NR 511 Quiz 1 Summer 2020 – Chamberlain College of Nursing (A grade)
Document Content and Description Below
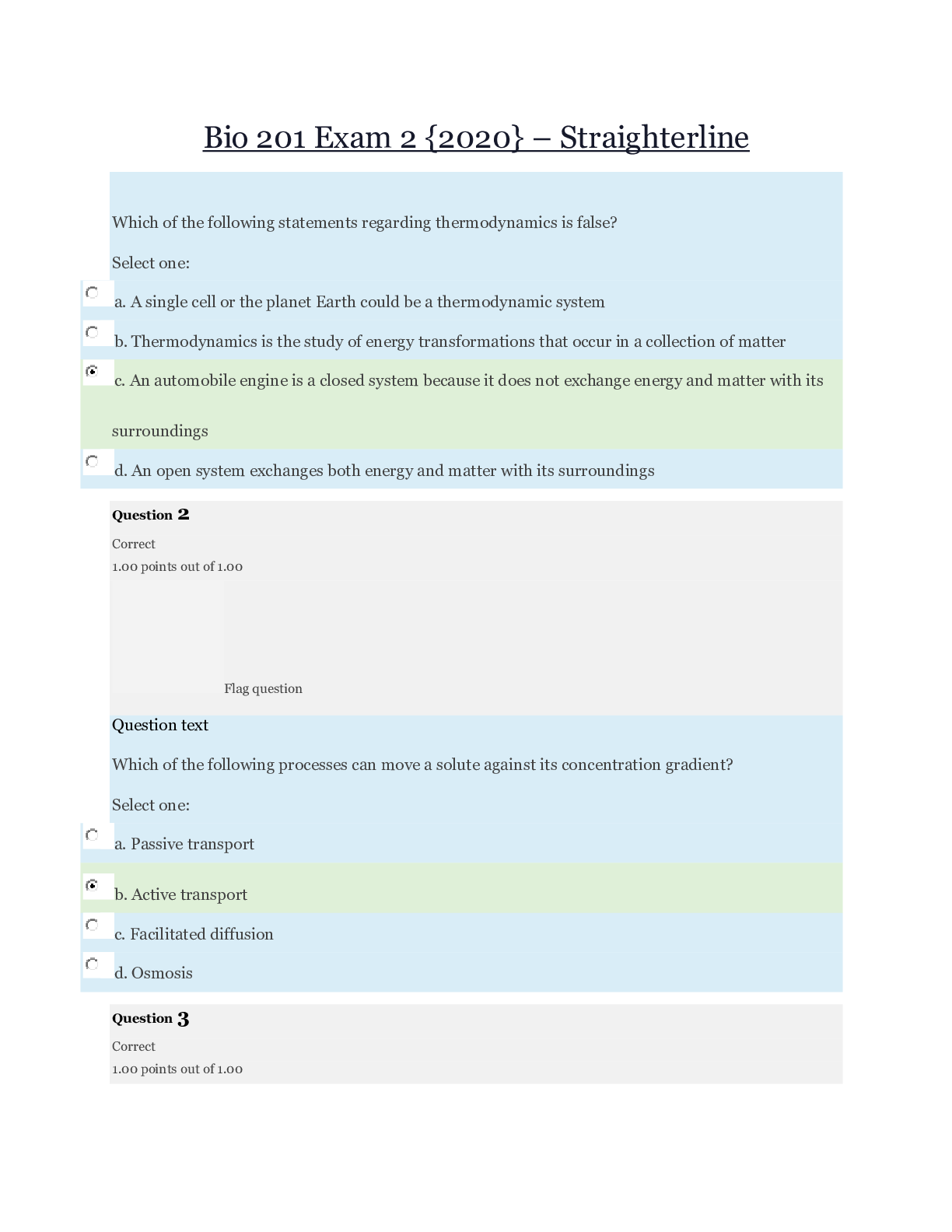
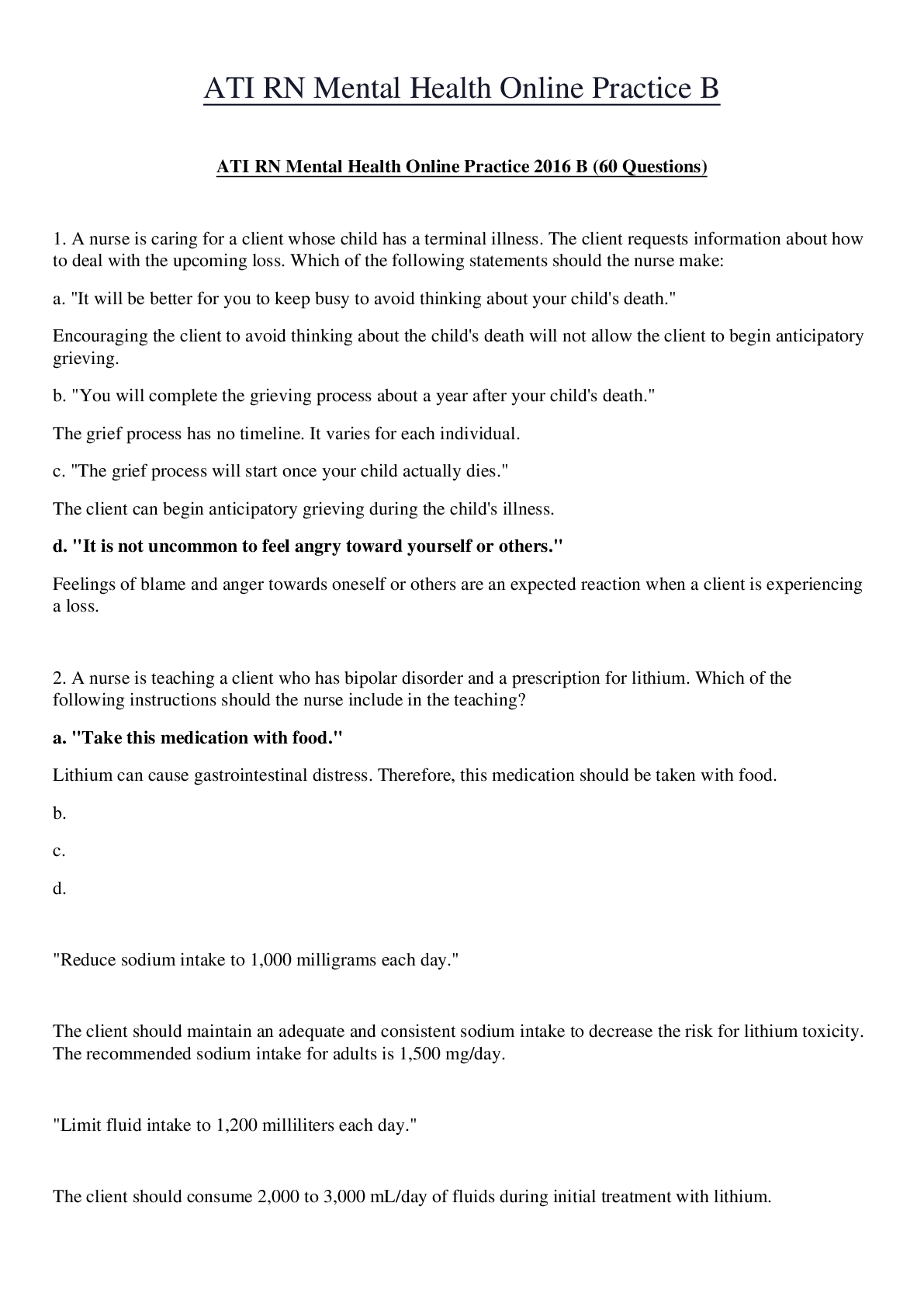
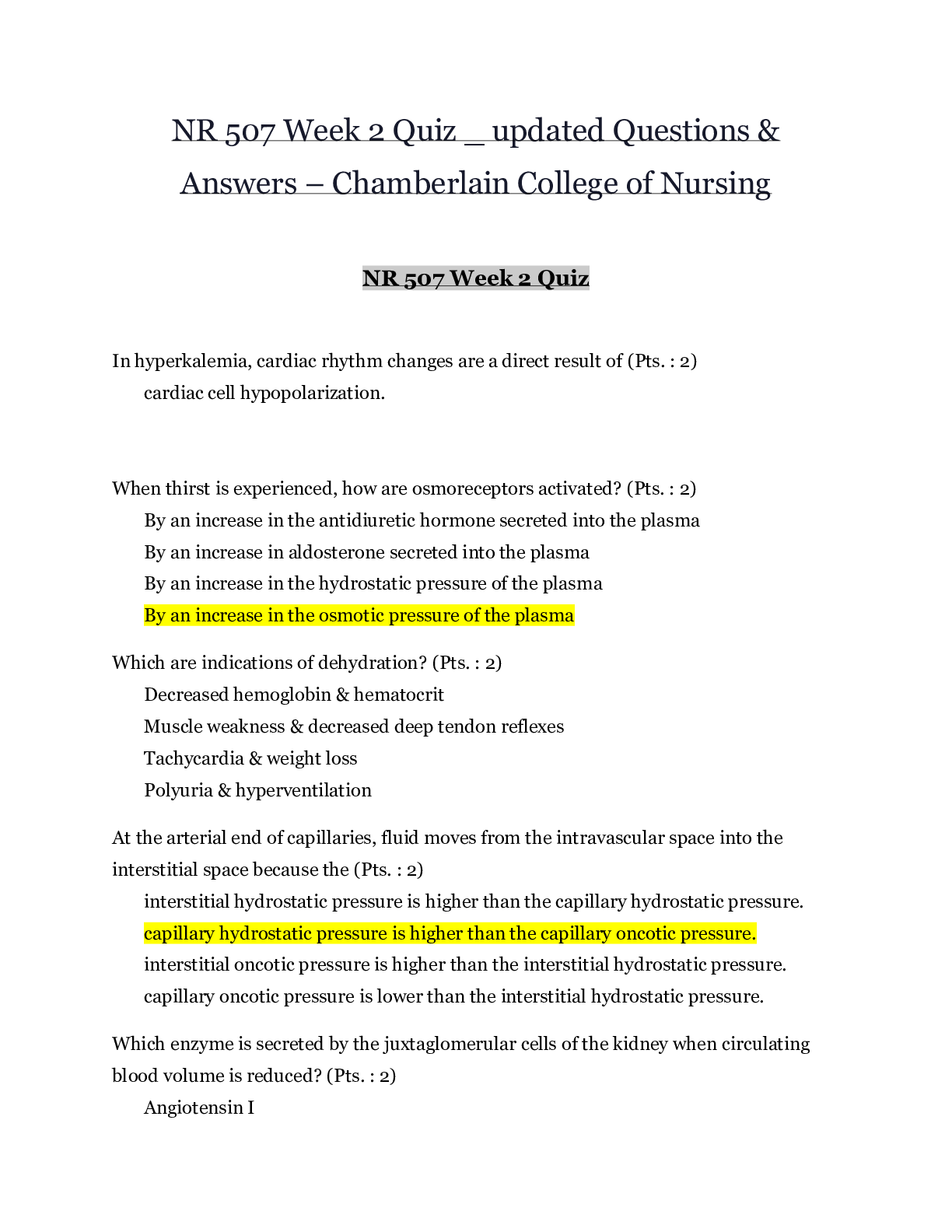
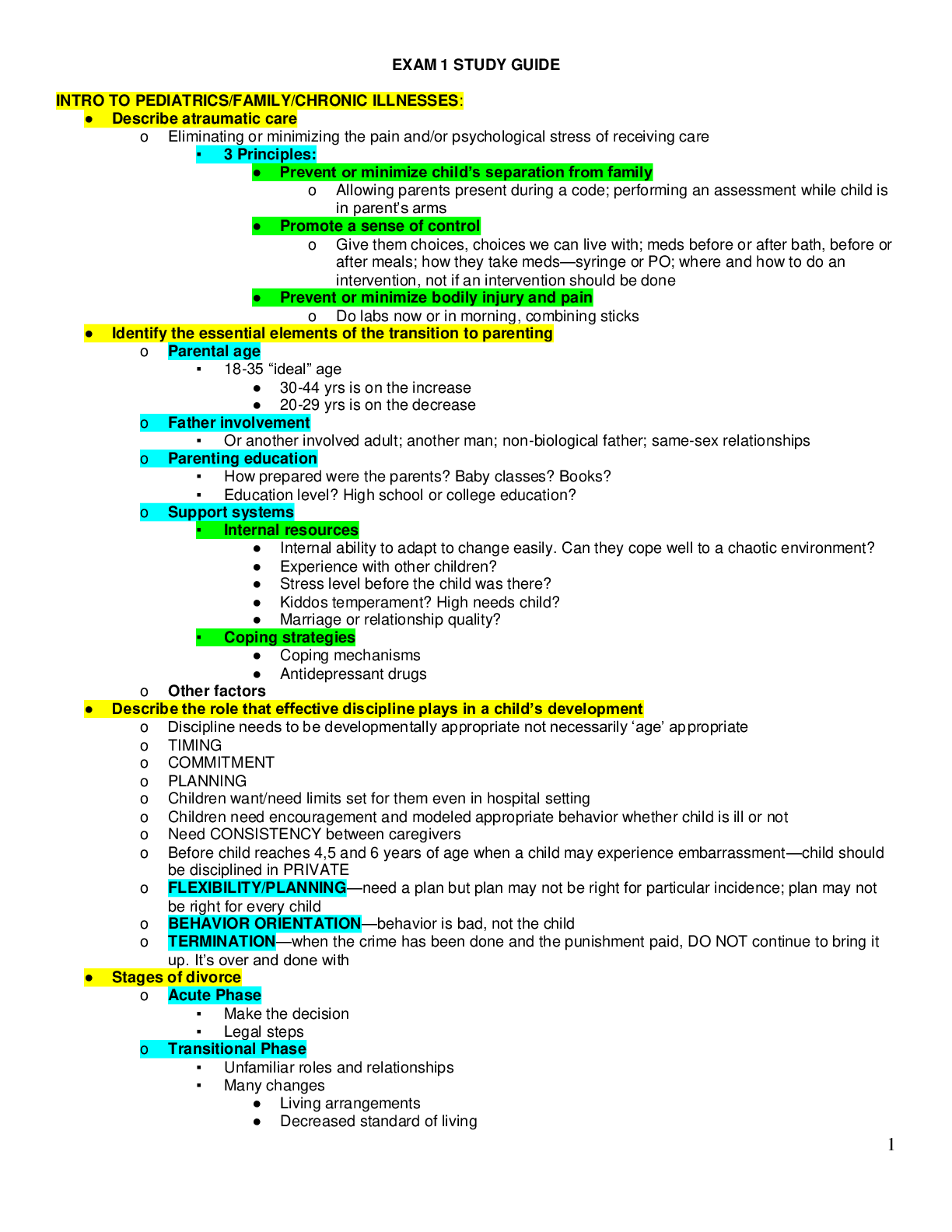
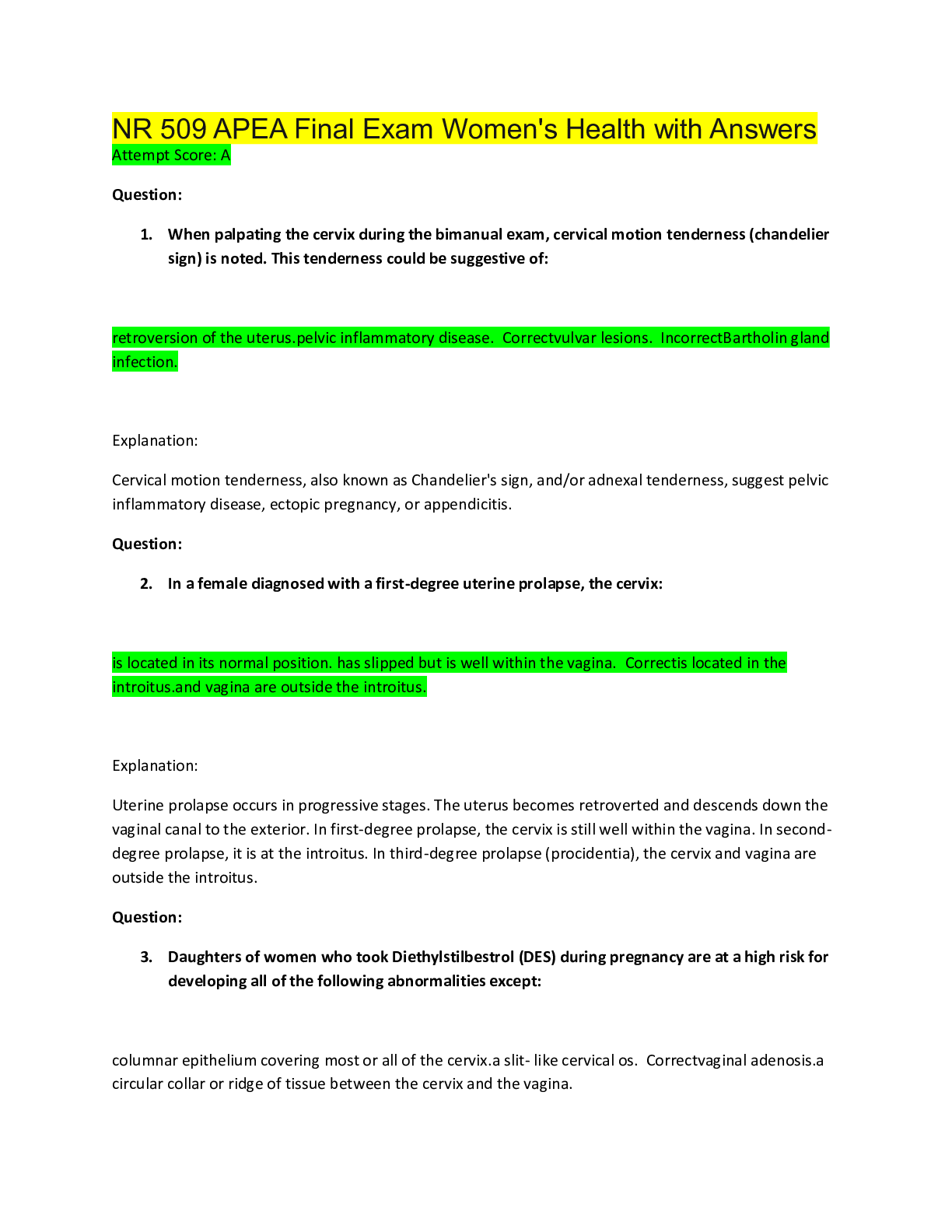
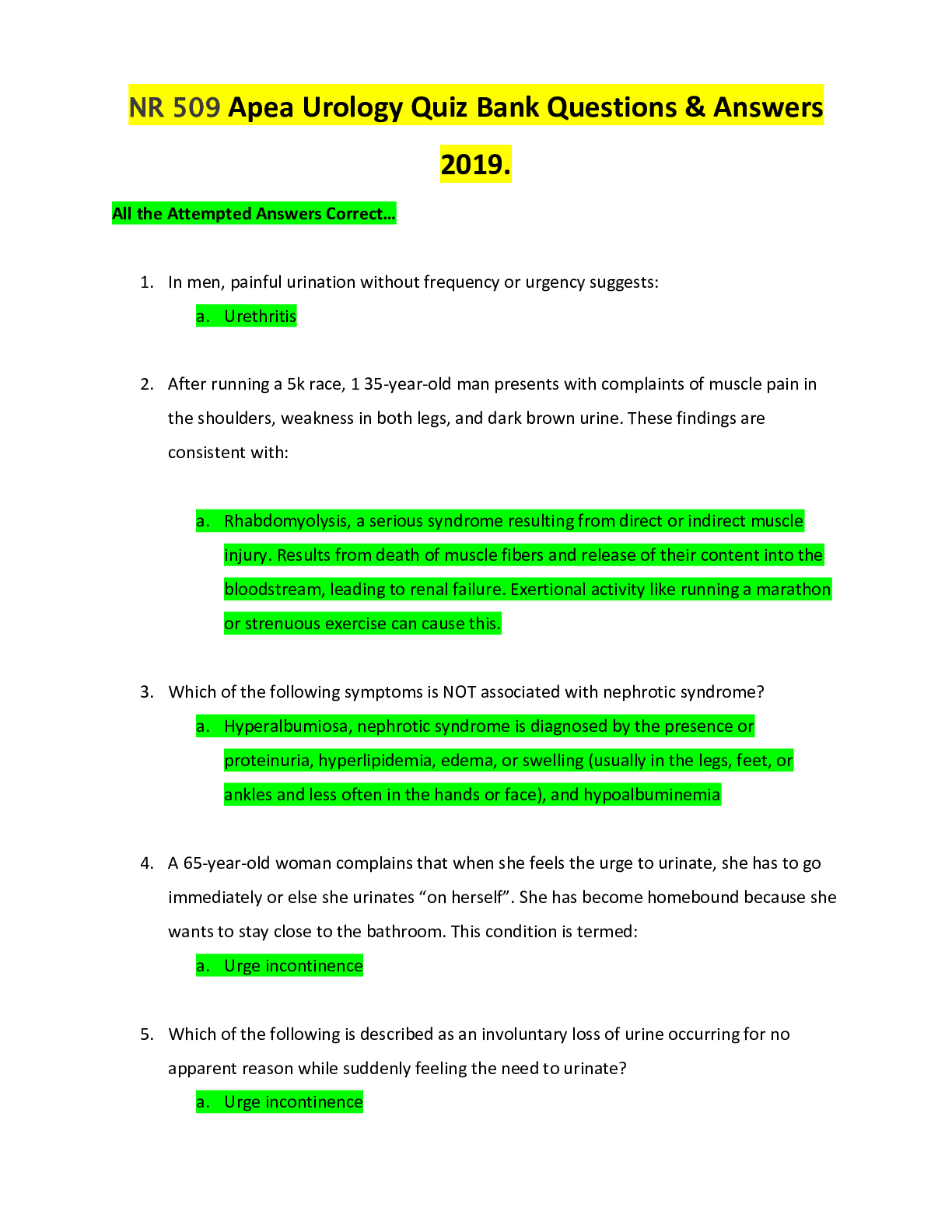
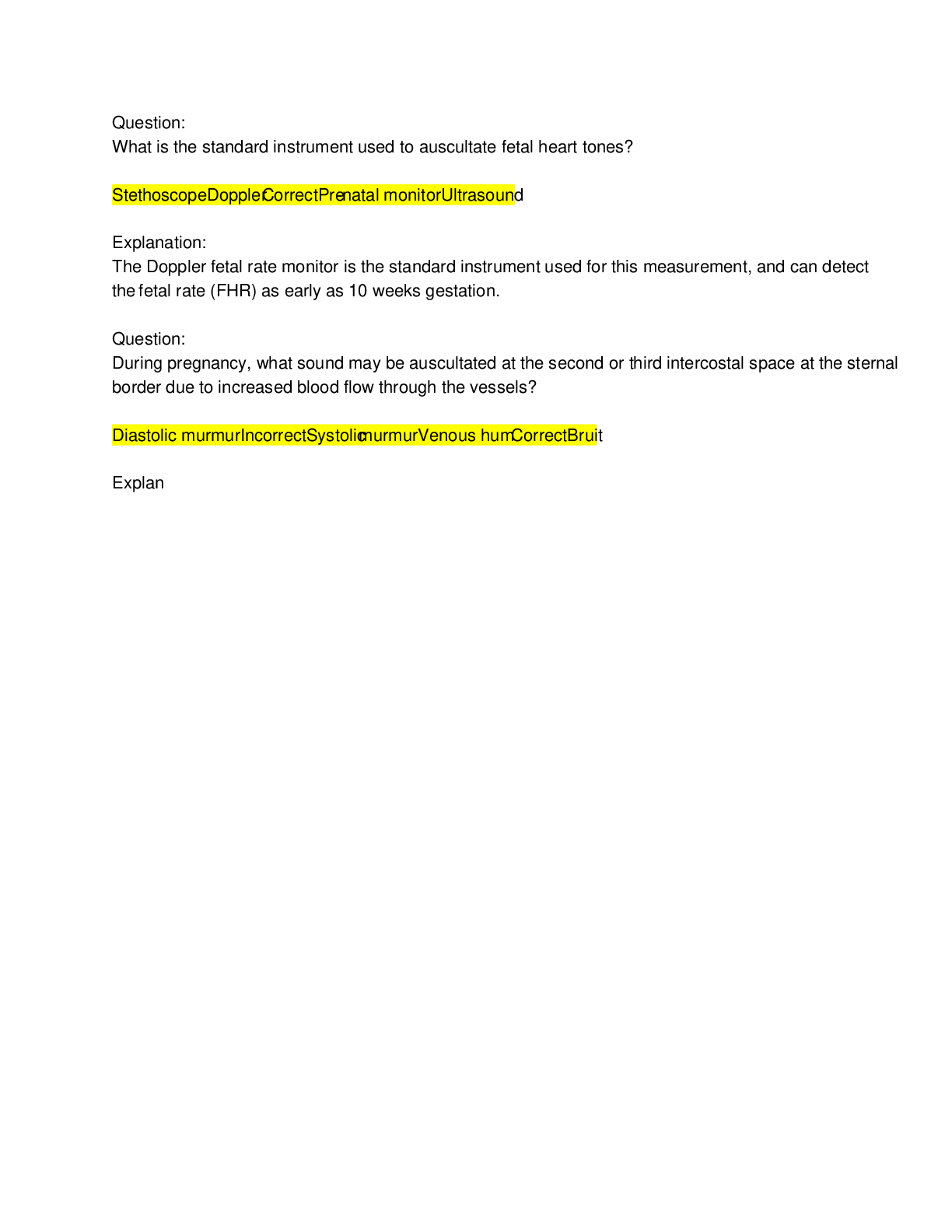
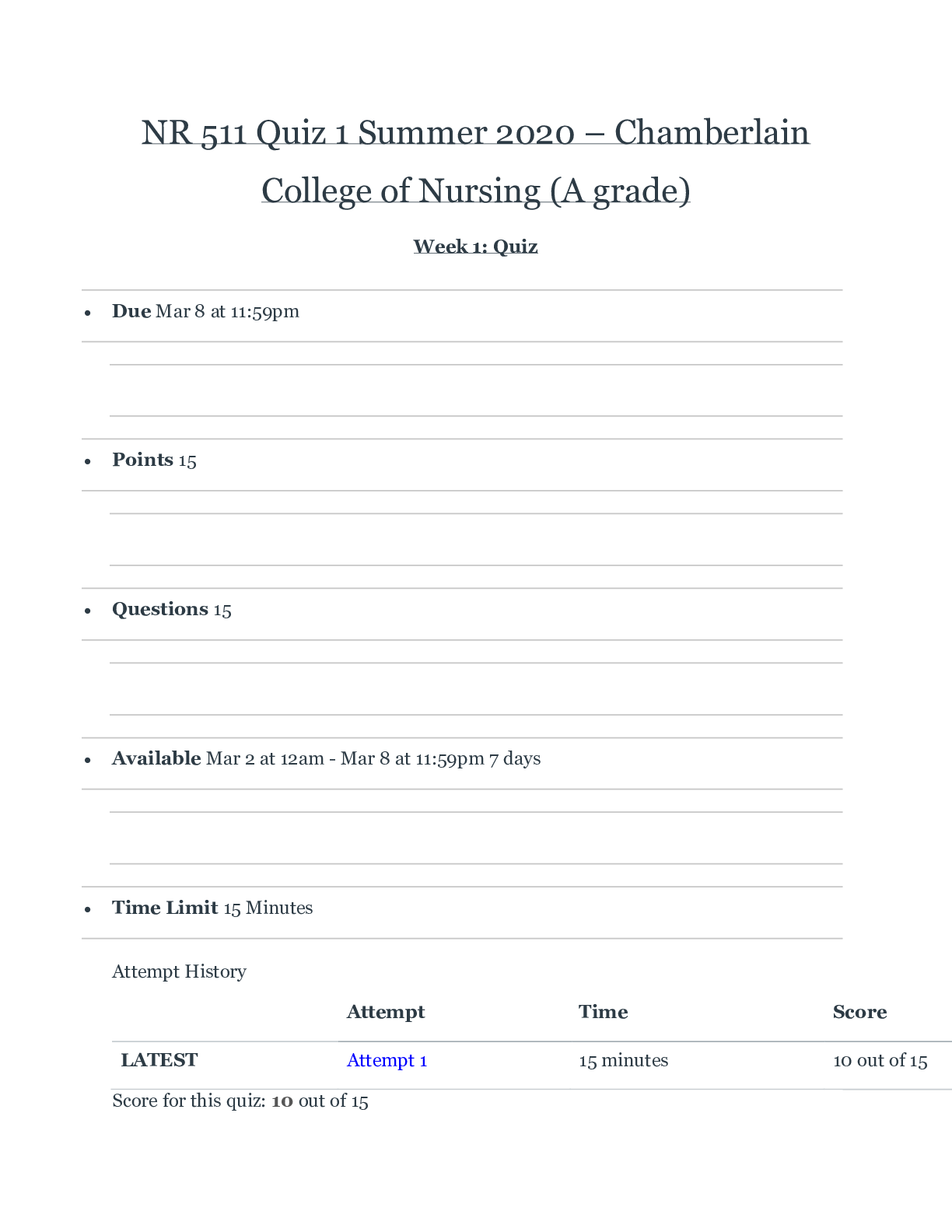
NR 511 Quiz 1 Summer 2020 – Chamberlain College of Nursing (A grade) Week 1: Quiz • Due Mar 8 at 11:59pm • Points 15 • Questions 15 • Available Mar 2 at 12am - Mar 8 at ... 11:59pm 7 days • Time Limit 15 Minutes Attempt History Attempt Time Score LATEST Attempt 1 15 minutes 10 out of 15 Score for this quiz: 10 out of 15 Submitted Mar 8 at 3:26pm This attempt took 15 minutes. Question 1 0 / 1 pts An 81-year-old patient presents for a physical. She recently had a fall and now has problems walking up her stairs. The only restroom in the house is on the second floor. She also has a flight of stairs outside her house she has to navigate in order to reach street level, and this is difficult for her. Where does this information belong in your chart note? Plan. Review of systems. You Answered Assessment. Functional health problems. The patient is having trouble with her normal routine and daily life due to her recent fall, so this information belongs in the functional health patterns section. Question 2 1 / 1 pts Which one of the following is true regarding the importance of documentation? It is only important in order to bill the patient for your service. It allows you to communicate your findings with the general public. Correct! It allows you to communicate your findings to other providers and serves as a record for the visit. It is only important for defending yourself in the event of a law suit. The purposes of documentation are to record the patient's report of symptoms, PMH, lifestyle and family factors, positive and negative findings on physical exam and the provider's plan. Documentation is important for billing purposes, communication with other providers and in the case litigation. Question 3 1 / 1 pts Most health maintenance organizations (HMOs) use a reimbursement mechanism called capitation. What does this mean? Correct! The HMO reimburses the provider a predetermined fee per client per month based on the client’s age and sex. The HMO is not responsible for provider reimbursement. The HMO reimburses the provider only if the patient has paid their deductible. The HMO reimburses the provider on a fee-for-service basis. The reimbursement mechanism called capitation that some HMOs use is one in which the HMO reimburses the provider a set fee per client per month based on the client's age and sex. HMOs are prepaid, comprehensive systems of health benefits that combine both financing and delivery of services to subscribers. They may pay providers on a capitated or fee-for-service basis. Question 4 1 / 1 pts What is an Accountable Care Organization (ACO)? A payment system for episodes of care to save money for the health care system. Correct! A group of providers and suppliers who come together voluntarily to give coordinated, high-quality care to Medicare patients. A bundling of pilot organizations. A risk pool that saves the overall organization money and maximizes reimbursement. ACOs are groups of doctors, hospitals and other health care providersd who come together voluntarily to give coordinated, high-quality care to the Medicare patients they serve. Coordinated care helps ensure that patients, especially the chronically ill, get the right care at the right time, with the goal of avoiding unnecessary duplication of services and preventing medical errors. When an ACO succeeeds in delivering high quality care and spending health care dollars more wisely, it will share in the savings it achieves for the Medicare program. Question 5 1 / 1 pts The phrase usual and customary refers to: Correct! How charges for a service compares with charges made to other persons receiving similar services and supplies. The success rate of a specified procedure. How an insurer evaluates the need for an ordered diagnostic test. How much an insurer will charge to provide coverage. The phrase usual and customary refers to the comparison of charges with other like charges for services and supplies received in the immediate vicinity as well as in a broader geographic area. Question 6 0 / 1 pts The Affordable Care Act (ACA) which passed in 2010 has a number of provisions, including the establishment of health exchanges. The purpose of a health insurance exchange is to: You Answered Reduce the overall out-of-pocket cost of health insurance to the consumer. Require each state to sell health insurance policies to consumers. Reduce the number of consumer health claims to the insurer. Create an online marketplace for the sale and purchase of health insurance for consumers. The health insurance exchange was created to provide a website for consumers to compare health insurance policies. Therefore, it is a marketplace for the sale and purchase of health insurance for consumers. Question 7 1 / 1 pts Denial of provider status is something that seriously impedes a nurse practitioner’s ability to practice. If that occurs, some steps one can take include: Correct! Writing letters to the organization’s president and chief executive officer (CEO), activating others to lobby on your behalf, and reapplying after a 6-month period. Requesting that your physician colleagues intervene on your behalf by writing critical letters to the organization in question. “Bashing” the organization to others and contacting an attorney. Requesting that your clients lobby on your behalf by going to the newspapers. There are many steps a nurse practitioner can take if denied provider status by a 3rd party reimburser. First, one should ascertain the reasons for this stance and determine whether it is the same across the board regarding nurse practitioners. If it is a consistent policy, attempt to find out why and begin marshaling evidence to overturn this stance in a constructive way. This may include having both clients and physician colleagues “lobby” on your behalf. Find out who the decision maker in the organization is and attempt to communicate directly with that person. Ascertain if there is a law in the state mandating this policy. Be prepared to testify at hearings and speak out at community meetings about this issue. Request language changes that specify “ask your doctor” and lobby to have these changes adopted. Reapplication in 6 months is reasonable. Question 8 1 / 1 pts What must you do as an advanced practice registered nurse (APRN) before billing for visits? Establish a collaborative agreement with a physician. Obtain a Drug Enforcement Administration (DEA) number. Correct! Obtain a provider number and familiarize yourself with the rules and policies of the third-party payer. Provide evidence of continuing medical education. To bill your clients for services, you must obtain a provider number and familiarize yourself with the rules and policies of each payor. Question 9 1 / 1 pts Which of the following demonstrates an objective finding? Ankle pain. Shortness of breath. Headache. Correct! Respiratory rate. Respiratory rate is the only objective finding which can be measured. Question 10 0 / 1 pts Which of the following statements about Medicaid is true? Medicaid is a federal plan created to provide care for indigent persons. You Answered Medicaid pays for family planning services, dental care, and eyeglasses. Medicaid is a program for the indigent financed jointly by the federal and state governments. Eligibility requirements for Medicaid are mandated by the Health Care Financing Administration. Financed jointly by the federal and state governments, Medicaid is a program created to pay for health care services for the indigent. Minimally, Medicaid must provide inpatients, skilled nursing facility, and home care; physician services, outpatients care; family planning services; and periodic sreening, detection, and treatment of children under age 12. Question 11 0 / 1 pts Which of the following is the best method for evaluating the efficacy of a new clinical intervention? You Answered A descriptive study. A correlational study. A case report. A randomized controlled trial. The best method for evaluating the efficacy of a new clinical intervention is a randomized controlled trial (RCT). Question 12 0 / 1 pts Which of the following statements does not belong in the past medical history portion of your chart note? Your patient had a cholecystectomy 3 years prior. Your patient had lab work done at their last appointment; CBC was normal. Your patient’s father passed away from lung cancer. You Answered Your patient has an allergy to penicillin. Allergies, family history and surgical history all belong in the history portion of your note. Test results are objective findings and should be in the diagnostic tests (objective) section of the note. Question 13 1 / 1 pts Which of the following demonstrates a subjective finding? Pulse rate. Extremity edema. Eye color. Correct! Pain level. Pain is a subjective finding, as patients self-report their level of pain. All other options are objective findings. Question 14 1 / 1 pts In relation to writing a patient encounter note, the acronym SOAP stands for which of the following? Symptoms, observations, assessment, plan. Symptoms, objective findings, assessment, plan. Correct! Subjective, objective, assessment, plan. Subjective, outward findings, assessment, plan. The acronym SOAP stands for subjective, objective, assessment and plan. Question 15 1 / 1 pts A screening test identified correctly identified 80 individuals who did not have breast cancer out of 100 individuals that were known to be free of the disease (true negatives). Thus, the test failed to recognize 20 individuals who did not have breast cancer. What is the specificity of the screening test? 40%. Correct! 80%. 60%. 20%. Specificity measures a screening test's ability to recognize individuals who are non-diseased or those with negative reactions (true negatives). It can be represented by a reaction of tested negatives to the total number of known, or true, negatives. In this case, the number of negatives that the test recognized was 80, with the total number of known, or true, negatives being 100. 80 out of 100=80%. Quiz Score: 10 out of 15 PreviousNext Submission Details: [Show More]
Last updated: 1 year ago
Preview 1 out of 13 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$12.50
Document information
Connected school, study & course
About the document
Uploaded On
Jun 30, 2020
Number of pages
13
Written in
Additional information
This document has been written for:
Uploaded
Jun 30, 2020
Downloads
0
Views
38