*NURSING > SOPHIA PATHWAY > NURS C475|Care of the older Adult study guide Objectives (complete) Latest 2022 (All)
NURS C475|Care of the older Adult study guide Objectives (complete) Latest 2022
Document Content and Description Below
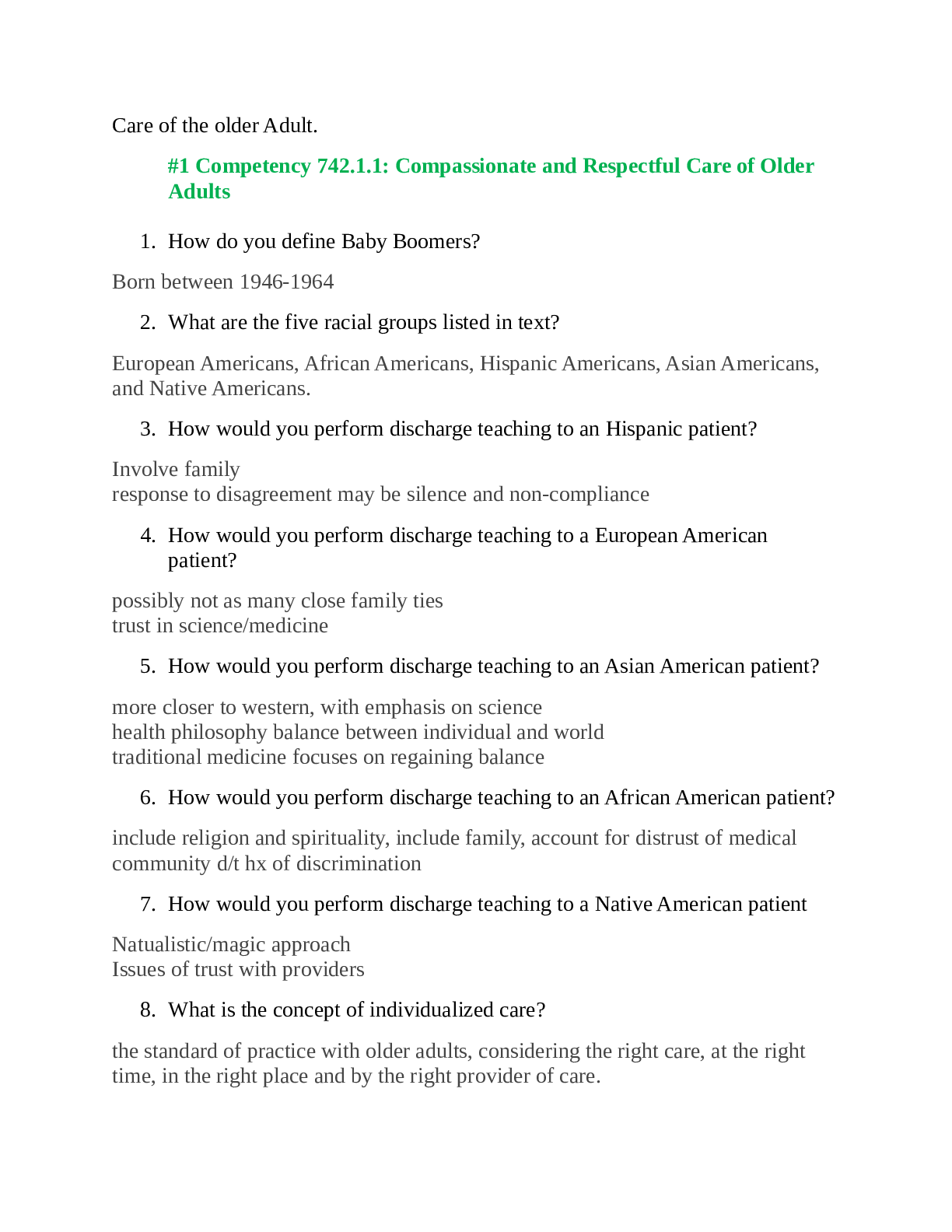
Care of the older Adult. #1 Competency 742.1.1: Compassionate and Respectful Care of Older Adults 1. How do you define Baby Boomers? Born between 1946-1964 2. What are the five racial groups lis... ted in text? European Americans, African Americans, Hispanic Americans, Asian Americans, and Native Americans. 3. How would you perform discharge teaching to an Hispanic patient? Involve family response to disagreement may be silence and non-compliance 4. How would you perform discharge teaching to a European American patient? possibly not as many close family ties trust in science/medicine 5. How would you perform discharge teaching to an Asian American patient? more closer to western, with emphasis on science health philosophy balance between individual and world traditional medicine focuses on regaining balance 6. How would you perform discharge teaching to an African American patient? include religion and spirituality, include family, account for distrust of medical community d/t hx of discrimination 7. How would you perform discharge teaching to a Native American patient Natualistic/magic approach Issues of trust with providers 8. What is the concept of individualized care? the standard of practice with older adults, considering the right care, at the right time, in the right place and by the right provider of care. 9. What are some visual changes related to aging? lens changes in color (more yellow), more opaque, denser, thinner and less flexible • pupil/iris- does not dilate as fully (more difficult to see in lower light) or contract as quickly (prob. sudden illumination 10. What are some communication accommodations that can be made for visual deficits? Position objects within visual field • verbal indications of actions about to impart • Large print type • avoiding dim-illumination or glare 11. What are some hearing changes related to aging? decreased sensitivity to pitch, with high-pitched consonants lost first (t, p, k, f, s, and ch) • Conductive problems - reduction of sound transmission - wave blocked from outer to inner. • Sesorinueral - sound wave transmission interrupted from inner ear to auditory cortex (possible damage to choclea and/or auditory nerve). 12. What is presbycusis? Old man's hearing - Presbycusis occurs following loss of hair and supporting cells and nerve fibers in the cochlea. 13. What are some communication accommodations that can be made for hearing deficits? Don't shout • Make use of unimpaired senses • Stand in front of pt in well-lit room • Limit background noise • short sentences, speak clearly • writing, pictograms, other modes 14. What are some speech/language changes associated with aging? ↓respirations strength, deeper voice and shaky/breathy • ↓saliva, teeth, elasticity and muscle tone may change articulation • cognitive changes may result in fewer words and making more semantic errors 15. What are some communication accommodations that can be made for speech/language deficits? environment low in distractions • close proximity (maintaining eye-contact) • rephrasing to check for comprehension 16. What are some somatosensory changes associated with aging? there is a reduction in tactile and vibration sensations as well as decreased sensitivity to warm or cold stimuli as we age , more prevalent in fingertips than other areas 17. What are some communication accommodations that can be made for somatosensory deficits? When engaging in physical activity with older adults, it is important to use verbal explanations to describe the physical activities as they take place. 18. What is an AAC? Augmentative and alternative communication (AAC): An integrated group of components or assistive devices and strategies that help individuals improve communication. 19. What are some communication tips for someone with dysarthria? Encourage the person to speak slowly and use simple sentences or single words. Allow time for the patient to respond. Don't try to complete their words or sentences. If there is no speech (aphasia, presence of an artificial airway, postoperatively after oral surgery): • Assess the individual's yes/no reliability. • Establish a system for yes/no communication (picture board or eye blink—1 = yes, 2 = no). Post rules for use at the bedside and in the medical record. • Ask yes/no questions and allow the person time to respond. Confirm response before acting. 20. Describe a BTE Behind the Ear BTEs are about 1 inch long and worn behind the outer ear. A small tube connects with the amplification device behind the ear and delivers amplified sound into the ear canal. The device has an adjustable volume control and is battery powered. It is the most common style of hearing aid. These devices are suitable for the entire range of hearing loss. 21. Describe an OTE Over the ear This is a new style that is very small and sits on top of the outer ear. 22. Describe an ITE In the ear ITEs are custom-fitted devices molded to the contour of the outer ear. The device has an adjustable volume control and a battery; however, both are much smaller than ones used in a BTE device. Some users have difficulty seeing or manipulating the control and battery. These devices are used for mild to moderate hearing loss. 23. Describe an ITC In the Canal ITCs are tiny devices that fit into the ear canal and are barely visible. They are customized to fit the size and shape of the ear canal. Although cosmetically appealing, their small size is a drawback for some individuals. 24. Describe a CIC Completely in the Canal CICs are the smallest type of device in the in the ear class. The entire device fits within the canal. Although cosmetically flattering, the small size is a true disadvantage because of difficulty handling and positioning the device. This device is the most expensive model of hearing aid. 25. What patients could benefit from an AAC? individuals with speech impairments 26. What are Satir's five principles of contact and communication? •invite • arrange environment • maximize communication • maximize understanding • follow through. #2 Competency 742.1.2: Health Promotion/Maintenance and Living Environments of Older Adults 1. What are the five A's to tobacco cessation? • Ask • Advise • Assess • Assist • Arrange 2. What are the Five R's to tobacco cessation? • Relevance • Risks • Rewards • Roadblocks • Repetition 3. What is the criterion for the pneumococcal vaccine? >65yo 4. What 5 areas do Healthy People 2010 and the USPSTF suggest that nurses focus on to promote health & prevent disability in the older adult? • Physical activity • Nutrition • Tobacco use • Safety • Immunization 5. Describe the difference between ADLs and IADLs (instrumental activities of daily living) • Activities of daily living (ADLs) are basic tasks that one needs to perform in order to survive • Instrumental activities of daily living (IADLs) are more complex tasks that include handling finances, preparing meals, or managing one's medications. 6. Review the USPSTF Screening Recommendations for Older Adults, Table 12-1 on page 376 in text. https://online.vitalsource.com/#/books/9781449679361/content/id/ch12table. 7. Review the I HATE FALLING risk assessment tool, Box 12-4 on page 361. What can the nurse recommend to reduce risk of falling? #3 Competency 742.1.3: Health Needs of Older Adults 1. What are the 5 most common geriatric syndromes? •pressure ulcers • incontinence • falls • functional decline • delirium, including hypokinetic delirium 2. What aspects of pharmacokinetics are affected by age-related changes? • Absorption • Distribution • Metabolism • Excretion • Pharmacodynamics 3. How is absorption of medications affected by age related changes? What is the significance? No significant changes in gastric pH; decreased absorptive surface and splanchnic blood flow Little significance; possibly delayed onset of action and peak effect of medications 4. How is distribution of medications affected by age related changes? What is the significance? • increased body fat (prolonged half-life of lipid soluble meds - benzodiazepines, phenytoin, phenothiazines) • decreased water compartment (Higher levels of water-soluble drugs (e.g., digoxin and theophylline), increasing risk for toxicity) • Decreased lean body mass (misread of creatinine levels leading to overestimate of kidney function) • Decreased serum albumin (Risk for toxicity of ****************Continued................................******************* [Show More]
Last updated: 1 year ago
Preview 1 out of 77 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 22, 2020
Number of pages
77
Written in
Additional information
This document has been written for:
Uploaded
Oct 22, 2020
Downloads
1
Views
102

.png)