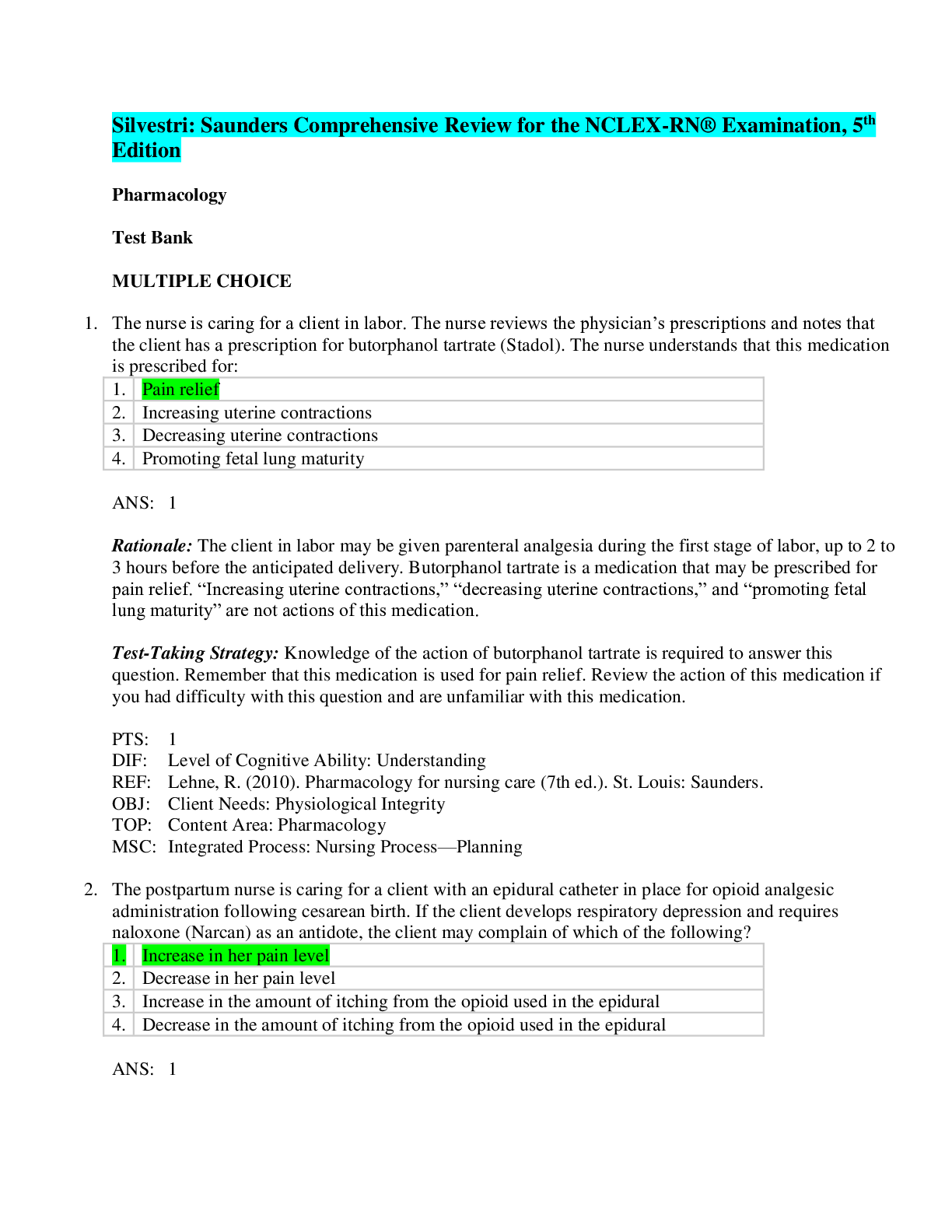
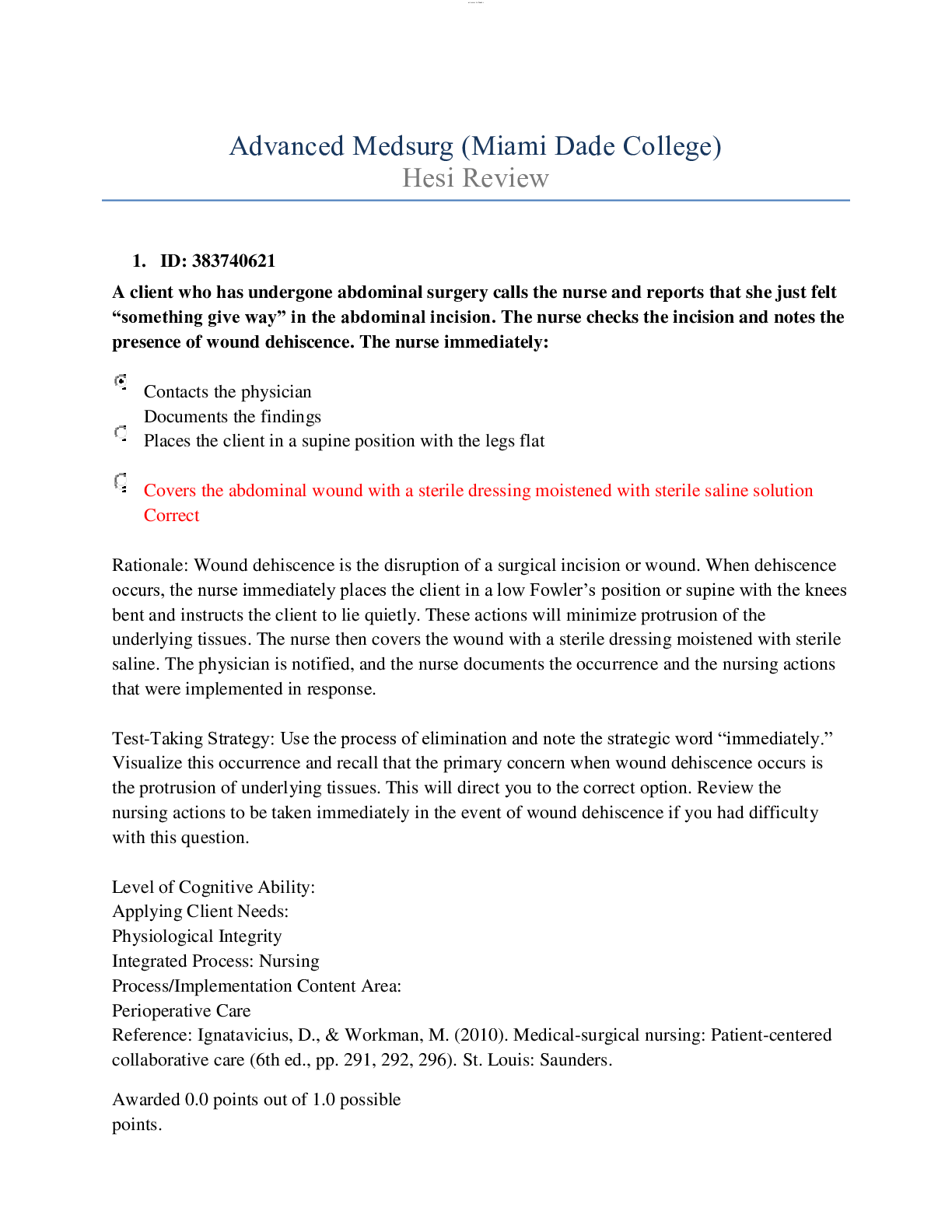
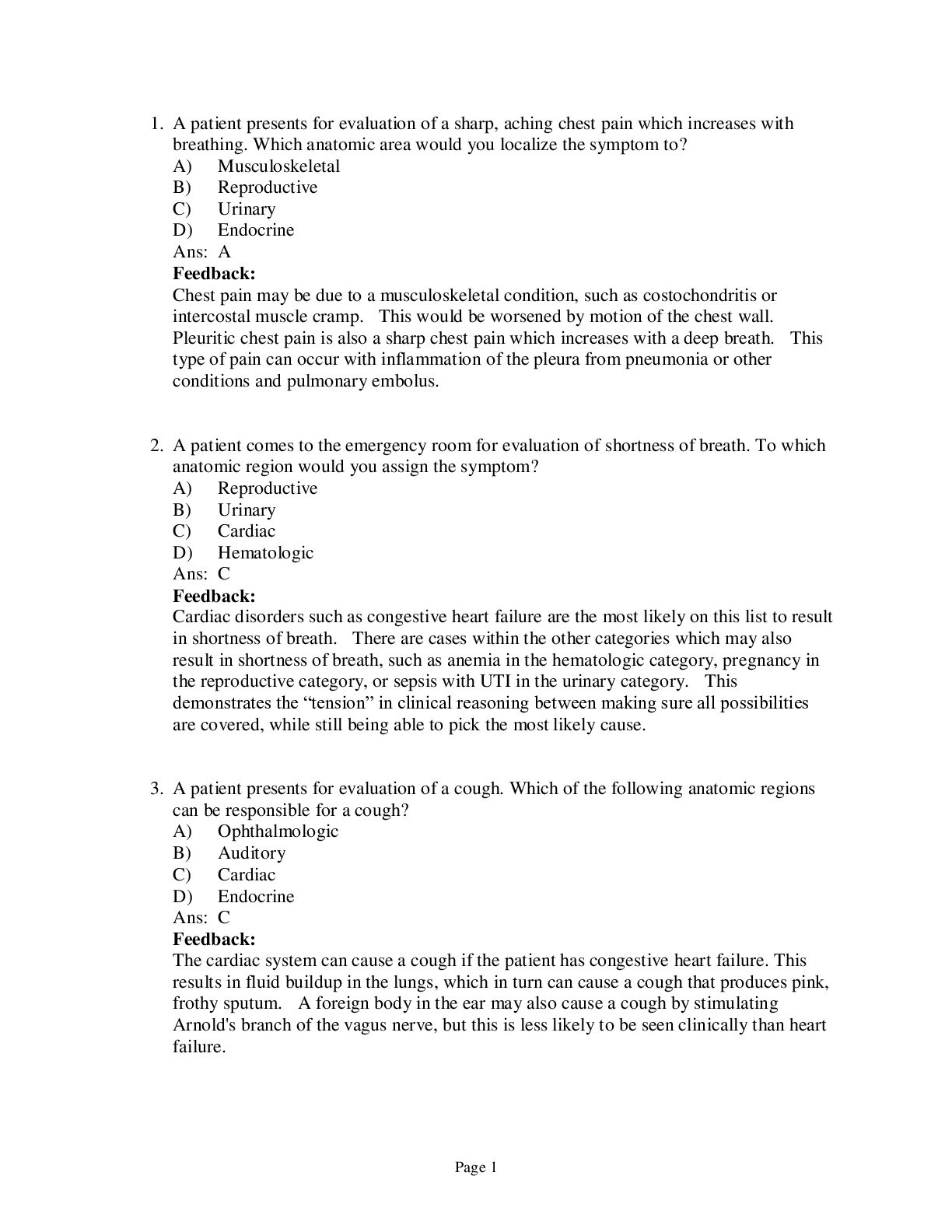
*NURSING > QUESTIONS & ANSWERS > Saunders Comprehensive Review for the NCLEX-RN® Examination - E-Book (Saunders Comprehensive Review (All)
Saunders Comprehensive Review for the NCLEX-RN® Examination - E-Book (Saunders Comprehensive Review for NCLEX-RN. 991 Questions and Answers with Rationale
Document Content and Description Below
Practice Questions and Answers The ambulatory care nurse is discussing preoperative procedures with a Japanese American client who is scheduled for surgery the following week. During the discussion, ... the client continually smiles and nods the head. How should the nurse interpret this nonverbal behavior? 1. Reflecting a cultural value 2. An acceptance of the treatment 3. Client agreement to the required procedures 4. Client understanding of the preoperative procedures 2. When communicating with a client who speaks a different language, which best practice should the nurse implement? 1. Speak loudly and slowly. 2. Arrange for an interpreter to translate. 3. Speak to the client and family together. 4. Stand close to the client and speak loudly. 3. The nurse educator is providing in-service education to the nursing staff regarding transcultural nursing care; a staff member asks the nurse educator to provide an example ofthe concept ofacculturation. The nurse educator should make which most appropriate response? 1. “A group of individuals identifying as a part of the Iroquois tribe among Native Americans.” 2. “A person who moves from China to the United States (U.S.) and learns about and adapts to the culture in the U.S.” 3. “A group of individuals living in the Azores that identify autonomously but are a part of the larger population of Portugal.” 4. “A person who has grown up in the Philippines and chooses to stay there because of the sense of belonging to his or her cultural group.” 4. The nurse is providing discharge instructions to a Chinese American client regarding prescribed dietary modifications. During the teaching session, the client continuously turns away from the nurse. The nurse should implement which best action? 1. Continue with the instructions, verifying client understanding. 2. Walk around the client so that the nurse constantly faces the client. 3. Give the client a dietary booklet and return later to continue with the instructions. 4. Tell the client about the importance of the instructions for the maintenance of health care. 5. A critically ill Hispanic client tells the nurse through an interpreter that she is Roman Catholic and firmly believes in the rituals and traditions of the Catholic faith. Based on the client’s statements, which actions by the nurse demonstrate cultural sensitivity and spiritual support? Select all that apply. 1. Ensures that a close kin stays with the client. 2. Makes a referral for a Catholic priest to visit the client. 3. Removes the crucifix from the wall in the client’s room. 4. Administers the sacrament of the sick to the client if death is imminent. 5. Offers to provide a means for praying the rosary if the client wishes. 6. Reminds the dietary department that meals served on Fridays during Lent do not contain meat. 6. Which clients have a high risk of obesity and diabetes mellitus? Select all that apply. 1. Latino American man 2. Native American man 3. Asian American woman 4. Hispanic American man 5. African American woman 7. The nurse is preparing a plan of care for a client, and is asking the client about religious preferences. The nurse considers the client’s religious preferences as being characteristic of a Jehovah’s Witness if which client statement is made? 1. “I cannot have surgery.” 2. “I cannot have any medicine.” 3. “I believe the soul lives on after death.” 4. “I cannot have any food containing or prepared with blood.” 8. Which meal tray should the nurse deliver to a client of Orthodox Judaism faith who follows a kosher diet? 1. Pork roast, rice, vegetables, mixed fruit, milk 2. Crab salad on a croissant, vegetables with dip, potato salad, milk 3. Sweet and sour chicken with rice and vegetables, mixed fruit, juice 4. Noodles and cream sauce with shrimp and vegetables, salad, mixed fruit, iced tea 40 UNIT II Professional Standards in Nursing 9. An Asian American client is experiencing a fever. The nurse plans care so that the client can self-treat the disorder using which method? 1. Prayer 2. Magnetic therapy 3. Foods considered to be yin 4. Foods considered to be yang 10. Which is the best nursing intervention regarding complementary and alternative medicine? 1. Advising the client about “good” versus “bad” therapies 2. Discouraging the client from using any alternative therapies 3. Educating the client about therapies that he or she is using or is interested in using 4. Identifying herbal remedies that the client should request from the health care provider 11. An antihypertensive medication has been prescribed for a client with hypertension. The client tells the clinic nurse that he would like to take an herbal substance to help lower his blood pressure. The nurse should take which action? 1. Advise the client to read the labels of herbal therapies closely. 2. Tell the client that herbal substances are not safe and should never be used. 3. Encourage the client to discuss the use of an herbal substance with the health care provider (HCP). 4. Tell the client that if he takes the herbal substance he will need to have his blood pressure checked frequently. 12. The nurse educator asks a student to list the 5 main categories of complementary and alternative medicine (CAM), developed by the National Center for Complementary and Alternative Medicine. Which statement, if made by the nursing student, indicates a need for further teaching regarding CAM categories? 1. “CAM includes biologically based practices.” 2. “Whole medical systems are a component of CAM.” 3. “Mind-body medicine is part of the CAM approach.” 4. “Magnetic therapy and massage therapy are a focus of CAM.” 13. The nurse hears a client calling out for help, hurries down the hallway to the client’s room, and finds the client lying on the floor. The nurse performs an assessment, assists the client back to bed, notifies the health care provider of the incident, and completes an incident report. Which statement should the nurse document on the incident report? 1. The client fell out of bed. 2. The client climbed over the side rails. 3. The client was found lying on the floor. 4. The client became restless and tried to get out of bed. 14. A client is brought to the emergency department by emergency medical services (EMS) after being hit by a car. The name of the client is unknown, and the client has sustained a severe head injury and multiple fractures and is unconscious. An emergency craniotomy is required. Regarding informed consent for the surgical procedure, which is the best action? 1. Obtain a court order for the surgical procedure. 2. Ask the EMS team to sign the informed consent. 3. Transport the victim to the operating room for surgery. 4. Call the police to identify the client and locate the family. 15. The nurse has just assisted a client back to bed after a fall. The nurse and health care provider have assessed the client and have determined that the client is not 54 UNIT II Professional Standards in Nursing injured. After completing the incident report, the nurse should implement which action next? 1. Reassess the client. 2. Conduct a staff meeting to describe the fall. 3. Document in the nurse’s notes that an incident report was completed. 4. Contact the nursing supervisor to update information regarding the fall. 16. The nurse arrives at work and is told to report (float) to the intensive care unit (ICU) for the day because the ICU is understaffed and needs additional nurses to care for the clients. The nurse has never worked in the ICU. The nurse should take which best action? 1. Refuse to float to the ICU based on lack of unit orientation. 2. Clarify with the team leader to make a safe ICU client assignment. 3. Ask the nursing supervisor to review the hospital policy on floating. 4. Submit a written protest to nursing administration, and then call the hospital lawyer. 17. The nurse who works on the night shift enters the medication room and finds a co-worker with a tourniquet wrapped around the upper arm. The co-worker is about to insert a needle, attached to a syringe containing a clear liquid, into the antecubital area. Which is the most appropriate action by the nurse? 1. Call security. 2. Call the police. 3. Call the nursing supervisor. 4. Lock the co-worker in the medication room until help is obtained. 18. A hospitalized client tells the nurse that an instructional directive is being prepared and that the lawyer will be bringing the document to the hospital today for witness signatures. The client asks the nurse for assistance in obtaining a witness to the will. Which is the most appropriate response to the client? 1. “I will sign as a witness to your signature.” 2. “You will need to find a witness on your own.” 3. “Whoever is available at the time will sign as a witness for you.” 4. “I will call the nursing supervisor to seek assistance regarding your request.” 19. The nurse has made an error in a narrative documentation of an assessment finding on a client and obtains the client’s record to correct the error. The nurse should take which actions to correct the error? Select all that apply. 1. Document a late entry in the client’s record. 2. Draw 1 line through the error, initialing and dating it. 3. Try to erase the error for space to write in the correct data. 4. Use whiteout to delete the error to write in the correct data. 5. Write a concise statement to explain why the correction was needed. 6. Document the correct information and end with the nurse’s signature and title. 20. Which identifies accurate nursing documentation notations? Select all that apply. 1. The client slept through the night. 2. Abdominal wound dressing is dry and intact without drainage. 3. The client seemed angry when awakened for vital sign measurement. 4. The client appears to become anxious when it is time for respiratory treatments. 5. The client’s left lower medial leg wound is 3 cm in length without redness, drainage, or edema. 21. Anursing instructor delivers a lecture to nursing students regarding the issue of client’s rights and asks a nursing student to identify a situation that represents an example of invasion of client privacy. Which situation, if identified by the student, indicates an understanding of a violation of this client right? 1. Performing a procedure without consent 2. Threatening to give a client a medication 3. Telling the client that he or she cannot leave the hospital 4. Observing care provided to the client without the client’s permission 22. Nursing staff members are sitting in the lounge taking their morning break. An unlicensed assistive personnel (UAP) tells the group that she thinks that the unit secretary has acquired immunodeficiency syndrome (AIDS) and proceeds to tell the nursing staff that the secretary probably contracted the disease from her husband, who is supposedly a drug addict. The registered nurse should inform the UAP that making this accusation has violated which legal tort? 1. Libel 2. Slander 3. Assault 4. Negligence 23. An 87-year-old woman is brought to the emergency department for treatment of a fractured arm. On physical assessment, the nurse notes old and new ecchymotic areas on the client’s chest and legs and asks the client how the bruises were sustained. The client, although reluctant, tells the nurse in confidence that her son frequently hits her if supper is not prepared on time when he arrives home from Fundamentals CHAPTER 6 Ethical and Legal Issues 55 work. Which is the most appropriate nursing response? 1. “Oh, really? I will discuss this situation with your son.” 2. “Let’s talk about the ways you can manage your time to prevent this from happening.” 3. “Do you have any friends who can help you out until you resolve these important issues with your son?” 4. “As a nurse, I am legally bound to report abuse. I will stay with you while you give the report and help find a safe place for you to stay.” 24. The nurse calls the heath care provider (HCP) regarding a new medication prescription because the dosage prescribed is higher than the recommended dosage. The nurse is unable to locate the HCP, and the medication is due to be administered. Which action should the nurse take? 1. Contact the nursing supervisor. 2. Administer the dose prescribed. 3. Hold the medication until the HCP can be contacted. 4. Administer the recommended dose until the HCP can be located. 25. The nurse employed in a hospital is waiting to receive a report from the laboratory via the facsimile (fax) machine. The fax machine activates and the nurse expects the report, but instead receives a sexually oriented photograph. Which is the most appropriate initial nursing action? 1. Call the police. 2. Cut up the photograph and throw it away. 3. Call the nursingsupervisor and report the incident. 4. Call the laboratory and ask for the name of the individual who sent the photograph. 26. The nurse is assigned to care for four clients. In planning client rounds, which client should the nurse assess first? 1. A postoperative client preparing for discharge with a new medication 2. A client requiring daily dressing changes of a recent surgical incision 3. A client scheduled for a chest x-ray after insertion of a nasogastric tube 4. A client with asthma who requested a breathing treatment during the previous shift 27. The nurse employed in an emergency department is assigned to triage clients coming to the emergency department for treatment on the evening shift. The nurse should assign priority to which client? 1. A client complaining of muscle aches, a headache, and history of seizures 2. A client who twisted her ankle when rollerblading and is requesting medication for pain 3. A client with a minor laceration on the index finger sustained while cutting an eggplant 4. Aclient with chest pain who states that he just ate pizza that was made with a very spicy sauce 28. Anursing graduate is attending an agency orientation regarding the nursing model of practice implemented in the health care facility. The nurse is told that the nursing model is a team nursing approach. The nurse determines that which scenario is characteristic of the team-based model of nursing practice? 1. Each staff member is assigned a specific task for a group of clients. 2. A staff member is assigned to determine the client’s needs at home and begin discharge planning. 3. A single registered nurse (RN) is responsible for providing care to a group of 6 clients with the aid of an unlicensed assistive personnel (UAP). 4. An RN leads 2 licensed practical nurses (LPNs) and 3 UAPs in providing care to a group of 12 clients. 29. The nurse has received the assignment for the day shift. After making initial rounds and checking all of the assigned clients, which client should the nurse plan to care for first? 1. A client who is ambulatory demonstrating steady gait 2. A postoperative client who has just received an opioid pain medication 3. A client scheduled for physical therapy for the first crutch-walking session 4. A client with a white blood cell count of 14,000 mm 3 (14Â109/L) and a temperature of 38.4 °C 30. The nurse is giving a bed bath to an assigned client when an unlicensed assistive personnel (UAP) enters the client’s room and tells the nurse that another assigned client is in pain and needs pain medication. Which is the most appropriate nursing action? 1. Finish the bed bath and then administer the pain medication to the other client. 2. Ask the UAP to find out when the last pain medication was given to the client. 3. Ask the UAP to tell the client in pain that medication will be administered as soon as the bed bath is complete. 4. Cover the client, raise the side rails, tell the client that you will return shortly, and administer the pain medication to the other client. 31. The nurse manager has implemented a change in the method of the nursing delivery system from functional to team nursing. An unlicensed assistive personnel (UAP) is resistant to the change and is not taking an active part in facilitating the process of change. Which is the best approach in dealing with the UAP? 1. Ignore the resistance. 2. Exert coercion on the UAP. 3. Provide a positive reward system for the UAP. 4. Confront the UAP to encourage verbalization of feelings regarding the change. 32. The registered nurse is planning the client assignments for the day. Which is the most appropriate assignment for an unlicensed assistive personnel (UAP)? 1. A client requiring a colostomy irrigation 2. A client receiving continuous tube feedings 3. A client who requires urine specimen collections 4. A client with difficulty swallowing food and fluids 33. The nurse manager is discussing the facility protocol in the event of a tornado with the staff. Which instructions should the nurse manager include in the discussion? Select all that apply. 1. Open doors to client rooms. 2. Move beds away from windows. 3. Close window shades and curtains. 4. Place blankets over clients who are confined to bed. 5. Relocate ambulatory clients from the hallways back into their rooms. 34. The nurse employed in a long-term care facility is planning assignments for the clients on a nursing unit. The nurse needs to assign four clients and has a licensed practical (vocational) nurse and 3 unlicensed assistive personnel (UAPs) on a nursing Fundamentals 72 UNIT II Professional Standards in Nursing team. Which client would the nurse most appropriately assign to the licensed practical (vocational) nurse? 1. A client who requires a bed bath 2. An older client requiring frequent ambulation 3. A client who requires hourly vital sign measurements 4. A client requiring abdominal wound irrigations and dressing changes every 3 hours 35. The charge nurse is planning the assignment for the day. Which factors should the nurse remain mindful of when planning the assignment? Select all that apply. 1. The acuity level of the clients 2. Specific requests from the staff 3. The clustering of the rooms on the unit 4. The number of anticipated client discharges 5. Client needs and workers’ needs and abilities 36. The nurse is caring for a client with heart failure. On assessment, the nurse notes that the client is dyspneic, and crackles are audible on auscultation. What additional manifestations would the nurse expect to note in this client if excess fluid volume is present? 1. Weight loss and dry skin 2. Flat neck and hand veins and decreased urinary output 3. An increase in blood pressure and increased respirations 4. Weakness and decreased central venous pressure (CVP) 37. The nurse is preparing to care for a client with a potassium deficit. The nurse reviews the client’s record and determines that the client is at risk for developing the potassium deficit because of which situation? 1. Sustained tissue damage 2. Requires nasogastric suction 3. Has a history of Addison’s disease 4. Uric acid level of 9.4 mg/dL (559 µmol/L) 38. The nurse reviews a client’s electrolyte laboratory report and notes that the potassium level is 2.5 mEq/L (2.5 mmol/L). Which patterns should the nurse watch for on the electrocardiogram (ECG) as a result of the laboratory value? Select all that apply. 1. U waves 2. Absent P waves 3. Inverted T waves 4. Depressed ST segment 5. Widened QRS complex CHAPTER 8 Fluids and Electrolytes 91 Fundamentals 39. Potassium chloride intravenously is prescribed for a client with hypokalemia. Which actions should the nurse take to plan for preparation and administration of the potassium? Select all that apply. 1. Obtain an intravenous (IV) infusion pump. 2. Monitor urine output during administration. 3. Prepare the medication for bolus administration. 4. Monitor the IV site for signs of infiltration or phlebitis. 5. Ensure that the medication is diluted in the appropriate volume of fluid. 6. Ensure that the bag is labeled so that it reads the volume of potassium in the solution. 40. The nurse provides instructions to a client with a low potassium level about the foods that are high in potassium and tells the client to consume which foods? Select all that apply. 1. Peas 2. Raisins 3. Potatoes 4. Cantaloupe 5. Cauliflower 6. Strawberries 41. The nurse is reviewing laboratory results and notes that a client’s serum sodium level is 150 mEq/L (150 mmol/L). The nurse reports the serum sodium level to the health care provider (HCP) and the HCP prescribes dietary instructions based on the sodium level. Which acceptable food items does the nurse instruct the client to consume? Select all that apply. 1. Peas 2. Nuts 3. Cheese 4. Cauliflower 5. Processed oat cereals 42. The nurse is assessing a client with a suspected diagnosis of hypocalcemia. Which clinical manifestation would the nurse expect to note in the client? 1. Twitching 2. Hypoactive bowel sounds 3. Negative Trousseau’s sign 4. Hypoactive deep tendon reflexes 43. The nurse is caring for a client with hypocalcemia. Which patterns would the nurse watch for on the electrocardiogram as a result of the laboratory value? Select all that apply. 1. U waves 2. Widened T wave 3. Prominent U wave 4. Prolonged QT interval 5. Prolonged ST segment 44. The nurse reviews the electrolyte results of an assigned client and notes that the potassium level is 5.7 mEq/L (5.7 mmol/L). Which patterns would the nurse watch for on the cardiac monitor as a result of the laboratory value? Select all that apply. 1. ST depression 2. Prominent U wave 3. Tall peaked T waves 4. Prolonged ST segment 5. Widened QRS complexes 45. Which client is at risk for the development of a sodium level at 130 mEq/L (130 mmol/L)? 1. The client who is taking diuretics 2. The client with hyperaldosteronism 3. The client with Cushing’s syndrome 4. The client who is taking corticosteroids 46. The nurse is caring for a client with heart failure who is receiving high doses of a diuretic. On assessment, the nurse notes that the client has flat neck veins, generalized muscle weakness, and diminished deep tendon reflexes. The nurse suspects hyponatremia. What additional signs would the nurse expect to note in a client with hyponatremia? 1. Muscle twitches 2. Decreased urinary output 3. Hyperactive bowel sounds 4. Increased specific gravity of the urine 47. The nurse reviews a client’s laboratory report and notes that the client’s serum phosphorus (phosphate) level is 1.8 mg/dL (0.45 mmol/L). Which condition most likely caused this serum phosphorus level? 1. Malnutrition 2. Renal insufficiency 3. Hypoparathyroidism 4. Tumor lysis syndrome 48. The nurse is reading a health care provider’s (HCP’s) progress notes in the client’s record and reads that the HCP has documented “insensible fluid loss of approximately 800 mL daily.” The nurse makes a notation that insensible fluid loss occurs through which type of excretion? 1. Urinary output 2. Wound drainage 3. Integumentary output 4. The gastrointestinal tract 49. The nurse is assigned to care for a group of clients. On review of the clients’ medical records, the nurse determines that which client is most likely at risk for a fluid volume deficit? 1. A client with an ileostomy 2. A client with heart failure 92 UNIT III Nursing Sciences 3. A client on long-term corticosteroid therapy 4. A client receiving frequent wound irrigations 50. The nurse caring for a client who has been receiving intravenous (IV) diuretics suspects that the client is experiencing a fluid volume deficit. Which assessment finding would the nurse note in a client with this condition? 1. Weight loss and poor skin turgor 2. Lung congestion and increased heart rate 3. Decreased hematocrit and increased urine output 4. Increased respirations and increased blood pressure 51. On review of the clients’ medical records, the nurse determines that which client is at risk for fluid volume excess? 1. The client taking diuretics and has tenting of the skin 2. The client with an ileostomy from a recent abdominal surgery 3. The client who requires intermittent gastrointestinal suctioning 4. The client with kidney disease and a 12-year history of diabetes mellitus 52. Which client is at risk for the development of a potassium level of 5.5 mEq/L (5.5 mmol/L)? 1. The client with colitis 2. The client with Cushing’s syndrome 3. The client who has been overusing laxatives 4. The client who has sustained a traumatic burn 53. The nurse reviews the arterial blood gas results of a client and notes the following: pH 7.45, PaCO2 of 30 mm Hg (30 mm Hg), and HCO 3 À of 20 mEq/L (20 mmol/L). The nurse analyzes these results as indicating which condition? 1. Metabolic acidosis, compensated 2. Respiratory alkalosis, compensated 3. Metabolic alkalosis, uncompensated 4. Respiratory acidosis, uncompensated 54. The nurse is caring for a client with a nasogastric tube that is attached to low suction. The nurse monitors the client for manifestations of which disorder that the client is at risk for? 1. Metabolic acidosis 2. Metabolic alkalosis 3. Respiratory acidosis 4. Respiratory alkalosis 55. A client with a 3-day history of nausea and vomiting presents to the emergency department. The client is hypoventilating and has a respiratory rate of 10 breaths/minute. The electrocardiogram (ECG) monitor displays tachycardia, with a heart rate of 120 beats/ minute. Arterial blood gases are drawn and the nurse reviews the results, expecting to note which finding? 1. A decreased pH and an increased PaCO 2 2. An increased pH and a decreased PaCO 2 3. A decreased pH and a decreased HCO 3 À 4. An increased pH and an increased HCO 3 À 56. The nurse is caring for a client having respiratory distress related to an anxiety attack. Recent arterial blood gas values are pH ¼7.53, PaO2¼72 mm Hg (72 mm Hg), PaCO2 ¼32 mm Hg (32 mm Hg), and HCO 3 À ¼28 mEq/L(28 mmol/L). Which conclusion about the client should the nurse make? 1. The client has acidotic blood. 2. The client is probably overreacting. 3. The client is fluid volume overloaded. 4. The client is probably hyperventilating. 57. The nurse is caring for a client with diabetic ketoacidosis and documents that the client is experiencing Kussmaul’s respirations. Which patterns did the nurse observe? Select all th at apply. 1. Respirations that are shallow 2. Respirations that are increased in rate 3. Respirations that are abnormally slow 4. Respirations that are abnormally deep 5. Respirations that cease for several seconds 58. A client who is found unresponsive has arterial blood gases drawn and the results indicate the following: pH is 7.12, PaCO2 is 90 mm Hg (90 mm Hg), and HCO 3 À is 22 mEq/L (22 mmol/L). The nurse interprets the results as indicating which condition? 1. Metabolic acidosis with compensation 2. Respiratory acidosis with compensation 3. Metabolic acidosis without compensation 4. Respiratory acidosis without compensation BOX 9-5 Analyzing Arterial Blood Gas Results If you can remember the following Pyramid Points and Pyramid Steps, you will be able to analyze any blood gas report. Pyramid Points In acidosis, the pH is decreased. In alkalosis, the pH is elevated. The respiratory function indicator is the PaCO2. The metabolic function indicator is the bicarbonate ion (HCO3À). Pyramid Steps Pyramid Step 1 Look at the blood gas report. Look at the pH. Is the pH elevated or decreased? If the pH is elevated, it reflects alkalosis. If the pH is decreased, it reflects acidosis. Pyramid Step 2 Look at the PaCO2. Is the PaCO2 elevated or decreased? If the PaCO2 reflects an opposite relationship to the pH, the condition is a respiratory imbalance. If the PaCO2 does not reflect an opposite relationship to the pH, go to Pyramid Step 3. Pyramid Step 3 Look at the HCO3À. Does the HCO3À reflect a corresponding relationship with the pH? If it does, the condition is a metabolic imbalance. Pyramid Step 4 Full compensation has occurred ifthe pH is in a normal range of 7.35 to 7.45. If the pH is not within normal range, look at the respiratory or metabolic function indicators. If the condition is a respiratory imbalance, look at the HCO3À to determine the state of compensation. If the condition is a metabolic imbalance, look at the PaCO2 to determine the state of compensation. 104 UNIT III Nursing Sciences Fundamentals 59. The nurse notes that a client’s arterial blood gas (ABG) results reveal a pH of 7.50 and a PaCO2 of 30 mm Hg (30 mm Hg). The nurse monitors the client for which clinical manifestations associated with these ABG results? Select all that apply. 1. Nausea 2. Confusion 3. Bradypnea 4. Tachycardia 5. Hyperkalemia 6. Lightheadedness 60. The nurse reviews the blood gas results of a client with atelectasis. The nurse analyzes the results and determines that the client is experiencing respiratory acidosis. Which result validates the nurse’s findings? 1. pH 7.25, PaCO2 50 mm Hg (50 mm Hg) 2. pH 7.35, PaCO2 40 mm Hg (40 mm Hg) 3. pH 7.50, PaCO2 52 mm Hg (52 mm Hg) 4. pH 7.52, PaCO2 28 mm Hg (28 mm Hg) 61. The nurse is caring for a client who is on a mechanical ventilator. Blood gas results indicate a pH of 7.50 and a PaCO2 of 30 mm Hg (30 mm Hg). The nurse has determined that the client is experiencing respiratory alkalosis. Which laboratory value would most likely be noted in this condition? 1. Sodium level of 145 mEq/L (145 mmol/L) 2. Potassium level of 3.0 mEq/L (3.0 mmol/L) 3. Magnesium level of 1.3 mEq/L (0.65 mmol/L) 4. Phosphorus level of 3.0 mg/dL (0.97 mmol/L) 62. The nurse is caring for a client with several broken ribs. The client is most likely to experience what type of acid-base imbalance? 1. Respiratory acidosis from inadequate ventilation 2. Respiratory alkalosis from anxiety and hyperventilation 3. Metabolic acidosis from calcium loss due to broken bones 4. Metabolic alkalosis from taking analgesics containing base products 63. A client with atrial fibrillation who is receiving maintenance therapy of warfarin sodium has a prothrombin time (PT) of 35 (35) seconds and an international normalized ratio (INR) of 3.5. On the basis of these laboratory values, the nurse anticipates which prescription? 1. Adding a dose of heparin sodium 2. Holding the next dose of warfarin 3. Increasing the next dose of warfarin 4. Administering the next dose of warfarin 64. A staff nurse is precepting a new graduate nurse and the new graduate is assigned to care for a client with chronic pain. Which statement, if made by the new graduate nurse, indicates the need for further teachin g regarding pain management? 1. “I will be sure to ask my client what his pain level is on a scale of 0 to 10.” 2. “I know that I should follow up after giving medication to make sure it is effective.” 3. “I know that pain in the older client might manifest as sleep disturbances or depression.” 4. “I will be sure to cue in to any indicators that the client may be exaggerating their pain.” 65. A client has been admitted to the hospital for urinary tract infection and dehydration. The nurse determines that the client has received adequate volume replacement if the blood urea nitrogen (BUN) level drops to which value? 1. 3 mg/dL (1.05 mmol/L) 2. 15 mg/dL (5.25 mmol/L) 3. 29 mg/dL (10.15 mmol/L) 4. 35 mg/dL (12.25 mmol/L) 66. The nurse is explaining the appropriate methods for measuring an accurate temperature to an unlicensed assistive personnel (UAP). Which method, if noted by the UAP as being an appropriate method, indicates the need for further teaching? 1. Taking a rectal temperature for a client who has undergone nasal surgery 2. Taking an oral temperature for a client with a cough and nasal congestion 3. Taking an axillary temperature for a client who has just consumed hot coffee 4. Taking a temporal temperature on the neck behind the ear for a client who is diaphoretic 67. A client is receiving a continuous intravenous infusion of heparin sodium to treat deep vein thrombosis. The client’s activated partial thromboplastin time (aPTT) is 65 seconds (65 seconds). The nurse anticipates that which action is needed? 1. Discontinuing the heparin infusion 2. Increasing the rate of the heparin infusion 3. Decreasing the rate of the heparin infusion 4. Leaving the rate of the heparin infusion as is 68. A client with a history of cardiac disease is due for a morning dose of furosemide. Which serum potassium level, if noted in the client’s laboratory report, should be reported before administering the dose of furosemide? 1. 3.2 mEq/L (3.2 mmol/L) 2. 3.8 mEq/L (3.8 mmol/L) 3. 4.2 mEq/L (4.2 mmol/L) 4. 4.8 mEq/L (4.8 mmol/L) 69. Several laboratory tests are prescribed for a client, and the nurse reviews the results of the tests. Which laboratory test results should the nurse report? Select all that apply. 1. Platelets 35,000 mm 3 (35 Â 109/L) 2. Sodium 150 mEq/L (150 mmol/L) 3. Potassium 5.0 mEq/L (5.0 mmol/L) 4. Segmented neutrophils 40% (0.40) 5. Serum creatinine, 1 mg/dL (88.3 µmol/L) 6. White blood cells, 3000 mm 3 (3.0 Â 109/L) Fundamentals CHAPTER 10 Vital Signs and Laboratory Reference Intervals 119 Fundamentals 70. The nurse is caring for a client who takes ibuprofen for pain. The nurse is gathering information on the client’s medication history, and determines it is necessary to contact the health care provider (HCP) if the client is also taking which medications? Select all that apply. 1. Warfarin 2. Glimepiride 3. Amlodipine 4. Simvastatin 5. Hydrochlorothiazide 71. A client with diabetes mellitus has a glycosylated hemoglobin A1c level of 9%. On the basis of this test result, the nurse plans to teach the client about the need for which measure? 1. Avoiding infection 2. Taking in adequate fluids 3. Preventing and recognizing hypoglycemia 4. Preventing and recognizing hyperglycemia 72. The nurse is caring for a client with a diagnosis of cancer who is immunosuppressed. The nurse would consider implementing neutropenic precautions if the client’s white blood cell count was which value? 1. 2000 mm 3 (2.0 Â 109/L) 2. 5800 mm 3 (5.8 Â 109/L) 3. 8400 mm 3 (8.4 Â 109/L) 4. 11,500 mm 3 (11.5 Â 109/L) 73. Aclient brought to the emergency department states that he has accidentally been taking 2 times his prescribed dose of warfarin for the past week. After noting that the client has no evidence of obvious bleeding, the nurse plans to take which action? 1. Prepare to administer an antidote. 2. Draw a sample for type and crossmatch and transfuse the client. 3. Draw a sample for an activated partial thromboplastin time (aPTT) level. 4. Draw a sample for prothrombin time (PT) and international normalized ratio (INR). 74. The nurse is caring for a postoperative client who is receiving demand-dose hydromorphone via a patient-controlled analgesia (PCA) pump for pain control. The nurse enters the client’s room and finds the client drowsy and records the following vital signs: temperature 97.2 °F (36.2 °C) orally, pulse 52 beats per minute, blood pressure 101/58 mm Hg, respiratory rate 11 breaths per minute, and SpO 2 of 93% on 3 liters of oxygen via nasal cannula. Which action should the nurse take next? 1. Document the findings. 2. Attempt to arouse the client. 3. Contact the health care provider (HCP) immediately. 4. Check the medication administration history on the PCA pump. 75. An adult female client has a hemoglobin level of 10.8 g/dL (108 mmol/L). The nurse interprets that this result is most likely caused by which condition noted in the client’s history? 1. Dehydration 2. Heart failure 3. Iron deficiency anemia 4. Chronic obstructive pulmonary disease 76. A client with a history of gastrointestinal bleeding has a platelet count of 300,000 mm 3 (300 Â 109/L). The nurse should take which action after seeing the laboratory results? 1. Report the abnormally low count. 2. Report the abnormally high count. 3. Place the client on bleeding precautions. 4. Place the normal report in the client’s medical record. 77. The nurse is teaching a client who has iron deficiency anemia about foods she should include in the diet. The nurse determines that the client understands the dietary modifications if which items are selected from the m enu? 1. Nuts and milk 2. Coffee and tea 3. Cooked rolled oats and fish 4. Oranges and dark green leafy vegetables 78. The nurse is planning to teach a client with m alabsorption syndrome about the necessity of following a low-fat diet. The nurse develops a list of high-fat foods to avoid and should include which food items on the list? Select all th at apply. 1. Oranges 2. Broccoli 3. Margarine 4. Cream cheese 5. Luncheon meats 6. Broiled haddock 79. The nurse instructs a client with chronic kidney disease who is receiving hemodialysis about dietary modifications. The nurse determines that the client understands these dietary modifications if the client selects which items from the dietary menu? 1. Cream of wheat, blueberries, coffee 2. Sausage and eggs, banana, orange juice 3. Bacon, cantaloupe melon, tomato juice 4. Cured pork, grits, strawberries, orange juice 80. The nurse is conducting a dietary assessment on a client who is on a vegan diet. The nurse provides dietary teaching and should focus on foods high in which vitamin that may be lacking in a vegan diet? Fundamentals 130 UNIT III Nursing Sciences 1. Vitamin A 2. Vitamin B12 3. Vitamin C 4. Vitamin E 81. A client with hypertension has been told to maintain a diet low in sodium. The nurse who is teaching this client about foods that are allowed should include which food item in a list provided to the client? 1. Tomato soup 2. Boiled shrimp 3. Instant oatmeal 4. Summer squash 82. Apostoperative client has been placed on a clear liquid diet. The nurse should provide the client with which items that are allowed to be consumed on this diet? Select all that apply. 1. Broth 2. Coffee 3. Gelatin 4. Pudding 5. Vegetable juice 6. Pureed vegetables 83. The nurse is instructing a client with hypertension on the importance of choosing foods low in sodium. The nurse should teach the client to limit intake of which food? 1. Apples 2. Bananas 3. Smoked sausage 4. Steamed vegetables 84. A client who is recovering from surgery has been advanced from a clear liquid diet to a full liquid diet. The client is looking forward to the diet change because he has been “bored” with the clear liquid diet. The nurse should offer which full liquid item to the client? 1. Tea 2. Gelatin 3. Custard 4. Ice pop 85. Aclient is recovering from abdominal surgery and has a large abdominal wound. The nurse should encourage the client to eat which food item that is naturally high in vitamin C to promote wound healing? 1. Milk 2. Oranges 3. Bananas 4. Chicken 86. The nurse is caring for a client with cirrhosis of the liver. To minimize the effects of the disorder, the nurse teaches the client about foods that are high in thiamine. The nurse determines that the client has the best understanding of the dietary measures to follow if the client states an intention to increase the intake of which food? 1. Milk 2. Chicken 3. Broccoli 4. Legumes 87. A client is being weaned from parenteral nutrition (PN) and is expected to begin taking solid food today. The ongoing solution rate has been 100 mL/hour. The nurse anticipates that which Fundamentals BOX 12-2 Home Care Instructions Teach the client and caregiver how to obtain, administer, and maintain parenteral nutrition fluids. Teach the client and caregiver how to change a sterile dressing. Obtain a daily weight at the same time of day in the same clothes. Stress that if a weight gain of more than 3 lb/week is noted, this may indicate excessive fluid intake and should be reported. Monitor the blood glucose level and report abnormalities immediately. Teach the client how to monitor for and manage hypoglycemia and hyperglycemia. Teach the client and caregiver about the signs and symptoms of side effects or adverse effects such as infection, thrombosis, air embolism, and catheter displacement. Teach the client and caregiver the actions to take if a complication arises and about the importance of reporting complications to the health care provider. For signs and symptoms of thrombosis, the client should report edema of the arm or at the catheter insertion site, neck pain, and jugular vein distention. Leaking of fluid from the insertion site or pain or discomfort as the fluids are infused may indicate displacement of the catheter; this must be reported immediately. Encourage the client and caregiver to contact the health care provider if theyhave questions about administration or any other questions. Inform the client and caregiver about the importance of follow-up care. Teach the client to keep electronic infusion devices fully CRITICAL THINKING What Should You Do? charged in case of electrical power failure. Answer: Difficultywith flushing the catheter indicates that the catheter is partially or fully blocked. Possible causes of a blockage include a clamped or kinked catheter, the tip of the catheter against the vein wall, thrombosis, or a precipitate buildup in the lumen. The nurse should not try to force the flushing because this could dislodge a clot or disrupt the integrity of the catheter. If the catheter becomes fully blocked, it may not be usable. The nurse should assess for and alleviate clamping or kinking. The nurse should also instruct the client to change position, raise the arm, and cough. If the blockage is due to a positional issue, this intervention will correct it. The nurse should attempt to flush again to see if the problem has been corrected. If it has not, this difficulty should be reported to the necessary personnel (i.e., health care provider or intravenous nurse) so that full functionality can be regained. Fluoroscopy may be performed to determine the cause of the blockage and anticoagulant or thrombolytic medications may be instilled into the catheter as prescribed to alleviate blockage. References: Lewis et al. (2014), p. 312; Perry, Potter, Ostendorf (2014), p. 504. 138 UNIT III Nursing Sciences Fundamentals prescription regarding the PN solution will accompany the diet prescription? 1. Discontinue the PN. 2. Decrease PN rate to 50 mL/hour. 3. Start 0.9% normal saline at 25 mL/hour. 4. Continue current infusion rate prescriptions for PN. 88. The nurse is preparing to change the parenteral nutrition (PN) solution bag and tubing. The client’s central venous line is located in the right subclavian vein. The nurse asks the client to take which essen tial action during the tubing change? 1. Breathe normally. 2. Turn the head to the right. 3. Exhale slowly and evenly. 4. Take a deep breath, hold it, and bear down. 89. A client with parenteral nutrition (PN) infusing has disconnected the tubing from the central line catheter. The nurse assesses the client and suspects an air embolism. The nurse should immediately place the client in which position? 1. On the left side, with the head lower than the feet 2. On the left side, with the head higher than the feet 3. On the right side, with the head lower than the feet 4. On the right side, with the head higher than the feet 90. Which nursing action is essential prior to initiating a new prescription for 500 mL of fat emulsion (lipids) to infuse at 50 mL/hour? 1. Ensure that the client does not have diabetes. 2. Determine whether the client has an allergy to eggs. 3. Add regular insulin to the fat emulsion, using aseptic technique. 4. Contact the health care provider (HCP) to have a central line inserted for fat emulsion infusion. 91. The nurse monitors the client receiving parenteral nutrition (PN) for complications of the therapy and should assess the client for which manifestations of hyperglycemia? 1. Fever, weak pulse, and thirst 2. Nausea, vomiting, and oliguria 3. Sweating, chills, and abdominal pain 4. Weakness, thirst, and increased urine output 92. The nurse is changing the central line dressing of a client receiving parenteral nutrition (PN) and notes that the catheter insertion site appears reddened. The nurse should next assess which item? 1. Client’s temperature 2. Expiration date on the bag 3. Time of last dressing change 4. Tightness of tubing connections 93. The nurse is preparing to hang fat emulsion (lipids) and notes that fat globules are visible at the top of the solution. The nurse should take which action? 1. Roll the bottle of solution gently. 2. Obtain a different bottle of solution. 3. Shake the bottle of solution vigorously. 4. Run the bottle of solution under warm water. 94. A client receiving parenteral nutrition (PN) suddenly develops a fever. The nurse notifies the health care provider (HCP), and the HCP initially prescribes that the solution and tubing be changed. What should the nurse do with the discontinued materials? 1. Discard them in the unit trash. 2. Return them to the hospital pharmacy. 3. Save them for return to the manufacturer. 4. Prepare to send them to the laboratory for culture. 95. A client has been discharged to home on parenteral nutrition (PN). With each visit, the home care nurse should assess which parameter most closely in monitoring this therapy? 1. Pulse and weight 2. Temperature and weight 3. Pulse and blood pressure 4. Temperature and blood pressure 96. The nurse, caring for a group of adult clients on an acute care medical-surgical nursing unit, determines that which clientswould be the most likelycandidates for parenteral nutrition (PN)? Select all that apply. 1. A client with extensive burns 2. A client with cancer who is septic 3. Aclient who has had an open cholecystectomy 4. A client with severe exacerbation of Crohn’s disease 5. A client with persistent nausea and vomiting from chemotherapy 97. The nurse is preparing to hang the first bag of parenteral nutrition (PN) solution via the central line of an assigned client. The nurse should obtain which most essential piece of equipment before hanging the solution? 1. Urine test strips 2. Blood glucose meter 3. Electronic infusion pump 4. Noninvasive blood pressure monitor 98. The nurse is making initial rounds at the beginning of the shift and notes that the parenteral nutrition (PN) bag of an assigned client is empty. Which solution should the nurse hang until another PN solution is mixed and delivered to the nursing unit? 1. 5% dextrose in water 2. 10% dextrose in water 3. 5% dextrose in Ringer’s lactate 4. 5% dextrose in 0.9% sodium chloride CHAPTER 12 Parenteral Nutrition 139 Fundamentals 99. The nurse is monitoring the status of a client’s fat emulsion (lipid) infusion and notes that the infusion is 1 hour behind. Which action should the nurse take? 1. Adjust the infusion rate to catch up over the next hour. 2. Increase the infusion rate to catch up over the next 2 hours. 3. Ensure that the fat emulsion infusion rate is infusing at the prescribed rate. 4. Adjust the infusion rate to run wide open until the solution is back on time. 100. A client receiving parenteral nutrition (PN) in the home setting has a weight gain of 5 lb in 1 week. The nurse should next assess the client for the presence of which condition? 1. Thirst 2. Polyuria 3. Decreased blood pressure 4. Crackles on auscultation of the lungs 101. The nurse is caring for a restless client who is beginning nutritional therapy with parenteral nutrition (PN). The nurse should plan to ensure that which action is taken to prevent the client from sustaining injury? 1. Calculate daily intake and output. 2. Monitor the temperature once daily. 3. Secure all connections in the PN system. 4. Monitor blood glucose levels every 12 hours. 102. A client receiving parenteral nutrition (PN) complains of a headache. The nurse notes that the client has an increased blood pressure, bounding pulse, jugular vein distention, and crackles bilaterally. The nurse determines that the client is experiencing which complication of PN therapy? 1. Sepsis 2. Air embolism 3. Hypervolemia 4. Hyperglycemia 103. A client had a 1000-mL bag of 5% dextrose in 0.9% sodium chloride hung at 1500. The nurse making rounds at 1545 finds that the client is complaining of a pounding headache and is dyspneic, experiencing chills, and apprehensive, with an increased pulse rate. The intravenous (IV) bag has 400 mL remaining. The nurse should take which action first? 1. Slow the IV infusion. 2. Sit the client up in bed. 3. Remove the IV catheter. 4. Call the health care provider (HCP). 104. The nurse has a prescription to hang a 1000-mL intravenous (IV) bag of 5% dextrose in water with 20 mEq of potassium chloride. The nurse also needs to hang an IV infusion of piperacillin/ Skeletal vertebra Epidural catheter FIGURE 13-7 Tunneled epidural catheter. CHAPTER 13 Intravenous Therapy 153 Fundamentals tazobactam. The client has one IV site. The nurse should plan to take which action first? 1. Start a second IV site. 2. Check compatibility of the medication and IV fluids. 3. Mix the prepackaged piperacillin/tazobactam per agency policy. 4. Prime the tubing with the IVsolution, and backprime the medication. 105. The nurse is completing a time tape for a 1000-mL intravenous (IV) bag that is scheduled to infuse over 8 hours. The nurse has just placed the 1100 marking at the 500-mL level. The nurse would place the mark for 1200 at which numerical level (mL) on the time tape? Fill in the blank. Answer: ______ mL 106. The nurse is making initial rounds on the nursing unit to assess the condition of assigned clients. Which assessment findings are consistent with infiltration? Select all that apply. 1. Pain and erythema 2. Pallor and coolness 3. Numbness and pain 4. Edema and blanched skin 5. Formation of a red streak and purulent drainage 107. The nurse is inserting an intravenous (IV) line into a client’s vein. After the initial stick, the nurse would continue to advance the catheter in which situation? 1. The catheter advances easily. 2. The vein is distended under the needle. 3. The client does not complain of discomfort. 4. Blood return shows in the backflash chamber of the catheter. 108. The nurse is assessing a client’s peripheral intravenous (IV) site after completion of a vancomycin infusion and notes that the area is reddened, warm, painful, and slightly edematous proximal to the insertion point of the IV catheter. At this time, which action by the nurse is best? 1. Check for the presence of blood return. 2. Remove the IV site and restart at another site. 3. Document the findings and continue to monitor the IV site. 4. Call the health care provider (HCP) and request that the vancomycin be given orally. 109. The nurse is preparing a continuous intravenous (IV) infusion at the medication cart. As the nurse goes to insert the spike end of the IV tubing into the IV bag, the tubing drops and the spike end hits the top of the medication cart. The nurse should take which action? 1. Obtain a new IV bag. 2. Obtain new IV tubing. 3. Wipe the spike end of the tubing with povidone iodine. 4. Scrub the spike end of the tubing with an alcohol swab. 110. A health care provider has written a prescription to discontinue an intravenous (IV) line. The nurse should obtain which item from the unit supply area for applying pressure to the site after removing the IV catheter? 1. Elastic wrap 2. Povidone iodine swab 3. Adhesive bandage 4. Sterile 2 Â 2 gauze 111. A client rings the call light and complains of pain at the site of an intravenous (IV) infusion. The nurse assesses the site and determines that phlebitis has developed. The nurse should take which actions in the care of this client? Select all that apply. 1. Remove the IV catheter at that site. 2. Apply warm moist packs to the site. 3. Notify the health care provider (HCP). 4. Start a new IV line in a proximal portion of the same vein. 5. Document the occurrence, actions taken, and the client’s response. 112. A client involved in a motor vehicle crash presents to the emergency department with severe internal bleeding. The client is severely hypotensive and unresponsive. The nurse anticipates that which intravenous (IV) solution will most likely be prescribed for this client? 1. 5% dextrose in lactated Ringer’s solution 2. 0.33% sodium chloride (1/3 normal saline) 3. 0.45% sodium chloride (1/2 normal saline) 4. 0.225% sodium chloride (1/4 normal saline) 113. The nurse provides a list of instructions to a client being discharged to home with a peripherally inserted central catheter (PICC). The nurse determines that the client needs further instructions if the client made which statement? 1. “I need to wear a MedicAlert tag or bracelet.” 2. “I need to restrict my activity while this catheter is in place.” 3. “I need to keep the insertion site protected when in the shower or bath.” 4. “I need to check the markings on the catheter each time the dressing is changed.” 114. A client has just undergone insertion of a central venous catheter at the bedside under ultrasound. The nurse would be sure to check which results 154 UNIT III Nursing Sciences before initiating the flow rate of the client’s intravenous (IV) solution at 100 mL/hour? 1. Serum osmolality 2. Serum electrolyte levels 3. Intake and output record 4. Chest radiology results 115. Intravenous (IV) fluids have been infusing at 100 mL/hour via a central line catheter in the right internal jugular for approximately 24 hours to increase urine output and maintain the client’s blood pressure. Upon entering the client’s room, the nurse notes that the client is breathing rapidly and coughing. For which additional signs of a complication should the nurse assess based on the previously known data? 1. Excessive bleeding 2. Crackles in the lungs 3. Incompatibility of the infusion 4. Chest pain radiating to the left arm 116. Packed red blood cells have been prescribed for a female client with a hemoglobin level of 7.6 g/dL (76 mmol/L) and a hematocrit level of 30% (0.30). The nurse takes the client’s temperature before hanging the blood transfusion and records 100.6 °F (38.1 °C) orally. Which action should the nurse take? 1. Begin the transfusion as prescribed. 2. Administer an antihistamine and begin the transfusion. 3. Delay hanging the blood and notify the health care provider (HCP). 4. Administer 2 tablets of acetaminophen and begin the transfusion. 117. The nurse has received a prescription to transfuse a client with a unit of packed red blood cells. Before explaining the procedure to the client, the nurse should ask which initial question? 1. “Have you ever had a transfusion before?” 2. “Why do you think that you need the transfusion?” 3. “Have you ever gone into shock for any reason in the past?” 4. “Do you know the complications and risks of a transfusion?” 118. Aclient receiving a transfusion of packed red blood cells (PRBCs) begins to vomit. The client’s blood pressure is 90/50 mm Hg from a baseline of 125/ 78 mm Hg. The client’s temperature is 100.8 °F CHAPTER 14 Administration of Blood Products 163 (38.2 °C) orally from a baseline of 99.2 °F (37.3 °C) orally. The nurse determines that the client may be experiencing which complication of a blood transfusion? 1. Septicemia 2. Hyperkalemia 3. Circulatory overload 4. Delayed transfusion reaction 119. The nurse determines that a client is having a transfusion reaction. After the nurse stops the transfusion, which action should be taken next? 1. Remove the intravenous (IV) line. 2. Run a solution of 5% dextrose in water. 3. Run normal saline at a keep-vein-open rate. 4. Obtain a culture of the tip of the catheter device removed from the client. 120. The nurse has just received a unit of packed red blood cells from the blood bank for transfusion to an assigned client. The nurse is careful to select tubing especially made for blood products, knowing that this tubing is manufactured with which item? Refer to figures 1-4. 1. 2. 3. 4. 121. A client has received a transfusion of platelets. The nurse evaluates that the client is benefiting most from this therapy if the client exhibits which finding? 1. Increased hematocrit level 2. Increased hemoglobin level 3. Decline of elevated temperature to normal 4. Decreased oozing of blood from puncture sites and gums 122. The nurse has obtained a unit of blood from the blood bank and has checked the blood bag properly with another nurse. Just before beginning the transfusion, the nurse should assess which priority item? 1. Vital signs 2. Skin color 3. Urine output 4. Latest hematocrit level 123. The nurse has just received a prescription to transfuse a unit of packed red blood cells for an assigned client. What action should the nurse take next? 1. Check a set of vital signs. 2. Order the blood from the blood bank. 3. Obtain Y-site blood administration tubing. 4. Check to be sure that consent for the transfusion has been signed. 124. Following infusion of a unit of packed red blood cells, the client has developed new onset of tachycardia, bounding pulses, crackles, and wheezes. Which action should the nurse implement first? 1. Maintain bed rest with legs elevated. 2. Place the client in high-Fowler’s position. 3. Increase the rate of infusion of intravenous fluids. 4. Consult with the health care provider (HCP) regarding initiation of oxygen therapy. 125. The nurse, listening to the morning report, learns that an assigned client received a unit of granulocytes the previous evening. The nurse makes a note to assess the results of which daily serum laboratory studies to assess the effectiveness of the transfusion? 1. Hematocrit level 2. Erythrocyte count 3. Hemoglobin level 4. White blood cell count 126. A client is brought to the emergency department having experienced blood loss related to an arterial laceration. Which blood component should the nurse expect the health care provider to prescribe? 1. Platelets 2. Granulocytes 3. Fresh-frozen plasma 4. Packed red blood cells 127. The nurse who is about to begin a blood transfusion knows that blood cells start to deteriorate after Fundamentals 164 UNIT III Nursing Sciences a certain period of time. The nurse takes which actions in order to prevent a complication of the blood transfusion as it relates to deterioration of blood cells? Select all that apply. 1. Checks the expiration date 2. Inspects for the presence of clots 3. Checks the blood group and type 4. Checks the blood identification number 5. Hangs the blood within the specified time frame per agency policy 128. A client requiring surgery is anxious about the possible need for a blood transfusion during or after the procedure. The nurse suggests to the client to take which actions to reduce the risk of possible transfusion complications? Select all that apply. 1. Ask a family member to donate blood ahead of time. 2. Give an autologous blood donation before the surgery. 3. Take iron supplements before surgery to boost hemoglobin levels. 4. Request that any donated blood be screened twice by the blood bank. 5. Take adequate amounts of vitamin C several days prior to the surgery date. 129. A client with severe blood loss resulting from multiple trauma requires rapid transfusion of several units of blood. The nurse asks another health team member to obtain which device for use during the transfusion procedure to help reduce the risk of cardiac dysrhythmias? 1. Infusion pump 2. Pulse oximeter 3. Cardiac monitor 4. Blood-warming device 130. A client has a prescription to receive a unit of packed red blood cells. The nurse should obtain which intravenous (IV) solution from the IV storage area to hang with the blood product at the client’s bedside? 1. Lactated Ringer’s 2. 0.9% sodium chloride 3. 5% dextrose in 0.9% sodium chloride 4. 5% dextrose in 0.45% sodium chloride 131. The nurse is caring for a client who is receiving a blood transfusion and is complaining of a cough. The nurse checks the client’s vital signs, which include temperature of 97.2 °F (36.2 °C), pulse of 108 beats per minute, blood pressure of 152/ 76 mm Hg, respiratory rate of 24 breaths per minute, and an oxygen saturation level of 95% on room air. The client denies pain at this time. Based on this information, what initial action should the nurse take? 1. Collect a urine sample for analysis. 2. Place the client in an upright position. 3. Compare current data to baseline data. 4. Slow the rate of the blood transfusion. 132. A Spanish-speaking client arrives at the triage desk in the emergency department and states to the nurse, “No speak English, need interpreter.” Which is the best action for the nurse to take? 1. Have one ofthe client’s family members interpret. 2. Have the Spanish-speaking triage receptionist interpret. 3. Page an interpreter from the hospital’s interpreter services. 4. Obtain a Spanish-English dictionary and attempt to triage the client. 133. The nurse is performing a neurological assessment on a client and elicits a positive Romberg’s sign. The nurse makes this determination based on which observation? 1. An involuntary rhythmic, rapid, twitching of the eyeballs 2. A dorsiflexion of the ankle and great toe with fanning of the other toes 3. A significant sway when the client stands erect with feet together, arms at the side, and the eyes closed 4. A lack of normal sense of position when the client is unable to return extended fingers to a point of reference 134. The nurse notes documentation that a client is exhibiting Cheyne-Stokes respirations. On assessment of the client, the nurse should expect to note which finding? 1. Rhythmic respirations with periods of apnea 2. Regular rapid and deep, sustained respirations 3. Totally irregular respiration in rhythm and depth 4. Irregular respirations with pauses at the end of inspiration and expiration 135. A client diagnosed with conductive hearing loss asks the nurse to explain the cause of the hearing problem. The nurse plans to explain to the client that this condition is caused by which problem? 1. A defect in the cochlea 2. A defect in cranial nerve VIII 3. A physical obstruction to the transmission of sound waves 4. A defect in the sensory fibers that lead to the cerebral cortex 136. While performing a cardiac assessment on a client with an incompetent heart valve, the nurse auscultates a murmur. The nurse documents the finding and describes the sound as which? 1. Lub-dub sounds 2. Scratchy, leathery heart noise 3. A blowing or swooshing noise 4. Abrupt, high-pitched snapping noise 137. The nurse is testing the extraocular movements in a client to assess for muscle weakness in the eyes. The nurse should implement which assessment technique to assess for muscle weakness in the eye? 1. Test the corneal reflexes. 2. Test the 6 cardinal positions of gaze. 3. Test visual acuity, using a Snellen eye chart. 4. Test sensory function by asking the client to close the eyes and then lightly touching the forehead, cheeks, and chin. 138. The nurse is instructing a client how to perform a testicular self-examination (TSE). The nurse should explain that which is the best time to perform this exam? 1. After a shower or bath 2. While standing to void 3. After having a bowel movement 4. While lying in bed before arising 139. The nurse is assessing a client for meningeal irritation and elicits a positive Brudzinski’s sign. Which finding did the nurse observe? 1. The client rigidly extends the arms with pronated forearms and plantar flexion of the feet. 2. The client flexes a leg at the hip and knee and reports pain in the vertebral column when the leg is extended. 3. The client passively flexes the hip and knee in response to neck flexion and reports pain in the vertebral column. 4. The client’s upper arms are flexed and held tightly to the sides of the body and the legs are extended and internally rotated. 188 UNIT IV Fundamentals of Care 140. A client with a diagnosis of asthma is admitted to the hospital with respiratory distress. Which type of adventitious lung sounds should the nurse expect to hear when performing a respiratory assessment on this client? 1. Stridor 2. Crackles 3. Wheezes 4. Diminished 141. The clinic nurse prepares to perform a focused assessment on a client who is complaining of symptoms of a cold, a cough, and lung congestion. Which should the nurse include for this type of assessment? Select all that apply. 1. Auscultating lung sounds 2. Obtaining the client’s temperature 3. Assessing the strength of peripheral pulses 4. Obtaining information about the client’s respirations 5. Performing a musculoskeletal and neurological examination 6. Asking the client about a family history of any illness or disease 142. The nurse is preparing to initiate an intravenous (IV) line containing a high dose of potassium chloride and plans to use an IV infusion pump. The nurse brings the pump to the bedside, prepares to plug the pump cord into the wall, and notes that no receptacle is available in the wall socket. The nurse should take which action? 1. Initiate the IV line without the use of a pump. 2. Contact the electrical maintenance department for assistance. 3. Plug in the pump cord in the available plug above the room sink. 4. Use an extension cord from the nurses’ lounge for the pump plug. 143. The nurse obtains a prescription from a health care provider to restrain a client and instructs an unlicensed assistive personnel (UAP) to apply the safety device to the client. Which observation of unsafe application of the safety device would indicate that further instruction is required by the UAP? 1. Placing a safety knot in the safety device straps 2. Safely securing the safety device straps to the side rails 3. Applying safety device straps that do not tighten when force is applied against them 4. Securing so that 2 fingers can slide easily between the safety device and the client’s skin 144. The community health nurse is providing a teaching session about anthrax to members of the community and asks the participants about the methods of transmission. Which answers by the participants would indicate that teaching was effective? Select all that apply. 1. Bites from ticks or deer flies 2. Inhalation of bacterial spores 3. Through a cut or abrasion in the skin 4. Direct contact with an infected individual 5. Sexual contact with an infected individual 6. Ingestion of contaminated undercooked meat 145. The nurse is giving a report to an unlicensed assistive personnel (UAP) who will be caring for a client who has hand restraints (safety devices). The nurse instructs the UAP to check the skin integrity of the restrained hands how frequently? 1. Every 2 hours 2. Every 3 hours 3. Every 4 hours 4. Every 30 minutes 146. The nurse is reviewing a plan of care for a client with an internal radiation implant. Which intervention, if noted in the plan, indicates the need for revision of the plan? 1. Wearing gloves when emptying the client’s bedpan 2. Keeping all linens in the room until the implant is removed 3. Wearing a lead apron when providing direct care to the client 4. Placing the client in a semiprivate room at the end of the hallway 147. Contact precautions are initiated for a client with a health care–associated (nosocomial) infection caused by methicillin-resistant Staphylococcus aureus. The nurse prepares to provide colostomy care and should obtain which protective items to perform this procedure? 1. Gloves and gown 2. Gloves and goggles 3. Gloves, gown, and shoe protectors 4. Gloves, gown, goggles, and a mask or face shield 148. The nurse enters a client’s room and finds that the wastebasket is on fire. The nurse immediately assists the client out of the room. What is the next nursing action? 1. Call for help. 2. Extinguish the fire. 3. Activate the fire alarm. 4. Confine the fire by closing the room door. 149. A mother calls a neighbor who is a nurse and tells the nurse that her 3-year-old child has just ingested liquid furniture polish. The nurse would direct the mother to take which immediate action? 1. Induce vomiting. 2. Call an ambulance. 3. Call the Poison Control Center. 4. Bring the child to the emergency department. 150. The emergency department (ED) nurse receives a telephone call and is informed that a tornado has hit a local residential area and that numerous casualties have occurred. The victims will be brought to the ED. The nurse should take which initial action? 1. Prepare the triage rooms. 2. Activate the emergency response plan. 3. Obtain additional supplies from the central supply department. 4. Obtain additional nursing staff to assist in treating the casualties. Fundamentals 200 UNIT IV Fundamentals of Care 151. The nurse is caring for a client with meningitis and implements which transmission-based precautions for this client? 1. Private room or cohort client 2. Personal respiratory protection device 3. Private room with negative airflow pressure 4. Mask worn by staff when the client needs to leave the room 152. The nurse working in the emergency department (ED) is assessing a client who recently returned from Liberia and presented complaining of a fever at home, fatigue, muscle pain, and abdominal pain. Which action should the nurse take next? 1. Check the client’s temperature. 2. Contact the health care provider. 3. Isolate the client in a private room. 4. Check a complete set of vital signs 153. A health care provider’s prescription reads 1000 mL of normal saline (NS) to infuse over 12 hours. The drop factor is 15 drops (gtt)/1 mL. The nurse prepares to set the flow rate at how many drops per minute? Fill in the blank. Record your answer to the nearest whole number. Answer: _______ drops per minute 154. A health care provider’s prescription reads to administer an intravenous (IV) dose of 400,000 units of penicillin G benzathine. The label on the 10-mL ampule sent from the pharmacy reads penicillin G benzathine, 300,000 units/mL. The nurse prepares how much medication to administer the correct dose? Fill in the blank. Record your answer using 1 decimal place. Answer: _______ mL 155. A health care provider’s prescription reads potassium chloride 30 mEq to be added to 1000 mL normal saline (NS) and to be administered over a 10-hour period. The label on the medication bottle reads 40 mEq/20 mL. The nurse prepares BOX 17-10 Infusions Prescribed by Unit Dosage per Hour Calculation ofthese problems can be done using a 2-step process. 1. Determine the amount of medication per 1 mL. 2. Determine the infusion rate or milliliters per hour. Problem 1 Prescription: Continuous heparin sodium byIVat 1000 units per hour Available: IV bag of 500 mL D5W with 20,000 units of heparin sodium How many milliliters per hour are required to administer the correct dose? Solution Step 1: Calculate the amount of medication (units) per milliliter (mL). Known amount of medication in solution Totalvolume of diluent ¼ Amount of medication permilliliter 20,000 units 500 mL ¼ 40 units=1mL Step 2: Calculate milliliters per hour. Dose per hour desired Concentration permilliliter ¼ Infusion rate, ormL=hour 1000 units 40 units ¼ 25mL=hour Problem 2 Prescription: Continuous regular insulin by IV at 10 units per hour Available: IV bag of 100 mL NS with 50 units regular insulin How many milliliters per hour are required to administer the correct dose? Solution Step 1: Calculate the amount of medication (units) per milliliter. Known amount of medication in solution Totalvolume of diluent ¼ Amount of medication permilliliter 50 units 100 mL ¼ 0:5units=1mL Step 2: Calculate milliliters per hour. Dose per hour desired Concentration permilliliter ¼ Infusion rate, ormL=hour 10 units 0:5units=mL¼ 20 mL=hour CHAPTER 17 Calculation of Medication and Intravenous Prescriptions 209 Fundamentals how many milliliters of potassium chloride to administer the correct dose of medication? Fill in the blank. Answer: _______ mL 156. A health care provider’s prescription reads clindamycin phosphate 0.3 g in 50 mL normal saline (NS) to be administered intravenously over 30 minutes. The medication label reads clindamycin phosphate 900 mg in 6 mL. The nurse prepares how many milliliters of the medication to administer the correct dose? Fill in the blank. Answer: _______ mL 157. A health care provider’s prescription reads phenytoin 0.2 g orally twice daily. The medication label states that each capsule is 100 mg. The nurse prepares how many capsule(s) to administer 1 dose? Fill in the blank. Answer: _______ capsule(s) 158. A health care provider prescribes 1000 mL of normal saline 0.9% to infuse over 8 hours. The drop factor is 15 drops (gtt)/1 mL. The nurse sets the flow rate at how many drops per minute? Fill in the blank. Record your answer to the nearest whole number. Answer: _______ drops per minute 159. A health care provider prescribes heparin sodium, 1300 units/hour by continuous intravenous (IV) infusion. The pharmacy prepares the medication and delivers an IV bag labeled heparin sodium 20,000 units/250 mLD5W. An infusion pump must be used to administer the medication. The nurse sets the infusion pump at how many milliliters per hour to deliver 1300 units/hour? Fill in the blank. Record your answer to the nearest whole number. Answer: _______ mL per hour 160. A health care provider prescribes 3000 mL of D5W to be administered over a 24-hour period. The nurse determines that how many milliliters per hour will be administered to the client? Fill in the blank. Answer: _______ mL per hour 161. Gentamicin sulfate, 80 mg in 100 mL normal saline (NS), is to be administered over 30 minutes. The drop factor is 10 drops (gtt)/1 mL. The nurse sets the flow rate at how many drops per minute? 168. The nurse has just reassessed the condition of a postoperative client who was admitted 1 hour ago to the surgical unit. The nurse plans to monitor which parameter most carefully during the next hour? 1. Urinary output of 20 mL/hour 2. Temperature of 37.6 °C (99.6 °F) 3. Blood pressure of 100/70 mm Hg 4. Serous drainage on the surgical dressing 169. The nurse is teaching a client about coughing and deep-breathing techniques to prevent postoperative complications. Which statement is most appropriate for the nurse to make to the client at this time as it relates to these techniques? 1. “Use of an incentive spirometer will help prevent pneumonia.” 2. “Close monitoring of your oxygen saturation will detect hypoxemia.” 3. “Administration of intravenous fluids will prevent or treat fluid imbalance.” 4. “Early ambulation and administration of blood thinners will prevent pulmonary embolism.” 170. The nurse is creating a plan of care for a client scheduled for surgery. The nurse should include which activity in the nursing care plan for the client on the day of surgery? 1. Avoid oral hygiene and rinsing with mouthwash. 2. Verify that the client has not eaten for the last 24 hours. 3. Have the client void immediately before going into surgery. 4. Report immediately any slight increase in blood pressure or pulse. 171. A client with a gastric ulcer is scheduled for surgery. The client cannot sign the operative consent form because of sedation from opioid analgesics that have been administered. The nurse should take which most appropriate action in the care of this client? 1. Obtain a court order for the surgery. 2. Have the charge nurse sign the informed consent immediately. 3. Send the client to surgery without the consent form being signed. 4. Obtain a telephone consent from a family member, following agency policy. 172. A preoperative client expresses anxiety to the nurse about upcoming surgery. Which response by the nurse is most likely to stimulate further discussion between the client and the nurse? 1. “If it’s any help, everyone is nervous before surgery.” 2. “I will be happy to explain the entire surgical procedure to you.” 3. “Can you share with me what you’ve been told about your surgery?” 4. “Let me tell you about the care you’ll receive after surgery and the amount of pain you can anticipate.” Fundamentals BOX 18-7 Postoperative Discharge Teaching Assess the client’s readiness to learn, educational level, and desire to change or modify lifestyle. Assess the need for resources needed for home care. Demonstrate care of the incision and how to change the dressing. Instruct the client to cover the incision with plastic if showering is allowed. Ensure that the client is provided with a 48-hour supply of dressings for home use. Instruct the client on the importance of returning to the surgeon’s office for follow-up. Instruct the client that sutures usually are removed in the surgeon’s office 7 to 10 days after surgery. Inform the client that staples are removed 7 to 14 days after surgery and that the skin may become slightly reddened when staples are ready to be removed. Sterile adhesive strips (e.g., Steri-Strips®) may be applied to provide extra support after the sutures are removed. Instruct the client on the use of medications, their purpose, dosages, administration, and side effects or adverse effects. Instruct the client on diet and to drink 6 to 8 glasses of liquid a day. Instruct the client about activity levels and to resume normal activities gradually. Instruct the client to avoid lifting for 6 weeks if a major surgical procedure was performed. Instruct the client with an abdominal incision not to lift anything weighing 10 pounds or more and not to engage in any activities that involve pushing or pulling. The client usuallycan return to work in 6 to 8 weeks depending on the procedure and as prescribed by the surgeon. Instruct the client about the signs and symptoms of complications and when to call the surgeon. CHAPTER 18 Perioperative Nursing Care 225 173. The nurse is conducting preoperative teaching with a client about the use of an incentive spirometer. The nurse should include which piece of information in discussions with the client? 1. Inhale as rapidly as possible. 2. Keep a loose seal between the lips and the mouthpiece. 3. After maximum inspiration, hold the breath for 15 seconds and exhale. 4. The best results are achieved when sitting up or with the head of the bed elevated 45 to 90 degrees. 174. The nurse has conducted preoperative teaching for a client scheduled for surgery in 1 week. The client has a history of arthritis and has been taking acetylsalicylic acid. The nurse determines that the client needs additional teaching if the client makes which statement? 1. “Aspirin can cause bleeding after surgery.” 2. “Aspirin can cause my ability to clot blood to be abnormal.” 3. “I need to continue to take the aspirin until the day of surgery.” 4. “I need to check with my health care provider about the need to stop the aspirin before the scheduled surgery.” 175. The nurse assesses a client’s surgical incision for signs of infection. Which finding by the nurse would be interpreted as a normal finding at the surgical site? 1. Red, hard skin 2. Serous drainage 3. Purulent drainage 4. Warm, tender skin 176. The nurse is monitoring the status of a postoperative client in the immediate postoperative period. The nurse would become most concerned with which sign that could indicate an evolving complication? 1. Increasing restlessness 2. A pulse of 86 beats/minute 3. Blood pressure of 110/70 mm Hg 4. Hypoactive bowel sounds in all 4 quadrants 177. Aclient who has had abdominal surgery complains of feeling as though “something gave way” in the incisional site. The nurse removes the dressing and notes the presence of a loop of bowel protruding through the incision. Which interventions should the nurse take? Select all that apply. 1. Contact the surgeon. 2. Instruct the client to remain quiet. 3. Prepare the client for wound closure. 4. Document the findings and actions taken. 5. Place a sterile saline dressing and ice packs over the wound. 6. Place the client in a supine position without a pillow under the head. 178. A client who has undergone preadmission testing has had blood drawn for serum laboratory studies, including a complete blood count, coagulation studies, and electrolytes and creatinine levels. Which laboratory result should be reported to the surgeon’s office by the nurse, knowing that it could cause surgery to be postponed? 1. Hemoglobin, 8.0 g/dL (80 mmol/L) 2. Sodium, 145 mEq/L (145 mmol/L) 3. Serum creatinine, 0.8 mg/dL (70.6 µmol/L) 4. Platelets, 210,000 cells/mm 3 (210 Â 103/µL/ 210 Â 109/L) 179. The nurse receives a telephone call from the postanesthesia care unit stating that a client is being transferred to the surgical unit. The nurse plans to take which action first on arrival of the client? 1. Assess the patency of the airway. 2. Check tubes or drains for patency. 3. Check the dressing to assess for bleeding. 4. Assess the vital signs to compare with preoperative measurements. 180. The nurse is reviewing a surgeon’s prescription sheet for a preoperative client that states that the client must be nothing by mouth (NPO) after midnight. The nurse should call the surgeon to clarify that which medication should be given to the client and not withheld? 1. Prednisone 2. Ferrous sulfate 3. Cyclobenzaprine 4. Conjugated estrogen 181. A client is being prepared for a thoracentesis. The nurse should assist the client to which position for the procedure? 1. Lying in bed on the affected side 2. Lying in bed on the unaffected side 3. Sims’ position with the head of the bed flat 4. Prone with the head turned to the side and supported by a pillow 182. The nurse iscaringfor a client followinga craniotomy, in which a large tumor wasremoved from the left side. In which position can the nurse safelyplace the client? Refer to the figures in options 1 to 4. 1. 2. 3. 4. 183. The nurse creates a plan of care for a client with deep vein thrombosis. Which client position or activity in the plan should be included? 1. Out-of-bed activities as desired 2. Bed rest with the affected extremity kept flat 3. Bed rest with elevation of the affected extremity 4. Bed rest with the affected extremity in a dependent position 184. The nurse is caring for a client who is 1 day postoperative for a total hip replacement. Which is the best position in which the nurse should place the client? 1. Side-lying on the operative side 2. On the nonoperative side with the legs abducted 3. Side-lying with the affected leg internally rotated 4. Side-lying with the affected leg externally rotated Fundamentals BOX 19-2 Devices Used for Proper Positioning Bed Boards These plywood boards are placed under the entire surface area of the mattress and are useful for increasing back support and body alignment. Foot Boots Foot boots are made of rigid plastic or heavy foam and keep the foot flexed at the proper angle. They should be removed 2 or 3 times a day to assess skin integrity and joint mobility. Hand Rolls Hand rolls maintain the fingers in a slightly flexed and functional position and keep the thumb slightly adducted in opposition to the fingers. Hand-Wrist Splints These splints are individually molded for the client to maintain proper alignment of the thumb in slight adduction and the wrist in slight dorsiflexion. Pillows Pillows provide support, elevate body parts, splint incisional areas, and reduce postoperative pain during activity, coughing, or deep breathing. Theyshould be of the appropriate size for the body part to be positioned. Sandbags Sandbags are soft devices filled with a substance that can be shaped to body contours to provide support. They immobilize extremities and maintain specific body alignment. Side Rails These bars, positioned along the sides of the length of the bed, ensure client safety and are useful for increasing mobility. They also provide assistance in rolling from side to side or sitting up in bed. Laws regarding the use of side rails vary state to state and these laws must be followed; therefore, agency policies must be followed. Trapeze Bar This bar descends from a securely fastened overhead bar attached to the bed frame. It allows the client to use the upper extremities to raise the trunk off the bed, assists in transfer from the bed to a wheelchair, and helps the client to perform upper arm–strengthening exercises. Trochanter Rolls These rolls prevent external rotation of the legs when the client is in the supine position. To form a roll, use a cotton bath blanket or a sheet folded lengthwise to a width extending from the greater trochanter of the femur to the lower border of the popliteal space. Wedge Pillow This triangular pillow is made of heavy foam and is used to maintain the legs in abduction following total hip replacement surgery. Adapted from Potter P, Perry A, Stockert P, Hall A: Fundamentals of nursing, ed 8, St. Louis, 2013, Mosby. CHAPTER 19 Positioning Clients 235 185. The nurse is providing instructions to a client and the family regarding home care after right eye cataract removal. Which statement by the client would indicate an understanding of the instructions? 1. “I should sleep on my left side.” 2. “I should sleep on my right side.” 3. “I should sleep with my head flat.” 4. “I should not wear my glasses at any time.” 186. The nurse is administering a cleansing enema to a client with a fecal impaction. Before administering the enema, the nurse should place the client in which position? 1. Left Sims’ position 2. Right Sims’ position 3. On the left side of the body, with the head of the bed elevated 45 degrees 4. On the right side of the body, with the head of the bed elevated 45 degrees 187. A client has just returned to a nursing unit after an above-knee amputation of the right leg. The nurse should place the client in which position? 1. Prone 2. Reverse Trendelenburg’s 3. Supine, with the residual limb flat on the bed 4. Supine, with the residual limb supported with pillows 188. The nurse is caring for a client with a severe burn who is scheduled for an autograft to be placed on the lower extremity. The nurse creates a postoperative plan of care for the client and should include which intervention in the plan? 1. Maintain the client in a prone position. 2. Elevate and immobilize the grafted extremity. 3. Maintain the grafted extremity in a flat position. 4. Keep the grafted extremity covered with a blanket. 189. The nurse is preparing to care for a client who has returned to the nursing unit following cardiac catheterization performed through the femoral vessel. The nurse checks the health care provider’s (HCP’s) prescription and plans to allow which client position or activity following the procedure? 1. Bed rest in high Fowler’s position 2. Bed rest with bathroom privileges only 3. Bed rest with head elevation at 60 degrees 4. Bed rest with head elevation no greater than 30 degrees 190. The nurse is preparing to insert a nasogastric tube into a client. The nurse should place the client in which position for insertion? 1. Right side 2. Low Fowler’s 3. High Fowler’s 4. Supine with the head flat 191. The nurse is preparing to administer medication using a client’s nasogastric tube. Which actions should the nurse take before administering the medication? Select all that apply. 1. Check the residual volume. 2. Aspirate the stomach contents. 3. Turn off the suction to the nasogastric tube. 4. Remove the tube and place it in the other nostril. 5. Test the stomach contents for a pH indicating acidity. 192. The nurse is preparing to administer medication through a nasogastric tube that is connected to suction. To administer the medication, the nurse should take which action? 1. Position the client supine to assist in medication absorption. 2. Aspirate the nasogastric tube after medication administration to maintain patency. 3. Clamp the nasogastric tube for 30 to 60 minutes following administration of the medication. 4. Change the suction setting to low intermittent suction for 30 minutes after medication administration. 193. The nurse is assessing for correct placement of a nasogastric tube. The nurse aspirates the stomach contents, checks the gastric pH, and notes a pH of 7.35. Based on this information, which action should the nurse take at this time? 1. Retest the pH using another strip. 2. Document that the nasogastric tube is in the correct place. 3. Check for placement by auscultating for air injected into the tube. 4. Call the health care provider to request a prescription for a chest radiograph. 194. The nurse caring for a client with a chest tube turns the client to the side and the chest tube accidentally disconnects from the water seal chamber. Which initial action should the nurse take? 1. Call the health care provider (HCP). 2. Place the tube in a bottle of sterile water. 3. Replace the chest tube system immediately. 4. Place a sterile dressingover the disconnection site. 195. The registered nurse is preparing to insert a nasogastric tube in an adult client. To determine the accurate measurement of the length of the tube to be inserted, the nurse should take which action? 1. Mark the tube at 10 inches (25.5 cm). 2. Mark the tube at 32 inches (81 cm). 3. Place the tube at the tip of the nose and measure by extending the tube to the earlobe and then down to the xiphoid process. 4. Place the tube at the tip of the nose and measure by extending the tube to the earlobe and then down to the top of the sternum. 196. The nurse is assessing the functioning of a chest tube drainage system in a client who has just returned from the recovery room following a thoracotomy with wedge resection. Which are the expected assessment findings? Select all that apply. 1. Excessive bubbling in the water seal chamber 2. Vigorous bubbling in the suction control chamber 3. Drainage system maintained below the client’s chest 4. 50 mL of drainage in the drainage collection chamber 5. Occlusive dressing in place over the chest tube insertion site 6. Fluctuation of water in the tube in the water seal chamber during inhalation and exhalation 197. The nurse is assisting a health care provider with the removal of a chest tube. The nurse should instruct the client to take which action? 1. Stay very still. 2. Exhale very quickly. 3. Inhale and exhale quickly. 4. Perform the Valsalva maneuver. 198. While changing the tapes on a newly inserted tracheostomy tube, the client coughs and the tube is dislodged. Which is the initial nursing action? 1. Call the health care provider to reinsert the tube. 2. Grasp the retention sutures to spread the opening. 3. Call the respiratory therapy department to reinsert the tracheotomy. 4. Cover the tracheostomy site with a sterile dressing to prevent infection. Fundamentals CHAPTER 20 Care of a Client with a Tube 251 199. The nurse is caring for a client immediately after removal of the endotracheal tube. The nurse should report which sign immediately if experienced by the client? 1. Stridor 2. Occasional pink-tinged sputum 3. Respiratory rate of 24 breaths/minute 4. A few basilar lung crackles on the right 200. The nurse checks for residual before administering a bolus tube feeding to a client with a nasogastric tube and obtains a residual amount of 150 mL. What is the most appropriate action for the nurse to take? 1. Hold the feeding and reinstill the residual amount. 2. Reinstill the amount and continue with administering the feeding. 3. Elevate the client’s head at least 45 degrees and administer the feeding. 4. Discard the residual amount and proceed with administering the feeding. 201. The nurse caring for a client with a pneumothorax and who has had a chest tube inserted notes continuous gentle bubbling in the water seal chamber. What action is most appropriate? 1. Do nothing, because this is an expected finding. 2. Check for an air leak, because the bubbling should be intermittent. 3. Increase the suction pressure so that the bubbling becomes vigorous. 4. Clamp the chest tube and notify the health care provider immediately. 202. The nurse is inserting a nasogastric tube in an adult client. During the procedure, the client begins to cough and has difficulty breathing. What is the most appropriate action? 1. Insert the tube quickly. 2. Notify the health care provider immediately. 3. Remove the tube and reinsert it when the respiratory distress subsides. 4. Pull back on the tube and wait until the respiratory distress subsides. 203. The clinic nurse is preparing to explain the concepts of Kohlberg’s theory of moral development with a parent. The nurse should tell the parent that which factor motivates good and bad actions for the child at the preconventional level? 1. Peer pressure 2. Social pressure 3. Parents’ behavior 4. Punishment and reward 204. The maternity nurse is providing instructions to a new mother regarding the psychosocial development of the newborn infant. Using Erikson’s psychosocial development theory, the nurse instructs the mother to take which measure? 1. Allow the newborn infant to signal a need. 2. Anticipate all needs of the newborn infant. 3. Attend to the newborn infant immediately when crying. 4. Avoid the newborn infant during the first 10 minutes of crying. 205. The nurse notes that a 6-year-old child does not recognize that objects exist even when the objects are outside of the visual field. Based on this observation, which action should the nurse take? BOX 21-4 Freud’s Psychosexual Stages of Development Oral Stage (Birth to 1 Year) During this stage, the infant is concerned with self-gratification. The infant is all id, operating on the Pleasure Principle and striving for immediate gratification of needs. When the infant experiences gratification of basic needs, a sense of trust and security begins. The ego begins to emerge as the infant begins to see self as separate from the mother; this marks the beginning of the development of a sense of self. Anal Stage (1 to 3 Years) Toilet training occurs during this period, and the child gains pleasure from the elimination of the feces and from their retention. The conflict of this stage is between those demands from society and the parents and the sensations of pleasure associated with the anus. The child begins to gain a sense of control over instinctive drives and learns to delay immediate gratification to gain a future goal. Phallic Stage (3 to 6 Years) The child experiences pleasurable and conflicting feelings associated with the genital organs. The pleasures of masturbation and the fantasy life of children set the stage for the Oedipus complex. The child’s unconscious sexual attraction to and wish to possess the parent of the opposite sex, the hostility and desire to remove the parent of the same sex, and the subsequent guilt about these wishes is the conflict the child faces. The conflict is resolved when the child identifies with the parent of the same sex. The emergence of the superego is the solution to and the result of these intense impulses. Latency Stage (6 to 12 Years) The latency stage is a tapering off of conscious biological and sexual urges. The sexual impulses are channeled and elevated into a more culturally accepted level of activity. Growth of ego functions and the ability to care about and relate to others outside the home is the task of this stage of development. Genital Stage (12 Years and Beyond) The genital stage emerges at adolescence with the onset of puberty, when the genital organs mature. The individual gains gratification from his or her own body. During this stage, the individual develops satisfying sexual and emotional relationships with members of the opposite sex. The individual plans life goals and gains a strong sense of personal identity. CHAPTER 21 Theories of Growth and Development 261 Fundamentals 1. Report the observation to the health care provider. 2. Move the objects in the child’s direct field of vision. 3. Teach the child how to visually scan the environment. 4. Provide additional lighting for the child during play activities. 206. A nursing student is presenting a clinical conference to peers regarding Freud’s psychosexual stages of development, specifically the anal stage. The student explains to the group that which characteristic relates to this stage of development? 1. This stage is associated with toilet training. 2. This stage is characterized by the gratification of self. 3. This stage is characterized by a tapering off of conscious biological and sexual urges. 4. This stage is associated with pleasurable and conflicting feelings about the genital organs. 207. The nurse is describing Piaget’s cognitive developmental theory to pediatric nursing staff. The nurse should tell that staff that which child behavior is characteristic of the formal operations stage? 1. The child has the ability to think abstractly. 2. The child begins to understand the environment. 3. The child is able to classify, order, and sort facts. 4. The child learns to think in terms of past, present, and future. 208. The mother of an 8-year-old child tells the clinic nurse that she is concerned about the child because the child seems to be more attentive to friends than anything else. Using Erikson’s psychosocial development theory, the nurse should make which response? 1. “You need to be concerned.” 2. “You need to monitor the child’s behavior closely.” 3. “At this age, the child is developing his own personality.” 4. “You need to provide more praise to the child to stop this behavior.” 209. The nurse educator is preparing to conduct a teaching session for the nursing staff regarding the theories of growth and development and plans to discuss Kohlberg’s theory of moral development. What information should the nurse include in the session? Select all that apply. 1. Individuals move through all 6 stages in a sequential fashion. 2. Moral development progresses in relationship to cognitive development. 3. A person’s ability to make moral judgments develops over a period of time. 4. The theory provides a framework for understanding how individuals determine a moral code to guide their behavior. 5. In stage 1 (punishment-obedience orientation), children are expected to reason as mature members of society. 6. In stage 2 (instrumental-relativist orientation), the child conforms to rules to obtain rewards or have favors returned. 210. A parent of a 3-year-old tells a clinic nurse that the child is rebelling constantly and having temper tantrums. Using Erikson’s psychosocial development theory, which instructions should the nurse provide to the parent? Select all that apply. 1. Set limits on the child’s behavior. 2. Ignore the child when this behavior occurs. 3. Allow the behavior, because this is normal at this age period. 4. Provide a simple explanation of why the behavior is unacceptable. 5. Punish the child every time the child says “no” to change the behaviour 211. A 4-year-old child diagnosed with leukemia is hospitalized for chemotherapy. The child is fearful of the hospitalization. Which nursing intervention should be implemented to alleviate the child’s fears? 1. Encourage the child’s parents to stay with the child. BOX 22-9 Physical Care of the Dying Client Pain Administer pain medication. Do not delay or deny pain medication. Dyspnea Elevate the head of the bed or position the client on his or her side. Administer supplemental oxygen for comfort. Suction fluids from the airway as needed. Administer medications as prescribed. Skin Assess color and temperature. Assess for breakdown. Implement measures to prevent breakdown. Dehydration Maintain regular oral care. Encourage taking ice chips and sips of fluid. Do not force the client to eat or drink. Use moist cloths to provide moisture to the mouth. Apply lubricant to the lips and oral mucous membranes. Anorexia, Nausea, and Vomiting Provide antiemetics before meals. Have family members provide the client’s favorite foods. Provide frequent small portions of favorite foods. Elimination Monitor urinary and bowel elimination. Place absorbent pads under the client and check frequently. Weakness and Fatigue Provide rest periods. Assess tolerance for activities. Provide assistance and support as needed for maintaining bed or chair positions. Restlessness Maintain a calm, soothing environment. Do not restrain. Limit the number of visitors at the client’s bedside (consider cultural practices). Allow a family member to stay with the client. BOX 22-10 Fear Associated with Dying Fear of Pain Fear of pain may occur, based on anxieties related to dying. Do not delay or deny pain-relief measures to a terminally ill client. Fear of Loneliness and Abandonment Allow family members to stay with the client. Holding hands, touching (if culturally acceptable), and listening to the client are important. Fear of Being Meaningless Client may feel hopeless and powerless. Encourage life reviews and focus on the positive aspects of the client’s life. Adapted from Lewis S, Dirksen S, Heitkemper M, Bucher L, Camera I: Medicalsurgical nursing: assessment and management of clinical problems, ed 8, St. Louis, 2011, Mosby. BOX 22-11 General Postmortem Procedures Close the client’s eyes. Replace dentures. Wash the body and change bed linens if needed. Place pads under the perineum. Remove tubes and dressings. Straighten the body and place a pillow under the head in preparation for family viewing. 276 UNIT V Growth and Development Across the Life Span Fundamentals 2. Encourage play with other children of the same age. 3. Advise the family to visit only during the scheduled visiting hours. 4. Provide a private room, allowing the child to bring favorite toys from home. 212. A 16-year-old client is admitted to the hospital for acute appendicitis and an appendectomy is performed. Which nursing intervention is most appropriate to facilitate normal growth and development postoperatively? 1. Encourage the client to rest and read. 2. Encourage the parents to room in with the client. 3. Allow the family to bring in the client’s favorite computer games. 4. Allow the client to interact with others in his or her (Adolescent) same age group. 213. Which car safety device should be used for a child who is 8 years old and 4 feet tall? 1. Seat belt 2. Booster seat 3. Rear-facing convertible seat 4. Front-facing convertible seat 214. The nurse assesses the vital signs of a 12-month-old infant with a respiratory infection and notes that the respiratory rate is 35 breaths/minute. On the basis of this finding, which action is most appropriate? 1. Administer oxygen. 2. Document the findings. 3. Notify the health care provider. 4. Reassess the respiratory rate in 15 minutes. 215. The nurse is monitoring a 3-month-old infant for signs of increased intracranial pressure. On palpation of the fontanels, the nurse notes that the anterior fontanel is soft and flat. On the basis of this finding, which nursing action is most appropriate? 1. Increase oral fluids. 2. Document the finding. 3. Notify the health care provider (HCP). 4. Elevate the head of the bed to 90 degrees. 216. The nurse is evaluating the developmental level of a 2-year-old. Which does the nurse expect to observe in this child? 1. Uses a fork to eat 2. Uses a cup to drink 3. Pours own milk into a cup 4. Uses a knife for cutting food 217. A 2-year-old child is treated in the emergency department for a burn to the chest and abdomen. The child sustained the burn by grabbing a cup of hot coffee that was left on the kitchen counter. The nurse reviews safety principles with the parents before discharge. Which statement by the parents indicates an understanding of measures to provide safety in the home? 1. “We will be sure not to leave hot liquids unattended.” 2. “I guess our children need to understand what the word hot means.” 3. “We will be sure that the children stay in their rooms when we work in the kitchen.” 4. “We will install a safety gate as soon as we get home so the children cannot get into the kitchen.” 218. A mother arrives at a clinic with her toddler and tells the nurse that she has a difficult time getting the child to go to bed at night. What measure is most appropriate for the nurse to suggest to the mother? 1. Allow the child to set bedtime limits. 2. Allow the child to have temper tantrums. 3. Avoid letting the child nap during the day. 4. Inform the child of bedtime a few minutes before it is time for bed. 219. The mother of a 3-year-old is concerned because her child still is insisting on a bottle at nap time and at bedtime. Which is the most appropriate suggestion to the mother? 1. Allow the bottle if it contains juice. 2. Allow the bottle if it contains water. 3. Do not allow the child to have the bottle. 4. Allow the bottle during naps but not at bedtime. 220. The nurse is preparing to care for a 5-year-old who has been placed in traction following a fracture of the femur. The nurse plans care, knowing that which is the most appropriate activity for this child? 1. A radio 2. A sports video 3. Large picture books 4. Crayons and a coloring book 221. The mother of a 3-year-old asks a clinic nurse about appropriate and safe toys for the child. The nurse should tell the mother that the most appropriate toy for a 3-year-old is which? 1. A wagon 2. A golf set 3. A farm set 4. A jack set with marbles 222. Which interventions are appropriate for the care of an infant? Select all that apply. 1. Provide swaddling. 2. Talk in a loud voice. CHAPTER 22 Developmental Stages 277 Fundamentals 3. Provide the infant with a bottle of juice at nap time. 4. Hang mobiles with black and white contrast designs. 5. Caress the infant while bathing or during diaper changes. 6. Allow the infant to cry for at least 10 minutes before responding. 223. The nurse is preparing to care for a dying client, and several family members are at the client’s bedside. Which therapeutic techniques should the nurse use when communicating with the family? Select all that apply. 1. Discourage reminiscing. 2. Make the decisions for the family. 3. Encourage expression of feelings, concerns, and fears. 4. Explain everything that is happening to all family members. 5. Touch and hold the client’s or family member’s hand if appropriate. 6. Be honest and let the client and family know they will not be abandoned by the nurse 224. The nurse is providing medication instructions to an older client who is taking digoxin daily. The nurse explains to the client that decreased lean body mass and decreased glomerular filtration rate, which are age-related body changes, could place the client at risk for which complication with medication therapy? 1. Decreased absorption of digoxin 2. Increased risk for digoxin toxicity 3. Decreased therapeutic effect of digoxin 4. Increased risk for side effects related to digoxin 225. The nurse is caring for an older client in a long-term care facility. Which action contributes to encouraging autonomy in the client? 1. Planning meals 2. Decorating the room 3. Scheduling haircut appointments 4. Allowing the client to choose social activities 226. The home care nurse is visiting an older client whose spouse died 6 months ago. Which behaviors by the client indicates effective coping? Select all that apply. 1. Neglecting personal grooming 2. Looking at old snapshots of family 3. Participating in a senior citizens program 4. Visiting the spouse’s grave once a month 5. Decorating a wall with the spouse’s pictures and awards received 227. The nurse is providing instructions to the unlicensed assistive personnel (UAP) regarding care of an older client with hearing loss. What should the nurse tell the UAP about older clients with hearing loss? 1. They are often distracted. 2. They have middle ear changes. 3. They respond to low-pitched tones. 4. They develop moist cerumen production. 228. The nurse is providing an educational session to new employees, and the topic is abuse of the older client. The nurse helps the employees to identify which client as most typically a victim of abuse? 1. A man who has moderate hypertension 2. A man who has newly diagnosed cataracts 3. Awoman who has advanced Parkinson’s disease 4. A woman who has early diagnosed Lyme disease 229. The nurse is performing an assessment on an older client who is having difficulty sleeping at night. Which statement by the client indicates the need for further teaching regarding measures to improve sleep? 1. “I swim 3 times a week.” 2. “I have stopped smoking cigars.” 3. “I drink hot chocolate before bedtime.” 4. “I read for 40 minutes before bedtime.” 230. The visiting nurse observes that the older male client is confined by his daughter-in-law to his room. When the nurse suggests that he walk to the den and join the family, he says, “I’m in everyone’s way; my daughter-in-law needs me to stay here.” Which is the most important action for the nurse to take? 1. Say to the daughter-in-law, “Confining your father-in-law to his room is inhumane.” 2. Suggest to the client and daughter-in-law that they consider a nursing home for the client. 3. Say nothing, because it is best for the nurse to remain neutral and wait to be asked for help. 4. Suggest appropriate resources to the client and daughter-in-law, such as respite care and a senior citizens center. 231. The nurse is performing an assessment on an older adult client. Which assessment data would indicate a potential complication associated with the skin? 1. Crusting 2. Wrinkling 3. Deepening of expression lines 4. Thinning and loss of elasticity in the skin 232. The home health nurse is visiting a client for the first time. While assessing the client’s medication history, it is noted that there are 19 prescriptions and several over-the-counter medications that the client has been taking. Which intervention should the nurse take first? 1. Check for medication interactions. 2. Determine whether there are medication duplications. 3. Call the prescribing health care provider (HCP) and report polypharmacy. 4. Determine whether a family member supervises medication administration. 233. The long-term care nurse is performing assessments on several of the residents. Which are normal age-related physiological changes the nurse should expect to note? Select all that apply. 1. Increased heart rate 2. Decline in visual acuity 3. Decreased respiratory rate 4. Decline in long-term memory 5. Increased susceptibility to urinary tract infections 6. Increased incidence of awakening after sleep onset 234. The nurse is preparing to teach a prenatal class about fetal circulation. Which statements should be included in the teaching plan? Select all that apply. 1. “The ductus arteriosus allows blood to bypass the fetal lungs.” 2. “One vein carries oxygenated blood from the placenta to the fetus.” 3. “The normal fetal heart tone range is 140 to 160 beats per minute in early pregnancy.” 4. “Two arteries carry deoxygenated blood and waste products away from the fetus to the placenta.” 5. “Two veins carry blood that is high in carbon dioxide and other waste products away from the fetus to the placenta.” 235. The nursing instructor asks the student to describe fetal circulation, specifically the ductus venosus. Which statement by the student indicates an understanding of the ductus venosus? 1. “It connects the pulmonary artery to the aorta.” 2. “It is an opening between the right and left atria.” CHAPTER 24 Reproductive System 295 Maternity 3. “It connects the umbilical vein to the inferior vena cava.” 4. “It connects the umbilical artery to the inferior vena cava.” 236. A pregnant client tells the clinic nurse that she wants to know the sex of her baby as soon as it can be determined. The nurse informs the client that she should be able to find out the sex at 12 weeks’ gestation because of which factor? 1. The appearance of the fetal external genitalia 2. The beginning of differentiation in the fetal groin 3. The fetal testes are descended into the scrotal sac 4. The internal differences in males and females become apparent 237. The nurse is performing an assessment on a client who is at 38 weeks’ gestation and notes that the fetal heart rate (FHR) is 174 beats/minute. On the basis of this finding, what is the priority nursing action? 1. Document the finding. 2. Check the mother’s heart rate. 3. Notify the health care provider (HCP). 4. Tell the client that the fetal heart rate is normal. 238. The nurse is conducting a prenatal class on the female reproductive system. When a client in the class asks why the fertilized ovum stays in the fallopian tube for 3 days, what is the nurse’s best response? 1. “It promotes the fertilized ovum’s chances of survival.” 2. “It promotes the fertilized ovum’s exposure to estrogen and progesterone.” 3. “It promotes the fertilized ovum’s normal implantation in the top portion of the uterus.” 4. “It promotes the fertilized ovum’s exposure to luteinizing hormone and follicle-stimulating hormone.” 239. The nursing instructor asks a nursing student to explain the characteristics of the amniotic fluid. The student responds correctly by explaining which as characteristics of amniotic fluid? Select all that apply. 1. Allows for fetal movement 2. Surrounds, cushions, and protects the fetus 3. Maintains the body temperature of the fetus 4. Can be used to measure fetal kidney function 5. Prevents large particles such as bacteria from passing to the fetus 6. Provides an exchange of nutrients and waste products between the mother and the fetus 240. A couple comes to the family planning clinic and asks about sterilization procedures. Which question by the nurse should determine whether this method of family planning would be most appropriate? 1. “Did you ever had surgery?” 2. “Do you plan to have any other children?” 3. “Do either of you have diabetes mellitus?” 4. “Do either of you have problems with high blood pressure?” 241. The nurse should make which statement to a pregnant client found to have a gynecoid pelvis? 1. “Your type of pelvis has a narrow pubic arch.” 2. “Your type of pelvis is the most favorable for labor and birth.” 3. “Your type of pelvis is a wide pelvis, but it has a short diameter.” 4. “You will need a cesarean section because this type of pelvis is not favorable for a vaginal delivery.” 242. Which purposes of placental functioning should the nurse include in a prenatal class? Select all that apply. 1. It cushions and protects the baby. 2. It maintains the temperature of the baby. 3. It is the way the baby gets food and oxygen. 4. It prevents all antibodies and viruses from passing to the baby. 5. It provides an exchange of nutrients and waste products between the mother and developing fetus. 243. A55-year-old male client confides in the nurse that he is concerned about his sexual function. What is the nurse’s best response? 1. “How often do you have sexual relations?” 2. “Please share with me more about your concerns.” 3. “You are still young and have nothing to be concerned about.” 4. “You should not have a decline in testosterone until you are in your 80s. 244. The nurse is providing instructions to a pregnant client who is scheduled for an amniocentesis. What instruction should the nurse provide? 1. Strict bed rest is required after the procedure. 2. Hospitalization is necessary for 24 hours after the procedure. 3. An informed consent needs to be signed before the procedure. 4. A fever is expected after the procedure because of the trauma to the abdomen. 245. A pregnant client in the first trimester calls the nurse at a health care clinic and reports that she has noticed a thin, colorless vaginal drainage. The nurse should make which statement to the client? 1. “Come to the clinic immediately.” 2. “The vaginal discharge may be bothersome, but is a normal occurrence.” 3. “Report to the emergency department at the maternity center immediately.” 4. “Use tampons if the discharge is bothersome, but be sure to change the tampons every 2 hours.” 246. A nonstress test is performed on a client who is pregnant, and the results of the test indicate nonreactive findings. The health care provider prescribes a contraction stress test, and the results are documented as negative. How should the nurse document this finding? 1. A normal test result 2. An abnormal test result 3. A high risk for fetal demise 4. The need for a cesarean section 247. A rubella titer result of a 1-day postpartum client is less than 1:8, and a rubella virus vaccine is prescribed to be administered before discharge. The nurse provides which information to the client about the vaccine? Select all that apply. 1. Breast-feeding needs to be stopped for 3 months. 2. Pregnancy needs to be avoided for 1 to 3 months. 3. The vaccine is administered by the subcutaneous route. 4. Exposure to immunosuppressed individuals needs to be avoided. 5. A hypersensitivity reaction can occur if the client has an allergy to eggs. 6. The area of the injection needs to be covered with a sterile gauze for 1 week. 248. The nurse in a health care clinic is instructing a pregnant client how to perform “kick counts.” Which statement by the client indicates a need for further instruction? 1. “I will record the number ofmovements or kicks.” 2. “I need to lie flat on my back to perform the procedure.” 3. “If I count fewer than 10 kicks in a 2-hour period, I should count the kicks again over the next 2 hours.” 4. “I should place my hands on the largest part of my abdomen and concentrate on the fetal movements to count the kicks.” 249. The nurse is performing an assessment of a pregnant client who is at 28 weeks of gestation. The nurse measures the fundal height in centimeters and notes that the fundal height is 30 cm. How should the nurse interpret this finding? 1. The client is measuring large for gestational age. 2. The client is measuring small for gestational age. 3. The client is measuring normal for gestational age. 4. More evidence is needed to determine size for gestational age. 310 UNIT VI Maternity Nursing Maternity 250. The nurse is performing an assessment on a client who suspects that she is pregnant and is checking the client for probable signs of pregnancy. The nurse should assess for which probable signs of pregnancy? Select all that apply. 1. Ballottement 2. Chadwick’s sign 3. Uterine enlargement 4. Positive pregnancy test 5. Fetal heart rate detected by a nonelectronic device 6. Outline of fetus via radiography or ultrasonography 251. A pregnant client is seen for a regular prenatal visit and tells the nurse that she is experiencing irregular contractions. The nurse determines that she is experiencing Braxton Hicks contractions. On the basis of this finding, which nursing action is appropriate? 1. Contact the health care provider. 2. Instruct the client to maintain bed rest for the remainder of the pregnancy. 3. Inform the client that these contractions are common and may occur throughout the pregnancy. 4. Call the maternity unit and inform them that the client will be admitted in a preterm labor condition. 252. Aclient arrives at the clinic for the first prenatal assessment. She tells the nurse that the first day of her last normal menstrual period was October 19, 2018. Using Na¨gele’s rule, which expected date of delivery should the nurse document in the client’s chart? 1. July 12, 2019 2. July 26, 2019 3. August 12, 2019 4. August 26, 2019 253. The nurse is collecting data during an admission assessment of a client who is pregnant with twins. The client has a healthy 5-year-old child who was delivered at 38 weeks and tells the nurse that she does not have a history of any type of abortion or fetal demise. Using GTPAL, what should the nurse document in the client’s chart? 1. G¼3, T¼2, P¼0, A¼0, L¼1 2. G¼2, T¼1, P¼0, A¼0, L¼1 3. G¼1, T¼1, P¼1, A¼0, L¼1 4. G¼2, T¼0, P¼0, A¼0, L¼1 254. The nurse is providing instructions to a pregnant client with human immunodeficiency virus (HIV) infection regarding care to the newborn after delivery. The client asks the nurse about the feeding options that are available. Which response should the nurse make to the client? 1. “You will need to bottle-feed your newborn.” 2. “You will need to feed your newborn by nasogastric tube feeding.” 3. “You will be able to breast-feed for 6 months and then will need to switch to bottle-feeding.” 4. “You will be able to breast-feed for 9 months and then will need to switch to bottle-feeding.” 255. The home care nurse visits a pregnant client who has a diagnosis of mild preeclampsia. Which assessment finding indicates a worsening of the preeclampsia and the need to notify the health care provider (HCP)? 1. Urinary output has increased. 2. Dependent edema has resolved. 3. Blood pressure reading is at the prenatal baseline. 4. The client complains of a headache and blurred vision. 256. A stillborn baby was delivered in the birthing suite a few hours ago. After the delivery, the family remained together, holding and touching the baby. Which statement by the nurse would assist the family in their period of grief? 1. “What can I do for you?” 2. “Now you have an angel in heaven.” 3. “Don’t worry, there is nothing you could have done to prevent this from happening.” 4. “We will see to it that you have an early discharge so that you don’t have to be reminded of this experience.” 257. The nurse implements a teaching plan for a pregnant client who is newly diagnosed with gestational diabetes mellitus. Which statement made by the client indicates a need for furth er teach ing? 1. “I should stay on the diabetic diet.” 2. “I should perform glucose monitoring at home.” 3. “I should avoid exercise because of the negative effects on insulin production.” 4. “I should be aware of any infections and report signs of infection immediately to my health care provider (HCP).” 258. The nurse is performing an assessment on a pregnant client in the last trimester with a diagnosis of severe preeclampsia. The nurse reviews the assessment findings and determines that which finding is most closely associated with a complication of this diagnosis? 1. Enlargement of the breasts 2. Complaints of feeling hot when the room is cool 3. Periods of fetal movement followed by quiet periods 4. Evidence of bleeding, such as in the gums, petechiae, and purpura 259. The nurse in a maternity unit is reviewing the clients’ records. Which clients should the nurse identify as being at the most risk for developing disseminated intravascular coagulation (DIC)? Select all that apply. 1. A primigravida with mild preeclampsia 2. A primigravida who delivered a 10-lb infant 3 hours ago 3. A gravida II who has just been diagnosed with dead fetus syndrome 4. A gravida IV who delivered 8 hours ago and has lost 500 mL of blood 5. A primigravida at 29 weeks of gestation who was recently diagnosed with severe preeclampsia CHAPTER 26 Risk Conditions Related to Pregnancy 327 Maternity 260. The home care nurse is monitoring a pregnant client with gestational hypertension who is at risk for preeclampsia. At each home care visit, the nurse assesses the client for which classic signs of preeclampsia? Select all that apply. 1. Proteinuria 2. Hypertension 3. Low-grade fever 4. Generalized edema 5. Increased pulse rate 6. Increased respiratory rate 261. The nurse is assessing a pregnant client with type 1 diabetes m ellitus about her understanding regarding changing insulin needs during pregnancy. The nurse determ ines that furth er teach in g is n eeded if the client m akes which statem ent? 1. “I will need to increase my insulin dosage during the first 3 months of pregnancy.” 2. “My insulin dose will likely need to be increased during the second and third trimesters.” 3. “Episodes of hypoglycemia are more likely to occur during the first 3 months of pregnancy.” 4. “My insulin needs should return to prepregnant levels within 7 to 10 days after birth if I am bottle-feeding.” 262. A pregnant client reports to a health care clinic, complaining of loss of appetite, weight loss, and fatigue. After assessment of the client, tuberculosis is suspected. A sputum culture is obtained and identifies Mycobacterium tuberculosis. Which instruction should the nurse include in the client’s teaching plan? 1. Therapeutic abortion is required. 2. Isoniazid plus rifampin will be required for 9 months. 3. She will have to stay at home until treatment is completed. 4. Medication will not be started until after delivery of the fetus. 263. The nurse is providing instructions to a pregnant client with a history of cardiac disease regarding appropriate dietary measures. Which statement, if made by the client, indicates an understanding of the information provided by the nurse? 1. “I should increase my sodium intake during pregnancy.” 2. “I should lower my blood volume by limiting my fluids.” 3. “I should maintain a low-calorie diet to prevent any weight gain.” 4. “I should drink adequate fluids and increase my intake of high-fiber foods.” 264. The clinic nurse is performing a psychosocial assessment of a client who has been told that she is pregnant. Which assessment findings indicate to the nurse that the client is at risk for contracting human immunodeficiency virus (HIV)? Select all that apply. 1. The client has a history of intravenous drug use. 2. The client has a significant other who is heterosexual. 3. The client has a history of sexually transmitted infections. 4. The client has had one sexual partner for the past 10 years. 5. The client has a previous history of gestational diabetes mellitus. 265. The nurse in a maternity unit is providing emotional support to a client and her significant other who are preparing to be discharged from the hospital after the birth of a dead fetus. Which statement made by the client indicates a component of the normal grieving process? 1. “We want to attend a support group.” 2. “We never want to try to have a baby again.” 3. “We are going to try to adopt a child immediately.” 4. “We are okay, and we are going to try to have another baby immediately.” 266. The nurse evaluates the ability of a hepatitis B–positive mother to provide safe bottle-feeding to her newborn during postpartum hospitalization. Which maternal action best exemplifies the mother’s knowledge of potential disease transmission to the newborn? 1. The mother requests that the window be closed before feeding. 2. The mother holds the newborn properly during feeding and burping. 3. The mother tests the temperature of the formula before initiating feeding. 4. The mother washes and dries her hands before and after self-care of the perineum and asks for a pair of gloves before feeding. 267. A client in the first trimester of pregnancy arrives at a health care clinic and reports that she has been experiencing vaginal bleeding. Athreatened abortion is suspected, and the nurse instructs the client regarding management of care. Which statement made by the client indicates a need for further instruction? 1. “I will watch for the evidence of the passage of tissue.” 2. “I will maintain strict bed rest throughout the remainder of the pregnancy.” 328 UNIT VI Maternity Nursing Maternity 3. “I will count the number of perineal pads used on a daily basis and note the amount and color of blood on the pad.” 4. “I will avoid sexual intercourse until the bleeding has stopped, and for 2 weeks following the last evidence of bleeding.” 268. The nurse is planning to admit a pregnant client who is obese. In planning care for this client, which potential client needs should the nurse anticipate? Select all that apply. 1. Bed rest as a necessary preventive measure may be prescribed. 2. Routine administration of subcutaneous heparin may be prescribed. 3. An overbed lift may be necessary if the client requires a cesarean section. 4. Less frequent cleansing of a cesarean incision, if present, may be prescribed. 5. Thromboembolism stockings or sequential compression devices may be prescribed. 269. The nurse is caring for a client in labor. Which assessment findings indicate to the nurse that the client is beginning the second stage of labor? Select all that apply. 1. The contractions are regular. 2. The membranes have ruptured. 3. The cervix is dilated completely. 4. The client begins to expel clear vaginal fluid. 5. The spontaneous urge to push is initiated from perineal pressure. Maternity CHAPTER 27 Labor and Birth 341 Maternity 270. The nurse in the labor room is caring for a client in the active stage of the first phase of labor. The nurse is assessing the fetal patterns and notes a late deceleration on the monitor strip. What is the most appropriate nursing action? 1. Administer oxygen via face mask. 2. Place the mother in a supine position. 3. Increase the rate of the oxytocin intravenous infusion. 4. Document the findings and continue to monitor the fetal patterns. 271. The nurse is performing an assessment of a client who is scheduled for a cesarean delivery at 39 weeks of gestation. Which assessment finding indicates the need to contact the health care provider (HCP)? 1. Hemoglobin of 11 g/dL (110 mmol/L) 2. Fetal heart rate of 180 beats/minute 3. Maternal pulse rate of 85 beats/minute 4. White blood cell count of 12,000 mm 3 (12.0 Â 109/L) 272. The nurse is reviewing the record of a client in the labor room and notes that the health care provider has documented that the fetal presenting part is at the –1 station. This documented finding indicates that the fetal presenting part is located at which area? Refer to figure. 1. 2. 4. 3. 1. 1 2. 2 3. 3 4. 4 273. A client arrives at a birthing center in active labor. Following examination, it is determined that her membranes are still intact and she is at a –2 station. The health care provider prepares to perform an amniotomy. What will the nurse relay to the client as the most likely outcomes of the amniotomy? Select all that apply. 1. Less pressure on her cervix 2. Decreased number of contractions 3. Increased efficiency of contractions 4. The need for increased maternal blood pressure monitoring 5. The need for frequent fetal heart rate monitoring to detect the presence of a prolapsed cord 274. The nurse is monitoring a client in labor. The nurse suspects umbilical cord compression if which is noted on the external monitor tracing during a contraction? 1. Variability 2. Accelerations 3. Early decelerations 4. Variable decelerations 275. Aclient in labor is transported to the delivery room and prepared for a cesarean delivery. After the client is transferred to the delivery room table, the nurse should place the client in which position? 1. Supine position with a wedge under the right hip 2. Trendelenburg’s position with the legs in stirrups 3. Prone position with the legs separated and elevated 4. Semi-Fowler’s position with a pillow under the knees 276. The nurse is monitoring a client in active labor and notes that the client is having contractions every 3 minutes that last 45 seconds. The nurse notes that the fetal heart rate between contractions is 100 beats/ minute. Which nursing action is most appropriate? 1. Notify the health care provider (HCP). 2. Continue monitoring the fetal heart rate. 3. Encourage the client to continue pushing with each contraction. 4. Instruct the client’s coach to continue to encourage breathing techniques. 277. The nurse is caring for a client in labor and is monitoring the fetal heart rate patterns. The nurse notes the presence of episodic accelerations on the electronic fetal monitor tracing. Which action is most appropriate? 1. Notify the health care provider of the findings. 2. Reposition the mother and check the monitor for changes in the fetal tracing. 3. Take the mother’s vital signs and tell the mother that bed rest is required to conserve oxygen. 4. Document the findings and tell the mother that the pattern on the monitor indicates fetal wellbeing. 278. The nurse is admitting a pregnant client to the labor room and attaches an external electronic fetal monitor to the client’s abdomen. After attachment of the electronic fetal monitor, what is the next nursing action? 1. Identify the types of accelerations. 2. Assess the baseline fetal heart rate. 3. Determine the intensity of the contractions. 4. Determine the frequency of the contractions. 342 UNIT VI Maternity Nursing Maternity 279. The nurse is reviewing true and false labor signs with a multiparous client. The nurse determines that the client understands the signs of true labor if she makes which statement? 1. “I won’t be in labor until my baby drops.” 2. “My contractions will be felt in my abdominal area.” 3. “My contractions will not be as painful if I walk around.” 4. “My contractions will increase in duration and intensity.” 280. Which assessment following an amniotomy should be conducted first? 1. Cervical dilation 2. Bladder distention 3. Fetal heart rate pattern 4. Maternal blood pressure 281. The nurse has been working with a laboring client and notes that she has been pushing effectively for 1 hour. What is the client’s primary physiological need at this time? 1. Ambulation 2. Rest between contractions 3. Change positions frequently 4. Consume oral food and fluids 282. The nurse is assisting a client undergoing induction of labor at 41 weeks of gestation. The client’s contractions are moderate and occurring every 2 to 3 minutes, with a duration of 60 seconds. An internal fetal heart rate monitor is in place. The baseline fetal heart rate has been 120 to 122 beats/minute for the past hour. What is the priority nursing action? 1. Notify the health care provider. 2. Discontinue the infusion of oxytocin. 3. Place oxygen on at 8 to 10 L/minute via face mask. 4. Contact the client’s primary support person(s) if not currently present. 283. The nurse is assessing a pregnant client in the second trimester of pregnancy who was admitted to the maternityunit with a suspected diagnosisofabruptio placentae. Which assessment finding should the nurse expect to note if this condition is present? 1. Soft abdomen 2. Uterine tenderness 3. Absence of abdominal pain 4. Painless, bright red vaginal bleeding 284. The maternity nurse is preparing for the admission of a client in the third trimester of pregnancy who is experiencing vaginal bleeding and has a suspected diagnosis of placenta previa. The nurse reviews the health care provider’s prescriptions and should question which prescription? 1. Prepare the client for an ultrasound. 2. Obtain equipment for a manual pelvic examination. 3. Prepare to draw a hemoglobin and hematocrit blood sample. 4. Obtain equipment for external electronic fetal heart rate monitoring. 285. An ultrasound is performed on a client at term gestation who is experiencing moderate vaginal bleeding. The results of the ultrasound indicate that abruptio placentae is present. On the basis of these findings, the nurse should prepare the client for which anticipated prescription? 1. Delivery of the fetus 2. Strict monitoring of intake and output 3. Complete bed rest for the remainder of the pregnancy 4. The need for weekly monitoring of coagulation studies until the time of delivery 286. The nurse is performing an assessment on a client who has just been told that a pregnancy test is positive. Which assessment finding indicates that the client is at risk for preterm labor? 1. The client is a 35-year-old primigravida. 2. The client has a history of cardiac disease. 3. The client’s hemoglobin level is 13.5 g/dL (135 mmol/L). 4. The client is a 20-year-old primigravida of average weight and height. 287. The nurse is monitoring a client who is in the active stage of labor. The nurse documents that the client is experiencing labor dystocia. The nurse determines that which risk factors in the client’s history placed her at risk for this complication? Select all that apply. 1. Age 54 2. Body mass index of 28 3. Previous difficulty with fertility 4. Administration of oxytocin for induction 5. Potassium level of 3.6 mEq/L (3.6 mmol/L) 288. The nurse in a birthing room is monitoring a client with dysfunctional labor for signs of fetal or maternal compromise. Which assessment finding should alert the nurse to a compromise? 1. Maternal fatigue 2. Coordinated uterine contractions CHAPTER 28 Problems with Labor and Birth 351 Maternity 3. Progressive changes in the cervix 4. Persistent nonreassuring fetal heart rate 289. The nurse in a labor room is preparing to care for a client with hypertonic uterine contractions. The nurse is told that the client is experiencing uncoordinated contractions that are erratic in their frequency, duration, and intensity. What is the priority nursing action? 1. Provide pain relief measures. 2. Prepare the client for an amniotomy. 3. Promote ambulation every 30 minutes. 4. Monitor the oxytocin infusion closely. 290. The nurse is reviewing the health care provider’s (HCP’s) prescriptions for a client admitted for premature rupture of the membranes. Gestational age of the fetus is determined to be 37 weeks. Which prescription should the nurse question? 1. Monitor fetal heart rate continuously. 2. Monitor maternal vital signs frequently. 3. Perform a vaginal examination every shift. 4. Administer an antibiotic per HCP prescription and per agency protocol. 291. The nurse has created a plan of care for a client experiencing dystocia and includes several nursing actions in the plan of care. What is the priority nursing action? 1. Providing comfort measures 2. Monitoring the fetal heart rate 3. Changing the client’s position frequently 4. Keeping the significant other informed of the progress of the labor 292. Fetal distress is occurring with a laboring client. As the nurse prepares the client for a cesarean birth, what is the most important nursing action? 1. Slow the intravenous flow rate. 2. Continue the oxytocin drip if infusing. 3. Place the client in a high Fowler’s position. 4. Administer oxygen, 8 to 10 L/minute, via face mask. 293. The nurse in the postpartum unit is caring for a client who has just delivered a newborn infant following a pregnancy with placenta previa. The nurse reviews the plan of care and prepares to monitor the client for which risk associated with placenta previa? 1. Infection 2. Hemorrhage 3. Chronic hypertension 4. Disseminated intravascular coagulation 294. The nurse is performing an assessment on a client diagnosed with placenta previa. Which assessment findings should the nurse expect to note? Select all that apply. 1. Uterine rigidity 2. Uterine tenderness 3. Severe abdominal pain 4. Bright red vaginal bleeding 5. Soft, relaxed, nontender uterus 6. Fundal height may be greater than expected for gestational age 295. The nurse in a labor room is performing a vaginal assessment on a pregnant client in labor. The nurse notes the presence of the umbilical cord protruding from the vagina. What is the first nursing action with this finding? 1. Gently push the cord into the vagina. 2. Place the client in Trendelenburg position. 3. Find the closest telephone and page the health care provider stat. 4. Call the delivery room to notify the staff that the client will be transported immediately. 296. The postpartum nurse is taking the vital signs of a client who delivered a healthy newborn 4 hours ago. The nurse notes that the client’s temperature is 100.2°F. What is the priority nursing action? 1. Document the findings. 2. Retake the temperature in 15 minutes. 3. Notify the health care provider (HCP). 4. Increase hydration by encouraging oral fluids. 297. The nurse is assessing a client who is 6 hours postpartum after delivering a full-term healthy newborn. The client complains to the nurse of feelings of faintness and dizziness. Which nursing action is most appropriate? 1. Raise the head of the client’s bed. 2. Obtain hemoglobin and hematocrit levels. 3. Instruct the client to request help when getting out of bed. 4. Inform the nursery room nurse to avoid bringing the newborn to the client until the client’s symptoms have subsided. 298. The postpartum nurse is providing instructions to a client after birth of a healthy newborn. Which time frame should the nurse relay to the client regarding the return of bowel function? 1. 3 days postpartum 2. 7 days postpartum 3. On the day of birth 4. Within 2 weeks postpartum 299. The nurse is planning care for a postpartum client who had a vaginal delivery 2 hours ago. The client required an episiotomy and has several hemorrhoids. What is the priority nursing consideration for this client? 1. Client pain level 2. Inadequate urinary output 3. Client perception of body changes 4. Potential for imbalanced body fluid volume 300. The nurse is providing postpartum instructions to a client who will be breast-feeding her newborn. The nurse determines that the client has understood the instructions if she makes which statements? Select all that apply. 1. “I should wear a bra that provides support.” 2. “Drinking alcohol can affect my milk supply.” 3. “The use of caffeine can decrease my milk supply.” 4. “I will start my estrogen birth control pills again as soon as I get home.” 5. “I know if my breasts get engorged, I will limit my breast-feeding and supplement the baby.” 6. “I plan on having bottled water available in the refrigerator so I can get additional fluids easily.” 301. The nurse is teaching a postpartum client about breast-feeding. Which instruction should the nurse include? 1. The diet should include additional fluids. 2. Prenatal vitamins should be discontinued. 3. Soap should be used to cleanse the breasts. 4. Birth control measures are unnecessary while breast-feeding. 302. The nurse is preparing to assess the uterine fundus of a client in the immediate postpartum period. After locating the fundus, the nurse notes that the uterus feels soft and boggy. Which nursing intervention is appropriate? 1. Elevate the client’s legs. 2. Massage the fundus until it is firm. 3. Ask the client to turn on her left side. 4. Push on the uterus to assist in expressing clots. 303. The nurse is caring for four 1-day postpartum clients. Which client assessment requires the need for follow-up? 1. The client with mild afterpains 2. The client with a pulse rate of 60 beats/minute 3. The client with colostrum discharge from both breasts 4. The client with lochia that is red and has a foulsmelling odor 304. When performing a postpartum assessment on a client, the nurse notes the presence of clots in the lochia. The nurse examines the clots and notes that they are larger than 1 cm. Which nursing action is most appropriate? 360 UNIT VI Maternity Nursing 1. Document the findings. 2. Reassess the client in 2 hours. 3. Notify the health care provider (HCP). 4. Encourage increased oral intake of fluids. 305. The nurse is monitoring the amount of lochia drainage in a client who is 2 hours postpartum and notes that the client has saturated a perineal pad in 15 minutes. How should the nurse respond to this finding initially? 1. Document the finding. 2. Encourage the client to ambulate. 3. Encourage the client to increase fluid intake. 4. Contact the health care provider (HCP) and inform the HCP of this finding. 306. The nurse has provided discharge instructions to a client who delivered a healthy newborn by cesarean delivery. Which statement made by the client indicates a need for further instruction? 1. “I will begin abdominal exercises immediately.” 2. “I will notify the health care provider if I develop a fever.” 3. “I will turn on my side and push up with my arms to get out of bed.” 4. “I will lift nothing heavier than my newborn baby for at least 2 weeks.” 307. After a precipitous delivery, the nurse notes that the new mother is passive and touches her newborn infant only briefly with her fingertips. What should the nurse do to help the woman process the delivery? 1. Encourage the mother to breast-feed soon after birth. 2. Support the mother in her reaction to the newborn infant. 3. Tell the mother that it is important to hold the newborn infant. 4. Document a complete account of the mother’s reaction on the birth record. 308. The nurse is monitoring a client in the immediate postpartum period for signs of hemorrhage. Which sign, if noted, would be an early sign of excessive blood loss? 1. A temperature of 100.4 °F (38 °C) 2. An increase in the pulse rate from 88 to 102 beats/minute 3. A blood pressure change from 130/88 to 124/80 mm Hg 4. An increase in the respiratory rate from 18 to 22 breaths/minute 309. The nurse is preparing a list of self-care instructions for a postpartum client who was diagnosed with mastitis. Which instructions should be included on the list? Select all that apply. 1. Wear a supportive bra. 2. Rest during the acute phase. 3. Maintain a fluid intake of at least 3000 mL/day. 4. Continue to breast-feed if the breasts are not too sore. 5. Take the prescribed antibiotics until the soreness subsides. 6. Avoid decompression of the breasts by breast-feeding or breast pump. 310. The nurse is providing instructions about measures to prevent postpartum mastitis to a client who is breast-feeding her newborn. Which client statement would indicate a need for further instruction? 1. “I should breast-feed every 2 to 3 hours.” 2. “I should change the breast pads frequently.” 3. “I should wash my hands well before breastfeeding.” 4. “I should wash my nipples daily with soap and water.” 311. The postpartum nurse is assessing a client who delivered a healthy infant by cesarean section for signs and symptoms of superficial venous thrombosis. Which sign should the nurse note if superficial venous thrombosis were present? 1. Paleness of the calf area 2. Coolness of the calf area 3. Enlarged, hardened veins 4. Palpable dorsalis pedis pulses 312. A client in a postpartum unit complains of sudden sharp chest pain and dyspnea. The nurse notes that the client is tachycardic and the respiratory rate is elevated. The nurse suspects a pulmonary embolism. Which should be the initial nursing action? 1. Initiate an intravenous line. 2. Assess the client’s blood pressure. 3. Prepare to administer morphine sulfate. 4. Administer oxygen, 8 to 10 L/minute, by face mask. 313. The nurse is assessing a client in the fourth stage of labor and notes that the fundus is firm, but that bleeding is excessive. Which should be the initial nursing action? 1. Record the findings. 2. Massage the fundus. 3. Notify the health care provider (HCP). 4. Place the client in Trendelenburg’s position. 314. The nurse is preparing to care for four assigned clients. Which client is at most risk for hemorrhage? 1. A primiparous client who delivered 4 hours ago 2. A multiparous client who delivered 6 hours ago 3. A multiparous client who delivered a large baby after oxytocin induction 4. A primiparous client who delivered 6 hours ago and had epidural anesthesia 315. A postpartum client is diagnosed with cystitis. The nurse should plan for which priority action in the care of the client? 1. Providing sitz baths 2. Encouraging fluid intake 3. Placing ice on the perineum 4. Monitoring hemoglobin and hematocrit levels 316. The nurse is monitoring a postpartum client who received epidural anesthesia for delivery for the presence of a vulvar hematoma. Which assessment finding would best indicate the presence of a hematoma? 1. Changes in vital signs 2. Signs of heavy bruising 3. Complaints of intense pain 4. Complaints of a tearing sensation 368 UNIT VI Maternity Nursing 317. The nurse is creating a plan of care for a postpartum client with a small vulvar hematoma. The nurse should include which specific action during the first 12 hours after delivery? 1. Encourage ambulation hourly. 2. Assess vital signs every 4 hours. 3. Measure fundal height every 4 hours. 4. Prepare an ice pack for application to the area. 318. On assessment of a postpartum client, the nurse notes that the uterus feels soft and boggy. The nurse should take which initial action? 1. Document the findings. 2. Elevate the client’s legs. 3. Massage the fundus until it is firm. 4. Push on the uterus to assist in expressing clots. 319. The nurse assisted with the birth of a newborn. Which nursing action is most effective in preventing heat loss by evaporation? 1. Warming the crib pad 2. Closing the doors to the room 3. Drying the infant with a warm blanket 4. Turning on the overhead radiant warmer 320. The mother of a newborn calls the clinic and reports that when cleaning the umbilical cord, she noticed that the cord was moist and that discharge was present. What is the most appropriate nursing instruction for this mother? 1. Bring the infant to the clinic. 2. This is a normal occurrence and no further action is needed. 3. Increase the number of times that the cord is cleaned per day. 4. Monitor the cord for another 24 to 48 hours and call the clinic if the discharge continues. 321. The nurse in a neonatal intensive care unit (NICU) receives a telephone call to prepare for the admission of a 43-week gestation newborn with Apgar scores of 1 and 4. In planning for admission of this newborn, what is the nurse’s highest priority? 1. Turn on the apnea and cardiorespiratorymonitors. 2. Connect the resuscitation bag to the oxygen outlet. 3. Set up the intravenous line with 5% dextrose in water. 4. Set the radiant warmer control temperature at 36.5 °C (97.6 °F). 322. The nurse is assessing a newborn after circumcision and notes that the circumcised area is red with a small amount of bloody drainage. Which nursing action is most appropriate? 1. Apply gentle pressure. 2. Reinforce the dressing. 3. Document the findings. 4. Contact the health care provider (HCP). 323. The nurse in a newborn nursery is monitoring a preterm newborn for respiratory distress syndrome. Which assessment findings should alert the nurse to the possibility of this syndrome? Select all that apply. 1. Cyanosis 2. Tachypnea 3. Hypotension 4. Retractions 5. Audible grunts 6. Presence of a barrel chest 324. The postpartum nurse is providing instructions to the mother of a newborn with hyperbilirubinemia who is being breast-fed. The nurse should provide which instruction to the mother? 1. Feed the newborn less frequently. 2. Continue to breast-feed every 2 to 4 hours. 3. Switch to bottle-feeding the infant for 2 weeks. 4. Stop breast-feeding and switch to bottle-feeding permanently. 325. The nurse is assessing a newborn who was born to a mother who is addicted to drugs. Which findings should the nurse expect to note during the assessment of this newborn? Select all that apply. 1. Lethargy 2. Sleepiness 3. Irritability 4. Constant crying 5. Difficult to comfort 6. Cuddles when being held 326. The nurse notes hypotonia, irritability, and a poor sucking reflex in a full-term newborn on admission to the nursery. The nurse suspects fetal alcohol syndrome and is aware that which additional sign would be consistent with this syndrome? 1. Length of 19 inches 2. Abnormal palmar creases 3. Birth weight of 6 lb, 14 oz (3120 g) 4. Head circumference appropriate for gestational age 388 UNIT VI Maternity Nursing 327. The nurse is creating a plan of care for a newborn diagnosed with fetal alcohol syndrome. The nurse should include which priority intervention in the plan of care? 1. Allow the newborn to establish own sleep-rest pattern. 2. Maintain the newborn in a brightly lighted area of the nursery. 3. Encourage frequent handling of the newborn by staff and parents. 4. Monitor the newborn’s response to feedings and weight gain pattern. 328. The nurse administers erythromycin ointment (0.5%) to the eyes of a newborn and the mother asks the nurse why this is performed. Which explanation is best for the nurse to provide about neonatal eye prophylaxis? 1. Protects the newborn’s eyes from possible infections acquired while hospitalized. 2. Prevents cataracts in the newborn born to a woman who is susceptible to rubella. 3. Minimizes the spread of microorganisms to the newborn from invasive procedures during labor. 4. Prevents an infection called ophthalmia neonatorum from occurring after birth in a newborn born to a woman with an untreated gonococcal infection. 329. The nurse is preparing to care for a newborn receiving phototherapy. Which interventions should be included in the plan of care? Select all that apply. 1. Avoid stimulation. 2. Decrease fluid intake. 3. Expose all of the newborn’s skin. 4. Monitor skin temperature closely. 5. Reposition the newborn every 2 hours. 6. Cover the newborn’s eyes with eye shields or patches. 330. The nurse creates a plan of care for a woman with human immunodeficiency virus (HIV) infection and her newborn. The nurse should include which intervention in the plan of care? 1. Monitoring the newborn’s vital signs routinely 2. Maintaining standard precautions at all times while caring for the newborn 3. Initiating referral to evaluate for blindness, deafness, learning problems, or behavioral problems 4. Instructing the breast-feeding mother regarding the treatment of the nipples with nystatin ointment 331. The nurse is planning care for a newborn of a mother with diabetes mellitus. What is the priority nursing consideration for this newborn? 1. Developmental delays because of excessive size 2. Maintaining safety because of low blood glucose levels 3. Choking because of impaired suck and swallow reflexes 4. Elevated body temperature because of excess fat and glycogen 332. Which statement reflects a new mother’s understanding of the teaching about the prevention of newborn abduction? 1. “I will place my baby’s crib close to the door.” 2. “Some health care personnel won’t have name badges.” 3. “I will ask the nurse to attend to my infant if I am napping and my husband is not here.” 4. “It’s okay to allow the nurse assistant to carry my newborn to the nursery.” 333. The nurse prepares to administer a phytonadione (vitamin K) injection to a newborn, and the mother asks the nurse why her infant needs the injection. What best response should the nurse provide? 1. “Your newborn needs the medicine to develop immunity.” 2. “The medicine will protect your newborn from being jaundiced.” 3. “Newborns have sterile bowels, and the medicine promotes the growth of bacteria in the bowel.” 4. “Newborns are deficient in vitamin K, and this injection prevents your newborn from bleeding.” 334. The nurse is monitoring a client who is receiving oxytocin to induce labor. Which assessment findings should cause the nurse to immediately discontinue the oxytocin infusion? Select all that apply. 1. Fatigue 2. Drowsiness 3. Uterine hyperstimulation 4. Late decelerations of the fetal heart rate 5. Early decelerations of the fetal heart rate 335. A pregnant client is receiving magnesium sulfate for the management of preeclampsia. The nurse determines that the client is experiencing toxicity from the medication if which findings are noted on assessment? Select all that apply. 1. Proteinuria of 3 + 2. Respirations of 10 breaths/minute CHAPTER 32 Maternity and Newborn Medications 399 Maternity 3. Presence of deep tendon reflexes 4. Urine output of 20 mL in an hour 5. Serum magnesium level of 4 mEq/L (2 mmol/L) 336. The nurse asks a nursing student to describe the procedure for administering erythromycin ointment to the eyes of a newborn. Which student statement indicates that further teaching is needed about administration of the eye medication? 1. “I will flush the eyes after instilling the ointment.” 2. “I will clean the newborn’s eyes before instilling ointment.” 3. “I need to administer the eye ointment within 1 hour after delivery.” 4. “I will instill the eye ointment into each of the newborn’s conjunctival sacs.” 337. A client in preterm labor (31 weeks) who is dilated to 4 cm has been started on magnesium sulfate and contractions have stopped. If the client’s labor can be inhibited for the next 48 hours, the nurse anticipates a prescription for which medication? 1. Nalbuphine 2. Betamethasone 3. Rh o(D) immune globulin 4. Dinoprostone vaginal insert 338. Methylergonovine is prescribed for a woman to treat postpartum hemorrhage. Before administration of methylergonovine, what is the priority assessment? 1. Uterine tone 2. Blood pressure 3. Amount of lochia 4. Deep tendon reflexes 339. The nurse is preparing to administer exogenous surfactant to a premature infant who has respiratory distress syndrome. The nurse prepares to administer the medication by which route? 1. Intradermal 2. Intratracheal 3. Subcutaneous 4. Intramuscular 340. An opioid analgesic is administered to a client in labor. The nurse assigned to care for the client ensures that which medication is readily accessible should respiratory depression occur? 1. Naloxone 2. Morphine sulfate 3. Betamethasone 4. Hydromorphone hydrochloride 341. Rh o(D) immune globulin is prescribed for a client after delivery and the nurse provides information to the client about the purpose of the medication. The nurse determines that the woman understands the purpose if the woman states that it will protect her next baby from which condition? 1. Having Rh-positive blood 2. Developing a rubella infection 3. Developing physiological jaundice 4. Being affected by Rh incompatibility 342. Methylergonovine is prescribed for a client with postpartum hemorrhage. Before administering the medication, the nurse should contact the health care provider who prescribed the medication if which condition is documented in the client’s medical history? 1. Hypotension 2. Hypothyroidism 3. Diabetes mellitus 4. Peripheral vascular disease 343. The nurse is monitoring a client in preterm labor who is receiving intravenous magnesium sulfate. The nurse should monitor for which adverse effects of this medication? Select all that apply. 1. Flushing 2. Hypertension 3. Increased urine output 4. Depressed respirations 5. Extreme muscle weakness 6. Hyperactive deep tendon reflexes 344. The nurse is monitoring a child with burns during treatment for burn shock. Which assessment provides the most accurate guide to determine the adequacy of fluid resuscitation? 1. Skin turgor 2. Level of edema at burn site 3. Adequacy of capillary filling 4. Amount of fluid tolerated in 24 hours 345. The mother of a 3-year-old child arrives at a clinic and tells the nurse that the child has been scratching the skin continuously and has developed a rash. The nurse assesses the child and suspects the presence of scabies. The nurse bases this suspicion on which finding noted on assessment of the child’s skin? 1. Fine grayish red lines 2. Purple-colored lesions 3. Thick, honey-colored crusts 4. Clusters of fluid-filled vesicles 346. Permethrin is prescribed for a child with a diagnosis of scabies. The nurse should give which instruction to the parents regarding the use of this treatment? 1. Apply the lotion to areas of the rash only. 2. Apply the lotion and leave it on for 6 hours. 3. Avoid putting clothes on the child over the lotion. 4. Apply the lotion to cool, dry skin at least 30 minutes after bathing. 347. The school nurse has provided an instructional session about impetigo to parents of the children attending the school. Which statement, if made by a parent, indicates a need for further instruction? 1. “It is extremely contagious.” 2. “It is most common in humid weather.” 3. “Lesions most often are located on the arms and chest.” 4. “It might show up in an area of broken skin, such as an insect bite.” Pediatrics RELATIVE PERCENTAGES OF AREAS AFFECTED BY GROWTH AREA A = B = C = ½ of he ad ½ of one thigh ½ of one leg BIRTH 9½ 2¾ 2½ AGE 1 YR 8½ 3¼ 2½ AGE 5 YR 6½ 42 ¾ RELATIVE PERCENTAGES OF AREAS AFFECTED BY GROWTH AREA A = B = C = ½ of he ad ½ of one thigh ½ of one leg AGE 10 YR 5½ 4½ 3 AGE 15 YR 4½ 4½ 3¼ YOUNG ADULT 3½ 4¾ 3½ B C A B B C 1 1 1 1 1 1 1 13 13 2 2 2 2 2 2 B C B C A A 1¾ 1¼ 1¼ 1¼ 1¼ 1¾ A B B C C 1 13 2 2 1¼ 1¼ 1¾ 1¾ 1½ 1½ A B B C C 1 1 13 2 2 1¼ 1¼ 1¾ 1¾ 1½ 1½ 2½ 2½ 1 1 FIGURE 33-3 Estimation of distribution of burns in children. A, Children from birth to age 5 years. B, Older children. 408 UNIT VII Pediatric Nursing Pediatrics 348. The clinic nurse is reviewing the health care provider’s prescription for a child who has been diagnosed with scabies. Lindane has been prescribed for the child. The nurse questions the prescription if which is noted in the child’s record? 1. The child is 18 months old. 2. The child is being bottle-fed. 3. A sibling is using lindane for the treatment of scabies. 4. The child has a history of frequent respiratory infections. 349. A topical corticosteroid is prescribed by the health care provider for a child with atopic dermatitis (eczema). Which instruction should the nurse give the parent about applying the cream? 1. Apply the cream over the entire body. 2. Apply a thick layer of cream to affected areas only. 3. Avoid cleansing the area before application of the cream. 4. Apply a thin layer of cream and rub it into the area thoroughly. 350. The school nurse is performing pediculosis capitis (head lice) assessments. Which assessment finding indicates that a child has a “positive” head check? 1. Maculopapular lesions behind the ears 2. Lesions in the scalp that extend to the hairline or neck 3. White flaky particles throughout the entire scalp region 4. White sacs attached to the hair shafts in the occipital area 351. The nurse caring for a child who sustained a burn injury plans care based on which pediatric considerations associated with this injury? Select all that apply. 1. Scarring is less severe in a child than in an adult. 2. A delay in growth may occur after a burn injury. 3. An immature immune system presents an increased risk of infection for infants and young children. 4. Fluid resuscitation is unnecessary unless the burned area is more than 25% of the total body surface area. 5. The lower proportion of body fluid to body mass in a child increases the risk of cardiovascular problems. 6. Infants and young children are at increased risk for protein and calorie deficiency because they have smaller muscle mass and less body fat than adults. 352. The nurse analyzes the laboratory results of a child with hemophilia. The nurse understands that which result will most likely be abnormal in this child? 1. Platelet count 2. Hematocrit level 3. Hemoglobin level 4. Partial thromboplastin time 353. The nurse is providing home care instructions to the parents of a 10-year-old child with hemophilia. Which sport activity should the nurse suggest for this child? 1. Soccer 2. Basketball 3. Swimming 4. Field hockey 354. The nursing student is presenting a clinical conference and discusses the cause of β-thalassemia. The nursing student informs the group that a child at greatest risk of developing this disorder is which of these? 1. A child of Mexican descent 2. A child of Mediterranean descent 3. A child whose intake of iron is extremely poor 4. A breast-fed child of a mother with chronic anemia 355. A child with β-thalassemia is receiving long-term blood transfusion therapy for the treatment of the disorder. Chelation therapy is prescribed as a result of too much iron from the transfusions. Which m edication should the nurse anticipate to be prescribed? 1. Fragmin 2. Meropenem 3. Metoprolol 4. Deferoxamine 356. The clinic nurse instructs parents of a child with sickle cell anemia about the precipitating factors related to sickle cell crisis. Which, if identified by the parents as a precipitating factor, indicates the need for further instruction ? 1. Stress 2. Traum a 3. Infection 4. Fluid overload 357. A 10-year-old child with hemophilia A has slipped on the ice and bumped his knee. The nurse should prepare to administer which prescription? 1. Injection of factor X 2. Intravenous infusion of iron 3. Intravenous infusion of factor VIII 4. Intramuscular injection of iron using the Z-track method 358. The nurse is instructing the parents of a child with iron deficiency anemia regarding the administration of a liquid oral iron supplem ent. Which instruction should the nurse tell the parents? 1. Administer the iron at m ealtim es. 2. Administer the iron through a straw. 3. Mix the iron with cereal to administer. 4. Add the iron to formula for easy administration. 359. Laboratory studies are perform ed for a child suspected to have iron deficiency anemia. The nurse reviews the laboratory results, knowing that which result indicates this type of anemia? 1. Elevated hemoglobin level 2. Decreased reticulocyte count 3. Elevated red blood cell count 4. Red blood cells that are microcytic and hypochromic 360. The nurse is reviewing a health care provider’s prescriptions for a child with sickle cell anemia who was admitted to the hospital for the treatm ent of vaso-occlusive crisis. Which prescriptions documented in the child’s record should the nurse question? Select all th at apply. 1. Restrict fluid intake. 2. Position for comfort. 3. Avoid strain on painful joints. 4. Apply nasal oxygen at 2 L/minute. 5. Provide a high-calorie, high-protein diet. 6. Give m eperidine, 25 mg intravenously, every 4 hours for pain. CHAPTER 34 Hematological Disorders 415 361. The nurse is conducting staff in-service training on von Willebrand’s disease. Which should the nurse include as characteristics of von Willebrand’s disease? Select all that apply. 1. Easy bruising occurs. 2. Gum bleeding occurs. 3. It is a hereditary bleeding disorder. 4. Treatment and care are similar to that for hemophilia. 5. It is characterized by extremely high creatinine levels. 6. The disorder causes platelets to adhere to damaged endothelium 362. The nurse is monitoring a child for bleeding after surgery for removal of a brain tumor. The nurse checks the head dressing for the presence of blood and notes a colorless drainage on the back of the dressing. Which intervention should the nurse perform immediately? 1. Reinforce the dressing. 2. Notify the health care provider (HCP). 3. Document the findings and continue to monitor. 4. Circle the area of drainage and continue to monitor. 363. A child undergoes surgical removal of a brain tumor. During the postoperative period, the nurse notes that the child is restless, the pulse rate is elevated, and the blood pressure has decreased significantly from the baseline value. The nurse suspects that the child is in shock. Which is the most appropriate nursing action? 1. Place the child in a supine position. 2. Notify the health care provider (HCP). 3. Place the child in Trendelenburg position. 4. Increase the flow rate of the intravenous fluids. 364. The mother of a 4-year-old child tells the pediatric nurse that the child’s abdomen seems to be swollen. During further assessment, the mother tells the nurse that the child is eating well and that the activity level of the child is unchanged. The nurse, suspecting the possibility of Wilms’ tumor, should avoid which during the physical assessment? 1. Palpating the abdomen for a mass 2. Assessing the urine for the presence of hematuria 3. Monitoring the temperature for the presence of fever 4. Monitoring the blood pressure for the presence of hypertension 365. The nurse provides a teaching session to the nursing staff regarding osteosarcoma. Which statement by a member of the nursing staff indicates a need for information? 1. “The femur is the most common site of this sarcoma.” 2. “The child does not experience pain at the primary tumor site.” 3. “Limping, if a weight-bearing limb is affected, is a clinical manifestation.” 4. “The symptoms of the disease in the early stage are almost always attributed to normal growing pains.” BOX 35-4 Positioning After Craniotomy Assess the health care provider’s prescription for positioning, including the degree of neck flexion. If a large tumor has been removed, the child is not placed on the operative side because the brain may shift suddenly to that cavity. In an infratentorial procedure, the child usually is positioned flat and on either side. In a supratentorial procedure, the head usually is elevated above the heart level to facilitate cerebrospinal fluid drainage and to decrease excessive blood flow to the brain to prevent hemorrhage. Never place the child in Trendelenburg position because it increases intracranial pressure and the risk of hemorrhage. CHAPTER 35 Oncological Disorders 425 366. The nurse analyzes the laboratory values of a child with leukemia who is receiving chemotherapy. The nurse notes that the platelet count is 19,500 mm 3 (19.5 Â 109/L). On the basis of this laboratory result, which intervention should the nurse include in the plan of care? 1. Initiate bleeding precautions. 2. Monitor closely for signs of infection. 3. Monitor the temperature every 4 hours. 4. Initiate protective isolation precautions. 367. The nurse is monitoring a 3-year-old child for signs and symptoms of increased intracranial pressure (ICP) after a craniotomy. The nurse plans to monitor for which early sign or symptom of increased ICP? 1. Vomiting 2. Bulging anterior fontanel 3. Increasing head circumference 4. Complaints of a frontal headache 368. A 4-year-old child is admitted to the hospital for abdominal pain. The mother reports that the child has been pale and excessively tired and is bruising easily. On physical examination, lymphadenopathy and hepatosplenomegaly are noted. Diagnostic studies are being performed because acute lymphocytic leukemia is suspected. The nurse determines that which laboratory result confirms the diagnosis? 1. Lumbar puncture showing no blast cells 2. Bone marrow biopsy showing blast cells 3. Platelet count of 350,000 mm 3 (350 Â 109/L) 4. White blood cell count 4500 mm 3 (4.5 Â 109/L) 369. A 6-year-old child with leukemia is hospitalized and is receiving combination chemotherapy. Laboratory results indicate that the child is neutropenic, and protective isolation procedures are initiated. The grandmother of the child visits and brings a fresh bouquet of flowers picked from her garden, and asks the nurse for a vase for the flowers. Which response should the nurse provide to the grandmother? 1. “I have a vase in the utility room, and I will get it for you.” 2. “I will get the vase and wash it well before you put the flowers in it.” 3. “The flowers from your garden are beautiful, but should not be placed in the child’s room at this time.” 4. “When you bring the flowers into the room, place them on the bedside stand as far away from the child as possible.” 370. A diagnosis of Hodgkin’s disease is suspected in a 12-year-old child. Several diagnostic studies are performed to determine the presence of this disease. Which diagnostic test result will confirm the diagnosis of Hodgkin’s disease? 1. Elevated vanillylmandelic acid urinary levels 2. The presence of blast cells in the bone marrow 3. The presence of Epstein-Barr virus in the blood 4. The presence of Reed-Sternberg cells in the lymph nodes 371. Which specific nursing interventions are implemented in the care of a child with leukemia who is at risk for infection? Select all that apply. 1. Maintain the child in a semiprivate room. 2. Reduce exposure to environmental organisms. 3. Use strict aseptic technique for all procedures. 4. Ensure that anyone entering the child’s room wears a mask. 5. Apply firm pressure to a needle-stick area for at least 10 minutes. 372. The nurse is performing an assessment on a 10- year-old child suspected to have Hodgkin’s disease. Which assessment findings are specifically characteristic of this disease? Select all that apply. 1. Abdominal pain 2. Fever and malaise 3. Anorexia and weight loss 4. Painful, enlarged inguinal lymph nodes 5. Painless, firm, and movable adenopathy in the cervical area 373. Aschool-age child with type 1 diabetes mellitus has soccer practice and the school nurse provides instructions regarding how to prevent hypoglycemia during practice. Which should the school nurse tell the child to do? 1. Eat twice the amount normally eaten at lunchtime. 2. Take half the amount of prescribed insulin on practice days. 3. Take the prescribed insulin at noontime rather than in the morning. 4. Eat a small box of raisins or drink a cup of orange juice before soccer practice. 374. The mother of a 6-year-old child who has type 1 diabetes mellitus calls a clinic nurse and tells the nurse that the child has been sick. The mother reports that she checked the child’s urine and it was positive for ketones. The nurse should instruct the mother to take which action? 1. Hold the next dose of insulin. 2. Come to the clinic immediately. 3. Encourage the child to drink liquids. 4. Administer an additional dose of regular insulin. 375. A health care provider prescribes an intravenous (IV) solution of 5% dextrose and half-normal saline (0.45%) with 40 mEq of potassium chloride for a child with hypotonic dehydration. The nurse performs which priority assessment before administering this IV prescription? 1. Obtains a weight 2. Takes the temperature 3. Takes the blood pressure 4. Checks the amount of urine output Pediatrics BOX 36-5 Sick Day Rules for a Diabetic Child Always give insulin, even if the child does not have an appetite, or contact the health care provider (HCP) for specific instructions. Test blood glucose levels at least every 4 hours. Test for urinary ketones with each voiding. Notify the HCP if moderate or large amounts of urinary ketones are present. Follow the child’s usual meal plan. Encourage liquids to aid in clearing ketones. Encourage rest, especially if urinary ketones are present. Notify the HCP if vomiting, fruity odor to the breath, deep rapid respirations, decreasing level of consciousness, or persistent hyperglycemia occurs. Adapted from Hockenberry M, Wilson D: Nursing care of infants and children, ed 9, St. Louis, 2011, Mosby. CHAPTER 36 Metabolic and Endocrine Disorders 435 376. An adolescent client with type 1 diabetes mellitus is admitted to the emergency department for treatment of diabetic ketoacidosis. Which assessment findings should the nurse expect to note? 1. Sweating and tremors 2. Hunger and hypertension 3. Cold, clammy skin and irritability 4. Fruity breath odor and decreasing level of consciousness 377. A mother brings her 3-week-old infant to a clinic for a phenylketonuria rescreening blood test. The test indicates a serum phenylalanine level of 1 mg/dL (60.5 mcmol/L). The nurse reviews this result and makes which interpretation? 1. It is positive. 2. It is negative. 3. It is inconclusive. 4. It requires rescreening at age 6 weeks. 378. A child with type 1 diabetes mellitus is brought to the emergency department by the mother, who states that the child has been complaining of abdominal pain and has been lethargic. Diabetic ketoacidosis is diagnosed. Anticipating the plan of care, the nurse prepares to administer which type of intravenous (IV) infusion? 1. Potassium infusion 2. NPH insulin infusion 3. 5% dextrose infusion 4. Normal saline infusion 379. The nurse has just administered ibuprofen to a child with a temperature of 102 °F (38.8 °C). The nurse should also take which action? 1. Withhold oral fluids for 8 hours. 2. Sponge the child with cold water. 3. Plan to administer salicylate in 4 hours. 4. Remove excess clothing and blankets from the child. 380. A child has fluid volume deficit. The nurse performs an assessment and determines that the child is improving and the deficit is resolving if which finding is noted? 1. The child has no tears. 2. Urine specific gravity is 1.035. 3. Capillary refill is less than 2 seconds. 4. Urine output is less than 1 mL/kg/hour. 381. The nurse should implement which interventions for a child older than 2 years with type 1 diabetes mellitus who has a blood glucose level of 60 mg/dL (3.4 mmol/L)? Select all that apply. 1. Administer regular insulin. 2. Encourage the child to ambulate. 3. Give the child a teaspoon of honey. 4. Provide electrolyte replacement therapy intravenously. 5. Wait 30 minutes and confirm the blood glucose reading. 6. Prepare to administer glucagon subcutaneously if unconsciousness occurs. 382. The clinic nurse reviews the record of an infant and notes that the health care provider has documented a diagnosis of suspected Hirschsprung’s disease. The nurse reviews the assessment findings documented in the record, knowing that which sign most likely led the mother to seek health care for the infant? 1. Diarrhea 2. Projectile vomiting 3. Regurgitation of feedings 4. Foul-smelling ribbon-like stools 383. An infant has just returned to the nursing unit after surgical repair of a cleft lip on the right side. The nurse should place the infant in which best position at this time? 1. Prone position 2. On the stomach 3. Left lateral position 4. Right lateral position 384. The nurse reviews the record of a newborn infant and notes that a diagnosis of esophageal atresia with tracheoesophageal fistula is suspected. The nurse expects to note which most likely sign of this condition documented in the record? 1. Incessant crying 2. Coughing at nighttime 3. Choking with feedings 4. Severe projectile vomiting CHAPTER 37 Gastrointestinal Disorders 453 Pediatrics 385. The nurse provides feeding instructions to a parent of an infant diagnosed with gastroesophageal reflux disease. Which instruction should the nurse give to the parent to assist in reducing the episodes of emesis? 1. Provide less frequent, larger feedings. 2. Burp the infant less frequently during feedings. 3. Thin the feedings by adding water to the formula. 4. Thicken the feedings by adding rice cereal to the formula. 386. A child is hospitalized because of persistent vomiting. The nurse should monitor the child closely for which problem? 1. Diarrhea 2. Metabolic acidosis 3. Metabolic alkalosis 4. Hyperactive bowel sounds 387. The nurse is caring for a newborn with a suspected diagnosis of imperforate anus. The nurse monitors the infant, knowing that which is a clinical manifestation associated with this disorder? 1. Bile-stained fecal emesis 2. The passage of currant jelly–like stools 3. Failure to pass meconium stool in the first 24 hours after birth 4. Sausage-shaped mass palpated in the upper right abdominal quadrant 388. The nurse admits a child to the hospital with a diagnosis of pyloric stenosis. On assessment, which data would the nurse expect to obtain when asking the parent about the child’s symptoms? 1. Watery diarrhea 2. Projectile vomiting 3. Increased urine output 4. Vomiting large amounts of bile 389. The nurse provides home care instructions to the parents of a child with celiac disease. The nurse should teach the parents to include which food item in the child’s diet? 1. Rice 2. Oatmeal 3. Rye toast 4. Wheat bread 390. The nurse is preparing to care for a child with a diagnosis of intussusception. The nurse reviews the child’s record and expects to note which sign of this disorder documented? 1. Watery diarrhea 2. Ribbon-like stools 3. Profuse projectile vomiting 4. Bright red blood and mucus in the stools 391. Which interventions should the nurse include when creating a care plan for a child with hepatitis? Select all that apply. 1. Providing a low-fat, well-balanced diet. 2. Teaching the child effective hand-washing techniques. 3. Scheduling playtime in the playroom with other children. 4. Notifying the health care provider (HCP) if jaundice is present. 5. Instructing the parents to avoid administering medications unless prescribed. 6. Arranging for indefinite home schooling because the child will not be able to return to school. 392. After a tonsillectomy, a child begins to vomit bright red blood. The nurse should take which initial action? 1. Turn the child to the side. 2. Administer the prescribed antiemetic. 3. Notify the health care provider (HCP). 4. Maintain NPO (nothing by mouth) status. 393. The mother of a 6-year-old child arrives at a clinic because the child has been experiencing itchy, red, and swollen eyes. The nurse notes a discharge from the eyes and sends a culture to the laboratory for analysis. Chlamydial conjunctivitis is diagnosed. On the basis of this diagnosis, the nurse determines that which requires further investigation? 1. Possible trauma 2. Possible sexual abuse 3. Presence of an allergy 4. Presence of a respiratory infection 394. The nurse prepares a teaching plan for the mother of a child diagnosed with bacterial conjunctivitis. Which, if stated by the mother, indicates a need for further teaching? 1. “I need to wash my hands frequently.” 2. “I need to clean the eye as prescribed.” 3. “It is okay to share towels and washcloths.” 4. “I need to give the eye drops as prescribed.” 395. The nurse is reviewing the laboratory results for a child scheduled for a tonsillectomy. The nurse determines that which laboratory value is most significant to review? 1. Creatinine level 2. Prothrombin time 3. Sedimentation rate 4. Blood urea nitrogen level 396. The nurse is preparing to care for a child after a tonsillectomy. The nurse documents on the plan of care to place the child in which position? 1. Supine 2. Side-lying 3. High Fowler’s 4. Trendelenburg 397. After a tonsillectomy, the nurse reviews the health care provider’s (HCP’s) postoperative prescriptions. Which prescription should the nurse question? 1. Monitor for bleeding. 2. Suction every 2 hours. 3. Give no milk or milk products. 4. Give clear, cool liquids when awake and alert. 398. The nurse is caring for a child after a tonsillectomy. The nurse monitors the child, knowing that which finding indicates the child is bleeding? 1. Frequent swallowing 2. A decreased pulse rate 3. Complaints of discomfort 4. An elevation in blood pressure 399. Antibiotics are prescribed for a child with otitis media who underwent a myringotomy with insertion of tympanostomy tubes. The nurse provides discharge instructions to the parents regarding the administration of the antibiotics. Which statement, if made by the parents, indicates understanding of the instructions provided? 1. “Administer the antibiotics until they are gone.” 2. “Administer the antibiotics if the child has a fever.” 3. “Administer the antibiotics until the child feels better.” 4. “Begin to taper the antibiotics after 3 days of a full course.” 460 UNIT VII Pediatric Nursing Pediatrics 400. The day care nurse is observing a 2-year-old child and suspects that the child may have strabismus. Which observation made by the nurse indicates the presence of this condition? 1. The child has difficulty hearing. 2. The child consistently tilts the head to see. 3. The child does not respond when spoken to. 4. The child consistently turns the head to hear. 401. A child has been diagnosed with acute otitis media of the right ear. Which interventions should the nurse include in the plan of care? Select all that apply. 1. Provide a soft diet. 2. Position the child on the left side. 3. Administer an antihistamine twice daily. 4. Irrigate the right ear with normal saline every 8 hours. 5. Administer ibuprofen for fever every 4 hours as prescribed and as needed. 6. Instruct the parents about the need to administer the prescribed antibiotics for the full course of therapy. 402. A10-year-old child with asthma is treated for acute exacerbation in the emergency department. The nurse caring for the child should monitor for which sign, knowing that it indicates a worsening of the condition? 1. Warm, dry skin 2. Decreased wheezing 3. Pulse rate of 90 beats/minute 4. Respirations of 18 breaths/minute 403. The mother of an 8-year-old child being treated for right lower lobe pneumonia at home calls the clinic nurse. The mother tells the nurse that the child complains of discomfort on the right side and that ibuprofen is not effective. Which instruction should the nurse provide to the mother? 1. Increase the dose of ibuprofen. 2. Increase the frequency of ibuprofen. 3. Encourage the child to lie on the left side. 4. Encourage the child to lie on the right side. 404. Anew parent expresses concern to the nurse regarding sudden infant death syndrome (SIDS). She asks the nurse how to position her new infant for sleep. In which position should the nurse tell the parent to place the infant? 1. Side or prone 2. Back or prone 3. Stomach with the face turned 4. Back rather than on the stomach 405. The clinic nurse is providing instructions to a parent of a child with cystic fibrosis regarding the immunization schedule for the child. Which statement should the nurse make to the parent? 1. “The immunization schedule will need to be altered.” 2. “The child should not receive any hepatitis vaccines.” 3. “The child will receive all of the immunizations except for the polio series.” 4. “The child will receive the recommended basic series of immunizations along with a yearly influenza vaccination.” 406. The emergency department nurse is caring for a child diagnosed with epiglottitis. In assessing the child, the nurse should monitor for which indication that the child may be experiencing airway obstruction? 1. The child exhibits nasal flaring and bradycardia. 2. The child is leaning forward, with the chin thrust out. 3. The child has a low-grade fever and complains of a sore throat. 4. The child is leaning backward, supporting himself or herself with the hands and arms. 407. A child with laryngotracheobronchitis (croup) is placed in a cool mist tent. The mother becomes concerned because the child is frightened, consistently crying and trying to climb out of the tent. Which is the most appropriate nursing action? 1. Tell the mother that the child must stay in the tent. 2. Place a toy in the tent to make the child feel more comfortable. 3. Call the health care provider and obtain a prescription for a mild sedative. 4. Let the mother hold the child and direct the cool mist over the child’s face. 408. The clinic nurse reads the results of a tuberculin skin test (TST) on a 3-year-old child. The results indicate an area of induration measuring 10 mm. The nurse should interpret these results as which finding? 1. Positive 2. Negative 3. Inconclusive 4. Definitive and requiring a repeat test 409. The mother of a hospitalized 2-year-old child with viral laryngotracheobronchitis (croup) asks the nurse why the health care provider did not prescribe antibiotics. Which response should the nurse make? 1. “The child may be allergic to antibiotics.” 2. “The child is too young to receive antibiotics.” 3. “Antibiotics are not indicated unless a bacterial infection is present.” 4. “The child still has the maternal antibodies from birth and does not need antibiotics.” 410. The nurse is caring for an infant with bronchiolitis, and diagnostic tests have confirmed respiratory syncytial virus (RSV). On the basis of this finding, which is the most appropriate nursing action? 1. Initiate strict enteric precautions. 2. Move the infant to a room with another child with RSV. 3. Leave the infant in the present room because RSV is not contagious. 4. Inform the staff that they must wear a mask, gloves, and a gown when caring for the child. 411. The nurse is preparing for the admission of an infant with a diagnosis of bronchiolitis caused by Pediatrics CHAPTER 39 Respiratory Disorders 475 respiratory syncytial virus (RSV). Which interventions should the nurse include in the plan of care? Select all that apply. 1. Place the infant in a private room. 2. Ensure that the infant’s head is in a flexed position. 3. Wear a mask at all times when in contact with the infant. 4. Place the infant in a tent that delivers warm humidified air. 5. Position the infant on the side, with the head lower than the chest. 6. Ensure that nurses caring for the infant with RSV do not care for other high-risk children 412. The nurse is monitoring an infant with congenital heart disease closely for signs of heart failure (HF). The nurse should assess the infant for which early sign of HF? 1. Pallor 2. Cough 3. Tachycardia 4. Slow and shallow breathing 413. The nurse reviews the laboratory results for a child with a suspected diagnosis of rheumatic fever, knowing that which laboratory study would assist in confirming the diagnosis? 1. Immunoglobulin 2. Red blood cell count 3. White blood cell count 4. Anti–streptolysin O titer 414. On assessment of a child admitted with a diagnosis of acute-stage Kawasaki disease, the nurse expects to note which clinical manifestation of the acute stage of the disease? 1. Cracked lips 2. Normal appearance 3. Conjunctival hyperemia 4. Desquamation of the skin 415. The nurse provides home care instructions to the parents of a child with heart failure regarding the procedure for administration of digoxin. Which statement made by the parent indicates the need for further instruction? 1. “I will not mix the medication with food.” 2. “I will take my child’s pulse before administering the medication.” 3. “If more than 1 dose is missed, I will call the health care provider.” 4. “If my child vomits after medication administration, I will repeat the dose.” BOX40-6 Parent Education for Kawasaki Disease Follow-up care is essential to recovery. Signs and symptoms of Kawasaki disease include the following: Irritability that may last for 2 months after the onset of symptoms Peeling of the hands and feet Pain in the joints that may persist for several weeks Stiffness in the morning, after naps, and in cold temperatures Record the temperature (because fever is expected) until the child has been afebrile for several days. Notify the health care provider if the temperature is 101 °F (38.3 °C) or higher. Salicylates such as acetylsalicylic acid (aspirin) may be prescribed. Signs of aspirin toxicity include tinnitus, headache, vertigo, and bruising; do not administer aspirin or aspirincontaining products if the child has been exposed to chickenpox or the flu. Signs and symptoms of bleeding include epistaxis (nosebleeds), hemoptysis (coughing up blood), hematemesis (vomiting up blood), hematuria (blood in urine), melena (blood in stool), and bruises on the body. Signs and symptoms of cardiac complications include chest pain or tightness (older children), cool and pale extremities, abdominal pain, nausea and vomiting, irritability, restlessness, and uncontrollable crying. The child should avoid contact sports, if age appropriate, if taking aspirin or anticoagulants. Avoid administration of measles, mumps, and rubella (MMR) or varicella vaccine to the child for 11 months after intravenous immunoglobulin therapy, if appropriate. CHAPTER 40 Cardiovascular Disorders 487 416. The nurse is closely monitoring the intake and output of an infant with heart failure who is receiving diuretic therapy. The nurse should use which most appropriate method to assess the urine output? 1. Weighing the diapers 2. Inserting a urinary catheter 3. Comparing intake with output 4. Measuring the amount of water added to formula 417. The clinic nurse reviews the record of a child just seen by a health care provider and diagnosed with suspected aortic stenosis. The nurse expects to note documentation of which clinical manifestation specifically found in this disorder? 1. Pallor 2. Hyperactivity 3. Exercise intolerance 4. Gastrointestinal disturbances 418. The nurse has provided home care instructions to the parents of a child who is being discharged after cardiac surgery. Which statement made by the parents indicates a need for further instruction? 1. “A balance of rest and exercise is important.” 2. “I can apply lotion or powder to the incision if it is itchy.” 3. “Activities in which my child could fall need to be avoided for 2 to 4 weeks.” 4. “Large crowds of people need to be avoided for at least 2 weeks after surgery.” 419. A child with rheumatic fever will be arriving to the nursing unit for admission. On admission assessment, the nurse should ask the parents which question to elicit assessment information specific to the development of rheumatic fever? 1. “Has the child complained of back pain?” 2. “Has the child complained of headaches?” 3. “Has the child had any nausea or vomiting?” 4. “Did the child have a sore throat or fever within the last 2 months?” 420. A health care provider has prescribed oxygen as needed for an infant with heart failure. In which situation should the nurse administer the oxygen to the infant? 1. During sleep 2. When changing the infant’s diapers 3. When the mother is holding the infant 4. When drawing blood for electrolyte level testing 421. Assessment findings of an infant admitted to the hospital reveal a machinery-like murmur on auscultation of the heart and signs of heart failure. The nurse reviews congenital cardiac anomalies and identifies the infant’s condition as which disorder? Refer to figure (the circled area) to determine the condition. 1. Aortic stenosis 2. Atrial septal defect 3. Patent ductus arteriosus 4. Ventricular septal defect 422. The nurse reviews the record of a child who is suspected to have glomerulonephritis. Which statement by the child’s parent should the nurse expect that is associated with this diagnosis? 1. “I’m so glad they didn’t find any protein in his urine.” 2. “I noticed his urine was the color of coca-cola lately.” 3. “His health care provider said his kidneys are working well.” 4. “The nurse who admitted my child said his blood pressure was low.” 423. The nurse performing an admission assessment on a 2-year-old child who has been diagnosed with nephrotic syndrome notes that which most common characteristic is associated with this syndrome? 1. Hypertension 2. Generalized edema 3. Increased urinary output 4. Frank, bright red blood in the urine 424. The nurse is planning care for a child with hemolytic-uremic syndrome who has been anuric and will be receiving peritoneal dialysis treatment. The nurse should plan to implement which measure? 1. Restrict fluids as prescribed. 2. Care for the arteriovenous fistula. 3. Encourage foods high in potassium. 4. Administer analgesics as prescribed. 425. A 7-year-old child is seen in a clinic, and the health care provider documents a diagnosis of primary nocturnal enuresis. The nurse should provide which information to the parents? 1. Primary nocturnal enuresis does not respond to treatment. 2. Primary nocturnal enuresis is caused by a psychiatric problem. 3. Primary nocturnal enuresis requires surgical intervention to improve the problem. 4. Primary nocturnal enuresis is usually outgrown without therapeutic intervention. CHAPTER 41 Renal and Urinary Disorders 495 426. The nurse provided discharge instructions to the parents of a 2-year-old child who had an orchiopexy to correct cryptorchidism. Which statement by the parents indicates the need for further instruction? 1. “I’ll check his temperature.” 2. “I’ll give him medication so he’ll be comfortable.” 3. “I’ll check his voiding to be sure there’s no problem.” 4. “I’ll let him decide when to return to his play activities.” 427. The nurse is reviewing a treatment plan with the parents of a newborn with hypospadias. Which statement by the parents indicates their understanding of the plan? 1. “Caution should be used when straddling the infant on a hip.” 2. “Vital signs should be taken daily to check for bladder infection.” 3. “Catheterization will be necessary when the infant does not void.” 4. “Circumcision has been delayed to save tissue for surgical repair.” 428. The nurse is caring for an infant with a diagnosis of bladder exstrophy. To protect the exposed bladder tissue, the nurse should plan which intervention? 1. Cover the bladder with petroleum jelly gauze. 2. Cover the bladder with a nonadhering plastic wrap. 3. Apply sterile distilled water dressings over the bladder mucosa. 4. Keep the bladder tissue dry by covering it with dry sterile gauze. 429. Which question should the nurse ask the parents of a child suspected of having glomerulonephritis? 1. “Did your child fall off a bike onto the handlebars?” 2. “Has the child had persistent nausea and vomiting?” 3. “Has the child been itching or had a rash anytime in the last week?” 4. “Has the child had a sore throat or a throat infection in the last few weeks?” 430. The nurse collects a urine specimen preoperatively from a child with epispadias who is scheduled for surgical repair. When analyzing the results of the urinalysis, which should the nurse most likely expect to note? 1. Hematuria 2. Proteinuria 3. Bacteriuria 4. Glucosuria 431. The nurse is performing an assessment on a child admitted to the hospital with a probable diagnosis of nephrotic syndrome. Which assessment findings should the nurse expect to observe? Select all that apply. 1. Pallor 2. Edema 3. Anorexia 4. Proteinuria 5. Weight loss 6. Decreased serum lipids 432. The parents of a child recently diagnosed with cerebral palsy ask the nurse about the limitations of the disorder. The nurse responds by explaining that the limitations occur as a result of which pathophysiological process? 1. An infectious disease ofthe central nervoussystem 2. An inflammation of the brain as a result of a viral illness 3. A chronic disability characterized by impaired muscle movement and posture 4. A congenital condition that results in moderate to severe intellectual disabilities 433. The nurse notes documentation that a child is exhibiting an inability to flex the leg when the thigh is flexed anteriorly at the hip. Which condition does the nurse suspect? 1. Meningitis 2. Spinal cord injury 3. Intracranial bleeding 4. Decreased cerebral blood flow 434. A mother arrives at the emergency department with her 5-year-old child and states that the child fell off a bunk bed. A head injury is suspected. The nurse 506 UNIT VII Pediatric Nursing checks the child’s airway status and assesses the child for early and late signs of increased intracranial pressure (ICP). Which is a late sign of increased ICP? 1. Nausea 2. Irritability 3. Headache 4. Bradycardia 435. The nurse is assigned to care for an 8-year-old child with a diagnosis of a basilar skull fracture. The nurse reviews the health care provider’s (HCP’s) prescriptions and should contact the HCP to question which prescription? 1. Obtain daily weight. 2. Provide clear liquid intake. 3. Nasotracheal suction as needed. 4. Maintain a patent intravenous line. 436. The nurse is reviewing the record of a child with increased intracranial pressure and notes that the child has exhibited signs of decerebrate posturing. On assessment of the child, the nurse expects to note which characteristic of this type of posturing? 1. Flaccid paralysis of all extremities 2. Adduction of the arms at the shoulders 3. Rigid extension and pronation of the arms and legs 4. Abnormal flexion of the upper extremities and extension and adduction ofthe lower extremities 437. A child is diagnosed with Reye’s syndrome. The nurse creates a nursing care plan for the child and should include which intervention in the plan? 1. Assessing hearing loss 2. Monitoring urine output 3. Changing body position every 2 hours 4. Providing a quiet atmosphere with dimmed lighting 438. The nurse creates a plan of care for a child at risk for tonic-clonic seizures. In the plan of care, the nurse identifies seizure precautions and documents that which item(s) need to be placed at the child’s bedside? 1. Emergency cart 2. Tracheotomy set 3. Padded tongue blade 4. Suctioning equipment and oxygen 439. A lumbar puncture is performed on a child suspected to have bacterial meningitis, and cerebrospinal fluid (CSF) is obtained for analysis. The nurse reviews the results of the CSF analysis and determines that which results would verify the diagnosis? 1. Clear CSF, decreased pressure, and elevated protein level 2. Clear CSF, elevated protein, and decreased glucose levels 3. Cloudy CSF, elevated protein, and decreased glucose levels 4. Cloudy CSF, decreased protein, and decreased glucose levels 440. The nurse is planning care for a child with acute bacterial meningitis. Based on the mode of transmission of this infection, which precautionary intervention should be included in the plan of care? 1. Maintain enteric precautions. 2. Maintain neutropenic precautions. 3. No precautions are required as long as antibiotics have been started. 4. Maintain respiratory isolation precautions for at least 24 hours after the initiation of antibiotics. 441. An infant with a diagnosis of hydrocephalus is scheduled for surgery. Which is the priority nursing intervention in the preoperative period? 1. Test the urine for protein. 2. Reposition the infant frequently. 3. Provide a stimulating environment. 4. Assess blood pressure every 15 minutes. 442. The nurse is creating a plan of care for a child who is at risk for seizures. Which interventions apply if the child has a seizure? Select all that apply. 1. Time the seizure. 2. Restrain the child. 3. Stay with the child. 4. Place the child in a prone position. 5. Move furniture away from the child. 6. Insert a padded tongue blade in the child’s mouth. 443. Achild has a right femur fracture caused by a motor vehicle crash and is placed in skin traction temporarily until surgery can be performed. During assessment, the nurse notes that the dorsalis pedis pulse is absent on the right foot. Which action should the nurse take? 1. Administer an analgesic. 2. Release the skin traction. 3. Apply ice to the extremity. 4. Notify the health care provider (HCP). 444. Achild is placed in skeletal traction for treatment of a fractured femur. The nurse creates a plan of care and should include which intervention? 1. Ensure that all ropes are outside the pulleys. 2. Ensure that the weights are resting lightly on the floor. 3. Restrict diversional and play activities until the child is out of traction. 4. Check the health care provider’s (HCP’s) prescriptions for the amount of weight to be applied. 445. A 4-year-old child sustains a fall at home. After an x-ray examination, the child is determined to have a fractured arm and a plaster cast is applied. The nurse provides instructions to the parents regarding care for the child’s cast. Which statement by the parents indicates a need for further instruction? 1. “The cast may feel warm as the cast dries.” 2. “I can use lotion or powder around the cast edges to relieve itching.” 3. “Asmall amount of white shoe polish can touch up a soiled white cast.” 4. “If the cast becomes wet, a blow drier set on the cool setting may be used to dry the cast.” Pediatrics 516 UNIT VII Pediatric Nursing 446. The parents of a child with juvenile idiopathic arthritis call the clinic nurse because the child is experiencing a painful exacerbation of the disease. The parents ask the nurse if the child can perform range-of-motion exercises at this time. The nurse should make which response? 1. “Avoid all exercise during painful periods.” 2. “Range-of-motion exercises must be performed every day.” 3. “Have the child perform simple isometric exercises during this time.” 4. “Administer additional pain medication before performing range-of-motion exercises.” 447. A child who has undergone spinal fusion for scoliosis complains of abdominal discomfort and begins to have episodes of vomiting. On further assessment, the nurse notes abdominal distention. On the basis of these findings, the nurse should take which action? 1. Administer an antiemetic. 2. Increase the intravenous fluids. 3. Place the child in a Sims’ position. 4. Notify the health care provider (HCP). 448. The nurse is providing instructions to the parents of a child with scoliosis regarding the use of a brace. Which statement by the parents indicates a need for further instruction? 1. “I will encourage my child to perform prescribed exercises.” 2. “I will have my child wear soft fabric clothing under the brace.” 3. “I should apply lotion under the brace to prevent skin breakdown.” 4. “I should avoid the use of powder because it will cake under the brace.” 449. The nurse is assisting a health care provider (HCP) examining a 3-week-old infant with developmental dysplasia of the hip. What test or sign should the nurse expect the HCP to assess? 1. Babinski’s sign 2. The Moro reflex 3. Ortolani’s maneuver 4. The palmar-plantar grasp 450. A1-month-old infant is seen in a clinic and is diagnosed with developmental dysplasia of the hip. On assessment, the nurse understands that which finding should be noted in this condition? 1. Limited range of motion in the affected hip 2. An apparent lengthened femur on the affected side 3. Asymmetrical adduction of the affected hip when the infant is placed supine with the knees and hips flexed 4. Symmetry of the gluteal skinfolds when the infant is placed prone and the legs are extended against the examining table 451. Parents bring their 2-week-old infant to a clinic for treatment after a diagnosis of clubfoot made at birth. Which statement by the parents indicates a need for further teaching regarding this disorder? 1. “Treatment needs to be started as soon as possible.” 2. “I realize my infant will require follow-up care until fully grown.” 3. “I need to bring my infant back to the clinic in 1 month for a new cast.” 4. “I need to come to the clinic every week with my infant for the casting.” 452. The nurse prepares a list of home care instructions for the parents of a child who has a plaster cast applied to the left forearm. Which instructions should be included on the list? Select all that apply. 1. Use the fingertips to lift the cast while it is drying. 2. Keep small toys and sharp objects away from the cast. 3. Use a padded ruler or another padded object to scratch the skin under the cast if it itches. 4. Place a heating pad on the lower end of the cast and over the fingers if the fingers feel cold. 5. Elevate the extremity on pillows for the first 24 to 48 hours after casting to prevent swelling. 6. Contact the health care provider (HCP) if the child complains of numbness or tingling in the extremity 453. An infant of a mother infected with human immunodeficiency virus (HIV) is seen in the clinic each month and is being monitored for symptoms indicative of HIV infection. With knowledge of the most common opportunistic infection of children infected with HIV, the nurse assesses the infant for which sign? 1. Cough 2. Liver failure 3. Watery stool 4. Nuchal rigidity 454. The nurse provides home care instructions to the parent of a child with acquired immunodeficiency syndrome (AIDS). Which statement by the parent indicates the need for further teaching? 1. “I will wash my hands frequently.” 2. “I will keep my child’s immunizations up to date.” 3. “I will avoid direct unprotected contact with my child’s body fluids.” 4. “I can send my child to day care if he has a fever, as long as it is a low-grade fever.” 455. The clinic nurse is instructing the parent of a child with human immunodeficiency virus (HIV) infection regarding immunizations. The nurse should provide which instruction to the parent? 1. The hepatitis B vaccine will not be given to the child. 2. The inactivated influenza vaccine will be given yearly. 3. The varicella vaccine will be given before 6 months of age. 4. A Western blot test needs to be performed and the results evaluated before immunizations. 456. Ahealth care provider prescribes laboratory studies for an infant of a woman positive for human immunodeficiency virus (HIV). The nurse anticipates that which laboratory study will be prescribed for the infant? 1. Chest x-ray 2. Western blot 3. CD4+ cell count 4. p24 antigen assay 457. The mother with human immunodeficiency virus (HIV) infection brings her 10-month-old infant to the clinic for a routine checkup. The health care provider has documented that the infant is asymptomatic for HIV infection. After the checkup, the mother tells the nurse that she is so pleased that the infant will not get HIV infection. The nurse should make which most appropriate response to the mother? 1. “I am so pleased also that everything has turned out fine.” 2. “Because symptoms have not developed, it is unlikely that your infant will develop HIV infection.” 3. “Everything looks great, but be sure to return with your infant next month for the scheduled visit.” 4. “Most children infected with HIV develop symptoms within the first 9 months of life, and some become symptomatic sometime before they are 3 years old.” 458. A 6-year-old child with human immunodeficiency virus (HIV) infection has been admitted to the hospital for pain management. The child asks the nurse if the pain will ever go away. The nurse should make which best response to the child? 1. “The pain will go away if you lie still and let the medicine work.” CHAPTER 44 Infectious and Communicable Diseases 531 Pediatrics 2. “Try not to think about it. The more you think it hurts, the more it will hurt.” 3. “I know it must hurt, but if you tell me when it does, I will try to make it hurt a little less.” 4. “Every time it hurts, press on the call button and I will give you something to make the pain go all away.” 459. The nurse is caring for a 4-year-old child with human immunodeficiency virus (HIV) infection. The nurse should expect which statement that is aligned with the psychosocial expectations of this age? 1. “Being sick is scary.” 2. “I know it hurts to die.” 3. “I know I will be healthy soon.” 4. “I know I am different than other kids.” 460. The home care nurse provides instructions regarding basic infection control to the parent of an infant with human immunodeficiency virus (HIV) infection. Which statement, if made by the parent, indicates the need for further instruction? 1. “I will clean up any spills from the diaper with diluted alcohol.” 2. “I will wash baby bottles, nipples, and pacifiers in the dishwasher.” 3. “I will be sure to prepare foods that are high in calories and high in protein.” 4. “I will be sure to wash my hands carefully before and after caring for my infant.” 461. Which home care instructions should the nurse provide to the parent of a child with acquired immunodeficiency syndrome (AIDS)? Select all that apply. 1. Monitor the child’s weight. 2. Frequent hand washing is important. 3. The child should avoid exposure to other illnesses. 4. The child’s immunization schedule will need revision. 5. Clean up body fluid spills with bleach solution (10:1 ratio of water to bleach). 6. Fever, malaise, fatigue, weight loss, vomiting, and diarrhea are expected to occur and do not require special intervention. 462. The nurse provides home care instructions to the parents of a child hospitalized with pertussis who is in the convalescent stage and is being prepared for discharge. Which statement by a parent indicates a need for further instruction? 1. “We need to encourage our child to drink fluids.” 2. “Coughing spells may be triggered by dust or smoke.” 3. “Vomiting may occur when our child has coughing episodes.” 4. “We need to maintain droplet precautions and a quiet environment for at least 2 weeks.” 463. An infant receives a diphtheria, tetanus, and acellular pertussis (DTaP) immunization at a well-baby clinic. The parent returns home and calls the clinic to report that the infant has developed swelling and redness at the site of injection. Which intervention should the nurse suggest to the parent? 1. Monitor the infant for a fever. 2. Bring the infant back to the clinic. 3. Apply a hot pack to the injection site. 4. Apply a cold pack to the injection site. 464. Achild is receiving a series of the hepatitis Bvaccine and arrives at the clinic with his parent for the second dose. Before administering the vaccine, the nurse should ask the child and parent about a history of a severe allergy to which substance? 1. Eggs 2. Penicillin 3. Sulfonamides 4. A previous dose of hepatitis B vaccine or component 465. A parent brings her 4-month-old infant to a wellbaby clinic for immunizations. The child is up to date with the immunization schedule. The nurse should prepare to administer which immunizations to this infant? 1. Varicella, hepatitis B vaccine (HepB) 2. Diphtheria, tetanus, acellular pertussis (DTaP); measles, mumps, rubella (MMR); inactivated poliovirus vaccine (IPV) 3. MMR, Haemophilus influenzae type b (Hib), DTaP 4. DTaP, Hib, IPV, pneumococcal vaccine (PCV), rotavirus vaccine (RV) 466. The clinic nurse is assessing a child who is scheduled to receive a live virus vaccine (immunization). What are the general contraindications associated with receiving a live virus vaccine? Select all that apply. 1. The child has symptoms of a cold. 2. The child had a previous anaphylactic reaction to the vaccine. 3. The mother reports that the child is having intermittent episodes of diarrhea. 4. The mother reports that the child has not had an appetite and has been fussy. 5. The child has a disorder that caused a severely deficient immune system. 6. The mother reports that the child has recently been exposed to an infectious disease. 467. The nurse is providing medication instructions to a parent. Which statement by the parent indicates a need for further instruction? 1. “I should cuddle my child after giving the medication.” 2. “I can give my child a frozen juice bar after he swallows the medication.” 3. “I should mix the medication in the baby food and give it when I feed my child.” 4. “If my child does not like the taste of the medicine, I should encourage him to pinch his nose and drink the medication through a straw.” 468. A health care provider’s prescription reads “ampicillin sodium 125 mg IV every 6 hours.” The medication label reads “when reconstituted with 7.4 mL of bacteriostatic water, the final concentration is 1 g/7.4 mL.” The nurse prepares to draw up how many milliliters to administer 1 dose? 1. 1.1 mL 2. 0.54 mL 3. 7.425 mL 4. 0.925 mL 469. A pediatric client with ventricular septal defect repair is placed on a maintenance dosage ofdigoxin. The dosage is 8 mcg/kg/day, and the client’s weight is 7.2 kg. The health care provider (HCP) prescribes the digoxin to be given twice daily. The nurse prepares how many mcg of digoxin to administer to the client at each dose? 1. 12.6 mcg 2. 21.4 mcg 3. 28.8 mcg 4. 32.2 mcg 470. Sulfisoxazole, 1 g orally twice daily, is prescribed for an adolescent with a urinary tract infection. The medication label reads “500-mg tablets.” The nurse has determined that the dosage prescribed is safe. The nurse administers how many tablets per dose to the adolescent? BOX 45-7 Developmental Considerations for Administering Medications Infants Perform procedure quickly, allowing the infant to swallow; then offer comfort measures, such as holding, rocking, and cuddling. Allow self-comforting measures, such as the use of a pacifier. Toddlers Offer a brief, concrete explanation of the procedure and then perform it. Accept aggressive behavior, within reasonable limits, as a healthy response, and provide outlets for the toddler. Provide comfort measures immediately after the procedure, such as touch, holding, cuddling, and providing a favorite toy. Preschoolers Offer a brief, concrete explanation of the procedure and then perform it. Accept aggressive behavior, within reasonable limits, as a healthy response, and provide outlets for the child. Provide comfort measures after the procedure, such as touch, holding, or providing a favorite toy. School-Age Children Explain the procedure, allowing for some control over the body and situation. Explore feelings and concepts through therapeutic play, drawings of own body and self in the hospital, and the use of books and realistic hospital equipment. Set appropriate behavior limits, such as it is all right to cry or scream, but not to bite. Provide activities for releasing aggression and anger. Use the opportunity to teach about how medication helps the disorder. Adolescents Explain the procedure, allowing for some control over body and situation. Explore concepts of self, hospitalization, and illness, and correct any misconceptions. Encourage self-expression, individuality, and self-care needs. Encourage participation in the procedure. Data from McKenry L, Salerno E: Mosby’s pharmacology in nursing, St. Louis, 2003, Mosby. 540 UNIT VII Pediatric Nursing 1. ½ tablet 2. 1 tablet 3. 2 tablets 4. 3 tablets 471. Penicillin G procaine, 1,000,000 units IM (intramuscularly), is prescribed for a child with an infection. The medication label reads “1,200,000 units per 2 mL.” The nurse has determined that the dose prescribed is safe. The nurse administers how many milliliters per dose to the child? 1. 0.8 mL 2. 1.2 mL 3. 1.4 mL 4. 1.7 mL 472. The nurse prepares to administer an intramuscular injection to a 4-month-old infant. The nurse selects which best site to administer the injection? 1. Ventrogluteal 2. Lateral deltoid 3. Rectus femoris 4. Vastus lateralis 473. Atropine sulfate, 0.6 mg intramuscularly, is prescribed for a child preoperatively. The nurse has determined that the dose prescribed is safe and prepares to administer how m any milliliters to the child? Fill in th e blank (refer to figure). Answer: ________ mL 474. The nurse is conducting a session about the principles of first aid and is discussing the interventions for a snakebite to an extremity. The nurse should inform those attending the session that the first priority intervention in the event of this occurrence is which action? 1. Immobilize the affected extremity. 2. Remove jewelry and constricting clothing from the victim. 3. Place the extremity in a position so that it is below the level of the heart. 4. Move the victim to a safe area away from the snake and encourage the victim to rest. 475. Aclient calls the emergency department and tells the nurse that he came directly into contact with poison ivy shrubs. The client tells the nurse that he cannot see anything on the skin and asks the nurse what to do. The nurse should make which response? 1. “Come to the emergency department.” 2. “Apply calamine lotion immediately to the exposed skin areas.” 3. “Take a shower immediately, lathering and rinsing several times.” 4. “It is not necessary to do anything if you cannot see anything on your skin.” 476. A client is being admitted to the hospital for treatment of acute cellulitis of the lower left leg. During the admission assessment, the nurse expects to note which finding? 1. An inflammation of the epidermis only 2. A skin infection of the dermis and underlying hypodermis 3. An acute superficial infection of the dermis and lymphatics 4. An epidermal and lymphatic infection caused by Staphylococcus 477. The clinic nurse assesses the skin of a client with psoriasis after the client has used a new topical treatment for 2 months. The nurse identifies which characteristics as improvement in the manifestations of psoriasis? Select all that apply. 1. Presence of striae 2. Palpable radial pulses 3. Absence of any ecchymosis on the extremities 4. Thinner and decrease in number of reddish papules 5. Scarce amount of silvery-white scaly patches on the arms 478. The clinic nurse notes that the health care provider has documented a diagnosis of herpes zoster (shingles) in the client’s chart. Based on an understanding of the cause of this disorder, the nurse determines that this definitive diagnosis was made by which diagnostic test? 1. Positive patch test 2. Positive culture results 3. Abnormal biopsy results 4. Wood’s light examination indicative of infection 479. A client returns to the clinic for follow-up treatment following a skin biopsy of a suspicious lesion performed 1 week ago. The biopsy report indicates that the lesion is a melanoma. The nurse understands that melanoma has which characteristics? Select all that apply. 1. Lesion is painful to touch. 2. Lesion is highly metastatic. 3. Lesion is a nevus that has changes in color. 4. Skin under the lesion is reddened and warm to touch. 5. Lesion occurs in body area exposed to outdoor sunlight. 562 UNIT VIII Integumentary Disorders of the Adult Client 480. When assessing a lesion diagnosed as basal cell carcinoma, the nurse most likely expects to note which findings? Select all that apply. 1. An irregularly shaped lesion 2. A small papule with a dry, rough scale 3. A firm, nodular lesion topped with crust 4. A pearly papule with a central crater and a waxy border 5. Location in the bald spot atop the head that is exposed to outdoor sunlight 481. A client arriving at the emergency department has experienced frostbite to the right hand. Which finding would the nurse note on assessment of the client’s hand? 1. A pink, edematous hand 2. Fiery red skin with edema in the nail beds 3. Black fingertips surrounded by an erythematous rash 4. A white color to the skin, which is insensitive to touch 482. The evening nurse reviews the nursing documentation in a client’s chart and notes that the day nurse has documented that the client has a stage II pressure ulcer in the sacral area. Which finding would the nurse expect to note on assessment of the client’s sacral area? 1. Intact skin 2. Full-thickness skin loss 3. Exposed bone, tendon, or muscle 4. Partial-thickness skin loss of the dermis 483. An adult client was burned in an explosion. The burn initially affected the client’s entire face (anterior half of the head) and the upper half of the anterior torso, and there were circumferential burns to the lower half of both arms. The client’s clothes caught on fire, and the client ran, causing subsequent burn injuries to the posterior surface of the head and the upper half of the posterior torso. Using the rule of nines, what would be the extent of the burn injury? 1. 18% 2. 24% 3. 36% 4. 48% 484. The nurse is preparing to care for a burn client scheduled for an escharotomy procedure being performed for a third-degree circumferential arm burn. The nurse understands that which finding is the anticipated therapeutic outcome of the escharotomy? 1. Return of distal pulses 2. Brisk bleeding from the site 3. Decreasing edema formation 4. Formation of granulation tissue 485. A client is undergoing fluid replacement after being burned on 20% of her body 12 hours ago. The nursing assessment reveals a blood pressure of 90/50 mm Hg, a pulse rate of 110 beats/minute, and a urine output of 20 mL over the past hour. The nurse reports the findings to the health care provider (HCP) and anticipates which prescription? 1. Transfusing 1 unit of packed red blood cells 2. Administering a diuretic to increase urine output 3. Increasing the amount of intravenous (IV) lactated Ringer’s solution administered per hour 4. Changing the IV lactated Ringer’s solution to one that contains 5% dextrose in water 486. A client is brought to the emergency department with partial-thickness burns to his face, neck, arms, and chest after trying to put out a car fire. The nurse should implement which nursing actions for this client? Select all that apply. 1. Restrict fluids. 2. Assess for airway patency. 3. Administer oxygen as prescribed. 4. Place a cooling blanket on the client. 5. Elevate extremities if no fractures are present. 6. Prepare to give oral pain medication as prescribed. 487. The nurse is caring for a client who sustained superficial partial-thickness burns on the anterior lower legs and anterior thorax. Which finding does the nurse expect to note during the resuscitation/emergent phase of the burn injury? 1. Decreased heart rate 2. Increased urinary output 3. Increased blood pressure 4. Elevated hematocrit levels 488. The nurse manager is planning the clinical assignments for the day. Which staff members cannot be assigned to care for a client with herpes zoster? Select all that apply. 1. The nurse who never had roseola 2. The nurse who never had mumps 3. The nurse who never had chickenpox 4. The nurse who never had German measles 5. The nurse who never received the varicellazoster vaccine 489. A client arrives at the emergency department following a burn injury that occurred in the basement Adult—Integumentary CHAPTER 46 Integumentary System 563 Adult—Integumentary at home, and an inhalation injury is suspected. What would the nurse anticipate to be prescribed for the client? 1. 100% oxygen via an aerosol mask 2. Oxygen via nasal cannula at 6 L/minute 3. Oxygen via nasal cannula at 15 L/minute 4. 100% oxygen via a tight-fitting, nonrebreather face mask 490. The nurse is administering fluids intravenously as prescribed to a client who sustained superficial partial-thickness burn injuries of the back and legs. In evaluating the adequacy of fluid resuscitation, the nurse understands that which assessment would provide the most reliable indicator for determining the adequacy? 1. Vital signs 2. Urine output 3. Mental status 4. Peripheral pulses 491. The nurse manager is observing a new nursing graduate caring for a burn client in protective isolation. The nurse manager intervenes if the new nursing graduate planned to implement which unsafe component of protective isolation technique? 1. Using sterile sheets and linens 2. Performing strict hand-washing technique 3. Wearing gloves and a gown only when giving direct care to the client 4. Wearing protective garb, including a mask, gloves, cap, shoe covers, gowns, and plastic apron 492. The nurse is caring for a client following an autograft and grafting to a burn wound on the right knee. What would the nurse anticipate to be prescribed for the client? 1. Out-of-bed activities 2. Bathroom privileges 3. Immobilization of the affected leg 4. Placing the affected leg in a dependent position 493. The nurse is caring for a client who suffered an inhalation injury from a wood stove. The carbon monoxide blood report reveals a level of 12%. Based on this level, the nurse would anticipate noting which sign in the client? 1. Coma 2. Flushing 3. Dizziness 4. Tachycardia 494. Salicylic acid is prescribed for a client with a diagnosis of psoriasis. The nurse monitors the client, knowing that which finding indicates the presence of systemic toxicity from this medication? 1. Tinnitus 2. Diarrhea 3. Constipation 4. Decreased respirations 495. The health education nurse provides instructions to a group of clients regarding measures that will assist in preventing skin cancer. Which instructions should the nurse provide? Select all that apply. 1. Sunscreen should be applied every 8 hours. 2. Use sunscreen when participating in outdoor activities. 3. Wear a hat, opaque clothing, and sunglasses when in the sun. 4. Avoid sun exposure in the late afternoon and early evening hours. 5. Examine your body monthly for any lesions that may be suspicious. 496. Silver sulfadiazine is prescribed for a client with a burn injury. Which laboratory finding requires the need for follow-up by the nurse? 1. Glucose level of 99 mg/dL (5.65 mmol/L) 2. Magnesium level of 1.5 mEq/L (0.75 mmol/L) 3. Platelet level of 300,000 mm 3 (300 Â 109/L) 4. White blood cell count of 3000 mm 3 (3.0 Â109/L) 497. A burn client is receiving treatments of topical mafenide acetate to the site of injury. The nurse monitors the client, knowing that which finding indicates that a systemic effect has occurred? 1. Hyperventilation 2. Elevated blood pressure 3. Local rash at the burn site 4. Local pain at the burn site 498. Isotretinoin is prescribed for a client with severe acne. Before the administration of this medication, the nurse anticipates that which laboratory test will be prescribed? 1. Potassium level 2. Triglyceride level 3. Hemoglobin A1C 4. Total cholesterol level 499. A client with severe acne is seen in the clinic and the health care provider (HCP) prescribes isotretinoin. The nurse reviews the client’s medication record and would contact the HCP if the client is also taking which medication? 1. Digoxin 2. Phenytoin 3. Vitamin A 4. Furosemide 500. The nurse is applying a topical corticosteroid to a client with eczema. The nurse should apply the medication to which body area? Select all that apply. 1. Back 2. Axilla 3. Eyelids 4. Soles of the feet 5. Palms of the hands 501. The clinic nurse is performing an admission assessment on a client and notes that the client is taking azelaic acid. The nurse determines that which CHAPTER 47 Integumentary Medications 575 client complaint may be associated with use of this medication? 1. Itching 2. Euphoria 3. Drowsiness 4. Frequent urination 502. Silver sulfadiazine is prescribed for a client with a partial-thickness burn and the nurse provides teaching about the medication. Which statement made by the client indicates a need for further teach ing about the treatments? 1. “The medication is an antibacterial.” 2. “The medication will help heal the burn.” 3. “The medication is likely to cause stinging every time it is applied.” 4. “The medication should be applied directly to the wound.” 503. The camp nurse asks the children preparing to swim in the lake if they have applied sunscreen. The nurse reminds the children that chemical sunscreens are most effective when applied at which times? 1. Immediately before swimming 2. 5 minutes before exposure to the sun 3. Immediately before exposure to the sun 4. At least 30 minutes before exposure to the sun 504. The nurse is reviewing the laboratory results of a client diagnosed with multiple myeloma. Which would the nurse expect to note specifically in this disorder? 1. Increased calcium level 2. Increased white blood cells 3. Decreased blood urea nitrogen level 4. Decreased number of plasma cells in the bone marrow 505. The nurse is creating a plan of care for the client with multiple myeloma and includes which priority intervention in the plan? 1. Encouraging fluids 2. Providing frequent oral care 3. Coughing and deep breathing 4. Monitoring the red blood cell count 506. When caring for a client with an internal radiation implant, the nurse should observe which principles? Select all that apply. 1. Limiting the time with the client to 1 hour per shift. 2. Keeping pregnant women out of the client’s room. 3. Placing the client in a private room with a private bath. 4. Wearing a lead shield when providing direct client care. 5. Removing the dosimeter film badge when entering the client’s room. 6. Allowing individuals younger than 16 years old in the room as long as they are 6 feet away from the client. 507. While giving care to a client with an internal cervical radiation implant, the nurse finds the implant in the bed. The nurse should take which initial action? 1. Call the health care provider (HCP). 2. Reinsert the implant into the vagina. 3. Pick up the implant with gloved hands and flush it down the toilet. 4. Pick up the implant with long-handled forceps and place it in a lead container. 508. The nurse should plan to implement which intervention in the care of a client experiencing neutropenia as a result of chemotherapy? 1. Restrict all visitors. 2. Restrict fluid intake. 3. Teach the client and family about the need for hand hygiene. 4. Insert an indwelling urinary catheter to prevent skin breakdown. 509. The home health care nurse is caring for a client with cancer who is complaining of acute pain. The most appropriate determination of the client’s pain should include which assessment? 1. The client’s pain rating 2. Nonverbal cues from the client 3. The nurse’s impression of the client’s pain 4. Pain relief after appropriate nursing intervention 510. The nurse is caring for a client who is postoperative following a pelvic exenteration and the health care provider changes the client’s diet from NPO (nothing by mouth) status to clear liquids. The nurse should check which priority item before administering the diet? 1. Bowel sounds 2. Ability to ambulate 3. Incision appearance 4. Urine specific gravity 511. Aclient is admitted to the hospital with a suspected diagnosis of Hodgkin’s disease. Which assessment finding would the nurse expect to note specifically in the client? 1. Fatigue 2. Weakness 3. Weight gain 4. Enlarged lymph nodes 512. During the admission assessment of a client with advanced ovarian cancer, the nurse recognizes which manifestation as typical of the disease? 606 UNIT IX Hematological and Oncological Disorders of the Adult Client Adult—Oncological 1. Diarrhea 2. Hypermenorrhea 3. Abnormal bleeding 4. Abdominal distention 513. The nurse is caring for a client with lung cancer and bone metastasis. What signs and symptoms would the nurse recognize as indications of a possible oncological emergency? Select all that apply. 1. Facial edema in the morning 2. Weight loss of 20 lb (9 kg) in 1 month 3. Serum calcium level of12 mg/dL(3.0 mmol/L) 4. Serum sodium level of 136 mg/dL (136 mmol/L) 5. Serum potassium level of 3.4 mg/dL (3.4 mmol/L) 6. Numbness and tingling of the lower extremities 514. A client who has been receiving radiation therapy for bladder cancer tells the nurse that it feels as if she is voiding through the vagina. The nurse interprets that the client may be experiencing which condition? 1. Rupture of the bladder 2. The development of a vesicovaginal fistula 3. Extreme stress caused by the diagnosis of cancer 4. Altered perineal sensation as a side effect of radiation therapy 515. The nurse is instructing a client to perform a testicular self-examination (TSE). The nurse should provide the client with which information about the procedure? 1. To examine the testicles while lying down 2. That the best time for the examination is after a shower 3. To gently feel the testicle with 1 finger to feel for a growth 4. That TSEs should be done at least every 6 months 516. The nurse is conducting a history and monitoring laboratory values on a client with multiple myeloma. What assessment findings should the nurse expect to note? Select all that apply. 1. Pathological fracture 2. Urinalysis positive for nitrites 3. Hemoglobin level of 15.5 g/dL (155 mmol/L) 4. Calcium level of 8.6 mg/dL (2.15 mmol/L) 5. Serum creatinine level of 2.0 mg/dL (176.6 mcmol/L) 517. A gastrectomy is performed on a client with gastric cancer. In the immediate postoperative period, the nurse notes bloody drainage from the nasogastric tube. The nurse should take which most appropriate action? 1. Measure abdominal girth. 2. Irrigate the nasogastric tube. 3. Continue to monitor the drainage. 4. Notify the health care provider (HCP). 518. The nurse is teaching a client about the risk factors associated with colorectal cancer. The nurse determines that further teaching is necessary related to colorectal cancer if the client identifies which item as an associated risk factor? 1. Age younger than 50 years 2. History of colorectal polyps 3. Family history of colorectal cancer 4. Chronic inflammatory bowel disease 519. The nurse is assessing the perineal wound in a client who has returned from the operating room following an abdominal perineal resection and notes serosanguineous drainage from the wound. Which nursing intervention is most appropriate? 1. Clamp the surgical drain. 2. Change the dressing as prescribed. 3. Notify the health care provider (HCP). 4. Remove and replace the perineal packing. 520. The nurse is assessing the colostomy of a client who has had an abdominal perineal resection for a bowel tumor. Which assessment finding indicates that the colostomy is beginning to function? 1. The passage of flatus 2. Absent bowel sounds 3. The client’s ability to tolerate food 4. Bloody drainage from the colostomy 521. The nurse is reviewing the history of a client with bladder cancer. The nurse expects to note documentation of which most common sign or symptom of this type of cancer? 1. Dysuria 2. Hematuria 3. Urgency on urination 4. Frequency of urination 522. The nurse is assessing a client who has a new ureterostomy. Which statement by the client indicates the need for more education about urinary stoma care? 1. “I change my pouch every week.” 2. “I change the appliance in the morning.” 3. “I empty the urinary collection bag when it is two-thirds full.” 4. “When I’m in the shower I direct the flow of water away from my stoma.” 523. A client with carcinoma of the lung develops syndrome of inappropriate antidiuretic hormone (SIADH) as a complication of the cancer. The nurse CHAPTER 48 Hematological and Oncological Disorders 607 anticipates that the health care provider will request which prescriptions? Select all that apply. 1. Radiation 2. Chemotherapy 3. Increased fluid intake 4. Decreased oral sodium intake 5. Serum sodium level determination 6. Medication that is antagonistic to antidiuretic hormone 524. The nurse is monitoring a client for signs and symptoms related to superior vena cava syndrome. Which is an early sign of this oncological emergency? 1. Cyanosis 2. Arm edema 3. Periorbital edema 4. Mental status changes 525. The nurse manager is teaching the nursing staff about signs and symptoms related to hypercalcemia in a client with metastatic prostate cancer, and tells the staff that which is a late sign or symptom of this oncological emergency? 1. Headache 2. Dysphagia 3. Constipation 4. Electrocardiographic changes 526. As part of chemotherapy education, the nurse teaches a female client about the risk for bleeding and self-care during the period of greatest bone marrow suppression (the nadir). The nurse understands that further teachin g is needed if the client makes which statement? 1. “I should avoid blowing my nose.” 2. “I may need a platelet transfusion if my platelet count is too low.” 3. “I’m going to take aspirin for my headache as soon as I get home.” 4. “I will count the number of pads and tampons I use when menstruating.” 527. The community health nurse is instructing a group of young female clients about breast selfexamination. The nurse should instruct the clients to perform the examination at which time? 1. At the onset of menstruation 2. Every month during ovulation 3. Weekly at the same time of day 4. 1 week after menstruation begins 528. A client is diagnosed as having a bowel tumor. The nurse should monitor the client for which complications of this type of tumor? Select all that apply. 1. Flatulence 2. Peritonitis 3. Hemorrhage 4. Fistula formation 5. Bowel perforation 6. Lactose intolerance 529. The nurse is caring for a client following a mastectomy. Which nursing intervention would assist in preventing lymphedema of the affected arm? 1. Placing cool compresses on the affected arm 2. Elevating the affected arm on a pillow above heart level 3. Avoiding arm exercises in the immediate postoperative period 4. Maintaining an intravenous site below the antecubital area on the affected side 530. Chemotherapy dosage is frequently based on total body surface area (BSA), so it is important for the nurse to perform which assessment before administering chemotherapy? 1. Measure the client’s abdominal girth. 2. Calculate the client’s body mass index. 3. Measure the client’s current weight and height. 4. Ask the client about his or her weight and height. 531. A client with squamous cell carcinoma of the larynx is receiving bleomycin intravenously. The nurse caring for the client anticipates that which diagnostic study will be prescribed? 1. Echocardiography 2. Electrocardiography 3. Cervical radiography 4. Pulmonary function studies 532. A client with acute myelocytic leukemia is being treated with busulfan. Which laboratory value would the nurse specifically monitor during treatment with this medication? 1. Clotting time 2. Uric acid level 3. Potassium level 4. Blood glucose level 533. A client with small cell lung cancer is being treated with etoposide. The nurse monitors the client during administration, knowing that which adverse effect is specifically associated with this medication? 1. Alopecia 2. Chest pain 3. Pulmonary fibrosis 4. Orthostatic hypotension 534. A clinic nurse prepares a teaching plan for a client receiving an antineoplastic medication. When implementing the plan, the nurse should make which statement to the client? 1. “You can take aspirin as needed for headache.” 2. “You can drink beverages containing alcohol in moderate amounts each evening.” 3. “You need to consult with the health care provider (HCP) before receiving immunizations.” 4. “It is fine to receive a flu vaccine at the local health fair without HCP approval because the flu is so contagious.” 535. A client with ovarian cancer is being treated with vincristine. The nurse monitors the client, knowing that which manifestation indicates an adverse effect specific to this medication? 1. Diarrhea 2. Hair loss 3. Chest pain 4. Peripheral neuropathy 536. The nurse is reviewing the history and physical examination of a client who will be receiving asparaginase, an antineoplastic agent. The nurse contacts the health care provider before administering the medication if which disorder is documented in the client’s history? 1. Pancreatitis 2. Diabetes mellitus 3. Myocardial infarction 4. Chronic obstructive pulmonary disease 537. Tamoxifen citrate is prescribed for a client with metastatic breast carcinoma. The client asks the nurse if her family member with bladder cancer can also take this medication. The nurse most appropriately responds by making which statement? 1. “This medication can be used only to treat breast cancer.” 2. “Yes, your family member can take this medication for bladder cancer as well.” 3. “This medication can be taken to prevent and treat clients with breast cancer.” 4. “This medication can be taken by anyone with cancer as long as their health care provider approves it.” 538. A client with metastatic breast cancer is receiving tamoxifen. The nurse specifically monitors which laboratory value while the client is taking this medication? 1. Glucose level 2. Calcium level 3. Potassium level 4. Prothrombin time 539. Megestrol acetate, an antineoplastic medication, is prescribed for a client with metastatic endometrial carcinoma. The nurse reviews the client’s history and should contact the health care provider if which diagnosis is documented in the client’s history? 1. Gout 2. Asthma 3. Myocardial infarction 4. Venous thromboembolism 540. The nurse is monitoring the intravenous (IV) infusion of an antineoplastic medication. During the infusion, the client complains of pain at the insertion site. On inspection of the site, the nurse notes redness and swelling and that the infusion of the medication has slowed in rate. The nurse suspects extravasation and should take which actions? Select all that apply. Adult—Oncological 620 UNIT IX Hematological and Oncological Disorders of the Adult Client 1. Stop the infusion. 2. Notify the health care provider (HCP). 3. Prepare to apply ice or heat to the site. 4. Restart the IVat a distal part of the same vein. 5. Prepare to administer a prescribed antidote into the site. 6. Increase the flow rate of the solution to flush the skin and subcutaneous tissue. 541. The nurse is analyzing the laboratory results of a client with leukemia who has received a regimen of chemotherapy. Which laboratory value would the nurse specifically note as a result of the massive cell destruction that occurred from the chemotherapy? 1. Anemia 2. Decreased platelets 3. Increased uric acid level 4. Decreased leukocyte count 542. The nurse is providing medication instructions to a client with breast cancer who is receiving cyclophosphamide. The nurse should tell the client to take which action? 1. Take the medication with food. 2. Increase fluid intake to 2000 to 3000 mL daily. 3. Decrease sodium intake while taking the medication. 4. Increase potassium intake while taking the medication. 543. A client with non–Hodgkin’s lymphoma is receiving daunorubicin. Which finding would indicate to the nurse that the client is experiencing an adverse effect related to the medication? 1. Fever 2. Sores in the mouth and throat 3. Complaints of nausea and vomiting 4. Crackles on auscultation of the lungs 544. The nurse is monitoring the laboratory results of a client receiving an antineoplastic medication by the intravenous route. The nurse plans to initiate bleeding precautions if which laboratory result is noted? 1. A clotting time of 10 minutes 2. An ammonia level of 10 mcg/dL (6 mcmol/L). 3. A platelet count of 50,000 mm 3 (50 Â 109/L) 4. A white blood cell count of 5000 mm 3 (5.0 Â 109/L) 545. A client is brought to the emergency department in an unresponsive state, and a diagnosis of hyperosmolar hyperglycemic syndrome is made. The nurse would immediately prepare to initiate which anticipated health care provider’s prescription? 1. Endotracheal intubation 2. 100 units of NPH insulin 3. Intravenous infusion of normal saline 4. Intravenous infusion of sodium bicarbonate 546. An external insulin pump is prescribed for a client with diabetes mellitus. When the client asks the nurse about the functioning of the pump, the nurse bases the response on which information about the pump? 1. It is timed to release programmed doses of either short-duration or NPH insulin into the bloodstream at specific intervals. 2. It continuously infuses small amounts of NPH insulin into the bloodstream while regularly monitoring blood glucose levels. 3. It is surgically attached to the pancreas and infuses regular insulin into the pancreas. This releases insulin into the bloodstream. 4. It administers a small continuous dose of shortduration insulin subcutaneously. The client can self-administer an additional bolus dose from the pump before each meal. BOX 50-17 Preventive Foot Care Instructions Provide meticulous skin care and proper foot care. Inspect feet daily and monitor feet for redness, swelling, or break in skin integrity. Notify the health care provider if redness or a break in the skin occurs. Avoid thermal injuries from hot water, heating pads, and baths. Wash feet with warm (not hot) water and dry thoroughly (avoid foot soaks). Avoid treating corns, blisters, or ingrown toenails. Do not cross legs or wear tight garments that may constrict blood flow. Apply moisturizing lotion to the feet but not between the toes. Prevent moisture from accumulating between the toes. Wear loose socks and well-fitting (not tight) shoes; do not go barefoot. Wear clean cotton socks to keep the feet warm and change the socks daily. Avoid wearing the same pair of shoes 2 days in a row. Avoid wearing open-toed shoes or shoes with a strap that goes between the toes. Check shoes for cracks or tears in the lining and for foreign objects before putting them on. Break in new shoes gradually. Cut toenails straight across and smooth nails with an emery board. Avoid smoking. 644 UNIT X Endocrine Disorders of the Adult Client Adult—Endocrine 547. A client with a diagnosis of diabetic ketoacidosis (DKA) is being treated in the emergency department. Which findings support this diagnosis? Select all that apply. 1. Increase in pH 2. Comatose state 3. Deep, rapid breathing 4. Decreased urine output 5. Elevated blood glucose level 548. The nurse teaches a client with diabetes mellitus about differentiating between hypoglycemia and ketoacidosis. The client demonstrates an understanding of the teaching by stating that a form of glucose should be taken if which symptom or symptoms develop? Select all that apply. 1. Polyuria 2. Shakiness 3. Palpitations 4. Blurred vision 5. Lightheadedness 6. Fruity breath odor 549. A client with diabetes mellitus demonstrates acute anxiety when admitted to the hospital for the treatment of hyperglycemia. What is the appropriate intervention to decrease the client’s anxiety? 1. Administer a sedative. 2. Convey empathy, trust, and respect toward the client. 3. Ignore the signs and symptoms of anxiety, anticipating that they will soon disappear. 4. Make sure that the client is familiar with the correct medical terms to promote understanding of what is happening. 550. The nurse provides instructions to a client newly diagnosed with type 1 diabetes mellitus. The nurse recognizes accurate understanding of measures to prevent diabetic ketoacidosis when the client makes which statement? 1. “I will stop taking my insulin if I’m too sick to eat.” 2. “I will decrease my insulin dose during times of illness.” 3. “I will adjust my insulin dose according to the level of glucose in my urine.” 4. “I will notify my health care provider (HCP) if my blood glucose level is higher than 250 mg/dL (14.2 mmol/L).” 551. A client is admitted to a hospital with a diagnosis of diabetic ketoacidosis (DKA). The initial blood glucose level is 950 mg/dL (54.2 mmol/L). A continuous intravenous (IV) infusion of short-acting insulin is initiated, along with IV rehydration with normal saline. The serum glucose level is now decreased to 240 mg/dL (13.7 mmol/L). The nurse would next prepare to administer which medication? 1. An ampule of 50% dextrose 2. NPH insulin subcutaneously 3. IV fluids containing dextrose 4. Phenytoin for the prevention of seizures 552. The nurse is monitoring a client newly diagnosed with diabetes mellitus for signs of complications. Which sign or symptom, if exhibited in the client, indicates that the client is at risk for chronic complications of diabetes if the blood glucose is not adequately managed? 1. Polyuria 2. Diaphoresis 3. Pedal edema 4. Decreased respiratory rate 553. The nurse is preparing a plan of care for a client with diabetes mellitus who has hyperglycemia. The nurse places priority on which client problem? 1. Lack of knowledge 2. Inadequate fluid volume 3. Compromised family coping 4. Inadequate consumption of nutrients 554. The home health nurse visits a client with a diagnosis of type 1 diabetes mellitus. The client relates a history of vomiting and diarrhea and tells the nurse that no food has been consumed for the last 24 hours. Which additional statement by the client indicates a need for further teaching? 1. “I need to stop my insulin.” 2. “I need to increase my fluid intake.” 3. “I need to monitor my blood glucose every 3 to 4 hours.” 4. “I need to call the health care provider (HCP) because of these symptoms.” 555. The nurse is caring for a client after hypophysectomy and notes clear nasal drainage from the client’s nostril. The nurse should take which initial action? 1. Lower the head of the bed. 2. Test the drainage for glucose. 3. Obtain a culture of the drainage. 4. Continue to observe the drainage. 556. The nurse is admitting a client who is diagnosed with syndrome of inappropriate antidiuretic hormone secretion (SIADH) and has serum sodium of 118 mEq/L (118 mmol/L). Which health care provider prescriptions should the nurse anticipate receiving? Select all that apply. 1. Initiate an infusion of 3% NaCl. 2. Administer intravenous furosemide. CHAPTER 50 Endocrine System 645 3. Restrict fluids to 800 mL over 24 hours. 4. Elevate the head of the bed to high Fowler’s. 5. Administer a vasopressin antagonist as prescribed. 557. A client is admitted to an emergency department, and a diagnosis of myxedema coma is made. Which action should the nurse prepare to carry out initially? 1. Warm the client. 2. Maintain a patent airway. 3. Administer thyroid hormone. 4. Administer fluid replacement. 558. The nurse is caring for a client admitted to the emergency department with diabetic ketoacidosis (DKA). In the acute phase, the nurse plans for which priority intervention? 1. Correct the acidosis. 2. Administer 5% dextrose intravenously. 3. Apply a monitor for an electrocardiogram. 4. Administer short-duration insulin intravenously. 559. Aclient with type 1 diabetes mellitus calls the nurse to report recurrent episodes of hypoglycemia with exercising. Which statement by the client indicates an adequate understanding of the peak action of NPH insulin and exercise? 1. “I should not exercise since I am taking insulin.” 2. “The best time for me to exercise is after breakfast.” 3. “The best time for me to exercise is mid- to late afternoon.” 4. “NPH is a basal insulin, so I should exercise in the evening.” 560. The nurse is completing an assessment on a client who is being admitted for a diagnostic workup for primary hyperparathyroidism. Which client complaint would be characteristic of this disorder? Select all that apply. 1. Polyuria 2. Headache 3. Bone pain 4. Nervousness 5. Weight gain 561. The nurse is teaching a client with hyperparathyroidism how to manage the condition at home. Which response by the client indicates the need for additional teaching? 1. “I should limit my fluids to 1 liter per day.” 2. “I should use my treadmill or go for walks daily.” 3. “I should follow a moderate-calcium, highfiber diet.” 4. “My alendronate helps to keep calcium from coming out of my bones.” 562. A client with a diagnosis of addisonian crisis is being admitted to the intensive care unit. Which findings will the interprofessional health care team focus on? Select all that apply. 1. Hypotension 2. Leukocytosis 3. Hyperkalemia 4. Hypercalcemia 5. Hypernatremia 563. The nurse is monitoring a client who was diagnosed with type 1 diabetes mellitus and is being treated with NPH and regular insulin. Which manifestations would alert the nurse to the presence of a possible hypoglycemic reaction? Select all that apply. 1. Tremors 2. Anorexia 3. Irritability 4. Nervousness 5. Hot, dry skin 6. Muscle cramps 564. The nurse is performing an assessment on a client with pheochromocytoma. Which assessment data would indicate a potential complication associated with this disorder? 1. A urinary output of 50 mL/hour 2. A coagulation time of 5 minutes 3. Aheart rate that is 90 beats/minute and irregular 4. A blood urea nitrogen level of 20 mg/dL (7.1 mmol/L) 565. The nurse is monitoring a client diagnosed with acromegaly who was treated with transsphenoidal hypophysectomy and is recovering in the intensive care unit. Which findings should alert the nurse to the presence of a possible postoperative complication? Select all that apply. 1. Anxiety 2. Leukocytosis 3. Chvostek’s sign 4. Urinary output of 800 mL/hour 5. Clear drainage on nasal dripper pad 566. The nurse performs a physical assessment on a client with type 2 diabetes mellitus. Findings include a fasting blood glucose level of 120 mg/dL (6.8 mmol/L), temperature of 101 °F (38.3 °C), pulse of 102 beats/minute, respirations of 22 breaths/minute, and blood pressure of 142/72 mm Hg. Which finding would be the priority concern to the nurse? 1. Pulse 2. Respiration 3. Temperature 4. Blood pressure Adult—Endocrine 646 UNIT X Endocrine Disorders of the Adult Client Adult—Endocrine 567. The nurse is preparing a client with a new diagnosis of hypothyroidism for discharge. The nurse determines that the client understands discharge instructions if the client states that which signs and symptoms are associated with this diagnosis? Select all that apply. 1. Tremors 2. Weight loss 3. Feeling cold 4. Loss of body hair 5. Persistent lethargy 6. Puffiness of the face 568. A client has just been admitted to the nursing unit following thyroidectomy. Which assessment is the priority for this client? 1. Hypoglycemia 2. Level of hoarseness 3. Respiratory distress 4. Edema at the surgical site 569. Aclient has been diagnosed with hyperthyroidism. The nurse monitors for which signs and symptoms indicating a complication of this disorder? Select all that apply. 1. Fever 2. Nausea 3. Lethargy 4. Tremors 5. Confusion 6. Bradycardia 570. The nurse is teaching a client how to mix regular insulin and NPH insulin in the same syringe. Which action, if performed by the client, indicates the need for further teachin g? 1. Withdraws the NPH insulin first 2. Withdraws the regular insulin first 3. Injects air into NPH insulin vial first 4. Injects an amount of air equal to the desired dose of insulin into each vial 571. The home care nurse visits a client recently diagnosed with diabetes mellitus who is taking Humulin NPH insulin daily. The client asks the nurse how to store the unopened vials of insulin. The nurse should tell the client to take which action? 1. Freeze the insulin. 2. Refrigerate the insulin. 3. Store the insulin in a dark, dry place. 4. Keep the insulin at room temperature. 572. Glimepiride is prescribed for a client with diabetes mellitus. The nurse instructs the client that which food items are most acceptable to consume while taking this medication? Select all that apply. 1. Alcohol 2. Red meats 3. Whole-grain cereals 4. Low-calorie desserts 5. Carbonated beverages 573. The nurse is providing discharge teaching for a client newly diagnosed with type 2 diabetes mellitus who has been prescribed metformin. Which client statement indicates the need for further teaching? 1. “It is okay if I skip meals now and then.” 2. “I need to constantly watch for signs of low blood sugar.” CHAPTER 51 Endocrine Medications 663 3. “I need to let my health care provider know if I get unusually tired.” 4. “I will be sure to not drink alcohol excessively while on this medication.” 574. The health care provider (HCP) prescribes exenatide for a client with type 1 diabetes mellitus who takes insulin. The nurse should plan to take which most appropriate intervention? 1. Withhold the medication and call the HCP, questioning the prescription for the client. 2. Administer the medication within 60 minutes before the morning and evening meal. 3. Monitor the client for gastrointestinal side effects after administering the medication. 4. Withdraw the insulin from the prefilled pen into an insulin syringe to prepare for administration. 575. Aclient is taking Humulin NPH insulin and regular insulin every morning. The nurse should provide which instructions to the client? Select all that apply. 1. Hypoglycemia may be experienced before dinnertime. 2. The insulin dose should be decreased if illness occurs. 3. The insulin should be administered at room temperature. 4. The insulin vial needs to be shaken vigorously to break up the precipitates. 5. The NPH insulin should be drawn into the syringe first, then the regular insulin. 576. The home health care nurse is visiting a client who was recently diagnosed with type 2 diabetes mellitus. The client is prescribed repaglinide and metformin. The nurse should provide which instructions to the client? Select all that apply. 1. Diarrhea may occur secondary to the metformin. 2. The repaglinide is not taken if a meal is skipped. 3. The repaglinide is taken 30 minutes before eating. 4. A simple sugar food item is carried and used to treat mild hypoglycemia episodes. 5. Muscle pain is an expected effect of metformin and may be treated with acetaminophen. 6. Metformin increases hepatic glucose production to prevent hypoglycemia associated with repaglinide. 577. The nurse is teaching the client about his prescribed prednisone. Which statement, if made by the client, indicates that further teachin g is necessary? 1. “I can take aspirin or my antihistamine if I need it.” 2. “I need to take the medication every day at the same time.” 3. “I need to avoid coffee, tea, cola, and chocolate in my diet.” 4. “If I gain more than 5 pounds (2.25 kg) a week, I will call my health care provider (HCP).” 578. A client with hyperthyroidism has been given methimazole. Which nursing considerations are associated with this medication? Select all that apply. 1. Administer methimazole with food. 2. Place the client on a low-calorie, lowprotein diet. 3. Assess the client for unexplained bruising or bleeding. 4. Instruct the client to report side and adverse effects such as sore throat, fever, or headaches. 5. Use special radioactive precautions when handling the client’s urine for the first 24 hours following initial administration. 579. The nurse is monitoring a client receiving levothyroxine sodium for hypothyroidism. Which findings indicate the presence of a side effect associated with this medication? Select all that apply. 1. Insomnia 2. Weight loss 3. Bradycardia 4. Constipation 5. Mild heat intolerance 580. The nurse provides instructions to a client who is taking levothyroxine. The nurse should tell the client to take the medication in which way? 1. With food 2. At lunchtime 3. On an empty stomach 4. At bedtime with a snack 581. The nurse should tell the client, who is taking levothyroxine, to notify the health care provider (HCP) if which problem occurs? 1. Fatigue 2. Tremors 3. Cold intolerance 4. Excessively dry skin 582. The nurse is providing instructions to the client newly diagnosed with diabetes mellitus who has been prescribed pramlintide. Which instruction should the nurse include in the discharge teaching? 1. “Inject the pramlintide at the same time you take your other medications.” Adult—Endocrine 664 UNIT X Endocrine Disorders of the Adult Client Adult—Endocrine 2. “Take your prescribed pills 1 hour before or 2 hours after the injection.” 3. “Be sure to take the pramlintide with food so you don’t upset your stomach.” 4. “Make sure you take your pramlintide immediately after you eat so you don’t experience a low blood sugar.” 583. The nurse teaches the client, who is newly diagnosed with diabetes insipidus, about the prescribed intranasal desmopressin. Which statements by the client indicate understanding? Select all that apply. 1. “This medication will turn my urine orange.” 2. “I should decrease my oral fluids when I start this medication.” 3. “The amount of urine I make should increase if this medicine is working.” 4. “I need to follow a low-fat diet to avoid pancreatitis when taking this medicine.” 5. “I should report headache and drowsiness to my health care provider since these symptoms could be related to my desmopressin.” 584. Adaily dose of prednisone is prescribed for a client. The nurse provides instructions to the client regarding administration of the medication and should instruct the client that which time is best to take this medication? 1. At noon 2. At bedtime 3. Early morning 4. Any time, at the same time, each day 585. The client with hyperparathyroidism is taking alendronate. Which statements by the client indicate understanding of the proper way to take this medication? Select all that apply. 1. “I should take this medication with food.” 2. “I should take this medication at bedtime.” 3. “I should sit up for at least 30 minutes after taking this medication.” 4. “I should take this medication first thing in the morning on an empty stomach.” 5. “I can pick a time to take this medication that best fits my lifestyle as long as I take it at the same time each day.” 586. A client with diabetes mellitus visits a health care clinic. The client’s diabetes mellitus previously had been well controlled with glyburide daily, but recently the fasting blood glucose level has been 180 to 200 mg/dL (10.2 to 11.4 mmol/L). Which medication, if added to the client’s regimen, may have contributed to the hyperglycemia? 1. Prednisone 2. Atenolol 3. Phenelzine 4. Allopurinol 587. The nurse is monitoring a client admitted to the hospital with a diagnosis of appendicitis who is scheduled for surgery in 2 hours. The client begins to complain of increased abdominal pain and begins to vomit. On assessment, the nurse notes that the abdomen is distended and bowel sounds are diminished. Which is the most appropriate nursing intervention? 1. Notify the health care provider (HCP). 2. Administer the prescribed pain medication. 3. Call and ask the operating room team to perform surgery as soon as possible. 4. Reposition the client and apply a heating pad on the warm setting to the client’s abdomen. 588 A client admitted to the hospital with a suspected diagnosis of acute pancreatitis is being assessed by the nurse. Which assessment findings would be consistent with acute pancreatitis? Select all that apply. 1. Diarrhea 2. Black, tarry stools 3. Hyperactive bowel sounds 4. Gray-blue color at the flank 5. Abdominal guarding and tenderness 6. Left upper quadrant pain with radiation to the back Adult—Gastrointestinal 690 UNIT XI Gastrointestinal Disorders of the Adult Client 589 The nurse is assessing a client who is experiencing an acute episode of cholecystitis. Which of these clinical manifestations support this diagnosis? Select all that apply. 1. Fever 2. Positive Cullen’s sign 3. Complaints of indigestion 4. Palpable mass in the left upper quadrant 5. Pain in the upper right quadrant after a fatty meal 6. Vague lower right quadrant abdominal discomfort 590. Aclient is diagnosed with viral hepatitis, complaining of “no appetite” and “losing my taste for food.” What instruction should the nurse give the client to provide adequate nutrition? 1. Select foods high in fat. 2. Increase intake of fluids, including juices. 3. Eat a good supper when anorexia is not as severe. 4. Eat less often, preferably only 3 large meals daily. 591. A client has developed hepatitis A after eating contaminated oysters. The nurse assesses the client for which expected assessment finding? 1. Malaise 2. Dark stools 3. Weight gain 4. Left upper quadrant discomfort 592 A client has just had a hemorrhoidectomy. Which nursing interventions are appropriate for this client? Select all that apply. 1. Administer stool softeners as prescribed. 2. Instruct the client to limit fluid intake to avoid urinary retention. 3. Encourage a high-fiber diet to promote bowel movements without straining. 4. Apply cold packs to the anal-rectal area over the dressing until the packing is removed. 5. Help the client to a Fowler’s position to place pressure on the rectal area and decrease bleeding. 593 The nurse is planning to teach a client with gastroesophageal reflux disease (GERD) about substances to avoid. Which items should the nurse include on this list? Select all that apply. 1. Coffee 2. Chocolate 3. Peppermint 4. Nonfat milk 5. Fried chicken 6. Scrambled eggs 594. A client has undergone esophagogastroduodenoscopy. The nurse should place highest priority on which item as part of the client’s care plan? 1. Monitoring the temperature 2. Monitoring complaints of heartburn 3. Giving warm gargles for a sore throat 4. Assessing for the return of the gag reflex 595. The nurse has taught the client about an upcoming endoscopic retrograde cholangiopancreatography (ERCP) procedure. The nurse determines that the client needs further information if the client makes which statement? 1. “I know I must sign the consent form.” 2. “I hope the throat spray keeps me from gagging.” 3. “I’m glad I don’t have to lie still for this procedure.” 4. “I’m glad some intravenous medication will be given to relax me.” 596. The health care provider has determined that a client has contracted hepatitis A based on flulike symptoms and jaundice. Which statement made by the client supports this medical diagnosis? 1. “I have had unprotected sex with multiple partners.” 2. “I ate shellfish about 2 weeks ago at a local restaurant.” 3. “I was an intravenous drug abuser in the past and shared needles.” 4. “I had a blood transfusion 30 years ago after major abdominal surgery.” 597 The nurse is providing dietary teaching for a client with a diagnosis of chronic gastritis. The nurse instructs the client to include which foods rich in vitamin B12 in the diet? Select all that apply. 1. Nuts 2. Corn 3. Liver 4. Apples 5. Lentils 6. Bananas 598. The nurse is assessing a client 24 hours following a cholecystectomy. The nurse notes that the T-tube has drained 750 mL of green-brown drainage since the surgery. Which nursing intervention is most appropriate? 1. Clamp the T-tube. 2. Irrigate the T-tube. 3. Document the findings. 4. Notify the health care provider. 599. The nurse is monitoring a client with a diagnosis of peptic ulcer. Which assessment finding would most likely indicate perforation of the ulcer? 1. Bradycardia 2. Numbness in the legs 3. Nausea and vomiting 4. A rigid, boardlike abdomen Adult—Gastrointestinal CHAPTER 52 Gastrointestinal System 691 600. The nurse is caring for a client following a gastrojejunostomy (Billroth II procedure). Which postoperative prescription should the nurse question and verify? 1. Leg exercises 2. Early ambulation 3. Irrigating the nasogastric tube 4. Coughing and deep-breathing exercises 601. The nurse is providing discharge instructions to a client following gastrectomy and should instruct the client to take which measure to assist in preventing dumping syndrome? 1. Ambulate following a meal. 2. Eat high-carbohydrate foods. 3. Limit the fluids taken with meals. 4. Sit in a high Fowler’s position during meals. 602 The nurse is reviewing the prescription for a client admitted to the hospital with a diagnosis of acute pancreatitis. Which interventions would the nurse expect to be prescribed for the client? Select all that apply. 1. Maintain NPO (nothing by mouth) status. 2. Encourage coughing and deep breathing. 3. Give small, frequent high-calorie feedings. 4. Maintain the client in a supine and flat position. 5. Give hydromorphone intravenously as prescribed for pain. 6. Maintain intravenous fluids at 10 mL/hour to keep the vein open. 603. The nurse is providing discharge teaching for a client with newly diagnosed Crohn’s disease about dietary measures to implement during exacerbation episodes. Which statement made by the client indicates a n eed for furth er instruction ? 1. “I should increase the fiber in my diet.” 2. “I will need to avoid caffeinated beverages.” 3. “I’m going to learn some stress reduction techniques.” 4. “I can have exacerbations and remissions with Crohn’s disease.” 604. The nurse is reviewing the record of a client with a diagnosis of cirrhosis and notes that there is documentation of the presence of asterixis. How should the nurse assess for its presence? 1. Dorsiflex the client’s foot. 2. Measure the abdominal girth. 3. Ask the client to extend the arms. 4. Instruct the client to lean forward. 605. The nurse is reviewing the laboratory results for a client with cirrhosis and notes that the ammonia level is 85 mcg/dL (51 mcmol/L). Which dietary selection does the nurse suggest to the client? 1. Roast pork 2. Cheese omelet 3. Pasta with sauce 4. Tuna fish sandwich 606. The nurse is doing an admission assessment on a client with a history of duodenal ulcer. To determine whether the problem is currently active, the nurse should assess the client for which sign(s)/ symptom(s) of duodenal ulcer? 1. Weight loss 2. Nausea and vomiting 3. Pain relieved by food intake 4. Pain radiating down the right arm 607. A client with hiatal hernia chronically experiences heartburn following meals. The nurse should plan to teach the client to avoid which action because it is contraindicated with a hiatal hernia? 1. Lying recumbent following meals 2. Consuming small, frequent, bland meals 3. Taking H2-receptor antagonist medication 4. Raising the head of the bed on 6-inch (15 cm) blocks 608. The nurse is providing care for a client with a recent transverse colostomy. Which observation requires immediate notification of the health care provider? 1. Stoma is beefy red and shiny 2. Purple discoloration of the stoma 3. Skin excoriation around the stoma 4. Semi-formed stool noted in the ostomy pouch 609. A client had a new colostomy created 2 days earlier and is beginning to pass malodorous flatus from the stoma. What is the correct interpretation by the nurse? 1. This is a normal, expected event. 2. The client is experiencing early signs of ischemic bowel. 3. The client should not have the nasogastric tube removed. 4. This indicates inadequate preoperative bowel preparation. 610. Aclient has just had surgery to create an ileostomy. The nurse assesses the client in the immediate postoperative period for which most frequent complication of this type of surgery? 1. Folate deficiency 2. Malabsorption of fat 3. Intestinal obstruction 4. Fluid and electrolyte imbalance Adult—Gastrointestinal 692 UNIT XI Gastrointestinal Disorders of the Adult Client 611. The nurse provides instructions to a client about measures to treat inflammatory bowel syndrome (IBS). Which statement by the client indicates a need for further teaching? 1. “I need to limit my intake of dietary fiber.” 2. “I need to drink plenty, at least 8 to 10 cups daily.” 3. “I need to eat regular meals and chew my food well.” 4. “I will take the prescribed medications because they will regulate my bowel patterns.” 612. The nurse is monitoring a client for the early signs and symptoms of dumping syndrome. Which findings indicate this occurrence? 1. Sweating and pallor 2. Bradycardia and indigestion 3. Double vision and chest pain 4. Abdominal cramping and pain 613. A client with Crohn’s disease is scheduled to receive an infusion of infliximab. What intervention by the nurse will determine the effectiveness of treatment? 1. Monitoring the leukocyte count for 2 days after the infusion 2. Checking the frequency and consistency of bowel movements 3. Checking serum liver enzyme levels before and after the infusion 4. Carrying out a Hematest on gastric fluids after the infusion is completed BOX 53-5 Commonly Administered Antiemetics Serotonin Antagonists ▪ Dolasetron ▪ Granisetron ▪ Ondansetron Glucocorticoids ▪ Dexamethasone ▪ Methylprednisolone Substance P/ Neurokinin-1Antagonists ▪ Aprepitant ▪ Fosaprepitant Benzodiazepine ▪ Lorazepam Dopamine Antagonists Phenothiazines ▪ Chlorpromazine ▪ Perphenazine ▪ Prochlorperazine ▪ Promethazine Butyrophenones ▪ Haloperidol ▪ Droperidol Others ▪ Metoclopramide ▪ Trimethobenzamide Cannabinoids ▪ Dronabinol ▪ Nabilone Anticholinergics ▪ Scopolamine transdermal Antihistamines ▪ Cyclizine ▪ Dimenhydrinate ▪ Diphenhydramine ▪ Hydroxyzine ▪ Meclizine hydrochloride Adapted from Burchum J, Rosenthal L: Pharmacology for nursing care, ed 9, St. Louis, 2016, Saunders. BOX 53-6 Laxatives Bulk-Forming ▪ Methylcellulose ▪ Polycarbophil ▪ Psyllium Stimulants ▪ Bisacodyl ▪ Senna Emollient ▪ Docusate sodium Osmotics ▪ Magnesium hydroxide ▪ Magnesium citrate ▪ Sodium phosphates ▪ Polyethylene glycol and electrolytes ▪ Lactulose BOX 53-7 Medications to Control Diarrhea Opioids and Related Medications ▪ Diphenoxylate with atropine sulfate ▪ Loperamide Other Antidiarrheals ▪ Bismuth subsalicylate ▪ Bulk-forming medications ▪ Anticholinergic antispasmodics: dicyclomine, glycopyrrolate 702 UNIT XI Gastrointestinal Disorders of the Adult Client 614. A client has an as needed prescription for loperamide hydrochloride. For which condition should the nurse administer this medication? 1. Constipation 2. Abdominal pain 3. An episode of diarrhea 4. Hematest-positive nasogastric tube drainage 615. Aclient has an as needed prescription for ondansetron. For which condition(s) should the nurse administer this medication? 1. Paralytic ileus 2. Incisional pain 3. Urinary retention 4. Nausea and vomiting 616. A client has begun medication therapy with pancrelipase. The nurse evaluates that the medication is having the optimal intended benefit if which effect is observed? 1. Weight loss 2. Relief of heartburn 3. Reduction of steatorrhea 4. Absence of abdominal pain 617. An older client recently has been taking cimetidine. The nurse monitors the client for which most frequent central nervous system side effect of this medication? 1. Tremors 2. Dizziness 3. Confusion 4. Hallucinations 618. A client with a gastric ulcer has a prescription for sucralfate 1 gram by mouth 4 times daily. The nurse should schedule the medication for which times? 1. With meals and at bedtime 2. Every 6 hours around the clock 3. One hour after meals and at bedtime 4. One hour before meals and at bedtime 619. A client who uses nonsteroidal antiinflammatory drugs (NSAIDs) has been taking misoprostol. The nurse determines that the misoprostol is having the intended therapeutic effect if which finding is noted? 1. Resolved diarrhea 2. Relief of epigastric pain 3. Decreased platelet count 4. Decreased white blood cell count 620. A client has been taking omeprazole for 4 weeks. The ambulatory care nurse evaluates that the client is receiving the optimal intended effect of the medication if the client reports the absence of which symptom? 1. Diarrhea 2. Heartburn 3. Flatulence 4. Constipation 621. Aclient with a peptic ulcer is diagnosed with a Helicobacter pylori infection. The nurse is teaching the client about the medications prescribed, including clarithromycin, esomeprazole, and amoxicillin. Which statement by the client indicates the best understanding of the medication regimen? 1. “My ulcer will heal because these medications will kill the bacteria.” 2. “These medications are only taken when I have pain from my ulcer.” 3. “The medications will kill the bacteria and stop the acid production.” 4. “These medications will coat the ulcer and decrease the acid production in my stomach.” 622. A client has a new prescription for metoclopramide. On review of the chart, the nurse identifies that this medication can be safely administered with which condition? 1. Intestinal obstruction 2. Peptic ulcer with melena 3. Diverticulitis with perforation 4. Vomiting following cancer chemotherapy 623. The nurse determines the client needs further instruction on cimetidine if which statements were made? Select all that apply. 1. “I will take the cimetidine with my meals.” 2. “I’ll know the medication is working if my diarrhea stops.” 3. “My episodes of heartburn will decrease if the medication is effective.” 4. “Taking the cimetidine with an antacid will increase its effectiveness.” 5. “I will notify my health care provider if I become depressed or anxious.” 6. “Some of my blood levels will need to be monitored closely since I also take warfarin for atrial fibrillation.” 624. The nurse has given instructions to a client who has just been prescribed cholestyramine. Which statement by the client indicates a need for further instruction? 1. “I will continue taking vitamin supplements.” 2. “This medication will help to lower my cholesterol.” 3. “This medication should only be taken with water.” 4. “A high-fiber diet is important while taking this medication. 625. The emergency department nurse is assessing a client who has sustained a blunt injury to the chest wall. Which finding indicates the presence of a pneumothorax in this client? 1. A low respiratory rate 2. Diminished breath sounds 3. The presence of a barrel chest 4. A sucking sound at the site of injury Adult—Respiratory TABLE 54-3 Classification of the Tuberculin Skin Test Reaction Induration 5 5 or > 5 mm Considered Positive in: Induration 5 10 or > 10 mm Considered Positive in: Induration 5 15or > 15 mm Considered Positive in: HIV-infected persons Recent contact of a person with TB disease Persons with fibrotic changes on chest x-ray consistent with prior TB Clients with organ transplants Persons immunosuppressed for other reasons Recent immigrants from high-prevalence countries Injection drug users Residents and employees in high-risk congregate settings Mycobacteriology laboratory personnel Persons with clinical conditions that place them at high risk Children < 4 years of age Infants, children, and adolescents exposed to adults in high-risk categories Any person, including persons with no known risk factors for TB HIV, Human immunodeficiency virus; TB, tuberculosis. From Centers for Disease Control and Prevention: Tuberculosis (TB) fact sheets (website): http:/ /www.cdc.gov/tb/publications/ factsheets/ testing/ skintesting.htm. BOX 54-15 Client Education: Tuberculosis Provide the client and family with information about tuberculosis and allayconcerns about the contagious aspect of the infection. Instruct the client to follow the medication regimen exactly as prescribed and always to have a supply of the medication on hand. Advise the client that the medication regimen is continued up to 12 months depending on the situation. Advise the client of the side and adverse effects of the medication and ways of minimizing them to ensure compliance. Reassure the client that after 2 to 3 weeks of medication therapy, it is unlikely that the client will infect anyone. Advise the client to resume activities gradually. Instruct the client about the need for adequate nutrition and a well-balanced diet (foods rich in iron, protein, and vitamin C) to promote healing and to prevent recurrence of the infection. Inform the client and family that respiratory isolation is not necessary because family members already have been exposed. Instruct the client to cover the mouth and nose when coughing or sneezing and to put used tissues into plastic bags. Instruct the client and family about thorough hand washing. Inform the client that a sputum culture is needed every 2 to 4 weeks once medication therapy is initiated. Inform the client that when the results of 3 sputum cultures are negative, the client is no longer considered infectious and usually can return to former employment. Advise the client to avoid excessive exposure to silicone or dust because these substances can cause further lung damage. Instruct the client regarding the importance of compliance with treatment, follow-up care, and sputum cultures, as prescribed. CHAPTER 54 Respiratory System 729 Adult—Respiratory 626. The nurse is caring for a client hospitalized with acute exacerbation of chronic obstructive pulmonary disease. Which findings would the nurse expect to note on assessment of this client? Select all that apply. 1. A low arterial PCo2 level 2. Ahyperinflated chest noted on the chest x-ray 3. Decreased oxygen saturation with mild exercise 4. A widened diaphragm noted on the chest x-ray 5. Pulmonary function tests that demonstrate increased vital capacity 627. The nurse instructs a client to use the pursed-lip method of breathing and evaluates the teaching by asking the client about the purpose of this type of breathing. The nurse determines that the client understands if the client states that the primary purpose of pursed-lip breathing is to promote which outcome? 1. Promote oxygen intake 2. Strengthen the diaphragm 3. Strengthen the intercostal muscles 4. Promote carbon dioxide elimination 628. The nurse is preparing a list of home care instructions for a client who has been hospitalized and treated for tuberculosis. Which instructions should the nurse include on the list? Select all that apply. 1. Activities should be resumed gradually. 2. Avoid contact with other individuals, except family members, for at least 6 months. 3. Asputum culture is needed every 2 to 4 weeks once medication therapy is initiated. 4. Respiratory isolation is not necessary because family members already have been exposed. 5. Cover the mouth and nose when coughing or sneezing and put used tissues in plastic bags. 6. When 1 sputum culture is negative, the client is no longer considered infectious and usually can return to former employment. 629. The nurse is caring for a client after a bronchoscopy and biopsy. Which finding, if noted in the client, should be reported immediately to the health care provider? 1. Dry cough 2. Hematuria 3. Bronchospasm 4. Blood-streaked sputum 630. The nurse is preparing to suction a client via a tracheostomy tube. The nurse should plan to limit the suctioning time to a maximum of which time period? 1. 5 seconds 2. 10 seconds 3. 30 seconds 4. 60 seconds 631. The nurse is suctioning a client via an endotracheal tube. During the suctioning procedure, the nurse notes on the monitor that the heart rate is decreasing. Which nursing intervention is appropriate? 1. Continue to suction. 2. Notify the health care provider immediately. 3. Stop the procedure and reoxygenate the client. 4. Ensure that the suction is limited to 15 seconds. 632. The nurse is assessing the respiratory status of a client who has suffered a fractured rib. The nurse should expect to note which finding? 1. Slow, deep respirations 2. Rapid, deep respirations 3. Paradoxical respirations 4. Pain, especially with inspiration 633. A client with a chest injury has suffered flail chest. The nurse assesses the client for which most distinctive sign of flail chest? 1. Cyanosis 2. Hypotension 3. Paradoxical chest movement 4. Dyspnea, especially on exhalation 634. Aclient has been admitted with chest trauma after a motor vehicle crash and has undergone subsequent intubation. The nurse checks the client when the high-pressure alarm on the ventilator sounds, and notes that the client has absence of breath sounds in the right upper lobe of the lung. The nurse immediately assesses for other signs of which condition? 1. Right pneumothorax 2. Pulmonary embolism 3. Displaced endotracheal tube 4. Acute respiratory distress syndrome 635. The nurse is assessing a client with multiple trauma who is at risk for developing acute respiratory distress syndrome. The nurse should assess for which earliest sign of acute respiratory distress syndrome? 1. Bilateral wheezing 2. Inspiratory crackles 3. Intercostal retractions 4. Increased respiratory rate 636. The nurse is discussing the techniques of chest physiotherapy and postural drainage (respiratory treatments) to a client having expectoration problems because of chronic thick, tenacious mucus production in the lower airway. The nurse explains that after the client is positioned for postural drainage the nurse will perform which action to help loosen secretions? 1. Palpation and clubbing 2. Percussion and vibration 730 UNIT XII Respiratory Disorders of the Adult Client 3. Hyperoxygenation and suctioning 4. Administer a bronchodilator and monitor peak flow 637. The nurse has conducted discharge teaching with a client diagnosed with tuberculosis who has been receiving medication for 2 weeks. The nurse determines that the client has understood the information if the client makes which statement? 1. “I need to continue medication therapy for 1 month.” 2. “I can’t shop at the mall for the next 6 months.” 3. “I can return to work if a sputum culture comes back negative.” 4. “I should not be contagious after 2 to 3 weeks of medication therapy.” 638. The nurse is preparing to give a bed bath to an immobilized client with tuberculosis. The nurse should wear which items when performing this care? 1. Surgical mask and gloves 2. Particulate respirator, gown, and gloves 3. Particulate respirator and protective eyewear 4. Surgical mask, gown, and protective eyewear 639. A client has experienced pulmonary embolism. The nurse should assess for which symptom, which is most commonly reported? 1. Hot, flushed feeling 2. Sudden chills and fever 3. Chest pain that occurs suddenly 4. Dyspnea when deep breaths are taken 640. A client who is human immunodeficiency virus (HIV)–positive has had a tuberculin skin test (TST). The nurse notes a 7-mm area of induration at the site of the skin test and interprets the result as which finding? 1. Positive 2. Negative 3. Inconclusive 4. Need for repeat testing 641. A client with acquired immunodeficiency syndrome (AIDS) has histoplasmosis. The nurse should assess the client for which expected finding? 1. Dyspnea 2. Headache 3. Weight gain 4. Hypothermia 642. The nurse is giving discharge instructions to a client with pulmonary sarcoidosis. The nurse concludes that the client understands the information if the client indicates to report which early sign of exacerbation? 1. Fever 2. Fatigue 3. Weight loss 4. Shortness of breath 643. The nurse is taking the history of a client with occupational lung disease (silicosis). The nurse should assess whether the client wears which item during periods of exposure to silica particles? 1. Mask 2. Gown 3. Gloves 4. Eye protection 644. An oxygen delivery system is prescribed for a client with chronic obstructive pulmonary disease to deliver a precise oxygen concentration. Which oxygen delivery system would the nurse prepare for the client? 1. Face tent 2. Venturi mask 3. Aerosol mask 4. Tracheostomy collar 645. The nurse is instructing a hospitalized client with a diagnosis of emphysema about measures that will enhance the effectiveness of breathing during dyspneic periods. Which position should the nurse instruct the client to assume? 1. Sitting up in bed 2. Side-lying in bed 3. Sitting in a recliner chair 4. Sitting up and leaning on an overbed table 646. The community health nurse is conducting an educational session with community members regarding the signs and symptoms associated with tuberculosis. The nurse informs the participants that tuberculosis is considered as a diagnosis if which signs and symptoms are present? Select all that apply. 1. Dyspnea 2. Headache 3. Night sweats 4. A bloody, productive cough 5. A cough with the expectoration of mucoid sputum 647. The nurse performs an admission assessment on a client with a diagnosis of tuberculosis. The nurse should check the results of which diagnostic test that will confirm this diagnosis? 1. Chest x-ray 2. Bronchoscopy 3. Sputum culture 4. Tuberculin skin test Adult—Respiratory CHAPTER 54 Respiratory System 731 648. The low-pressure alarm sounds on a ventilator. The nurse assesses the client and then attempts to determine the cause of the alarm. If unsuccessful in determining the cause of the alarm, the nurse should take what initial action? 1. Administer oxygen 2. Check the client’s vital signs 3. Ventilate the client manually 4. Start cardiopulmonary resuscitation 649. A client has a prescription to take guaifenesin. The nurse determines that the client understands the proper administration of this medication if the client states that he or she will perform which action? 1. Take an extra dose if fever develops 2. Take the medication with meals only 3. Take the tablet with a full glass of water 4. Decrease the amount of daily fluid intake 650. The nurse is preparing to administer a dose of naloxone intravenously to a client with an opioid overdose. Which supportive medical equipment should the nurse plan to have at the client’s bedside if needed? 1. Nasogastric tube 2. Paracentesis tray 3. Resuscitation equipment 4. Central line insertion tray 651. The nurse teaches a client about the effects of diphenhydramine, which has been prescribed as a cough suppressant. The nurse determines that the client needs further instruction if the client makes which statement? 1. “I will take the medication on an empty stomach.” 2. “I won’t drink alcohol while taking this medication.” 3. “I won’t do activities that require mental alertness while taking this medication.” 4. “I will use sugarless gum, candy, or oral rinses to decrease dryness in my mouth.” 652. Acromolyn sodium inhaler is prescribed for a client with allergic asthma. The nurse provides instructions regarding the adverse effects of this medication and should tell the client that which undesirable effect is associated with this medication? 1. Insomnia 2. Constipation 3. Hypotension 4. Bronchospasm 653. Terbutaline is prescribed for a client with bronchitis. The nurse checks the client’s medical history for which disorder in which the medication should be used with caution? 1. Osteoarthritis 2. Hypothyroidism 3. Diabetes mellitus 4. Polycystic disease 654. Zafirlukast is prescribed for a client with bronchial asthma. Which laboratory test does the nurse expect to be prescribed before the administration of this medication? 1. Platelet count 2. Neutrophil count 3. Liver function tests 4. Complete blood count 655. A client has been taking isoniazid for 2 months. The client complains to the nurse about numbness, paresthesias, and tingling in the extremities. The nurse interprets that the client is experiencing which problem? 1. Hypercalcemia 2. Peripheral neuritis 3. Small blood vessel spasm 4. Impaired peripheral circulation 656. A client is to begin a 6-month course of therapy with isoniazid. The nurse should plan to teach the client to take which action? 1. Use alcohol in small amounts only. 2. Report yellow eyes or skin immediately. 3. Increase intake of Swiss or aged cheeses. 4. Avoid vitamin supplements during therapy. 657. Aclient has been started on long-term therapy with rifampin. The nurse should provide which information to the client about the medication? 1. Should always be taken with food or antacids 2. Should be double-dosed if 1 dose is forgotten 3. Causes orange discoloration of sweat, tears, urine, and feces 4. May be discontinued independently if symptoms are gone in 3 months 658. The nurse has given a client taking ethambutol information about the medication. The nurse determines that the client understands the instructions if the client states that he or she will immediately report which finding? 1. Impaired sense of hearing 2. Gastrointestinal side effects 3. Orange-red discoloration of body secretions 4. Difficulty in discriminating the color red from green 659. A client with tuberculosis is being started on antituberculosis therapy with isoniazid. Before giving the client the first dose, the nurse should ensure that which baseline study has been completed? 1. Electrolyte levels 2. Coagulation times 3. Liver enzyme levels 4. Serum creatinine level 660. The nurse has a prescription to give a client salmeterol, 2 puffs, and beclomethasone dipropionate, 2 puffs, by metered-dose inhaler. The nurse should administer the medication using which procedure? 1. Beclomethasone first and then the salmeterol 2. Salmeterol first and then the beclomethasone CHAPTER 55 Respiratory Medications 749 Adult—Respiratory 3. Alternating a single puff of each, beginning with the salmeterol 4. Alternating a single puff of each, beginning with the beclomethasone 661. Rifabutin is prescribed for a client with active Mycobacterium avium complex (MAC) disease and tuberculosis. For which side and adverse effects of the medication should the nurse monitor? Select all that apply. 1. Signs of hepatitis 2. Flulike syndrome 3. Low neutrophil count 4. Vitamin B6 deficiency 5. Ocular pain or blurred vision 6. Tingling and numbness of the fingers 662. A client has begun therapy with theophylline. The nurse should plan to teach the client to limit the intake of which items while taking this medication? 1. Coffee, cola, and chocolate 2. Oysters, lobster, and shrimp 3. Melons, oranges, and pineapple 4. Cottage cheese, cream cheese, and dairy creamers 663. The nurse has just administered the first dose of omalizumab to a client. Which statement by the client would alert the nurse that the client may be experiencing a life-threatening effect? 1. “I have a severe headache.” 2. “My feet are quite swollen.” 3. “I am nauseated and may vomit.” 4. “My lips and tongue are swollen.” 664. The nurse is caring for a client with a diagnosis of influenza who first began to experience symptoms yesterday. Antiviral therapy is prescribed and the nurse provides instructions to the client about the therapy. Which statement by the client indicates an understanding of the instructions? 1. “I must take the medication exactly as prescribed.” 2. “Once I start the medication, I will no longer be contagious.” 3. “I will not get any colds or infections while taking this medication.” 4. “This medication has minimal side effects and I can return to normal activities.” 665. A client is admitted to the emergency department with chest pain that is consistent with myocardial infarction based on elevated troponin levels. Heart sounds are normal and vital signs are noted on the client’s chart. The nurse should alert the health care provider because these changes are most consistent with which complication? Refer to ch art. 1. Cardiogenic shock 2. Cardiac tamponade 3. Pulmonary embolism 4. Dissecting thoracic aortic aneurysm 666. A client admitted to the hospital with chest pain and a history of type 2 diabetes mellitus is scheduled for cardiac catheterization. Which medication would need to be withheld for 24 hours before the procedure and for 48 hours after the procedure? 1. Glipizide 2. Metformin 3. Repaglinide 4. Regular insulin 667. Aclient in sinus bradycardia, with a heart rate of 45 beats/minute, complains of dizziness and has a blood pressure of 82/60 mm Hg. Which prescription should the nurse anticipate will be prescribed? 1. Administer digoxin. 2. Defibrillate the client. 3. Continue to monitor the client. 4. Prepare for transcutaneous pacing. Adult—Cardiovascular Client’s Chart Time: Pulse: 11:00 a.m. 92 beats/min 96 beats/ min 104 beats/ min 118 beats/ min Respiratory rate: 24 breaths/min 26 breaths/ min 28 breaths/ min 32 breaths/min Blood pressure: 140/88 mm Hg 128/82 mm Hg 104/ 68 mm Hg 88/58 mm Hg BOX 56-10 Education for the Client with Hypertension Describe the importance of compliance with the treatment plan. Describe the disease process, explaining that symptoms usually do not develop until organs have suffered damage. Initiate and assist the client in planning a regular exercise program, avoiding heavy weight-lifting and isometric exercises. Emphasize the importance of beginning the exercise program gradually. Encourage the client to express feelings about daily stress. Assist the client to identify ways to reduce stress. Teach relaxation techniques. Instruct the client in how to incorporate relaxation techniques into the daily living pattern. Instruct the client and family in the technique for monitoring blood pressure (BP). Instruct the client to maintain a diary of BP readings. Emphasize the importance of lifelong medication. Instruct the client and family about dietary restrictions, which may include sodium, fat, calories, and cholesterol. Instruct the client in how to shop for and prepare low-sodium meals. Provide a list of products that contain sodium. Instruct the client to read labels of products to determine sodium content, focusing on substances listed as sodium, NaCl, or MSG (monosodium glutamate). Instruct the client to bake, roast, or boil foods; avoid salt in preparation of foods; and avoid using salt at the table. Instruct the client that fresh foods are best to consume, and to avoid canned foods. Instruct the client about the actions, side effects, and scheduling of medications. Advise the client that if uncomfortable side effects occur, to contact the health care provider and not to stop the medication. Instruct the client to avoid over-the-counter medications. Stress the importance of follow-up care. CHAPTER 56 Cardiovascular System 789 668. The nurse in a medical unit is caring for a client with heart failure. The client suddenly develops extreme dyspnea, tachycardia, and lung crackles and the nurse suspects pulmonary edema. The nurse immediately asks another nurse to contact the health care provider and prepares to implement which priority interventions? Select all that apply. 1. Administering oxygen 2. Inserting a Foley catheter 3. Administering furosemide 4. Administering morphine sulfate intravenously 5. Transporting the client to the coronary care unit 6. Placing the client in a low Fowler’s side-lying position 669. A client with myocardial infarction suddenly becomes tachycardic, shows signs of air hunger, and begins coughing frothy, pink-tinged sputum. Which finding would the nurse anticipate when auscultating the client’s breath sounds? 1. Stridor 2. Crackles 3. Scattered rhonchi 4. Diminished breath sounds 670. A client with myocardial infarction is developing cardiogenic shock. Because of the risk of myocardial ischemia, what condition should the nurse carefully assess the client for? 1. Bradycardia 2. Ventricular dysrhythmias 3. Rising diastolic blood pressure 4. Falling central venous pressure 671. A client who had cardiac surgery 24 hours ago has had a urine output averaging 20 mL/hour for 2 hours. The client received a single bolus of 500 mL of intravenous fluid. Urine output for the subsequent hour was 25 mL. Daily laboratory results indicate that the blood urea nitrogen level is 45 mg/dL(16 mmol/L) and the serum creatinine level is 2.2 mg/dL (194 mcmol/L). On the basis of these findings, the nurse would anticipate that the client is at risk for which problem? 1. Hypovolemia 2. Acute kidney injury 3. Glomerulonephritis 4. Urinary tract infection 672. The nurse is reviewing an electrocardiogram rhythm strip. The P waves and QRS complexes are regular. The PR interval is 0.16 seconds, and QRS complexes measure 0.06 seconds. The overall heart rate is 64 beats/minute. Which action should the nurse take? 1. Check vital signs. 2. Check laboratory test results. 3. Notify the health care provider. 4. Continue to monitor for any rhythm change. 673. A client is wearing a continuous cardiac monitor, which begins to sound its alarm. The nurse sees no electrocardiographic complexes on the screen. Which is the priority nursing action? 1. Call a code. 2. Call the health care provider. 3. Check the client’s status and lead placement. 4. Press the recorder button on the electrocardiogram console. 674. The nurse is watching the cardiac monitor and notices that the rhythm suddenly changes. There are no P waves, the QRS complexes are wide, and the ventricular rate is regular but more than 140 beats/minute. The nurse determines that the client is experiencing which dysrhythmia? 1. Sinus tachycardia 2. Ventricular fibrillation 3. Ventricular tachycardia 4. Premature ventricular contractions 675. A client has frequent bursts of ventricular tachycardia on the cardiac monitor. What should the nurse be most concerned about with this dysrhythmia? 1. It can develop into ventricular fibrillation at any time. 2. It is almost impossible to convert to a normal rhythm. 3. It is uncomfortable for the client, giving a sense of impending doom. 4. It produces a high cardiac output that quickly leads to cerebral and myocardial ischemia. 676. A client is having frequent premature ventricular contractions. The nurse should place priority on assessment of which item? 1. Sensation of palpitations 2. Causative factors, such as caffeine 3. Blood pressure and oxygen saturation 4. Precipitating factors, such as infection 677. The client has developed atrial fibrillation, with a ventricular rate of 150 beats/minute. The nurse should assess the client for which associated signs and/or symptoms? 1. Flat neck veins 2. Nausea and vomiting 3. Hypotension and dizziness 4. Hypertension and headache 678. The nurse is watching the cardiac monitor, and a client’s rhythm suddenly changes. There are no P Adult—Cardiovascular 790 UNIT XIII Cardiovascular Disorders of the Adult Client Adult—Cardiovascular waves; instead, there are fibrillatory waves before each QRS complex. How should the nurse correctly interpret the client’s heart rhythm? 1. Atrial fibrillation 2. Sinus tachycardia 3. Ventricular fibrillation 4. Ventricular tachycardia 679. The nurse is assisting to defibrillate a client in ventricular fibrillation. After placing the pad on the client’s chest and before discharge, which intervention is a priority? 1. Ensure that the client has been intubated. 2. Set the defibrillator to the “synchronize” mode. 3. Administer an amiodarone bolus intravenously. 4. Confirm that the rhythm is actually ventricular fibrillation. 680. A client in ventricular fibrillation is about to be defibrillated. To convert this rhythm effectively, the monophasic defibrillator machine should be set at which energy level (in joules, J) for the first delivery? 1. 50 J 2. 120 J 3. 200 J 4. 360 J 681. The nurse should evaluate that defibrillation of a client was most successful if which observation was made? 1. Arousable, sinus rhythm, blood pressure (BP) 116/72 mm Hg 2. Nonarousable, sinus rhythm, BP 88/60 mm Hg 3. Arousable, marked bradycardia, BP 86/ 54 mm Hg 4. Nonarousable, supraventricular tachycardia, BP 122/60 mm Hg 682. The nurse is evaluating a client’s response to cardioversion. Which assessment would be the priority? 1. Blood pressure 2. Status of airway 3. Oxygen flow rate 4. Level of consciousness 683. The nurse is caring for a client who has just had implantation of an automatic internal cardioverter-defibrillator. The nurse should assess which item based on priority? 1. Anxiety level of the client and family 2. Presence of a MedicAlert card for the client to carry 3. Knowledge of restrictions on postdischarge physical activity 4. Activation status of the device, heart rate cutoff, and number ofshocks it is programmed to deliver 684. A client’s electrocardiogram strip shows atrial and ventricular rates of110 beats/minute. The PRinterval is 0.14 seconds, the QRScomplexmeasures 0.08 seconds, and the PP and RR intervals are regular. How should the nurse correctly interpret this rhythm? 1. Sinus tachycardia 2. Sinus bradycardia 3. Sinus dysrhythmia 4. Normal sinus rhythm 685. The nurse is assessing the neurovascular status of a client who returned to the surgical nursing unit 4 hours ago after undergoing aortoiliac bypass graft. The affected leg is warm, and the nurse notes redness and edema. The pedal pulse is palpable and unchanged from admission. How should the nurse correctly interpret the client’s neurovascular status? 1. The neurovascular status is normal because of increased blood flow through the leg. 2. The neurovascular status is moderately impaired, and the surgeon should be called. 3. The neurovascular status is slightly deteriorating and should be monitored for another hour. 4. The neurovascular status is adequate from an arterial approach, but venous complications are arising. 686. The nurse is evaluating the condition of a client after pericardiocentesis performed to treat cardiac tamponade. Which observation would indicate that the procedure was effective? 1. Muffled heart sounds 2. A rise in blood pressure 3. Jugular venous distention 4. Client expressions of dyspnea 687. The nurse is caring for a client who had a resection of an abdominal aortic aneurysm yesterday. The client has an intravenous (IV) infusion at a rate of 150 mL/hour, unchanged for the last 10 hours. The client’s urine output for the last 3 hours has been 90, 50, and 28 mL (28 mL is most recent). The client’s blood urea nitrogen level is 35 mg/dL (12.6 mmol/L) and the serum creatinine level is 1.8 mg/dL (159 mcmol/L), measured this morning. Which nursing action is the priority? 1. Check the urine specific gravity. 2. Call the health care provider (HCP). 3. Put the IV line on a pump so that the infusion rate is sure to stay stable. 4. Check to see if the client had a blood sample for a serum albumin level drawn. 688. A client with variant angina is scheduled to receive an oral calcium channel blocker twice daily. Which statement by the client indicates the need for further teachin g? CHAPTER 56 Cardiovascular System 791 1. “I should notify my doctor if my feet or legs start to swell.” 2. “My doctor told me to call his office if my pulse rate decreases below 60.” 3. “Avoiding grapefruit juice will definitely be a challenge for me, since I usually drink it every morning with breakfast.” 4. “My spouse told me that since I have developed this problem, we are going to stop walking in the mall every morning.” 689. The nurse notes that a client with sinus rhythm has a premature ventricular contraction that falls on the T wave of the preceding beat. The client’s rhythm suddenly changes to one with no P waves, no definable QRS complexes, and coarse wavy lines of varying amplitude. How should the nurse correctly interpret this rhythm? 1. Asystole 2. Atrial fibrillation 3. Ventricular fibrillation 4. Ventricular tachycardia 690. Aclient with atrial fibrillation is receiving a continuous heparin infusion at 1000 units/hour. The nurse determines that the client is receiving the therapeutic effect based on which results? 1. Prothrombin time of 12.5 seconds 2. Activated partial thromboplastin time of 60 seconds 3. Activated partial thromboplastin time of 28 seconds 4. Activated partial thromboplastin time longer than 120 seconds 691. The nurse provides discharge instructions to a client who is taking warfarin sodium. Which statement, by the client, reflects the need for further teach ing? 1. “I will avoid alcohol consumption.” 2. “I will take my pills every day at the same time.” 3. “I have already called my family to pick up a MedicAlert bracelet.” 4. “I will take coated aspirin for my headaches because it will coat my stomach.” 692. A client who is receiving digoxin daily has a serum potassium level of 3 mEq/L (3 mmol/L) and is complaining of anorexia. The health care provider prescribes a serum digoxin level to be done. The nurse checks the results and should expect to note which level that is outside of the therapeutic range? 1. 0.3 ng/mL 2. 0.5 ng/mL 3. 0.8 ng/mL 4. 1.0 ng/mL 693. A client is being treated with procainamide for a cardiac dysrhythmia. Following intravenous administration of the medication, the client complains of dizziness. What intervention should the nurse take first? 1. Measure the heart rate on the rhythm strip. 2. Administer prescribed nitroglycerin tablets. 3. Obtain a 12-lead electrocardiogram immediately. 4. Auscultate the client’s apical pulse and obtain a blood pressure. 694. The nurse is monitoring a client who is taking propranolol. Which assessment finding indicates a potential adverse complication associated with this medication? 1. The development of complaints of insomnia 2. The development of audible expiratory wheezes 3. Abaseline blood pressure of 150/80 mm Hg followed by a blood pressure of 138/72 mm Hg after 2 doses of the medication 4. A baseline resting heart rate of 88 beats/minute followed by a resting heart rate of 72 beats/ minute after 2 doses of the medication 695. A client with a clot in the right atrium is receiving a heparin sodium infusion at 1000 units/hour and warfarin sodium 7.5 mg at 5:00 p.m. daily. The morning laboratory results are as follows: activated partial thromboplastin time (aPTT), 32 seconds; international normalized ratio (INR), 1.3. The nurse should take which action based on the client’s laboratory results? 1. Collaborate with the health care provider (HCP) to discontinue the heparin infusion and administer the warfarin sodium as prescribed. 2. Collaborate with the HCP to obtain a prescription to increase the heparin infusion and administer the warfarin sodium as prescribed. 3. Collaborate with the HCP to withhold the warfarin sodium since the client is receiving a heparin infusion and the aPTT is within the therapeutic range. 4. Collaborate with the HCP to continue the heparin infusion at the same rate and to discuss use of dabigatran etexilate in place of warfarin sodium. 696. A client is diagnosed with an ST segment elevation myocardial infarction (STEMI) and is receiving a tissue plasminogen activator, alteplase. Which action is a priority nursing intervention? Adult—Cardiovascular 810 UNIT XIII Cardiovascular Disorders of the Adult Client Adult—Cardiovascular 1. Monitor for kidney failure. 2. Monitor psychosocial status. 3. Monitor for signs of bleeding. 4. Have heparin sodium available. 697. The nurse is planning to administer hydrochlorothiazide to a client. The nurse should monitor for which adverse effects related to the administration of this medication? 1. Hypouricemia, hyperkalemia 2. Increased risk of osteoporosis 3. Hypokalemia, hyperglycemia, sulfa allergy 4. Hyperkalemia, hypoglycemia, penicillin allergy 698. The home health care nurse is visiting a client with elevated triglyceride levels and a serum cholesterol level of 398 mg/dL (10 mmol/L). The client is taking cholestyramine and the nurse teaches the client about the medication. Which statement, by the client, indicates the need for further teachin g? 1. “Constipation and bloating might be a problem.” 2. “I’ll continue to watch my diet and reduce my fats.” 3. “Walking a mile each day will help the whole process.” 4. “I’ll continue my nicotinic acid from the health food store.” 699. The nurse is monitoring a client who is taking digoxin for adverse effects. Which findings are characteristic of digoxin toxicity? Select all that apply. 1. Tremors 2. Diarrhea 3. Irritability 4. Blurred vision 5. Nausea and vomiting 700. Prior to administering a client’s daily dose of digoxin, the nurse reviews the client’s laboratory data and notes the following results: serum calcium, 9.8 mg/dL (2.45 mmol/L); serum magnesium, 1.0 mEq/L (0.5 mmol/L); serum potassium, 4.1 mEq/L (4.1 mmol/L); serum creatinine, 0.9 mg/ dL (79.5 mcmol/L). Which result should alert the nurse that the client is at risk for digoxin toxicity? 1. Serum calcium level 2. Serum potassium level 3. Serum creatinine level 4. Serum magnesium level 701. A client being treated for heart failure is administered intravenous bumetanide. Which outcome indicates that the medication has achieved the expected effect? 1. Cough becomes productive of frothy pink sputum. 2. Urine output increases from 10 mL/hour to greater than 50 mL hourly. 3. The serum potassium level changes from 3.8 to 3.1 mEq/L (3.8 to 3.1 mmol/L). 4. B-type natriuretic peptide (BNP) factor increases from 200 to 262 pg/mL (200 to 262 ng/L). 702. Intravenous heparin therapy is prescribed for a client. While implementing this prescription, the nurse ensures that which medication is available on the nursing unit? 1. Vitamin K 2. Protamine sulfate 3. Potassium chloride 4. Aminocaproic acid 703. A client receiving thrombolytic therapy with a continuous infusion of alteplase suddenly becomes extremely anxious and complains of itching. The nurse hears stridor and notes generalized urticaria and hypotension. Which nursing action is the priority? 1. Administer oxygen and protamine sulfate. 2. Cut the infusion rate in half and sit the client up in bed. 3. Stop the infusion and call for the Rapid Response Team (RRT). 4. Administer diphenhydramine and epinephrine and continue the infusion. 704. The nurse should report which assessment finding to the health care provider (HCP) before initiating thrombolytic therapy in a client with pulmonary embolism? 1. Adventitious breath sounds 2. Temperature of 99.4 °F (37.4 °C) orally 3. Blood pressure of 198/110 mm Hg 4. Respiratory rate of 28 breaths/minute 705. A client is prescribed nicotinic acid for hyperlipidemia and the nurse provides instructions to the client about the medication. Which statement by the client indicates an understanding of the instructions? 1. “It is not necessary to avoid the use of alcohol.” 2. “The medication should be taken with meals to decrease flushing.” 3. “Clay-colored stools are a common side effect and should not be of concern.” 4. “Ibuprofen IB taken 30 minutes before the nicotinic acid should decrease the flushing. 706. Aclient with acute kidney injury has a serum potassium level of 7.0 mEq/L (7.0 mmol/L). The nurse should plan which actions as a priority? Select all that apply. 1. Place the client on a cardiac monitor. 2. Notify the health care provider (HCP). 3. Put the client on NPO (nothing by mouth) status except for ice chips. 4. Review the client’s medications to determine if any contain or retain potassium. 5. Allow an extra 500 mL of intravenous fluid intake to dilute the electrolyte concentration. 707. A client being hemodialyzed suddenly becomes short of breath and complains of chest pain. The client is tachycardic, pale, and anxious and the nurse suspects air embolism. What are the priority nursing actions? Select all that apply. 1. Administer oxygen to the client. 2. Continue dialysis at a slower rate after checking the lines for air. 3. Notify the health care provider (HCP) and Rapid Response Team. 4. Stop dialysis, and turn the client on the left side with head lower than feet. 5. Bolus the client with 500 mL of normal saline to break up the air embolus. 708. A client arrives at the emergency department with complaints of low abdominal pain and hematuria. The client is afebrile. The nurse next assesses the client to determine a history of which condition? 1. Pyelonephritis 2. Glomerulonephritis 3. Trauma to the bladder or abdomen 4. Renal cancer in the client’s family 709. The nurse discusses plans for future treatment options with a client with symptomatic polycystic kidney disease. Which treatment should be included in this discussion? Select all th at apply. B C A Retropubic Perineal Suprapubic FIGURE 58-8 Surgical approaches for prostatectomy. A, Retropubic approach involves a low abdominal incision. B, Perineal approach involves an incision between the scrotum and anus. C, Suprapubic approach involves a midline abdominal incision. CHAPTER 58 Renal and Urinary System 843 1. Hemodialysis 2. Peritoneal dialysis 3. Kidney transplant 4. Bilateral nephrectomy 5. Intense immunosuppression therapy 710. A client is admitted to the emergency department following a fall from a horse and the health care provider (HCP) prescribes insertion of a urinary catheter. While preparing for the procedure, the nurse notes blood at the urinary meatus. The nurse should take which action? 1. Notify the HCP before performing the catheterization. 2. Use a small-sized catheter and an anesthetic gel as a lubricant. 3. Administer parenteral pain medication before inserting the catheter. 4. Clean the meatus with soap and water before opening the catheterization kit. 711. The nurse is assessing the patency of a client’s left arm arteriovenous fistula prior to initiating hemodialysis. Which finding indicates that the fistula is patent? 1. Palpation of a thrill over the fistula 2. Presence of a radial pulse in the left wrist 3. Visualization of enlarged blood vessels at the fistula site 4. Capillary refill less than 3 seconds in the nail beds of the fingers on the left hand 712. A male client has a tentative diagnosis of urethritis. The nurse should assess the client for which manifestation of the disorder? 1. Hematuria and pyuria 2. Dysuria and proteinuria 3. Hematuria and urgency 4. Dysuria and penile discharge 713. The nurse is assessing a client with epididymitis. The nurse anticipates which findings on physical examination? 1. Fever, diarrhea, groin pain, and ecchymosis 2. Nausea, painful scrotal edema, and ecchymosis 3. Fever, nausea, vomiting, and painful scrotal edema 4. Diarrhea, groin pain, testicular torsion, and scrotal edema 714. A client complains of fever, perineal pain, and urinary urgency, frequency, and dysuria. To assess whether the client’s problem is related to bacterial prostatitis, the nurse reviews the results of the prostate examination for which characteristic of this disorder? 1. Soft and swollen prostate gland 2. Swollen, and boggy prostate gland 3. Tender and edematous prostate gland 4. Tender, indurated prostate gland that is warm to the touch 715. The nurse is collecting data from a client. Which symptom described by the client is characteristic of an early symptom of benign prostatic hyperplasia? 1. Nocturia 2. Scrotal edema 3. Occasional constipation 4. Decreased force in the stream of urine 716. The nurse monitoring a client receiving peritoneal dialysis notes that the client’s outflow is less than the inflow. Which actions should the nurse take? Select all that apply. 1. Check the level of the drainage bag. 2. Reposition the client to his or her side. 3. Contact the health care provider (HCP). 4. Place the client in good body alignment. 5. Check the peritoneal dialysis system for kinks. 6. Increase the flow rate of the peritoneal dialysis solution. 717. A hemodialysis client with a left arm fistula is at risk for arterial steal syndrome. The nurse should assess for which manifestations of this complication? 1. Warmth, redness, and pain in the left hand 2. Ecchymosis and audible bruit over the fistula 3. Edema and reddish discoloration of the left arm 4. Pallor, diminished pulse, and pain in the left hand 718. The nurse is reviewing a client’s record and notes that the health care provider has documented that the client has chronic renal disease. On review of the laboratory results, the nurse most likely would expect to note which finding? 1. Elevated creatinine level 2. Decreased hemoglobin level 3. Decreased red blood cell count 4. Increased number of white blood cells in the urine 719. A client with chronic kidney disease returns to the nursing unit following a hemodialysis treatment. On assessment, the nurse notes that the client’s temperature is 38.5 °C (101.2 °F). Which nursing action is most appropriate? 1. Encourage fluid intake. 2. Notify the health care provider. 3. Continue to monitor vital signs. 4. Monitor the site of the shunt for infection. Adult—Renal and Urinary 844 UNIT XIV Renal and Urinary Disorders of the Adult Client 720. The nurse is performing an assessment on a client who has returned from the dialysis unit following hemodialysis. The client is complaining of headache and nausea and is extremely restless. Which is the priority nursing action? 1. Monitor the client. 2. Elevate the head of the bed. 3. Assess the fistula site and dressing. 4. Notify the health care provider (HCP). 721. A client with severe back pain and hematuria is found to have hydronephrosis due to urolithiasis. The nurse anticipates which treatment will be done to relieve the obstruction? Select all that apply. 1. Peritoneal dialysis 2. Analysis of the urinary stone 3. Intravenous opioid analgesics 4. Insertion of a nephrostomy tube 5. Placement ofa ureteral stent with ureteroscopy 722. The nurse is instructing a client with diabetes mellitus about peritoneal dialysis. The nurse tells the client that it is important to maintain the prescribed dwell time for the dialysis because of the risk of which complication? 1. Peritonitis 2. Hyperglycemia 3. Hyperphosphatemia 4. Disequilibrium syndrome 723. A week after kidney transplantation, a client develops a temperature of 101 °F (38.3 °C), the blood pressure is elevated, and there is tenderness over the transplanted kidney. The serum creatinine is rising and urine output is decreased. The x-ray indicates that the transplanted kidney is enlarged. Based on these assessment findings, the nurse anticipates which treatment? 1. Antibiotic therapy 2. Peritoneal dialysis 3. Removal of the transplanted kidney 4. Increased immunosuppression therapy 724. Aclient is admitted to the hospital with a diagnosis of benign prostatic hyperplasia, and a transurethral resection of the prostate is performed. Four hours after surgery, the nurse takes the client’s vital signs and empties the urinary drainage bag. Which assessment finding indicates the need to notify the health care provider (HCP)? 1. Red, bloody urine 2. Pain rated as 2 on a 0–10 pain scale 3. Urinary output of 200 mL higher than intake 4. Blood pressure, 100/50 mm Hg; pulse, 130 beats/minute 725. The client newly diagnosed with chronic kidney disease recently has begun hemodialysis. Knowing that the client is at risk for disequilibrium syndrome, the nurse should assess the client during dialysis for which associated manifestations? 1. Hypertension, tachycardia, and fever 2. Hypotension, bradycardia, and hypothermia 3. Restlessness, irritability, and generalized weakness 4. Headache, deteriorating level of consciousness, and twitching 726. A client who has a cold is seen in the emergency department with an inability to void. Because the client has a history of benign prostatic hyperplasia, the nurse determines that the client should be questioned about the use of which medication? 1. Diuretics 2. Antibiotics 3. Antilipemics 4. Decongestants 727. Nitrofurantoin is prescribed for a client with a urinary tract infection. The client contacts the nurse and reports a cough, chills, fever, and difficulty breathing. The nurse should make which interpretation about the client’s complaints? 1. The client may have contracted the flu. 2. The client is experiencing anaphylaxis. 3. The client is experiencing expected effects of the medication. 4. The client is experiencing a pulmonary reaction requiring cessation of the medication. 728. The nurse is providing discharge instructions to a client receiving trimethoprim-sulfamethoxazole. Which instruction should be included in the list? 1. Advise that sunscreen is not needed. 2. Drink 8 to 10 glasses of water per day. 3. If the urine turns dark brown, call the health care provider (HCP) immediately. 4. Decrease the dosage when symptoms are improving to prevent an allergic response. 729. Trimethoprim-sulfamethoxazole is prescribed for a client. The nurse should instruct the client to report which symptom if it develops during the course of this medication therapy? 1. Nausea 2. Diarrhea 3. Headache 4. Sore throat 730. Phenazopyridine is prescribed for a client with a urinary tract infection. The nurse evaluates that the medication is effective based on which observation? 1. Urine is clear amber. 2. Urination is not painful. 3. Urge incontinence is not present. 4. A reddish-orange discoloration of the urine is present. 731. Bethanechol chloride is prescribed for a client with urinary retention. Which disorder would be a contraindication to the administration of this medication? 1. Gastric atony 2. Urinary strictures 3. Neurogenic atony 4. Gastroesophageal reflux 732. The nurse, who is administering bethanechol chloride, is monitoring for cholinergic overdose associated with the medication. The nurse should check the client for which sign of overdose? 1. Dry skin 2. Dry mouth 3. Bradycardia 4. Signs of dehydration Adult—Renal and Urinary BOX 59-7 Hematopoietic Growth Factors Erythropoietic Growth Factors ▪ Epoetin alfa ▪ Darbepoetin alfa ▪ Peginesatide Leukopoietic Growth Factors ▪ Filgrastim ▪ Pegfilgrastim ▪ Sargramostim CHAPTER 59 Renal and Urinary Medications 855 Adult—Renal and Urinary 733. Oxybutynin chloride is prescribed for a client with urge incontinence. Which sign would indicate a possible toxic effect related to this medication? 1. Pallor 2. Drowsiness 3. Bradycardia 4. Restlessness 734. Following kidney transplantation, cyclosporine is prescribed for a client. Which laboratory result would indicate an adverse effect from the use of this medication? 1. Hemoglobin level of 14.0 g/dL (140 mmol/L) 2. Creatinine level of 0.6 mg/dL (53 mcmol/L) 3. Blood urea nitrogen level of 25 mg/dL (8.8 mmol/L) 4. Fasting blood glucose level of 99 mg/dL (5.5 mmol/L) 735. The nurse is providing dietary instructions to a client who has been prescribed cyclosporine. Which food item should the nurse instruct the client to exclude from the diet? 1. Red meats 2. Orange juice 3. Grapefruit juice 4. Green, leafy vegetables 736. Tacrolimus is prescribed for a client who underwent a kidney transplant. Which instruction should the nurse include when teaching the client about this medication? 1. Eat at frequent intervals to avoid hypoglycemia. 2. Take the medication with a full glass of grapefruit juice. 3. Change positions carefully due to risk of orthostatic hypotension. 4. Take the oral medication every 12 hours at the same times every day. 737. The nurse is reviewing the laboratory results for a client receiving tacrolimus. Which laboratory result would indicate to the nurse that the client is experiencing an adverse effect of the medication? 1. Potassium level of 3.8 mEq/L (3.8 mmol/L) 2. Platelet count of 300,000 mm 3 (300 Â 109/L) 3. Fasting blood glucose of 200 mg/dL (11.1 mmol/L) 4. White blood cell count of 6000 mm 3 (5 to 10 Â 109/L) 738. The nurse receives a call from a client concerned about eliminating brown-colored urine after taking nitrofurantoin for a urinary tract infection. The nurse should make which appropriate response? 1. “Continue taking the medication; the brown urine occurs and is not harmful.” 2. “Take magnesium hydroxide with your medication to lighten the urine color.” 3. “Discontinue taking the medication and make an appointment for a urine culture.” 4. “Decrease your medication to half the dose, because your urine is too concentrated.” 739. A client with chronic kidney disease is receiving epoetin alfa. Which laboratory result would indicate a therapeutic effect of the medication? 1. Hematocrit of 33% (0.33) 2. Platelet count of 400,000 mm 3 (400 Â 109/L) 3. White blood cell count of 6000 mm 3 (6.0 Â 109/L) 4. Blood urea nitrogen level of 15 mg/dL (5.25 mmol/L) 740. A client with a urinary tract infection is receiving ciprofloxacin by the intravenous (IV) route. The nurse appropriately administers the medication by performing which action? 1. Infusing slowly over 60 minutes 2. Infusing in a light-protective bag 3. Infusing only through a central line 4. Infusing rapidly as a direct IV push medication 741. During the early postoperative period, a client who has undergone a cataract extraction complains of nausea and severe eye pain over the operative site. What should be the initial nursing action? 1. Call the health care provider (HCP). 2. Reassure the client that this is normal. 3. Turn the client onto his or her operative side. 4. Administer the prescribed pain medication and antiemetic. 742. The nurse is developing a teaching plan for a client with glaucoma. Which instruction should the nurse include in the plan of care? 1. Avoid overuse of the eyes. 2. Decrease the amount of salt in the diet. 3. Eye medications will need to be administered for life. 4. Decrease fluid intake to control the intraocular pressure. 743. The nurse is performing an admission assessment on a client with a diagnosis of detached retina. Which sign or symptom is associated with this eye disorder? 1. Total loss of vision 2. Pain in the affected eye 3. A yellow discoloration of the sclera 4. A sense of a curtain falling across the field of vision 744. The nurse is performing an otoscopic examination on a client with mastoiditis. On examination of the tympanic membrane, which finding should the nurse expect to observe? 1. A pink-colored tympanic membrane 2. A pearly colored tympanic membrane 3. A transparent and clear tympanic membrane 4. A red, dull, thick, and immobile tympanic membrane 745. A client is diagnosed with a disorder involving the inner ear. Which is the most common client complaint associated with a disorder involving this part of the ear? 1. Pruritus 2. Tinnitus 3. Hearing loss 4. Burning in the ear 746. The nurse is performing an assessment on a client with a suspected diagnosis of cataract. Which clinical manifestation should the nurse expect to note in the early stages of cataract formation? 1. Diplopia 2. Eye pain 3. Floating spots 4. Blurred vision 747. Aclient arrives in the emergency department followingan automobile crash. The client’s forehead hit the steering wheel and a hyphema is diagnosed. The nurse should place the client in which position? 1. Flat in bed 2. A semi-Fowler’s position 3. Lateral on the affected side 4. Lateral on the unaffected side 748. The client sustains a contusion of the eyeball following a traumatic injury with a blunt object. Which intervention should be initiated immediately? 1. Apply ice to the affected eye. 2. Irrigate the eye with cool water. 3. Notify the health care provider (HCP). 4. Accompany the client to the emergency department. 749. Aclient arrives in the emergency department with a penetrating eye injury from wood chips that occurred while cutting wood. The nurse assesses the eye and notes a piece of wood protruding from the eye. What is the initial nursing action? 876 UNIT XV Eye and Ear Disorders of the Adult Client 1. Apply an eye patch. 2. Perform visual acuity tests. 3. Irrigate the eye with sterile saline. 4. Remove the piece of wood using a sterile eye clamp. 750. The nurse is caring for a client following enucleation and notes the presence of bright red drainage on the dressing. Which action should the nurse take at this time? 1. Document the finding. 2. Continue to monitor the drainage. 3. Notify the health care provider (HCP). 4. Mark the drainage on the dressing and monitor for any increase in bleeding. 751. A woman was working in her garden. She accidentally sprayed insecticide into her right eye. She calls the emergency department, frantic and screaming for help. The nurse should instruct the woman to take which immediate action? 1. Irrigate the eyes with water. 2. Come to the emergency department. 3. Call the health care provider (HCP). 4. Irrigate the eyes with diluted hydrogen peroxide. 752. The nurse is preparing a teaching plan for a client who had a cataract extraction with intraocular implantation. Which home care measures should the nurse include in the plan? Select all that apply. 1. Avoid activities that require bending over. 2. Contact the surgeon if eye scratchiness occurs. 3. Take acetaminophen for minor eye discomfort. 4. Expect episodes of sudden severe pain in the eye. 5. Place an eye shield on the surgical eye at bedtime. 6. Contact the surgeon if a decrease in visual acuity occurs. 753. Tonometry is performed on a client with a suspected diagnosis of glaucoma. The nurse looks at the documented test results and notes an intraocular pressure (IOP) value of 23. What should be the nurse’s initial action? 1. Apply normal saline drops. 2. Note the time of day the test was done. 3. Contact the health care provider (HCP). 4. Instruct the client to sleep with the head of the bed flat. 754. The nurse is caring for a client following craniotomy for removal of an acoustic neuroma. Assessment of which cranial nerve would identify a complication specifically associated with this surgery? 1. Cranial nerve I, olfactory 2. Cranial nerve IV, trochlear 3. Cranial nerve III, oculomotor 4. Cranial nerve VII, facial nerve 755. The nurse notes that the health care provider has documented a diagnosis of presbycusis on a client’s chart. Based on this information, what action should the nurse take? 1. Speak loudly, but mumble or slur the words. 2. Speak loudly and clearly while facing the client. 3. Speak at normal tone and pitch, slowly and clearly. 4. Speak loudly and directly into the client’s affected ear. 756. A client with Meniere’s disease is experiencing severe vertigo. Which instruction should the nurse give to the client to assist in controlling the vertigo? 1. Increase sodium in the diet. 2. Avoid sudden head movements. 3. Lie still and watch the television. 4. Increase fluid intake to 3000 mL a day. 757. The nurse is preparing to test the visual acuity of a client, using a Snellen chart. Which identifies the accurate procedure for this visual acuity test? 1. The right eye is tested, followed by the left eye, and then both eyes are tested. 2. Both eyes are assessed together, followed by an assessment of the right eye and then the left eye. 3. The client is asked to stand at a distance of 40 feet (12 meters) from the chart and to read the largest line on the chart. 4. The client is asked to stand at a distance of 40 feet (12 meters) from the chart and to read the line that can be read 200 feet (60 meters) away by an individual with unimpaired vision. 758. Aclient’svision istested with a Snellen chart.Theresults of the tests are documented as 20/60. What action should the nurse implement based on this finding? 1. Provide the client with materials on legal blindness. 2. Instruct the client that he or she may need glasses when driving. 3. Inform the client of where he or she can purchase a white cane with a red tip. 4. Inform the client that it is best to sit near the back of the room when attending lectures. 759. The nurse is caring for a hearing-impaired client. Which approach will facilitate communication? 1. Speak loudly. 2. Speak frequently. 3. Speak at a normal volume. 4. Speak directly into the impaired 760. Betaxolol hydrochloride eye drops have been prescribed for a client with glaucoma. Which nursing action is most appropriate related to monitoring for side and adverse effects of this medication? 1. Assessing for edema 2. Monitoring temperature 3. Monitoring blood pressure 4. Assessing blood glucose level 761. The nurse is preparing to administer eye drops. Which interventions should the nurse take to administer the drops? Select all that apply. 1. Wash hands. 2. Put gloves on. 3. Place the drop in the conjunctival sac. 4. Pull the lower lid down against the cheekbone. 5. Instruct the client to squeeze the eyes shut after instilling the eye drop. 6. Instruct the client to tilt the head forward, open the eyes, and look down. 762. The nurse prepares a client for ear irrigation as prescribed by the health care provider. Which action should the nurse take when performing the procedure? 1. Warm the irrigating solution to 98.6 °F(37.0 °C). 2. Position the client with the affected side up following the irrigation. 3. Direct a slow, steady stream of irrigation solution toward the eardrum. 4. Assist the client to turn his or her head so that the ear to be irrigated is facing upward. 763. The nurse is providing instructions to a client who will be self-administering eye drops. To minimize systemic absorption of the eye drops, the nurse should instruct the client to take which action? 1. Eat before instilling the drops. 2. Swallow several times after instilling the drops. 3. Blink vigorously to encourage tearing after instilling the drops. 4. Occlude the nasolacrimal duct with a finger after instilling the drops. 764. A client is prescribed an eye drop and an eye ointment for the right eye. How should the nurse best administer the medications? 1. Administer the eye drop first, followed by the eye ointment. 2. Administer the eye ointment first, followed by the eye drop. 3. Administer the eye drop, wait 15 minutes, and administer the eye ointment. 4. Administer the eye ointment, wait 15 minutes, and administer the eye drop. CHAPTER 61 Eye and Ear Medications 889 Adult—Eye/Ear 765. Which medication, if prescribed for the client with glaucoma, should the nurse question? 1. Betaxolol 2. Pilocarpine 3. Erythromycin 4. Atropine sulfate 766. A miotic medication has been prescribed for the client with glaucoma and the client asks the nurse about the purpose of the medication. Which response should the nurse provide to the client? 1. “The medication will help dilate the eye to prevent pressure from occurring.” 2. “The medication will relax the muscles of the eyes and prevent blurred vision.” 3. “The medication causes the pupil to constrict and will lower the pressure in the eye.” 4. “The medication will help block the responses that are sent to the muscles in the eye.” 767. Aclient was just admitted to the hospital to rule out a gastrointestinal (GI) bleed. The client has brought several bottles of medications prescribed by different specialists. During the admission assessment, the client states, “Lately, I have been hearing some roaring sounds in my ears, especially when I am alone.” Which medication would the nurse identify as the cause of the client’s complaint? 1. Doxycycline 2. Atropine sulfate 3. Acetylsalicylic acid 4. Diltiazem hydrochloride 768. In preparation for cataract surgery, the nurse is to administer cyclopentolate eye drops at 0900 for surgery that is scheduled for 0915. What initial action should the nurse take in relation to the characteristics of the medication action? 1. Provide lubrication to the operative eye prior to giving the eye drops. 2. Call the surgeon, as this medication will further constrict the operative pupil. 3. Consult the surgeon, as there is not sufficient time for the dilative effects to occur. 4. Give the medication as prescribed; the surgeon needs optimal constriction of the pupil. 769. The nurse is assessing the motor and sensory function of an unconscious client. The nurse should use which technique to test the client’s peripheral response to pain? 1. Sternal rub 2. Nail bed pressure 3. Pressure on the orbital rim 4. Squeezing of the sternocleidomastoid muscle 770. The nurse is caring for the client with increased intracranial pressure. The nurse would note which trend in vital signs if the intracranial pressure is rising? 1. Increasing temperature, increasing pulse, increasing respirations, decreasing blood pressure 2. Increasing temperature, decreasing pulse, decreasing respirations, increasing blood pressure 3. Decreasing temperature, decreasing pulse, increasing respirations, decreasing blood pressure 4. Decreasing temperature, increasing pulse, decreasing respirations, increasing blood pressure 771. A client recovering from a head injury is participating in care. The nurse determines that the client understands measures to prevent elevations in intracranial pressure if the nurse observes the client doing which activity? 1. Blowing the nose 2. Isometric exercises 3. Coughing vigorously 4. Exhaling during repositioning 772. A client has clear fluid leaking from the nose following a basilar skull fracture. Which finding would alert the nurse that cerebrospinal fluid is present? 1. Fluid is clear and tests negative for glucose. 2. Fluid is grossly bloody in appearance and has a pH of 6. 3. Fluid clumps together on the dressing and has a pH of 7. 4. Fluid separates into concentric rings and tests positive for glucose. 773. A client with a spinal cord injury is prone to experiencing autonomic dysreflexia. The nurse should include which measures in the plan of care to minimize the risk of occurrence? Select all that apply. 1. Keeping the linens wrinkle-free under the client 2. Preventing unnecessary pressure on the lower limbs 3. Limiting bladder catheterization to once every 12 hours 4. Turning and repositioning the client at least every 2 hours 5. Ensuring that the client has a bowel movement at least once a week 774. The nurse is evaluating the neurological signs of a client in spinal shock following spinal cord 916 UNIT XVI Neurological Disorders of the Adult Client injury. Which observation indicates that spinal shock persists? 1. Hyperreflexia 2. Positive reflexes 3. Flaccid paralysis 4. Reflex emptying of the bladder 775. The nurse is caring for a client who begins to experience seizure activity while in bed. Which actions should the nurse take? Select all that apply. 1. Loosening restrictive clothing 2. Restraining the client’s limbs 3. Removing the pillow and raising padded side rails 4. Positioning the client to the side, if possible, with the head flexed forward 5. Keeping the curtain around the client and the room door open so when help arrives they can quickly enter to assist 776. The nurse is assigned to care for a client with complete right-sided hemiparesis from a stroke (brain attack). Which characteristics are associated with this condition? Select all that apply. 1. The client is aphasic. 2. The client has weakness on the right side of the body. 3. The client has complete bilateral paralysis of the arms and legs. 4. The client has weakness on the right side of the face and tongue. 5. The client has lost the ability to move the right arm but is able to walk independently. 6. The client has lost the ability to ambulate independently but is able to feed and bathe himself or herself without assistance. 777. The nurse has instructed the family of a client with stroke (brain attack) who has homonymous hemianopsia about measures to help the client overcome the deficit. Which statement suggests that the family understands the measures to use when caring for the client? 1. “We need to discourage him from wearing eyeglasses.” 2. “We need to place objects in his impaired field of vision.” 3. “We need to approach him from the impaired field of vision.” 4. “We need to remind him to turn his head to scan the lost visual field.” 778. The nurse is assessing the adaptation of a client to changes in functional status after a stroke (brain attack). Which observation indicates to the nurse that the client is adapting most successfully? 1. Gets angry with family if they interrupt a task 2. Experiences bouts of depression and irritability 3. Has difficulty with using modified feeding utensils 4. Consistently uses adaptive equipment in dressing self 779. The nurse is teaching a client with myasthenia gravis about the prevention of myasthenic and cholinergic crises. Which client activity suggests that teaching is most effective? 1. Taking medications as scheduled 2. Eating large, well-balanced meals 3. Doing muscle-strengthening exercises 4. Doing all chores early in the day while less fatigued 780. The nurse is instructing a client with Parkinson’s disease about preventing falls. Which client statement reflects a need for further teachin g? 1. “I can sit down to put on my pants and shoes.” 2. “I try to exercise every dayand rest when I’m tired.” 3. “My son removed all loose rugs from my bedroom.” 4. “I don’t need to use my walker to get to the bathroom.” 781. The nurse has given suggestions to a client with trigeminal neuralgia about strategies to minimize episodes of pain. The nurse determines that the client needs further teaching if the client makes which statement? 1. “I will wash my face with cotton pads.” 2. “I’ll have to start chewing on my unaffected side.” 3. “I should rinse my mouth if toothbrushing is painful.” 4. “I’ll try to eat my food either very warm or very cold.” 782. The client is admitted to the hospital with a diagnosis of Guillain-Barre syndrome. Which past medical history finding makes the client most at risk for this disease? 1. Meningitis or encephalitis during the last 5 years 2. Seizures or trauma to the brain within the last year 3. Back injury or trauma to the spinal cord during the last 2 years 4. Respiratory or gastrointestinal infection during the previous month 783. A client with Guillain-Barre syndrome has ascending paralysis and is intubated and receiving mechanical ventilation. Which strategy should the nurse incorporate in the plan of care to help the client cope with this illness? Adult—Neurological CHAPTER 62 Neurological System 917 1. Giving client full control over care decisions and restricting visitors 2. Providing positive feedback and encouraging active range of motion 3. Providing information, giving positive feedback, and encouraging relaxation 4. Providing intravenously administered sedatives, reducing distractions, and limiting visitors 784. A client has a neurological deficit involving the limbic system. On assessment, which finding is specific to this type of deficit? 1. Is disoriented to person, place, and time 2. Affect is flat, with periods of emotional lability 3. Cannot recall what was eaten for breakfast today 4. Demonstrates inability to add and subtract; does not know who is the president of the United States 785. The nurse is instituting seizure precautions for a client who is being admitted from the emergency department. Which measures should the nurse include in planning for the client’s safety? Select all that apply. 1. Padding the side rails of the bed 2. Placing an airway at the bedside 3. Placing the bed in the high position 4. Putting a padded tongue blade at the head of the bed 5. Placing oxygen and suction equipment at the bedside 6. Flushing the intravenous catheter to ensure that the site is patent 786. The nurse is evaluating the status of a client who had a craniotomy 3 days ago. Which assessment finding would indicate that the client is developing meningitis as a complication of surgery? 1. A negative Kernig’s sign 2. Absence of nuchal rigidity 3. A positive Brudzinski’s sign 4. A Glasgow Coma Scale score of 15 787. The nurse has completed discharge instructions for a client with application of a halo device. Which statement indicates that the client needs further clarification of the instructions? 1. “I will use a straw for drinking.” 2. “I will drive only during the daytime.” 3. “I will be careful because the device alters balance.” 4. I will wash the skin daily under the lamb’s wool liner of the vest.” 788. The nurse is admitting a client with Guillain-Barre syndrome to the nursing unit. The client has ascending paralysis to the level of the waist. Knowing the complications of the disorder, the nurse should bring which most essential items into the client’s room? 1. Nebulizer and pulse oximeter 2. Blood pressure cuff and flashlight 3. Flashlight and incentive spirometer 4. Electrocardiographic monitoring electrodes and intubation tray 789. Carbidopa-levodopa is prescribed for a client with Parkinson’s disease. The nurse monitors the client for side and adverse effects of the medication. Which finding indicates that the client is experiencing an adverse effect? 1. Pruritus 2. Tachycardia 3. Hypertension 4. Impaired voluntary movements 790. The home health nurse visits a client who is taking phenytoin for control of seizures. During the assessment, the nurse notes that the client is taking birth control pills. Which information should the nurse include in the teaching plan? 1. Pregnancy must be avoided while taking phenytoin. 2. The client may stop the medication if it is causing severe gastrointestinal effects. 3. There is the potential of decreased effectiveness of birth control pills while taking phenytoin. 4. There is the increased risk of thrombophlebitis while taking phenytoin and birth control pills together. 791. The nurse is caring for a client in the emergency department who has been diagnosed with Bell’s palsy. The client has been taking acetaminophen, and acetaminophen overdose is suspected. Which antidote should the nurse prepare for administration if prescribed? 1. Pentostatin 2. Auranofin 3. Fludarabine 4. Acetylcysteine 792. Meperidine has been prescribed for a client to treat pain. Which side and adverse effects should the nurse monitor for? Select all that apply. 1. Diarrhea 2. Tremors 3. Drowsiness 4. Hypotension 5. Urinary frequency 6. Increased respiratory rate 793. A client is taking the prescribed dose of phenytoin to control seizures. Results of a phenytoin blood level study reveal a level of 35 mcg/mL (140 mcmol/L). Which finding would be expected as a result of this laboratory result? 1. Hypotension 2. Tachycardia 3. Slurred speech 4. No abnormal finding 794. The client arrives at the emergency department complaining of back spasms. The client states, “I have been taking 2 to 3 aspirin every 4 hours for the last week, and it hasn’t helped my back.” Since acetylsalicylic acid intoxication is suspected, the nurse should assess the client for which manifestation? 1. Tinnitus 2. Diarrhea 3. Constipation 4. Photosensitivity 795. A client with trigeminal neuralgia is being treated with carbamazepine, 400 mg orally daily. Which value indicates that the client is experiencing an adverse effect to the medication? 1. Sodium level, 140 mEq/L (140 mmol/L) 2. Uric acid level, 4.0 mg/dL (0.24 mmol/L) 3. White blood cell count, 3000 mm 3 (3.0 Â 109/L) 4. Blood urea nitrogen level, 10 mg/dL (3.6 mmol/L) 796. The nurse is caring for a client with chronic back pain. Codeine has been prescribed for the client. Specific to this medication, which intervention should the nurse include in the plan of care while the client is taking this medication? 1. Monitor radial pulse. 2. Monitor bowel activity. 3. Monitor apical heart rate. 4. Monitor peripheral pulses. 797. The nurse has given medication instructions to a client receiving phenytoin. Which statement indicates that the client has an adequate understanding of the instructions? 1. “Alcohol is not contraindicated while taking this medication.” 2. “Good oral hygiene is needed, including brushing and flossing.” 3. “The medication dose may be self-adjusted, depending on side effects.” 4. “The morning dose of the medication should be taken before a serum medication level is drawn.” 932 UNIT XVI Neurological Disorders of the Adult Client 798. A client with myasthenia gravis has become increasingly weaker. The health care provider prepares to identify whether the client is reacting to an overdose of the medication (cholinergic crisis) or an increasing severity of the disease (myasthenic crisis). An injection of edrophonium is administered. Which finding would indicate that the client is in cholinergic crisis? 1. No change in the condition 2. Complaints of muscle spasms 3. An improvement of the weakness 4. A temporary worsening of the condition 799. A client with trigeminal neuralgia tells the nurse that acetaminophen is taken daily for the relief of generalized discomfort. Which laboratory value would indicate toxicity associated with the medication? 1. Sodium level of 140 mEq/L (140 mmol/L) 2. Platelet count of 400,000 mm 3 (400 Â 109/L) 3. Prothrombin time of 12 seconds (12 seconds) 4. Direct bilirubin level of 2 mg/dL (34 mcmol/L) 800. The nurse is conducting health screening for osteoporosis. Which client is at greatest risk of developing this disorder? 1. A 25-year-old woman who runs 2. A 36-year-old man who has asthma 3. A70-year-old man who consumes excess alcohol 4. A sedentary 65-year-old woman who smokes cigarettes 801. The nurse has given instructions to a client returning home after knee arthroscopy. Which statement by the client indicates that the instructions are understood? 1. “I can resume regular exercise tomorrow.” 2. “I can’t eat food for the remainder of the day.” 3. “I need to stay off the leg entirely for the rest of the day.” 4. “I need to report a fever or swelling to my health care provider.” 802. The nurse witnessed a vehicle hit a pedestrian. The victim is dazed and tries to get up. Aleg appears fractured. Which intervention should the nurse take? 1. Try to reduce the fracture manually. 2. Assist the victim to get up and walk to the sidewalk. 3. Leave the victim for a few moments to call an ambulance. 4. Stay with the victim and encourage him or her to remain still. 803. Which cast care instructions should the nurse provide to a client who just had a plaster cast applied to the right forearm? Select all that apply. 1. Keep the cast clean and dry. 2. Allow the cast 24 to 72 hours to dry. 3. Keep the cast and extremity elevated. 4. Expect tingling and numbness in the extremity. 5. Use a hair dryer set on a warm to hot setting to dry the cast. 6. Use a soft, padded object that will fit under the cast to scratch the skin under the cast. 804. The nurse is evaluating a client in skeletal traction. When evaluating the pin sites, the nurse would be most concerned with which finding? 1. Redness around the pin sites 2. Pain on palpation at the pin sites 3. Thick, yellow drainage from the pin sites 4. Clear, watery drainage from the pin sites 805. The nurse is assessing the casted extremity of a client. Which sign is indicative of infection? 1. Dependent edema 2. Diminished distal pulse 3. Presence of a “hot spot” on the cast 4. Coolness and pallor of the extremity 806. A client has sustained a closed fracture and has just had a cast applied to the affected arm. The client is complaining of intense pain. The nurse elevates the limb, applies an ice bag, and administers an analgesic, with little relief. Which problem may be causing this pain? 952 UNIT XVII Musculoskeletal Disorders of the Adult Client Adult—Musculoskeletal 1. Infection under the cast 2. The anxiety of the client 3. Impaired tissue perfusion 4. The recent occurrence of the fracture 807. The nurse is admitting a client with multiple trauma injuries to the nursing unit. The client has a leg fracture and had a plaster cast applied. Which position would be best for the casted leg? 1. Elevated for 3 hours, then flat for 1 hour 2. Flat for 3 hours, then elevated for 1 hour 3. Flat for 12 hours, then elevated for 12 hours 4. Elevated on pillows continuously for 24 to 48 hours 808. A client is being discharged to home after application of a plaster leg cast. Which statement indicates that the client understands proper care of the cast? 1. “I need to avoid getting the cast wet.” 2. “I need to cover the casted leg with warm blankets.” 3. “I need to use my fingertips to lift and move my leg.” 4. “I need to use something like a padded coat hanger end to scratch under the cast if it itches.” 809. A client being measured for crutches asks the nurse why the crutches cannot rest up underneath the arm for extra support. The nurse responds knowing that which would most likely result from this improper crutch measurement? 1. A fall and further injury 2. Injury to the brachial plexus nerves 3. Skin breakdown in the area of the axilla 4. Impaired range of motion while the client ambulates 810. The nurse has given the client instructions about crutch safety. Which statement indicates that the client understands the instructions? Select all that apply. 1. “I should not use someone else’s crutches.” 2. “I need to remove any scatter rugs at home.” 3. “I can use crutch tips even when they are wet.” 4. “I need to have spare crutches and tips available.” 5. “When I’m using the crutches, my arms need to be completely straight.” 811. The nurse is caring for a client being treated for fat embolus after multiple fractures. Which data would the nurse evaluate as the most favorable indication of resolution of the fat embolus? 1. Clear mentation 2. Minimal dyspnea 3. Oxygen saturation of 85% 4. Arterial oxygen level of 78 mm Hg (10.3 kPa) 812. The nurse has conducted teaching with a client in an arm cast about the signs and symptoms of compartment syndrome. The nurse determines that the client understands the information if the client states that he or she should report which early symptom of compartment syndrome? 1. Cold, bluish-colored fingers 2. Numbness and tingling in the fingers 3. Pain that increases when the arm is dependent 4. Pain that is out of proportion to the severity of the fracture 813. A client with diabetes mellitus has had a right below-knee amputation. Given the client’s history of diabetes mellitus, which complication is the client at most risk for after surgery? 1. Hemorrhage 2. Edema of the residual limb 3. Slight redness of the incision 4. Separation of the wound edges 814. The nurse is caring for a client who had an aboveknee amputation 2 days ago. The residual limb was wrapped with an elastic compression bandage, which has come off. Which immediate action should the nurse take? 1. Apply ice to the site. 2. Call the health care provider (HCP). 3. Rewrap the residual limb with an elastic compression bandage. 4. Apply a dry, sterile dressing and elevate the residual limb on 1 pillow. 815. A client is complaining of low back pain that radiates down the left posterior thigh. The nurse should ask the client if the pain is worsened or aggravated by which factor? 1. Bed rest 2. Ibuprofen 3. Bending or lifting 4. Application of heat 816. The nurse is caring for a client who has had spinal fusion, with insertion of hardware. The nurse would be most concerned with which assessment finding? 1. Temperature of 101.6°F (38.7°C) orally 2. Complaints of discomfort during repositioning 3. Old bloody drainage outlined on the surgical dressing 4. Discomfort during coughing and deepbreathing exercises 817. The nurse is caring for a client with a diagnosis of gout. Which laboratory value would the nurse expect to note in the client? 1. Calcium level of 9.0 mg/dL (2.25 mmol/L) 2. Uric acid level of 9.0 mg/dL (0.54 mmol/L) CHAPTER 64 Musculoskeletal System 953 Adult—Musculoskeletal 3. Potassium level of 4.1 mEq/L (4.1 mmol/L) 4. Phosphorus level of 3.1 mg/dL (1.0 mmol/L) 818. A client with a hip fracture asks the nurse about Buck’s (extension) traction that is being applied before surgery and what is involved. The nurse should provide which information to the client? 1. Allows bony healing to begin before surgery and involves pins and screws 2. Provides rigid immobilization of the fracture site and involves pulleys and wheels 3. Lengthens the fractured leg to prevent severing of blood vessels and involves pins and screws 4. Provides comfort by reducing muscle spasms, provides fracture immobilization, and involves pulleys and wheels 819. A client has been on treatment for rheumatoid arthritis for 3 weeks. During the administration of etanercept, which is most important for the nurse to assess? 1. The injection site for itching and edema 2. The white blood cell counts and platelet counts 3. Whether the client is experiencing fatigue and joint pain 4. Whether the client is experiencing a metallic taste in the mouth, and a loss of appetite 820. Allopurinol is prescribed for a client and the nurse provides medication instructions to the client. Which instruction should the nurse provide? 1. Drink 3000 mL of fluid a day. 2. Take the medication on an empty stomach. 3. The effect of the medication will occur immediately. 4. Any swelling of the lips is a normal expected response. 821. Colchicine is prescribed for a client with a diagnosis of gout. The nurse reviews the client’s record, knowing that this medication would be used with caution in which disorder? 1. Myxedema 2. Kidney disease 3. Hypothyroidism 4. Diabetes mellitus 822. Alendronate is prescribed for a client with osteoporosis and the nurse is providing instructions on administration of the medication. Which instruction should the nurse provide? 1. Take the medication at bedtime. 2. Take the medication in the morning with breakfast. 3. Lie down for 30 minutes after taking the medication. 4. Take the medication with a full glass of water after rising in the morning. 823. The nurse is preparing discharge instructions for a client receiving baclofen. Which instruction should be included in the teaching plan? 1. Restrict fluid intake. 2. Avoid the use of alcohol. 3. Stop the medication if diarrhea occurs. 4. Notify the health care provider (HCP) if fatigue occurs. 824. The nurse is analyzing the laboratory studies on a client receiving dantrolene. Which laboratory test would identify an adverse effect associated with the administration of this medication? 1. Platelet count 2. Creatinine level 962 UNIT XVII Musculoskeletal Disorders of the Adult Client 3. Liver function tests 4. Blood urea nitrogen level 825. Cyclobenzaprine is prescribed for a client for muscle spasms and the nurse is reviewing the client’s record. Which disorder, if noted in the record, would indicate a need to contact the health care provider about the administration of this medication? 1. Glaucoma 2. Emphysema 3. Hypothyroidism 4. Diabetes mellitus 826. In monitoring a client’s response to diseasemodifying antirheumatic drugs (DMARDs), which assessment findings would the nurse consider acceptable responses? Select all that apply. 1. Control of symptoms during periods of emotional stress 2. Normal white blood cell, platelet, and neutrophil counts 3. Radiological findings that show no progression of joint degeneration 4. An increased range of motion in the affected joints 3 months into therapy 5. Inflammation and irritation at the injection site 3 days after the injection is given 6. A low-grade temperature on rising in the morning that remains throughout the day 827. The nurse is administering an intravenous dose of methocarbamol to a client with multiple sclerosis. For which adverse effect should the nurse monitor? 1. Tachycardia 2. Rapid pulse 3. Bradycardia 4. Hypertension 828. The nurse prepares to give a bath and change the bed linens of a client with cutaneous Kaposi’s sarcoma lesions. The lesions are open and draining a scant amount of serous fluid. Which would the nurse incorporate into the plan during the bathing of this client? 1. Wearing gloves 2. Wearing a gown and gloves 3. Wearing a gown, gloves, and a mask 4. Wearing a gown and gloves to change the bed linens, and gloves only for the bath 829. The nurse provides home care instructions to a client with systemic lupus erythematosus and tells the client about methods to manage fatigue. Which statement by the client indicates a need for further instruction? 1. “Ishould take hot baths because theyare relaxing.” 2. “I should sit whenever possible to conserve my energy.” 3. “I should avoid long periods of rest because it causes joint stiffness.” 4. “I should do some exercises, such as walking, when I am not fatigued.” 830. A client develops an anaphylactic reaction after receiving morphine. The nurse should plan to institute which actions? Select all that apply. 1. Administer oxygen. 2. Quickly assess the client’s respiratory status. 3. Document the event, interventions, and client’s response. 4. Leave the client briefly to contact a health care provider (HCP). 5. Keep the client supine regardless of the blood pressure readings. 6. Start an intravenous (IV) infusion of D5W and administer a 500-mL bolus. 831. The nurse is conducting a teaching session with a client on their diagnosis of pemphigus. Which statement by the client indicates that the client understands the diagnosis? 1. “My skin will have tiny red vesicles.” 2. “The presence of the skin vesicles is caused by a virus.” 3. “I have an autoimmune disease that causes blistering in the epidermis.” 4. “The presence of red, raised papules and large plaques covered by silvery scales will be present on my skin.” 832. The nurse is assisting in planning care for a client with a diagnosis of immunodeficiency and should incorporate which action as a priority in the plan? 1. Protecting the client from infection 2. Providing emotional support to decrease fear 3. Encouraging discussion about lifestyle changes 4. Identifying factors that decreased the immune function 833. Aclient calls the nurse in the emergency department and states that he was just stung by a bumblebee while gardening. The client is afraid of a severe reaction because the client’s neighbor experienced such a reaction just 1 week ago. Which action should the nurse take? 1. Advise the client to soak the site in hydrogen peroxide. CHAPTER 66 Immune Disorders 975 Adult—Immune 2. Ask the client if he ever sustained a bee sting in the past. 3. Tell the client to call an ambulance for transport to the emergency department. 4. Tell the client not to worry about the sting unless difficulty with breathing occurs. 834. The community health nurse is conducting a research study and is identifying clients in the community at risk for latex allergy. Which client population is most at risk for developing this type of allergy? 1. Hairdressers 2. The homeless 3. Children in day care centers 4. Individuals living in a group home 835. Which interventions apply in the care of a client at high risk for an allergic response to a latex allergy? Select all that apply. 1. Use nonlatex gloves. 2. Use medications from glass ampules. 3. Place the client in a private room only. 4. Keep a latex-safe supply cart available in the client’s area. 5. Avoid the use of medication vials that have rubber stoppers. 6. Use a blood pressure cuff from an electronic device only to measure the blood pressure. 836. A client presents at the health care provider’s office with complaints of a ring-like rash on his upper leg. Which question should the nurse ask first? 1. “Do you have any cats in your home?” 2. “Have you been camping in the last month?” 3. “Have you or close contacts had any flu-like symptoms within the last few weeks?” 4. “Have you been in physical contact with anyone who has the same type of rash?” 837. Aclient is diagnosed with scleroderma. Which intervention should the nurse anticipate to be prescribed? 1. Maintain bed rest as much as possible. 2. Administer corticosteroids as prescribed for inflammation. 3. Advise the client to remain supine for 1 to 2 hours after meals. 4. Keep the room temperature warm during the day and cool at night. 838. Aclient arrives at the health care clinic and tells the nurse that she was just bitten by a tick and would like to be tested for Lyme disease. The client tells the nurse that she removed the tick and flushed it down the toilet. Which actions are most appropriate? Select all that apply. 1. Tell the client that testing is not necessary unless arthralgia develops. 2. Tell the client to avoid any woody, grassy areas that may contain ticks. 3. Instruct the client to immediately start to take the antibiotics that are prescribed. 4. Inform the client to plan to have a blood test 4 to 6 weeks after a bite to detect the presence of the disease. 5. Tell the client that if this happens again, to never remove the tick but vigorously scrub the area with an antiseptic. 839. The nurse is preparing a group of Cub Scouts for an overnight camping trip and instructs the Scouts about the methods to prevent Lyme disease. Which statement by one of the Scouts indicates a need for further instruction? 1. “I need to bring a hat to wear during the trip.” 2. “I should wear long-sleeved tops and long pants.” 3. “I should not use insect repellents because it will attract the ticks.” 4. “I need to wear closed shoes and socks that can be pulled up over my pants.” 840. The client with acquired immunodeficiency syndrome isdiagnosed with cutaneousKaposi’ssarcoma. Based on this diagnosis, the nurse understands that this has been confirmed by which finding? 1. Swelling in the genital area 2. Swelling in the lower extremities 3. Positive punch biopsy of the cutaneous lesions 4. Appearance of reddish-blue lesions noted on the skin 841. The nurse is conducting allergy skin testing on a client. Which postprocedure interventions are most appropriate? Select all that apply. 1. Record site, date, and time of the test. 2. Give the client a list of potential allergens if identified. 3. Estimate the size of the wheal and document the finding. 4. Tell the client to return to have the site inspected only if there is a reaction. 5. Have the client wait in the waiting room for at least 1 to 2 hours after injection. 842. The nurse isperformingan assessment on a client who has been diagnosed with an allergy to latex. In determining the client’s risk factors, the nurse should question the client about an allergy to which food item? 1. Eggs 2. Milk 3. Yogurt 4. Bananas 843. The client with acquired immunodeficiency syndrome and Pneumocystis jiroveci infection has been receiving pentamidine. The client develops a temperature of 101 °F (38.3 °C). The nurse continues to assess the client, knowing that this sign most likely indicates which condition? 1. That the dose of the medication is too low 2. That the client is experiencing toxic effects of the medication 3. That the client has developed inadequacy of thermoregulation 4. That the client has developed another infection caused by leukopenic effects of the medication 844. The nurse caring for a client who is taking an aminoglycoside should monitor the client for which adverse effects of the medication? Select all that apply. 1. Seizures 2. Ototoxicity 3. Renal toxicity 4. Dysrhythmias 5. Hepatotoxicity 845. Ketoconazole is prescribed for a client with a diagnosis of candidiasis. Which interventions should the nurse include when administering this medication? Select all that apply. 1. Restrict fluid intake. 2. Monitor liver function studies. 3. Instruct the client to avoid alcohol. 4. Administer the medication with an antacid. 5. Instruct the client to avoid exposure to the sun. 6. Administer the medication on an empty stomach. 846. The nurse is caring for a client who has been taking a sulfonamide and should monitor for signs and symptoms of which adverse effects of the medication? Select all that apply. 1. Ototoxicity 2. Palpitations 3. Nephrotoxicity 4. Bone marrow suppression 5. Gastrointestinal (GI) effects 6. Increased white blood cell (WBC) count 847. The nurse is reviewingthe results ofserum laboratory studies drawn on a client with acquired immunodeficiency syndrome who is receiving didanosine. The nurse interprets that the client may have the medication discontinued by the health care provider if which elevated result is noted? 1. Serum protein level 2. Blood glucose level 3. Serum amylase level 4. Serum creatinine level 848. The nurse is caring for a postrenal transplantation client taking cyclosporine. The nurse notes an increase in one of the client’s vital signs and the client is complaining of a headache. What vital sign is most likely increased? 1. Pulse 2. Respirations 3. Blood pressure 4. Pulse oximetry 849. Amikacin isprescribed fora client with a bacterialinfection. The nurse instructs the client to contact the health care provider (HCP) immediately if which occurs? 1. Nausea 2. Lethargy 3. Hearing loss 4. Muscle aches Adult—Immune TABLE 67-1 Antibiotics and Their Adverse Effects—cont’d Classification Adverse Effects Tetracyclines Gastrointestinal effects Hepatotoxicity Teeth (staining) and bone damage Superinfections Dermatological reactions, including rash and photosensitivity Hypersensitivity reactions Antimycobacterials, leprostatics Gastrointestinal effects Neuritis, dizziness, headache, malaise, drowsiness, hallucinations Antifungals Gastrointestinal effects Headache, rash, anemia, hepatotoxicity Hearing loss, peripheral neuritis 984 UNIT XVIII Immune Disorders of the Adult Client Adult—Immune 850. The nurse is assigned to care for a client with cytomegalovirus retinitis and acquired immunodeficiency syndrome who is receiving foscarnet, an antiviral medication. The nurse should monitor the results of which laboratory study while the client is taking this medication? 1. CD4+ T cell count 2. Lymphocyte count 3. Serum albumin level 4. Serum creatinine level 851. A client who is human immunodeficiency virus seropositive has been taking stavudine. The nurse should monitor which most closely while the client is taking this medication? 1. Gait 2. Appetite 3. Level of consciousness 4. Gastrointestinal function 869. A client says to the nurse, “The federal guards were sent to kill me.” Which is the best response by the nurse to the client’s concern? 1. “I don’t believe this is true.” 2. “The guards are not out to kill you.” 3. “Do you feel afraid that people are trying to hurt you?” 4. “What makes you think the guards were sent to hurt you?” 870. A client diagnosed with delirium becomes disoriented and confused at night. Which intervention should the nurse implement initially? 1. Move the client next to the nurses’ station. 2. Use an indirect light source and turn off the television. 3. Keep the television and a soft light on during the night. 4. Play soft music during the night, and maintain a well-lit room. 871. Aclient is admitted to the mental health unit with a diagnosis of depression. The nurse should develop a plan of care for the client that includes which intervention? 1. Encouraging quiet reading and writing for the first few days 2. Identification of physical activities that will provide exercise 3. No socializing activities, until the client asks to participate in milieu 4. A structured program of activities in which the client can participate 872. When planning the discharge of a client with chronic anxiety, the nurse directs the goals at promoting a safe environment at home. Which is the most appropriate maintenance goal? 1. Suppressing feelings of anxiety 2. Identifying anxiety-producing situations 3. Continuing contact with a crisis counselor 4. Eliminating all anxiety from daily situations 873. Aclient is unwilling to go to his church because his ex-girlfriend goes there and he feels that she will laugh at him if she sees him. Because of this hypersensitivity to a reaction from her, the client remains homebound. The home care nurse develops a plan of care that addresses which personality disorder? 1. Avoidant 2. Borderline 3. Schizotypal 4. Obsessive-compulsive 874. The nurse is conducting a group therapy session. During the session, a client diagnosed with mania CRITICAL THINKING What Should You Do? Answer: If a client is actively hallucinating, the nurse should intervene with one-on-one contact. The nurse should ask the client directly about the hallucination and avoid reacting to the hallucination as if it were real. The nurse should decrease stimuli or move the client to another area and avoid indicating to the client that others also are experiencing the hallucination. The nurse should encourage the client to express feelings, focus on reality-based topics, and respond verbally to anything real that the client talks about. The nurse also should avoid touching the client. During a hallucination, the nurse should attempt to engage the client’s attention through a concrete activity and monitor for signs of increasing anxiety or agitation, which may indicate that the hallucinations are increasing. Reference: Varcarolis (2013), pp. 312, 318. 1014 UNIT XIX Mental Health Disorders of the Adult Client Mental Health consistently disrupts the group’s interactions. Which intervention should the nurse initially implement? 1. Setting limits on the client’s behavior 2. Asking the client to leave the group session 3. Asking another nurse to escort the client out of the group session 4. Telling the client that they will not be able to attend any future group sessions 875. Aclient is admitted to a medical nursing unit with a diagnosis of acute blindness after being involved in a hit-and-run accident. When diagnostic testing cannot identify any organic reason why this client cannot see, a mental health consult is prescribed. The nurse plans care based on which condition that should be the focus of this consult? 1. Psychosis 2. Repression 3. Conversion disorder 4. Dissociative disorder 876. A manic client begins to make sexual advances toward visitors in the dayroom. When the nurse firmly states that this is inappropriate and will not be allowed, the client becomes verbally abusive and threatens physical violence to the nurse. Based on the analysis of this situation, which intervention should the nurse implement? 1. Place the client in seclusion for 30 minutes. 2. Tell the client that the behavior is inappropriate. 3. Escort the client to their room, with the assistance of other staff. 4. Tell the client that their telephone privileges are revoked for 24 hours. 877. Which nursing interventions are appropriate for a hospitalized client with mania who is exhibiting manipulative behavior? Select all that apply. 1. Communicate expected behaviors to the client. 2. Ensure that the client knows that they are not in charge of the nursing unit. 3. Assist the client in identifying ways of setting limits on personal behaviors. 4. Follow through about the consequences of behavior in a nonpunitive manner. 5. Enforce rules by informing the client that he/she will not be allowed to attend therapy groups. 6. Have the client state the consequences for behaving in ways that are viewed as unacceptable. 878. The nurse observes that a client is pacing, agitated, and presenting aggressive gestures. The client’s speech pattern is rapid, and affect is belligerent. Based on these observations, which is the nurse’s immediate priority of care? 1. Provide safety for the client and other clients on the unit. 2. Provide the clients on the unit with a sense of comfort and safety. 3. Assist the staff in caring for the client in a controlled environment. 4. Offer the client a less stimulating area in which to calm down and gain control. 879. The nurse is preparing a client with a history of command hallucinations for discharge by providing instructions on interventions for m anaging hallucinations and anxiety. Which statement in response to these instructions suggests to the nurse that the client has a n eed for additional information? 1. “My medications will help my anxious feelings.” 2. “I’ll go to support group and talk about what I am feeling.” 3. “I need to get enough sleep and eat well to help prevent feeling anxious.” 4. “When I have command hallucinations, I’ll call a friend and ask him what I should do.” 880. The nurse is caring for a client just admitted to the mental health unit and diagnosed with catatonic stupor. The client is lying on the bed in a fetal position. Which is the most appropriate nursing intervention? 1. Ask direct questions to encourage talking. 2. Leave the client alone so as to minimize external stimuli. 3. Sit beside the client in silence with occasional open-ended questions. 4. Take the client into the dayroom with other clients so that they can help watch them. 881. The nurse is caring for a client diagnosed with paranoid personality disorder who is experiencing disturbed thought processes. In formulating a nursing plan of care, which best intervention should the nurse include? 1. Increase socialization of the client with peers. 2. Avoid using a whisper voice in front of the client. 3. Begin to educate the client about social supports in the community. 4. Have the client sign a release of information to appropriate parties for assessment purposes. 882. The nurse is planning activities for a client diagnosed with bipolar disorder with aggressive social behavior. Which activity would be most appropriate for this client? 1. Chess 2. Writing 3. Ping pong 893. The nurse observes that a client with a potential for violence is agitated, pacing up and down the hallway, and is making aggressive and belligerent gestures at other clients. Which statement would be most appropriate to make to this client? 1. “You need to stop that behavior now.” 2. “You will need to be placed in seclusion.” 3. “You seem restless; tell me what is happening.” 4. “You will need to be restrained if you do not change your behavior.” 894. The nurse is reviewing the assessment data of a client admitted to the mental health unit. The nurse notes that the admission nurse documented that the client is experiencing anxiety as a result of a situational crisis. The nurse plans care for the client, determining that this type of crisis could be caused by which event? 1. Witnessing a murder 2. The death of a loved one 3. A fire that destroyed the client’s home 4. A recent rape episode experienced by the client 895. The nurse is conducting an initial assessment of a client in crisis. When assessing the client’s perception of the precipitating event that led to the crisis, which is the most appropriate question? 1. “With whom do you live?” 2. “Who is available to help you?” Mental Health CRITICAL THINKING What Should You Do? Answer: The nurse should first take the victim to a quiet and private room and assess the victim’s stress level before performing treatments and procedures. The nurse needs to stay with the victim. The victim should not shower, bathe, douche (female), or change clothing until an examination is performed. The nurse should obtain consent for an examination, photographs, laboratory tests, release of information, and laboratory samples. The nurse should assist with the female pelvic examination (the pelvic examination may trigger a flashback of the attack). A shower and fresh clothing should be made available to the client after the examination. Any evidence needs to be preserved and physical injuries need to be treated. The nurse should provide for client safety, document all events in the care of the victim, and reinforce to the victim that surviving the assault is most important; if the victim survived the rape, she did exactly what was necessary to stay alive. When appropriate, the nurse should refer the victim to crisis intervention and support groups. Reference: Varcarolis (2013), pp. 439–440. 1038 UNIT XIX Mental Health Disorders of the Adult Client 3. “What leads you to seek help now?” 4. “What do you usually do to feel better?” 896. The nurse is creating a plan of care for a client in a crisis state. When developing the plan, the nurse should consider which factor? 1. A crisis state indicates that the client has a mental illness. 2. Acrisis state indicates that the client has an emotional illness. 3. Presenting symptoms in a crisis situation are similar for all clients experiencing a crisis. 4. A client’s response to a crisis is individualized and what constitutes a crisis for one client may not constitute a crisis for another client. 897. The nurse in the emergency department is caring for a young female victim of sexual assault. The client’s physical assessment is complete, and physical evidence has been collected. The nurse notes that the client is withdrawn, confused, and at times physically immobile. How should the nurse interpret these behaviors? 1. Signs of depression 2. Reactions to a devastating event 3. Evidence that the client is a high suicide risk 4. Indicative of the need for hospital admission 898. A depressed client on an inpatient unit says to the nurse, “My family would be better off without me.” Which is the nurse’s best response? 1. “Have you talked to your family about this?” 2. “Everyone feels this waywhen theyare depressed.” 3. “You will feel better once your medication begins to work.” 4. “You sound very upset. Are you thinking of hurting yourself?” 899. The nurse has been closely observing a client who has been displaying aggressive behaviors. The nurse observes that the behavior displayed by the client is escalating. Which nursing intervention is most helpful to this client at this time? Select all that apply. 1. Initiate confinement measures. 2. Acknowledge the client’s behavior. 3. Assist the client to an area that is quiet. 4. Maintain a safe distance from the client. 5. Allow the client to take control ofthe situation. 900. Which behavior observed by the nurse indicates a suspicion that a depressed adolescent client may be suicidal? 1. The adolescent gives away a DVD and a cherished autographed picture of a performer. 2. The adolescent runs out of the therapy group, swearing at the group leader, and to her room. 3. The adolescent becomes angry while speaking on the telephone and slams down the receiver. 4. The adolescent gets angry with her roommate when the roommate borrows the client’s clothes without asking. 901. The police arrive at the emergency department with a client who has lacerated both wrists. Which is the initial nursing action? 1. Administer an antianxiety agent. 2. Assess and treat the wound sites. 3. Secure and record a detailed history. 4. Encourage and assist the client to ventilate feelings. 902. A moderately depressed client who was hospitalized 2 days ago suddenly begins smiling and reporting that the crisis is over. The client says to the nurse, “I’m finally cured.” How should the nurse interpret this behavior as a cue to modify the treatment plan? 1. Suggesting a reduction of medication 2. Allowing increased “in-room” activities 3. Increasing the level of suicide precautions 4. Allowing the client off-unit privileges as needed 903. The nurse is planning care for a client being admitted to the nursing unit who attempted suicide. Which priority nursing intervention should the nurse include in the plan of care? 1. One-to-one suicide precautions 2. Suicide precautions with 30-minute checks 3. Checking the whereabouts of the client every 15 minutes 4. Asking the client to report suicidal thoughts immediately 904. The emergency department nurse is caring for an adult client who is a victim of family violence. Which priority instruction should be included in the discharge instructions? 1. Information regarding shelters 2. Instructions regarding calling the police 3. Instructions regarding self-defense classes 4. Explaining the importance of leaving the violent situation 905. A female victim of a sexual assault is being seen in the crisis center. The client states that she still feels “as though the rape just happened yesterday,” even though it has been a few months since the incident. Which is the most appropriate nursing response? 1. “You need to try to be realistic. The rape did not just occur.” Mental Health CHAPTER 71 Crisis Theory and Intervention 1039 Mental Health 2. “It will take some time to get over these feelings about your rape.” 3. “Tell me more about the incident that causes you to feel like the rape just occurred.” 4. “What do you think that you can do to alleviate some of your fears about being raped again?” 906. A client is admitted to the mental health unit after an attempted suicide by hanging. The nurse can best ensure client safety by which action? 1. Requesting that a peer remain with the client at all times 2. Removing the client’s clothing and placing the client in a hospital gown 3. Assigning to the client a staff member who will remain with the client at all times 4. Admitting the client to a seclusion room where all potentially dangerous articles are removed 907. A client is admitted with a recent history of severe anxiety following a home invasion and robbery. During the initial assessment interview, which statement by the client should indicate to the nurse the possible diagnosis of posttraumatic stress disorder? Select all that apply. 1. “I’m afraid of spiders.” 2. “I keep reliving the robbery.” 3. “I see his face everywhere I go.” 4. “I don’t want anything to eat now.” 5. “I might have died over a few dollars in my pocket.” 6. “I have to wash my hands over and over again many times.” 908. A client’s medication sheet contains a prescription for sertraline. To ensure safe administration of the medication, how should the nurse administer the dose? 1. On an empty stomach 2. At the same time each evening 3. Evenly spaced around the clock 4. As needed when the client complains of depression 909. A client with schizophrenia has been started on medication therapy with clozapine. The nurse should assess the results of which laboratory study to monitor for adverse effects from this medication? 1. Platelet count 2. Blood glucose level 3. Liver function studies 4. White blood cell count 910. A client is scheduled for discharge and will be taking phenobarbital for an extended period. The nurse would place highest priority on teaching the client which point that directly relates to client safety? 1. Take the medication only with meals. 2. Take the medication at the same time each day. 3. Use a dose container to help prevent missed doses. 4. Avoid drinking alcohol while taking this medication. 911. The nurse is describing the medication side and adverse effects to a client who is taking oxazepam. Which information should the nurse incorporate in the discussion? 1. Consume a low-fiber diet. 2. Increase fluids and bulk in the diet. 3. Rest if the heart begins to beat rapidly. 4. Take antidiarrheal agents if diarrhea occurs. 912. The nurse is administeringrisperidone to a client who isscheduled to bedischarged.Beforedischarge,which instruction should the nurse provide to the client? 1. Get adequate sunlight. 2. Continue driving as usual. 3. Avoid foods rich in potassium. 4. Get up slowly when changing positions. 913. The nurse is teaching a client who is being started on imipramine about the medication. The nurse should inform the client to expect maximum desired effects at which time period following initiation of the medication? 1. In 2 months 2. In 2 to 3 weeks 3. During the first week 4. During the sixth week of administration 914. A hospitalized client is started on phenelzine for the treatment of depression. The nurse should instruct the client that which foods are acceptable to consume while taking this medication? Select all that apply. 1. Figs 2. Yogurt 3. Crackers 4. Aged cheese 5. Tossed salad 6. Oatmeal raisin cookies 915. The nurse notes that a client with schizophrenia and receiving an antipsychotic medication is moving her mouth, protruding her tongue, and grimacing as she watches television. The nurse determines that the client is experiencing which medication complication? 1. Parkinsonism 2. Tardive dyskinesia 3. Hypertensive crisis 4. Neuroleptic malignant syndrome 916. The nurse is performing a follow-up teaching session with a client discharged 1 month ago. The client is taking fluoxetine. Which information would be important for the nurse to obtain during this client visit regarding the side and adverse effects of the medication? 1. Cardiovascular symptoms 2. Gastrointestinal dysfunctions 3. Problems with mouth dryness 4. Problems with excessive sweating Mental Health 1052 UNIT XIX Mental Health Disorders of the Adult Client 917. A client who has been taking buspirone for 1 month returns to the clinic for a follow-up assessment. The nurse determines that the medication is effective if the absence of which manifestation has occurred? 1. Paranoid thought process 2. Rapid heartbeat or anxiety 3. Alcohol withdrawal symptoms 4. Thought broadcasting or delusions 918. A client taking lithium reports vomiting, abdominal pain, diarrhea, blurred vision, tinnitus, and tremors. The lithium level is 2.5 mEq/L (2.5 mmol/L). The nurse plans care based on which representation of this level? 1. Toxic 2. Normal 3. Slightly above normal 4. Excessively below normal 919. Aclient gives the home health nurse a bottle of clomipramine. The nurse notes that the medication has not been taken by the client in 2 months. Which behavior observed in the client would validate noncompliance with this medication? 1. Complaints of insomnia 2. Complaints of hunger and fatigue 3. A pulse rate less than 60 beats/minute 4. Frequent hand washing with hot, soapy water 920. A hospitalized client has begun taking bupropion as an antidepressant agent. The nurse determines that which is an adverse effect, indicating that the client is taking an excessive amount of medication? 1. Constipation 2. Seizure activity 3. Increased weight 4. Dizziness when getting upright 921. Aclient receiving tricyclic antidepressants arrives at the mental health clinic. Which observation would indicate that the client is following the medication plan correctly? 1. Client reports not going to work for the past week. 2. Client complains of not being able to “do anything” anymore. 3. Client arrives at the clinic neat and appropriate in appearance. 4. Client reports sleeping 12 hours per night and 3 to 4 hours during the day. 922. The emergency department nurse is caring for a client who has been identified as a victim of physical abuse. In planning care for the client, which is the priority nursing action? 1. Adhering to the mandatory abuse-reporting laws 2. Notifying the caseworker of the family situation 3. Removing the client from any immediate danger 4. Obtaining treatment for the abusing family member 923. The nurse assesses a client with the admitting diagnosis of bipolar affective disorder, mania. Which client symptoms require the nurse’s immediate action? 1. Incessant talking and sexual innuendoes 2. Grandiose delusions and poor concentration 3. Outlandish behaviors and inappropriate dress 4. Nonstop physical activity and poor nutritional intake 924. The nurse is caring for a client who was involuntarily hospitalized to a mental health unit and is scheduled for electroconvulsive therapy. The nurse notes that an informed consent has not been obtained for the procedure. Based on this information, what is the nurse’s best determination in planning care? 1. The informed consent does not need to be obtained. 2. The informed consent should be obtained from the family. 3. The informed consent needs to be obtained from the client. 4. The health care provider will provide the informed consent. 925. A client newly diagnosed with diabetes mellitus is instructed by the health care provider to obtain glucagon for emergency home use. The client asks a home care nurse about the purpose of the medication. What is the nurse’s best response to the client’s question? 1. “It will boost the cells in your pancreas if you have insufficient insulin.” 2. “It will help to promote insulin absorption when your glucose levels are high.” 3. “It is for the times when your blood glucose is too low from too much insulin.” 4. “It will help to prevent lipoatrophy from the multiple insulin injections over the years.” 926. The nurse is providing care to a Puerto Rican– American client who is terminally ill. Numerous family members are present most of the time, and many of the family members are very emotional. What is the most appropriate nursing action for this client? 1. Restrict the number of family members visiting at one time. 2. Inform the family that emotional outbursts are to be avoided. 3. Make the necessary arrangements so that family members can visit. 4. Contact the health care provider to speak to the family regarding their behaviors. 927. Aclient presents to the emergency department with upper gastrointestinal bleeding and is in moderate distress. In planning care, what is the priority nursing action for this client? 1. Assessment of vital signs 2. Completion of abdominal examination 3. Insertion of the prescribed nasogastric tube 4. Thorough investigation of precipitating events 928. The nurse is performing an assessment on a client with dementia. Which piece of data gathered during the assessment indicates a manifestation associated with dementia? 1056 1. Use of confabulation 2. Improvement in sleeping 3. Absence of sundown syndrome 4. Presence of personal hygienic care 929. The nurse is caring for a client with anorexia nervosa. Which behavior is characteristic of this disorder and reflects anxiety management? 1. Engaging in immoral acts 2. Always reinforcing self-approval 3. Observing rigid rules and regulations 4. Having the need always to make the right decision 930. The nurse provides instructions to a malnourished pregnant client regarding iron supplementation. Which client statement indicates an understanding of the instructions? 1. “Iron supplements will give me diarrhea.” 2. “Meat does not provide iron and should be avoided.” 3. “The iron is best absorbed if taken on an empty stomach.” 4. “On the days that I eat green leafy vegetables or calf liver I can omit taking the iron supplement.” 931. Levothyroxine is prescribed for a client diagnosed with hypothyroidism. Upon review of the client’s record, the nurse notes that the client is taking warfarin. Which modification to the plan of care should the nurse review with the client’s health care provider? 1. A decreased dosage of levothyroxine 2. An increased dosage of levothyroxine 3. A decreased dosage of warfarin sodium 4. An increased dosage of warfarin sodium 932. The nurse is teaching a client with emphysema about positions that help breathing during dyspneic episodes. The nurse instructs the client that which positions alleviate dyspnea? Select all that apply. 1. Sitting up and leaning on a table 2. Standing and leaning against a wall 3. Lying supine with the feet elevated 4. Sitting up with the elbows resting on knees 5. Lying on the back in a low Fowler’s position 933. A client is about to undergo a lumbar puncture. The nurse describes to the client that which position will be used during the procedure? 1. Side-lying with a pillow under the hip 2. Prone with a pillow under the abdomen 3. Prone in slight Trendelenburg position 4. Side-lying with the legs pulled up and the head bent down onto the chest 934. The nurse recognizes that which interventions are likely to facilitate effective communication between a dying client and family? Select all that apply. 1. The nurse encourages the client and family to identify and discuss feelings openly. 2. The nurse assists the client and family in carrying out spiritually meaningful practices. 3. The nurse removes autonomy from the client to alleviate any unnecessary stress for the client. 4. The nurse makes decisions for the client and family to relieve them of unnecessary demands. 5. The nurse maintains a calm attitude and one of acceptance when the family or client expresses anger. 935. A depressed client verbalizes feelings of low selfesteem and self-worth typified by statements such as “I’m such a failure. I can’t do anything right.” How should the nurse plan to respond to the client’s statement? 1. Reassure the client that things will get better. 2. Tell the client that this is not true and that we all have a purpose in life. 3. Identify recent behaviors or accomplishments that demonstrate the client’s skills. 4. Remain with the client and sit in silence; this will encourage the client to verbalize feelings. 936. The nurse has just admitted to the nursing unit a client with a basilar skull fracture who is at risk for increased intracranial pressure. Pending specific health care provider prescriptions, the nurse should safely place the client in which positions? Select all that apply. 1. Head midline 2. Neck in neutral position 3. Head of bed elevated 30 to 45 degrees 4. Head turned to the side when flat in bed 5. Neck and jaw flexed forward when opening the mouth 937. The nurse reviews the arterial blood gas results of an assigned client and notes that the laboratory report indicates a pH of 7.30, PaCO2 of 58 mm Hg, PaO2 of 80 mm Hg, and HCO 3 of 27 mEq/L (27 mmol/L). The nurse interprets that the client has which acid–base disturbance? 1. Metabolic acidosis 2. Metabolic alkalosis 3. Respiratory acidosis 4. Respiratory alkalosis 938. The nurse has admitted a client to the clinical nursing unit after undergoing a right mastectomy. The nurse should plan to place the right arm in which position? Comprehensive Test UNIT XX Comprehensive Test 1057 1. Elevated on a pillow 2. Level with the right atrium 3. Dependent to the right atrium 4. Elevated above shoulder level 939. On the second postpartum day, a client complains of burning on urination, urgency, and frequency of urination. A urinalysis indicates the presence of a urinary tract infection. The nurse instructs the client regarding measures to take for the treatment of the infection. Which client statement indicates to the nurse the need for further instruction? 1. “I need to urinate frequentlythroughout the day.” 2. “The prescribed medication must be taken until it is finished.” 3. “My fluid intake should be increased to at least 3000 mL daily.” 4. “Foods and fluids that will increase urine alkalinity should be consumed.” 940. Aclient received 20 units of Humulin N insulin subcutaneously at 08:00. At what time should the nurse plan to assess the client for a hypoglycemic reaction? 1. 10:00 2. 11:00 3. 17:00 4. 24:00 941. The nurse is the first responder after a tornado has destroyed many homes in the community. Which victim should the nurse attend to first? 1. A pregnant woman who exclaims, “My baby is not moving.” 2. Achild who is complaining, “My leg is bleeding so bad, I am afraid it is going to fall off!” 3. A young child standing next to an adult family member who is screaming, “I want my mommy!” 4. An older victim who is sitting next to her husband sobbing, “My husband is dead. My husband is dead.” 942. A pregnant client at 10 weeks’ gestation calls the prenatal clinic to report a recent exposure to a child with rubella. The nurse reviews the client’s chart. What is the nurse’s best response to the client? Refer to chart. 1. “You should avoid all school-age children during pregnancy.” 2. “There is no need to be concerned if you don’t have a fever or rash within the next 2 days.” 3. “You were wise to call. Your rubella titer indicates that you are immune and your baby is not at risk.” 4. “Be sure to tell the health care provider in 2 weeks, as additional screening will be prescribed during your second trimester.” 943. A breast-feeding mother of an infant with lactose intolerance asks the nurse about dietary measures. What foods should the nurse tell the mother are acceptable to consume while breast-feeding? Select all that apply. 1. 1% milk 2. Egg yolk 3. Dried beans 4. Hard cheeses 5. Green leafy vegetables 944. A client with diabetes mellitus is told that amputation of the leg is necessary to sustain life. The client is very upset and tells the nurse, “This is all my health care provider’s fault. I have done everything I’ve been asked to do!” Which nursing interpretation is best for this situation? 1. An expected coping mechanism 2. An ineffective defense mechanism 3. A need to notify the hospital lawyer 4. An expression of guilt on the part of the client 945. A client with terminal cancer arrives at the emergency department dead on arrival (DOA). After an autopsy is prescribed, the client’s family requests that no autopsy be performed. Which response to the family is most appropriate? 1. “The decision is made by the medical examiner.” 2. “An autopsy is mandatory for any client who is DOA.” 3. “I will contact the medical examiner regarding your request.” 4. “It is required by federal law. Tell me why you don’t want the autopsy done.” 946. A client who is positive for human immunodeficiency virus (HIV) delivers a newborn infant. The nurse provides instructions to help the client with care of her infant. Which client statement indicates the need for further instruction? 1. “I will be sure to wash my hands before and after bathroom use.” 2. “I need to breast-feed, especially for the first 6 weeks postpartum.” 3. “Support groups are available to assist me with understanding my diagnosis of HIV.” Comprehensive Test History and Physical Laboratory and Diagnostic Results Medications Gravida, Term Births, Preterm Births, Abortions, Living Children (GTPAL) 1,0,0,0,0 Venereal Disease Research Laboratory (VDRL) nonreactive Prenatal vitamins Weight 135 lb (61 kg) Rubella immune Positive Goodell and Chadwick Rh positive, Type O 1058 UNIT XX Comprehensive Test 4. “My newborn infant should be on antiviral medications for the first 6 weeks after delivery.” 947. An adolescent client is diagnosed with conjunctivitis, and the nurse provides information to the client about the use of contact lenses. Which client statement indicates the need for further information? 1. “I should obtain new contact lenses.” 2. “I should not wear my contact lenses.” 3. “My old contact lenses should be discarded.” 4. “My contact lenses can be worn if they are cleaned as directed.” 948. The nurse teaches a client newly diagnosed with type 1 diabetes about storing Humulin N insulin. Which statement indicates to the nurse that the client understood the discharge teaching? 1. “I should keep the insulin in the cabinet during the day only.” 2. “I know I have to keep my insulin in the refrigerator at all times.” 3. “I can store the open insulin bottle in the kitchen cabinet for 1 month.” 4. “The best place for my insulin is on the window sill, but in the cupboard is just as good.” 949. The nurse is caring for a client scheduled for a transsphenoidal hypophysectomy. The preoperative teaching instructions should include which statement? 1. “Your hair will need to be shaved.” 2. “You will receive spinal anesthesia.” 3. “You will need to ambulate after surgery.” 4. “Brushing your teeth needs to be avoided for at least 2 weeks after surgery.” 950. During a routine prenatal visit, a client complains of gums that bleed easily with brushing. The nurse performs an assessment and teaches the client about proper nutrition to minimize this problem. Which client statement indicates an understanding of the proper nutrition to minimize this problem? 1. “I will drink 8 oz of water with each meal.” 2. “I will eat 3 servings of cracked wheat bread each day.” 3. “I will eat 2 saltine crackers before I get up each morning.” 4. “I will eat fresh fruits and vegetables for snacks and for dessert each day.” 951. A 6-year-old child has just been diagnosed with localized Hodgkin’s disease, and chemotherapy is planned to begin immediately. The mother of the child asks the nurse why radiation therapy was not prescribed as a part of the treatment. What is the nurse’s best response? 1. “It’s very costly, and chemotherapy works just as well.” 2. “I’m not sure. I’ll discuss it with the health care provider.” 3. “Sometimes age has to do with the decision for radiation therapy.” 4. “The health care provider would prefer that you discuss treatment options with the oncologist.” 952. An infant born with an imperforate anus returns from surgery after requiring a colostomy. The nurse assesses the stoma and notes that it is red and edematous. Based on this finding, which action should the nurse take? 1. Elevate the buttocks. 2. Document the findings. 3. Apply ice immediately. 4. Call the health care provider. 953. The nurse is performing an initial assessment on a newborn infant. When assessing the infant’s head, the nurse notes that the ears are low-set. Which nursing action is most appropriate? 1. Document the findings. 2. Arrange for hearing testing. 3. Notify the health care provider. 4. Cover the ears with gauze pads. 954. The clinic nurse is assessing jaundice in a child with hepatitis. Which anatomical area would provide the best data regarding the presence of jaundice? 1. The nail beds 2. The skin in the sacral area 3. The skin in the abdominal area 4. The membranes in the ear canal 955. The nurse is assigned to care for a client in traction. The nurse creates a plan of care for the client and should include which action in the plan? 1. Ensure that the knots are at the pulleys. 2. Check the weights to ensure that they are off of the floor. 3. Ensure that the head of the bed is kept at a 45- to 90-degree angle. 4. Monitor the weights to ensure that they are resting on a firm surface. 956. The nurse is setting up the physical environment for an interview with a client and plans to obtain subjective data regarding the client’s health. Which interventions are appropriate? Select all that apply. Comprehensive Test UNIT XX Comprehensive Test 1059 1. Set the room temperature at a comfortable level. 2. Remove distracting objects from the interviewing area. 3. Place a chair for the client across from the nurse’s desk. 4. Ensure comfortable seating at eye level for the client and nurse. 5. Provide seating for the client so that the client faces a strong light. 6. Ensure that the distance between the client and nurse is at least 7 feet (2.1 meters). 957. The nurse is caring for an older adult who has been placed in Buck’s extension traction after a hip fracture. On assessment of the client, the nurse notes that the client is disoriented. What is the best nursing action based on this information? 1. Apply restraints to the client. 2. Ask the family to stay with the client. 3. Place a clock and calendar in the client’s room. 4. Ask the laboratory to perform electrolyte studies. 958. The nurse is creating a plan of care for a client in skin traction. The nurse should monitor for which priority finding in this client? 1. Urinary incontinence 2. Signs of skin breakdown 3. The presence of bowel sounds 4. Signs of infection around the pin sites 959. The home care nurse is visiting a client who is in a body cast. While performing an assessment, the nurse plans to evaluate the psychosocial adjustment of the client to the cast. What is the most appropriate assessment for this client? 1. The need for sensory stimulation 2. The amount of home care support available 3. The ability to perform activities of daily living 4. The type of transportation available for followup care 960. What action should the nurse consider when counseling a client of the Amish tradition? 1. Speak only to the husband. 2. Use complex medical terminology. 3. Avoid using scientific or medical jargon. 4. Stand close to the client and speak loudly. 961. A client has refused to eat more than a few spoonfuls of breakfast. The health care provider has prescribed that tube feedings be initiated if the client fails to eat at least half of a meal because the client has lost a significant amount of weight during the previous 2 months. The nurse enters the room, looks at the tray, and states, “If you don’t eat any more than that, I’m going to have to put a tube down your throat and get a feeding in that way.” The client begins crying and tries to eat more. Based on the nurse’s actions, the nurse may be accused of which violation? 1. Assault 2. Battery 3. Slander 4. Invasion of privacy 962. When creating an assignment for a team consisting of a registered nurse (RN), 1 licensed practical nurse (LPN), and 2 unlicensed assistive personnel (UAP), which is the best client for the LPN? 1. A client requiring frequent temperature checks 2. A client requiring assistance with ambulation every 4 hours 3. A client on a mechanical ventilator requiring frequent assessment and suctioning 4. A client with a spinal cord injury requiring urinary catheterization every 6 hours 963. To perform cardiopulmonary resuscitation (CPR), the nurse should use the method pictured to open the airway in which situation? Refer to figure. 1. If neck trauma is suspected 2. In all situations requiring CPR 3. If the client has a history of seizures 4. If the client has a history of headaches 964. The nurse teaches skin care to a client receiving external radiation therapy. Which client statement indicates the need for further instruction? 1. “I will handle the area gently.” 2. “I will wear loose-fitting clothing.” 3. “I will avoid the use of deodorants.” 4. “I will limit sun exposure to 1 hour daily.” 965. The health care provider’s prescription reads levothyroxine, 150 mcg orally daily. The medication label reads levothyroxine, 0.1 mg per tablet. The nurse should administer how many tablet(s) to the client? Fill in the blank. Answer: _____ tablet(s) Comprehensive Test 1060 UNIT XX Comprehensive Test Comprehensive Test 966. Metformin is prescribed for a client with type 2 diabetes mellitus. What is the most common side effect that the nurse should include in the client’s teaching plan? 1. Weight gain 2. Hypoglycemia 3. Flushing and palpitations 4. Gastrointestinal disturbances 967. Which nursing actions apply to the care of a child who is having a seizure? Select all that apply. 1. Time the seizure. 2. Restrain the child. 3. Stay with the child. 4. Insert an oral airway. 5. Loosen clothing around the child’s neck. 6. Place the child in a lateral side-lying position. 968. The nurse is conducting an interview of an older client and is concerned about the possibility of benign prostatic hyperplasia (BPH). Which are characteristics of this disorder? Select all that apply. 1. Nocturia 2. Incontinence 3. Enlarged prostate 4. Nocturnal emissions 5. Decreased desire for sexual intercourse 969. The nursing instructor asks a nursing student to identify the priorities of care for an assigned client. Which statement indicates that the student correctly identifies the priority client needs? 1. Actual or life-threatening concerns 2. Completing care in a reasonable time frame 3. Time constraints related to the client’s needs 4. Obtaining needed supplies to care for the client 970. A client arrives at the clinic complaining of fatigue, lack of energy, constipation, and depression. Hypothyroidism is diagnosed, and levothyroxine is prescribed. What is an expected outcome of the medication? 1. Alleviate depression 2. Increase energy levels 3. Increase blood glucose levels 4. Achieve normal thyroid hormone levels 971. The community health nurse is creating a poster for an educational session for a group of women and will be discussing the risk factors associated with breast cancer. Which risk factors for breast cancer should the nurse list on the poster? Select all that apply. 1. Multiparity 2. Early menarche 3. Early menopause 4. Family history of breast cancer 5. High-dose radiation exposure to chest 6. Previous cancer of the breast, uterus, or ovaries 972. The nurse is caring for a client with acute pancreatitis and is monitoring the client for paralytic ileus. Which piece of assessment data should alert the nurse to this occurrence? 1. Inability to pass flatus 2. Loss of anal sphincter control 3. Severe, constant pain with rapid onset 4. Firm, nontender mass palpable at the lower right costal margin 973. The nurse inspects the color of the drainage from a nasogastric tube on a postoperative client approximately 24 hours after gastric surgery. Which finding indicates the need to notify the health care provider (HCP)? 1. Dark red drainage 2. Dark brown drainage 3. Green-tinged drainage 4. Light yellowish-brown drainage 974. The nurse is preparing to discontinue a client’s nasogastric tube. The client is positioned properly, and the tube has been flushed with 15 mL of air to clear secretions. Before removing the tube, the nurse should make which statement to the client? 1. “Take a deep breath when I tell you, and hold it while I remove the tube.” 2. “Take a deep breath when I tell you, and bear down while I remove the tube.” 3. “Take a deep breath when I tell you, and slowly exhale while I remove the tube.” 4. “Take a deep breath when I tell you, and breathe normally while I remove the tube.” 975. A client with a history of lung disease is at risk for developing respiratory acidosis. The nurse should assess the client for which signs and symptoms characteristic of this disorder? 1. Bradycardia and hyperactivity 2. Decreased respiratory rate and depth 3. Headache, restlessness, and confusion 4. Bradypnea, dizziness, and paresthesias 976. The nurse is caring for a client with a resolved intestinal obstruction who has a nasogastric tube in place. The health care provider has now prescribed that the nasogastric tube be removed. What is the priority nursing assessment prior to removing the tube? 1. Checking for normal serum electrolyte levels 2. Checking for normal pH of the gastric aspirate UNIT XX Comprehensive Test 1061 3. Checking for proper nasogastric tube placement 4. Checking for the presence of bowel sounds in all 4 quadrants 977. The nurse has reviewed with the preoperative client the procedure for the administration of an enema. Which statement by the client would indicate the need for further instruction? 1. “The enema will be given while I am sitting on the toilet.” 2. “I should try and hold the fluid as long as possible after it is instilled.” 3. “I know that there will be some cramping after the enema administration.” 4. “I should tell the nurse if cramping occurs during the instillation of the fluid.” 978. A client experiencing a great deal of stress and anxiety is being taught to use self-control therapy. Which statement by the client indicates a need for further teachin g about the therapy? 1. “This form of therapy can be applied to new situations.” 2. “An advantage of this technique is that change is likely to last.” 3. “Talking to oneself is a basic component of this form of therapy.” 4. “This form of therapy provides a negative reinforcement when the stimulus is produced.” 979. The nurse is preparing a list of home care instructions regarding stoma and laryngectomy care for a client with laryngeal cancer who had a laryngectomy. Which instructions should be included in the list? Select all that apply. 1. Restrict fluid intake. 2. Obtain a MedicAlert bracelet. 3. Keep the humidity in the home low. 4. Prevent debris from entering the stoma. 5. Avoid exposure to people with infections. 6. Avoid swimming and use care when showering. 980. The health care provider prescribes 2000 mLof 5% dextrose and half-normal saline to infuse over 24 hours. The drop factor is 15 drops (gtt)/mL. The nurse should set the flow rate at how many drops per minute? Fill in the blank. Record your answer to the nearest whole number. Answer: _____ gtt/minute 981. A client is returned to the nursing unit after thoracic surgery with chest tubes in place. During the first few hours postoperatively, what type of drainage should the nurse expect? 1. Serous 2. Bloody 3. Serosanguineous 4. Bloody, with frequent small clots 982. A client has had radical neck dissection and begins to hemorrhage at the incision site. The nurse should take which actions in this situation? Select all that apply. 1. Monitor vital signs. 2. Monitor the client’s airway. 3. Apply manual pressure over the site. 4. Lower the head of the bed to a flat position. 5. Call the health care provider (HCP) immediately. 983. A sexually active young adult client has developed viral hepatitis. Which client statement indicates the need for further teachin g? 1. “I should avoid drinking alcohol.” 2. “I can go back to work right away.” 3. “My partner should get the vaccine.” 4. “A condom should be used for sexual intercourse.” 984. The nurse should include which interventions in the plan of care for a client with hypothyroidism? Select all that apply. 1. Provide a cool environment for the client. 2. Instruct the client to consume a high-fat diet. 3. Instruct the client about thyroid replacement therapy. 4. Encourage the client to consume fluids and high-fiber foods in the diet. 5. Inform the client that iodine preparations will be prescribed to treat the disorder. 6. Instruct the client to contact the health care provider (HCP) if episodes of chest pain occur. 985. The nurse is preparing to care for a client who will be weaned from a cuffed tracheostomy tube. The nurse is planning to use a tracheostomy plug and plans to insert it into the opening in the outer cannula. Which nursing action is required before plugging the tube? 1. Deflate the cuff on the tube. 2. Place the inner cannula into the tube. 3. Ensure that the client is able to speak. 4. Ensure that the client is able to swallow. 986. A client is diagnosed with glaucoma. Which piece of nursing assessment data identifies a risk factor associated with this eye disorder? 1. Cardiovascular disease 2. Frequent urinary tract infections 3. A history of migraine headaches 4. Frequent upper respiratory infections Comprehensive Test 1062 UNIT XX Comprehensive Test 987. A client with retinal detachment is admitted to the nursing unit in preparation for a repair procedure. Which prescription should the nurse anticipate? 1. Allowing bathroom privileges only 2. Elevating the head of the bed to 45 degrees 3. Wearing dark glasses to read or watch television 4. Placing an eye patch over the client’s affected eye 988. The nurse is caring for a client who is on strict bed rest and creates a plan of care with goals related to the prevention of deep vein thrombosis and pulmonary emboli. Which nursing action is most helpful in preventing these disorders from developing? 1. Restricting fluids 2. Placing a pillow under the knees 3. Encouraging active range-of-motion exercises 4. Applying a heating pad to the lower extremities 989. The nurse is caring for a client who is at risk for suicide. What is the priority nursing action for this client? 1. Provide authority, action, and participation. 2. Display an attitude of detachment, confrontation, and efficiency. 3. Demonstrate confidence in the client’s ability to deal with stressors. 4. Provide hope and reassurance that the problems will resolve themselves. 990. A client with tuberculosis whose status is being monitored in an ambulatory care clinic asks the nurse when it is permissible to return to work. What factor should the nurse include when responding to the client? 1. Five blood cultures are negative. 2. Three sputum cultures are negative. 3. A blood culture and a chest x-ray are negative. 4. A sputum culture and a tuberculin skin test are negative. 991. A client comes to the emergency department after an assault and is extremely agitated, trembling, and hyperventilating. What is the priority nursing action for this client? 1. Begin to teach relaxation techniques. 2. Encourage the client to discuss the assault. 3. Remain with the client until the anxiety decreases. [Show More]
Last updated: 1 year ago
Preview 1 out of pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 19, 2020
Number of pages
Written in
Additional information
This document has been written for:
Uploaded
Jun 19, 2020
Downloads
0
Views
24