*NURSING > UWorld > UWorld Leadership and Management Test, Questions and Answers {2021). Already Graded A (All)
UWorld Leadership and Management Test, Questions and Answers {2021). Already Graded A
Document Content and Description Below
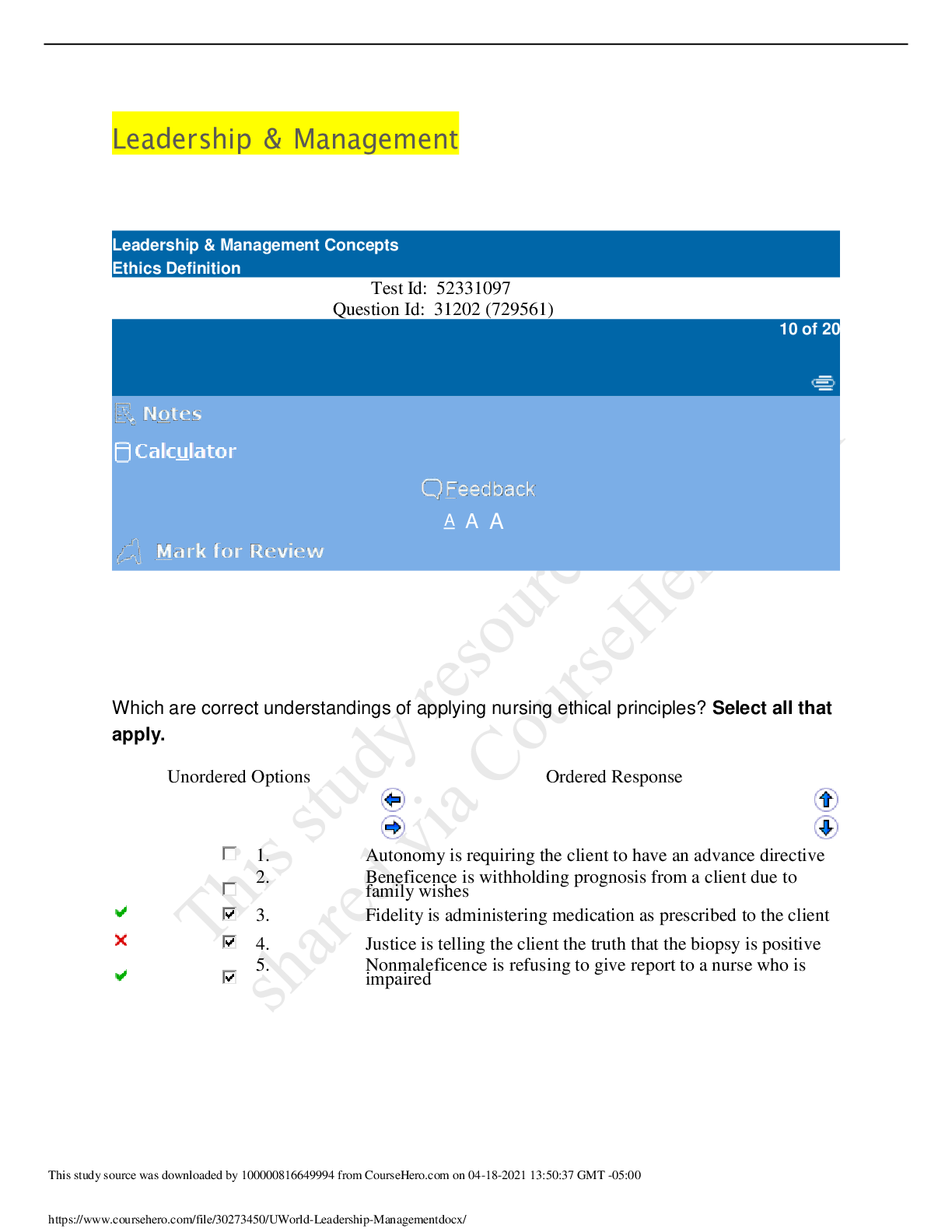
Leadership & Management Test Id: 52331097 Question Id: 31202 (729561) Which are correct understandings of applying nursing ethical principles? Select all that apply. Unordered Options O... rdered Response 1. Autonomy is requiring the client to have an advance directive 2. Beneficence is withholding prognosis from a client due to family wishes 3. Fidelity is administering medication as prescribed to the client 4. Justice is telling the client the truth that the biopsy is positive 5. Nonmaleficence is refusing to give report to a nurse who is impaired Explanation Ethical principles guide the nurse in making appropriate decisions and acting accordingly. They speak to the essence but not to the specifics of the law. Fidelity is exhibiting loyalty and fulfilling commitments made to oneself and others. It includes meeting the expected responsibilities of professional nursing practice and provides the basis of accountability (taking responsibility for one's actions) (Option 3). Nonmaleficence means to do no harm and relates to protecting clients from danger when they are unable to do so themselves due to a mental/physical condition (eg, children, client with Alzheimer disease) and from a nurse who is impaired (Option 5). (Option 1) Autonomy is the right to make decisions for oneself (eg, informed consent). Although having an advance directive is an example of autonomy, requiring one violates this principle. The client has a right to refuse even if the nurse believes it is in the client's best interest. (Option 2) When a diagnosis is withheld, even if due to the nurse's or family's good intentions, it violates the principle of autonomy. Beneficence means to do good (eg, implementing interventions to promote the client's well-being). (Option 4) The principle of justice refers to treating all clients fairly (ie, without bias). Veracity is telling the truth as a fundamental part of building a trusting relationship. Educational objective: Nonmaleficence is doing no harm, fidelity is loyalty and commitment, justice is equal treatment for all, beneficence is doing good for the client's best interest, and autonomy is making decisions for oneself. Test Id: 52180127 Question Id: 33538 (729561) The nurse verifies a signed informed consent for an inguinal hernia repair. During the procedure, the surgeon discovers a secondary ventral hernia that also requires repair. What nursing action needs to be completed? Unordered Options Ordered Response 1. Document that an additional hernia was found and will require surgery at a later time 2. Explain the need for additional repair to the client's family member before proceeding 3. Witness a signed consent for the added procedure after the client is awake 4. Witness a signed consent for the new procedure immediately with a family member Explanation Informed consent consists of 3 principles: 1. The surgeon clearly explains the current diagnosis, planned procedure along with risks and benefits, expected outcome, alternate treatment options, and prognosis if the procedure is not performed. 2. The client has indicated understanding of the information. 3. The client is giving voluntary, legal consent for the procedure. The nurse is responsible for witnessing the client's signature and ensuring that the client understands the information given by the surgeon. Procedures not listed on the consent may not be performed without further authorization. If the need for an additional procedure is discovered during surgery, the client's family may give consent after speaking with the surgeon (Option 4). (Option 1) Unless family members deny consent or cannot be reached, it is in the client's best interest to have the hernia repaired during this surgery rather than go through the physical and financial strain of a second surgery. (Option 2) Notifying the family is not sufficient; the surgeon must obtain informed consent for the additional procedure. (Option 3) The only appropriate time to perform a procedure without first obtaining consent is when lifesaving measures are needed. Waiting until the client is awake to obtain consent for a procedure already performed is illegal and would warrant charges of assault and battery. Educational objective: Informed consent is required before any procedure is performed. The nurse is responsible for witnessing this occurrence. If the need for an additional procedure is discovered during surgery, the client's family may give consent after speaking with the surgeon. Test Id: 52084841 Question Id: 33898 (729561) A licensed practical nurse is discussing some client findings with the registered nurse (RN). Which client would be the priority for the RN to assess? Unordered Options Ordered Response 1. 72-year-old client with pneumonia who is receiving intravenous fluids and has a new S3 heart sound 2. Client on metoprolol for hypertension with pulse of 54/min and blood pressure of 154/82 mm Hg 3. Client who is 8 hours postoperative hip arthroplasty with 205 mL drainage in the suction drain 4. Client with 345 mL gastric residual volume aspirated from a PEG tube before an enteral feed Explanation An S3 sound is made when blood from the atrium is pumped into a noncompliant ventricle. S3 is heard after S2 (ventricular gallop). It can present as a normal finding in young adults. In older clients, S3 is a significant finding as it often indicates heart failure or volume overload. This client may be receiving excessive IV fluids that are causing volume overload. (Option 2) The normal heart rate is 60-100/min; however, the client's medications and baseline numbers need to be assessed when analyzing vital signs. A heart rate of 54/min in a client on beta blockers (eg, metoprolol, atenolol, propranolol) is not the priority to assess unless signs of decreased cardiac output are evident. The nurse should discuss this client's medication regimen with the health care provider as the blood pressure remains elevated. (Option 3) An output of 205 mL in the first 8 hours after hip arthroplasty is an expected finding due to the highly vascular nature of the hip. Drainage is considered excessive if there is >250 mL in the first 8 hours. (Option 4) Enteral feeds may need to be adjusted if high residual volumes (>250 mL) continue due to the high risk of aspiration, but this client would not be a priority over one with possible new-onset heart failure. Educational objective: An S3 sound can be an expected finding in young adults. However, a new S3 sound in older adults should be evaluated as it may be the first sign of heart failure or volume overload. Test Id: 52036792 Question Id: 33875 (729561) The nurse is working on a busy medical-surgical unit and is responding to the client call lights. Which statement would be the priority to assess first? Unordered Options Ordered Response A 65-year-old female client recently started on celecoxib says, "I am 1. having some nausea and my upper back and shoulder are hurting quite a bit." 2. A client's child says, "My parent has been here for 2 days without anything to eat or drink." 3. A paraplegic client with multiple stage 4 pressure ulcers says, "I have had a bowel movement and need to be cleaned up." 4. A postoperative client says, "I am very nauseous and just threw up. This pain medicine is making me really sick." Explanation Celecoxib (Celebrex), a COX-2 inhibitor, has a black box warning for increased risk of cardiovascular complications. Myocardial infarction symptoms, which can be vague in female clients, include nausea and upper back and shoulder pain. These symptoms would be the priority to assess first, and immediate testing (ie, ECG, cardiac enzymes) would be warranted. (Option 2) This client's nutritional status is concerning and needs to be addressed but would not be a priority over a client experiencing a possible acute myocardial infarction. (Option 3) This client needs cleaning as soon as possible to prevent fecal matter from entering into wounds. Cleaning the client can be delegated to a licensed practical nurse or unlicensed assistive personnel and would not be a priority over a client experiencing a possible acute myocardial infarction. The registered nurse can assess the wounds and dressings later. (Option 4) This client's nausea and pain medication need to be addressed; they would not be a priority over a client experiencing a possible acute myocardial infarction. Educational objective: COX-2 inhibitors (eg, celecoxib) and nonsteroidal anti-inflammatory drugs (eg, ibuprofen) are associated with increased risk of cardiovascular events. Myocardial infarction in an elderly woman can present with atypical symptoms (eg, shoulder pain, nausea). Test Id: 51996952 Question Id: 31201 (729561) Which statements related to ethical nursing practices are correct? Select all that apply. Unordered Options Ordered Response 1. Accountability is documenting that the nurse administered the wrong medication 2. Autonomy is informing the client of the decision the family made for the client 3. Confidentiality is respecting a client's request to keep suicidal ideation a secret 4. Justice is providing the same cardiac care to a homeless person as a businessperson 5. Nonmaleficence is reporting abuse for a client with Alzheimer disease Explanation Ethical principles guide decision making and appropriate behavior. Justice is treating every client equally regardless of gender, sexual orientation, religion, ethnicity, disease, or social standing (Option 4). Accountability refers to accepting responsibility for one's actions and admitting errors (Option 1). Nonmaleficence means doing no harm. It also relates to protecting clients who are unable to protect themselves due to their physical or mental condition. Examples include infants/children, clients under the effects of anesthesia, and clients with dementia (Option 5). (Option 2) Autonomy is freedom for a competent client to make decisions for oneself, even if the nurse or family does not agree (eg, informed consent, advanced directive). The nurse can provide information and should respect the client's decisions. (Option 3) Confidentiality means that information shared with the nurse is kept in confidence unless permission is given to share or it is required by law to be shared to protect the client and/or community (eg, reportable infectious diseases). If a client discusses suicidal ideation with the nurse, it must be appropriately reported to protect the client from self-harm. Educational objective: Accountability is accepting responsibility for one's actions. Autonomy is making an informed decision about treatment for oneself. Confidentiality is not sharing information unless permission is given or required by law. Justice is treating every client equally. Nonmaleficence is doing no harm. [Show More]
Last updated: 1 year ago
Preview 1 out of 10 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Apr 18, 2021
Number of pages
10
Written in
Additional information
This document has been written for:
Uploaded
Apr 18, 2021
Downloads
0
Views
90