Pathophysiology > EXAM > NURS 3366 PATHO ASSIGNMENT #1 (GRADED A) ANSWERS & RATIONALES | Download To Score A (All)
NURS 3366 PATHO ASSIGNMENT #1 (GRADED A) ANSWERS & RATIONALES | Download To Score A
Document Content and Description Below
1 Basic Concepts of Pathophysiology & Implications for Nursing Questions 1 & 2 below refer to the following situation: A 55-year-old man with emphysema (a type of chronic lung disease) who has sm... oked 2 packs of cigarettes per day for 40 years is hospitalized for acute onset of cough productive of bloody sputum (sputum=secretions from deep in the lungs). After a few days of testing and treatment, the patient’s nurse reads a physician’s note on the chart: “I have told the patient that the etiologies of his hemoptysis are: 1) exacerbation of his chronic emphysema and 2) the new diagnosis of lung cancer. The onsets of both were contributed to by his longstanding smoking.” 1. The patient asks the nurse for more information. Which of the following explanations to the patient best indicates a full understanding of the patient’s situation? a. “You have a disease process that was iatrogenically caused by cigarette smoking.” Incorrect: “iatrogenically” means caused by a medical person. b. “You have a sudden onset of a chronic lung disease that was brought on by lung cancer.” Incorrect: the chronic lung disease was part of the medical history of the patient; the term “chronic” means a long-standing disease, not a “sudden onset.” c. “The coughing up of blood is caused by a worsening of a disease you’ve had for a long time plus a new problem-- lung cancer.” d. “These diseases have been creeping up on you for probably 20 years; it just goes to show that you should never have taken up smoking.” Incorrect: no evidence in the scenario to support this sentence. (Besides, it sounds very judgmental.) 2. Based on all the information you have on the patient, which statement is most likely correct? a. The patient has a poor prognosis because of the comorbidities of lung cancer and cigarette smoking. Incorrect: Smoking is a risk factor not a disease that would fit the term “comorbidity.” b. Lung cancer was a sequela of the bloody sputum. Incorrect: the bloody sputum was part of the S&S of cancer; this answer implies the bloody sputum caused the cancer. c. A precipitating factor for the acute hospitalization was overexertion when the patient started an exercise class. Incorrect: no evidence in the scenario to support this sentence. d. Heavy cigarette smoking was a risk factor in the patient’s developing emphysema and lung cancer. 2 Questions 3 & 4 refer to the following situation: An 80-year-old patient is in shock from loss of blood following an accident. His vital signs are: BP 80/50 (normal ~ 120/80), HR 120 (norm = 60-100), RR 20 (norm = 12 to 20), T 98.6 (norm ~ 98.6). 3. In assessing this patient, the nurse understands that the abnormal HR is a. probably the etiology for the patient’s low BP. Incorrect: the shock is due to the “loss of blood.” A state of shock has a “big picture” of low BP, high HR, cool hands, weakness, feeling faint, and/or passing out. In this context the high HR doesn’t CAUSE the low BP. b. due to the patient’s heart compensating for low blood volume by pumping faster. c. the normal compensatory response of shunting blood volume to the periphery. Incorrect: shunting blood to the periphery IS a compensatory response, but it is a “co-response” with high HR; one doesn’t cause the other. d. due to multiple risk factors. Incorrect: no evidence in the scenario to support this sentence. (TIP: when you are deciding on answers, plug them each into the stem of the question & ask yourself if it makes sense. Ex—does this sentence make sense? “In assessing this patient, the nurse understands that the abnormal HR is due to multiple risk factors.” Hopefully you see that no, it doesn’t make sense.) 4. The patient would also most likely have all of the following EXCEPT a. S&S of cool feet and hands from the body’s compensatory response to shock. b. S&S of feeling faint and weak from blood loss. c. a risk factor of shock. In an except question, remind yourself that 3 things go together. The 4th one is the one you choose—it doesn’t fit. d. a more guarded (ie, “poorer”) prognosis because of his age. 5. A young, otherwise healthy patient is admitted to the hospital with a diagnosis of heart failure of unknown cause. The etiology of the heart failure would be termed a. iatrogenic. b. idiopathic. c. nosocomial. d. acute. 6. To do well in this course, a student should a. memorize the notes thoroughly. Incorrect: memorize only a few things that are unavoidable. Otherwise, study concepts and contexts! b. be able to apply concepts to different situations. c. begin each assignment Wednesdays at 7am. Incorrect: you should begin and try to finish assignments way before an hour before they are due! d. hurriedly take tests one hour before their stop-time. Incorrect: you should begin and finish tests way before an hour before they are due! Questions 7-10 refer to the following situation A 55 year old male is in the ER having a myocardial infarction (heart attack, AKA “M.I.”), which is caused by coronary arteries that are clogged with fat and narrowed so that not enough oxygen–rich blood is getting to his heart. He admits that his daily nutrition is poor, consisting mainly of high-fat fast food. He has a family history of cardiac disease-- his father had a heart attack at age 46. The patient is obese and is a heavy cigarette smoker-- 2 PPD (packs per day). The patient said he had decided to take up jogging today and after a few minutes began having chest pain, nausea and shortness of breath. He went to the ER and was noted to have profuse diaphoresis (heavy sweating), tachycardia (rapid heart rate), and significant changes on his electrocardiogram (ECG or EKG). The patient recovers from this acute heart attack but his heart is so damaged that subsequently he has many episodes of congestive heart failure and many hospitalizations. 3 7. Without even having further knowledge of course material related to MI’s, you can tell a lot about the scenario from careful reading and knowledge of basic patho verbiage. Example: The paragraph above suggests that the direct pathophysiologic etiology of the heart attack (MI) is most likely related to a. not eating green vegetables. Incorrect: not eating nutritiously is not a DIRECT patho etiology; we do have a hint that he has a risk factor of eating unhealthily (fast food), but don’t “overthink.” b. congestive heart failure. Incorrect: heart failure is a sequela in this context. c. lack of oxygen that narrows the coronary arteries. . Incorrect: the scenario tells you that the MI is “caused by coronary arteries that are clogged with fat and narrowed so that not enough oxygen–rich blood is getting to his heart.” It doesn’t say that oxygen causes the narrowing, which is what this answer says. d. oxygen not reaching tissue that is distal to narrowing of the coronary arteries. See sentence above… also, you are asked to use the knowledge from the RRD about what the term distal means. (See top of page 5 of RRD 1 for reviewing that info) 8. In reading the paragraph above, it is easy to find 4 risk factors—things that “set the stage” for this patient to have a heart attack. They include all the following EXCEPT a. being a heavy cigarette smoker. b. having profuse diaphoresis. This is the correct choice, because it is one of the S&S, not a risk factor. c. a parent with heart disease. d. high-fat diet. 9. Which mini-concept map do you think best describes accurate linkage between underlying pathophysiology and signs and symptoms (S&S) described in this scenario? a. Jogging increased heart rateblood pumped throughout body fastertissues (including lungs and stomach) receive too much bloodpatient complains of shortness of breath and nausea. Incorrect: there is nothing about this situation that implies that “too much blood” is being pumped to the organs. b. History of heart disease in familypatient worries about it constantlybecomes anxioussmokes too muchnicotine causes narrowing of all arteries in body, including coronariesheart attack from narrowed coronaries. c. High levels of fat in the blood from high-fat dietclogs in coronary arteries develop over time oxygenated blood cannot get to distal tissues of heartunoxygenated tissues “cry out” (send pain messages to brain) patient complains of chest pain. d. Obesity increased pressure on diaphragmbreathing becomes more difficultshortness of breathless oxygen EKG changes. 4 10. A sequela of the MI was a. having to be hospitalized frequently because of problems associated with the damaged heart. b. having to be hospitalized frequently with repeat heart attacks. c. needing to jog more often. d. continuing to smoke 2 PPD. 11. The most likely sequela of not submitting a weekly assignment by Wednesdays at 8am is a. being allowed to submit the assignment later because you had a bad cold during the days leading up to the assignment due date. Incorrect: if a student waits till the last minute to submit an assignment, there is increased risk of something going wrong, such as not feeling well. b. getting a zero on that assignment. (If there are special, urgent contingencies, especially ones that have documentation, a student may email before the due date to explain why he or she cannot get the assignment in on time. The excuse may or may not be accepted and extra time may or may not be allowed, depending on the circumstances.) c. instructor’s lack of concern, because you will be able to drop the lowest assignment grade. Incorrect: no assignment grades are dropped d. being allowed to submit the assignment later because you thought it wasn’t due till the next day. Incorrect: In this course there are many reminders of due dates and consequences of not getting assignments and tests in on time. To be considered for late submission, a student needs a documented, urgent excuse. 12. At the end of the semester, a student has a total assignment average grade of 100% and a 69.7% total test average grade. What grade did the student make for this semester (see syllabus)? a. 84.85% (B) b. 69.7 % (D) (See box on last page of Course Overview or look in your syllabus) c. 71.43% (C) d. 93.03% (A) 13. Student Katniss Everdeen has been submitting her assignments and tests before the deadlines and making good grades. One day during an unexpected storm, her internet connection goes down in the middle of a test. Since she is a consistently focused and dedicated student, what action do you think she will take? She will a. email her coach that “A pack of wolfmutts attacked and ate my computer. Can I take the test tomorrow?” b. resign herself to getting a zero, since she didn’t read the procedures in the syllabus and Course Overview. c. take the test the next day, since she knows that multiple test entry and submission is allowed. d. immediately email her coach, instructor, and tech support with a detailed report of what happened. 5 14. After not eating since breakfast 6 hours ago, a student taking a test notices a period of hunger and fatigue. He doesn’t have access to food because he is taking the test. About 10 minutes later, though, he begins to feel ok again and finishes the test with flying colors. What has happened in his body? a. A compensatory response called glycogenolysis allowed him to access stored glucose for energy. b. A decompensatory response occurred, in which adrenalin increased and caused more blood flow to the brain. c. Since his blood sugar was likely low, the heart underwent a compensatory response known as hypertrophy in order to increase blood flow to central organs. Incorrect: An acute hypoglycemia will not cause the heart to increase in size. Hypertrophy is a compensatory response that usually occurs over time. d. Using a control mechanism known as hyperventilation, the student was able to “blow off” excess CO2 and thus have a clearer thinking process. Incorrect: Often if a person hyperventilates, acid/base balance is thrown off (causing respiratory alkalosis) and this certainly would not help the thinking process. 15. Which sets of sentences match each other correctly? a. After several days of little sleep a student’s cold turns into pneumonia. Insomnia is a precipitating factor for the change. b. A person with a chronic lung disease gets pneumonia. The pneumonia is considered an acute illness. c. Freshly oxygenated blood flows from the aorta through coronary arteries to various parts of the heart muscle. Blockage in the coronaries would cause decreased oxygenation in the cardiac muscle tissue proximal to the blockage. Incorrect: The correct answer would have said “distal” to the blockage, meaning “beyond” the blockage. d. A and B. Genetic Influence in Disease 16. A child is born to a couple, one of whom is heterozygous for an autosomal dominant disease. The other parent is homozygous normal. What would be the child’s chances of having the disease? (Use a Punnett square to figure this out). a. 0% b. 25% c. 50% Heterozygous for autosomal DOMINANT: Dd (with the “big D” being the BAD gene). Homozygous normal: dd (normal gene in these disorders is the “little,” recessive gene—just the opposite of autosomal recessive diseases.) So do Punnett square and the possible kids’ genotypes are: Dd Dd dd dd. With homozygous dominant disorders, if you have a “big letter” in the genotype, you WILL have the disease. d. 75% 6 17. A child is born to a couple, one of whom is a carrier for a sex-linked recessive disease. The other parent has the disease (“having” the disease means the phenotype is seen—ie, S&S). What would be the chances that the couple has a child with the disease? (Use a Punnett square to figure this out.) a. 0% b. 25% c. 50% In sex-linked diseases, ONLY the woman can be a carrier, so you know that it is the mom that has the genotype of XGXg (in any kind of recessive disorder, the “little” letter—the recessive gene—is the BAD gene and the big letter is the NORMAL gene, so this woman does not HAVE the disease, since the “big” dominant NORMAL gene is overcoming the recessive BAD gene). The dad, then, HAS the disease, so we know he MUST have the little recessive, BAD gene on his X chromosome (part of the definition of a sex-linked disease is that it is interchangeable with “X-linked”). So his genotyped is XgY. Punnett square: XGXg (female carrier—won’t have disease). XgXg—female WITH the disease (a bit unusual—stats show males get the disease much more often), XGY (male with normal genotype), XgY (male WITH the disease). d. 75% 18. In the question above, what are the chances that the child will be a carrier? a. 0% b. 25% (see explan. above) c. 50% d. 75% 19. An RN is taking care of a cocaine addict who has just given birth to a baby with a teratogenic defect. A student nurse asks him what the probable etiology was. The RN shows understanding of genetic disorders when he says a. “It’s hard to know the exact cause, but it’s likely that fetal chromosomal development was impaired by the mom’s intra-pregnancy cocaine ingestion.” b. “The baby inherited a structural chromosomal defect that resulted in a problem called aneuploidy.” Aneuploidy is a problem of numbers, not structure. Also, this question is linking teratogenic defect to intra-pregnancy issues, not inherited one such as suggested in this answer. c. “The baby inherited a gene that caused a defect called trisomy 21.” A single gene doesn’t cause trisomy 21—an extra chromosome does. Also, this question is linking teratogenic defect to intra-pregnancy issues, not inherited one such as suggested in this answer. d. “Since the little guy was born with the Philadelphia chromosome, he will be a life-long Phillies fan.” 20. A child with sickle cell anemia presents with pain all over, especially the joints. Which of the following best links the patho with S&S? a. Cyst formation in the kidneys leads to blood spillage from the circulation into the urine, thus causing anemia. This sentence might be correct if we were talking about PKD. b. A single-gene mutation causes malfunction of genetic coding for clotting properties, leading to bleeding and ischemic pain of the joints. This sentence might be correct if we were talking about hemophilia. c. Chromosomal aberrancy causes malformation of RBCs in the blood supply to the joints and subsequent pain due to lack of oxygen. This is kind of a hodge-podge answer that is incorrect. d. A single-gene mutation causes malfunction in RBC O2-carrying capacity, leading to ischemic pain in the joint tissues. 7 Questions 22-26 are based on this scenario: A 25-year old pregnant women voices concerns about the genetic health of her fetus because she has sickle cell disease. Her husband has been genetically tested and has a heterozygous genotype. Tips: The questions assume that you are taking the following critical thinking steps: • You read the question and by knowing (from your readings) that sickle cell disease is an autosomal recessive disease and thus has a certain pattern of inheritance (do your Punnett square work below) • You know that in most genetic diseases, the gene that has been mutated will not code properly for certain proteins that are important for certain normal functions. You will ask yourself, in sickle cell, how does the mutation lead to the phenotype, ie, the signs and symptoms? First figure out the Punnett square for this couple (blue highlight) & then the possible kids’ genotypes (yellow) — (use the letter “s” for the parents’ genotypes—stands for sickle cell; see pgs 50-51 as needed): s 21. Mom’s genotype is a. ss b. Ss c. SS d. none of the above. 22. Which is true about the dad? a. His genotype is ss. b. He is a carrier of sickle cell. c. He likely has the typical S&S of sickle cell. d. All of the above. 23. What is the percent possibility of this couple’s child having a completely normal genotype? a. 0% (“SS” would be completely normal in this situation and it is not possible with these parents) b. 25% c. 50% d. 100% 24. What is the percent possibility of this couple’s child having sickle cell trait? a. 0% b. 25% c. 50% Having the trait means that the genotype is exactly the same as a carrier, but normally when you are a carrier, you have NO S&S of the disease. Rarely, the “small, bad guy” gene “peeks out” and the person will have some S&S which are usually milder than that of the full blown genotype, ss. d. 75% 25. What is the percent possibility of this couple’s child having the disease, sickle cell anemia? a. 0% b. 25% c. 50% (“ss”) d. 75% 8 26. The parents of a new baby with Down’s syndrome ask their nurse what to expect. She bases her answer on her understanding that the child will have a. developmental problems brought on by a sex-linked monosomy. This answer has several things wrong, including that Down’s is a chromosomal polysomy, not a single gene disorder. b. developmental problems brought on by the pathologic interaction of 3 chromosomes where there should be only two. c. a phenotype based on defective mitochondrial protein synthesis that created aneuploidy. This answer has several things wrong, including that Down’s is a nucleic problem, not mitochondrial. d. the phenotype of diminished IQ and physical differences that are caused by a single-gene disorder. The first part matches; the second part doesn’t. 27. A person has hemophilia. Which is the correct genotype? a. HH This would be a normal genotype in the context of an autosomal (not sex-linked) recessive disorder. b. XHY This would be a normal genotype in the context of sex-linked disorders. c. XhY This is a classic genotype for a sex-linked single-gene disorder, which hemophilia is. d. hh This would be the correct genotype for someone who has an autosomal (not sex-linked) recessive disorder. 28. The phenotype of the person in question 27 includes having ________ because _. a. joint pain : the gene that codes for coagulation factors is defective, causing easy bleeding into the joints. b. joint pain : the joint tissue is oxygen-starved due to deformed hemoglobin in the RBCs. This would be correct if we were talking about sickle cell anemia. c. simian facial features : hemophilia is a teratogenic disorder caused by maternal alcohol abuse. d. severely shortened arms and legs : a drug called thalidomide caused the mutated genotype. Intracellular Function and Disorders Questions 29-31 apply to this scenario: The parents of a five year old girl complain anxiously to her pediatrician that in the last couple of weeks, no matter how much she eats, she keeps losing weight. She appears quite thin, well below her normal weight. Her blood sugar is 300 (normal range 75-110). She is diagnosed with Type I diabetes mellitus (DM 1). 29. In this scenario, the explanation that bests links pathophysiology with S&S in this child is that in DM1, the pancreas a. quits producing glucagon so that glycogen stores are inaccessible, thus causing weight loss. b. increases insulin production so that glucose stays in the blood, causing hyperglycemia. c. quits producing insulin so that glycogenolysis is stimulated and too much glucose enters the blood. Glycogenolysis is stimulated by the hormone glucagon when the body in HYPOglycemic. In DM & in this scenario, the patient is HYPERglycemic. d. quits producing insulin so that glucose cannot be used as energy in the cells, thus causing the body to burn up fat and protein for energy. 9 30. If ABGs were done on this patient, you would expect all the following EXCEPT: a. a blood pH of 7.32 because sustained gluconeogenesis causes acidic byproducts to accumulate. b. a HCO3 of 20 because the high numbers of acids in her body “take over” and “overcome” the HCO3, which then diminishes in number. c. a HCO3 of 30 because the low numbers of acids in her body stimulate increase in HCO3. If you chose this one you were likely overthinking. The others all fit metabolic acidosis. d. this acid/base imbalance to be called metabolic acidosis because it is an acidotic state caused by a metabolic disorder. 31. This girl’s body needs to compensate for the acid/base imbalance noted above. Knowing that the lungs will compensate when the “metabolic” side is “sick” and the kidneys will compensate when the lungs are “sick,” which compensatory response would you expect? a. Hyperventilation --increased respiratory rate (RR)-- to “blow off” CO2; this is the lungs’ way to get rid of acids. b. Hypoventilation—decreased RR-- to “hold onto” CO2, since CO2 is an alkali that will counteract the acidosis. CO2 is an acid… it will make acidosis worse. c. Kidneys will excrete more HCO3 into the urine to get rid of acidic byproducts. Remember the kidneys are considered “sick” in metabolic problems and therefore cannot help. d. By hyperventilating and blowing off CO2, the body will bring the pH down to normal range. The lungs will indeed blow off CO2, and acid, which will bring pH UP to normal range, not DOWN. Ex—it will bring 7.32 up to 7.38. 32. A child accidentally ingests an insecticide with the ingredient cyanide. Knowing that cyanide suppresses the actions of cytochrome oxidase in the electron transport chain, what signs might an RN expect and why? (see page 2 of metabolic pathway concept map) a. Ketonuria due to increased glycogenesis. Gluconeogenesis has byproducts of ketones; glycogenesis does not. But neither have anything to do with this scenario. b. Confusion due to glycolysis. Glycolysis is the normal first step inside a cell of all glucose molecules in the metabolic pathway, so it’s a normal process & doesn’t cause confusion. c. Mild euphoria due to enhanced production of ATP. Anything that suppresses cytochrome oxidase will also SUPPRESS, not ENHANCE ATP. d. Shortness of breath due to decreased ATP to use for the work of breathing. 33. A patient with a serum calcium of 6.0 (norm = 8.5- 10.5) is most likely to because . a. be lethargic: the cells are hypopolarized. b. have muscle spasms: more Na+ has entered the cells. The state of being hypocalcemia causes cells to be more permeable to INFLUX of Na+ increases cations in cell increased positivity of the RMP moves RMP electrical setting closer to the “goal pole” of +30mV hypopolarization pathologically less time/distance to reach depolarization cells are hypersensitive & may spasm. c. be weak: more Na+ has left the cells. d. have hyperirritable muscles: the cells are hyperpolarized. 34. A patient has been vomiting copiously for 3 days. He is probably in because . a. metabolic acidosis : vomiting often leads to hyperventilation. b. respiratory alkalosis : vomiting often leads to hyperventilation c. metabolic alkalosis : vomiting of the normal acidic digestive secretions of the stomach eventually depletes the body’s acids. d. metabolic acidosis : vomiting of the normal acidic digestive secretions of the stomach eventually depletes the body’s acids. 10 Questions 35-37 apply to this scenario: A 78 year old patient with cancer of the esophagus has not been able to eat, has lost 80 pounds and appears cachectic (extremely thin & wasted; the noun is cachexia). He is struggling to breathe, is very weak, and has generalized edema. His breath smells fruity, like acetone. He has an oxygen (O2) saturation level of only 80% (normal is 98 to 100%...less than 95 means patient’s cells are probably becoming hypoxic). His pH is 7.14 and HCO3 18. (normal HCO3 is 24-28) 35. What acid/base imbalance is he in? a. respiratory alkalosis. b. metabolic alkalosis. c. metabolic acidosis. Low ph = acidosis; low HCO3 = metabolic. d. respiratory acidosis. 36. Link aspects of his clinical presentation to the pathophysiology underlying them. a. Patient can’t eat hypoglycemiainsulin secreted from pancreas triggers glycogenolysis as a back-up plan raises blood sugar but byproducts include ketones. b. Difficulty breathing increased metabolic needsuses up all energy sources body begins to use HCO3 as source of energyHCO3 depleted HCO3 decreases to 18, causing pH to increase from normal to 7.14. Tip: even if you weren’t sure about everything else, the part of the answer that should stand out as wrong is the fact that if HCO3 decreases (ie, “the alkali guy” decreases), then acidity will INCREASE and the pH will go DOWN even more, not INCREASE. c. Chronic illnessincreased stressincrease in counterregulatory hormonesglycogenesis triggeredtoo much glucose being stored rather than being readily availablecachexia. d. Given the description of the patient's debilitated state, he is probably in sustained gluconeogenesisgives energy but also increases accumulation of ketones body tries to get rid of them via many ways, including as acetone in the breath. 37. A scene in the ER: A CIA operative who has had no previous medical history presents with initial complaints of nausea, vomiting, severe weakness. Now he is also short of breath. His pH is 7.20 and his HCO3 is 17. What is most likely going on in his body? a. Poisoning (by an enemy spy) cellular hypoxiacells must repeatedly go through anaerobic glycolysis to gain some ATPSincreases pyruvatelactic acidosis metabolic acidosis. Normally, when there is plenty of O2, the first step in breaking down glucose is AEROBIC glycolysis. But if there is not enough O2 (hypoxia), the back-up system is ANAEROBIC glycolysis, whose downside is accumulation of acids. This can cause acidosis. Because a metabolic reason caused this (the poisoning) and not a respiratory problem like hypercapnea (retention of CO2), metabolic acidosis would be the end result. Also, as soon as you see that the HCO3 is out of normal range, you KNOW the problem is metabolic. b. Poisoning (by an enemy spy) hypoxiacells must continuously go through aerobic glycolysis instead of continuing down normal metabolic pathway low ATPSrespiratory acidosis. Aerobic glycolysis is normal, so this doesn’t fit. c. Gastrointestinal flu can’t eat low blood sugarglucagon secretedtriggers glycogenolysis glucose released into blood, but also there are acidotic byproducts that must be countered by more HCO3increased alkalinitymetabolic alkalosis. This is a hodge-podge that doesn’t make a lot of sense. d. Job stresslow oxygenation body compensates by increasing respiratory rate (hyperventilation) too much CO2 blown off respiratory alkalosis. A CIA operative would have a lot of job stress, and anxiety does cause respiratory alkalosis, but the low pH and low HCO3 point to metabolic acidosis. 11 38. A patient in the ER is about to get a laceration stitched up. First the ER nurse practitioner (NP) will infiltrate the area with Lidocaine, a drug that will prevent the patient from feeling pain as the stitches go in. The medication’s mechanism of action is to change the permeability of nerve cell membranes so that they decrease the number of Na+ ions that are normally allowed to come into the cell. Using critical thinking and knowledge of RMP issues, what do you think is the next step? a. The nerve cells in the area become filled with anions and the RMP is reset from -90mV to -60mV. b. Because of the increased influx of cations, the local nerve cell membranes become more positively charged. c. Because of the decreased influx of cations, the local nerve cell RMPs will be reset from -90mV to -120mV. Less-than-normal Na+ enter the cell, thus causing the RMP to be more negative (-120) d. The sodium/potassium pump of the cell membranes will cease to work properly, and the cells will become incapable of holding their normal RMP charge. 39. Link the correct answer in question 39 with the effect of numbing the skin in the area to be stitched. a. Since the RMPs of the area nerve cells are now more positively charged, they are hypopolarized and therefore will conduct pain sensations very slowly or not at all. b. Since the RMPs of the area nerve cells are now more negatively charged, they are hyperpolarized and therefore will conduct pain sensations very slowly or not at all. The RMP setting of -120 is now “further away” from the “goal pole” of +30mV. The process of depolarization & “doing its job” is now much slower for the nerve cell, to the point of very sluggish pain signals to the brain…. thus the area is anesthetized. c. Since the RMPs of the area nerve cells are now more negatively charged, they are hypopolarized and therefore will be so hyperactive that pain sensation will be negligible. d. Since the RMPs of the area nerve cells are now more positively charged, they are hyperpolarized and therefore will conduct pain sensations very slowly or not at all. 40. Patho student Haymitch Abernathy spent 4 days in the hospital with pancreatitis. He gets out on a Wednesday evening feeling much better but knows he missed the 8am deadline for weekly assignment submission. What should he do, according to course policy? a. Send an email to the instructor and his coach right away to explain about his hospitalization, understanding that excuses must be offered within 24 hours after the deadline. b. Scan his doctor note and email the copy to his coach and instructor. c. Opt to use this assignment zero score as the one grade he can drop at the end of the semester. d. A and B. Alterations in Fluids and Electrolytes 1. Remember the patient in Assignment #1, with cancer who can’t eat and has lost 80 pounds? Let’s add to his assessment findings: let’s say he has generalized edema and a serum protein of 4gm/dl (normal = 6.0 to 8.3 gm/dl ). Which is the most accurate mini-concept map linking low protein with edema? a. hypoproteinemia concentration in blood is now lower than the normal concentration of fluids inside cells fluid goes from B to T. b. hypoproteinemia concentration in blood is now higher than the normal concentration of fluids inside cells fluid goes from B to T c. hypoproteinemia blood is now hyperosmolar compared to the cells fluid goes from T to B d. hyperproteinemiablood now has lower oncotic pressure than normal fluid goes from T to B 2. All of the following are accurate possible findings in the patient above EXCEPT that a. he has confusion due swollen brain cells. b. he has crackles in his lungs from fluid in the alveoli (lung tissue). c. his serum osmolality is 302 (norm = 280- 295). d. he will need a hypertonic IV solution to return fluid status to normal. Rationales for questions 1 & 2: After something has changed the concentration status of the blood, figure out which has the higher concentration of solutes. Does blood (B) now have a higher concentration than tissue (T)? Or does T now have a higher concentration than B? Fluids will always move by the principle of osmosis TOWARDS the higher concentration, higher osmolality, higher tonicity, higher oncotic pressure, etc (all these terms have the same PRINCIPLES driving them.) Remember: CONCENTRATION CALLS! and OSMOLALITY ORDERS! In this question, proteins in the blood have diminished, so the blood has become LESS concentrated than normal, ie less concentrated than the tissues, which INITIALLY are normal concentration. But when the CHANGED blood (now HYPOproteinemic compared to the tissues NORMAL protein levels) gets to the tissue, an osmotic shift BEGINS. That shift will be that fluid will be “called in” to the higher concentration—the TISSUE in this case. So with fluid going INTO the tissues, you then develop edema, which explains the next question….“Swollen” brain cells means edema in the brain; crackles in the lungs means edema in the lung tissue; a hypertonic IV is appropriate to help REVERSE edema (this treatment will quickly change the blood concentration to hypertonicity --B more concentrated than T now—so that water will COME OUT of cells). So, C is the OUTLIER—remember, this is an EXCEPT question, so C, with its HIGH osmolality is the one that doesn’t fit with the rest. Summary: A, B, D all fit with this scenario and C does not, so C is the answer. 3. A 28-year-old man presents with a low blood pressure due to blood loss from a gunshot wound. The regulatory action that will best compensate for this patient’s fluid volume deficit is: a. increased action of the natriuretic peptide system. b. increased action of the RAAS. c. inhibition of renin secretion. d. conversion of aldosterone into angiotensin II. 4. As a result of the action in the previous question, all the following will occur EXCEPT: a. the patient’s body will “hang on” to fluids. b. Na+ will be retained by the kidneys. c. water excretion into the urine will increase. d. blood pressure will increase. Rationale for 3 & 4: When there is a diminished blood volume (fluid volume DEFICIT) sensed by the kidneys, they respond by secreting renin; renin stimulates the secretion of aldosterone from the adrenal cortex aldosterone “tells” the kidneys to hang on to Na by not excreting it in the urine & instead keeping it in the blood stream when the kidneys hang on to Na, H2O follow. As a result of hanging on to H2O in the body, urine output is DECREASED and blood volume is INCREASED. Also, renin stimulates the process of angiotensin II creation; angiotensin II constricts blood vessels in the periphery blood volume that normally circulates out to peripheral vessels is decreased due to the constriction, so that a larger part of the blood volume can be shunted to the central areas where it is most needed—heart, lungs, kidneys. So in essence the main, most important circulatory areas have a compensatory increase in volume (and a much needed increase in blood pressure), whereas the periphery gets a decrease (that’s why this patient probably has cool & pale hands & feet). Answer 3A is wrong because the natriuretic system kicks in when the heart senses an excessive amount of volume returning to it atrial natriuretic peptide or b-type natriuretic peptide is secreted by the heart & the kidneys respond by increasing urination, therefore reducing the fluid volume; a reduction in blood volume is NOT what this person needs! Inhibition of renin secretion (3C) is the opposite of what is needed in this case. 3D is wrong because aldosterone doesn’t convert into angiotensin II (be sure you know the basic steps of the RAAS). The explanation above should answer the “why” of question 4. A,B,D are all applicable to this scenario. C is the outlier, so it is the correct choice (As discussed above, part of the RAAS is to have aldosterone “tell” the kidneys to hang onto Na+, thus ALSO hanging onto water—keeping it in the blood-- instead of excreting in the urine). PEARL OF WISDOM: Any time you have a PROBLEM and then a COMPENSATION for the problem (just like when you are figuring out acidosis/alkalosis & compensations), be sure you clearly separate them in your mind: “Here’s the problem and what caused it. THEN here’s the body’s compensation for that problem. Or if you are given a scenario with the compensation, be sure you can trace it back to the problem… that’s called studying from both the “front door” and the “back door.” See the How-to” manual if you need more study tips like that. (Normal labs: Na+ = 135 to 145; K+ = 3.5 – 5.0; osmo = 280- 295; HCO3 = 22-28). 5. A patient is hospitalized in renal failure. Because of her kidneys’ inability to excrete water, she has generalized edema & a serum sodium of 129. Because the kidneys have also lost the ability to appropriately regulate potassium, she also has a serum potassium of 5.9. These lab results show: a. hypernatremia & hypokalemia. b. hyperkalemia & hyponatremia. c. hyperosmolality & hypernatremia. d. hypoosmolality & hypocalcemia. 6. In the previous question, the edema is most likely due to fluid shifting from the intravascular space into interstitial spaces secondary to all the following EXCEPT: a. hypertonicity of the plasma space. b. hypotonicity of the plasma space. c. hypoosmolality of the blood. d. diminished osmotic pressure of the blood. Rationale for #5: Na levels < 135 = hyponatremia, or “low sodium in the blood,” and K levels > 4.5 = hyperkalemia, or “high potassium in the blood.” Therefore answers A and C cannot be right, since they mention hypernatremia. And D is wrong because nothing in the lab results that I gave you in the scenario relates to calcium, so hypocalcemia is not correct. Pearl: Be sure to read your scenario thoroughly to understand what information you are given. But also don’t read anything MORE into it. Rationale for #6 In the beginning scenario you are told that the Na is low in the plasma space—serum Na of 129 (remember that the plasma space is also called “the blood,” the “intravascular space,” the “vasculature,” the “vascular space,” and so forth), so you already know that the patient is hyponatremic, which correlates with HYPOtonicity, not HYPERtonicity (answer B). When you are given a scenario in which the patient has edema, always correlate this with FLUID VOLUME OVERLOAD—picture a patient who for some reason (in this case “sick kidneys” which aren’t getting rid of H2O properly) has extra water in the blood, thus diluting it & decreasing its concentration—this goes along with decreased osmolality (C) and diminished osmotic pressure (D). Thus B, C, D go together, and will cause fluid to shift into the tissues, causing edema. [Remember, the tissues will initially be NORMAL in their osmolality & tonicity, therefore, their concentration is now greater than that of the blood, so according to the rule – CONCENTRATION CALLS—the tissue cells will pull water into them from the blood (“B to T”), causing edema.] Answer A is the outlier in this EXCEPT question, thus it is the correct answer. Pearl: Draw pictures! Now, did you see the similarities in questions 1,2, 5, & 6? In one way or another they ALL resulted in LESS concentration in the blood, thus the patient pictures were ultimately similar. Same thing with questions 7, 9-11, and some of the ones in question 14. Think about their commonalities and then think about situations that would be the opposite. 7. A patient has advanced liver disease. Blood tests reveal that his serum albumin (albumin is one of the protein molecules found in the blood) level is very low. What eventually happens in this patient situation? a. Water would shift from blood (B) to tissue (T) because of decreased plasma oncotic pressure. b. There would be an increased intravascular volume due to increased plasma oncotic pressure. c. There would be dehydrated brain cells due to fluid shifting from T to B. d. Water would shift from T to B because of increased osmolality of the vascular space. 8 The physiologic process underlying fluid shifts in the patient situation above is that a. “concentration calls” fluid into hypoosmolar compartments from hyperosmolar ones. b. the principle of diffusion results in albumin molecules going from lower to higher concentration. c. “concentration calls” fluid into compartments with higher oncotic pressure from compartments with lower oncotic pressure. The tissues initially have normal oncotic/osmotic pressure, but compared to the blood that has become hypoosmolar, the tissues are the higher concentration so fluid is “called into” the tissue compartment from the lower-concentrated blood compartment. d. the proteinemia means that protein molecules will diffuse throughout the blood and tissue. 9. A patient who just came out of general anesthesia has lab work done. The serum osmo is 165. The nurse taking care of this patient suspects that the is due to . a. hyperosmolality: dehydration. b. hypoosmolality: syndrome of inappropriate ADH (SIADH). c. hypertonicity: SIADH. d. high oncotic pressure: a state of hyperpolarization inside the cells. 10. The nurse in the previous question (9) would expect all the following S&S EXCEPT: a. signs of cerebral edema such as irritability. b. signs of cerebral cell dehydration such as headache. c. pitting edema d. crackles in the lungs upon auscultation. 11. Re: the patient in the previous two questions (9 & 10): As an intervention to return the patient to normal serum osmolality, the nurse is likely to be ordered to hang an IV bag of because once the fluid is distributed in the blood it will and help return fluid compartment status to homeostasis. a. 0.45 NaCl: cause water to shift from tissue (T) to blood (B). b. 3% NaCl : cause water to shift from T to B. c. 0.25 NaCl : shift water from B to T. d. NS : shift water from B to T. Rationales: #9-- A low serum osmolality (165) means the patient is HYPOosmolar. B is correct, since the more ADH you have being secreted, the larger the volume the fluid in your circulation, which causes blood concentration to be diluted, thus giving rise to blood that is LESS concentrated than usual—hypoosmolality, hypotonicity, etc, would go along with this, NOT the “hypers” that you see as part of the rest of the answers. Pearl: After you figure out a CTQ like this, turn it around in various ways to help you expand your studying. For instance, you could ask yourself, “how could I change the question to make answer A the correct answer?” #10 Three of the answers in an EXCEPT question “go together.” In this case, A, C, & D paint a picture of someone with fluid overload, which is the sequela for SIADH. Too much ADH = too much volume being “held onto” & less volume of urine that is more concentrated (higher specific gravity) decreased osmolality in the vascular compartment water is “pulled” into the next door compartment, ie, the surrounding tissue that has normal osmolality edema signs of cerebral edema such as irritability (headache is also a definitive sign of cerebral edema, but in this case not due to cerebral dehydration). Pearl: A good example of critical thinking is to realize that headache and irritability are both examples of altered cerebral cell status, but the underlying mechanism can be different, depending on the scenario. #11 NS—normal saline—is isotonic fluid, meaning it is the same tonicity (and osmolality) as the blood). One way to think of tonicity, especially in nursespeak, is in terms of sodium traveling in the blood as NaCl. The normal tonicity (isotonic) of the blood is 0.9% NaCl. Any IV fluid lower than that—answers A & C—would further dilute the blood & cause worse edema. Giving NS (D) might eventually help the problem, but the best answer in terms of quickest way to get fluid to come back from T to B is to give a hypertonic fluid such as 3%NS (B). 12. A patient who is having hyposecretion of ADH (antidiuretic hormone) would MOST LIKELY have the following sign: a. serum osmolality of 270. b. oliguria (low urine output). c. serum osmolality of 300. d. edema. Rationale: Hyposecretion of ADH is the OPPOSITE picture of SIADH, in which one would have HYPERsecretion of ADH, low osmolality due to fluid overload, decreased urine output, and edema. Not enough ADH results in S&S of fluid volume deficit, which would include a high osmolality. (FYI--This state, the opposite of SIADH, is called diabetes insipidus (DI)…we will have info on DI later in the semester, but as you can see, you don’t need a particular name to figure out fluid shifts, if you are provided certain info and go step by step). Pearl: Again, be sure that all parts of your patient picture are consistent, that taken together it all makes sense. As corrected above, A, B & D paint a picture of ADH hypersecretion. C is the only one that fits with hyposecretion of ADH. 13. If you had a patient whose labwork showed that he was hyperproteinemic, what would you know about that patient? a. He has a low osmotic pressure. b. He has a low blood oncotic pressure. c. His blood is more concentrated than usual. d. You may need to hang an IV bottle of albumin. Rationale: If there are more than normal protein molecules in the blood, a person would have high oncotic pressure, high osmolality, higher concentration than normal blood—all the “highs” go together and all the “lows” go together. Certainly you wouldn’t want to give them MORE protein (D). 14. You have two patients whose serum osmolality results are as follows: Albus Dumbledore (Mr. D.) has a serum osmolality of 263. Minerva McGonagall (Ms. M) has a serum osmolality of 326. (normal serum osmo = 280- 295). Based on understanding the links between fluid imbalances, lab results, and S&S, you will expect that a. Ms. M. will have an overall puffy appearance. b. Mr. D will have poor skin turgor and dry mucus membranes. c. Ms. M. will need a hypertonic IV to get her fluid status back to normal. d. Mr. D will have generalized pitting edema. 15. On a more cellular level, which is true regarding the two patients in question 14? a. Mr. D’s tissue cells are likely shrunken from fluid being pulled from tissue to blood. b. Ms. M’s tissue cells are likely shrunken from fluid being pulled from tissue to blood. c. Ms. M has more dilute blood than Mr. D. d. Mr. D’s blood is hyperosmolar compared to normal. Rationale: Mr. D: serum osmo of 263 = hypoosmolar--means blood is more dilute, AKA LESS concentrated than usual, so when it flows to normal-concentrated tissues, “concentration calls” water from B to T and Mr. D becomes edematous (edema is “extra fluid in the tissues than normal”). A hypertonic (ie, hyperconcentrated) IV fluid like 3%NaCl can help return homeostasis. Ms. M: serum osmo of 326 = hyperosmolar--means blood is more concentrated than usual, so when it flows to normal- concentrated tissues, “concentration calls” water from T to B and Ms. M’s tissues are “sucked dry.” A hypotonic IV fluid like 0.45%NaCl can help return homeostasis. 16. A diabetic patient has pathological changes to his arteries that result in narrowing and blockage. He is diagnosed with gangrene of the toes (gangrene is when LOTS of cells die).. Lab work is drawn and shows an elevated CK. Which pathological process accurately explains this type of occurrence? a. necrosisgangreneischemia creatine kinase spillage into blood. b. infarct cellular differentiation release of urea. c. ischemia cell injuryswellingspillage of cellular enzymes into blood. d. metastasis superoxide dismutase release of free radicals. Rationale: C is the only answer that follows the general correct steps: in this case there has been ischemia from a blocked artery. Ischemia leads to hypoxia, which leads to loss of ATP for energy to drive processes like Na/K pump, which then fail and allow Na & water to freely come into the cell. This process culminates with swelling & leakiness and/or rupture of the cell membrane. The final step is leakage of intracellular substances (enzymes like CK) into the blood. 17. A patient says she has read that free radicals might be partly responsible for the development of her disease process. She wants to know more information and if there is anything that can counteract free radicals. The nurse’s explanation will be based on understanding that all of the following statements are true EXCEPT a. an example of a free radical is cytochrome oxide. b. free radical molecules initiate harmful reactions such as lipid peroxidation, which damages the lipids of cell membranes. c. the body’s way to counteract free radicals include enzymes such as superoxide dismutase. d. free radicals are molecules that are in a highly reactive state and can be calmed by taking certain vitamins. Rationale: Remember that this is an except question, so 3 things go together and are true. Free radicals are highly reactive and out-of-control molecules that can damage cells in several ways, including by destroying cell membranes (B, D). Our body can “calm” free radicals by using defusing enzymes (C) and vitamins (D). Answer A is wrong. Superoxide is an example of a free radical; cytochrome oxide is a made-up mix of a couple of terms (cytochrome oxidase is the enzyme that facilitates ECT reactions.) Pearl: You are looking for 3 correct pieces of information about free radicals, which are B, C, & D. Answer A is the outlier, the incorrect piece of information & therefore the correct answer. 18. A patient who smokes expresses concern to his nurse about the metaplastic changes of the bronchi that were seen during his bronchoscopy. The nurse bases her response on the knowledge that this type of cellular change is a. an irreversible cellular adaptation pattern. b. considered a precancerous cellular change. c. reversible if the change agent is removed. d. due to a physiologic hyperplasia. Rationale: To correctly answer this you must understand the different adaptive processes; atrophy, hypertrophy, hyperplasia, metaplasia—are all considered reversible if the irritant or change agent is removed. Therefore answer A can be eliminated. B is wrong because it is dysplasia that is considered to be a precancerous change. D is wrong because a metaplasia (change in type of cell) is not the same as any type of hyperplasia (increased number of cells). 19. Which sets of information are correctly linked? a. a patient with decreased RBC production: erythropoietin injections are needed to counteract overproliferation of red blood cells. b. arterial embolus blocks blood flow: decrease in venous circulation to tissue with resultant hypoxia of cells. c. gout: caused by diet high in urea. d. carbon monoxide: binds to Hgb in oxygen’s place. Rationale: Answer A is wrong because erythropoietin actually helps to increase proliferation of RBCs (not counteract) in patients such as those with kidney disease (since erythropoietin is made by the kidneys, a person in kidney failure would have less erythropoietin made & therefore be anemic from less RBCs). B is wrong because the second half implies that VEINS bring oxygen to the tissue; if a person has blockage in an artery, then the distal tissue becomes ischemic/hypoxic because of lack of arterial flow. (Veins carry deoxygenated blood.) C is wrong because gout is caused by a diet high in uric acid, a by-product of purine breakdown. Urea is a byproduct of other protein breakdown. Questions 20-23 refer to this scenario: A large bookcase falls upon an elderly man in his home. His left leg is pinned and he cannot move for 2 days until his neighbor finds him. He is hospitalized with massive trauma to his left leg, with resultant rhabdomyolysis (rhabdomyo means striated muscle tissue; lysis means “break down”). His pulses in that foot are unpalpable and the foot is pale and cool. Eventually his foot must be amputated. 20. Which mini-concept map, showing one event leading to the next, best fits with the scenario above? a. Massive mechanical trauma to leg distal arterial flow blocked ischemia to foot infarction of foot tissue amputation. b. Rhabdomyolysis damage to striated cells spreads to arteries proximal to the trauma ischemia infection amputation. Several things are wrong in this answer, one of them being that if there is any type of blockage of arterial flow, the tissue at risk is DISTAL to the blockage, as in correct answer A, not proximal. If you don’t understand this concept relating to how arteries flow, and the concepts of proximal and distal, be sure to review it until you understand it, and/or ask for help. c. Mechanical trauma interrupt cell membrane functions such as Na/K pump solute imbalance leg edema amputation. Swelling would occur in any kind of trauma, but the mechanisms have more to do with inflammatory response rather than direct solute imbalance. And edema isn’t a clear enough reason for amputation. It is not emphasized in the scenario in the way that arterial flow problems is emphasized. d. Cool foot tissues become too cold to conduct metabolic pathway functions cells become dormant distal arterial flow increases pathologically amputation. This is a hodge-podge of info… The foot is cool & pale because the arterial flow is decreased (not Increased), thus not bringing warm blood to the area. The cells will THEN not get O2 and have metabolic pathway problems. But the problems don’t BEGIN with a cool foot (as opposed to, say, frostbite). 21. Initial lab work is drawn that show a CK of 100,000 (normal serum CK is 0 to 200). Why is it so high? a. As a compensatory response, the production of the enzyme creatine kinase (CK) is increased in the cells and then is excreted to “clean up” the cellular debris. CK production doesn’t increase, per se; the level of it increases in the blood because injured cells are leaking it. b. As a result of injury, the striated cell membranes lose integrity and there is leakage of intracellular substances such as CK into the surrounding tissue bed. CK is an enzyme that is normally found INSIDE cells and in very small amts in the blood, so when it increases in the blood, we know there is cellular injury somewhere. c. Creatine kinase (CK) is only found in striated muscle cells, so it makes sense that rhabdomyolysis would result in greater release of CK. CK is a generic cellular substance found in many types of cells. When its blood levels rise, you only know there is injury, but it doesn’t tell you exactly what tissue is injured. d. Local tissue response to injury includes release of toxic, lytic substances such as CK. Very large amounts of CK can be problematic for the kidneys to deal with, and in that way it could in a way be considered toxic at high levels. But it is not normally considered toxic nor lytic. 22. Because of massive cellular injury, myoglobin leaks from cells into blood. The patient develops kidney failure from this myoglobinemia. All the following are true about this situation EXCEPT a. the patient may need injections of erythropoietin because of the kidney failure. b. myoglobinuria will likely be present. c. erythropoietin will be dangerously high in the blood secondary to kidney involvement. In the long run, a person with kidney failure often gets anemic because of LOW levels of erythropoietin, not HIGH levels of it. d. the etiology of the kidney failure is the inability of the kidneys to process such high amounts of myoglobin. 23. After many months the patient finally has recovered enough to be able to get up and have some physical therapy. What change of the musculature will the therapist have to deal with in the injured leg (besides loss of a foot)? a. Presence of decubiti because of scarring. b. Muscle cell shrinkage called atrophy. This is sometimes called disuse atrophy, because as the cells are not used & stimulated, they shrink in size. c. Increase in numbers of muscle cells, called hyperplasia d. Hypertrophy of the striated muscle cells. 24. Which correctly links the picture below with its name and an example? a. D = dysplasia. Example: pre-cancerous cells on a biopsy. The cells are not completely wild & undifferentiated, like cancer cells are (E) but there is enough deviation from normal to cause worry. b. C = hypertrophy. Ex: the heart undergoes hypertrophy when stressed. The heart does undergo hypertrophy when stressed, but the definition of hypertrophy—individual cells that enlarge—goes with picture B, not C. c. E = cancer cells. Ex: increased cellular differentiation of the skin after sun exposure. Picture E is of cancer cells, but they are DEcreased in their differentiation, not INcreased. Remember that the more differentiated a cell is, the more specialized and complex it is; cancer cells are the opposite—they grow via a process called anaplasia— lack of differentiation. d. B = hyperplasia. Ex: BPH—benign prostatic hyperplasia. Hyperplasia is when cells multiply, so picture C (not B) is hyperplasia. Notice the cells aren’t bigger—just more of them than normal. Tissue cells Normal A. B. C. D. E. 25. A patient that has been recently diagnosed with a neuroma on the sole of his foot is very anxious. Of the following, which information shows that the nurse understands the nomenclature of neoplasms when explaining the situation to the patient? a. “You should have the neuroma removed, as this is a cancer that will spread to other parts of the body.” b. “This is most likely a malignancy that will metastasize to your lymph nodes.” c. “Neuromas are benign growths that usually will not spread.” d. “You will soon have the irresistible urge to put on tap shoes and dance in a Broadway musical.” Rationale: If this were a cancerous growth, the name would be neuroblastoma. Pearl: Note that A & B are essentially saying very close to the same thing, so it wouldn’t have made sense to choose one of them. You can rule out D too in this case (even though neuromas are not a form of cancer, they are still painful & certainly wouldn’t trigger the desire to tap dance—ouch! ) So that leaves C. 26. A family nurse practitioner (FNP) tells a patient that her biopsy shows leiomyosarcoma staged at T2N2M0. This patient has a a. benign tumor of the endometrium. b. smooth muscle malignancy that has spread to the lymph nodes. c. a malignancy of the uterus that has spread to distant sites. d. muscle cell tumor that is a carcinoma. Rationale: The “T” of staging means “is there a malignant tumor?” The fact that it is staged at T1 automatically gives you the answer “yes,” so you can rule out A. N2 means lymph node involvement but M0 means no distant metastasis, so rule out C. The nomenclature of the growth means (sarcoma) that it is a malignant connective tissue growth, not an epithelial growth (carcinoma). So you are left with B, which fits with all the information given in the stem of the question. 27. Which mini-concept map has correct linkage in describing cancer genesis? a. angiogenesiscachexialack of nutritioncellular starvationcancerous changes b. growth factor signalsincreased cellular differentiationanaplasiacancer. c. oncogeneclonal proliferationincreased cellular differentiationcancer. d. oncogeneclonal proliferationanaplasiacancer cells. 28. A 59 year old man is diagnosed with CML—chronic myelocytic leukemia. All of the following help to explain the genetic etiology of the CML EXCEPT a. a chromosomal structural defect called translocation occurs. b. pieces of two chromosomes are exchanged. c. a chromosomal aneuploidy defect called translocation occurs. An aneuploidy is a chromosomal problem of numbers. For instance, trisomy 21—Down’s syndrome—is a problem of too many chromosomes, so it is an aneuploidy (specifically it is a polysomy, and even MORE specifically, a trisomy). A translocation is a structural problem, so you have two words that shouldn’t be in the same sentence. d. a short, defective chromosome called the Philadelphia chromosome develops. 29. Link CML etiology with its S&S: a. Genes on a defective chromosome malfunction and code for extreme leukocytosis. b. Myelocytic leukocytes attack cells in the blood and cause changes known as The Philadelphia Story. c. A genetic defect causes cancerous changes in the blood vessels, producing hemangiosarcomas. Correct in general, except doesn’t apply to CML. d. Genes on an extra chromosome malfunction and cause defects in leukocyte development, resulting in leukopenia. Leukopenia means “less than normal leukocytes.” CML is a problem of leukocytosis—“too many” leukocytes. 30. All of the linkages below are correct EXCEPT a. cancer-related angiogenesis leaches nutrition from our cells cachexia, weakness. b. cancer injures prostate cells release into blood of high levels of a tumor marker called PSA (prostate-specific antigen) c. ingestion of foods high in preservatives increase genetic “hits” increased risk of cancer. d. age-related wear and tear of cells increased risk of cancerous lesions such as lipomas. This sentence is correct until “lipomas,” which are NON-cancerous lesions. Questions 1-3 refer to this scenario: A man presents to an ER with a large laceration sustained at a construction site a few hours before. The area around the laceration is erythematous, painful, and swollen. 1. The erythema and swelling can be explained at a cellular level by all the following EXCEPT a. mast cell degranulation and release of histamine. True (see concept map) b. pro-inflammatory prostaglandins released. True c. increased vasomotor tone (tightening) of the capillaries in the area. False statement, so this is the CORRECT answer. Any inflammatory response involves some degree of DECREASED vasomotor tone—ie, capillaries in the area must VASODILATE (relax, have less tone) in order for substances to “ooze out”-- leak out of the blood to go “help” healing in the tissue. So usually we equate “dilation and leakage” with inflammation. This is why you often see swelling with inflammation—the swelling is caused by the dilated blood vessels and accumulation of leakage. d. local reaction to acute phase reactants. True 2. The patient is given a TIG (tetanus immunoglobulin) injection because the wound is high risk for tetanus exposure and he doesn’t remember ever having a tetanus vaccination. The purpose of the TIG is to a. prevent any tetanus bacteria from activating the inflammatory system. Wrong—inflammation will be activated as soon as any cell in the body is irritated and/or injured. Giving antibodies (immunoglobulins)– the “IG” in TIG— doesn’t prevent inflammation. b. introduce tetanus bacteria so that the immunocyte system can create antibodies to tetanus. Wrong— TIG is antibodies, not the microbe itself. c. give the patient natural active acquired immunity. Wrong—the word “natural” implies that a person contracted tetanus (HAD the disease) and created their own antibodies as a result of the active disease. d. provide tetanus antibodies to fight any tetanus bacteria that might be present. CORRECT—just in case this person’s body was invaded by a tetanus bacteria, giving them antibodies NOW will help them fight the microbe NOW. This is called conferring artificial passive acquired immunity. 3. The patient (should or should not) be instructed to also get a tetanus vaccination, because . a. should: he needs protection against future tetanus exposure. CORRECT : passive immunity (when you DON’T make the antibodies in your own body, but are given them) is very short-lived. The antibodies that are GIVEN to you, that you DON’T create on your own, will disintegrate within a few weeks. So you WILL need a vaccination, which confers artificial ACTIVE immunity— having a weak tetanus injected in you will make you create your OWN antibodies, which are long-lived. b. should: the vaccination will provide additional passive immunity. Wrong—see above (vaccination and PASSIVE shouldn’t be in the same sentence; vACcination = ACtive) c. should not: the TIG is enough, as it will provide long term active acquired immunity Wrong—see above d. should not: the vaccine will do nothing for the current exposure. Wrong—see above. Look at this answer closely. The last part is true. A vaccination WILL NOT help a person RIGHT NOW, because creating your antibodies takes time. But the question asked should he go ahead and get a vaccination? Yes, he should. No, it won’t help him NOW, but it will help him if he ever gets a tetanus microbe inside his body in the future—his antibodies can THEN kill the microbe swiftly. 4. A microbe invades the body for the first time. Which statement is most likely about the processes that follow? a. Plasma cells (a type of B-lymphocyte) will immediately secrete T-cells specific to that microbe. Wrong. Plasma cells secrete antibodies, not T-cells. b. CD4 cells will introduce remnants of the microbe to the plasma cells, which directly phagocytize the remnants. Wrong— plasma cells are not phagocytes. They are a form of B lymphocyte. c. Antigens will be created from the memory cells of immunocytes. Wrong—doesn’t make sense. Don’t confuse the word antigen with the word antibody. d. Immunocytes will begin the process of developing memory to that microbe. Correct—During the inflammatory process, if a microbe is involved, the T-cells and/or B-cells are “called in” and begin to develop microbe-specific memory. Especially let’s focus on the antibodies… the Bcells will begin the memory process, and as a result, antibodies that are specific to that particular microbe will be formed and will be on hand for the next time the body “sees” that microbe. (Tcells do similar process, but don’t create antibodies.) 5. A patient has a systemic inflammation. All the following are likely associated with his condition EXCEPT a. increased acute phase reactants. True – acute phase reactants have the job of increasing inflammation as needed—“fuel on the fire”; especially they increase circulating in the blood when there is a systemic inflammation. b. lab results showing a high C-reactive protein (CRP). True—CRP is one of the acute phase reactants. c. lab results showing leukopenia. False, so this is CORRECT answer. During systemic inflammation, leukocytes will increase in number so as to participate in the various parts of the inflammatory response, especially neutrophils, which act as phagocytes (see concept map). So leukocytosis and neutrophilia are part of inflammation, not leukopenia (PENIA= “lower numbers than normal”). d. increased pro-inflammatory prostaglandins. True – remember that prostaglandins have two subcategories— the duty of INCREASING inflammation is called “pro-inflammatory.” The other types of prostaglandins are “protective”—they bolster certain aspects of body function 6. A baby who has received immunoglobulins against the “XYZ” virus via its mother’s milk now has a. natural active acquired immunity. Wrong—an example of this is getting chicken pox. b. natural passive acquired immunity. Correct—natural (from mom); passive = baby did NOT make its own antibodies. c. passive innate immunity. Wrong—mixed up terms. Remember that when we are talking about immunoglobulins, we are automatically thinking of the third line of defense – ACQUIRED immunity, not innate. (Innate involves first and second line of defense) d. active innate immunity. Wrong—see above about acquired vs innate. 7. The baby in the previous question will . a. have lifelong immunity to the XYZ virus because of receiving the immunoglobulins that are specific to that particular microbe. Wrong—can’t get lifelong immunity from receiving SOMEONE ELSE’s antibodies. b. develop temporary immunity to the XYZ virus due to receiving Mom’s antibodies that are specific to that particular microbe. Correct—passive acquired immunity is ok for right NOW, but the antibodies will disintegrate within a short time—hence “temporary.” c. now have complete 2nd line of defense protection, having received it in the breast milk. Wrong— remember that when we are talking about immunoglobulins, we are automatically thinking of the third line of defense d. develop alphabetophobia due overdose of anti-XYZ immunoglobulins. 8. A person starts Jazzercise for the first time and becomes very sore all over. The most appropriate self- treatment for this person is to , because . a. take an NSAID such as Aleve : it powerfully suppresses phospholipase enzymes in the arachidonic pathway. Wrong—steroids suppress phospholipase. NSAID are non-steroidal antiinflammatories that work further down in the arachidonic pathway. See page 19 of RRD. b. take an NSAID such as Advil : it is an effective suppressor of certain levels of pro-inflammatory prostaglandin activity. Correct c. go in for a CRP test: it will determine the degree of pain. Wrong --CRP is an acute phase reactant that will increase when you have an inflammation but it is very non-specific—you can’t judge degree of pain by that (besides that, FYI—everyone’s pain is different—not something that can be generically measured.) d. take an antihistamine: it will suppress steroidal influence. Wrong—we haven’t discussed antihistamines, but we have talked about histamine, which you know to be a substance that is part of the inflammatory response. So in a sense an anti-histamine suppresses a certain part of inflammation. Steroids also, in a much different way, suppress inflammation—you know this too—via suppressing prostaglandins. So antihistamines suppressing steroids doesn’t make sense. 9. A patient has been in the hospital for treatment of an infection. One day his BP drops to 80/50 (normal ~ 120/80), he has a fever of 102, and he becomes restless and confused. All the following are correct about this situation EXCEPT a. a likely diagnosis is septic shock, partly because his BP is low, and he has S&S related to low blood volume to the brain. True – the definition of shock is low BP that causes S&S. And since he has an infection, it makes sense that sepsis has become involved (sepsis— the inflammatory response to a systemic infection) b. a good mini-concept map would be: infection goes systemic (sepsis) increases circulating acute phase reactantssystemic vasodilationless blood centrally low BP. True—this is exactly how septic shock works. It is the massive vasodilation from massive, systemic inflammatory response that causes the BP go become so low that the patient can’t get enough blood to the brain restless, confused. c. a good mini-concept map would be: local infection gets worse invades lining of blood vessels in the arealocal sepsis develops chronic inflammation results in hypotension. False, so this is the CORRECT answer. The term “local sepsis” is an oxymoron—by definition, sepsis is not local but systemic. d. the patient’s blood work will show leukocytosis, neutrophilia, and high CRP as part of the high degree of inflammatory response in his body. True. See the table on the next page. It is numbered I-XIV. In the right column are words and phrases that link in some way with each of the numbered items on the left. In other words, this is a typical “matching” exercise. Fill out the table, and use it to answer questions 10-15 directly below. ONLY ONE ANSWER TO EACH LEFT-HAND TERM, AND DO NOT CHOOSE THE SAME ANSWER MORE THAN ONCE—CHOOSE THE BEST FIT. 10. Granuloma (#I) a. I b. N--local chronic inflammatory tissue reaction c. A d. F 11. Example of qualitative defect of “not enough” inflammatory function (#IV) a. K-- chemotactic defect – without chemotaxis, certain important cells (phagocytes, immunocytes) wouldn’t be “called” in to help at the site of a defense breach. b. L c. G d. N 12. Leukopenia (#V11) a. D b. E --example of quantitative defect of “not enough” inflammatory function—leukopenia means less numbers of WBCs than usual, making this a quantitative defect. c. K d. O 13. Part of inflammation in which vasomotor tone of capillaries “relaxes” (#X) a. H b. N c. A vasodilation d. J 14. Steroidal suppression of protective prostaglandins (#XII) a. B b. F c. M d. G –Remember that steroids do what you WANT them to do when they suppress the pro- inflammatory side of prostaglandins. So if someone gets a course of steroids for an acute back injury, and the patient feels better, it’s because the steroid is suppressing the inflammation that causes pain. If that person were to STAY on steroids for a long time, though, the side effects could include problems such as stomach ulcers. This risk is related to the fact that steroids are non-specific—as they are suppressing inflammation, they are also suppressing the “protective” aspect of prostaglandins, including protecting the stomach lining from stomach acid. So, long-term steroids use (such as for someone with chronic inflammatory diseases like autoimmune diseases) sometimes has bad side effects. This is an important concept. See RRD 3, page 14. 15. A way of conferring artificial active acquired immunity. (#XI) a. D b. A c. B booster shot—a booster is a vaccination shot that is given periodically to keep stimulating your immunocytes to create antibodies to certain microbes. Because you are stimulated to create your OWN antibodies, this is classified as an ACTIVE acquired immunity. The artificial part is because the microbe did not naturally make its way into your body—it was injected into your body artificially. d. C MATCH up words or phrases that are most appropriately related and then answer questions 10-15 above (10-15 are what you submit electronically). ONLY ONE ANSWER TO EACH LEFT-HAND TERM, AND DO NOT CHOOSE THE SAME ANSWER MORE THAN ONCE—CHOOSE THE BEST FIT. I. granuloma N A. vasodilation II. erythema I B. booster shot III. decrease in phagocytic functions J C. steroid IV. example of qualitative defect of “not enough” inflammatory function K D. oncogenic event resulting in defective creation of multiple cells V. breach of first line of defense M E. example of quantitative defect of “not enough” inflammatory function VI. serosanguinous exudate H F. degranulation releases histamine, prostaglandins, leukotrienes VII. leukopenia E G. stomach ulcers VIII. benign neoplasm of the bone O H. wound fluid leakage contains serous fluid and blood IX. mast cells of tissue F I. reddened, inflamed appearance of skin X. part of inflammation in which vasomotor tone of capillaries “relaxes” A J. results in decreased inflammatory response and less healing ability K. chemotactic defect XI. a way of conferring artificial active acquired immunity B L. can have negative effect on normal bowel flora, resulting in breach of body’s defenses XII. steroidal suppression of protective prostaglandins G M. Sjogren’s syndrome XIII. suppresses pro-inflammatory aspects of prostaglandins C N. local chronic inflammatory tissue reaction XIV. antibiotics L O. osteoma 16. A patient has just had a liver transplant and is beginning to display S&S consistent with rejection. The following is most likely a true statement about the situation: a. The patient is undergoing an autoimmune hypersensitivity. Wrong—no evidence of self-attack, so no autoimmune problem. b. The patient is undergoing an IgE-mediated hypersensitivity reaction. Wrong—IgE-mediated hypersensitivities are basically allergic reactions—doesn’t fit scenario. c. The donor’s immunoglobulins are attacking the HLA’s on the patient’s RBCs. Wrong—RBCs don’t have HLAs; HLAs are found on almost all tissue cells’ cell membranes ESCEPT RBCs—RBCs instead have ABO & Rh. d. The recipient’s immunoglobulins are attacking the HLA’s on the donor liver. Correct—rejection is a type of alloimmune hypersensitivity. Questions 17-19 refer to the following scenario: A woman has just been diagnosed with SLE (lupus). 17. In educating the patient about her disease, the nurse shows complete understanding of the pathophysiology of SLE when he tells the patient: a. “Unfortunately, you will need to be on a gluten-free diet.” Wrong—would apply to celiac disease b. “You should expect to have swelling in the area of your thyroid.” Wrong—would apply to Grave’s disease. c. “Fortunately SLE only affects one area, usually the joints in your hands.” Wrong—SLE is a systemic disease; hand joints MAY be involved, but usually other areas are too. d. “You may have a variety of symptoms that come and go.” Correct—this is true of most autoimmune diseases—have waxing and waning of their symptoms. 18. Some labs are done. Which of the following is a likely finding? a. Test results that indicate hemolytic anemia. b. A low CRP. Wrong—in almost any inflammatory situation such as an autoimmune disease, there is SOME inflammation and therefore high likelihood that the CRP (an acute phase reactant) would be HIGH, not low. c. A positive ANA. Correct—ANA stands for anti-nuclear antibody. So this test “looks” for a molecule that is an antibody against nucleic (DNA) material. The immune complex formed in SLE is exactly that—an autoantibody coupled to a piece of random DNA. A positive test indicates likelihood of having SLE. d. Test results that indicate a low ANA. 19. The pathophysiology related to the above test is best described by which of the following? a. Vasculitis caused breakdown of RBCs, resulting in anemia that the lab test detects. Wrong—SLE does involve vasculitis (inflammation of the blood vessels that the immune complex irritates), but vasculitis doesn’t cause hemolysis—breakdown of RBCs. b. SLE is a hypersensitivity disorder in which autoantibodies attack nucleic acids and form detectable complexes that circulate in the blood. Correct—the complexes then “land” in the lining of tiny blood vessels within organs and other body parts vasculitis inflammation S&S. c. SLE is a hypersensitivity disorder in which autoantibodies attack DNA form detectable complexes that migrate to one type of tissue. Wrong—SLE is systemic, doesn’t just affect one tissue. d. Immune complexes invade CD4 cells, a phenomenon which is detected by lab tests as a low ANA. Wrong—this is a mix references to SLE (immune complexes) and invasion of CD4s (HIV/AIDS) 20. A patient tells his nurse practitioner (NP) that he had rheumatic fever as a child. Knowing the pathophysiology behind this disease, the NP will need to assess the patient for a. angioedema. Wrong—this is a swelling that is related to anaphylaxis. b. S&S of immunodeficiency. Wrong—rheumatic fever increases risk for an autoimmune disease, as disease of “too much” inflammation, whereas immunodeficiency falls in category of “too little” immunocyte response. c. heart valve problems. Correct—following a strep throat infection, sometimes the antibodies to strep become autoantibodies and attack our own tissue, such as our kidneys and our heart valves, giving S&S known as rheumatic fever. If the heart valves were attacked, there might be lingering problems and malfunctions of the heart valves in adulthood. d. urticaria. Wrong—this is medical term for hives, which occurs in anaphylaxis. 21. A patient who receives blood with an incompatible blood type may develop a. an alloimmune reaction. Correct—alloimmune means self against another person’s tissue b. an opportunistic infection. Wrong—an opportunistic infection is likely with a suppressed immune system; opportunistic infections are the result of immunodeficiency rather than a hypersensitivity situation such as this. c. a humoral autoimmune reaction. Wrong—“autoimmune” has to do with self against self. d. a cell-mediated hyposensitive reaction. 22. Which of the following compatibility situations is most likely? A patient who is a. B positive and receives B negative blood will have a transfusion reaction. Wrong—the “B” part is the same. Re: the Rh part: the donor RBCs have no Rh antigen on their RBCs, so whether the recipient is + or neg, Rh negative blood can be given. NO transfusion reaction will occur. b. AB positive and receives B negative blood will do fine. Correct—AB recipients have no A or B antibodies in their plasma that will attack the B antigen on a donor’s RBCs. c. A negative and receives A positive blood will do fine. Wrong—if an Rh negative recipient gets Rh pos blood, he will begin creating antibodies to that Rh factor. He may not have a problem THIS time, but if he ever receives Rh pos blood again, there will be a reaction. So things are not “fine.” d. A negative and receives O negative blood will have a transfusion reaction. Wrong— the O donor has no A or B antigens on the RBCs & the AB recipient has no A or B antibodies in its plasma, so this is a double “OK.” It is even a TRIPLE ok, because the recipient is receiving blood without the Rh antigen (the “negative” part). So NO transfusion reaction. 23. A patient presents with generalized itching, urticaria, and wheezing. She says it started after she was stung by a bee. The patient is most likely experiencing a. the effects of complement system opsonization of an invading microbe. b. localized effects of mast cell degranulation. Wrong—the scenario is a systemic problem (“generalized”) c. a cell-mediated response. Wrong—allergic reactions MUST be humoral because they involve an immunoglobulin – IgE. d. anaphylaxis. Correct 24. The wheezing in the patient scenario above is at least partly caused by a. bronchoconstriction due to leukotriene over-release from mast cells throughout the body. Correct— this is one of the rare situations where you see the term “constriction” in the same mix with inflammation, since usually with inflammatory situations there is dilation of blood vessels. But here we are talking about actual bronchial muscle constriction—not blood vessels. In asthma there will ALSO be blood vessel dilation of the capillaries in the bronchi, but over-abundance of leukotrienes in this case specifically cause bronchial tightening—like trying to breathe from a thin straw. b. over-active response to immune complex deposition in the lung tissue. Wrong—this might be true if this question was about SLE. c. bronchoconstriction from humoral immunodeficiency. Wrong—see answer c in #8. d. vasoconstriction from the effect of autoimmune over-degranulation. Wrong—much mixing of different processes here: autoimmunity is a different kind of hypersensitivity than allergic; also, any kind of inflammatory response, whether as part of an allergy or autoimmunity will involve vasodilation, not CONSTRICTION. Questions 25-28 refer to the following scenario: Upon his yearly physical a 68 year old male patient was found to be HIV positive. Six months later he had a CD4 count of 400 and for many years it stays at this level. Now the patient presents to his NP with complaints of difficult and painful swallowing (dysphagia); upon examination, the NP notes white patchy areas in the mouth and throat. The NP orders a CD4 count, which is 198. (Norm CD4 ct = >600) 25. To establish the diagnosis of being HIV positive, all the following were true of this patient picture EXCEPT that the a. ELISA test showed antibodies to HIV. ELISA is done first. If it is positive, then Western Blot is done. b. Western blot was positive. The Western Blot is confirmatory & is part of establishing HIV+ status. c. CD4 count was 198. A CD4 count is not used to initially establish HIV status. d. ELISA was positive. This answer says basically same thing as “a”—presence of HIV antibodies = a positive ELISA. 26. Which is true? a. A diagnosis of AIDS was established when the patient’s CD4 count was 400. CD4 of 400 is low, but not low enough for AIDS dx, plus no mention of opportunistic infection. b. The patient officially has AIDS because of the opportunistic infection in his mouth and because of his HIV+ status. No—all AIDS patients are HIV+ so that’s a given. c. An AIDS diagnosis is automatic when the ELISA test shows antibodies to HIV. d. The patient officially has AIDS because of the opportunistic infection in his mouth and because of the CD4 count of 198. Once a person is HIV+ (as determined by the ELISA & Western Blot), her or she may or may not ever have AIDS. It usually takes a CD4 count of <200 to make a person completely unable to fight opportunistic infections. So CD4<200 PLUS presence of opportunistic infection = AIDS. 27. The patient’s nurse describes to him a couple of opportunistic disease processes that he is at high risk for. Which of the following shows that the nurse has a complete understanding of the link between AIDS and opportunistic infections? a. “You are more likely to get PCP (pneumocystis carinii pneumonia) because your HIV antibody level is so high.” The two parts of this sentence don’t go together. If the second half said “your CD4 cells are so low,” then the whole sentence would be correct. b. “The numbers of your infection-fighting cells is low, so you are more likely to get unusual infections such as CMV retinitis.” Most people with CD4 levels above 200 won’t usually get a “strange” infection like CMV retinitis. But if the CD4 cells fall below 200, you are especially vulnerable to microbes that otherwise wouldn’t have a chance to flourish. “Opportunistic” means taking advantage of a situation that is unusually conducive. c . “The numbers of your infection-fighting cells is low, so you are more likely to get autoimmune diseases such as lupus.” Autoimmunity implies a pathologically “ramped-up” immunocyte system, so it is actually the opposite of immunodeficiency states. d. “Your CD4 count of 198 is ok for now, but when it drops below 50 you will need to avoid people with common infections such as a cold or the flu.” 28. This patient is put on several medications. All the following are steps in the HIV invasion process that a medication might target EXCEPT the a. use of viral protease to make new viral proteins in the CD4 cell. b. insertion of the HIV DNA molecule into the CD4 cytoplasm. HIV is an RNA retrovirus, not a DNA virus. c. use of the viral enzyme reverse transcriptase. d. use of integrase to insert viral DNA into the CD4 nucleus. 29. A patient presents to the ED with fever, chills, myalgia, and a dry cough. He says he has recently traveled to China. He says he got a flu shot a year ago. Which is most likely in this case? a. This disease is pertussis, probably contracted from an unvaccinated contact when he visited China. b. The disease is probably not influenza, since he had a flu shot during last year’s flu season. c. The diagnosis is influenza, probably contracted via fecal/oral route while in China. Flu is transmitted by coughing, sneezing etc, so not by fecal/oral route. d. The diagnosis is influenza, possibly contracted because patient did not have this year’s flu shot. 30 The disease mentioned above has the following characteristic: a. The causative microbe can also cause a membrane across the pharynx. Diphtheria. b. This disease is difficult to treat because of the antigenic drift of its exotoxin. Flu is a virus and thus doesn’t have exotoxins like bacteria. c. New mutations of proteins on its cell membrane cause a variety of types each year. The two cell membrane antigens that undergo antigenic shift each year are hemagglutinin (H) and neuraminidase (N), which give the flu virus its name each year (H1N1, H5N1, etc). d. A later outbreak may include skin lesions in a dermatome pattern. Shingles. 31. A commonality of herpetic organisms that cause diseases like chicken pox and shingles is that a. each is caused by a bacterial organism that penetrates the nervous system. Herpetic organisms are viruses, not bacteria. b. the causative microbe can remain dormant in the nervous system. These diseases are one of a variety of herpes viruses, which have the commonality of invading peripheral nerve system and remaining dormant there for “X” amount of time, depending on individual. c. the causative microbe causes bloody diarrhea. Wrong—this would be true if asked about shigella. d. each is transmitted via vector. Wrong— chicken pox is acquired via airborne transmission. Shingles develops from a harbored chicken pox virus. 32. An otherwise healthy Texas rancher whose water supply comes from a well is more at risk for a infection than a Dallas suburbanite. a. giardia Giardia is a protozoa that is more common in untreated water such as from wells in rural areas. b. trichinosis the state of having a helminth that commonly invades the GI tract via undercooked pork & then migrates to tissues. c. C. diff it is usually a non-pathogen unless antibiotics wipe out intestinal flora competition. d. cysticercosis a version of “b” that walls itself off in cyst-like partitions in the brain 33. A 4 year old patient presents with bloody diarrhea. Possible causes include because a. shigella: the microbe has caused inflammation in the lining of the intestines. Correct—there are many modes of action to give the S&S of infectious diarrhea; when an organism causes a great deal of inflammation of the intestinal lining, this is when there is dysentery-- bloody diarrhea-- (inflammation capillary dilation, leakage of substances from blood to stool); shigella is one of these b. pseudomembranous colitis: C. diff has eradicated normal flora. Wrong—a person gets pseudomembranous colitis when antibiotics eradicate normal flora—that allows C diff invasion. c. giardia: this protozoa invades the intestinal wall and causes necrosis. Wrong—giardia causes decreased absorption of fat, so the S&S include foul, fatty diarrhea, not bloody diarrhea. d. diphtheria: this bacteria causes parotid enlargement. Wrong—mumps virus causes parotid enlargement. 34. After coming home from an overseas assignment a young army officer begins complaining of extreme fatigue and arthralgia. He has a very high fever and shaking chills, and he is anemic. The most likely etiology of his S&S is a. infection with rabies virus. Wrong—rabies has neurologic S&S such as confusion, agitation, dysphagia. b. protozoal invasion of his RBCs Correct—look at the WHOLE picture and link S&S with patho: this is a picture of malaria—protozoa invade RBCs, cause them to rupture the extreme hemolysis causes anemia & release of acute phase reactants fatigue, fever, arthralgia. c. Staph aureus-related cellulitis. Wrong—scenario has nothing about skin infection. d. Guinea worm infestation—Wrong—guinea worm would not cause the high fever and other classic S&S of malaria. Questions 35-38 refer to the following scenario: A patient presents to the ED with a local skin infection (cellulitis). She says she has no idea how she got it. She is told that it is a staph infection. A penicillin-type antibiotic called Augmentin is prescribed, and she is sent home. A week later, despite taking all her Augmentin, she is back with worsening of the local infection, plus fever and leukocytosis. She is hospitalized. A culture of the wound shows MRSA and she is placed on more appropriate antibiotics. 35. Which best describes the pathology behind the events in this scenario? a. A certain Staphylococcus aureas species developed special bonding affinity with methicillin. Wrong not affinity, but instead, “attack” capabilities. b. The patient likely had a compromised immune system, as evidenced by the leukocytosis. Wrong --leukocytosis is a normal and desired fighting force in people with normal inflammatory capability. c. A certain Staphylococcus aureas species developed beta-lactamase, which destroyed the penicillin molecule. The beta lactam ring is an essential structural part of all penicillins such as methicillin. Certain strains of staph aureas (SA) called methicillin-resistant SA (MRSA) have developed an enzyme called beta-lactamase that can destroy the ring and render the antibiotic ineffective. d. Staphyloccocus areas is an organism that doesn’t respond to any kind of penicillin. Some non- resistant strains of staph still respond to the penicillin class of antibiotics. 36. The fever and leukocytosis a. are evidence that the staph infection may have become systemic. Local infections don’t usually cause systemic responses like leukocytosis and fever. b. show that the patient is unable to mount an appropriate inflammatory response to the infection. c. show that the patient’s third line of defense is not needed. d. are evidence that the patient likely has VRE. VRE—vancomycin-resistant enterococcus—is a different microbe and is not related to this scenario. 37. After three of weeks of being on strong antibiotics, the patient develops chronic diarrhea. Her stool is cultured. In THIS context, what organism would you expect the stool culture to grow? a. MRSA. b. VRE. c. Salmonella. d. C. diff. Clostridium difficile—C. diff—is usually a non-pathogen that can live in the gut of many people without causing problems. However, if anything wipes out the competition of the normal “friendly” flora in the GI tract, C. diff can fall into the category of opportunistic infection and take over, causing diarrhea. 38. Choose the mini-concept map that best describes the links from the events and pathophysiology to the diagnosis. a. 3 weeks on antibiotics normal bowel flora wiped out Clostridium difficile has no competition and flourishespseudomembranous colitis. C. diff microbial infection causes diarrhea that is also associated with the development of a membranous coating on the inner wall of the intestines. This gives the condition its name—pseudomembranous colitis. b. 3 weeks on antibiotics normal bowel flora proliferate bowel walls are irritated inflammationantibiotic-associated diarrhea. Antibiotics destroy normal flora, not cause it to proliferate. c. vancomycin destroys enterococcus in bowel other bowel flora have no competition and flourish pseudomembranous diarrhea. The term pseudomembranous is associated with C. diff infection, not enterococcus infection. d. iatrogenic antibiotics normal bowel flora wiped out giardia invades bowel inflammation nosocomial diarrhea. Giardia is a protozoa that invades via tainted water and doesn’t need normal flora to be wiped out to cause diarrhea. Also, “nosocomial” refers to something hospital-caused. There is nothing here to suggest a patient was in the hospital. 39. A patient who is undergoing a course of chemotherapy for cancer contracts chicken pox and almost dies. What is the most likely reason for this severe response to a fairly mild disease? a. Because of the cancer, the patient likely has neutropenia, which is a state of overabundance of nonfunctional WBCs. “Neutropenia” means lower-than-usual-numbers of neutrophils, not “overabundance,” which would be the word “neutrophilia.” b. Because of the chemotherapy, the patient likely has acquired combined B-cell and T-cell immunodeficiency. Correct—essentially, the chemo wiped out all (or most) of the leukocyte growth (see RRD 3 and concept map). c. The patient developed shingles, which is a secondary infection that is harder to treat. No mention of shingles in scenario. d. The patient probably has severe combined immunodeficiency syndrome (SCIDS). This is a congenital disease and was not mentioned in the scenario. 40. A woman whose blood type is AB+ is pregnant with a baby who is B- (B negative) Which is true about getting a Rhogam shot? a. Mom would not need a Rhogam shot, since the baby’s RBCs have a B antigen, which is compatible with mom’s AB blood. The baby’s RBCs do indeed have a B antigen—that is what gives the baby the blood type “B.” But Rhogam has to do with the Rh factor, so the first part of this answer doesn’t match with the second half. b. Mom will always need a Rhogam shot following pregnancies in which the baby is Rh negative, such as this baby. Only one situation sets up the possibility of the mom needing a Rhogam shot: when a mom is Rh negative and her fetus is Rh positive, because the mom’s body will see the Rh factor of the baby as being a foreign substance and will develop antibodies to it. With the next Rh+ baby, her antibodies will attach that baby’s RBCs. A Rhogam kills any antibodies she has developed, prior to the next pregnancy. This mom is Rh+, so her body will never see an Rh factor as being “foreign” and so there will never be a need for Rhogam, no matter what Rh type the fetus is. c. The baby will need Rhogam; otherwise he will develop Rh-antibodies that will attack the Rh antigen on the mom’s RBCs. Rhogam is for the mother, as needed, not the baby. d. Mom will never need a Rhogam shot with any pregnancy; she will never develop antibodies to Rh antigens on an Rh+ baby’s RBCs. Correct—see explanation for B. Questions 1-4 refer to the following scenario: A young woman presents to her nurse practitioner complaining of SOB and fatigue. She states that her menstrual periods have been very heavy. (norm RBC = 4-6million; norm MCV = 80-95). 1. What is her most likely diagnosis and CBC results? a. macrocytic anemia; RBCs = 3 mill & MCV = 102. Wrong—MCV high, meaning cells BIG in size—doesn’t fit with scenario of losing blood (and iron) steadily during menses, which usually results in compensatorily SMALLER RBCs. b. microcytic anemia; RBCs = 3 mill & MCV = 70. Correct—RBCs < 4mill anemia (with its “usual” S&S of SOB & fatigue); MCV <80= small cells, which goes along with steady blood loss (see answer A) c. normocytic anemia; RBCs = 5 mill & MCV = 90. Wrong—RBCs are in normal range (not even an anemia) & so is MCV. d. polycythemia vera; RBCs = 20 mill & MCV = 90. Wrong—RBCs numbers are very HIGH, indicating erythrocytosis; diagnosis of polycythemia would be consistent with high RBCs, but NOT consistent with this scenario. 2. Based on the diagnosis, the patient’s S&S can be explained by the following: a. a malfunction in DNA during erythropoiesis causes inadequate ATP formation. Wrong—this is a mix of facts that doesn’t relate to each other or scenario. b. an underlying chronic disease causes a sudden loss in RBCs. Wrong—usually chronic diseases result in slow loss of RBCs or Hgb (not sudden), and the result is a normocytic anemia, not microcytic (the correct MCV answer of 70 above, answer B in question 1 = microcytic anemia). c. a steady loss of iron results in insufficient hemoglobin production. Correct-- with chronically heavy menses, there is loss of iron because of loss of RBCs. Eventually the body runs low on iron to create Hgb. d. a malformed hemoglobin molecule that decreases oxygen-carrying capacity of each RBC. Wrong—this is descriptive of sickle cell rather than blood loss situation. 3. The patient probably has a certain degree of hypoxemia because a. her low levels of iron have decreased the O2-carrying capacity of her Hgb. Correct— each Hgb molecule can carry 4 O2 molecules, so less Hgb = less O2. b. a secondary polycythemia has resulted from an underlying lung disease. Wrong—you are given in answer 1 that her RBCs are 3million = anemia, not polycythemia. c. she is not breathing in enough oxygen, resulting in unsaturated Hgb molecules. Wrong—there is no indication that this patient is having trouble breathing, as is implied in this answer. Instead, she is having shortness of breath BECAUSE of the underlying anemia. d. her heavy periods have led to a loss of Von Willebrand factor. Wrong—the coagulopathy known as von Willebrand disease can CAUSE heavy periods, not vice versa. 4. Which of the following will most likely be part of the treatment rationales for this patient? a. Iron (Fe) supplements will help the SOB by increasing the capacity of Hgb to carry O2. Correct—as explained in previous question, patient is losing iron, so this treatment will fix that. b. A well-rounded diet will provide nutrients to increase production of intrinsic factor. Wrong—a well-rounded diet is always a good thing, but it will not increase production of the hormone called intrinsic factor that is made by the parietal cells of the stomach and is needed to absorb vitamin B12. Low intrinsic factor is a cause of pernicious anemia, not iron-deficient anemia. c. Give her blood thinners for the polycythemia. Wrong—if this patient did have polycythemia, blood thinners would be appropriate, but she has anemia, which is the opposite of polycythemia. d. Injections of vitamin B12 will increase the size of the RBCs. Wrong—injections of B12 will help pernicious anemia, which is not the problem here; the other wrong aspect is that B12 doesn’t increase RBC size, but instead helps to correct the malfunction that made the RBCs too big. 5. A patient recently diagnosed with a vertebral fracture says, “I can’t understand how I broke it. I sat down a little too hard, but not hard enough to break anything.” His diagnosis is possibly because . a. Hodgkin’s lymphoma: it causes widespread lymphadenopathy. Wrong—Hodgkin’s is a cancer that does cause lymphadenopathy but doesn’t fit the scenario. b. idiopathic thrombocytopenia purpura (ITP): the low platelet count causes increased risk of bleeding. Wrong—these two parts do go together but don’t fit the scenario. c. anemia: suppression of bone marrow stem cell proliferation causes pancytopenia. Wrong—again, in some situations these two parts match, but don’t fit scenario. d. multiple myeloma: increased osteoclastic activity causes osteoporosis. Correct— multiple myeloma is a cancer in which pathologically increased plasma cells create overabundance of immunoglobulins, which attack bone and cause increase osteoclastic activity. This means more calcium goes from bone to blood, leeching the bone of strength. 6. The patient above most likely has additional S&S of this disease, including a. multiple petechiae due to coagulopathy. Wrong—petechiae would be seen in diseases of easy bleeding but this is not a part of the patho of multiple myeloma. b. leukocytosis due to the infection and inflammation. Wrong—infection is not a part of the usual patho of multiple myeloma. c. lethargy from the hypercalcemia. Correct—as osteoclastic activity increases, more calcium is resorbed (moves from bone to blood); hypercalcemia hyperpolarization lethargy, fatigue, etc. d. decreased production of clotting factors. Wrong—problems with clotting factors are not part of the typical picture of multiple myeloma 7. A person with cirrhosis (bad liver disease) and splenomegaly notices ecchymosis under her skin in several areas of her body but denies any substantial trauma to those areas. These ecchymoses are most likely related to the presence of all the following EXCEPT: a. hypoproteinemia. The sick liver can’t make proteins, and coagulation factors are proteins easy bleeding, as manifested by ecchymosis. b. increased thrombosis. This is the only answer that does NOT relate to increased bleeding which one associates with ecchymosis, so it is the answer in this except question. Thrombosis = increased CLOTTING. c. hypersplenism. This happens in splenomegaly when the spleen pathologically “chews up” more RBCs, WBCs, and platelets; less platelets easy bleeding, as manifested by ecchymosis. d. thrombocytopenia. less platelets easy bleeding as manifested by ecchymosis. 8. The patient in the previous question is also anemic. What mechanism is most likely? a. Increased hemolysis of RBCs from hypersplenism. Correct hypersplenism chews up (hemolyzes) RBCs less RBCs anemia.. b. Parasitic infection that caused leeching of nutrients. Wrong—no mention of parasite in scenario. c. Thrombocytosis from hypersplenism. Wrong – thrombocytosis means too many platelets too much clotting, not RBC hemolysis. d. Decreased hemolysis of RBCs because of splenic shrinkage. Wrong—hypersplenism is a condition caused by an enlarged spleen (not shrunken) in which increased #s of RBCs & other cells get destroyed than normal. 9. A 92-year old patient presents with complaints of fatigue and strange burning sensations of the legs. Upon assessment the nurse notes an appearance of undernourishment and pallor, and a CBC that shows: RBCs 2.5 mill; MCV 110; platelets 200,00. (norm RBC = 4- 6million; norm MCV = 80-95; norm platelets = 150,000-400,000; norm WBCs = 6-10,000). Which of the following is the best mini-concept map to explain aspects of this scenario? a. older adult less parietal cell function in stomachdiminished ability to absorb nutrients normocytic anemia. Wrong—first few phrases are plausible, but a HIGH MCV in the scenario above negates the possibility of a NORMOcytic anemia. b. paresthesia of legs general discomfort less appetite less vitamin B12 absorption faulty DNA coding of RBCserythrocytosis. Wrong—this is a mix of things that have some credible parts, but the order is all wrong, plus obviously this person is anemic (2.5 million RBCs), the opposite of having erythrocytosis. c. older adultless intrinsic factor produced less vitamin B12 absorbedfaulty DNA coding of RBCsmacrocytic anemia. Correct—older adults have aging parietal cells and they often don’t make enough intrinsic factor, which leads, step-by-step, to the other problems. d. macrocytic anemiatoo fatigued to eat muchnot eating enough vitamin B12 less intrinsic factor producedparesthesia of legs. Wrong—macrocytic anemia is associated with low B12; low B12 often causes malfunction of sensory perception the result is strange sensations in the legs (paresthesia). What makes this wrong is the order of the events in the concept map. 10. A patient has developed random ecchymotic areas on her skin over the last few months. A CBC shows: RBCs 1.5 mill; MCV 95; platelets 95,000; WBCs 50,0000 (see norms above). Which of the following is the best mini-concept map to explain aspects of this scenario? a. She has developed leukemiapathologic leukocyte proliferation has crowded out development of other cells like platelets thrombocytopeniaeasy bleeding. Correct – this is classic leukemia (too many WBCs in blood); the HUGE number of 50,000 WBC plus LOW numbers of RBCs & platelets fit with cancerous overproliferation of WBCs in bone marrow. b. An infection has developed WBCs and coagulation factors are used up leukopenia and easy bleedinganemia. Wrong—order is mixed and doesn’t make sense. c. Bone marrow cancerpathologic leukocyte, RBC, and thrombocyte proliferation erythrocytosis, leukocytosis, thrombocytosis thickening of the blood. Wrong—as noted above, there is leukocytosis (high WBCs) but thrombocytoPENIA occurs in leukemia, not thrombocytosis. d. She has developed hemophilia lack of coagulation factorseasy bleeding anemia. Wrong—scenario doesn’t fit hemophilia, in which there is easy bleeding due to clotting factors missing from a genetic disorder. Lack of clotting factors doesn’t cause low RBCs, etc, though it can explain the ecchymotic areas. See the table below. It is numbered I-X. In the right column are words and phrases that link in some way with each of the numbered items on the left. In other words, this is a typical “matching” exercise. Fill out the table, and use it to answer questions 11-15 directly below. ONLY ONE ANSWER TO EACH LEFT-HAND TERM, AND DO NOT CHOOSE THE SAME ANSWER MORE THAN ONCE—CHOOSE THE BEST FIT. MATCH CORRECT LETTER FROM RIGHT COLUMN TO NUMBER ON LEFT I. easy bleeding due to diminished platelet-binding tissue substance. H A. hypocalcemia II. glossitis K B. idiopathic thrombocytopenia purpura (ITP) III. a type of neuropathy I C. pathologically increased osteoclastic activity IV. pinpoint-sized pathological bleeding under the skin_J D. associated with stasis of blood that can increase thrombosis V. easy bleeding due to diminished numbers of platelets. B E. hypercalcemia VI. causes increased resorption of calcium C F. Hodgkin’s lymphoma VII. a blood electrolyte abnormality associated with multiple myeloma E G. splenomegaly VIII. associated with increased hemolysis of blood cells G H. von Willebrand disease IX. polycythemia D I. paresthesia X. type of cancer associated with lymphadenopathy F J. petechiae K. a pathologic sign associated with the need to get extra vitamin B12 11. Polycythemia (#IX) a. G b. K c. D Polycythemia= too many RBCs ”thick” blood that will move more slowly or not at all (stasis) and thus provide ideal pathological clotting environment. d. B 12. Glossitis (#II) a. K Glossitis = inflammation of the tongue; a sign of low B12. b. H c. F d. J 13. A blood electrolyte abnormality associated with multiple myeloma (#V11) a. A b. E In multiple myeloma, an over-abundance of antibodies attacks the bone & causes increased osteoclastic activity increased resorption of calcium (Ca++ goes from bone to blood) hypercalcemia. c. I d. B 14. Associated with increased hemolysis of blood cells (#VIII) a. H b. G Splenomegaly = enlarged spleen. If spleen is enlarged (such as often happens in conjunction with cirrhosis), a condition called hypersplenism results pathologically increased numbers of RBCs, WBCs, & thrombocytes are broken down, with resultant anemia, leukopenia, thrombocytopenia. c. B d. D 15. A type of neuropathy (III) a. I Neuropathy—any nerve pathology, especially relating to interpretation of sensation. Paresthesia—disruption of sensate signal propagation, due to nerve pathology. Most commonly used to describe complaints of “strange,” often “creepy-crawly” or “stinging” sensations in legs especially. Or sometimes can describe numbness. Seen in diseases that affect nerve cell metabolic pathway such as thiamine deficiency, or, in this case, B12 deficiency. B12 not only helps RBCs grow to their proper size and function, but also is important in normal nerve function. Lack of B12 (as in pernicious anemia) results in too-large, non-function RBCs, and mal-functioning peripheral nerves, causing “misinterpretation” of sensation b. H c. F d. J 1. A patient has intermittent claudication and a history of atherosclerosis. What other findings are most likely? a. pitting edema of the ankles. Wrong—edema is associated with venous issues, not arterial (everything in stem of question points to arterial: intermittent claudication = PAD, atherosclerosis = arterial prob.) b. jugular vein distention. Wrong—associated with RHF in which there is back up of venous blood into jugular veins. c. cool feet with diminished pulses. Correct—atherosclerosis blocks arterial flow to distal areas; intermittent claudication means basically “limping because of ischemic pain,” so you link this with PAD & diminished flow to feet. d. S&S of increased preload. Wrong—increased volume is not a part of this scenario. 2. A patient is diagnosed with venous insufficiency. What treatment is most likely and why? a. a clot-busting medication, because it is used to dissolve arterial clots that block off flow. Wrong—venous insufficiency = venous prob, not arterial (“arterial clots” is in stem of question) b. drop the legs lower than the heart so that circulation can bypass DVTs. Wrong—venous issues = raise feet. c. complete bedrest, as venous stasis is the best way to prevent thrombosis. Wrong— blood should never be static increases risk for thrombus. d. elevation of feet as often as possible, because it enhances venous return. Correct – think of venous insufficiency as “insufficient ability to get venous flow back UP to the heart” (often due to incompetent venous valves) so that blood pools in veins in the feet. ***Questions 3-7 refer to this scenario: A patient with a history of atherosclerosis and HTN is complaining of chest pain, SOB, and pain radiating to his left arm. He is diagnosed with an MI of his left ventricular wall. 3. What S&S would be expected and would indicate decreased CO /perfusion? a. ankle edema and varicose veins. Wrong—atherosclerosis & HTN are arterial dzs; ankle edema & varicose veins relate to venous issues. b. decreased urine output and capillary refill of 4 seconds. Correct – an MI will be a negative inotrope—it will decrease contractility of the heart muscle and thus decrease stroke volume, which in turn decreases CO (see concept map); decreased CO means less perfusion to the bodydelayed capillary refill as well as diminishment of organ efficiency such as that of the kidneys. c. BP of 190/90 and capillary refill of 2 seconds. Wrong—capillary refill of 2 sec. is normal. d. strong, bounding DP & PT pulses. Wrong—with decreased CO, you are more likely to have decreased, weaker pulses. 4. Lab work done during the MI most likely shows high blood levels of certain substances, including: a. troponin. Correct—increase in serum troponin almost always means cardiomyocytes injury/death, since troponin is a substance usually only found in the heart cells. b. BNP. Wrong—BNP is increased in HF, not MI. c. histamine Wrong—histamine MAY be increased because of inflammatory side of MI, but it is more subtle and not measured as lab work. d. inotropes. Wrong—the word inotrope means having to do with contractility; it’s not usually a measurement in terms of labs, etc. 5. He develops a blood pressure of 80/50. Which statement is most accurate? a. The patient is in cardiogenic shock and should be given meds to increase SVR (systemic vascular resistance). Wrong—the first part is correct, but you would never give medications to increase afterload for a patient whose heart is already struggling (cardiogenic = heart-related). b. The patient should be given a negative inotrope, as this will cause vasodilation. Wrong—inotrope means related to contractility; a negative inotrope means something that suppresses contractility, not causes vasodilation. .c. The patient is hypotensive and should be given large volumes of fluid. Wrong—by increasing preload in this case you will add to the heart’s workload—the heart “says”: ‘here I am sick, and now I have more fluid coming in—I have to work even harder!’ d. The patient is in cardiogenic shock and should be given a positive inotrope. Correct-- anything that is a positive inotrope will increase the contractility of the heart, thus giving it the strength to eject more blood and increase the ailing BP. 6. Several days later the patient manifests S&S of heart failure. Given the area of his heart involved in the MI, which are the most likely S&S? a. increased preload & ankle edema. Wrong—increased preload (ie, increased blood volume, AKA fluid volume overload,) is usually present in any type of HF; ankle edema is one of S&S of RHF, not left (in stem of question it mentions LV MI). b. decreased afterload & intermittent claudication. Wrong—random answers not applying to this situation. c. tricuspid regurgitation & right atrial hypertrophy. Wrong—both of these situations occur on right side of heart, not the problem area of our scenario (left side.) d. shortness of breath and lung crackles. Correct – you are given the fact that this was an MI in the LV, so most likely, as the LV gets too tired to pump blood forward, some of it will go backward— into the lungs, causing pulmonary edema & related S&S (“Lung crackles” means if you listen to the lungs with a stethoscope, you can hear the crackling of air going in and out of fluid-filled alveoli). BE SURE TO KNOW HEART FLOW BOTH FORWARD and BACKWARD. 7. When the patient was suspected of developing the heart failure (HF), lab work was drawn that specifically corroborated the diagnosis of HF by showing that the was elevated. a. CRP Wrong—likely that a CRP would be elevated, but only indicates that there is inflammation, not where it is. b. BNP. Correct – BNP (B-type natriuretic peptide) is secreted by the heart when there is TOO MUCH preload (ie, fluid volume overload)—BNP circulates to the kidneys & “tells them” they need to increase urination as a compensatory response for high blood volume, because a “bad” heart cannot tolerate extra fluid; heart failure should ALWAYS be considered a problem of fluid volume overload because of the effect of the RAAS (see concept map on page 26 of RRD6). c. CK Wrong— likely that a CK would be elevated, but only indicates non-specific cell injury (in an MI, both CK AND troponin would be elevated, but CK by itself would not be diagnostic.) d. RBC. 8. A 40-year-old man is undergoing a yearly physical. Everything is fine except that the nurse practitioner hears a murmur. All the following are likely etiologies EXCEPT: a. pulmonic valve insufficiency. b. a heart valve that is ischemic from a coronary artery blockage. c. incompetent venous valves. . Correct – the other answers are appropriate to the scenario; this is the exception, since it is talking about valves in the veins; vein valves don’t usually have murmurs that can be heard in this fashion. (Be sure you think about venous valves & heart valves as very different entities) d. a stenotic mitral valve. 9. A patient with CAD reports that he gets angina only when he walks more than a mile. It always goes away when he rests or takes a NTG. Which statement best fits this patient? a. He has unstable angina due to worsening of an atherosclerotic plaque. Wrong—the consistency and mildness of this patient’s S&S indicates stable, not unstable angina. b. He has ACS that is stable due to development of collateral circulation over time. Wrong—ACS (acute coronary syndrome) is used to describe unstable types of CAD status; ACS is an umbrella term that covers unstable angina and MI. c. He has stable angina due to development of collateral circulation over time. . Correct stable angina (a category of CAD that basically means “ischemic heart problems that remain stable”) is almost always related to SLOW development of obstruction of blood flow (such as slow-developing plaque), giving the body a chance to develop collateral circulation & thus feed oxygen-deprived tissue on an ongoing basis. d. His pain is caused by increased preload from venous congestion. Wrong— a mix of terms that doesn’t apply here. 10. The patient in the question above is on medications. All the following are likely EXCEPT that he takes a. NTG to maximize coronary artery patency. b. NTG to dilate coronaries. c. aspirin to prevent inflammation that leads to increased plaque formation. d. negative inotropic medications Correct—anything that is a negative inotrope will decrease contractility of the heart muscle, decreasing stroke volume, and thus decreasing cardiac output. 11. A patient in atrial fibrillation has an increased likelihood of a. no cardiac output and dying immediately. Wrong—this answer would be correct if the question asked about ventricular fibrillation; usually with atrial fibrillation the ventricles are still working fine. b. an arterial embolus to the lungs. Wrong—this would be correct if it said “venous” embolus to the lungs… remember that it would be a venous embolus that flows through the right ventricle and into the pulmonary artery. c. a venous embolus to the brain. Wrong— this would be correct if it said “arterial” embolus to the brain… remember that it would be an arterial embolus that flows through the left ventricle and into the aorta, then possibly up the carotid to the brain. d. a thromboembolic event. Correct-- when the atria are quivering, there is no “atrial kick”—no ejection of a last bit of blood from atria to ventricles; this means some blood can pool in the atria; pooled blood increase risk of thrombus increased risk of embolus. 12. Lab work done on a heart patient shows a potassium of 5.5 (normal = 3.5 – 5.0). The patient is at risk for a. ventricular fibrillation because his heart cells will be more irritable. Correct – hyperkalemia can lead to more cations (K+) diffusing into myocardial cells; more cations resetting of RMP at a more positive charge “closer” to the depolarization/contraction point of +30mV hypopolarization heart cells more irritable & thus more likely to become irregular. b. bradycardia because his heart cells will be more sluggish. Wrong—the opposite is true. c. atrial fibrillation because he will be in heart failure. Wrong—no mention of HF. d. increased afterload for the left ventricular because of systemic vasoconstriction. Wrong— systemic vasoconstriction would indeed cause an increased afterload for the LV, but this scenario would not likely cause systemic vasoconstriction. \ 13. A patient has a DVT of the right calf. Which of the following is the LEAST LIKELY to develop? a. Pain at the DVT site. Wrong—pain IS a typical symptom. b. Loss of perfusion in right foot because of the thrombus blocking distal arterial flow. Correct -- DVT = deep VENOUS thrombosis; there might be thrombophlebitis (pain, erythema) as the vein & surrounding area become more inflamed, but since this is not an arterial situation, loss of pulse isn’t likely. c. Erythema of the skin in the local DVT area. Wrong—erythema IS a typical symptom of DVT. d. Shortness of breath secondary to an embolus that breaks off the DVT. Wrong— this may happen if an embolus develops form the DVT & travels to the lungs, so this IS a true fact about DVT, at least potentially. 14. An otherwise healthy patient has had hypertension (HTN) for many years. Which of the following is most likely true? a. He has secondary hypertension. Wrong— unless you are told otherwise in the scenario, assume that the patient has essential hypertension, which is MUCH more common than secondary HTN. b. Etiologic factors of the HTN include epinephrine depletion. Wrong—HTN’s etiology includes pathological overaction of the sympathetic nervous system, including subtly increased epinephrine levels. c. The atrial natriuretic peptide system is in overdrive. d. Etiologic factors of the HTN include pathologic overaction of the RAAS. Correct— instead of ONLY kicking in when we have low BP or low volume, the RAAS pathologically kicks in a low-level way that results in subtly higher blood volume and pressure. 15. A patient with chronic bronchitis says: “Look how swollen my legs and feet and belly are. This has been increasing over the last couple of years. What’s going on?” As his nurse, you would most likely suspect that the patient has all the following EXCEPT a. venous backflow from LHF. Correct -- this answer is the only one that ISN’T about right-heart- failure-induced venous back-up; LHF would cause fluid back-up into the lungs, not the periphery like this scenario suggests (note: even though in REAL life, a patient can have S&S of both LHF and RHF—very common—we will consider them separately, with RHF causing venous backflow to periphery and LHF causing backflow to lungs.) b. cor pulmonale. c. ascites from RHF backflow. d. venous backflow from increased PVR. ***Questions 16 & 17 refer to this scenario: An 80-year old woman with a medical history of HTN and CAD goes to her NP for a check-up. She complains that her vision has been slightly blurry but otherwise has no changes in her usual S&S. Her VS (vital signs) are as follows: BP 168/100, HR 100, RR 20. Lab work is done which shows a high LDL and HDL of 38 (desired = > 40). Urinalysis is normal except for proteinuria and hematuria (normally there is no protein or blood in the urine). 16. The patient’s blurred vision is likely caused by a. accumulation of cholesterol on the sclera of both eyes. Wrong—this isn’t a disorder that fits this scenario. b. coronary arterial blockage causing sudden myocardial infarction with resultant lack of blood flow to the eyes. Wrong—the scenario says nothing about an MI. c. chronic hypertensive damage to the retinal arterioles. Correct—HTN affects the entire arterial system, including and especially the ones in the retina (and kidneys.) d. the low heart rate causing low cardiac output and thus ischemia to the optic nerve. Wrong --the HR is within normal limits. 17. Which concept map best explains the proteinuria and/or hematuria? a. Heart disease high density lipoproteins accumulate and overcome renal threshold spill into urine proteinuria HDL now too low. b. HTN + CAD weakened walls of renal veinssubstances such as RBCs pathologically spill into urine hematuria. c. Interaction between HDLs and LDLs cause damage to kidneys spillage of lipoproteins into urine proteinuria. d. Chronic HTN high pressures inside renal arterial system cause damage and “leakiness”spillage of substances into urine from renal capillaries hematuria. Correct—HTN affects the entire arterial system, including and especially the ones in the kidneys. Often the sequelae include the inability to appropriately “hang on” to substances because the tiny renal arterioles and capillaries are ravaged from the effects of HTN. ***Questions 18 -20 refer to this patient scenario: A patient with CAD presents to her NP with a change in her usual pattern of angina. Her usual pattern for the last several years is to have anginal pain (rated “3/10”) after walking up a flight of stairs, but the pain usually quickly subsides after resting a few minutes. Now she says she has pain rated at “6/10” with minimal activity and it will only go away after taking 2 NTG pills. The NP hospitalizes the patient with a diagnosis of ACS. 18. To which category of CAD did this patient belong before the current change in anginal pattern? a. Unstable angina. b. Stable angina. CAD is usually divided into 2 main categories—stable angina and ACS. This scenario in the beginning is typical of stable angina, because of being unchanged for years. c. Stable aortic aneurysm. d. CVI (chronic venous insufficiency). 19. What concept map best explains the pathology behind the several years of unchanged anginal pattern? a. Slow-developing plaque in coronary arterycompensatory collateral circulation developsdistal tissue receives enough O2 for all but most strenuous activities. The key to stability of CAD is that the blocking mechanism such as a plaque develops so slowly that over many years the heart muscle has a chance to create “collateral” arteries that feed O2 to the tissues that are at risk as the diseased artery slowly stops giving that tissue what it needs. b. Small thrombi grow in coronary arteries emboli develop slowlyblood flow not blocked off till emboli break off and fill lumen. Wrong—Emboli break off from thrombi or are otherwise introduced in some acute fashion. They don’t “slowly” develop. c. Slow-developing plaque in coronary arterycompensatory higher venous pressures in distal tissue perfusion stays steady for many years. Wrong-- “Venous” doesn’t belong in any discussion of arterial problems. d. Ischemic pain from CAD actually worsens but patient ignores the angina only seeks help when higher activity levels cause shortness of breath (SOB) and nausea. Wrong—nothing in the scenario suggests that the patient ignored the pain. If you chose this one you may have been “overthinking” because it is true that many people don’t recognize or choose to ignore angina (women especially)…but again, that is not described here. 20. In the hospital, the patient begins complaining of worsening pain (“8/10”). The RN suspects she is having a myocardial infarction, and the MI is located in her right ventricle. All of the following fit with the RN’s thinking EXCEPT a. the patient’s EKG monitor shows bradycardia, which is often associated with sino- atrial (SA) node ischemia from a right coronary artery blockage. b. it is likely that a previously stable right coronary plaque has ruptured and completely blocked off flow to distal tissue. c. the high level of pain indicates there are areas of myocardial tissue that are undergoing necrosis because of lack of O2. d. the patient has a heart rate (HR) of 90 beats/minute and a BP of 118/80, indicating probable high preload and afterload. A, B, and C are all correct about right coronary artery blockage and its S&S. D is incorrect because the VS are within normal limits and don’t connect with “high preload and afterload.” See the table on next page. It is numbered I-X. In the right column are words and phrases that link in some way with each of the numbered items on the left. In other words, this is a typical “matching” exercise. Fill out the table FIRST, then use it to answer questions 21-25 directly below. ONLY ONE ANSWER TO EACH LEFT-HAND TERM, AND DO NOT CHOOSE THE SAME ANSWER MORE THAN ONCE. CHOOSE THE BEST FIT. 21. Person has chronic lung diseaselungs very stiffpulmonary vascular resistance increasesRV struggles to push blood into the high pressure pulmonary system RV fails back pressure eventually results in peripheral edema (III) a. E The concept map describes cor pulmonale, which is when the right ventricle begins to struggle to push blood into the pulmonary artery because of the high pressure of diseased lungs. In other words, the diseased lungs are causing high pulmonary vascular resistance (PVR) and the right heart begins to fail. So, cor pulmonale is when you have RHF because of lung problems. b. G c. C d. J 22. Pathology underlying why diuretics (meds that increase urination) are given in a person with heart failure (I) a. F b. B HF always involves lower-than-normal cardiac output because of the failure of the heart to be able to pump blood forward efficiently. Part of the job of the kidneys is to sense low cardiac output (“seen” by them as low blood volume) and try to compensate by increasing the RAAS—“revving up the RAAS.” This results in HANGING ON TO WATER as a way to increase blood volume. The kidneys are not at fault—they are just trying to help, but in this case it just exacerbates the problem, and the patient ends up in fluid overload (ie, pathologically high preload). c. H d. E 23. BNP (B-type natriuretic peptide) (IX) a. A b. J c. F (first read answer above)….As preload gets higher, the right atrium “sees” this and tries to counteract it by increasing secretion of BNP (a hormone secreted by the heart as part of the NPS— natriuretic peptide system, which is the direct opposite of the RAAS). BNP “tells” the kidneys to urinate more, so as to get rid of all the extra fluid on board. Well, that helps to some degree, but not enough, so the preload just keeps on being high and the heart keeps on putting out a huge amount of BNP in sort of a frantic fashion. So when we get our patient’s BNP level back from the lab and it is pretty high, we know the patient is in heart failure. And the higher it is, the worse the heart failure. d. B 24. Mini-concept map that explains S&S of LHF (II) a. A b. D c. G-- left ventricular MImyocardial tissue damageLV can’t pump forward as well back pressure accumulatesfluid eventually forced from capillaries of lungs into the alveoli (pulmonary edema) d. J 25. A treatment for a person with heart failure (V) a. F b. C c. H d. I Anything that will diminish the resistance (afterload) that the heart has to “push” against will help a failing heart. So think about what the left ventricle has to push against—the pressures in the aorta and the arterial system in general. If arteries are too constricted, or if blood pressure is too high, that means high systemic vascular resistance (SVR), AKA high afterload. What helps with that is to “relax” the SVR by using a medication that vasodilates—the opposite of vasoconstriction. Matching (put ONE correct letter next to the term in first column). I. pathology underlying why diuretics (meds that increase urination) are given in a person with heart failure B A. decreased cardiac outputkidneys sense this and increase renin as a compensatory response RAAS kicks in but its results exacerbate the problem. II. mini-concept map that explains S&S of LHF G B. increased preload is almost always part of the heart failure picture III. person has chronic lung diseaselungs very stiffpulmonary vascular resistance increasesRV struggles to push blood into the high pressure pulmonary system RV fails back pressure eventually results in peripheral edema E C. one of the S&S associated with RHF IV. clinical presentation of LHF J D. right ventricular MImyocardial tissue damageRV can’t pump forward as well back pressure accumulatesfluid eventually forced from veins of legs and feet into tissue (peripheral edema) V. a treatment for a person with heart failure I E classic picture of cor pulmonale VI. jugular venous distention C F. increases during heart failure because body is “frantically” trying to rid of fluid VII. main etiology of fluid overload in any kind of heart failure A G. left ventricular MImyocardial tissue damageLV can’t pump forward as well back pressure accumulatesfluid eventually forced from capillaries of lungs into the alveoli (pulmonary edema) VIII. mini-concept map that explains S&S of RHF D H. sound of air going through fluid in alveoli when there is pulmonary edema IX. BNP (B-type natriuretic peptide) F I. decrease systemic vascular resistance (SVR), a type of afterload, by giving vasodilating drugs X. explains crackles heard in lungs upon auscultation with a stethoscope H J. classic pulmonary edema S&S of SOB, orthopnea, hemoptysis Questions 1-3 refer to the following: A patient in the hospital is recovering from hip surgery. She begins to complain of chest pain and dyspnea. Her RR is 30. 1. A lung scan is performed and the V/Q ratio is reported to the nurse as “high.” This patient has most likely suffered a(n) a. MI. b. pulmonary embolus. c. atelectasis. d. episode of pulmonary edema. Rationale: A pulmonary embolus would decrease lung perfusion (perfusion = “Q”). That means that the denominator of the fraction “V / Q” would be less, so that the ratio number itself would be higher (dividing by a lesser number gives a bigger number answer). A pulmonary embolus also fits with the picture of a patient who is immobile and has had injury to her vessels (part of Virchow’s triad of risk for a DVT). Answers A & D don’t fit the scenario. Atelectasis—the collapse of portions of alveolar tissue-- (answer C) could happen in someone who has had surgery and is in bed, simply because they might not be breathing as deeply as usual. However, if a VQ scan were done in someone with atelectasis, it would more likely show a low V/Q, since ventilation would be low &perfusion would be normal. 2. Arterial blood gases (ABGs) are drawn. The results are: pH: 7.50; PO2: 100; PCO2: 29; HCO3: 26. This altered state is called a. respiratory acidosis b. metabolic acidosis c. respiratory alkalosis. d. metabolic alkalosis. Rationale: 7.50 = alkalosis. Next, see which has changed, the pCO2 or the HCO3. The PCO2 has changed automatically then this is a respiratory problem respiratory alkalosis. 3. What mechanism is likely causing the disturbance noted in question #2? a. Hypoventilation b. Hyperventilation c. Hemoptysis. d. Orthopnea. Rationale: An alkalosis means there is less-than-usual CO2 in the blood. Since this is a respiratory alkalosis, we know that the low CO2 was caused from “blowing off” too much CO2; hyperventilation would cause that, not hypoventilation (A), which would cause the opposite— retention of CO2. Hemoptysis is bloody sputum, and orthopnea is the feeling of dyspnea upon lying down—neither directly causes respirator alkalosis. 4. A child with laryngotracheobronchitis is likely to a. have stridor from trying to exhale air from inflamed alveoli. b. develop a walled-off area of viral infection in the laryngeal area. c. have stridor from trying to inhale air through inflamed bronchi. d. need a warm mist treatment. Rationale: Laryngotracheobronchitis (croup) is a restrictive (ie, probs with inhalation) disease in which inflammation from a viral infection decreases the size of the upper respiratory tract. Upon inhaling the patient will have a high pitched sound (stridor), indicating there is turbulence from the passageways from not enough room for air to pass. Answer A is wrong because the alveoli aren’t involved. B is nonsense. D would be correct if it said “cool” mist.. remember that inflammation means you have swollen tissue— heat will only make swelling worse. 5. A victim of a stab wound to the chest develops a pneumothorax. Which type of pneumothorax is most likely in his case? a. Consolidative. b. Tension c. Bronchial d. Open Rationale: An open pneumothorax occurs when an outside force causes rips in the lung tissue, resulting in air escaping into the thorax, changing its pressure from negative to positive—that pressure then bears down on the lung, collapsing it. A “tension” pneumothorax (B) is interchangeable with a “closed” pneumothorax & refers to a case in which the visceral pleura is breached & air escapes into the thorax. An example of this would be when an emphysemic patient ruptures one of the stiff alveoli clusters (bleb) by coughing, sneezing, etc. Answers A and C don’t make sense as used to apply to a pneumothorax. 6. A common denominator of a bed-ridden nursing home patient and an unconscious alcoholic is their high risk for a. aspiration pneumonia. b. bronchogenic carcinoma. c. nosocomial pneumonia. d. miliary tuberculosis. Rationale: The key here is the concept that anyone who might have a diminished cough or gag reflex, and/or diminished ability to swallow would be at risk for getting vomitus into the lungs ( a nursing home patient is usually debilitated, and an unconscious alcoholic might not be able to “protect his airway”—that is, keep stuff out of the lungs that isn’t supposed to go into the lungs.) Answer C would be correct if these two were in the hospital. B & D are wrong because there is nothing to indicate that either of these patients has those diseases. Pearl: In this scenario you are not told directly that a nursing home patient and an alcoholic both are at risk for a diminished cough reflex. You must think critically; e.g., “what is a nursing home patient usually like?’’ Answer: under most circumstances, this person would be elderly and debilitated, maybe even bedridden, and therefore would have many impairments. (see page 9 of RRD6) Then ask, “what impairment would cause aspiration pneumonia?” And so on…. Questions 7-8 refer to the following: The nurse taking care of a pulmonary patient notes that he is very thin and barrel-chested, has a respiratory rate of 28, and uses accessory muscles to breathe. 7. The nurse thinks it is most likely that the patient’s S&S are due to a. chronic bronchitis. b. a VQ ratio. c. emphysema. d. Kussmaul respirations. Rationale: Being thin and barrel-chested, using accessory muscles and pursed-lipped breathing, and having a RR of 28 (due to chronic compensatory hyperventilation—“pink puffer”) are typical signs of emphysema, not usually chronic bronchitis (A—“blue bloater” because he does NOT hyperventilate). Answer B is nonsensical, since it is NORMAL to have a VQ ratio—what is abnormal is to have a VQ mismatch. Kussmaul respirations are seen as a respiratory compensation for a metabolic acidosis & involves somewhat rapid and very deep breathing to blow off CO2—this doesn’t fit the scenario. This scenario is a respiratory problem not a metabolic one. 8. An arterial blood gas report shows pH = 7.50, PCO2 = 32, PO2= 90, SO2= 92% HCO3 = 26. These numbers mean the patient a. is in metabolic alkalosis. b. has hypercapnia, which is his normal state of compensation. c. is probably in respiratory failure. d. is probably in his normal state of compensatory hyperventilation. Rationale: As mentioned in the previous rationale, it is typical for an emphysemic patient to be in a state of hyperventilation as a compensatory way of getting in more O2. There is nothing to show that this patient is in respiratory failure (C) …with an emphysemic, you would usually think respiratory failure if his ABGs showed that he was beginning to retain CO2—that is, if his compensatory response was failing him. Instead, his ABGS show a LOW CO2 (not a high one, as in answer B), which is typical of respiratory alkalosis. Answer A is wrong, because this is a respiratory patient picture, plus remember the study tip that if the HCO3 has change, it is a metabolic imbalance, & if the CO2 has changed, it is respiratory. The HCO3 in this case is normal, so you know right away this is NOT metabolic alkalosis. 9. A patient complains of a one-week history of fever, cough, and purulent sputum. The nurse listening to the patient’s lungs notes greatly diminished breath sounds in one area of the left lung and concludes that it is probably an area of consolidation. What statement reflects that the nurse has a good understanding of this situation? a. The patient probably has TB, since he is coughing up blood. b. The diagnosis is probably lobar pneumonia, which is consistent with having a consolidated area of lung tissue. c. The nurse will prepare to help the physician insert a chest tube to reinflate the left lung, as the patient probably has a pneumothorax. d. It is likely that the patient has chronic bronchitis and has developed cor pulmonale. Rationale: Consolidation occurs in an area of the lung that usually has been infiltrated by a bacteria, causing inflammatory responses & the filling of the alveoli with inflammatory debris (WBCs, bacteria, exudate, etc)…this often causes the alveoli not to be able to get O2 inside them & they collapse. Collapse of groups of alveoli for whatever reason is known as atelectasis. If enough alveoli collapse, the whole area becomes sort of “clay-like” & is called consolidation. No air can get in, so often there will be diminished breath sounds in that area. Answer A is wrong, as there is no mention of hemoptysis (coughing up blood) in the scenario. Answer C is not consistent with the scenario—a pneumothorax is usually an acute situation which usually develops suddenly-- not over a week’s time—plus usually doesn’t have S&S of fever, etc. Answer D is wrong because though chronic bronchitis is certainly something that can cause cor pulmonale, both disorders occur over a period of YEARS, not one week. 10. A patient with a medical history of CHF presents to her health care provider complaining of PND, 2-pillow orthopnea, DOE, and hemoptysis. She most likely has a. primary pulmonary hypertension. b. noncardiogenic pulmonary edema. c. cardiogenic pulmonary edema. d. pleural effusion. Rationale: These are classic S&S of the pulmonary edema that is caused by left heart failure. Noncardiogenic pulmonary edema (B) is usually caused by direct pulmonary disease or injury rather than having a LHF origin. A pleural effusion (D) is the development of inflammatory exudate between the visceral & parietal pleura of the lung. It is different than having fluid in the alveoli, which is what pulmonary edema is. Answer A is a fairly rare diagnosis that doesn’t fit this scenario. 11. A patient has overdosed with heroin. He is unconscious and his RR is 8. Which of the following set of blood gases is most likely, given this information alone? a. pH= 7.25; PO2= 70; PCO2 = 50; HCO3= 24. b. pH= 7.49; PO2= 90; PCO2= 25; HCO3 = 25. c. pH = 7.20; PO2 = 80; PCO2 = 38; HCO3 = 18. d. pH = 7.37; PO2 = 85; PCO2 = 36; HCO3 = 26. Rationale: The key here is getting a mental picture of this patient. He is hypoventilating— breathing very slow & probably shallow (RR is only 8/min)—what would happen in that case? The patient would not be able to blow off the normal amount of CO2 and would retain CO2, resulting in hypercapnia—high pCO2 (50). B is wrong because respiratory alkalosis—a low pCO2—is consistent with increased RR (hyperventilation), not decreased RR. C is metabolic acidosis which is not consistent with this scenario. D is a normal set of ABGs. 12. The correct answer above is called a. respiratory acidosis b. metabolic acidosis c. respiratory alkalosis. d. metabolic alkalosis Rationale: Low pH-- acidosis. Change in pCO2pulmonary involvement. (Always ask yourself: does this fit the patient presentation? In this case, respiratory acidosis does fit—see explanation in question 11). ~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~ For questions 13-19, choose one of A –T from box above to answer questions about the scenario below. Don’t re-use letter. Choose BEST FIT from the choices (a-d) you are given. The scenario: A 50 year old male is evaluated in the emergency room (ER) for a complaint of dyspnea. The dyspnea has become worse over many years but today is especially bad. He reports a history of smoking. His breath sounds are clear but greatly diminished throughout his lungs. ABGs, peak flow test (PF), VQ scan and chest x-ray (CXR) are completed. Results are below. ABGs: pH 7.48, PCO2: 30, HCO3 : 24, PO2 80, SO2 94%. PF: 50% of predicted norm (ie, “low” PF). V/Q scan 0.8. CXR shows hyperinflated aveoli and air trapping. 13. Putting together all information given, what is the most likely diagnosis on this patient? a. D b. B c. C d. A 14. Using the “patient picture” scenario & correct answer from #13, what is the expected breathing rate & pattern of this patient? a. L b. M c. O d. Q 15. What do you expect his general appearance to be like? a. I b. F c. K d. O 16. The low PF in this scenario indicates _. a. Q b. M c. C d. J 17. What acid base imbalance does this patient have? a. S b. T c. N d. P 18. The acid/base imbalance above is part of a compensatory response to keep the body a. F b. G c. H d. K 19. If you could look at this patient’s lungs directly, you would expect to see _. a. D b. E c. I d. R RATIONALES: Emphysema—the “pink puffer”. This is an obstructive pulmonary disorder in which the walls of alveoli are destroyed. The destruction begins when the lung passageways are irritated by cigarette smoke & the many different toxins in cigarettes. This irritation triggers inflammation and “over-action” of proteases such as elastase, which begins “eating” at the alveolar structures. Over time, the destruction results in loss of elastic recoil and large areas of the lung that are like stiff balloons—this causes air trapping & blebs--cave-like areas of trapped air-- and generally larger lungs (as confirmed by CXR). The more the air is trapped, the more difficult it is to exhale it & the less likely the ability to get fresh O2 into the alveoli & blood—the body experiences “air hunger.” Re: patient appearance: the patient’s body can partially make up for his air hunger by hyperventilating; this generally keeps the patient oxygenated and usually not cyanotic (remains “pink” by “puffing.”). However, this takes a lot of energy and uses up calories, so this type of disorder produces a thin patient. Usually he has a barrel chest as well in order to accommodate the larger lungs. The CXR of an emphysemic typically shows big, over-inflated lungs because of the destruction of the normal alveolar walls so that there are now just huge “blebs” of air.) A peak flow (PF) is a measurement of how much can be forcibly exhaled in one second. It is low in people with obstructive diseases, which by definition are diseases that inhibit ease of exhalation. This patient has a low PF—only 50% of what it should be—which is typical of obstructive diseases. Emphysema is an obstructive disease--the patient can inhale ok but then: #1—there is decreased elastic recoil that normally would allow air to passively be exhaled, plus #2— these air traps get bigger and bigger and more air cannot get out, as well a less fresh O2 getting in. This patient’s ABGs show respiratory alkalosis. Most emphysemics stay in respiratory alkalosis chronically because of their compensatory hyperventilation. This keeps them fairly well oxygenated—“pink”—but also takes a heavy metabolic toll, and they are often very thing. Here I want to make an important point: For our purposes, I want you to always think: “If a patient’s lungs are sick, then the compensatory response is governed by the metabolic side – ie, the kidneys. If a patient’s metabolic side is sick (kidney failure, DKA, etc), then the compensatory response is governed by the respiratoyr side – ie, the lungs. BUT in CHRONIC problems like emphysema, the respiratory side will OVER TIME, slowly, provide compensation itself by increasing respiratory rate & depth subtly, till this becomes the patient’s “norm.” Please let me know if any of that needs clarifying. [Note: if emphysemics tire and they cannot keep up the hyperventilation, then they may retain CO2 & have a high pCO2 (hypercapnia), which leads to acidosis. In general an emphysemic with respiratory acidosis is in trouble (ie, is decompensating), whereas a person with chronic bronchitis tends to be in a mild state of respiratory acidosis chronically. (However, a worsening acidosis from his “usual” indicates decompensation.)] ~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~ A. RESP ACIDOSIS G. KIDNEYS WILL HANG ON TO HCO3 M. HAS MILIARY TB B. RESP ALKALOSIS H. KIDNEYS WILL GET RID OF HCO3 N. HAS BRONCHOGENIC C. METABOLIC ACIDOSIS I. HAS RR OF 18/MIN. CANCER. D. METABOLIC ALKALOSIS J. IS HAVING A PANIC ATTACK O. HAS BEEN VOMITING. E. RR WILL INCREASE. K. HAS HYPERCAPNIA P. IS IN DKA. F. RR WILL DECREASE. L. HAS KUSSMAUL RESPIRATIONS For questions 20-30 below, use the choices A- P above. One letter per answer. Don’t reuse letters. Choose BEST FIT from the choices (a-d) you are given. 20. The acid/base imbalance in the box above is called . a. A b. B c. C d. D 21. The cause of this imbalance (#20) is that the patient a. J b. K c. L d. P 22. The compensatory response to the imbalance in #20 will be that the . a. E b. F c. G d. H RATIONALES Classic patient with resp acidosis: Patient unconscious & RR decreases from normal (16- 20) to 8 breaths a minute not breathing out enough CO2 retains CO2 (hypercapnia) blood CO2 level is high, making pH low. Also, PO2 & SO2 are low—only breathing 8/min less oxygen coming in hypoxemia. COMPENSATION: Lungs are “sick,” so compensation is by the kidneys. To buffer (counteract) the CO2 (acid gang) accumulation the kidneys will increase amount of HCO3 they make or decrease its excretion. 23. The acid/base imbalance in the box above is called . a. A b. B c. C d. D 24. One cause of this imbalance (#23) could be that the patient a. P b. N c. O d. L 25. The compensatory response for #23 will be that the . a. E b. F c. G d. H RATIONALES Patient with extreme vomiting loss of HClblood acid level becomes low, making pH high COMPENSATION: Metabolic side of the body is “sick,” so compensation is by the lungs. The lungs can increase amount of acid in the blood by decreasing RR & therefore retaining CO2. 26. The acid/base imbalance in the box above is called . a. A b. B c. C d. D 27. One cause of this imbalance (#26) could be that the patient a. J b. K c. I d. O 28. The compensatory response to 26 will be that the . a. E b. F c. G d. H RATIONALES Classic state that causes hyperventilation: anxiety, panic attack. (Also can be seen in pts having acute asthma or emphysema exacerbations.) RR increases from normal (16- 20) to 28 breaths a minute breathing out too much CO2 blood CO2 level is low, making pH high. COMPENSATION: Lungs are “sick,” so compensation is by the kidneys. To increase the CO2 in the blood, the kidneys can decrease amount of HCO3 made or increase its excretion. (Or they can “hang on” to acid gang substances like H+.) 29. The acid/base imbalance in the box above is called . a. A b. B c. C d. D 30. One cause of this imbalance (29) could be that the patient . a. P b. I c. M d. O RATIONALES Patient with DKA (diabetic ketoacidosis) has accumulated byproducts of sustained gluconeogenesis-- acidic ketones (acid gang) blood acid level is high, making pH low. 1. A patient with a history of chronic kidney disease sustains a stress fracture of the vertebra. Her increased risk of this kind of event is most likely due to a. dehydration from postrenal AKI. b. osteoporosis from decreased activation of vitamin D. c. osteoporosis from decreased phosphate. d. anemia due to lack of erythropoietin. Rationale: A vitamin D precursor is activated by the kidneys—without that activation, vitamin D cannot effectively enhance calcium absorption in the GI tract hypocalcemia = not enough calcium for bone maintenance osteoporosis (poor bone density). Dehydration is a prerenal example, not postrenal (A) and besides, it has nothing to do directly with increased risk of stress fracture. Erythropoietin (D) is diminished in chronic kidney and will cause anemia but is not directly related to osteoporosis. 2. Over a 30 hour period a patient develops oliguria. Blood work is done & he is found to have a BUN of 26 and serum creatinine of 1.1. What type of problem is most likely? a. prerenal acute kidney injury b. acute tubular necrosis c. postrenal chronic kidney injury d. glomerulonephritis Rationale: Prerenal acute kidney injury (AKI) is when AKI is caused by a problem that usually has to do with low blood volume; the main characteristics are 1) S&S of dehydration PLUS 2) oliguria. Also a BUN that may be a bit high, and a creatinine that is often in the normal range (this is an event caused by an increased concentration of the blood, not so much a renal problem itself at this point… that’s why it’s called “PRE-renal”). ATN (B), on the other hand, is present in AKI that is caused by intrarenal damage such as the effect of renal infection, drugs, etc. With intrarenal problems, the BUN & creatinine are usually BOTH high. Postrenal problems (C) in our notes describe usually an AKI that is caused by an obstructive problem in the urinary apparatus leading from the kidneys to the urethral meatus. It doesn’t fit this scenario. Glomerulonephritis (D) would qualify as an intrarenal ARF cause. 3. Findings consistent with the above problem would be all of the following EXCEPT a. poor skin turgor. b. a urinalysis (UA) that shows an increased urine specific gravity. c. a urinalysis (UA) that shows decreased urine specific gravity. d. hypovolemia. Rationale: A, B, & D are all consistent with dehydration, which is a prerenal cause of AKI. C is the outlier, as a decreased urine specific gravity usually means a more dilute urine. (The higher the specific gravity, the more concentrated the urine is. A concentrated urine means less water in the urine, which is consistent with dehydration.) 4. Drugs that should not be used in chronic renal failure (CKD). a. enhance potassium secretion in the distal convoluted tubule (DCT) b. enhance potassium reabsorption in the DCT c. decrease pruritis. d. enhance diuresis. Rationale: In CKD, often the DCT has become unresponsive to stimuli that govern the normal exchange of Na & K. For instance, it doesn’t respond to aldosterone, which usually causes it to hang on to Na & excrete K in exchange. So the patient in CKD is often hyperkalemic, and one wouldn’t want to do anything to increase absorption of K on top of that hyperkalemia. Instead, giving drugs that do the opposite would be a good thing (A), as well as drugs that decrease the itching from urea on the skin (C) and decrease the higher blood volumes that are the result of water-absorption malfunction in CKD (D—enhancing diuresis = decreasing blood volume). 5. The reason for the answer above is a. pruritis is caused by increased urea levels in the blood. b. in CKD aldosterone pathologically increases K+ excretion into the DCT. c. diuresis would increase the risk of hypokalemia. d. in CKD, K+ excretion into the DCT is decreased because of pathologic unresponsiveness to aldosterone. Rationale: See rationales for previous question. Basically these questions are asking you to think of appropriate interventions based on what you know about the usual patho of CKD. You know that CKD patients get pruritis because of urea deposits on the skin, so anything that decreases high urea would decrease pruritis. You know that CKD causes alterations that end up causing too much K+ to be held in the bloodstream rather than appropriately being excreted in the urine, so anything that facilitates excretion of K+ is a good thing in CKD…so any drug that causes diuresis (C) would likely normalize levels of K+ in the blood. Mini concept map: pathologic hyperkalemia caused by CKDDO give drugs that cause the patient to “pee out” the K+ NOT drugs that cause the patient to hang onto K+ and cause worse hyperkalemia. 6. The parents of a 12-year-old boy who is having surgery to remove a testis that didn’t descend before birth asks the nurse why the surgery is necessary since his other testis is fine and in the scrotal sac. The nurse’s explanation is based on the understanding that a. the retained testis can lead to a urinary obstruction later in life. b. the retained testis can lead to a cancerous condition called cryptorchidism. c. cryptorchidism is a risk factor for testicular cancer. d. having both testes in the scrotal sac is of acute life-threatening importance. Rationale: A testis that has not descended (cryptorchidism) cannot be checked regularly for testicular cancer & thus just by being inaccessible, the chances of detecting a cancer early are greatly diminished (this is like with the ovary situation—because the ovaries are deep in the abdomen, it is difficult to detect cancer in them.) B is wrong, since it is basically expressed backwards and thus nonsensical. A is wrong since it would be highly unlikely for a testis to be in the ureter or urethral area, where obstructions occur most often. There are several reasons for surgery, including decreasing the risk of infertility and cancer, and even the psychological reason of eventually wanting cosmetic “normality,” but cryptorchidism is not an acutely life-threatening problem (D). 7. A 70 year old man with emphysema develops postrenal AKI. What is the most likely cause? a. dehydration from chronic hyperventilation. b. a positive PSA. c. benign prostatic hyperplasia. d. a UTI. Rationale: BPH is common in men over 50 and in a man with postrenal AKI, it is the most probable cause of the AKI—if urine cannot get past the blockage of the urethra caused by the enlarged prostate, it can back up and cause hydronephrosis & eventual malfunction of nephrons. Dehydration (A) would be correct if the question asked about prerenal AKI. Answer D, a UTI (urinary tract infection), would not of itself cause blockage. A positive PSA (B) doesn’t say much --all men normally have some PSA in their blood. An ELEVATED PSA is always abnormal & can sometimes mean they have prostate cancer. Also, answer B is not a “cause” of anything. PEARL—be sure to read questions & answers CAREFULLY. 8. The patient above develops CKD. His ABGs are: pH 7.32, pCO2 40, HCO3 19, PO2 80. This acid/base imbalance is likely caused by impairment in the kidneys’ ability to a. buffer respiratory alkalosis. b. get rid of normal amounts of HCO3 into the urine. c. create normal amounts of HCO3 for the body’s needs. d. reabsorb the usual amount of urea. Rationale: The ABGs show metabolic acidosis: pH is low (= acidosis), HCO3 is low (remember, if the HCO3 changes from normal, it’s a metabolic problem); PCO2 is normal (so it’s definitely not a respiratory issue). Once you establish what the abnormality is—metabolic acidosis, ask yourself, “what is the most likely reason in the context of CKD for HCO3 to be low? Ok, the kidneys are sick. Would they be less able to buffer respiratory alkalosis (answer A)?” Yes, but respiratory alkalosis doesn’t have anything to do with this situation. (Plus these ABGs are not what you would see in a case of buffering which I told you we wouldn’t deal with in this course—ABG numbers that suggest buffering is an advanced concept). RE: answer B: Would sick kidneys be unable to get rid of normal amounts of HCO3? Yes, this might be a problem with sick kidneys…but if that WAS the problem, you would have abnormally high HCO3 in the blood, and the resultant pH would be high, too (alkalosis, not acidosis). RE: answer D: in CKD there is not a problem with reabsorbing the waste product urea, but instead a problem with excreting it—getting rid of it in the urine so that it doesn’t accumulate in the blood. So the correct answer is C: One of the many “duties” of the kidneys is to make HCO3 according to the body’s needs. Sick kidneys can’t do this so there is not enough HCO3 to balance the acidic substances in the body, and metabolic acidosis results. 9. A 32 year old woman presents with hematuria and sudden onset of severe, spasmodic right flank pain. Her diagnosis is most likely a. ureteral lithiasis. b. PID. c. pyelonephritis. d. salpingitis. Rationale: Hematuria (due to stone scraping ureter walls; “lithiasis” means state of having a stone) and right flank pain (from ureteral colic) would be classic signs of a stone in the right ureter. PID—pelvic inflammatory disease, which involve salpingoopheritis (B & D), would have S&S of lower abdominal pain that was constant & worsened with movement. Pearl: Remember pain patterns… “colicky” type pain that more closely matches this scenario is associated with kidney stones, while inflammatory pain such as with B, C, D would be constant & the patient would want to be still (as opposed to a patient with colicky pain often being restless.) 10. A 32 year old woman presents to her nurse practitioner with vague complaints of bloating, constipation, and diffuse pelvic pain, onset several months ago. What should the N.P. suspect? a. Endometriosis. b. Ovarian cancer. c. AKI. d. Dysmenorrhea. Rationale: The S&S described are classic for ovarian cancer. Endometriosis (A) would have S&S of pain usually associated with the menstrual cycle, since its patho is that of ectopic endometrial tissue that bleeds & cramps no matter where it has been implanted. AKI (C) is acute kidney injury… this scenario doesn’t match the oliguria and other S&S of AKI. Answer D— dysmenorrhea—is when a woman has pathologies having to do with menstrual flow such as too much flow or too much pain during her period, etc. This can be a complaint in many situations (including occasionally ovarian cancer), but it doesn’t go along with the S&S described here. ~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~ Read scenario I. Then decide which of sentences A – J are correct (there are 5 correct ones) and which are incorrect. Answer questions 11 & 12 as they apply to scenario I. Scenario I: Ms. Dolores Umbridge is a 63-year-old patient who has been on a nephrotoxic dose of antibiotics. She develops ATN (acute tubular necrosis) as a result. Her S&S are as follows: acute oliguria & generalized edema. Blood work: BUN = 27, creatinine = 3.0. UA: casts are noted. (Blue highlighting = correct statements. Note: I have not included any rationales with questions 11-18, because I felt they were self-explanatory based on the blue highlighted statements and your RRDs…but if you have any questions, please ask.) A. This patient’s AKI (acute kidney injury) is considered to be in the prerenal AKI category because an acute event likely caused a low BP. B. As cells of the tubules die, they slough off into the urinary tubules and are seen as “casts” in the analysis of the urine. C. The patient is oliguric because when the kidney is “sick,” the GFR pathologically increases and allows too much urine to be filtered into tubules. D. The following mini-concept map explains the patient’s edema: sick kidneys diminished ability to decide how much Na+ and H2O should be secreted in the urine water is pathologically retained fluid overload eventual edema. E. As cells of the tubules die, they slough off into the urinary tubules and are often reabsorbed into the peritubular capillaries, causing arterial blockages called casts. F. The following mini-concept map explains the patient’s edema: slow, insidious disease process affects kidneys over time, DCT becomes refractory to aldosterone Na+ and H2O are not retained as they should be and instead are secreted in the urine (water follows sodium) excess water in urine fluid overload eventual edema. G. This patient has a guarded prognosis because few people get better after having a pre-renal AKI, even after appropriate treatment. H. This patient may have a good prognosis because many times people completely recover following appropriate treatment of an AKI. I. This patient’s AKI (acute kidney injury) is considered to be in the intrarenal AKI category because an acute event has caused the tubules of the nephrons to become ischemic and malfunction. J. The following explains the patient’s azotemia: in ATN, tubular cells die and there is diminishing renal function, including the loss of the ability to get rid of wastes. 11. Which one of the following is correct about the patient in the scenario? a. A b. B c. C d. E 12. All of the following are correct EXCEPT: a. G b. H c. I d. D Read scenario II. Then decide which of sentences A – K are correct (there are 6 correct ones) and which are incorrect. Answer questions 13 – 15 as they apply to scenario II. Scenario II: Over a few years, Ms. Umbridge goes on to develop chronic kidney disease (CKD). Her S&S are numerous, and include edema, SOB, HTN, and pruritis. Choose the correct statements about the patient’s current status. A. The edema is caused by the pathological retention of Na & water as the diseased tubules lose the ability to appropriately “choose” what to hold onto & what to get rid of. B. An RN assessing this patient may expect to hear crackles in the lungs due to pulmonary edema related to pathologically increased preload. C Assessment findings on this patient may include a BP of 180/110 because renin secretion from the JGA is pathologically decreased. D. In CKD the tubules lose the ability to respond appropriately to aldosterone, resulting in a high preload that contributes to the patient’s edema. E. Lab results consistent with this patient picture would typically include, for example, a BUN of 29 and creatinine of 1.1. F. Urinalysis results consistent with this patient picture may include low specific gravity because the kidneys lose the ability to concentrate urine appropriately. G. Because the patient likely has a high BUN, she is considered to be in a state of uremia. H. In CKD the tubules lose the ability to respond appropriately to aldosterone, resulting in accumulation of aldosterone in the blood; this is called azotemia. I. The nurse taking care of this patient finds her to be confused and is not surprised, since this symptom is sometimes found in uremic patients. J. The pruritis is likely due to salt-like deposits of urea on the skin related to the patient’s azotemia. K. Uremic encephalopathy may be seen in this patient as a result of osmotic changes that include shift of fluid from brain cells to the hyperosmolar blood. 13. Which one of the following is correct about the patient in the scenario? a. G b. E c. C d. D 14. All of the following are correct EXCEPT: a. A b. B c. C d. I 15. Which one of the following is correct about the patient in the scenario? a. J b. H c. K d. C Read scenario III. Then decide which of sentences A – I are correct (there are 4 correct ones) and which are incorrect. Answer questions 16 – 18 as they apply to scenario III. Scenario III: Ms. Umbridge’s CKD will need a certain treatment plan which is described correctly in some of the statements below. A. Diuretics are not usually given to a CKD patient, since potassium is likely to be urinated out as well, worsening the hypokalemia that is always a danger in patients with CKD. B. A patient with CKD is likely to be malnourished, so a diet high in protein, vitamins, and calcium is crucial. C. Since a CKD patient is almost always in a potentially dangerous state of fluid overload, a diuretic will be given to “mobilize” fluids—get them out of the tissue into the blood, and then help the kidneys to urinate them out of the body. D. Phosphate is often not metabolized properly by diseased kidneys, so phosphate supplements will be important for the nurse to give to the CKD patient. E. Calcium supplements will also be important, since diseased kidneys cannot properly activate vitamin D, thus lessening dietary calcium absorption. F. A diet low in protein is important so that there will be less urea nitrogen created when the proteins are catabolized in the liver. G. The patient will be highly fatigued due to anemia related to less erythropoietin; her nurse will likely need to give her erythropoietin injections. H. An RN caring for this patient will need to watch for S&S of “thickened blood” since there will often be an over-abundance of RBCs related to increased erythropoietin secretion. I. The nurse caring for this patient will be giving hypotonic IV fluids to counteract the hyperosmolality of the blood. 16. Choose the correct statement about treating this patient in CKD. a. A b. B c. C d. D 17. Choose another correct statement about treating this patient in CKD. a. I b. H c. A d. F 18. Dolores Umbridge is a. an evil professor in the Harry Potter series. b. an evil nursing professor at UTA. c. the competent head nurse on the TV series, ER. d. the evil head nurse in One Flew Over the Cuckoo’s Nest. 19. A 29-year old woman has dull pain in two separate focal areas of her abdomen that seems to come and go cyclically. She also complains of occasional dyspareunia. Her abdomen is tender to palpation in the areas she described. Which of the following most accurately matches S&S to pathology? a. The cyclical pain is probably related to dysmenorrhea from hormonal malfunction. b. Because of monthly retrograde bleeding, there are bits of ectopic endometrium in the abdomen that cause pain. c. PID has caused bilateral salpingo-oopheritis. d. Endometriosis has caused ectopic areas of cancerous tissue in the abdomen that cause pain on a cyclical basis. Rationale: Endometriosis is when tiny bits of the inner lining of the uterus (called the endometrium), which is supposed to slough off during menses and exit via the vagina, flows in a retrograde fashion through the fallopian tubes into the pelvis and abdomen (remember anatomically the fallopian tubes have a trumpet-like opening & there is a gap between them and the ovaries, through which substances such as retrograde blood & tissue can pathologically pass out of the uterus into the pelvic cavity and beyond). Often these bits of tissue attach to random places—the pelvic wall, places in the abdomen, the intestines, the bladder, etc—and we call them ectopic growths or ectopic areas (because they are in places out of the norm—the meaning of the word “ectopic”). They are affected by hormones and will cramp and bleed and cause pain, the pattern of which is different for each individual but often occurs during menses or with activities that aggravate the ectopic area, such as intercourse, or even sometimes bowel movements or urination. This is not a cancer (D), nor is it an infection (C), nor does it exactly fit answer A, because a person doesn’t have to have dysmenorrhea (heavy or irregular periods) to have endometriosis. 20. Several years later the patient in question 19 has a bowel obstruction and has emergency surgery. How does this surgical incident relate to the situation above? a. The cancerous tissue spread and invaded the bowel. b. The PID infection spread to the bowels and caused chronic inflammation. c. Ectopic endometrial bleeding eventually caused adhesions that obstructed the bowel. d. Adhesions from hormonally-triggered amenorrhea eventually caused bowel obstruction. Rationale—Adhesions are the term given when scar tissue (in this case caused by chronic periods of bleeding from the ectopic endometrium) causes parts of the anatomy to “stick together” inappropriately. To understand why A & B are wrong and C is correct, see rationales in previous question. D is wrong because amenorrhea is lack of menstruation; no bleeding = no problem with retrograde endometrial flow. 1. A person diagnosed with meningitis will be at risk for a. increased intracranial pressure. b. decreased cerebral edema. c. a negative Kernig’s sign. d. motor tract decussation. Rationale: Meningitis causes irritation around the spinal cord & brain, which can result in edema and increased intracranial pressure, not decreased cerebral edema (B). Some kind of meningeal irritation is suspected when there is a positive Kernig’s, not a negative one (C). Motor tract decussation (D) is a normal anatomic finding—the corticospinal tract (AKA pyramidal tract) crosses over (decussates) at the medulla. 2. Upon assessing his patient, a nurse notes hemiparesis of the right arm & leg and dysphasia which the patient states began 2 days ago. The nurse therefore thinks it is most likely that the patient has had a. basal ganglion issues. b. a stroke involving the left hemisphere of the brain. c. a brain attack involving the right hemisphere of the brain. d. a TIA involving the left hemisphere of the brain. Rationale: Because of decussation of the corticospinal tract, hemispheric lesion effects show up on the contralateral (opposite) side of the body below the shoulders, thus a right-sided weakness (hemiparesis) would indicate a left brain lesion, not a right brain lesion (C) in which one would expect left-sided weakness. Also, it is the left brain that houses the centers for speech, so it makes sense that the patient also is dysphasic. Answer A is wrong because there is no mention of S&S related to basal ganglion disorders such as Parkinson’s. A TIA (transient ischemic attack) can be ruled out (D): although the S&S of the scenario can be seen in a TIA, they would have disappeared within 24hours, not still be there 2 days later. 3. A nurse reviewing the drug list of a Parkinson’s patient notes that he is on an anticholinergic drug. The nurse knows that the reason for the patient to be on this drug is most likely a. due to risk for increased environmental allergies. b. to suppress some of the function of acetylcholine in the brain. c. to stimulate adrenergic receptors in the eyes. d. to decrease dopamine levels of the brain. Rationale: An anticholinergic drug suppresses the parasympathetic (cholinergic) nervous system & its main neurotransmitter, acetylcholine. Because Parkinson’s etiology is related to a decrease in dopamine, the lack of dopamine inhibition (in the basal ganglion system, dopamine exerts an inhibitory effect) results in increased basal ganglionic excitatory activity (due to unimpeded acetylcholine effect). So an anticholinergic drug would help to suppress this activity. Certainly you wouldn’t want to give a drug that decreased the already low levels of dopamine (D). Answer A is wrong; many antihistamines like Benadryl have anticholinergic effects, which is why they are given to Parkinson’s patients, but in this case their purpose would not be allergy-related. A sympathetic drug would stimulate adrenergic receptors (C), and this has nothing to do with our scenario anyway. 4. A patient with myasthenia gravis is on a drug to block an enzyme called cholinesterase. This drug’s action will help the patient by decreasing the a. amount of acetylcholine in neuromuscular junctions. b. build-up of senile plaques. c. effect of hypertonia. d. breakdown of acetylcholine in neuromuscular junctions. Rationale: Myasthenia is an autoimmune disease whose etiology is the destruction of acetylcholine receptors at the distal side of a neuromuscular junction synapse. Less receptors = less response to acetylcholine weakness. Cholinesterase is the enzyme that breaks down any extra acetylcholine in the synapse, so a drug that blocks cholinesterase would essentially result in MORE acetylcholine, which would compensate at least somewhat for the decreased numbers of functioning receptors. A drug that decreased acetylcholine (A) would be detrimental. Senile plaques (B) are seen in Alzheimer’s. Hypertonia (rigidity), answer C, is not a problem in myasthenia (it is often seen in Parkinson’s). 5. A patient complains of severe vertigo and nausea. The RN notes the presence of nystagmus. Which of the following would be the most likely diagnosis? a. brain stem stroke. b. papilledema. c. age-related macular degeneration (AMD). d. cerebellar stroke. Rationale: Cerebellar CVAs (stroke) usually involves dizziness, coordination problems, nystagmus (eyes rapidly move back and forth), & balance problems. A brain stem stroke (A) would cause S&S related to primitive reflexes, diminished autonomic function, and certainly a person wouldn’t be alert enough to complain of nausea and vomiting. Papilledema (B) is when swelling is noted in the retina via an ophthalmoscope—it often is an indicator of cerebral edema & IICP “pushing” on the retina; it is part of the S&S of IICP, but not a diagnosis, and may or may not occur in this situation. AMD (C) is an eye disease involving deterioration of the macula, which controls central vision. It doesn’t fit with this scenario. 6. S&S of unconsciousness and unilateral decerebrate posturing would indicate a. a diffuse lesion involving edema throughout the brain. b. a focal lesion involving an increase in ICP on one side of the brain. c. Alzheimer’s disease. d. multiple sclerosis. Rationale: The situation in the scenario describes some of the more severe signs of focal cerebral injury and edema -- asymmetric signs like, for instance, one-sided decerebrate posturing. Diffuse lesion (“all over the brain”-- A) would result in more or less bilateral, symmetric problems instead of unilateral. Alzheimer’s problems (C) would involve memory problems and physical S&S that are not usually unilateral. Multiple sclerosis (D) is an intra-brain disorder of deterioration of myelin sheaths; conceivably a patient with a severe case of MS could end up with a similar scenario to this one, but the S&S would be asymmetric, not diffuse & bilaterally equal as implied in this scenario. 7. A patient reports a pattern of periodic severe headaches and is diagnosed with migraine. He is given a prescription for a medication that will help. His nurse shows understanding of the pathology of a migraine when she instructs the patient to a. take the medication at the first sign of the migraine. b. wait to take the medication until the migraine’s postdrome. c. take the medication at the peak of the migraine. d. avoid taking the medication during the migraine’s prodrome. Rationale: Many of the migraine-related drugs are considered “abortive”—that is, the earlier they are given (ie, during the prodrome), the better the result. So that makes answer A correct and answer D wrong. Many migraine medications are useless after the migraine already has a good “hold” on the patient, so it is not likely to be helpful to take it at the peak (C). And certainly the nurse knows that a postdrome is that periods of tiredness and weakness after the migraine is gone—there is no reason to take the medication then (B). 8. CSF testing on a patient with fever and neck stiffness shows a high protein level. This is most likely due to a. leakage of protein into the CSF from traumatic injury. b. edema from an embolic stroke. c. the presence of bacteria in the CSF. d. the presence of amyloid in the CSF. Rationale: Meningitis is an infection of the meninges, and bacteria is usually found in the fluid (CSF) that flows between two of the meningeal layers. Bacteria is seen in the CSF test as a type of increase in protein (normally there is only a small amount of protein in the CSF). A spinal cord injury (A) might result in leakage of CSF (depending on the mechanism of injury) but it would not be consistent with other clues in the scenario, such as fever & neck stiffness, which are characteristic of meningitis. Any kind of a stroke (B) usually results in some degree of cerebral edema & increased ICP, but the scenario does not suggest stroke, and also an embolic stroke would not increase protein in the CSF. Amyloid (D) is a substance that accumulates pathologically in the brain tissue (not CSF) & causes Alzheimer’s. ***Questions 9 - 11 refer to the following patient: A 74 year old man in the ER has had a severe MI, which led to Vfib. He then had a several-minute period of pulselessness & apnea before his breathing was finally restored. His BP is 78/56. He is unconscious and unresponsive to any kind of stimulus. 9. Which mini-concept map is best to describe causal events and likely patient presentation in this scenario? (you may need to review a bit of cardiac info for this question) a. MI & ventricular fibrillation diminished cardiac output to brain decreased cerebral perfusion pressure (CPP)diffuse ischemic brain tissuediffuse cerebral edemaincreased intracranial pressure (ICP)comatose state. b. Pulselessnesslow BP increased CPPdiffuse arterial bleeding onto brain tissue irritation of brain cellsdiffuse cerebral edemaincreased ICP comatose state. c. MI & ventricular fibrillationembolus thrown from right ventricle directly to brain stem via brain stem ischemia respiratory and other reflex functions affectedpulselessness, low BP, and apneacomatose state. d. MI & ventricular fibrillation diminished cardiac output to brain decreased cerebral perfusion pressure (CPP)focal cerebral edemaincreased ICP of left side of brainleft pupil fixed and dilated and right arm and leg flaccid. Rationale: The scenario is descriptive of a severe ischemic event that results from no cardiac output/no BP/no perfusion/no O2, because heart is in vfib. This would affect the whole brain diffusely in exactly the way described in answer A. Answer D, on the other hand, describes a FOCAL event affecting only one area of the brain. B is wrong because if you are pulseless you will have no BP and therefore NO CPP (cerebral perfusion pressure) at all, not an increased CPP. C is wrong because again, if you are in vfib and pulseless there is NO flow at all from the heart to the brain and therefore no embolus can flow anywhere from the heart, not to mention that an embolus coming from the right ventricle would go into the pulmonary vessel system, not up into the brain. (NOTE: this scenario asks you to remember a bit of your cardiac knowledge. Bear in mind that the final exam will have questions with a “mix of knowledge” like this, since it is a comprehensive exam.) Choose from this list for questions 10 & 11: (in blue are the choices that match the scenario) A. decorticate posturing of the right arm and leg; left side normal. B. symmetric decerebrate posturing of arms and legs. C. complaint of severe nausea and dizziness. D. asymmetric grip strength. E. garbled speech. F. bilateral positive plantar reflexes. G. positive Babinski on the right, negative on the left. H. Cheyne-Stokes respirations. I. “upgoing big toe” bilaterally. 10. Additional S&S most consistent with the correct answer in #9 include a. A b. B This is the only one of the choices that is consistent with diffuse brain edema. c. E d. G 11. Additional S&S most consistent with the correct answer in #9 include a. C b. D c. A d. F This is the only one of the choices that is consistent with diffuse brain edema. Rationale: First, review what you know about this patient neurologically: he is comatose, meaning he is not responding to most stimuli appropriately. Certainly he would not be speaking while in coma, so C and E are wrong. (C might be correct if we were talking about a cerebellar problem, and E might be correct if about a stroke of the left hemisphere.) Secondly, the brain “injury” is a diffuse one— the ischemia is diffuse, meaning not in a focal area, so A, D, & G are wrong—they might be correct in other questions having to do with focal injury. B is correct because diffuse brain injury correlates with fairly symmetric abnormalities, including symmetry in the motor abnormality called decerebrate posturing. (see page 338 in book for pics). Answers F and I are correct because bilateral means both sides, which goes with diffuse injury, and “positive planter reflexes” is the same thing as positive Babinski and “upgoing toe.” http://i.quizlet.com/i/8oU2EC_ciAN_3oOZSR8SzA_m.jpg The Babinski reflex is positive when the big toe goes up as the plantar side of the foot is being stroked from heel to toe—this is also known as a positive plantar reflex and sometimes just “upgoing big toe” response. This positive response is normal in children under two, but after this age the big toe should no longer “go up”; if it does, this indicates some sort of neural abnormality—the pathologic recurrence of an infantile reflex. So it is quite likely that this patient (having had diffuse brain ischemia) would have bilateral positive Babinski reflexes. Similarly, the brain stem is probably quite ischemic, so respirations may be abnormal, as in answer H—Cheyne Stokes is a form of irregular breathing seen in some comatose patients. ***Questions 12-15 refer to the following patient: (see concept map of brain attack) A 28-year-old woman with a history of severe HTN presents to the ER with certain S&S that are consistent with brain attack (stroke). A CAT scan shows bleeding in one hemisphere of the cerebrum. List for questions 12 - 15: (in blue are the choices that could match the scenario) A. The bleeding in the brain is likely caused by decreased cerebral perfusion pressure secondary to hypertension. (HTN would cause INcreased CPP, not decreased) B. If the patient denies the presence of people standing on her left side, this would be consistent with a problem called left-sided neglect. C. The bleeding caused irritation of the brain, inflaming the area and causing edema to press pathologically on certain corticospinal tracts that control the contralateral side of the body below the shoulders. D. Right-sided neglect is the term given when, due to impaired spatiality controlled by the left hemisphere, a patient denies the presence of people standing on her right side. (The RIGHT hemisphere controls spatiality, and when impaired, can cause LEFT sided neglect. To my knowledge, right- sided neglect is non-existent, or at least rare.) E. Sensorimotor changes above the shoulders usually reflect impairment that is ipsilateral to the brain hemisphere that has bleeding and/or edema. F. If the patient is unable to talk, she is also probably unable to smile on the right side of her face. (Speech is usually controlled by the left hemisphere; so if she can’t talk, she can’t smile on the ipsilateral side, which would be the left side. This is because cranial nerves don’t cross—they simply go directly and control the same-side of the body above the shoulders.) G. The bleeding caused irritation of the brain, inflaming the area and causing edema to press pathologically on certain corticospinal tracts that control the ipsilateral side of the body below the shoulders. (Below the shoulders, ie, below the control of the cranial nerves, the halves of the body have motor control by corticospinal tracts that have crossed from the opposite side—contralateral side-- of the brain). H. If the bleeding is in the left hemisphere, the patient is likely to have right-sided neglect related to impairment of spatiality. (See explanation for D) I. If the patient’s right pupil does not react to light (ie, doesn’t constrict), she likely also has hemiparesis of the right arm and leg. (Right eye not constricting is likely due to the same-side controlling cranial nerve being impaired. That implies that the control of the corticospinal tracts that originate in the right hemisphere would also be impaired and therefore, since they decussate before taking signals to the body from the brain, the below-the-shoulders impairment would be on the left, such as left arm & leg hemiparesis. PEARL: DRAW PICTURES when y’all are trying to figure out questions like these). J. Interventions for this patient should include raising the head of the bed to about 30 degrees to minimize increased ICP. K. Sensorimotor changes above the shoulders reflect impairment that is contralateral to the brain hemisphere that has bleeding and/or edema. (Correct would be IPSIlateral…see some of above explanations) L. Interventions for this patient should include an anticoagulant to prevent pathological clotting in the areas of cerebral edema. (If this was a pure ischemic stroke—no hemorrhage involved—this patient likely would need anticoagulation. But it wouldn’t be a good idea to put her on an anticoagulant since she is already bleeding onto the brain.) M. If the bleeding is in the right hemisphere, the patient is likely to deny that she has any illness or impairment at all. N. If the patient is unable to talk, she is also probably unable to smile on the left side of her face. O. If upon assessment, the patient has a weak hand grip on the left and normal strength of the right hand grip, the brain bleed is most likely in the right cerebral hemisphere. P. Testing shows that the patient has lost some math skills, demonstrating the likelihood that a “special functions” portion of the right cerebral hemisphere has been compromised. (The left cerebral hemisphere usually controls math skills.) Q. Assessment findings on this patient likely include nystagmus, a typical problem in hemispheric strokes. (Nystagmus is most likely seen in cerebellar problems, not hemispheric ones) In each of questions 12, 13, 14, & 15, choose the answer that is correct from A-Q SUMMARY: You could do a concept map like this: HTN = increased CPP too much pressure on an arterial wall in the brain blood leaks out onto brain tissue irritates inflammation edema. Further, you are given the information that the bleeding is occurring in one side of the cerebrum (focal as opposed to diffuse)… The edema at the end of our mini-concept map will put pressure on motor tracts (AKA corticospinal tracts, AKA pyramidal tracts) that are located in that area of the brain. Since the tracts physically cross (decussate) to the other side of the body below the shoulders, the abnormal messages they send will be seen as motor abnormalities on the opposite side of (ie, contralateral to) the site of edema in the brain. Above the shoulders, when there is a lesion (‘lesion’ being used generically to mean edema, tumor, bleed, etc) in one side of the cerebrum, the abnormal assessment finding will be seen on the same side (ipsilateral) as the lesion… why? Because the cranial nerves (which travel from brain stem through brain tissue to enervate face, neck, shoulders, etc) do NOT decussate. Also, it is important to remember that each hemisphere has its own “special functions;” a left hemisphere bleed would result in problems with speaking, or perhaps problems with math. It is the right hemisphere that usually controls ‘spatiality’—the ability to correctly note things in your environment. When the right hemisphere has bleeding/edema/tumor/ischemia, etc, a person may fail to acknowledge that the “world” on the left side of her isn’t “there.” Plus the right hemisphere controls insight, so if you have a right hemispheric stroke, you may not have the insight to know that there is something wrong with you. As for interventions, it is a good rule of thumb to raise the head of the bed anytime there are brain “issues” since that facilitates the goal of avoiding increased ICP by being flat (flat= easier for more fluid to enter brain more edema IICP.) 16. Which is true? a. An eye drop that constricts the pupil belongs in a medication category that mimics the effect of the sympathetic nervous system (sympathomimetic). b. An eye drop that causes miosis belongs in a sympathomimetic medication category. c. If an eye drop causes mydriasis, it has probably blocked the adrenergic effect of an ipsilateral cranial nerve. d. If an eye drop causes mydriasis, it has probably blocked the cholinergic effect of an ipsilateral cranial nerve. Rationale: The reflexive action of your pupils constricting when exposed to light (miosis) is controlled by a cranial nerve (CN) that secretes a cholinergic (ie, governed by the parasympathetic nervous system) substance—acetylcholine—which causes the constriction. So if you were given an eye drop that inhibits that process, you would end up with non-constricting pupils; ie, your pupils might dilate (mydriasis)— answer D. Adrenergic effect on your pupils is what happens in a “fight or flight” situation—your body says, “prepare for flight by allowing the most light that is possible into your eyes so you can have the best vision possible for running away”…so your body is flooded with adrenergic (sympathetic nervous system) substances such as epinephrine (AKA adrenalin) and your pupils become dilated. So C is wrong because blocking the adrenergic effect would cause miosis (constriction), not mydriasis (dilation). These rationales cover the reasons why A & B are wrong also. 17. A patient complains of sudden intolerable pain in the right eye. Glaucoma is considered as a diagnosis. Which statement is true? a. Open-angle glaucoma is likely, since this disorder causes sudden painful increase in intraocular pressure. b. Closed-angle glaucoma is likely, since this disorder allows too much aqueous humor to be absorbed at once, causing pain. c. Decrease in peripheral vision should be tested for, as this occurs in most cases of glaucoma. d. Decrease in central vision should be tested for, as this is a cardinal sign of glaucoma. Rationale: Closed-angle glaucoma is most often associated with sudden pain, because the angles of the eyes suddenly close off so that the aqueous humor cannot circulate and be absorbed properly; then it accumulates and causes pain from increased intraocular pressure. B is wrong because glaucoma’s pathophysiology is related to LACK of ability to absorb, not INcreased absorption. Answer A is wrong because open-angle glaucoma is usually very gradual, and normally the angles remain at least somewhat open—enough so that some of the aqueous humor continues to be absorbed. No matter what kind of glaucoma it is, the type of vision to be most affected is the peripheral vision—what you notice to the sides of you, so answer C is correct. Central vision (D) is what is affected in AMD. 18. Which statement would most likely lead to a diagnosis of cataracts? a. A 75-year-old woman who states: “My vision has gotten cloudy over the last few years.” b. A 20-year-old diabetic who states: “I’ve got blurred vision.” c. A 65-year-old man who states: “I’ve got this black spot in the middle of my vision.” d. The son of an 80-year-old who states: “My dad has been dizzy for a few hours, and look how his eyeballs are going back and forth! Weird, dude!” Rationale: Cataracts are when a pathologic, proteinacious film begins to accumulate on the lens of the eye, gradually causing less clarity of vision, which best fits with answer A. A diabetic having blurred vision (B) implies that his diabetes is causing vision issues, but cataracts are not a commonly seen long-term effect in diabetes, plus cataracts usually cause people to complain more of cloudiness or a fog rather than blurriness. Answer C fits with age-related macular degeneration (AMD); and answer D most likely describes nystagmus, which is a jerky, back-and- forth pattern of eye-movement most often related to cerebellar problems (or sometime inner ear situations). 19. A patient who is unconscious following brain trauma has a right pupil that is fixed and dilated (ie, will not constrict to light). All the following are likely true about this patient EXCEPT a. The trauma is on the right side of the patient’s cranium. b. Cerebral edema affected cranial nerve (CN) function on the side ipsilateral to the trauma. c. The right eye is not responding normally because of less-than-normal cholinergic functioning of a CN. d. The right eye is not responding normally because of less-than-normal adrenergic functioning of a CN. Rationale: All choices go together except D, so that is the answer. See previous rationales to understand various aspects of this question. 20. The patient above likely a. has flaccidity the right arm and leg. b. will need rehabilitation of the right arm and leg. c. will need speech therapy as part of recovery. d. will need spatial-awareness therapy as part of recovery. Rationale Once you know that this patient has trauma (“lesion”) to the right side of the brain, you know that: 1) special functions that are “ruled” by the right cerebral hemisphere will be affected, and 2) above the shoulders you will see RIGHT-sided problems (ipsilateral to the brain lesion) and below the shoulders you will see LEFT-sided problems (contralateral to the brain lesion). Answers A, B, and C, then, apply with a left cerebral hemisphere problem. The only one that applies to a right hemispheric problem is D, since the patient’s right hemisphere special functions include spatial awareness. (see concept map of brain attack) ***A note for the future: Remember in your neuro RRD I said that in “real life” neuro nursing you might not see S&S exactly like I have presented in the stroke sections. There are so many variables such as SOME branches of the cranial nerves that do decussate, and SOME spinal tracts that don’t decussate, and so forth, but I chose to keep as simple as possible and put all the CNs in one “bucket”—that is, we are going to say that their actions are always ipsilateral; and put corticospinal nerves in another “bucket” in which their actions are contralateral because of decussation. If in the future your patient assessment doesn’t fit into these rules, ask “why?” It may be that they have a more subtle mix of deficits than we study in this class. 1. Following an illness, a patient becomes hypocalcemic. Which of the following negative feedback compensatory mechanisms will increase the calcium in her blood? a. The pituitary will decrease its secretion of T4. b. The thyroid will increase secretion of calcitonin. c. The pituitary will decrease its secretion of parathyroid hormone (PTH). d. The parathyroid will increase its secretion of PTH. Rationale: If a patient is hypocalcemic, the body will sense that more calcium needs to be freed up from bone storage and sent out into the blood, so PTH will be increased (low calcium triggers increase of PTH secretion—“low triggers high”—classic negative feedback), not decreased (C)…. PTH increases osteoclastic activity & resorption, therefore increasing calcium in the blood to normal levels. Calcitonin (B) would do the opposite—“CALCITONIN = “BONE IN “(so its secretion would be triggered if the problem was hypercalcemia.) Answer A is wrong, as T4 is secreted by the thyroid, not the pituitary, and besides T4 has little to do with calcium movement. 2. A person with Graves' disease likely has all the following EXCEPT: a. an autoimmune disease b. Hashimoto’s thyroiditis c. goiter. d. a heart rate of 120. Rationale: Hashimoto’s thyroiditis is the outlier in this except question—it is a cause of hypothyroidism, not Graves’ disease, which is an autoimmune disease that results in hyperthyroidism. A goiter can be seen in either hypo or hyperthyroidism. A heart rate of 120 is too high—this is part of the “overdrive” metabolic situation found in hyperthyroidism. 3. Lab work is done on the patient above. The expected findings would be a ___TSH and a T4. a. low; high b. high; low c. normal; high d. high; normal. Rationale: T4 is high in hyperthyroidism, and because of negative feedback, it continually keeps the TSH suppressed (low), whereas if everything was normal, the two would keep each other in the normal ranges. B would be true in hypothyroidism. C & D are not the most likely combinations seen in the usual thyroid diseases. 4. The patient in question 2 goes into a crisis state, which is called a. myxedema coma. b. tetany. c. thyroid storm. d. cretinism. Rationale: Answer A would be true of a hypothyroid person whose condition significantly deteriorated. Tetany (B) is the state of hyper-toned, rigid muscle reaction & it is associated with hypoparathyroidism or hypercalcitoninism. Cretinism (D) is the state found in a child who has been born of a mother who did not get enough iodide in her diet & therefore did not have adequate thyroid function. Because of this her fetus may not develop properly and may be born with significant mental & physical handicaps; its physical features may also resemble the usual myxedema facies (“facies” = facial characteristics) – puffiness, frog- like-- of a severely hypothyroid person. 5. Osteopenia is likely associated with all the following EXCEPT: a. low dietary calcium. b. hyperparathyroidism. c. high levels of calcitonin. d. increased osteoclastic activity. Rationale: A, B, & D all result in the same situation: Low dietary calciumless calcium to use for bone strengthening. Hyperparathyroidism is basically an increased secretion of PTH increased osteoclastic activity more calcium resorption leeching bone of its calciumhypercalcemia & osteopenia (or worse, osteoporosis). A similar situation might exist with hypocalcitonin states, but high levels of calcitonin (C—the outlier) would cause all the opposite states. 6. A patient who just came out of general anesthesia has lab work done. The serum osmo is 165. The nurse taking care of this patient suspects that his is due to . a. hyperosmolality: diabetes insipidus (DI). b. hypoosmolality: syndrome of inappropriate ADH (SIADH). c. dry mucus membranes: SIADH. d. shift of calcium into blood: a state of hypopolarization inside the cells. Rationale: A serum osmolality of 165 is lower than normal, so think of the blood being more dilute, or hypoosmolar, than usual (not hyperosmolar, as in answer A). The second part of the question, SIADH, is what it is called when there is TOO MUCH ADH circulating. It causes the retention of water, which dilutes the blood. As mentioned in the notes, a postanesthesia situation often triggers the secretion of too much ADH, so the scenario and BOTH parts of the question fit together. DI is the OPPOSITE—it occurs when there is NOT ENOUGH ADH—then the kidneys do not hold on to water, you void it out with the urine in HUGE volumes, and eventually become dehydrated (which goes with hyperosmolality of the blood, answer A). Dry mucus membranes (C) also goes with DI & dehydration, NOT SIADH. Answer D has nothing to do with the scenario you were given. 7. The nurse in the previous question would expect all the following S&S EXCEPT: a. signs of cerebral edema such as decreased LOC. b. signs of cerebral cell dehydration such as headache. c. generalized edema d. crackles in the lungs upon auscultation. Rationale: Three things go together in “except” questions… in this case A, C, & D all go together as being common in a patient with fluid overload. So you WOULD see all those things in a person with SIADH (the correct answer in #6). The only thing you wouldn’t see is answer B, which goes with a dehydration (fluid deficit) picture. 8. A 68 year old female patient’s bone density scan shows osteoporosis. Her healthcare provider is trying to figure out the primary etiology. One possible cause is related to her past history of having had a thyroidectomy. Which statement is most likely correct in linking this surgery with the risk of osteoporosis? a. When the thyroid is taken out, calcitonin decreases, thus diminishing the body's ability to absorb calcium from food into the blood. b. Often accidentally removed with the thyroid are parts of the parathyroid, so there will be less calcitonin from the parathyroid and less calcium staying in the bone. c. When the thyroid is taken out, calcitonin decreases, thus decreasing calcium movement into the bone. d. The surgery actually has less to do with osteoporosis than the patient’s age does; greater age means decreased osteoclast activity, and less calcium being resorbed. Rationale: The thyroid secretes calcitonin, whose job is to move calcium from blood to bone (“bone IN” rhymes with calcitonin). If you take out the thyroid, less calcitonin less calcium goes into bone and greater risk of osteoporosis. Answer A is wrong, since the second half of the answer is not correctly linked to the first half. B is wrong because the parathyroids “rule” PTH, and if they were taken out, it would be less PTH rather than “less calcitonin” that would affect the patient. Greater age means INcreased osteoclastic activity (not decreased), and thus GREATER calcium resorption—movement of calcium out of bone into blood. (D) Greater age would indeed contribute to osteopenia and osteoporosis, but the reasons here are not correct. 9. A patient with Type I diabetes has a pH of 7.32. This is most likely caused from the byproducts of increased: a. insulin resistance. b. hyperinsulinism. c. gluconeogenesis. d. glucagon. Rationale: Type I diabetics have no insulin at all, therefore must rely on alternate energy-providing means. They quickly use up their glycogen stores & so cannot further rely on glycogenolysis. So they essentially live in a state of gluconeogenesis; for this they first break down their fat, then their muscles (protein). This yields glycerol (a form of sugar) & ketones, which can serve as energy but also can result in ketonemia, ketonuria, and acidosis hence the pH of 7.32. Insulin resistance (A) is found in Type II diabetics & results in a temporary state of hyperinsulinism (B). Glucagon (D) is a counterregulatory hormone which is released when we are hypoglycemic—it will stimulate glycogenolysis so that we have access to stored sugar; it doesn’t apply in this case because diabetes is a problem with hyperglycemia, not hypo. First go through this list and decide if the choice is classically seen in either Type I or Type II diabetes mellitus. Or may the statement/word be equally applicable to BOTH? Then use the list to choose the correct answers to questions 10-15. (Be sure you understand the pathologic “why” of all your choices.) A. macroangiopathy. B. polyphagia. C. neuropathy. D. risk for dehydration. E. use of Kussmaul respirations as a compensatory response to a crisis. F. risk for high serum osmolality. G. microangiopathy. H. presence of acetone breath in a crisis. I. insulin as a possible/ probable medication. J. oral anti-hyperglycemic meds as possible/ probable medications. K. sweaty skin in a crisis (this is a maybe as a “both” but only if they are taking antiglycemic meds & have a hypoglycemic reaction) L. blood pH < 7.35 in a crisis M. insulin coma (this is a maybe as a “both” but only if they are taking antiglycemic meds & have a hypoglycemic reaction that includes unconsciousness) N. diabetic coma O. DKA P. insidious onset of S&S Q. HHNKS 10. Type I and Type II diabetes usually have in common all the following EXCEPT a. A b. C c. D d. L <7.35 is acidosis, which is seen in the crisis state of Type I DM (DKA—diabetic ketoacidosis. In Type II DM, the crisis state is HHNKS (hyperglycemic hyperosmotic non-ketotic syndrome,) which often does NOT involve an acidosis. So they do NOT have this in common. 11. Ways that Type I and Type II diabetes usually differ include all the following EXCEPT: a. E b. H c. G d. J 12. A person with DM has a BS of 350. He is not on any medications. He is likely to have one or more of the issues below EXCEPT a. K (sweaty skin is seen in someone with HYPOglycemia; if a diabetic is taking antiglycemic meds such as insulin & takes too much, plunging them into severe hypoglycemia, then they might have a crisis state in which they have sweaty skin, but as it stands, with only hyperglycemia in your question and no other info, K is the best answer.) b. F c. D d. G 13. In which case would you give glucagon as an emergency medication? a. L b. M An insulin coma is almost saying the same thing as “hypoglycemic” coma; it is a severe hypoglycemic state caused by too much insulin or other antiglycemic medication. You rarely see someone in a hypoglycemic coma that is NOT related to being a diabetic and accidentally taking too much med (unless they have an underlying disease like Addison’s); that is why sometimes insulin coma is used interchangeably with hypoglycemic coma. c. N d. O 14. An emaciated 18-year-old man presents with complaints of polydipsia and weight loss. His blood glucose is 258. All the following likely apply to his situation EXCEPT: a. F b. P Thin, young patient most often means DM1, with its more acute S&S—not usually insidious like DM2 S&S are. c. B d. O 15. An obese 59-year-old man in an unconscious state is brought to the emergency room. His blood sugar is 800. All the following likely apply to his situation EXCEPT: a. N b. O Obese, older age most often means DM 2; DKA is most likely in DM 1. c. Q d. P Further rationales on choices A-Q : Apply only to one but not the other: B—polyphagia— increased hunger & eating is seen in Type I diabetes in an attempt to make up for no glucose in the cells secondary to no insulin (despite eating, they stay thin, because of gluconeogenesis—breaking down of fat & muscle); Type II diabetics have SOME insulin, therefore have SOME glucose in their cells & don’t get extreme hunger & need to eat (usually). E—Kussmaul respirations are seen in Type 1 diabetics with DKA; the lungs try to compensate for the metabolic acidosis by increasing depth of breathing so as to blow off CO2. Type II diabetics don’t get DKA (usually—remember, in “real life” there may be compounding circumstances), so usually don’t have Kussmaul respirations. H—energy is provided to cells via gluconeogenesis in Type I diabetics; a byproduct is acetone. Type II’s still have some glucose for their energy needs. J—oral anti-hyperglycemic meds aren’t effective in Type I diabetics, who need insulin alone; they ARE effective in Type II’s because each med approaches the complex problems (such as insulin resistance) in a different way. L-- type I diabetics can go into a type of acidosis (DKA) because of the high ketone levels, whereas Type IIs, if not treated or undertreated, can go into a nonketotic state of severe S&S —HHNK. P & Q are problems seen in DM2, which comes on very slowly and insidiously, allowing the blood glucose to get extra high before S&S become a crisis state; if they do go into a crisis state, it usually doesn’t have acidosis involved, and in fact is called HHNKS—hyperglycemic hyperosmolar non-ketotic syndrome. Apply to both: A,C,D,F,G are things that Type I & II DO have in common. A, G are long-term changes in large & small arterial vessels that occur in both types of diabetes. C occurs in both because of damage to the nerves from toxic levels of glucose. D & F-- both types of DM involve hyperglycemia, which means glucose spills into urine, draws the water out of the blood & causing high serum osmolality & risk for dehydration. K—sweaty skin MAY be seen in either types of DM, but ONLY IF the person is on meds and become hypoglycemic : if a diabetic who is on an anti-glycemic medication develops LOW blood glucose, he may have the S&S of hypoglycemia such as sweating, tachycardia, etc (see “DM and hypoglycemia concept map”) due to presence of counterregulatory hormones. USUALLY any kind of diabetes is considered a “dry” disease, with S&S of dehydration. 16. A patient recently had his parathyroids removed. What S&S might be present as a result of this situation? a. A positive Chvostek’s sign might be elicited as a result of hypocalcemia. b. A negative Chvostek’s sign might be elicited as a result of hypocalcemia. c. The patient might feel fatigued due to hypercalcemia. d. PTH and calcitonin would become competitors for calcium, resulting in a calcium- movement war. Rationale: To understand this question, ask yourself what the parathyroids normally do—they secrete PTH (parathyroid hormone). When PTH secretion is increased for whatever reason, two things happen then: 1) high circulating PTH suppresses the secretion of calcitonin from the thyroid gland, 2) osteoclasts INcrease their destruction of bone cells, setting free calcium, 3) calcium goes from bone to blood, which is called resorption. Result/correction- - more calcium in the blood, less in the bone. And pretty soon as things stabilize everything goes back to normal levels. (see your endocrine prep for more A&P as needed) So knowing the normals, what will happen when they are taken out? No PTH = less osteoclastic activity = no resorption of calcium into blood = hypocalcemia (NOT hypercalcemia, answer B.). Because hypocalcemia causes HYPOpolarization of cell membranes, the cells are more sensitive and irritable (hypercalcemia does the opposite. When you test the hypocalcemic patient for Chvostek’s sign, you are using their cheek as a measurement of cell hyperirritability. If the cheek draws upward in sort of a smile INVOLUNTARILY, that is a pathologic sign called a positive Chvostek. It means, yes, they are probably hypocalcemic, and a serum calcium level lab test will tell you for sure. 17. The nurse caring for a woman with Cushing’s disease may expect assessment finding of all below except: a. exophthalmos. b. hirsutism. c. truncal obesity. d. high blood pressure. Rationale: This is an except question. Answer A (bulging eyes from extra tissue behind them, caused by metabolic changes of too much thyroid hormone) is associated with hyperthyroidism; the rest occur with abnormally increased cortisol levels, which is a cornerstone of Cushing’s. 18. A patient presents with S&S of dehydration, weight loss, and a blood glucose of 50. A likely diagnosis is: a. Cushing’s disease. b. hyperpituitarism. c. hypothyroidism. d. Addison’s disease. Rationale: Because of abnormally decreased aldosterone in Addison’s, the body doesn’t “hang on” to sodium & therefore also doesn’t hang on to water— there is polyuria & subsequent dehydration. Also, because there is abnormally low cortisol, blood glucose is low—the patient will be fatigued, weak, underweight. Cushing’s (A) is the opposite of many of these S&S, since there is excess cortisol. B is wrong because though Addison’s can possibly be caused by pituitary problems, it wouldn’t be HYPER pituitary problems—more likely HYPO pituitary. C is wrong, because Addison’s is an adrenal problem. 19. Complaints of polydipsia and polyuria could be linked to all the following disease processes EXCEPT: a. DM b. Addison’s disease. c. diabetes insipidus. d. SIADH. Rationale: This is an except question. Syndrome of inappropriate antidiuretic hormone (SIADH) would result in “holding on” to water & not urinating as much, because of an excess of ADH. 20. If you were the NP prescribing for a patient with osteoporosis, you would prescribe a medication that would . a. increase osteoclastic activity b. increase calcium resorption c. decrease osteoclastic activity d. increase osteopenia Rationale: Anytime you have increased osteoclastic activity, it means the osteoclasts are breaking down more bone tissue and bring calcium from bone to blood (calcium resorption). Sometimes this is appropriate; other times, when it causes too much calcium coming out of the bone, it is pathologic, and the person ends up with “porous” bones— osteoporosis (or not quite as bad—osteopenia). So if you have osteoporosis, you would want to take a medication that decreases the calcium-leaching process, ie, diminishes osteoclastic activity and thus lessens resorption. ~~~~~~~~~~~~~~~~~~~~~~~~~~~~~ 1. A patient with cirrhosis and all its associated problems has an RBC count of 2 million, and thombocytopenia. These low numbers are most likely caused by: a. cellular hemolysis from pancreatitis. b. splenomegaly secondary to portal hypertension. c. esophageal varices secondary to portal stricture. d. cholecystitis due to malfunctioning lithotripsy. Rationale: Cirrhosis means the liver has become full of fibrotic tissue, which means it is essentially a “stiff” resistance to the venous blood that usually flows to it from the portal vein, which is a large vein that receives blood from the other abdominal organs (spleen, GB, stomach, intestines). If the portal vein cannot empty into the liver, there will be back pressure (“portal HTN”) into the venous systems of those organs. The spleen will become larger (splenomegaly) from the venous congestion and hypersplenism will take place—the process of pathological breakdown of RBCs (hemolysis), WBCs, and platelets. Answer A is wrong, because though this person does have anemia from hemolysis, it does not occur in the pancreas. Esophageal varices (congested veins in the esophagus) will occur in portal HTN, but have nothing to do with the anemia. D is an off-the-subject question —stones in cholelithiasis can be broken down by an ultrasound process called lithotripsy, but cholecystitis would not likely be a sequela and doesn’t relate to the patient’s anemia. 2. The patient in question 1 also has ascites. In reviewing the patient’s lab work, the nurse understands that one likely cause of the ascites is: (normal osmolality is 280-295) a. serum osmolality of 275 due to decreased serum proteins. b. serum osmolality of 300 due to increased serum proteins. c. hypernatremia due to decreased levels of aldosterone. d. hypernatremia due to increased levels of aldosterone. Rationale: A cirrhotic liver cannot adequately produce proteins, so the patient likely has a low osmolality from hypoproteinemia fluid shifts into tissues, including the abdominal tissues (ascites). Answer B (an osmolality of 300) would draw water into the plasma space, not cause ascites (in fact, this is why we sometimes give an IV of albumin to these patients—to draw off ascites & other edema fluid). A decreased aldosterone (C) would cause spillage of Na & H2O into the polyuria, thus resulting in a hyponatremia, not hyper. A hypernatremia might result from increased aldosterone, but hypernatremia is a hypertonic state of the plasma state & would not result in edema in the abdomen (ascites) or anywhere else. 3. A jaundiced patient has a higher than normal direct bilirubin. The mechanism most likely responsible for this is , and a likely responsible disease process is . a. prehepatic obstruction; erythroblastosis fetalis b. increased unconjugated bilirubin; hepatitis. c. posthepatic obstruction; cholelithiasis. d. transmural intestinal ulceration; Crohn’s disease. Rationale: Bilirubin is conjugated in the liver and passes into the intestines and/or GB as part of bile. If there is an obstruction to this passage, such as stones in the GB and/or ducts, bile can back up & the bilirubin can leak back into the blood stream, resulting in a high DIRECT (conjugated) bilirubin. This patient would have posthepatic jaundice. Answer A is wrong because “prehepatic obstruction” doesn’t make sense; what would have made sense would be prehepatic jaundice secondary to erythroblastosis fetalis. However, prehepatic jaundice corresponds to high INDIRECT bili, not direct. In answer B, increased unconjugated (indirect) bilirubin does correspond to hepatitis, but not to the question’s stem, which asks about high direct bili. D is another off-the-subject question: Crohn’s disease does correspond with transmural intestinal ulceration, but not with the stem of this question. 4. The nurse caring for a patient with cirrhosis notices signs and symptoms of encephalopathy such as confusion and asterixis. The cause of these is most likely: a. increased serum lipase. b. low serum liver enzymes. c. decreased conjugated bilirubin. d. increased serum ammonia. Rationale: The liver not only produces proteins, but also participates in their breakdown as needed. Ammonia, for instance, is a protein product that circulates to the liver & is broken down to urea, then secreted by the kidneys. If ammonia cannot be broken down by a diseased liver, it collects in the blood & causes irritation to many tissues, including and especially the brain. Irritation to brain tissue = inflammation = cerebral edema = confusion, etc. Answer B is generally a true statement in cirrhosis; that is, decrease in protein production also means decrease in clotting factors, which means increase in the time it takes to clot prolonged PT & PTT. However, this fact doesn’t answer this question. Decreased conjugated bili (C) will not cause encephalopathy. Answer A correlates with pancreatitis. 5. A patient is having melena stools. This is most likely due to: a. low level of intrinsic factor in the gut. b. digested blood from a duodenal ulcer. c. gastroparesis causing slow emptying. d. hematemesis from PUD. Rationale: Melena is black tarry stools; the color and consistency is due to the presence of digested blood (digestion takes place in stomach & duodenum). Gastroparesis (C) does mean slow emptying of the stomach but this would not cause melena; gastroparesis is most often associated with diabetic autonomic neuropathy. Hematemesis is having blood in the vomit and is associated with PUD. However, melena is not due to hematemesis—they can both be signs of PUD. Pearl: Be careful of how a question is phrased. Plug each answer into the question. Also, as a study tool when you are going over these answers, think of situations when the wrong answer in this situation could be the right answer in another. For instance, ask yourself: when would answer A be correct? The answer-- if this question asked “what can result in pernicious anemia?” Or “what can cause low B12 absorption?”…. etc. 6. The patient at most risk for an intestinal obstruction would be one who a. smokes and consumes large amounts of caffeine. b. is on prolonged bedrest. c. is eating a high fiber diet. d. has diverticulosis. Rationale: Someone on prolonged bedrest would be at risk for a paralytic ileus, which “acts like” an intestinal obstruction because peristalsis stops & toxins, gas, fluids, etc collect in the intestines & can result in inflammation & infection. Answer A more likely corresponds with someone with PUD. Answer C is wrong because eating a high fiber diet is usually a good thing to do to increase peristalsis and thus avoid an obstruction. Someone with diverticulosis would be at risk if they progressed to diverticulitis & the inflammation & scarring caused obstruction; but if a person only has un-inflamed diverticula (“osis” = “state of”, “itis” = inflammation), obstruction is not that high a risk. 7. A patient with ulcerative colitis will have a. a paralytic ileus. b. patchy area of inflammation of the jejunum. c. intestinal polyps. d. hematochezia Rationale: Frankly bloody stool (hematochezia) is mostly seen in ulcerative colitis. Answer B would classically correspond to Crohn’s and not ulcerative colitis. C is sometimes associated with colon cancer (though polyps can be completely benign) and A is a functional obstructive problem caused by cessation of peristalsis. 8. All the following are consistent with upper GI problems EXCEPT a. GERD. b. H. pylori. c. esophageal varices. d. diverticulitis. Rationale: Diverticula usually form in the sigmoid colon, part of the lower GI. The rest are all upper GI related: GERD (A) is reflux of stomach contents into the esophagus; H. pylori is a bacteria that increases risk for PUD; esophageal varices occur when there is venous congestion in the esophageal veins from portal HTN. 9. A patient with choledocholithiasis is likely to have a because . a. high serum direct bilirubin: obstruction of bile duct results in leakage of conjugated bilirubin into the blood. b. normal level of conjugated bilirubin; prehepatic breakdown of RBCs is unaffected. c. low serum direct bilirubin: obstruction of bile duct results in leakage of unconjugated bilirubin into the blood. d. high level of indirect bilirubin: a stone in the bile duct causes bleeding and hemolysis. Rationale: Answer A says it all— this is a good summation of posthepatic (obstructive) jaundice. The other answers have bits and pieces that are wrong. Pearl: For practice, take an answer like this that corresponds to posthepatic jaundice & redo it so that it is a summary for prehepatic jaundice. 10. All the following statements could apply to a child with cystic fibrosis EXCEPT: a. He presents with difficulty coughing up phlegm due to its increased viscosity. b. Secretions in the pancreas and lungs are excessively dilute because of a genetic mutation. c. Sodium imbalance across the plasma membrane of pancreatic cells leads to cellular dehydration and blocking of pancreatic enzymes. d. Increased cellular concentration of salt results in a positive sweat test. Rationale: The genetic mutation that causes cystic fibrosis negatively affects chloride channels of certain tissue cells, including those in the lungs, pancreas, and sweat glands. Because sodium & chloride go together so closely, the malfunctioning chloride channels cause changes in the salt concentration of cells’ secretions. These changes result in more highly concentrated secretions, so instead of having normal secretions that lubricate the lungs, for example, the secretions are very thick & mucoid due to their higher solute / less water concentration. Same in the pancreas, where the thickening of normal, lubricating secretions don’t allow amylase & lipase into the intestines to help with digestion. In the sweat glands the situation is the same, and results in much saltier sweat. So A,C, & D are all consistent with cystic fibrosis, whereas B is the outlier due to the words “excessively dilute,” which is the OPPOSITE of the primary patho. See the table. It is numbered I-XV. In the right column are words and phrases that link in some way with each of the numbered items on the left. In other words, this is a typical “matching” exercise. Read the scenario and fill out the table FIRST, then use it to answer questions 11-20 below. THERE IS ONE ANSWER TO EACH LEFT-HAND TERM, AND DO NOT CHOOSE THE SAME ANSWER MORE THAN ONCE. CHOOSE THE BEST FIT. Scenario: A 47 y/o female patient presents to the ER with the following complaints: “I’m short of breath and swollen all over.” She reports a history of heavy ETOH (alcohol) use & has had worsening cirrhosis for many years. On examination she is noted to be confused and to have icteric sclera, various areas of bruising, infected skin sores, crackles in her lungs, & a distended abdomen. Labs are done. The following matching exercise describes various aspects of the patient’s presentation and pathophysiology, and also some problems that might occur because of her cirrhosis. I. etiology of “swollen all over” G A. increased destruction of WBCs due to hypersplenism II. direct bilirubin level L B. AST 1000 (normal 10-40); ALT 1100 (normal 10-55) III. has caused fatigue, and also caused some of SOB E C. causes retrograde venous flowesophageal varices may be present IV. hyperaldosteronemia I D. serum osmolality of 260 (normal = 280- 295) fluid shifts into alveoli V. damaged hepatocytes intra-cellular enzymes leak into blood B E. hypersplenismincreased destruction of blood cells RBC count = 2.5 mill (norm = 4 to 6 mill) VI. icteric sclera K F. decreased metabolism of cortisol hypercortisolism VII. portal HTN C G. malfunctioning hepatocytes hypoproteinemia fluid shift from blood to tissue VIII. unconjugated bilirubin not being conjugated by cirrhotic liver J H. ascites IX. etiology of infected sores A I. malfunctioning hepatocytes decreased breakdown of aldosterone X. hypersplenismthrombocytopenia N J. high indirect bilirubin in the blood. XI. decreased ability to break down ammonia high serum ammonia levels. O K. assessment finding related to presence of pathologically high bilirubin in tissue cells XII. blood glucose of 37 M L. low because liver unable to conjugate unconjugated bilirubin XIII. crackles in lungs D M. decreased ability to institute glycogenolysis or gluconeogenesis as needed XIV. development of Cushing’s syndrome F N. bruising & other S&S of easy bleeding XV. hypoosmolality fluid shift into abdominal cavity H O. etiology of asterixis 11. The patient has obvious generalized pitting edema. Etiology for “swollen all over” (I): a. B b. F c. G d. H 12. Understanding the many possible sequelae of cirrhosis, the patient’s RN does a quick bedside glucose fingerstick. The blood glucose is 37 (XII). Which choice links best to this finding? a. L b. I c. K d. M 13. Labs on the patient come back with hardly a normal number. The serum ammonia level is especially high, and the RN knows to expect certain problems related to that. Choose the answer that best links to “decreased ability to break down ammonia high serum ammonia levels” (XI). a. O b. K c. F d. A 14. The serum osmolality is 260 (norm – 280-295). Which answer best links to “hypoosmolality fluid shift into abdominal cavity?” (XV). a. C b. H c. J d. B 15. Other lab results noted to be abnormal are the bilirubin levels. Which answer best goes with “unconjugated bilirubin not being conjugated by cirrhotic liver?” (VIII) a. E b. J c. K d. L 16. Another reason for the patient’s complaint of being “puffy” has to do with this problem: “development of Cushing’s syndrome” (XIV). What’s going on with that? a. B b. N c. I d. F 17. The scenario mentions infected sores (and probably she has other infections, as well). Do you think someone with normal mechanisms of defense would have that many infections? Definitely not…so, what is it about cirrhosis that increases this propensity? Link the correct answer with “etiology of infected sores.” (IX) a. A b. E c. J d. M 18. In assessing this patient, the RN hears “crackles in the lungs.” (XIII) What is the best link to that assessment finding? a. O b. D c. K d. C 19. “Has caused fatigue, and also caused some of SOB” (III)—this statement is partly explained by the issue in question 18. What other factor is involved? a. A b. D c. G d. E 20. The RN taking care of this patient knows to watch for many dangers related to “portal HTN” (VII). Several choices might be linked to this potentially severe cirrhosis-related problem, but out of the following, which choice is best? a. C b. F c. K d. G Note: many of the answers to questions 11-20 have been explained by earlier questions, but also the Cirrhosis Concept Map and your RRD pages 13-16 go into cirrhosis in depth and should help you form rationales. Email me if you need any clarification, though. [Show More]
Last updated: 1 year ago
Preview 1 out of 74 pages
Instant download
.png)
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Also available in bundle (1)

NURS 3366 Quizzes 1,2,4 and 5 BUNDLE
NURS 3366 Quizzes 1,2,4 and 5 BUNDLE/NURS 3366 Quizzes 1,2,4 and 5 BUNDLE
By A+ Solutions 3 years ago
$14.5
5
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jun 16, 2021
Number of pages
74
Written in
Additional information
This document has been written for:
Uploaded
Jun 16, 2021
Downloads
0
Views
84


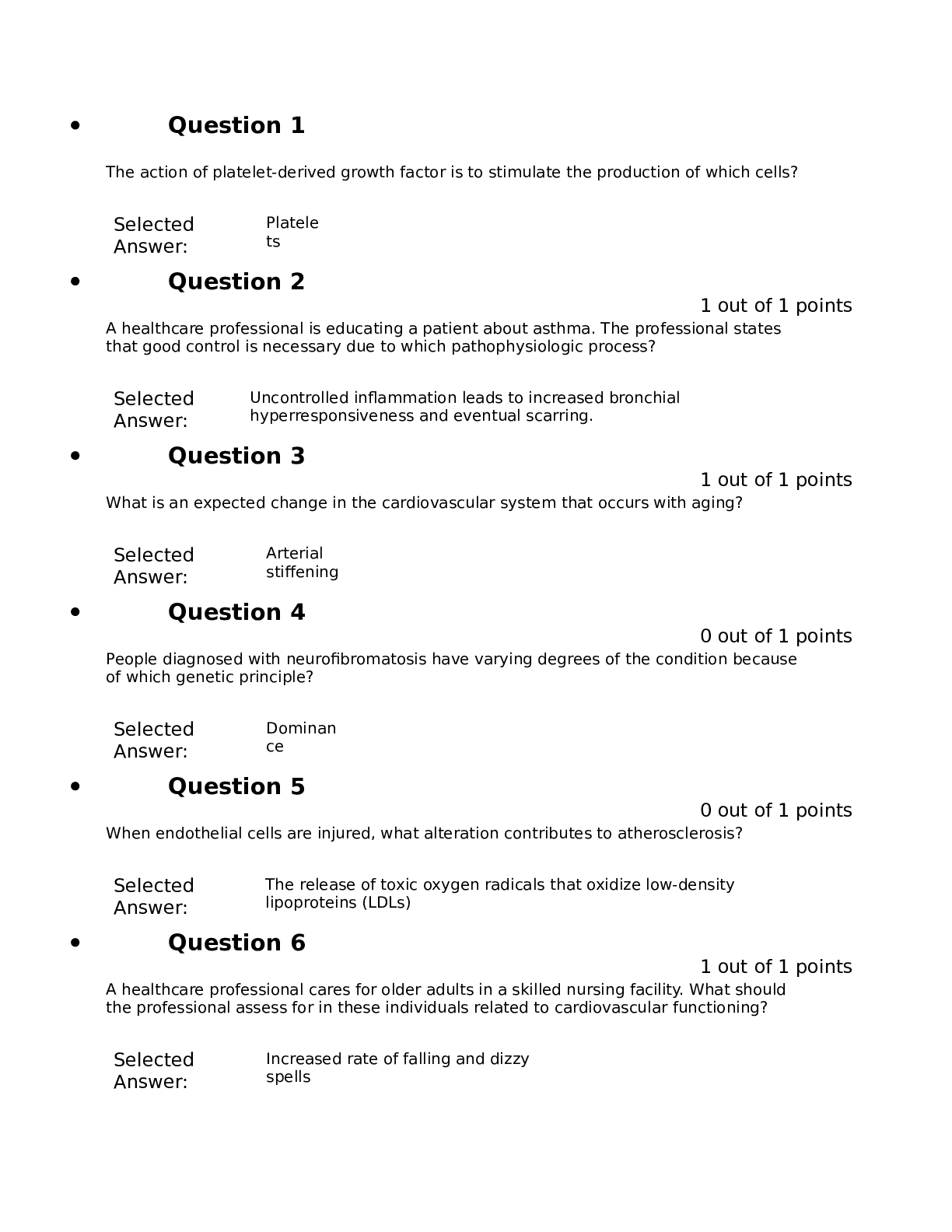
.png)
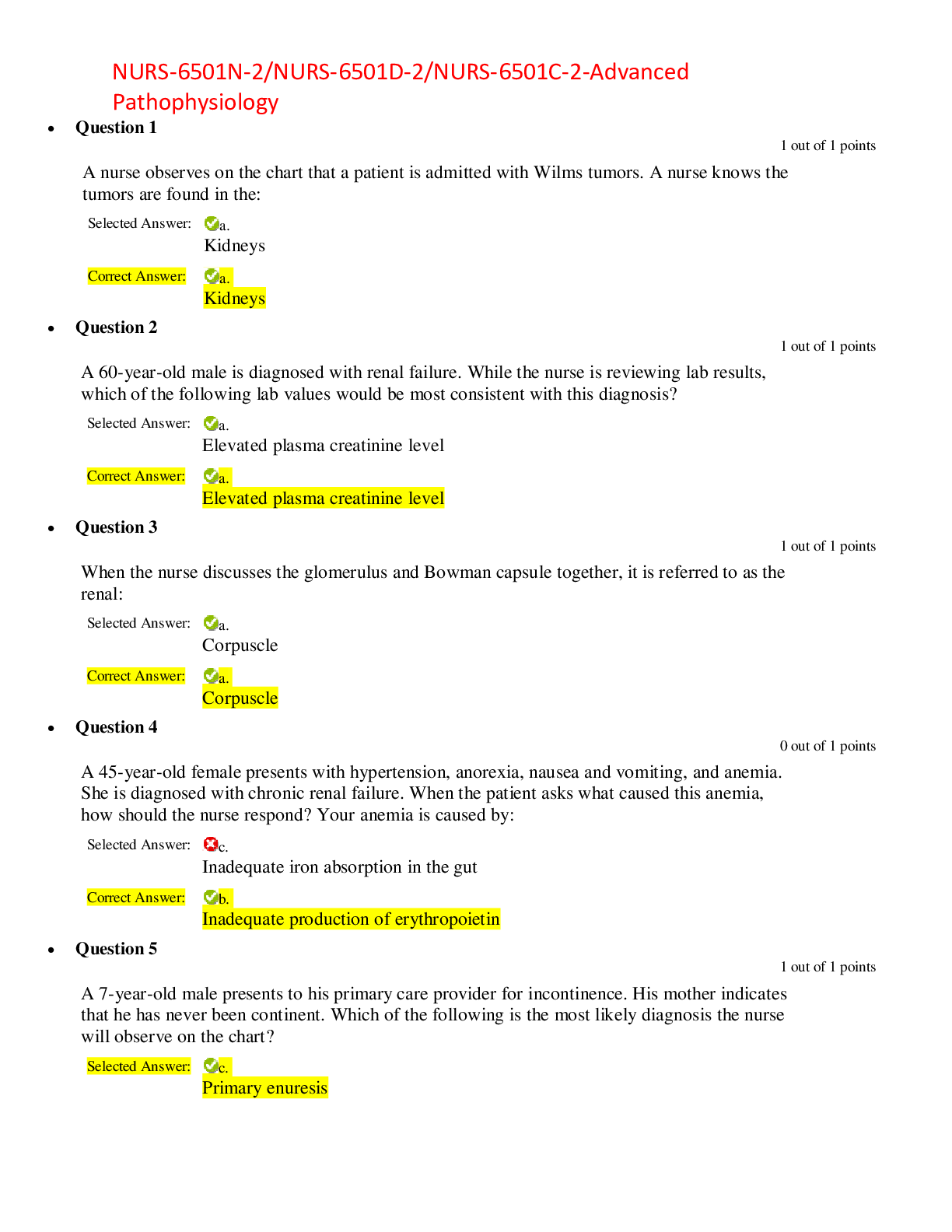
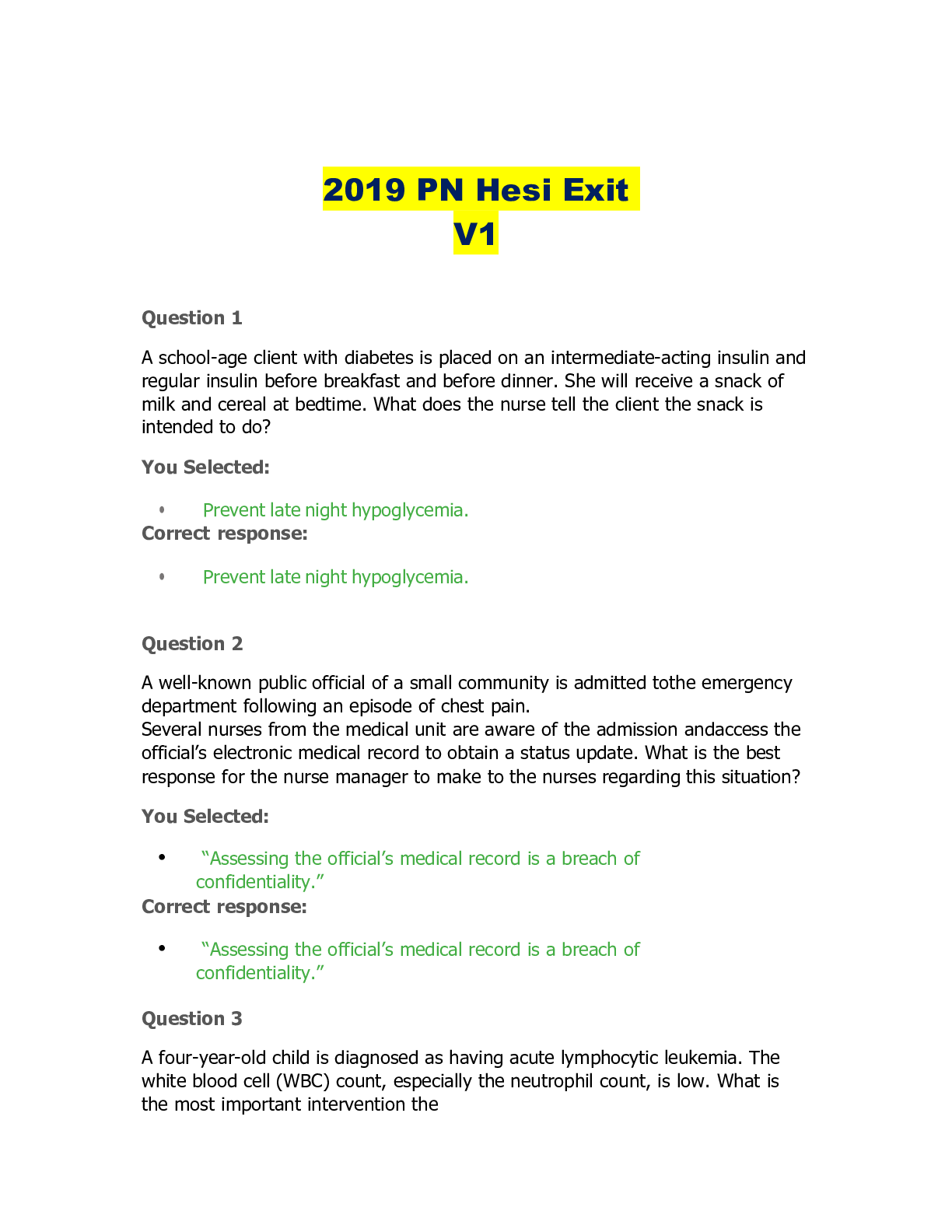

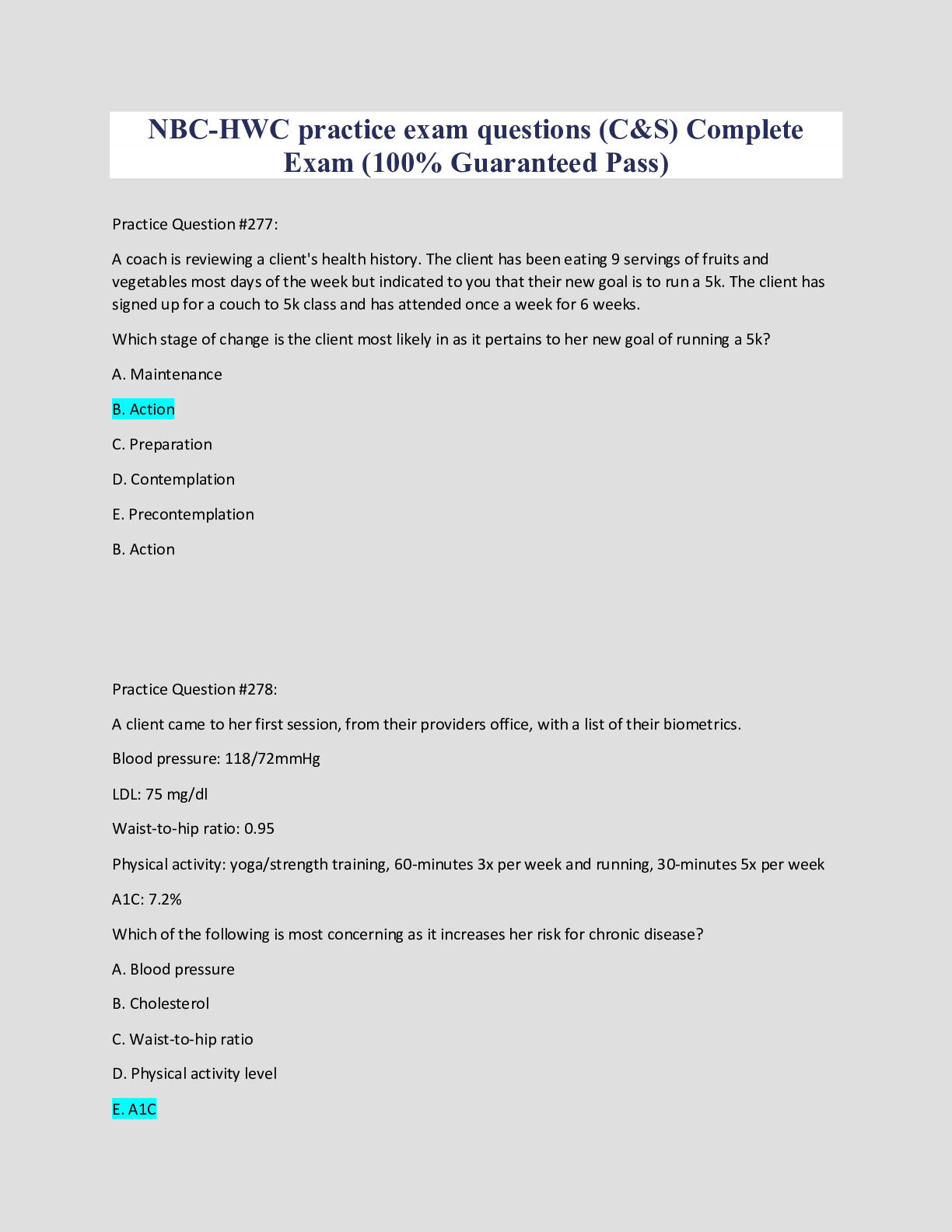
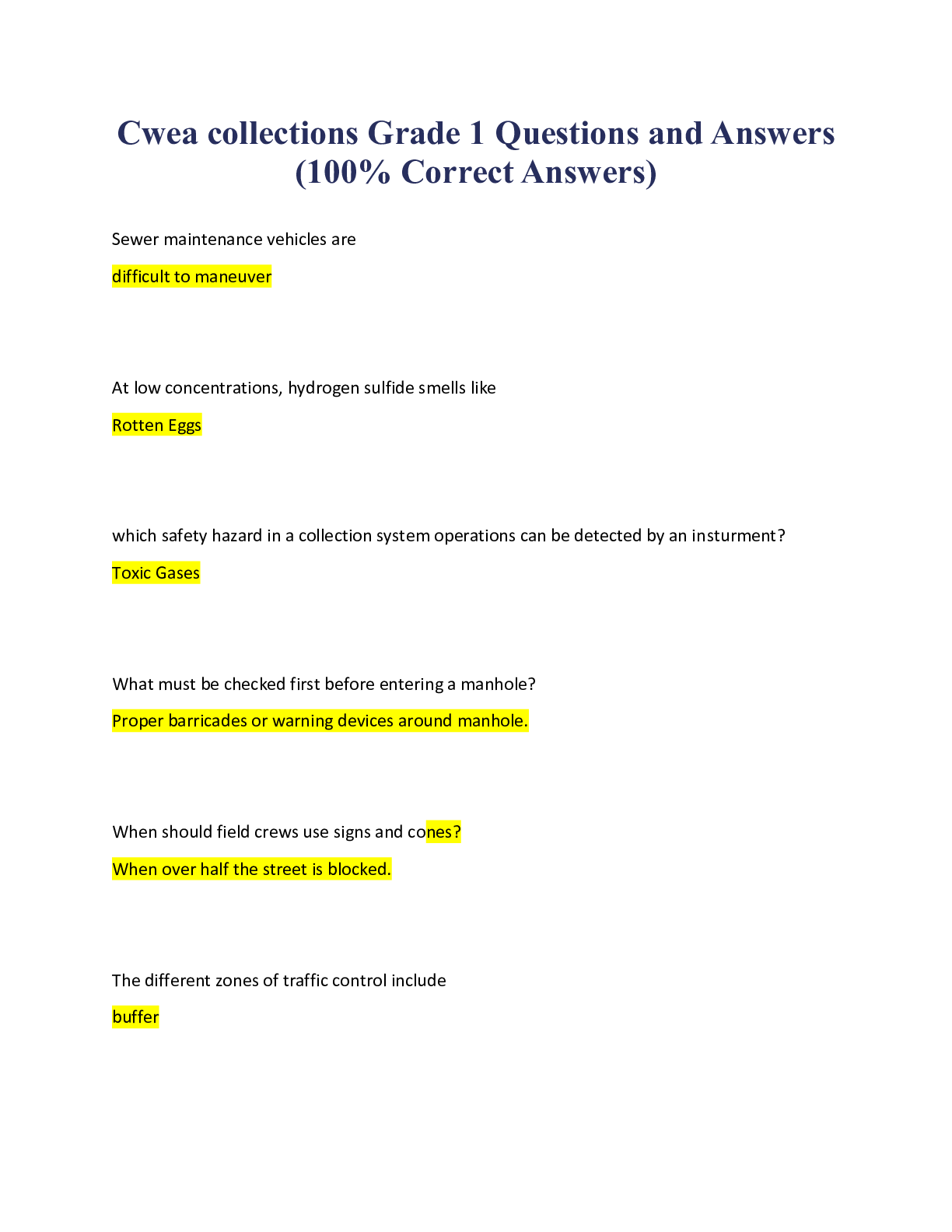
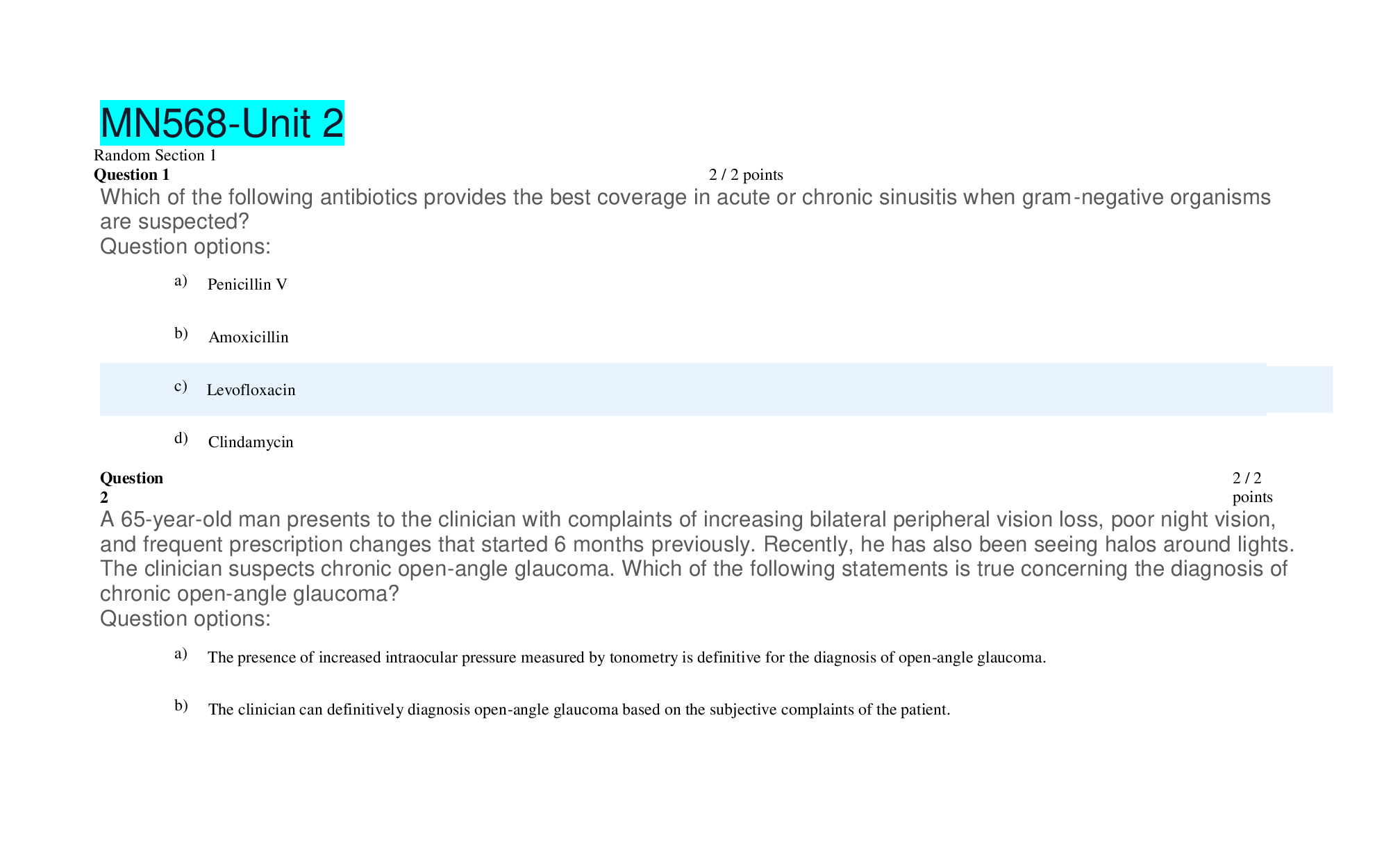
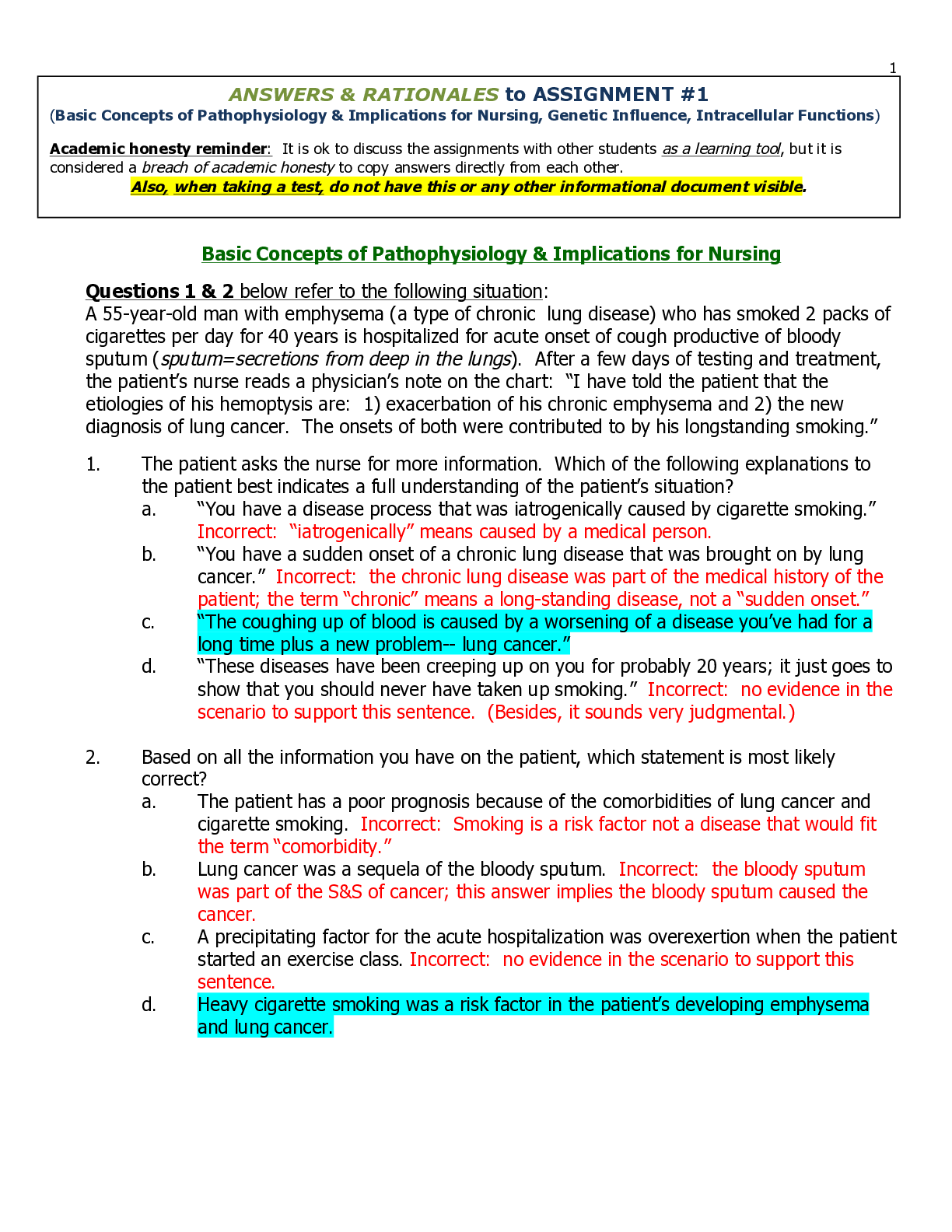
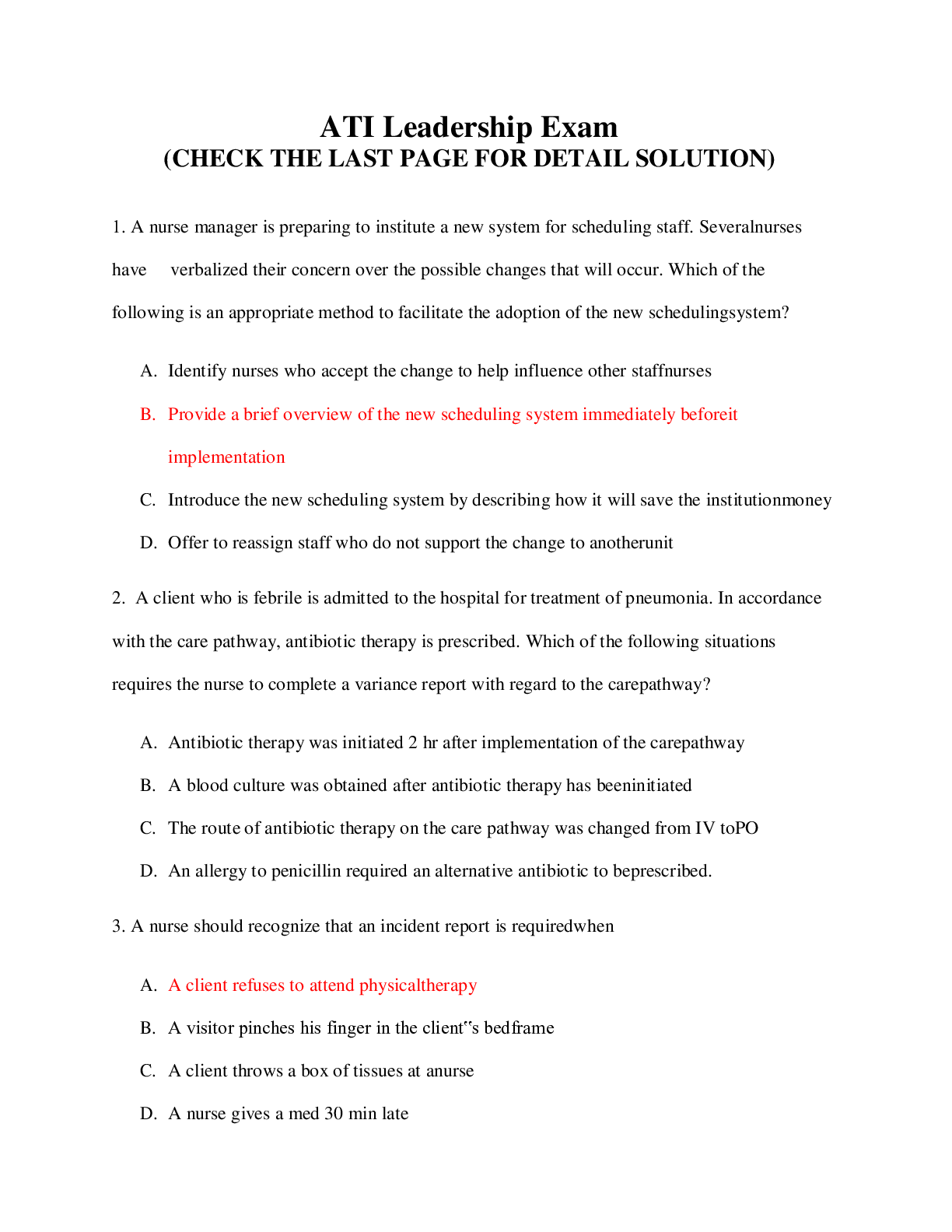
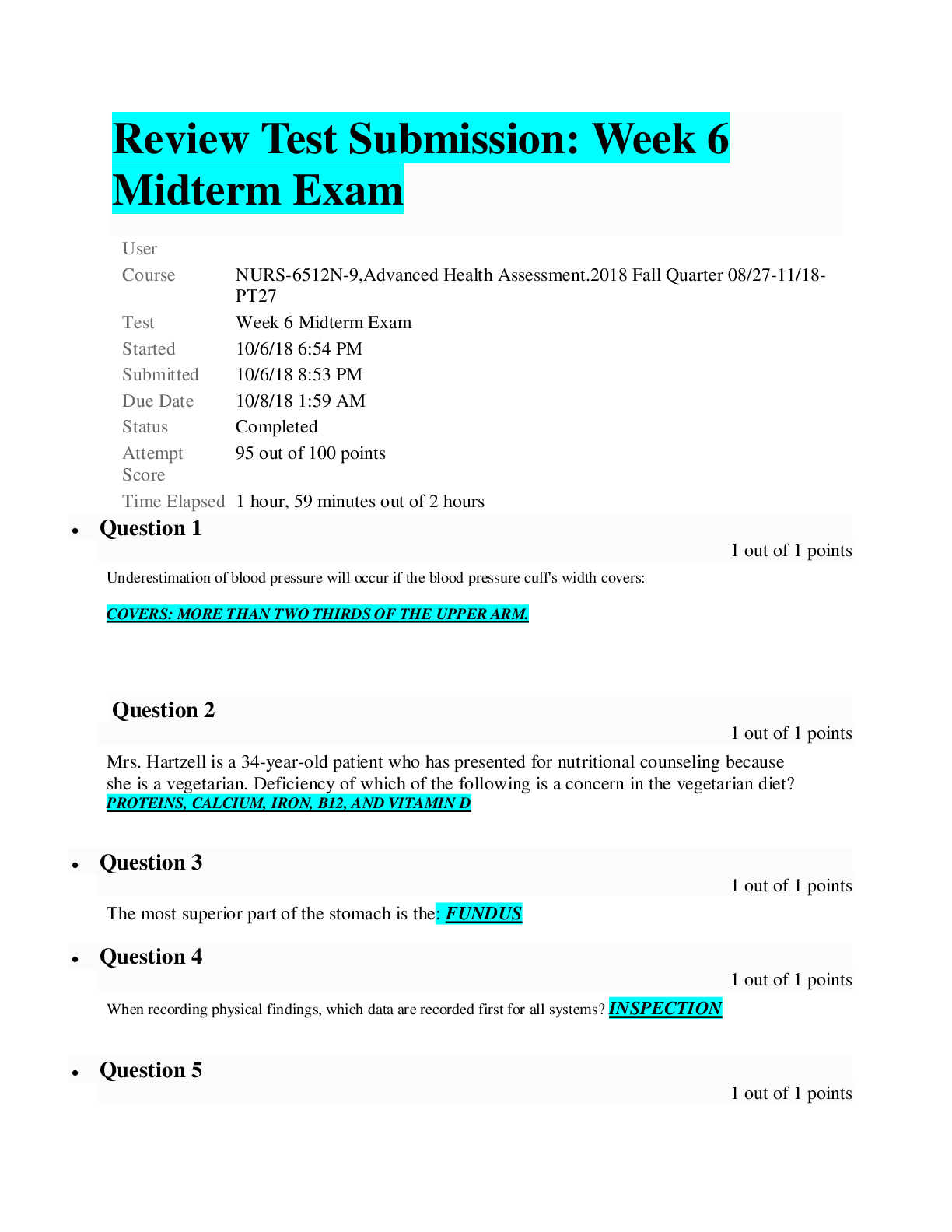
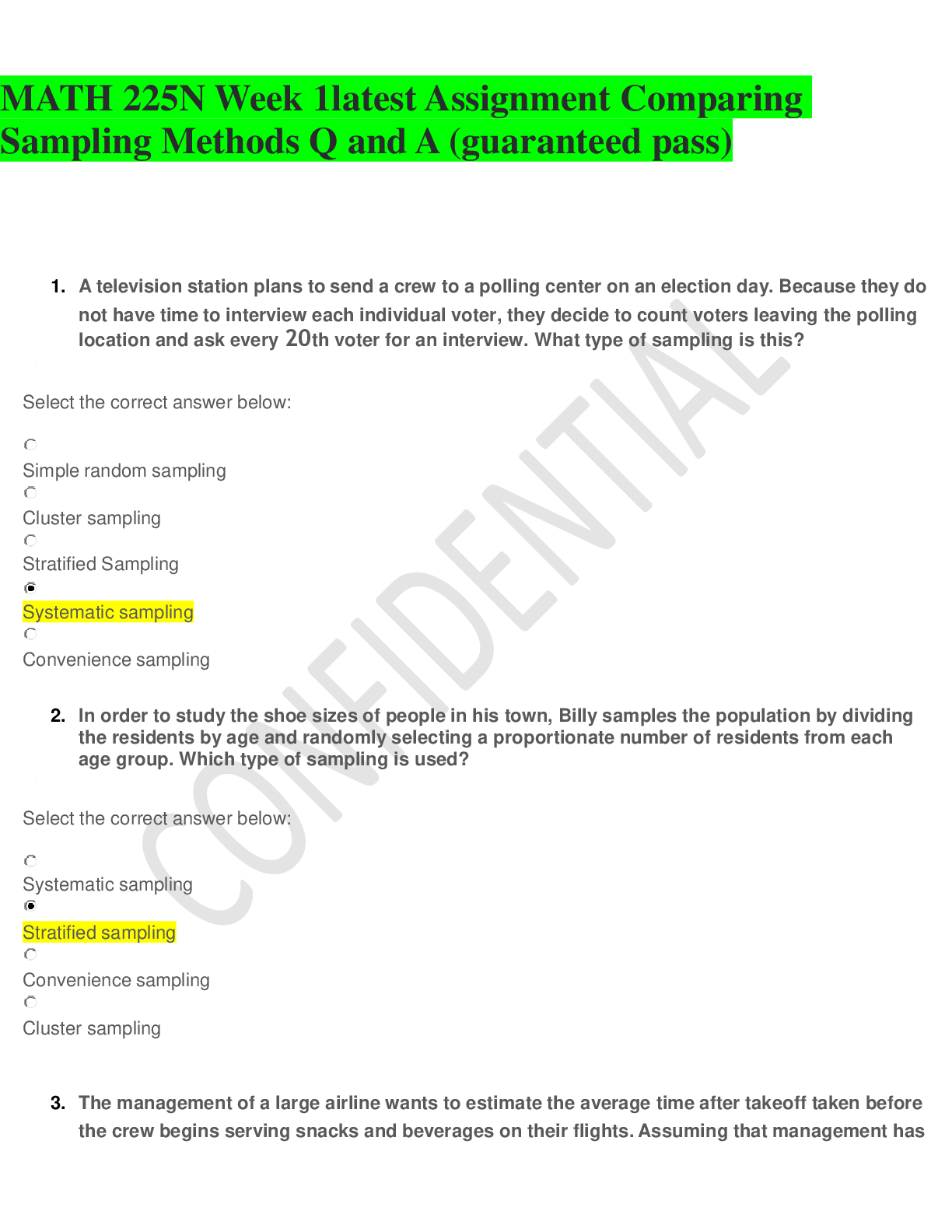
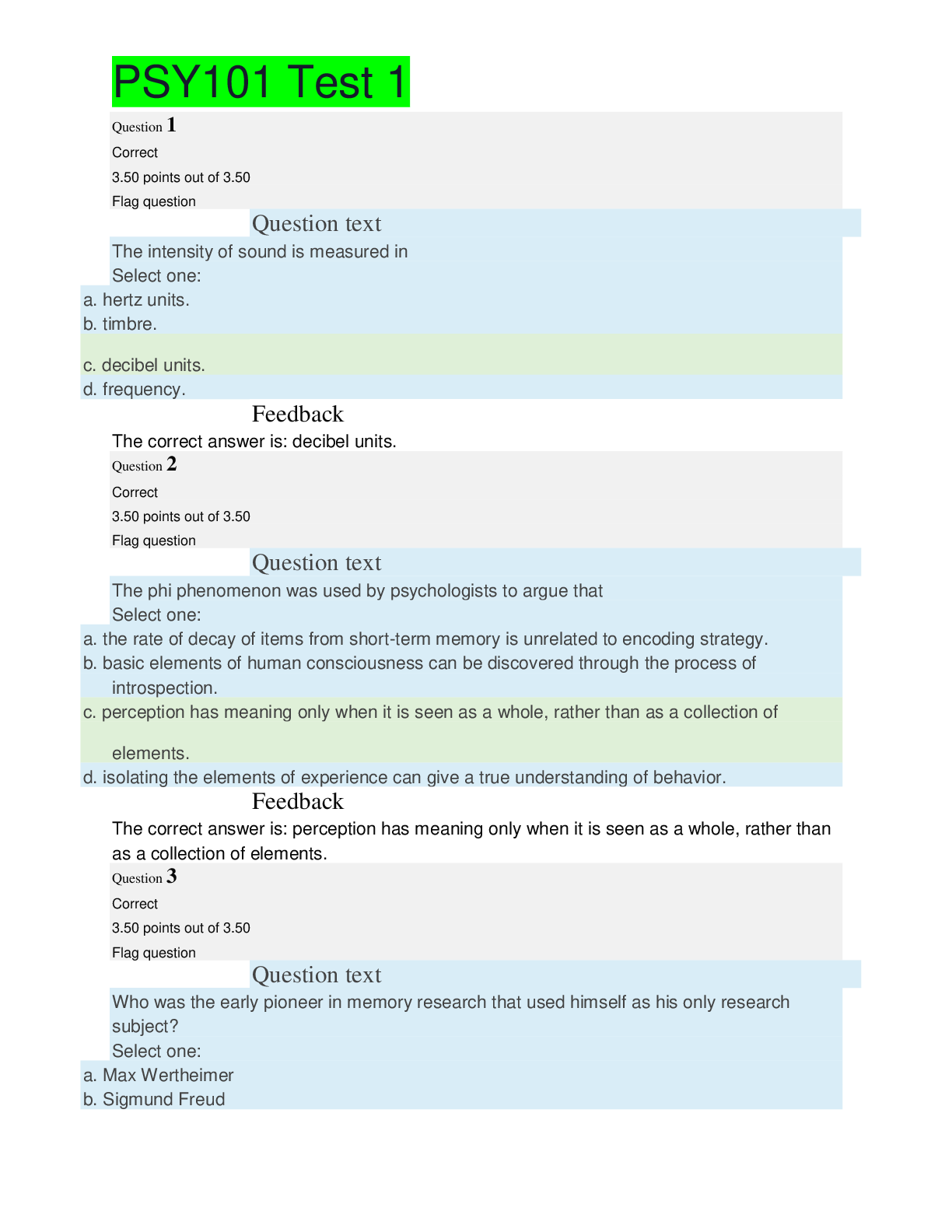

.png)
.png)