*NURSING > SHADOW HEALTH > NR 509 Abdominal Pain Documentation Shadow Health (All)
NR 509 Abdominal Pain Documentation Shadow Health
Document Content and Description Below
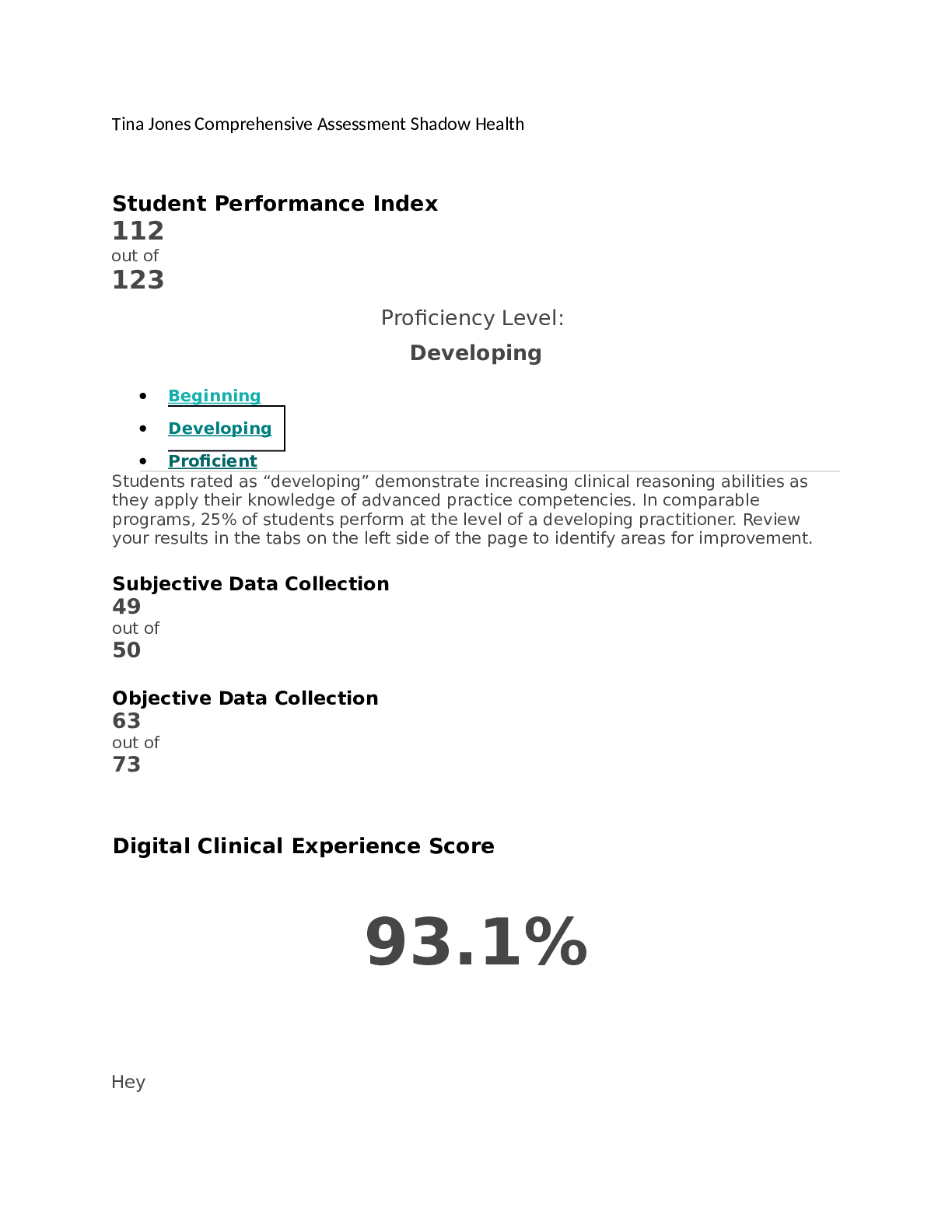
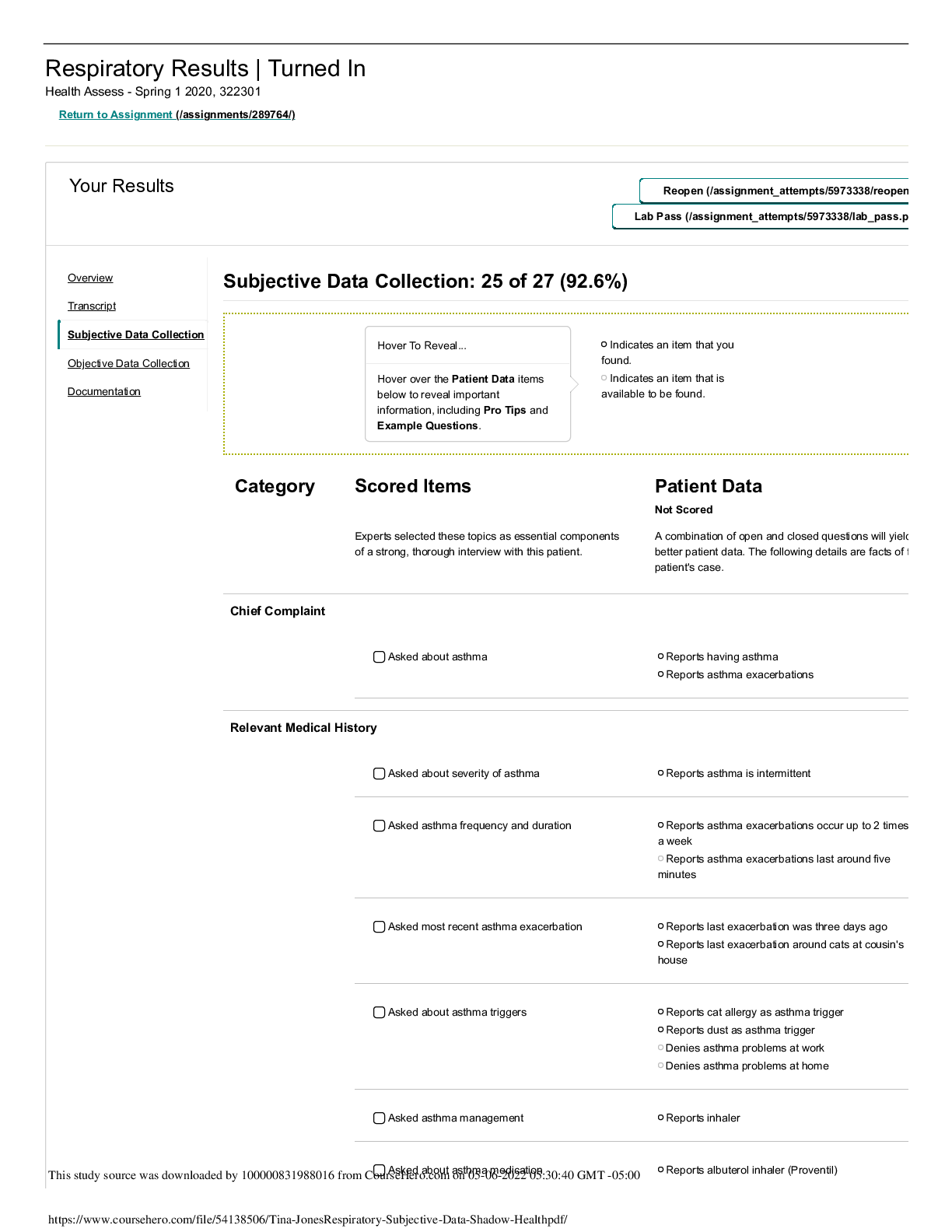
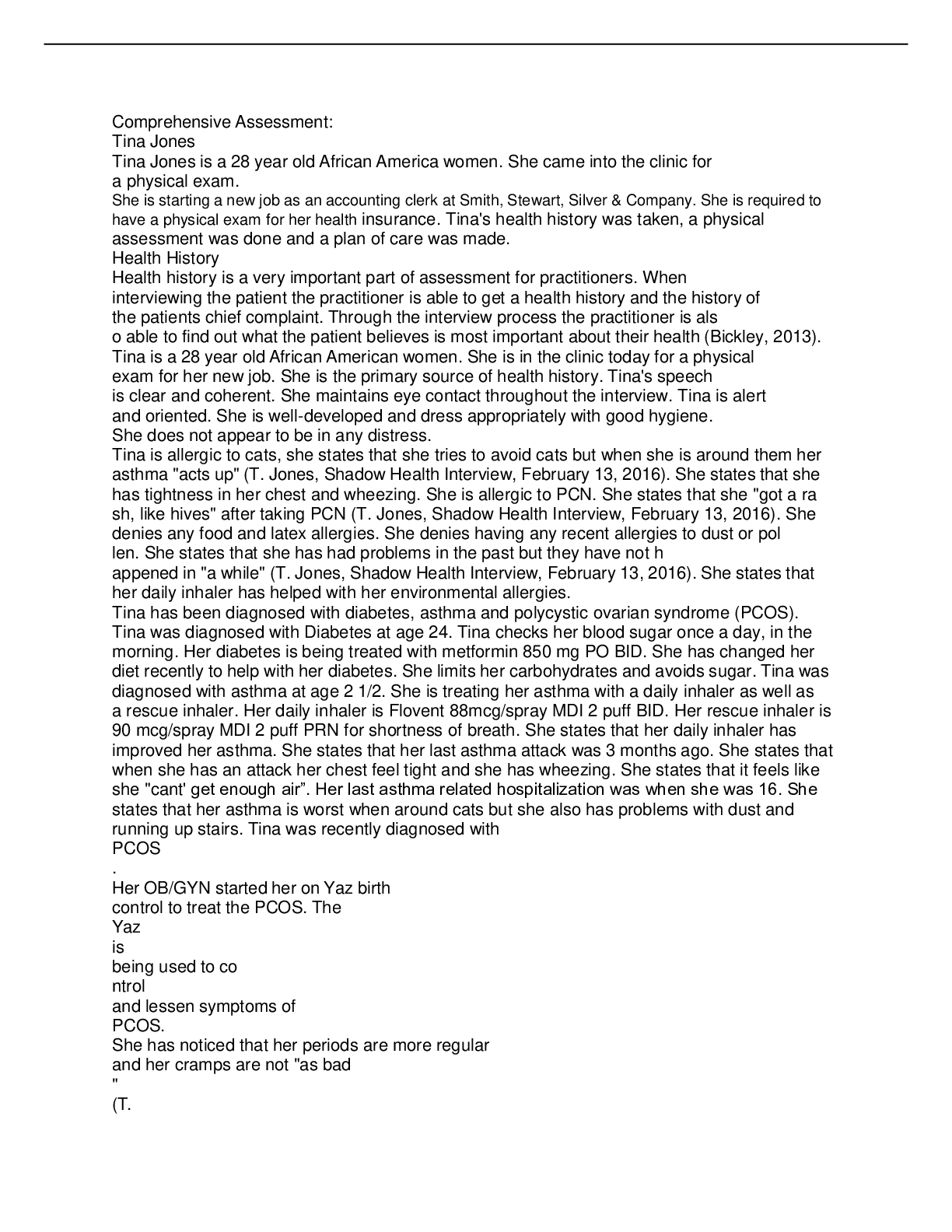
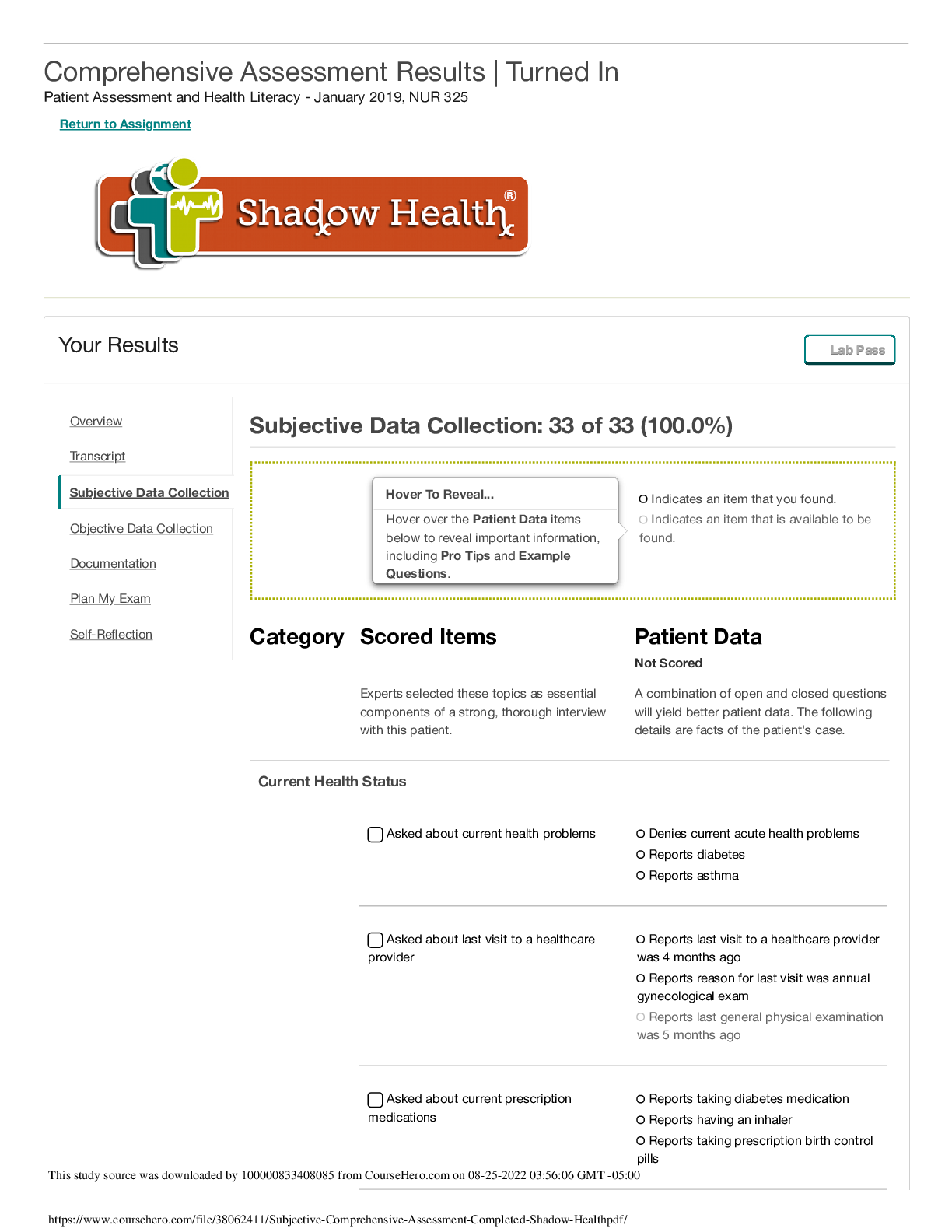
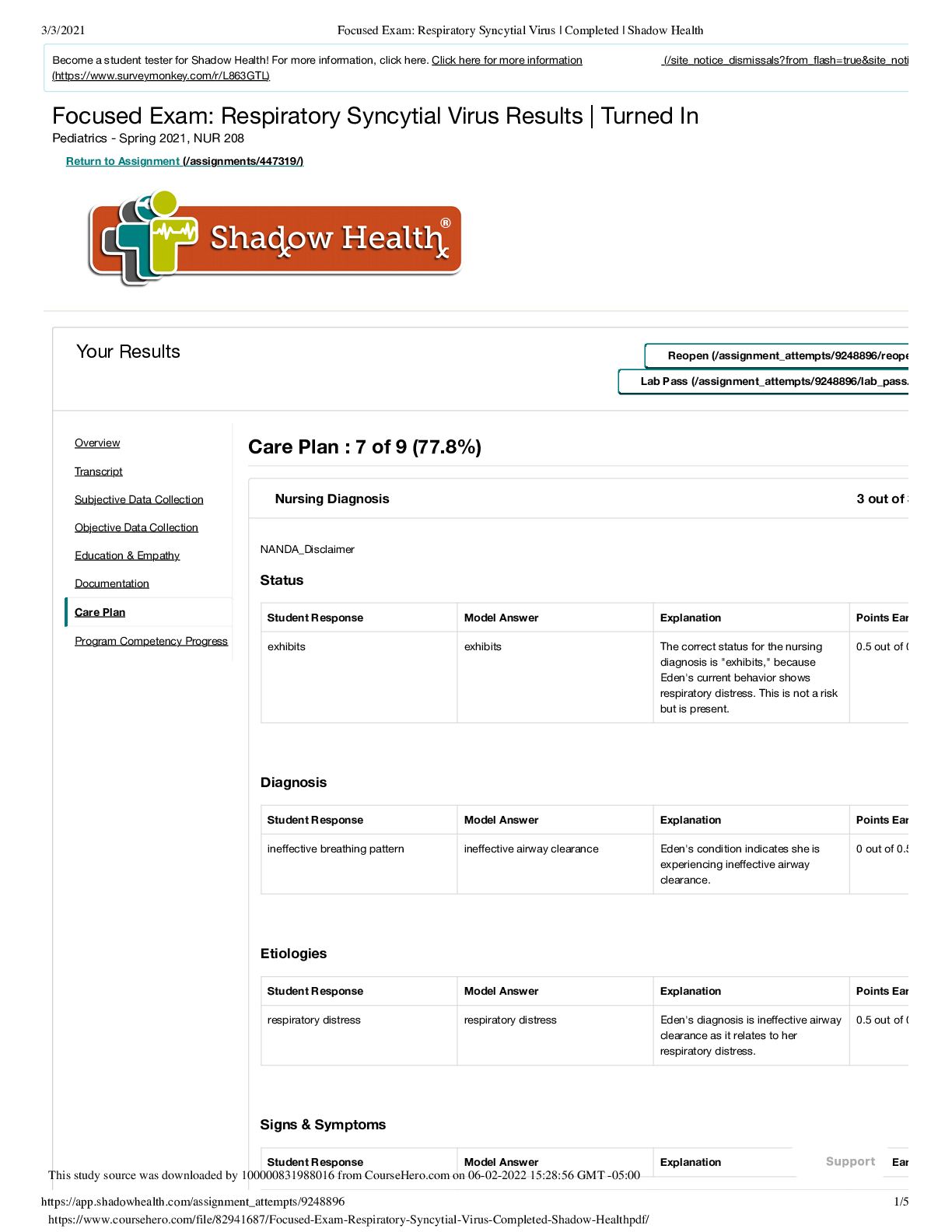
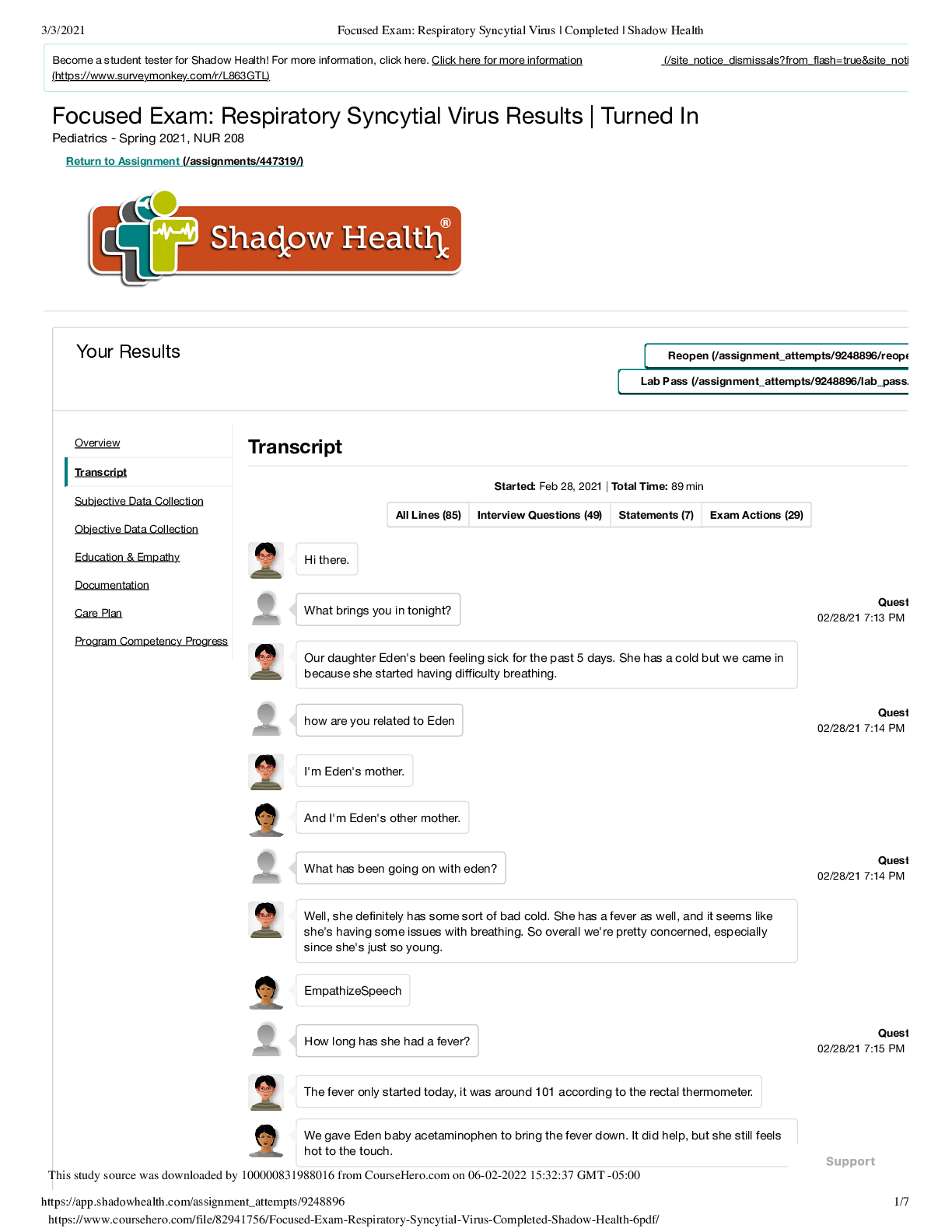
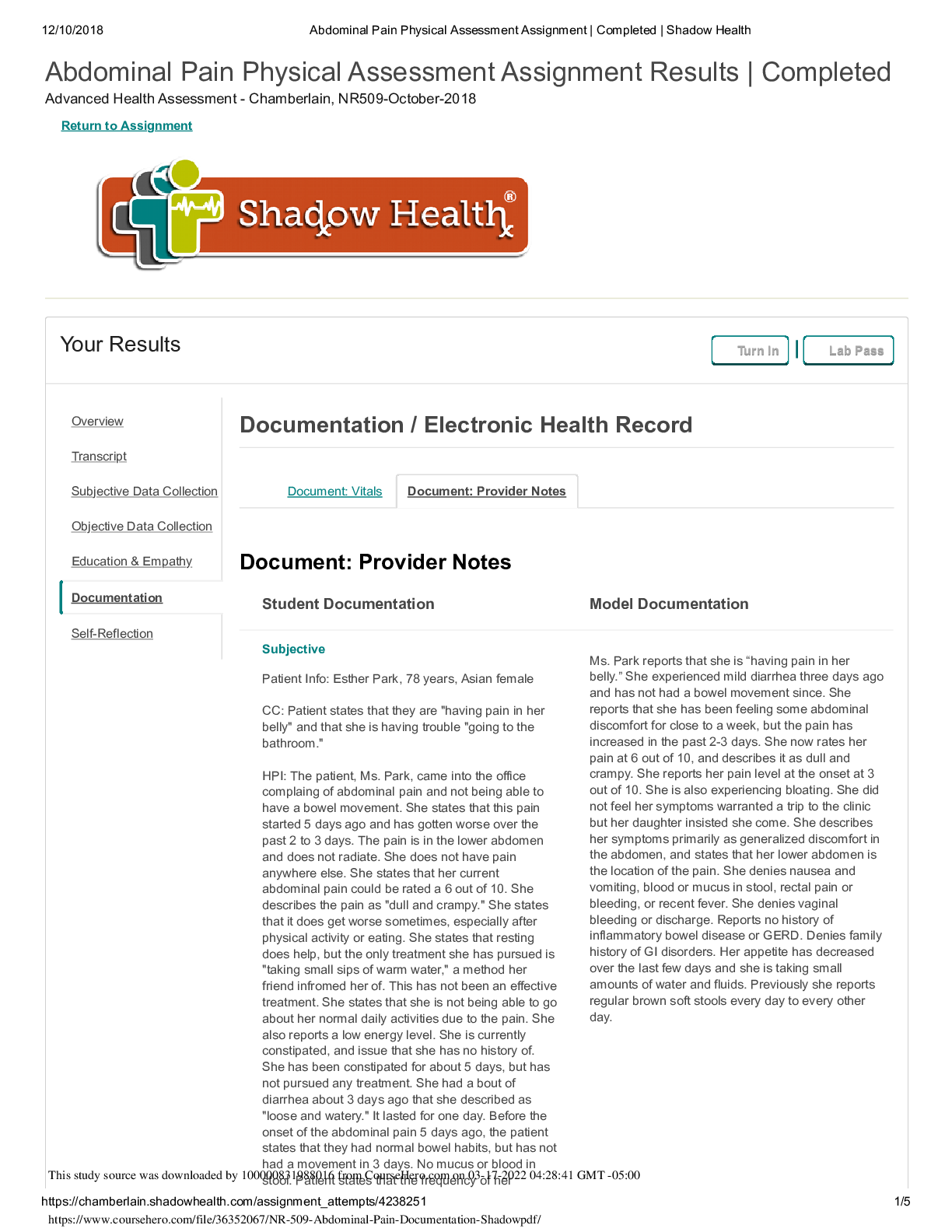
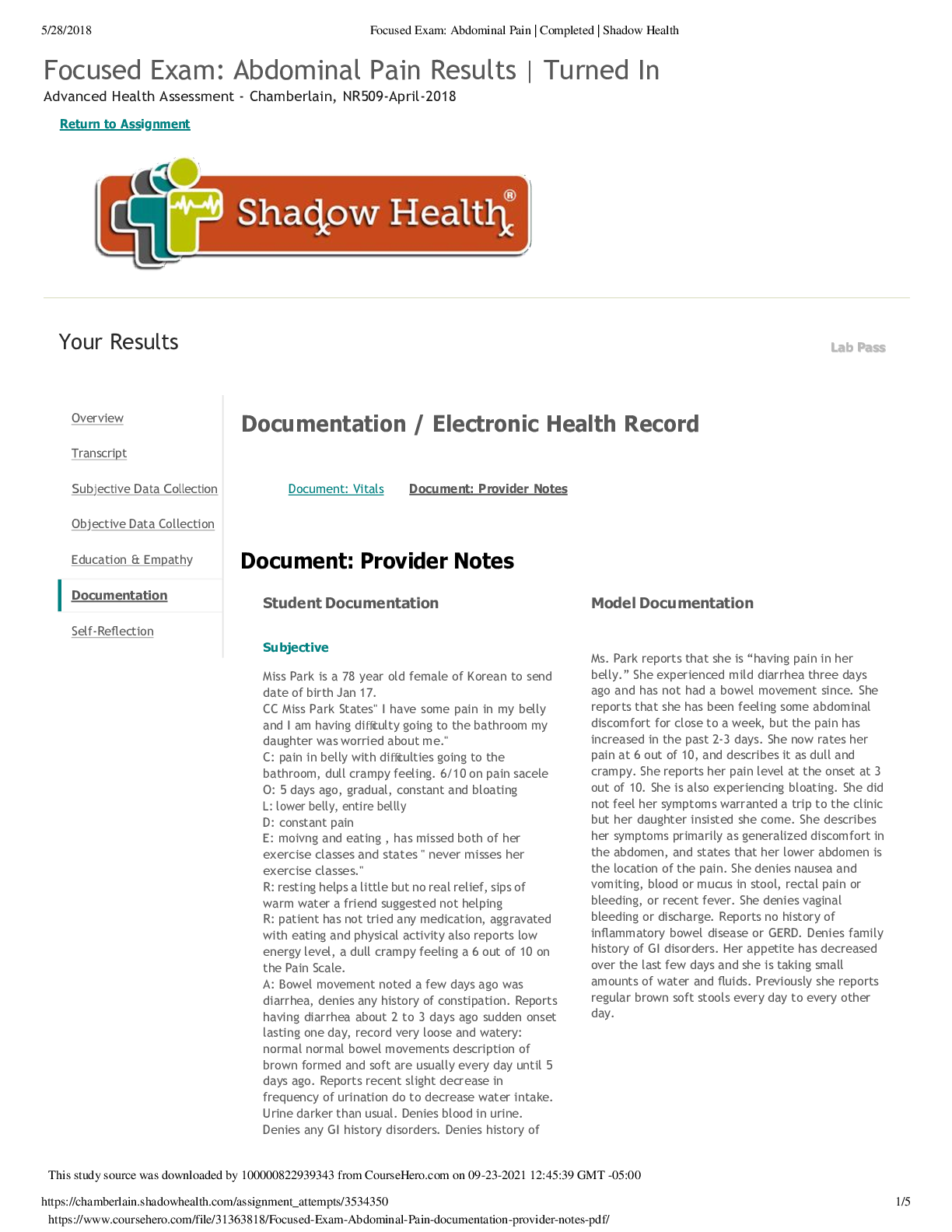
Abdominal Pain Physical Assessment Assignment Results | Completed Advanced Health Assessment - Chamberlain, NR509-October-2018 Return to Assignment Your Results Turn In Lab Pass ... Documentation / Electronic Health Record Document: Vitals Document: Provider Notes Document: Provider Notes Student Documentation Model Documentation Subjective Patient Info: Esther Park, 78 years, Asian female CC: Patient states that they are "having pain in her belly" and that she is having trouble "going to the bathroom." HPI: The patient, Ms. Park, came into the office complaing of abdominal pain and not being able to have a bowel movement. She states that this pain started 5 days ago and has gotten worse over the past 2 to 3 days. The pain is in the lower abdomen and does not radiate. She does not have pain anywhere else. She states that her current abdominal pain could be rated a 6 out of 10. She describes the pain as "dull and crampy." She states that it does get worse sometimes, especially after physical activity or eating. She states that resting does help, but the only treatment she has pursued is "taking small sips of warm water," a method her friend infromed her of. This has not been an effective treatment. She states that she is not being able to go about her normal daily activities due to the pain. She also reports a low energy level. She is currently constipated, and issue that she has no history of. She has been constipated for about 5 days, but has not pursued any treatment. She had a bout of diarrhea about 3 days ago that she described as "loose and watery." It lasted for one day. Before the onset of the abdominal pain 5 days ago, the patient states that they had normal bowel habits, but has not had a movement in 3 days. No mucus or blood in Ms. Park reports that she is “having pain in her belly.” She experienced mild diarrhea three days ago and has not had a bowel movement since. She reports that she has been feeling some abdominal discomfort for close to a week, but the pain has increased in the past 2-3 days. She now rates her pain at 6 out of 10, and describes it as dull and crampy. She reports her pain level at the onset at 3 out of 10. She is also experiencing bloating. She did not feel her symptoms warranted a trip to the clinic but her daughter insisted she come. She describes her symptoms primarily as generalized discomfort in the abdomen, and states that her lower abdomen is the location of the pain. She denies nausea and vomiting, blood or mucus in stool, rectal pain or bleeding, or recent fever. She denies vaginal bleeding or discharge. Reports no history of inflammatory bowel disease or GERD. Denies family history of GI disorders. Her appetite has decreased over the last few days and she is taking small amounts of water and fluids. Previously she reports regular brown soft stools every day to every other day. This study source was downloaded by 1000s0to08o3l.1P98a8ti0e1n6t fsrtoamteCs othurastetHheerofr.ceoqmueonnc1y0o-1f 0h-e20r 21 06:32:36 GMT -05:00 urination has had a small decrease, as well as a darker yellow color. There is no blood in her urine. Current Meds: Patient takes Accupril 10mg daily for hypertension. She does not take any over the counter medication. Allergies: Patient has a latex allergy. No food, medication, or environmental allergies noted. Past Medical: Patient does have hypertension. Patient has no history of gastro issues, heartburns, or ulcers. She has not had appendicitis. She did have Cholecystectomy at 42 and a caesarean section at 40. No other major medical issues or hospitilizations. Patient is up to date on vaccines except for her seasonal flu shot. Social History: Patient eats a failry healthy diet and no fiber supplements. She drinks around 6 glasses of water a day and has no changes in thirst level. She does not drink caffeinated beverages. Patient denies any smoking or illicet drug use. She usually has around 4 drinks per month, usually white wine. She seems her doctor regularly and states that she is in good health for her age. Last colonoscopy was 10 years ago. She is generally physically active, but not recently due to the abdominal pain. She attends fitness class, gardens, and considers herself independent. She has had three pregnancies. She has a strong support system as she lives with her daughter. She is a widow. Her husband of 50 years passed away 6 years ago. She currently dates a man named Max who she is sexually active with. No vaginal intercourse, though, just oral sex. Family History: Mother: passed away at age 88 from strok. Had hypertension and Type II diabetes. Father: Passed away at age 82 and she had hypertension and high cholesterol. Maternal grandparents: history of coronary artery disease and Type II diabetes. Paternal grandparents: History of obesity, hypertension, and CVAs. Siblings: 80 year old brother with hypertension, high cholesterol, and prostate cancer. 81 year old brother with hypertension. Son: 48 and healthy. Daughter: 46 and healthy. ROS: General: Patient denies any fever or chills. She notes feeling exhausted lately. Gastro: Patient notes some bloating, increased gas, loss of appetite. She denies any nausea or vomiting. She denies any changes in weight. Genitourinary: Patient denies any pain while urinating, no incontinence, no history of UTIs, no history of gyno issues, no vaginal bleeding or abnormal discharge. Started menopause at 45. No bladder or kidney issues. Student Documentation Model Documentation Respiratory: Patient denies any coughing or sore throat. Denies any difficulty breathing or chest pain. Objective Ms. Park seemed to be in distress and pain, but she was alert and answered questions fully. She seemed to be in good hygiene and was pleasant. HEENT: Skull and facial features were symmetric. Patient's face was flushed. Nose and mouth muscus membranes were pink and moist. Normal turgor of skin with no tenting. RESPIRATORY: Breath sounds were present and clear in all areas, with no adventituous sounds. Breathing did not seem labored and she was speaking well. CARDIO: No lower extremity edema. S1 and S2 heart sounds audible, with no extra sounds. No S3 or S4 rubs. ABDOMINAL: Abdomen was symmetrical and flat. Some scarring is evident from past cholecystectomy (RUQ) and caesarean section (midline suprapubic area). Abdominal aorta had no bruit. Bowel sounds were normoactive in all quadrants. All arteries had no bruit. No friction rub in liver or spleen. Percussed abdomen found some dull areas and some tympanic areas. Spleen was tympanic. Liver was between 6 and 12 cm. No CVA tenderness. Palpation found tenderness in the lower left quadrant with guarding and distension. Palpable mass was found in lower left quadrant. Aortic width was 3cm or less. Liver palpable. Spleen not palpable. Bladder not palpable. Kidneys not palpable. Rectal exam: No hemorrhoids, no fissures, no ulcers, strong sphincter tone, fecal mass located in fecal vault Pelvic exam: No inflammation or irritation of vulva, no abnotmal discharge, no bleeding, no growths or masses, no tenderness. Urinalysis: Urine was clear and dark yellow, normal odor, No abnormal findings, pH was 6.5, SG was 1.017. • General Survey: Uncomfortable and flushed appearing elderly woman seated on exam table grimacing at times. Appears stable but mildly distressed. • HEENT: Mucus membranes are moist. Normal skin turgor; no tenting. • Cardiovascular: S1, S2, no murmurs, gallops or rubs; no S3, S4 rubs. No lower extremity edema. • Respiratory: Respirations quiet and unlabored, able to speak in full sentences. Breath sounds clear to auscultation. • Abdominal: 6 cm scar in RUQ and 10 cm scar at midline in suprapubic region. An abdominal exam reveals no discoloration; normoactive bowel sounds in all quadrants; no bruits; no friction sounds over spleen or liver; tympany presides with scattered dullness over LLQ; abdomen soft in all quadrants; an oblong mass is noted in the LLQ with mild guarding, distension; no organomegaly; no CVA tenderness; liver span 7 cm @ MCL; no hernias. • Rectal: No hemorrhoids, no fissures or ulceration; strong sphincter tone, fecal mass in rectal vault. • Pelvic: No inflammation or irritation of vulva, abnormal discharge, or bleeding; no masses, growths, or tenderness upon palpation. • Urinalysis: Urine clear, dark yellow, normal odor. No nitrites, WBCs, RBCs, or ketones detected; pH 6.5, SG 1.017. Assessment Lower left quadrant abdominal mass. 1. Constipation: the mass in the LLQ and the fecal matter in the rectal vault point toward constipation. 2. Obstruction: The tenderness that the patient felt, along with the constipation and the episode of diarrhea, could point toward an intestinal obstruction. 3. Diverticulitis: The tenderness and constipation could be signs of diverticulitis, but as the patient is not running a fever or vomiting, I believe that this is less likely. LLQ abdominal mass. Differential diagnoses include constipation, diverticulitis, and intestinal obstruction. Student Documentation Model Documentation Plan Diagnostics: I would like to order a CT scan or an x-ray to identify the mass in the patient's LLQ. I would also like to order a CBC as this can help diagnose diverticulitis if the white blood cell count is elevated. Medication: Depending on the test results, I might prescribe an over the counter nonstimulant laxative like Miralax to help the patient with constipation. Education: I educated the patient on the importance of a fiber rich diet. This included information on foods high in fiber like fruits and vegetables, as well as a suggestion for the use of supplements like Metamucil to keep her regular. I also educated the patient on the importance of remaining hydrated and the effects that dehydration can have on the gastrointstinal system. I asked her to keep track of all the water she drank in a day so that she could remind herself to stay hydrated. Referral: Depending on the test results, like a possible diagnosis of diverticulitis, she might need a referral to a gastrointeroligist for further testing. Follow up: I educated the patient on worsening symptoms that should prompt her to seek mergency care including a fever, vomiting, or if the pain worsens significantly. If nothing changes, I would lik [Show More]
Last updated: 1 year ago
Preview 1 out of 5 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 10, 2021
Number of pages
5
Written in
Additional information
This document has been written for:
Uploaded
Oct 10, 2021
Downloads
0
Views
54

.png)
.png)
.png)
 Transcript.png)

