*NURSING > NCLEX-RN > C H A P T E R 6: Ethical and Legal Issues: From Saunders Comprehensive Review for the NCLEX-RN Exami (All)
C H A P T E R 6: Ethical and Legal Issues: From Saunders Comprehensive Review for the NCLEX-RN Examination 8th Edition. (Available: https://bit.ly/2HeJuMt ). Contains Practice questions and Answers with the Rationale, Test-Taking Strategy, Level of Cognitive Ability, Client Needs, Integrated Process, Content Area, Health Problem, Priority Concepts and Reference.
Document Content and Description Below
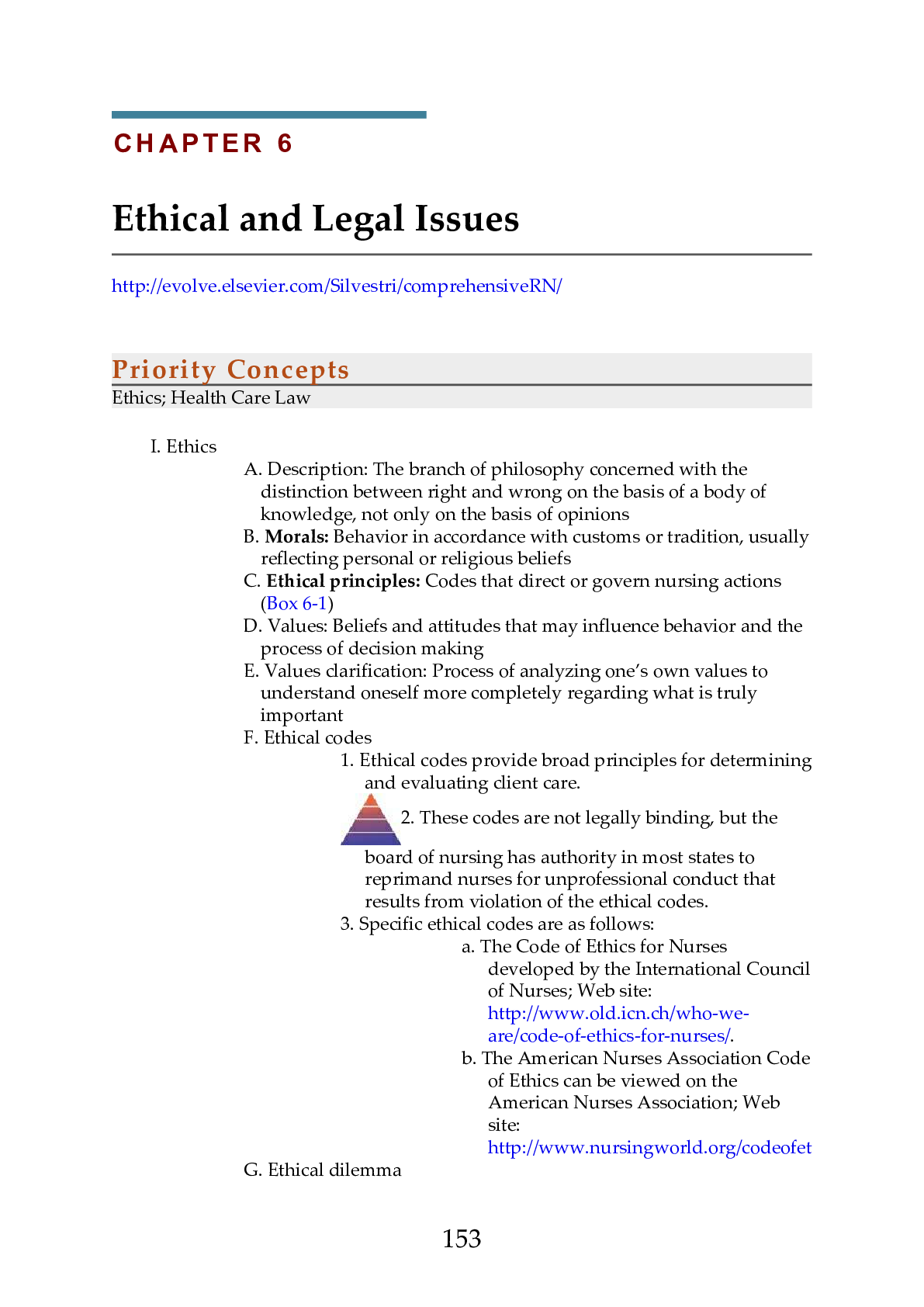
Priority Concepts Ethics; Health Care Law I. Ethics A. Description: The branch of philosophy concerned with the distinction between right and wrong on the basis of a body of knowledge, not only o... n the basis of opinions B. Morals: Behavior in accordance with customs or tradition, usually reflecting personal or religious beliefs C. Ethical principles: Codes that direct or govern nursing actions (Box 6-1) D. Values: Beliefs and attitudes that may influence behavior and the process of decision making E. Values clarification: Process of analyzing one’s own values to understand oneself more completely regarding what is truly important F. Ethical codes 1. Ethical codes provide broad principles for determining and evaluating client care. 2. These codes are not legally binding, but the board of nursing has authority in most states to reprimand nurses for unprofessional conduct that results from violation of the ethical codes. 3. Specific ethical codes are as follows: a. The Code of Ethics for Nurses developed by the International Council of Nurses; Web site: http://www.old.icn.ch/who-weare/code-of-ethics-for-nurses/. b. The American Nurses Association Code of Ethics can be viewed on the American Nurses Association; Web site: http://www.nursingworld.org/codeofethics G. Ethical dilemma 1531. An ethical dilemma occurs when there is a conflict between two or more ethical principles. 2. No correct decision exists, and the nurse must make a choice between two alternatives that are equally unsatisfactory. 3. Such dilemmas may occur as a result of differences in cultural or religious beliefs. 4. Ethical reasoning is the process of thinking through what one should do in an orderly and systematic manner to provide justification for actions based on principles; the nurse should gather all information to determine whether an ethical dilemma exists, examine his or her own values, verbalize the problem, consider possible courses of action, negotiate the outcome, and evaluate the action taken. H. Advocate 1. An advocate is a person who speaks up for or acts on the behalf of the client, protects the client’s right to make his or her own decisions, and upholds the principle of fidelity. 2. An advocate represents the client’s viewpoint to others. 3. An advocate avoids letting personal values influence advocacy for the client and supports the client’s decision, even when it conflicts with the advocate’s own preferences or choices. I. Ethics committees 1. Ethics committees take an interprofessional approach to facilitate dialogue regarding ethical dilemmas. 2. These committees develop and establish policies and procedures to facilitate the prevention and resolution of dilemmas. An important nursing responsibility is to act as a client advocate and protect the client’s rights. II. Regulation of Nursing Practice A. Nurse Practice Act 1. A nurse practice act is a series of statutes that have been enacted by each state legislature to regulate the practice of nursing in that state. 2. Nurse practice acts set educational requirements for the nurse, distinguish between nursing practice and medical practice, and define the scope of nursing practice. 1543. Additional issues covered by nurse practice acts include licensure requirements for protection of the public, grounds for disciplinary action, rights of the nurse licensee if a disciplinary action is taken, and related topics. 4. All nurses are responsible for knowing the provisions of the act of the state or province in which they work. B. Standards of care 1. Standards of care are guidelines that identify what the client can expect to receive in terms of nursing care. 2. The guidelines determine whether nurses have performed duties in an appropriate manner. 3. If the nurse does not perform duties within accepted standards of care, the nurse may be in jeopardy of legal action. 4. If the nurse is named as a defendant in a malpractice lawsuit and proceedings show that the nurse followed neither the accepted standards of care outlined by the state or province nurse practice act nor the policies of the employing institution, the nurse’s legal liability is clear; he or she is liable. C. Employee guidelines 1. Respondeat superior: The employer is held liable for any negligent acts of an employee if the alleged negligent act occurred during the employment relationship and was within the scope of the employee’s responsibilities. 2. Contracts a. Nurses are responsible for carrying out the terms of a contractual agreement with the employing agency and the client. b. The nurse–employee relationship is governed by established employee handbooks and client care policies and procedures that create obligations, rights, and duties between those parties. 3. Institutional policies a. Written policies and procedures of the employing institution detail how nurses are to perform their duties. b. Policies and procedures are usually specific and describe the expected behavior on the part of the nurse. c. Although policies are not laws, courts generally rule against nurses 155who violate polic Practice Questions 16. The nurse hears a client calling out for help, hurries down the hallway to the client’s room, and finds the client lying on the floor. The nurse performs an assessment, assists the client back to bed, notifies the primary health care provider, and completes an occurrence report. Which statement should the nurse document on the occurrence report? 1. The client fell out of bed. 2. The client climbed over the side rails. 3. The client was found lying on the floor. 4. The client became restless and tried to get out of bed. 17. A client is brought to the emergency department by emergency medical services (EMS) after being hit by a car. The name of the client is unknown, and the client has sustained a severe head injury and multiple fractures and is unconscious. An emergency craniotomy is required. Regarding informed consent for the surgical procedure, which is the best action? 1. Obtain a court order for the surgical procedure. 2. Ask the EMS team to sign the informed consent. 3. Transport the victim to the operating room for surgery. 4. Call the police to identify the client and locate the family. 18. The nurse has just assisted a client back to bed after a fall. The nurse and primary health care provider have assessed the client and have determined that the client is not injured. After completing the occurrence report, the nurse should implement which action next? 1. Reassess the client. 2. Conduct a staff meeting to describe the fall. 3. Contact the nursing supervisor to update information regarding the fall. 4. Document in the nurse’s notes that an occurrence report was completed. 19. The nurse arrives at work and is told to report (float) to the intensive care unit (ICU) for the day because the ICU is understaffed and needs additional nurses to care for the clients. The nurse has never worked in the ICU. The nurse should take which best action? 1. Refuse to float to the ICU based on lack of unit orientation. 2. Clarify the ICU client assignment with the team leader to ensure that it is a safe assignment. 3. Ask the nursing supervisor to review the hospital policy on floating. 4. Submit a written protest to nursing administration, and then call the hospital lawyer. 20. The nurse who works on the night shift enters the medication room and finds a coworker with a tourniquet wrapped around the upper arm. The coworker is about to insert a needle, attached to a syringe containing a clear liquid, into the antecubital area. Which is the most appropriate action by the nurse? 1. Call security. 2. Call the police. 1793. Call the nursing supervisor. 4. Lock the coworker in the medication room until help is obtained. 21. A hospitalized client tells the nurse that an instructional directive is being prepared and that the lawyer will be bringing the document to the hospital today for witness signatures. The client asks the nurse for assistance in obtaining a witness to the will. Which is the most appropriate response to the client? 1. “I will sign as a witness to your signature.” 2. “You will need to find a witness on your own.” 3. “Whoever is available at the time will sign as a witness for you.” 4. “I will call the nursing supervisor to seek assistance regarding your request.” 22. The nurse has made an error in documentation of the dose administered of an opioid pain medication in the client’s record. The nurse draws 1 mg from the vial and another registered nurse (RN) witnesses wasting of the remaining 1 mg. When scanning the medication, the nurse entered into the medication administration record (MAR) that 2 mg of hydromorphone was administered instead of the actual dose administered, which was 1 mg. The nurse should take which action(s) to correct the error in the MAR? Select all that apply. 1. Complete and file an occurrence report. 2. Right-click on the entry and modify it to reflect the correct information. 3. Document the correct information and end with the nurse’s signature and title. 4. Obtain a cosignature from the RN who witnessed the waste of the remaining 1 mg. 5. Document in a nurse’s note in the client’s record detailing the corrected information. 23. Which identifies accurate nursing documentation notation(s)? Select all that apply. 1. The client slept through the night. 2. Abdominal wound dressing is dry and intact without drainage. 3. The client seemed angry when awakened for vital sign measurement. 4. The client appears to become anxious when it is time for respiratory treatments. 5. The client’s left lower medial leg wound is 3 cm in length without redness, drainage, or edema. 24. A nursing instructor delivers a lecture to nursing students regarding the issue of clients’ rights and asks a nursing student to identify a situation that 180represents an example of invasion of client privacy. Which situation, if identified by the student, indicates an understanding of a violation of this client right? 1. Performing a procedure without consent 2. Threatening to give a client a medication 3. Telling the client that he or she cannot leave the hospital 4. Observing care provided to the client without the client’s permission 25. Nursing staff members are sitting in the lounge taking their morning break. An assistive personnel (AP) tells the group that she thinks that the unit secretary has acquired immunodeficiency syndrome (AIDS) and proceeds to tell the nursing staff that the secretary probably contracted the disease from her husband, who is supposedly a drug addict. The registered nurse should inform the AP that making this accusation has violated which legal tort? 1. Libel 2. Slander 3. Assault 4. Negligence 26. An older woman is brought to the emergency department for treatment of a fractured arm. On physical assessment, the nurse notes old and new ecchymotic areas on the client’s chest and legs and asks the client how the bruises were sustained. The client, although reluctant, tells the nurse in confidence that her son frequently hits her if supper is not prepared on time when he arrives home from work. Which is the most appropriate nursing response? 1. “Oh, really? I will discuss this situation with your son.” 2. “Let’s talk about the ways you can manage your time to prevent this from happening.” 3. “Do you have any friends who can help you out until you resolve these important issues with your son?” 4. “As a nurse, I am legally bound to report abuse. I will stay with you while you give the report and help find a safe place for you to stay.” 27. The nurse calls the primary health care provider (PHCP) regarding a new medication prescription, because the dosage prescribed is higher than the recommended dosage. The nurse is unable to locate the PHCP, and the medication is due to be administered. Which action should the nurse take? 1. Contact the nursing supervisor. 2. Administer the dose prescribed. 3. Hold the medication until the PHCP can be contacted. 4. Administer the recommended dose until the PHCP can be located. 28. The nurse employed in a hospital is waiting to receive a report from the laboratory via the facsimile (fax) machine. The fax machine activates and the nurse expects the report, but instead receives a sexually oriented photograph. Which is the most appropriate initial nursing action? 1. Call the police. 2. Cut up the photograph and throw it away. 3. Call the nursing supervisor and report the occurrence. 1814. Call the laboratory and ask for the name of the individual who sent the photograph. [Show More]
Last updated: 1 year ago
Preview 1 out of 35 pages
Reviews( 0 )
Document information
Connected school, study & course
About the document
Uploaded On
Oct 22, 2020
Number of pages
35
Written in
Additional information
This document has been written for:
Uploaded
Oct 22, 2020
Downloads
0
Views
56