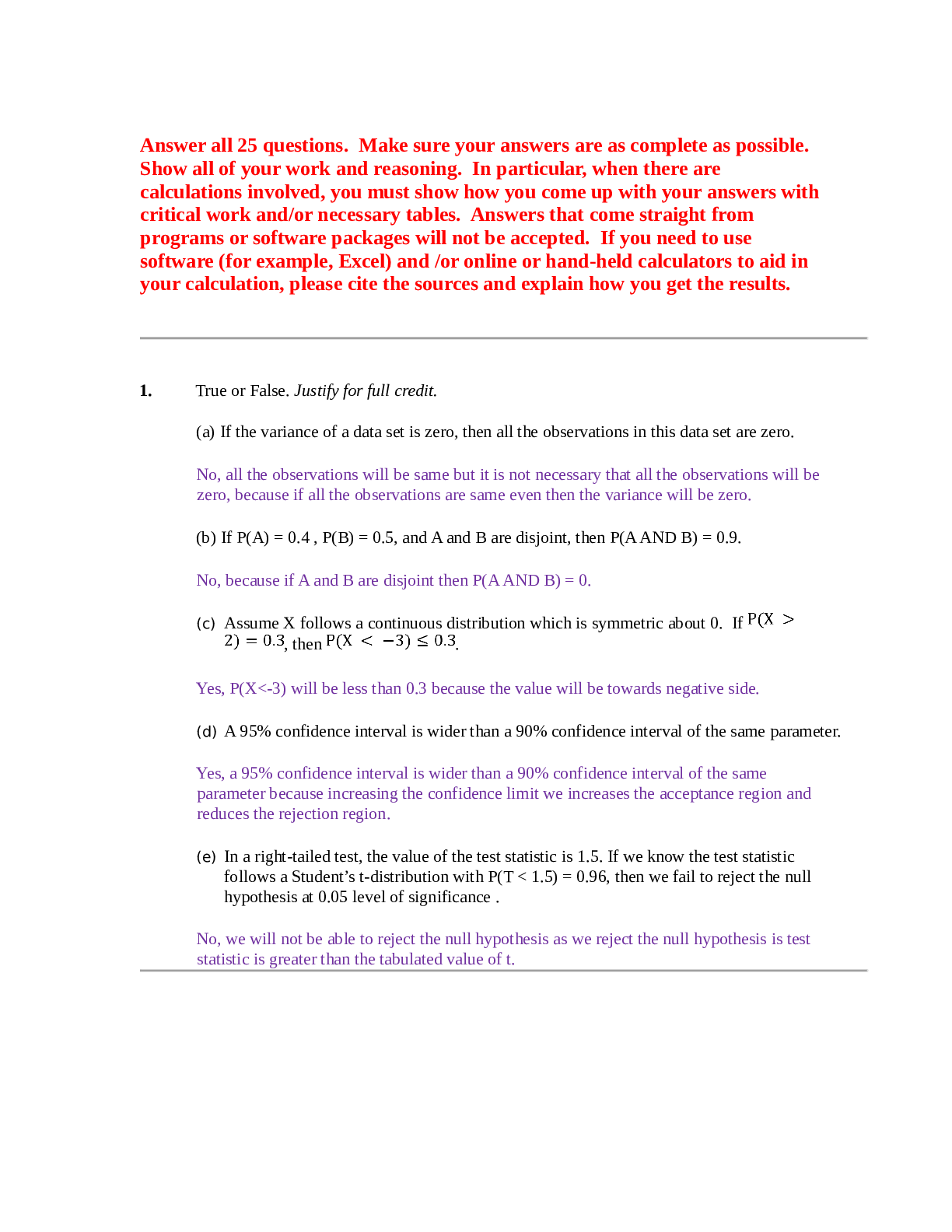
PATHO TEST 1. QUESTIONS AND ANSWERS. CHAPTER 1 – 30/GRADE A
Document Content and Description Below
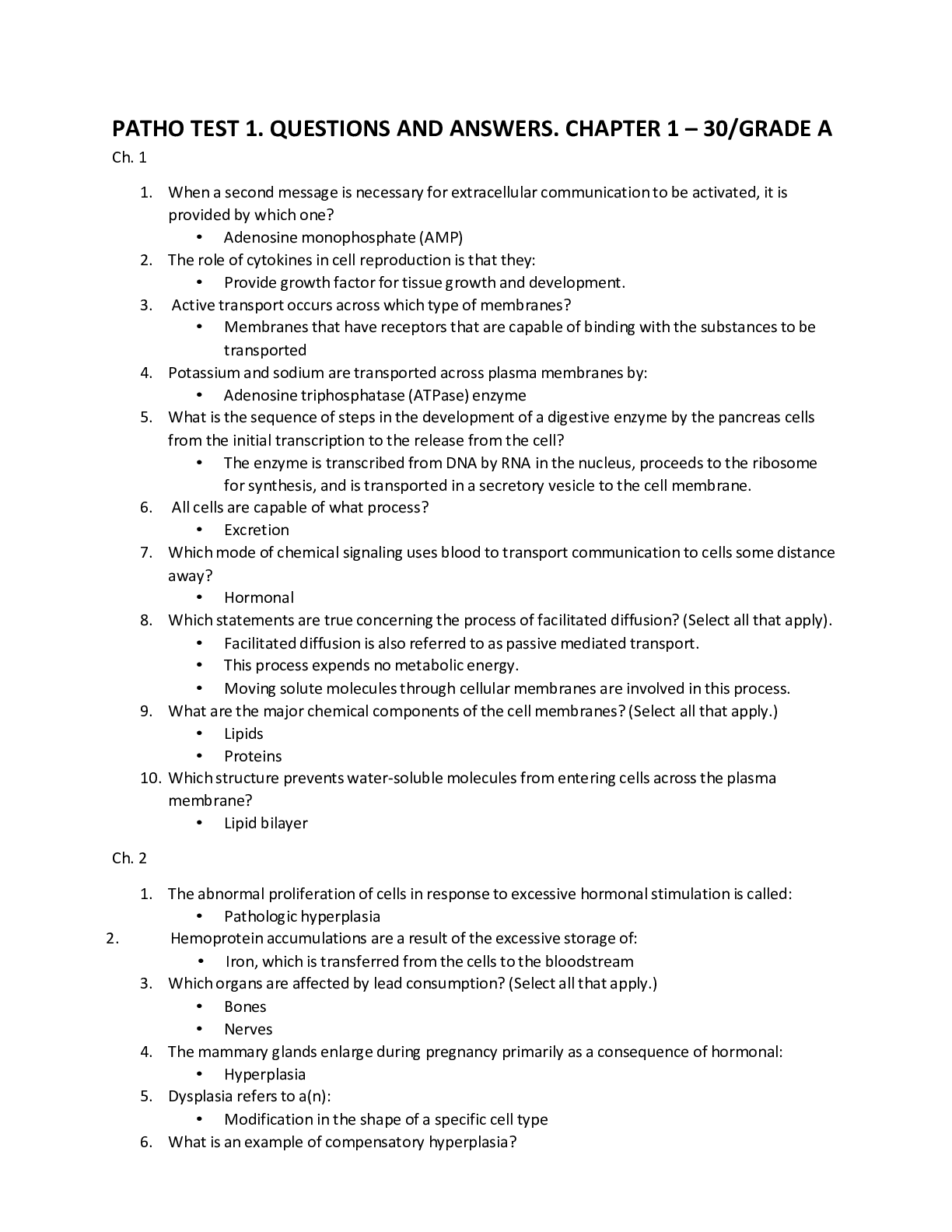
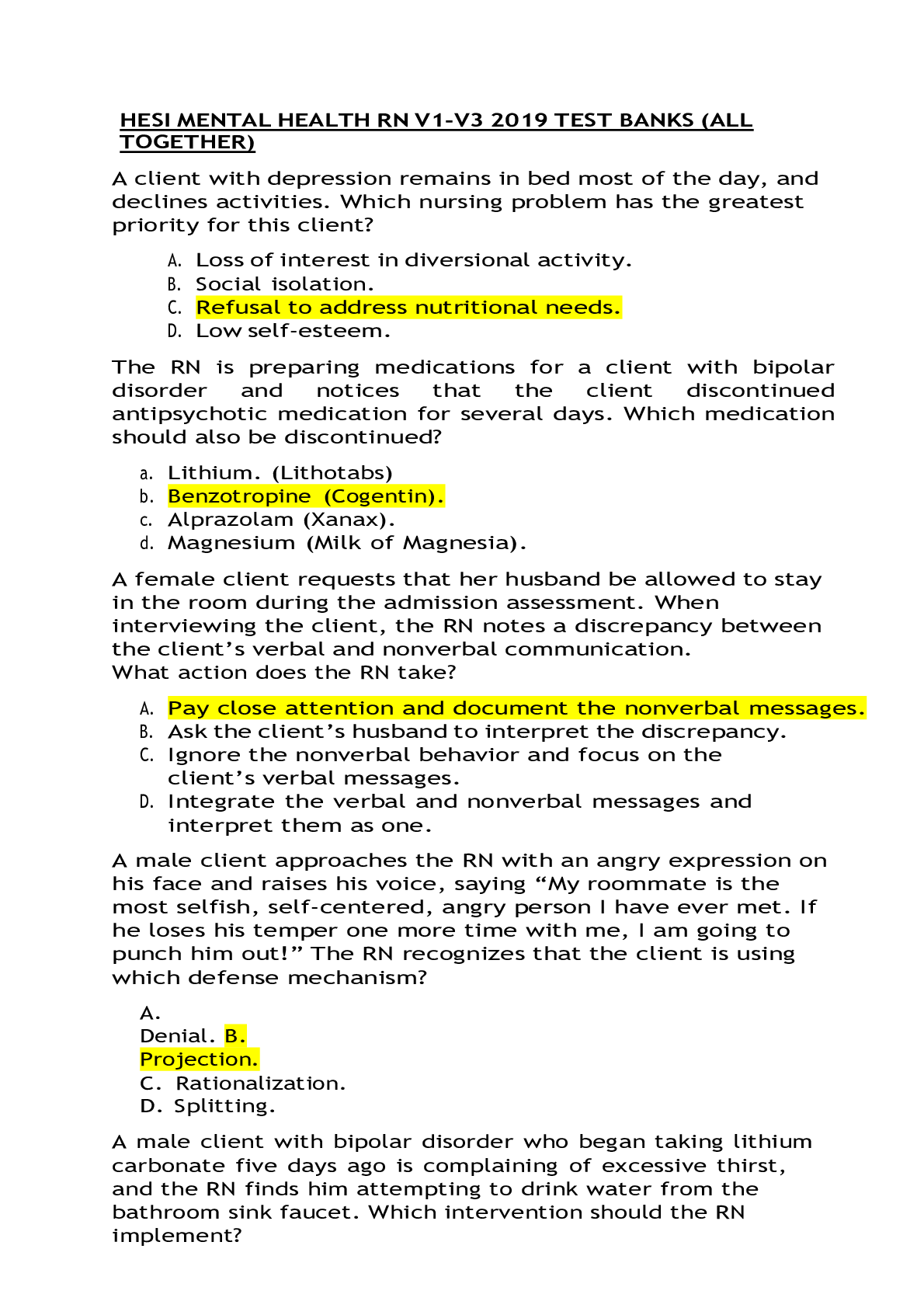
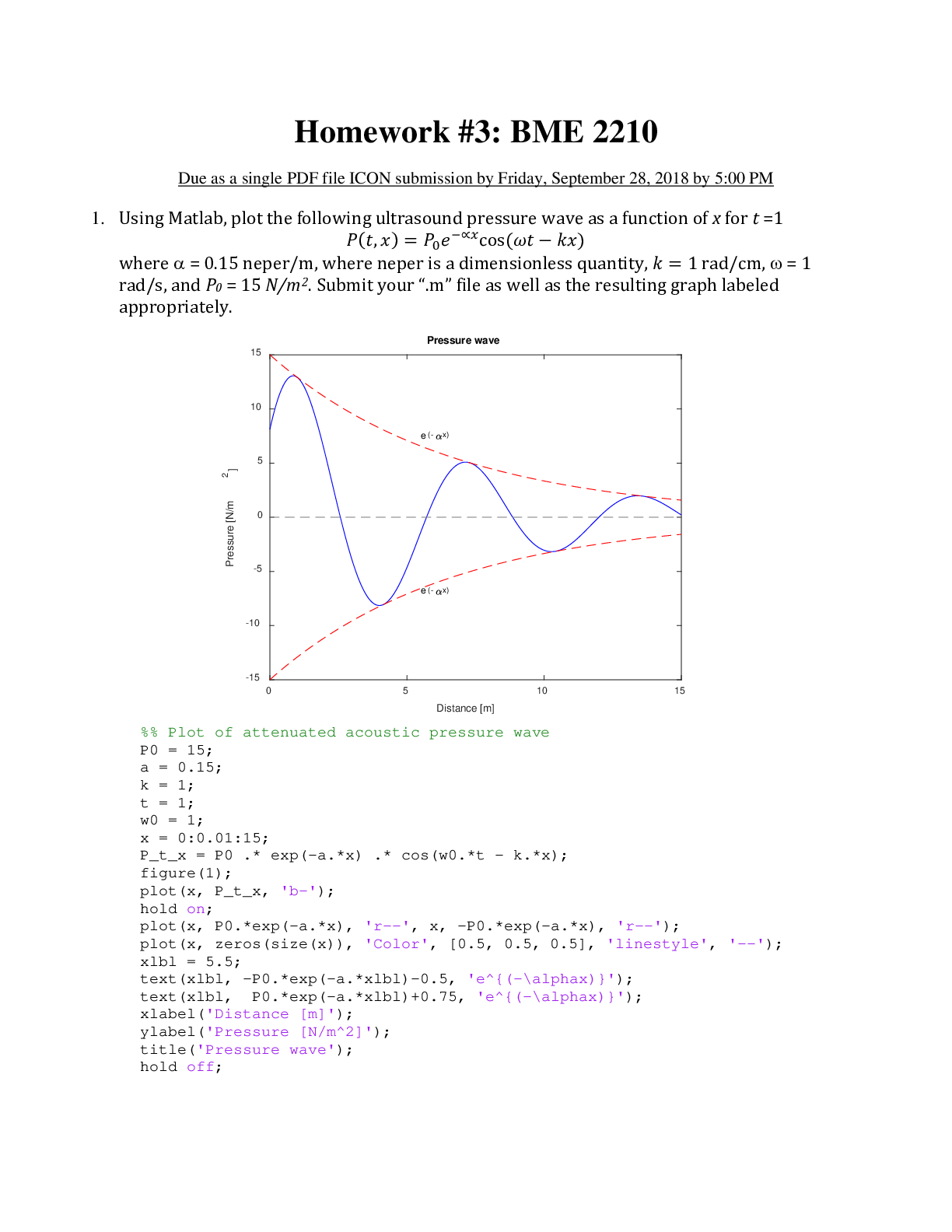
PATHO TEST 1. QUESTIONS AND ANSWERS. CHAPTER 1 – 30/GRADE A Ch. 1 1. When a second message is necessary for extracellular communication to be activated, it is provided by which one? 2. The role o... f cytokines in cell reproduction is that they: 3. Active transport occurs across which type of membranes? 4. Potassium and sodium are transported across plasma membranes by: 5. What is the sequence of steps in the development of a digestive enzyme by the pancreas cells from the initial transcription to the release from the cell? 6. All cells are capable of what process? • 7. Which mode of chemical signaling uses blood to transport communication to cells some distance away? 8. Which statements are true concerning the process of facilitated diffusion? (Select all that apply). • . 9. What are the major chemical components of the cell membranes? (Select all that apply.) 10. Which structure prevents water-soluble molecules from entering cells across the plasma membrane? Ch. 2 1. The abnormal proliferation of cells in response to excessive hormonal stimulation is called: 2. Hemoprotein accumulations are a result of the excessive storage of: 3. Which organs are affected by lead consumption? (Select all that apply.) 4. The mammary glands enlarge during pregnancy primarily as a consequence of hormonal: • 5. Dysplasia refers to a(n): • 6. What is an example of compensatory hyperplasia? • Hepatic cells increase cell division after part of the liver is excised. 7. Examples of adaptive cellular responses include: (Select all that apply.) • 8. What physiologic change occurs during heat exhaustion? • . 9. Which type of cell adaptation occurs when normal columnar ciliated epithelial cells of the bronchial lining have been replaced by stratified squamous epithelial cells? 10. Lead causes damage within the cell by interfering with the action of: 11. Free radicals cause cell damage by: 12. What effect does fetal alcohol syndrome have on newborns? (Select all that apply.) 13. Carbon monoxide causes tissue damage by: 14. Which statement is true regarding the difference between subdural hematoma and epidural hematoma? 15. Which statements are true regarding the effects of marijuana use? (Select all that apply.) 16. Which statement is a description of the characteristics of apoptosis? 17. What is the single most common cause of cellular injury? 18. What is a consequence of leakage of lysosomal enzymes during chemical injury? • . 19. Hemosiderosis is a condition that results in the excess of what substance being stored as hemosiderin in cells of many organs and tissues? 20. What organs are affected by the type of necrosis that results from either severe ischemia or chemical injury? (Select all that apply.) 21. What is the most common site of lipid accumulation? • 22. What is a consequence of plasma membrane damage to the mitochondria? • Influx of calcium ions halts ATP production. 23. In hypoxic injury, sodium enters the cell and causes swelling because: • ATP is insufficient to maintain the pump that keeps sodium out of the cell. 24. Which is an effect of ionizing radiation exposure? • DNA aberrations 25. What type of necrosis is associated with wet gangrene? • Liquefactive 26. What type of necrosis results from ischemia of neurons and glial cells? • Liquefactive 27. It is true that nondividing cells are: • Affected by only hypertrophy 28. Current research has determined that chemical-induced cellular injury: • Is often the result of the damage caused by reactive free radicals. 29. What type of necrosis is often associated with pulmonary tuberculosis? • Caseous 30. Acute alcoholism mainly affects which body system? • Central nervous 31. After ovulation, the uterine endometrial cells divide under the influence of estrogen. This process is an example of hormonal: • Hyperplasia 32. What two types of hearing loss are associated with noise? • Acoustic trauma and noise-induced 33. During cell injury caused by hypoxia, sodium and water move into the cell because: • The pump that transports sodium out of the cell cannot function because of a decrease in ATP levels. 34. What mechanisms occur in the liver cells as a result of lipid accumulation? • Increased synthesis of triglycerides from fatty acids and decreased synthesis of apoproteins 35. Removal of part of the liver leads to the remaining liver cells undergoing compensatory: • Hyperplasia 36. What is the cause of free calcium in the cytosol that damages cell membranes by uncontrolled enzyme activation? • Depletion of ATP normally pumps calcium from the cell. 37. Current research supports the believe that, after heart muscle injury, the damage: • Is repaired by newly matured cardiomyocytes. 38. Lead poisoning affects the nervous system by: • Interfering with the function of neurotransmitters 39. During cell injury caused by hypoxia, an increase in the osmotic pressure occurs within the cell because: • Sodium chloride enters the cell. 40. The loss of the adenosine triphosphate (ATP) during ischemia causes cells to: • Swell because of the influx of sodium chloride (NaCl). 41. It is true that melanin is: (Select all that apply.) • Found in cells called keratinocytes, which are present in the retina • A factor in the prevention of certain types of cancer • Accumulated in specific cells found in the skin 42. Blunt force injuries would include a: (Select all that apply.) • Bruise to the upper arm, resulting from a fall • Simple tibia fracture sustained in a skiing accident • Spleen laceration caused by a punch during a physical fight 43. Free radicals play a major role in the initiation and progression of which diseases? • Cardiovascular diseases such as hypertension and ischemic heart disease 44. In decompression sickness, emboli are formed by bubbles of: • Nitrogen Ch. 3 1. Chvostek and Trousseau signs indicate which electrolyte imbalance? • Hypocalcemia 2. Thirst activates osmoreceptors by an increase in which blood plasma? • Osmotic pressure 3. A patient’s blood gases reveal the following findings: pH, 7.3; bicarbonate (HCO3) 27 mEq/L; carbon dioxide (CO2), 58 mm Hg. What is the interpretation of these gases? • Respiratory acidosis 4. During acidosis, the body compensates for the increase in serum hydrogen ions by shifting hydrogen ions into the cell in exchange for which electrolyte? • Potassium 5. The pathophysiologic process of edema is related to which mechanism? • Lymphatic obstruction 6. Causes of hyperkalemia include: • Renal failure and Addison disease 7. In addition to osmosis, what force is involved in the movement of water between the plasma and interstitial fluid spaces? • Hydrostatic pressure 8. In hyperkalemia, what change occurs to the cells’ resting membrane potential? • Hypopolarization 9. Water movement between the intracellular fluid (ICF) compartment and the extracellular fluid (ECF) compartment is primarily a function of: • Osmotic forces 10. Which arterial pH will initiate the formation of ammonium (NH4) from ammonia (NH3), referred to as academia, in the tubular lumen of the kidney? • 7.25 11. The most common cause of hypermagnesemia is: • Renal failure 12. Obesity creates a greater risk for dehydration in people because: • Adipose cells contain little water because fat is water repelling. 13. A major determinant of the resting membrane potential necessary for the transmission of nerve impulses is the ratio between: • Intracellular and extracellular Na+ 14. Secretion of antidiuretic hormone (ADH) and the perception of thirst are stimulated by a(n): • Increase in plasma osmolality 15. Low plasma albumin causes edema as a result of a reduction in which pressure? • Plasma oncotic 16. Venous obstruction is a cause of edema because of an increase in which pressure? • Capillary hydrostatic 17. It is true that Kussmaul respirations indicate: • A compensatory measure is needed to correct metabolic acidosis. 18. Infants are most susceptible to significant losses in total body water because of an infant’s: • Kidneys are not mature enough to counter fluid losses 19. Vomiting-induced metabolic alkalosis, resulting in the loss of chloride, causes: • Retention of bicarbonate to maintain the anion balance 20. At the arterial end of capillaries, fluid moves from the intravascular space into the interstitial space because the: • Capillary hydrostatic pressure is higher than the capillary oncotic pressure. 21. Insulin is used to treat hyperkalemia because it: • Transports potassium from the blood to the cell along with glucose. 22. Increased capillary hydrostatic pressure results in edema because of: • Sodium and water retention 23. What causes the clinical manifestations of confusion, convulsions, cerebral hemorrhage, and coma in hypernatremia? • High sodium in the blood vessels pulls water out of the brain cells into the blood vessels, causing brain cells to shrink. 24. It is true that when insulin is administered: • The liver increases its potassium levels. 25. The calcium and phosphate balance is influenced by which three substances? • Parathyroid hormone, calcitonin, and vitamin D 26. Which enzyme is secreted by the juxtaglomerular cells of the kidney when circulating blood volume is reduced? • Renin 27. The existence of hyperkalemia is likely to result in which changes to a person’s electrocardiogram (ECG)? • Peaked T waves 28. When changes in total body water are accompanied by proportional changes in electrolytes, what type of alteration occurs? • Isotonic 29. What mechanism can cause hypernatremia? • Hypersecretion of aldosterone 30. Physiologic pH is maintained at approximately 7.4 because bicarbonate (HCO3) and carbonic acid (H2CO3) exist in a ratio of: • 20:1 31. An excessive use of magnesium-containing antacids and aluminum-containing antacids can result in: • Hypophosphatemia 32. It is true that natriuretic peptides: • Decrease blood pressure and increase sodium and water excretion. 33. Two thirds of the body’s water is found in its: • Intracellular fluid compartments Ch. 4 1. The most clinically useful technique for prenatal diagnosis of chromosomal abnormalities at 3 months’ (12 weeks’) gestation is: • Chorionic villus sampling 2. What is the risk for the recurrence of autosomal dominant diseases? • 50% 3. DNA replication requires the enzyme DNA polymerase to: • Travel along the single DNA strand, adding the correct nucleotide to the new strand 4. Which is an important criterion for discerning autosomal recessive inheritance? • Consanguinity is sometimes present. 5. Cystic fibrosis is caused by what type of gene? • Autosomal recessive 6. A person with 47, XXY karyotype has the genetic disorder resulting in which syndrome? • Klinefelter 7. Males are more often affected by which type of genetic disease? • Sex-linked recessive 8. The purpose of a staining technique of chromosomes such as Giemsa is to: • Allow for the numbering of chromosomes and the identification of variations. 9. Which statement is true regarding X-linked recessive conditions? • These conditions are passed from affected father to all of his female children. 10. Transcription is best defined as a process by which: • RNA is synthesized from a DNA template. 11. The term for an error in which homologous chromosomes fail to separate during meiosis or mitosis is: • Aneuploidy 12. Which clinical manifestations would be expected for a child who has complete trisomy of the twenty-first chromosome? • An IQ of 25 to 70, low nasal bridge, protruding tongue, and flat, low-set ears 13. DNA formation occurs in which of the cell’s structures? • Nucleus 14. What syndrome, characterized by an absent homologous X chromosome with only a single X chromosome, exhibits features that include a short stature, widely spaced nipples, and webbed neck? • Turner 15. A child with which genetic disorder has a characteristic cry? • Cri du chat 16. Which genetic disease has been linked to a mutation of the tumor-suppressor gene? • Retinoblastoma 17. What is the most common cause of Down syndrome? • Maternal nondisjunction 18. An individual’s genetic makeup is referred to as his or her: • Genotype 19. What is the blood type of a person who is heterozygous, having A and B alleles as codominant? • AB 20. People diagnosed with neurofibromatosis have varying degrees of the condition because of the genetic principle of: • Expressivity 21. An amniocentesis is recommended for pregnant women who: • Have a family history of genetic disorders 22. The presence of a zygote having one chromosome with the normal complement of genes and one with a missing gene is characteristic of which genetic disorder? • Cri du chat 23. A couple has two children diagnosed with an autosomal dominant genetic disease. What is the probability that the next child will have the same genetic disease? • One half 24. When a child inherits a disease that is autosomal recessive, it is inherited from: • Both parents 25. What is the chromosomal variation that causes Klinefelter syndrome? • Nondisjunction of X chromosome in the mother 26. An amniocentesis indicates a neural tube defect when an increase in which protein is evident? • Alpha fetoprotein 27. Inserting bone marrow cells into an individual who produces abnormal erythrocytes is an example of what type of therapy? • Somatic cell 28. Consanguinity refers to the mating of persons: • Having common family relations 29. An X-linked recessive disease can skip generations because: • The disease can be transmitted through female carriers. 30. What is the second most commonly recognized genetic cause of mental retardation? • Fragile X syndrome 31. Males, having only one X chromosome (as is expected), are said to be: • Hemizygous Ch 5. 1. Regarding type 2 diabetes, obesity is considered to be what type of risk? a. Modifiable 2. When a woman has one first-degree relative with breast cancer, her risk of developing breast cancer is how many times greater? a. 2 3. The BRCA1 and BRCA2 mutations increase the risk of which cancer in women? a. Ovarian 4. A major characteristic of type 1 diabetes mellitus is that there is: a. An autoimmune cause factor 5. Blood pressure variations are associated with: a. The renin-angiotensin system’s effect on vasoconstriction 6. Which risk factor for hypertension is influenced by genetic factors and lifestyle? a. Obesity 7. The number of new cases of a disease reported during a specific period divided by the number of individuals in the population is defined as which characteristic of a disease? a. Incidence rate 8. The two most important risk factors for type 2 diabetes are: a. Obesity and positive family history 9. Studies have identified several genes that play a role in the prevention of obesity by affecting what? a. Regulation of appetite 10. It is currently believed that the risk for developing Alzheimer disease: a. Doubles among those with an affected first-degree relative. 11. Which type of cancer is said to aggregate among families? a. Breast 12. The data reporting that sickle cell disease affects approximately 1 in 600 American blacks is an example of which concept? a. Prevalence 13. What percentage of all cases of breast cancer are identified as an autosomal dominant form? a. 5 14. The number of persons living with a specific disease at a specific point in time is referred to by which term? a. Prevalence 15. Which dietary lifestyle choice has been associated with a decreased risk for developing colon cancer? a. Decreased consumption of foods high in fat 16. The ratio of the disease among the exposed population to the disease rate in an unexposed population is referred to as what type of risk? a. Relative 17. Adoption studies have shown that the offspring of an alcoholic parent when raised by nonalcoholic parents have what amount of an increased risk of developing alcoholism? a. Fourfold 18. Traits caused by the combined effects of multiple genes are referred to by which term? a. Polygenic 19. Obesity acts as an important risk factor for type 2 diabetes mellitus by: a. Increasing the resistance to insulin by cells 20. What is the cause of familial hypercholesterolemia (FH)? a. Reduction in the number of low-density lipoprotein (LDL) receptors on cell surfaces 21. Empirical risks for most multifactorial diseases are based on: a. Direct observation 22. Which disease form is identified on the basis of empirical risk observation? a. Multifactorial Ch. 6 1. A malfunction in DNA methylation can lead to: a. Cancer 2. Prader-Willi syndrome causes a chromosomal defect that is: a. Inherited from the father 3. When microRNA (miRNA) are methylated their messenger RNA (mRNA) targets are over- expressed, the resulting effect on existing cancer would be: a. Metastasis 4. Genes responsible for the maintenance of all cells are referred to as: a. Housekeeping 5. The shape of the face of a child diagnosed with Russell-Silver syndrome is likely to be: a. Triangular 6. Hypomethylation and the resulting effect on oncogenes result in a(an): a. Increase in tumor progression from benign to malignant 7. What is the belief regarding twins who adopt dramatically different lifestyles? a. They may experience very different aging processes. 8. Which statement is true regarding the embryonic development of stem cells? a. They are said to be pluripotent. 9. What genetic process is likely responsible for the occurrence of asthma in only one of a pair of identical twins? a. Epigenetic modifications 10. Which term refers to the silenced gene of a gene pair? a. Imprinted 11. The difference between DNA sequence mutations and epigenetic modifications is: a. Epigenetic modifications can be reversed. 12. When a chromosome lacking 4 Mb is inherited from the mother, the child is at risk for developing which syndrome? a. Angelman Ch. 7 1. Which chemical interacts among all plasma protein systems by degrading blood clots, activating complement, and activating the Hageman factor? • Plasmin 2. Activation of the classical pathway begins with: • Antigen-antibody complexes 3. The acute inflammatory response is characterized by fever that is produced by the hypothalamus being affected by: • Endogenous pyrogens 4. The chemotactic factor affects the inflammatory process by: • Directing leukocytes to the inflamed area 5. In the later stages of an inflammatory response, which phagocytic cell is predominant? • Monocytes 6. A keloid is the result of which dysfunctional wound healing response? • Collagen matrix assembly 7. During phagocytosis, what is occurring during the step referred to as opsonization? • Phagocytes recognize and adhere to the bacteria. 8. Which cell is the body’s primary defense against parasite invasion? • Eosinophil 9. What occurs during the process of repair after tissue damage? • Nonfunctioning scar tissue replaces destroyed tissue. 10. Which manifestation of inflammation is systemic? • Fever and leukocytosis 11. When considering white blood cell differentials, acute inflammatory reactions are related to elevations of which leukocyte? • Neutrophils 12. In regulating vascular mediators released from mast cells, the role of eosinophils is to release: • Histaminase, which limits the effects of histamine during acute inflammation 13. Which bacterium grows in the intestines after prolonged antibiotic therapy? • Clostridium difficile 14. Which cytokine is produced and released from virally infected host cells? • IFN-a 15. Newborns often have deficiencies in collectin-like proteins, making them more susceptible to what type of infection? • Respiratory 16. Which solution is best to use when cleaning a wound that is healing by epithelialization? • Normal saline 17. Many neonates have a transient depressed inflammatory response as a result of which condition? • Complement and chemotaxis are deficient. 18. What is the inflammatory effect of nitric oxide (NO)? • Decreases mast cell function, and decreases platelet aggregation. 19. The function of opsonization related to the complement cascade is to: • Tag of pathogenic microorganisms for destruction by neutrophils and macrophages. 20. Which secretion is a first line of defense against pathogen invasion that involves antibacterial and antifungal fatty acids, as well as lactic acid? • Sebaceous gland sebum 21. Which component of the plasma protein system tags pathogenic microorganisms for destruction by neutrophils and macrophages? • Complement cascade 22. When cellular damage occurs and regeneration is minor with no significant complications, the process of returning the cells to preinjury function is referred to as: • Resolution 23. What process causes heat and redness to occur during the inflammatory process? • Vasodilation of blood vessels 24. What is the role of a natural killer (NK) cells? • Elimination of malignant cells 25. The role of fibroblasts during the reconstructive phase of wound healing is to: • Synthesize and secrete collagen and the connective tissue proteins. 26. Frequently when H1 and H2 receptors are located on the same cells, they act in what fashion? • Antagonistically 27. Which chemical mediator derived from mast cells retracts endothelial cells to increase vascular permeability and to cause leukocyte adhesion to endothelial cells? • Leukotrienes 28. What causes the edema that occurs during the inflammatory process? • Increased capillary permeability 29. What is an outcome of the complement cascade? • Lysis of bacterial cell membranes 30. What is the vascular effect of histamine released from mast cells? • Vasodilation 31. What is the correct sequence in phagocytosis? • Recognition, engulfment, fusion, destruction 32. What affect does the process of histamine binding to the histamine-2 (H2) receptor have on inflammation? • Inhibition 33. IFN-a is secreted from which cells? • Macrophages 34. Fusion is the step in phagocytosis during which: • Lysosomal granules enter the phagocyte. 35. Which action is a purpose of the inflammatory process? • To prevent infection of the injured tissue 36. How do surfactant proteins A through D provide innate resistance? • Secrete mucus. 37. In the coagulation (clotting) cascade, the intrinsic and the extrinsic pathways converge at which factor? • X 38. Some older adults have impaired inflammation and wound healing because of which problem? • Underlying chronic illness(es) exists. 39. What plasma protein system forms a fibrinous meshwork at an inflamed site? • Coagulation 40. During the process of endocytosis, the phagosome step results in: • An intracellular phagocytic vacuole is formed. Ch. 8 1. Increased age may cause which change in lymphocyte function? • Increased production of antibodies against self-antigens 2. The generation of clonal diversity includes a process that: • Takes place in the primary (central) lymphoid organs. 3. Which antibody initially indicates a typical primary immune response? • IgM 4. The generation of clonal diversity occurs primarily during which phase of life? • Fetal 5. Which T cell controls or limits the immune response to protect the host’s own tissues against an autoimmune response? • Regulatory T (Treg) cells 6. How does the aging process of the T-cell activity affect older adults? • Tendency to develop various infections 7. Cytokines are vital to a cell’s ability to do which function? • Communicate 8. Th2 cells produce IL-4 and suppress which cells? • Th1 cells 9. Which cytokine is needed for the maturation of a functional helper T cell? • IL-2 10. Evaluation of umbilical cord blood can confirm that which immunoglobulin level is near adult levels? • IgG 11. How do antibodies protect the host from bacterial toxins? • Binding to the toxins to neutralize their biologic effects 12. Vaccinations are able to provide protection against certain microorganisms because of the: • Level of protection provided by IgG 13. Which cell has a role in developing cell-mediated immunity? • Th1 14. Which type of immunity is produced by an individual after either natural exposure to the antigen or after immunization against the antigen? • Active-acquired immunity 15. Which statement is believed to be true concerning Th1 cells? • They are induced by antigens derived from cancer cells. 16. Antibodies that are associated with mucosal immune system, such as immunoglobulins, function to prevent which type of infections? • Infections that focus on epithelial surfaces of the body 17. Which characteristic is the most important determinant of immunogenicity when considering the antigen? • Foreignness 18. The B-cell receptor (BCR) complex functions uniquely by: • Communicating information about the antigen to the cell nucleus 19. What type of immunity is produced when an immunoglobulin crosses the placenta? • Passive-acquired immunity 20. Which cell has the ability to recognize antigens presented by the MHC class I molecules? • CD 8 21. An individual is more susceptible to infections of mucous membranes when he or she has a seriously low level of which immunoglobulin antibody? • IgA 22. The portion of the antigen that is configured for recognition and binding is referred to as what type of determinant? • Epitope 23. Which statement is true concerning clonal selection? • This theory involves antigens that select those lymphocytes with compatible receptors. 24. When antigens are administered to produce immunity, why are different routes of administration considered? • Each route stimulates a different lymphocyte-containing tissue, resulting in different types of cellular and humoral immunity. 25. Which primary characteristic is unique for the immune response? • The immune response is specific to the antigen that initiates it. 26. Why is the herpes virus inaccessible to antibodies after the initial infection? • The virus does not circulate in the blood. 27. Which immunoglobulin is present in blood, saliva, breast milk, and respiratory secretions? • IgA 28. What is the term for the process during which lymphoid stem cells migrate and change into either immunocompetent T cells or immunocompetent B cells? • Clonal diversity 29. When a person is exposed to most antigens, antibodies can be usually detected in his or her circulation within: • 6 days 30. Where are antibodies produced? • Plasma cells 31. Which statement is true regarding maternal antibodies provided to the neonate? • The antibodies enter into the fetal circulation by means of active transport. 32. The functions of the major histocompatibility complex (MHC) and CD1 molecules are alike because both: • Are antigen-presenting molecules. 33. Which statement is believed to be true concerning Th2 cells? • Th2 cells are induced by antigens derived from allergens. 34. Which statement is true concerning the IgM? • IgM is the first antibody produced during the initial response to an antigen. 35. Which is an example of an endogenous antigen? • Cancer cells 36. In which structure does B lymphocytes mature and undergo changes that commit them to becoming B cells? • Bone marrow Ch. 9 1. During an IgE-mediated hypersensitivity reaction, the degranulation of mast cells is a result of which receptor action? • Histamine bound to H2 2. Graves disease is an autoimmune disease that results in which maternal antibody? • Affecting the receptor for TSH, causing neonatal hyperthyroidism 3. Deficiencies in which element can produce depression of both B- and T-cell function? • Zinc 4. During an IgE-mediated hypersensitivity reaction, what causes bronchospasm? • Smooth muscle contraction caused by histamine bound to H1 receptors 5. During an IgE-mediated hypersensitivity reaction, which leukocyte is activated? • Eosinophils 6. What characteristic do atopic individuals have that make them genetically predisposed to develop allergies? • Greater quantities of IgE 7. A hypersensitivity reaction that produces an allergic response is called: • Anaphylaxis 8. When the maternal immune system becomes sensitized against antigens expressed by the fetus, what reaction occurs? • Alloimmunity 9. Graves disease is a result of: • Autoantibodies binding to thyroid-stimulating hormone (TSH)-receptor sites 10. Which statement is true concerning an atopic individual? • They tend to produce more Fc receptors. 11. Which statement is true regarding immunodeficiency? • Immunodeficiency is generally not present in other family members. 12. Graves disease (hyperthyroidism) is an example of which type II hypersensitivity reaction? • Modulation 13. Which type of antibody is involved in type I hypersensitivity reaction? • IgE 14. Tissue damage caused by the deposition of circulating immune complexes containing an antibody against the host DNA is the cause of which disease? • Systemic lupus erythematosus 15. Hypersensitivity is best defined as a(an): • Altered immunologic response to an antigen that results in disease 16. Which component of the immune system is deficient in individuals with infections caused by viruses, fungi, or yeast? • T cells 17. How many months does it take for the newborn to be sufficiently protected by antibodies produced by its own B cells? • 6 to 8 18. Immunoglobulin E (IgE) is associated with which type of hypersensitivity reaction? • I 19. Urticaria are a manifestation of a which type of hypersensitivity reaction? • I 20. Type III hypersensitivity reactions are a result of which of the following? • Antibodies binding to soluble antigens that were released into body fluids and the immune complexes being deposited in the tissues 21. How are target cells destroyed in a type II hypersensitivity reaction? • Natural killer cells 22. When soluble antigens from infectious agents enter circulation, tissue damage is a result of: • Neutrophil granules and toxic oxygen products 23. What is the mechanism that results in type II hypersensitivity reactions? • Antibodies bind to the antigens on the cell surface. 24. Blood transfusion reactions are an example of: • Alloimmunity 25. In a type III hypersensitivity reaction, the harmful effects after the immune complexes that are deposited in tissues are a result of: • Complement activation 26. In which primary immune deficiency is there a partial-to-complete absence of T-cell immunity? • DiGeorge syndrome 27. Why does tissue damage occurs in acute rejection after organ transplantation? • Th1 cells release cytokines that activate infiltrating macrophages, and cytotoxic T cells directly attack the endothelial cells of the transplanted tissue. 28. Considering the effects of nutritional deficiencies on the immune system, severe deficits in calories and protein lead to deficiencies in the formation of which immune cells? • T cells 29. A type IV hypersensitivity reaction causes which result? • Lymphokine-producing Th1 cells directly attacking and destroying cellular targets 30. When mismatched blood is administered causing an ABO incompatibility, the erythrocytes are destroyed by: • Complement-mediated cell lysis 31. Which class of immunoglobulins forms isohemagglutinins? • IgM 32. A person with type O blood is considered to be the universal blood donor because type O blood contains which of the following? • No antigens 33. Raynaud phenomenon is classified as a type III hypersensitivity reaction and is due to: • Immune complexes that are deposited in capillary beds, blocking circulation 34. The common hay fever allergy is expressed through a reaction that is mediated by which class of immunoglobulins? • IgE 35. When antibodies are formed against red blood cell antigens of the Rh system, the blood cells are destroyed by: • Phagocytosis in the spleen 36. Which blood cell carries the carbohydrate antigens for blood type? • Erythrocytes 37. A person with type O blood is likely to have high titers of which anti-antibodies? • A and B 38. Raynaud phenomenon is an example of which type of hypersensitivity? • III Ch. 10 1. The ability of the pathogen to invade and multiply in the host is referred to as: • Infectivity 2. Which statement concerning exotoxins is true? • Exotoxins are released during bacterial growth. 3. After sexual transmission of HIV, a person can be infected yet seronegative for how many months? • 6 to 14 4. What is the final stage of the infectious process? • Spread 5. Considering the hypothalamus, a fever is produced by: • Endogenous pyrogens acting directly on the hypothalamus. 6. What area in the body may act as a reservoir in which HIV can be relatively protected from antiviral drugs? • Central nervous system 7. Some bacterial surface proteins bind with the crystalline fragment (Fc) portion of an antibody to: • Produce a protective “self” protein 8. Which type of microorganism reproduces on the skin? • Bacteria and fungi 9. Once they have penetrated the first line of defense, which microorganisms do natural killer (NK) cells actively attack? • Viruses 10. Phagocytosis involves neutrophils actively attacking, engulfing, and destroying which microorganisms? • Bacteria 11. What is the role of reverse transcriptase in HIV infection? • It converts RNA into double-stranded DNA. 12. Which statement about vaccines is true? • Vaccines require booster injections to maintain life-long protection. 13. AIDS produces a striking decrease in the number of which cells? • CD4+ Th cells 14. Vaccines against viruses are created from: • Live organisms weakened to produce antigens 15. Toxigenicity is defined as the: • Pathogen’s ability to produce disease by the production of a soluble toxin 16. Which cells are primary targets for HIV? • CD4+ Th cells, macrophages, and natural killer cells 17. HIV antibodies appear within how many weeks after infection through blood products? • 4 to 7 18. Which statement is a characteristic of HIV? • HIV is a retrovirus. 19. Which disease is an example of a rickettsial infection? • Rocky Mountain spotted fever 20. What is a significant cause of morbidity and mortality worldwide? • Infectious disease 21. Which statement is true concerning a fungal infection? • Phagocytes and T lymphocytes control fungal infections. 22. Cytokines are thought to cause fevers by stimulating the synthesis of which chemical mediator? • Prostaglandin 23. What is the first stage in the infectious process? • Colonization 24. Which organism is a common sexually transmitted bacterial infection? • Treponema pallidum Ch. 11 1. The action of which hormone helps explain increases in affective anxiety and eating disorders, mood cycles, and vulnerability to autoimmune and inflammatory diseases in women as a result of stimulation of the CRH gene promoter and central norepinephrine system? • Estrogen 2. What effect does estrogen have on lymphocytes? • Depression of T-cell functions and enhancement of B-cell functions 3. Which hormone prompts increased anxiety, vigilance, and arousal during a stress response? • Norepinephrine 4. Diagnostic blood work on individuals who perceive themselves to be in a chronic stress state will likely demonstrate: • Decreased Tc cells 5. What effect do androgens have on lymphocytes? • Suppression of B- and T-cell responses 6. During a stress response, the helper T (Th) 1 response is suppress by which hormone? • Cortisol 7. Stress-age syndrome directly results in depressed function of which system? • Immune 8. Exhaustion occurs if stress continues when which stage of the general adaptation syndrome is not successful? • Adaptation 9. Perceived stress elicits an emotional, anticipatory response that begins where? • Limbic system 10. Which organ is stimulated during the alarm phase of the general adaptation syndrome (GAS)? • Hypothalamus 11. What is the effect that low-serum albumin has on the central stress response? • Impaired circulation of epinephrine and norepinephrine 12. Released stress-induced cortisol results in the stimulation of gluconeogenesis by affecting which structure? • Adrenal cortex 13. Which statement is true concerning the differences between stress-induced hormonal alterations of men and women? • Androgens appear to induce a greater degree of immune cell apoptosis after injury, creating greater immunosuppression in injured men than in injured women. 14. Which cytokines initiate the production of corticotropin-releasing hormone (CRH)? • IL–1 and IL-6 15. Which gland regulates the immune response and mediates the apparent effects of circadian rhythms on immunity? • Pineal 16. Stress-induced norepinephrine results in: • Peripheral vasoconstriction 17. A reduction is an individual’s number of natural killer (NK) cells appears to correlate with an increased risk for the development of: • Depression 18. A nurse is providing care to a terminally ill adult who has been with his life partner for over 56 years. Research supports the nurse’s assessment of the life partner for signs of: • Severe stress reaction 19. What are the signs that a patient is in the adaptive stage of the general adaptation syndrome? • The patient perceives his or her only options are to run away or fight back. 20. The most influential factor in whether a person will experience a stress reaction is his or her: • Ability to cope 21. Which hormone increases the formation of glucose from amino acids and free fatty acids? • Cortisol 22. The release of which cytokines is triggered by bacterial or viral infections, cancer, and tissue injury that, in turn, initiate a stress response? • IFN, TNF-ß, and IL-6 23. What is the effect of increased secretions of epinephrine, glucagon, and growth hormone? • Hyperglycemia 24. During an anticipatory response to stress, the reaction from the limbic system is stimulated by the: • Paraventricular nucleus of the hypothalamus 25. Stress-induced sympathetic stimulation of the adrenal medulla causes the secretion of: • Epinephrine and norepinephrine Ch. 12 1. Which gastrointestinal tract condition can be an outcome of both chemotherapy and radiation therapy? • Stomatitis 2. In a normal, nonmutant state, an oncogene is referred to as a: • Proto-oncogene 3. It has been determined that a tumor is in stage 2. What is the meaning of this finding? • Cancer is locally invasive. 4. Which cancer originates from connective tissue? • Osteogenic sarcoma 5. What is the role of vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (bFGF) in cell metastasis? • To develop new blood vessels to feed cancer cells 6. Autocrine stimulation is the ability of cancer cells to: • Secrete growth factors that stimulate their own growth. 7. Chronic inflammation causes cancer by: • Releasing compounds such as reactive oxygen species that promote mutations 8. How do cancer cells use the enzyme telomerase? • To switch on the telomerase to enable cells to divide indefinitely 9. What aberrant change causes the abnormal growth in retinoblastoma? • The tumor-suppressor gene is turned off. 10. Carcinoma refers to abnormal cell proliferation originating from which tissue origin? • Epithelial cells 11. Which statement is true regarding pain and cancer? • Pain is generally associated with late-stage cancer. 12. What are characteristics of benign tumors? • Benign tumors include the suffix -oma. 13. What is the role of caretaker genes? • Maintenance of genomic integrity 14. What are tumor cell markers? • Hormones, enzymes, antigens, and antibodies that are produced by cancer cells 15. Which terms represent the correct nomenclature for benign and malignant tumors of adipose tissue, respectively? • Lipoma, liposarcoma 16. What is the cause of anemia in a patient diagnosed with pancreatic cancer? • Malabsorption of iron 17. Burkitt lymphomas designate a chromosome that has a piece of chromosome 8 fused to a piece of chromosome 14. This is an example of which mutation of normal genes to oncogenes? • Chromosome translocation 18. Which statement is true regarding pleomorphic cells? • They are a result of anaplasia. 19. The survival rate for stage IV Hodgkin disease can be as high as: • 70% 20. What is the major virus involved in the development of cervical cancer? • Human papillomavirus 21. The ras gene converts from a proto-oncogene to an oncogene by: • Altering one or more nucleotide base pairs 22. Which cancer may be treated with radiation delivered by brachytherapy? • Cervical 23. What is the most commonly reported symptom of cancer treatment? • Fatigue 24. Which term is used to describe a muscle cell showing a reduced ability to form new muscle while appearing highly disorganized? • Anaplasia 25. Two “hits” are required to inactivate tumor-suppressor genes because: • Each allele must be altered, and each person has two copies, or alleles, of each gene, one from each parent. 26. Which statement supports the hypothesis that intestinal polyps are benign neoplasms and the first stage in the development of colon cancer? • An accumulation of mutations in specific genes is required for the development of cancer. 27. Many cancers create a mutation of ras. ras is a(an): • Intracellular-signaling protein that regulates cell growth 28. The function of the tumor cell marker is to: • Screen individuals at high risk for cancer. 29. What is the skin-related health risk induced by some types of chemotherapy? • Infection 30. In childhood neuroblastoma, the N-myc oncogene undergoes which type of mutation of normal gene to oncogene? • Gene amplification 31. What is the consequence for cells when the functioning TP53 gene is lost as a result of mutation? • Cells escape apoptosis. 32. Apoptosis is a(an): • Normal mechanism for cells to self-destruct when growth is excessive 33. Which cancers are all associated with chronic inflammation? • Colon, thyroid gland, and urinary bladder 34. The Papanicolaou (Pap) test is used to screen for which cancer? • Cervical 35. By what process do cancer cells multiply in the absence of external growth signals? • Autocrine stimulation 36. The most common site of metastasis for a patient diagnosed with prostate cancer is which location? • Bones 37. Which statement concerning benign tumors is true? • The cells are well-differentiated. 38. Carcinoma in situ is characterized by which changes? • Cells remain localized in the glandular or squamous cells. 39. Inherited mutations that predispose to cancer are almost invariably what kind of gene? • Tumor-suppressor genes 40. Oncogenes are genes that are capable of: • Directing synthesis of proteins to regulate growth and to provide necessary replacement of tissue Ch. 27 1. The drug heparin acts in hemostasis by which processes? • Inhibiting thrombin and antithrombin III (AT-III) 2. Where are Kupffer cells located? • Liver 3. Blood cells that differentiate into macrophages are known as: • Monocytes 4. Which of the following is the role of nitric oxide (NO) in hemostasis? • Controls platelet activation through cyclic adenosine monophosphate (cAMP)–mediated signaling. 5. Which hemoglobin is made from oxidized ferric iron (Fe3+) and lacks the ability to bind oxygen? • Methemoglobin 6. Granulocytes that contain granules of vasoactive amines, such as histamine, are called: • Basophils 7. What is the life span of an erythrocyte (in days)? • 100 to 120 8. Which nutrients are necessary for hemoglobin synthesis? • Iron and vitamin B6 (pyridoxine) 9. What is the function of erythrocytes? • Tissue oxygenation 10. Without prior exposure to an antigen, which cells are able to destroy some types of tumor cells and some virus-infected cells? • Natural killer (NK) cells 11. Where are alveolar macrophages found? • Lungs 12. Which form of iron (Fe) can be used in the formation of normal hemoglobin? • Fe2+ 13. Which substance is used to correct the chronic anemia associated with chronic renal failure? • Erythropoietin 14. Fetal hematopoiesis occurs in which structure? • Spleen 15. What is the most abundant class of plasma protein? • Albumin 16. What is plasmin’s role in the clotting process? • Degrades the fibrin within blood clots. 17. What is the life span of platelets (in days)? • 10 18. What is the consequence of a splenectomy? • The number of defective cells in circulation increases. 19. The absence of parietal cells would prevent the absorption of an essential nutrient necessary to prevent which type of anemia? • Pernicious anemia 20. During an infection, why do lymph nodes enlarge and become tender? • B lymphocytes proliferate. 21. Recycling of iron from erythrocytes is made possible by which of the following? • Transferrin 22. What is the effect of low plasma albumin? • Osmotic pressure decreases, thus water moves from the capillaries to the interstitium. 23. Where are Langerhans cells found? • Skin 24. Which blood cells are the chief phagocytes involved in the early inflammation process? • Neutrophils 25. What changes to the hematologic system is related to age? • Lymphocyte function decreases. 26. What is the role of thromboxane A (TXA2) in the secretion stage of hemostasis? • Stimulates platelet aggregation. 27. Which of the following are formed elements of the blood that are not cells but are disk- shaped cytoplasmic fragments essential for blood clotting? • Platelets 28. What is the role of collagen in the clotting process? • Activates platelets. 29. Which nutrients are necessary for the synthesis of DNA and the maturation of erythrocytes? • Cobalamin (vitamin B12) and folate 30. What does polycythemia at birth indicate? • Hypoxia in utero 31. Which blood cells are biconcave in shape and have the capacity to be reversibly deformed? • Erythrocytes 32. By which structure are mature erythrocytes removed from the bloodstream? • Spleen 33. Which statement concerning erythrocytes is true? • Erythrocytes have the ability to change shape to squeeze through microcirculation. Ch. 28 1. The paresthesia that occurs in vitamin B12 deficiency anemia is a result of which of the following? • Myelin degeneration in the spinal cord 2. Considering iron replacement therapy prescribed for iron deficiency anemia, who is likely to require long-term daily maintenance dosage? • A woman who has not yet experienced menopause 3. The underlying disorder of which anemia is a result of the defective secretion of the intrinsic factor, which is essential for the absorption of vitamin B 12? • Pernicious 4. Which type of anemia is characterized by fatigue, weakness, and dyspnea, as well as conjunctiva of the eyes and brittle, concave nails? • Iron deficiency 5. What is the most common cause of iron deficiency anemia (IDA)? • Chronic blood loss 6. What is the treatment of choice for pernicious anemia (PA)? • Vitamin B12 by injection 7. Which statement best describes a Schilling test? • Administration of radioactive cobalamin and the measurement of its excretion in the urine to test for vitamin B12 deficiency 8. Which statement is true regarding the physical manifestations of vitamin B12 deficiency anemia? • Symptoms are a result of demyelination. 9. Considering sideroblastic anemia, what would be the expected effect on the plasma iron levels? • Plasma iron levels would be high. 10. What is the fundamental physiologic manifestation of anemia? • Hypoxia 11. Which anemia produces small, pale erythrocytes? • Iron deficiency 12. Which condition resulting from untreated pernicious anemia (PA) is fatal? • Heart failure 13. Treatment for polycythemia vera involves which of the following? • Therapeutic phlebotomy and radioactive phosphorus 14. Deficiencies in folate and vitamin B12 alter the synthesis of which of the following? • DNA 15. Continued therapy of pernicious anemia (PA) generally lasts how long? • The rest of one’s life 16. Clinical manifestations of mild-to-moderate splenomegaly and hepatomegaly, bronze-colored skin, and cardiac dysrhythmias are indicative of which anemia? • Sideroblastic 17. Which statement is true regarding warm autoimmune hemolytic anemia? • Erythrocytes are bound to macrophages and sequestered in the spleen. 18. An allogenic bone marrow transplantation remains the preferred method for treating which anemia? • Aplastic 19. When considering hemolytic anemia, which statement is true regarding the occurrence of jaundice? • Heme destruction exceeds the liver’s ability to conjugate and excrete bilirubin. 20. Which statement about folic acid is false? • Folic acid absorption is dependent on the enzyme folacin. 21. After a person has a subtotal gastrectomy for chronic gastritis, which type of anemia will result? • Iron deficiency 22. What term is used to describe the capacity of some erythrocytes to vary in size, especially in relationship to some anemias? • Anisocytosis 23. How is the effectiveness of vitamin B12 therapy measured? • Reticulocyte count 24. Sideroblastic anemia can occasionally result from an autosomal recessive transmission inherited from which relative? • Mother 25. What is the primary cause of the symptoms of polycythemia vera? • Increased blood viscosity 26. What causes the atrophy of gastric mucosal cells that result in pernicious anemia? • Vitamin B12 malabsorption 27. Which of the following describes how the body compensates for anemia? • Increasing rate and depth of breathing 28. In aplastic anemia (AA), pancytopenia develops as a result of which of the following? • Suppression of the bone marrow to produce adequate amounts of erythrocytes, leukocytes, and thrombocytes 29. Which of the following is classified as a megaloblastic anemia? • Pernicious 30. Erythrocyte life span of less than 120 days, ineffective bone marrow response to erythropoietin, and altered iron metabolism describe the pathophysiologic characteristics of which type of anemia? • Anemia of chronic disease 31. What is the most common pathophysiologic process that triggers aplastic anemia (AA)? • Autoimmune disease against hematopoiesis by activated cytotoxic T (Tc) cells Ch. 29 1. Which term is used to describe a red-purple discoloration caused by diffuse hemorrhage into the skin tissue? • Purpura 2. In disseminated intravascular coagulation (DIC), what activates the coagulation cascade? • Tissue factor (TF) located in the endothelial layer of blood vessels and subcutaneous tissue 3. What is the most common cause of vitamin K deficiency? • Total parenteral nutrition with antibiotic therapy 4. Vitamin _____ is required for normal clotting factor synthesis by the _. • K; liver 5. Hodgkin disease is characterized by the presence of which of the following? • Reed-Sternberg (RS) cells 6. Which disorder is described as an unregulated release of thrombin with subsequent fibrin formation and accelerated fibrinolysis? • Disseminated intravascular coagulation (DIC) 7. Which statement relates to immune thrombocytopenic purpura (ITP)? • Mononuclear phagocytes in the spleen remove antibody-coated platelets from circulation. 8. Which electrolyte imbalance accompanies multiple myeloma (MM)? • Hypercalcemia 9. Which of the following is characterized by what is referred to as pathognomonic pentad of symptoms? • Acute idiopathic thrombotic thrombocytopenic purpura 10. Reed-Sternberg (RS) cells represent malignant transformation and proliferation of which of the following? • B cells 11. Which statement best describes heparin-induced thrombocytopenia (HIT)? • Immunoglobulin G immune–mediated adverse drug reaction that reduces circulating platelets 12. Which proinflammatory cytokines are responsible for the development and maintenance of disseminated intravascular coagulation (DIC)? • Tumor necrosis factor-alpha (TNF-); IL-1, IL-6, and IL-8; and platelet-activating factor (PAF) 13. Which description is consistent with acute lymphocytic leukemia (ALL)? • ALL is a progressive neoplasm defined by the presence of greater than 30% lymphoblasts in the bone marrow or blood. 14. Which virus is associated with Burkitt lymphoma in African children? • Epstein-Barr virus 15. Local signs and symptoms of Hodgkin disease–related lymphadenopathy are a result of which of the following? • Pressure and obstruction 16. When the demand for mature neutrophils exceeds the supply, immature neutrophils are released indicating: • A shift to the left 17. Which description is consistent with chronic lymphocytic leukemia (CLL)? • B cells fail to mature into plasma cells that synthesize immunoglobulins. 18. What term is used to identify thrombi that occlude arterioles and capillaries and are made up of platelets with minimal fibrin and erythrocytes? • Thrombotic thrombocytopenic purpura (TTP) 19. Immune thrombocytopenia (ITP) is a(n) _____ condition in adults and a(n) condition in children. • Chronic; acute 20. What is the most reliable and specific test for diagnosing disseminated intravascular coagulation (DIC)? • D-dimer 21. In infectious mononucleosis (IM), what does the Monospot test detect? • Immunoglobulin M (IgM) 22. Which description is consistent with chronic myelogenous leukemia (CML)? • The translocation of genetic material from genes 9 and 22 creates an abnormal, fused protein identified as BCR-ABL1. 23. What change is observed in leukocytes during an allergic disorder (type I hypersensitivity) often caused by asthma, hay fever, and drug reactions? • Eosinophilia 24. In disseminated intravascular coagulation (DIC), what are the indications of microvascular thrombosis? • Symmetric cyanosis of fingers and toes Ch. 30 1. How does hemolytic disease of the newborn (HDN) cause acquired congenital hemolytic anemia? • HDN is an alloimmune disease in which the mother’s immune system produces antibodies against fetal erythrocytes, which are recognized as foreign and removed from circulation. 2. Fetuses who do not survive anemia in utero are usually stillborn with gross edema of the entire body. Which term is used to identify this condition? • Hydrops fetalis 3. Which vitamin improves the absorption of oral iron taken to treat iron deficiency anemia in children? • C 4. Hemophilia A is considered to be what type of inherited disorder? • X-linked recessive 5. What treatment prevents the development of kernicterus in an infant born with hemolytic disease of the newborn (HDN)? • Replacement transfusion of new Rh-positive blood that is not contaminated with anti-Rh antibodies 6. Which disease is an autosomal dominant inherited hemorrhagic disease? • von Willebrand disease 7. When does fetal erythrocyte production shift from the liver to the bone marrow? • Fifth month of gestation 8. Which hemophilia occurs equally in both men and women? • Hemophilia C 9. Hemolytic disease of the newborn (HDN) can occur if the mother: • Is Rh-negative and the fetus is Rh-positive 10. What is the most common cause of insufficient erythropoiesis in children? • Iron deficiency 11. Which disease is caused by clotting factor VIII deficiency and is an autosomal dominant trait? • von Willebrand disease 12. In a full-term infant, the normal erythrocyte life span is days, whereas the adult erythrocyte life span is days. • 60 to 80; 120 13. The alpha- and beta-thalassemias are considered what types of inherited disorder? • Autosomal recessive 14. An infant’s hemoglobin must fall below g/dl before signs of pallor, tachycardia, and systolic murmurs occur. • 5 15. When diagnosed with hemolytic disease of the newborn (HDN), why does the newborn develop hyperbilirubinemia after birth but not in utero? • Excretion of unconjugated bilirubin through the placenta into the mother’s circulation is no longer possible. 16. What is the name of the disorder in which levels of bilirubin remain excessively high in the newborn and are deposited in the brain? • Kernicterus 17. Why does fetal hemoglobin have a greater affinity for oxygen than adult hemoglobin? • Fetal hemoglobin interacts less readily with diphosphoglycerate (DPG), which inhibits hemoglobin-oxygen binding. 18. What is the significance of hyperdiploidy when diagnosing and treating leukemia? • Hyperdiploidy indicates a poor prognosis. 19. Sickle cell disease is classified as a(an): • Disorder initiated by hypoxemia and acidosis 20. Sickle cell disease (SCD) is what type of inherited disorder? • Autosomal recessive 21. Glucose 6-phosphate dehydrogenase (G6PD) deficiency is what type of inherited disorder? • X-linked recessive 22. Which blood cell type is elevated at birth but decreases to adult levels during the first year of life? • Monocytes 23. Erythroblastosis fetalis is defined as an: • Alloimmune disease in which maternal blood and fetal blood are antigenically incompatible 24. What is the fundamental defect that results in beta-thalassemia major? • A severe uncoupling of a- and b-chain synthesis occurs. 25. Idiopathic thrombocytopenic purpura (ITP) is an autoimmune process involving antibodies attacking which type of cells? • Platelets 26. Which type of anemia occurs as a result of thalassemia? • Microcytic, hypochromic 27. Which type of hemophilia affects only men? • Hemophilia A 28. Which disorder results in decreased erythrocytes and platelets with changes in leukocytes and has clinical manifestations of pallor, fatigue, petechiae, purpura, bleeding, and fever? • Acute lymphocytic leukemia (ALL) 29. Which manifestations of vasoocclusive crisis are associated with sickle cell disease (SCD) in infants? • Edema of the hands and feet 30. Hemophilia B is caused by a deficiency of which clotting factor? • IX 31. What is the chance with each pregnancy that a child born to two parents with the sickle trait will have sickle cell disease (SCD)? • 25% 32. Hemoglobin S (HbS) is formed in sickle cell disease as a result of which process? • Genetic mutation in which one amino acid (valine) is replaced by another (glutamic acid). 33. During childhood, when is dietary iron deficiency commonly diagnosed? • Between 6 months and 2 years 34. What is the cause of polycythemia in the fetus? • Increased erythropoiesis occurs in response to the hypoxic intrauterine environment. 35. What is the reason most children diagnosed with sickle cell anemia are not candidates for either bone marrow or stem cell transplants? • Well-matched stem cell donors are difficult to find. [Show More]
Last updated: 1 year ago
Preview 1 out of 29 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 14, 2021
Number of pages
29
Written in
Additional information
This document has been written for:
Uploaded
Apr 14, 2021
Downloads
0
Views
52

 HESI VI EXIT EXAM.png)


.png)
.png)
.png)