*NURSING > SHADOW HEALTH > Focused Exam Abdominal Pain Documentation Provider Notes 100% PASS (All)
Focused Exam Abdominal Pain Documentation Provider Notes 100% PASS
Document Content and Description Below
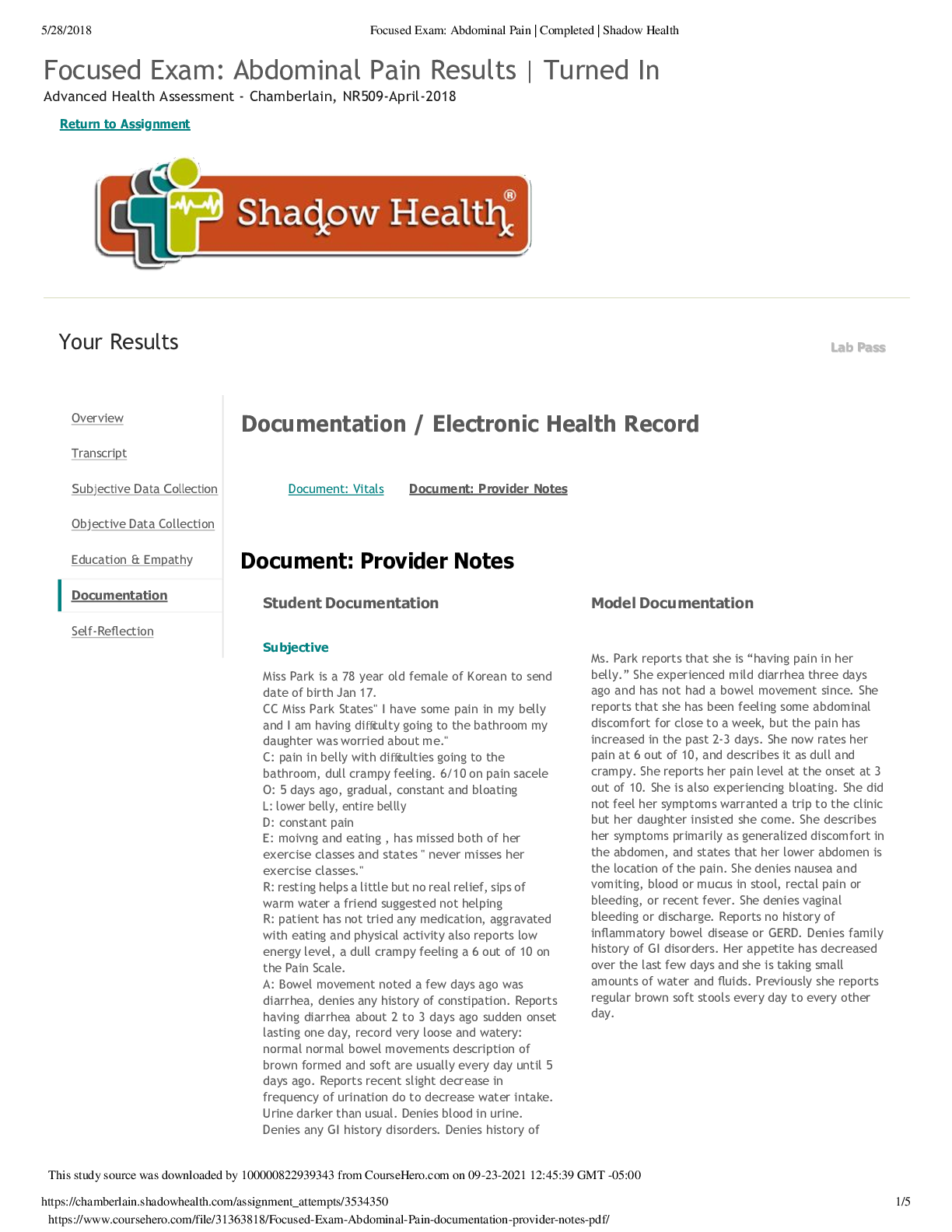
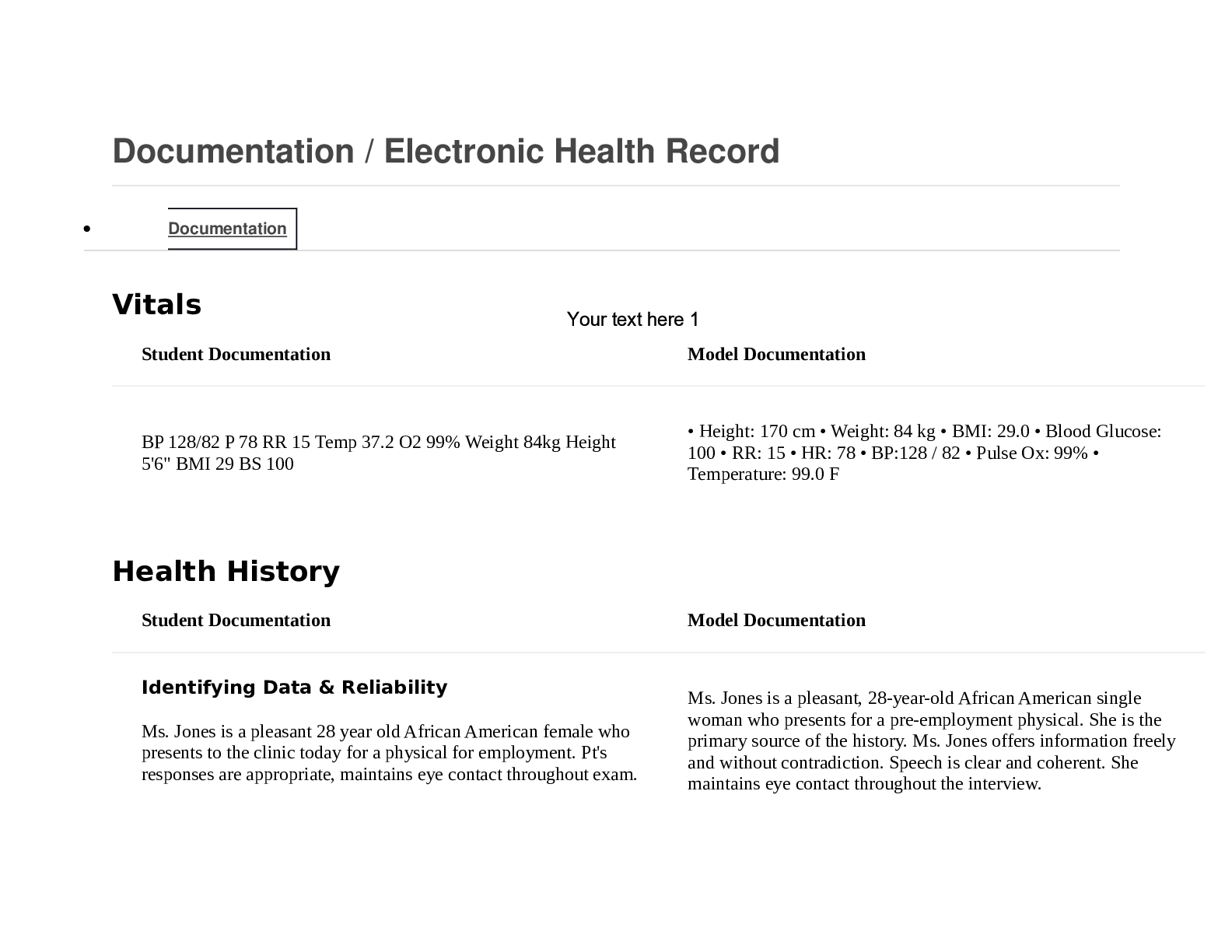
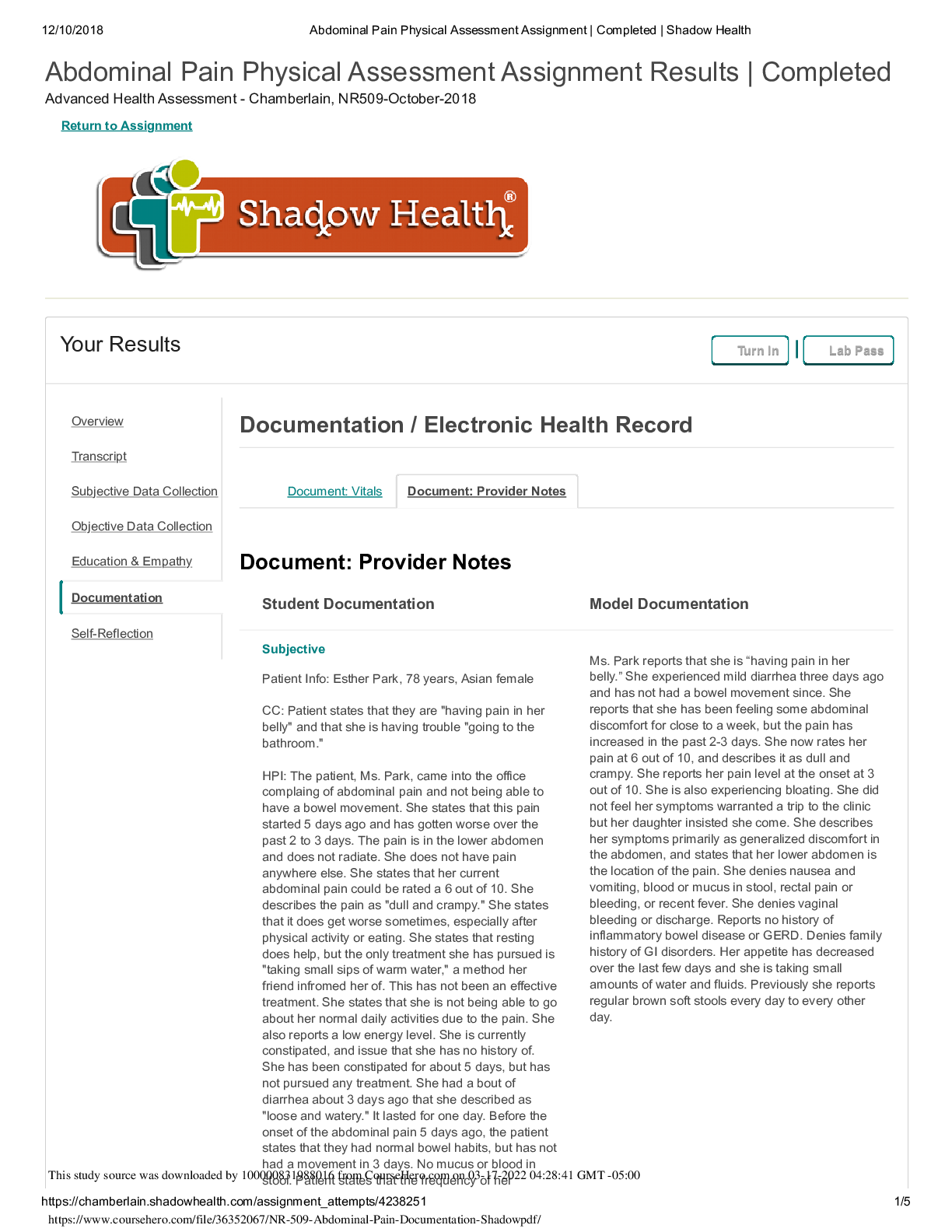
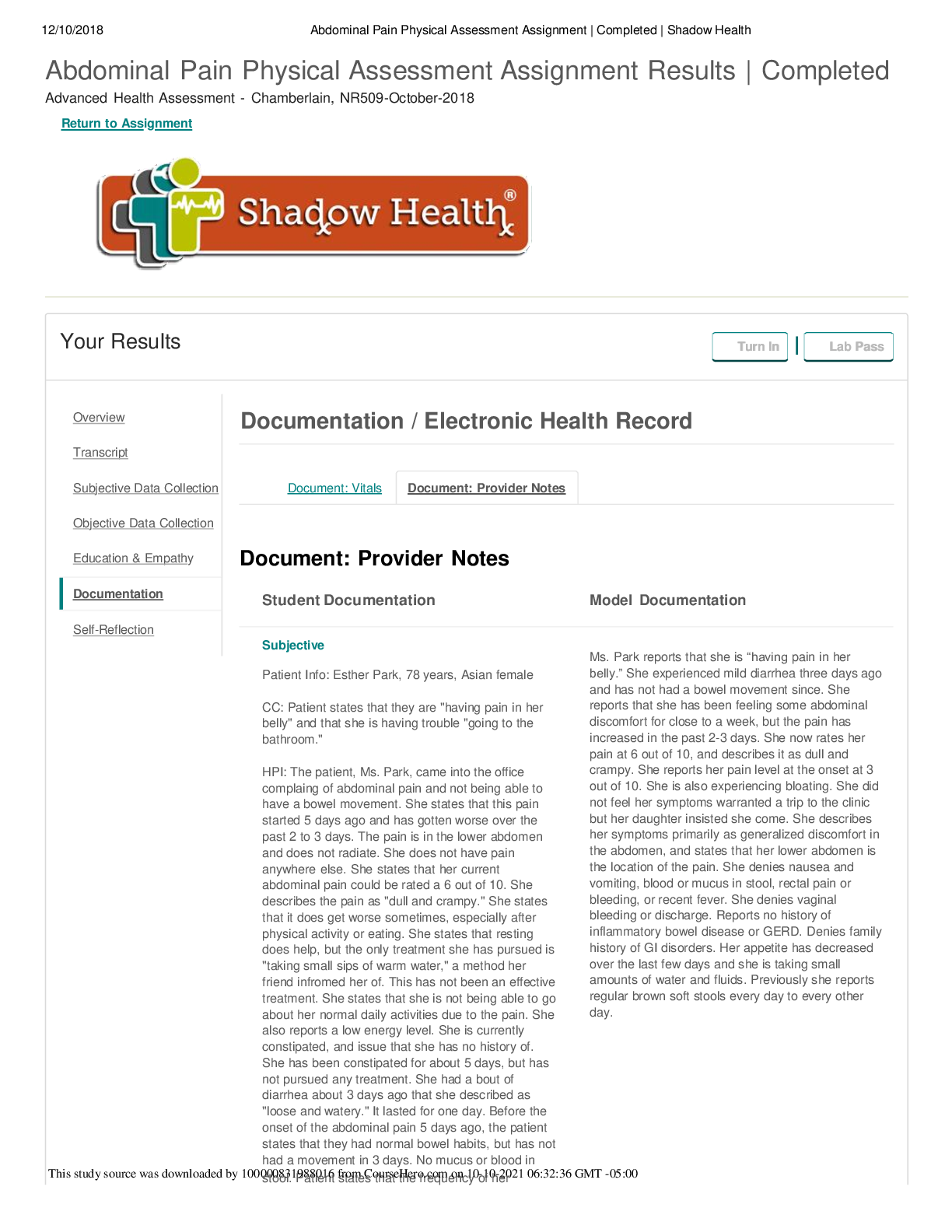
Focused Exam: Abdominal Pain Results | Turned In Advanced Health Assessment - Chamberlain, NR509-April-2018 Return to Assignment Your Results Lab Pass Documentation / Electronic Health Record ... Document: Vitals Document: Provider Notes Document: Provider Notes Student Documentation Model Documentation Subjective Miss Park is a 78 year old female of Korean to send date of birth Jan 17. CC Miss Park States" I have some pain in my belly and I am having difficulty going to the bathroom my daughter was worried about me." C: pain in belly with difficulties going to the bathroom, dull crampy feeling. 6/10 on pain sacele O: 5 days ago, gradual, constant and bloating L: lower belly, entire bellly D: constant pain E: moivng and eating , has missed both of her exercise classes and states " never misses her exercise classes." R: resting helps a little but no real relief, sips of warm water a friend suggested not helping R: patient has not tried any medication, aggravated with eating and physical activity also reports low energy level, a dull crampy feeling a 6 out of 10 on the Pain Scale. A: Bowel movement noted a few days ago was diarrhea, denies any history of constipation. Reports having diarrhea about 2 to 3 days ago sudden onset lasting one day, record very loose and watery: normal normal bowel movements description of brown formed and soft are usually every day until 5 days ago. Reports recent slight decrease in frequency of urination do to decrease water intake. Urine darker than usual. Denies blood in urine. Denies any GI history disorders. Denies history of Ms. Park reports that she is “having pain in her belly.” She experienced mild diarrhea three days ago and has not had a bowel movement since. She reports that she has been feeling some abdominal discomfort for close to a week, but the pain has increased in the past 2-3 days. She now rates her pain at 6 out of 10, and describes it as dull and crampy. She reports her pain level at the onset at 3 out of 10. She is also experiencing bloating. She did not feel her symptoms warranted a trip to the clinic but her daughter insisted she come. She describes her symptoms primarily as generalized discomfort in the abdomen, and states that her lower abdomen is the location of the pain. She denies nausea and vomiting, blood or mucus in stool, rectal pain or bleeding, or recent fever. She denies vaginal bleeding or discharge. Reports no history of inflammatory bowel disease or GERD. Denies family history of GI disorders. Her appetite has decreased over the last few days and she is taking small amounts of water and fluids. Previously she reports regular brown soft stools every day to every other day. Overview Transcript Subjective Data Collection Objective Data Collection Education & Empathy Documentation Self-Reflection 5/28/2018 Focused Exam: Abdominal Pain | Completed | Shadow Health GERD heartburn or ulcers. No history of appendicitis, stomach cancer, or history of liver disease. Report C-section at age 40 in cholecystectomy at age 42 no post-op complications noted. Last pap smear noted about 10 years ago Current medications: Accupril 10 po QD( last dose at (0800 this morning), denies any OTC medications Allergies: Latex : contact dermatitis PMHx: 1. Hypertension diagnosed at age 54 2.3 Pregnancies 4. Surgical history C-section at age of 40; cholecystectomy at age 42 Reports hospitalizations for past surgeries as noted above and after childbirth denies any other hospitalizations. Last pap smear and colonoscopy 10 years ago. SocHx: Last meal with toast for breakfast not eating well. Usually appetite is three meals a day does not eat snacks. Typical meal for breakfast is usually some sort of fruit usually a banana. Typical lunch is usually soup reports sometimes skipping lunch period and typical dinner is chicken or fish with some sort of rice or vegetable. No fiber supplements reported. Patient reports believes gets enough fiber supports eating a vegetable or fruit each day. Reports decrease in thirst especially over the last few days typically patient drinks 6 typically patient drink 6 denies caffeinated drinks such as coffee or soda on occasion drinks chamomile tea. Deny sexual activity reports no STI testing. Report moderate activity attend Fitness classes and reports gardening as a hobby. Lives with her daughter named Jennifer and has a strong support system with her daughter and gentleman friend Max denies any recent travel. Report sexually active no vaginal intercourse reported does report oral sex. 1. No past or present tobacco use 2. Reports drinking one alcoholic (wine)beverage per week, 4 per month only on Sunday's white wine 3. Denies using marijuana, cocaine, heroin or illicit drugs FAM Hx: 1. Mother- deceased at age 88 history of hypertension and Diabetes Type 2 2. Father: deceased at 82 history of hypertension and hypercholesterolemia 3. Maternal grandparents: family history of coronary artery disease and Diabetes Type 2 4. Paternal grandparents: history of obesity, CVA, hypertension 5. Siblings: brother had history of hypertension, hypercholesterolemia, prostate cancer 6. Son: healthy age 48 7. Daughter: healthy age 46 ROS: General: denies any recent fever chills or night sweats although patient does report short-term feeling of tiredness I need to rest more often. GI: reports bloating, slight increase in flatus, recent loss of appetite. No reports of nausea vomiting or 5/28/2018 Focused Exam: Abdominal Pain | Completed | Shadow Health recent weight changes or possible food exposure for food poisoning. GU: denies painful urination no burning upon urination no urinary incontinence no history of UTIs no gynecological problems no vaginal bleeding no vaginal discharge onset of menopause 54. Reports no history of kidney or bladder problems. Respiratory: patient denies any sore throat, cough, dysphagia, difficulty breathing, chest pain or chest tightness. Denies any change of taste. Objective VS B/P: 110/70 mmhg ( MAP 83 mmhg) HR: 92 RR: 16 Temp: 37.2 C ( 98.6 F) Pain 6/10 on pain scale Inspection: Inspection Head and face- flight flushing of the cheeks Inspection Nose- dry appearance Inspection Mouth and throat- dry appearance Inspection Abdominal- scarring noted approximately 6 in a scar to the right upper quadrant and a approximately 10-cm scar at midline Supra pubic region Inspection Lower extremities- inspected lower extremities for edema no edema noted bilaterally. Ausculte Auscultate Heart sounds- S1 and S2 audible no [Show More]
Last updated: 1 year ago
Preview 1 out of 5 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Sep 28, 2021
Number of pages
5
Written in
Additional information
This document has been written for:
Uploaded
Sep 28, 2021
Downloads
0
Views
78

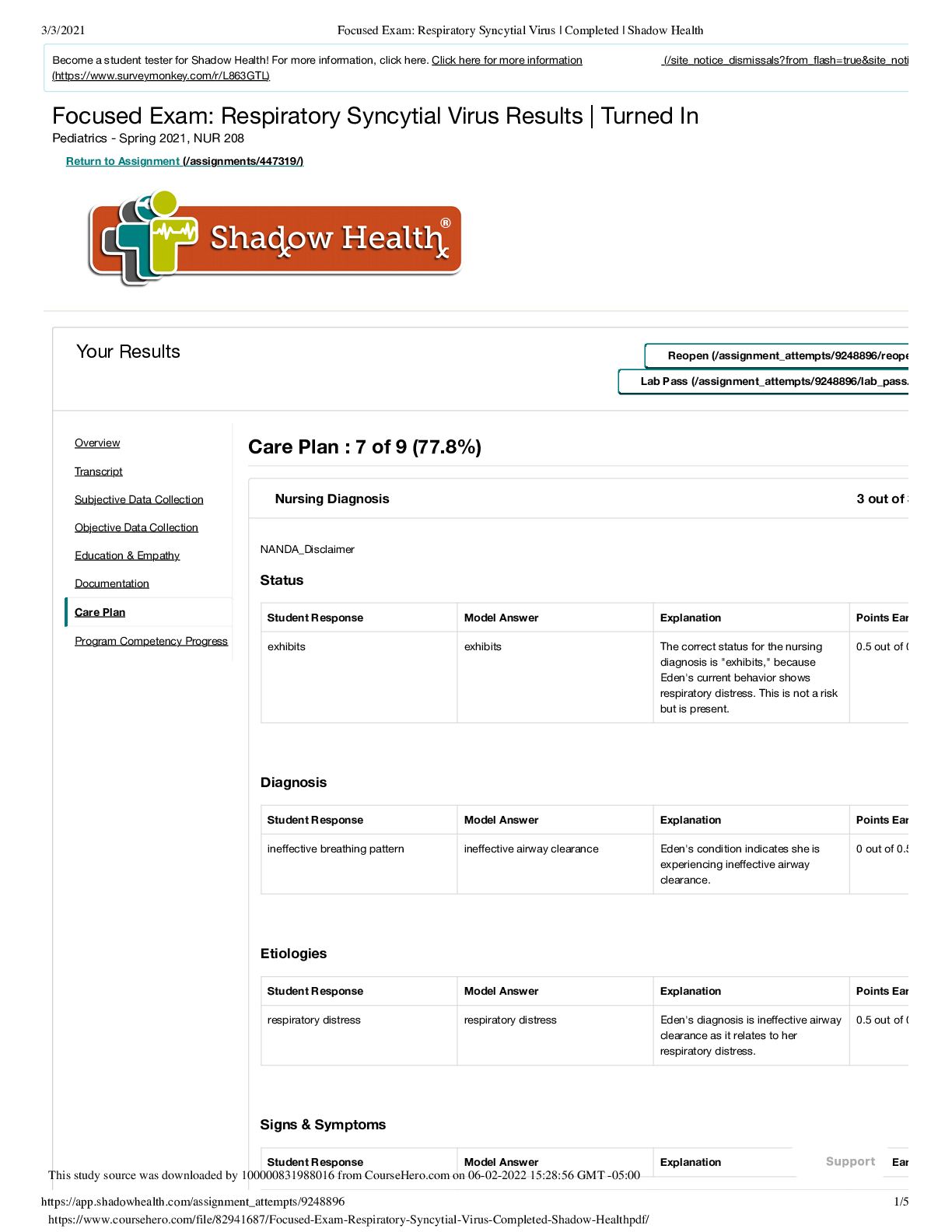
.png)
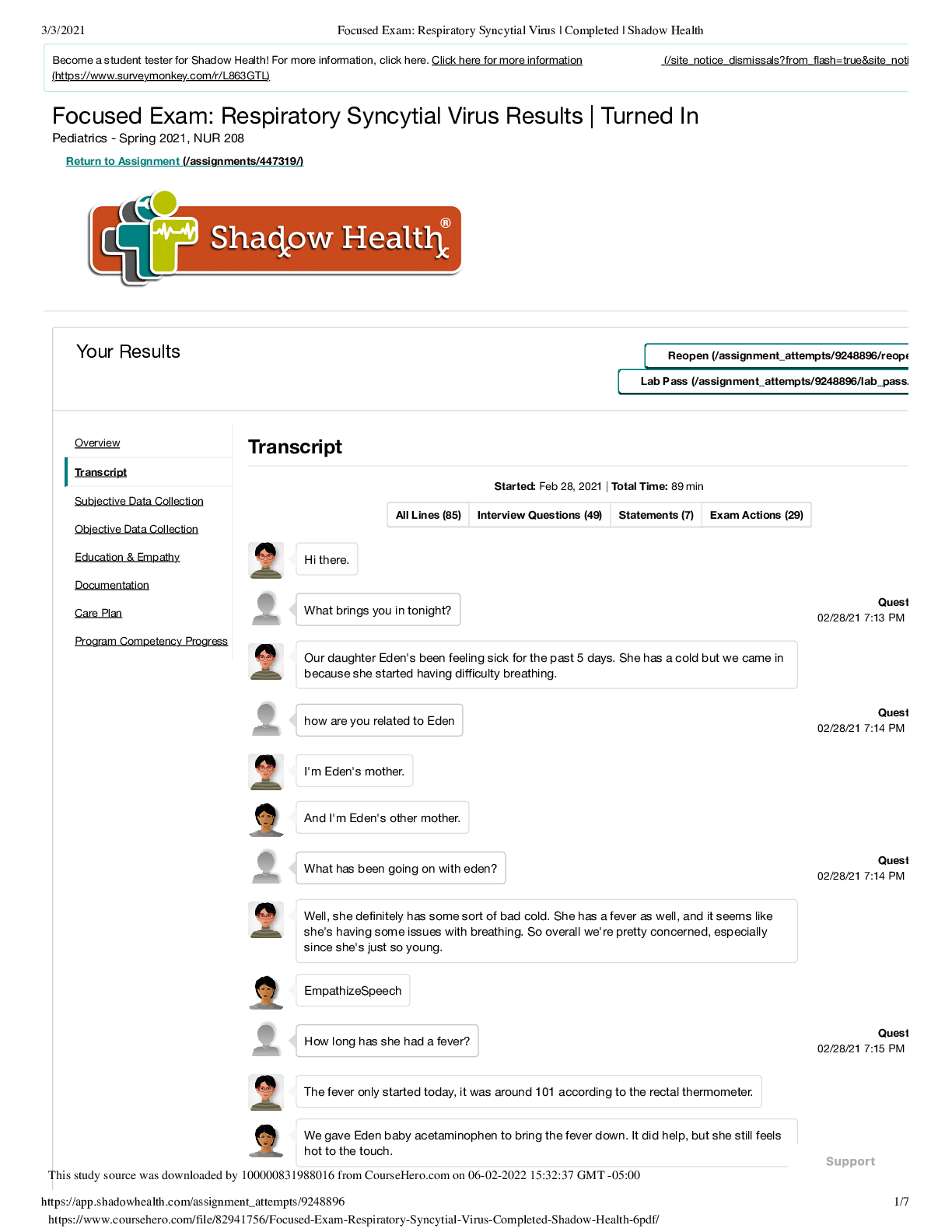
.png)
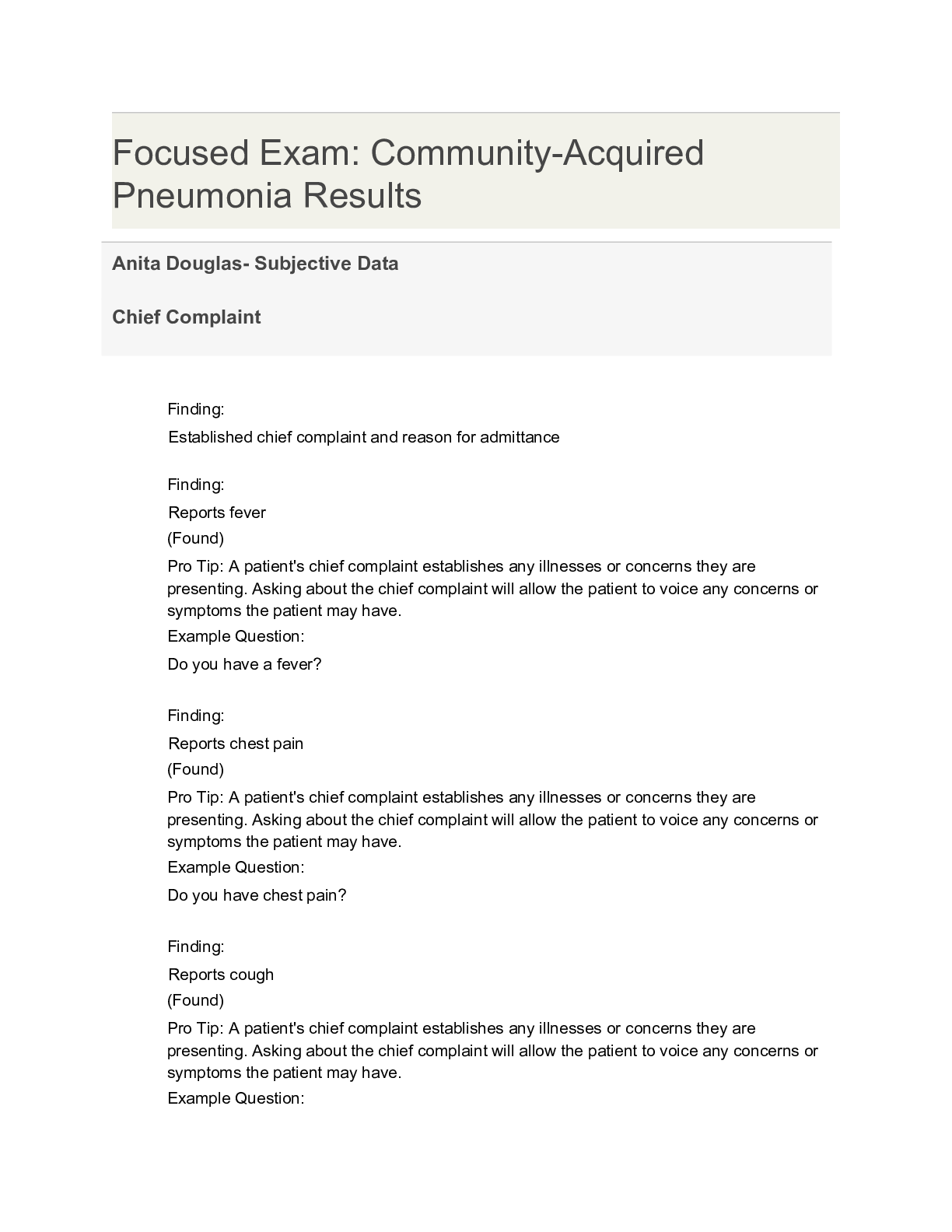
.png)
 Transcript.png)