*NURSING > STUDY GUIDE > NURS MATERNITY EXAM 3 OB STUDY GUIDE FINAL | Download To Score A (All)
NURS MATERNITY EXAM 3 OB STUDY GUIDE FINAL | Download To Score A
Document Content and Description Below
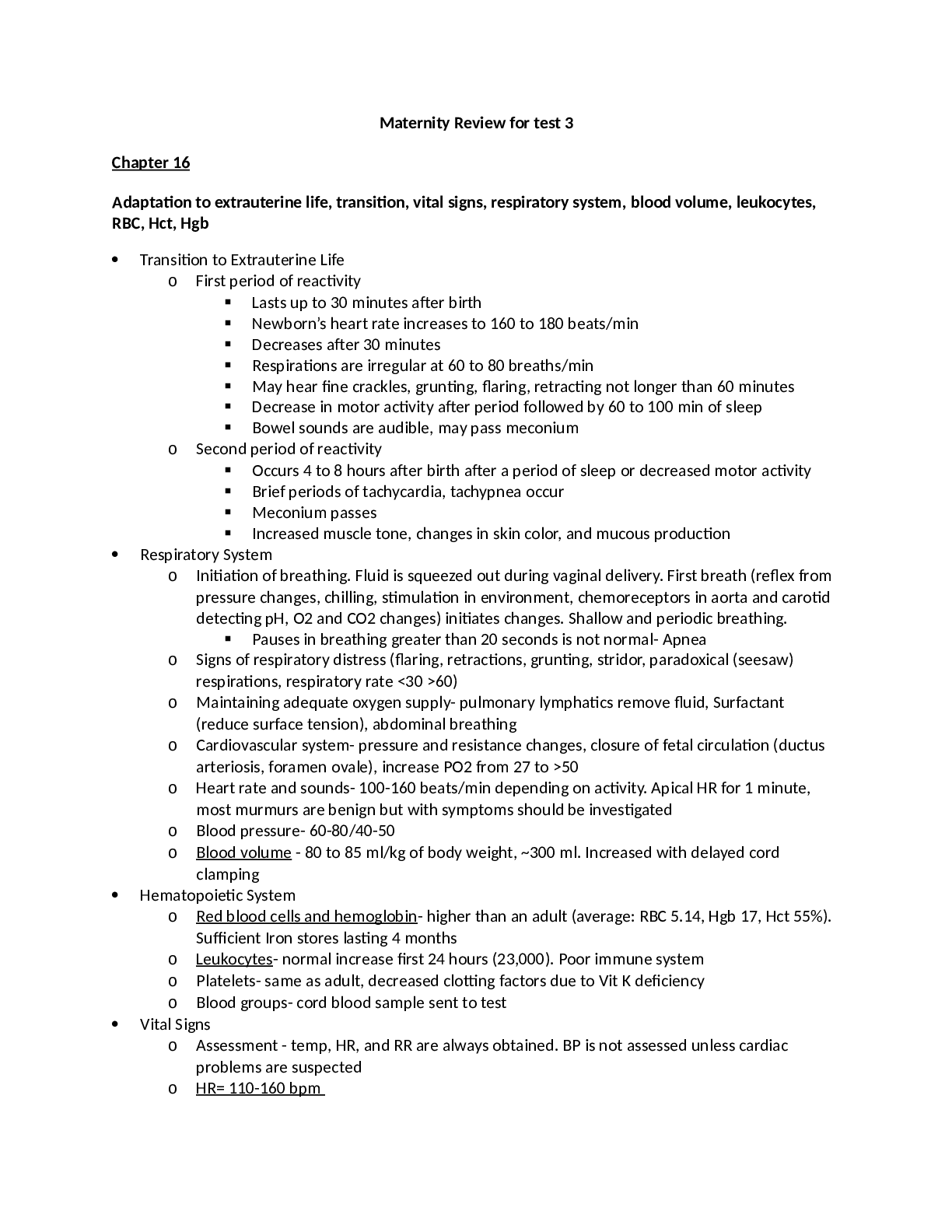
Maternity Review for test 3 Chapter 16 Adaptation to extrauterine life, transition, vital signs, respiratory system, blood volume, leukocytes, RBC, Hct, Hgb • Transition to Extrauterine Life ... o First period of reactivity ▪ Lasts up to 30 minutes after birth ▪ Newborn’s heart rate increases to 160 to 180 beats/min ▪ Decreases after 30 minutes ▪ Respirations are irregular at 60 to 80 breaths/min ▪ May hear fine crackles, grunting, flaring, retracting not longer than 60 minutes ▪ Decrease in motor activity after period followed by 60 to 100 min of sleep ▪ Bowel sounds are audible, may pass meconium o Second period of reactivity ▪ Occurs 4 to 8 hours after birth after a period of sleep or decreased motor activity ▪ Brief periods of tachycardia, tachypnea occur ▪ Meconium passes ▪ Increased muscle tone, changes in skin color, and mucous production • Respiratory System o Initiation of breathing. Fluid is squeezed out during vaginal delivery. First breath (reflex from pressure changes, chilling, stimulation in environment, chemoreceptors in aorta and carotid detecting pH, O2 and CO2 changes) initiates changes. Shallow and periodic breathing. ▪ Pauses in breathing greater than 20 seconds is not normal- Apnea o Signs of respiratory distress (flaring, retractions, grunting, stridor, paradoxical (seesaw) respirations, respiratory rate <30 >60) o Maintaining adequate oxygen supply- pulmonary lymphatics remove fluid, Surfactant (reduce surface tension), abdominal breathing o Cardiovascular system- pressure and resistance changes, closure of fetal circulation (ductus arteriosis, foramen ovale), increase PO2 from 27 to >50 o Heart rate and sounds- 100-160 beats/min depending on activity. Apical HR for 1 minute, most murmurs are benign but with symptoms should be investigated o Blood pressure- 60-80/40-50 o Blood volume - 80 to 85 ml/kg of body weight, ~300 ml. Increased with delayed cord clamping • Hematopoietic System o Red blood cells and hemoglobin- higher than an adult (average: RBC 5.14, Hgb 17, Hct 55%). Sufficient Iron stores lasting 4 months o Leukocytes- normal increase first 24 hours (23,000). Poor immune system o Platelets- same as adult, decreased clotting factors due to Vit K deficiency o Blood groups- cord blood sample sent to test • Vital Signs o Assessment - temp, HR, and RR are always obtained. BP is not assessed unless cardiac problems are suspected o HR= 110-160 bpm ▪ Apical HR for 1 minute, most murmurs are benign but with symptoms should be investigated o RR= 30-60 ▪ Count for a full minute while at rest; RR varies with the state of alertness and activity after birth; Abdominal Breathing o Temp= 97.5-99.5°F (98.6) ▪ Axillary= Method of Choice; temporal, oral and intra-auricular thermometers are not effective/considered accurate in measuring newborn temp o BP= 60-80(Systolic)/40-50(Diastolic) mmHg o Pulses ▪ APICAL Pulse for full minute; Femoral & brachial pulses for equality and strength • Renal System o Fluid and electrolyte balance- urinate 15 to 60 ml of urine/kg/day (Term). Limited capacity to concentrate urine. • Hepatic system o Iron storage- site of production of Hgb. o Carbohydrate metabolism- rapid depletion of glycogen stores. o Jaundice- conjugation of bilirubin. Jaundice within 24 hours of life is pathological o Coagulation- activated by Vit K. , given Vit K until intestinal bacteria can make it. • Immune system o Immune cells are not active for weeks to months after birth. Passive immunity, IgA in breast milk. IgG at 40% of adult by 12 months. • Reproductive system o Female- all potential ova are present. Increased vaginal discharge from mom’s increased estrogen, can be blood tinged (Pseudomenses) o Male- testes should be descended in term. Hydrocele- fluid around testes may be present o Swelling of breast tissue- due to increased estrogen, may have thin discharge which subsides as hormones decrease. • Neuromuscular system o Limited neuromuscular control, spontaneous motor activity such as transient tremors Thermogenesis, regulation, heat loss, cold stress • Thermogenesis - unable to shiver, uses brown fat to generate heat until depleted. Less in preterm. • Heat loss: Convection (drafts), Radiation (being near cold surface), Conduction (touching cold surface), Evaporation (water loss) • Temperature regulation - neutral thermal environment - heat loss minimal and O2 consumption low. Cold stress increases O2 consumption, respiratory distress, hypoglycemia. Radiant warmers and Skin to Skin. Rapid warming can cause apnea. Unable to sweat, risk for hyperthermia Stool and the newborn • Meconium - Infant's first stool is composed of amniotic fluid and its constituents, intestinal secretions, shed mucosal cells. Change to transitional. • GI System adaptation o Digestion- capable of swallowing, digesting, metabolizing, and absorbing proteins and simple carbs and emulsifying fats. Epstein pearls- white patches on palate, gums. Sucking pads in cheeks. newborns coordinate the breathing, sucking, and swallowing reflexes. Integumentary system, mongolian spots, erythema toxicum • Sweat glands- present but do not respond to increased temperature • Vernix caseosa- cheese like substance protective covering • Desquamation- peeling, more in post mature infant • Mongolian spots- blue/black mark in dark skinned, fade over time • Nevi- stork bites, pink, easy blanched. Fade by age 2 • Erythema toxicum- Newborn rash in first 3 weeks, inflammatory response. Not treatment needed. Caput, cephalohematoma, subgaleal • Caput succedaneum - swelling under scalp, crosses suture line, found on the occiput, caused by sustained pressure on the presenting vertex against cervix, present at birth, disappears spontaneously within 3-4 days. Infants born with the assistance of vacuum extraction usually have caput in the area where the cup was applied • Cephalohematoma - blood collection between skull and periosteum. Does NOT cross suture line. Bleeding may occur with spontaneous birth from pressure against the maternal bony pelvis; appears several hours or the day after birth and may not become apparent until a caput succedaneum is absorbed. Usually largest on 2-3rd day, when the bleeding stops. fullness of a cephalohematoma spontaneously resolves in 3 to 6 weeks; not aspirated because risk of infection; as it resolves, hemolysis of RBCs occurs, and jaundice may result • Subgaleal hematoma - bleeding in subgaleal compartment, potential for hypovolemic shock and anemia; Injury occurs as result of forces that compress and then drag the head through the pelvic outlet; The bleeding extends beyond bone, often posteriorly into the neck, and continues after birth; Early detection is important - head circumference measurements/ inspection of back of neck for ↑ edema/ firm mass/ change LOC, decrease in hematocrit, increased serum bilirubin; Early Signs include: boggy scalp, pallor, tachycardia, increasing head circumference, and forward/lateral positioning of ears; Replacement of blood loss and clotting factors required for acute cases Hip dysplasia • Skeletal system o At birth more cartilage then ossified bone o Hips are checked for dysplasia, Ortolani’s maneuver to check. o Appear bow legged Reflexes in the newborn • Sucking, rooting, swallowing, grasp, tonic neck, Moro, stepping, crawling, Babinski, trunk incurvation, sneezing, blinking Chapter 17 Apgar, airway maintenance, bulb syringe use • Initial assessment and Apgar scoring ➢ Rapid assessment of transition: Heart rate, respirations, muscle tone, reflex irritability, color ➢ Scoring: 0 to 3 =severe distress, 4 to 6= moderate difficulty, 7 to 10 = the infant is having minimal or no difficulty adjusting to extrauterine life. SIGN 0 SCORE 1 2 Heart rate Absent Slow (<100) >100 Respiratory rate Absent Slow, weak cry Good cry Muscle tone Flaccid Some flexion of extremities Well flexed Reflex irritability No response Grimace Cry Color Blue, pale Body pink, extremities blue Completely pink • Airway maintenance & Bulb Syringe ➢ the healthy term infant born vaginally has little difficulty clearing the airway. Most secretions are moved by gravity and brought by the cough reflex to the oropharynx to be drained or swallowed. The infant is often maintained in a side-lying position (head stabilized) with a rolled blanket at the back to facilitate drainage. ➢ If the infant has excess mucus in the respiratory tract, the mouth and nasal passages can be gently suctioned with a bulb syringe. Routine chest percussion and suctioning of healthy term or late preterm infants is avoided. The infant who is choking on secretions should be supported with the head to the side. The mouth is suctioned first to prevent the infant from inhaling pharyngeal secretions by gasping as the nares are touched. The bulb is compressed and inserted into one side of the mouth. The center of the mouth is avoided because the gag reflex could be stimulated. The nasal passages are suctioned one nostril at a time. ➢ Fine crackles may be auscultated for several hours after birth. If the bulb syringe does not clear mucus interfering with respiratory effort, mechanical suction can be used. • Bulb syringe use ➢ Bulb syringe must be compressed before insertion ** ➢ The bulb syringe should always be kept in the infant's crib. ➢ If the newborn has an obstruction that is not cleared with suctioning, further investigation must occur to determine if a mechanical defect is causing the obstruction. ➢ Deeper suctioning may be needed to remove mucus from the newborn's nasopharynx or posterior oropharynx. However, this type of suctioning should be performed only after an assessment of the risks involved. Proper tube insertion and suctioning for 5 seconds or less per tube insertion helps prevent vagal stimulation and hypoxia. If wall suction is used, the pressure should be adjusted to less than 80 mm Hg. After the catheter is properly placed, suction is created by intermittently placing one's thumb over the control as the catheter is carefully rotated and gently withdrawn. This procedure may need to be repeated until the infant has a clear airway Eye prophylaxis, vitamin K, IM injections • Eye prophylaxis- against ophthalmia neonatorum, which is an inflammation of the eyes resulting from gonorrheal or chlamydial infection contracted by the newborn during passage through the mother's birth canal. ➢ Administer 1-2 hours after birth if possible ➢ erythromycin, tetracycline, or silver nitrate • Intramuscular injection- Vit K, Hep B, HBIG, vastus lateralis, 0.5ml (max 1 ml) • Vit K ➢ A single intramuscular injection of 0.5 to 1 mg of vitamin K is given soon after birth to prevent hemorrhagic disease of the newborn. Vitamin K is produced in the gastrointestinal tract by bacteria starting soon after microorganisms are introduced. By day 8, healthy newborns are able to produce their own vitamin K ➢ Newborns➔ DO NOT have the normal intestinal flora to synthesize Vitamin K until 1 week after birth. ➢ Vitamin K is needed to activate the synthesis in the liver of coagulation factors. ➢ Vitamin K is never administered by the intravenous route for the prevention of hemorrhagic disease Jaundice, phototherapy • Conjugation of bilirubin- released with breakdown of RBC and myoglobin (unconjugated), conjugated in the liver to a soluble form excreted in bile, then into feces and urine • However, the unbound bilirubin can leave the vascular system and permeate other extravascular tissues (e.g., skin, sclera, oral mucous membranes)➔ The resulting yellow coloring➔JAUNDICE • Newborns have a higher rate of bilirubin production than an adult • Considerable reabsorption of bilirubin occurs in the neonatal small intestine • In term infants➔jaundice first appears after 24 hours and disappears by the end of the seventh day • In preterm infants➔ jaundice is first evident after 48 hours and disappears by the ninth or tenth day. • The infant's predischarge total serum bilirubin falls below the high risk category (<95th percentile) on the hour-specific nomogram • Direct bilirubin does not exceed 1 to 1.5 mg/dl. Indirect or unconjugated bilirubin concentration does not increase by more than 5 mg/dl per day. The serum concentration of unconjugated bilirubin usually does not exceed 12 mg/dl in term infants and 15 mg/dl in preterm infants. • Kernicterus- stains the brain • Jaundice associated with breastfeeding- early onset (less fluid and calories causing decreased hepatic clearance) Late onset (due to a factor in milk delaying conjugation or decreased excretion) • Phototherapy Therapy for hyperbilirubinemia • Jaundice within 24 hours of life is pathological**=BAD Chapter 18 Benefits of breastfeeding • Human milk designed specifically for human infants; nutritionally superior to any alternative • Contains growth factors that promote development of the brain and GI system • Bacteriologically safe and always fresh • Nutrients in breast milk more easily absorbed than those in formula Fluid and calorie requirements, vitamin needs for newborn • Fluids- day 0-2 (60-80 ml/kg), 3-7 (100-150 ml/kg), 8-30 (120-180 ml/kg) • Energy- 110 calories/kg/day (breast milk/ formula is 20 calories/ounce • Carbohydrate- 60g/day • Fat- 31g/day • Protein- 9.1 g/day • Vitamins ➢ Vitamin D- fortified formula, need supplement for breastfed ➢ Vitamin K- given at birth, produce from normal intestinal flora about 8 days • Minerals- better absorbed from breastmilk Lactogenesis, assess proper latch, weight loss of newborn, Storage of breastmilk • Prolactin levels are highest during first 10 days after birth ➢ Gradually decline but remain above baseline levels for duration of lactation • Prolactin is produced in response to infant suckling and emptying of breasts ➢ Lactating breasts never completely empty ➢ Milk is constantly produced as infant feeds ➢ Supply meets demand system • Oxytocin: other hormone essential to lactation • As nipple is stimulated by suckling infant, posterior pituitary, prompted by hypothalamus, produces oxytocin ➢ Responsible for milk-ejection reflex or let-down reflex • Nipple-erection reflex is integral to lactation • Lactogenesis stage I ➢ Beginning at 16 to 18 weeks of pregnancy ➢ Colostrum: a clear, yellowish fluid o More concentrated than mature milk o Extremely rich in immune globulins o Higher concentration of protein and minerals o Less fat than mature milk • Lactogenesis stage II ➢ Occurs by day 3 to 5 when copious amount of milk comes in to breast • Assess proper latch ➢ Placement of the infant's mouth over the nipple, areola, and breast, making a seal between the mouth and breast to create adequate suction for milk removal ➢ In preparation for latch during early feedings the mother should manually express a few drops of colostrum or milk and spread it over the nipple. This action lubricates the nipple and may entice the baby to open the mouth as the milk is tasted. ➢ To facilitate latch the mother supports her breast in one hand with the thumb on top and four fingers underneath at the back edge of the areola. The breast is compressed slightly, so that an adequate amount of breast tissue is taken into the mouth with latch. Most mothers need to support the breast during feeding for at least the first days until the infant is adept at feeding. ➢ With the baby held close to the breast with the mouth directly in front of the nipple the mother tickles the baby's lower lip with her nipple, stimulating the mouth to open. When the mouth is open wide and the tongue is down the mother quickly “hugs” the baby to the breast, bringing the baby onto the nipple. She brings the infant to the breast, not the breast to the infant. ➢ In general, the baby's mouth should cover the nipple and an areolar radius of approximately 2 to 3 cm all around the nipple. If breastfeeding is painful, the baby likely has not taken enough of the breast into the mouth, and the tongue is pinching the nipple. ➢ When latched correctly, the baby's cheeks and chin are touching the breast. ➢ If the baby is nursing appropriately, (1) the mother reports a firm tugging sensation on her nipples but feels no pinching or pain, (2) the baby sucks with cheeks rounded, not dimpled, (3) the baby's jaw glides smoothly with sucking, and (4) swallowing is usually audible. • Weight loss of Newborn ➢ Newborn infants typically lose 5% to 10% of body weight before they begin to demonstrate weight gain. Weight loss of 7% in a breastfeeding infant during the first 3 days of life needs to be investigated ➢ Medications or diets that promote weight loss are not recommended for breastfeeding mothers. Many women will experience a gradual weight loss while lactating as fat stores deposited during pregnancy are used. Rapid loss of large amounts of weight may be detrimental, given that fat-soluble contaminants to which the mother has been exposed are stored in body fat reserves, and these may be released into the breast milk. Another potential consequence of weight loss is reduced milk production. For most women, weight loss of 1 to 2 kilograms per month is safe; however, if weight loss exceeds this amount, careful evaluation of infant weight and feeding pattern is recommended • Storage of Breastmilk ➢ The preferred containers for long-term storage of breast milk are hard sided, such as hard plastic or glass, with an airtight seal. For short-term storage (<72 hours), plastic bags designed for human milk storage can be safely used. ➢ For full-term, healthy infants, freshly expressed breast milk can be safely stored at room temperature for up to 8 hours, and it can be refrigerated safely for up to 5 to 8 days. Milk can be frozen for up to 6 months in the freezer section of a refrigerator with a separate door and for up to 12 months in a deep freezer. Storage guidelines for hospitalized infants are somewhat stricter. When breast milk is stored, the container should be dated, and the oldest milk should be used first ➢ Frozen milk is thawed by placing the container in the refrigerator for gradual thawing or in warm water for faster thawing. It cannot be refrozen and should be used within 24 hours. After thawing the container needs to be shaken so as to mix the layers that have separated Method Healthy Infant Hospitalized Infant Room temperature (77° F or 25° C) <8 hours <4 hours Refrigerator (39° F or 4° C) 5-8 days <8 days Freezer compartment of a one door refrigerator 2 weeks Not recommended Freezer compartment of a two door refrigerator (23° F or −5° C) (not in door) <6 months <3 months Deep freezer(−4° F or −20° C) <12 months <6 months Mastitis • Common concern with breastfeeding • Inflammation of the breast, often associated with infection, characterized by influenza-like symptoms and redness and tenderness in the affected breast Chapter 20 Gestational diabetes • Any degree of glucose intolerance with onset or recognition during pregnancy- whether or not insulin is used to treat • Metabolic changes associated with pregnancy- alterations in glucose metabolism, insulin production and metabolic homeostasis o Glucose crosses placenta, but insulin does not o Increased insulin resistance, increased insulin requirements • Pre-gestational diabetes mellitus o Preconception counseling o Maternal risks and complications: miscarriage, HTN, infections, macrosomia, hydramnios, ketoacidosis, hyperglycemia (being 14-16 weeks as insulin resistance increases), hypoglycemia- first trimester when glucose is lower, insulin is enhanced • Fetal risks- less if developed after 1st trimester • Screening for gestational diabetes mellitus • Antepartum care: o Diet and exercise- standard diabetic diet 1500-2000 calorie, exercise lowers blood glucose, monitoring blood glucose levels, medications for controlling blood sugar levels- 20% require insulin, Glyburide, fetal surveillance • Poor maternal glycemic control before conception and in the first trimester may be responsible for fetal congenital malformations • Maternal insulin requirements increase as pregnancy progresses and may quadruple by term as a result of insulin resistance created by placental hormones, insulinase, and cortisol • Poor glycemic control during pregnancy can lead to maternal complications such as miscarriage, infection, and dystocia • Close glucose monitoring, insulin administration, and dietary counseling are used to create a normal intrauterine environment for fetal growth • Because GDM is asymptomatic in most cases, all women should undergo routine screening Anemia • 20-60% of women. Decreased oxygen carrying capacity of blood, increases CO, can result in CHF, difficulty in tolerating blood loss at birth o Iron deficiency anemia- most asses ferritin levels o Folate deficiency- increase in folate demands and less GI absorption of folate o Sickle cell hemoglobinopathy o Thalassemia Substance abuse • Refers to the continued use of substances despite related problems in physical, social, or interpersonal areas of life • Any use of alcohol or illicit drugs in pregnancy is considered abuse • Due to under-reporting it is difficult to ascertain the prevalence of the issue • Approximately 15% or pregnant women have a substance abuse problem • Barriers to treatment o Less than 10% of woman receive adequate treatment due to: ▪ Social stigma ▪ Labeling ▪ Guilt • Substance-abuse treatment programs do not address issues affecting pregnant women • Long waiting lists and lack of health insurance present further barriers to treatment • Legal considerations o Women who abuse substances may face criminal charges o Nurses who encourage prenatal care, counseling, and treatment are of greater benefit to mother and child than prosecution o Nurses should become involved in efforts to block punitive legislation • Screening o Should be done at the first prenatal visit o Urine toxicology • Assessment o Lifestyle increases risks for STIs, HIV o Lab assessment for syphilis, Hepatitis B and C, HIV o Ultrasound to determine gestational age • Initial care: o Consequences of drug use should be clearly communicated, and abstinence recommended o Women more receptive to making lifestyle changes during pregnancy than at any other time o More likely to stop smoking during pregnancy o Women for Sobriety o Methadone maintenance treatment for pregnant women is the standard of care o Cocaine use during pregnancy has increased dramatically • Follow-up care o Breastfeeding definitely contraindicated in women who continue to use amphetamines, alcohol, cocaine, heroin, or marijuana o Home situation must be assessed for safe environment o Someone must be available to meet infant’s needs if mother is unable o If infant’s well-being is questionable, case will be referred to child protective services agency Chapter 21 Gestational HTN, preeclampsia, eclampsia, HELLP • HTN in pregnancy o Significance and incidence: hypertensive disorders of pregnancy are the most common medical complication reported during pregnancy, preeclampsia complicates approximately 5-10% of all pregnancies, significant contributor to maternal and perinatal morbidity and mortality • Gestational HTN o Onset of HTN without proteinuria after the 20th week of pregnancy ▪ Systolic BP > 140 mmHG ▪ Diastolic > 90 mmHg o Diagnosis of onset during pregnancy based on two measurements that meet criteria for gestational BP elevation within a 1-week period • Preeclampsia o Pregnancy-specific syndrome o HTN develops after 20 weeks of gestation in previously normo-tensive woman o Disease of reduced organ perfusion with presence of HTN and proteinuria o Complicates 3-7% of all pregnancies o Etiology: unique to human pregnancies, S+S develop only during pregnancy and disappear after birth, associated high risk factors: primigravidity, multifetal pregnancy, obesity, preexisting medical condition, preeclampsia in a prior pregnancy o Patho: may be caused by disruptions in placental perfusion and endothelial cell dysfunction ▪ Main pathogenic factor is not an increase in BP but poor perfusion resulting from vasospasm ▪ Arteriolar vasospasm diminishes diameter of blood vessels, which impedes blood flow to all organs and increases BP ▪ Significant decreases in placental, kidney, liver and brain function • HELLP syndrome o Laboratory diagnostic variant of severe preeclampsia involves hepatic dysfunctions, characterized by: hemolysis (H), elevated liver enzymes (EL), low platelets (LP) o Associated with increased risk for: pulmonary edema, acute renal failure, DIC, placental abruption, liver hemorrhage or failure, ARDs, sepsis, stroke (high risk for maternal death) • Eclampsia o Seizure activity or coma in woman diagnosed with preeclampsia o No Hx of previous seizure disorder o Presentation varies ▪ One third in labor ▪ One third during delivery ▪ One third within 72 hours postpartum o S+S- headache, blurred vision, severe epigastric pain, altered mental status o Tonic-clonic convulsions, hypotension, coma o Immediate care: ensure patent airway, pt safety is a major concern, post-seizure decision regarding timing and method of birth , HELLP syndrome (lab eval and infusion of blood products) • Care management: o Physical exam: consistency in taking BP readings and recording them in a standardized manner, electronic BP devices are less accurate, readings are affected by maternal position (dependent edema, pitting edema, DTR), lab tests o Mild gestational HTN and mild preeclampsia ▪ Goal is to ensure maternal safety and deliver a healthy newborn ▪ May be safely managed at home • Maternal and fetal assessment, activity restriction, diet o Severe gestational HTN or severe preeclampsia ▪ At greater risk for pregnancy complications ▪ Should be hospitalized for at least 24 hours for observation and tx if necessary • Intrapartum care, magnesium sulfate is the drug of choice, load 4-6 grams then 2 grams/hr. levels 4-7. Calcium gluconate for toxicity • Control of BP- hydralazine is the drug of choice • Postpartum care Magnesium sulfate therapy, toxicity, effects on labor • Magnesium sulfate, the anticonvulsant of choice for preventing eclampsia, requires careful monitoring; its antidote, calcium gluconate, should be at the bedside Hyperemesis • Hyperemesis gravidarum- excessive vomiting accompanied by weight loss, electrolyte imbalance and ketonuria o Etiology: 0.5% of all live births o Management: assessment, initial care- IV therapy, electrolytes, antiemetic meds, follow- up care Types of miscarriage • Miscarriage (spontaneous abortion) – a pregnancy that ends as a result of natural causes prior to 20 weeks gestation • Types: threatened, inevitable, complete, missed, recurrent • Threatened slight spotting, mild uterine cramping, managed w/ bed rest (controversial), sedation, avoidance of stress, sexual stimulation and orgasm usually recommended, acetaminophen analgesics, further tx depending on woman’s response • Inevitable moderation bleeding, mild to sever uterine cramping, cervical dilation, managed with bed rest if no pain, fever or bleeding present- if rupture of membranes, bleeding, pain or fever present then prompt termination of pregnancy accomplished by dilation & curettage • Complete sight bleeding, mild uterine cramping, no cervical dilation (cervix already closed), no further intervention may be needed if contractions adequate enough to prevent hemorrhage and no infection present • Missed no bleeding or spotting, if spontaneous evacuation of uterus does not occur within 1 month uterus is emptied by method appropriate to duration of pregnancy, blood clotting factors are monitored until uterus is empty, DIC and incoagulability of blood with uncontrolled hemorrhage may develop in cases of fetal death after the 12th week, if products of conception are retained for longer than 5 weeks, may be treated with dilation and curettage or misoprostol given orally or vaginally Incompetent cervix, management • Management: conservative management of bed rest, progesterone, anti-inflammatory drugs and antibiotics o Prophylactic cerclage is placed at 11-15 weeks of gestation o Nursing care and home care o Removed at 37 weeks or when labor begins Hydatidiform mole, diagnosis (Molar Pregnancy) • Gestational trophoblastic disease is a spectrum of pregnancy-related trophoblastic disorders without a viable fetus • Two distinct types of hydatidiform moles are: o Complete (or classic) ▪ Mole results from fertilization of egg with lost or inactivated nucleus ▪ No fetus, placenta, or amniotic membrane o Partial mole ▪ Result of two sperm fertilizing a normal ovum ▪ Embryonic parts present and an amniotic sac • Clinical manifestations o Early stages: a normal pregnancy o Later stages: bright red or brown vaginal bleeding o Excessively enlarged uterus • Management o Most pass spontaneously o Suction curettage is safe o Oxytocin induction is not recommended Placenta previa, Abruptio placenta, DIC • Placenta previa o Placenta implanted in lower uterine segment near or over internal cervical os o Classification based on degree to which internal cervical os is covered by placenta ▪ Complete placenta previa ▪ Partial placenta previa ▪ Marginal placenta previa o Incidence and etiology o Clinical manifestations o Maternal and fetal outcomes ▪ Maternal morbidity and mortality ▪ Complications ▪ Fetal risks include malpresentation and fetal anemia ▪ Preterm birth o Diagnosis and medical management ▪ Standard diagnosis is transabdominal ultrasound examination • Any woman with painless vaginal bleeding after 20 weeks gestation should be evaluated for a previa o Management ▪ Expectant management: observation and bed rest ▪ Cesarean birth ▪ Hospital and home care • Premature separation of placenta (Placental abruption) o Incidence and etiology o Classification systems ▪ Grades: 1 (mild), 2 (moderate), 3 (severe) o Clinical manifestations ▪ Vaginal bleeding ▪ Abdominal pain ▪ Uterine tenderness and contractions o Maternal, fetal, and neonatal outcomes ▪ Perinatal mortality of 20% to 30% ▪ IUGR and preterm birth o Management ▪ Depends upon severity of blood loss and fetal status ▪ Delivery is the treatment of choice • DIC o DIC – disseminated intravascular coagulation o Pathologic form of diffuse clotting causing widespread external and internal bleeding o Often triggered by the release of large amounts of thromboplastin o HELLP and preeclampsia may trigger DIC Chapter 22 Preterm labor, biochemical markers, tocolytics o Preterm Labor: Cervical changes and uterine contractions occurring between 20-37 weeks of pregnancy o Preterm Birth: Any birth occurring before completion of 37 weeks of pregnancy o Preterm birth is very dangerous to the infant ▪ Decreased length of time in utero correlates with immaturity of body systems o Two categories of preterm labor/birth ▪ Spontaneous • Preterm labor, preterm premature rupture of membranes (PPROM), cervical insufficiency, amnionitis ▪ Indicated • A means to resolve maternal or fetal risk related to continuing the pregnancy o Predicting spontaneous preterm labor and birth ▪ Known Risk Factors • History of preterm birth, multiple gestation, bleeding after 1st trimester, low maternal BMI ▪ Biochemical Markers • Fetal fibronectin o Glycoprotein found in plasma during fetal life o Protein that attaches the amniotic sac o Normal in vaginal mucous before 22 weeks and late in pregnancy o Best if done 22-24 weeks o Cost of determining biochemical markers is high ▪ Endocervical length • Changes occurs before uterine activity • Over 30 cm is less likely to give birth premature even with contractions present o Causes if preterm labor/birth ▪ Infections – bacterial vaginosis ▪ Bleeding at site of placental implantation ▪ Multiple pathologic processes • Stress, uterine overdistention, allergic reaction, decreased progesterone, o Care Management ▪ Prevention to address risk factors ▪ Education about early symptoms of preterm labor ▪ Teach what to do ▪ Early recognition and diagnosis • Gestational age between 20-37 weeks • Uterine activity (contractions) • Progressive cervical changes • Effacement of 80%, cervical dilation of 2 cm or greater ▪ Suppression of uterine activity • Tocolytics: Goal is to delay birth long enough to institute interventions that delay neonatal morbidity and mortality o Magnesium sulfate most commonly used o Beta adrenergic ▪ Terbutaline (Brethine) o Nifedipine (CCB) o Indomethacin (Indocin) (NSAID), decreases prostaglandins which increase uterine contractility • antenatal glucocorticoids o Promotion of fetal lung maturity o Antenatal Glucocorticoids ▪ IM Injection ▪ NIH recommends for all women at risk for preterm (24-34 weeks) ▪ Reduces Incidence of: • Respiratory distress syndrome • Necrotizing enterocolitis • Intraventricular hemorrhage • Death • PROM, PPROM- o Premature Rupture of Membranes (PROM) ▪ Rupture of amniotic sac and leakage of amniotic fluid beginning at least 1 hour before onset of labor at any gestational age ▪ Membrane rupture at less than 37 weeks is responsible for one third of all preterm (PPROM) o Preterm Premature Rupture of Membranes (PPROM) ▪ Results from pathologic weakness of the fetal membranes • Infection, stress from uterine contractions, inflammation, other factors ▪ Chorioamnionitis • Infection of the amniotic cavity is the most common complication • dysfunctional labor, types- o Dystocia AKA dysfunctional labor ▪ Defined as long, difficult, or abnormal labor ▪ Dysfunctional labor describes as abnormal uterine contractions that prevent the normal progress of: • Cervical dilation, effacement (primary powers), Descent (secondary powers) o Dystocia can be caused by any one of the following: ▪ Ineffective uterine contractions or maternal bearing-down efforts (the powers), the most common cause of dystocia ▪ Alterations in the pelvic structure (the passage) ▪ Fetal causes that include abnormal presentation or position, anomalies, excessive size, and number of fetuses (the passenger) ▪ Maternal position during labor and birth ▪ Psychologic responses of the mother to labor related to past experiences, preparation, culture and heritage, and support system o Dysfunctional Labor ▪ Hypertonic uterine dysfunction • Or primary dysfunctional labor, painful, frequent contractions, but ineffective in causing cervical dilation or effacement to progress ▪ Hypotonic uterine dysfunction • Or secondary uterine inertia, normal progress, then contractions become weak or stop ▪ Secondary powers- • Exhaustion with pushing, being too numb, poor position ▪ Abnormal labor patterns • Prolonged latent stage, protracted (long) active phase dilation, secondary arrest, no change, protracted descent, arrest (stopped) of descent, failure to descend ▪ Precipitous labor • Lasts less than 3 hours from onset of contractions to birth • May result from hypertonic uterine contractions that are tetanic in intensity o Conditions often associated with this type of uterine contractions are placental abruption, an excessive number of uterine contractions, and recent cocaine use • Maternal complications can include uterine rupture, lacerations, amniotic embolism (anaphylactoid syndrome of pregnancy), postpartum hemorrhage • Fetal complications include hypoxia, caused by decreased periods of uterine relaxation between contractions, and in rare instances, intracranial trauma related to rapid birth • Women who have experienced precipitous labor often describe feelings of disbelief that their labor began so quickly, alarm that their labor progressed so rapidly, panic about the possibility they would not make it to the hospital in time to give birth, and finally relief when they arrived at the hospital. In addition, women have expressed frustration when nurses did not believe them when they reported their readiness to push. o Alterations in pelvic structure ▪ Pelvic dystocia • Contractures of pelvic diameters that reduce capacity of bony pelvis, inlet, midpelvis, or outlet ▪ Soft-tissue dystocia • Results from obstruction of birth passage by an anatomic abnormality other than bony pelvis (previa, fibroids, full bladder) o Fetal causes of dystocia ▪ Anomalies (tumors, neural tube defects, hydrocephalus) ▪ CPD- Cephalopelvic disproportion ▪ Malposition- persistent occipitoposterior position ▪ Malpresentation- presenting part other than head ▪ Multifetal pregnancy • Cephalopelvic Disproportion(CPD) o Condition in which the infant's head is of such a shape, size, or position that it cannot pass through the mother's pelvis, or the maternal pelvis is too small, abnormally shaped, or deformed to allow the passage of a fetus of average size. ▪ FETAL CAUSE OF Increased Risk For Uterine Dystocia ▪ In order to have a Vacuum-Assisted Birth➔ABSENCE of CPD • Care Management of Dystocia➔ Obstetric Procedures o Version ▪ Turning of fetus from one position to another ▪ External Cephalic Version • Used in attempt to turn fetus from breech or shoulder presentation to vertex presentation • Attempted in L& B Setting After 37 Weeks • Before Attempted➔ o Assess Fetus(Using US) o Do an NST o Informed Consent Obtained o Tocolytic Given(To relax uterus& facilitate maneuver) o Procedure Most Successful When=Women Has Normal Amount Amniotic Fluid & Fetus is Not Yet Engaged In Pelvic • During Procedure Nurse➔ Continuously Monitors FHR, Maternal VS and Women’s Level of Comfort ▪ Internal Version • Physician inserts hand to change presentation to cephalic or podalic • Rare➔Mostly with Delivering 2nd Twin • Induction of Labor o Chemical or mechanical initiations of uterine contractions before their spontaneous onset for the purpose of bringing about the birth o May be Induced ▪ Electively • No Medical Purpose/ Women Should Be @least 39 Weeks • Risks➔↑Rates Cesarean Birth & Iatrogenic Prematurity ▪ Indicated Reasons • If continuing pregnancy dangerous to women/fetus & if no contraindications exist to artificial rupture of membranes or augmenting uterine contractions) o Indications➔ HTN Comp, DM,Fetal death, Chorioamnionitis, Postterm pregnancy(esp. w/ oligohydramnios), Intrauterine growth restriction, PROM w/ established fetal maturity • Augmentation of Labor o Contraindications➔ Acute/severe fetal distress, Shoulder presentation(transverse lie), Floating fetal presenting part, Uncontrolled hemorrhage, Placenta previa, Previous uterine incision that prohibits a trial of labor o Stimulation of uterine contractions after but progress is unsatisfactory o Implemented for management of hypotonic uterine dysfunction o Common augmentation methods➔Oxytocin infusion, Amniotomy, Nipple stimulation • Methods o Amniotomy ▪ Artificial rupture of membranes when the condition of the cervix is favorable(ripe) or to augment(help) labor if progress begins to slow. ▪ Actual rupture of membranes is PAINLESS but she may experience some discomfort when the Amnihook is inserted through vagina/cervix + the presenting part of the fetus should be engaged and well applied before procedure to prevent cord prolapse. ▪ Risks➔Infection, Umbilical cord prolapse o Oxytocin ▪ Hormone normally produced by posterior pituitary gland➔Stimulates uterine contractions ▪ Used to induce labor or augment a labor progressing slowly because of inadequate uterine contractions ▪ Can present hazards to mother or fetus- pain, abruption, uterine rupture, unnecessary C/S, postpartum hemorrhage, infection, Hypoxemia for fetus ▪ Tachysystole➔More than 5 contractions in 10 minutes • Cesarean Delivery o Transabdominal Incision of Uterus o Stats=31% of live births in 2006, Highest rate ever reported in the U.S. o (+)=Preserve life or health of mother and her fetus o (-)May have a negative effect on the woman’s perception of her birth experience o Contributing Factors=Fetal macrosomia, Advanced maternal age, Obesity, Gestational diabetes, Multifetal pregnancy, Malpractice concerns o Indications= Conditions that threaten mom or baby o Types=➔ ▪ Scheduled=Elective(or on demand ▪ Unplanned= Forced(ethical considerations) o Surgery ▪ Incision Types • Skin Incisions determined By the Urgency of the Surgery, The Type of Skin Incisions DOESN’T necessarily indicate the type of Uterine Incision • Low Transverse o Performed More Often+ PREFFERED • Vertical Incision o Extending From Near Umbilicus to the Mons Pubis o Complications=↑risk of rupture in subsequent pregnancies & ↑ blood loss ▪ Complications and Risks➔Aspiration, hemmorhage, atelectasis, endometritis, wound dehiscence, infection, UTI, injury to bladder or bowel, anesthesia complications ▪ Pre-Op • Preparation➔ CBC, blood type and Rh ▪ Intra-Operative • Anesthesia➔spinal, epidural, spinal • Care ▪ Post-Op • IMMEDIATE Postoperative Period➔vitals q 15 minutes, incision, fundus, lochia, IV, foley, pain medication, deep breathing, bonding • Postoperative and Postpartum Care➔ pain from incision and intestinal gas, advancing diet, ambulation, pericare, hygiene, voiding, vitals, fundus, lochia, breasts, psychological adaptation, bonding, care of infant, breastfeeding o Vaginal Birth After Cesarean ▪ Unless contraindicated, vaginal birth is possible after a cesarean birth ▪ Indications for primary cesarean birth such as dystocia, breech presentation, or fetal distress often are nonrecurring ▪ A woman who has had a cesarean birth may subsequently become pregnant and not have any contraindications to labor and vaginal birth in that pregnancy and may attempt a vaginal birth after cesarean (VBAC) ▪ 9% of women attempt a trial of labor (TOL) after C/S • Prolapsed Umbilical Cord o When cord lies below presenting part of fetus o Contributing Factors ▪ Long cord (longer than 100 cm) ▪ Malpresentation (breech) ▪ Unengaged presenting part o Management ▪ Prompt recognition ▪ Relieve pressure on the cord Chapter 23 • Postpartum Hemorrhage o Definition and Incidence ▪ PPH traditionally defined as loss of more than: • 500 ml of blood after vaginal birth • 1000 ml after cesarean birth • 10% drop in hematocrit ▪ Leading cause of maternal morbidity and mortality ▪ Life-threatening with little warning ▪ Often unrecognized until profound symptoms o Etiology and Risk Factors➔Causes ▪ LEADING CAUSE➔Uterine Atony • Marked hypotonia of uterus ▪ Lacerations of genital tract ▪ Hematomas- unrelenting pain ▪ Retained placenta • Nonadherent retained placenta • Adherent retained placenta o Accreta- into myometrium, increta- deep through myometrium, percreta- perforation of uterus o Inversion of Uterus ▪ Turning inside out of uterus ▪ Potentially life threatening/ 1 in 2500 births o Subinvolution of uterus ▪ Late postpartum bleeding ▪ Prolonged lochial discharge and excessive bleeding o Nursing Care Management➔Assessment • Early recognition is critical • First step is evaluation of contractility of uterus • Firm massage of fundus • Administration of intravenous fluids and medication to manage bleeding • Administration of medications to contract the uterus Mastitis: Mastitis affects approximately 1% to 10% of women soon after childbirth, most of whom are first-time mothers who are breastfeeding. Mastitis is almost always unilateral and develops well after the flow of milk has been established. The infecting organism is generally the hemolytic S. aureus. An infected nipple fissure is usually the initial lesion, but the ductal system is involved next. Inflammatory edema and engorgement of the breast soon obstruct the flow of milk in a lobe; regional, then generalized, mastitis follows. If treatment is not prompt, mastitis may progress to a breast abscess. • Symptoms rarely appear before the end of the first postpartum week and are more common in the second to fourth weeks. Chills, fever, malaise, and local breast tenderness are noted first. Localized breast tenderness, pain, swelling, redness, and axillary adenopathy also may occur. • The first symptom of postpartum infection is usually fever greater than 38° C on two consecutive days Postpartum depression, psychosis, screening: • Postpartum “blues”- about 80% or woman-Emotionally labile and crying for no apparent reason, Period of emotional and physical vulnerability, Postpartum fatigue • 10% to 15 % of women go on to experience postpartum depression- Postpartum depression screening should be performed on all women • Postpartum Depression (PPD)- Postpartum depression is a nonpsychotic depressive episode that begins in the postpartum period due to decreased estrogen level o Symptoms: changes in appetite or weight, sleep, and psychomotor activity; decreased energy; feeling of worthlessness or guilt; difficulty thinking, concentrating or making decisions; or recurrent thoughts of death or suicidal ideation, plans, or attempts. • Postpartum Psychosis- A very serious type of PPD illness that can affect new mothers. Begin 2-3 weeks post delivery, Fatigue, restlessness, insomnia, crying liable emotions, inability to move, irrationally statements incoherence confusion and obsessive concerns about the infant’s health, Psychiatric emergency • Mental health disorders in postpartum period have implications for mother, newborn, and entire family-Interfere with attachment to newborn and family integration, May threaten safety and well-being of mother, newborn, and other children • Mood disorders- Many women experience a mild depression or “baby blues”, 13% of women develop more serious depression, Can eventually incapacitate them to point of being unable to care for themselves and their babies • Postpartum depression without psychotic features---Postpartum depression: an intense and pervasive sadness with severe and labile mood swings • Treatment options - Antidepressants, anxiolytic agents, and electroconvulsive therapy, Psychotherapy focuses on fears and concerns related to new responsibilities and roles; monitoring for suicidal or homicidal thoughts • Postpartum depression with psychotic features---Postpartum psychosis: syndrome characterized by depression, delusions, and thoughts of harming either infant or herself , Psychiatric emergency; may require psychiatric hospitalization, Antipsychotics and mood stabilizers such as lithium are treatments of choice • Identification of women at greatest risk for postpartum depression can be facilitated by the use of screening tools Chapter 24 Respiratory distress, respirations in preterm infant: • Flaring • Intercostal or Subcostal Retractions (In-drawing of the tissue between the ribs or below the ribcage) • Grunting • Stridor or Gasping (Most Often Represent Upper Airway Obstruction) • Paradoxical (SEESAW) Respirations (Exaggerated Rise in the Abdomen, With Respiration, As the Chest Falls) Should Be Reported • RR<30 >60 • Apnea- Pauses in breathing greater than 20 seconds is NOT Normal--Can Be Related To Rapid ↑ Body Temp, Hypothermia, Hypoglycemia, Sepsis) • Tachypnea --May result from Inadequate clearance of lung fluid or Respiratory Distress Syndrome Neutral thermal environment, care of hypothermia: Maintain body temperature-Care of the hypothermic infant, Warming should occur over a period of hours, Transition to the incubator o ➔***Heat Loss MINIMAL and O2 Consumption LOW ▪ Newborns Reaction to Cold Stress • ↑ Need For O2 and ↑ RR o Oxygen consumption and energy are DIVERTED from maintaining normal brain and cardiac function and growth ➔ THERMOGENESIS for survival o If the infant cannot maintain an adequate oxygen tension➔vasoconstriction follows➔ jeopardizes pulmonary perfusion➔ PO2 is decreased, and the blood pH drops➔ Respiratory Distress • ↑ Basal Metabolic Rate o Anaerobic glycolysis➔ Production of Acid➔ Metabolic Acidosis(+ Resp. Acidosis if ↓Respiratory Function Present) o Excessive Fatty Acids➔ May Displace Bilirubin from the albumin-binding sites➔ EXACERBATING HYPERBILIRUBINEMIA • HYPOGlycemia o Anaerobic glycolysis➔ Uses 3-4x the amount of blood glucose➔ Depleting existing stores (Hypoglycemia may be Asymptomatic) • HYPERthermia o Unable to Sweat➔Risk for HYPERTHERMIA o Develops more rapidly b/c➔ ↓ ability to increase evaporative skin water losses o Although newborns have 6x MORE sweat glands than adults they DO NOT FUCTION SUFFICENTLY TO ALLOW THE INFANT TO SWEAT➔ Serious Overheating➔ Cerebral damage from dehydration, heat stroke, or death • Rapid Warming➔Can Cause APNEA Surfactant: reduces surface tension • Immaturity of pulmonary surfactant system in immature infants Increased risk of atelectasis and respiratory distress syndrome; increased work of breathing Meconium aspiration syndrome: Meconium staining of the amniotic fluid can be indicative of nonreassuring fetal status, especially in a vertex presentation. • If meconium is not removed from the airway at birth, it can migrate down to the terminal airways, causing mechanical obstruction and leading to meconium aspiration syndrome (MAS). The fetus may have aspirated meconium in utero, which can cause a chemical pneumonitis. These infants may develop persistent pulmonary hypertension of the newborn (PPHN), further complicating their management. Infants with MAS who received surfactant had improved oxygenation, decreased severity of respiratory failure, and reduced need for ECMO and fewer leaks • Many infants with meconium staining exhibit no signs of depression at birth; however, the presence of meconium in the amniotic fluid necessitates close supervision of labor and monitoring of fetal well-being. The presence of a team skilled in neonatal resuscitation is required at the birth of any infant with meconium-stained amniotic fluid • Appears in 10% to 15% of all birth, Primarily in term and postterm births NAS: A term used to describe a set of behaviors exhibited by the infant who was exposed to chemical substances in utero, Neonatal Behavioral Assessment Scale (NBAS) • Nursing care- Feeding ad lib, Swaddling, holding, reducing stimuli, Individualized developmental care Rh and ABO incompatibility: Only Rh-positive offspring of Rh-negative mother is at risk, If fetus is Rh positive and mother Rh negative, mother forms antibodies against fetal blood cells • ABO incompatibility -Occurs if fetal blood type is A, B, or AB, and maternal type is O • Incompatibility arises because naturally occurring anti-A and anti-B antibodies are transferred across placenta to fetus • Exchange transfusions required occasionally [Show More]
Last updated: 1 year ago
Preview 1 out of 24 pages
Instant download
Buy this document to get the full access instantly
Instant Download Access after purchase
Add to cartInstant download
Also available in bundle (1)

NURSING 306 - OB Exam 1-3, Quizzes 5&6 BUNDLED Study Guide & Proctored Exam
NURSING 306 - OB Exam 1-3, Quizzes 5&6 BUNDLED Study Guide & Proctored Exam
By A+ Solutions 2 years ago
$12.5
8
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Jul 17, 2021
Number of pages
24
Written in
Additional information
This document has been written for:
Uploaded
Jul 17, 2021
Downloads
0
Views
51