*NURSING > EXAM > South University - NSG 64355 Week: Stevens_K: Pediatric SOAP Note: Complete Version. (All)
South University - NSG 64355 Week: Stevens_K: Pediatric SOAP Note: Complete Version.
Document Content and Description Below
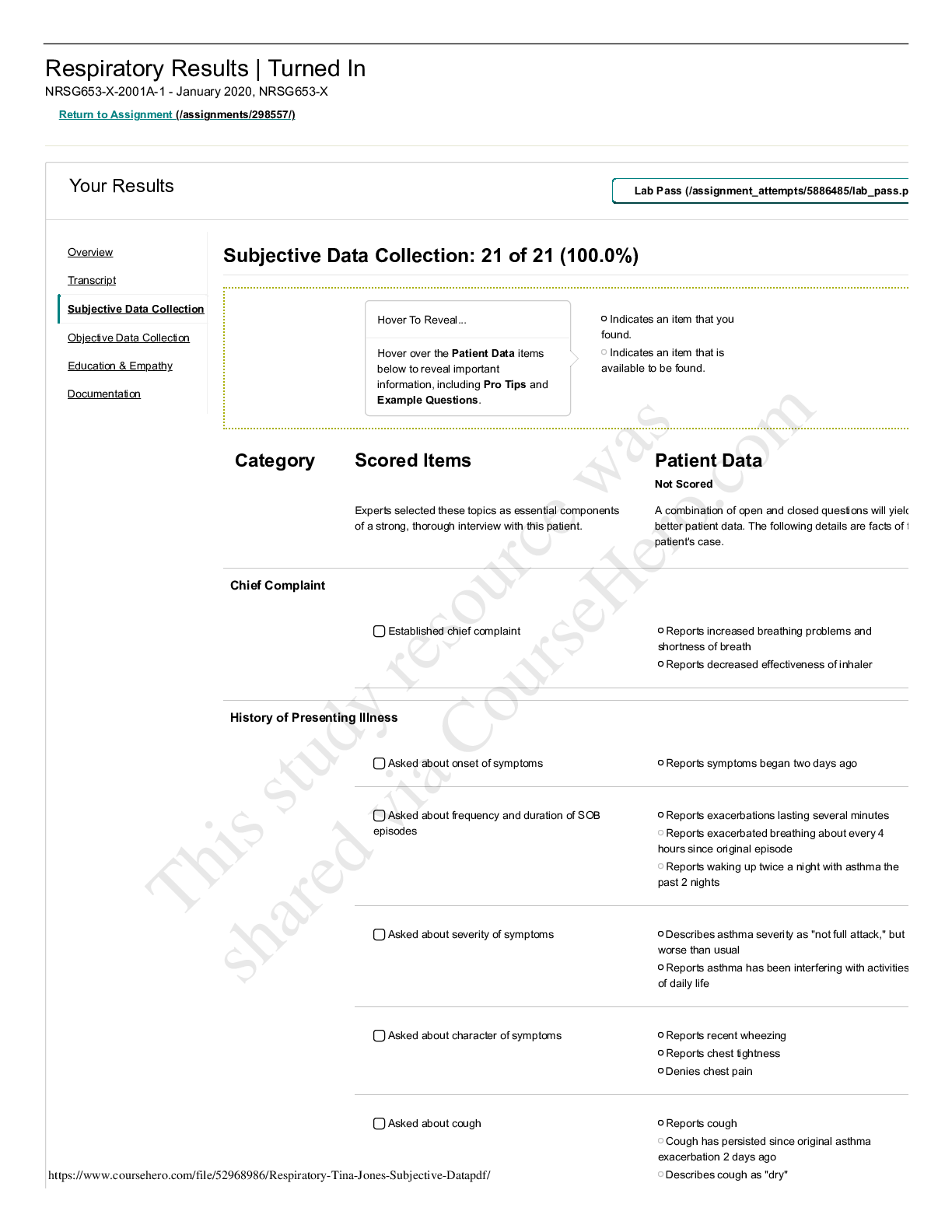
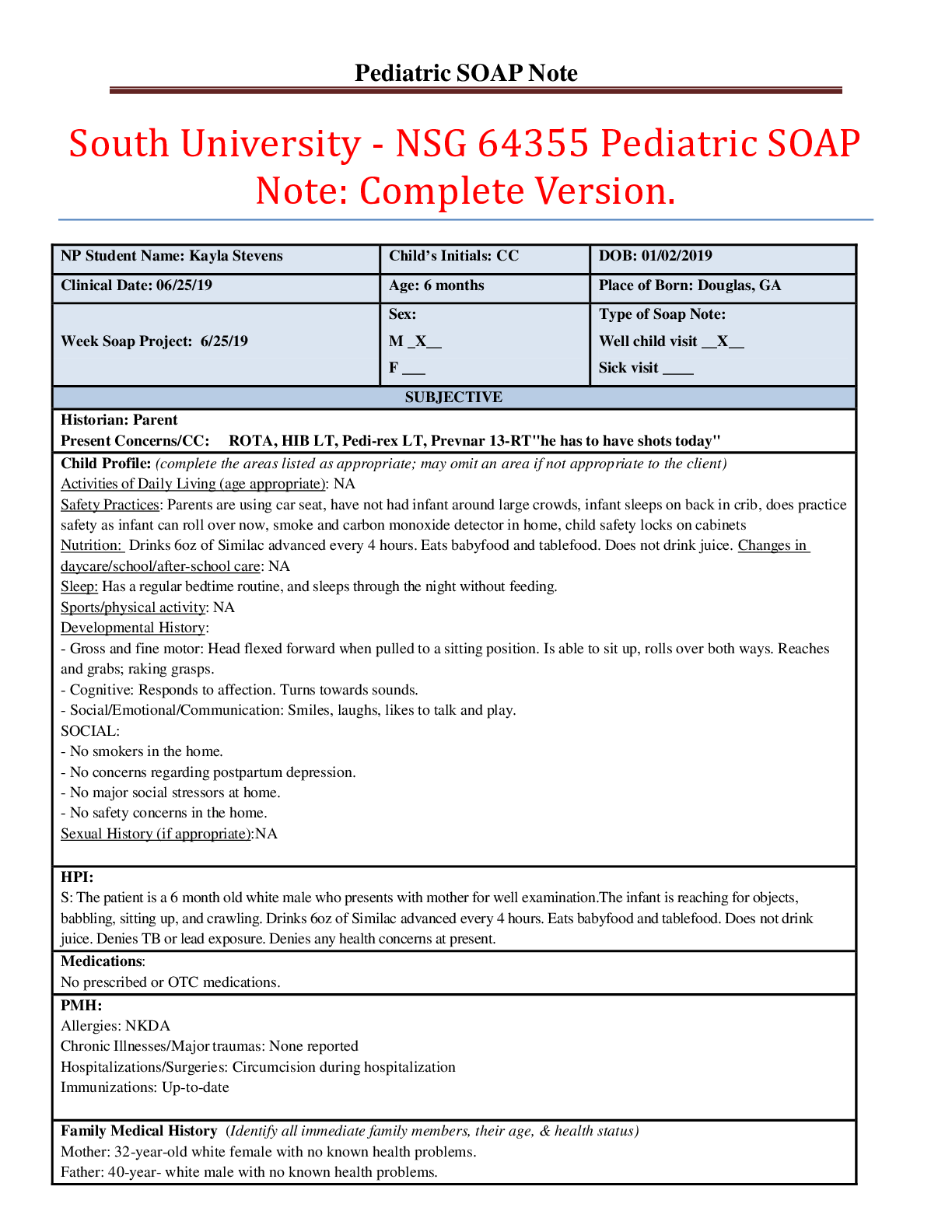
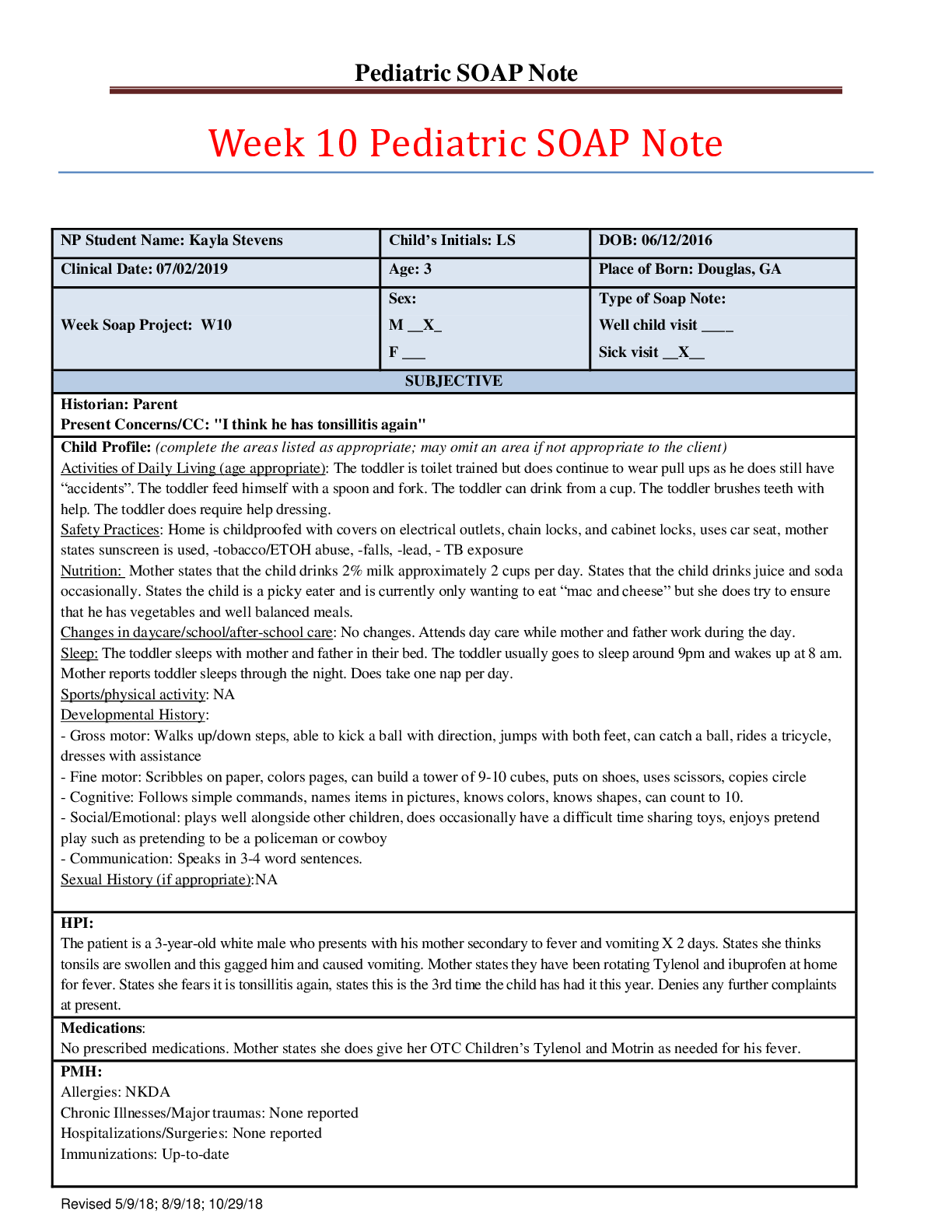
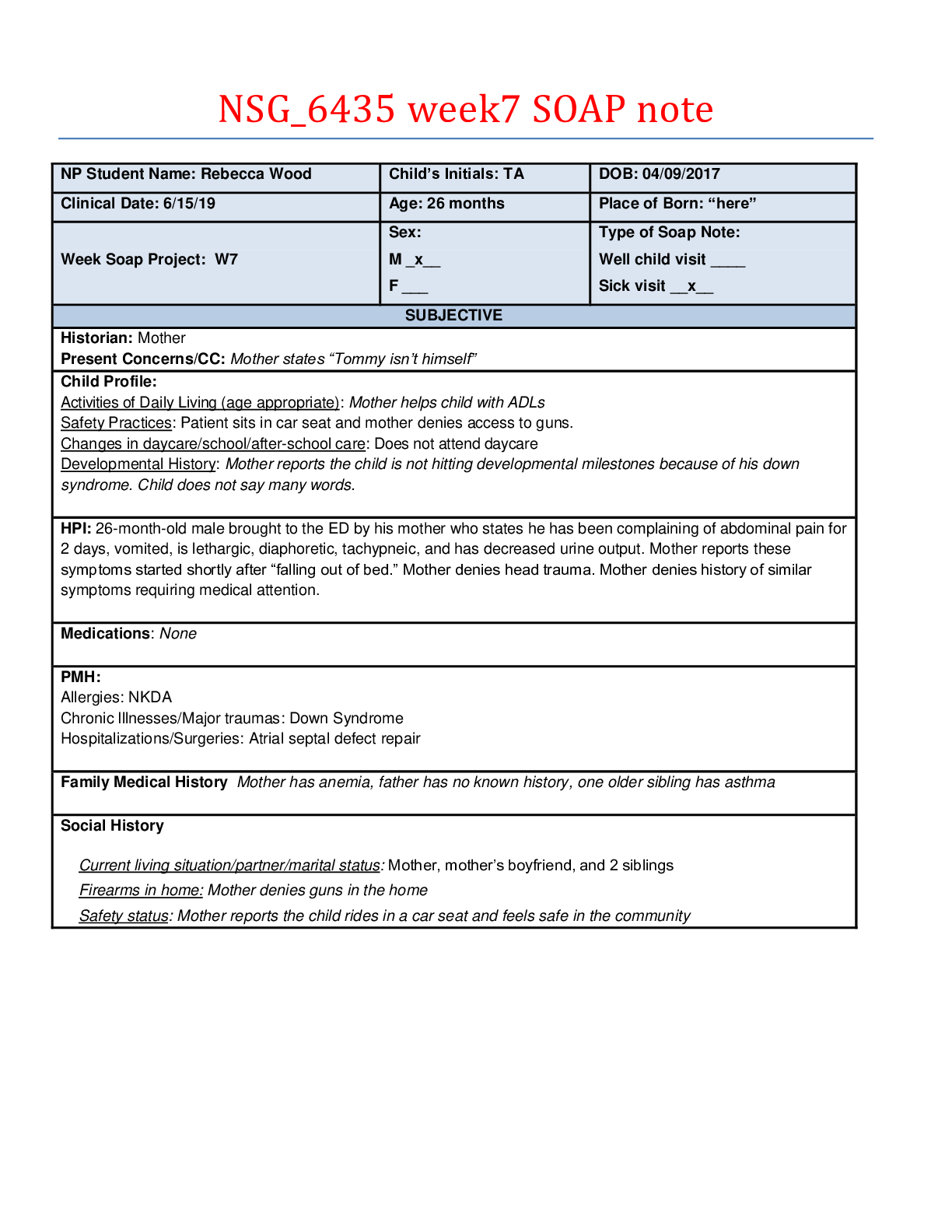
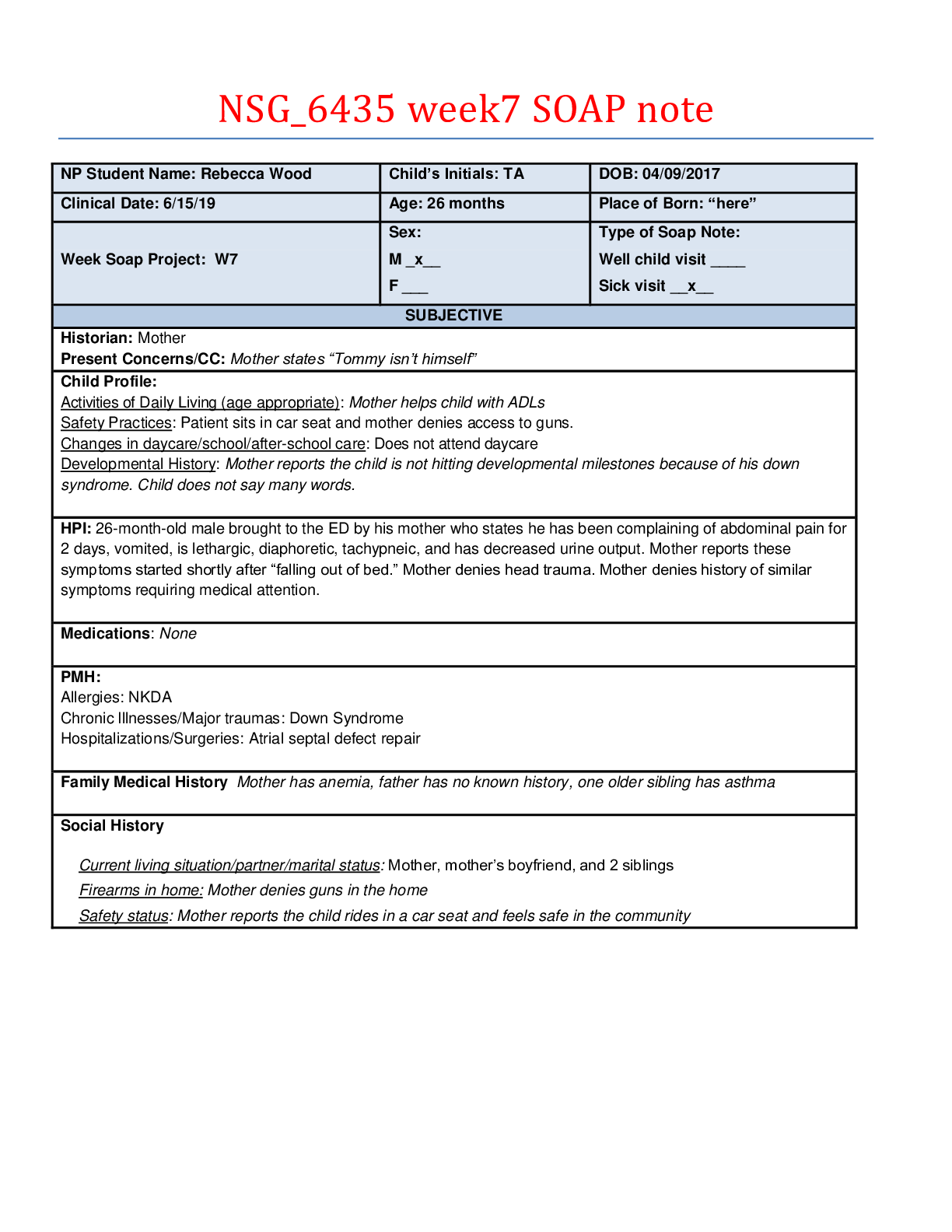
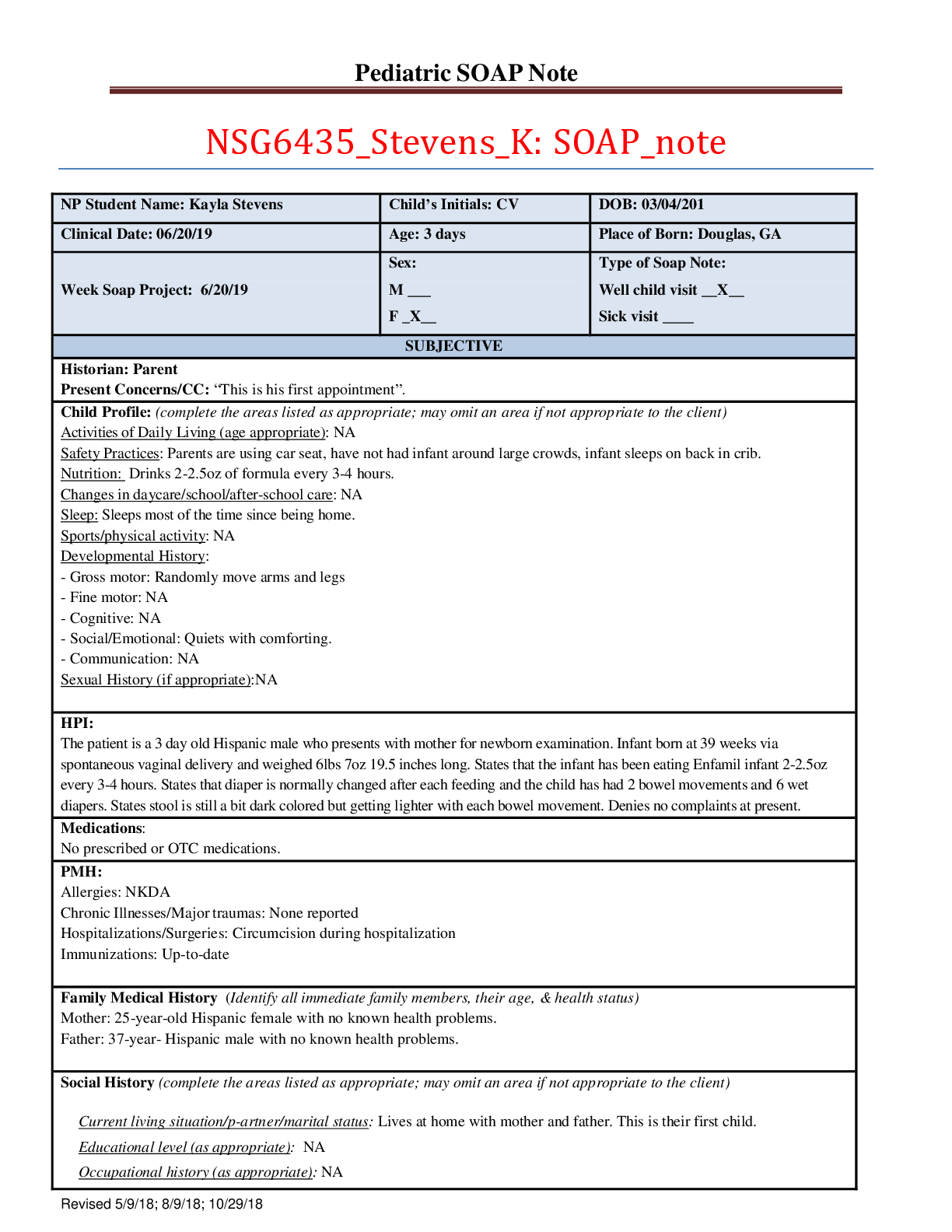
NP Student Name: Kayla Stevens Child’s Initials: CV DOB: 03/04/201 Clinical Date: 06/20/19 Age: 3 days Place of Born: Douglas, GA Week Soap Project: 6/20/19 Sex: M ___ F _X__ Type of Soap Not... e: Well child visit __X__ Sick visit ____ SUBJECTIVE Historian: Parent Present Concerns/CC: “This is his first appointment”. Child Profile: (complete the areas listed as appropriate; may omit an area if not appropriate to the client) Activities of Daily Living (age appropriate): NA Safety Practices: Parents are using car seat, have not had infant around large crowds, infant sleeps on back in crib. Nutrition: Drinks 2-2.5oz of formula every 3-4 hours. Changes in daycare/school/after-school care: NA Sleep: Sleeps most of the time since being home. Sports/physical activity: NA Developmental History: - Gross motor: Randomly move arms and legs - Fine motor: NA - Cognitive: NA - Social/Emotional: Quiets with comforting. - Communication: NA Sexual History (if appropriate):NA HPI: The patient is a 3 day old Hispanic male who presents with mother for newborn examination. Infant born at 39 weeks via spontaneous vaginal delivery and weighed 6lbs 7oz 19.5 inches long. States that the infant has been eating Enfamil infant 2-2.5oz every 3-4 hours. States that diaper is normally changed after each feeding and the child has had 2 bowel movements and 6 wet diapers. States stool is still a bit dark colored but getting lighter with each bowel movement. Denies no complaints at present. Medications: No prescribed or OTC medications. PMH: Allergies: NKDA Chronic Illnesses/Major traumas: None reported Hospitalizations/Surgeries: Circumcision during hospitalization Immunizations: Up-to-date Family Medical History (Identify all immediate family members, their age, & health status) Mother: 25-year-old Hispanic female with no known health problems. Father: 37-year- Hispanic male with no known health problems. Social History (complete the areas listed as appropriate; may omit an area if not appropriate to the client) Current living situation/p-artner/marital status: Lives at home with mother and father. This is their first child. Educational level (as appropriate): NA Occupational history (as appropriate): NA Substance use/abuse (ETOH, tobacco, and marijuana): NA Firearms in home: No guns in home. Safety status: Parents are using car seat, have not had infant around large crowds, infant sleeps on back in crib. [Show More]
Last updated: 1 year ago
Preview 1 out of 6 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
We Accept:

Reviews( 0 )
$9.00
Document information
Connected school, study & course
About the document
Uploaded On
Aug 04, 2020
Number of pages
6
Written in
Additional information
This document has been written for:
Uploaded
Aug 04, 2020
Downloads
0
Views
41