*NURSING > MED-SURG EXAM > Med Surg Final Exam. (All)
Med Surg Final Exam.
Document Content and Description Below
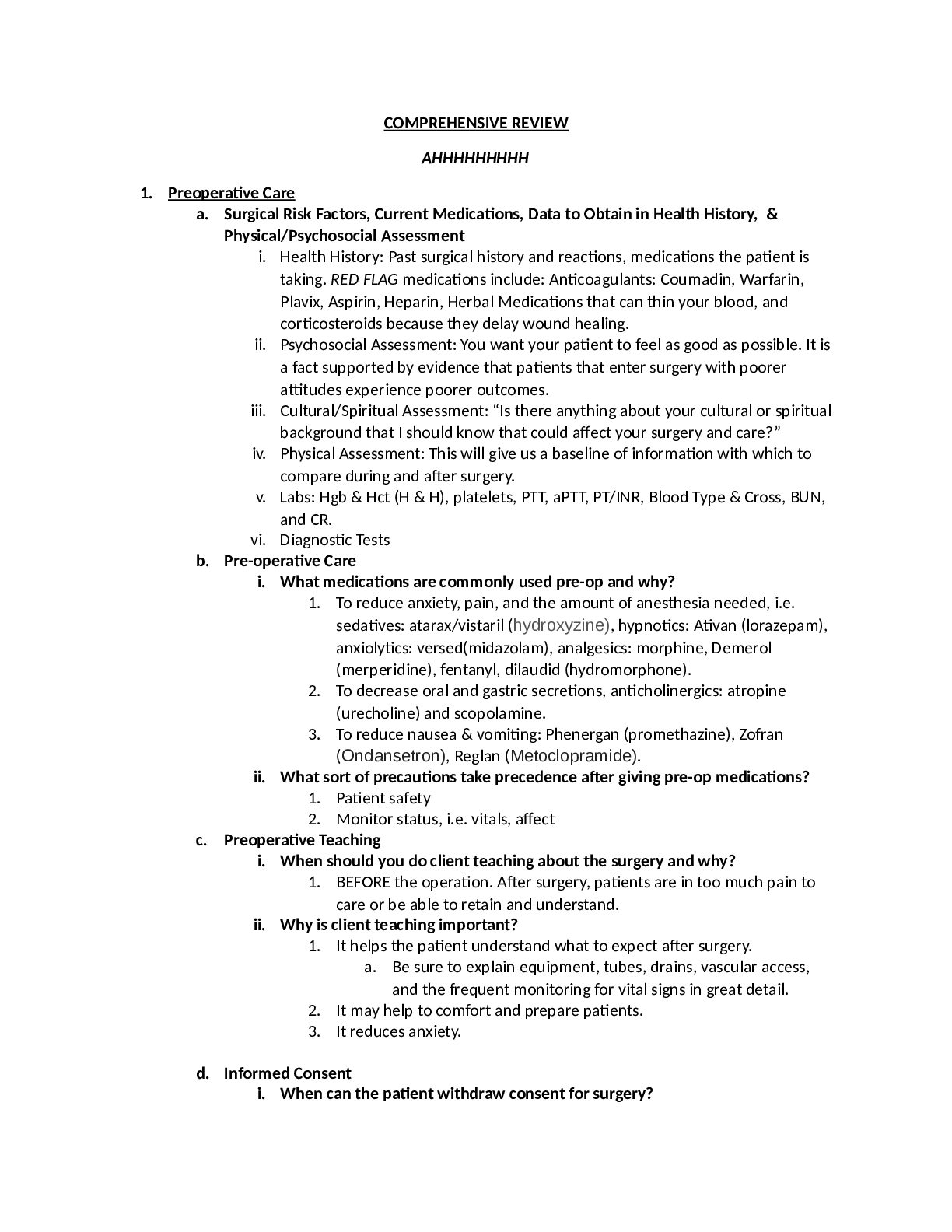
Lewis: Chapter 55 Review pathology of Benign prostatic hyperplasia (BPH), recognize clinical manifestations. ➜ Increased hormones DHT (dihydrotestosterone) ➜ Stimulation of cell growth and over... growth of prostate tissue from excessive androgen (DHT) ➜ BPH develops in the inner part of the prostate, cancer grows more commonly on the outer part. ➜ It doesn’t matter how big prostate gets, but where does enlargement occur - how close to urethra ➜ Risk Factors: ○ Aging, obesity, lack of exercise, ETOH consumption, erectile dysfunction, smoking and diabetes, positive family history. ➜ Obstructive Signs & Symptoms: ○ Decrease in caliber of force of urinary stream Difficulty in initiating urination (hesitancy) Intermittency Dribbling at end of voiding (due to urinary retention) ➜ Irritative Signs & Symptoms: ○ Urinary frequency and urgency ○ Dysuria/hematuria ○ Bladder pain ○ Nocturia (usually the first symptom) ○ Incontinence ➜ (AUA) American Urological Association uses a symptom index to assess, quantify and determine the extent of symptom severity. ➜ Complications are rare; but could include acute urinary retention ○ Urinary retention- will see sudden PAINFUL inability to urinate ○ Other complications: UTI (residual urine- favorable environment for bacteria) ○ Sepsis and urinary bladder calculi (residual urine is alkaline- calculi) ➜ When we cant get foley in ○ Treatment- catheterization (may need a coude’) ○ Placed by urology, need orders before taking out ➜ Identify medical management of BPH: ➜ Combination therapy has proven more effective than just one drug ➜ 5a reductase inhibitors ○ Examples: finasteride (Proscar), dutasteride (Avodart) ○ Block conversion of testosterone to DHT ○ Decrease size of prostate gland (decreases growth), takes a while to be effective: 3-6 months ○ Side effects: Decreased libido, decreased volume of ejaculation, erectile dysfunction ○ Drug alert: finasteride (Proscar)- increased risk of orthostatic hypotension with use of ED drugs ➜ Alpha-adrenergic blockers ○ Examples: Tamsulosin (Flomax), doxazosin (Cardura) ○ Promotes smooth muscle relaxation of bladder outlet ; facilitates urinary flow ○ Improvement in 2 to 3 weeks ○ Side effects: Orthostatic hypotension and dizziness, nasal congestion ○ Adverse drug interaction: cimetidine (Tagamet) Nursing care of the patient having a TURP: ➜ Transurethral resection (TURP) “gold standard” ○ Removal of obstructing prostate tissue using resectoscope inserted through urethra ○ Outcome for 80% to 90% is excellent ○ Relatively low risk ○ Performed under spinal or general anesthesia and requires hospital stay ○ Minimally invasive, increasing as alternative to watchful waiting or surgery ○ Less hospitalization ➜ Pre-Op: ○ Acute pain (painful-bladder distention) ○ Risk for infection from catheter stasis or pathogens ○ Ineffective therapeutic regimen management ○ Urge urinary incontinence ○ Impaired urinary elimination ○ Care: coude’ catheter, antibiotics, sexual discussion ➜ Post-Op: ○ Acute pain ○ Risk for infection ○ Risk for bleeding ○ Knowledge deficit ○ Sexual dysfunction ○ Incontinence ○ Clot retention ○ Dilutional hyponatremia ➜ TURP-surgery is still the gold standard and most commonly done procedure, however it is decreasing due to other less invasive procedures: ○ Cystoscope (camera) inserted into urethra and trims away excess prostatic tissue- enlarging passageway of urethra through prostate gland ○ Transurethral Microwave Thermotherapy- relieves obstruction by applying heat to tissue (causes death to tissue) ○ Transurethral Needle Ablation-low wave radio-frequency is used to heat the prostate, only tissue affected is that in direct contact ○ Laser Prostatectomy- laser beam is delivered-cutting, coagulation, and vaporization of prostatic tissue Nursing management of continuous bladder irrigation. ➜ Interventions: ○ CBI used to remove clotted blood from the bladder and ensure drainage of urine ○ Adjust irrigation flow rate to maintain light pink drainage (clots are expected the first 24-36 hours) ○ Encourage fluids ○ Maintain strict asepsis of indwelling catheter ○ Irrigation usually stopped after 24 hours ○ Patient may go home with regular Foley catheter ○ If outflow is less than inflow assess catheter patency for kinks or clots ○ Questionable obstruction or clotting (irrigate manually with 50 ml toomey syringe) (flush and pull back clots using sterile normal saline) ○ High risk for infection (every time you add syringe etc. direct entry) ○ If unable to irrigate and patency is blocked, notify physician. Or, if bright red and copious (notify surgeon, may be displaced cath, active arterial bleeding, dislodged clot, or increased abdominal pressure) ○ Calculate urine output: look at the amount that came out into bag (but then subtract how much fluid went in) ○ Administer analgesics/anti-spasmodics/antibiotics ○ If spasms occur, check for clots and urine flow and medicate with belladonna and opium suppositories or other antispasmodics ○ Spasms caused by resectoscope, catheter, clots leading to obstruction of catheter ○ Watch for hemorrhage for 24-48 hr (removal of the tissue can cause bleeding and clots) ○ Maintain catheter traction (3 way cath balloon used to apply gentle pressure on the prostatic fossa to prevent bleeding, 30ml balloon) How is prostate cancer diagnosed? ➜ Digital rectal exam- because cells grow on outside, will be able to feel on the outside ➜ Abnormal prostate findings include hardness, non-mobile, nodular and asymmetric. ➜ If PSA levels are continually elevated, or if the DRE is abnormal, a biopsy of the prostate tissue is usually indicated ○ PSA normal level 0-4 ➜ Usually asymptomatic in early stages (good to get the screenings to detect early) ➜ Later on: similar to BPH: dysuria, hesitancy, dribbling, frequency, urgency, hematuria, nocturia, retention, also prostate cancer grows compresses urethra like BPH, interruption of urinary stream, inability to urinate Meaning of PSA? ➜ Prostate-specific antigen, or PSA, is a protein produced by normal, as well as malignant, cells of the prostate gland. The PSA test measures the level of PSA in a man's blood. What is the nursing care after a total prostatectomy? ➜ Entire gland, seminal vesicles, and part of bladder neck are removed ➜ Retroperitoneal lymph node dissection usually done ➜ Considered most effective for long-term survival ➜ Radical prostatectomy is not an option for those with advanced disease. Used when Cancer confined to prostate, less than 70 y/o ➜ Traditional approaches are retropubic midline abdominal incision. ➜ Other new techniques include: laparoscopic and robotic-assisted ➜ There are other medications that can reduce growth or depending on staging may need chemo ➜ Patient teaching: ○ All greater than 50 years old (DRE and PSA screenings) ○ Encourage to seek support group to bond if they have been diagnosed ○ Care post-op surgical repair (VERY similar to surgery of BPH) (TURP) ➜ Major complications: ○ Erectile dysfunction: nerves needed for erection are destroyed during surgery ✗ Can be seen in aging (see Touhy) changes to erections, length of time and increased stimulation ✗ Need to be able to get adequate H & P to determine cause ✗ Could be medication related SSRI big one, chronic illness table on Touhy 33-2 (causes either psychological and physical components) ✗ Elderly female lack of estrogen, or vaginal atrophy, dryness and pain with intercourse ➜ Incontinence: bladder must be reattached to the urethra after the prostate is removed ○ Incontinence: happen over the first few months due to need to remove the neck of bladder and reattach urethra to the bladder. Over time the bladder adjusts but Kegel exercises may help (contract circumferential and perirectal muscles) ○ 10 seconds, relax for 10 seconds ○ 30-80 times daily ○ Abdominal muscles relaxed during contractions ○ Can use phosphodiesterase inhibitors (sildenafil) viagra, kegels (also for incontinence) ➜ ND: ○ Impaired urinary elimination ○ Acute pain ○ Sexual dysfunction ○ Problems with bowel ➜ Other complications are: hemorrhage, urinary retention and infection, wound dehiscence, and DVT and PE ➜ Patient catheterized for a couple of days and stay in hospital for 1 to 3 days Describe clinical manifestations, emotional component, and nursing management of problems related to male sexual function. ➜ Male erectile dysfunction involves the inability to achieve or maintain an erection suitable to complete sexual intercourse. Erection involves neurological, hormonal, arterial, cavernosal, and psychological factors. ➜ Men with ED commonly isolate themselves from others because of shame, embarrassment, and stress. Misinformation about ED may prevent the patient from seeking help for treatable problems. Many men may accept this dysfunction as a natural result of aging. ➜ Teach about possible drug treatment options: ○ Clinical trials for ED have focused on surgical techniques, PDE5 inhibitors, intracavernosal injections, and vacuum devices to decrease the incidence of ED following prostatectomy. Nerve- sparing surgical techniques promise better functioning for a large number of men with the combination of drug therapy. Lewis: Chapter 20 & 21 Explain the pathophysiology, clinical manifestations, medications used to treat conjunctivitis, cataracts, macular degeneration and glaucoma. ➜ Conjunctivitis ○ Inflammation of the conjunctiva ○ Allergic ✗ From some type of allergen or irritant and is not contagious ✗ Edema, burning, tearing, itching and bloodshot eyes ✗ Treatment: vasoconstrictors and corticosteroid eye drops ○ Infectious ✗ Caused from bacteria commonly Staph A. Haemophilus influenza, or pseudomonas aeruginosa ✗ Highly contagious ✗ Known as “pink eye” ✗ Edema, tearing and discharge with mucus ✗ Treatment: cultures, antibiotic ointment and prevention of spread of disease, HAND WASHING! ➜ Cataracts ○ Opacity within crystalline lens ○ Leading cause of blindness ○ Most common surgical procedure for those aged over 65 ○ Influencing factors ✗ Age ✗ Blunt trauma ○ Congenital factors ✗ Radiation/UV light exposure ✗ Long-term corticosteroid use ✗ Ocular inflammation ○ Senile cataract ✗ Most common type ✗ Altered metabolic processes cause ≫ Accumulation of water ≫ Altered lens fiber structure ○ Clinical manifestations: ✗ EARLY: blurred vision, decreased color perception, glaring vision ✗ LATE: diplopia, decreased visual acuity progressing to blindness, absence of red reflex, presence of white pupil ○ Classified by onset: may be present at birth or may develop at any time. ○ Cataracts may be age related, result from trauma or exposure to toxic substances. Also is associated with specific diseases or ocular disorders. ✗ Age related: lens water loss, and fiber compaction ✗ Trauma: blunt eye injury, penetrating eye injury, foreign bodies, radiation therapy ✗ Toxic cataracts: corticosteroids, miotic agents, phenothiazines ✗ Disease associated: DM, Hypothyroidism, down's syndrome, chronic sunlight exposure, glaucoma, retinal detachment ➜ Diagnostic Studies ○ History and physical examination ○ Visual acuity measurement ○ Ophthalmoscopy ○ Slit lamp microscope ○ Glare testing ➜ Glaucoma ○ A group of disorders characterized by increased IOP and consequences of elevated pressure ○ Optic nerve atrophy ○ Peripheral visual field loss ○ 2nd leading cause of blindness ○ 1st leading cause in african americans ○ Causes ✗ Aging ✗ Heredity ✗ Neurovascular disorders ✗ Trauma ✗ Ocular tumors ✗ Hx of eye surgery ✗ Associated illness: DM, HTN, severe myopia, retinal detachment ✗ Balance between aqueous production and reabsorption needed for normal level of IOP ✗ Glaucoma related to elevation of IOP ✗ When the pressure in the eye is greater than the tissue can tolerate, the cells of the retina and the optic nerve are damaged. If the condition progresses, blindness can result. ✗ IOP is the fluid pressure in the eye. Aqueous humor which is located in the anterior chamber of the eye ✗ Normal pressure is 10-21 mmHg and there is a balance between outflow and production of aqueous humor. In people with glaucoma there is a buildup of aqueous humor in the eye inside the eye, which causes pressure and a blood flow reduction to the optic nerve and retina ○ Two types ✗ Primary open-angle: most common usually bilateral and asymptomatic. Reduced outflow through the chamber angle, causing increased IOP ✗ Angle-closure glaucoma: (closed angle, narrow angle or acute glaucoma) less common, sudden onset, unilateral with pain and must be treated as an emergency, the problem is from a forward displacement of the iris causing a narrowed angle. ○ Etiology and Pathophysiology: two distinct types ✗ Open-angle glaucoma (POAG) ≫ 90% of primary glaucoma cases ≫ Outflow of aqueous humor is ↓ in trabecular meshwork ✗ Primary angle-closure Primary glaucoma (PACG) ≫ 10% of glaucoma cases ≫ Angle closure decreases the flow of aqueous humor ➜ Clinical Manifestations ○ POAG ✗ No symptoms ✗ Unnoticed until all peripheral vision is lost ✗ Eventual c/o tunnel vision ○ PACG ✗ Sudden severe pain around eye/unilateral ✗ Nausea and vomiting ✗ Seeing colored halos around lights ✗ Blurred vision ✗ Ocular redness ✗ Corneal edema ○ Diagnostic Studies ✗ Peripheral and central vision test ✗ Tonometry: screening tool, measures IOP of the eye, open angle 22-32, closed angel >50 ✗ Be sure to measure various levels throughout different times of day as they may fluctuate ✗ Gonioscopy: view of the drainage angle in the anterior chamber, the entire iridocorneal angle is examined ➜ Collaborative care ○ POAG: ✗ Drug therapy ✗ Argon laser trabeculoplasty ≫ Therapeutic option to lower IOP ≫ Laser stimulates scarring and contraction of trabecular meshwork ✗ Trabeculectomy ≫ Removal of part of iris and trabecular meshwork ≫ Aqueous humor percolates out area of missing iris ✗ Cyclocryotherapy ≫ Cryoprobe freezes part of ciliary tissue causing local destruction and ↓ aqueous production ➜ Drug therapy for COAG ○ B-adrenergic blockers ✗ Decreases aqueous humor production ✗ timolol or levobunolol (nonselective) ✗ betaxolol (cardioselective) ○ Alpha2-Adrenergic agonists ✗ Decrease aqueous humor production/increases outflow ✗ brimonidine ○ Prostaglandin Analogs: ✗ Increase aqueous humor outflow ✗ Latanoprost, travoprost ○ Carbonic anhydrase inhibitors: ✗ Decrease aqueous humor production ✗ Acetazolamide (systemic given orally) ✗ Dorzolamide (given topical) ○ Parasympathetic: ✗ Causes miosis (pupillary constriction) ✗ carbachol ✗ pilocarpine ○ PACG: emergency care required ✗ Cholinergic drops: Miotics ✗ Oral/IV hyperosmotic: Mannitol ✗ Laser peripheral iridotomy ✗ Surgical iridectomy Describe the nursing measures that promote the health of eyes and ears. ➜ Eyes ○ Wear sunglasses ○ Avoid unnecessary radiation ○ Adequate antioxidant vitamins ○ Good nutrition ○ Wear sunglasses to protect eyes ○ Wear eye protection as appropriate ○ Wash hands frequently ○ No smoking/limit alcohol ○ Control BP, glucose levels, & cholesterol ○ Eat antioxidants/green leafy veggies ○ Annual eye exams with tonometry after 40 ➜ Ears ○ Care of the ear ○ Monitor for s/s infection, drainage ○ Avoid sharp objects ○ Earplugs for swim ○ Avoid loud volume ○ Hearing protection with loud noise ○ Proper ear irrigation ○ Assistive devices ○ Telephone amplifiers ○ Hearing aids ○ Cochlear implants Explain the general pre-op and post-op care of the patient undergoing surgery of the eye. ➜ Cataracts Treatment ○ Nonsurgical therapy ✗ Visual aids (palliative) ✗ Reading glasses ✗ Magnifiers ✗ Increased lighting ✗ Lifestyle adjustments ✗ No night driving ○ Treatment for Cataracts is surgical removal of lens with implant placement ○ Surgical Therapy ✗ Preoperative phase/Preoperative Teaching ✗ Check eyesight in non-operative eye ✗ Administer eye drops using punctal occlusion (Table 22-5 in Lewis) ✗ Local anesthesia and sedatives for procedure ✗ Administer meds: sedative, diamox (acetazolamide) to reduce IOP ✗ Sympathomimetic (atropine) - drugs to achieve dilation (mydriasis and vasoconstriction) ≫ Mydriatics: dilators (atropine 1% ophthalmic soln) ✗ Parasympathomimetic drops (tropicamide) to induce paralysis to prevent lens movement ≫ Cycloplegics: to induce paralysis (tropicamide) ✗ Postoperative care: Focus on reducing IOP ✗ NO bending at waist, sneezing, coughing, straining , vomiting, sexual intercourse ✗ Outpatient procedure unless complications ✗ Antibiotic and corticosteroid eye drops ✗ Mild analgesics, NO ASPIRIN ○ Dramatic change in vision day #1 with improved vision over several weeks ○ Antibiotic ointment, and steroid ointment instillation and drops , semi-Fowler’s position or non operative side, shield may be used, watch and report drainage, analgesics and cool compresses for pain, avoid aspirin, also teaching about activities reduce IOP. ○ Notify physician immediately for pain with N and V, or s/s of infection, dramatic change in vision. ○ Most experience a dramatic change in vision the first day, but many may not have best vision until 4-6 weeks later. ➜ Ambulatory and home care ○ Educate on postoperative visual acuity ○ Instruct family to modify activities and environment ○ Remove area rugs ○ Prepare frozen meals ○ Provide audio books Explain the pathophysiology, clinical manifestations, and nursing management and collaborative care of common ear problems: Labyrinthitis & Meniere’s ➜ Labyrinthitis ○ Infection of the labyrinth, which may be a complication of otitis media ○ May be from infective materials into inner ear or the invasion of cholesteatoma (cellular overgrowth) into semicircular canal ○ Most common complication is meningitis ➜ Manifestations ○ Hearing loss ○ Tinnitus ○ Nystagmus to affected side (involuntary rapid twitching of the eyeball with EOM checks) ○ Vertigo ○ Nausea and vomiting ➜ Treatment ○ Systemic antibiotics such as ampicillin ○ Keep clients in bed in a dark room ○ Safety precautions ○ Antiemetics and antivertigo meds to treat symptoms ○ Psychosocial support ➜ Meniere’s disease ○ Endolymphatic hydrops ○ Episodes of vertigo, tinnitus, unilateral sensorineural hearing loss ○ Occurs in those 30-60 years old ○ Debilitating attacks followed by symptom free periods ○ Sense of fullness progresses to “drop attacks” ○ Severe vertigo with rapid eye movements ○ Permanent hearing loss occurs with continued attacks ○ Caused by overproduction or decreased reabsorption of endolymphatic fluid causing a distortion in the inner canal system ○ Causes thought to be from viral or bacterial infections, allergic reactions, increased fluid balances ○ Continuous ringing or noise perception in the ear, symptoms range from mild ringing - loud roaring ○ Caused by many factors: presbycusis, otosclerosis, Meniere’s, certain drugs, exposure to loud noise, inner-ear abnormalities ○ True vertigo is a real sense of whirling or turning in space. ○ Function of the vestibular system, vision and or the proprioception all contribute to the cerebellum. If any of these areas have a deficit it will cause a disturbed sense of balance or motion. ➜ Collaborative Care/Nursing Care ○ Nonsurgical ✗ Bedrest, slow head movements ✗ Dietary: salt and fluid restrictions ✗ Diuretics, antihistamines, antiemetics and sedatives ○ Surgical ✗ Labyrinthectomy (hearing is sacrificed) ✗ Endolymphatic decompression: drain placed (vertigo and hearing improved) ○ Dx: tests to R/O other causes ✗ Sensorineural hearing loss ✗ Vestibular testing. ✗ Glycerol test- improved hearing after dose of glycerol because it pulls fluid from the inner ear ○ Condition is not life threatening but decreases quality of life What are the biggest complications with labyrinthitis and Meniere’s disease? ➜ Labyrinthitis ○ Meningitis ➜ Meniere’s disease ○ Permanent hearing loss Compare the causes of conductive and sensorineural hearing losses and identify the collaborative care to treat these causes. ➜ Causes of conductive hearing loss ○ Inflammatory process of external ear ○ Obstruction of external ear with cerumen or foreign body ○ Changes in tympanic membrane (retractions, bulges, perforations) ○ Otitis media ○ Tumors, scar tissue build-up ○ Otosclerosis ○ Those associated with outer and middle ear diseases ○ Hears well in noisy environment ○ AC > BC ○ Lateralization to affected ear ➜ Causes of sensorineural hearing loss ○ Damage to CN VIII ○ Prolonged exposure to noise ○ Meniere’s disease ○ Ototoxicity ○ Presbycusis ➜ Associated with inner ear diseases: ○ Ototoxic drugs (antibiotics): gentamicin, amikacin, metronidazole ○ Diuretics: lasix, diamox, bumex and edecrin ○ NSAIDS: aspirin, ibuprofen, naproxen ○ Chemo drugs: cisplatin, vincristine ○ Miscellaneous: tegretol, plaquen [Show More]
Last updated: 1 year ago
Preview 1 out of 49 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Mar 26, 2021
Number of pages
49
Written in
Additional information
This document has been written for:
Uploaded
Mar 26, 2021
Downloads
0
Views
92

.png)