Medical Surgical Question and Answers. 100%.
Document Content and Description Below
1. A 60-year-old male client comes into the emergency department with complaints of crushing substernal chest pain that radiates to his shoulder and left arm. The admitting diagnosis is acute myocardi... al infraction (MI). Immediate admission orders include oxygen by nasal cannula at 4 L/minute, blood work, a chest radiograph, a 12-lead electrocardiogram (ECG), and 2 mg of morphine sulfate given intravenously. The nurse should first: a. Administer the morphine b. Obtain a 12-lead ECG c. Obtain the blood work d. Order the chest radiograph 2. When administering a thrombolytic drug to the client experiencing an MI, the nurse explains to him that the purpose of the drug is to: a. Help keep him well hydrated b. Dissolve clots that he may have c. Prevent kidney failure d. Treat potential cardiac dysrhythmias 3. If the client who has admitted for MI develops cardiogenic shock, which characteristic signs should the nurse expect to observe? a. Oliguria b. Bradycardia c. Elevated blood pressure d. Fever 4. The physician orders continuous intravenous nitroglycerin infusion for the client with MI. essential nursing action include which of the following? a. Obtaining an infusion pump for the medication b. Monitoring blood pressure every 4 hours c. Monitoring urine output hourly d. Obtaining serum potassium levels daily 5. When teaching the client with MI, the nurse explains that the pain associated with MI is caused by: a. Left ventricular overload b. Impending circulatory collapse c. Extracellular electrolyte imbalances d. Insufficient oxygen reaching the heart muscle 6. Aspirin is administered to the client experiencing an MI because of its: a. Antipyretic action b. Antithrombotic action c. Antiplatelet action d. Analgesic action 7. While caring for a client who has sustained an MI, the nurse notes eight PVCs in 1 minute on the cardiac monitor. The client is receiving an intravenous infusion of 5% dextrose in water and oxygen at 2 L/minute. The nurse’s first course of action should be to: a. Increase the intravenous infusion rate b. Notify the physician promptly c. Increase the oxygen concentration d. Administer a prescribed analgesic 8. Which of the following is an expected outcome for a client on the second day of hospitalization after an MI? The client: a. Has minimal chest pain b. Can identify risk factors for MI c. Agrees to participate in a cardiac rehabilitation program d. Can perform personal self-care activities without pain 9. When teaching a client about the expected outcomes after intravenous administration of furosemide, the nurse would include which outcome? a. Increased blood pressure b. Increased urine output c. Decreased pain d. Decreased PVCs 10. After an MI, the hospitalized client is taught to move the legs about while resting in bed. This type of exercise is recommended primarily to help: a. Prepare the client for ambulation b. Promote urinary and intestinal elimination c. Prevent thrombophlebitis and blood clot formation d. Decrease the likelihood of decubitus ulcer formation 11. Which of the following reflects the principle on which a client’s diet will most likely be based during the acute phase of MI? a. Liquids as desired b. Small, easily digested meals c. Three regular meals per day d. Nothing by mouth 12. Of the following controllable risk factors for coronary artery disease (CAD) appears most closely linked to the development of the disease? a. Age b. Medication usage c. High cholesterol levels d. Gender 13. Which of the following is an uncontrollable risk factor that has been linked to the development of CAD? a. Exercise b. Obesity c. Stress d. Heredity 14. If a client displays risk factors for CAD such as smoking cigarettes, eating a diet high in saturated fat, or leading a sedentary lifestyle, technique of behavior modification may be used to help the client change behavior. The nurse can best reinforce new adaptive behaviors by: a. Explaining how the old behavior leads to poor health b. Withholding praise until the new behavior is well established c. Rewarding the client whenever the acceptable behavior is performed d. Instilling mild fear into the client to extinguish the behavior 15. Alteplase recombinant. Or tissue plasminogen activator (t-PA), a thrombolytic enzyme, is administered during the first 6 hours after onset of MI to: a. Control chest pain b. Reduce coronary artery vasospasm c. Control the dysrhythmias associated with MI d. Revascularize the blocked coronary artery 16. After the administration of t-PA, the nurse understands that a nursing assessment priority is to: a. Observe the client for chest pain b. Monitor for fever c. Monitor the 12-lead ECG every 4 hours d. Monitor breath sounds 17. When monitoring a client who is receiving t-PA, the nurse understands it is important to monitor vital signs and have resuscitation equipment available because reperfusion of the cardiac tissue can result in which of the following? a. Cardiac dysrhythmias b. Hypertension c. Seizure d. Hypothermia 18. Contraindication to the administration of t-PA include which of the following? a. Age greater than 60 years b. History of cerebral hemorrhage c. History of heart failure d. Cigarette smoking 19. A client has driven himself into the emergency room. He is 50 years old, has a history of hypertension, and informs the nurse that his father died from a heart attack at 60 years of age. The client is presently complaining of indigestion. The nurse connects him to an ECG monitor and begins administering oxygen at 2 L/minute per nasal cannula. The nurse’s next action would be to: a. Call for the doctor b. Start an intravenous line c. Obtain a portable chest radiograph d. Draw blood for laboratory studies 20. Crackles heard on lung auscultation indicate which of the following? a. Cyanosis b. Bronchospasm c. Airway narrowing d. Fluid-filled alveoli 21. A 68-year-old female client on day 2 after hip surgery has no cardiac history but starts to complain of chest heaviness. The first nursing action should be to: a. Inquire about the onset, duration, severity, and precipitating factors of the heaviness b. Administer oxygen via nasal cannula c. Offer pain medication for the chest heaviness d. Inform the physician of the chest heaviness 22. The nurse receives emergency laboratory results for a client with chest pain and immediately informs the physician. An increased myoglobin level suggests which of the following? a. Cancer b. Hypertension c. Liver disease d. Myocardial damage 23. An older, sedentary adult may not respond to emotional or physical stress as well as a younger individual because of: a. Left ventricular atrophy b. Irregular heart beats c. Peripheral vascular occlusion d. Pacemaker placement 24. A 69-year-old woman has a history of heart failure. She is admitted to the emergency department with heart failure complicated by pulmonary edema. On admission of this client, which of the following should be assessed first? a. Blood pressure b. Skin breakdown c. Serum potassium d. Urine output 25. In which of the following should the nurse place a client with suspected heart failure? a. Semi-sitting (Low Fowler’s position) b. Lying on the right side (Sims’ position) c. Sitting almost upright (High Fowler’s position) d. Lying on the back with the head lowered (Trendelenburg position) 26. Which of the following would be a priority nursing diagnosis for the client with heart failure and pulmonary edema? a. Risk for infection related to line placements b. Impaired skin integrity related to pressure c. Activity intolerance related to imbalance between oxygen supply and demand d. Constipation related to immobility 27. The major goal of therapy for a client with heart failure and pulmonary edema would be to: a. Increase cardiac output b. Improve respiratory edema c. Decrease peripheral edema d. Enhance comfort 28. Digoxin is administered intravenously to a client with heart failure, primarily because the drug acts to: a. Dilate coronary arteries b. Increase myocardial contractility c. Decrease cardiac dysrhythmias d. Decrease electrical conductivity in the heart 29. Captopril, an antigiotensin-converting enzyme (ACE) inhibitor, may be administered to a client with heart failure because it acts as a: a. Vasopressor b. Volume expander c. Vasodilator d. Potassium-sparing diuretic 30. Furosemide is administered intravenously to a client with heart failure. How soon after administration should the nurse begin to see evidence of the drug’s desired effect? a. 5 to 10 minutes b. 30 to 60 minutes c. 2 to 4 hours d. 6 to 8 hours 31. The nurse teaches a client with heart failure to take oral Furosemide in the morning. The primary reason for this is to help: a. Prevent electrolyte imbalances b. Retard rapid drug absorption c. Excrete excessive fluids accumulated during the night d. Prevent sleep disturbances during the night 32. Clients with heart failure are prone to atrial fibrillation. During physical assessment, the nurse would suspect atrial fibrillation when palpation of the radial pulse reveals: a. Two regular beats followed by one irregular b. An irregular pulse rhythm c. Pulse rate below 60 bpm d. A weak, thready pulse 33. When teaching the client about complications of atrial fibrillation, the nurse understands that the complications can be caused by: a. Stasis of blood in the atria b. Increased cardiac output c. Decreased pulse rate d. Elevated blood pressure 34. The nurse should teach the client that signs of digitalis toxicity include which of the following? a. Skin rash over the chest and back b. Increased appetite c. Visual disturbances such as seeing yellow spots d. Elevated blood pressure 35. The nurse should be especially alert for signs and symptoms of digitalis toxicity if serum levels indicate that the client has a: a. Low sodium level b. High glucose level c. High calcium level d. Low potassium level 36. Which of the following foods should the nurse teach a client with heart failure to avoid or limit when following a 2-g sodium diet? a. Apples b. Tomato juice c. Whole wheat bread d. Beef tenderloin 37. To help maintain a normal blood serum level of potassium, the client receiving a loop diuretic should be encouraged to eat such foods as bananas, orange juice, and, a. Spinach b. Skimmed milk c. Baked chicken d. Brown rice 38. The nurse finds the apical impulses below the fifth intercostals space. The nurse suspects a. Left atrial enlargement b. Left ventricular enlargement c. Right atrial enlargement d. Right ventricular enlargement 39. The nurse is admitting a 69-year old man to the clinical unit. The client has a history of left ventricular enlargement. During the assessment the nurse notes +3 pitting edema of the ankles bilaterally. The client does not have chest pain. The nurse observes that the client does have dyspnea at rest. The nurse infers that the client may have a. Arteriosclerosis b. Congestive heart failure c. Chronic bronchitis d. Acute myocardial infarction 40. The nurse’s discharge teaching plan for the client with congestive heart failure would stress the significance of which of the following? a. Maintaining a high-fiber diet b. Walking 2 miles every day c. Obtaining daily weights at the same time each day d. Remaining sedentary for most of the day 41. A 70-year-old woman is scheduled to undergo mitral valve replacement for severe mitral stenosis and mitral regurgitation. Although the diagnosis was made during childhood, she did not have symptoms until 4 years ago. Recently, she noticed increased symptoms, despite daily doses of digoxin and furosemide. During the initial interview with the client, the nurse would most likely learn that the client’s childhood health history included: a. Chicken pox b. Poliomyelitis c. Rheumatic fever d. Meningitis 42. A client experiences some initial signs of excitation after having an intravenous infusion of lidocaine hydrochloride started. The nurse would assess that the client is demonstrating a typical adverse reaction to lidocaine hydrochloride when the client complains of: a. Palpitations b. Tinnitus c. Urinary frequency d. Lethargy 43. A woman with severe mitral stenosis and mitral regurgitation has a pulmonary artery catheter inserted. The physician orders pulmonary capillary wedge pressures. The purpose of this is to help assess the: a. Degree of coronary artery stenosis b. Peripheral arterial pressure c. Pressure from fluid within the left ventricle d. Oxygen and carbon dioxide concentrations in the blood 44. Which of the following signs and symptoms would most likely be found in a client with mitral regurgitation? a. Exertional dyspnea b. Confusion c. Elevated creatine phosphokinase concentration d. Chest pain 45. The nurse expects that a client with mitral stenosis would demonstrate symptoms associated with congestion in the: a. Aorta b. Right atrium c. Superior vena cava d. Pulmonary circulation 46. Because a client has mitral stenosis and is a prospective valve recipient, the nurse preoperatively assesses the client’s past compliance with medical regimens. Lack of compliance with which of the following regimens would pose the greatest health hazard to this client? a. Medication therapy b. Diet modification c. Activity restrictions d. Dental care 47. In preparing the client and the family for a postoperative stay in the intensive care unit after open heart surgery, the nurse should explain that: a. The client will remain in the intensive care unit for 5 days b. The client will sleep most of the time while in the intensive care unit c. Noise and activity within the intensive care unit are minimal d. The client will receive medication to relieve pain 48. A client who has undergone a mitral valve replacement experiences persistent bleeding from the surgical incision during the early postoperative period. Which of the following pharmaceutical agents should the nurse be prepared to administer to this client? a. Vitamin C b. Protamine sulfate c. Quinidine sulfate d. Warfarin sodium (Coumadin) 49. The most effective measure the nurse can use to prevent wound infection when changing a client’s dressing after coronary artery bypass surgery is to: a. Observe careful handwashing procedures b. Cleanse the incisional area with an antiseptic c. Use prepackaged sterile dressings to cover the incision d. Place soiled dressings in a waterproof bag before disposing of them 50. For a client who excretes excessive amounts of calcium during the postoperative period after open surgery, which of the following measures should the nurse institute to help prevent complications associated with excessive calcium excretion? a. Ensure a liberal fluid intake b. Provide an alkaline-ash diet c. Prevent constipation d. Enrich the client’s diet with dairy products 51. The nurse teaches the client who is receiving warfarin sodium that: a. Partial thromboplastin time values determine the dosage of warfarin sodium b. Protamine sulfate is used to reverse the effects of warfarin sodium c. The international normalized ration (INR) is used to assess effectiveness d. Warfarin sodium will facilitate clotting of the blood 52. Good dental care is an important measure in reducing risk of endocarditis. A teaching plan to promote good dental care in a client with mitral stenosis should include demonstration of the proper use of: a. A manual toothbrush b. An electric toothbrush c. An irrigation device d. Dental floss. 53. Before a client’s disease discharge after mitral valve replacement surgery, the nurse should evaluate the client’s understanding of postsurgery activity restrictions. Which of the following should the client not engage in until after the 1-month-old postdischarge appointment with the surgeon? a. Showering b. Lifting anything heavier than 10 pounds c. A program of gradually progressive walking d. Light housework 54. Three days after mitral valve surgery, a 45-year-old woman comments that she hears a “ clicking” noise coming from her chest and her “ rather large” chest incision. The nurse’s response should reflect the understanding that the client may be experiencing which of the following? a. Anxiety related to altered body image b. Anxiety related to altered health status c. Altered tissue perfusion d. Lack of knowledge regarding the postoperative course 55. An industrial health nurse at a large printing plant finds a male employee’s blood pressure to be elevated on two occasions 1 month apart and refers him to his provide physician. The employee is about 25 pounds overweight and has smoked a pack of cigarettes daily for more than 20 years. The client’s physician prescribes atenolol for the hypertension. The nurse should instruct the client to: a. Avoid sudden discontinuation of the drug b. Monitor the blood pressure annually c. Follow a 2-g sodium diet d. Discontinue the medication if severe headaches develop 56. The nurse teaches her client, who has recently been diagnosed with hypertension, about his dietary restrictions: a low-calorie, low-fat, low-sodium diet. Which of the following menu selections would best meet the client’s? a. Mixed green salad with blue cheese dressing, crackers, and cold cuts b. Ham sandwich on rye bread and an orange c. Baked chicken, an apple, and a slice of white bread d. Hot dogs, baked beans, and celery and carrot sticks 57. A client’s job involves working in a warm, dry room, frequently bending and crouching to check the underside of a high-speed press, and wearing eye guards. Given this information, the nurse should assess the client for which of the following? a. Muscle aches b. Thirst c. Lethargy d. Postural hypotension 58. An exercise program is prescribed for the client with hypertension. Which intervention would be most likely to assist the client in maintaining an exercise program? a. Giving the client a written exercise program. b. Explaining the exercise program to the client’s spouse. c. Reassuring the client that he or she can do the exercise program. d. Tailoring a program to the client’s needs and abilities.. 59. The client realizes the importance of quitting smoking, and the nurse develops a plan to help the client achieve this goal. Which of the following nursing interventions should be the initial step in this plan? a. Review the negative effects of smoking on the body. b. Discuss the effects of passive smoking on environmental pollution. c. Established the client’s smoking pattern. d. Explain how smoking worsens high blood pressure. 60. Essential Hypertension would be diagnosed in a 40-year-old man whose blood pressure readings were consistently at or above which of the following? a. 120/90 mmHg b. 130/85 mmHg c. 140/90 mmHg d. 160/80 mmHg 2. greater than 90 mmHg. . When teaching a client about propranolol hydrochloride, the nurse should base the information on the knowledge that propranolol hydrochloride a. Blocks beta-adrenergic stimulation and thus causes decreased heart rate, myocardial contractility, and conduction. b. Increases norepinephrine secretion and thus decreases blood pressure and heart rate. c. Is a potent arterial and venous vasodilator that reduces peripheral vascular resistance and lowers blood pressure. d. Is an angiotensin-converting enzyme (ACE) inhibitor that reduces blood pressure by blocking the conversion of angiotensin I to angiotensin II. 2. The nurse understands that a priority nursing diagnosis for the client with hypertension would be a. Pain. b. Deficient Fluid Volume. c. Impaired skin integrity. d. Ineffective health maintenance. 3. The most important long-term goal for a client with hypertension would be to a. Learn how to avoid stress. b. Explore a job change or early retirement. c. Make a commitment to long-term therapy. d. Control high blood pressure. 4. The client with hypertension is prone to long-term complications of the disease. Which of the following is a long-term complication of hypertension? a. Renal insufficiency and failure. b. Valvular heart disease. c. Endocarditis d. Peptic ulcer disease. 5. Hypertension is known as the silent killer. This phrase is associated with the fact that hypertension often goes undetected until symptoms of other system failures occur. This may occur in the form of a. Cerebrovascular accidents (CVA’s) b. Liver disease. c. Myocardial infarction. d. Pulmonary disease. 6. During the past few months, a 56-year old woman has felt brief twinges of chest pain while working in her garden and has had frequent episodes of indigestion. She comes to the hospital after experiencing severe anterior chest pain while raking leaves. Her evaluation confirms a diagnosis of stable angina pectoris. After stabilization and treatment, the client is discharged from the hospital. At her follow-up appointment, she is discouraged because she is experiencing pain with increasing frequency. She states that she visits an invalid friend twice a week and now cannot walk up the second flight of steps to the friend’s apartment without pain. Which of the following measures that the nurse could suggest would most likely help the client deal with this problem? a. Visit her friend b. Rest for at least an hour before climbing the stairs c. Take a nitroglycerin tablet before climbing the stairs. d. Lie down once she reaches the friend’s apartment. 7. The client who experiences angina pectoris has been told to follow a low-cholesterol diet. Which of the following meals should the nurse tell the client would be best on her low –cholesterol diet? a. Hamburger, salad, and milkshake. b. Baked liver, green beans, and coffee. c. Spaghetti with tomato sauce, salad, and coffee d. Fried chicken, green beans, and skim milk 8. Which of the following symptoms should the nurse teach the client with unstable angina to report immediately to her physician? a. A change in the pattern of her pain b. Pain during sexual activity c. Pain during an argument with her husband d. Pain during or after an activity such as lawn mowing 9. The physician refers the client with unstable angina for a cardiac catheterization. The nurse explains to the client that this procedure is being used in this specific case to: a. Open and dilate blocked coronary arteries b. Assess the extent of arterial blockage c. Bypass obstructed vessels d. Assess the functional adequacy of the valves and heart muscle 10. The client is scheduled for a percutaneous transluminal coronary angioplasty (PTCA) to treat angina. Priority goals for the client immediately after PTCA would include: a. Minimizing dyspnea b. Maintaining adequate blood pressure control c. Decreasing myocardial contractility d. Preventing fluid volume deficit 11. Which of the following is not generally considered to be a risk factor for the development of atheroclerosis? a. Family history of early heart attack b. Late onset of puberty c. Total blood cholesterol level greater than 220 mg/dL d. Elevated fasting blood sugar concentration 12. Many more men than women younger than 50 years of age have coronary artery disease as a result of atherosclerosis. The leading cause of death in women is: a. Acquired immunodeficiency syndrome b. Breast cancer c. Coronary artery disease d. Chronic obstructive pulmonary disease . 13. A client angina asks the nurse, “ What information does an ECG provide?” The nurse would respond that an electrocardiogram (ECG) primarily gives information about the: a. Electrical conduction of the myocardium b. Oxygenation and perfusion of the heart c. Contractile status of the ventricles d. Physical integrity of the heart muscle 14. As an initial step in treating a client with angina, the physician prescribes nitroglycerin tablets, 0.3 mg given sublingually. This drug’s principal effects are produced by: a. Antispasmodic effects on the pericardium b. Causing an increased myocardial oxygen demand c. Vasodilation of peripheral vasculature d. Improved conductivity in the myocardium . 15. The nurse teaches the client with angina about the common expected side effects of nitroglycerin, including: a. Headache b. High blood pressure c. Shortness of breath d. Stomach cramps 16. Sublingual nitroglycerin tablets begin to work within 1 to 2 minutes. How should the nurse instruct the client to use the drug when chest pain occurs? a. Take one tablet every 2 to 5 minutes until the pain stops b. Take one tablet and rest for 10 minutes. Call the physician if pain persists after 10 minutes c. Take one tablet, then an additional tablet every 5 minutes for a total of three tablets. Call the physician if pain persists after these tablets d. Take one tablet. If pain still persists 5 minutes later, call the physician 17. A client with angina has been taking nifedipine. The client should be taught to: a. Monitor blood pressure monthly b. Perform daily weights c. Inspect gums daily d. Limit intake of green leafy vegetables 18. A 74-year-old woman is admitted to the telemetry unit for placement of a permanent pacemaker would be to: a. Maintain skin integrity b. Maintain cardiac conduction stability c. Decrease cardiac output d. Increase activity level 19. The client who had a permanent pacemaker implanted 2 days earlier is being discharged from the hospital. Outcome criteria include that the client: a. Selects a low-cholesterol diet to control coronary artery disease b. States a need for bed rest for 1 week after discharge c. Verbalizes safety precautions needed to prevent pacemaker malfunction d. Explain sign and symptoms of myocardial infraction The Client Requiring Cardiopulmonary Resuscitation 20. A rescuer is called to a neighbor’s home after a 56-year-old man collapses. After quickly assessing the victim, the rescuer determines that the victim is unresponsive. To determine unresponsiveness, the rescuer can: a. Call the victim’s name and gently shake the victim b. Perform the chin-tilt to open the victim’s airway c. Feel for any air movement from the victim’s nose or mouth d. Watch the victim’s chest for respirations 21. Proper hand placement for chest compressions during cardiopulmonary resuscitation (CPR) is essential to reduce the risk of which of the following complications? a. Gastrointestinal bleeding b. Myocardial infraction c. Emesis d. Rib fracture 22. The American Heart Association guidelines urge greater availability of automated external defibrillators (AEDs) and people trained to use them. AEDs are used in cardiac arrest situations for: a. Early defibrillation in cases of atrial fibrillation b. Cardioversion in cases of atrial fibrillation c. Pacemaker placement d. Early defibrillation in cases of ventricular fibrillation 23. A client who has been given CPR is transported by ambulance to the hospital’s emergency department, where the admitting nurse quickly assesses the client’s condition. Of the following observations, the one most often recommended for determining the effectiveness of CPR is noting whether the: a. Pulse rate is normal b. Pupils are reacting to light c. Mucous membranes are pink d. Systolic blood pressure is at least 80 mmHg 24. The client receives epinephrine during resuscitation in the emergency department. This drug is administered primarily because of its ability to: a. Dilate bronchioles b. Constrict arterioles c. Free glycogen from the liver d. Enhance myocardial contractility 25. The rescuer understands that the compression-to-ventilation ratio for one-rescuer adult CPR is: a. 5:1 b. 15:1 c. 5:2 d. 15:2 26. During CPR, the xiphoid process at the lower end of the sternum should not be compressed when performing cardiac compressions. Which of the following organs would be most likely at risk for laceration by forceful compressions over the xiphoid process? a. Lung b. Liver c. Stomach d. Diaphragm 27. When performing external chest compressions on an adult during CPR, the rescuer should depress the sternum. a. 0.5 to 1 inch b. 1 to 1.5 inches c. 1.5 to 2 inches d. 2 to 2.5 inches 28. The American Heart Association guidelines for Basic Cardiac Life Support recommend that the rescuer after first establishing unresponsiveness, should: a. Perform CPR for 2 minutes on the adult victim then place a call for emergency assistance b. Place a call for emergency assistance immediately c. Begin rescue breathing for the victim d. Begin CPR on the adult victim and wait until help comes on the scene 29. If the victim’s chest wall fails to rise with each inflammation when rescue breathing is administered during CPR, the most likely reason is that the: a. Airway is not opened properly b. Victim is beyond resuscitation c. Inflations are being given at too rapid a rate d. Rescuer is using inadequate force for cardiac compression 30. During rescue breathing in CPR, the victim with exhale by: a. Normal relaxation of the chest b. Gentle pressure of the rescuer’s hand on the upper chest c. The presence of cardiac compressions d. Turning the head to the side 1. If parents or legal guardians aren't available to give consent for treatment of a life-threatening situation in a minor child, which of the following statements is most accurate? a.)Consent may be obtained from a neighbor or close friend of the family. b.)Consent may not be needed in a life-threatening situation. c.)Consent must be in the form of a signed document; therefore, parents or guardians must be contacted. d.)Consent may be given by the family physician. 2. You're admitting a 15-month-old boy who has bilateral otitis media and bacterial meningitis. Which room arrangements would be best for this client? a.)In isolation off a side hallway b.)A private room near the nurses' station c.)A room with another child who also has meningitis d.)A room with two toddlers who have croup 3. Which of the following points should a team leader consider when delegating work to team members in order to conserve time? a.)Assign unfinished work to other team members. b.)Explain to each team member what needs to be done. c.)Relinquish responsibility for the outcome of the work. d.)Assign each team member the responsibility to obtain dietary trays. 4. The nurse is caring for a client admitted to the emergency department after a motor vehicle accident. Under the law, the nurse must obtain informed consent before treatment unless: a.)the client is mentally ill. b.)the client refuses to give informed consent. c.)the client is in an emergency situation. d.)the client asks the nurse to give substituted consent. 5. The nurse is assigned to care for an elderly client who is confused and repeatedly attempts to climb out of bed. The nurse asks the client to lie quietly and leaves her unsupervised to take a quick break. While the nurse is away, the client falls out of bed. She sustains no injuries from the fall. Initially, the nurse should treat this occurrence as: a.)a quality improvement issue. b.)an ethical dilemma. c.)an informed consent problem. d.)a risk-management incident. 6. The nurse receives an assignment to provide care to 10 clients. Two of them have had kidney transplantation surgery within the last 36 hours. The nurse feels overwhelmed with the number of clients. In addition, the nurse has never cared for a client who has undergone recent transplantation surgery. What's the appropriate action for the nurse to take? a.)Speak to the manager and document in writing all concerns related to the assignment. b.)Refuse the assignment. c.)Ignore the assignment and leave the unit. d.)Trade assignments with another nurse. 7. The nurse works with a colleague who consistently fails to use standard precautions or wear gloves when caring for clients. The nurse calls the colleague's attention to these oversights. The colleague tells the nurse that standard precautions and gloves aren't necessary unless the client is known to have tested positive for the human immunodeficiency virus. What's the most appropriate action for the nurse to take? a.)Ignore it because it isn't directly the nurse's problem b.)Document the problem in writing for the manager. c.)Talk to other staff members to ascertain their practices. d.)Instruct the clients to remind this colleague to wear gloves. 8. An adult client is diagnosed with acquired immunodeficiency syndrome. The nurse who is caring for the client is also his friend. The nurse tells the client's parents about the diagnosis; after all, they know their son is the nurse's friend. Several weeks later, the nurse receives a letter from the client's attorney stating that the nurse has committed an intentional tort. Which intentional tort has this nurse committed? a.)Fraud b.)Defamation of character c.)Assault and battery d.)Breach of confidentiality 9. A nurse accidentally administers 40 mg of propranolol (Inderal) to a client instead of 10 mg. Although the client exhibits no adverse reactions to the larger dose, the nurse should: a.)call the facility's attorney. b.)inform the client's family. c.)complete an incident report. d.)do nothing because the client's condition is stable. 10. The nurse is assigned to care for a postoperative client who has diabetes mellitus. During the assessment interview, the client reports that he's impotent and says that he's concerned about its effect on his marriage. In planning this client's care, the most appropriate intervention would be to: a.)encourage the client to ask questions about personal sexuality. b.)provide time for privacy. c.)provide support for the spouse or significant other. d.)suggest referral to a sex counselor or other appropriate professional. 11. The nurse is assigned to care for eight clients. Two nonprofessionals are assigned to work with the nurse. Which statement is valid in this situation? a.)The nurse may assign the two nonprofessionals to work independently with a client assignment. b.)The nurse is responsible to supervise assistive personnel. c.)Nonprofessionals aren't responsible for their own actions. d.)Nonprofessionals don't require training before they work with clients. 12. Each state has guidelines that regulate the different levels of nursing & licensed practical or vocational nurse, registered nurse, or advanced practice nurse. Legal guidelines outlining the scope of practice for nurses are known as: a.)consent to treatment. b.)client's bill of rights. c.)nurse practice acts. d.)licensure requirements. 13. A client is dissatisfied with his hospitalization. He decides to leave against medical advice and refuses to sign the paperwork. The nurse's next course of action is to: a.)detain him until he signs the paperwork. b.)detain him until his physician arrives. c.)call security for assistance. d.)let him leave. 14. A nurse needs assistance transferring an elderly, confused client to bed. The nurse leaves the client to find someone to assist her with the transfer. While the nurse is gone, the client falls and hurts herself. The nurse is at fault because she hasn't: a.)properly educated this client about safety measures. b.)restrained the client. c.)documented that she left the client. d.)arranged for continual care of the client. 15. When prioritizing a client's care plan based on Maslow's hierarchy of needs, the nurse's first priority would be: a.)allowing the family to see a newly admitted client. b.)ambulating the client in the hallway. c.)administering pain medication. d.)placing wrist restraints on the client. 16. When developing a therapeutic relationship with a client, the nurse should begin preparing the client for termination of the relationship: a.)at discharge. b.)during the first meeting. c.)at the midpoint of the relationship. d.)when the client demonstrates the ability to function independently. 17. To be effective, a clinical nurse-manager in a managed care environment must: a.)expect all staff to accept change. b.)go along with a proposed change. c.)be a catalyst for change. d.)document staff nurses' reactions to change. 18. In community-based nursing, primary responsibility for decisions related to health care belongs to the: a.)nurse. b.)client. c.)health care team. d.)physician. 19. A client became seriously ill after a nurse gave him the wrong medication. After his recovery, he files a lawsuit. Who is most likely to be held liable? a.)No one because it was an accident b.)The hospital c.)The nurse d.)The nurse and the hospital 20. The nurse is providing care for a client who underwent mitral valve replacement. The best example of a measurable client outcome goal is to: a.)change his own dressing. b.)walk in the hallway. c.)walk from his room to the end of the hall and back before discharge. d.)eat a special diet. 21. A client with end-stage liver cancer tells the nurse he doesn't want extraordinary measures used to prolong his life. He asks what he must do to make these wishes known and legally binding. How should the nurse respond to the client? a.)Tell him that it's a legal question beyond the scope of nursing practice. b.)Give him a copy of the client's bill of rights. c.)Provide information on active euthanasia. d.)Discuss documenting his wishes in an advance directive. 22. While admitting a client with pneumonia, the nurse notes multiple bruises in various stages of healing. The client has Alzheimer's disease and a history of multiple fractures. Legally, the most important action for the nurse to take is to: a.)document findings thoroughly. b.)question the client about the bruising. c.)inform appropriate local authorities. d.)tell the client's physician. 23. The nurse is providing care for a client with multiple myeloma, a disorder characterized by episodes of remissions and exacerbations. Which resource can best help the client adapt to the disease? a.)The client's family b.)Pastoral care c.)Support group .)Hospice care 24. A client with brain cancer is deteriorating and the prognosis is poor. The client meets brain-death criteria. Which nursing intervention is most appropriate at this time? a.)Approach the client's family about organ donation. b.)Make the decision to withdraw life support. c.)Sedate the client. d.)Talk to the staff about their feelings. 25. A client is scheduled to have a descending colostomy. He's very anxious and has many questions concerning the surgical procedure, care of a stoma, and lifestyle changes. It would be most appropriate for the nurse to make a referral to which member of the health care team? a.)Social worker b.)Registered dietitian c.)Occupational therapist d.)Enterostomal nurse therapist 26. A 92-year-old client with prostate cancer and multiple metastases is in respiratory distress and is admitted to a medical unit from a skilled nursing facility. His advance directive states that he doesn't want to be placed on a ventilator or receive cardiopulmonary resuscitation. Based on the client's advance directive, which intervention should the nursing care plan include? a.)Check on the client once per shift. b.)Provide mouth and skin care only if the family requests it. c.)Turn the client only if he's uncomfortable. d.)Provide emotional support and pain relief. 27. The registered nurse has an unlicensed assistant working with her for the shift. When delegating tasks, the registered nurse understands that the unlicensed assistant: a.)interprets clinical data. b.)collects clinical data. c.)is trained in the nursing process. d.)can function independently. 28. A nurse on a medical-surgical floor is making assignments for an 8-hour shift. Which of the following considerations has the highest priority? a.)Complexity of care required b.)Age of the clients c.)Skills of the assigned personnel d.)The number of clients 29. The nurse is caring for a homeless client with active tuberculosis. The client is almost ready for discharge; however, the nurse is concerned about the client's ability to follow the medical regimen. Which intervention will best ensure that the client complies with treatment? a.)Referring the client to a social worker for discharge planning b.)Providing individualized client education c.)Having the client attend a formal education session d.)Attempting to contact a member of the client's family to provide assistance 30. The nurse is following a critical pathway to help a client who underwent hip replacement surgery meet specific objectives. What's a critical pathway? a.)A nursing care plan that helps the nurse to decide which intervention to perform first b.)A multidisciplinary care plan that helps the nurse to use a variety of critical interventions c.)A standardized care plan that lists basic interventions for the nurse to use with every client d.)A clinical management tool that organizes the major interventions for a multidisciplinary health care team 1. Thiamine has been prescribed for an alcoholic patient. The rationale for administration of this medication is the prevention of: a. Alcoholic dementia b. Huntington’s disease c. Wernicke-korsakoff syndrome d. Alcohol withdrawal syndrome 2. When caring for a patient with organic brain disorder, the nurse evaluates outcomes by: a. The emotional and financial support of a family b. The elimination of antipsychotic medications c. Maintenance of optimal level functioning d. How safety the patient performs ADLs 3. The patient is experiencing a fixed, false vbelief that cannot be corrected by logical reasoning. This is a/an: a. Delusion b. Hallucination c. Illusion d. Symbolism 4. A patient complains that he cannot get rid of the idea that harm is looming all around him. The thought comes, unbidden, and upsets him. This repeated, unbidden thought is a/an: a. Obsession b. Compulsion c. Delusion d. Illusion 5. An acutely patient is screaming, “I’m dead; I’m dying; my body is greeting stiff.” The nurse attempts to refocus on reality by stating to the patient: a. “You are very upset. Let me help you” b. “That’s hard to believe c. “Why do you keep saying that?” d. “You’re not dead. Your heart is still beating.” 6. In planning care for the patient with a personally disorder, the nurse realizes that this patient will most likely. a. Not need long-term therapy b. Will not require medication c. Require anti-anxiety medication d. Resist any change in behavior 7. To understand the meaning of the cleaning rituals the nurse must realize: a. The patient cannot help herself b. The patient cannot change c. Rituals relieve intense anxiety d. Medications cannot help 8. The nursing assessment indicates the patient is creating new words. This is documented as: a. Cryptic language b. Magical thinking c. Loose associations d. Neologisms 9. You have been working with a nine-year-old client, and his parents, to help him stop sucking his thumb. Each time he sucks his thumb, you note it on the chart, and he does not get to have his next dessert. When he no longer sucks most thumbs, you evaluate his thumb-sucking behavior as most likely. a. Reinforced b. Faded c. Extinguished d. Generalized 10. Shaping of behavior occurs when: a. Reinforcement is directed toward a desired is achieved b. Behavior is separated in situations similar to the originally reinforced situation c. The client changes behavior d. Learning of appropriate behavior is achieved 11. A patient has been given a diagnosis of Neuroleptic Malignant Syndrome (NMS). What would the movement plan include? a. Monitor temperature and blood pressure b. Administer neulroeptic medications c. Encourage mild activity d. Increase antipsychotic medication 12. In providing supportive therapy to the depressed patient, the nurse is aware that depression is often caused by the repression of: a. Anxiety b. Anger c. Fear d. Grief 13. One morning, the patient says to the nurse.” I do love my mother, but sometimes I wish she would just go ahead and die.” This statement reflects feelings of: a. Conversion b. Ambivalence c. Anxiety d. Conflict 14. A priority nursing intervention initially with this patient is to: a. Help her substitute feeling for her mother b. Encourage her to find other interests c. Develop a trusting relationship with her d. Tell her to forget the past 15. A patient with Organic Brain Syndrome (OBS) is confused at night. The plan of care should include: a. Keep the room well lighted b. Keep sensory stimulation to a minimum c. Offer a sedative at about 10 p.m d. Always use physical restraints 16. When a patient freely expresses his feelings, thoughts, anxieties and gets a sense of emotional relief. This experience is termed: a. Revelation b. Déjà vu c. Catharsis d. Projection 17. A suspicious patient says, “Its not for us to talk in the hospital. They are everything.” The nurse responds: a. “Don’t worry about it. It is safe here.” b. “Don’t be silly. We could see the recorders if they were here.” c. “Who told you that you are being recorded?” d. “You appear to be stressed. Let’s take a walk.” 18. A patient is staying in his room very quite and withdrawn. The nurse approaches the patient and say: a. “I’ve noticed that you have been very quiet.” b. “Get out and join the others.” c. You are suicidal today, aren’t you?” d. “The doctor won’t like you staying secluded.” 19. A patient speaks in a whisper. The nurse replies: a. “I cannot hear you. Please speak more loudly.” b. “Are you saying something?” c. “Why aren’t you talking right?” d. “Are you afraid someone is listening?” 20. A patient complains,” My sister always hated me. She was jealous.” The nurse respond: a. “Your sister was jealous?” b. “Tell me about on e of the times she was jealous.” c. “Why was she so hate full and jealous?” d. “Mother are often jealous and teach their daughters.” 21. While teaching the patient the nurse explains the purpose of antipsychotic drugs. These medications have been proven to be effective in: a. Curing symptoms b. Controlling symptoms c. Preventing psychosis d. Curing mental illness 22. The nursing interventions most effective in working with substances patient are: a. Firm and Directive b. Instillation of values c. Helpful and advisory d. Subjective and non-judgmental 23. The nurse promptive reports which symptom when the patient is taking psychotic medications? a. Mild rash b. Dry mouth c. Sore throat d. Photosensitivity 24. A very angry patient is threatening to leave the hospital AMA. What action should be taken? a. Let him check out of the hospital b. Inform him of the consequences of leaving AMA c. Tell him that no one is allowed to leave the hospital d. Put the patient in restraints until the physician comes 25. A 79-year-old patient spends a lot of time just talking about the past. What action is appropriate regarding their behavior? a. Get him involved with others his age b. Tell him he should talk about current events c. Reorient him to present and ignore past d. Listen attentively and encourage talking 26. A patient is masturbating in his room. There is no one present. The nurse should: a. Ask the patient to stop at once b. Sternly criticize the patient’s behavior c. Threaten to tell the doctor if he doesn’t stop d. Quietly leave, allow the behavior 27. A patient states, “I am a bird, you know, rat, cat, no one knows. He, That it.” This is an example of: a. Word salad b. Associate looseness c. Flight of ideas d. Cognitive distortion 28. The best response to a patient who is verbalizing words that cannot be understood is: a. “You are not making sense.” b. “Go on says what you really mean.” c. “Say that so I can understand.” d. “Please repeat yourself.” 29. Maslow see the individual being capable of reaching a peak capacity of fulfilling his human potential and of being satisfied with this no matter what it is. Maslow called this peak experience: a. Homeostesis b. Alarm reaction c. Existentialism d. Self-actualization 30. In attempting to control a patient who is suffering panic, the nursing priority is: a. Provide safety b. Hold the patient c. Describe crisis in detail d. Demonstrate ADLs frequently 31. The patient states, “ I want to talk about elusive bombardment.” The nurse respond: a. “You don’t know what you are talking about.” b. “Just what is elusive bombardment.” c. “Tell me more about this.” d. “Where did you study that?” 32. The nurse-therapies utilizing cognitive therapy in working with a 35-year-old woman diagnosed with depression. The focus of his approach to therapy is to: a. Learn to intellectualize feelings b. Learn to focus on thought, not feeling c. Replace concrete thinking with abstract d. Replace irrational, negative thinking 33. A patient is constantly complaining with a variety of vague aches and pains. A physical exam shows no reason for her symptoms. The nurse: a. Explains that she is not all b. Encourage her to talk c. Gives her sympathy 34. During a family therapy session, the family is complaining about excessive bickering at mealtimes. The nurse instructs them to engage in bickering for the minutes at the beginning of each meal. This therapeutic techniques is: a. Self- disclosure b. Paradoxical intervention c. Friendly confrontation d. Family collaboration 35. The nurse is teaching new parents about parenting skills. She explains that a child’s mental health is best promoted by: a. Material goods b. Parents who stay together c. Unconditional love d. Strict discipline 36. After several meetings, then nurse realizes that she has not been able to establish a therapeutic relationship with the patient. What action should be a priority in this situation? a. Refer the patient to another nurse or another unit b. Do a self-assessment on interactions with the patient c. Limit the amount of time with this particular patient d. Ask the unit manager to change nursing assignment 37. For patient in group therapy, the goal is: a. Exchanging information and ideas b. Developing insight by relating to others c. Learning that everyone has problems d. Identifying with other group members e. All of the above 38. A 76-year-old man is sobbing and is quite agitated following the death of his wife from cancer just 6 hours ago. He is not following anyone to talk with or comfort him. He repeats, “I can’t go on without her. I don’t know what I am going to do.” The nurse includes in the plan of care: a. Nutritional needs b. Sleep and rest c. Calling family members d. Suicide precautions 39. A 19-year-old female has been diagnosed with bulimia and is hospitalized. The nurse enters the room when the patient’s mothers is visiting and asks the patient a question. The mother interrupts as her daughter begins to answer, and the mother answers for her. The nurse should respond by saying: a. To the mother: “ Thank you. I think you are correct.” b. To the patient: “I would like for you to answer.” c. To the patient: “ Do you always let your mother speak for you?” d. To the patient: “ Do you agree with what your mother is saying?” Ans: B-This reply speaks directly to the patient, and elicits a direct response from the patient while indirectly implying to the mother not to answer. 40. The priority in working with a patient with a thought disorder is: a. Get him to understand what you’ve saying b. Get him to do his ADLs c. Reorient him to reality d. Administer antipsychotic medications 41. The nurse is taking a history on a female patient with migraine headaches. It is noted that the husband appears more attentive when the patient is complaining of headache pain. This attention may be assessed as a: a. Coping mechanism b. Caring behavior c. Secondary gain d. Positive reinforcement 42. The family is being taught the safety issues in taking care of the Alzheimer’s patient at home. I initiating the discharge planning, the nurse cautions: a. Medications should be avoided b. That nursing care is very expensive c. Self-care can be accomplished eventually d. Burn-out among family members is common 43. Frustrated parents of a 5-year-old boy are being taught new parenting skills. The man problem is that he throws temper tantrums when he does not get his way. When the parents reward him for handling his frustration in ways other than throwing a tantrum, this concept is called: a. Negative reinforcement b. Positive reinforcement c. Parental modeling d. Cognitive reinforcement 44. The nurse-therapist is utilizing cognitive therapy in working with 35-year-old woman diagnosed with depression. The focus of this approach to therapy is to: a. Learn to intellectualize feelings b. Learn to focus on thoughts, not feeling c. Replace concrete thinking with abstract d. Replace irrational, negative thinking 45. The function of encouraging communication and facilitating group interaction is accomplished by the: a. Contributor b. Hamonizer c. Gate-keeper d. Standard keeper. 46. The nurse is assessing a patient’s nonverbal behavior. Which is a priority in interpreting this behavior? a. Consider the usual meaning of the behavior b. Consider the patient’s cultural background c. Validate any perceptions with patient d. Consult best reference on nonverbal behavior. 47. The nurse finds a female patient crying in her room. The patient asks the nurse to leave. As the nurse lightly touches her shoulder, the nurse states, “ I would like to stay with you for a while.” The rationale for this action is: a. To show sympathy and understanding b. To show the patient how to help herself c. Convey empathy and a willingness to listen d. Find out what the patient is crying about. 48. A young adolescent patient is to be discharged in two days. He has been prescribed Haldol for hallucinations, and will be given a prescription when he goes home. Patient teaching regarding Haldol should begin: a. The day of discharge b. With the discharge summary c. Before the medication is administered d. Whenever the patient can come to the hospital 49. The patient diagnosed with schizophrenia exhibits an inappropriate affect and shows no interest in communicating with others. This is a part of the schizophrenia process called: a. Paranoia b. Delusions c. Loosening d. Ambivalence 50. The nurse is explaining why the family of the schizophrenia patient should participate in therapy. The focus of therapy is: a. Communication and interaction b. Explanation of medications c. Finding the identified patient d. Establishing boundaries 51. An alcoholic patient asks. “Is there any medication to help me get over this alcoholism?” Which drug may be prescribed? a. Xanax b. Librium c. Antabuse d. Catapres 52. In taking with the manipulative patient, the nurse realizes that she must set firm limits. This is particularly necessary because she realizes what this patient is attempting is to: a. Help b. Control c. Gain acceptance d. Be appreciated 53. The nurse is providing patient to the patient who has just diagnosed with major depression and prescribed amitriptyline (Elavil) 50 mg hs. The patient is instructed that medication will take effect. a. Immediately b. In about 36 hours c. In 14-21 days d. In about a month 54. In giving a patient information regarding psychotropic medications, the nurse stresses that the primary purpose of these medications is to: a. Cure most psychosis b. Modify learned behavior c. Provide missing chemicals d. Decrease psychotic symptoms 55. The patient asks the nurse, “What is this therapy for anyway. I just don’t understand it.” The best reply is: a. “It keeps you from being put on medications.” b. It helps you to change other in the family.” c. “The purpose of therapy is to help you change.” d. NO one but professionals can really understand it.”. 56. Blood levels are drawn on the patient who has been taking Lithium for about six months. The present level is 2.1 mEq/L. The nurse evaluate this level as: a. Therapeutic b. Below therapeutic c. Potentially dangerous d. Fatally toxic 57. A manipulative alcoholic patients asks the nurse to go out with him when he gets out of the hospital. She discusses her role and the importance of a therapeutic relationship with him. Which techniques is she implementing? a. Defining professionalism b. Telling him no politely c. Quietly reprimanding him d. Defining boundaries 58. While discussing his recent divorce, the nurse states to the patient,” I notice you become anxious when we start talking out your ex-wife.” What communication techniques is being implement? a. Confronting behavior b. Initiating awareness c. Initiating change d. Making an observation 59. The new patient states,” I just don’t understand this therapy business. What does it do anyway?” The nurse explains that the focus of the therapeutic process is: a. Identifying significant others as support system b. Therapist telling patient what he needs to do c. Recognizing needs and discovering ways to change d. Discovering goals in life 60. In working with a difficult patient, the nurse recognizes that transference is most likely to occur in which stages of therapy? a. Initial b. Working c. Termination d. Preorientation 61. The nursing staff notes that a patient is constantly seeking attention and approval from the staff and other patients. The care plan must address the problem of: a. Displacement b. Regression c. Manipulation d. Compensation 62. A 16-year-old girl states that she doesn’t get along with her mother,” I hate her for what she has done to me.” Then, a few minutes later she tells the therapist, “I can’t help but love my mother for all she has done form e.” The patient is exhibiting: a. Confusion b. Helplessness c. Manipulation d. Ambivalence 63. An adolescent,16, who has been diagnosed with schizophrenia, is boasting to peers that he doesn’t need an education or “anything else.” He keeps insisting that he can make a million dollars before he is twenty by creating his own business. He is exhibiting: a. Delusion thinking b. Unrealistic thinking c. Magical thinking d. Delusions of grandeurs 64. The nurse is assigned to assist in the administration of electroconvulsive therapy (ECT). She prepares to administer: a. Valium b. Ativan c. Brevital d. Morphine 65. The priority nursing intervention while ECT is being administered to the patient? a. Controlling seizure b. Controlling movements c. Watching vital signs d. Maintaining airway 66. In caring for the alcoholic patient, the nurse recognizes the early signs and symptoms of DTs are: a. Apathy and helplessness b. Fever and chills c. Headaches and restlessness d. Sudden decrease in vital signs 67. A patient is admitted with physical restlessness and generalized apprehension. He is expressing pessimism and is having difficulty concentrating in therapy. He states. “I just don’t know what is the matter with me.” The nurse assesses the patient is experiencing: a. Depression b. Obsessions c. Paranoid thoughts d. Free-floating anxiety 68. The depressed patient who has been taking Nardil states she is going to stop taking the drug. She asks the nurse, ”When can I start eating normally again?” The information that the nurse to a tyramine-free diet for: a. 2-3 days b. About a week c. About 2 weeks d. About a month 69. The patient has been taking in therapy six weeks working on experiencing and resolving issues related to anger. During on session the patient suddenly states,” I am really getting angry, ”The nurse evaluates this as: a. Repression b. Regression c. Progress d. Hopeless 70. The fight-flight response causes increasing blood pressure and heart rate, quickening respiration, dilated pupils, and sweating. What body system initiates this physical stimulation to a psychological stressors? a. Neurological b. Cardiovascular c. Sympathetic nervous system d. Parasympathetic nervous system . 71. A Retired postal worker is being admitted to the psychiatric unit He states to the nurse that he is the president of foreign country and postal executives from all over the world seek his advice on mailing letters. He is exhibiting : a. Delirium b. Illusions c. Grandiosity d. Confabulation 72. While performing an initial assessment on a patient admitted with depression, what physical aspect is most important to assess? a. Height and weight b. Urinary functioning c. Last menstrual period d. Sleeping patterns 73. The nurse assesses increasing restless, agitation, swinging of legs, and pacing in the patient who has been talking Thorazine 400 mg daily. The nursing evaluation is: a. EPS b. NMS c. Dystonia d. Akathisia Ans: D-Akathisia, a common side effect of phenothiazines is a feeling of uncontrollable restlessness. It is treated by decreasing dose, changing medications, and administering Benadryl. 74. The nurse calls the physician and requires an order for restraints. Which factor will be most decisive when the nurse is face with decision to implement the use of restraints? a. Cooperation b. Safety c. Court orders d. Family request Ans: B-When a patient’s safety is at issue; the use of restrains is warranted. Then nurse should carefully document the safety issue. 75. The nurse is caring for a client with hypochondriasis. Which behavior would the nurse most likely encounter? a.)Ready acceptance of the physician's explanation that all medical and laboratory tests are normal b.)Expression of fear of dying after being diagnosed with advanced breast cancer c.)Expression of fear of colorectal cancer following 3 days of constipation d.)Lack of concern about having a serious disease 76. The nurse is caring for a client who has been diagnosed with hypochondriasis. The client attributes his cough to tuberculosis. A chest X-ray and skin test are negative for tuberculosis. The client begins to complain about the sudden onset of chest pain. How should the nurse react initially? a.)Let the client know the nurse understands his fears of serious illness. b.)Encourage the client to discuss his fear of having a serious illness. c.)Report the complaint of chest pain to the physician. d.)Determine if the illness is fulfilling a psychological need for the client. 77. The nurse is talking with a client who recently attempted suicide. The client asks her not to tell anyone one about their conversation. How should the nurse respond? a.)I'll need to share information with the rest of your health care team if it's important to your care. b.)I promise I won't tell anyone about the information you share with me today. c.)I promise I won't tell anyone about the information you share with me today unless you give me permission to do so. d.)Please don't tell me anything that you wouldn't want others on your health care team to know. 78. The nurse is administering atropine sulfate to a client about to undergo electroconvulsive therapy. Which assessment indicates that the medication is effective? a.)The client's heart rate is 48 beats/minute. b.)The client states that his mouth is dry. c.)The client appears calm and relaxed. d.)The client falls asleep.. 79. The nurse is documenting a care plan for a client who has undergone electroconvulsive therapy. Which intervention should the nurse include? a.)Monitoring the client's vital signs every hour for 4 hours b.)Placing the client in Trendelenburg's position c.)Encouraging early ambulation d.)Reorienting the client to time and place 80. The nurse is caring for a client in the manic phase of bipolar disorder who is ready for discharge from the psychiatric unit. As the nurse begins to terminate the nurse-client relationship, which client response is most appropriate? a.)Expressing feelings of anxiety b.)Displaying anger, shouting, and banging the table. c.)Withdrawing from the nurse in silence d.)Rationalizing the termination, saying that everything comes to an end 81. A client with a borderline personality disorder has been playing one staff member against another. In formulating a care plan for this client, the nursing staff should include which intervention? a.)Assigning the same staff members to work with the client b.)Avoiding setting limits c.)Rotating staff members who work with the client d.)Avoiding interaction with the client until splitting behaviors stop 82. The nurse is planning care for a client admitted to the psychiatric unit with a diagnosis of paranoid schizophrenia. Which nursing diagnosis should receive the highest priority? a.)Risk for self- or other-directed violence b.)Imbalanced nutrition c.)Ineffective coping d.)Impaired verbal communication 83. The nurse is teaching a psychiatric client about her prescribed drugs, chlorpromazine and benztropine. Why is benztropine administered? a.)To reduce psychotic symptoms b.)To reduce extrapyramidal symptoms c.)To control nausea and vomiting d.)To relieve anxiety 84. The nurse is leading group therapy with psychiatric clients. During the working phase, what should the nurse do? a.)Explain the purposes and goals of the group. b.)Offer advice to help resolve conflicts. c.)Encourage group cohesiveness. d.)Encourage a discussion of feelings of loss regarding termination of the group. 85. A client is admitted to the substance abuse unit for alcohol detoxification. Which of the following medications is the nurse most likely to administer to reduce the symptoms of alcohol withdrawal? a.)Naloxone (Narcan) b.)Haloperidol (Haldol) c.)Magnesium sulfate d.)Chlordiazepoxide (Librium) D. RATIONALE: Chlordiazepoxide and other tranquilizers help reduce the symptoms of alcohol withdrawal. Haloperidol may be given to treat clients with psychosis, severe agitation, or delirium. Naloxone is administered for narcotic overdose. Magnesium sulfate and other anticonvulsant medications are administered to treat seizures only if they occur during withdrawal. 86. The client tells the nurse he was involved in a car accident while he was intoxicated. What would be the most therapeutic response from the nurse? a.)Why didn't you get someone else to drive you? b.)Tell me how you feel about the accident. c.)You should know better than to drink and drive. d.)I recommend that you attend an Alcoholics Anonymous meeting. 87. A client suffers from depression after the accidental death of her daughter. After a suicide attempt, the client is admitted to the psychiatric unit. During the admission interview, the client tells the nurse that she no longer wants to die. The nurse should: a.)suggest that the client no longer requires close observation. b.)place the client in a private room, away from the nurses' station, so that she has privacy to work through the stages of the grieving process. c.)inspect the client's personal belongings for potentially dangerous objects. d.)avoid any further discussion of suicide, unless the client brings up the topic. 88. The nurse is caring for a client diagnosed with panic disorder. The client begins to hyperventilate. How should the nurse respond initially? a.)Stay with the client during the panic attack. b.)Shout for help and obtain assistance. c.)Teach the client relaxation exercises. d.)Help the client explore the reason for the anxiety. 89. The nurse is caring for a client with panic disorder who has difficulty sleeping. Which nursing intervention would best help the client achieve healthy long-term sleeping habits? a.)Administering sleeping pills b.)Encouraging the use of relaxation exercises c.)Suggesting he talk with other clients until he feels ready to sleep d.)Telling him to play ping-pong in the day room 90. A teenager was driving a car that slipped off a road in Tagaytay, killing two of his friends. He repeatedly tells the nurse that he should be dead instead of his friends. The client's behavior is an example of: a.)survivor's guilt. b.)denial. c.)anticipatory grief. d.)repression. 91. The nurse is caring for a client with schizophrenia. Which of the following outcomes is least desirable? a.)The client spends more time by himself. b.)The client doesn't engage in delusional thinking. c.)The client doesn't harm himself or others. d.)The client demonstrates the ability to meet his own self-care needs. 92. The nurse is caring for a client with schizophrenia who experiences auditory hallucinations. The client appears to be listening to someone who isn't visible. He gestures, shouts angrily, and stops shouting in mid-sentence. Which nursing intervention is the most appropriate? a.)Approach the client and touch him to get his attention. b.)Encourage the client to go to his room where he'll experience fewer distractions. c.)Acknowledge that the client is hearing voices, but make it clear that the nurse doesn't hear these voices. d.)Ask the client to describe what the voices are saying. 93. A client with schizophrenia who receives fluphenazine (Prolixin) develops pseudoparkinsonism and akinesia. What drug would the nurse administer to minimize extrapyramidal symptoms? a.)Benztropine (Cogentin) b.)Dantrolene (Dantrium) c.)Clonazepam (Klonopin) d.)Diazepam (Valium) 94. The nurse is caring for a client being treated for alcoholism. Before initiating therapy with disulfiram (Antabuse), the nurse teaches the client that he must read labels carefully on which of the following products? a.)Carbonated beverages b.)Aftershave lotion c.)Toothpaste d.)Cheese 95. Which statement about somatoform pain disorder is accurate? a.)The pain is intentionally fabricated by the client in order to receive attention. b.)The pain is real to the client, even though there may not be an organic etiology for the pain. c.)The pain is less than would be expected from what the client identifies as the underlying disorder. d.)The pain is what would be expected from what the client identifies as the underlying disorder. 96. The nurse is caring for a client diagnosed with antisocial personality disorder. The client has a history of fighting, cruelty to animals, and stealing. Which of the following traits would the nurse be most likely to uncover during assessment? a.)History of gainful employment b.)Frequent expression of guilt regarding antisocial behavior c.)Demonstrated ability to maintain close, stable relationships d.)A low tolerance for frustration 97. The nurse is caring for a client with antisocial personality disorder. Which of the following statements is most appropriate for the nurse to make when explaining unit rules and expectations to the client? a.)"I and other members of the health care team would like you to attend group therapy each day." b.)"You'll find your condition will improve much faster if you attend group therapy each day." c.)"You'll be expected to attend group therapy each day." d.)"Please try to attend group therapy each day." 98. A 58-year-old client on a mental health unit has lost control, despite having been properly medicated, and is threatening to harm himself and others. He has been placed in four-point restraints. Which nursing measure should be taken next? a.)Release one restraint every 15 minutes. b.)Have a staff member stay with the client at all times. c.)Leave the client alone to reduce his sensory stimulation and allow him to regain control. d.)Restrict fluids until the restraint period is over. 99. Which nursing assessment has priority while a client's extremities are restrained? a.)Measuring urine output b.)Checking circulation in extremities c.)Assessing pupillary responses d.)Noting respiratory pattern 100. A psychiatric client who was voluntarily admitted now wishes to be discharged from the hospital, against medical advice. What's the most important assessment the nurse should make of the client? a.)Ability to care for himself b.)Degree of danger to self and others c.)Level of psychosis d.)Intended compliance with aftercare 51. The client asks the nurse what causes a peptic ulcer to develop. The nurse responds that research indicates that many peptic ulcer are the result of which of the following? a. Work-related stress b. Helicobacter pylori infection c. Diets high in fat d. A genetic defect in the gastric mucosa 52. A client with a peptic ulcer reports epigastric pain that frequently awakens her during the night, a feeling of fullness in the abdomen, and a feeling of anxiety about her health. Based on this information which nursing diagnosis would be most appropriate? a. Imbalanced nutrition: less than body requirements related to anorexia b. Disturbed sleep pattern related to epigastric pain c. Ineffective coping related to exacerbation of duodenal ulcer d. Activity intolerance related to abdominal pain 53. The nurse is preparing to teach a client with a peptic ulcer about the diet that should be followed after discharge. The nurse should explain that the diet will most likely consist of which of the following? a. Bland foods b. High-protein foods c. Any foods that are tolerated d. Large amounts of milk 54. The nurse finds a client who has been diagnosed with a peptic ulcer surrounded by papers from his briefcase and arguing on the telephone with a coworker. The nurse’s response to observing these actions should be based on knowledge that: a. Involvement with his job will keep the client from becoming bored b. A relaxed environment will promote ulcer healing c. Not keeping up with his job will increase the client’s stress level d. Setting on the client’s behavior is an important nursing responsibility 55. A client with peptic ulcer has been instructed to avoid intense physical activity and stress. Which activity should the client incorporate into the home care plan? a. Conduct physical activity in the morning so that he can rest in the afternoon b. Have the family agree to perform the necessary yard work at home c. Give up jogging and substitute a less demanding hobby d. Incorporate periods of physical and mental rest in his daily schedule 56. A client is to take one daily dose of ranitidine (Zantac) at home to treat her peptic ulcer. The nurse knows that the client understands proper drug administration of ranitidine when she says that she will take the drug at which of the following times? a. Before meals b. With meals c. At bedtime d. When pain occurs 57. A client has been taking aluminum hydroxide (Amphojel) 30 mL is six times per day at home to treat his peptic ulcer. He tells the nurse that he has been unable to have a bowel movement for 3 days. Based on this information, the nurse would determine that which of the following is the most likely cause of the client’s constipation? a. The client has not been including enough fiber in his diet b. The client needs to increase his daily exercise c. The client is experiencing a side effect of the aluminum hydroxide d. The client has developed a gastrointestinal obstruction 58. A client is taking an antacid for treatment of peptic ulcer. Which of the following statements best indicates that the client understands how to correctly take the antacid? a. “ I should take my antacid before I take my other medications.” b. “ I need to decrease my intake of fluids so that I don’t dilute the effects of my antacid.” c. “ My antacid will be most effective if I take it whenever I experience stomach pains.” d. “ It is best for me to take my antacid 1 to 3 hours after meals.” 59. Which of the following would be an expected outcome for a client with peptic ulcer disease? a. The client will demonstrate appropriate use of analgesics to control pain b. The client will explain the rationale for eliminating alcohol from the diet c. The client will verbalize the importance of monitoring hemoglobin and hematocrit every 3 months d. The client will eliminate contact sports from his or her lifestyle 60. A client with suspected gastric cancer undergoes an endoscopy of the stomach. Which of the following assessments made after the procedure would indicate the development of potential complication? a. The client complains of a sore throat b. The client displays signs of sedation c. The client experiences a sudden increase in temperature d. The client demonstrates a lack of appetite 61. The nurse is completing a health assessment of a 42-year-old woman with suspected Grave’s disease. The nurse should asses this client for: a. Anorexia b. Tachycardia c. Weight gain d. Cold skin 62. A female client with thyrotoxicosis would probably report which changes related to the menstrual cycle during initial assessment? a. Dysmenorrhea b. Metrorrhagia c. Oligomenorrhea d. Menorrhagia 63. Prophylthiouracil (PTU) is prescribed for a client with Grave’s disease to decrease circulating thyroid hormone. The nurse should teach the client to immediately report which of the following signs and symptoms? a. Sore throat b. Painful, excessive menstruation c. Constipation d. Increased urine output 64. A client with thyrotoxicosis says to the nurse, “ I am so irritable. I am having problems at work because I lose my temper very easily.” Which of the following responses by the nurse would give the client the most accurate explanation of her behavior? a. “ Your behavior is caused by temporary confusion brought on by your illness.” b. “ Your behavior is caused by the excess thyroid hormone in your system.” c. “ Your behavior is caused by your worrying about the seriousness of your illness.” d. “ Your behavior is caused by the stress of trying to manage a career and cope with illness.” 65. Serum concentrations of thyroid hormones and thyroid-stimulating hormone (TSH) are tests ordered for the client with thyrotoxicosis. Which of the following laboratory values are indicative of thyrotoxicosis? a. Elevated thyroid hormone concentrations and normal TSH b. Elevated TSH and normal concentrations and elevated TSH c. Decreased thyroid hormone concentrations and elevated TSH d. Elevated thyroid hormone concentrations and decreased TSH 66. The nurse should teach the client to prevent corneal irritation from mild exophthalmos by: a. Massaging the eyes at regular intervals b. Instilling an ophthalmic anesthetic as ordered c. Wearing dark-colored glasses d. Covering both eyes with moistened gauze pads . 67. A client with Grave’s disease is treated with radioactive iodine (RAI) in the form of sodium iodide 131I. Which of the following statements by the nurse will explain to the client how the drug works? a. “ The radioactive iodine stabilizes the thyroid hormone levels before a thyroidectomy.” b. “ The radioactive iodine reduces uptake of thyroxine and thereby improves your condition.” c. “ The radioactive iodine lowers the levels of thyroid hormones by slowing your body’s production of them.” d. “ The radioactive iodine destroys thyroid tissue so that thyroid hormones are no longer produced.” 68. Which of the following nursing diagnoses would most likely be appropriate for a client with Grave’s disease performing self-care after treatment with RAI in the form of sodium iodide 131I? a. Risk for injury related to altered level of consciousness b. Ineffective breathing pattern related to effects of radioactive iodine c. Total self-care deficit related to the need for immobilization after RAI therapy d. Risk for ineffective therapeutic regimen related to lack of knowledge about disease management 69. After treatment with RAI in the form of sodium iodide 131I, the nurse teaches the client to: a. Monitor signs and symptoms of hyperthyroidism b. Rest for 1 week to prevent complications of the medication c. Take thyroxine replacement of the remainder of the client’s life d. Assess for hypertension and tachycardia resulting from altered activity 70. A client with a large goiter is scheduled for a subtotal thyroidectomy to treat thyrotoxicosis. Saturated solution of potassium iodide (SSKI) is prescribed preoperatively for the client. The primary reason for using this drug is that it helps; a. Slow progression of exophthalmos b. Reduce the vascularity of the thyroid gland c. Decrease the body’s ability to store thyroxine d. Increase the body’s ability to excrete thyroxine 71. Which of the following measures is most recommended when preparing SSKI for administration? a. Pour the solution over ice chips b. Mix the solution with water, milk or fruit d. Dilute the solution with water, milk fruit juice and have the client drink it with a straw Disguise the solution in a pureed fruit or vegetable 72. The nurse asks the client to state her name as soon as she regains consciousness postoperatively after a subtotal thyroidectomy and at each assessment. The nurse does this primarily to monitor for signs of which of the following? a. Internal hemorrhage b. Decreasing level of consciousness c. Laryngeal nerve damage d. Upper airway obstruction 73. A client who has undergone a subtotal thyroidectomy is subject to complications in the first 48 hours after surgery. The nurse should obtain and keep at the bedside equipment to: a. Begin total parenteral nutrition b. Start a cutdown infusion c. Administer tube feedings d. Perform a tracheostomy 74. Which of the following symptoms might indicate that a client was developing tetany after a subtotal thyroidectomy? a. Pains in the joints of the hands and feet b. Tingling in the fingers c. Bleeding on the back of the dressing d. Tension on the suture line 75. Which of the following medications should be available to provide emergency treatment if a client develops tetany after a subtotal thyroidectomy? a. Sodium phosphate b. Calcium gluconate c. Echothiophate iodide d. Sodium bicarbonate 76. A 60-year-old woman is diagnosed with hypothyroidism. Signs and symptoms of hypothyroidism include: a. Tachycardia b. Weight gain c. Diarrhea d. Anorexia 77. Appropriate nursing diagnoses for a client with hypothyroidism would probably include which of the following? a. Risk for injury (corneal abrasion) related to incomplete closure of eyelid b. Imbalanced nutrition: less than body requirements related to hypermetabolism c. Deficient fluid volume related to diarrhea d. Activity intolerance related to fatigue associated with the disorder 78. When discussing recent onset of feelings of sadness and depression in a client with hypothyroidism, the nurse should inform the client that these feelings are: a. The effects of thyroid hormone replacement therapy and will diminish over time b. Related to the thyroid hormone replacement therapy and will not diminish over time c. A normal part of having a chronic illness d. Most likely related to low thyroid hormone levels and will improve with treatment 79. A 55-year-old male client has recently been diagnosed with type 2 diabetes mellitus (DM) and is prescribed the sulfonylurea compound tolbutamide (Orinase). He is concerned about the diagnosis and says he knows nothing about diabetes. The nurse determines that the client needs teaching and support. The nurse explains that tolbutamide is believed to lower the blood glucose level by which of the following actions? a. Potentiating the action of insulin b. Lowering the renal threshold of glucose c. Stimulating insulin release from functioning beta cells in the pancreas d. Combining with glucose to render it inert. 80. When teaching the diabetic client about foot care, the nurse should instruct the client to do which of the following: a. Avoid going barefoot b. Buy shoes a half size larger c. Cut toenails at angles d. Use heating pads for sore throat 81. A client with DM asks the nurse to recommend something to remove corns from his toes. The nurse should advise him to: a. Apply a high-quality corn plaster to the area b. Consult his physician or podiatrist about removing the corns c. Apply iodine to the corns before peeling them off d. Soak his feet in borax solution to peel off the corns 82. A client with DM presents to the clinic for a regular 3-month follow-up appointment. The nurse notes several small bandages covering cuts on the client’s hands. The client says, “ I’m so clumsy. I’m always cutting my finger cooking or burning myself on the iron.” Which of the following responses by the nurse would be most appropriate? a. “ Wash all wounds in isopropyl alcohol.” b. “ Keep all cuts clean and covered.” c. “ Why don’t you have your children to do the cooking and ironing?” d. “ You really should be fine as long as you take your daily medication.” 83. The client with DM says, “ If I could just avoid what you call carbohydrates in my diet, I guess I would be okay.” The nurse should base the response to this comment on the knowledge that diabetes affects metabolism of which of the following? a. Carbohydrates only b. Fats and carbohydrates only c. Protein and carbohydrates only d. Proteins, fats, and carbohydrates 84. A client with type 1 DM is admitted to the emergency department. Which of the following respiratory patterns requires immediate action? a. Deep, rapid respirations with long expirations b. Shallow respirations alternating with long expirations c. Regular depth of respirations with frequent pauses d. Short expirations and inspirations 85. The nurse should caution the client with DM who is taking a sulfonylurea medication that alcoholic beverages should be avoided while taking these drugs because they can cause which of the following? a. Hypokalemia b. Hyperkalemia c. Hypocalcemia d. Disulfiram (Antabuse)-like symptoms 86. A client with allergic rhinitis is instructed on the correct technique for using an intranasal inhaler. Which of the following statements would demonstrate to the nurse that the client understands the instructions? a) “ I should limit the use of the inhaler to early morning and bedtime use.” b) “ It is important to not shake the canister, because that can damage the spray device.” c) “ I should hold one nostril closed while I insert the spray into the other nostril.” d) “ The inhaler tip is inserted into the nostril and pointed toward the inside nostril wall.” 87. Which of the following would be an expected outcome for a client recovering from an upper respiratory tract infection? a) The client maintains a fluid intake of 800 mL every 24 hours b) The client experiences chills only once a day c) The client coughs productively without chest discomfort d) The client experiences less nasal obstruction and discharge 88. The nurse teaches the client how to instill nasal drops. Which of the following techniques is correct? a) The client uses sterile technique when handling the dropper b) The client blows the nose gently before instilling drops c) The client uses a new dropper for each installation d) The client sits in a semi-fowler’s position with the head tilted forward after administration of the drops 89. A client with acute sinusitis is examined in an ambulatory clinic. The nurse can anticipate the use of which of the following medications in the client’s treatment plan? a) Antibiotics b) Antihistamines c) Bronchodilators d) Oral corticosteroids 90. The nurse should include which of the following instructions in the teaching plan for a client with chronic sinusitis? a) Avoid the use of caffeinated beverages b) Perform postural drainage every day c) Take hot showers twice daily d) Report a temperature of 102oF (38.9oC) or higher 91. Which of the following individuals would the nurse consider to have the highest priority for receiving an influenza vaccination? a) A 60-year-old man with a hiatal hernia b) A 36-year-old woman with three children c) A 50-year-old woman caring for a spouse with cancer d) A 60-year-old woman with osteoarthritis 92. A client with allergic rhinitis asks the nurse what he should do to decrease his symptoms. Which of the following instructions would be appropriate for the nurse to give the client? a) “ Use your nasal decongestant spray regularly to help clear your nasal passages.” b) “ Ask the doctor for antibiotics. Antibiotics will help decrease the secretion.” c) “ It is important to increase you activity. A daily brisk walk will help promote drainage.” d) “ Keep a diary of when your symptoms occur. This can help you identify what precipitates your attacks.” 93. An elderly client has been ill with the flu, experiencing headache, fever, and chills. After 3 days, she develops a cough productive of yellow sputum. The nurse auscultates her lungs and hears diffuse crackles. How would the nurse best interpret these assessment findings? a) It is likely that the client is developing a secondary bacterial pneumonia. b) The assessment findings are consistent with influenza and are to be expected c) The client is getting dehydrated and needs to increase her fluid intake to decrease secretions d) The client has not been taking her decongestants and bronchodilators as prescribed 94. Guaifenesin 300 mg four times a day has been ordered as an expectorant. The dosage strength of the liquid is 200 mg/5 mL. How many milliliters should the nurse administer for each dose? a) 5.0 mL b) 7.5 mL c) 9.5 mL d) 10.0 mL 95. Pseudoephedrine (Sudafed) has been ordered as a nasal decongestant. Which of the following is a possible side effect of this drug? a) Constipation b) Bradycardia c) Diplopia d) Restlessness 96. A 27-year-old woman has had elective nasal surgery for a deviated septum. Which of the following would be an important initial clue that bleeding was occurring even if the nasal drip pad remained dry and intact? a) Complaints of nausea b) Repeated swallowing c) Increased respiratory rate d) Increased pain 97. A client who has undergone outpatient nasal surgery is ready for discharge and has nasal packing in place. Which of the following discharge instructions would be appropriate for the client? a) Avoid activities that elicit the valsalva maneuver b) Take aspirin to control nasal discomfort c) Avoid brushing the teeth until the nasal packing is removed d) Apply heat to the nasal area to control swelling 98. Which of the following statements would indicate to the nurse that a client has understood the discharge instructions provided after her nasal surgery? a) “ I should not shower until my packing is removed.” b) “ I will take stool softeners and modify my diet to prevent constipation.” c) “ Coughing every 2 hours is important to prevent respiratory complications.” d) “ It is important to blow my nose each day to remove the dried secretions.” 99. The nurse is planning to give preoperative instructions to a client who will be undergoing rhinoplasty. Which of the following instructions should be included? a) After surgery, nasal packing will be place for 7 to 10 days b) Normal saline dose drops will need to be administered preoperatively c) The results of the surgery will be immediately obvious postoperatively d) Aspirin-containing medications should not be taken for 2 weeks before surgery 100. Which of the following assessments would be a priority immediately after nasal surgery? a) Assessing the client’s pain b) Inspecting for periorbital ecchymosis c) Assessing respiratory status d) Measuring intake and output . At which of the following times would the nurse instruct the client to take ibuprofen (Motrin), prescribed for left hip pain secondary to osteoarthritis, to minimize gastric mucosal irritation? a. At bedtime b. On arising c. Immediately after a meal d. On an empty stomach 2. When preparing a teaching plan for the client with osteoarthitis who is taking celexocib (Celebrex), the nurse expects to explain that the major advantage of celecoxib over diclofenac (Voltaren) is that celecoxib is less likely to produce which of the following? a. Hepatotoxicity b. Renal toxicity c. Gastrointestinal (GI) bleeding d. Nausea and vomiting 3. The client diagnosed with osteoarthritis states, “ My friend takes steroid pills for her rheumatoid arthritis. Why don’t take steroids for my osteoarthritis?” The nurse’s response to the client is based on an understanding of which of the following? a. Intra-articular corticosteroid injections are used to treat osteoarthritis b. Oral corticosteroids can be used in osteoarthritis c. A systemic effect is needed in osteoarthritis d. Rheumatoid arthritis and osteoarthritis are two similar diseases 4. In preparation for total knee surgery, a 200-pound client with osteoarthritis is being discharged from the hospital to lose weight to reduce the risks of anesthesia. In conjunction with a weight loss program, which of the following exercises would the nurse recommend as best if t he client has no contraindications? a. Weight lifting b. Walking c. Aquatic exercise d. Tai chi exercise - 5. The physician recommends a total hip replacement for a client with osteoporosis who reports increasingly severe pain in the left hip. The nurse would initiate the preoperative teaching plan for the client, beginning with which of the following? a. Teaching how to prevent hip flexion b. Demonstrating coughing and deep breathing techniques c. Showing the client what an actual hip prosthesis looks like d. Assessing the client’s fears about the procedure 6. After the client undergoes a total knee replacement for severe osteoarthritis, which of the following assessment findings would lead the nurse to suspect possible nerve damage? a. Numbness b. Bleeding c. Dislocation d. Pinkness 7. After surgery and insertion of a total joint prosthesis, a client develops severe sudden pain and inability to move the extremity. The nurse interprets these findings as indicating which of the following? a. A developing infection b. Bleeding in the operative site c. Joint dislocation d. Glue seepage into soft tissue 8. Which of the following would the nurse assess in a client with an intracapsular hip fracture? a. Internal rotation b. Muscle flaccidity c. Shortening of affected leg d. Absence of pain in the fracture area 9. When developing the plan of care for an older adult client with a hip fracture, which of the following chronic health problems would the nurse be lest likely to assess in the client? a. Hypertension b. Cardiac decompensation c. Pulmonary disease d. Multiple sclerosis 10. When teaching a client with an extracapsular hip fracture scheduled for surgical internal fixation with the insertion of a pin, the nurse bases the teaching on the understanding that this surgical repair is the treatment of choice for which of the following reasons? a. Hemorrhage at the fracture site is prevented b. Neurovascular impairment risk is decreased c. The risk for infection at the site is lessened d. The client is able to be mobilized sooner 11. A client with an extracapsular hip fracture returns to the nursing unit after internal fixation and pin insertion with a drainage tube at the incision site. Her husband asks, “ Why does she have this tube inserted in her hip?” Which of the following responses by the nurse demonstrates understanding of the primary purpose for this drainage tube? a. “ The tube helps us to detect a wound infection early on.” b. “ This way we won’t have to irrigate the wound.” c. “ Fluid won’t be allowed to accumulate at the site.” d. “ We have a way to administer antibiotics into the wound.” 12. When assessing a client who has just received a femoral head prosthesis, which of the following would alert the nurse to the possibility of neurologic a. Decreased distal pulse b. Inability to move c. Diminished capillary refill d. Coolness to the touch Ans: B – being unable to move the affected leg suggest neurologic impairment. A decrease in the distal pulse, diminished capillary refill, and coolness to touch of the affected extremity suggest vascular compromise. 13. A client with a hip fracture has undergone surgery for insertion of a femoral head prosthesis. Which of the following activities would the nurse instruct the client to avoid? a. Crossing the legs while sitting down b. Sitting on a raised commode seat c. Using an abductor splint while lying on the side d. Rising straight from a chair to a standing position 14. The nurse encourages the client who has had a femoral head prosthesis placement to use which of the following types of chairs to sit in during the first 6 to 8 weeks after surgery? a. A desk-type swivel chair b. A padded upholstered chair c. A high-backed chair with armrests d. A recliner with an attached footrest 15. While assessing the home environment of an elderly client who is using crutches during the postoperative recovery phase after hip pinning, which of the following would pose the greatest hazard to the client as a risk for falling at home? a. A 4-year-old cooker spaniel b. Scatter rugs c. Snack tables d. Rocking chairs 16. Which of the following activities would the nurse instruct the client with low back pain to avoid? a. Keeping light objects below the level of the elbows when lifting b. Leaning forward while bending the knees c. Exceeding prescribed exercise program d. Sleeping on the side with legs flexed 17. A client was brought to the hospital because he could not get out of bed because of low back pain radiating down to his right heel and lateral foot. When developing the client’s plan of care, which of the following categories of medication would the nurse anticipate the physician’s ordering? a. Angiotensin-converting enzyme (ACE) inhibitors b. - adrenergic blocking agentsb c. Nonsteroidal anti-inflammatory drugs (NSAIDs) d. Barbiturates 18. A client with a ruptured intervertebral disc at L4-5 stands with a flattened spine slightly tilted forward and slightly flexed to the affected side. The nurse interprets this finding as indicating which of the following? a. Motor changes b. Postural deformity c. Alteration of reflexes d. Sensory changes 19. Which of the following positions would be most comfortable for a client with a ruptured disc at L5-S1 right? a. Prone b. Supine with the legs flexed c. High fowler’s d. Right Sims’ 20. The client with a herniated intervertebral disc schedule for a myelogram asks the nurse about the procedure. The nurse explains that radiographs will be taken of the client’s spine after an injection of which of the following? a. Sterile water b. Normal saline solution c. Liquid nitrogen d. Radiopaque dye 21. Which of the following would be inappropriate to include when preparing a client for magnetic resonance imaging (MRI) to evaluate a ruptured disc? a. Informing the client that the procedure is painless b. Taking a thorough history of past surgeries c. Checking for previous complaints of claustrophobia d. Starting an intravenous line at keep-open rate 22. A client complaining of numbness from the back of his left buttock to the dorsum of his foot and big toe is scheduled to undergo a laminectomy. The operative consent form states,” a left lumbar laminectomy of L3-4.” Based on the nurse’s understanding of the client’s complaints and intended surgical procedure which of the following would the nurse do next? a. Have the client sign the consent form b. Call the surgeon c. Change the consent form d. Review the client’s history 23. After a bilateral lumbar laminectomy at L5-S1, which of the following is a priority nursing diagnosis for the client in the immediate postoperative phase? a. Impaired physical mobility related to back pain b. Imbalanced nutrition: less than body requirements related to postoperative status c. Bowel incontinence related to decreased physical activity d. Disturbed body image related to fear of disfiguring surgical scar 24. Immediately after the lumbar laminectomy, the nurse administers ondansetron hydrochloride (Zofran) to the client as ordered. The nurse determines that the drug is effective when which of the following is controlled? a. Muscles spasms b. Nausea c. Shivering d. Dry mouth 25. After a laminectomy, the client states, “ The doctor said that I can do anything I want to.” Which of the following activities, if stated by the client, indicates need for further teaching? a. Drying the dishes b. Sitting outside on firm cushions c. Making the bed walking from side to side d. Sweeping the front porch 26. When developing the drainage teaching plan for a client who has undergone a lumbar laminectomy L4-5 left and will be returning to work in 6 weeks, which of the following actions would the nurse encourage the client to avoid? a. Placing one foot on a stepstool during prolonged standing b. Sleeping on the back with support under the knees c. Maintaining average body weight for height d. Sitting whenever possible 27. A male client, who had normal preoperative baseline data except for dysfunction associated with this operative diagnosis, underwent a spinal fusion yesterday. Which of the following nursing assessments would alert the nurse to the development of a possible complication? a. Lateral rotation of the head and neck b. Clear yellowish fluid on the dressing c. Use of the standing position to void d. Nonproductive cough 28. After a spinal fusion, a client is required to wear a back brace. Which of the following would the nurse expect to do before applying the brace? a. Have the client in bed lying on the side b. Verify with the physician the position to use c. Ask the client to stand with arms held out to the side d. Encourage the client to sit in a straight chair 29. After teaching a client required to wear a back brace after a spinal fusion, which of the following client statements indicate effective teaching about skin protection measures with the brace? a. “ I will apply lotion before putting on the brace.” b. “ I will be sure to pad area around my iliac crest.” c. “ I can use baby powder under the brace to absorb perspiration.” d. “ I should wear a thin cotton undershirt under the brace.” 30. When developing the teaching plan for a client scheduled for a spinal fusion, which of the following would the nurse expect to include? a. The client typically experiences more pain at the donor site than at the fusion site than at the fusion site b. The surgeon will apply a simple gauze dressing to the donor site c. Neurovascular checks are unnecessary if the fibula is the donor site d. The client’s level of activity restriction is determined by the amount of pain 31. The nurse determines that the client who has had a lumbar laminectomy with a spinal fusion understands his protective instructions when he places his feet in which of the following positions when sitting in a chair? a. On the floor with the feet flat b. On a low footstool c. In any comfortable position with legs uncrossed d. On a high footstool so the feet are level with the chair seat 32. When developing the plan of care for a client undergoing a lumbar laminectomy, which of the following activities would be contraindicated during the initial postoperative period? a. Assisting with her daily hygiene activities b. Lying flat in bed c. Walking in the hall d. Sitting all afternoon in her room 33. Which of the following exercises would the nurse advise the client to avoid after a lumbar laminetcomy? a. Knee-to-chest lifts b. Hip tilts c. Sit-ups d. Pelvic tilts 34. When obtaining the history of a client with peripheral vascular disease who requires an amputation, which of the following would the nurse identify as the least likely factor contributing to the client’s peripheral vascular disease? a. Uncontrolled diabetes mellitus for 15 years b. A 20-pack-year history of cigarette smoking c. Current age of 39 years d. A serum cholesterol concentration of 275 mg/dL 35. When assessing the client with severe arterial occlusive disease and gangrene of the left great toe, which of the following findings would the nurse observe in the client’s left leg and foot? a. Edema around the ankle b. Loss of hair on the lower leg c. Thin, soft toenails d. Warmth in the foot 36. A client with absent peripheral pulses and pain at rest is scheduled for an arterial Droppler study of the affected extremity. Which of the following would the nurse include when preparing the client for this test? a. Have the client sign a consent form of the procedure b. Administer a pretest sedative as appropriate c. Keep the client tobacco-free for 30 minutes before the test d. Wrap the client’s affected foot with a blanket 37. The client with peripheral arterial disease says, “ I’ve really tried to manage my condition well.” Which of the following, if reported by the client during the history, would the nurse determine as appropriate for this client? a. Resting with the legs elevated above the level of the heart b. Walking slowly but steadily for 30 minutes twice a day c. Minimizing activity as much and as often as possible d. Wearing antiembolism stockings at all times when out of bed 38. Which of the following would the nurse include in the teaching plan for a client with arterial insufficiency to the feet is being managed conservatively? a. Daily lubrication of the feet b. Soaking the feet in warm water c. Applying antiembolism stocking s d. Wearing firm, supportive leather shoes 39. While the nurse is providing preoperative teaching, the client says, “ I hate the idea of being an invalid after they cut off my leg.” Which of the following would be the nurse’s most thermometric response? a. “ At least you will still have one good leg to use.” b. “ Tell me more about how you’re feeling.” c. “ Let’s finish the preoperative teaching.” d. “ You’re lucky to have a wife to care for you.” 40. The client asks the nurse, “ Why can’t the doctor tell me exactly how much of my leg he’s going to take off? Don’t you think I should know that?” The nurse responds based on the understanding that the final decision about the level of amputation required depends primarily on which of the following? a. The need to remove as much of the leg as possible b. The adequacy of the blood supply to the tissues c. The ease with which a prosthesis can be fitted d. The client’s ability to walk with a prosthesis 41. A client who has a history of mitral valve prolapse tells the nurse during a clinical visit that she is scheduled to get her teeth cleaned. Which of the following replies by the nurse is most appropriate? a. “ The physician will need to revaluate the status of your heart condition before your dental appointment.” b. “ Be sure to remind your dentist that you have a heart condition.” c. “ It is important for you to care for your teeth because your heart condition makes you more susceptible to developing oral infections.” d. “ We will prescribe a prophylactic antibiotic for you to take before getting your teeth cleaned.” 42. The nurse instructs the nursing assistant on how to provide oral hygiene for a client who cannot perform this task for himself. Which of the following techniques should the nurse tell the assistant to incorporate into the client’s daily care? a. Assess the oral cavity each time mouth care is given and record observations b. Use a soft toothbrush to brush the client’s teeth after each meal c. Swab the client’s tongue, gums, and lips with a soft foam applicator every 2 hours d. Rinse the client’s mouth with mouthwash several times a day 43. During the assessment of a client’s mouth, the nurse notes the absence of saliva. The client is complaining of pain in the area of t he ear. The client has been NPO for several days because of the insertion of a nasogastric tube. Based on these findings, the nurse suspects that the client may be developing which of the following mouth conditions? a. Stomatitis b. Oral candidiasis c. Parotitis d. Gingivitis 44. The nurse is preparing a community presentation on oral cancer. Which of the following is a primary risk factor for oral cancer that the nurse should include in the presentation? a. Use of alcohol b. Frequent use of mouthwash c. Lack of vitamin B12 d. Lack of regular teeth cleaning by a dentist Ans: A – chronic and excessive use of alcohol can lead to oral cancer. Smoking and use of smokeless tobacco are other significant risk factors. Additional risk factors include chronic irritation such as a broken tooth or ill-fitting dentures, poor dental hygiene, overexposure to sun (lip cancer), and syphilis. Use of mouthwash, lack of vitamin B12 and lack of regular teeth cleaning appointments have not been implicated as primary risk factors for oral cancer. 45. A client has entered a smoking cessation program to quit a two-pack-a-day cigarette habit. He tells the occupational health nurse at his place of employment that he has not smoked a cigarette for 3 weeks, but is afraid he is going to “slip up” and smoke because of current job pressures. What would be the most appropriate reply for the nurse to make in response to the client’s comments? a. “ Don’t worry about it. Everybody has difficulty quitting smoking, and you should expect to as well.” b. “ If you increase your self-control, I am sure you will be able to avoid smoking.” c. “ Try taking a couple of days of vacation to relieve the stress of your job.” d. “ It is good that you can talk about your concerns. Try calling a friend when you want to smoke.” 46. A client who was in a motor vehicle accident has a fractured mandible. Surgery has been performed to immobilize the injury by wiring the jaw. What is the nurse’s priority in regard to care in the immediate postoperative phase? a. Prevent nausea and vomiting b. Maintain a patent airway c. Provide frequent airway d. Establish a way for the client to communicate 47. A client has returned from surgery during which her jaws were wired as treatment for a fractured mandible. The client is in stable condition. The nurse is instructing the assistant on how to properly position the client. Which instructions about positioning would be appropriate for the nurse to give the assistant? a. Keep the client in a side-lying position with the head slightly elevated b. Do not reposition the client without the assistance of a registered nurse c. The client can assume any position that is comfortable d. Keep the client’s head elevated on two pillows at all times 48. A client who has had her jaws wired begins to vomit. What should be the nurse’s first action? a. Insert a nasogastric tube and connect it to suction b. Use wire cutters to cut the wire c. Suction the client’s airway as needed d. Administer an antiemetic intravenously 49. A client is admitted to the hospital after vomiting bright red blood and is diagnosed with a bleeding duodenal ulcer. The client develops a sudden, sharp pain in the midepigastric region along with a rigid, boardlike abdomen. These clinical manifestations most likely indicate which of the following? a. An intestinal obstruction has developed b. Additional ulcers have developed c. The esophagus has become inflamed d. The ulcer is perforated 50. A client with peptic ulcer disease tells the nurse that he has black stools, which he has not reported to his physician. Based on this information, which nursing diagnosis would be appropriate for this client? a. Ineffective coping related to fear of diagnosis of chronic illness b. Deficient knowledge related to unfamiliarity with significant signs and symptoms c. Constipation related to decreased gastric motility d. Imbalanced nutrition: less than body requirements related to gastric bleeding 1. Assessment of a pregnant client reveals that she feels very anxious because of a lack of knowledge about giving birth. The client is in her second trimester. Which nursing intervention is most appropriate for this client? a.)Provide her with the information and teach her the skills she'll need to understand and cope during birth. b.)Provide her with written information about the birthing process. c.)Have a more experienced pregnant woman assist her. d.)Do nothing in hopes that she'll begin coping as the pregnancy progresses. 52. The nurse is assessing a pregnant woman in the clinic. In the course of the assessment, the nurse learns that this woman smokes one pack of cigarettes per day. The first step the nurse should take to help the woman stop smoking is to: a.)assess the client's readiness to stop. b.)suggest that the client reduce the daily number of cigarettes smoked by one-half. c.)provide the client with the telephone number of a formal smoking cessation program. d.)help the client develop a plan to stop. 53. The nurse is recording an Apgar score for a neonate. The nurse should assess: a.)heart rate, respiratory effort, temperature, reflex irritability, and color. b.)heart rate, respiratory effort, reflex irritability, and color. c.)heart rate, respiratory effort, temperature, and color. d.)heart rate, respiratory effort, temperature, sucking reflex, and color. 54. The nurse is teaching the mother of a neonate about the importance of immunizations. The nurse should teach her that active immunity: a.)develops rapidly and is temporary. b.)occurs by antibody transmission. c.)results from exposure of an antigen through immunization or disease contact. d.)may be transferred by mother to neonate. 55. When evaluating a client's knowledge of symptoms to report during her pregnancy, which statement would indicate to the nurse that the client understands the information given to her? a.)"I'll report increased frequency of urination." b.)"If I have blurred or double vision, I should call the clinic immediately." c.)"If I feel tired after resting, I should report it immediately." d.)"Nausea should be reported immediately." 56. The nurse has a client at 30 weeks' gestation who has tested positive for the human immunodeficiency virus (HIV). What should the nurse tell the client when she says that she wants to breast-feed her neonate? a.)Encourage breast-feeding so that she can get her rest and get healthier. b.)Encourage breast-feeding because it's healthier for the neonate. c.)Encourage breast-feeding to facilitate bonding. d.)Discourage breast-feeding because HIV can be transmitted through breast milk. 57. A neonate of a client with type 1 diabetes mellitus is at high risk for hypoglycemia. An initial sign the nurse should recognize as indicating hypoglycemia in a neonate is: a.)peripheral acrocyanosis. b.)bradycardia. c.)lethargy. d.)jaundice. C. RATIONALE: Lethargy in the neonate may be seen with hypoglycemia because of a lack of glucose in the nerve cells. Peripheral acrocyanosis is normal in the neonate because of immature capillary function. Tachycardia, not bradycardia, is seen with hypoglycemia. Jaundice isn't a sign of hypoglycemia. 58. The nurse is assessing a neonate. When maternal estrogen has been transferred to the fetus, which sign will the nurse see in the neonate? a.)Weak sucking response b.)Enlarged breast tissue c.)Soft skin d.)Vernix caseosa 59. A 20-year-old female's pregnancy is confirmed at a clinic. She says her husband will be excited but she's concerned because she isn't excited. She fears this may mean she'll be a bad mother. The nurse should respond by: a.)referring her to counseling. b.)telling her such feelings are normal in the beginning of pregnancy. c.)exploring her feelings. d.)recommending she talk her feelings over with her husband. 60. A woman who is 10 weeks pregnant tells the nurse that she's worried about her fatigue and frequent urination. The nurse should: a.)recognize these as normal early pregnancy signs and symptoms. b.)question her further about these signs and symptoms. c.)tell her that she'll need blood work and urinalysis. d.)tell her that she may be excessively worried. 61. A client with hypotonic labor dysfunction has been started on oxytocin (Pitocin). Despite adequate contractions, the fetus doesn't descend lower than 0 station. The physician recommends cesarean delivery. The client and her husband are confused because she had given birth previously to an average-size neonate. They ask several questions about cesarean birth. What would be the most accurate nursing diagnosis for this client? a.)Anger related to loss of planned birth experience b.)Anxiety related to lack of knowledge about the need for cesarean birth c.)Acute pain related to long, unproductive labor d.)Fear related to the unknown 62. The nurse is providing care for a pregnant woman. The woman asks the nurse how she can best deal with her fatigue. The nurse should instruct her to: a.)take sleeping pills for a restful night's sleep. b.)try to get more rest by going to bed earlier. c.)take her prenatal vitamins. d.)tell her not to worry because the fatigue will go away soon. 63. The nurse is providing care for a pregnant 16-year-old client. The client says that she's concerned she may gain too much weight and wants to start dieting. The nurse should respond by saying: a.)"Now isn't a good time to begin dieting because you are eating for two." b.)"Let's explore your feelings further." c.)"Nutrition is important because depriving your baby of nutrients can cause developmental and growth problems." d.)"The prenatal vitamins should ensure the baby gets all the necessary nutrients." 64. The nurse is providing care for a pregnant client in her second trimester. Glucose tolerance test results show a blood glucose level of 160 mg/dl. The nurse should anticipate that the client will need to: a.)start using insulin. b.)start taking an oral antidiabetic drug. c.)monitor her urine for glucose. d.)be taught about diet. 65. The nurse is providing care for a pregnant client with gestational diabetes. The client asks the nurse if her gestational diabetes will affect her delivery. The nurse should know that: a.)the delivery may need to be induced early. b.)the delivery must be by cesarean. c.)the mother will carry to term safely. d.)it's too early to tell. 66. A newly pregnant woman tells the nurse that she hasn't been taking her prenatal vitamins because they make her nauseated. In addition to stressing the importance of taking the vitamins, the nurse should advise the client to: a.)switch brands. b.)take the vitamin on a full stomach. c.)take the vitamin with orange juice for better absorption. d.)take the vitamin first thing in the morning. 67. A neonate born 2 hours ago has just arrived in the nursery. Which nursing measure will prevent the neonate from losing heat due to evaporation? a.)Keeping him away from drafts b.)Putting a blanket between him and cold surfaces c.)Putting a cap on his head d.)Drying him thoroughly after a bath 68. The nurse is caring for a neonate with a myelomeningocele. The priority nursing care of a neonate with a myelomeningocele is primarily directed toward: a.)ensuring adequate nutrition. b.)preventing infection. c.)promoting neural tube sac drainage. d.)conserving body heat. 69. nurse is conducting a neonate assessment of a boy, born 3 hours earlier. Which assessment would make the nurse suspect a congenital hip dislocation? a.)Limited abduction of the affected leg b.)Unequal gluteal folds c.)Lengthening of the limb on the affected side d.)Crepitus of the affected hip on movement 70. The nurse has been teaching a new mother how to feed her infant son who was born with a cleft lip and palate. Which action by the mother would indicate that the teaching has been successful? a.)Placing the neonate flat during feedings b.)Providing fluids with a small spoon c.)Placing the nipple in the cleft palate d.)Burping the neonate frequently 71. A client who is 34 weeks pregnant is experiencing bleeding caused by placenta previa. The fetal heart sounds are normal, and the client isn't in labor. Which nursing intervention should the nurse perform? a.)Allow the client to ambulate with assistance. b.)Perform a vaginal examination to check for cervical dilation. c.)Monitor the amount of vaginal blood loss. d.)Notify the physician for a fetal heart rate of 130 beats/minute. 72. A nurse in a prenatal clinic is assessing a 28-year-old who is 24 weeks pregnant. Which findings would lead this nurse to suspect that the client has mild preeclampsia? a.)Glycosuria, hypertension, seizures b.)Hematuria, blurry vision, reduced urine output c.)Burning on urination, hypotension, abdominal pain d.)Hypertension, edema, proteinuria 73. A client who is 24 weeks pregnant and diagnosed with preeclampsia is sent home with orders for bed rest and a referral for home health visits by a community health nurse. Which comment made by the client should indicate to the nurse that the client understands the reasons for home health visits? a.)"The community health nurse will help fix my meals." b.)"The community health nurse will give me my antihypertensive medication." c.)"The community health nurse will check me and my baby and talk with my physician." d.)"The community health nurse will give me prenatal care so that I won't have to see my physician." 74. A client who is 12 weeks pregnant is complaining of severe left lower quadrant pain and vaginal spotting. She's admitted for treatment of an ectopic pregnancy. Which nursing diagnosis takes the highest priority? a.)Risk for deficient fluid volume b.)Anxiety c.)Acute pain d.)Impaired gas exchange 75. A client delivered a healthy full-term baby girl 2 hours ago by cesarean delivery. When assessing this client, which finding requires immediate nursing action? a.)Tachycardia and hypotension b.)Gush of vaginal blood when she stands up c.)Blood stain (5.1 cm) in diameter on the abdominal dressing d.)Complaints of abdominal pain 76. A nurse in the nursery is preparing to perform phenylketonuria (PKU) testing. Which neonate is ready for the nurse to test? a.)A 3-day-old neonate who has been fed I.V. since birth b.)A 2-day-old neonate who has been breast-fed c.)A 1-day-old neonate receiving formula d.)A breast-fed neonate being discharged within 24 hours of birth 77. The nurse is teaching a client who is 28 weeks pregnant and has gestational diabetes how to control her blood glucose levels. Diet therapy alone has been unsuccessful in controlling her blood glucose levels, so she has started insulin therapy. The nurse should consider the teaching effective when the client says: a.)"I won't use insulin if I'm sick." b.)"I need to use insulin each day." c.)"If I give myself an insulin injection, I don't need to watch what I eat." d.)"I'll monitor my blood glucose levels twice a week." 78. A client's gestational diabetes is poorly controlled throughout her pregnancy. She goes into labor at 38 weeks and delivers a boy. Which priority intervention should be included in the care plan for the neonate during his first 24 hours? a.)Administer insulin subcutaneously. b.)Administer a bolus of glucose I.V. c.)Provide frequent early feedings with formula. d.)Avoid oral feedings. 79. A 28-year-old woman gave birth 1 hour ago to a full-term baby boy. Which finding should the nurse expect when palpating the client's fundus? a.)Soft, at the level of the umbilicus b.)Firm (1.9 cm) below the umbilicus c.)Firm, at the level of the umbilicus d.)Boggy, midway between the umbilicus and symphysis pubis 80. Which finding is considered normal in a neonate during the first few days after birth? a.)Weight loss of 25% b.)Birth weight of 2,000 to 2,500 g c.)Weight loss then return to birth weight d.)Weight gain of 25% 81. The mother of a neonate expresses concern about how she'll continue to breast-feed when she returns to work in 6 weeks. What's the best response by the nurse? a.)"Why don't you wait and see how things go? You may be tired of breast-feeding by then." b.)"Let your daycare provider give the baby formula in a bottle and breast-feed when you're home." c.)"Your baby won't need breast-feeding by then, so just switch completely to formula when you return to work." d.)"You can continue breast-feeding after you go back to work. You can pump your breasts and put the milk in a bottle." 82. Early detection of an ectopic pregnancy is paramount in preventing a life-threatening rupture. Which symptoms should alert the nurse to the possibility of an ectopic pregnancy? a.)Abdominal pain, vaginal bleeding, and a positive pregnancy test b.)Hyperemesis and weight loss c.)Amenorrhea and a negative pregnancy test d.)Copious discharge of clear mucus and prolonged epigastric pain 83. The client has just given birth to her first child, a healthy, full-term baby girl. The client is Rh (D)-negative and her neonate is Rh-positive. What intervention will be performed to reduce the risk of Rh incompatibility? a.)Administration of Rh (D) Immune Globulin I.M. to the neonate within 72 hours b.)Administration of Rh (D) Immune Globulin I.M. to the mother within 72 hours c.)Injection of Rh (D) Immune Globulin to the mother during her 6 week follow-up visit d.)Administration of Rh (D) Immune Globulin I.M. to the mother within 3 months 84. On the 9th postpartum day, a client breast-feeding her neonate experiences pain, redness, and swelling of her left breast. She's diagnosed with mastitis. The nurse teaching the client how to care for her infected breast should include which information? a.)Wear a loose-fitting bra to avoid constricting the milk ducts. b.)Stop breast-feeding permanently. c.)Take antibiotics until the pain is relieved. d.)Use a warm moist compress over the painful area. 85. The nurse teaches a postpartum client about breast-feeding. Which statement best indicates that the client knows how to avoid breast engorgement? a.)"I'll apply warm, moist compresses to my breasts." b.)"I'll breast-feed every 1& to 3 hours." c.)"I'll use an electric breast pump." d.)"I'll wear a bra 24 hours per day." 86. The nurse is assessing a client who gave birth yesterday. Where should the nurse expect to find the top of the client's fundus? a.)One fingerbreadth above the umbilicus b.)One fingerbreadth below the umbilicus c.)At the level of the umbilicus d.)Below the symphysis pubis 87. The nurse is helping to prepare a client for discharge following childbirth. During a teaching session, the nurse instructs the client to do Kegel exercises. What's the purpose of these exercises? a.)To prevent urine retention b.)To relieve lower back pain c.)To tone the abdominal muscles d.)To strengthen the perineal muscles 88. The nurse is using Doppler ultrasound to assess a pregnant woman. When should the nurse expect to hear fetal heart tones? a.)7 weeks b.)11 weeks c.)17 weeks d.)21 weeks 89. The nurse is planning care for a 16-year-old client in the prenatal clinic. Adolescents are prone to which complication during pregnancy? a.)Iron deficiency anemia b.)Varicosities c.)Nausea and vomiting d.)Gestational diabetes 90. The nurse is caring for a 16-year-old pregnant client. The client is taking an iron supplement. What should this client drink to increase the absorption of iron? a.)A glass of milk b.)A cup of hot tea c.)A liquid antacid d.)A glass of orange juice 91. The nurse is caring for a client who is on ritodrine therapy to halt premature labor. What condition indicates an adverse reaction to ritodrine therapy? a.)Hypoglycemia b.)Crackles c.)Bradycardia d.)Hyperkalemia 92. The nurse is caring for a client in her 34th week of pregnancy who wears an external monitor. Which statement by the client would indicate an understanding of the nurse's teaching? a.)"I'll need to lie perfectly still." b.)"You won't need to come in and check on me while I'm wearing this monitor." c.)"I can lie in any comfortable position, but I should stay off my back." d.)"I know that the external monitor increases my risk of a uterine infection." 93. The nurse is developing a care plan for a client in her 34th week of gestation who is experiencing premature labor. What nonpharmacologic intervention should the plan include to halt premature labor? a.)Encouraging ambulation b.)Serving a nutritious diet c.)Promoting adequate hydration d.)Performing nipple stimulation 94. A client treated for premature labor is ready for discharge. Which instruction should the nurse include in the discharge teaching plan? a.)Report a heart rate greater than 120 beats/minute to the physician. b.)Take terbutaline every 4 hours, during waking hours only. c.)Call the physician if the fetus moves 10 times in 1 hour. d.)Increase activity daily if not fatigued. 95. The nurse is caring for a client in labor. Which assessment finding indicates fetal distress? a.)Lack of meconium staining b.)Early decelerations in fetal heart rate during contractions c.)An increase in fetal heart rate with fetal scalp stimulation d.)Fetal blood pH less than 7.20 96. The nurse is assessing a woman in labor. Her cervix is dilated 8 cm. Her contractions are occurring every 2 minutes. She's irritable and in considerable pain. What type of breathing should the nurse instruct the woman to use during the peak of a contraction? a.)Deep breathing b.)Shallow chest breathing c.)Deep, cleansing breaths d.)Chest panting 97. The nurse is caring for a woman receiving a lumbar epidural anesthetic block to control labor pain. What should the nurse do to prevent hypotension? a.)Administer ephedrine to raise her blood pressure. b.)Administer oxygen using a mask. c.)Place the woman flat on her back with her legs raised. d.)Ensure adequate hydration before the anesthetic is administered. 98. A woman in labor shouts to the nurse, "My baby is coming right now! I feel like I have to push!" An immediate nursing assessment reveals that the head of the fetus is crowning. After asking another staff member to notify the physician and setting up for delivery, which nursing intervention is most appropriate? a.)Gently pulling at the neonate 's head as it's delivered b.)Holding the neonate 's head back until the physician arrives c.)Applying gentle pressure to the neonate 's head as it's delivered d.)Placing the mother in a Trendelenburg position until the physician arrives 99. The nurse is caring for a client who is in labor. The physician still isn't present. After the neonate's head is delivered, which nursing intervention would be most appropriate? a.)Checking for the umbilical cord around the neonate 's neck b.)Placing antibiotic ointment in the neonate 's eyes c.)Turning the neonate's head to the side, to drain secretions d.)Assessing the neonate for respirations 100. The nurse is caring for a client during the first postpartum day. The client asks the nurse how to relieve pain from her episiotomy. What should the nurse instruct the woman to do? a.)Apply an ice pack to her perineum. b.)Take a Sitz bath. c.)Perform perineal care after voiding or a bowel movement. d.)Drink plenty of fluids. [Show More]
Last updated: 1 year ago
Preview 1 out of 110 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$12.00
Document information
Connected school, study & course
About the document
Uploaded On
Jun 19, 2020
Number of pages
110
Written in
Additional information
This document has been written for:
Uploaded
Jun 19, 2020
Downloads
0
Views
248


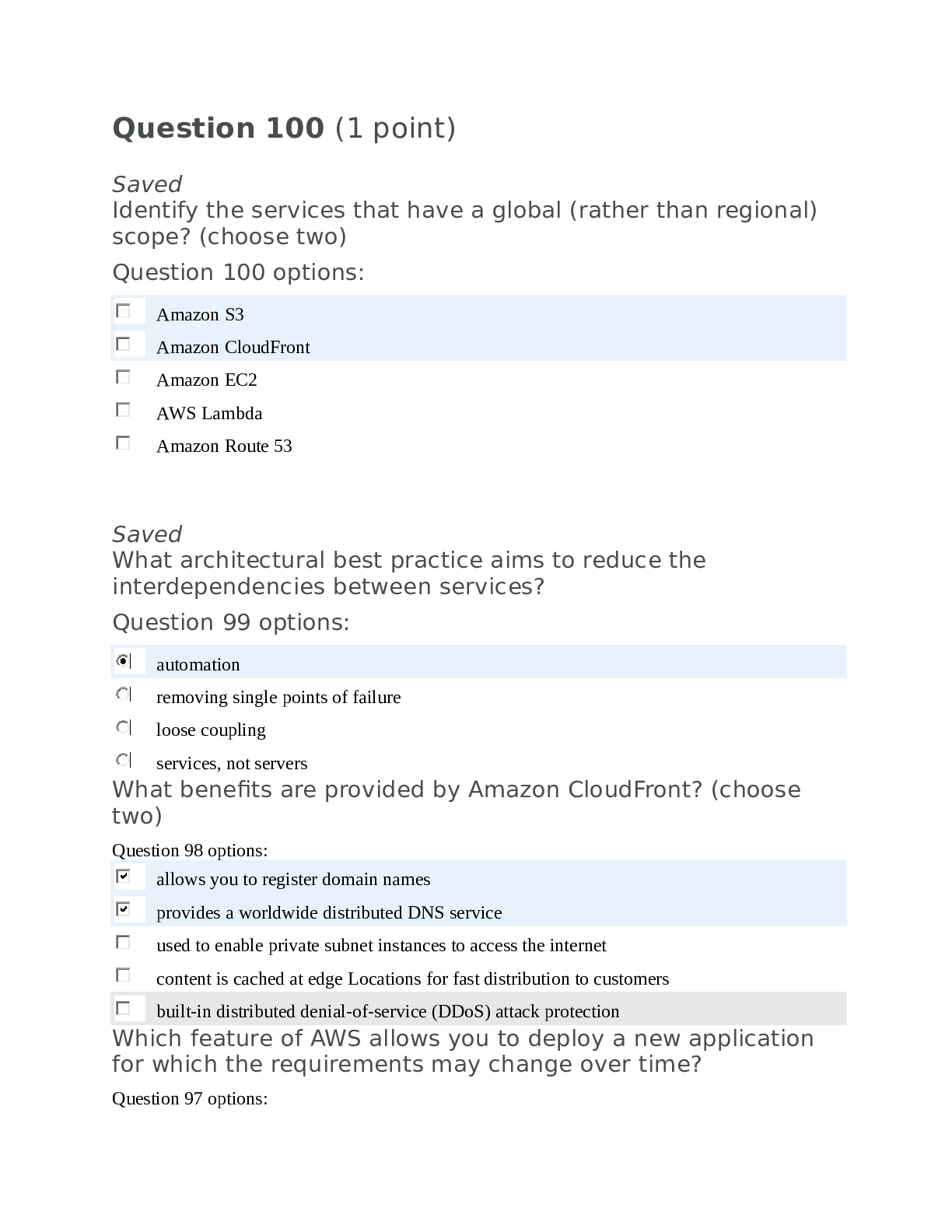
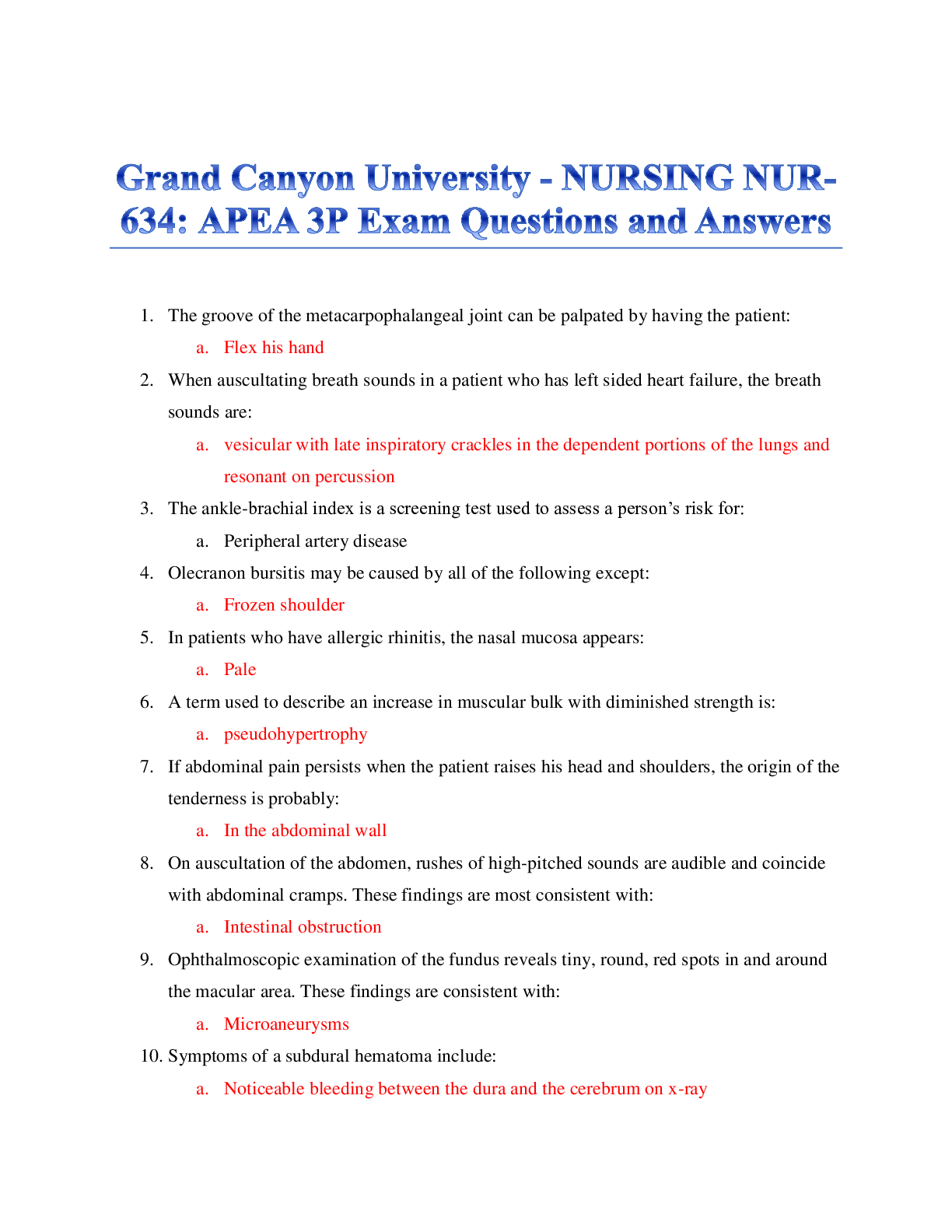
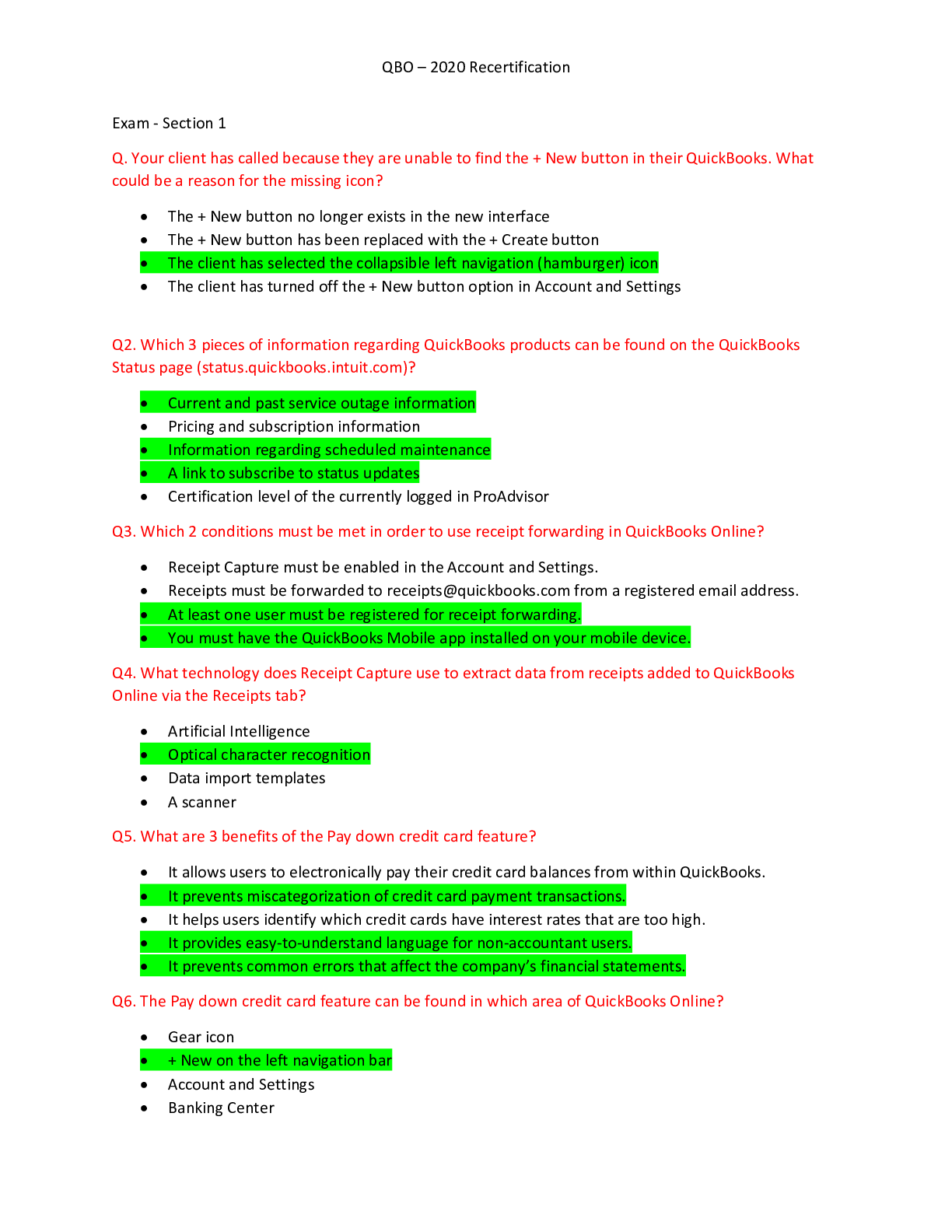


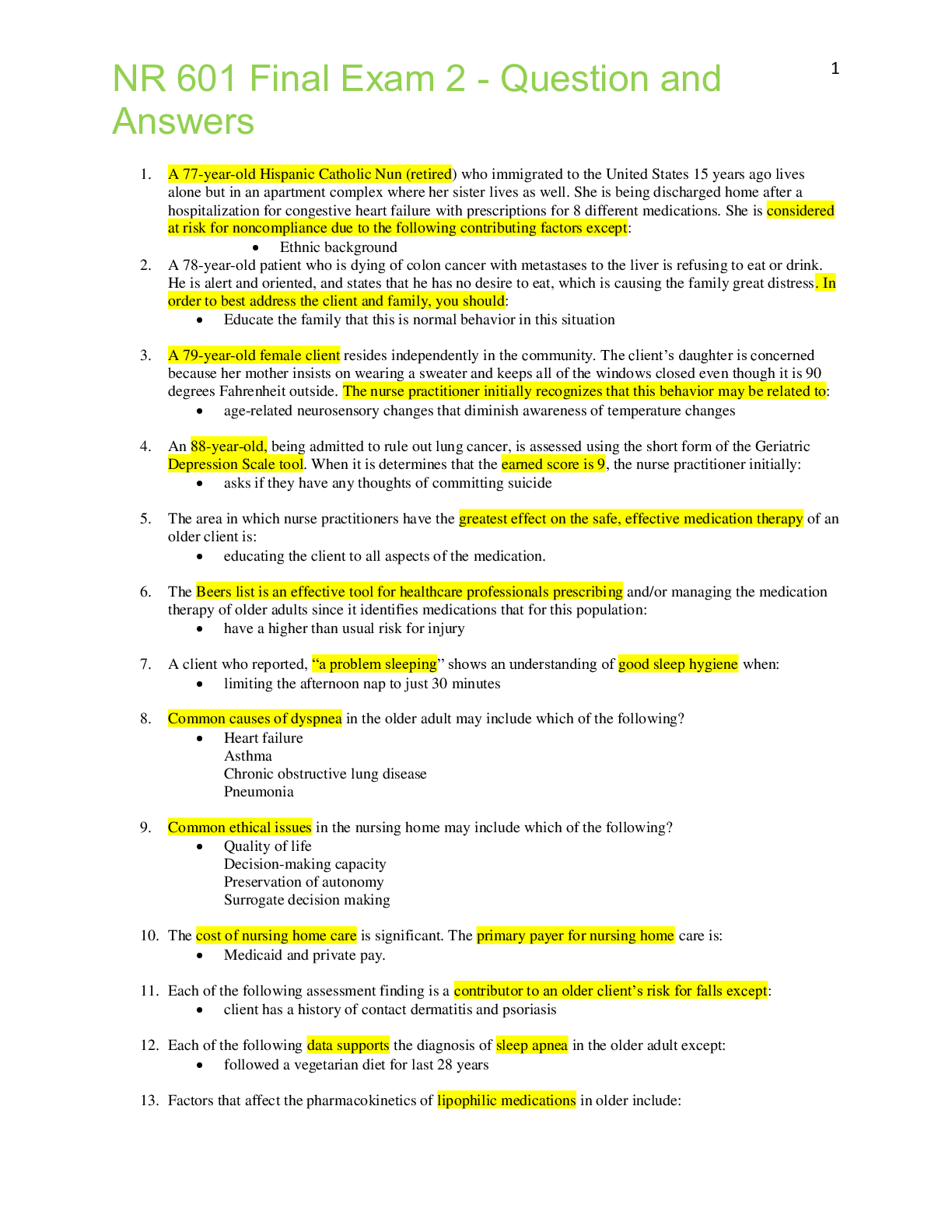
.png)
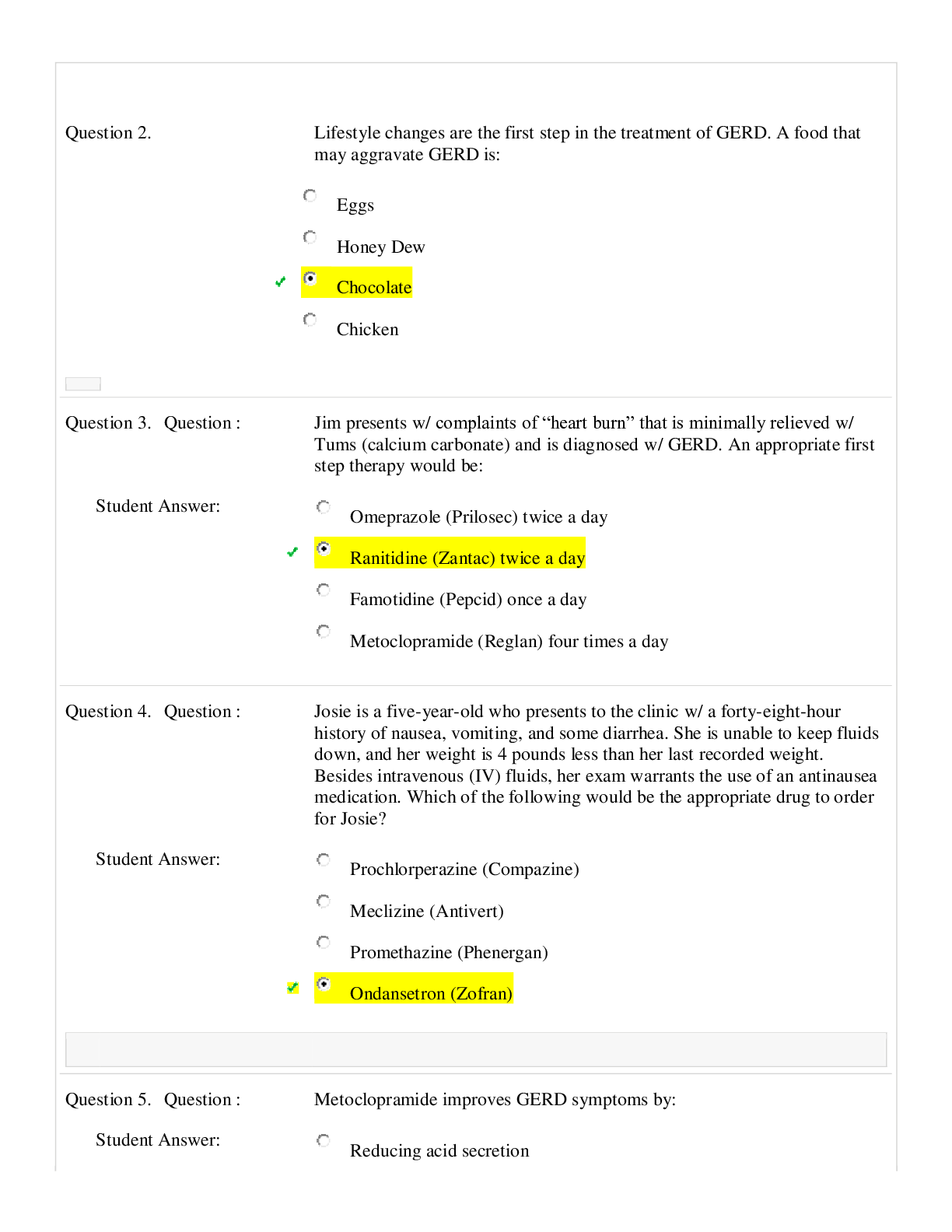
.png)