UWorld Maternity Nursing Test Questions and Answers (Verified 2021)
Document Content and Description Below
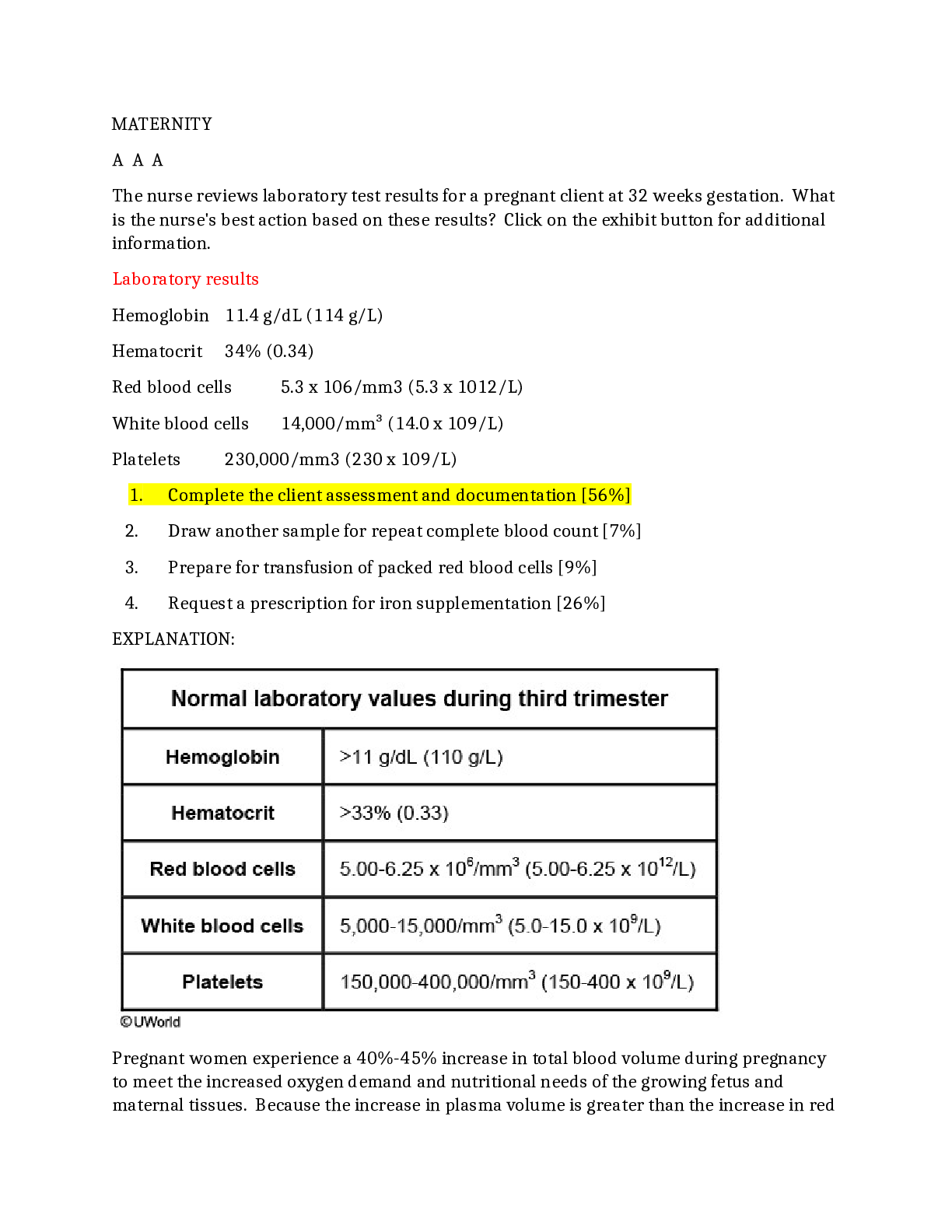
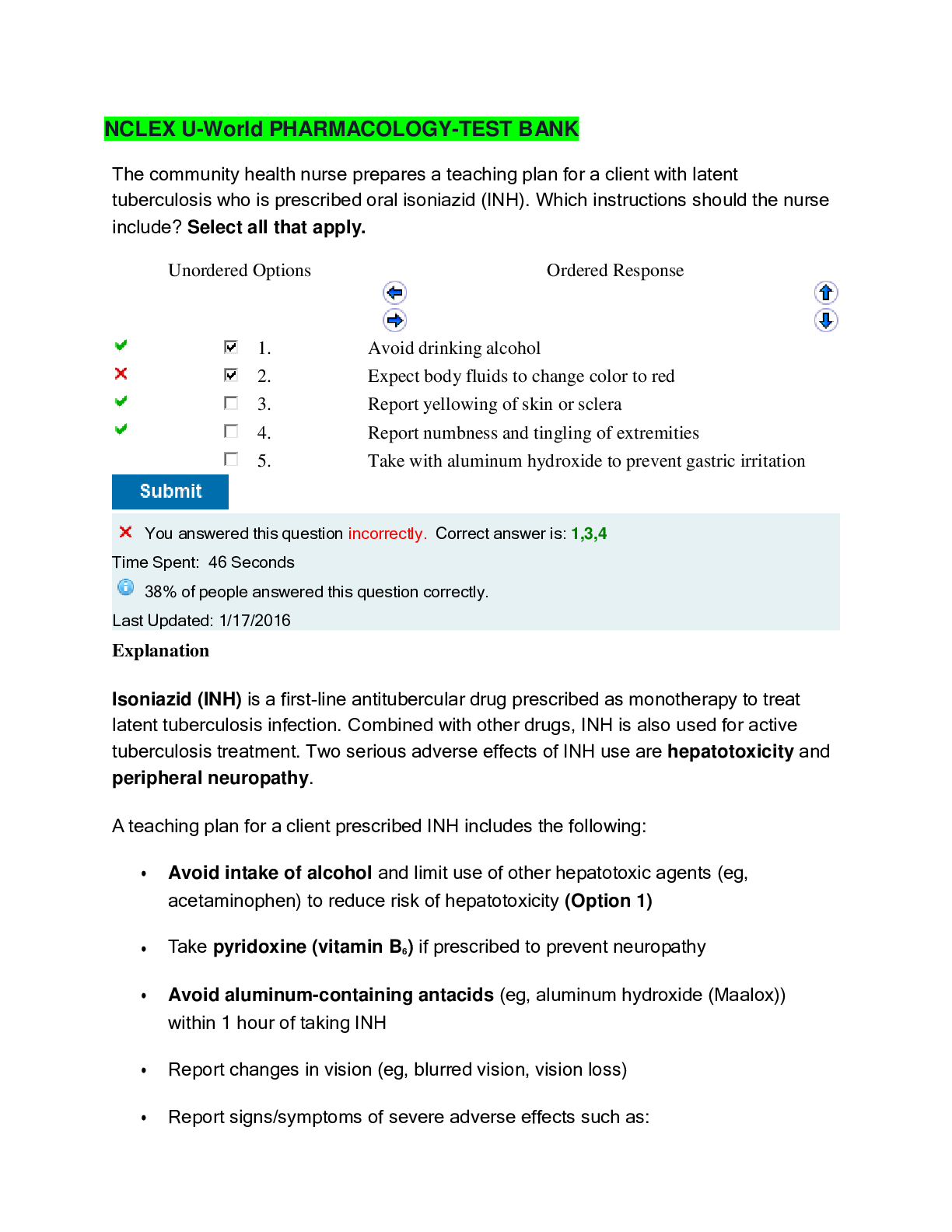
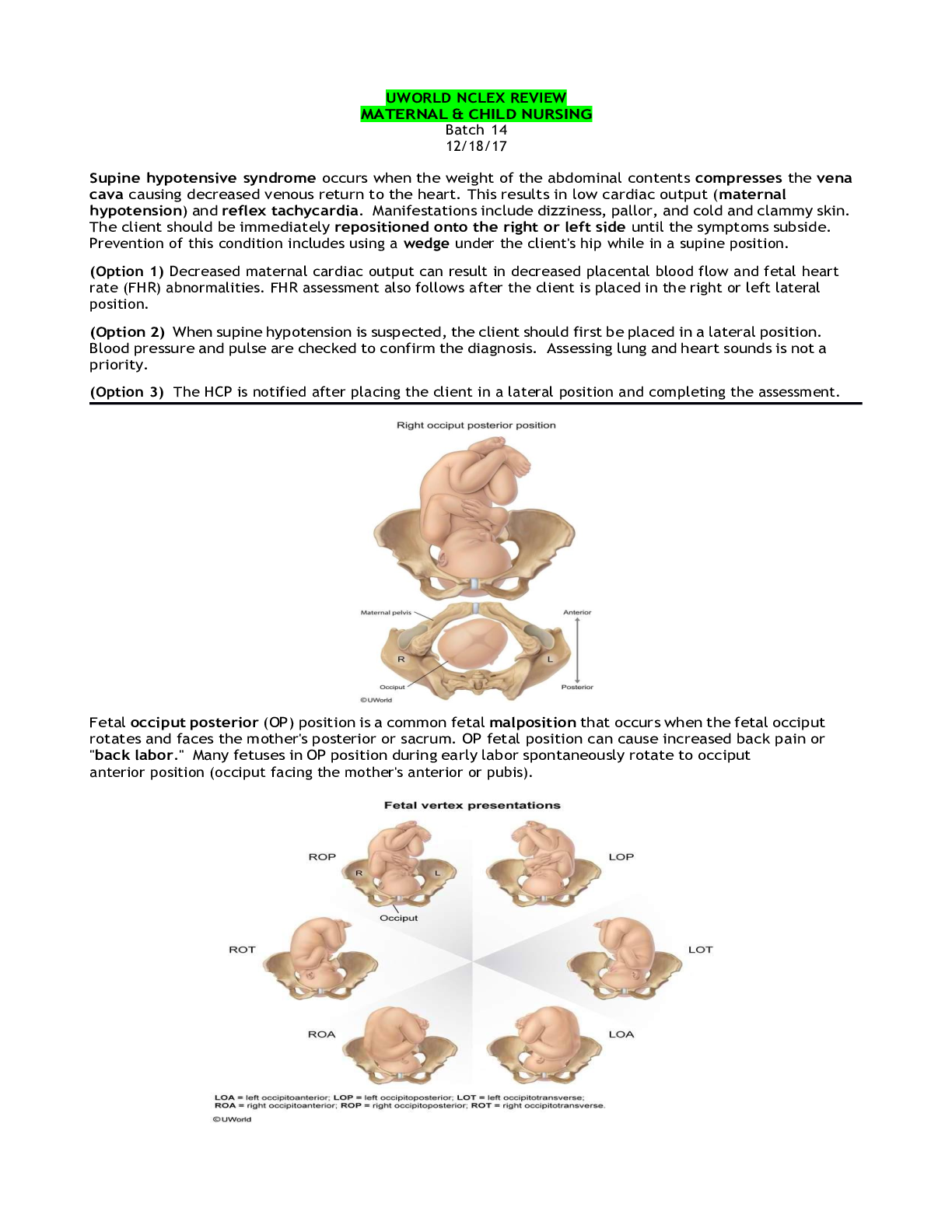
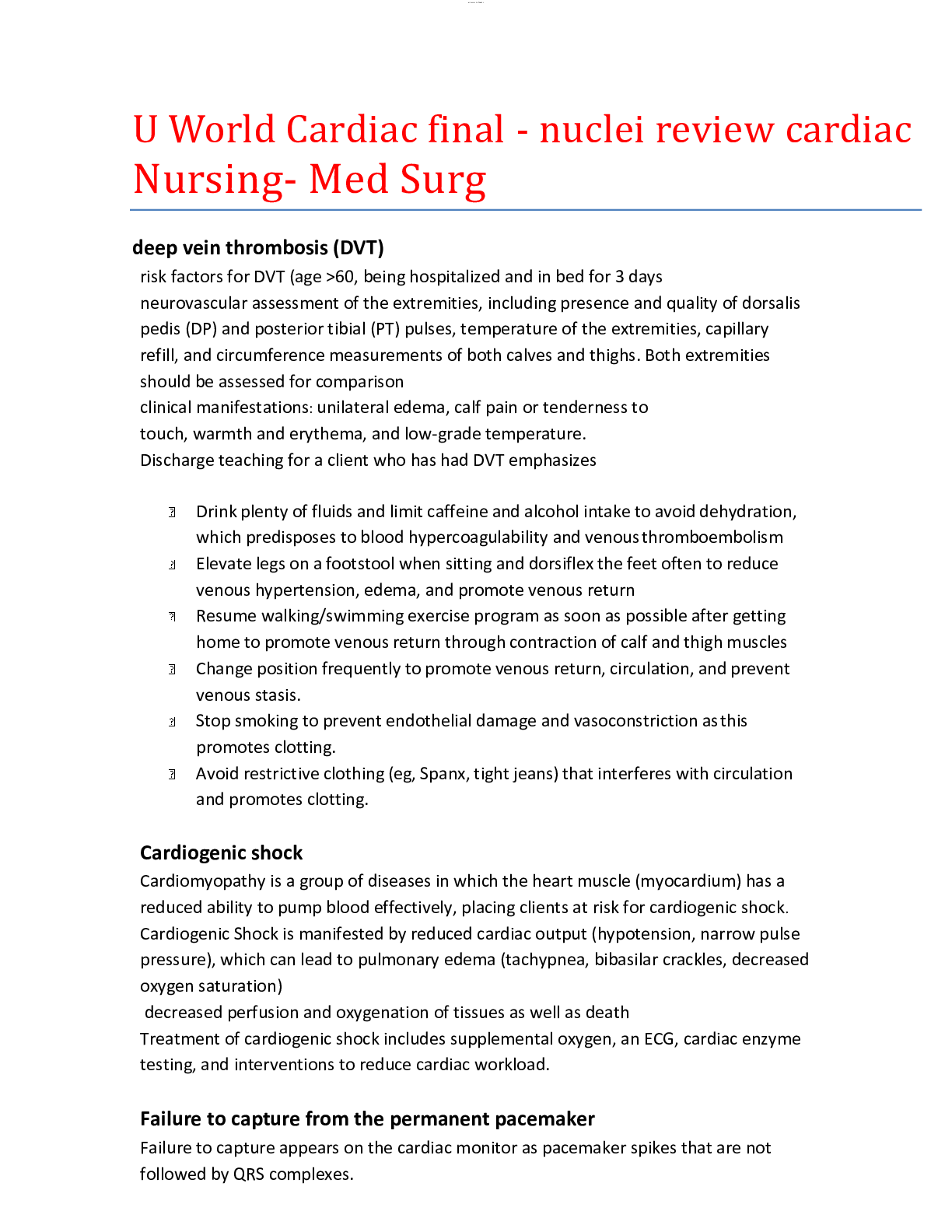
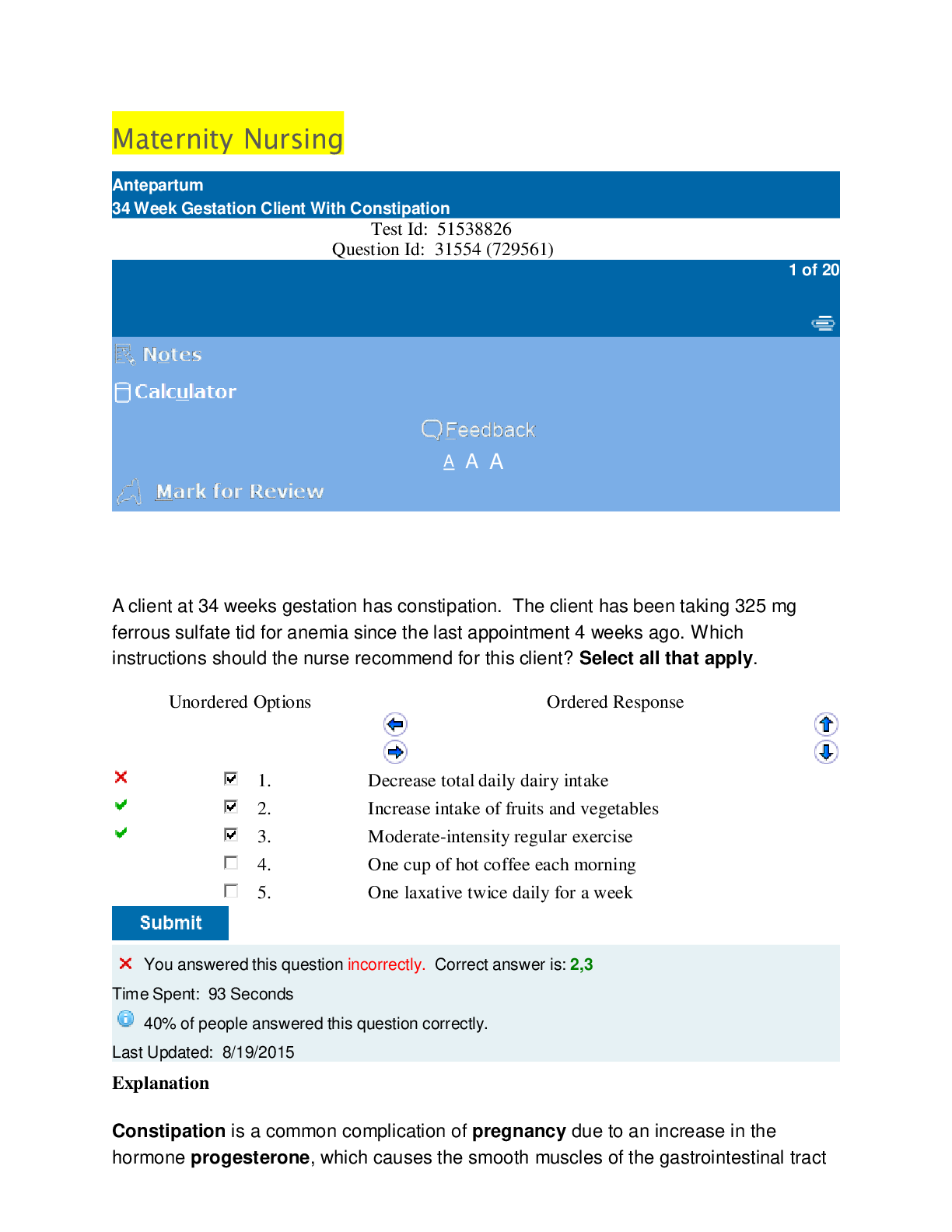
Maternity Nursing Test Id: 51538826 Question Id: 31554 (729561) A client at 34 weeks gestation has constipation. The client has been taking 325 mg ferrous sulfate tid for anemia since the la... st appointment 4 weeks ago. Which instructions should the nurse recommend for this client? Select all that apply. Unordered Options Ordered Response 1. Decrease total daily dairy intake 2. Increase intake of fruits and vegetables 3. Moderate-intensity regular exercise 4. One cup of hot coffee each morning 5. One laxative twice daily for a week Explanation Constipation is a common complication of pregnancy due to an increase in the hormone progesterone, which causes the smooth muscles of the gastrointestinal tract to relax. This leads to constipation from slowing of stool movement. Ferrous sulfate (iron) may also cause constipation. Interventions to prevent and treat constipation include: 1. High-fiber diet – increase fruits and vegetables and add breakfast cereals and whole-grain bread; prunes also help constipation 2. Increased fluid intake – drink at least 10-12 cups of fluid daily. In combination with a high-fiber diet, fluids help the most to treat constipation. 3. Regular exercise – moderate-intensity exercise (eg, walking, swimming, aerobics) is recommended throughout pregnancy 4. Bulk-forming fiber supplements – bulk-forming agents such as psyllium (eg, Metamucil), methylcellulose (eg, Citrucel), and wheat dextran (eg, Benefiber) are natural synthetic fiber products. These agents absorb water and create bulk to the stool. They have very few adverse effects. (Option 1) Dairy is a great source of calcium, which is essential for fetal bone development. (Option 4) Coffee may contain caffeine and should be avoided during pregnancy. Coffee can also lead to heartburn. (Option 5) Laxatives are not recommended during pregnancy due to the risk of dehydration and electrolyte imbalance. Dehydration can lead to preterm labor. The client should contact the health care provider (HCP) regarding any over-the-counter drugs, including stool softeners and laxatives. Educational objective: Constipation in pregnancy may be caused by increased progesterone levels and from ferrous sulfate. It is best treated with 10-12 cups of fluid daily, a high-fiber diet, and regular exercise. Clients should not take laxatives without first discussing these with the primary HCP. Test Id: 51538826 Question Id: 30515 (729561) A 28-year-old client is admitted to the labor and delivery unit for severe preeclampsia. She is started on IV magnesium sulfate infusion. Which signs indicate that the client has developed magnesium sulfate toxicity? Select all that apply. Unordered Options Ordered Response 1. 0/4 patellar reflex 2. Blood pressure is 156/84 mm Hg 3. Client voided 600 mL in 8 hours 4. Respirations are 10/min 5. Serum magnesium level is 6 mg/dL Explanation Although the normal blood level of magnesium is 1.5-2.5 mEq/L, a therapeutic magnesium level of 5-8 mg/dL is necessary to prevent seizures in a preeclamptic client (Option 5). Magnesium that exceeds the therapeutic level causes toxicity by acting as a central nervous system depressant and by blocking neuromuscular transmission. Loss of deep-tendon reflexes (DTRs) is the earliest sign of magnesium sulfate toxicity (9.6-12 mg/dL). If not recognized at this level, clients progress to respiratory depression (12-18 mg/dL), followed by cardiac arrest (24-30 mg/dL). Urine output is also reduced. The treatment for magnesium sulfate toxicity is immediate discontinuation of the infusion. Administration of calcium gluconate (antidote) is recommended only for cardiorespiratory compromise (not for loss of DTRs). (Option 1) DTRs are scored on a scale of 0-4; normal findings are 2+. DTRs should be assessed every 2 hours during magnesium administration. Decreased reflexes could be a sign of pending respiratory depression. (Option 2) Hypertension is a sign of preeclampsia. Hydralazine (Apresoline), methyldopa (Aldomet), or labetalol (beta blockers) is used to lower blood pressure if needed (usually considered when >160/110 mm Hg). (Option 3) Urine output below the obligatory amount of 30 mL/hr is a sign of magnesium toxicity. The client can always void more and would be expected to do so with additional fluid administration. (Option 4) Respiratory depression (rate <12/min) is an assessment finding indicating magnesium toxicity. Assessments (including vital signs) should initially be performed every 5-15 minutes during the loading dose and then every 30-60 minutes until the client stabilizes. Educational objective: The therapeutic level of magnesium for preeclampsia-eclampsia treatment is 5-8 mg/dL. Signs of magnesium toxicity are decreased/loss of DTRs, respiratory depression (<12/min), decreased urine output (<30 mL/hr), and cardiac arrest if these are not recognized. Calcium gluconate (antidote) should be readily available for cardiorespiratory compromise. Test Id: 51538826 Question Id: 30616 (729561) A client is at 24 weeks gestation and preeclampsia-eclampsia syndrome is suspected. Which of the following are significant signs/symptoms criteria related to this syndrome? Select all that apply. Unordered Options Ordered Response 1. 2+ pitting pedal edema 2. 300 mg/24 hr (0.3 g/day) protein in urine 3. Frequent urination 4. Headache, blurry vision 5. Hemoglobin 10 g/dL (100 g/L) Explanation Preeclampsia is hypertension and a multisystem disorder that occurs after the 20th week of pregnancy. There is reduced organ perfusion secondary to vasospasm and endothelial activation. Preeclampsia is defined as new-onset hypertension (≥140/90 mm Hg) after 20 weeks gestation plus proteinuria or signs of end-organ damage. Proteinuria is defined as ≥300 mg/24-hr (0.3 g/day) urine collection, protein/creatinine ratio ≥0.3, or dipstick of ≥1+. Cerebral symptoms, such as headache and visual changes, are reasons for concern. There is risk of cerebral edema, hemorrhage, and stroke. The most severe form is HELLP (Hemolysis, Elevated Liver enzymes, and Low Platelets). It is important to prevent progression of eclampsia (new-onset seizure, coma in the presence of preeclampsia) to grand mal seizure. (Option 1) Edema occurs in many normal pregnant women as well as those with preeclampsia. Edema is not part of the diagnostic criteria for preeclampsia. (Option 3) Frequent urination is common in pregnancy and is not considered part of preeclampsia-eclampsia criteria. (Option 5) Pregnancy causes an intravascular volume expansion larger than the rise in red blood cells, resulting in hemodilution. Inadequate iron stores or intake can also play a role. Anemia is defined as hemoglobin <11 g/dL (110 g/L) in the first and third trimesters and <10.5 g/dL (105 g/L) in the second trimester. Anemia is not a specific indicator or criterion for preeclampsia-eclampsia syndrome. Educational objective: Preeclampsia is defined as new-onset hypertension (≥140/90 mm Hg) plus proteinuria or signs of end-organ damage after 20 weeks gestation. Edema is not a diagnostic criterion for preeclampsia. Test Id: 51538826 Question Id: 31552 (729561) A client at 20 weeks gestation states that she started consuming an increased amount of cornstarch about 3 weeks ago. Based on this assessment, the nurse should anticipate that the health care provider will order which laboratory test(s)? Unordered Options Ordered Response 1. Hemoglobin and hematocrit levels 2. Human chorionic gonadotropin level 3. Serum folate level 4. White blood cell count Explanation Pica is the abnormal, compulsive craving for and consumption of substances normally not considered nutritionally valuable or edible. Common substances include ice, cornstarch, chalk, clay, dirt, and paper. Although the condition is not exclusive to pregnancy, many women only have pica when they are pregnant. Pica is often accompanied by iron deficiency anemia due to insufficient nutritional intake or impaired iron absorption. However, the exact relationship between pica and anemia is not fully understood. The health care provider would likely order hemoglobin and hematocrit levels to screen for the presence of anemia. (Option 2) Human chorionic gonadotropin is the hormone detected in a urine or serum pregnancy test to determine if a client is pregnant. It is not affected by iron deficiency anemia or pica. (Option 3) Increased folic acid consumption is necessary during pregnancy to reduce the risk for neural tube defects in the developing fetus. However, folate levels are not related to pica. (Option 4) A white blood cell count should be assessed when a client is suspected of having an infection. There is no indication that this client has an infection. Educational objective: Pica is the constant craving for and consumption of nonfood and/or nonnutritive food substances that may occur in pregnancy. It may be accompanied by iron deficiency anemia. Hemoglobin and hematocrit levels are useful in these clients to screen for anemia. Test Id: 51538826 Question Id: 30521 (729561) A client comes to the health care provider for a checkup. The client is G5T1P2A1L2M. Which explanation(s) represent a correct understanding of this terminology? Select all that apply. Unordered Options Ordered Response 1. The client had 1 child born later than 37 weeks gestation 2. The client had 1 pregnancy that ended before 20 weeks gestation 3. The client is currently pregnant 4. The L indicates the number of live births 5. The P indicates parity, the number of deliveries after 20 weeks gestation Explanation The GTPALM system is a shorthand system for recording a client's obstetrical history on the health care record. • G – gravida indicates the number of times a woman has been pregnant • T – indicates a term pregnancy (delivered after at least 37 weeks gestation) • P – indicates a preterm pregnancy (delivered between the beginning of 20 weeks and the end of 37 weeks gestation) • A – indicates an abortion, spontaneous or elective (termination of pregnancy prior to the beginning of 20 weeks gestation) • L – indicates children currently living • M – indicates multiple gestation This client (G5T1P2A1L2M) has been pregnant 5 times (including current pregnancy) (Option 3), had 1 term delivery (Option 1), 2 preterm deliveries, and 1 abortion (Option 2) , and has 2 living children. A two-digit, shorter version of gravidity and parity is sometimes used. In this version, gravida (G) represents the total number of pregnancies without reference to the number of fetuses or when the pregnancy ended. Para (P) refers to the number of births after 20 weeks gestation, regardless of whether they were live births or stillbirths. The number of fetuses delivered is not referenced, and abortions (spontaneous or induced) are not counted. (Option 4) The number following the L in the GTPALM notational system indicates the number of current living children, not the number of live births. (Option 5) The number following the P in the GTPALM notational system indicates the number of preterm births, not parity. Educational objective: GTPALM terminology is as follows: G – gravida, T – term infants, P – preterm infants (born between 20 and 37 completed weeks or 36 6/7 weeks gestation), A – abortions, L – currently living children, and M – multiple gestation Test Id: 51538826 Question Id: 33149 (729561) A client at 30 weeks gestation is hospitalized for preeclampsia. Which assessment finding requires priority intervention? Unordered Options Ordered Response 1. Elevated liver enzymes 2. Lower abdominal pain and vaginal bleeding 3. Swelling of the hands, feet, and face 4. Urine output of 25 mL/hr Explanation Placental abruption is a possible complication of preeclampsia that can be life- threatening to mother and baby. It occurs when the placenta tears away from the wall of the uterus due to stress, causing significant bleeding to the mother and depriving the baby of oxygen. Bleeding can be concealed inside the uterus. This may require immediate delivery of the baby. (Option 1) Elevated liver enzymes can indicate the start of a more serious condition called HELLP (Hemolysis, Elevated Liver enzymes, Low Platelets), another complication of preeclampsia. This client will need additional laboratory work. If HELLP is diagnosed, the only treatment is delivery. (Option 3) Swelling of the hands, feet, and face are expected findings of preeclampsia and should be assessed frequently. (Option 4) Normal urine output is 30 mL/hr; anything less represents a potential problem. Oliguria and elevated creatinine levels indicate kidney failure and require intervention. This client's urine output of 25 mL/hr does not represent an immediate, life-threatening condition. Educational objective: Preeclampsia in pregnancy manifests with high blood pressure and protein in the urine. Edema is expected, although it is not part of the criteria. Complications of preeclampsia include eclampsia, placental abruption, and HELLP (Hemolysis, Elevated Liver enzymes, Low Platelets) syndrome. Test Id: 51538826 Question Id: 31587 (729561) A client who reports sudden-onset severe right lower abdominal pain and dizziness is being evaluated for suspected ectopic pregnancy. Which assessment findings should the nurse anticipate? Select all that apply. Unordered Options Ordered Response 1. Blood pressure 82/64 mm Hg 2. Crackles on auscultation 3. Distended jugular veins 4. Pulse 120/min 5. Shoulder pain Explanation Ectopic pregnancy occurs when a fertilized ovum implants outside the uterine cavity. The majority of ectopic pregnancies occur in the fallopian tubes. Risk factors are sexually transmitted infections, tubal damage or infection, intrauterine devices, and tubal surgeries. Clinical manifestations are lower-quadrant abdominal pain on one side, mild to moderate vaginal bleeding, and missed or delayed menses. Signs of subsequent hypovolemic (hemorrhagic) shock from tubal rupture include dizziness, hypotension, tachycardia, and decreased urinary output to <30 mL/hr. Free intraperitoneal blood pooling under the diaphragm can cause referred shoulder pain. Peritoneal signs (eg, tenderness, rigidity, low-grade fever) develop subsequently. (Options 2 and 3) Distended jugular veins and lung crackles indicate volume overload conditions. The main risk with ectopic pregnancy is hypovolemic (internal hemorrhage) shock. Jugular veins would be flat in hypovolemic shock. Educational objective: The most common site for an ectopic pregnancy is the fallopian tubes. As the ovum grows and expands, tubal rupture may occur and result in active bleeding that progresses to life-threatening hypovolemic (hemorrhagic) shock. Copyright © UWorld. All rights reserved. Test Id: 51538826 Question Id: 31587 (729561) A client who reports sudden-onset severe right lower abdominal pain and dizziness is being evaluated for suspected ectopic pregnancy. Which assessment findings should the nurse anticipate? Select all that apply. Unordered Options Ordered Response 1. Blood pressure 82/64 mm Hg 2. Crackles on auscultation 3. Distended jugular veins 4. Pulse 120/min 5. Shoulder pain Explanation Ectopic pregnancy occurs when a fertilized ovum implants outside the uterine cavity. The majority of ectopic pregnancies occur in the fallopian tubes. Risk factors are sexually transmitted infections, tubal damage or infection, intrauterine devices, and tubal surgeries. Clinical manifestations are lower-quadrant abdominal pain on one side, mild to moderate vaginal bleeding, and missed or delayed menses. Signs of subsequent hypovolemic (hemorrhagic) shock from tubal rupture include dizziness, hypotension, tachycardia, and decreased urinary output to <30 mL/hr. Free intraperitoneal blood pooling under the diaphragm can cause referred shoulder pain. Peritoneal signs (eg, tenderness, rigidity, low-grade fever) develop subsequently. (Options 2 and 3) Distended jugular veins and lung crackles indicate volume overload conditions. The main risk with ectopic pregnancy is hypovolemic (internal hemorrhage) shock. Jugular veins would be flat in hypovolemic shock. Educational objective: The most common site for an ectopic pregnancy is the fallopian tubes. As the ovum grows and expands, tubal rupture may occur and result in active bleeding that progresses to life-threatening hypovolemic (hemorrhagic) shock. Copyright © UWorld. All rights reserved. Test Id: 51538826 Question Id: 30072 (729561) The nurse is returning the results of a urine pregnancy test to a client currently taking several medications. Which of the following prescriptions are contraindicated in pregnancy? Select all that apply. Unordered Options Ordered Response 1. Doxycycline 2. Fluticasone 3. Insulin aspart 4. Isotretinoin 5. Lisinopril 6. Thyroxine Explanation Doxycycline (Doryx) should not be used during pregnancy as it can impair bone mineralization in the fetus. Isotretinoin (Accutane) is a category X medication in pregnancy and causes severe birth defects. Retinoids may not be prescribed to a premenopausal client without a formal agreement to participate in the iPledge prescription tracking program. A commitment to always use at least 2 forms of birth control to prevent pregnancy is required. Angiotensin-converting enzyme (ACE) inhibitors such as lisinopril (Prinivil) should also not be used in pregnancy as they can affect kidney development in the fetus. (Option 2) Inhaled corticosteroids are classified under the United States Food and Drug Administration Pregnancy Category C – the drug has not been conclusively proven to be safe during pregnancy, but the prescription should be continued if there is a clear medical need (eg, severe asthma). (Option 3) Insulin is safe for use during pregnancy. (Option 6) The use of thyroxine (Synthroid) in pregnancy should be monitored carefully to provide an appropriate dose for the physiological changes of maternity, but it is not teratogenic. Educational objective: Commonly used medications that are absolutely contraindicated in pregnancy include doxycycline, isotretinoin, and ACE inhibitors. Copyright © Test Id: 51538826 Question Id: 31585 (729561) A 36-year-old multigravida is admitted with a diagnosis of severe preeclampsia. IV magnesium sulfate is prescribed. Which nursing measures should the nurse include in this client's plan of care? Select all that apply. Unordered Options Ordered Response 1. Assess for right upper quadrant pain 2. Check deep tendon reflex frequently 3. Ensure bright lighting to prevent falls 4. Ensure calcium gluconate is available 5. Have suction equipment ready to use Explanation Seizures are a complication of preeclampsia. Seizure precautions should be included in the plan of care. Hard side rails should be padded and the bed kept in the lowest position with the wheels locked to prevent trauma during a seizure. Suction equipment should be tested and ready to use (Option 5). The client should be placed in the side- lying position to promote placental blood flow and diuresis. Maternal findings that may precede seizures are hyperreflexia, the presence of clonus, or both. Findings of hyporeflexia may indicate magnesium toxicity (Option 2). Calcium gluconate should be immediately available to reverse effects of excess magnesium sulfate, a central nervous system depressant commonly prescribed to prevent seizures (Option 4). HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome is a severe complication of preeclampsia. The prominent symptom of HELLP syndrome is pain in the right upper quadrant (Option 1). (Option 3) Bright lights are contraindicated in the care plan for preeclampsia. In the presence of cerebral irritability, seizures may be precipitated by excessive visual or auditory stimuli. Educational objective: Safety measures for preeclampsia include seizure precautions and prevention and monitoring for complications such as HELLP syndrome. Magnesium sulfate is commonly prescribed to prevent seizures and is a central nervous system depressant that requires close monitoring. Test Id: 51538826 Question Id: 30565 (729561) A client comes to the clinic indicating that a home pregnancy test was positive. The client's last menstrual period (LMP) was September 7. Today is December 7. Which of the following are true statements for this client? Select all that apply. Unordered Options Ordered Response 1. According to Naegele's Rule, the expected date of delivery (EDD) is June 14 2. Auscultation of the fetal heart rate is possible 3. Fundal height should be 24 cm above the symphysis pubis 4. The client should be feeling fetal movement 5. Urinary frequency is a common sign Explanation The formula for Naegele's Rule to determine the EDD is the LMP minus 3 months plus 7 days. It is a "best guess" as this can be influenced by the regularity and length of a menstrual cycle. September 7 minus 3 months is June 7, plus 7 days is June 14 (Option 1). Detection of a fetal heart rate (FHR) is possible by auscultation with a Doppler by 10– 12 weeks gestation (Option 2). Urination frequency is a common symptom starting in the first trimester. It is primarily a result of hormonal changes and may be due to anatomical changes in the renal system. The client should be checked for a urinary tract infection if reporting dysuria, urgency, fever/chills, back pain, or sediment/blood/pus in the urine (Option 5). (Option 3) Uterine growth is assessed after 10–12 weeks gestation. It is assessed by measuring the height of the fundus with a centimeter measuring tape. The zero point of the tape is placed on the symphysis pubic and the tape is extended to the top of the fundus. The measurement should equal approximately the number of weeks pregnant. The client should empty the bladder before the measurement as a full bladder can displace the uterus. (Option 4) Quickening, the awareness of fetal movements, occurs around 18–20 weeks gestation in primigravidas (at 14–16 weeks in multigravidas). Educational objective: Naegele's Rule for determining EDD is LMP minus 3 months plus 7 days. FHR is auscultated at 10–12 weeks; quickening is felt at 18–20 weeks in a primigravida. Urinary frequency is a presumptive sign of pregnancy Test Id: 51538826 Question Id: 30448 (729561) A client visits the prenatal clinic for the first time. Which of the following are presumptive signs of pregnancy that the client may report during the intake assessment by the nurse? Select all that apply. Unordered Options Ordered Response 1. Breast fullness and tenderness 2. Last menstrual period 8 weeks ago 3. Nausea and vomiting that are worsening every day 4. Painless contractions at irregular intervals 5. Positive home pregnancy test 3 weeks ago Explanation Subjective (presumptive) signs of pregnancy are those that are self-reported by a pregnant client. These signs may have pathologic medical causes and therefore cannot be considered diagnostic for pregnancy. Subjective signs include: • Breast fullness and tenderness (may occur just prior to menstrual periods or with use of birth control hormones) • Amenorrhea (may be seen with early menopause, endocrine dysfunction, acute or chronic diseases, or psychological stress) • Nausea and vomiting that begin around the sixth week after the last menstrual period (may be result of many other conditions, such as gastroenteritis) Objective (probable) signs of pregnancy are those that can be observed by the health care provider during assessment and examination. Combined with subjective signs, these may be more indicative of pregnancy but may still have some pathologic causes. Positive signs of pregnancy represent conclusive proof of pregnancy and cannot be confused with any pathologic state as they are all related to the fetus. (Option 4) Braxton Hicks contractions are painless and occur at irregular intervals. They can occur as early as 6 weeks gestation and are considered a probable sign of pregnancy. (Option 5) A positive pregnancy test is considered an objective sign of pregnancy. Hormonal disturbances, endocrine disease, and gestational trophoblastic disease can cause false positive pregnancy test results. Educational objective: Subjective (self-reported) signs of pregnancy include amenorrhea, nausea and vomiting, breast tenderness, and fatigue. Objective signs include uterine and cervical changes, palpable Braxton Hicks contractions, skin changes, and positive pregnancy tests. Diagnostic signs include a distinguishable fetal heartbeat, fetal movement palpated by the health care provider, and ultrasound visualization of the fetus. Test Id: 51538826 Question Id: 30484 (729561) A 27-year-old client at 10 weeks gestation comes to the prenatal clinic. Which vaccines can be safely given to this client during the pregnancy? Select all that apply. Unordered Options Ordered Response 1. Influenza inactivated vaccine 2. Influenza nasal spray vaccine 3. Measles-mumps-rubella vaccine (MMR) 4. Tetanus, diphtheria, and pertussis (Tdap) immunization 5. Varicella vaccine Explanation During influenza season (October-March), it is safe for pregnant women to receive the inactivated influenza vaccine (intramuscular [IM]) regardless of the trimester. Pregnant women are at increased risk of hospitalization and of contracting a more severe illness due to influenza; the resulting complications to the fetus include premature labor/delivery and a small for gestational age baby. Maternal immunization offers passive immunity to the infant in the first months of life. Tdap is administered to pregnant women ideally between the 27th and the end of the 36th week of gestation. The Centers for Disease Control and Prevention (CDC) guidelines indicate that 1 dose of Tdap should be given with each pregnancy. Pertussis can cause severe, life-threatening complications if contracted by an immunocompromised infant. Maternal antibodies provide passive immunity via the placenta to protect the newborn until the DTaP vaccine can be administered to the infant. (Option 2) The influenza nasal spray vaccine is a live, attenuated influenza vaccine (LAIV) given to individuals age 2-49 years. Live vaccines are not safe for pregnant women as they have a teratogenic effect on the developing embryo and fetus. (Option 3) MMR is also a live vaccine that is not safe for pregnant women due to risk of severe birth defects and miscarriage from the rubella component. (Option 5) Varicella (chickenpox) vaccine is a category X, live, attenuated vaccine that is contraindicated for pregnancy or a planned pregnancy within 4 weeks of administration. Varicella vaccine may be given after birth and is safe to give to a woman who is breastfeeding her infant. Educational objective: Influenza inactivated vaccine IM may be given at any time during pregnancy from October through March. Tdap vaccine is also an inactivated vaccine that is ideally given between the 27th and the end of the 36th week of gestation. Live virus vaccines (MMR, varicella, and LAIV) can be teratogenic and are not recommended in pregnancy. Test Id: 51538826 Question Id: 30479 (729561) The nurse is teaching a client, gravida 1 para 0, at 8 weeks gestation about expected weight gain in pregnancy. The client's prepregnancy BMI is 21 kg/m2. Which of the following statements made by the client indicates an understanding about weight gain? Unordered Options Ordered Response 1. "I should gain 10 lb (4.5 kg) during the first trimester." 2. "I should gain about 30 lb (13.6 kg) during pregnancy." 3. "I should gain no more than 0.5 lb (0.2 kg) per week during the second and third trimesters." 4. "If I keep my weight gain to less than 20 lb (9.1 kg) during pregnancy, it will be easier to lose it after the baby is born." Explanation According to recommendations made by the Institute of Medicine in 2009, weight gain during pregnancy should be determined by prepregnancy BMI. Underweight clients need to gain more weight (1 lb [0.5 kg]/wk) during the second and third trimesters of pregnancy than do obese clients (0.5 lb [0.2 kg]/wk). However, weight gain in the first trimester should be 1.1-4.4 lbs (0.5-2.0 kg) regardless of BMI. With a prepregnancy BMI of 21 kg/m2, this client is classified as an appropriate-weight client and should gain 25-35 lb (11.3-15.9 kg). (Option 1) Weight gain during the first trimester should be approximately 1.1-4.4 lb (0.5-2.0 kg). A 10-lb (4.5-kg) weight gain during the first 3 months of pregnancy would be too much in any client. (Option 3) A client of normal weight, such as this client, should gain approximately 1 lb (0.5 kg)/wk during the second and third trimesters of pregnancy. A weight gain of only 0.5 lb (0.2 kg)/wk is recommended for obese clients. (Option 4) A weight gain of 20 lb (9.1 kg) during pregnancy is inadequate for a client of normal weight. Restricting weight gain could put the fetus at risk for low birth weight (<2500 g) and preterm birth. Educational objective: Appropriate total weight gain during pregnancy decreases risks to the client and fetus. • An underweight client should gain 28-40 lb (12.7-18.1 kg) • An appropriate-weight client should gain 25-35 lb (11.3-15.9 kg) • An overweight client should gain 15-25 lb (6.8-11.3 kg) • An obese client should gain 11-20 lb (5.0-9.1 kg) Weight gain in the first trimester should be 1.1-4.4 lb (0.5-2.0 kg) regardless of BMI. Test Id: 51538826 Question Id: 31457 (729561) Which client in a prenatal clinic should the nurse assess first? Unordered Options Ordered Response 1. An 11-week gestation client with backache and 5-lb (2.26-kg) weight gain since conception 2. A 16-week gestation client with hemorrhoid pain and sinus congestion 3. A 21-week gestation client with blurred vision and increased facial edema 4. A 32-week gestation client with chloasma and urinary frequency Explanation Gestational hypertension refers to high blood pressure that occurs as a result of pregnancy. It is considered a serious condition and can lead to potentially life- threatening eclampsia. Gestational hypertension is a blood pressure ≥140/90 mm Hg that occurs after 20 weeks gestation without proteinuria. The diagnosis is changed to preeclampsia with the development of proteinuria or signs of end-organ dysfunction. This client should be assessed first because the client is exhibiting classic symptoms of preeclampsia. The nurse should assess the client's blood pressure as soon as possible. (Option 1) Backache and weight gain are common pregnancy discomforts and physical changes seen in the first trimester. (Option 2) Hemorrhoid pain and sinus congestion are common discomforts during pregnancy. This client should be assessed but is not the highest priority. (Option 4) Chloasma and urinary frequency are common physical changes of pregnancy seen in the third trimester. Chloasma (melasma) appears as a symmetrical, blotchy, brownish pigmentation on the face. Educational objective: The nurse should assess the client with unexpected symptoms first and then assess the remaining clients. Gestational hypertension refers to high blood pressure that occurs as a result of pregnancy. Test Id: 51538826 Question Id: 31459 (729561) A nurse is caring for a pregnant client who has hyperemesis gravidarum. Which assessment findings should the nurse anticipate? Select all that apply. Unordered Options Ordered Response 1. Blood pressure 160/94 mm Hg 2. Large urine protein 3. Positive urine ketones (moderate) 4. Pulse 106/min 5. Urine specific gravity 1.010 Explanation Hyperemesis gravidarum is a disorder that causes pregnant clients to have severe nausea and vomiting. This leads to fluid and electrolyte imbalances, nutritional deficiencies, ketonuria, and weight loss. On assessment, the nurse should expect signs and symptoms of dehydration, which include dry mucous membranes, poor skin turgor, decreased urine output, tachycardia, and low blood pressure. Ketonuria indicates that the body is breaking down fat to use for energy due to the client's starvation state. (Options 1 and 5) The client with hyperemesis gravidarum is dehydrated. Blood pressure is expected to be low due to lack of blood volume. The urine specific gravity will be increased (>1.030) as the urine is in a concentrated state. Blood urea nitrogen is also elevated (>20 mg/dL). (Option 2) Proteinuria is associated with kidney disease or preeclampsia. Hyperemesis does not cause proteinuria. Educational objective: Excessive vomiting (hyperemesis gravidarum) leads to fluid and electrolyte imbalances (hypokalemia, metabolic alkalosis), weight loss, nutritional deficiencies, and ketonuria. The signs and symptoms of dehydration include poor skin turgor, decreased urine output, tachycardia, low blood pressure, and dry mucous membranes. Test Id: 51538826 Question Id: 30397 (729561) A client at 39 weeks gestation is brought to the emergency department after a motor vehicle crash. The client, who is secured supine on a backboard, suddenly becomes pale with a blood pressure of 88/50 mm Hg. What action should the nurse take first? Unordered Options Ordered Response 1. Administer normal saline fluid bolus 2. Assess cervix for presenting part 3. Obtain fetal heart rate 4. Turn client laterally Explanation Supine hypotensive syndrome results from compression of the maternal inferior vena cava by the large gravid uterus in mid to late pregnancy when the client is in the supine position. The venous return is reduced, causing maternal hypotension from reduced cardiac output. The client can also report feeling dizzy and faint. The first step is to rectify the cause by turning the client laterally while still strapped on the backboard. (Option 1) The etiology is not hypovolemia but perfusion. A fluid bolus of isotonic fluids (normal saline or lactated Ringer's) can be administered if the position change does not relieve the symptoms. Mean arterial pressure (MAP) should be >60 mm Hg for effective organ perfusion. Normal MAP is 70-105 mm Hg. (Option 2) The client does not have classic signs of a precipitous or impending delivery. Classic signs or symptoms of the second stage of labor/delivery of the baby include feeling the need to push, an intense urge to bear down, or a sensation of cervical pressure. A pelvic examination can be performed, but it is not the first priority. (Option 3) The etiology is related not to the fetus, but to the maternal circulation. Because the client does not have adequate cardiac output, circulation to the fetus could be compromised. The first priority is to rectify the client's perfusion issue and check the fetus. The best indicators of fetal health are heart rate and movement. Educational objective: Supine hypotensive syndrome results from compression of the maternal inferior vena cava by the large gravid uterus in mid to late pregnancy when the client is in the supine position. It can be corrected by first positioning the client laterally. Test Id: 51538826 Question Id: 31621 (729561) A nurse is measuring a uterine fundal height for a client who is at 36 weeks gestation in supine position. The client suddenly reports dizziness and the nurse observes pallor and damp, cool skin. What should the nurse do first? Unordered Options Ordered Response 1. Assess fetal heart rate and pattern 2. Assess heart and lung sounds 3. Notify the health care provider (HCP) immediately 4. Reposition the client into a lateral position Explanation Supine hypotensive syndrome occurs when the weight of the abdominal contents compresses the vena cava causing decreased venous return to the heart. This results in low cardiac output (maternal hypotension) and reflex tachycardia. Manifestations include dizziness, pallor, and cold and clammy skin. The client should be immediately repositioned onto the right or left side until the symptoms subside. Prevention of this condition includes using a wedge under the client's hip while in a supine position. (Option 1) Decreased maternal cardiac output can result in decreased placental blood flow and fetal heart rate (FHR) abnormalities. FHR assessment also follows after the client is placed in the right or left lateral position. (Option 2) When supine hypotension is suspected, the client should first be placed in alateral position. Blood pressure and pulse are checked to confirm the diagnosis. Assessing lung and heart sounds is not a priority. (Option 3) The HCP is notified after placing the client in a lateral position and completing the assessment. Educational objective: Supine hypotensive syndrome is usually seen in the third trimester of pregnancy when the weight of the uterine contents compresses the inferior vena cava. The resultant maternal hypotension is best treated initially by turning the client to the right or left side to relieve pressure on the vena cava. Test Id: 51538826 Question Id: 30644 (729561) A pregnant client comes for a routine first prenatal examination. According to the last menstrual period, the estimated gestational age is 14 weeks. Where would the nurse expect to palpate the uterine fundus in this client? Unordered Options Ordered Response 1. 14 cm above the symphysis pubis 2. 14 cm above the umbilicus 3. Just above the symphysis pubis 4. Just below the umbilicus Explanation The enlarging pregnant uterus rises above the symphysis pubis at 12-14 weeks gestation. It reaches the umbilicus at 20-22 weeks gestation and approaches the xiphoid process around 36 weeks gestation. At 38-40 weeks, the fetus engages into the maternal pelvis and the fundal height drops. From approximately 18-32 weeks gestation, the fundal height, measured in cm from the symphysis pubis to the top of the fundus, is approximately the same as the estimated weeks gestation. (Options 1, 2 and 4) At 14 weeks gestation, the uterine fundus should be just above the symphysis pubis. Educational objective: The fundus rises above the symphysis pubis at 12-14 weeks gestation, reaches the umbilicus at 20-22 weeks gestation, and reaches the xyphoid process at 36 weeks gestation. From 18-32 weeks gestation, the fundal height in cm is approximately the same as the weeks gestation. Test Id: 51538826 Question Id: 31836 (729561) While triaging pregnant clients in the obstetrics clinic, the nurse should alert the health care provider to see which client first? Unordered Options Ordered Response 1. First-trimester client reporting frequent nausea and vomiting 2. Second-trimester client with multiple star-shaped vascular spiders 3. Second-trimester client with obesity reporting lack of fetal movement 4. Third-trimester client with epigastric pain and elevated liver enzymes Explanation Elevated liver enzymes and epigastric pain could be an indication of HELLP syndrome, a severe form of preeclampsia. HELLP syndrome involves multisystem failure represented by Hemolysis, Elevated Liver enzymes, and Low Platelet count. The clinical presentation of HELLP syndrome is variable, but most clients have epigastric pain accompanied by nausea, vomiting, and malaise. HELLP syndrome is often mistaken for viral gastroenteritis due to the syndrome's nonspecific presentation. Proteinuria and hypertension, which are classic for preeclampsia, can be absent. Therefore, misdiagnosis is common and has resulted in severe morbidity (eg, placental abruption, liver failure or hemorrhage, acute respiratory distress syndrome, stroke) and maternal death. (Option 1) Nausea and vomiting during the first trimester are normal, expected findings. Vomiting that continues past the first trimester or that is accompanied by fever, pain, or weight loss is considered abnormal and requires intervention. (Option 2) Angiomas (vascular spiders) are a common, expected finding in pregnancy due to increased circulating estrogen. Angiomas can be tiny, star-shaped, or branched; blue or red; slightly elevated; or pulsating. Multiple angiomas may be present. They typically resolve after birth. (Option 3) Maternal perception of fetal movement can be altered by obesity, maternal position, fetal sleep cycle, fetal position (fetal spine anterior), anterior placenta, and amniotic fluid volume (increased or decreased). This client should be assessed to determine the cause but is not the priority. Educational objective: HELLP syndrome is a severe form of preeclampsia. However, its clinical presentation is quite variable and may include nonspecific symptoms such as epigastric pain, nausea, vomiting, and malaise. Proteinuria and hypertension can be [Show More]
Last updated: 1 year ago
Preview 1 out of 39 pages
Also available in bundle (2)
UWorld Nursing Tests Bundle (Pharmacology, Medical-Surgical , Maternity, Pediatric, Prioritization, Leadership and Management , Mental Health) ALL Answers 100% CORRECT (2021 Version)
UWorld Nursing Tests Bundle (Pharmacology, Medical-Surgical , Maternity, Pediatric, Prioritization, Leadership and Management , Mental Health) ALL Answers 100% CORRECT (2021 Version)
By A+ Solutions 3 years ago
$14.5
7

HESI MATERNITY QUESTIONS & ANSWERS, UWorld Maternity Nursing Tests, HESI MATERNITY 2 TEST BANK, HESI MATERNITY ALL PRACTICE QUESTIONS, Maternity HESI 1,2 Test Bank (Summer 2021) Questions, Answers & Rationale, A+ Guide,OB HESI 2 TEST BANK / OB HESI 2 TEST BANK:LATEST SPRING 2021.
HESI MATERNITY QUESTIONS & ANSWERS, UWorld Maternity Nursing Tests, HESI MATERNITY 2 TEST BANK, HESI MATERNITY ALL PRACTICE QUESTIONS, Maternity HESI 1,2 Test Bank (Summer 2021) Questions, Answers & R...
By A+ Solutions 3 years ago
$15
17
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 18, 2021
Number of pages
39
Written in
Additional information
This document has been written for:
Uploaded
Apr 18, 2021
Downloads
0
Views
99