cord (afferent pathway). o The anterior branch transmits motor impulses to the muscles of the body to allow MOBILITY (efferent pathway). o The area controlled by each spinal nerve is roughly reflected in the dermatomes. ▪ Dermatomes represent sensory input from spinal nerves to specific areas of the skin. ▪ Ex: the patient with an injury to cervical spinal nerves C6 and C7 has sensory changes in the thumb, index finger, middle finger, middle of the palm, and back of the hand. o As each nerve axon leaves the spinal cord, it joins other spinal nerves to form plexuses (clusters of nerves). ▪ Plexuses continue as trunks, divisions, and cords and finally branch into individual peripheral nerves. • The reflex arc is a closed circuit of spinal and peripheral nerves and therefore requires no control by the brain. • Reflexes consist of sensory input from: - Skeletal muscles, tendons, skin, organs, and special senses. - Small cells in the spinal cord lying between the posterior and anterior gray matter (interneurons). - Anterior motor neurons, along with the muscles they innervate. • There are 12 cranial nerves. • Oh – Olfactory Some • Oh – Optic Say • Oh – Occulomotor Marry • To – Trochlear Money • Take – Trigeminal But • A – Abducent My • Family – Facial Brother • Vacation! – Vestibulocochlear Says • Go – Glossopharyngeal Big • Vegas – Vagus Brains • After – Accessory Matter • Hours – Hypoglossal Most ◆ Autonomic Nervous System (ANS) o Composed of two parts: the sympathetic nervous system (SNS) and the parasympathetic nervous system. o ANS functions are not usually under conscious control but may be altered in some people by using biofeedback and other methods. o The SNS stimulates the functions of the body needed for “fight or flight” (heart and respiratory rate). It also inhibits certain functions not needed in urgent and stressful situations. o The parasympathetic nervous system can slow body functions when needed and contribute to digestion and reproduction (“feed and breed”)/ (“Rest & Digest”). ◆ Neurologic Changes Associated with Aging o Neurologic changes associated with aging often affect MOBILITY and SENSORY PERCEPTION. o Motor changes in late adulthood can cause slower movement and response time and decreased sensory perception. o Determining functional status (a combination of COGNITION, MOBILITY, and SENSORY PERCEPTION) is a recommended Core Measure for patients with complex chronic conditions. • Sensory changes in older adults can also affect their ADLs. o Pupils decrease in size, which restricts the amount of light entering the eye, and adapt more slowly. o Older adults need increased lighting to see. • Cognitive functions of perceiving, registering, storing, and using information often change as a normal part of aging. o Intellect does not decline as a result of aging. • Cognitive decline is frequently caused by drug interactions or toxicity or by an inadequate oxygen supply to the brain (hypoxia). • Subtle memory changes can occur for many older people. Long-term memory often seems better than recall (recent) or immediate (registration) memory. Older adults may need more time to retrieve information. o Recall memory – Recent o Immediate – Registration o Long-term – Long-term • Circadian responses are reduced in older adults, and the sleep-wake cycle may become less responsive to stimuli that signal patterns of sleep. o Older adults may experience changes in sleep habits and sleeping patterns. o On average, an older person needs as much sleep as a younger person but is more likely to nap in the afternoon. o Sleep deprivation is related to both the earlier onset and greater severity of delirium (acute confusion) in older adults. o Lack of sleep can worsen symptoms of mild dementia (chronic confusion). o Sleep deprivation can also interfere with normal immune function and wound healing. ▪ Mental status may be impaired as a result of infection, hypoxia, and hypoglycemia or hyperglycemia in the older adult. These conditions are usually easily assessed and managed. o During an acute change in mental status, assess the adult for peripheral oxygenation saturation (SpO2), serum glucose (fingerstick), and potential infection. ▪ Ex: fever, urine with sediment or odor, sputum production, red or draining wound). o Often a decrease or change in mental status (acute confusion) is a key early sign of an infectious process in the older patient, such as a urinary tract infection. ◆ Health Promotion and Maintenance o Avoid Risky behaviors & practicing a healthy lifestyle. o Remind adults of any age to avoid excessive alcohol or other substances that can impair judgement and cause an accident. o Active military men and women who are in or near combat areas are also at risk for neurologic problems, especially traumatic brain injury (TBI). ▪ The most common cause of TBI in this population is a blast from an improvised explosive device (IED). o Smoking cessation. o Teach patients that proper nutrition and regular exercise are also important to prevent neurologic impairment. o Skipping meals or poor nutrition can affect the function of the body's neurons. • “Educate pt. at a 4th grade level. Question: The nurse performs an initial assessment on an older client. Which assessment findings would the nurse expect to be the result of normal physiologic aging? A. Confusion B. Hearing loss C. Decerebrate positioning D. Slurred speech E. Constipation F. Urinary incontinence B,E ◆ Assessment: o During your introduction, note the patient's appearance and assess his or her speech, affect, and movement. o If he or she seems to have COGNITION deficits or has trouble speaking or hearing, ask a family member or significant other to stay during the interview to help obtain an accurate history. o Be sure that glasses, contact lenses, and hearing aids are available if the patient wears any of these devices. o Ask whether the patient is right handed or left handed. This information is important for several reasons: • The patient may be somewhat stronger on the dominant side, which is expected. • The effects of cerebral injury or disease are more pronounced if the dominant hemisphere is involved. ◆ Physical Assessment o Compare each assessment with the patient's baseline, between right and left sides, and between upper and lower extremities. o Two types of neurologic assessments may be performed: a complete assessment and a focused assessment. o Some focused assessments are specifically designed to be rapid to ease repetition when recurrent neurologic assessments are needed to monitor the patient's condition over time. ▪ The type chosen depends on the information needed, the time available with the patient, and your clinical skill level. o Advanced practice registered nurses (APRNs) and other primary health care providers usually perform the complete assessment, with selected parts done by the nurse generalist or staff nurse. ◆ Complete Neurologic Assessment o A complete neurologic assessment includes a history and evaluation of mental status, cranial nerves, mobility and motor system function, deep tendon reflexes, sensory perception, and cerebellar function. o The complete neurologic assessment is performed by the primary health care provider (PHCP) to consider whether a single lesion or more than one site in the nervous system may be contributing to abnormal physical assessment findings. o If the lesion or injury is in the CNS, the assessment can further help the health care provider determine if abnormalities are in the cortex, below the cortex, or multifocal. ▪ These findings, along with patient history, help determine the urgency of treatment. o The nurse completes a focused or rapid assessment to detect major changes in signs and symptoms. ◆ NURSING ALERT: o A change in LOC and orientation is the earliest and most reliable indication that central neurologic function has declined! o If a decline occurs, contact the Rapid Response Team or PHCP immediately. o Perform a focused neurologic assessment to determine if additional changes are present. ◆ Assessment of Mental Status o Mental status assessment is generally divided into assessment of consciousness and cognition. o Consciousness is the ability to be aware of the environment, an object, and oneself. ▪ Documented as one's level of consciousness. ▪ Level of consciousness (LOC) usually refers to the degree of alertness or amount of stimulation needed to engage a patient's attention and can range from alert to coma. ▪ The patient who is described as alert is awake, engaged, and responsive. ▪ A patient may be alert but not oriented to person, place, or time. o Patients who are less than alert are labeled lethargic, stuporous, or comatose. ▪ A lethargic patient is drowsy but is easily awakened. ▪ One who is arousable only with vigorous or painful stimulation is stuporous. ▪ The comatose patient is unconscious and cannot be aroused despite vigorous or noxious simulation. o After determining alertness, the next step is to evaluate orientation. Once the patient's attention is engaged, ask questions to determine orientation. ▪ Varying the sequence of questioning on repeated assessments prevents the patient from memorizing the answers. ▪ Responses that indicate orientation include ability to answer questions about person, place, and time. o Time of day, drug therapy, and the need for sleep, glucose, or oxygen may affect these responses. o Be sure to link any changes in orientation with respiratory status, changes in drug regimens or use of intermittent drugs, time of day/sleep deprivation, or current serum glucose values. o Education, occupation, interest, culture, anxiety, and depression affect performance during assessment of mental status. ◆ QUESTION: During a client’s neurologic assessment, the nurse finds that the client continues to be drowsy but is easily awakened. How does the nurse document this client’s LOC? A. Stuporous B. Lethargic C. Comatose D. Alert B • Cognition typically is evaluated in a rapid or focused manner using tests of memory and attention that require verbal or written ability. • Loss of memory, especially recent memory, tends to be an early sign of neurologic problems. • Three types of memory can be tested: 1. Long-term (Remote) memory 2. Recall (recent) memory 3. Immediate memory. • Many speech and language skills can be assessed during the initial interview. o Language skills include understanding the spoken or written word and being able to speak or write. o The patient demonstrates understanding by following directions on admission (ex: getting undressed). o If he or she hesitates, it may be that he or she does not understand the vocabulary or word. o When speech hesitation or performance hesitation occurs, point to objects and ask the patient to name them, such as the door or bed. o Speech is assessed as being normal, slow, garbled, difficult to find words, or other impairments. o If the change in speech is new and represents a deterioration from a previous ability to communicate, this change must be urgently reported to the primary health care provider because it may indicate a stroke, new onset of confusion, or other serious neurologic condition. ◆ Assessment of Cranial Nerves o They are not routinely tested unless the patient has a suspected problem affecting one or more of them. o Testing pupils is a common cranial nerve test performed by nurses. ▪ Pupil constriction is a function of cranial nerve III, the oculomotor nerve. ▪ Pupils should be equal in size, round and regular in shape, and react to light and accommodation (PERRLA). o Patients who have had eye surgery for cataracts or glaucoma often have irregularly shaped pupils. ▪ Those using eyedrops for either cataracts or glaucoma may have unequal pupils if only one eye is being treated, and the pupillary response may be altered. o To test for pupil constriction, ask the patient to close his or her eyes and dim the room lights. ▪ Bring a penlight in from the side of the patient's head and shine the light in the eye being tested as soon as the patient opens his or her eyes. ▪ The pupil being tested should constrict (direct response). ▪ The other pupil should also constrict slightly (consensual response). o To test accommodation, ▪ Relight the room and ask the patient to focus on a distant object and then immediately look at an object 4 to 5 inches from the nose. ▪ The eyes should converge, and the pupils should constrict. ▪ Pinpoint or severely dilated nonreactive pupils are usually late signs of neurologic deterioration. ◆ Assessment of Motor Function o Throughout the physical assessment, observe the patient for involuntary tremors or movements. o Describe these movements as accurately as possible, such as “pill-rolling with the thumbs and fingers at rest” or “intention tremors of both hands” (tremors that occur when the patient tries to do something). ▪ These abnormalities can indicate certain diseases, such as multiple sclerosis, or the effects of selected psychotropic drugs. o In addition, assess the patient for motor movements that indicate irritability, hyperactivity, or slowed movements. o Measure the patient's hand strength by: o Asking to grasp and squeeze two fingers of each of your hands. Then compare the grasps for equality of strength. o Another means of evaluating strength: try to withdraw the fingers from the patient's grasp and compare the ease or difficulty. ▪ He or she should release the grasps on command—another assessment of consciousness and the ability to follow commands. o To test strength against resistance, ask the patient to resist the examiner's bending or straightening of the arm, hand, leg, or foot being tested. ▪ A five-point rating scale is commonly used. Always evaluate and compare strength on each side. o Report all decreases to the PHCP. • Cerebral motor or brainstem integrity may also be assessed. o Ask the patient to close his or her eyes and hold the arms perpendicular to the body with the palms up for 15 to 30 seconds. ▪ If there is a cerebral or brainstem reason for muscle weakness, the arm on the weak side will start to fall, or “drift,” with the palm pronating (turning inward). This is called a pronator drift. ▪ The same can be done for the lower extremities, with the patient lying on his or her stomach with the legs bent upward at the knees. • Decortication is abnormal motor movement seen in the patient with lesions that interrupt the corticospinal pathways. o The patient's arms, wrists, and fingers are flexed with internal rotation and plantar flexion of the legs. • Decerebration is abnormal movement with rigidity. o Characterized by extension of the arms and legs, pronation of the arms, plantar flexion, and opisthotonos (body spasm in which the body is bowed forward). o Decerebration is usually associated with dysfunction in the brainstem area. ◆ Assessment of Reflex Activity o The deep tendon reflexes of the biceps, triceps, brachioradialis, and quadriceps muscles and of the Achilles tendon can be tested as part of the complete neurologic assessment. ▪ Striking the tendon with the reflex hammer should cause contraction of the muscle. ▪ The appropriate muscle contraction indicates an intact reflex arc. o The cutaneous (superficial) reflexes usually tested are the plantar reflexes and sometimes the abdominal reflexes. ▪ The plantar reflex is tested with a pointed (but not sharp) object, such as the handle end of the reflex hammer or the rounded end of bandage scissors. ▪ The normal response is plantar flexion of all toes. ▪ Babinski's sign, a dorsiflexion of the great toe and fanning of the other toes, is abnormal in anyone older than 2 years. ▪ Represents the presence of central nervous system (CNS) disease. ▪ The terms positive Babinski's sign (abnormal response) and negative Babinski's sign (normal response) are clinically used terms but are not technically accurate. ▪ Babinski's sign can occur with drug and alcohol intoxication, after a seizure, or in patients with multiple sclerosis or severe liver disease. o Hyperactive reflexes indicate possible upper motor neuron disease (damage to the brain or upper spinal cord). o Hypoactive reflexes may result from lower motor neuron disease (damage to the lower o spinal cord) or neuromuscular diseases. o Asymmetry of reflexes is an important finding because it probably indicates a disease process or injury. The results of reflex testing are recorded by the use of a stick figure and a scale of 0 to 4. ▪ A score of 2 is considered normal, although scores of 1 (hypoactive) or 3 (stronger than normal) may be normal for a particular patient. o Clonus (also called myoclonus) is the sudden, brief, jerking contraction of a muscle or muscle group often seen in seizures. ◆ Assessment of Sensory Function o The acuity level of the patient determines how often the sensory assessment is done. ▪ Example: Patients with acute spinal cord trauma or ascending Guillain- Barré syndrome (GBS) are assessed every hour until stable and then every 4 hours. As the condition improves, sensory assessment may be needed only once each shift. o Pain and temperature sensation are transmitted by the same nerve endings. ▪ Therefore if one sensation is tested and found to be intact, it can safely be assumed that the other is intact. o Testing temperature sensation can usually be accomplished using a cold reflex hammer and the warm touch of the hand for patients with known or suspected spinal problems. o Assess for pain perception with any sharp or dull object, such as the tips of a cotton-tipped applicator. ▪ While the patient's eyes are open, demonstrate what will be done. Then ask him or her to keep eyes closed and to indicate whether the touch is sharp or dull. ▪ The sharp and dull ends should be changed at random so they don’t not anticipate the next type of stimulus for SENSORY PERCEPTION. o Compare reactions on each side. o The sensation reported as dull when the stimulus was actually sharp requires further testing. o A patient with sensory loss as a result of diabetes mellitus or peripheral vascular disease may or may not be aware of the loss until tested. o Some patients with chronic illness may report that they have had sensory losses for a long time. o Before testing for pain, the nurse must check to determine whether the patient is on anticoagulant therapy. ▪ If the patient is on anticoagulant therapy, avoid any testing with a sharp object because it can cause bleeding. o For testing touch discrimination, the patient closes his or her eyes. The practitioner touches the patient with a finger and asks that he or she point to the area touched. ▪ This procedure is repeated on each extremity at random rather than at sequential points. o CNS problems in the brainstem, thalamus, and cortex generally result in loss of sensation on the contralateral (opposite) side of the body. o Cerebellar lesions result in sensory deficits on the same o side of the body. ◆ Assessment of the Cerebellar Function o Most of the assessment of cerebellar function can be performed with the patient sitting on the side of the bed or examining table. o Fine coordination of muscle activity is tested. o If cerebellar problems are suspected or diagnosed, ask the patient to perform these tasks with his or her eyes closed: • Run the heel of one foot down the shin of the other leg and repeat with the other leg (the patient should be able to do this smoothly and keep the heel on the shin). • Place the hands palm-up and then palm-down on each thigh, repeating as fast as possible (this can normally be done rapidly). • With arms out at the side, touch the finger to the nose two or three times, with eyes open and then with eyes closed (this can be done with alternating arms or with each arm individually). o For the last part of the cerebellar assessment, the ambulatory patient stands for testing of gait and equilibrium. o Gait and equilibrium are usually tested at the end or beginning of the entire neurologic assessment. ▪ Ask the patient to walk across the room, turn, and return. Observe for uneven steps, difficulty walking, and so forth. ▪ To evaluate balance, ask him or her to stand on one foot and then on the other. ▪ Tiptoe and heel-to-toe walking can also demonstrate gait problems. ▪ For patients with sciatic nerve involvement, pain may worsen when they walk on their toes or heels. o To test equilibrium, ask the patient to stand with arms at the sides, feet and knees close together, and eyes open. ▪ Check for swaying and then ask him or her to close his or her eyes and maintain position. ▪ If the pt. sways with the eyes closed but not when the eyes are open (the Romberg sign), the problem is probably proprioceptive (awareness of body position). ▪ If the patient sways with the eyes both open and closed, the neurologic disturbance is probably cerebellar in origin. ◆ Rapid/Focused Neurologic Assessment o A rapid/focused neurologic assessment, or “neuro check,” is completed when the patient is admitted to a health care facility on an emergent basis. ▪ It is also a major part of frequent ongoing patient assessment and performed in the event of a sudden change in neurologic status. o The typical record contains data related to alertness, orientation, movement of arms and legs, and pupil size and reaction to light. o Be sure to document all aspects of the rapid neurologic assessment frequently in the designated or standardized part of the electronic record as needed per agency protocol or HCP request. ▪ An example of a standard rapid neurologic assessment tool is the Glasgow Coma Scale (GCS). ▪ The GCS is used in many acute care settings to establish baseline data in each of these areas: - Eye opening - Motor response - Verbal response. ▪ The patient is assigned a numeric score for each of these areas. ▪ The lower the score, the lower the patient's neurologic function. ▪ For patients who are intubated and cannot talk, record their score with a “t” after the number for verbal response. • The reliability of the GCS is based on recording the patient's “best” response. • If the patient responds fully to voice or light touch, there is no need to progress to more vigorous or painful stimuli. • Start with the least noxious irritation or pressure and proceed to more painful stimulation if the • patient does not respond. • Begin each phase of the assessment by speaking in a normal voice. If no response is obtained, use a loud voice. If the patient does not respond, gently shake him or her. o The shaking should be similar to that used in attempting to wake up a child. • If that is unsuccessful, apply painful stimuli using one of these methods: • Supraorbital (above eyes) pressure by placing a thumb under the orbital rim in the middle of the eyebrow and pushing upward (Do not use this technique if the patient has orbital or facial fractures.) • Trapezius muscle squeeze by pinching or squeezing the trapezius muscle located at the angle of the shoulder and neck muscle. • Mandibular (jaw) pressure to the jaw by using your index and middle fingers to pinch the lower jaw. • Sternal (breastbone) rub by making a fist and rubbing/twisting your knuckles against the sternum. • Peripheral pain is assessed with pressure at the base of the nail on one finger or one toe, both on the right and left. • If the patient does not respond after 20 to 30 seconds, stop applying the painful stimulus. ◆ CRITICAL RESCUE: o A decrease of 2 or more points in the Glasgow Coma Scale total is clinically significant and should be communicated to the primary health care provider (PHCP) immediately. o Other findings requiring urgent communication with the health care provider include a new finding of abnormal flexion or extension, particularly of the upper extremities (decerebrate or decorticate posturing); o pinpoint or dilated nonreactive pupils; and sudden or subtle changes in mental status. o Remember, a change in level of consciousness is the earliest sign of neurologic deterioration. Communicate early recognition of neurologic changes to the Rapid Response Team or primary health care provider for the best opportunity to prevent complications and preserve CNS function. ◆ Psychosocial Assessment o Depression can result in cognitive and behavioral changes that are similar to delirium or dementia. o Consider using a depression screening tool such as the Center for Epidemiological Studies Depression-Revised (CESD-R) or the Geriatric Depression Scale (short form) to identify patients with depressive symptoms. ◆ Diagnostic Assessment o Fluid, electrolyte, and glucose abnormalities can cause neurologic impairment. ▪ The basic metabolic panel (BMP) and serum calcium, phosphorus, and magnesium are evaluated. o Both anemia and malnutrition can contribute to neurologic disorders. ▪ A complete blood count and serum levels of albumin and minerals/vitamins (particularly B vitamins) are collected. o Arterial blood to evaluate pH, oxygen, and carbon dioxide levels may be collected because these three results, when either too high or too low, can alter neurologic status. o For patients with a neurologic problem resulting from an infection, cultures are necessary to identify the pathogen. ◆ Imaging Assessment o For any image that involves being placed in a scanner, the nurse needs to be aware of special circumstances that can either prevent the procedure from taking place or interfere with it. o If the patient is alert and claustrophobic, two options are available: ▪ One is a mild sedative such as diazepam (Valium) to calm the patient; ▪ The other option is an open scanner. o The nurse must determine whether the patient has any metal prosthetics, such as heart valves or shrapnel in the part of the body to be scanned. ▪ If he or she does have any type of metal object in the body part to be examined, the nurse must notify the radiology department immediately because the procedure may need to be cancelled. ◆ Plain X-Rays o Used to determine bony fractures, curvatures, bone erosion, bone dislocation, and possible calcification of soft tissue, which can damage the nervous system. o In head trauma and multiple injuries, after assessing the ABCs (airway, breathing, and circulation), one of the first priorities is to rule out cervical spine fracture. o The patient must remain still during the procedure. Remind him or her that the exposure to radiation is minimal. o Any patient who cannot walk from a wheelchair to the x-ray table should be transferred to the radiology department on a stretcher. ◆ Cerebral Angiography o Cerebral angiography (arteriography) is done to visualize the cerebral circulation to detect blockages in the arteries or veins in the brain, head, or neck that impair PERFUSION. o It remains the gold standard for the diagnosis of intracranial vascular disease and is required for any transcatheter therapy or for surgical intervention. o Angiography may be used to identify aneurysms, traumatic o injuries, strictures/occlusions, tumors, blood vessel displacement from edema, and arteriovenous o (AV) malformations. • Patient Preparation o Risk factors for adverse events must be determined before scheduling the test. o Patients sensitive to iodine may be sensitive to iodinated contrast agents. o Patients with a history of hypersensitivity in general (e.g., multiple food allergies or asthma) are more likely to have an adverse reaction than the general population. o Seafood allergies are no longer considered an indicator of iodinated contrast allergy. o Patients with known contrast sensitivity are pre-treated with steroids. o To minimize the risk for aspiration during the procedure, assess for the presence of nausea or recent vomiting and medicate as needed before the test. o Ensure that the patient is NPO 4 to 6 hours before the test. o Reinforce these important points: • Your head is immobilized during the procedure. • Do not move during the procedure. • Contrast dye is injected through a catheter placed in the femoral artery. You will feel a warm or hot sensation when the dye is injected; this is normal. • You will be able to talk to the physician; let him or her know if you are in pain or have any concerns. • After all the vessels have been imaged, the radiologist reviews all the images and consults with the referring physician to decide whether the patient could benefit from a therapeutic radiologic procedure or surgery to treat the problem. • An arterial closure device is typically used to seal the artery and prevent bleeding. ◆ Follow-up Care o Follow agency policy regarding care of the injection site, which may include: • Check the dressing for bleeding and swelling around the site. • Apply an ice pack to site. • Keep the extremity straight and immobilized. • Maintain the pressure dressing for 2 hours. o Check the extremity for adequate circulation to include skin color and temperature, pulses distal to the injection site, and capillary refill. o Be sure to monitor for the risks of the procedure, including contrast reaction (usually manifested by hives and flushing), thrombosis (clotting), and bleeding o from the entry site. ▪ If bleeding is present, maintain manual pressure on the site and notify the physician immediately. ◆ Computed Tomography (CT) Scan o Quick, easy, noninvasive, painless, and least-expensive method of diagnosing neurologic problems. o Using x-rays (ionizing radiation), pictures are taken at many horizontal levels, or slices, of the brain or spinal cord. A computer then generates three-dimensional detailed anatomic pictures of tissues, typically the brain, spinal cord, or peripheral neuromuscular system in neurologic testing. o A contrast medium may be used to enhance the image. o CT scans distinguish bone, soft tissue (the brain, vascular system, and ventricular system), and fluids such as cerebrospinal fluid (CSF) or blood. ▪ Tumors, infarctions, hemorrhage, hydrocephalus, and bone malformations can also be identified. o Contrast-enhanced CT is especially useful in locating and identifying tumor types and abscesses. o For situations in which bleeding is the only concern (in trauma patients), contrast scans are not usually required. o CT angiography involves administering contrast dye IV before the CT scan. It is used to identify blockages or narrowing of blood vessels, aneurysms, and other blood vessel abnormalities. ◆ Magnetic Resonance Imaging o It does not use ionizing radiation but instead relies on magnetic fields. o Multiple sets of images are taken that are used to determine normal and abnormal anatomy. o Images may be enhanced with the use of gadolinium, a non–iodine-based contrast medium. o MRIs of the spine have largely replaced CT scans and myelography for evaluation. o Bony structures CANNOT be viewed with MRI; CT scans are the best way to see bones. o In addition to the traditional MRI, magnetic resonance angiography (MRA), magnetic resonance spectroscopy (MRS), or diffusion imaging (DI) may be requested. ▪ MRA is used to evaluate PERFUSION and blood vessel abnormalities such as an arterial blockage, intracranial aneurysms, and AV malformations. ▪ MRS is used to detect abnormalities in the brain's biochemical processes, such as that which occurs in epilepsy, Alzheimer's disease, and brain attack (stroke). ▪ DI uses MRI techniques to evaluate ischemia in the brain to determine the location and severity of a stroke. o MRI has been contraindicated for patients with cardiac pacemakers, other implanted pumps or devices, and ion-containing metal aneurysm clips. o MRI may also be contraindicated in patients who are confused or agitated, have unstable vital signs, are on continuous life support, or have older tattoos (which contain lead). ◆ Computed Tomography-Positron Emission Tomography o They are particularly useful in staging brain, spinal cord, and other primary cancers. o The physician or nuclear medicine technologist injects the patient with IV deoxyglucose, which is tagged to an isotope. The isotope emits activity in the form of positrons, which are scanned and converted into a color image by computer. o This test is used to evaluate drug metabolism and detect areas of metabolic alteration that occur in dementia, epilepsy, psychiatric and degenerative disorders, neoplasms, and Alzheimer's disease. o The level of radiation is equivalent to that of five or six x-rays but much less than exposure during CT. o Teach the patient that he or she will be NPO the night before morning testing and 4 hours before afternoon testing. o Patients with diabetes have their test in the morning before taking their antidiabetic drugs. o During this 2- to 3-hour procedure, the patient may be blindfolded and have earplugs inserted for all or part of the test. o He or she is asked to perform certain mental functions to activate different areas of the brain. ◆ Electromyography (EMG) o Used to identify nerve and muscle disorders, as well as spinal cord o disease. o Electromyography and electroneurography or nerve-conduction velocity studies (NCVSs) are usually used together and are referred to as electromyoneurography. ◆ Electroencephalography (EEG) o Records the electrical activity of the cerebral hemispheres. Each graphic recording represents electrical impulses within the brain. o The frequency, amplitude, and characteristics of the brain waves are recorded. ▪ Example: a cerebral tumor or infarct may have abnormally slow waveforms. • Pt. Prep for EEG: o Fasting is avoided before EEG testing because hypoglycemia can alter the test results. o Ensure that hair is clean and without conditioners, hair creams, lotions, sprays, or styling gels. o Teach the patient to avoid the use of sedatives or stimulants (Coffee) in the 12 to 24 hours preceding the EEG. o Ensure a quiet room with signage to inform visitors of EEG recording in progress. o Instruct the patient or family members about the reasons for periodic or continuous monitoring. The reasons for EEG monitoring include: • Determining the general activity of the cerebral hemispheres • Determining the origin of seizure activity (epilepsy) • Determining cerebral function in epilepsy and other pathologic conditions such as tumors, abscesses, cerebrovascular disease, hematomas, injury, metabolic diseases, degenerative brain disease, and drug intoxication. • Differentiating between organic and hysterical or feigned blindness or deafness • Monitoring cerebral activity during surgical anesthesia or sedation in the intensive care unit • Diagnosing sleep disorders (If the EEG is related to a sleep disorder diagnosis, the patient may be asked to sleep less the night before the EEG.) • Assisting in the determination of brain death • EEG Procedure o The patient is placed on a reclining chair or bed. Multiple electrodes are applied to the scalp with a jellylike substance and connected to the machine. o The physician or EEG technician places glue over the electrodes to prevent slippage. o The patient must lie still with his or her eyes closed during the initial recording. The rest of the test engages the patient in certain activities: hyperventilation, photic stimulation, and sleep. o Hyperventilation produces cerebral vasoconstriction and alkalosis, which increase the likelihood of seizure activity. ▪ The patient is asked to breathe deeply 20 times per minute for 3 minutes. o In photic stimulation, a flashing bright light is placed in front of the patient. Frequencies of 1 to 20 flashes per second are used with the patient's eyes open and then closed. ▪ If the patient's seizures are photosensitive in origin, seizure activity may be seen on the EEG. o A sleep EEG may be performed to aid in the detection of abnormal brain waves that are seen only when the patient is sleeping. ◆ Evoked Potentials o (Also called evoked response) measure the electrical signals to the brain generated by sound, touch, or light. These tests are used to assess sensory nerve problems and confirm neurologic conditions, including multiple sclerosis, brain tumor, acoustic neuroma (small tumors of the inner ear), and spinal cord injury. o Evoked potentials are also used to monitor brain activity in comatose patients and confirm brain death. o During evoked potentials, a second set of electrodes is attached to the part of the body that will experience sensation. A stimulus is applied, and the amount of time it takes for the impulse generated by the stimulus to reach the brain is recorded. ◆ Lumbar Puncture o Lumbar puncture (spinal tap) is the insertion of a spinal needle into the subarachnoid space between the third and fourth (sometimes the fourth and fifth) lumbar vertebrae. o A lumbar puncture (LP) is used to: • Obtain cerebrospinal fluid (CSF) pressure readings with a manometer • Obtain CSF for analysis • Check for spinal blockage caused by a spinal cord lesion • Inject contrast medium or air for diagnostic study • Inject spinal anesthetics • Inject selected drugs • Patient Prep for Lumbar Puncture o A lumbar puncture is NOT DONE for patients with symptoms indicating severely increased intracranial pressure (ICP). ▪ The procedure is also not performed in patients with skin infections at or near the puncture site because of the danger of introducing infective organisms into the CSF. • ALERT: It is very important that the patient not move during a lumbar puncture. If the patient is restless or cannot cooperate, two people may need to assist instead of one. The patient may need a sedative to reduce movement. Consider patient needs for additional assistance or sedation before beginning the procedure. o Monitor for complications, especially increased ICP (severe headache, nausea, vomiting, photophobia, and change in level of consciousness). o Serious complications of lumbar puncture, although not common, include o brainstem herniation, infection, CSF leakage, and hematoma formation. ▪ Observe the needle insertion site for leakage and notify the physician if it occurs. ▪ Provide the prescribed medication for patient report of headache. Be sure to notify the health care provider if the medication does not relieve pain. [Show More]
Last updated: 1 year ago
Preview 1 out of 34 pages
Instant download
Instant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 21, 2021
Number of pages
34
Written in
Additional information
This document has been written for:
Uploaded
Mar 21, 2021
Downloads
0
Views
28