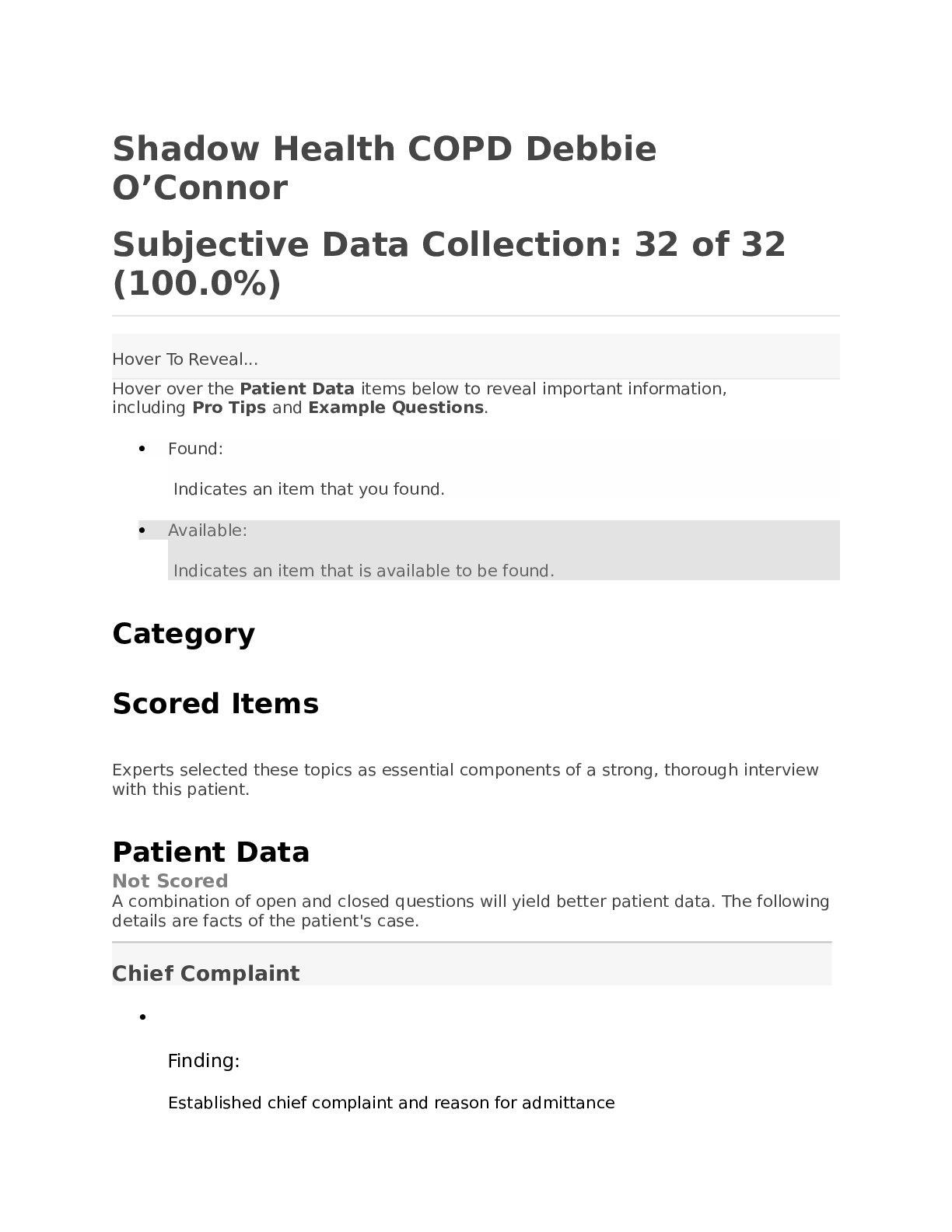
*NURSING > STUDY GUIDE > Nursing 500 Subjective Data Collection: 28 of 32 (87.5%) (All)
Nursing 500 Subjective Data Collection: 28 of 32 (87.5%)
Document Content and Description Below
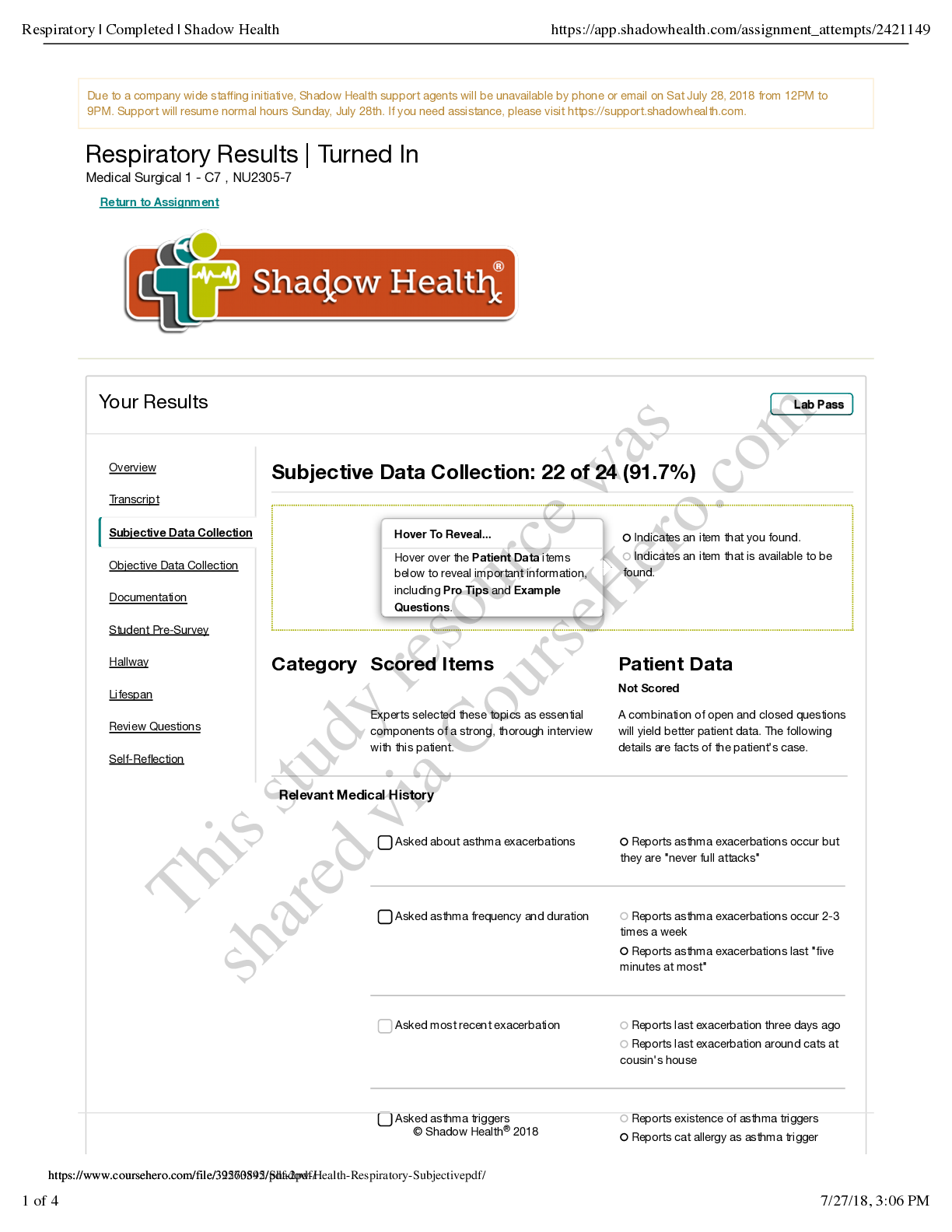
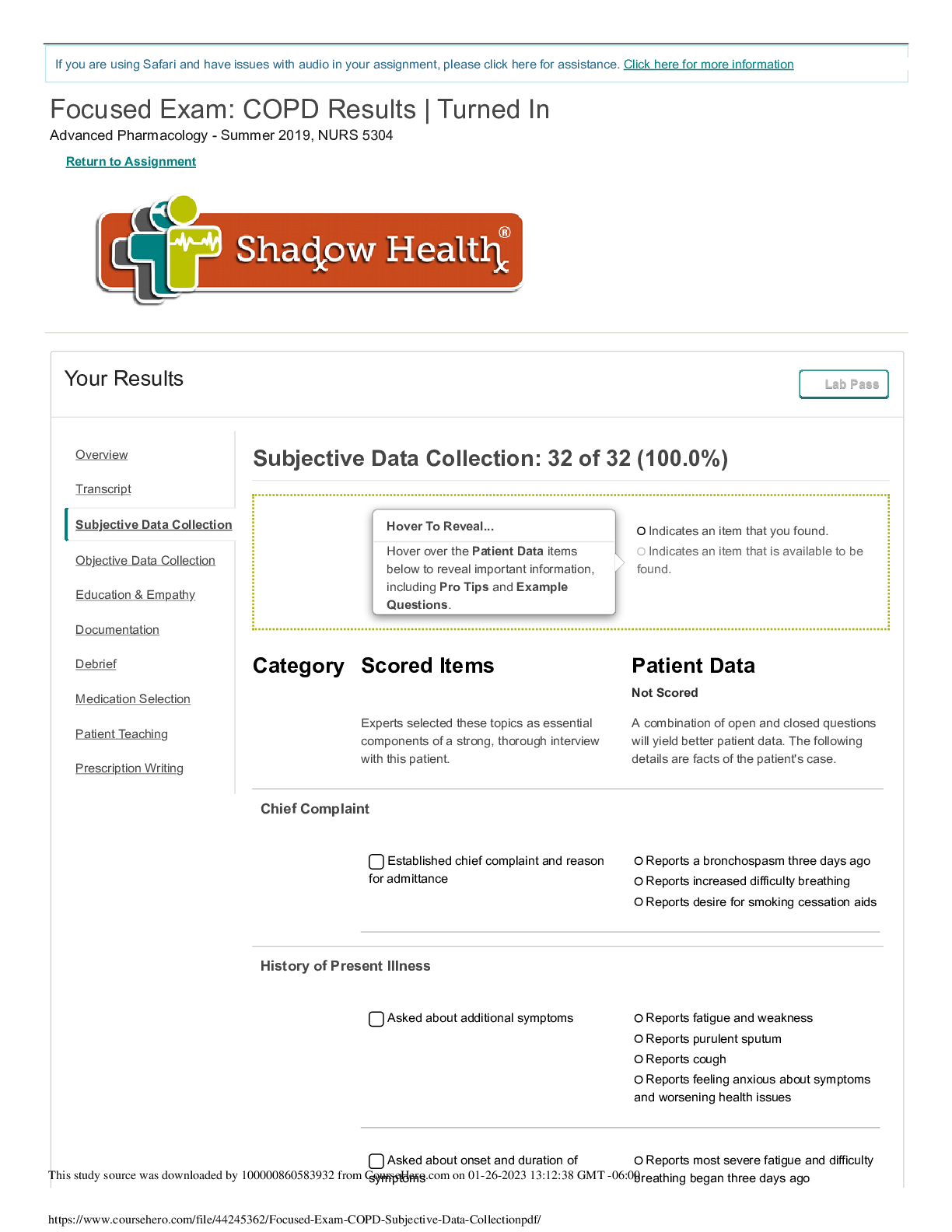
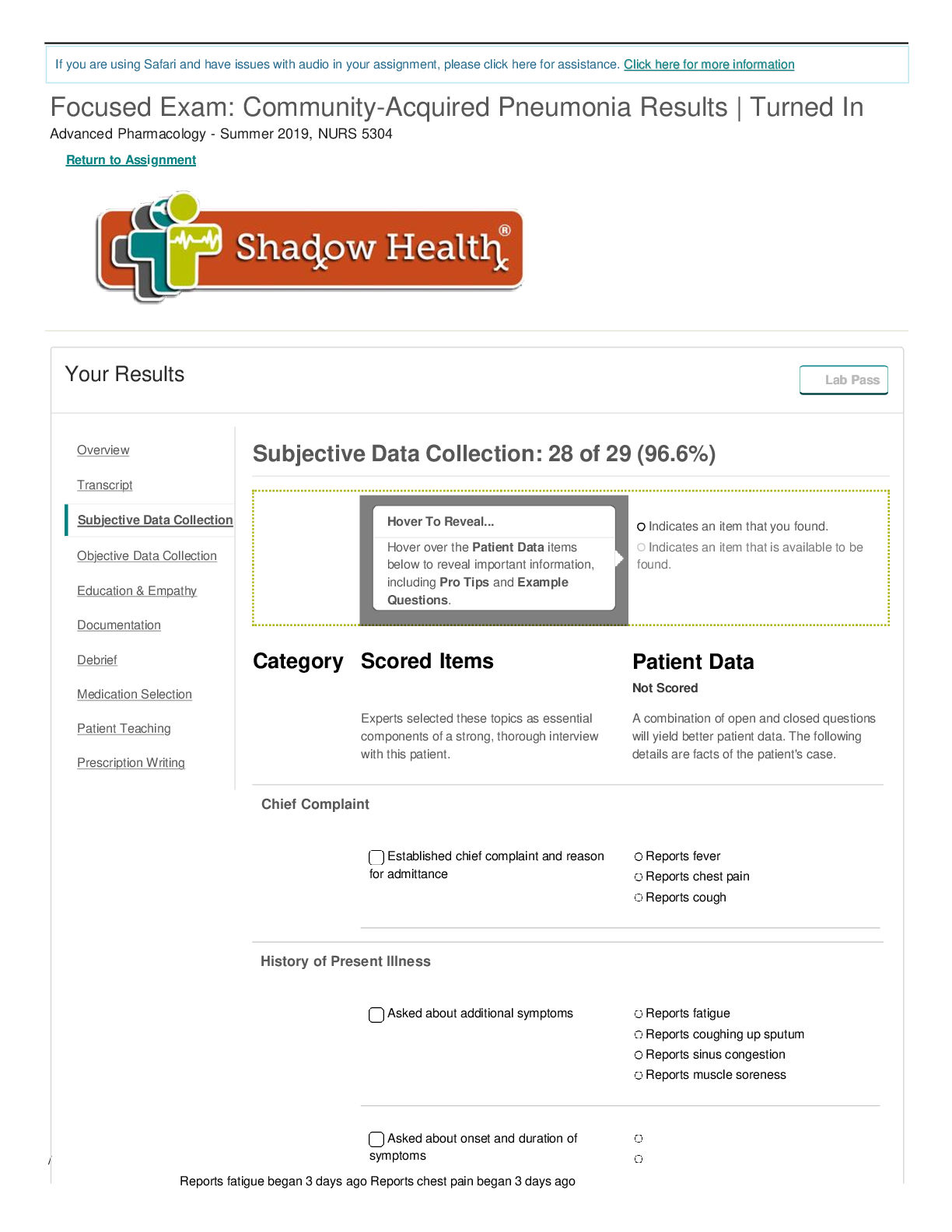
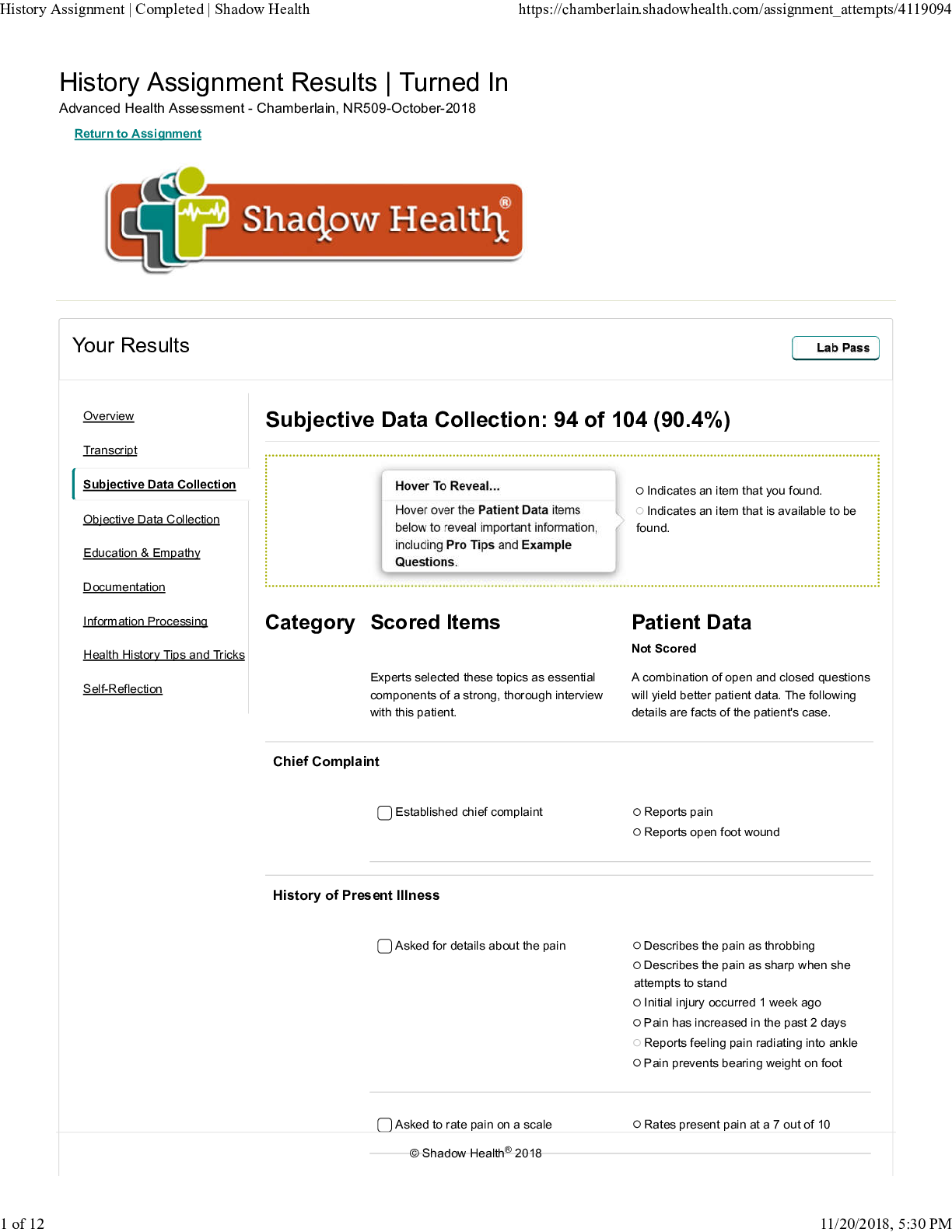
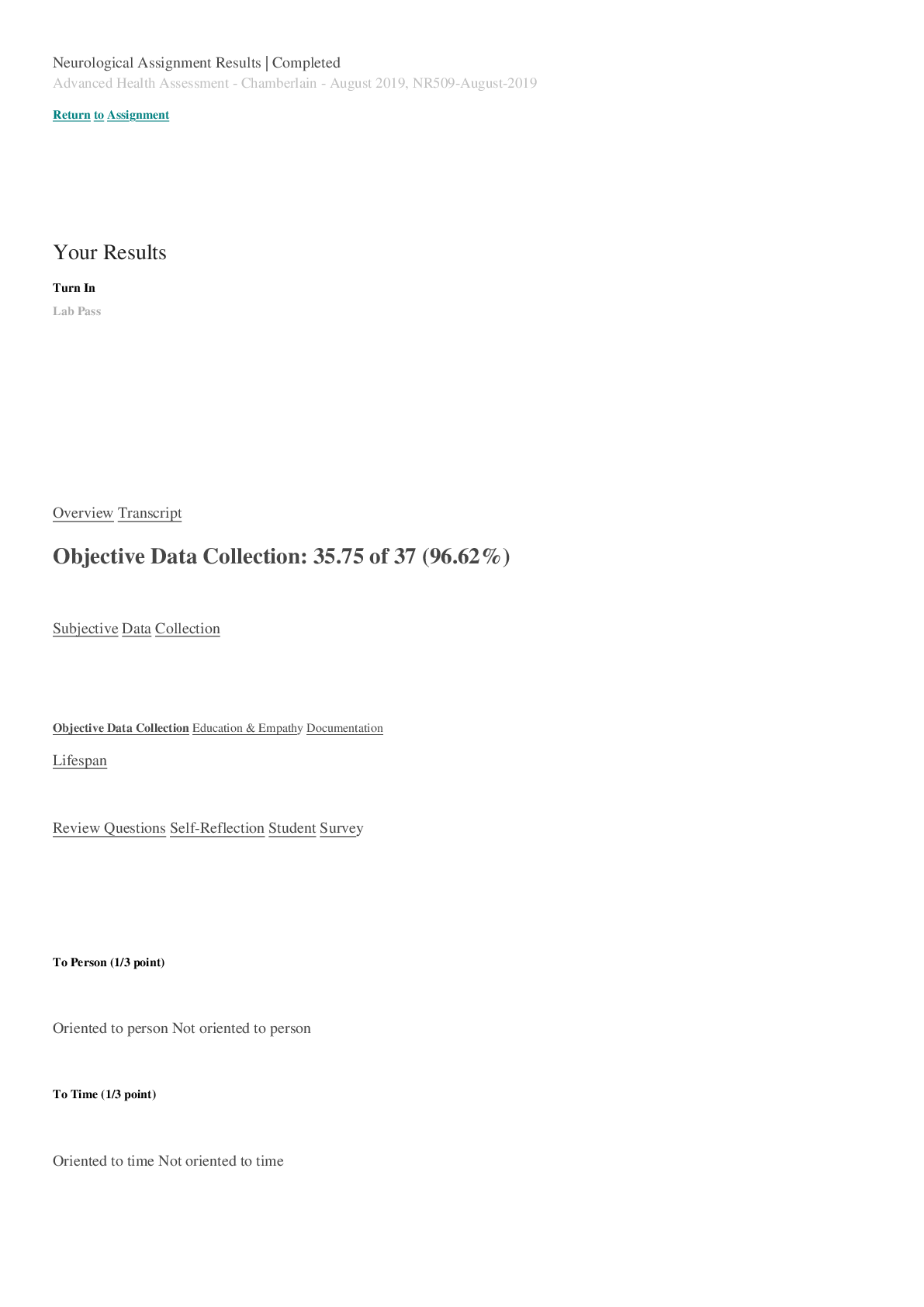
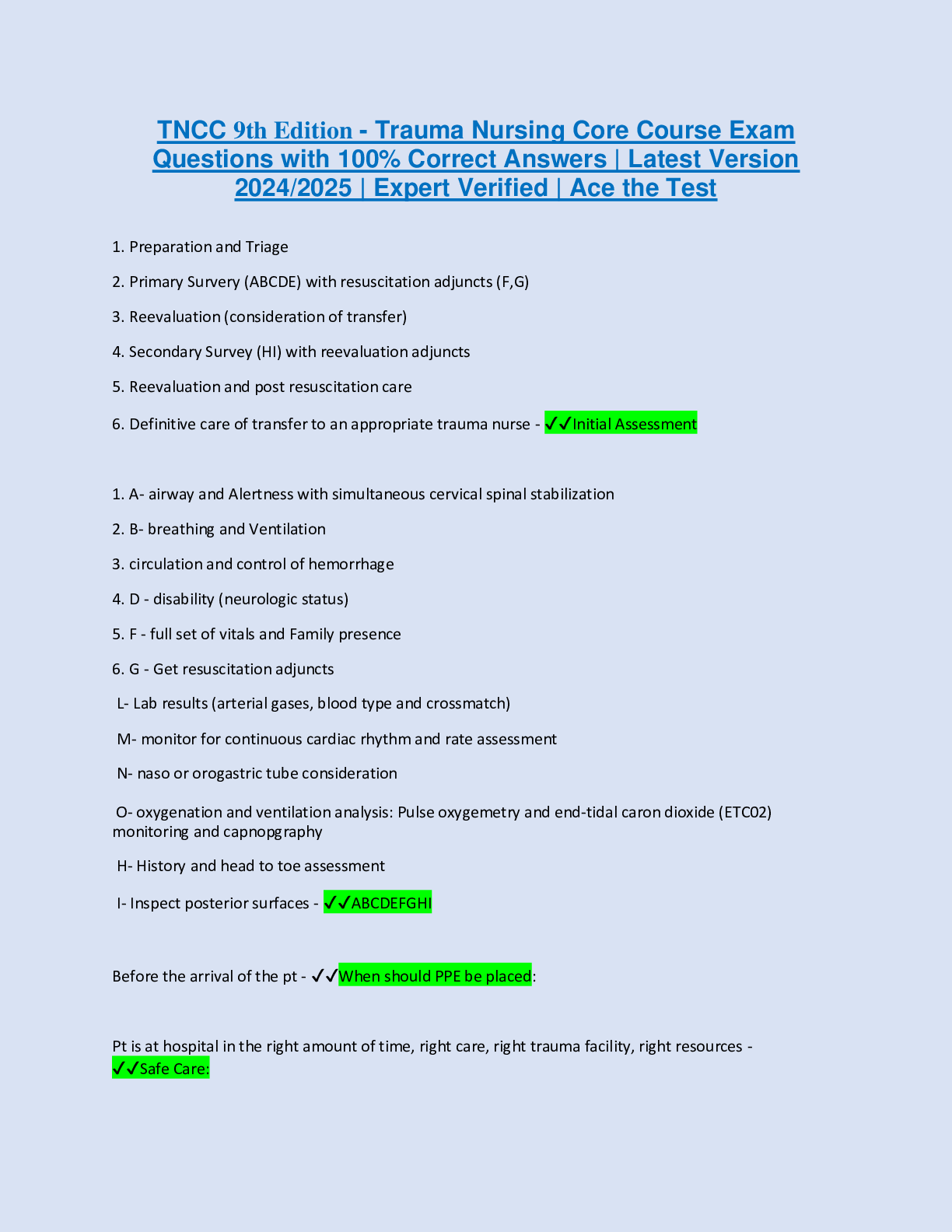
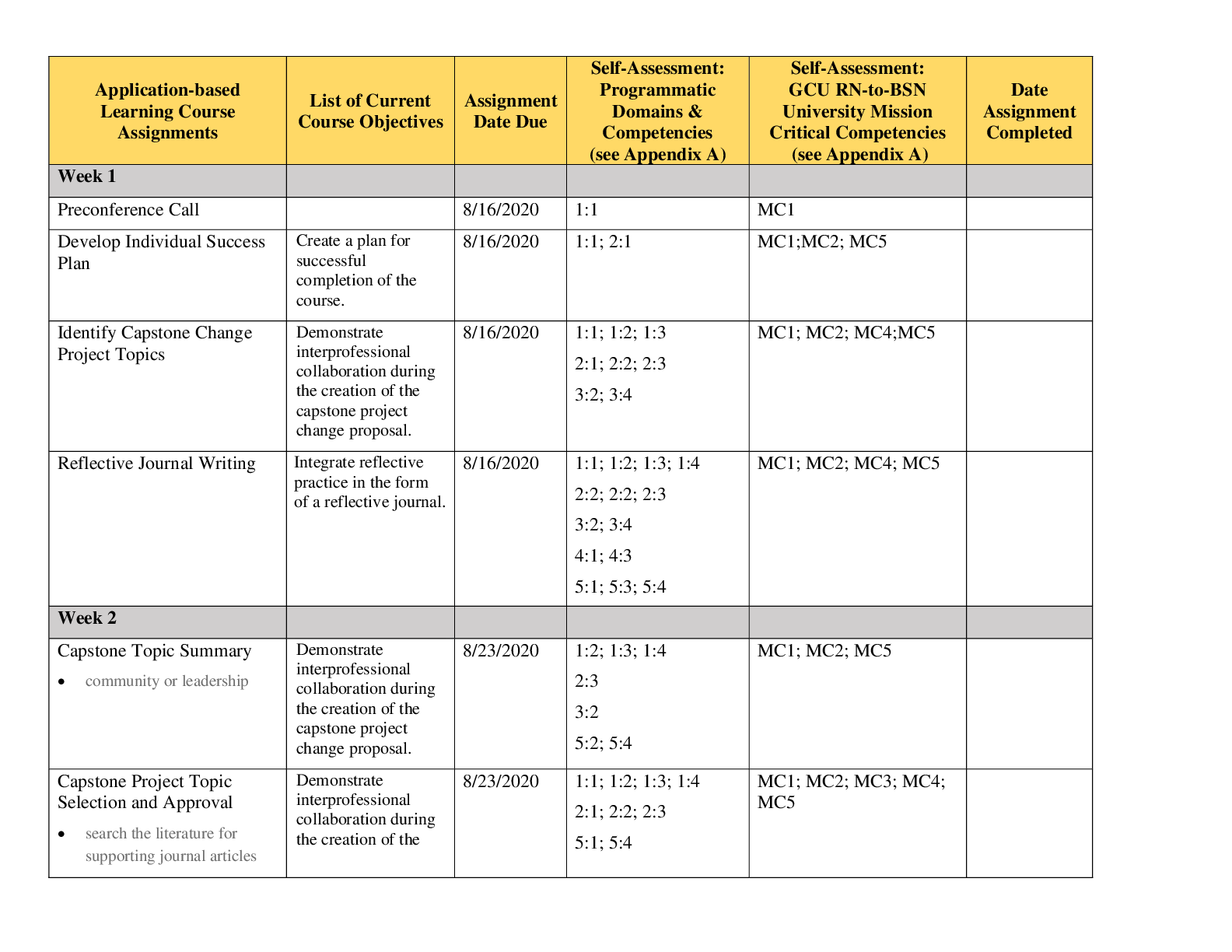
Nursing 500 Subjective Data Collection: 28 of 32 (87.5%) Hover To Reveal... Hover over the Patient Data items below to reveal important information, including Pro Tips and Example Questions. •... Found: Indicates an item that you found. • Available: Indicates an item that is available to be found. Category Scored Items Experts selected these topics as essential components of a strong, thorough interview with this patient. Patient Data Not Scored A combination of open and closed questions will yield better patient data. The following details are facts of the patient's case. Chief Complaint • Finding: Established chief complaint • Finding: Reports abdominal pain (Found) Pro Tip: Abdominal pain can be caused by problems in the underlying organs, peritoneum, muscles, or blood vessels, changes in electrolytes or other blood contents, or even anxiety. Asking for details about the pain helps to determine the origin. Example Question: Do you have any abdominal pain? • Finding: Reports difficulty "going to the bathroom" (Found) Pro Tip: Understanding all of a patient's reason for visiting is an important foundation to establish. If there are multiple symptoms, follow up on each one during your interview. Example Question: Are you able to make a bowel movement? History of Present Illness • Finding: Asked about onset, frequency, and duration of pain • Finding: Reports a feeling of discomfort for the past five days (Found) Pro Tip: Whenever you are assessing a symptom or a health condition, inquiring about onset assesses the severity and the progression of the problem. Example Question: How long have you had stomach pain? • Finding: Reports pain with gradual onset that worsened 2-3 days ago (Found) Pro Tip: Whenever you are assessing a symptom or a health condition, inquiring about onset assesses the severity and the progression of the problem. Example Question: Has the stomach pain changed? • Finding: Asked about location of pain • Finding: Reports pain in lower abdomen (Found) Pro Tip: Identification of the location of your patient's discomfort can provide important clues about its cause and how it should be best treated. Example Question: Where is your discomfort located? • Finding: Reports pain is not localized (Found) Pro Tip: Identifying the location of your patient's pain provides important clues about its cause and how to treat it best. Example Question: Is the pain in a specific spot? • Finding: Reports attempts to treat pain by drinking small sips of warm water (Available) Pro Tip: Flank pain often occurs with disorders of the urinary tract. When a patient complains of flank pain, assess for co-occurring symptoms such as fever, chills, hematuria, and dysuria. Example Question: Do you have pain on your sides? • Finding: Confirmed pain rating on a scale • Finding: Reports pain rating of 6/10 (Found) Pro Tip: For many people, it is difficult to clearly describe pain. Asking your patient to rate her pain on a scale from 0 to 10 develops a consistent measure of pain severity. Example Question: How would you rate your pain on a scale of one to ten? • Finding: Asked about character of pain • Finding: Describes pain as dull and crampy (Found) Pro Tip: Asking your patient to describe her pain helps identify its cause and the severity. Patients may not know how to answer, so you may need to suggest words like sharp, dull, burning, throbbing, or shooting. Example Question: Can you describe the pain? • Finding: Reports pain is intermittent with aggravating factors (Found) Pro Tip: It's important to ask your patient if her pain is constant or intermittent in order to determine her level of discomfort and identify the cause of the pain. Constant pain is often best managed with around-the-clock pain medications. Example Question: Is your pain constant? • Finding: Asked about treatment and relieving factors • Finding: Reports that resting helps (Found) Pro Tip: It's important to assess the nature of pain by asking about relief. If you know your patient is taking pain medication, asking about the medication's effectiveness can help you adjust treatment as needed. Example Question: What relieves your pain? • Finding: Reports attempts to treat pain by drinking small sips of warm water (Found) Pro Tip: Asking about how your patient has been managing her pain assesses her current condition and her approach to self-care. The results of her previous treatment may be helpful in your diagnosis and the development of her new treatment plan, as well as a good opportunity to educate your patient on effective self-care practices. Example Question: How have you been treating the pain? • Finding: Reports no pain medication for stomach (Found) Pro Tip: Asking about how your patient has been managing her pain assesses her current condition and her approach to self-care. The results of her previous treatment may be helpful in your diagnosis and the development of her new treatment plan, as well as a good opportunity to educate your patient on effective self-care practices. Example Question: Have you taken medication for the stomach pain? • Finding: Asked about aggravating factors • Finding: Reports pain is aggravated by eating (Found) Pro Tip: Asking you patient what aggravates her pain can point to factors that exacerbate symptoms and the ways in which your patient is approaching self-care. Example Question: Is the pain aggravated by eating? • Finding: Reports pain is aggravated by physical activity (Found) Pro Tip: Asking you patient what aggravates her pain can point to factors that exacerbate symptoms and the ways in which your patient is approaching self-care. Example Question: Is the pain aggravated by physical activity? • Finding: Asked about activities of daily life • Finding: Reports recent difficulty participating in usual activities (Available) Pro Tip: Asking about changes in activity level will help determine the level of disability caused by your patient's condition. Example Question: How has your illness affected your daily life? • Finding: Reports low energy level (Available) Pro Tip: Asking about changes in energy level will help determine the level of disability caused by your patient's condition. Example Question: Do you have low energy? • Finding: Asked about constipation • Finding: Reports current constipation (Found) Pro Tip: In geriatric patients, constipation is often caused by inadequate fluid intake, medication side effects, low-fiber diets, and difficulty ambulating to the toilet, which can result in deliberate retention of stool. Example Question: Are you constipated? • Finding: Reports no history of constipation (Found) Pro Tip: In geriatric patients, constipation is often caused by inadequate fluid intake, medication side effects, low-fiber diets, and difficulty ambulating to the toilet, which can result in retention of stool. Example Question: Are you typically constipated? • Finding: Followed up about constipation • Finding: Reports constipation for 5 days (Found) Pro Tip: Whenever you are assessing a symptom or a health condition, inquiring about onset assesses the severity and the progression of the problem. Example Question: For how long have you been constipated? • Finding: Reports no attempt to treat constipation (Found) Pro Tip: Asking about how your patient has been managing her pain assesses her current condition and her approach to self-care. The results of her previous treatment may be helpful in your diagnosis and the development of her new treatment plan, as well as a good opportunity to educate your patient on effective self-care practices. Example Question: How have you tried to treat the constipation? • Finding: Asked about diarrhea • Finding: Reports recent diarrhea (Found) Pro Tip: Whenever you are assessing a symptom or a health condition, inquiring about onset assesses the severity and the progression of the problem. Example Question: Have you recently had diarrhea? • Finding: Followed up about diarrhea • Finding: Reports diarrhea 3 days ago (Found) Pro Tip: It's important to ask about changes in stool characteristics because it may be a sign of a new onset of a gastrointestinal disease or disorder. Diarrhea is a common symptom of inflammatory bowel diseases, food allergies and intolerance, gastrointestinal infections, and many other conditions. Example Question: How long ago did you get diarrhea? • Finding: Reports diarrhea had a sudden onset (Available) Pro Tip: It's important to ask about changes in stool characteristics because it may be a sign of a new onset of a gastrointestinal disease or disorder. Diarrhea is a common symptom of inflammatory bowel diseases, food allergies and intolerance, gastrointestinal infections, and many other conditions. Example Question: Did the diarrhea happen suddenly? • Finding: Reports diarrhea lasted one day (Found) Pro Tip: It's important to ask about changes in stool characteristics because it may be a sign of a new onset of a gastrointestinal disease or disorder. Diarrhea is a common symptom of inflammatory bowel diseases, food allergies and intolerance, gastrointestinal infections, and many other conditions. Example Question: How long did your diarrhea last? • Finding: Describes diarrhea as loose and watery (Available) Pro Tip: Asking a patient who has diarrhea to describe her stool helps identify its cause and the severity. Patients may not know how to answer, so you may need to suggest words like frothy, greasy, floating, or watery. It is also important to inquire about the presence of blood or mucus. Example Question: How would you describe the diarrhea? • Finding: Asked about bowel movement patterns • Finding: Reports last bowel movement 3 days ago (Found) Pro Tip: Whenever you are assessing a symptom or a health condition, inquiring about onset assesses the severity and the progression of the problem. Example Question: When did the constipation start? • Finding: Reports some discomfort during bowel movement (Available) Pro Tip: It's important to ask about changes in stool characteristics because it may be a sign of a new onset of a gastrointestinal disease or disorder. Example Question: Do you have pain during bowel movements? • Finding: Last bowel movement was diarrhea (Found) Pro Tip: It's important to ask about changes in stool characteristics because it may be a sign of a new onset of a gastrointestinal disease or disorder. Diarrhea is a common symptom of inflammatory bowel diseases, food allergies and intolerance, gastrointestinal infections, and many other conditions. Example Question: What was the character of your last bowel movement? • Finding: Reports no mucus in stool (Available) Pro Tip: While small amounts of mucus may be present in normal stool, increased mucus in the stool is associated with a variety of intestinal disorders. Example Question: Has there been mucus in your stool? • Finding: Reports no blood in stool (Found) Pro Tip: Bloody stool is an alarming symptom that indicates bleeding in the digestive tract. Bright red bloody stool suggests bleeding in the colon or rectum. Bloody stool that appears black or tarry suggests bleeding in upper digestive tract, such as the small intestine or stomach. Example Question: Has there been blood in your stool? • Finding: Reports typically having a bowel movement almost every day (Found) Pro Tip: Asking about usual bowel movements facilitates baseline data collection. Asking specifically about bowel movement frequency aids in the identification of abnormalities. Example Question: How many bowel movements do you typically have per week? • Finding: Reports stools usually brown, formed, and soft (Found) Pro Tip: Asking about usual bowel movements facilitates baseline data collection. Asking specifically about bowel movement frequency aids in the identification of abnormalities. Example Question: Can you describe a typical bowel movement? • Finding: Asked about urination • Finding: Reports recent, slight decrease in frequency of urination (Found) Pro Tip: Frequency of urination can be an important clue to many underlying conditions. It's important to ask whether your patient has noticed changes in her typical habits. Example Question: Have you had any changes in the frequency of your urination? • Finding: Reports darker urine recently (Found) Pro Tip: Darker urination can be an important clue to many underlying conditions like cirrhosis or hepatitis. It's important to ask whether your patient has noticed changes in her typical urinary patterns. Example Question: Has your urine been darker recently? • Finding: Reports no blood in urine (Found) Pro Tip: Blood in the urine can be an important clue to many underlying conditions like cancer or kidney problems. It's important to ask whether your patient has noticed changes in her typical urinary patterns. Example Question: Have you had blood in your urine? Medical History • Finding: Asked about medications • Finding: Reports blood pressure medication (Found) Pro Tip: The medication that a patient takes will indicate any relevant health conditions, their treatment plan, and how well they comply with it. Asking about relevant medication will help you to treat your patient. Example Question: Do you take medication for your blood pressure? • Finding: Reports Accupril (Found) Pro Tip: The medication that a patient takes will indicate any relevant health conditions, their treatment plan, and how well they comply with it. Asking about relevant medication will help you to treat your patient. Example Question: What medication do you take for your blood pressure? • Finding: Accupril is 10 mg (Found) Pro Tip: The medication that a patient takes will indicate any relevant health conditions, their treatment plan, and how well they comply with it. Asking about relevant medication will help you to treat your patient. Example Question: What dose of blood pressure medication do you take? • Finding: Taken daily at 8 a.m. (Available) Pro Tip: The medication that a patient takes will indicate any relevant health conditions, their treatment plan, and how well they comply with it. Asking about relevant medication will help you to treat your patient. Example Question: When did you last take blood pressure medication? • Finding: Reports no OTC use (Found) Pro Tip: Patients should always be asked specifically about over-the-counter medications, as many patients will overlook talking about them. Over-the-counter medications can cause medical complications of their own or can indicate medical problems that your patient has been attempting to self-treat. Example Question: Do you take any over-the-counter medications? • Finding: Asked about allergies • Finding: Reports latex allergy (Found) Pro Tip: Latex allergies can cause severe and even life-threatening consequences. Always asking specifically about allergies can help ensure that your patient does not receive medication or treatment that will do her harm. Example Question: Are you allergic to latex? • Finding: Reports no medication allergies (Found) Pro Tip: Medication allergies can cause severe and even life-threatening consequences. Always asking specifically about these allergies can help ensure that your patient does not receive medication that will do her harm. Example Question: Are you allergic to any medications? • Finding: Reports no food allergies (Found) Pro Tip: Knowing your patient's food allergies prevents your patient from receiving harmful food, and it helps to identify specific allergies--such as shellfish or eggs--which can contraindicate the administration of common medications or treatments that include derivatives of these substances. Example Question: Do you have any food allergies? • Finding: Asked about general known health conditions • Finding: Reports hypertension (Found) Pro Tip: It's best to determine specifically whether or not the condition has been diagnosed by a healthcare professional. Example Question: Do you have high blood pressure? • Finding: Diagnosed with hypertension at age 54 (Available) Pro Tip: Learning the diagnosis date of your patient's illness is an essential element of the illness's history. Example Question: At what age were you diagnosed with hypertension? • Finding: Asked about relevant gastrointestinal history • Finding: Reports no history of gastrointestinal disorders (Found) Pro Tip: Broad open questions are efficient and useful in eliciting a large amount of information from your patient. Asking about any gastrointestinal problems helps guide your assessment. Example Question: Do you have any GI conditions? • Finding: Reports no history of GERD, heartburn, or ulcer (Available) Pro Tip: If a patient has a history of GERD, ulcer, heartburn, or perceived indigestion, it could contribute to her present condition. Example Question: Do you have a history of heartburn? • Finding: Reports no history of appendicitis (Available) Pro Tip: In patients with lower quadrant abdominal pain, confirming a previous appendectomy can help rule out appendicitis as a cause for her current symptoms. It is important to note that elderly patients with appendicitis may present atypically and often lack certain classic symptoms such as rebound tenderness, right lower quadrant pain, fever, and anorexia. Example Question: Have you ever had appendicitis? • Finding: Reports no history of stomach cancer (Available) Pro Tip: If a patient has a history of stomach cancer, abdominal pain could be a sign of recurrence. Example Question: Do you have a history of stomach cancer? • Finding: Reports no history of liver disease (Available) Pro Tip: A history of liver disease could cause additional gastrointestinal complaints for a patient. Example Question: Do you have a history of liver disease? • Finding: Asked about relevant history of surgery • Finding: Reports c-section (Found) Pro Tip: Information about your patient's pregnancy complications can provide you with insight into past medical conditions. Example Question: Did you have any complications during pregnancy? • Finding: C-section at age 40 (Found) Pro Tip: Information about your patient's pregnancy can provide you with insight into past medical conditions. Example Question: At what age did you have a C-section? • Finding: Reports cholecystectomy (Found) Pro Tip: Information about your patient's past surgeries can provide you with insight into past medical conditions. Example Question: Have you had your gallbladder removed? • Finding: Cholecystectomy at age 42 (Found) Pro Tip: Establishing a timeline about your patient's past surgeries can provide you with insight into past medical conditions. Example Question: At what age did you have your gallbladder removed? • Finding: Reports no post-operative complications (Found) Pro Tip: Asking about any postoperative complications in your patient's history may provide information relevant to identifying her present condition. Example Question: Did you have any complications after your surgery? Social History • Finding: Asked about diet • Finding: Reports last meal was toast at breakfast (Found) Pro Tip: A healthy and balanced diet is crucial for maintaining good health. Asking Esther about her last meal will indicate her typical eating habits and allow you to assess whether her eating habits put her at risk of cardiovascular disease or other health complications. Example Question: What was your last meal? • Finding: Typically eats 3 meals (Available) Pro Tip: A healthy and balanced diet is crucial for maintaining good health. Asking Esther about what she typically eats will allow you to assess whether her eating habits put her at risk of cardiovascular disease or other health complications. Example Question: How many meals do you typically eat in a day? • Finding: Typically does not eat snacks (Available) Pro Tip: A healthy and balanced diet is crucial for maintaining good health. Asking Esther about what she typically has for a snack will allow you to assess whether her eating habits put her at risk of cardiovascular disease or other health complications. Example Question: What is a typical snack for you? • Finding: Typical breakfast is a piece of fruit (Found) Pro Tip: A healthy and balanced diet is crucial for maintaining good health. Asking Esther about what she typically eats for breakfast will allow you to assess whether her eating habits put her at risk of cardiovascular disease or other health complications. Example Question: What do you usually eat for breakfast? • Finding: Typical lunch is soup, sometimes skips lunch (Available) Pro Tip: A healthy and balanced diet is crucial for maintaining good health. Asking Esther about what she typically eats for lunch will allow you to assess whether her eating habits put her at risk of cardiovascular disease or other health complications. Example Question: What do you usually eat for lunch? • Finding: Typical dinner is chicken or fish with vegetables and rice (Available) Pro Tip: A healthy and balanced diet is crucial for maintaining good health. Asking Esther about what she typically eats for dinner will allow you to assess whether her eating habits put her at risk of cardiovascular disease or other health complications. Example Question: What do you usually eat for dinner? • Finding: Asked about fiber intake • Finding: Reports no fiber supplements (Available) Pro Tip: A high fiber diet helps to reduce constipation. Asking Esther if she takes fiber supplements will help you to assess whether she gets enough fiber in her diet. Example Question: Do you take fiber supplements? • Finding: Reports belief that she gets enough fiber (Available) Pro Tip: A high fiber diet helps to reduce constipation. Asking Esther about her fiber consumption will help you to assess whether she gets enough fiber in her diet. Example Question: Do you think you get enough fiber? • Finding: Reports getting fiber from a daily vegetable (Available) Pro Tip: A high fiber diet helps to reduce constipation. Asking Esther what sources of fiber she eats will help you to assess whether she gets enough fiber in her diet. Example Question: What sources of fiber do you eat? • Finding: Reports getting fiber from a daily piece of fruit (Available) Pro Tip: A high fiber diet helps to reduce constipation. Asking Esther what sources of fiber she eats will help you to assess whether she gets enough fiber in her diet. Example Question: Do you eat fruit? • Finding: Asked about fluid intake • Finding: Reports no increase in thirst (Available) Pro Tip: An increase in thirst can mean a variety of underlying conditions. Asking your patient if she has been thirstier than usual can indicate a possible underlying symptom. Example Question: Have you had an increase in thirst? • Finding: Reports decreased fluid intake for the last few days (Found) Pro Tip: Asking about fluid intake is a key component of a thorough health assessment. Inadequate fluid intake is a common problem among aging adults. Example Question: Have you had changes in your fluid intake? • Finding: Typical fluid intake is six glasses of water a day (Found) Pro Tip: Asking about fluid intake is a key component of a thorough health assessment. Inadequate fluid intake is a common problem among aging adults. Example Question: What is your typical fluid intake in a day? • Finding: Reports sometimes drinking chamomile tea (Available) Pro Tip: Asking about fluid intake is a key component of a thorough health assessment. Inadequate fluid intake or dehydration can be a common problem among aging adults. Example Question: What fluids do you drink? • Finding: Denies drinking caffeinated drinks such as coffee or soda (Available) Pro Tip: Asking about fluid intake is a key component of a thorough health assessment. Inadequate fluid intake or dehydration can be a common problem among aging adults. Example Question: Do you drink caffeinated beverages? • Finding: Asked about substance use • Finding: Reports no illicit drug use (Found) Pro Tip: Many drugs affect the central nervous system or can cause cardiovascular complications. Asking Esther if she uses illicit drugs will indicate whether drug use puts her at risk for health complications. Example Question: Do you use illicit drugs? • Finding: Reports no cigarette smoking (Found) Pro Tip: Tobacco affects the heart by reducing the amount of oxygen the blood is able to carry. Asking Esther if she uses tobacco will allow you to assess whether the condition is caused, in part, by tobacco use. Example Question: Do you smoke cigarettes? • Finding: Reports low alcohol consumption (Found) Pro Tip: Chronic alcohol use can result in cardiomyopathy. Asking Esther whether she drinks alcohol will allow you to assess whether she has any indicators of alcoholism. Example Question: Do you consume alcohol? • Finding: Followed up about alcohol consumption • Finding: Reports drinking 1 night a week (Found) Pro Tip: Finding out the number of nights a patient drinks each week is a good baseline for asking additional questions about alcohol consumption. Example Question: How many nights a week do you drink alcohol? • Finding: Reports 1 drink per sitting (Found) Pro Tip: The number of drinks the patient has in one sitting is in important indicator of binge drinking. Example Question: How many drinks do you have in one sitting? • Finding: Reports 4 drinks per month (Available) Pro Tip: Asking the patient how many drinks she has per month is a way to gauge her understanding of her own level of drinking. Example Question: How many alcoholic drinks do you have in a month? • Finding: Reports typical drink is white wine (Available) Pro Tip: The type of drink the patient consumes gives you a basic indicator of what proof of alcohol the patient is ingesting. Example Question: When you have alcohol, what do you typically drink? • Finding: Asked about health maintenance • Finding: Reports annual check-ups (Available) Pro Tip: Access to healthcare and resources heavily influences one's health condition. This information can be helpful when educating your patient and developing a discharge plan. Example Question: Do you have a primary care doctor? • Finding: Reports most recent Pap smear > 10 years ago (Available) Pro Tip: A regular Pap smear is indicated for female patients between 21 and 65. Checking your patient's screening status can give important information about overall health care compliance as well as gynecological health. Example Question: When was your last pap smear? • Finding: Reports belief that her level of health and activity is very good for her age (Found) Pro Tip: Your patient's perception of health provides insight into her self-awareness, her health goals, and her approach to self-care. This information should be considered when developing her plan of care. Example Question: Do you feel you are healthy? • Finding: Reports no STI testing (Available) Pro Tip: When assessing your patient's sexual health, it is critical to ask whether she has been tested for sexually transmitted infections. As many sexually transmitted infections are asymptomatic in women, your patient may not recognize if she has been infected. Example Question: Have you ever been tested for STIs? • Finding: Reports colonoscopy 10 years ago (Available) Pro Tip: Colonoscopies are an important part of geriatric health maintenance. Establishing Esther's last colonoscopy will help you assess any possible complications with her colon. Example Question: Have you had a colonoscopy? • Finding: Asked about activity level • Finding: Reports high level of mobility and independence (Available) Pro Tip: Determining your patient's typical level of mobility will help you assess any current disability related to their illness. Example Question: Do you stay active? • Finding: Reports moderate activity level (Available) Pro Tip: Assessing your patient's typical level of activity will help you determine the level of disability associated with their current medical condition. Example Question: What is your typical activity level? • Finding: Regularly attends fitness class (Available) Pro Tip: Assessing your patient's typical level of activity will help you determine the level of disability associated with their current medical condition. Example Question: Do you exercise? • Finding: Reports gardening as a hobby (Available) Pro Tip: Assessing your patient's typical level of activity will help you determine the level of disability associated with their current medical condition. Example Question: What are your hobbies? • Finding: Asked about family and support system • Finding: Reports living with her daughter (Found) Pro Tip: Asking your patient whom she lives with will help to identify any caregivers in the home who are available to assist her. Living situation can also relay information about your patient's relationships, socioeconomic status, functional ability, and sense of self. Example Question: Do you live with anyone? • Finding: Reports strong familial support system (Found) Pro Tip: Social support is important for coping with daily stressors and for maintaining quality of life. Your patient's relationships with others can be assessed by your asking about social support. Example Question: Who can you go to for support? • Finding: Reports no recent travel (Available) Pro Tip: Recent travel or new experiences can result in gastrointestinal or other stressors. Asking Esther if she's traveled recently might reveal a new experience that's affected her health. Example Question: Have you traveled recently? • Finding: Asked about current sexual activity • Finding: Reports currently sexually active (Available) Pro Tip: Sexual activity can increase your patient's risk factor for sexually transmitted infections, so it's important to ask specifically about current sexual activity. Example Question: Are you sexually active? • Finding: Reports no vaginal intercourse (Available) Pro Tip: Sexual intercourse can increase your patient's risk factor for sexually transmitted infections. If your patient engages in vaginal or anal intercourse, it is important to ask specifically about number of partners and measures taken to reduce the risk of STIs. Example Question: Do you have vaginal intercourse? • Finding: Reports oral sex (Available) Pro Tip: Oral sex can increase your patient's risk factor for sexually transmitted infections. If your patient engages in oral sex, it is important to ask specifically about number of partners and measures taken to reduce the risk of STIs. Example Question: Do you have oral sex? Review of Systems • Finding: Asked about general symptoms • Finding: Reports no recent fever (Found) Pro Tip: When a patient presents with abdominal pain, the presence or absence of fever may help identify the patient's condition. Example Question: Have you had a fever recently? • Finding: Reports no chills (Found) Pro Tip: If a patient has chills, it could indicate the onset of a fever. Example Question: Have you had chills recently? • Finding: Reports no night sweats (Available) Pro Tip: Night sweats can be a symptom of conditions such as perimenopause, or diseases or serious physical ailments. Example Question: Have you had night sweats? • Finding: Reports short-term feeling of exhaustion (Available) Pro Tip: Asking about fatigue as a symptom is an important gauge for the seriousness of a patient's condition, and as an indicator of the impact on the patient's daily life. Example Question: Do you have fatigue? • Finding: Asked review of systems for gastrointestinal • Finding: Reports bloating (Available) Pro Tip: Bloating can occur alone or as a symptom of an underlying disorder. It is important to assess other symptoms in order to determine the cause of bloating. Example Question: Do you feel bloated? • Finding: Reports slight increase in flatus (Found) Pro Tip: While the normal frequency of burping and flatus varies widely, a sudden or marked increase in gas can be a symptom of a gastrointestinal disorder. When a patient complains of increased gas, it is important to identify any co-occurring symptoms. Example Question: Do you have more gas than usual? • Finding: Reports loss of appetite (Found) Pro Tip: Assessing appetite guides understanding of patient health. Lack of appetite may indicate an abnormality. Example Question: How is your appetite? • Finding: Reports no nausea (Found) Pro Tip: Nausea is an important subjective symptom to understand in any gastrointestinal complaint. Example Question: Do you have nausea? • Finding: Reports no vomiting (Found) Pro Tip: Presence of vomiting would indicate a complaint such as food poisoning or infection. Example Question: Have you been vomiting? • Finding: Reports no recent weight changes (Found) Pro Tip: Changes in weight can be a symptom of many medical conditions or may simply be a result of a change in lifestyle. Asking about weight changes during your assessment will enable you to more effectively understand your patient's overall health. Example Question: Have you had any recent weight changes? • Finding: Reports no exposure to food poisoning (Available) Pro Tip: If a patient has a past experience with food poisoning, she may be able to compare and contrast her present symptoms with previous illnesses. Example Question: Do you have food poisoning? • Finding: Asked review of systems for genitourinary • Finding: Reports no painful urination (Available) Pro Tip: It is important to ask about dysuria to assess for infection or inflammation of the urinary tract. Example Question: Do you have any pain when you urinate? • Finding: Reports no burning with urination (Found) Pro Tip: It is important to ask about dysuria to assess for infection or inflammation of the urinary tract. Example Question: Do you have burning with urination? • Finding: Reports no urinary incontinence (Found) Pro Tip: Stress incontinence is common in geriatric women, particularly those who have had multiple vaginal deliveries. It's important to ask about incontinence, especially during physical strain, laughing, coughing, or sneezing. Example Question: Do you have problems holding your urine? • Finding: Reports no history of UTIs (Available) Pro Tip: A history of frequent or severe UTIs could lead to scar tissue in the urinary tract, bladder, or kidneys. Example Question: Do you have a history of urinary tract infections? • Finding: Reports no gynecological problems (Found) Pro Tip: Broad open questions are efficient and useful in eliciting a large amount of information from your patient. Asking about any gynecological problems should guide your assessment. Example Question: Do you have any gynecological problems? • Finding: Reports no vaginal bleeding (Available) Pro Tip: Postmenopausal vaginal bleeding is an abnormal finding that can often be attributed to the thinning of uterine and vaginal linings. However, it may also occur due to trauma, certain cancers, and infections, including STDs. Example Question: Do you have vaginal bleeding? • Finding: Reports no vaginal discharge (Found) Pro Tip: A patient whose vaginal discharge is foul-smelling, yellow or green, or curdlike, or irritating should be assessed for disorders of the reproductive system, including STIs. Example Question: Do you have vaginal discharge? • Finding: Onset of menopause was age 54 (Available) Pro Tip: Establishing a timeline for when Esther began menopause is important in assessing her gynecological history and understanding any concerns she might have. Example Question: When did you start menopause? • Finding: Reports no history of kidney problems (Available) Pro Tip: If a patient has a history of kidney problems, it could contribute or relate to her present condition. Example Question: Do you have a history of kidney disease? • Finding: Reports no history of bladder problems (Found) Pro Tip: If a patient has a history of bladder problems, it could contribute or relate to her present condition. Example Question: Do you have a history of bladder disease? • Finding: Asked review of systems for respiratory • Finding: Denies sore throat (Available) Pro Tip: A sore throat could be a symptom of gastrointestinal conditions such as GERD. Example Question: Do you have a sore throat? • Finding: Denies coughing (Found) Pro Tip: Coughing could be a symptom of gastrointestinal conditions such as GERD. Example Question: Have you been coughing? • Finding: Denies dysphagia (Found) Pro Tip: Difficulty swallowing could be a symptom of gastrointestinal conditions such as GERD. Example Question: Do you have dysphagia? Denies dysphagia (Found) Subjective Action Pro Tip: Difficulty swallowing could be a symptom of gastrointestinal conditions such as GERD. Example Question: "Do you have dysphagia?" • Finding: Denies difficulty breathing (Found) Pro Tip: Difficulty breathing could be an indicator that the patient's condition is serious. It's important to confirm that a patient is able to breathe without problems. Example Question: Have you had difficulty breathing? • Finding: Denies chest pain or tightness (Found) Pro Tip: Chest discomfort could be a symptom of gastrointestinal conditions such as GERD. Example Question: Do you have chest pain? • Finding: Denies change in sense of taste (Available) Pro Tip: Changes in a patient's sense of taste Example Question: Have you had a change in taste? [Show More]
Last updated: 1 year ago
Preview 1 out of 39 pages
Instant download
Instant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 08, 2021
Number of pages
39
Written in
Additional information
This document has been written for:
Uploaded
Apr 08, 2021
Downloads
0
Views
47


.png)
.png)